Abstract
Background:
Patients can present with symptomatic gallbladder disease after cholecystectomy due to a remnant gallbladder. This is a rare problem and challenging diagnosis with limited prior characterization, thus we present a large series of patients with a gallbladder remnant.
Methods:
A retrospective review was performed of all patients presenting with symptomatic gallbladder remnant at a tertiary care center from 2002–2016. Data on presenting symptoms, diagnostic tests, treatments, and follow-up were collected.
Results:
Thirty-one patients diagnosed and treated for a symptomatic gallbladder remnant were identified. The most common presenting symptoms included right upper quadrant pain (87%) and nausea (55%). The median time from symptom presentation to definitive diagnosis was 60 days. Diagnostic modalities utilized in the evaluation of these patients demonstrated that ERCP and MRCP were effective with sensitivities of 85% and 90%, respectively. Twenty-three (76.2%) patients underwent completion cholecystectomy, which proved to be definitive treatment. Additionally, 8 (25.8%) patients were non-operative candidates and underwent ERCP and sphincterotomy, 3 of whom developed recurrent symptoms.
Conclusion:
A symptomatic gallbladder remnant after cholecystectomy is infrequently seen, however the diagnosis should be considered in patients with recurrent biliary symptoms after cholecystectomy. Completion cholecystectomy can be challenging but is highly effective for definitive treatment.
Keywords: Remnant gallbladder, retained gallbladder, partial cholecystectomy
INTRODUCTION
Cholecystectomy is the treatment of choice for symptomatic gallbladder disease with approximately 700,000 performed each year in the United States.[1] Unfortunately, between 5 and 47% of patients present post-operatively with recurrent gastrointestinal symptoms such as abdominal pain, dyspepsia, nausea, vomiting, fever, diarrhea, and jaundice.[2–5] The etiology of the majority of these symptoms are extra-biliary, comprising diagnoses such as peptic ulcer disease, gastroesophageal reflux disease, and irritable bowel syndrome. However, some patients present with symptoms referable to the biliary tract, including: biliary strictures, biliary leaks, retained or recurrent stones, etc.[6,7] A small minority are diagnosed with recurrent gallbladder disease secondary to a remnant gallbladder, often in the setting of acute cholecystitis, symptomatic cholelithiasis, choledocholithiasis, gallstone pancreatitis, and/or cholangitis.[8]
A remnant gallbladder, first reported by Beye in 1936, was described as the “wider part of the free end of the remnant cystic duct, giving the impression of a diminutive gallbladder.”[9,10] It results from incomplete resection, either unintended or deliberate, during cholecystectomy. Prior studies indicate its occurrence following both open and laparoscopic cholecystectomies without a difference in frequency between the two approaches.[11–18] Symptoms of a remnant gallbladder may arise shortly after a surgery or many years later.[19] Upon presentation, providers often overlook a remnant gallbladder as a potential diagnosis given the patient’s history of cholecystectomy and rarity of the condition. Consequently, patients frequently endure persistent symptoms, while undergoing multiple diagnostic and therapeutic procedures, before the diagnosis is made. One potential reason for this lengthened diagnostic time is the relative dearth of reports describing diagnostic and treatment options for this entity.
Currently, there are no large-scale studies published that have reported the clinical outcomes of patients diagnosed with remnant gallbladder disease. Since the diagnosis and treatment outcomes of this population are relatively limited, the objective of this study is to review our experience with the presenting symptoms, diagnostic work-up, and management of patients with a gallbladder remnant. We hope to heighten the awareness of this entity in the differential diagnosis of post-cholecystectomy syndromes.
METHODS
We performed a retrospective chart review of all patients evaluated or treated for a symptomatic remnant gallbladder at Barnes-Jewish Hospital, a tertiary care center, from 2002 to 2016. Approval for the study was obtained from the Washington University Institutional Review Board (#201406145). Patients who underwent index cholecystectomy at Barnes-Jewish Hospital or an outside hospital were included. The diagnosis of remnant gallbladder was based on available imaging exams and confirmed by reviewing the operative and pathology reports, in patients who had surgery. Data from clinical records were reviewed and subsequently extracted for analysis. This included demographic, past medical and surgical history, clinical presentation, diagnostic studies, therapeutic interventions, and outcomes.
RESULTS
Thirty-one patients with a remnant gallbladder diagnosis were identified in our review. The mean age at diagnosis was 51±17 years, with 71% of the patients being female and 84% Caucasian. See Table 1 for a summary of patient demographic data. Twenty-seven (87%) patients underwent their index cholecystectomy at an outside hospital. The most common symptoms at presentation included right upper quadrant pain (77%), nausea (44%), vomiting (31%), and fever (19%). Subsequently, the indications for the index operations were acute cholecystitis (58%), symptomatic cholelithiasis (29%), and choledocholithiasis (3%).
Table 1.
Patient Demographics
| Patient Factor | Result |
|---|---|
| Number of patients in study | 31 |
|
Age* Mean ± SD (range) |
51±17 (21–81) |
|
BMI Mean ± SD (range) |
31.37 ± 6.59 (21–53) |
|
Gender Female Male |
22 (71%) 9 (29%) |
|
Race White Black Asian |
26 (83.9%) 4 (12.9%) 1 (3.2%) |
|
Smoker Yes No Unknown |
5 (16.1%) 25 (80.6%) 1 (3.2%) |
|
Alcohol Use Yes No Unknown |
3 (9.7%) 27 (87.1%) 1 (3.2%) |
At time of diagnosis of remnant gallbladder
Review of the operative reports revealed that 5 (16%) were planned as open operations with the remaining 24 (77%) planned as laparoscopic. Operative reports of two patients could not be obtained, therefore the method of their index surgery is unknown. Of the 24 laparoscopic cases, 11 were converted to open procedures. Reasons for conversion included adhesions (8 patients), bleeding (1 patient), and intrahepatic gallbladder (1 patient). Of note, one case could not be completed even after conversion to an open procedure, thus was transferred to Barnes-Jewish Hospital for completion of the cholecystectomy. Detailed within the operative reports of the index procedures the surgeons documented challenging dissections, referencing “extensive inflammation” and/or “adhesions” in the operative notes of 11(36%) and 10 (32%) of the cases, respectively. Four (13%) patients had descriptions of gangrenous gallbladders, and four patients had descriptions of hydrops of the gallbladder. In six (19%) cases the operative report explicitly stated that a subtotal cholecystectomy was performed due to the difficulty. Four of these were performed with a reconstituting technique28, however the technique performed for the other two could not be determined. Five (16%) patients underwent intraoperative cholangiogram. Five (16%) patients had a post-operative biliary leak, which was treated with ERCP stent placement and sphincterotomy. One patient developed a right upper quadrant fluid collection, which was found to be serous on percutaneous drainage.
Symptoms began from three days to 41 years (median 2 years) after index cholecystectomy. All patients complained of abdominal pain, in the epigastric and/or right upper quadrant regions. This was similar in character to their pain prior to cholecystectomy in 52% of patients. Most pain was colicky, while some patients’ pain evolved acutely into constant pain. A variety of other signs and symptoms were observed, including nausea (17), vomiting (15), back pain (6) fever (5), diarrhea (3), jaundice (3), acholic stools (2), dark urine (2), and rigors (1). Eleven patients had elevated liver enzymes, 10 had elevated alkaline phosphatase, 9 had elevated total bilirubin, 6 patients had an elevated white blood cell count, and 3 had an elevated lipase.
There were a wide variety of diagnostic modalities utilized in the evaluation of these patients. An average of 3 (range 1–8) total diagnostic tests were performed on patients in the process of diagnosing a remnant gallbladder. The initial imaging modality utilized most often was abdominal CT scan, which was performed in 23 patients and identified a remnant gallbladder in 16 for a sensitivity of 70%. See Figure 1 for a representative CT of a remnant gallbladder. Abdominal ultrasound was performed in 16 patients and identified a remnant gallbladder in 13, for a sensitivity of 81%. Ten patients underwent MRCP and 9 were diagnosed with a remnant gallbladder, for a sensitivity of 90% (Figure 2). ERCP was performed in 20 and was diagnostic in 17, for a sensitivity of 85% (Figure 3). Additional studies performed included HIDA, endoscopic ultrasound, esophagogastroduodenoscopy, gastric emptying studies, and esophageal manometry. CT and ultrasound made the initial correct diagnosis in 10 patients each. ERCP and MRCP each first diagnosed 5 patients. Of note, seven patients had imaging that became diagnostic once read by Barnes Jewish Hospital specialized radiologists. Evaluation lead to the diagnosis of remnant gallbladder in as little as one day to as late as 11 years (median 2 months), after initial symptoms. Time from initial cholecystectomy to remnant gallbladder treatment was a median of 4 years (range: 22 days to 42 years).
Figure 1.
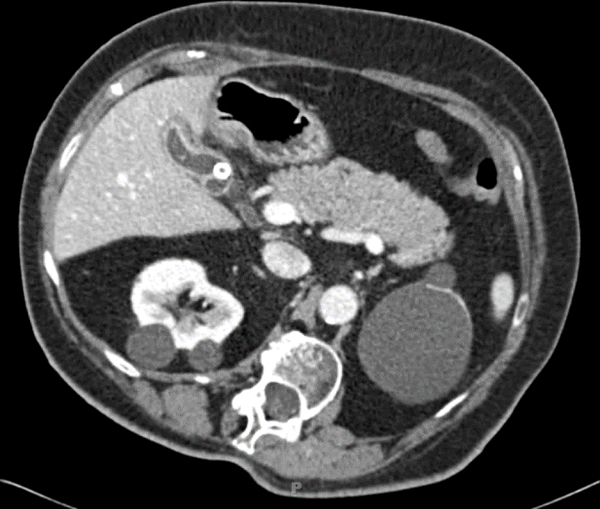
CT scan showing calculi within remnant gallbladder and gallbladder wall thickening.
Figure 2.
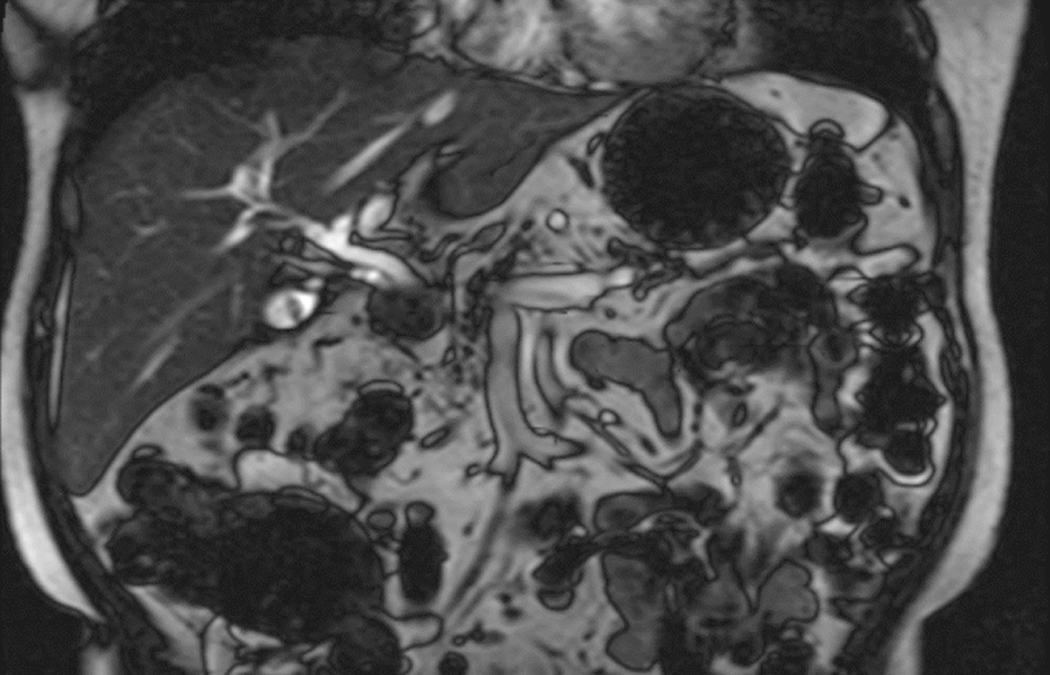

Retained gallbladder remnant identified by MRCP showing (a) cystic structure in the gallbladder fossa with internal filling defect and (b) cholelithiasis with choledocholithiasis resulting in mild intrahepatic dilatation.
Figure 3.
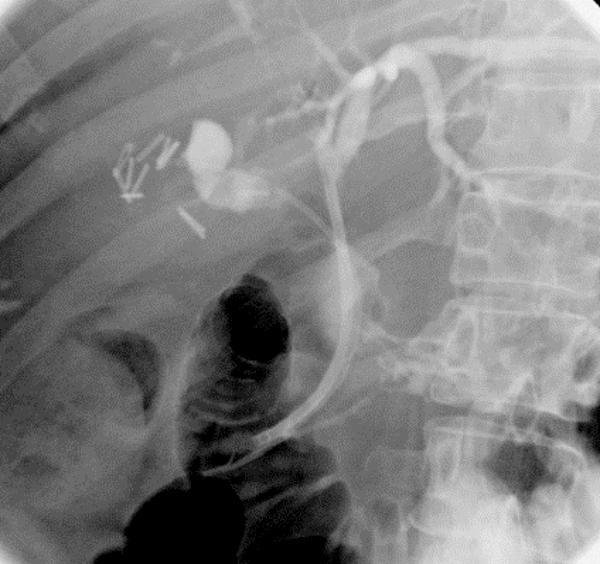
ERCP with stones in cystic duct exerting mass effect on common bile duct. Note the large number of clips within the gallbladder fossa.
Of the 31 patients, 23(76.2%) underwent completion cholecystectomy which definitely treated the symptoms in 100% of patients. The indication for surgery was biliary colic in 13 patients, choledocholithiasis in 6 patients, acute cholecystitis in 3 patients, and gallstone pancreatitis in 1 patient. The majority underwent open cholecystectomy (17 patients), one of which was laparoscopic converted to open surgery due to adhesions. The remaining six patients underwent laparoscopic cholecystectomy. In five patients an intraoperative cholangiogram was performed. Two patients had postoperative complications. One patient had a superficial surgical site infection treated with antibiotics. The other patient, necessitated readmission, for dehydration and diarrhea treated by intravenous fluids. On final pathology, chronic cholecystitis was identified in 17 (74%) patients, cholelithiasis in 14 (61%) patients, acute cholecystitis in three (13%) patients, and a cholecystoenteric fistula in one (4%) patient.
The remaining eight patients were treated with ERCP and sphincterotomy. One patient was also treated with lithotripsy. Six were not felt to be candidates for surgery due to comorbidities, while the other two were referred for surgery, but lost to follow-up. The final diagnoses were choledocholithiasis in four patients, gallstone pancreatitis in two patients, and cholangitis in two patients. There were no ERCP-related complications.
The average follow-up after treatment for the remnant gallbladder was 3.4 years. After completion cholecystectomy, only one patient had symptom recurrence. He presented six years after surgery with choledocholithiasis and was successfully treated with ERCP. Of the eight patients treated non-operatively with ERCP, 3 had recurrent symptoms necessitating admission, presenting 1.5 months to 3 years after treatment. All three were diagnosed with recurrent choledocholithiasis and underwent repeat ERCP.
DISCUSSION
Residual gallstone disease occurs in only 0.18% of laparoscopic cholecystectomies, thus it requires a high index of suspicion for diagnosis. [16] In our study, four patients had an extensive extra-biliary investigation with up to three years of pain and symptoms, prior to having a biliary workup and treatment. One patient had percutaneous drainage of the remnant gallbladder and antibiotic treatment, due to misdiagnosis as an infected biloma. Three other patients were diagnosed with reflux disease and treated over multiple years before persistent symptoms led to further workup, diagnosis, and completion cholecystectomy. Zhu et al. reported that three of their 11 cases were erroneously diagnosed with esophagitis and/or gastritis prior to definitive treatment. [20]
The barrier to diagnosis may be due to limited information on symptomatic remnant gallbladder disease. A PubMed search (performed on May 8, 2018) for “gallbladder remnant,” “retained gallbladder,” and “residual gallbladder” returned 17 publications, most of which were single case reports. The six modern case series identified are summarized in Table 3. These series include 3 to 11 patients with time spans ranging from 3 to 9 years. It has been shown both, in our series and the literature that patients present over a highly variable and wide-ranging amount of time after initial cholecystectomy (range, 1 month to 40 years).[13,16–20] CT, MRCP, ultrasound, and ERCP were used most often for diagnosis, with MRCP being the only modality used in all studies. The definitive treatment in every study was completion cholecystectomy, either open or laparoscopic. In addition, one study utilized extracorporeal shockwave therapy and endoscopic biliary laser lithotripsy for treatment. [13]
Table 3.
Modern case-series of patients treated with remnant gallbladder
| Reference | Time span of study |
Number of patients |
Mean age in years (range) |
Initial surgical procedure |
Presentation of remnant gallbladder |
Average years from initial surgery to secondary intervention (range) |
Diagnostic modalities |
Treatment |
|---|---|---|---|---|---|---|---|---|
| Walsh R et al. 2002*13 | 1/1994–12/2000 | 7 | 50 (35–70) | Open cholecystectomy, laparoscopic cholecystectomy |
Recurrent biliary symptoms, jaundice, pancreatitis |
9.5 (1.2–20) | ERCP, MRCP | Open cholecystectomy, extracorporeal shockwave therapy, laparoscopic cholecystectomy, endoscopic biliary holmium laser lithotripsy |
| Tantia O et al. 2008 18 | 1/2001–12/2006 | 7 | 52.6 (22–70) | Open cholecystectomy, laparoscopic cholecystectomy |
Recurrent biliary symptoms |
12.9 (1–40) | US, ERCP, MRCP | Laparoscopic cholecystectomy |
| Demetriades H et al. 2008 17 | 11/2000–10/2003 | 3 | 55.3 (52–58) | Laparoscopic cholecystectomy |
Recurrent biliary symptoms, jaundice |
2.94 (0.3–5) | US, CT, ERCP, MRCP | Laparoscopic cholecystectomy |
| Chowbey P et al. 2010 16 | 1/1998–12/2007 | 3 | 51 (32–67) | Open partial cholecystectomy, laparoscopic cholecystectomy |
Recurrent biliary symptoms, jaundice |
4.1 (0.5–12) | US, ERCP, MRCP, EUS | Laparoscopic cholecystectomy |
| Jayant M et al. 2013 19 | - | 7 | 43.4 (29–70) | Open partial cholecystectomy |
Recurrent biliary symptoms, jaundice, biliary pancreatitis, acute cholecystitis |
5.2 (1–12) | US, CT, MRCP | Cholecystectomy, ERCP |
| Zhu J et al. 2015* 20 | 1/2010–9/2013 | 11 | 62 (33–83) | Open cholecystectomy, laparoscopic cholecystectomy |
Recurrent biliary symptoms, jaundice |
13 (4–23) | CT, MRCP | Open cholecystectomy, laparoscopic cholecystectomy |
| Current series | 1/2002–12/2016 | 31 | 50 (21–81) | Open cholecystectomy, laparoscopic cholecystectomy, partial cholecystectomy |
Recurrent biliary symptoms, jaundice, pancreatitis, acute cholecystitis, cholangitis |
6.3 (0.1–42) | US, ERCP, MRCP, EUS, esophageal manometry, HIDA, gastric emptying study |
Open cholecystectomy, laparoscopic cholecystectomy, ERCP |
When assessing a patient with post-cholecystectomy symptoms, one must carefully review the operative history. Only 5% of all elective laparoscopic cholecystectomies are converted to open, typically due to inflammation and adhesions impairing safe dissection.[21] This inflammatory environment predisposes the patient to having, intentionally or unintentionally, a gallbladder remnant left behind.[19,22 ] In our series, 11 patients had a laparoscopic converted to open cholecystectomy at the initial surgery. Thus, a history of “complicated” or “difficult” cholecystectomy, particularly a laparoscopic converted to open cholecystectomy, should increase the suspicion of a remnant gallbladder.
We recommend abdominal ultrasound as the initial imaging modality of choice. In addition to being inexpensive, widely available and easily accessible, ultrasound has a sensitivity greater than 95% for gallstones.[23] We found a sensitivity of 81% for the diagnosis of remnant gallbladders. Consider CT, if ultrasound is inconclusive or MRCP if clinical suspicion is high that the pain is of hepatobiliary origin. MRCP is highly diagnostic for remnant gallbladder and remnant cystic duct pathologies.[24–27] Additionally, MRCP provides information about the location of retained stones and the length and nature of the cystic duct. Of note, seven of the patients in our series had prior studies, which became diagnostic once reviewed by our radiologists who specialize in abdominal imaging. It may be advantageous to consider consultation of specialists at a tertiary care center, where they have more exposure to rare problems, such as this.
Once the diagnosis of symptomatic remnant gallbladder has been made, completion cholecystectomy is the definitive treatment. In 1966, Bodvall published a series of 26 cases of symptomatic remnant gallbladders that were effectively treated by cholecystectomy.[9] Subsequently, both open and laparoscopic resections have been described.[11–18] The decision to choose one versus the other should be based on the laparoscopic capabilities of the institution with a low threshold for conversion to open surgery. If presenting with choledocholithiasis, the patient should have therapeutic ERCP prior to surgery or intraoperative cholangiogram. In our institution, both options are used and the decision is attending-driven. Intraoperative cholangiogram should also be performed if the biliary anatomy is unclear.
These can be challenging cases due to the complex re-operative field and delay between presentation and diagnosis, so there should be a low threshold for referral to an experienced hepatobiliary center. If the cystic duct can be safely isolated, the procedure can be treated much like a routine cholecystectomy. However, if this dissection is not possible due to inflammation and/or fibrosis, our preferred technique is a subtotal cholecystectomy without ligation or over-sewing of the gallbladder remnant in order to avoid creating another remnant gallbladder. The technique used at our institution has been previous been published for performing a subtotal fenestrating cholecystectomy in difficult cholecystectomies.[28] When performing a sub-total cholecystectomy we recommend a fenestrating cholecystectomy because it is less likely to result in a remnant gallbladder. However, we must acknowledge that although a reconstituting cholecystectomy has an increased risk of a remnant gallbladder, there is a decreased risk of bile fistula. For patients who are not surgical candidates, ERCP can be utilized to treat choledocholithiasis and its complications, however, there is a significant risk of recurrent symptoms.
CONCLUSION
Recurrent biliary symptoms caused by a remnant gallbladder after cholecystectomy are rare. However, given the long delays in diagnosis, characteristic presentations, and effectiveness of completion cholecystectomy, there are likely numerous patients who could be helped by increased provider awareness. The diagnosis should be considered in all patients with recurring symptoms consistent with biliary disease. Completion cholecystectomy provides definitive treatment for healthy patients with a symptomatic remnant gallbladder.
Table 2.
Imaging and diagnostic modalities utilized in the evaluation of post-cholecystectomy syndrome
| Investigation | Number performed |
Number diagnosed |
Sensitivity | First study to diagnose the remnant |
|---|---|---|---|---|
| Ultrasound | 16 | 13 | 81% | 10 |
| CT | 23 | 16 | 70% | 10 |
| ERCP | 20 | 17 | 85% | 5 |
| MRCP | 10 | 9 | 90% | 5 |
| HIDA | 7 | 3 | 41% | 0 |
| EUS | 2 | 1 | 50% | 1 |
| Upper Endoscopy | 4 | 0 | 0% | 0 |
| Esophageal Manometry |
1 | 0 | 0% | 0 |
| Gastric emptying study |
1 | 0 | 0% | 0 |
CREDITS/GRANT ACKNOWLEDGMENTS
REDCap Supported by Clinical and Translational Science Award (CTSA) Grant [UL1 TR000448] and Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant P30 CA091842.
Footnotes
DISCLOSURES
Dr. Hammill reports other from Medtronic, other from Novadaq, other from Intuitive Surgical, from null, outside the submitted work. Drs. Hawkins, Fowler, Grossman & Mr. Williams and Johnston have no conflicts of interest or financial ties to disclose.
REFERENCES
- 1.Shaffer E (2005) Epidemiology and risk factors for gallstone disease: Has the paradigm changed in the 21st century? Curr Gastroenterology Reps 7:132–140. [DOI] [PubMed] [Google Scholar]
- 2.Glasgow R, Mulvihill S (2006) Treatment of gallstone disease In: Feldman M, Friedman L, Brandt L (8th eds), Sleisenger & Fordtran’s gastrointestinal and liver diseases, Saunders, Philadelphia,pp 1419–1437. [Google Scholar]
- 3.Bisgaard T, Rosenberg J, Kehlet H (2005) From acute to chronic pain after laparoscopic cholecystectomy: A prospective follow-up analysis. Scand J Gastroenterol 40:1358–1364. [DOI] [PubMed] [Google Scholar]
- 4.Russello D, Di Stefano A, Scala R, Favetta A, Emmi S, Guastella T, et al. (1997) Does cholecystectomy always resolve biliary disease? Minerva Chir 52:1435–1439. [PubMed] [Google Scholar]
- 5.Anand A, Sharma R, Kapur B, Tandon R (1995) Analysis of symptomatic patients after cholecystectomy: Is the term post-cholecystectomy syndrome an anachronism? Trop Gastroenterol 6:126–131. [PubMed] [Google Scholar]
- 6.Rogy M, Függer R, Herbst F, Schulz F (1991) Reoperation after cholecystectomy: The role of the cystic duct stump. HPB Surg 4:129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scofer JM (2010) Biliary causes of postcholecystectomy syndrome. J Emerg Med 39: 406–410. [DOI] [PubMed] [Google Scholar]
- 8.Vyas F, Nayak S, Perakath B, Pradhan N (2005) Gallbladder remnant and cystic duct stump calculus as a cause of postcholecystectomy syndrome. Trop Gastroenterol 26:159–160. [PubMed] [Google Scholar]
- 9.Bodvall B, Overgaard B (1966) Cystic duct remnant after cholecystectomy: Incidence studied by cholegraphy in 500 cases, and significance in 103 reoperations. Ann Surg 163:382–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beye HL (1936) Conditions necessitating surgery following cholecystectomy surgery. Gynecol Obstet 62:191–202. [Google Scholar]
- 11.Kroh M, Chalikonda S, Chand B, Walsh R (2013) Laparoscopic completion cholecystectomy and common bile duct exploration for retained gallbladder after single-incision cholecystectomy. JSLS 17:143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pernice L, Andreoli F (2009) Laparoscopic treatment of stone recurrence in a gallbladder remnant: Report of an additional case and literature review. J Gastrointest Surg 13:2084–2091. [DOI] [PubMed] [Google Scholar]
- 13.Walsh R, Ponsky J, Dumot J (2002) Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surg Endosc 16:981–984. [DOI] [PubMed] [Google Scholar]
- 14.Whitson B, Wolpert S (2007) Cholelithiasis and cholecystitis in a retained gallbladder remnant after cholecystectomy. JACS 205:814–815. [DOI] [PubMed] [Google Scholar]
- 15.Judd S, Miller L, Antaki F (2014) Symptomatic calculi in a remnant gallbladder: A rare cause of post-cholecystectomy syndrome and biliary pancreatitis. Endoscopy 46(S01):E67–E68. [DOI] [PubMed] [Google Scholar]
- 16.Chowbey P, Soni V, Sharma A, Khullar R, Baijal M (2010) Residual gallstone disease — Laparoscopic management. Indian J Surg 72:220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demetriades H, Pramateftakis M, Kanellos I, Angelopoulos S, Mantzoros I, Betsis D (2008) Retained gallbladder remnant after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech 18:276–279. [DOI] [PubMed] [Google Scholar]
- 18.Tantia O, Jain M, Khanna S, Sen B (2008) Post cholecystectomy syndrome: Role of cystic duct stump and re-intervention by laparoscopic surgery. J Minim Access Surg 4:71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jayant M (2013) Presentation and management of gallbladder remnant after partial cholecystectomy. Trop Gastroenterol 34:99–103. [DOI] [PubMed] [Google Scholar]
- 20.Zhu J, Zhang Z (2015) Laparoscopic remnant cholecystectomy and transcystic common bile duct exploration for gallbladder/cystic duct remnant with stones and choledocholithiasis after cholecystectomy. J Laparoendosc Adv Surg Tech 25:7–11. [DOI] [PubMed] [Google Scholar]
- 21.Shamiyeh A, Danis J, Wayand W, Zehetner J (2007) A 14-year analysis of laparoscopic cholecystectomy: Conversion—when and why? Surg Laparosc Endosc Percutan Techn. 17:271–276. [DOI] [PubMed] [Google Scholar]
- 22.Soleimani M, Mehrabi A, Mood Z, Fonouni H, Kashfi A, Büchler M, et al. (2007) Partial cholecystectomy as a safe and viable option in the emergency treatment of complex acute cholecystitis: A case series and review of the literature. Am Surg. 73:498–507. [PubMed] [Google Scholar]
- 23.Cooperberg PL (1987) Imaging of the gallbladder, 1987. Radiology 163:605–613. [DOI] [PubMed] [Google Scholar]
- 24.Elsayed NM, Binyahib HS, Albalbeesi LJ (2016) Usefulness of abdominal ultrasound and magnetic resonance cholangiopancreatography (MRCP) in the diagnosis of hepatobiliary disorders: A comparative study. Int J Diagnost Imag 3:26–36. [Google Scholar]
- 25.O’Connor H, Hamilton I, Ellis W, Watters J, Lintott D, Axon A (1986) Ultrasound detection of choledocholithiasis: Prospective comparison with ERCP in the postcholecystectomy patient. Gastrointest Radiol 11:161–164. [DOI] [PubMed] [Google Scholar]
- 26.Baron RL (1987) Common bile duct stones: Reassessment of criteria for CT diagnosis. Radiology 162:419–424. [DOI] [PubMed] [Google Scholar]
- 27.Hakansson K, Ekberg O, Hakansson H, Leander P (2002) MR and ultrasound in screening of patients with suspected biliary tract disease. Acta Radiologica. 43:80–86. [DOI] [PubMed] [Google Scholar]
- 28.Strasberg S, Pucci M, Brunt M, Deziel D (2016) Subtotal cholecystectomy–”Fenestrating” vs “Reconstituting” subtypes and the prevention of bile duct injury: Definition of the optimal procedure in difficult operative conditions. JACS 222:89–96. [DOI] [PubMed] [Google Scholar]


