Abstract
Objective:
Understanding suicide risk is a priority for the U.S. military. We aimed to estimate associations of childhood maltreatment with pre-enlistment suicidal behaviors in new Army soldiers.
Method:
Cross-sectional survey data from 38,237 soldiers reporting for basic training from April 2011 through November 2012 were analyzed. Scales assessing retrospectively-reported childhood abuse and neglect were derived and subjected to latent class analysis, which yielded 5 profiles: No Maltreatment, Episodic Emotional Maltreatment, Frequent Emotional/Physical Maltreatment, Episodic Emotional/Sexual Abuse, and Frequent Emotional/Physical/Sexual Maltreatment. Discrete-time survival analysis was used to estimate associations of maltreatment profiles with suicidal behaviors (assessed with a modified Columbia Suicidal Severity Rating Scale), adjusting for socio-demographics and mental disorders.
Results:
Nearly 1 in 5 new soldiers was classified as experiencing childhood maltreatment. Relative to no maltreatment, all multivariate maltreatment profiles were associated (ps < .001) with elevated odds of lifetime suicidal ideation [AORs = 3.10–4.93], plan [AORs = 3.75–10.77], attempt [AORs = 3.60–15.95], and onset of plan among those with ideation [AORs = 1.40–3.10]. Several profiles also predicted attempts among those with plans [AORs = 2.01–2.47], and Frequent Emotional/Physical/Sexual Maltreatment predicted unplanned attempts among ideators [AOR = 5.32]. Adjustment for mental disorders attenuated but did not eliminate these associations.
Conclusions:
Childhood maltreatment is strongly associated with suicidal behavior among new soldiers, even after adjusting for intervening mental disorders. Among soldiers with lifetime ideation, certain maltreatment profiles are associated with elevated odds of subsequently planning and/or attempting suicide. Focus on childhood maltreatment might reveal avenues for risk reduction among new soldiers.
INTRODUCTION
Suicide is a national public health problem, with deaths from suicide now exceeding those from motor vehicle accidents.1 Reduction of suicide deaths is also a priority for the US military.2 Studies investigating risk for suicide and non-fatal suicidal behaviors among servicemembers have begun to elucidate contributions of diverse factors including mental disorders3–6, deployment2,7–9, and sexual trauma10,11.
Understanding suicide among military personnel also requires improved characterization of risk that is present upon enlistment, before exposure to military-specific stressors. Certain early-life traumas, notably those involving childhood maltreatment, are established risk factors for adult suicidal behavior in the general population.12–17 Although this can inform understanding of suicide risk in servicemembers, the unique nature of the military experience mandates that research also be conducted with military personnel.18
Among active duty soldiers, prevalence of childhood trauma has been reported as 43% among suicide decedents and 65% among non-lethal suicide attempters.19 However, very few studies of military samples have examined childhood maltreatment as a risk factor for suicidal behavior. A recent study of Canadian servicemembers found that childhood physical abuse, sexual abuse, and exposure to domestic violence were associated with suicidal behaviors.20 However, effects of other forms of maltreatment and contributions of mental disorders were not evaluated. Studies of servicemembers have not investigated whether maltreatment history increases risk for progression from suicidal ideation to plan or attempt; associations that (if present) could have implications for targeted prevention efforts.
We evaluated associations of childhood maltreatment with lifetime suicidal behaviors in over 38,000 soldiers entering the US Army. We considered specific forms of maltreatment, their aggregate, and multivariate maltreatment profiles to better characterize the joint associations of these exposures. Because risk factors for ideation and attempts differ,21 we looked separately at associations of maltreatment with onset of plans and attempts in soldiers with ideation, in order to improve understanding of where – in the progression from thinking about suicide to planning suicide to making an attempt – a history of maltreatment may be implicated. Finally, we evaluated the extent to which mental disorders accounted for relationships of childhood maltreatment with suicidal behavior.
METHOD
Participants and Procedures
The Army STARRS New Soldier Survey (NSS) was administered at three basic training installations from April 2011-November 2012.22,23 Soldiers were surveyed prior to Basic Combat Training, while completing intake procedures. Representative samples of 200–300 soldiers per installation site were selected weekly to attend a study overview and informed consent session. Nearly all (99.9%) selected soldiers consented to the self-administered questionnaire (SAQ) and 93.5% of those who consented completed the full SAQ. Of those SAQ completers, 77.1% consented to linkage of responses to their Army/Department of Defense (DoD) Administrative records. Recruitment, consent, and data protection procedures were approved by the Human Subjects Committees of all collaborating institutions. Other details regarding study design and methodology are provided elsewhere.22,23
The analysis was restricted to respondents whose SAQ data were successfully linked to their Army/DoD Administrative records (n = 38,507), then further constrained to those with age-at-enlistment at or below the 99th percentile (≤ 33 years), yielding a sample of 38,237 soldiers (31,758 males and 6,479 females). Analyses incorporate a combined analysis weight that adjusts for differential administrative record linkage consent among SAQ completers, and includes a post-stratification of these consent weights to known demographics and service traits of the population of soldiers attending Basic Combat Training during the study period.24
Measures
Childhood maltreatment.
Fifteen NSS items assessed childhood abuse and neglect. They were prefaced by, “How often did you have each of the following experiences up through the age of 17?” and described forms of emotional, physical, and sexual maltreatment. All were rated by respondents on a scale from 1 (“never”) to 5 (“very often”). To produce conservative estimates of associations of maltreatment with suicidal behavior, missing responses were imputed as 1. During preliminary factor analysis, it was observed that elimination of one item enhanced discrimination of two factors that aligned with well-established constructs (emotional abuse and physical abuse). Analyses are therefore based on 14 maltreatment items.
Suicidal behavior.
Lifetime suicidal behavior was assessed using a modified self-report baseline version of the Columbia Suicidal Severity Rating Scale,25 which incorporated assessment of ages of onset of suicidal thoughts and behaviors. Ideation was considered present if respondents endorsed ever having thoughts of killing themselves; or wishing they were dead or would go to sleep and never wake up. Plan was considered present if respondents endorsed thinking about methods of ending their lives or developing a plan of how to kill themselves. All respondents who reported ideation (regardless of intent/plan) were asked if they had ever attempted suicide; attempt was considered present if respondents endorsed ever purposefully hurting themselves with at least some intention to die. Lifetime prevalence of ideation, plans, and attempts in NSS was 14.1, 2.3, and 1.9%, respectively.26
Socio-demographic and Army service variables.
All models adjusted for person-year, sex, race-ethnicity, religion, marital status, education (soldier and parental), nativity, service component (Regular Army, National Guard, or Army Reserve), and basic training site.
Mental disorders.
Additional models adjusted for mental disorders with ages of onset prior to the age of onset of the suicidal behavior under consideration. Survey items assessed the symptoms of each mental disorder, and algorithms based on DSM-IV definitions were used to establish whether criteria were met for each diagnosis. Diagnoses were validated against independent structured clinical interviews in the Army STARRS Clinical Reappraisal Study.27 Disorders included lifetime major depressive episode, mania/hypomania, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, intermittent explosive disorder, conduct disorder, oppositional defiant disorder, substance use disorder, and persistent attention deficit-hyperactivity disorder (i.e., symptomatic during past 6 months). The sensitivity models also adjusted for total number of mental disorders with onset prior to the emergence of the suicidal behavior in question.
Other trauma.
Because victims of childhood maltreatment may be at increased risk for subsequent traumatic events28 that may themselves by associated with risk for suicidal behaviors, we derived a global index of other lifetime trauma exposure and adjusted for this in sensitivity models. The 0–12 index was calculated by counting the number of lifetime traumatic events endorsed by respondents. Physical and sexual assault were excluded due to potential overlap with maltreatment. A limitation was that timing of traumatic events was not assessed and events could have occurred after the onset of suicidal behaviors. Thus, this sensitivity analysis was conducted solely to evaluate whether associations of maltreatment with suicidal behaviors could be statistically explained by exposure to non-maltreatment events (e.g., “re-victimization”).
Data analysis
Unless otherwise indicated, analyses were conducted using R, version 3.0.2.29 Scales quantifying frequency of exposure to different maltreatment types were derived by submitting the 14 retained maltreatment items to Parallel Analysis and Exploratory Factor Analysis (EFA) with minimum residual estimation and promax rotation. To characterize co-occurrence of maltreatment types, the scales were used as latent class indicators for a latent profile analysis30,31 performed in Mplus 7.3.32 Competing solutions were compared on model fit and conceptual interpretability of derived classes. Fit statistics under consideration included the log-likelihood, Akaike information criteria, Bayes information criteria (BIC), entropy, and Lo-Mendell-Rubin (LMR) adjusted likelihood ratio test. BIC and LMR were prioritized given evidence they are the most robust measures of model fit.33
Discrete-time survival analysis (using R library survey34), with person-year the unit of analysis and a logistic link function,35 was used to estimate associations of maltreatment with suicidal behaviors. All models presented in this report are based on the full sample, as analyses stratified by gender showed that associations of maltreatment with suicidal ideation, plan, and attempt were evident among both males and females. Reported ages of onset of suicidal behaviors were used to create person-year files for models of lifetime ideation, plan, and attempt; and, for the subset of respondents with lifetime ideation, onset of plan subsequent to ideation, attempt subsequent to plan (“planned attempt”), and attempt without a prior suicide plan (“unplanned attempt”). Childhood maltreatment was assumed to have occurred prior to onset of suicidal behavior. The person-year file was limited to 12–33 years of age due to exceedingly low prevalence of suicidal behavior prior to age 12 and of enlistment after age 33. Survival coefficients were exponentiated to create odds ratios (ORs) with 95% confidence intervals. We estimated population attributable risk proportions (PARPs) for the final model. PARPs represent proportions of cases of suicidal behavior that would be avoided (net of the covariates) if maltreatment had been prevented, assuming a causal relation between maltreatment and suicidal behavior. Because NSS data were clustered and weighted, the design-based Taylor series linearization method was used to estimate standard errors. Multivariate significance was examined using design-based Wald Χ2 tests. Two-tailed p values < .05 were considered significant.
RESULTS
Derivation of childhood maltreatment variables
Parallel analysis of the maltreatment items indicated that 5 factors should be extracted. Inspection of 1- to 6-factor EFA solutions (Supplementary eTable 1) confirmed that a 5-factor model provided good overall fit for the data (RMSEA = .066, 90% CI .065-.068; RMR = .02; TLI = .95). All items loaded on one of the 5 factors and no salient cross-loadings were evident. The pattern matrix was interpretable, with factors corresponding to Sexual Abuse, Physical Abuse, Emotional Abuse, Physical Neglect, and Emotional Neglect (Table 1). Model validity was further supported by good factor determinacies (.88 to .97) and concordance with the factor structure of another well-validated measure.36
Table 1.
Latent structure of 14 survey items assessing childhood abuse and neglect: Results of exploratory factor analysis
| Promax-rotated factor loadings | |||||
|---|---|---|---|---|---|
| Sexual Abuse | Physical Abuse | Emotional Abuse | Physical Neglect | Emotional Neglect | |
| Unwanted sexual touching | .78 | −.05 | .07 | −.01 | .00 |
| Sexually abused at home | .79 | .05 | −.08 | −.02 | .00 |
| Hit so hard it left bruises | −.01 | .87 | .04 | −.03 | .01 |
| Physically abused at home | −.01 | .90 | −.02 | .00 | .00 |
| Family member said hurtful/insulting things | −.01 | .01 | .89 | −.01 | .00 |
| Someone in your family hated you | .02 | .07 | .73 | .01 | −.05 |
| Chores too difficult/dangerous for your age | .00 | .12 | .11 | .43 | .02 |
| Nobody to take care of/protect you | −.03 | −.05 | −.03 | .91 | .00 |
| Nobody concerned about your basic needs | .05 | .00 | −.02 | .68 | −.01 |
| Family member made you feel important | .01 | −.02 | .03 | .02 | .83 |
| Felt loved and cared for | .00 | −.03 | .05 | −.03 | .88 |
| Family member looked out for you | .00 | −.01 | .05 | −.06 | .87 |
| Felt close to family | −.02 | .03 | −.05 | .04 | .91 |
| Family a source of strength/support | .01 | .02 | −.08 | .02 | .88 |
Note. Primary loadings are in bold. The last five items (which loaded on the Emotional Neglect factor) were all reverse-scored. Exploratory factor analysis was conducted with minimum residual estimation and promax rotation.
Scores for maltreatment scales were derived by averaging the ratings for each factor’s constituent items. The Sexual Abuse, Physical Abuse, Emotional Abuse, Physical Neglect, and Emotional Neglect scales had good internal consistency (Cronbach’s α = .73–.94) and were inter-correlated (ρs = .12 to .57; ps < .001). A Global Maltreatment score (Cronbach’s α = .76) was calculated by averaging the Sexual Abuse, Physical Abuse, Emotional Abuse, Physical Neglect, and Emotional Neglect scores. Descriptive statistics appear in Supplementary eTable 2; total scores for all maltreatment scales range from 1 (average per-item response of “never”) to 5 (average response of “very often”).
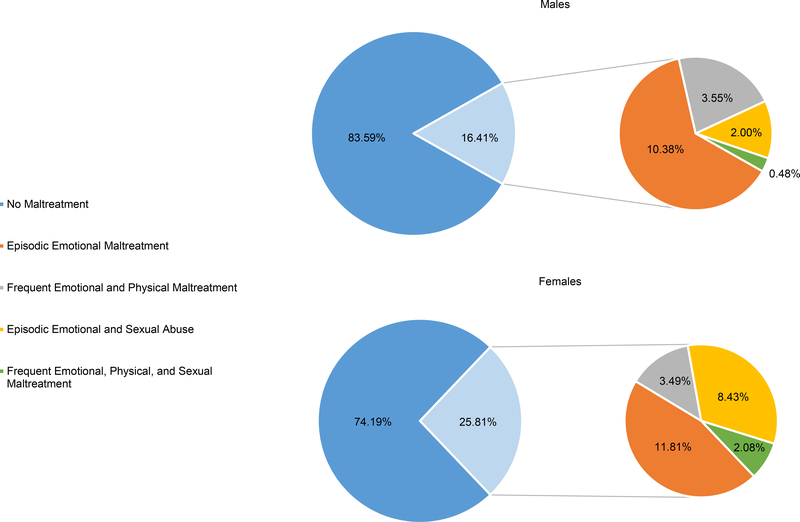
When scores on the Sexual Abuse, Physical Abuse, Emotional Abuse, Physical Neglect, and Emotional Neglect scales were subjected to latent class analyses, 1- through 6-class solutions converged (Supplementary eTable 3). BIC did not reach a minimum. However, the 5-class model was selected because it was interpretable and demonstrated improved fit relative to the 4-class model [BIC = 267,018; entropy = 0.972; LMR p = .0003]. The 6-class model did not evidence better fit than the 5-class model (LMR p = .73). Based on each latent class’s mean scores on the maltreatment subtype scales (Figure 1), we labeled the profiles “No Maltreatment” (81.6% of soldiers), “Episodic Emotional Maltreatment” (10.7%), “Frequent Emotional and Physical Maltreatment” (3.6%), “Episodic Emotional and Sexual Abuse” (3.2%), and “Frequent Emotional, Physical, and Sexual Maltreatment” (0.9%). Maltreatment profile was associated with gender (p < .001); proportions of males and females belonging to each profile are displayed in Figure 2.
Figure 1.
Mean scores on the maltreatment subtype scales for the 5-class solution of a Latent Class Analysis. Scores reflect average per-item rating of the frequency of each type of maltreatment, where 1 = never; 2 = rarely; 3 = sometimes, 4 = often, and 5 = very often. Defining features of each profile are noted in the figure legend.
Figure 2.
Proportions of males (n = 31,758) and females (n = 6,479) classified as members of each latent maltreatment profile.
Associations of global maltreatment and maltreatment types with suicidal behavior
Binary discrete-time survival models (Table 2) showed that higher scores on Global Maltreatment and on each of the 5 subtype scales predicted increased odds of lifetime suicidal ideation, plan, and attempt. Adjusted ORs ranged from 1.46 (95% CI 1.41–1.51; p < .001) for the association between Physical Neglect score and ideation to 2.70 (95% CI 2.49–2.93; p < .001) for the association between Global Maltreatment score and attempt. ORs in Table 2 can be exponentiated to understand risk associated with increasing frequency of maltreatment. For example, adjusted odds of lifetime attempt are 1.77, 3.13 (1.772), 5.54 (1.773), and 9.82 (1.774) for respondents whose respective average ratings of physical abuse items were “rarely,” “sometimes,” “often,” and “very often”.
Table 2:
Bivariate models of associations between childhood maltreatment and lifetime suicidal behaviors
| Total Sample (N = 38237) | Among Lifetime Ideators | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ideation | Plan | Attempt | Plan (n = 5280) | Planned Attempt (n = 807) | Unplanned Attempt (n = 4595) | |||||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Global Maltreatment | 2.24** | 2.14–2.34 | 2.66** | 2.47–2.88 | 2.70** | 2.49–2.93 | 1.52** | 1.39–1.67 | 1.36** | 1.16–1.60 | 1.31* | 1.11–1.55 |
| Sexual Abuse | 1.65** | 1.57–1.73 | 1.91** | 1.75–2.08 | 2.05** | 1.86–2.26 | 1.37** | 1.21–1.55 | 1.26* | 1.06–1.51 | 1.53** | 1.28–1.84 |
| Physical Abuse | 1.51** | 1.46–1.56 | 1.77** | 1.66–1.89 | 1.77** | 1.66–1.89 | 1.31** | 1.23–1.40 | 1.89* | 1.07–1.32 | 1.17* | 1.05–1.29 |
| Emotional Abuse | 1.64** | 1.60–1.67 | 1.80** | 1.72–1.89 | 1.79** | 1.70–1.89 | 1.22** | 1.16–1.29 | 1.16* | 1.05–1.28 | 1.08 | 0.98–1.19 |
| Physical Neglect | 1.46** | 1.41–1.51 | 1.63** | 1.52–1.75 | 1.70** | 1.59–1.83 | 1.20** | 1.11–1.30 | 1.22* | 1.07–1.40 | 1.18* | 1.02–1.37 |
| Emotional Neglect | 1.53** | 1.48–1.57 | 1.69** | 1.59–1.80 | 1.67** | 1.56–1.79 | 1.19** | 1.11–1.27 | 1.14* | 1.01–1.29 | 1.05 | 0.92–1.20 |
Notes. AOR = adjusted odds ratio. CI = confidence interval. Each cell displays the result of a separate bivariate model where the row label denotes the predictor and the column label denotes the outcome variable. All models adjust for age, gender, ethnicity, marital status, religion, soldier and parental education level, nativity, service component, site of Basic Combat Training, and person-year.
p < .05, two-sided test
p <.001, two-sided test.
Analyses among the subgroup of respondents with lifetime ideation (n = 5280) showed that Global Maltreatment and each of the 5 maltreatment subtypes were associated with onset of suicide plan. Similarly, analyses among respondents with lifetime plan (n = 807) showed that Global Maltreatment and each of the 5 maltreatment subtypes were associated with subsequent suicide attempt (“planned attempt”). Adjusted ORs ranged from 1.14 (95% CI 1.01–1.29; p <.05) for the association between Emotional Neglect score and planned attempt to 1.52 (95% CI 1.39–1.67; p < .001) for the association between Global Maltreatment score and plan among ideators. Among ideators without a plan (n = 4595), it was observed that Sexual Abuse, Physical Abuse, Physical Neglect, and Global Maltreatment were associated with increased odds of suicide attempt (“unplanned attempt”). Significant adjusted ORs ranged from 1.17 (95% CI 1.05–1.29; p < .005) for Physical Abuse score to 1.53 (95% CI 1.28–1.84; p < .001) for Sexual Abuse score.
Associations of maltreatment profiles with suicidal behavior
Bivariate analyses provide basic information about the relationships of sexual, physical, and emotional maltreatment to suicidal behavior. But because effects of other maltreatment types are not concurrently modeled, they fail to quantify unique effects of individual maltreatment types or joint effects of multiple forms of maltreatment. Multivariate models that included all 5 subtype scales were attempted but yielded invalid results due to multicollinearity.35 We therefore used the latent maltreatment profiles illustrated in Figure 1 to address these questions.
Multivariate additive discrete-time survival models showed that maltreatment profile was associated with all outcomes (Table 3). Relative to no maltreatment, all maltreatment profiles were associated with elevated odds of lifetime ideation [Χ2 (4, N = 38237) = 1491.22, p < .001], plan [Χ2 (4, N = 38237) = 517.14, p < .001], attempt [Χ2 (4, N = 38237) = 411.98, p < .001], and plan among ideators [Χ2 (4, n = 5280) = 73.47, p < .001]. Maltreatment profile also predicted planned attempts [Χ2 (4, n = 807) = 22.35, p < .001], with members of the Frequent Emotional and Physical Maltreatment; Episodic Emotional and Sexual Abuse; and Frequent Emotional, Physical, and Sexual Maltreatment classes displaying increased odds of this outcome. Maltreatment profile was further associated with unplanned attempts [Χ2 (4, n = 4595) = 28.26, p < .001]; with members of the Frequent Emotional, Physical, and Sexual Maltreatment class having elevated odds of this outcome. PARPs from these multivariate models indicate that maltreatment was implicated in 26.1% of cases of suicidal ideation, 41.7% of plans, and 43.0% of attempts; as well as 20.1% of suicide plans among those with ideation, 16.2% of planned attempts, and 9.5% of unplanned attempts.
Table 3:
Multivariate models of associations between childhood maltreatment profile and lifetime suicidal behaviors
| Total Sample (N = 38,237) | Among Lifetime Ideators | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ideation | Plan | Attempt | Plan (n = 5280) | Planned Attempt (n = 807) | Unplanned Attempt (n = 4595) | |||||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| No Maltreatment | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Episodic Emotional Maltreatment | 3.10 | 2.88–3.35 | 3.75 | 3.13–4.49 | 3.60 | 2.85–4.54 | 1.40 | 1.17–1.67 | 1.20 | 0.83–1.75 | 1.04 | 0.72–1.51 |
| Frequent Emotional and Physical Maltreatment | 3.87 | 3.37–4.46 | 6.45 | 4.90–8.51 | 6.17 | 4.70–8.09 | 2.09 | 1.60–2.73 | 2.01 | 1.34–3.02 | 1.01 | 0.65–1.56 |
| Episodic Emotional and Sexual Abuse | 3.85 | 3.38–4.39 | 6.86 | 5.16–9.11 | 7.13 | 5.42–9.39 | 2.28 | 1.67–3.12 | 2.26 | 1.50–3.39 | 1.46 | 0.89–2.39 |
| Frequent Emotional, Physical, and Sexual Maltreatment | 4.93 | 3.85–6.33 | 10.77 | 7.31–15.86 | 15.95 | 10.70–23.77 | 3.10 | 1.94–4.95 | 2.47 | 1.19–5.16 | 5.32 | 2.83–10.00 |
Notes. AOR = adjusted odds ratio. CI = confidence interval. Rows represent levels of the predictor variable (childhood maltreatment profile). Results for 6 separate models are displayed in the columns; column labels (e.g., “Ideation”) denote the dependent variable. All models adjust for age, gender, ethnicity, marital status, religion, soldier and parental education level, nativity, service component, site of Basic Combat Training, and person-year. Adjusting for these variables, childhood maltreatment profile was a significant predictor of all 6 outcomes (ps < .001).
Because previous studies have encountered obstacles to isolating effects of sexual abuse,37 we contrasted associations with suicidal behaviors exhibited by profiles that were similar except for presence/absence of sexual abuse. Compared to Episodic Emotional Maltreatment, the Episodic Emotional and Sexual Abuse profile was associated with increased odds of lifetime ideation (AOR = 1.24; p = .003), plan (AOR = 1.83; p = .001), attempt (AOR = 1.98; p < .001), plan among ideators (AOR = 1.63; p = .012), and planned attempt (AOR = 1.87; p = .009). Relative to Frequent Emotional and Physical Maltreatment, the Frequent Emotional, Physical, and Sexual Maltreatment profile was associated with increased odds of lifetime plan (AOR = 1.67; p = .027), attempt (AOR = 2.59; p < .001), and unplanned attempt (AOR = 5.28; p < .001).
Sensitivity analyses
Maltreatment profile remained significantly associated with all suicidal behaviors (ps < .001) after adjusting for type and number of mental disorders; however, magnitudes of AORs decreased (Supplementary eTable 4). The relationship of maltreatment to suicidal behavior thus appeared partially mediated by mental disorders and overall psychiatric comorbidity.
The global index of other lifetime trauma exposure was next added to the sensitivity models that adjusted for mental disorders. Maltreatment profile remained significantly associated with all suicidal behaviors (all ps < .001, except p = .007 for its association with planned attempts) and AORs were only modestly attenuated (results available upon request). Exposure to other types of trauma did not appear to explain the associations of maltreatment profile with suicidal behaviors.
DISCUSSION
The associations of childhood maltreatment with adult health are profound and enduring. They extend from health behaviors to physical illness to mental disorders and suicidal behavior.38 Whereas childhood maltreatment has long been appreciated as a risk factor for suicide attempts and deaths in the general population, it is only recently that its contribution to suicidal behavior in servicemembers has been considered.39 In this study of young adults entering the U.S. Army, we show that all forms of childhood maltreatment are associated with lifetime suicidal behavior. This includes purely emotional maltreatment as well as physical neglect, which have not been examined previously as risk factors for suicidal behavior in servicemembers.
The current analysis is novel in other respects. Using latent profile analysis, we identified groups of soldiers with similar patterns of endorsement of sexual, physical, and emotional maltreatment. Final models of suicidal behaviors utilized these profiles, conveying information about risk exacerbation for individuals with specific maltreatment histories. The study also advances understanding of harms associated with maltreatment by documenting its associations with planning and attempting suicide among soldiers with ideation.
There are also important limitations to our study. The current analysis focuses on only a subset of the wide range of traumas that can occur between the ages of 0–17 years. Some research has found differential associations of maltreatment with mental health outcomes depending on the age of onset of abuse or neglect.40 We were unable to investigate this in the current analysis because exact age of onset of maltreatment was not assessed; it was only established that the abuse or neglect occurred prior to age 18. For the purpose of the discrete-time survival models, we assumed that the onset of maltreatment occurred before the emergence of suicidal behaviors. However, this may not hold true universally; it is possible that some suicidal behaviors with onset prior to age 18 predated abuse and/or neglect. We did not restrict outcomes to those occurring at age 18 or later, as this would have resulted in exclusion of a majority of cases of suicidal behaviors in this young adult sample. More importantly, such an analysis would fail to adequately represent the population of maltreated individuals, who often have early onset of mental health problems.41
Maltreatment was assesed retrospectively via self-report, and may be subject to recall and response biases. The latter could include minimization of maltreatment (e.g., due to concerns about disclosing personal experiences), which has been found in prior studies that assessed maltreatment history via self-report.42 We also lack a comparison to a civilian sample and cannot characterize differences in rates of maltreatment and strength of associations vis a vis soldiers. Cross-study differences in sample characteristics and variability in the measurement and definition of maltreatment43,44 make it difficult to draw conclusions about the relative prevalence of maltreatment in Army soldiers versus the US general population.16
Because this study examined suicidal behaviors among new soldiers reporting for basic combat training (without subsequent follow-up assessment), we were unable to investigate whether childhood maltreatment is a risk factor for suicidal behaviors following exposure to deployment-related stressors; this remains an important question for future study. Additionally, the cross-sectional nature of the data, obtained at entry into Army service, limits any causal inferences and precludes examination of possible interactions of maltreatment history with military stressors such as deployment. Some factors that are associated with both maltreatment and suicidal behavior (e.g., social support) were not included in the models and may contribute to the observed associations. Lastly, a comprehensive examination of associations of maltreament with suicidal behavior should ideally incorporate biological predictors.45
Overall, profiles reflecting more frequent and pervasive maltreatment were more strongly associated with suicidal behavior. This observation converges with prior findings highlighting adverse outcomes of poly-victimization, which tends to be more norm than exception.46,47 Examining unique effects of maltreatment subtypes is fraught with challenges, such as statistical problems related to unidirectional redundancy of rarer forms of maltreatment (e.g., sexual abuse) with other types of abuse and neglect.37,48 We were able to estimate odds of suicidal behaviors for subgroups of soldiers with distinct maltreatment profiles, as well as infer specific effects of sexual abuse by contrasting profiles that were similar except for presence or absence of this exposure. Profiles involving sexual abuse were associated with elevated odds of several suicidal behaviors relative to maltreatment profiles characterized solely by emotional and physical abuse.
Importantly, we found that those reporting frequent childhood sexual, physical, and emotional maltreatment – a small (< 1 % of new soldiers) group composed primarily of women – had markedly increased odds of suicidal ideation (~ 5X), plan (~ 10X), and attempt (~ 15X), compared to soldiers who were not maltreated. This profile also displayed strong associations with progression from ideation to plan and plan to attempt; and was uniquely associated with risk for impulsive attempts that occurred in the absence of a plan. Such observations may be actionable in that identification of soldiers at this magnified risk for suicidal behavior could provide a point of entry into risk mitigation programs.
Although mental disorders such as major depression are clearly associated with increased risk for suicidal behavior, we found strong, independent effects of childhood maltreatment that were only partially mediated by mental disorders. These observations, along with robust population attributable risk proportions (>40% for lifetime plan and attempt), lend plausibility to the notion that childhood maltreatment played a role in the emergence of suicidal behaviors in these young adults, and signal the potential value of targeting maltreatment to prevent suicide in the military. A focus in early adulthood on reduction of harm associated with childhood maltreatment also might have broader benefits such as reducing incidence of mental disorders. These remain important questions for future study.
Supplementary Material
Clinical Points:
Childhood maltreatment is known to increase the risk for subsequent mental disorders and suicidal behaviors, but the extent to which this applies to military personnel entering the army is unclear.
Knowing that childhood maltreatment is often associated with suicidality in military personnel may provide an opportunity for specific intervention.
Acknowledgments
Financial Support: Army STARRS was sponsored by the Department of the Army and funded under cooperative agreement number U01MH087981 with the U.S. Department of Health and Human Services, National Institutes of Health, and National Institute of Mental Health (NIH/NIMH), Bethesda, MD, USA.
Role of the Funding Agency: The funding agency (NIMH) had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Other acknowledgments: The Army STARRS Team consists of Co-Principal Investigators: Robert J. Ursano, MD (Uniformed Services University of the Health Sciences) and Murray B. Stein, MD, MPH (University of California San Diego and VA San Diego Healthcare System)
Site Principal Investigators: Steven Heeringa, PhD (University of Michigan) and Ronald C. Kessler, PhD (Harvard Medical School)
National Institute of Mental Health (NIMH) collaborating scientists: Lisa J. Colpe, PhD, MPH and Michael Schoenbaum, PhD
Army liaisons/consultants: COL Steven Cersovsky, MD, MPH (USAPHC (Provisional)) and Kenneth Cox, MD, MPH (USAPHC (Provisional))
Other team members: Pablo A. Aliaga, MA (Uniformed Services University of the Health Sciences); COL David M. Benedek, MD (Uniformed Services University of the Health Sciences); K. Nikki Benevides, MA (Uniformed Services University of the Health Sciences); Paul D. Bliese, PhD (University of South Carolina); Susan Borja, PhD (NIMH); Evelyn J. Bromet, PhD (Stony Brook University School of Medicine); Gregory G. Brown, PhD (University of California San Diego); Laura Campbell-Sills, PhD (University of California San Diego); Catherine L. Dempsey, PhD, MPH (Uniformed Services University of the Health Sciences); Carol S. Fullerton, PhD (Uniformed Services University of the Health Sciences); Nancy Gebler, MA (University of Michigan); Robert K. Gifford, PhD (Uniformed Services University of the Health Sciences); Stephen E. Gilman, ScD (Harvard School of Public Health); Marjan G. Holloway, PhD (Uniformed Services University of the Health Sciences); Paul E. Hurwitz, MPH (Uniformed Services University of the Health Sciences); Sonia Jain, PhD (University of California San Diego); Tzu-Cheg Kao, PhD (Uniformed Services University of the Health Sciences); Karestan C. Koenen, PhD (Columbia University); Lisa Lewandowski-Romps, PhD (University of Michigan); Holly Herberman Mash, PhD (Uniformed Services University of the Health Sciences); James E. McCarroll, PhD, MPH (Uniformed Services University of the Health Sciences); James A. Naifeh, PhD (Uniformed Services University of the Health Sciences); Tsz Hin Hinz Ng, MPH (Uniformed Services University of the Health Sciences); Matthew K. Nock, PhD (Harvard University); Rema Raman, PhD (University of California San Diego); Holly J. Ramsawh, PhD (Uniformed Services University of the Health Sciences); Anthony Joseph Rosellini, PhD (Harvard Medical School); Nancy A. Sampson, BA (Harvard Medical School); CDR Patcho Santiago, MD, MPH (Uniformed Services University of the Health Sciences); Michaelle Scanlon, MBA (NIMH); Jordan W. Smoller, MD, ScD (Harvard Medical School); Amy Street, PhD (Boston University School of Medicine); Michael L. Thomas, PhD (University of California San Diego); Leming Wang, MS (Uniformed Services University of the Health Sciences); Christina L. Wassel, PhD (University of Vermont); Simon Wessely, FMedSci (King’s College London); Christina L. Wryter, BA (Uniformed Services University of the Health Sciences); Hongyan Wu, MPH (Uniformed Services University of the Health Sciences); LTC Gary H. Wynn, MD (Uniformed Services University of the Health Sciences); and Alan M. Zaslavsky, PhD (Harvard Medical School).
Footnotes
Conflict of Interest: Dr. Stein has in the past three years been a consultant for Actelion, Dart Neuroscience, Healthcare Management Technologies, Janssen, Oxeia Biopharmaceuticals, Pfizer, Resilience Therapeutics, and Tonix Pharmaceuticals. In the past three years, Dr. Kessler has been a consultant for Hoffman-La Roche, Inc., Johnson & Johnson Wellness and Prevention, and Sonofi-Aventis Groupe. Dr. Kessler has served on advisory boards for Mensante Corporation, Plus One Health Management, Lake Nona Institute, and U.S. Preventive Medicine. Dr. Kessler owns 25% share in DataStat, Inc. The remaining authors report nothing to disclose.
Disclaimer: The contents are solely the responsibility of the authors and do not necessarily represent the views of the Department of Health and Human Services, NIMH, the Veterans Administration, Department of the Army, or the Department of Defense.
REFERENCES
- 1.Rockett IR, Regier MD, Kapusta ND, et al. Leading causes of unintentional and intentional injury mortality: United States, 2000–2009. Am J Public Health. 2012;102(11):e84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reger MA, Smolenski DJ, Skopp NA, et al. Risk of suicide among US military service members following Operation Enduring Freedom or Operation Iraqi Freedom deployment and separation from the US military. JAMA Psychiatry. 2015;72(6):561–569. [DOI] [PubMed] [Google Scholar]
- 3.Ramchand R, Rudavsky R, Grant S, Tanielian T, Jaycox L. Prevalence of, risk factors for, and consequences of posttraumatic stress disorder and other mental health problems in military populations deployed to Iraq and Afghanistan. Curr Psychiatry Rep. 2015;17(5):37. [DOI] [PubMed] [Google Scholar]
- 4.Ramsawh HJ, Fullerton CS, Mash HB, et al. Risk for suicidal behaviors associated with PTSD, depression, and their comorbidity in the U.S. Army. J Affect Disord. 2014;161:116–122. [DOI] [PubMed] [Google Scholar]
- 5.Ursano RJ, Kessler RC, Stein MB, et al. Suicide attempts in the US Army during the wars in Afghanistan and Iraq, 2004 to 2009. JAMA Psychiatry. 2015;72(9):917–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nock MK, Stein MB, Heeringa SG, et al. Prevalence and correlates of suicidal behavior among soldiers: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA Psychiatry. 2014;71(5):514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.LeardMann CA, Powell TM, Smith TC, et al. Risk factors associated with suicide in current and former US military personnel. JAMA. 2013;310(5):496–506. [DOI] [PubMed] [Google Scholar]
- 8.Ursano RJ, Kessler RC, Stein MB, et al. Deployment, Mental Health, and Suicide Attempts among U.S. Army Soldiers: Risk Factors, Methods, and Time. JAMA Psychiatry. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schoenbaum M, Kessler RC, Gilman SE, et al. Predictors of suicide and accident death in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA Psychiatry. 2014;71(5):493–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barth SK, Kimerling RE, Pavao J, et al. Military sexual trauma among recent veterans: correlates of sexual assault and sexual harassment. Am J Prev Med. 2016;50(1):77–86. [DOI] [PubMed] [Google Scholar]
- 11.Kimerling R, Makin-Byrd K, Louzon S, Ignacio RV, McCarthy JF. Military sexual trauma and suicide mortality. Am J Prev Med. 2015. Published online December 14, 2015. [DOI] [PubMed] [Google Scholar]
- 12.Borges G, Nock MK, Haro Abad JM, et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71(12):1617–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bruffaerts R, Demyttenaere K, Borges G, et al. Childhood adversities as risk factors for onset and persistence of suicidal behaviour. Br J Psychiatry. 2010;197(1):20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286(24):3089–3096. [DOI] [PubMed] [Google Scholar]
- 15.Enns MW, Cox BJ, Afifi TO, De Graaf R, Ten Have M, Sareen J. Childhood adversities and risk for suicidal ideation and attempts: a longitudinal population-based study. Psychol Med. 2006;36(12):1769–1778. [DOI] [PubMed] [Google Scholar]
- 16.Hoertel N, Franco S, Wall MM, et al. Childhood maltreatment and risk of suicide attempt: a nationally representative study. J Clin Psychiatry. 2015;76(7):916–923. [DOI] [PubMed] [Google Scholar]
- 17.Joiner TE Jr., Sachs-Ericsson NJ, Wingate LR, Brown JS, Anestis MD, Selby EA. Childhood physical and sexual abuse and lifetime number of suicide attempts: a persistent and theoretically important relationship. Behav Res Ther. 2007;45(3):539–547. [DOI] [PubMed] [Google Scholar]
- 18.Nock MK, Deming CA, Fullerton CS, et al. Suicide among soldiers: a review of psychosocial risk and protective factors. Psychiatry. 2013;76(2):97–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Youssef NA, Green KT, Dedert EA, et al. Exploration of the influence of childhood trauma, combat exposure, and the resilience construct on depression and suicidal ideation among U.S. Iraq/Afghanistan era military personnel and veterans. Arch Suicide Res. 2013;17(2):106–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Afifi TO, Taillieu T, Zamorski MA, Turner S, Cheung K, Sareen J. Association of child abuse exposure with suicidal ideation, suicide plans, and suicide attempts in military personnel and the general population in Canada. JAMA Psychiatry. 2016;73(3):229–238. [DOI] [PubMed] [Google Scholar]
- 21.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Colpe LJ, Fullerton CS, et al. Design of the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int J Methods Psychiatr Res. 2013;22(4):267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ursano RJ, Colpe LJ, Heeringa SG, et al. The Army study to Assess Risk and Resilience in Servicemembers (Army STARRS). Psychiatry. 2014;77(2):107–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kessler RC, Heeringa SG, Colpe LJ, et al. Response bias, weighting adjustments, and design effects in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int J Methods Psychiatr Res. 2013;22(4):288–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ursano RJ, Heeringa SG, Stein MB, et al. Prevalence and correlates of suicidal behavior among new soldiers in the U.S. Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Depress Anxiety. 2015;32(1):3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Santiago PN, Colpe LJ, et al. Clinical reappraisal of the Composite International Diagnostic Interview Screening Scales (CIDI-SC) in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int J Methods Psychiatr Res. 2013;22(4):303–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McMahon K, Hoertel N, Wall MM, Okuda M, Limosin F, Blanco C. Childhood maltreatment and risk of intimate partner violence: A national study. J Psychiatr Res. 2015;69:42–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.R: A language and environment for statistical computing [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 30.Roesch SC, Villodas M, Villodas F. Latent class/profile analysis in maltreatment research: a commentary on Nooner et al., Pears et al., and looking beyond. Child Abuse Negl. 2010;34(3):155–160. [DOI] [PubMed] [Google Scholar]
- 31.Ballard ED, Van Eck K, Musci RJ, Hart SR, Storr CL, Breslau N, Wilcox HC. Latent classes of childhood trauma exposure predict the development of behavioral health outcomes in adolescence and young adulthood. Psychol Med. 2015;45(15):3305–16. [DOI] [PubMed] [Google Scholar]
- 32.Mplus 7.3 [Computer software] [computer program]. Los Angeles, CA: Author; 1998–2014. [Google Scholar]
- 33.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structl Equ Modeling. 2007;14:535–569. [Google Scholar]
- 34.survey: analysis of complex survey samples [computer program]. 2012.
- 35.Efron B Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Stat Assoc. 1988;83:414–425. [Google Scholar]
- 36.Spinhoven P, Penninx BW, Hickendorff M, van Hemert AM, Bernstein DP, Elzinga BM. Childhood Trauma Questionnaire: factor structure, measurement invariance, and validity across emotional disorders. Psychol Assess. 2014;26(3):717–729. [DOI] [PubMed] [Google Scholar]
- 37.Vachon DD, Krueger RF, Rogosch FA, Cicchetti D. Assessment of the harmful psychiatric and behavioral effects of different forms of child maltreatment. JAMA Psychiatry. 2015;72(11):1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blosnich JR, Bossarte RM. Childhood abuse and military experience-important information to better serve those who have served. JAMA Psychiatry. 2016;73(3):195–196. [DOI] [PubMed] [Google Scholar]
- 40.Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. J Abnorm Psychol. 2007;116(1):176–87. [DOI] [PubMed] [Google Scholar]
- 41.Teicher MH, Samson JA. Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am J Psychiatry. 2013;170(10):1114–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MacDonald K, Thomas ML, Sciolla AF, et al. Minimization of Childhood Maltreatment Is Common and Consequential: Results from a Large, Multinational Sample Using the Childhood Trauma Questionnaire. PLoS One. 2016;11(1):e0146058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hovdestad W, Campeau A, Potter D, Tonmyr L. A systematic review of childhood maltreatment assessments in population-representative surveys since 1990. PLoS One. 2015;10(5):e0123366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jud A, Fegert JM, Finkelhor D. On the incidence and prevalence of child maltreatment: a research agenda. Child Adolesc Psychiatry Ment Health. 2016;10:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Labonte B, Yerko V, Gross J, et al. Differential glucocorticoid receptor exon 1(B), 1(C), and 1(H) expression and methylation in suicide completers with a history of childhood abuse. Biol Psychiatry. 2012;72(1):41–48. [DOI] [PubMed] [Google Scholar]
- 46.Turner HA, Shattuck A, Finkelhor D, Hamby S. Effects of Poly-Victimization on Adolescent Social Support, Self-Concept, and Psychological Distress. J Interpers Violence. In press. Published online June 1, 2015. [DOI] [PubMed] [Google Scholar]
- 47.Turner HA, Finkelhor D, Ormrod R. Poly-victimization in a national sample of children and youth. Am J Prev Med. 2010;38(3):323–330. [DOI] [PubMed] [Google Scholar]
- 48.Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. 1997;27(5):1101–1119. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.