Introduction
Nonalcoholic fatty liver disease (NAFLD) is a condition where there is accumulation of fat in the liver1,2. Normally there is some fat in the liver; however when the fat content of the liver exceeds about 5–10% of the liver weight then the condition is called steatosis or fatty liver disease3.
While fatty liver disease used to be noted in patients who drank alcohol, patients with NAFLD get such disease without a history of any significant alcohol intake. Interestingly, even under a microscope NAFLD looks very similar to liver disease noted in patients with alcoholic intake4.
Of concern is that NAFLD is becoming a global health problem, with prevalence estimates at 20% to 30% of the general population5. In fact, NAFLD is now the most common liver disease in children today with an estimated prevalence of 7 million affected children in the US6. Reports of NAFLD in patients as young as 2 years of age have been documented. It tends to be more common in children who are obese but has been known to occur in patients who have normal weight7.
Children with NAFLD are at increased risk of early onset type 2 diabetes and NAFLD is estimated to increase the risk of early cardiovascular disease by almost five-fold. Additionally in patients, NAFLD is also closely associated with obesity, lipid abnormalities, hypertension, obstructive sleep apnea as well as polycystic ovary syndrome. Recent data also points to an alteration in the gut microbiota8 in patients with NAFLD as a driver of liver injury5,9. There is increasing evidence that the gut microbiome which has a genomic load almost 100 times of the host can modulate nutrient and bile acid signaling within the gut lumen10 and thus influence gut originating signaling which is known to regulate hepatic health11–13.
NAFLD has been reported in people of all ethnicities and races. While NAFLD is known to be less common in African Americans it occurs most commonly in Hispanic patients. For reasons not completely understood, Asian Americans are more likely to get NAFLD than any other ethnicity or race.
While in NAFLD there is fat accumulation, when there is accompanying inflammation in the liver, then the condition is known as Nonalcoholic steatohepatitis (NASH). The drivers for progression of NAFLD to NASH remains unknown and research into mechanisms of such injury and its progression is a major focus in the field of gastroenterology and hepatology14,15. Additionally the natural progression of NASH in children also remains ill defined. Many children with NASH can develop fibrosis, which is a form of liver scarring1,4. Such fibrosis can advance to cirrhosis and ultimately result in liver failure and the need for liver transplantation to sustain life. In fact, in adults NASH is the second most common cause of liver transplantation. It is generally believed that if this trend is not halted then NASH could fast become the number one cause of liver transplantation in adults16,17. Addressing NASH in the pediatric world can have a major impact in reducing complications as children grow to become adults.
An additional concern in patients with NASH is cancer, which is now the third leading cause of mortality in patients with fatty liver disease18,19. Primary liver tumors have had a significant rise in patient populations and this this thought to be driven at least in part due to NASH.
Clinical Features
A majority of patients with NAFLD / NASH do not report clinical problems and are asymptomatic. Some children can have nonspecific abdominal discomfort below the rib cage or have increased fatigue20. There can also be dark pigmentation of the armpits, knees, knuckles, elbows or neck, which we now know is a sign of insulin resistance. While symptoms of aches and muscle pain, feel of bloating, acid reflux and sleepiness have been reported in patients with NAFLD/NASH, their relationship to the disease process is uncertain and possibly represent complications from obesity which is prominently seen in patients with NAFLD21.
On examination such patients may have liver or splenic enlargement. Signs of liver failure like jaundice, encephalopathy, ascites, abdominal wall angiomata or palmar erythema are rarely noted at presentation in children. However this is being increasing seen in adult patients22,23.
Diagnosing NAFLD/NASH
A liver biopsy remains the gold standard for diagnosing NAFLD or NASH. Previous reliance on serum aminotransferases as well as ultrasound of the liver has not proven to stand the test of time or the rigors of reliability, validity or objectivity. In fact patients with NAFLD and NASH can have normal alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase, and gamma glutamyl transpeptidase (GGT). Ultrasound remains unreliable in diagnosing or estimating the hepatic fat content or inflammation1,24.
Nevertheless, with a paucity of a reliable surrogate marker (other than an invasive liver biopsy), ALT is still widely used in clinical decision making. There has also been recent literature to support the use of newer ALT cutoffs, which lowers the ALT level to 26U/L for boys and 22U/L for girls as a predictor for liver disease. Liver transaminases and GGT remain useful in excluding other causes for liver disease like primary sclerosing cholangitis in pediatric patients25. Thus patients presenting with ALT elevation are routinely tested for a host of liver diseases like autoimmune hepatitis, alpha 1 antitrypsin, Wilson disease, infectious hepatitis to rule out other etiologies. Rare diseases like inborn errors of metabolism, drug toxicities and lysosomal acid lipase deficiency can also present with fat accumulation in the liver and need to be ruled out26.
Given this diagnostic dilemma a general approach is that in the absence of other causes of liver disease, NAFLD can be placed high on the differential diagnosis in an obese patient with ALT elevation. As with any other disease process a thorough history, review of systems, physical examination and laboratory testing is mandatory. Certainly, a confirmation of NAFLD/NASH can be undertaken with a subsequent liver biopsy, which can also help in grading the severity of liver damage3,17.
The liver biopsy is scored based on the NAS (NAFLD activity scoring) system. The degree of hepatic steatosis as well as lobular inflammation is each graded from 0–3. Similarly hepatocyte ballooning is graded from 0–2. The final number is the sum of each of the final steatosis, lobular inflammation and ballooning score, to derive a NAS score. In addition there is grading for the degree of fibrosis. The NAS score and fibrosis can help clinicians in determining the severity of liver disease in patients with NAFLD/NASH24,25.
Laboratory Evaluation
Since in patients presenting with a high ALT and obesity; while NAFLD would be a consideration, given the low specificity and sensitivity of serological testing for NAFLD it is generally recommended that the following testing be performed to rule out other etiologies. Complete Blood Count (CBC), Liver panel, GGT, Prothrombin Time, INR, Lipid panel, TSH, Creatinine Kinase and testing for celiac disease (total IgA and Tissue transglutaminase)27.
Additional testing to rule out other specific liver disease would include a viral hepatitis panel. It is also recommended to test serum ceruloplasmin levels and possibly a 24 hour urinary copper screen if there is suspicion for Wilson Disease (WD). Patients with WD can also have hematological as well as neuropsychiatric problems and a liver biopsy with copper estimation may eventually be needed28,29.
As noted in recent literature, it is important to rule out autoimmune hepatitis and thus a total IgG, anti-nuclear antibody (ANA), liver kidney microsomal antibody and anti-smooth muscle antibody is recommended. Most hepatologists would also recommend testing for alpha 1 antitrypsin with a serum alpha 1 antitrypsin assay3,30. This could be paired with phenotypic/genotypic typing25. Since hepatic fat accumulation, advanced fibrosis as well as lipid dysfunction is noted in lysosomal acid lipase deficiency (LAL-D), some centers recommend an enzyme assay for lysosomal acid lipase activity if the presentation is suspicious for LAL-D25.
While, ultrasound as note above is poorly co-relative of NAFLD/NASH it remains an important modality to rule out hepatic cysts, intra or extra hepatic masses, portal hypertension as well as biliary problems and thus a baseline ultrasound is recommended26.
Newer Diagnostic Modalities
Several diagnostic strategies are being developed to non-invasively (without liver biopsy), diagnose and longitudinally follow NAFLD / NASH31. Estimation of the hepatic fibrosis using a special ultrasound probe which can track hepatic stiffness is increasingly being utilized in research and clinical assessments. Proton Density Fat Fraction (PDFF) which is a Magnetic Resonance Imaging (MRI) based estimation of hepatic fat has also shown significant co-relation with liver biopsy in NAFLD/NASH. Several other blood tests and imaging modalities continue to push the research forward for better diagnostic tools32.
Progression of NAFLD/NASH
Major lacunae in our understanding of fatty liver disease stem from a lack of well-defined pathways that drive fat accumulation and its subsequent culmination in hepatic inflammation33. The earlier idea of a ‘two-hit hypothesis’, where it was believed that there is triglyceride accumulation as a first hit secondary to metabolic syndrome which then leads to the second hit via oxidative stress and progression to hepatitis via the Kupffer cells is increasingly being replaced by the ‘multiple or parallel hit hypothesis4. This has taken greater significance due to recent literature supporting the role of gut microbiota, environmental factors, genetic factors and the knowledge that NASH can occur in lean individuals.
It is thus now believed that inflammation may precede steatosis, and that inflammatory changes are driven due to an early Kupffer cell activation and release of cytokines, via several mechanisms which propagate liver injury, ultimately leading to fibrosis and cirrhosis29.
Treatment/Management
Weight Loss, Exercise and Lifestyle Change
In patients with NAFLD/NASH the only established modality to drive improvement is weight loss and exercise. While diet changes can lead to weight loss and exercise are part of lifestyle modification, they are traditionally very hard to achieve and sustain for long periods. However, it is generally believed that replacing trans and saturated fats with monounsaturated and polyunsaturated fats can reduce cardiac disease in patients with NAFLD34. There has also been recent data supporting the use of omega 3-fatty acids and avoidance of processed foods and diets rich in simple sugars35.
Instead, a diet rich in plant based ingredients has been recommended in several studies. In fact data supports the consumption of whole grains, fruits and vegetables, which are considered low glycemic index foods for beneficial effects in patients with fatty liver disease. Limiting portion sizes is also critically important as part of lifestyle changes in patients with fatty liver disease.
Weight loss has been consistently shown to help patients with NAFLD/NASH. Most studies recommend a gradual weight loss, in association with life style changes. Paradoxically very rapid weight loss can have detrimental side effects and is not encouraged. Several studies have reported an improvement in serology as well as histology upon sustained weight loss and exercise regimen34. A multispecialty family and patient centric approach has been most effective in weight management programs.
Additional liver diseases may complicate NAFLD/NASH. In fact data from adult studies supports that alcohol consumption, especially heavy or binge drinking can drive progressive liver disease and patients should be counseled against alcohol consumption. The physician should review the immunization records to verify vaccination against hepatitis A and B34,36.
Medications
Many medications have been trailed and continue to be tested for NAFLD/NASH. One of the drugs that remains in common use but has not shown to be effective for treatment is Metformin22. Several studies have concluded that Metformin is not superior to placebo in significantly modifying histology or ALT in patients with NAFLD. However Metformin has an important role in patients with diabetes. Many researchers have evaluated the role of antioxidant treatment. In fact some natural antioxidants have been reported to have beneficial effects in NAFLD preclinical models and small pilot clinical studies but none of them are recommended for treatment of NAFLD/NASH and their use needs further research.
Among the many other treatments that continue to be used for NAFLD/NASH is Vitamin E22. While some reports have suggested that vitamin E may have important benefits in modulating histology and serology in patients with NAFLD, there have been recent concerns with regard to its long term safety. Saint Louis University was closely involved in trials of metformin as well as Vitamin E.
A recently trialed drug for use in pediatric NAFLD is Cysteamine bitartrate. Given its antioxidant role it was, tested in children with NAFLD as part of a multicenter trial with Saint Louis University as a study site. Although there was some reduction in hepatic inflammation as well as a decrease in serum aminotransferase with Cysteamine bitartrate, there was no significant improvement in the severity of NAFLD histological markers against placebo treatment23.
There has also been an increased interest in the role of probiotics and prebiotics as a therapeutic option for patients with NAFLD/NASH37. While probiotics are organisms that can reside as commensals in the host to modulate the intestinal microbiome and influence gut-systemic signaling, prebiotics are ingredients that can stimulate the growth and / or activity of gut bacteria for the benefit of the host38. Given that both probiotics and prebiotics have been used in patients with several gastrointestinal diseases (like diarrhea, inflammatory bowel disease, etc.), there is a large body of clinical expertise that affirms to their perceived safety for human use39. However a unified approach to their dosing, selection and attestation to their efficacy in patients with NAFLD remains a focus for several research studies.
Bariatric Surgery
While bariatric surgery remains an option40, it is reserved for patients at significant risks of continued morbidity and mortality in whom medical measures have failed. It has been speculated that improvement in NAFLD/NASH post bariatric surgery is not only due to weight loss but also driven by an alteration of bile acid homeostasis due to the renewed anatomy created via the bypass procedure. It has been postulated that there is a significant influence on liver histology via an alteration of gut derived signals in patients post bypass surgery41,42. The surgery is also known to induce adaptive changes in gut morphology as well as changes in the absorption of micro and macronutrients43,44. In fact recently Saint Louis University physicians led an NIH funded research workshop evaluating the role of the gut in modulating disease in patients post bariatric surgery41.
Follow-up
It is generally recommended that patients with NAFLD/NASH have close follow-up. Many physicians routinely measure ALT levels as well as anthropometrics to monitor patients every three to six month; however it is well known that changes in ALT do not always track disease severity. Some centers also recommend a repeat liver biopsy, however protocols for such continue to be developed based ongoing research and the increased availability or noninvasive testing.
NIH NIDDK NASH CRN
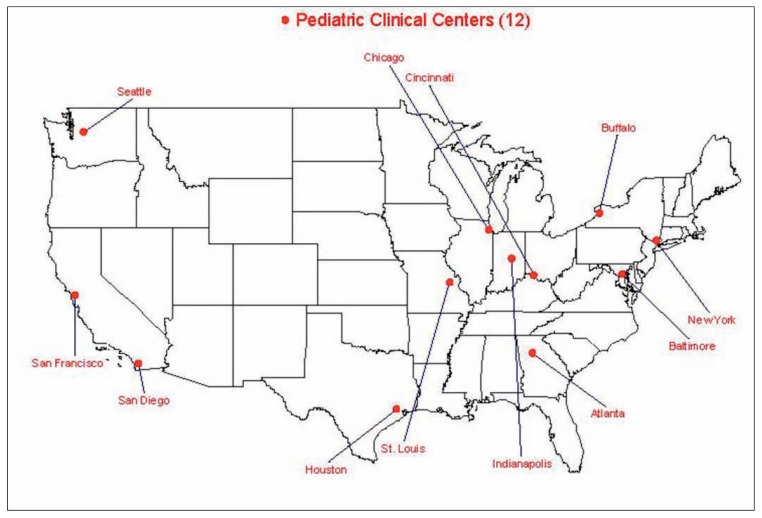
To further our understanding of NAFLD / NASH, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) sponsored the creation of the Clinical Research Network (CRN) in Nonalcoholic Steatohepatitis (NASH). A major focus of the NASH CRN is to collaboratively work on the etiology, the contributing factors, natural history, associated complications, and therapy of NAFLD and NASH23,45.
This consortium includes 12 pediatric centers, including Saint Louis University. Figure 1, throughout the US and several adult clinical sites throughout the country.
Figure 1.
Pediatric Clinical Centers – NASH CRN
The NASH CRN has been at the forefront in our understanding of NAFLD/NASH and the development of both diagnostic and therapeutic modalities. Evaluating the utility of Vitamin E, Metformin, as well as the anti-oxidant Cysteamine bitartrate has been systemically tested in children as part of NASH CRN funded studies. The NASH CRN continues to work on developing diagnostics and therapeutics to advance our understanding of pediatric fatty liver disease31,46. Figure 1.
Footnotes
Ajay Jain, MD, is in the Department of Pediatrics, Saint Louis University, St. Louis, Missouri.
Contact: ajain3@slu.edu
Disclosure
None reported.
References
- 1.Satapathy SK, Sanyal AJ. Epidemiology and Natural History of Nonalcoholic Fatty Liver Disease. Seminars in liver disease. 2015;35(3):221–35. doi: 10.1055/s-0035-1562943. [DOI] [PubMed] [Google Scholar]
- 2.Streba LA, Vere CC, Rogoveanu I, Streba CT. Nonalcoholic fatty liver disease, metabolic risk factors, and hepatocellular carcinoma: an open question. World journal of gastroenterology : WJG. 2015;21(14):4103–10. doi: 10.3748/wjg.v21.i14.4103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suzuki A, Diehl AM. Nonalcoholic Steatohepatitis. Annu Rev Med. 2017;68:85–98. doi: 10.1146/annurev-med-051215-031109. [DOI] [PubMed] [Google Scholar]
- 4.Vos MB. Nutrition, nonalcoholic fatty liver disease and the microbiome: recent progress in the field. Curr Opin Lipidol. 2014;25(1):61–6. doi: 10.1097/MOL.0000000000000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2017 doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 6.Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123–33. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577–86. doi: 10.1002/hep.28785. [DOI] [PubMed] [Google Scholar]
- 8.Loomba R, Seguritan V, Li W, et al. Gut Microbiome-Based Metagenomic Signature for Non-invasive Detection of Advanced Fibrosis in Human Nonalcoholic Fatty Liver Disease. Cell metabolism. 2017;25(5):1054–62 e5. doi: 10.1016/j.cmet.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quigley EM, Stanton C, Murphy EF. The gut microbiota and the liver. Pathophysiological and clinical implications. Journal of hepatology. 2013;58(5):1020–7. doi: 10.1016/j.jhep.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 10.Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457(7228):480–4. doi: 10.1038/nature07540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain AK, Sharma A, Arora S, et al. Preserved Gut Microbial Diversity Accompanies Upregulation of TGR5 and Hepatobiliary Transporters in Bile Acid-Treated Animals Receiving Parenteral Nutrition. JPEN Journal of parenteral and enteral nutrition. 2016 doi: 10.1177/0148607116661838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giannelli V, Di Gregorio V, Iebba V, et al. Microbiota and the gut-liver axis: bacterial translocation, inflammation and infection in cirrhosis. World journal of gastroenterology : WJG. 2014;20(45):16795–810. doi: 10.3748/wjg.v20.i45.16795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krajmalnik-Brown R, Ilhan ZE, Kang DW, DiBaise JK. Effects of gut microbes on nutrient absorption and energy regulation. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition. 2012;27(2):201–14. doi: 10.1177/0884533611436116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foster BA, Farragher J, Parker P, Sosa ET. Treatment Interventions for Early Childhood Obesity: A Systematic Review. Academic pediatrics. 2015;15(4):353–61. doi: 10.1016/j.acap.2015.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arena R, Guazzi M, Lianov L, et al. Healthy Lifestyle Interventions to Combat Noncommunicable Disease-A Novel Nonhierarchical Connectivity Model for Key Stakeholders: A Policy Statement From the American Heart Association, European Society of Cardiology, European Association for Cardiovascular Prevention and Rehabilitation, and American College of Preventive Medicine. Mayo Clinic proceedings. 2015 doi: 10.1016/j.mayocp.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 16.Kelishadi R, Azizi-Soleiman F. Controlling childhood obesity: A systematic review on strategies and challenges. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences. 2014;19(10):993–1008. [PMC free article] [PubMed] [Google Scholar]
- 17.Rinella ME. Nonalcoholic fatty liver disease: a systematic review. Jama. 2015;313(22):2263–73. doi: 10.1001/jama.2015.5370. [DOI] [PubMed] [Google Scholar]
- 18.Zoller H, Tilg H. Nonalcoholic fatty liver disease and hepatocellular carcinoma. Metabolism. 2016;65(8):1151–60. doi: 10.1016/j.metabol.2016.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Marengo A, Rosso C, Bugianesi E. Liver Cancer: Connections with Obesity, Fatty Liver, and Cirrhosis. Annu Rev Med. 2016;67:103–17. doi: 10.1146/annurev-med-090514-013832. [DOI] [PubMed] [Google Scholar]
- 20.Singer C, Stancu P, Cosoveanu S, Botu A. Non-alcoholic Fatty liver disease in children. Current health sciences journal. 2014;40(3):170–6. doi: 10.12865/CHSJ.40.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brunt EM, Tiniakos DG. Histopathology of nonalcoholic fatty liver disease. World journal of gastroenterology : WJG. 2010;16(42):5286–96. doi: 10.3748/wjg.v16.i42.5286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lavine JE, Schwimmer JB, Van Natta ML, et al. Effect of vitamin E or metformin for treatment of nonalcoholic fatty liver disease in children and adolescents: the TONIC randomized controlled trial. Jama. 2011;305(16):1659–68. doi: 10.1001/jama.2011.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwimmer JB, Lavine JE, Wilson LA, et al. In Children With Nonalcoholic Fatty Liver Disease, Cysteamine Bitartrate Delayed Release Improves Liver Enzymes but Does Not Reduce Disease Activity Scores. Gastroenterology. 2016;151(6):1141–54 e9. doi: 10.1053/j.gastro.2016.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Byrne CD, Targher G. NAFLD: a multisystem disease. Journal of hepatology. 2015;62(1 Suppl):S47–64. doi: 10.1016/j.jhep.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Kohli R, Sunduram S, Mouzaki M, et al. Pediatric Nonalcoholic Fatty Liver Disease: A Report from the Expert Committee on Nonalcoholic Fatty Liver Disease (ECON) The Journal of pediatrics. 2016;172:9–13. doi: 10.1016/j.jpeds.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schwimmer JB. Clinical advances in pediatric nonalcoholic fatty liver disease. Hepatology. 2016;63(5):1718–25. doi: 10.1002/hep.28441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schneier AT, Citti CC, Dieterich DT. Management and diagnosis of fatty liver disease. Expert Rev Gastroenterol Hepatol. 2015;9(5):671–83. doi: 10.1586/17474124.2015.1003209. [DOI] [PubMed] [Google Scholar]
- 28.Wooton-Kee CR, Jain AK, Wagner M, et al. Elevated copper impairs hepatic nuclear receptor function in Wilson’s disease. The Journal of clinical investigation. 2015;125(9):3449–60. doi: 10.1172/JCI78991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Antonucci L, Porcu C, Iannucci G, Balsano C, Barbaro B. Non-Alcoholic Fatty Liver Disease and Nutritional Implications: Special Focus on Copper. Nutrients. 2017;9(10) doi: 10.3390/nu9101137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teckman JH, Jain A. Advances in alpha-1-antitrypsin deficiency liver disease. Current gastroenterology reports. 2014;16(1):367. doi: 10.1007/s11894-013-0367-8. [DOI] [PubMed] [Google Scholar]
- 31.Vuppalanchi R, Jain AK, Deppe R, et al. Relationship between changes in serum levels of keratin 18 and changes in liver histology in children and adults with nonalcoholic fatty liver disease. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2014;12(12):2121–30 e1–2. doi: 10.1016/j.cgh.2014.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Middleton MS, Heba ER, Hooker CA, et al. Agreement Between Magnetic Resonance Imaging Proton Density Fat Fraction Measurements and Pathologist-Assigned Steatosis Grades of Liver Biopsies From Adults With Nonalcoholic Steatohepatitis. Gastroenterology. 2017;153(3):753–61. doi: 10.1053/j.gastro.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paradies G, Paradies V, Ruggiero FM, Petrosillo G. Oxidative stress, cardiolipin and mitochondrial dysfunction in nonalcoholic fatty liver disease. World journal of gastroenterology : WJG. 2014;20(39):14205–18. doi: 10.3748/wjg.v20.i39.14205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harlow KE, Africa JA, Wells A, et al. Clinically Actionable Hypercholesterolemia and Hypertriglyceridemia in Children with Nonalcoholic Fatty Liver Disease. The Journal of pediatrics. 2018;198:76–83 e2. doi: 10.1016/j.jpeds.2018.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Obert J, Pearlman M, Obert L, Chapin S. Popular Weight Loss Strategies: a Review of Four Weight Loss Techniques. Current gastroenterology reports. 2017;19(12):61. doi: 10.1007/s11894-017-0603-8. [DOI] [PubMed] [Google Scholar]
- 36.Hassan K, Bhalla V, El Regal ME, HHAK Nonalcoholic fatty liver disease: a comprehensive review of a growing epidemic. World journal of gastroenterology : WJG. 2014;20(34):12082–101. doi: 10.3748/wjg.v20.i34.12082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DiBaise JK, Zhang H, Crowell MD, Krajmalnik-Brown R, Decker GA, Rittmann BE. Gut microbiota and its possible relationship with obesity. Mayo Clinic proceedings. 2008;83(4):460–9. doi: 10.4065/83.4.460. [DOI] [PubMed] [Google Scholar]
- 38.Esteve E, Ricart W, Fernandez-Real JM. Gut microbiota interactions with obesity insulin resistance and type 2 diabetes: did gut microbiote co-evolve with insulin resistance? Current opinion in clinical nutrition and metabolic care. 2011;14(5):483–90. doi: 10.1097/MCO.0b013e328348c06d. [DOI] [PubMed] [Google Scholar]
- 39.Liou AP, Paziuk M, Luevano JM, Jr, Machineni S, Turnbaugh PJ, Kaplan LM. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Science translational medicine. 2013;5(178):178ra41. doi: 10.1126/scitranslmed.3005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Golzarand M, Toolabi K, Farid R. The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surgical endoscopy. 2017;31(11):4331–45. doi: 10.1007/s00464-017-5505-1. [DOI] [PubMed] [Google Scholar]
- 41.Jain AK, le Roux CW, Puri P, et al. Proceedings of the 2017 ASPEN Research Workshop-Gastric Bypass: Role of the Gut. JPEN Journal of parenteral and enteral nutrition. 2018;42(2):279–95. doi: 10.1002/jpen.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kohli R, Kirby M, Setchell KD, et al. Intestinal adaptation after ileal interposition surgery increases bile acid recycling and protects against obesity-related comorbidities. American journal of physiology Gastrointestinal and liver physiology. 2010;299(3):G652–60. doi: 10.1152/ajpgi.00221.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tremaroli V, Karlsson F, Werling M, et al. Roux-en-Y Gastric Bypass and Vertical Banded Gastroplasty Induce Long-Term Changes on the Human Gut Microbiome Contributing to Fat Mass Regulation. Cell metabolism. 2015;22(2):228–38. doi: 10.1016/j.cmet.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwenger KJP, Fischer SE, Jackson TD, Okrainec A, Allard JP. Non-alcoholic Fatty Liver Disease in Morbidly Obese Individuals Undergoing Bariatric Surgery: Prevalence and Effect of the Pre-Bariatric Very Low Calorie Diet. Obesity surgery. 2017 doi: 10.1007/s11695-017-2980-3. [DOI] [PubMed] [Google Scholar]
- 45.Bazick J, Donithan M, Neuschwander-Tetri BA, et al. Clinical Model for NASH and Advanced Fibrosis in Adult Patients With Diabetes and NAFLD: Guidelines for Referral in NAFLD. Diabetes Care. 2015;38(7):1347–55. doi: 10.2337/dc14-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brunt EM. Nonalcoholic Fatty Liver Disease: Pros and Cons of Histologic Systems of Evaluation. Int J Mol Sci. 2016;17(1) doi: 10.3390/ijms17010097. [DOI] [PMC free article] [PubMed] [Google Scholar]