Abstract
Background
Many women experience perineal pain after childbirth, especially after having sustained perineal trauma. Perineal pain‐management strategies are thus an important part of postnatal care. Non‐steroidal anti‐inflammatory drugs (NSAIDs) are a commonly used type of medication in the management of postpartum pain and their effectiveness and safety should be assessed.
Objectives
To determine the effectiveness of a single dose of an oral NSAID for relief of acute perineal pain in the early postpartum period.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (31 March 2016), OpenSIGLE, ProQuest Dissertations and Theses, the ISRCTN Registry and ClinicalTrials.gov (31 March 2016). We also reviewed reference lists of retrieved papers and contacted experts in the field.
Selection criteria
Randomised controlled trials (RCTs) assessing a single dose of a NSAID versus a single dose of placebo, paracetamol or another NSAID for women with perineal pain in the early postpartum period. Quasi‐RCTs and cross‐over trials were excluded.
Data collection and analysis
Two review authors (FW and VS) independently assessed all identified papers for inclusion and risk of bias. Any discrepancies were resolved through discussion and consensus. Data extraction, including calculations of pain relief scores, was also conducted independently by two review authors and checked for accuracy.
Main results
We included 28 studies that examined 13 different NSAIDs and involved 4181 women (none of whom were breastfeeding). Studies were published between 1967 and 2013, with the majority published in the 1980s. Of the 4181 women involved in the studies, 2642 received a NSAID and 1539 received placebo or paracetamol. Risk of bias was generally unclear due to poor reporting, but in most studies the participants and personnel were blinded, outcome data were complete and the outcomes that were specified in the methods section were reported.
None of the included studies reported on any of this review's secondary outcomes: prolonged hospitalisation or re‐hospitalisation due to perineal pain; breastfeeding (fully or mixed) at discharge; breastfeeding (fully or mixed) at six weeks; perineal pain at six weeks; maternal views; postpartum depression; instrumental measures of disability due to perineal pain.
NSAID versus placebo
Compared to women who received a placebo, more women who received a single dose NSAID achieved adequate pain relief at four hours (risk ratio (RR) 1.91, 95% confidence interval (CI) 1.64 to 2.23, 10 studies, 1573 participants (low‐quality evidence)) and adequate pain relief at six hours (RR 1.92, 95% CI 1.69 to 2.17, 17 studies, 2079 participants (very low‐quality evidence)). Women who received a NSAID were also less likely to need additional analgesia compared to women who received placebo at four hours (RR 0.39, 95% CI 0.26 to 0.58, four studies, 486 participants (low‐quality evidence)) and at six hours after initial administration (RR 0.32, 95% CI 0.26 to 0.40, 10 studies, 1012 participants (low‐quality evidence)). Fourteen maternal adverse effects were reported in the NSAID group (drowsiness (5), abdominal discomfort (2), weakness (1), dizziness (2), headache (2), moderate epigastralgia (1), not specified (1)) and eight in the placebo group (drowsiness (2), light headed (1), nausea (1), backache (1), dizziness (1), epigastric pain (1), not specified (1)), although not all studies assessed adverse effects. There was no difference in overall maternal adverse effects between NSAIDs and placebo at six hours post‐administration (RR 1.38, 95% CI 0.71 to 2.70, 13 studies, 1388 participants (very low‐quality evidence)). One small study (with two treatment arms) assessed maternal adverse effects at four hours post‐administration, but there were no maternal adverse effects observed (one study, 90 participants (low‐quality evidence)). Neonatal adverse effects were not assessed in any of the included studies.
NSAID versus paracetamol
NSAIDs versus paracetamol were also more effective for adequate pain relief at four hours (RR 1.54, 95% CI 1.07 to 2.22, three studies, 342 participants) but not at six hours post‐administration. There was no difference in the need for additional analgesia between the two groups at four hours (RR 0.55, 95% CI 0.27 to 1.13, one study, 73 participants), but women in the NSAID group were less likely to need any additional analgesia at six hours (RR 0.28, 95% CI 0.12 to 0.67, one study, 59 participants). No maternal adverse effects were reported four hours after drug administration (one study). Six hours post‐administration, there was no difference between the groups in the number of maternal adverse effects (RR 0.74, 95% CI 0.27 to 2.08, three studies, 300 participants), with one case of pruritis in the NSAID group and one case of sleepiness in the paracetamol group. Neonatal adverse effects were not assessed in any of the included studies.
Comparisons of different NSAIDs and different doses of the same NSAID did not demonstrate any differences in their effectiveness on any of the primary outcome measures; however, few data were available on some NSAIDs.
Authors' conclusions
In women who are not breastfeeding and who sustained perineal trauma, NSAIDs (compared to placebo) provide greater pain relief for acute postpartum perineal pain and fewer women need additional analgesia when treated with a NSAID. However, the risk of bias was unclear for many of the included studies, adverse effects were often not assessed and breastfeeding women were not included in the studies. The overall quality of the evidence (GRADE) was low with the evidence for all outcomes rated as low or very low. The main reasons for downgrading were inclusion of studies with high risk of bias and inconsistency of findings of individual studies.
NSAIDs also appear to be more effective in providing relief for perineal pain than paracetamol, but few studies were included in this analysis.
Future studies should examine NSAIDs' adverse effects profile including neonatal adverse effects and the compatibility of NSAIDs with breastfeeding, and assess other important secondary outcomes of this review. Moreover, studies mostly included women who had episiotomies. Future research should consider women with and without perineal trauma, including perineal tears. High‐quality studies should be conducted to further assess the efficacy of NSAIDs versus paracetamol and the efficacy of multimodal treatments.
Keywords: Female; Humans; Pregnancy; Postpartum Period; Acetaminophen; Acetaminophen/administration & dosage; Administration, Oral; Analgesia; Analgesics, Non‐Narcotic; Analgesics, Non‐Narcotic/administration & dosage; Anti‐Inflammatory Agents, Non‐Steroidal; Anti‐Inflammatory Agents, Non‐Steroidal/administration & dosage; Anti‐Inflammatory Agents, Non‐Steroidal/adverse effects; Neuralgia; Neuralgia/drug therapy; Perineum; Perineum/injuries; Randomized Controlled Trials as Topic; Time Factors
Anti‐inflammatory drugs for relief of perineal pain after childbirth
What is the issue?
Following childbirth, many women experience pain in the perineum, an area between the anus and the vagina. This Cochrane review asked if this pain can be reduced by one dose of a non‐steroidal anti‐inflammatory drug (NSAIDs), such as aspirin or ibuprofen.
Why is this important?
The pain some women experience in the perineum after childbirth can be particularly acute if the perineum tears during the birth, or needs to be cut (a procedure known as an episiotomy). Even a woman without tearing or surgery often experiences a degree of discomfort in her perineum, which can affect her mobility as well as her ability to care for her baby. This review is part of a series of reviews on the effectiveness of different drugs for pain relief for perineal pain immediately after birth. It is looking specifically at NSAIDs, such as aspirin and ibuprofen.
What evidence did we find?
We found 28 studies with 4181 women that examined 13 different NSAIDs (aspirin, ibuprofen etc.). We included studies up to 31 March 2016. The studies we found only included women who had trauma of the perineum and who were not breastfeeding. Studies were conducted between 1967 and 2013, were small and not of high quality.
The studies showed that a single dose of a NSAID provided greater pain relief at either four hours (low‐quality evidence) or six hours (very low‐quality evidence) after administration when compared to a placebo (dummy pill) or no treatment in non‐breastfeeding women who had sustained perineal trauma during childbirth. Women who received a single dose of NSAID were also less likely to need additional pain relief at four hours (low‐quality evidence) or six hours (low‐quality evidence) after initial administration compared to women who received placebo or no treatment. Not all of the studies assessed adverse effects of the intervention but some studies reported maternal adverse effects such as drowsiness, headache, weakness, nausea, gastric discomfort but there was no clear difference in the incidence of maternal adverse effects between groups at six hours post‐administration (very low‐quality evidence). One small study reported that there were no maternal adverse effects at four hours post‐administration (low‐quality evidence). None of the studies measured possible adverse effects on the baby.
A NSAID also appeared to be better than paracetamol in providing pain relief at four (but not six hours) after administration, although only three small studies looked at this comparison. Women who received a single dose of NSAID were also less likely to need additional pain relief at six (but not four) hours after administration compared to women who received paracetamol. There were no maternal adverse effects observed at four hours (one small study). Three small studies reported maternal adverse effects at six hours after administration but there were no clear differences between groups. Adverse effects on the baby were not reported in any of the included studies and all studies excluded women who were breastfeeding.
Comparisons of different NSAIDs and different doses of the same NSAID did not demonstrate any clear differences in their effectiveness on any of the main outcomes measured in this review. However, few data were available for some NSAIDs.
None of the included studies reported on any of this review's secondary outcomes, including: extended hospital stay or readmission to hospital due to perineal pain; breastfeeding, perineal pain at six weeks after having the baby; women's views, postpartum depression or measures of disability due to perineal pain.
What does this mean?
For women who are not breastfeeding, a single dose of a NSAIDs may help with perineal pain, after four and six hours. Paracetamol may be similarly helpful. No serious side effects were reported, but not all studies examined this. For women who breastfeed, there are no data and these women should seek help as some NSAIDs are not recommended for women who breastfeed.
Summary of findings
Summary of findings for the main comparison.
NSAID compared with placebo for perineal pain in the early postpartum period
| NSAID compared with placebo for perineal pain in the early postpartum period | ||||||
| Patient or population: women with perineal pain in the early postpartum period Settings: maternity hospitals in the USA, UK, Belgium, Spain, France, Italy, Venezuela, India, Malaysia, Thailand, and Iran. Intervention: NSAID Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | NSAID | |||||
| Adequate pain relief number of participants with adequate pain relief Follow‐up: 4 hours | 284 per 1000 | 543 per 1000 (466 to 634) | RR 1.91 (1.64 to 2.23) | 1573 (10 studies) | ⊕⊕⊝⊝ low1,2 | |
| Adequate pain relief number of participants with adequate pain relief Follow‐up: 6 hours | 321 per 1000 | 615 per 1000 (542 to 696) | RR 1.92 (1.69 to 2.17) | 2079 (17 studies) | ⊕⊝⊝⊝ very low2,3,4 | |
| Need for additional analgesia number of participants who received additional analgesia Follow‐up: 4 hours | 305 per 1000 | 119 per 1000 (79 to 177) | RR 0.39 (0.26 to 0.58) | 486 (4 studies) | ⊕⊕⊝⊝ low4,5 | |
| Need for additional analgesia number of participants who received additional analgesia Follow‐up: 6 hours | 438 per 1000 | 140 per 1000 (114 to 175) | RR 0.32 (0.26 to 0.40) | 1012 (10 studies) | ⊕⊕⊝⊝ low4,5 | |
| Maternal drug adverse effects number of women experiencing adverse effects Follow‐up: 4 hours | See comment | See comment | Not estimable | 90 (1 study) | ⊕⊕⊝⊝ low6 | One small study reported no maternal drug adverse events in either the intervention or control group |
| Maternal drug adverse effects number of women experiencing adverse effects Follow‐up: 6 hours | 22 per 1000 | 31 per 1000 (16 to 60) | RR 1.38 (0.71 to 2.70) | 1388 (13 studies) | ⊕⊝⊝⊝ very low4,7,8 | |
| Neonatal drug adverse effects | No data | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Downgraded one level due to serious risk of bias: two studies included in this outcome had instances of high risk of bias. The remaining studies had a mix of low and unclear risk of bias 2 Downgraded based on visual inspection of funnel plot which indicates likely publication bias 3 Downgraded two levels due to the serious risk of bias: four studies included in this outcome had instances of high risk of bias. The remaining studies had a mix of low and unclear risk of bias 4 Downgraded one level due to inconsistency resulting from different NSAIDs at different doses included in the overall outcome meta‐analysis 5 Downgraded one level due to serious risk of bias: one study included in this outcome had instances of high risk of bias. The remaining studies had a mix of low and unclear risk of bias.
6 Downgraded two levels due to imprecision ‐ small sample size and no events
7 Downgraded one level due to serious risk of bias: two studies included in this outcome had instances of high risk of bias. The remaining studies had a mix of low and unclear risk of bias. 8 Downgraded one level due to few events and 95% CI around the pooled estimate includes no effect
Background
Description of the condition
The perineum in women is a diamond‐shaped area between the vagina and the anus (Chou 2009). Pain in this area is particularly common following childbirth. A study conducted in the UK found that 92% of all women, with or without perineal trauma, reported perineal pain in the first day after birth, although this resolved for 88% of women at two months postpartum (Andrews 2008). Macarthur 2004, in a prospective cohort study involving 447 women in Canada, reported an incidence of perineal pain, in the first day after birth, of 75% in women with an intact perineum. This shows that perineal pain is not limited to women who sustain perineal trauma. However, women who have perineal trauma, which is approximately 70% of women giving birth, more commonly experience perineal pain (Laws 2009), report more severe pain and are more likely to use analgesic medicines (Leeman 2009). Spontaneous trauma to the perineum during childbirth has a four‐degree classification system depending on the tissues affected, varying from tearing of only the skin, subcutaneous tissue and/or vaginal mucosa in a first‐degree tear, to tearing of the deep and superficial perineal muscles and anal sphincter in a third‐degree tear. In a fourth‐degree tear, the ano‐rectal epithelium is also disrupted (Kettle 2004). Episiotomy is another type of trauma to the perineum and involves a surgical incision of the perineum to increase the diameter of the vulval outlet (Kettle 2004). In Macarthur 2004, perineal pain was experienced by 95% (210/220) of women with first‐/second‐degree tears, 97% (94/96) of those who had undergone episiotomies, and 100% (46/46) of women with third‐/fourth‐degree tears, but by six weeks postpartum, the frequency of perineal pain was not different between trauma groups. Preventing perineal trauma, as far as is possible, is thus vital for minimising the experience of perineal pain. A recent Cochrane review evaluating perineal techniques to avoid perineal trauma during childbirth (Aasheim 2011) found that the use of warm compresses reduces third‐ and fourth‐degree tears. However, perineal trauma is not fully preventable and women without perineal trauma also frequently experience perineal pain (Andrews 2008; Macarthur 2004). Consequently, pain‐management strategies for perineal pain are an important part of postpartum care, particularly as perineal pain can interfere with a woman’s mobility, affect her ability to care for her baby (East 2012a), and, if the pain persists, may be associated with urinary/faecal incontinence and dyspareunia (Andrews 2008; Thompson 2002).
The majority of women experience short‐term perineal pain following childbirth, but between 6% to 30% of women continue to report perineal pain at one year postpartum (Schytt 2007; Williams 2007). Definitions of acute and chronic pain vary in the literature, however, chronic pain is often described as pain present for more than 12 weeks (Airaksinen 2006). Pain up to 12 weeks duration is generally considered acute pain, although pain lasting between six and 12 weeks has been further classified as sub‐acute (van Tulder 2006). More recently, rather than defining pain according to set time‐frames of duration, chronic pain has been defined as pain that persists longer than the usual course (Loeser 2011). Acute pain presenting in the early postpartum period should be differentiated from chronic perineal pain in this context (Chou 2009), because of different pathophysiological processes that occur when acute pain becomes chronic (Voscopoulus 2010). The term 'early postpartum period' is equally challenging to define and varies in time‐frame durations in the literature. Early postpartum period has previously been defined as a time period of between three and 12 weeks after a baby's birth (Moodley 2003; Nicklas 2013; O'Brien 2003), a time period of one‐week duration (Abou Saleh 1997), a time period of up to six months postpartum (Goodman 2003; Teich 2014), or without any specified time limit. In this review, for consistency with previous Cochrane reviews examining interventions for early postpartum perineal pain (Chou 2009; Chou 2013), the first four weeks after the birth are considered the 'early postpartum period'. When women experience postpartum perineal pain in this period, it can thus be considered acute pain.
Several methods of pharmacological and non‐pharmacological pain relief are currently being used in managing acute postpartum perineal pain. These include cooling treatments, topical anaesthetics, analgesics and non‐steroidal anti‐inflammatory drugs (NSAIDs). Previous Cochrane reviews evaluating the effectiveness of several treatment strategies for acute perineal pain postpartum concluded that rectal NSAID suppositories are associated with less pain up to 24 hours postpartum compared to placebo (Hedayati 2003) and paracetamol provides more pain relief to women compared to placebo (Chou 2013). In addition, there is non‐compelling evidence for the use of topical anaesthesia (Hedayati 2005), limited evidence for the use of local cooling treatments (East 2012b), and a lack of evidence to support the use of therapeutic ultrasound (Hay‐Smith 1998).
This review will focus on oral NSAIDs (single dose) for alleviating perineal pain in the early postpartum period; that is during the first four weeks after birth.
Description of the intervention
NSAIDs are a group of medicines that have been used for centuries for their analgesic, anti‐pyretic and anti‐inflammatory properties. Salicin was first extracted from willow bark in 1829 by Leroux (Brunton 2011), and the derivative aspirin was produced in 1899 (Rao 2008). In the 20th century, many NSAIDs were developed, however, it was not until the 1970s that a mechanism of action was identified (Rainsford 2007; Vane 1971), and our understanding of their effects as well as their use in the treatment and management of various conditions continues to evolve. NSAIDs are mainly categorised according to their inhibitory effects on two isoforms of cyclo‐oxygenase (COX1 and COX2), as described further below.
Various routes for NSAID administration are available including intra‐muscular injection, intravenously, per rectum, topically and orally (Tramèr 1998). This review examines the effectiveness of NSAIDs taken orally. More specifically, this review evaluates the effectiveness of a single oral dose of a NSAID, whereby a single dose is defined as a dose taken at one time, rather than dosage regimens that would involve more than one dose of a given NSAID over time (Howard 2013). The speed at which an oral NSAID is absorbed into the bloodstream varies for different NSAIDs. For example, for ibuprofen, peak plasma concentrations are observed 15 to 30 minutes after ingesting the drug, with a half‐life in the plasma of approximately two hours (Davies 1998). This is an example of a fast‐acting NSAID, whereas slow‐acting NSAIDs such as naproxen show later peak plasma concentrations and have a longer half‐life (Vree 1993). The recommended dosage at which NSAIDs are administered also depends on the individual NSAID, as well as the route of administration and the purpose for taking the drug. For acute pain, for instance, a single oral dose of 400 mg of ibuprofen is generally taken, which can be repeated every four to six hours up to a maximum daily dose of 2400 mg. Naproxen, as another example, has a maximum daily dose of 1250 mg and is given orally for acute pain in an initial dose of 500 mg followed by 250 mg doses every six to eight hours afterwards, as required (BNF 2014).
The most common adverse effects of NSAIDs include abdominal pain, nausea, dyspepsia, headache, pruritis, urticaria and other skin rashes. Rarely, NSAIDs can lead to perforation of gastric ulcers and gastrointestinal bleeding, hypersensitivity reactions, bronchospasm, haematopoietic disorders, hypertension, cardiac failure and renal failure. Adverse effects are more likely in elderly patients and may be minimised by using the lowest effective dose for the shortest duration necessary (Irish Pharmaceutical Healthcare Association 2014).
How the intervention might work
During childbirth, due to pressure on, or trauma of the perineum, a local inflammatory response occurs causing perineal pain. NSAIDs may improve perineal pain through their anti‐inflammatory action. Moreover, they have a known analgesic effect particularly for pain that is associated with tissue trauma/injury and inflammation (Rao 2008). This review focuses on the effectiveness of a single dose of a NSAID in relieving perineal pain, which, if effective, will mainly be due to its early analgesic properties as its anti‐inflammatory effect will be minimal at this dosage. NSAIDs are believed to act peripherally by inhibiting COX enzymes that catalyse the conversion of arachidonic acid into prostaglandin (PG) (Rao 2008). There are two main isoforms of COX: COX1 and COX2. COX1 is normally present in most tissues and cells and is not related to inflammation, whereas COX2 is induced by inflammatory mediators and is only found in tissues in the presence of inflammation. In addition, COX2 catalyses the production of pro‐inflammatory prostaglandin G2 (Seibert 1994; Smith 1998). Selective COX2 inhibitors were developed to diminish the side effects of non‐selective NSAIDs that result from COX1 inhibition, particularly the inhibition of gastro‐protective prostaglandin synthesis. However, selective COX2 NSAIDs exhibit cardiovascular adverse effects (Solomon 2004).
Pain experienced in the perineal area is transmitted through the pudendal nerve to the spinal segments S2‐S4. NSAIDs thus act peripherally by inhibiting pro‐inflammatory prostaglandin production and by subsequently reducing inflammation in the perineal area and decreasing pudendal pain nerve fibres excitation.
This review examines the effectiveness of a single dose of any NSAID for the management of perineal pain in the early postpartum period.
Why it is important to do this review
Postpartum perineal pain is a very common post‐childbirth complaint. It can have negative consequences for mother and child including disability in daily functioning for the mother; for example, it can interfere in taking care of her infant and in breastfeeding. Early pain management is thus relevant to provide relief and prevent chronicity.
NSAIDs are commonly used in the management of postpartum pain (Leeman 2009). Therefore, it is important to consider their effectiveness and safety, including their safety for the neonate in breastfeeding mothers. The use of NSAID rectal suppositories has been examined in a previous Cochrane review (Hedayati 2003). Adding to the evidence from previous Cochrane reviews evaluating alternative management strategies for postpartum perineal pain, this systematic review evaluates and synthesises studies examining the effectiveness of NSAIDs that are administered orally and in a single dose.
Objectives
To determine the effectiveness of a single dose of an oral non‐steroidal anti‐inflammatory drug (NSAID) for relief of acute perineal pain in the early postpartum period.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) only, comparing a non‐steroidal anti‐inflammatory drug (NSAID) with another NSAID, aspirin, paracetamol or placebo/no drug treatment. Quasi‐RCTs and cross‐over trials were excluded.
Types of participants
All women who had acute perineal pain or who had been treated for acute perineal pain in the early postpartum period; that is the first four weeks after giving birth or as defined by the authors of the studies.
Types of interventions
Single dose of a NSAID compared with placebo/no drug treatment
Single dose of a NSAID compared with a single dose of another NSAID/aspirin
Single dose of a NSAID compared with a single dose of paracetamol
Studies examining NSAIDs administered as suppositories were excluded as these have been examined in another Cochrane review (Hedayati 2003). This review only includes studies examining the effectiveness of NSAIDs administered orally (single dose). Studies that evaluated more than one dose of NSAIDs were included in the review if data on the effectiveness of a single dose were collected and reported separately.
Types of outcome measures
Primary outcomes
Adequate pain relief as reported by the woman, or by determination of > 50% relief of pain (as either stated by the woman or calculated using a formula)*
Need for additional analgesia for relief of perineal pain
Maternal drug adverse effects, e.g. nausea, vomiting, sedation, constipation, diarrhoea, drowsy, sleepy, psychological impact
Neonatal drug adverse effects, e.g. nausea, vomiting, sedation, constipation, diarrhoea, drowsy, sleepy, psychological impact
* Assessment of 50% pain relief via Total Pain Relief (TOTPAR) and Summed Pain Intensity Difference (SPID) scores (see Assessment of pain section)
Secondary outcomes
Prolonged hospitalisation due to perineal pain (days)
Rehospitalisation due to perineal pain
Fully breastfeeding at discharge
Mixed feeding at discharge
Fully breastfeeding at six weeks
Mixed feeding at six weeks
Perineal pain at six weeks
Maternal views (using a validated questionnaire), for example, women’s satisfaction with the intervention
Maternal postpartum depression – measured using a validated depression scale, for example the Edinburgh Postnatal Depression (EPD) scale
Instrumental measures of disability due to perineal pain/activities of daily living (ADLs)/quality of life (QoL), for example, 15D Health‐Related Quality of Life (HRQoL) instrument
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group
Electronic searches
We contacted the Information Specialist to search the Cochrane Pregnancy and Childbirth Group’s Trials Register (31 March 2016).
The Register is a database containing over 21,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate the Pregnancy and Childbirth Group’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth Group in the Cochrane Library and select the ‘Specialized Register ’ section from the options on the left side of the screen.
Briefly, the Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above are reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth Group review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set which has been fully accounted for in the relevant review sections (Included studies; Excluded studies).
We also searched the OpenSIGLE database to identify grey literature and the ProQuest Dissertations and Theses to retrieve dissertation theses related to our topic of interest (31 March 2016). We searched the ISRCTN Registry and ClinicalTrials.gov (31 March 2016) to identify potential ongoing trials (see: Appendix 1 for search terms used).
Searching other resources
We reviewed the reference lists of all selected papers to identify any additional potentially eligible studies not captured by the electronic searches. We also contacted experts in the field of pain relief and maternity care, and, where appropriate, authors of studies published in abstract format only, to identify any unpublished studies.
We did not apply any language or date restrictions.
Data collection and analysis
Assessment of pain
The number of participants achieving adequate pain relief was defined as one of the following.
The number of participants reporting “good” or “excellent” pain relief when asked about their level of pain relief four to six hours after receiving their allocated treatment (the data were extracted as dichotomous data).
The number of women who reported 50% pain relief, or greater.
The number of participants who achieved 50% pain relief, or greater, as calculated by using derived pain relief scores (TOTPAR (total pain relief) or SPID (summed pain intensity differences)) over four to six hours.
TOTPAR or SPID (or both) were calculated provided sufficient data were present. Examples of possible pain measures included the five‐point pain relief (PR) scale with standard or comparable wording (none, slight, moderate, good, complete), the four‐point pain intensity (PI) scale (none, mild, moderate, severe), and/or the visual analogue scale (VAS) for pain relief or pain intensity. From these categorical scales, it was possible to convert results into dichotomous data (the proportion of participants achieving at the least 50%, or greater, max TOTPAR) using standard formulae (Moore 1996; Moore 1997b). Conversion of data in this way allowed the use of these data in a meta‐analysis (Moore 1997a; Moore 1997b). The following equations were used to estimate the proportions of participants achieving at least 50% of maximum TOTPAR.
Proportion with greater than 50% maxTOTPAR = (1.33 x mean %maxTOTPAR – 11.5)
With %maxTOTPAR = mean TOTPAR x 100/(maximum score x number of hours)
Proportion with greater than 50% maxTOTPAR = (1.36 x mean %maxSPID – 2.3)
With %maxSPID = mean SPID x 100/(maximum score x number of hours)
The number of participants achieving at least 50% maxTOTPAR was then calculated by multiplying the proportions of participants with at least 50% maxTOTPAR by the total number of participants in the treatment groups. The number of participants with at least 50% maxTOTPAR was then used to calculate the relative benefit and number needed to treat to benefit. Where studies used more than one method of calculating adequate pain relief, preference for analyses and reporting purposes, in order of decreasing preference, was as follows; i) the proportion with at least 50% maxTOTPAR calculated using SPID; ii) the proportion with at least 50% maxTOTPAR calculated using TOTPAR; and iii) the number of participants reporting 'good' or 'excellent' pain relief/number of participants reporting at least 50% pain relief. We also assessed the number of participants who re‐medicated in the period of four to eight hours, as well as the median time to re‐medication, if the information was available.
Selection of studies
Two review authors (FW and VS) independently assessed for inclusion all of the potential studies identified by the search strategy. We resolved any disagreement through discussion or, if necessary, we would have consulted a third person, however, this was not required. Studies presented only as abstracts were included if the abstract provided sufficient information to assess eligibility and where the authors provided relevant data to include in the analysis.
We created a study flow diagram to map out the number of records identified, included and excluded (Figure 1).
Figure 1.
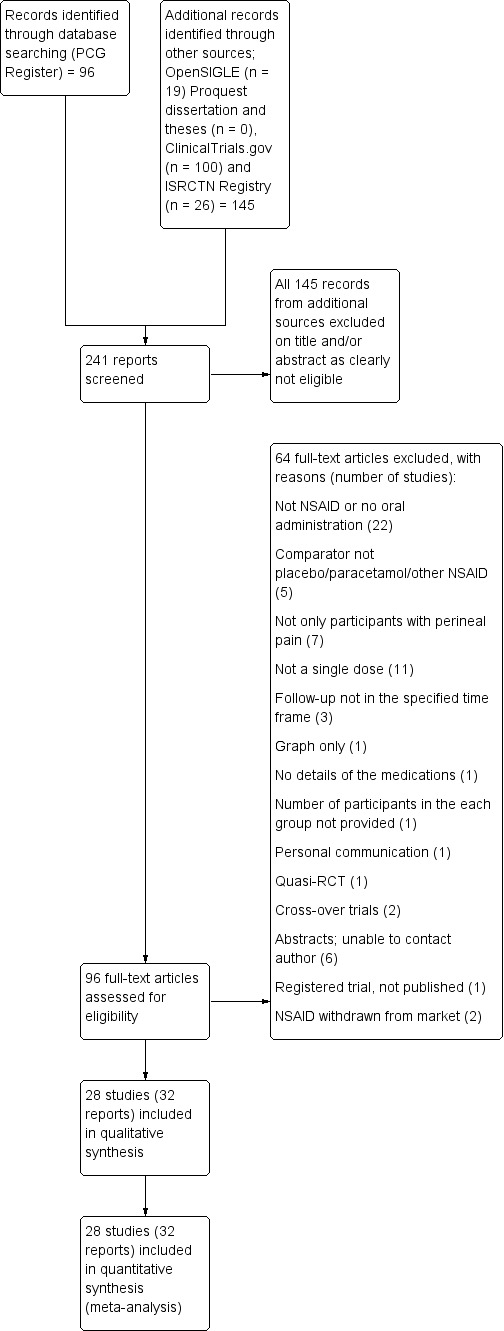
Study flow diagram.
Data extraction and management
We designed a form to extract data based on the Cochrane Pregnancy and Childbirth Group's data extraction template form. For eligible studies, two review authors (FW and VS) extracted the data independently using the agreed form. We resolved discrepancies through discussion or, if necessary, we would have consulted a third person, however, this was not required. We entered data into Review Manager software, version 5.3 (RevMan 2014) and FW and VS independently checked these data for accuracy.
Where information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors (FW and VS) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreement by discussion or, if necessary, we would have involved a third assessor, however, this was not required.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the methods used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that a lack of blinding would be unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome, the completeness of data including attrition and exclusions from the analysis. We state whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we re‐included missing data in the relevant analyses.
We assessed the methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria described in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We intended to explore the impact of the level of bias in sensitivity analyses ‐ seeSensitivity analysis.
Measures of treatment effect
We carried out statistical analyses using the Review Manager software, version 5.3 (RevMan 2014). We used fixed‐effect meta‐analyses for combining data in the absence of significant heterogeneity. Where there was heterogeneity, where results were pooled from studies examining different interventions, or where it was not clear that the same outcome was being measured in all studies, we used random‐effects meta‐analyses.
Dichotomous data
For dichotomous data, we presented the results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we planned to use the mean difference if outcomes were measured in the same way between trials. We also planned to use the standardised mean difference to combine trials that measured the same outcome, but used different methods; however, these were not required, there were no continuous data in the included studies to include in a meta‐analysis.
Assessing the quality of the body of evidence using the GRADE approach
We assessed the quality of the evidence using the GRADE approach as outlined in the GRADE handbook in order to assess the quality of the body of evidence relating to the following outcomes for the main comparison (any NSAID versus placebo).
Adequate pain relief as reported by the woman, or by determination of > 50% relief of pain
Need for additional analgesia for relief of perineal pain
Maternal drug adverse effects
Neonatal drug adverse effects
We used GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create a 'Summary of findings’ table. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Unit of analysis issues
Cluster‐randomised trials
We did not identify any cluster‐randomised trials on the topic. However, if we had found any, we would have included them using the guidance in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Multi‐armed trials
For multi‐armed trials, only the comparisons of intervention arms that were relevant to the systematic review were included. For example, if a study compared ibuprofen, codeine and placebo, only the ibuprofen versus placebo comparison was included in the review.
If comparisons shared intervention or control groups then we divided the number of participants approximately evenly among the comparisons (Higgins 2011). For example, in the studies with two (or more) intervention groups and one control group we divided the number of participants and the number of events in the control group by half (or more where there were more intervention groups).
Dealing with missing data
For included studies, we noted levels of attrition. We explored the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses, and all participants were analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial is the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the T2, I² and Chi² statistics. We regarded heterogeneity as substantial if an I2 was greater than 30% and either a T2 was greater than zero, or there was a low P value (< 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
Where there were 10 or more studies in a meta‐analysis we investigated reporting biases (such as publication bias) using funnel plots. We assessed funnel plot asymmetry visually.
Where we suspected reporting bias (see ‘Selective reporting bias’ above), we attempted to contact study authors to ask them to provide missing outcome data. Where this was not possible, we planned to explore the impact of including such studies in the overall assessment of results using a sensitivity analysis, but this was not required.
Data synthesis
We carried out statistical analysis using the Review Manager software version 5.3 (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials examined the same intervention, and the trials’ populations and methods were judged sufficiently similar. If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average of the range of possible treatment effects and we discuss the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we did not combine trials.
If we used random‐effects analyses, the results are presented as the average treatment effect with 95% confidence intervals, and the estimates of T² and I².
Subgroup analysis and investigation of heterogeneity
Where we identified substantial heterogeneity, we investigated it using subgroup analyses. We considered whether an overall summary was meaningful in the presence of heterogeneity, and if it was, used random‐effects analysis to produce it.
We had planned to carry out the following subgroup analyses.
Drugs compatible with breastfeeding versus those that are not compatible with breastfeeding because they have adverse effects on the infant
Primiparous versus multiparous women
Women with perineal trauma versus women who gave birth over an intact perineum
Different NSAIDs
Different doses of the same NSAID
Women who used prior pain relief versus women who did not use prior pain relief
Different time‐frames of when the dose was taken after the birth
We conducted subgroup analyses for 4. different NSAIDs and 5. different doses of the same NSAID. We were unable to carry out the other planned subgroup analyses due to the absence of relevant data in the included studies.
We used the following outcomes in subgroup analyses.
Adequate pain relief as reported by the woman, or by determination of > 50% relief of pain (as either stated by the woman or calculated using a formula)*
Need for additional analgesia for relief of perineal pain
Maternal drug adverse effects, e.g. nausea, vomiting, sedation, constipation, diarrhoea, drowsy, sleepy, psychological impact
* Assessment of 50% pain relief via TOTPAR and SPID scores (see Assessment of pain section).
We assessed subgroup differences by interaction tests available within RevMan (RevMan 2014). We report the results of subgroup analyses quoting the Chi2 statistic and P value, and the interaction test I² value.
We had also planned to use the outcome neonatal drug adverse effects in subgroup analyses, however, this outcome was not measured in any of the included studies.
Sensitivity analysis
Where appropriate, we carried out planned sensitivity sensitivity analysis to explore the effect of trial quality (risk of bias) for important outcomes in the review. We carried out sensitivity analysis for the primary outcomes, where appropriate, by excluding those studies judged to be at a high risk of bias for any of the the following risk of bias domains: random sequence generation, allocation concealment, blinding of participants and personnel, and incomplete outcome data, reporting bias or other bias.
Results
Description of studies
Results of the search
See: Figure 1.
The search of the Cochrane Pregnancy and Childbirth Group's Trials Register identified 96 reports. The search of additional sources yielded 145 records (OpenSIGLE = 19, ProQUEST dissertation and theses = 0, ISCRTN Registry = 26 and ClinicalTrials.gov = 100), all of which were screened and considered to be ineligible based on title and/or abstract. This resulted in 96 reports being screened at full‐text level.
Included studies
Design and setting
Twenty‐eight studies (32 reports) were included of which two studies were reported in one publication (Laska 1981; Laska 1981a). Twenty‐two studies were multi‐arm studies; in such cases we extracted the data for any non‐steroidal anti‐inflammatory drug (NSAIDs) compared with placebo, paracetamol or other NSAID, only. The details of these studies are described in the Characteristics of included studies section. The effectiveness of paracetamol versus placebo has been examined in a previous Cochrane review (Chou 2013) and the effectiveness of NSAIDs compared with other non‐NSAID drugs will be assessed in future reviews based on the generic protocol (Chou 2009).
Included studies were published between 1967 and 2013; one study was published in the 1960s, two in the 1970s, 18 in the 1980s and four in the 1990s. Only three studies were published since 2000; two in 2008 and one in 2013. Of the 28 included studies, 11 were conducted in USA and six in other high‐income countries (UK, Belgium, Spain, France, Italy). Six studies were conducted in Venezuela. The remaining five studies were conducted in other low‐ or middle‐income countries (India, Malaysia, Thailand, Iran).
Participants and sample sizes
A total of 4539 women were included in this review. of which 358 women received other drugs not included in this review and were subsequently excluded from the analysis. Of the 4181 women included in the analyses, 2642 received a NSAID and 1539 received placebo or paracetamol. Twenty‐seven of the 28 studies examined the effectiveness of NSAIDs for relief of post‐episiotomy pain. One study (Lim 2008) only included women with any perineal trauma requiring repair but excluded third‐ or higher‐degree tears. All trials excluded women who were breastfeeding and none of the included trials reported neonatal adverse outcomes.
Interventions and comparisons
Thirteen different NSAIDs were examined in the studies included in the review. These were aspirin, ibuprofen, diclofenac, diflunisal, dipyrone, fenoprofen, fluproquazone, zomepirac, meclofenamate sodium, aceclofenac, ketoprofen, flurbiprofen, and celecoxib. Studies, or data from studies, reporting on indoprofen, zomepirac and fluproquazone were subsequently removed from the analyses as these NSAIDs are presently withdrawn from the market due to causing the following adverse effects: fluproquazone due to adverse effects on the liver (Kaplowitz 2013), indoprofen due to reports of adverse reactions including reports of carcinogenicity in animal studies (Brayfield 2014), and zomepirac due to being associated with fatal and near‐fatal anaphylactoid reactions (Brayfield 2014).
Doses of the intervention drugs varied across studies and the different doses of individual drugs were compared in subgroup analyses. Drugs deemed to have equivalent doses, that is aspirin 500 mg to 650 mg and ibuprofen 300 mg to 400 mg, were combined for analyses purposes.
Outcomes
For 26 of the 28 included studies, some measure of adequate pain relief could be extracted four to six hours after drug administration. Seven studies provided data on adequate pain relief four hours after taking the medication, nine studies reported this outcome measure at six hours, and seven studies reported adequate pain relief at both four hours and six hours. In addition, three studies (two publications) reported adequate pain relief outcomes at five hours after drug administration (Jain 1985; Laska 1981; Laska 1981a). We included these data in the six hours post‐administration outcomes for analyses purposes. Twenty studies reported summed pain intensity differences (SPID). Eleven of these studies also reported total pain relief (TOTPAR), and five studies also reported adequate pain relief as a good/excellent rating or the number of women reporting at least 50% pain relief. The remaining six studies only reported adequate pain relief as good/excellent or the number of women with at least 50% pain relief. In 20 of the 26 studies that reported SPID, we calculated the number of participants with adequate pain relief via the SPID measure as per protocol. In four of the 11 studies that provided both SPID and TOTPAR (Gleason 1987; Hebertson 1986; Jain 1988; Schachtel 1989), the SPID and TOTPAR calculations of the number of participants with adequate pain relief did not match and the raw data for pain intensity or pain relief were not available. In these cases, we used the SPID data to calculate the number of women with adequate pain relief. It is not entirely clear from the studies the reasons for the discrepancy in the number of participants with adequate pain relief when calculated using SPID versus TOTPAR, however, it may be due to calculation errors in the reports or inaccurate time weighting. The formula to calculate %max TOTPAR contains the number of hours over which pain relief was measured. Some studies for example, measured pain relief at half‐hour and one‐hour post‐administration initially and then hourly thereafter up to six hours providing a total of seven measurements of pain relief. To accurately apply these data to the formula, adjustments need to be made to account for the half‐hour periods or the %maxTOTPAR would otherwise be overestimated. We encountered this absence of adjustment in a study that additionally provided the raw data and we were able to check the calculations. Also, in one of the five studies that reported adequate pain relief as good/excellent, or as the number of women with at least 50% pain relief in addition to SPID, there was a significant unexplained discrepancy between these two measures of adequate pain relief (Hopkinson 1980).
Fifteen studies reported on the need for additional analgesia and 18 studies reported on any maternal drug adverse effects. None of the secondary outcomes pre‐specified in the review were reported in any of the included studies.
Excluded studies
Sixty‐four of the 96 identified studies did not meet the review's inclusion criteria and were excluded as follows: the intervention drug was not a NSAID or was administered by a route other than orally in 22 studies; the comparator was neither a placebo, paracetamol or an other NSAID in five studies; in seven studies perineal pain was not reported separately for included women, rather was reported collectively with other sources of pain or pain in other areas; and, 11 studies did not report on a single dose. The remaining 19 studies were excluded for the following reasons: three studies reported data outside of the reviews specified time‐frames of four and six hours (for example, at eight and 12 hours) (Bloomfield 1970; Melzack 1983; Okun 1982); one study presented a graph only (Jain 1978); one study did not provide details of the medications (Gruber 1979); one study did not provide the number of participants in the each group (Trop 1983); one was a personal communication (Bloomfield 1991); one was a quasi‐randomised controlled trial (Bhounsule 1990); two were cross‐over trials (Finch 1971; Harrison 1992); six were abstracts, all published between 1978 and 1989 (Levin 1978; Olson 1984; Sunshine 1983c; Sunshine 1985; Sunshine 1987b; Sunshine 1989), for which we tried to contact the authors to obtain full reports, but were unable to obtain their contact details; one was a registered trial, which following personal communication was confirmed that the study had not been published and would not be published in the future (Bloomfield 1991); one study (Cater 1985) was excluded because it only examined the NSAID zomepirac which was withdrawn voluntarily from the market by the manufacturer in 1983 because it was associated with fatal and near‐fatal anaphylactoid reactions; and one study (Pedronetto 1975) was excluded because it only examined the NSAID indoprofen, which was withdrawn from markets in the 1980s due to reports of adverse reactions including reports of carcinogenicity in animal studies.
Risk of bias in included studies
There was generally poor reporting in the studies included in this review, particularly around methods of randomisation sequence generation, allocation concealment, and blinding of the outcome assessor, with 17 studies receiving unclear risk of bias judgements for all three of these 'Risk of bias' criteria (Figure 2 and Figure 3).
Figure 2.
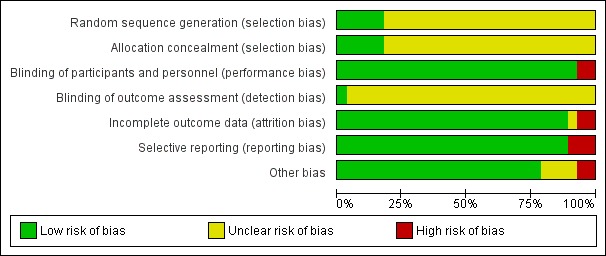
'Risk of bias' graph: review authors' judgements on each risk of bias item presented as percentages across all included studies.
Figure 3.
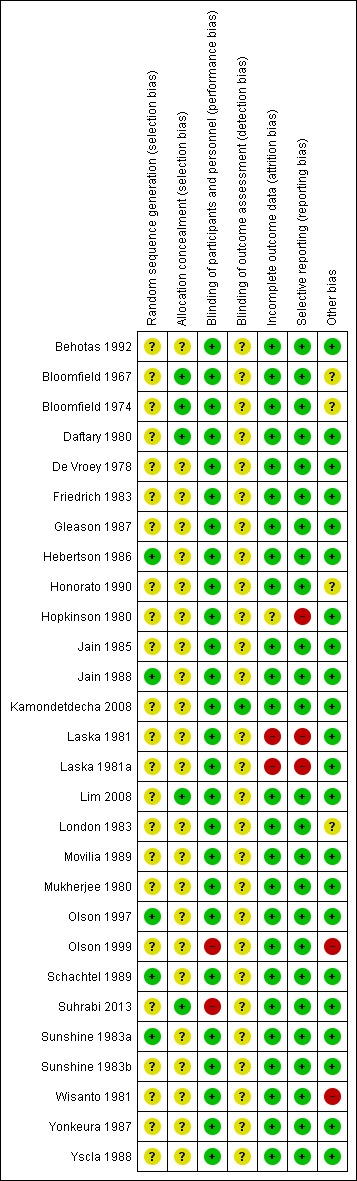
'Risk of bias' summary: review authors' judgements on each risk of bias item for each included study.
Allocation
Only five of the 28 studies described their sequence generation process. All five described using a computer‐generated random sequence (Hebertson 1986; Jain 1988; Olson 1997; Schachtel 1989; Sunshine 1983a). Adequate allocation concealment was described in five studies (Bloomfield 1967; Bloomfield 1974; Daftary 1980; Lim 2008; Suhrabi 2013), but was unclear for all other included studies.
Blinding
Twenty‐six of the 28 included studies were described as double‐blind, defined as blinding of the participants as well as the personnel providing the treatment to the participants, reducing performance bias. Two studies were single‐blind with only the participants blinded to the treatment they received (Olson 1999; Suhrabi 2013). However, all but one study (Kamondetdecha 2008) did not clearly report whether or not the outcome assessor was blinded, making the extent of potential detection bias unclear.
Incomplete outcome data
We assessed all studies as adequately reporting outcomes for all participants and clearly specifying any missing data with reasons provided for this, with the exception of three studies (Hopkinson 1980; Laska 1981; Laska 1981a). In Laska 1981 and Laska 1981a information on withdrawals due to the need for rescue medication was not provided (both assessed as high risk of bias). In Hopkinson 1980 there appeared to be missing data (possibly due to drop‐outs or withdrawals) at two‐, three‐ and four‐hour assessments without a clear statement of reasons for this in the study publication (unclear risk of bias).
Selective reporting
The potential for reporting bias was judged as low for the majority of the studies; however, it is important to note that in the absence of trial protocols it is not truly possible to assess for reporting bias. We judged three studies (Hopkinson 1980; Laska 1981; Laska 1981a) as high risk of bias because they did not report one of the outcomes they had pre‐specified in the methods sections of their papers.
Other potential sources of bias
For one study there was an imbalance in some baseline characteristics including body weight and marital status (Bloomfield 1974). Two studies (Honorato 1990; London 1983) did not provide a clear statement on whether baseline characteristics were balanced or not and we judged these as unclear risk of bias. One study that was stopped early due to administrative changes also received a high risk of bias judgement (Olson 1999). Lastly, one study (Wisanto 1981) received a high risk of bias judgement for this criterion because the time‐lag between episiotomy and drug intake was significantly (P < 0.05) shorter in the placebo group (8.08 hours ± 0.81) compared to the intervention group (10.21 hours ± 0.70). In Bloomfield 1967 there could have been potential carry‐over of effect of intrapartum analgesia. No other potential sources of bias were identified in any of the other included studies.
Effects of interventions
See: Table 1
Any NSAID versus placebo
Primary outcomes
Adequate pain relief
At four hours after drug administration, more women who had received a NSAID experienced adequate pain relief compared to women who received placebo (risk ratio (RR) 1.91, 95% confidence interval (CI) 1.64 to 2.23, 10 studies, 1573 participants (Analysis 1.1)), although the quality of the evidence (GRADE) for this outcome was low (Table 1). Downgrading decisions were due to risk of bias and publication bias (see Figure 4).
Analysis 1.1.
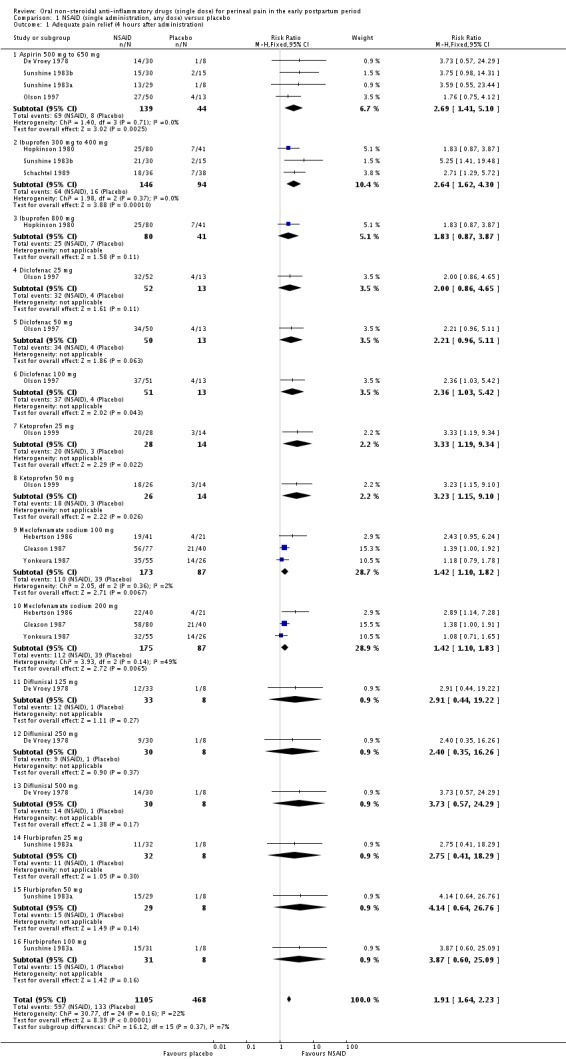
Comparison 1 NSAID (single administration, any dose) versus placebo, Outcome 1 Adequate pain relief (4 hours after administration).
Figure 4.
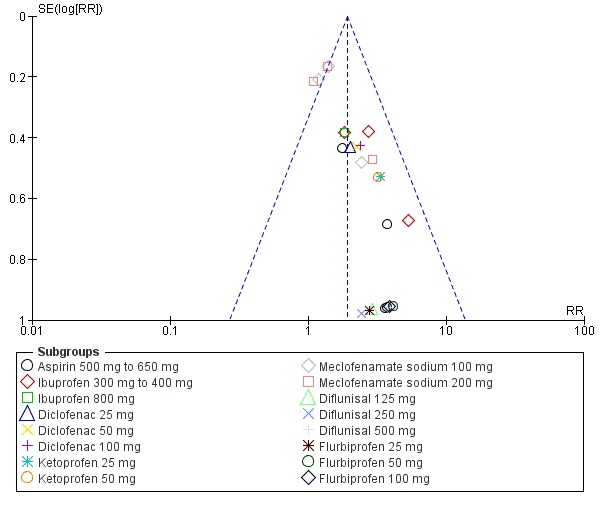
Funnel plot of comparison: 1 NSAID (single administration, any dose) versus placebo, outcome: 1.1 Adequate pain relief (4 hours after administration).
More women reported adequate pain relief in the NSAID compared to the placebo group also at six hours post‐administration (RR 1.92, 95% CI 1.69 to 2.17, 17 studies, 2079 participants (Analysis 1.2)), but the quality of the evidence (GRADE) for this outcome was very low (Table 1). The number needed to treat to have adequate pain relief is four (95% CI 3 to 4) at four hours after drug administration and four (95% CI 3 to 5) at six hours post‐administration. GRADE decisions for downgrading the quality of the evidence for this outcome were based on inconsistency, risk of bias and publication bias (see Figure 5).
Analysis 1.2.
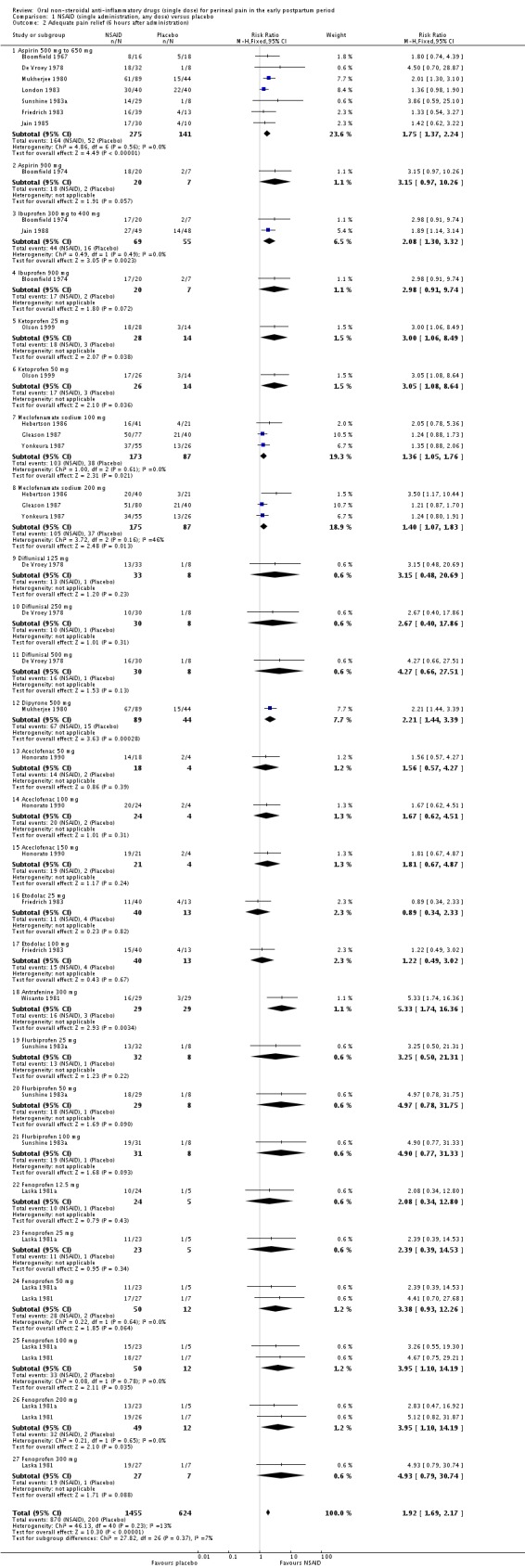
Comparison 1 NSAID (single administration, any dose) versus placebo, Outcome 2 Adequate pain relief (6 hours after administration).
Figure 5.
Funnel plot of comparison: 1 NSAID (single administration, any dose) versus placebo, outcome: 1.2 Adequate pain relief (6 hours after administration).
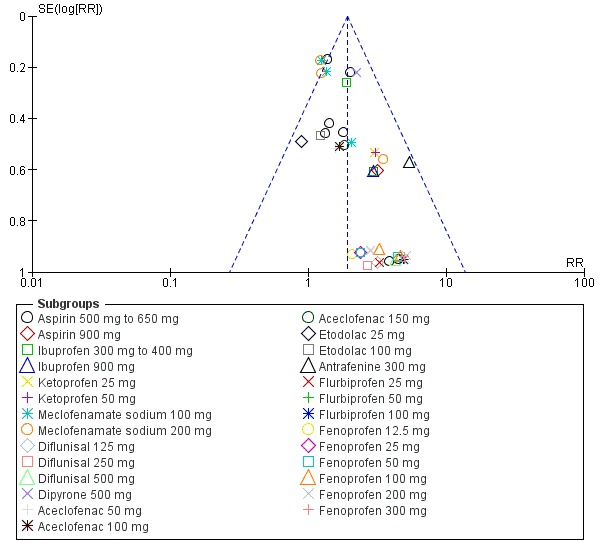
Additional analgesia
Women who received a NSAID were less likely to require additional analgesia at four hours (RR 0.39, 95% CI 0.26 to 0.58, four studies, 486 participants (Analysis 1.3)) and at six hours after initial administration (RR 0.32, 95% CI 0.26 to 0.40, 10 studies, 1012 participants (Analysis 1.4)). The quality of the evidence (GRADE) for this outcome was low at four hours and at six hours follow‐up (Table 1) with downgrading due to inconsistency and risk of bias. A visual inspection of the funnel plot for this outcome suggests that there is no publication bias Figure 6.
Analysis 1.3.
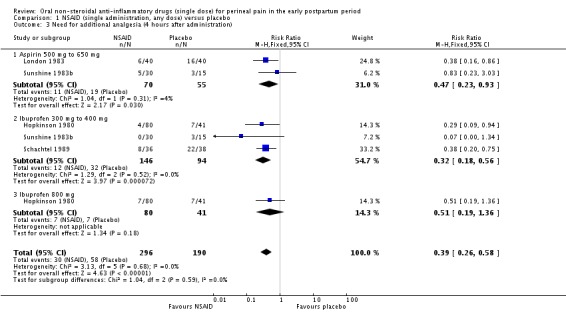
Comparison 1 NSAID (single administration, any dose) versus placebo, Outcome 3 Need for additional analgesia (4 hours after administration).
Analysis 1.4.
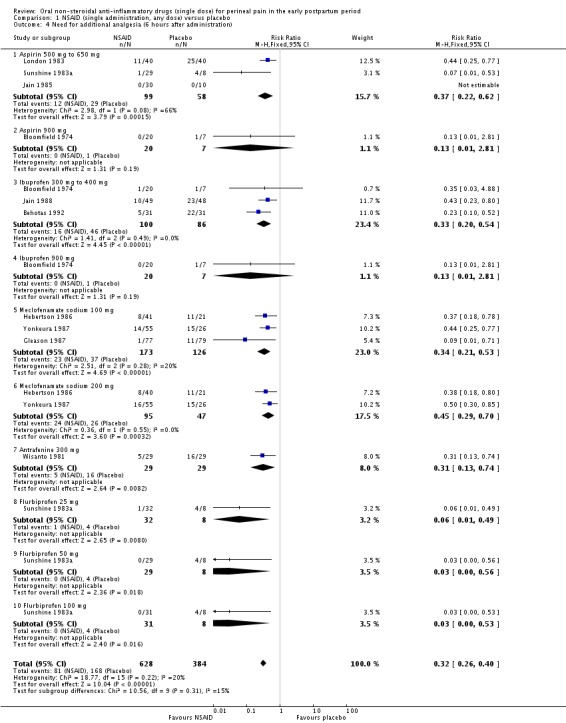
Comparison 1 NSAID (single administration, any dose) versus placebo, Outcome 4 Need for additional analgesia (6 hours after administration).
Figure 6.
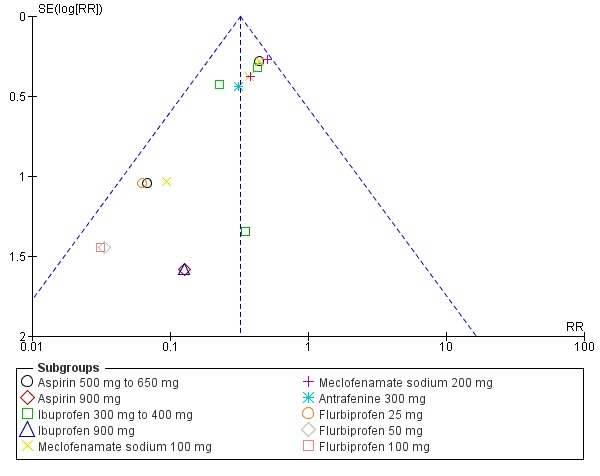
Funnel plot of comparison: 1 NSAID (single administration, any dose) versus placebo, outcome: 1.4 Need for additional analgesia (6 hours after administration).
Maternal adverse effects
The RR for maternal drug adverse effects at four hours post‐administration could not be estimated as no adverse effects were observed in either the NSAID or the placebo groups in the one study (with two treatment arms) reporting at this follow‐up time (Analysis 1.5); the quality of the evidence for this outcome was low, with downgrading decisions due to imprecision (small sample size and no events).
Analysis 1.5.
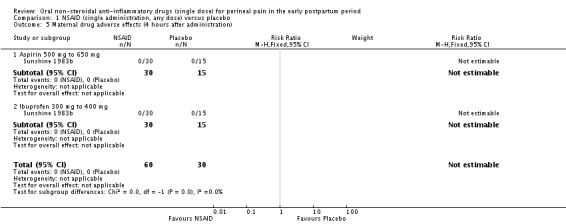
Comparison 1 NSAID (single administration, any dose) versus placebo, Outcome 5 Maternal drug adverse effects (4 hours after administration).
At six hours after drug administration, six of the 17 comparisons (a NSAID versus placebo) across 13 studies reported adverse effects (Analysis 1.6). These were drowsiness (n = 5), abdominal discomfort (n = 2), weakness (n = 1), dizziness (n = 2), headache (n = 2), moderate epigastralgia (n = 1) for the NSAID groups, and drowsiness (n = 2), light headed (n = 1), nausea (n = 1), backache (n = 1), dizziness (n = 1) and epigastric pain (n = 1) for the placebo group. In two studies that reported adverse effects (Bloomfield 1967; Daftary 1980), the specific adverse effects were not stated. There was no difference in overall adverse effects six hours post‐administration (risk ratio (RR) 1.38, 95%CI 0.71 to 2.70, 13 studies, 1388 participants), but the quality of the evidence (GRADE) was very low due to the small number of events, inconsistency and risk of bias (Table 1). A visual inspection of the funnel plot for this outcome (Figure 7) suggests that there is no publication bias.
Analysis 1.6.
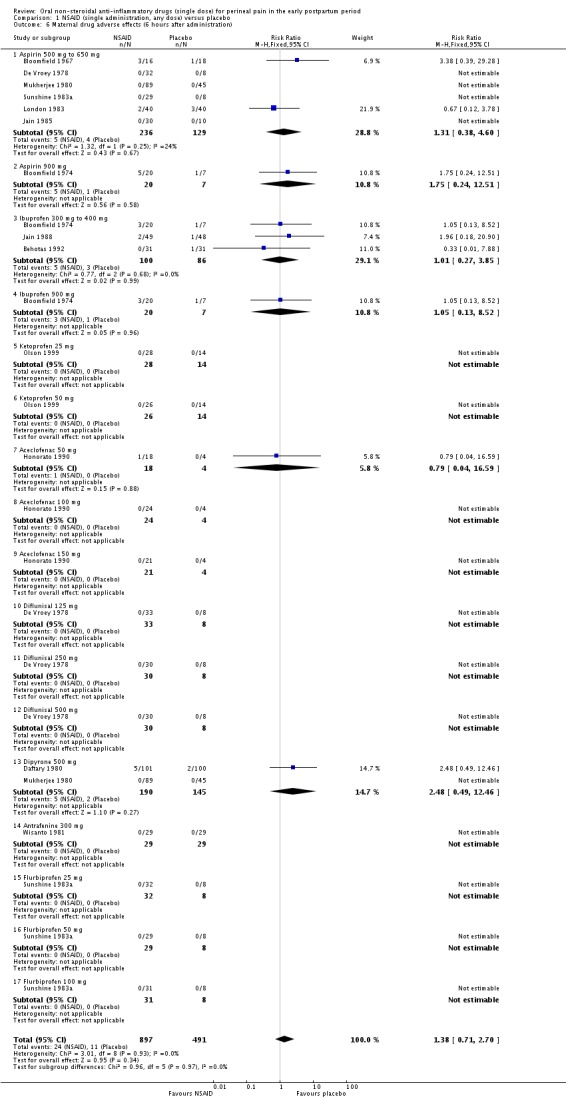
Comparison 1 NSAID (single administration, any dose) versus placebo, Outcome 6 Maternal drug adverse effects (6 hours after administration).
Figure 7.
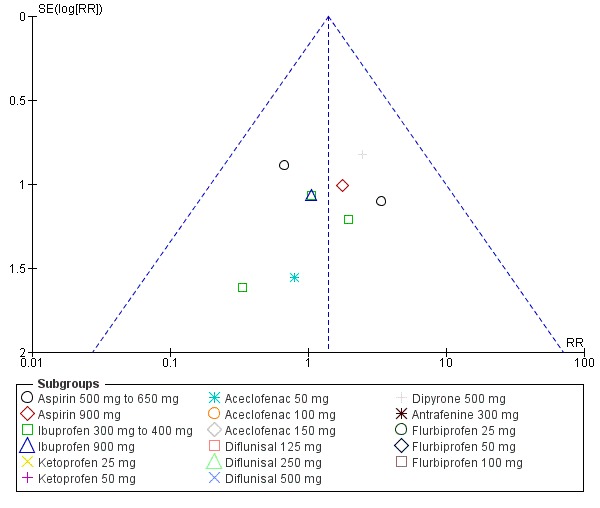
Funnel plot of comparison: 1 NSAID (single administration, any dose) versus placebo, outcome: 1.6 Maternal drug adverse effects (6 hours after administration).
Neonatal adverse effects
Neonatal drug adverse effects were not reported in any of the included studies.
Secondary outcomes
None of the studies assessed any of the reviews pre‐specified secondary outcomes.
Any NSAID versus paracetamol
Primary outcomes
Adequate pain relief
Women who received any NSAID were more likely to report adequate pain relief four hours after drug administration than women who received paracetamol (RR 1.54, 95% CI 1.07 to 2.22, three studies, 342 participants, fixed‐effect (Chi2 P = 0.81, I2 = 0%) Analysis 2.1). Only two studies (Movilia 1989; Yscla 1988) examined a NSAID (aceclofenac 100 mg) versus paracetamol six hours after administration. The results of the analysis did not demonstrate a difference in the number of women with adequate pain relief (RR 1.82, 95% CI 0.61 to 5.47, two studies, 99 participants, random‐effects (Tau2 = 0.38, Chi2 P = 0.12, I2 = 59%) Analysis 2.2).
Analysis 2.1.
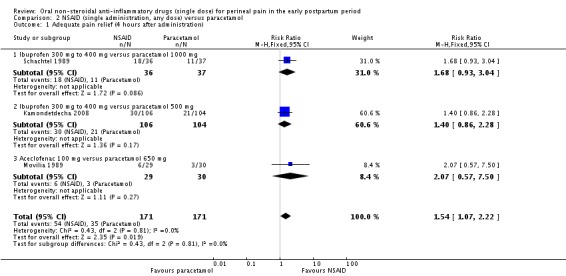
Comparison 2 NSAID (single administration, any dose) versus paracetamol, Outcome 1 Adequate pain relief (4 hours after administration).
Analysis 2.2.
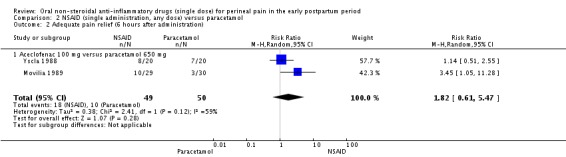
Comparison 2 NSAID (single administration, any dose) versus paracetamol, Outcome 2 Adequate pain relief (6 hours after administration).
Additional analgesia
One study (Schachtel 1989) assessed the need for additional analgesia four hours after NSAID (ibuprofen) administration compared with paracetamol (1000 mg). The analysis demonstrated no statistically significant difference between the two drugs (RR 0.55, 95% CI 0.27 to 1.13, 73 participants, Analysis 2.3). Another study (Behotas 1992) examined the need for additional analgesia six hours after NSAID (ibuprofen) administration compared with paracetamol (1000 mg). The results showed that women in the NSAID group were less likely to need any additional analgesia than women in the paracetamol group (RR 0.28, 95% CI 0.12 to 0.67, 59 participants, Analysis 2.4).
Analysis 2.3.
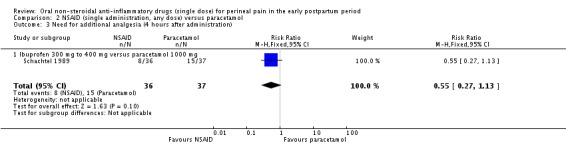
Comparison 2 NSAID (single administration, any dose) versus paracetamol, Outcome 3 Need for additional analgesia (4 hours after administration).
Analysis 2.4.
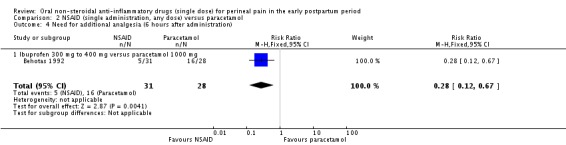
Comparison 2 NSAID (single administration, any dose) versus paracetamol, Outcome 4 Need for additional analgesia (6 hours after administration).
Maternal adverse effects
No maternal adverse drugs adverse effects were reported in the one study (Kamondetdecha 2008) that reported this outcome at four hours after drug administration (Analysis 2.5). Six hours post‐administration, two of three studies reported the following maternal drug adverse effects; pruritis (n = 1) for the NSAID group and sleepiness (n = 1) for the paracetamol group (Analysis 2.6) and there was no difference in overall adverse effects between the groups (risk ratio (RR) 0.74, 95% CI 0.27 to 2.08, three studies, 300 participants, fixed‐effect (Chi2 P = 0.82, I2 = 0%).
Analysis 2.5.
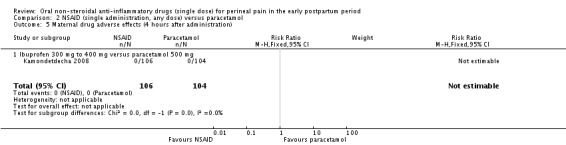
Comparison 2 NSAID (single administration, any dose) versus paracetamol, Outcome 5 Maternal drug adverse effects (4 hours after administration).
Analysis 2.6.
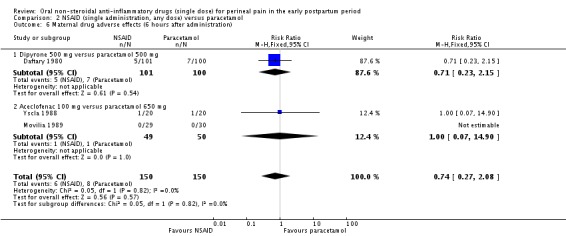
Comparison 2 NSAID (single administration, any dose) versus paracetamol, Outcome 6 Maternal drug adverse effects (6 hours after administration).
Neonatal adverse effects
Neonatal drug adverse effects were not reported in any of the included studies.
Secondary outcomes
None of the studies assessed any of the reviews pre‐specified secondary outcomes.
Any NSAID versus another NSAID
Primary outcomes
Adequate pain relief
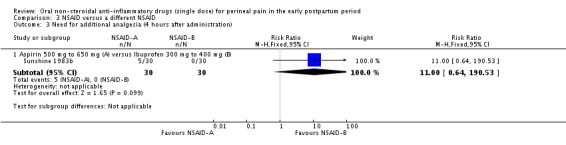
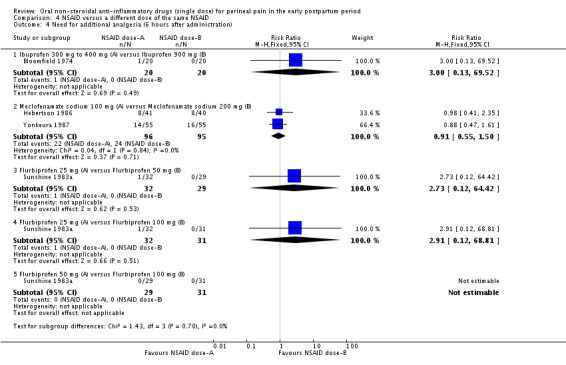
Analysis comparing the effectiveness of different NSAIDs in providing adequate pain relief (Analysis 3.1; Analysis 3.2), and subgroup analysis comparing different doses of the same NSAID (Analysis 4.1; Analysis 4.2), indicated no difference between NSAIDs in terms of efficacy. Even though comparisons between different NSAIDs did not show statistical differences, the direction of effect was in favour of aspirin when compared to diflunisal, in favour of diclofenac when compared to aspirin, in favour of etodolac when compared to aspirin, in favour of dipyrone when compared to aspirin, in favour of ibuprofen when compared to aspirin at four hours but not at six hours, and in favour of flurbiprofen when compared to aspirin except at a lower dose (25 mg) (Analysis 3.1; Analysis 3.2).
Analysis 3.1.
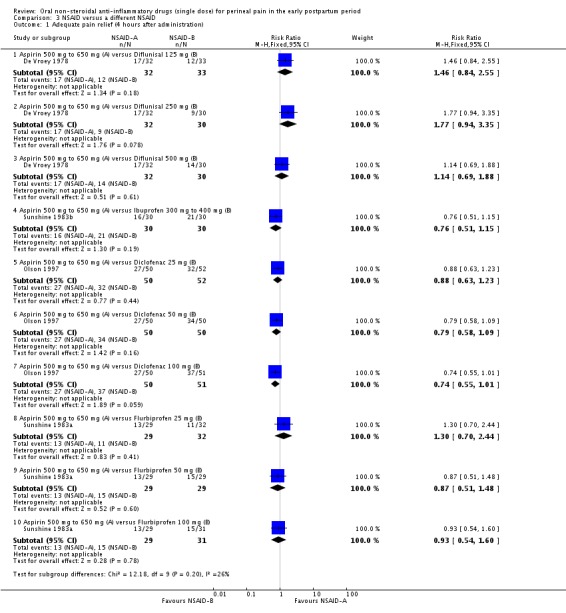
Comparison 3 NSAID versus a different NSAID, Outcome 1 Adequate pain relief (4 hours after administration).
Analysis 3.2.
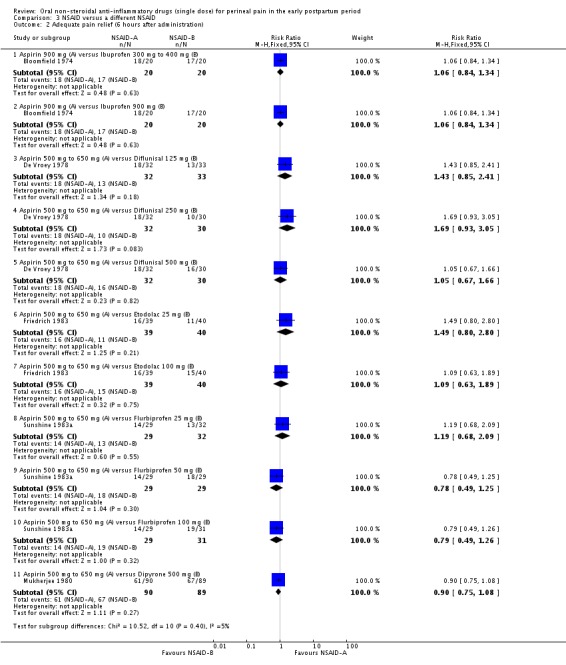
Comparison 3 NSAID versus a different NSAID, Outcome 2 Adequate pain relief (6 hours after administration).
Analysis 4.1.
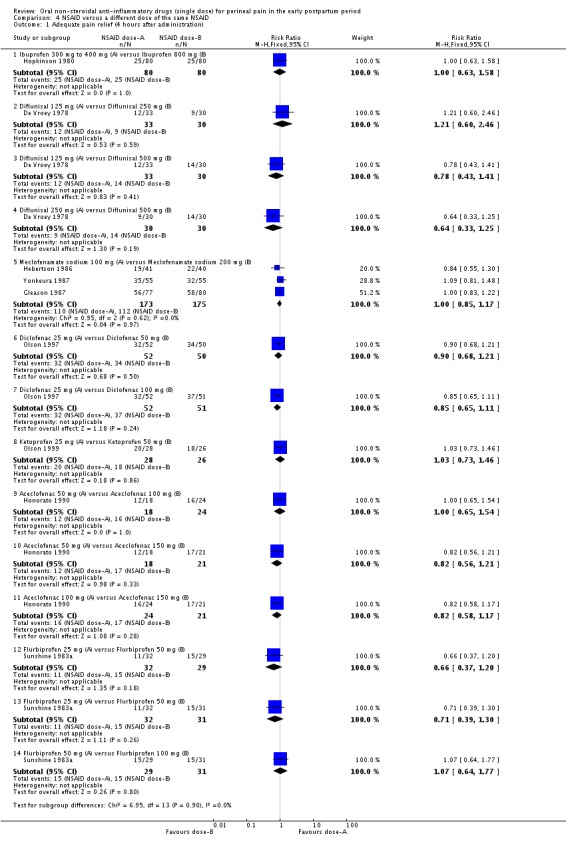
Comparison 4 NSAID versus a different dose of the same NSAID, Outcome 1 Adequate pain relief (4 hours after administration).
Analysis 4.2.
Comparison 4 NSAID versus a different dose of the same NSAID, Outcome 2 Adequate pain relief (6 hours after administration).
Similarly, the different doses of the same NSAID that were investigated were equally effective, with the exception of fenoprofen 50 mg providing adequate pain relief to more women than fenoprofen 100 mg six hours after administration (Laska 1981). All but one comparison showed no difference, but the direction of effect in the included studies was in favour of a lower dose of diflunisal (125 mg) compared to a higher dose (250 mg or 500 mg), in favour of a higher dose of diclofenac (50 mg or 100 mg) versus a lower dose (25 mg), in favour of flurbiprofen 50 mg or 100 mg versus 25 mg, in favour of aceclofenac 150 mg versus 50 mg or 100 mg, in favour of etodolac 100 mg versus 25 mg, in favour of a higher dose of fenoprofen (25 mg, 50 mg, 100 mg, 200 mg, 300 mg) versus a lower dose of fenoprofen (12.5 mg, 25 mg, 50 mg). In contrast, there was no/minimal direction of effect between ibuprofen 300 mg to 400 mg and ibuprofen 800 mg, meclofenamate sodium 100 mg and 200 mg, aceclofenac 50 mg and 100 mg, ketoprofen 25 mg and 50 mg, flurbiprofen 50 mg and 100 mg, fenoprofen 25 mg and 50 mg, and between fenoprofen 100 mg, 200 mg and 300 mg (Analysis 4.1; Analysis 4.2). Suhrabi 2013 was not included in the meta‐analysis as it did not report any of the review's pre‐specified outcome measures, but only reported pain intensity scores four hours post‐administration on a 10 cm visual analogue scale. Using this measure of pain, no difference between celecoxib 100 mg (mean 2.57, standard deviation (SD) 1.4) and ibuprofen 400 mg (mean 2.7, SD 1.4) was found.
Additional analgesia
The need for additional analgesia did not significantly differ between the different NSAID groups (Analysis 3.3; Analysis 3.4) or between groups examining different doses of the same NSAID (Analysis 4.3; Analysis 4.4).
Analysis 3.3.
Comparison 3 NSAID versus a different NSAID, Outcome 3 Need for additional analgesia (4 hours after administration).
Analysis 3.4.
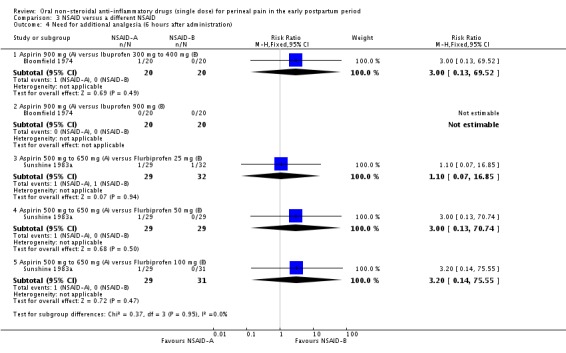
Comparison 3 NSAID versus a different NSAID, Outcome 4 Need for additional analgesia (6 hours after administration).
Analysis 4.3.
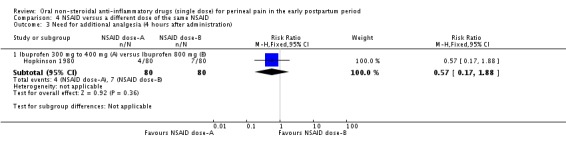
Comparison 4 NSAID versus a different dose of the same NSAID, Outcome 3 Need for additional analgesia (4 hours after administration).
Analysis 4.4.
Comparison 4 NSAID versus a different dose of the same NSAID, Outcome 4 Need for additional analgesia (6 hours after administration).
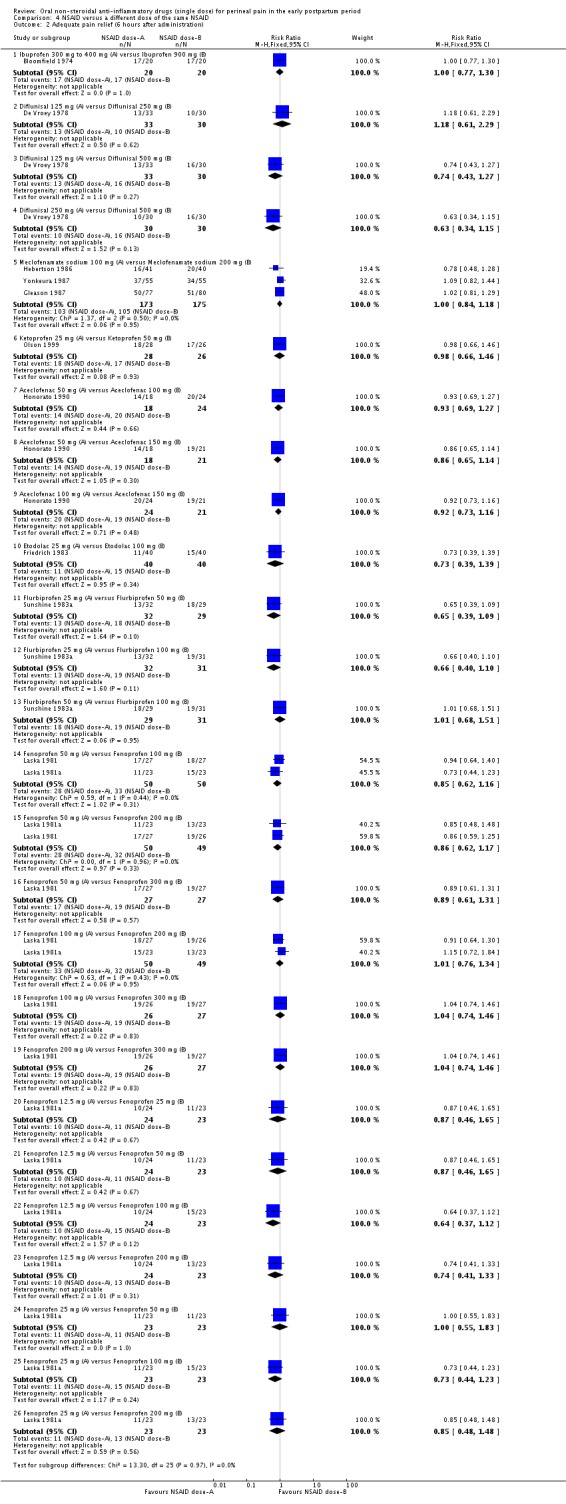
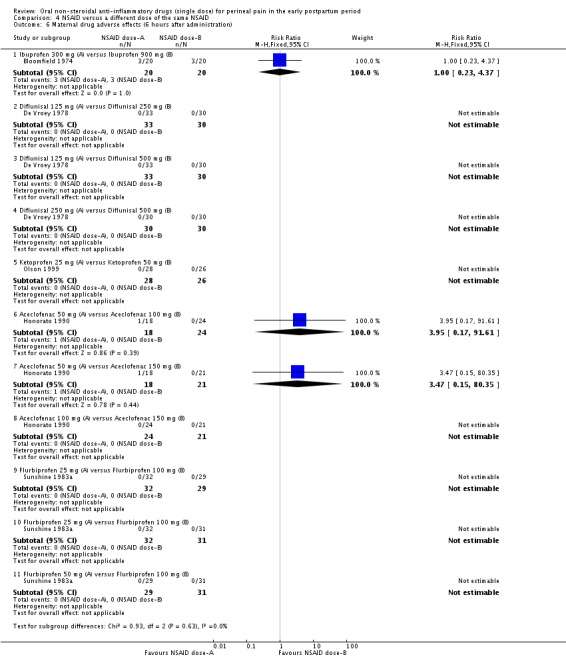
Maternal adverse effects
No differences in maternal drug adverse effects were found between the different NSAID groups (Analysis 3.5; Analysis 3.6), and between doses with respect to maternal drug adverse effects (Analysis 4.5; Analysis 4.6), but this may be due to a lack of power in the included studies as reported adverse outcomes were rare events and not all studies assessed adverse outcomes.
Analysis 3.5.
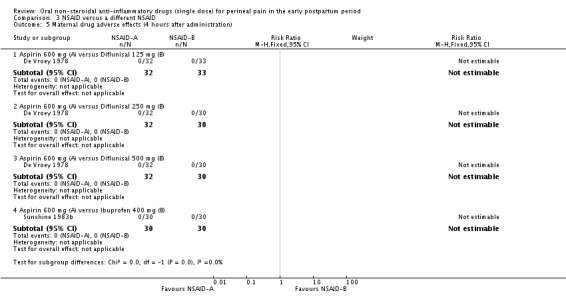
Comparison 3 NSAID versus a different NSAID, Outcome 5 Maternal drug adverse effects (4 hours after administration).
Analysis 3.6.
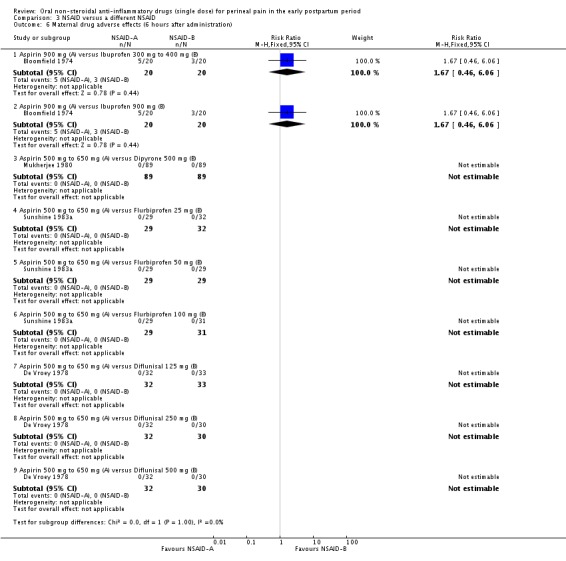
Comparison 3 NSAID versus a different NSAID, Outcome 6 Maternal drug adverse effects (6 hours after administration).
Analysis 4.5.
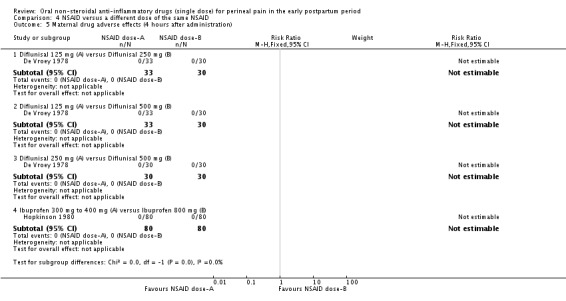
Comparison 4 NSAID versus a different dose of the same NSAID, Outcome 5 Maternal drug adverse effects (4 hours after administration).
Analysis 4.6.
Comparison 4 NSAID versus a different dose of the same NSAID, Outcome 6 Maternal drug adverse effects (6 hours after administration).
Neonatal adverse effects
Neonatal drug adverse effects were not reported in any of the included studies.
Secondary outcomes
None of the studies assessed any of the pre‐specified secondary outcomes.
Sensitivity analysis
Where appropriate, we carried out sensitivity analysis for primary outcomes of this review to examine the effect of trial quality by excluding trials that we judged to be at a high risk of bias for any of the risk of bias domains assessed. Sensitivity analyses for comparison 1 (NSAID versus placebo) and comparison 4 (NSAID versus a different dose of the same NSAID) did not make any difference to the results. The other comparisons (comparisons 2 and 3) did not include studies rated high risk of bias for any domain.
Discussion
Summary of main results
This review involved 4181 women with perineal pain in the early postpartum period, mostly following episiotomy, of whom 2642 received a non‐steroidal anti‐inflammatory drugs (NSAIDs) and 1539 were given paracetamol or placebo. Aspirin 500 mg to 650 mg was the most studied NSAID/dose in the included studies (nine studies), followed by ibuprofen (six studies), while many other NSAIDs were only examined in one study.
Any NSAID was more effective at providing adequate pain relief than placebo at four and six hours for women who sustained perineal trauma during childbirth. However, the quality of the evidence (GRADE) was low and very low, respectively, at these time‐points (Table 1). NSAIDs were also more effective at providing adequate pain relief than paracetamol at four hours. There was no difference in effectiveness between the different NSAIDS or the different doses of a NSAID examined in the included studies. For example, ibuprofen 300 mg to 400 mg was equally effective in relieving perineal pain in the early postpartum period as ibuprofen 800 mg to 900 mg at four and at six hours after drug administration. Women who received a NSAID were also less likely to need additional analgesia, with the quality of the evidence (GRADE) being low for this outcome, at both four‐hour and six‐hour follow‐up (Table 1). Maternal adverse effects were rare in both the NSAID group and the placebo or paracetamol group. In the studies that reported adverse effects, more than one adverse effect was reported in the aspirin, ibuprofen and dipyrone groups. Fewer adverse effects were reported for ibuprofen compared to aspirin, which, together with the findings that seem to favour ibuprofen in providing adequate pain relief and requiring less additional analgesia (although this result was not statistically significant), may indicate recommending, clinically, the use of ibuprofen over aspirin. Moreover, aspirin is best avoided during breastfeeding (LacMed 2015), although the compatibility with breastfeeding was not examined in the studies included in this review (all of the included studies excluded women who were breastfeeding). An equal number of adverse effects was reported at a lower dose of ibuprofen (300 mg to 400 mg) and a higher dose (800 mg), but their effectiveness in providing pain relief was also equivalent. Information on adverse effects of diclofenac, another commonly used NSAID, was not present in the included studies, but more women in the diclofenac group reported adequate pain relief than women in the aspirin group.
Only five studies compared a NSAID with paracetamol. NSAIDs were more effective than paracetamol four hours after administration, but not six hours post‐administration, although less women needed additional analgesia at six hours in the NSAID group. This review only examined the effectiveness of a single dose while in practice more than one dose is often given and women might receive a combination of paracetamol and a NSAID. The findings seem to support the practice of 'stepping up the pain ladder' to a NSAID if paracetamol does not provide sufficient pain relief or providing multimodal pain relief (Berry 2001), combining paracetamol and a NSAID.
The studies in this review did not examine the compatibility of NSAIDs with breastfeeding and did not report on neonatal adverse effects. In general, NSAIDs should be used with caution when breastfeeding and paracetamol is the preferred choice of analgesic for breastfeeding women (BNF 2014). If a NSAID is required, of the NSAIDs that were examined in the studies included in this review, ibuprofen, fenoprofen, diclofenac sodium would be preferred when breastfeeding, while diflunisal, aceclofenac, aspirin, celecoxib, etodolac, flurbiprofen, ketoprofen, dipyrone, meclofenamate sodium should be avoided (BNF 2014; LacMed 2015).
Overall completeness and applicability of evidence
Only three of the 14 pre‐specified outcomes were examined in the included studies. Although NSAIDs seem to provide better pain relief than placebo four and six hours postpartum, there is no evidence available to evaluate the effect of NSAIDs on neonatal outcomes since the studies in this review only included non‐breastfeeding mothers. In addition, there are no data on outcomes, such as disability and depression, that can be related to experiencing pain. Other pre‐specified outcomes that are important for women and service providers, including prolonged hospitalisation and re‐hospitalisation due to perineal pain, were also not examined in the included studies.
Quality of the evidence
The majority of the included studies did not report details on how they generated the random sequence, whether allocation was concealed, and whether the outcome assessment was blinded. Only three studies were published after the year 2000 and most included studies were conducted in the 1980s or before.Trial registries were only introduced in the past two decades; for example, ClinicalTrials.gov was launched in the year 2000. Moreover, the first CONSORT (Consolidated Standards of Reporting Trials) statement to improve reporting in clinical trials was only published in 1996 (Begg 1996). This may explain the lack of reporting on these key methodological aspects in the studies included in this review.
The GRADE quality of evidence was assessed for the main comparison (NSAID versus placebo) for all primary outcomes at four‐ and six‐hour follow‐up (Table 1). The quality of evidence for findings concerning the outcome 'adequate pain relief' was low and very low at four‐ and six‐hour follow‐up, respectively due to high risk of bias in some included studies, suspected publication bias and inconsistency in findings between individual studies. Findings for the outcome 'need for additional analgesia' were based on low‐quality evidence because of high risk of bias in one of the studies and inconsistency in the results. High risk of bias in two studies, inconsistency, and the presence of only few events, led to downgrading of the quality of evidence for maternal adverse effects to very low.
Potential biases in the review process
Assymmetry in the funnel plots (for the outcome adequate pain relief), with a gap in the bottom left corner of the plots (Figure 4; Figure 5), suggests that additional smaller studies comparing the use of a NSAID versus placebo may not have been published, which may lead to an overestimation of the intervention effect (Higgins 2011). In addition, one trial registration report identified in the search strategy of the review included a letter from the authors confirming that their study would not be published (McCallum 1991). The funnel plots for the outcomes additional analgesia (Figure 6) and adverse effects (Figure 7) at six hours post‐administration were more symmetrical, but did still not show an equal spread across the triangle.
Agreements and disagreements with other studies or reviews
The results of this review are in agreement with a Cochrane review assessing analgesia for relief of pain due to uterine cramping/involution after birth (Deussen 2011). This review found that NSAIDs were significantly more effective than placebo in improving pain relief based on three studies including 204 women, but adverse effects reported were similar in the placebo and control groups.
Authors' conclusions
The findings of this review need to be interpreted in the context of the quality of evidence and risk of bias of the included studies, which was unclear for many studies because of a lack of reporting on the random sequence generation, allocation concealment and blinding of the outcome assessment.
Non‐steroidal anti‐inflammatory drugs (NSAIDs) are effective analgesics for women with perineal pain postpartum. Although there is limited evidence, maternal adverse effects seem rare. The different NSAIDs (examined in the included studies) are all effective compared to placebo and no particular NSAIDs were more effective than others; the choice of NSAIDs may thus be guided by its compatibility with breastfeeding, which was not examined in this review as all trials excluded women who were breastfeeding. However, none of the studies included in this review reported on neonatal adverse effects or any data of the secondary outcomes of this review. The dosages that were compared in the included studies did not seem to significantly impact on the effectiveness of a NSAID. Although NSAIDs may be more effective than paracetamol, the evidence is sparse and inconclusive. Other analgesia may also further be considered, but this is beyond the remit of this review and will be examined in further reviews in this series of reviews on pain relief for perineal pain in the early postpartum period.
Future studies may examine NSAIDs' adverse‐effects profile including neonatal adverse effects and the compatibility of NSAIDs with breastfeeding, and assess other important secondary outcomes of this review including (re‐)hospitalisation, maternal disability and maternal views. Moreover, studies mostly included women who had episiotomies. Future research needs to be extended to women with and without perineal trauma, including perineal tears. Finally, the small size of the studies and poor reporting limits the strength of the results of this review. Methodologically high‐quality studies should be conducted to further assess the efficacy of NSAIDs versus paracetamol and the efficacy of multimodal treatments.
Acknowledgements
A Cochrane Fellowship was awarded by the Health Research Board Ireland to F Wuytack to support the conduct of this review.
As part of the pre‐publication editorial process, this review has been commented on by five peers (an editor and four referees who are external to the editorial team), members of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Search terms
episiotomy OR (perineal OR perineum) AND (tear OR tears OR pain)
Data and analyses
Comparison 1.
NSAID (single administration, any dose) versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adequate pain relief (4 hours after administration) | 10 | 1573 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.91 [1.64, 2.23] |
| 1.1 Aspirin 500 mg to 650 mg | 4 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.69 [1.41, 5.10] |
| 1.2 Ibuprofen 300 mg to 400 mg | 3 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.64 [1.62, 4.30] |
| 1.3 Ibuprofen 800 mg | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.87, 3.87] |
| 1.4 Diclofenac 25 mg | 1 | 65 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.86, 4.65] |
| 1.5 Diclofenac 50 mg | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.96, 5.11] |
| 1.6 Diclofenac 100 mg | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.36 [1.03, 5.42] |
| 1.7 Ketoprofen 25 mg | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.33 [1.19, 9.34] |
| 1.8 Ketoprofen 50 mg | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.23 [1.15, 9.10] |
| 1.9 Meclofenamate sodium 100 mg | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [1.10, 1.82] |
| 1.10 Meclofenamate sodium 200 mg | 3 | 262 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [1.10, 1.83] |
| 1.11 Diflunisal 125 mg | 1 | 41 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.44, 19.22] |
| 1.12 Diflunisal 250 mg | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.4 [0.35, 16.26] |
| 1.13 Diflunisal 500 mg | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.73 [0.57, 24.29] |
| 1.14 Flurbiprofen 25 mg | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.75 [0.41, 18.29] |
| 1.15 Flurbiprofen 50 mg | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.14 [0.64, 26.76] |
| 1.16 Flurbiprofen 100 mg | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.87 [0.60, 25.09] |
| 2 Adequate pain relief (6 hours after administration) | 17 | 2079 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [1.69, 2.17] |
| 2.1 Aspirin 500 mg to 650 mg | 7 | 416 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [1.37, 2.24] |
| 2.2 Aspirin 900 mg | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.15 [0.97, 10.26] |
| 2.3 Ibuprofen 300 mg to 400 mg | 2 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.30, 3.32] |
| 2.4 Ibuprofen 900 mg | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.98 [0.91, 9.74] |
| 2.5 Ketoprofen 25 mg | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [1.06, 8.49] |
| 2.6 Ketoprofen 50 mg | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.05 [1.08, 8.64] |
| 2.7 Meclofenamate sodium 100 mg | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [1.05, 1.76] |
| 2.8 Meclofenamate sodium 200 mg | 3 | 262 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.07, 1.83] |
| 2.9 Diflunisal 125 mg | 1 | 41 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.15 [0.48, 20.69] |
| 2.10 Diflunisal 250 mg | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.67 [0.40, 17.86] |
| 2.11 Diflunisal 500 mg | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.27 [0.66, 27.51] |
| 2.12 Dipyrone 500 mg | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [1.44, 3.39] |
| 2.13 Aceclofenac 50 mg | 1 | 22 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.56 [0.57, 4.27] |
| 2.14 Aceclofenac 100 mg | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.62, 4.51] |
| 2.15 Aceclofenac 150 mg | 1 | 25 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.81 [0.67, 4.87] |
| 2.16 Etodolac 25 mg | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.34, 2.33] |
| 2.17 Etodolac 100 mg | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.49, 3.02] |
| 2.18 Antrafenine 300 mg | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.33 [1.74, 16.36] |
| 2.19 Flurbiprofen 25 mg | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.50, 21.31] |
| 2.20 Flurbiprofen 50 mg | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.97 [0.78, 31.75] |
| 2.21 Flurbiprofen 100 mg | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.90 [0.77, 31.33] |
| 2.22 Fenoprofen 12.5 mg | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.08 [0.34, 12.80] |
| 2.23 Fenoprofen 25 mg | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [0.39, 14.53] |
| 2.24 Fenoprofen 50 mg | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.38 [0.93, 12.26] |
| 2.25 Fenoprofen 100 mg | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.95 [1.10, 14.19] |
| 2.26 Fenoprofen 200 mg | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.95 [1.10, 14.19] |
| 2.27 Fenoprofen 300 mg | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.93 [0.79, 30.74] |
| 3 Need for additional analgesia (4 hours after administration) | 4 | 486 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.26, 0.58] |
| 3.1 Aspirin 500 mg to 650 mg | 2 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.23, 0.93] |
| 3.2 Ibuprofen 300 mg to 400 mg | 3 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.18, 0.56] |
| 3.3 Ibuprofen 800 mg | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.19, 1.36] |
| 4 Need for additional analgesia (6 hours after administration) | 10 | 1012 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.26, 0.40] |
| 4.1 Aspirin 500 mg to 650 mg | 3 | 157 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.22, 0.62] |
| 4.2 Aspirin 900 mg | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.81] |
| 4.3 Ibuprofen 300 mg to 400 mg | 3 | 186 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.20, 0.54] |
| 4.4 Ibuprofen 900 mg | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.81] |
| 4.5 Meclofenamate sodium 100 mg | 3 | 299 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.21, 0.53] |
| 4.6 Meclofenamate sodium 200 mg | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.29, 0.70] |
| 4.7 Antrafenine 300 mg | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.13, 0.74] |
| 4.8 Flurbiprofen 25 mg | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.01, 0.49] |
| 4.9 Flurbiprofen 50 mg | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.56] |
| 4.10 Flurbiprofen 100 mg | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.53] |
| 5 Maternal drug adverse effects (4 hours after administration) | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Aspirin 500 mg to 650 mg | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Ibuprofen 300 mg to 400 mg | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Maternal drug adverse effects (6 hours after administration) | 13 | 1388 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.71, 2.70] |
| 6.1 Aspirin 500 mg to 650 mg | 6 | 365 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.38, 4.60] |
| 6.2 Aspirin 900 mg | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.24, 12.51] |
| 6.3 Ibuprofen 300 mg to 400 mg | 3 | 186 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.27, 3.85] |
| 6.4 Ibuprofen 900 mg | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.13, 8.52] |
| 6.5 Ketoprofen 25 mg | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.6 Ketoprofen 50 mg | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.7 Aceclofenac 50 mg | 1 | 22 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.04, 16.59] |
| 6.8 Aceclofenac 100 mg | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.9 Aceclofenac 150 mg | 1 | 25 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.10 Diflunisal 125 mg | 1 | 41 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.11 Diflunisal 250 mg | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.12 Diflunisal 500 mg | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.13 Dipyrone 500 mg | 2 | 335 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.48 [0.49, 12.46] |
| 6.14 Antrafenine 300 mg | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.15 Flurbiprofen 25 mg | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.16 Flurbiprofen 50 mg | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.17 Flurbiprofen 100 mg | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2.
NSAID (single administration, any dose) versus paracetamol
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adequate pain relief (4 hours after administration) | 3 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [1.07, 2.22] |
| 1.1 Ibuprofen 300 mg to 400 mg versus paracetamol 1000 mg | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.93, 3.04] |
| 1.2 Ibuprofen 300 mg to 400 mg versus paracetamol 500 mg | 1 | 210 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.86, 2.28] |
| 1.3 Aceclofenac 100 mg versus paracetamol 650 mg | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.07 [0.57, 7.50] |
| 2 Adequate pain relief (6 hours after administration) | 2 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.61, 5.47] |
| 2.1 Aceclofenac 100 mg versus paracetamol 650 mg | 2 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.61, 5.47] |
| 3 Need for additional analgesia (4 hours after administration) | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.27, 1.13] |
| 3.1 Ibuprofen 300 mg to 400 mg versus paracetamol 1000 mg | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.27, 1.13] |
| 4 Need for additional analgesia (6 hours after administration) | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.12, 0.67] |
| 4.1 Ibuprofen 300 mg to 400 mg versus paracetamol 1000 mg | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.12, 0.67] |
| 5 Maternal drug adverse effects (4 hours after administration) | 1 | 210 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Ibuprofen 300 mg to 400 mg versus paracetamol 500 mg | 1 | 210 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Maternal drug adverse effects (6 hours after administration) | 3 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.27, 2.08] |
| 6.1 Dipyrone 500 mg versus paracetamol 500 mg | 1 | 201 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.23, 2.15] |
| 6.2 Aceclofenac 100 mg versus paracetamol 650 mg | 2 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 14.90] |
Comparison 3.
NSAID versus a different NSAID
Comparison 4.
NSAID versus a different dose of the same NSAID
What's new
Last assessed as up‐to‐date: 31 March 2016.
| Date | Event | Description |
|---|---|---|
| 22 October 2016 | Amended | Correction of a typographical error in the plain language summary. |
Differences between protocol and review
We have used GRADE to assess the quality of the body of the evidence and produced Table 1. This was not pre‐specified in our protocol (Wuytack 2014).
We were unable to carry out the following pre‐specified methods. Subgroup analyses (Protocol) Primary outcome: “Neonatal drug adverse effects, e.g. nausea, vomiting, sedation, constipation, diarrhoea, drowsy, sleepy, psychological”.
This outcome was not measured in any of the included studies.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Multi‐arm RCT ‐ 3 groups. | |
| Participants | Women whose post‐episiotomy pain warranted analgesia, in Hospital ‘Sainte‐Antonie’, Paris. Participants were followed up on day‐1 postpartum. Women with hepatic or renal malfunction, a previous duodenal ulcer and those whose condition contra‐indicated treatment with NSAIDs, were excluded. |
|
| Interventions | Intervention: ibuprofen 400 mg (N = 31). Comparison: paracetamol 1 g (N = 28) and placebo (N = 31). |
|
| Outcomes |
4‐ and 6‐hourly pain data were only available for ibuprofen and not for the comparator treatments. Need for additional analgesia data (6 hours) were the only outcome data available for inclusion in the review. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Identical white containers only – insufficient information as to whether these were sequentially numbered and sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 90 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Participants were similar in terms of geographical background, socio‐professional status and their overall clinical picture. |
| Methods | Multi‐arm RCT ‐ 5 groups. | |
| Participants | All women having a painful mediolateral episiotomy, an uncomplicated labour and delivery, and consenting to take an investigational drug in the obstetric service of Cincinnati General Hospital. The study was conducted between December 7th 1965 and April 22nd 1966. Women who were breastfeeding, were under age 18 and were known to have ASA sensitivity were excluded. |
|
| Interventions | Intervention: chlorphenesin 400 mg (N = 16); chlorphenesin 800 mg (N = 16); chlorphenesin 400 mg + ASA 300 mg (N = 18) and ASA 600 mg (N = 16). Comparison: placebo (N = 18). |
|
| Outcomes |
ASA 300 mg were the only data used in the review as the other drug treatment regimens were not NSAIDs. Pain intensity was measured immediately before treatment and then hourly for 6 hours after administration. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned under controlled conditions but does not state how sequence was generated. |
| Allocation concealment (selection bias) | Low risk | Coded medication; identical black capsules. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind; code could be broken without revealing the treatment received by other patients. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5% attrition rate (1 of 16 women) in the ASA 600 mg group; 0% attrition in the placebo group (N = 18). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Unclear risk | Potential carry‐over of effect of intrapartum analgesia. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | An homogenous population of postpartum women with moderate to very severe episiotomy pain (mediolateral or midline incision) within 48 hours of an uncomplicated delivery at the University of Cincinnati Medical Centre; homogenous population of postpartum women. Women who were unmarried, < 18 years old (but included if married and < 18 years), with history of aspirin allergy, given analgesics or sedatives, or other psychotropic drugs in the previous 6 hours, breastfeeding and with known drug dependence were excluded. |
|
| Interventions | Intervention: ibuprofen 300 mg (N = 20); ibuprofen 900 mg (N = 20) and aspirin 900 mg (N = 20). Comparison: lactose placebo (N = 20). |
|
| Outcomes |
Only 6‐hour data available in extractable format. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Low risk | All treatments were in the form of film‐coated tablets identical in appearance and taste and pre‐packaged in coded number individual dose‐vials. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 80 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Unclear risk | Some baseline differences between group characteristics (e.g. weight higher in group receiving ibuprofen 900 mg and more unmarried in ibuprofen 300 mg group). Chance occurrences but with an uncertain influence on the results. |
| Methods | Multi‐arm RCT – 3 groups. | |
| Participants | Postpartum women, reporting moderate and severe pain in Noerosjee Wadia Hospital, Bombay, India. Concurrent therapy with hypnotic‐sedative drugs was not permitted from 23.00 the previous night until the end of the evaluation. |
|
| Interventions | Intervention: dipyrone 500 mg (N = 101). Comparison: placebo (N = 98) and paracetamol 500 mg (N = 100). |
|
| Outcomes |
Pain relief was evaluated at 30 minutes and hourly intervals thereafter up to 6 hours following therapy; however, we were unable to accurately extract data on pain relief as graphical data only were available; thus side effects data only were extracted and reported in the review. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Low risk | Tablets were identical in appearance and from numbered sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 299 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Participant baseline characteristics were comparable. |
| Methods | Multi‐arm RCT ‐ 5 groups. | |
| Participants | Primiparous women aged between 16‐40 years who had a medio‐lateral episiotomy during the course of an otherwise uncomplicated delivery; delivery within previous 48 hours and complained of moderate to severe pain, at the Department of Obstetrics and Gynaecology of the St. Christiana Clinic, Belgium. | |
| Interventions | Intervention: diflunisal 125 mg (N = 30); diflunisal 250 mg (N = 30); diflunisal 500 mg (N = 30) and aspirin 600 mg (N = 32). Comparison: placebo (N = 31). |
|
| Outcomes |
Pain severity was assessed before drug administration and then at hourly intervals up to 6‐8 hours; 4‐ and 6‐hour data available and extracted separately. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Clear information, including reasons, were provided on 5 exclusions after randomisation and on 3 withdrawals (9%) of the 32 women in the aspirin 600 mg group after treatment. (The attrition rate was 0% for all other groups.) |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None obvious; all women were primiparas with equal distribution, based on initial severity of pain, across groups. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | Women aged between 18 and 34 years with moderate or severe pain following episiotomy, at least 16 hours but no more than 48 hours following induction of anaesthesia, at the Department of Obstetrics and Gynaecology, Barnes Hospital Plaza, Washington Univeristy. Women were excluded if they had current or recent history of gastrointestinal bleeding, peptic ulcer or other gastrointestinal disorders, alcohol or drug abuse, or disorders of the nervous system, kidney, heart or blood, known allergies to aspirin, or aspirin‐like analgesia, conditions likely to interfere with absorption, distribution, metabolism or excretion of drugs, other pain requiring narcotic analgesics, acute dermatitis or other skin lesions, past or present malignancies, taking corticosteroids or other NSAIDs, anticoagulants or other drugs that might interfere with the study medication, experiencing pain due to other conditions or were breastfeeding. |
|
| Interventions | Intervention: aspirin 650 mg (N = 39); etodolac 25 mg (N = 40) and etodolac 100 mg (N = 40). Comparison: placebo (N = 40). |
|
| Outcomes |
Pain assessed at baseline, 30 minutes after and hourly thereafter up to 8 hours; data for 6 hours provided and used in the review as per protocol. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Stated double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 159 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Groups were balanced on demographics and clinical features. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | Women aged 15 years and older with moderate to severe episiotomy pain within 24 hours of an uncomplicated vaginal birth and could read, comprehend and sign a consent form, in a hospital setting in Kansas. Nursing mothers, women with a history of reaction or hypersensitivity to NSAIDs or salicylates or women who had received topical perineal anaesthetic or analgesic, NSAID, sedative or psychotropic medication within 3.5 hours of study entry, were excluded. |
|
| Interventions | Intervention: meclofenamate 100 mg (N = 77); meclofenamate 200 mg (N = 80) and codeine 60 mg (N = 79). Comparison intervention: placebo (N = 79). |
|
| Outcomes |
Pain measured before 1st dose, 30 minutes after and thereafter hourly up to 6 hours. |
|
| Notes | Codeine 60 mg was not considered in the review as not a NSAID. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | Only states each dose was packaged separately. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 327 women selected, 12 (4%) were excluded from the analysis due to protocol violations (taking other analgesic medication during the duration of the study). The attrition rates in the individual groups were: 1 of 81 (1%) in the meclofenamate 200 mg group, 3 of 80 (4%) in the meclofenamate 100 mg group, 3 of 83 (4%) in the placebo group (and 3 of 83 (4%) in the codeine group which was not included in this review). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | The 4 treatment groups did not differ significantly with respect to demographic characteristics. |
| Methods | Multi‐arm RCT– 4 groups. | |
| Participants | Women aged 15 years and older, moderate to severe episiotomy pain and uncomplicated vaginal birth at Latter Day Saints Hospital, Utah. Women with a history of reaction or hyper‐sensitivity to NSAIDs or salicylates, active gastric intestinal disease or other disease and received an analgesic, sedative or psychotropic medication or topical perineal anaesthetic within 3.5 hours of entry into the study, were excluded. |
|
| Interventions | Intervention: meclofenamate sodium 200 mg (N = 40); meclofenamate sodium 100 mg (N = 41) and codeine 60 mg (N = 39). Comparison: placebo (N = 41). |
|
| Outcomes |
Pain intensity was rated just prior to the treatment and together with pain relief was measured at 30 minutes after administration and 1 hourly thereafter up to 6 hours. |
|
| Notes | Codeine 60 mg was not considered in the review as not a NSAID. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random table. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 168 women selected, 7 (4%) were excluded from the analysis due to protocol violations (i.e. had medication within 3.5 hours before study entry). The attrition rates in the individual groups were: 2 of 42 (5%) in the meclofenamate 200 mg group, 1 of 42 (2%) in the meclofenamate 100 mg group, 3 of 42 (7%) in the placebo group (and 1 of 42 (2%) in the codeine group which was not included in this review). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | No differences in the distribution of participants across groups. |
| Methods | Multi‐arm RCT – 4 groups | |
| Participants | Women aged 18‐35 years with intense post‐episiotomy pain requiring analgesia 3 centres; Navarre Teaching Hospital, Pamplona, Spain; Legnano Civil Hospital, Legnano, Italy and Montebelluna Civil Hospital, Montebelluna, Spain. Women suffering little or no pain, who had peptic ulcer, serious liver or kidney failure, puerperal fever or any complication within the puerperium or any serious general disease that could interfere with the results and were already being treated with NSAID agents or systemic steroids, tranquillisers, sedatives, narcotics and/or local anaesthetics, were excluded. Participants were not allowed to take any other drug that might interfere with the results. |
|
| Interventions | Intervention: aceclofenac 50 mg (N = 18); aceclofenac 100 mg (N = 24) and aceclofenac 150 mg (N = 21). Comparison: placebo (N = 13). |
|
| Outcomes |
Degree of pain was measured at baseline, 30 minutes after and hourly thereafter up to 6 hours. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | Suggests only that treatments were prepared so that neither the participant or the investigator could distinguish between the doses. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss of blood sample data in 18 of 45 participants of the four groups (not specified which groups); reasons provided. However, this outcome (serum concentration of aceclofenac) was not included in this review. 0% attrition rate for outcomes included in this review. |
| Selective reporting (reporting bias) | Low risk | Results on the outcome 'overall evaluation' are not provided, but important pain outcome data were all reported. |
| Other bias | Unclear risk | No clear statement on balanced between group characteristics; also less numbers in placebo group. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | Women with moderate or severe post‐episiotomy pain at Abington Memorial Hospital, Pennsylvania. Women with eclampsia and those who had received analgesic drugs within 12 hours prior to study, were excluded. |
|
| Interventions | Intervention: ibuprofen 400 mg (N = 80); ibuprofen 800 mg (N = 80) and propoxyphene 65 mg (N = 81). Comparison: placebo (N = 81). |
|
| Outcomes |
Evaluations of pain were recorded 30 minutes, and hourly thereafter up to 4 hours after treatment administration. |
|
| Notes | Propoxyphene 65 mg was not considered in the review as not a NSAID. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on methods used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Appears to be missing data (drop‐outs or withdrawals) at 2‐, 3‐ and 4‐hour assessments; no clear statement as to reasons in study publication. |
| Selective reporting (reporting bias) | High risk | Side effects not mentioned/reported; no reason provided. |
| Other bias | Low risk | There was no statistically significant differences between any of the groups on baseline parameters or characteristics. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | Postpartum women at least 18 years old who had undergone episiotomy and had at least moderate intensity pain at Tulane Univeristy School of Medicine and Clinical Research Centre, New Orleans. Women who received analgesics or tranquillisers within at least 4 hours of study entry, intended to breastfeed, had a history of convulsive disorders, known peptic ulcer, renal, hepatic or haematological disease or known allergic reactions to NSAIDs, were excluded. |
|
| Interventions | Intervention: aspirin 600 mg (N = 30); indoprofen 50 mg (N = 30); indoprofen 100 mg (N = 30). Comparison: placebo (N = 30). |
|
| Outcomes |
Pain assessed at baseline, 30 minutes after and thereafter through to 5 hours. 5‐hour data were used in the review (considered within 6‐hour time‐frame data). |
|
| Notes | Only aspirin included in the review since indoprofen was withdrawn from the market. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 120 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Demographic data indicated groups were similar in terms of age, race, height, weight and initial pain intensity. |
| Methods | Multi‐arm RCT – 3 groups. | |
| Participants | Women with moderate to severe pain following episiotomy at a clinical research centre, New Orleans. Women with known hypersensitivity to NSAID agents, history of allergy to aspirin, ibuprofen or caffeine, history of asthma, clinically significant renal, hepatic, endocrine, pulmonary, cardiac, neurologic, or cerebral dysfunction or with a history of peptic ulcer disease or gastrointestinal blood loss, uncontrolled diabetes, drug abuse or alcoholism, were excluded. Use of caffeine, anti‐inflammatory agent, tranquilliser or sedative was prohibited during the 4 hours prior to administration of test medication as well as during the study period. |
|
| Interventions | Intervention: caffeine 100 mg + ibuprofen 200 mg (N = 50) and ibuprofen 400 mg (N = 49). Comparison: placebo (N = 48). |
|
| Outcomes |
Pain assessed at baseline and 30 minutes after and thereafter hourly up to 6 hours. Only 6‐hour data used in this review (4‐hour data could not be extracted). |
|
| Notes | Caffeine 100 mg + ibuprofen 200 mg combination therapy not include in the review as not pure NSAID. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule. |
| Allocation concealment (selection bias) | Unclear risk | Supplied in unit dose bottles containing identical tablets; no information if sequentially numbered and sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 161 women selected, 14 (9%) were excluded from the analysis; 11 due to rescue medication before the 2‐hour follow‐up (4 in the ibuprofen 400 mg group, 4 in the placebo group (and 3 in the ibuprofen 200 mg + caffeine group which was not included in this review), 2 due to use of confounding agents and 1 because she was under 18 years old (not specified from which group). Attrition rates could not be calculated due to non‐report of the exact number of participants in each group at the start of the study. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | No statistical differences across groups in terms of demographic variables and baseline pain intensity measures. |
| Methods | Parallel RCT ‐ 2 groups. | |
| Participants | Women with mediolateral episiotomy without a third‐ or fourth‐degree tear after a normal uncomplicated delivery, at term, who had not used any analgesic drugs within 4 hours preceding the study at the King Chulalongkorn Memorial Hospital between June 2006 and November 2006. Women with an allergy to either study drug, a history of drug dependence, regular use of analgesic drugs before or during pregnancy, and any medical condition known to be potentially exacerbated by acetaminophen or NSAIDS, including a history of gastrointestinal ulcer or bleeding, significant renal or liver impairment and asthma, postpartum haemorrhage or any other major postpartum complications, were excluded. |
|
| Interventions | Intervention: ibuprofen 400 mg (N = 106). Comparison: acetaminophen 500 mg (N = 104). |
|
| Outcomes |
An initial pain rating was recorded before participants took the first dose of analgesia and at 1, 2, 3 and 4 hours after. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used; states only "stratified random sampling technique". |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor blind to treatment group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 210 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Treatment groups were similar in demographic data and clinical features; the severity of perineal pain did not differ between the groups before the treatment. |
| Methods | Multi‐arm RCT (2 studies reported in 1 publication; study E1). | |
| Participants | Women with severe pain only, who gave consent, no complicating illness, were not breastfeeding and were expected to tolerate medication well at a maternity hospital, Caracus, Venezuela. | |
| Interventions | Intervention: E1 study: fenoprofen 50 mg (N = 27); fenoprofen 100 mg (N = 27); fenoprofen 200 mg (N = 26) and fenoprofen 300 mg (N = 27). | |
| Outcomes |
Data were obtained at baseline, and 1, 2, 3, 4 and 5 hours after taking the medication. 5‐hour data used in this review (included at 6‐hour time‐frame). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data on withdrawals due to need for rescue medication at < 2 hours not provided (or referred to in results section). |
| Selective reporting (reporting bias) | High risk | Need for rescue medication not reported. |
| Other bias | Low risk | None apparent; ‘no significant differences between treatment groups’. |
| Methods | Multi‐arm RCT (2 studies reported in 1 publication; study E2). | |
| Participants | Women with severe pain only, who gave consent, no complicating illness, were not breastfeeding and were expected to tolerate medication well at a maternity hospital, Caracus, Venezuela. | |
| Interventions |
E2 study: fenoprofen 12.5 mg (N = 24); fenoprofen 25 mg (N = 23); fenoprofen 50 mg (N = 23); fenoprofen 100 mg (N = 23) and fenoprofen 200 mg (N = 23). Comparison: placebo in both E1 study (N = 27) and E2 study (N = 23). |
|
| Outcomes |
Data were obtained at baseline, and 1, 2, 3, 4 and 5 hours after taking the medication. 5‐hour data used in this review (included at 6‐hour time‐frame). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data on withdrawals due to need for rescue medication at < 2 hours not provided (or referred to in results section). |
| Selective reporting (reporting bias) | High risk | Need for rescue medication not reported. |
| Other bias | Low risk | None apparent; ‘no significant differences between treatment groups’. |
| Methods | Parallel RCT – 2 groups. | |
| Participants | Women who spontaneously delivered a singleton fetus and sustained perineal damage requiring repair in a state‐funded public maternity hospital which also serves as an affiliated teaching hospital in Penang, Malaysia. Recruitment took place between January and June 2006; women were randomised as soon as possible after completion of perineal suturing. Women with known allergy to NSAIDs, epidural during labour, third‐ or higher‐degree tear, instrumental vaginal birth, a history of peptic ulcer, asthma, thrombocytopenia, renal impairment or severe postpartum haemorrhage > 1500 mL, were excluded. |
|
| Interventions | Intervention: celecoxib 200 mg (N = 163). Comparison: diclofenac 100 mg (N = 165). |
|
| Outcomes |
Pain score (VAS) were completed by women at baseline and 1, 2, 4, 8, 12 and 24 hours. 4‐hour data used in the review. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Low risk | Numbered sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete outcome data balanced across groups (attrition rates: 15 of 164 (9%) in the celecoxib groups and 15 of 165 (9%) in the diclofenac group). Analysis by intention‐to‐treat. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | No significant differences between the groups in any characteristics. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | Women between the ages of 18 and 40, no systemic medical illness and experienced moderate to severe episiotomy pain within 48 hours following an otherwise uncomplicated vaginal delivery at the Department of Obstetrics and Gynaecology, Sinai Hospital of Baltimore. Exclusion criteria were those used by Hermann et al 1980 and included; women with pain not due directly to the episiotomy (e.g. uterine cramps), except for cleansing, all wound care was suspended for the whole study period; patients who appeared unlikely to communicate meaningful information about their pain; women with only mild pain; those under 16 years of age; history of drug allergy; any relevant psychiatric, neurologic, cardiovascular, pulmonary, hepatic, gastrointestinal, or renal disorders and women given analgesics, sedatives, or other psychotropic drugs within 3 hours were excluded. |
|
| Interventions | Intervention: fluproquazone 200 mg (N = 39); fluproquazone 100 mg (N = 41) and aspirin 650 mg (N = 40). Comparison: placebo (N = 40). |
|
| Outcomes |
Rating scale information for pain intensity and pain relief measures are not provided; unable to use formula to calculate adequate pain relief, but adequate pain relief could be derived from good to excellent overall impression rating. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement. |
| Allocation concealment (selection bias) | Unclear risk | States sealed envelopes, but unclear if consecutively numbered or opaque. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The attrition rate was 0%, but of the 166 participants, 160 were included in the analysis (4% excluded). Provides reasons for exclusions after entering study; the data of 6 patients were not included since they did not follow the assigned protocol. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Unclear risk | No clear statement regarding baseline characteristics or balance across groups. |
| Methods | Parallel RCT– 2 groups. | |
| Participants | Women aged 18‐38 years with intense post‐episiotomy pain requiring analgesia at Legnano Civil Hospital, Italy. Women with liver or kidney failure, peptic ulcer and hypersensitivity to paracetamol or NSAID, were excluded. |
|
| Interventions | Intervention: aceclofenac single tablet 100 mg (N = 30; pain intensity could not be assessed in 1 due to vomiting; N = 29). Comparison: paracetamol 650 mg (N = 30). |
|
| Outcomes |
Pain assessed before treatment administration, at 30 minutes after and hourly thereafter through to 6 hours. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 (3%) of 30 lost to analysis for pain intensity in aceclofenac 100 mg group due to vomiting. 0% attrition rate for the paracetamol 650 mg group. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Randomisation produced 2 homogenous groups. |
| Methods | Multi‐arm RCT – 3 groups. | |
| Participants | Women were selected from an otherwise healthy population of parturient women whose chief complaint was moderate to severe pain following episiotomy in New Delhi, India. Women with known sensitivity to dipyrone and aspiring or who had received analgesics 8 hours before entry to the study, were excluded. |
|
| Interventions | Intervention: dipyrone 500 mg (N = 89) and aspirin 500 mg (N = 90). Comparison: placebo (N = 88). |
|
| Outcomes |
Pain relief was measured at baseline, at 30 minutes post‐treatment and hourly thereafter to 6 hours. We were unable to accurately extract mean pain relief scores from the graphs; numbers converted from percentages of reported pain as provided in the paper for 6‐hour time‐frame. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 267 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Baseline characteristics comparable. |
| Methods | Multi‐arm RCT – 5 groups. | |
| Participants | Women 18 years or older and able to communicate meaningfully with the nurse‐observer, severe episiotomy pain after uncomplicated delivery, could tolerate oral medication and had no medications that might confound the results were permitted during the study or for the 4 hours before entry to the study at Hospital Maternidad Concepcion Palacios, Caracas, Venezuela. Women planning to breastfeed within 24 hours after administration of study medication, with serious complicating illness, abnormal postpartum bleeding, active peptic ulcer disease or other gastrointestinal disease associated with blood loss, who received any other investigational drug within 1 month before enrolment to study or with a history of drug or alcohol abuse or known allergic sensitivities to the study medications, were excluded. |
|
| Interventions | Intervention: diclofenac 25 mg (N = 52); diclofenac 50 mg (N = 50); diclofenac 100 mg (N = 51) and aspirin 650 mg (N = 50). Comparison: placebo (N = 52). |
|
| Outcomes |
Pain intensity was measured prior to, 30 minutes after, and hourly thereafter up to 8 hours following drug administration. 4‐hour data used in the review (6‐hour data could not be extracted). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐program generated random permutation. |
| Allocation concealment (selection bias) | Unclear risk | Doses were identical in appearance and packaging; however, no indication if sequentially numbered and sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 255 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | No significant differences between groups in terms of characteristics and clinical features; all had severe episiotomy pain on entry to the study. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | Women 18 years or older and able to communicate meaningfully with nurse‐observer, hospitalised and were in good health, could tolerate oral medication and had severe post‐episiotomy pain after term delivery with no medical complications at Hospital Maternidad Concepcion Palacios, Caracas, Venezuela. Women who were breastfeeding or who planned to breastfeed within 48 hours after drug administration, with none or suspected hypersensitivity to dipyrone, ketoprofen or other NSAID agents or who received any other investigational drug within 1 month prior to enrolment in the study were excluded. |
|
| Interventions | Intervention: ketoprofen oral solution 5%, 25 mg prepared in 0.45 mL (N = 28); ketoprofen oral solution 5%, 50 mg prepared in 0.90 mL (N = 26) and dipyrone oral solution 500 mg prepared in 1 mL or 30 drops (N = 27). Comparison: placebo oral solution (N = 27). |
|
| Outcomes |
Pain intensity and relief collected at baseline prior to treatment, at; 15, 30, 60, 90 and 120 minutes after treatment and hourly thereafter for a total of 6 hours. |
|
| Notes | Dipyrone oral solution not considered for the review as not NSAID. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | States individual randomisation envelope was prepared for each patient, and sealed (and opened later by nurse A), but does not state if opaque and consecutively labelled. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Nurse A prepared and gave the medication to the participants, so was aware of their allocation; although Nurse B was the observer and did not know the allocations, there is a risk of bias here as nurse A (although instructed not to disclose drug) could have. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 108 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | High risk | No significant differences among the treatment groups with respect to characteristics and clinical features; The study, however, was prematurely terminated due to administrative changes; thus less than half of the sample size estimate was recruited. |
| Methods | Multi‐arm RCT – 3 groups. | |
| Participants | Hospitalised women with moderate or severe episiotomy pain after normal uncomplicated birth, New York. Women with eclampsia or any other medical complication, allergic hypersensitivity to treatment drugs or had any analgesia or NSAID in 4 hours prior to study entry, were excluded. |
|
| Interventions | Intervention: ibuprofen 400 mg (N = 36). Comparison: placebo (N = 38) and acetaminophen 1000 mg (N = 37). |
|
| Outcomes |
Pain measured before medication, 30 minutes and 1‐4 hours after. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random code. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 of 115 (3%) participants removed after randomisation due to re‐medicated but time not known and not specified from which group. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | The groups were similar in terms of demographics and clinical features. |
| Methods | Parallel RCT – 2 groups. | |
| Participants | Women 18‐35 years of age, vaginal birth with mediolateral episiotomy, absorbable and continuous sutures and singleton, live baby, Iran. Women were recruited between March 2009 and November 2010. Women were excluded if they had known allergy to NSAIDs or a history of alimentary canal disorders, underlying illness, instrumental delivery, perineal rupture (3rd or 4th degree), postpartum haemorrhage, pre‐eclampsia and eclampsia. |
|
| Interventions | Intervention: celecoxib 100 mg every 12 hours (N = 85). Comparison: ibuprofen 400 mg every 6 hours (N = 85). |
|
| Outcomes |
Pain levels were measured before the intervention and at 1, 2, 4, 8 and 12 hours after suturing using a VAS; however, no information provided on scale intervals. 4‐hour continuous data only included in the review. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Single‐blind only (the person assessing pain was blinded, but no report of blinding of the participants). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 170 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | No significant differences between the groups in terms of demographics or clinical characteristics. |
| Methods | Multi‐arm RCT – 5 groups. | |
| Participants | Women 18 years or older who were able to communicate meaningfully with the nurse observer and gave written consent and had moderate or severe post‐episiotomy pain after an uncomplicated birth and could tolerate oral medication at Hospital Maternidad Concepcion Palacios, Caracas, Venezuela. Women who were breastfeeding, had any complicating illness or abnormal postpartum bleeding, received any other investigational drug within 1 month prior to enrolment in the study or history of drug dependence or known allergic sensitivities to propionic acid derivatives and aspirin, were excluded. |
|
| Interventions | Intervention: aspirin 600 mg (N = 29); flurbiprofen 25 mg (N = 32); flurbiprofen 50 mg (N = 29) and flurbiprofen 100 mg (N = 31). Comparison: placebo (N = 31). |
|
| Outcomes |
Pain assessed prior to and hourly up to 6 hours after drug administration. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐program generated. |
| Allocation concealment (selection bias) | Unclear risk | States identical in appearance and packaging but insufficient information regarding sequentially numbered and sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16 of 168 (10%) were dropped from the analysis because they received oxytocic medication (4 of 33 (12%) in the aspirin 600 mg group, 3 of 35 (9%) in the flurbiprofen 25 mg group, 5 of 34 (15%) in the flurbiprofen 50 mg group, 3 of 34 (9%) in the flurbiprofen 100 mg group, and 1 of 32 (3%) in the placebo group). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | No significant differences between groups in terms of characteristics and clinical features; all had moderate or severe episiotomy pain on entry to the study. |
| Methods | Multi‐arm RCT – 4 groups. | |
| Participants | Women with severe post‐episiotomy pain after uncomplicated delivery, > 18 years old and could tolerate oral medication at Hospital Maternidad Concepcion Palacios, Caracus, Venezuela. Women with known allergic sensitivities to study medications, abnormal postpartum bleeding, or complicated illnesses, breastfeeding or with a history of drug dependence or had received other investigational drugs prior to entry into study, were excluded. No medications were given within 4 hours of the study medication being given; if women required additional analgesia within 1 hour after administration of study medication, they were subsequently excluded from the study. |
|
| Interventions | Intervention: ibuprofen 400 mg (N = 30); zomepirac 100 mg (N = 30) and aspirin 600 mg (N = 30). Comparison: placebo (N = 30). |
|
| Outcomes |
Measurements were taken at the time of medication, 30 minutes later, and then hourly up to 4 hours. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement.. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 120 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Similar group baseline characteristics. |
| Methods | Parallel RCT – 2 groups. | |
| Participants | Primiparas over 18 years old, had deliveries and episiotomies without complications and moderate to severe pain within 48 hours of procedure with an intensity of at least 60% on a VAS in Belgium. All participants had undergone medio‐lateral episiotomies with 3‐4 non‐absorbable surgical sutures using a local anaesthetic. Women with mild pain (< 60% on VAS), breastfeeding and excessive anxiety or emotional instability, were excluded. 1 dose of rescue analgesia was permitted in cases of excessive pain 2 hours after study drugs administered ‐ all other treatments were excluded. |
|
| Interventions | Intervention: antrafenine 300 mg (N = 30). Comparison: placebo (N = 30). |
|
| Outcomes |
Pain measured at baseline, before drug administration, and hourly thereafter up to 6 hours. Only 6‐hour data included in the review (4‐hour data could not be extracted). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | States identical‐appearing tablets but no other details. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 of 60 (3%) of participants were excluded from the study after taking another analgesic (1 (3%) in each group). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | High risk | Delay between episiotomy and drug intake was significantly shorter in the placebo group; also 16 placebo‐treated patients withdrew from the study due to lack of efficacy compared to 5 in the antrafenine group. (Participants who withdrew from the study due to lack of efficacy were still included in the analysis: their last self‐rating on VAS was repeated.) |
| Methods | Multi‐arm RCT – 4 group. | |
| Participants | Women > 15 years with moderate to severe episiotomy pain after normal vaginal birth at Women’s Hospital, Los Angeles County. Women with a history of reaction or hypersensitivity to NSAID or salicylates, receiving perineal < 1 hour before entry to study, received analgesics, sedatives, psychotropic medications, or topical perineal anaesthetics within 4 hours of entering study or had an active disease that might interfere with the evaluation of study medications, were excluded. |
|
| Interventions | Intervention: meclofenamate 200 mg (N = 55); meclofenamate 100 mg (N = 55) and codeine 60 mg (N = 53). Comparison: placebo (N = 52). |
|
| Outcomes |
Pain measures were assessed at baseline prior to treatment, at 30 minutes after and hourly thereafter to 6 hours. |
|
| Notes | Codeine 60 mg not considered for the review as not an NSAID. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | No clear statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The attrition rate was 0%, but 5 of 220 (2%) participants were excluded from efficacy analysis because of protocol violation. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | No differences in baseline characteristics. |
| Methods | Parallel RCT – 2 groups. | |
| Participants | Only women those with severe episiotomy pain aged 18‐39 years in the 48 hours following an uncomplicated delivery at Mollet General Hospital, Barcelona. Women with slight or moderate pain, gastroduodenal disorders, and liver or kidney failure, a known history of hypersensitivity to phynylacetic acid derivatives or to acetylsalicylic acid and similar substances, treated with NSAIDs or systemic steroids or exceeding the age limits and who did not give consent, were excluded. |
|
| Interventions | Intervention: aceclofenac 100 mg (N = 20). Comparison: placebo (N = 20). |
|
| Outcomes |
Pain intensity was measured before treatment, 30 minutes and 1 hourly to 6 hours thereafter, but these data could not be extracted. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No clear statement on method used. |
| Allocation concealment (selection bias) | Unclear risk | Packaged in identical packs identifiable only by the letters A and B; but does not state if sequentially numbered and sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No clear statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided for all 40 participants (0% attrition rate in all groups). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were all reported. |
| Other bias | Low risk | Groups similar at baseline. |
ASA: acetylsalicylic acid NSAID: non‐steroidal anti‐inflammatory drug RCT: randomised controlled trial SPID: Summed Pain Intensity Difference TOTPAR: Total Pain Relief VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abedzadeh 2009 | Treatment was not oral (gel versus suppository). |
| Akil 2014 | Treatment was not oral (intravenous). |
| Altungul 2012 | Treatment was not oral (suppository). |
| Bettigole 1981 | Not a single dose. |
| Bhounsule 1990 | Not a RCT; quasi‐RCT with concurrent allocation – 2‐group comparison without randomisation. |
| Bloomfield 1970 | Measures outcomes at 8 hours; did not measure outcomes for the 4‐ and 6‐hour time‐frames included in this review. |
| Bloomfield 1979 | Treatment not a NSAID. |
| Bloomfield 1980 | Treatment not a NSAID. |
| Bloomfield 1991 | Not a RCT; personal communication related to non‐completion of a registered trial. |
| Bruni 1965 | Not specific to perineal pain; rather postpartum pain in general. |
| Bucheli 1994 | Not a single dose. |
| Buck 1978 | Not a single dose. |
| Cater 1985 | Ibuprofen and codeine phosphate combination treatment was excluded from the review as not a pure NSAID. Zomepirac is an NSAID but was withdrawn voluntarily from the market by the manufacturer in 1983 because it was associated with fatal and near‐fatal anaphylactoid reactions. |
| Choi 2000 | Treatment not oral (suppository). |
| Coburn 1966 | Not a single dose. |
| Cunha 2011 | Not a single dose. |
| De los Santos 1998 | Comparator drug is a combination of paracetamol and codeine. |
| Delaram 2012 | Treatment not a NSAID. |
| Delaram 2014 | Comparator drug is Lidocaine topical cream. |
| Facchinetti 2005 | Examine the effectiveness of multiple doses (not a single dose). |
| Finch 1971 | Not a RCT; cross‐over trial and not exclusive to perineal pain. |
| Fragen 1982 | Comparator drug is a combination of NSAID and opioid. |
| Gindhart 1971 | Treatment not a NSAID. |
| Gruber 1962 | Examines postpartum pain (not specifically perineal pain). |
| Gruber 1976 | Comparator drug is not an NSAID. |
| Gruber 1979 | Data on the individual medications not available. |
| Harrison 1987 | Not exclusively oral treatment. |
| Harrison 1992 | Not a RCT; cross‐over trial. |
| Jain 1978 | Graph only on participants self‐rating of pain relief ‐ no data for extraction. |
| Kantor 1984 | Data not exclusive to perineal pain; treatment was administered for postpartum pain which may or may not have included post‐episiotomy pain. |
| Levin 1978 | Abstract only. Author's contact details not found. |
| Mazzarella 1989 | Treatment not a NSAID. |
| McCallum 1991 | Registration form only – does not appear to focus on management of perineal pain. |
| Melzack 1983 | Measures outcomes at 12 hours; did not measure outcomes for the 4‐ and 6‐hour time‐frames specified for this review. |
| Norman 1985 | Intervention drug is a combination of NSAID and opioid. |
| Odigie 1988 | Treatment was not oral (suppository). |
| Offen 1985 | Examines postpartum pain and pain related to general surgery (not specifically perineal pain). |
| Ogunbode 1987 | Not a single dose. |
| Okun 1982 | Outcomes reported at 8 hours; > 50% pain relief at 1 and 2 hours only; did not report outcomes for the 4‐ and 6‐hour time‐frames specified for this review. |
| Olson 1984 | Insufficient data – abstract for Poster presentation; also unclear if data for episiotomy pain are reported separately to other types of postpartum pain. We could not identify author's contact details. |
| Pedronetto 1975 | Indoprofen was withdrawn from the market worldwide following reports of adverse reactions including reports of carcinogenicity in animal studies. |
| Peter 2001 | Comparator drug is not a NSAID. |
| Pitton 1982 | Treatment was not oral (intra‐muscular injection). |
| Radman 1961 | Not a single dose. |
| Ray 1993 | Treatment was not oral (suppository). |
| Rezaei 2014 | Treatment was not oral (suppository). |
| Searles 1995 | Treatment was not oral (suppository) |
| Searles 1998 | Treatment was not oral (suppository) |
| Sunshine 1982 | Treatment not a NSAID. |
| Sunshine 1983c | Abstract, insufficient data available; also unclear if episiotomy pain is reported separate to other types of postpartum pain. Author's contact details could not be identified. |
| Sunshine 1983d | Treatment not a NSAID. |
| Sunshine 1985 | Abstract only; insufficient information to include; unclear also if pain is reported separately by pain type. Author's contact details could not be identified. |
| Sunshine 1986 | Examines postpartum pain (not specifically perineal pain). |
| Sunshine 1987a | Examines postpartum pain and incisional pain following surgery.(not specifically perineal pain). |
| Sunshine 1987b | Insufficient data provided to consider including (abstract information only). Author's details could not be identified. |
| Sunshine 1989 | Abstract only, insufficient information. Author's contact details could not be identified. |
| Szabados 1986 | Not a single dose. |
| Taina 1981 | Not a single dose. |
| Trop 1983 | Number of participants randomised to each group is not provided. |
| Van Wering 1972 | Examines postpartum pain (not specifically perineal pain). |
| Von Pein 1974 | Not a single dose. |
| Walters 1984 | Comparator treatment does not meet inclusion criteria. |
| Walters 1985 | Comparator is an opioid; does not meet comparator inclusion criteria. |
| Yoong 1997 | Treatment was not oral (suppository). |
NSAID: NSAID: non‐steroidal anti‐inflammatory drug RCT: randomised controlled trial
Contributions of authors
F Wuytack drafted the protocol and is guarantor for the review. F Wuytack and V Smith conducted the study selection, data extraction and 'Risk of bias' assessment. F Wuytack, V Smith and B Cleary conceptualised the data analysis. F Wuytack entered data into RevMan, performed the analysis and drafted the manuscript. F Wuytack, V Smith and B Cleary reviewed the review for intellectual content and interpretation of the data. All authors read and commented on the final draft of the manuscript prior to submission.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Health Research Board, Ireland.
A Health Research Board, Ireland, Cochrane Fellowship was awarded to F Wuytack to support the conduct of this review.
Declarations of interest
Francesca Wuytack: has received a Cochrane Fellowship, awarded by the Health Research Board Ireland, to support the conduct of this review.
Valerie Smith has acted in the capacity of Ms Wuytack's supervisor and PI on the Cochrane HRB Fellowship grant application. The awarded grant is not salary or such support, rather support for Ms Wuytack to attend Cochrane training workshops and other necessary consumables.
Brian J Cleary's institution has received €500from the State Claims Agency for a lecture that he gave about the historical context of the development and marketing of thalidomide in Ireland to a mediation process between the Irish state and survivors of the Thalidomide disaster. A sum of €1500 was also paid to his institution (by Ferring Pharmaceuticals) for training provided to private sector pharmacies and an infertility clinic on the use of a specialised drug delivery system used to delivery an infertility treatment from Ferring (Lutrelef). Brian's brother works for a drug company that sells analgesic products (Grunenthal). However Brian's institution does not currently use their products for the management of peripartum pain and their products are irrelevant to the content of this review. Brian has been publicly critical of Grunenthal and their historical actions in the context of the thalidomide disaster.
Edited (no change to conclusions)
References
References to studies included in this review
- Behotas S, Chauvin A, Castiel J, Martin A, Boureau F, Barrat J, et al. Analgesic effect of ibuprofen in pain after episiotomy [Effets antalgiques de l'ibuprofene dans les douleurs apres episiotomie]. Annales Francaises d Anesthesie et de Reanimation 1992;11(1):22‐6. [] [DOI] [PubMed] [Google Scholar]; 3226420
- Bloomfield SS, Gaffney TE, Howett M. Comparative analgesic efficacy of chlorphenesin carbamate and acetylsalicylic acid after episiotomy. Anesthesia and Analgesia 1967;46:515‐20. [] [PubMed] [Google Scholar]; 3226422
- Bloomfield SS, Barden TP, Mitchell J. Comparative efficacy of ibuprofen and aspirin in episiotomy pain. Clinical Pharmacology and Therapeutics 1974;15:565‐70. [] [DOI] [PubMed] [Google Scholar]; 3226424
- Daftary SN, Mehta AC, Nanavati M. A controlled comparison of dipyrone and paracetamol in post‐episiotomy pain. Current Medical Research and Opinion 1980;6:614‐8. [] [DOI] [PubMed] [Google Scholar]; 3226426
- Vroey P. A double‐blind comparison of diflunisal and aspirin in the treatment of post‐operative pain after episiotomy. Current Medical Research and Opinion 1978;5:544‐7. [] [DOI] [PubMed] [Google Scholar]; Vroey P. The treatment of postoperative pain with a single dose of diflunisal. Clinical Therapeutics 1977;1(Suppl A):30‐3. [] [Google Scholar]; 3226428
- Friedrich E. A comparison of etodolac (Ultradol) with aspirin and placebo in patients with episiotomy pain. Current Therapeutic Research, Clinical and Experimental 1983;33(1):100‐7. [] [Google Scholar]; 3226431
- Gleason JA, Winer W, Turner JL. Comparison of meclofenamate sodium with codeine and placebo for the treatment of episiotomy pain. Clinical Therapeutics 1987;9(6):585‐93. [] [PubMed] [Google Scholar]; 3226433
- Hebertson RM, Storey N, Turner JL. Analgesic efficacy of meclofenamate sodium in episiotomy pain. Pharmacotherapy 1986;6:205‐10. [] [DOI] [PubMed] [Google Scholar]; 3226435
- Honorato J, Caballero R, Giorgiani G, Movilia PG, Tapounet R. Dose‐analgesic response study and aceclofenac plasma levels in humans. Current Therapeutic Research, Clinical and Experimental 1990;47(4):605‐11. [] [Google Scholar]; 3226437
- Hopkinson JH. Ibuprofen vs propoxyphene hydrochloride and placebo in the relief of postepisiotomy pain. Current Therapeutic Research 1980;27:55‐63. [] [Google Scholar]; 3226439
- Jain AK, McMahon FG, Ryan JR, Smith GB. Analgesic efficacy of indoprofen in postpartum episiotomy pain. Current Therapeutic Research, Clinical and Experimental 1985;38(5):677‐81. [] [Google Scholar]; 3226441
- Jain AK, Mcmahon FG, Ryan JR, Narcisse C. A double‐blind study of ibuprofen 200 mg in combination with caffeine 100 mg, ibuprofen 400 mg, and placebo in episiotomy pain. Current Therapeutic Research, Clinical and Experimental 1988;43(4):762‐9. [] [Google Scholar]; 3226443
- Kamondetdecha R, Tannirandorn Y. Ibuprofen versus acetaminophen for the relief of perineal pain after childbirth: a randomized controlled trial. Journal of the Medical Association of Thailand 2008;91(3):282‐6. [] [PubMed] [Google Scholar]; 3226445
- Laska EM, Sunshine A. Fenoprofen and codeine analgesia (E1 study). Clinical Pharmacology and Therapeutics 1981;29:606‐16. [] [DOI] [PubMed] [Google Scholar]; Sunshine A, Laska E, Zighelboim I, Desenne J. A comparison of the analgesic responses of fenoprofen, codeine, and placebo in postpartum and postoperative pain. Current Therapeutic Research, Clinical and Experimental 1981;29(5):771‐7. [] [Google Scholar]; 3226447
- Laska EM, Sunshine A. Fenoprofen and codeine analgesia (E2 study). Clinical Pharmacology and Therapeutics 1981;29:606‐16. [] [DOI] [PubMed] [Google Scholar]; 3226450
- Lim SS, Tan PC, Sockalingam JK, Omar SZ. Oral celecoxib versus oral diclofenac for post‐perineal repair analgesia after spontaneous vaginal birth: a randomised trial. Australian and New Zealand Journal of Obstetrics and Gynaecology 2008;48(1):71‐7. [] [DOI] [PubMed] [Google Scholar]; 3226452
- London R, Sundaram GS, Feldman S, Goldstein PJ. Episiotomy pain: efficacy and safety of fluproquazone compared to aspirin and placebo. International Journal of Gynecology & Obstetrics 1983;21:251‐5. [] [DOI] [PubMed] [Google Scholar]; 3226454
- Movilia PG. Evaluation of the analgesic activity and tolerability of aceclofenac in the treatment of post‐episiotomy pain. Drugs under Experimental and Clinical Research 1989;15(1):47‐51. [] [PubMed] [Google Scholar]; 3226456
- Mukherjee S, Sood S. A controlled evaluation of orally administered aspirin dipyrone and placebo in patients with post‐operative pain. Current Medical Research and Opinion 1980;6:619‐23. [] [DOI] [PubMed] [Google Scholar]; 3226458
- Olson NZ, Sunshine A, Zighelboim I, DeCastro A. Onset and duration of analgesia of diclofenac potassium in the treatment of postepisiotomy pain. American Journal of Therapeutics 1997;4:239‐46. [] [DOI] [PubMed] [Google Scholar]; 3226460
- Olson NZ, Sunshine A, Zighelboim I, Lange R. Analgesic efficacy of liquid ketoprofen compared to liquid dipyrone and placebo administered orally as drops in postepisiotomy pain. International Journal of Clinical Pharmacology & Therapeutics 1999;37(4):168‐74. [] [PubMed] [Google Scholar]; 3226462
- Schachtel BP, Thoden WR. Efficacy of ibuprofen 400mg, acetaminophen 1000mg and placebo in post‐episiotomy pain. Clinical Pharmacology and Therapeutics 1989;45:175. [] [Google Scholar]; Schachtel BP, Thoden WR, Baybutt RI. Ibuprofen and acetaminophen in the relief of postpartum episiotomy pain. Journal of Clinical Pharmacology 1989;29:550‐3. [] [DOI] [PubMed] [Google Scholar]; 3226464
- Suhrabi Z, Taghinejad H. A comparative study on the efficacy of Ibuprofen and celecoxib on the intensity of perineal pain following episiotomy: a randomized clinical trial. Iranian Red Crescent Medical Journal 2013;15(12):e9980. [] [DOI] [PMC free article] [PubMed] [Google Scholar]; 3226467
- Sunshine A, Olson NZ, Laska EM, Zighelboim I, Castro A, Sarrazin C. Analgesic effect of graded doses of flurbiprofen in post‐episiotomy pain. Pharmacotherapy 1983;3(3):177‐81. [] [DOI] [PubMed] [Google Scholar]; 3226469
- Sunshine A, Olson NZ, Laska EM, Zighelboim I, Castro A, Sarrazin C. Ibuprofen, zomepirac, aspirin, and placebo in the relief of postepisiotomy pain. Clinical Pharmacology and Therapeutics 1983;34:254‐8. [] [DOI] [PubMed] [Google Scholar]; 3226471
- Visanto J, Dubois D, Coquelin JPH. Comparative study between antrafenine and placebo in patients with pain due to episiotomy [abstract]. European Journal of Clinical Investigation 1980;10:39; Abstract no: 229. [] [Google Scholar]; Wisanto A, Caudron J, Dubois D, Narbonne G, Coquelin JPH. A double‐blind placebo‐controlled single‐dose study comparing antrafenine and placebo in patients with post‐episiotomy pain. Current Therapeutic Research, Clinical and Experimental 1981;29:171‐82. [] [Google Scholar]; 3226473
- Yonkeura ML, Petrone S, Turner JL, Zerega GS. Double‐blind comparison of meclofenamate sodium with codeine and placebo for the pain of episiotomy. Clinical Therapeutics 1987;9:578‐84. [] [PubMed] [Google Scholar]; 3226476
- Yscla A. Aceclofenac and paracetamol in episiotomal pain. Drugs Under Experimental and Clinical Research 1988;7:491‐4. [] [PubMed] [Google Scholar]; 3226478
References to studies excluded from this review
- Abedzadeh M, Sadat Z, Saberi F. The efficacy of 2% lidocaine gel versus diclofenac suppository in pain reliving after episiotomy. Koomesh 2009;10(4):301‐5. [] [Google Scholar]; 3226480
- Akil A, Api O, Bektas Y, Yilmaz AO, Yalti S, Unal O. Paracetamol vs dexketoprofen for perineal pain relief after episiotomy or perineal tear. Journal of Obstetrics and Gynaecology 2014;34(1):25‐8. [] [DOI] [PubMed] [Google Scholar]; 3226482
- Altungul AC, Sapmaz E, Kale A. Comparison of diclofenac sodium with indomethacin suppositories for mediolateral episiotomies. Clinical and Experimental Obstetrics and Gynecology 2012;39(1):112‐4. [] [PubMed] [Google Scholar]; 3226484
- Bettigole JB. A double‐blind comparison of placebo, codeine, and fenoprofen in patients with postpartum pain. Current Therapeutic Research 1981;29:778‐84. [] [Google Scholar]; 3226486
- Bhounsule SA, Nevreker PR, Agshikar NV, Pal MN, Dhume VG. A comparison of four analgesics in post‐episiotomy pain. Indian Journal of Physiology and Pharmacology 1990;34(1):34‐8. [] [PubMed] [Google Scholar]; 3226488
- Bloomfield SS, Barden TP, Hille R. Clinical evaluation of flufenisal, a long‐acting analgesic. Clinical Pharmacology and Therapeutics 1970;11:747‐54. [] [DOI] [PubMed] [Google Scholar]; 3226490
- Bloomfield SS, Barden TP, Mitchell J. Nefopam and propoxyphene in episiotomy pain [abstract]. Clinical Pharmacology & Therapeutics 1979;25(2):214‐5. [] [DOI] [PubMed] [Google Scholar]; 3226492
- Bloomfield SS, Barden TP, Mitchell J. Nefopam and propoxyphene in episiotomy pain. Clinical Pharmacology and Therapeutics 1980;27:502‐7. [] [DOI] [PubMed] [Google Scholar]; 3226494
- Bloomfield SS. The comparative efficacy of Voltaren(R) (diclofenac), naproxen sodium and placebo in the treatment of postepisiotomy pain. Personal communication1991. [] ; 3226496
- Bruni JR, Holt RE. Controlled double‐blind evaluation of three analgesic medications for postpartum discomfort. Obstetrics & Gynecology 1965;25:76‐81. [] [PubMed] [Google Scholar]; 3226498
- Bucheli R, Davalos V, Neto N, Naranjo I, Calderon D, Alamo C, et al. A randomized, double‐blind study of the efficacy and safety of microcapsulated butibufen and naproxen in the treatment of post‐episiotomy pain. Current Therapeutic Research, Clinical and Experimental 1994;55(12):1527‐37. [] [Google Scholar]; 3226500
- Buck ME, Paintin DB. Diflunisal in post‐episiotomy pain: a preliminary report of a double‐blind comparative study. Current Medical Research and Opinion 1978;5:548‐9. [] [DOI] [PubMed] [Google Scholar]; 3226502
- Cater M, O'Brien PMS, Pickvance NJ. A double‐blind comparison of the new ibuprofen‐codeine phosphate combination, zomepirac, and placebo in the relief of postepisiotomy pain. Clinical Therapeutics 1985;7:442‐7. [] [PubMed] [Google Scholar]; 3226504
- Choi DM, Peter EA, Douglas MJ, Janssen P. Naproxen and epidural morphine for perineal pain after forceps delivery [abstract]. Anesthesiology 2000;92 Suppl:Abstract no: A79. [] [Google Scholar]; 3226506
- Coburn WA, Rutherford RN, Banks AL. Short‐term use of oxyphenbutazone in the postpartum period. Obstetrics & Gynecology 1966;28:484‐90. [] [PubMed] [Google Scholar]; 3226508
- Cunha A, Almeida A, Almeida L, Cruz A, Vilhena I, Costa C, et al. Pospartum analgesia ‐ What can we do?. Regional Anesthesia and Pain Medicine 2011;36(5 Suppl 2):E239. [] [Google Scholar]; 3226510
- Delaram M. Comparison of the effects of lidocaine pomade , indomethacin suppository and mefenamic acid on the relief of post episiotomy pain in primiparous women. IRCT Iranian Registry of Clinical Trials [accessed 15 March 2014]. IRCT201104253078N7 2012. [] ; 3226512
- Delaram M, Dadkhah N. Comparing the effects of lidocaine cream and mefenamic acid on post episiotomy pain. Iranian Journal of Obstetrics, Gynecology and Infertility 2014;17(96):6‐11. [] [Google Scholar]; 3226514
- Santos AR, Marti MI, Espinosa D, Girolamo G, Vinacur JC, Casadei‐A. Lysine clonixinate vs paracetamol/codeine in postepisiotomy pain. Acta Physiologica, Pharmacologica et Therapeutica Latinoamericana 1998;48:52‐8. [] [PubMed] [Google Scholar]; 3226516
- Facchinetti F, Casini ML, Costabile L, Malavasi B, Unfer V. Diclofenac pyrrolidine versus ketoprofen for the relief of pain from episiotomy: a randomized controlled trial. Acta Obstetricia et Gynecologica Scandinavica 2005;84(10):951‐5. [] [DOI] [PubMed] [Google Scholar]; 3226518
- Finch JS, DeKornfeld TJ. Clonixin: a clinical evaluation of a new oral analgesic. Journal of Clinical Pharmacology & New Drugs 1971;11(5):371‐7. [] [PubMed] [Google Scholar]; 3226520
- Fragen RJ, Vlasuk L. Analgesic efficacy of a combination of fenoprofen and codeine administered orally. Current Therapeutic Research, Clinical and Experimental 1982;31(2):129‐37. [] [Google Scholar]; 3226522
- Gindhart JD. A rationale for studying analgesia. A double blind study in postpartum patients. Current Therapeutic Research 1971;13:240‐50. [] [PubMed] [Google Scholar]; 3226524
- Gruber CM, Baptisti A, Chernish SM. Comparative evaluation of analgesic agents in postpartum patients: oral dextropropoxyphene, codeine and meperidine. Anesthesia and Analgesia 1962;41:538‐44. [] [PubMed] [Google Scholar]; 3226526
- Gruber CM. Evaluating interactions between fenoprofen and propoxyphene: analgesia and adverse reports by postepisiotomy patients. Journal of Clinical Pharmacology 1976;16(8‐9):407‐17. [] [DOI] [PubMed] [Google Scholar]; 3226528
- Gruber CM, Bauer RO, Bettigole JB, Lash AF, McDonald JS. A multicenter study for analgesia involving fenoprofen, propoxyphene [alone or in combination] with placebo and aspirin controls in postpartum pain. Journal of Medicine 1979;10(1‐2):65‐98. [] [PubMed] [Google Scholar]; 3226530
- Harrison RF, Brennan M. Comparison of two formulations of lignocaine spray with mefenamic acid in the relief of post‐episiotomy pain: a placebo‐controlled study. Current Medical Research and Opinion 1987;10:375‐9. [] [DOI] [PubMed] [Google Scholar]; 3226532
- Harrison RF, Devitt M. Indomethacin and ethamsylate alone and in combination for the relief of post episiotomy pain. Irish Journal of Medical Science 1992;161(8):493‐7. [] [DOI] [PubMed] [Google Scholar]; 3226534
- Jain AK, McMahon FG, Ryan JR, Raphan H, Richard W. Piroxicam, a novel analgesic in postpartum pain. European Journal of Rheumatology and Inflammation 1978;1(3):356‐9. [] [Google Scholar]; 3226536
- Kantor T, Cavaliere MB, Hopper M, Roepke S. A double‐blind parallel comparison of ketoprofen, codeine, and placebo in patients with moderate to severe postpartum pain. Journal of Clinical Pharmacology 1984;24:228‐34. [] [DOI] [PubMed] [Google Scholar]; 3226538
- Levin HM. Relative potency assay comparing zomepirac sodium, propoxyphene napsylate, propoxyphene napsylate with acetaminophen, codeine, and placebo in patients with episiotomy pain. International Journal of Clinical Pharmacology and Therapeutics 1978;23(1):118. [] [Google Scholar]; 3226540
- Mazzarella B, Mastronardi P, Rossi AE, Cafiero T, Chiefari M, Ceccarelli G. Controlled clinical evaluation of the analgesic efficacy of flupirtine and ketoprofen in postepisiotomy pain. Proceedings of 4th European Congress of Allied Specialists in Maternal and Neonatal Care; 1989 Sept; Bruges, Belgium. 1989. [] [Google Scholar]; 3226542
- McCallum KA. Trial to assess Ponstan vs placebo, given within an hour of birth, to women who had had epidural and forceps deliveries, as a means of prophylactic analgesia, by measuring time to first postnatal analgesic consumption. Personal communication1991. [] ; 3226544
- Melzack R, Jeans ME, Kinch RA, Katz J. Diflunisal (1000 mg single dose) vs acetaminophen (650 mg) and placebo for the relief of post‐episiotomy pain. Current Therapeutic Research 1983;34:929‐39. [] [Google Scholar]; 3226546
- Norman SL, Jeavons BI, O'Brien PM, Johnson IR, Hitchcock A, Noyelle RM, et al. A double‐blind comparison of a new ibuprofen‐codeine phosphate combination, codeine phosphate, and placebo in the relief of postepisiotomy pain. Clinical Therapeutics 1985;7(5):549‐54. [] [PubMed] [Google Scholar]; 3226548
- Odigie EA. Effectiveness of indomethacin (indocid) suppositories as post‐episiotomy analgesia. International Journal of Gynecology & Obstetrics 1988;26:57‐60. [] [DOI] [PubMed] [Google Scholar]; 3226550
- Offen WW, Gruber CM. Dose response to fenoprofen calcium using placebo and codeine as controls. Journal of Medicine 1985;16(4):439‐52. [] [PubMed] [Google Scholar]; 3226552
- Ogunbode O. A comparative trial of piroxicam and paracetamol after episiotomy wound repair. Current Therapeutic Research, Clinical & Experimental 1987;41:89‐94. [] [Google Scholar]; 3226554
- Okun R. Evaluation of the analgesic effect of fendosal in patients with postpartum uterine cramp or episiotomy pain. Current Therapeutic Research, Clinical and Experimental 1982;32(1):65‐73. [] [Google Scholar]; 3226556
- Olson N, Sunshine A, Roure C, Colon A, Laska EM, Santiago H, et al. Analgesic efficacy of suprofen, codeine and placebo. Pain 1984;2 Suppl:238. [] [Google Scholar]; 3226558
- Pedronetto S, Gorini F, Mandelli V, Fuccella LM. Double blind trial of the new analgesic and anti inflammatory drug indoprofen in post episiotomic pain. Journal of International Medical Research 1975;3:16‐20. [] [Google Scholar]; 3226560
- Peter EA, Janssen PA, Grange CS, Douglas MJ. Ibuprofen versus acetaminophen with codeine for the relief of perineal pain after childbirth: a randomized controlled trial. CMAJ: Canadian Medical Association Journal 2001;165:1203‐9. [] [PMC free article] [PubMed] [Google Scholar]; 3226562
- Pitton MA, Vincenti E, Polato D, Tambuscio B, Salvia D. Double‐blind study on diclofenac in pain relief after episiotomy [Studio clinico a doppio cieco con diclofenac sodico nel controllo del dolore post‐operatorio in ostetricia. Ii. Episiotomia]. Acta Anaesthesiologica Italica 1982;33(4):717‐20. [] [Google Scholar]; 3226564
- Radman HM, Campbell C, Coplan RS. Anti‐inflammatory drugs in obstetrics and gynaecology. American Journal of Obstetrics and Gynecology 1961;81:344‐9. [] [DOI] [PubMed] [Google Scholar]; 3226566
- Ray S, Swami A, Kadim M, Morgan B. Efficacy of diclofenac in a single prophylactic dose in post partum pain. International Journal of Obstetric Anesthesia 1993;2:58. [] [Google Scholar]; 3226568
- Rezaei Z, Haghighi Z, Haeri G, Hekmatdoust A. A comparative study on relieving post‐episiotomy pain with diclofenac and indomethacin suppositories or placebo. Journal of Obstetrics and Gynaecology : the Journal of the Institute of Obstetrics and Gynaecology 2014;34(4):293‐6. [] [DOI] [PubMed] [Google Scholar]; 3226570
- Searles JA, Pring DW. Improving perineal pain relief. 27th British Congress of Obstetrics and Gynaecology; 1995 July 4‐7; Dublin, Ireland. 1995:Abstract no: 499. [] [Google Scholar]; 3226572
- Searles JA, Pring DW. Effective analgesia following perineal injury during childbirth: a placebo controlled trial of prophylactic rectal diclofenac. British Journal of Obstetrics and Gynaecology 1998;105(6):627‐31. [] [DOI] [PubMed] [Google Scholar]; 3226574
- Sunshine A, Zighelboim I, Laska E. Oral analgesic study of nalbuphine hydrochloride, codeine, and placebo in postpartum pain. Clinical Pharmacology & Therapeutics 1982;31(2):274. [] [Google Scholar]; 3226576
- Sunshine A, Olson JZ, Siegel C, Laska EM. Oral analgesic study of ketoprofen, aspirin and placebo in post‐partum pain. Clinical Pharmacology and Therapeutics 1983;33:154. [] [Google Scholar]; 3226578
- Sunshine A, Zighelboim I, Sarrazin C. A study of the analgesic efficacy of nalbuphine hydrochloride in patients with postpartum pain. Current Therapeutic Research, Clinical and Experimental 1983;33(1):108‐14. [] [Google Scholar]; 3226580
- Sunshine A, Roure C, Zorrilla C, Laska EM, Olson N, Rivera J. The analgesic efficacy of ibuprofen, codeine and placebo. Clinical Pharmacology and Therapeutics 1985;37:232. [] [DOI] [PubMed] [Google Scholar]; 3226582
- Sunshine A, Zighelboim I, Laska E, Siegel C, Olson NZ, Castro A. A double‐blind, parallel comparison of ketoprofen, aspirin, and placebo in patients with postpartum pain. Journal of Clinical Pharmacology 1986;26(8):706‐11. [] [DOI] [PubMed] [Google Scholar]; 3226584
- Sunshine A, Roure C, Olson N, Laska EM, Zorrilla C, Rivera J. Analgesic efficacy of two ibuprofen‐codeine combinations for the treatment of postepisiotomy and postoperative pain. Clinical Pharmacology and Therapeutics 1987;42:374‐80. [] [DOI] [PubMed] [Google Scholar]; 3226586
- Sunshine A, Zighelboim I, Olson N, Laska E. Flurbiprofen, flurbiprofen dextrorotatory component (BTS 24332) and placebo in post‐episiotomy pain. Clinical Pharmacology and Therapeutics 1987;41:162. [] [Google Scholar]; 3226588
- Sunshine A, Laska E, Siegel C, Zighelboim I, Castro A, Sorrentino J, et al. Analgesic adjuvancy of caffeine with ibuprofen in three different postpartum pain populations. Clinical Pharmacology and Therapeutics 1989;45:174. [] [Google Scholar]; 3226590
- Szabados T. Acemetacine and phenylbutazone: Double‐blind study in pain and inflammations following episiotomy [Doppelblindprüfung von Acemetacin und Phenylbutazon bei Schmerzen und Entzündungen nach Episiotomie]. Medizinische Welt 1986;37:703‐6. [] [Google Scholar]; 3226592
- Taina E. Ibuprofen vs placebo in the relief of post‐episiotomy pain. Current Medical Research and Opinion 1981;7:423‐8. [] [DOI] [PubMed] [Google Scholar]; 3226594
- Trop D, Nucci C, Elie R, Gareau J. Double‐blind comparative evaluation of tiaprofenic acid (Surgam) versus acetylsalicylic acid (ASA) in relieving pain following episiotomy. Current Therapeutic Research, Clinical and Experimental 1983;34(2I):274‐9. [] [Google Scholar]; 3226596
- Wering RF, Bleker OP. Oral analgesia in post‐partum pain: a comparison of ibuprofen ('Brufen') and dextropropoxyphene. Current Medical Research and Opinion 1972;1:49‐52. [] [DOI] [PubMed] [Google Scholar]; 3226598
- Pein W. Double blind study using benzydamine in the puerperium. Gynakologische Rundschau 1974;14:327‐8. [] [PubMed] [Google Scholar]; 3226600
- Walters BNJ, Smith VA, Swiet M. Comparative trial of suprofen and dihydrocodeine in post‐episiotomy pain. Pain 1984;2:236. [] [Google Scholar]; 3226602
- Walters BNJ, Smith VA, Swiet M, Mustill TA. Pain relief after episiotomy ‐ a comparative study of suprofen and dihydrocodeine. British Journal of Obstetrics and Gynaecology 1985;92:1160‐3. [] [DOI] [PubMed] [Google Scholar]; 3226604
- Yoong WC, Biervliet F, Nagrani R. The prophylactic use of diclofenac (voltarol) suppositories in perineal pain after episiotomy. A random allocation double‐blind study. Journal of Obstetrics & Gynaecology 1997;17(1):39‐41. [] [DOI] [PubMed] [Google Scholar]; 3226606
Additional references
- Aasheim V, Nilsen ABV, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD006672.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abou‐Saleh MT, Ghubash R. The prevalence of early postpartum psychiatric morbidity in Dubai: transcultural perspective. Acta Psychiatrica Scandinavica 1997;95:428‐32. [DOI] [PubMed] [Google Scholar]
- Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber‐Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. European Spine Journal 2006;15 Suppl 2:192‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews V, Thakar R, Sultan AH, Jones PW. Evaluation of postpartum perineal pain and dyspareunia‐‐a prospective study. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2008;137:152‐6. [DOI] [PubMed] [Google Scholar]
- Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA 1996;276(8):637‐9. [DOI] [PubMed] [Google Scholar]
- Berry PH, Chapman CR, Covington EC, Dahl JL, Katz JA, Miaskowski C, et al. Pain: Current Understanding of Assessment, Management, and Treatments. Reston: National Pharmaceutical Council, Inc, 2001. [Google Scholar]
- BNF: Joint Formulary Committee. British National Formulary. 67. London: BMJ Publishing Group and Pharmaceutical Press, 2014. [Google Scholar]
- Brayfield A. Martindale: The Complete Drug Reference. Pharmaceutical Press, 2014. [Google Scholar]
- Brunton L. Goodman and Gilman's The Pharmacological Basis of Therapeutics. Twelfth. The McGraw‐Hill Companies, Inc, 2011. [Google Scholar]
- Chou D, Abalos E, Gyte GML, Gülmezoglu AM. Drugs for perineal pain in the early postpartum period: generic protocol. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007734] [DOI] [PubMed] [Google Scholar]
- Chou D, Abalos E, Gyte GM, Gülmezoglu AM. Paracetamol/acetaminophen (single administration) for perineal pain in the early postpartum period. Cochrane Database of Systematic Reviews 2013, Issue 1. [DOI: 10.1002/14651858.CD008407.pub2] [DOI] [PubMed] [Google Scholar]
- Cooper SA. Commentary: Single‐dose analgesic studies: the upside and downside of assay sensitivity. In: Max M, Portenov R, Laska E editor(s). Advances in Pain Research and Therapy. Vol. 18, New York: Raven Press, 1991:117–24. [Google Scholar]
- Davies NM. Clinical pharmacokinetics of ibuprofen. The first 30 years. Clinical Pharmacokinetics 1998;34(2):101‐54. [DOI] [PubMed] [Google Scholar]
- Deussen AR, Ashwood P, Martis R. Analgesia for relief of pain due to uterine cramping/involution after birth. Cochrane Database of Systematic Reviews 2011, Issue 5. [DOI: 10.1002/14651858.CD004908.pub2] [DOI] [PubMed] [Google Scholar]
- East CE, Sherburn M, Nagle C, Said J, Forster D. Perineal pain following childbirth: prevalence, effects on postnatal recovery and analgesia usage. Midwifery 2012;28:93‐7. [DOI] [PubMed] [Google Scholar]
- East CE, Begg L, Henshall NE, Marchant PR, Wallace K. Local cooling for relieving pain from perineal trauma sustained during childbirth. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD006304.pub3] [DOI] [PubMed] [Google Scholar]
- Goodman JH. Postpartum depression beyond the early postpartum period. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2003;33:410‐20. [DOI: 10.1177/0884217504266915] [DOI] [PubMed] [Google Scholar]
- Hay‐Smith EJ. Therapeutic ultrasound for postpartum perineal pain and dyspareunia. Cochrane Database of Systematic Reviews 1998, Issue 3. [DOI: 10.1002/14651858.CD000495] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedayati H, Parsons J, Crowther CA. Rectal analgesia for pain from perineal trauma following childbirth. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD003931] [DOI] [PubMed] [Google Scholar]
- Hedayati H, Parsons J, Crowther CA. Topically applied anaesthetics for treating perineal pain after childbirth. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD004223.pub2] [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
- Howard CA. Pharmaceutical Calculations. 14th Edition. Lippincott Williams & Wilkins, 2013. [Google Scholar]
- Irish Pharmaceutical Healthcare Association. Summary of product characteristics Nurofen 200 mg coated tablets. www.medicines.ie2014.
- Kaplowitz N, DeLeve LD. Drug‐induced Liver Disease. 3. London: Elsevier Inc, 2013. [Google Scholar]
- Kettle C. The pelvic floor. In: Henderson C, Macdonald S editor(s). Mayes’ Midwifery: A Textbook for Midwives. Vol. 13, Edinburgh: Bailliere Tindall, 2004. [Google Scholar]
- LacMed, a ToxNet database. U.S. National Library of Medicine, National Institutes of Health, Health & Human Services2015; Vol. toxnet.nlm.nih.gov/.
- Laws P, Sullivan EA. Australia’s Mothers and Babies 2007. AIHW National Perinatal Statistics Unit, Sydney2009.
- Leeman L, Fullilove AM, Borders N, Manocchio R, Albers LL, Rogers RG. Postpartum perineal pain in a low episiotomy setting: association with severity of genital trauma, labor care, and birth variables. Birth 2009;36(4):283‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeser JD, Arendt‐Nielsen L, Baron R, Basbaum A, Bond M, Breivik H, et al. Part III: Pain terms: A current list with definitions and notes on usage. In: Merskey H, Bogduk N editor(s). Classification of Chronic Pain. 2nd Edition. Seattle: International Society of the Study of Pain Press, 2011. [Google Scholar]
- Macarthur AJ, Macarthur C. Incidence, severity, and determinants of perineal pain after vaginal delivery: a prospective cohort study. American Journal of Obstetrics and Gynecology 2004;191(4):1199‐204. [DOI] [PubMed] [Google Scholar]
- Moodley D, Moodley J, Coovadia H, Gray G, McIntyre J, Hofmyer J, et al. A multicenter randomized controlled trial of nevirapine versus a combination of zidovudine and lamivudine to reduce intrapartum and early postpartum mother‐to‐child transmission of human immunodeficiency virus type 1. Journal of Infectious Diseases 2003;187:725–35. [DOI: 0022-1899/2003/18705-0002] [DOI] [PubMed] [Google Scholar]
- Moore A, McQuay H, Gavaghan D. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesics. Pain 1996;66:229–37. [DOI] [PubMed] [Google Scholar]
- Moore A, Moore O, McQuary H, Gavaghan D. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesia: use of pain intensity and visual analogue scales. Pain 1997;96:311–5. [DOI] [PubMed] [Google Scholar]
- Moore A, McQuay H, Gavaghan D. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesia: verification from independent data. Pain 1997;69:127–30. [DOI] [PubMed] [Google Scholar]
- Nicklas JM, Miller LJ, Zera CA, Davis RB, Levkoff SE, Seely EW. Factors associated with depressive symptoms in the early postpartum period among women with recent gestational diabetes mellitus. Maternal and Child Health Journal 2013;17:1665‐72. [DOI: 10.1007/s10995-012-1180-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien KO, Nathanson MS, Mancini J, Witter FR. Calcium absorption is significantly higher in adolescents during pregnancy than in the early postpartum period. American Journal of Clinical Nutrition 2003;78:1188–93. [DOI] [PubMed] [Google Scholar]
- Rainsford KD. Anti‐inflammatory drugs in the 21st century. Sub‐cellular Biochemistry 2007;42:3‐27. [DOI] [PubMed] [Google Scholar]
- Rao PNP, Knaus EE. Evolution of nonsteroidal anti‐inflammatory drugs (NSAIDs): cyclooxygenase (COX) inhibition and beyond. Journal of Pharmacy and Pharmaceutical Sciences 2008;11(2):81s‐110s. [DOI] [PubMed] [Google Scholar]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- Schytt E, Waldenstrom U. Risk factors for poor self‐rated health in women at 2 months and 1 year after childbirth. Journal of Women's Health 2007;16(3):390‐405. [DOI: 10.1089/jwh.2006.0030] [DOI] [PubMed] [Google Scholar]
- Seibert K, Hang Y, Leahy K, Hauser S, Masferrer J, Perkins W, et al. Pharmacological and biochemical demonstration of the role of cyclooxygenase‐2 in inflammation and pain. Proceedings of the National Academy of Sciences of the USA. 1994; Vol. 91:12013‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CJ, Zhang Y, Koboldt CM, Muhammad J, Zweifel BS, Shaffer A, et al. Pharmacological analysis of cyclooxygenase‐1 in inflammation. Proceedings of the National Academy of Sciences of the USA. 1998; Vol. 95:13313‐331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon DH, Schneeweiss S, Glynn RJ, Kiyota Y, Levin R, Mogun H, et al. Relationship between selective cyclooxygenase‐ 2 inhibitors and acute myocardial infarction in older adults. Circulation 2004;109:2068‐73. [DOI] [PubMed] [Google Scholar]
- Teich AS, Barnett J, Bonuck K. Women's perceptions of breastfeeding barriers in early postpartum period: a qualitative analysis nested in two randomized controlled trials. Breastfeeding Medicine 2014;9(1):9‐15. [DOI: 10.1089/bfm.2013.0063] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JF, Roberts CL, Currie M, Ellwood DA. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth 2002;29(2):83‐93. [DOI] [PubMed] [Google Scholar]
- Tramèr MR, Williams JE, Carroll D, Wiffen PJ, Moore RA, McQuay HJ. Comparing analgesic efficacy of non‐steroidal anti‐inflammatory drugs given by different routes in acute and chronic pain: a qualitative systematic review. Acta Anaesthesiologica Scandinavica 1998;42(1):71‐9. [DOI] [PubMed] [Google Scholar]
- Tulder M, Becker A, Bekkering T, Breen A, Real MT, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. European Spine Journal 2006;15 Suppl 2:169‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin‐like drugs. Nature: New Biology 1971;43:232‐5. [DOI] [PubMed] [Google Scholar]
- Voscopoulos C, Lema M. When does acute pain become chronic?. British Journal of Anaesthesia 2010;105 Suppl 1:69‐85. [DOI: 10.1093/bja/aeq323] [DOI] [PubMed] [Google Scholar]
- Vree TB, Biggelaar‐Martea M, Verwey‐van Wissen CP, Vree JB, Guelen PJ. Pharmacokinetics of naproxen, its metabolite O‐desmethylnaproxen, and their acyl glucuronides in humans. Biopharmaceutics & Drug Diposition 1993;14(6):491‐502. [DOI] [PubMed] [Google Scholar]
- Williams A, Herron‐Marx S, Knibb R. The prevalence of enduring postnatal perineal morbidity and its relationship to type of birth and birth risk factors. Journal of Clinical Nursing 2007;16(3):549‐61. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Wuytack F, Smith V. Oral non‐steroidal anti‐inflammatory drugs (single dose) for perineal pain in the early postpartum period. Cochrane Database of Systematic Reviews 2014, Issue 10. [DOI: 10.1002/14651858.CD011352] [DOI] [Google Scholar]


