Abstract
Measles virus (MeV) is an immunosuppressive, extremely contagious RNA virus that remains a leading cause of death among children. MeV is dual-tropic: it replicates first in lymphatic tissue, causing immunosuppression, and then in epithelial cells of the upper airways, accounting for extremely efficient contagion. Efficient contagion is counter-intuitive because the enveloped MeV particles are large and relatively unstable. However, MeV particles can contain multiple genomes, which can code for proteins with different functional characteristics. These proteins can cooperate to promote virus spread in tissue culture, prompting to question of whether multi-genome MeV transmission may promote efficient MeV spread also in vivo. Consistent with this hypothesis, in well-differentiated primary human airway epithelia large genome populations spread rapidly through intercellular pores. In another line of research, it was shown that distinct lymphocytic-adapted and epithelial-adapted genome populations exist; cyclical adaptation studies indicate that suboptimal variants in one environment may constitute a low frequency reservoir for adaptation to the other environment. Altogether, these observations suggest that, in humans, MeV spread relies on en bloc genome transmission, and that genomic diversity is instrumental for rapid MeV dissemination within hosts.
Keywords: cyclical adaptation, epithelial spread, measles virus, quasispecies, tissue adaptation, virus transmission
1. INTRODUCTION
Measles remains a leading cause of death among children because it suppresses immune function, facilitating secondary infections (Griffin, 2013). Although eradication is possible, and the WHO has established measles elimination goals in all six regions, measles virus (MeV) still caused about 110,000 deaths worldwide in 2017 alone (WHO Key Facts, Nov. 2018, https://www.who.int/news-room/fact-sheets/detail/measles). Vaccine hesitancy is favoring measles re-emergence in Europe and North America, now reporting costly epidemics (Dabbagh et al., 2017; Hotez, 2016). However, several aspects of MeV multiplication and spread, within and between hosts, are incompletely understood.
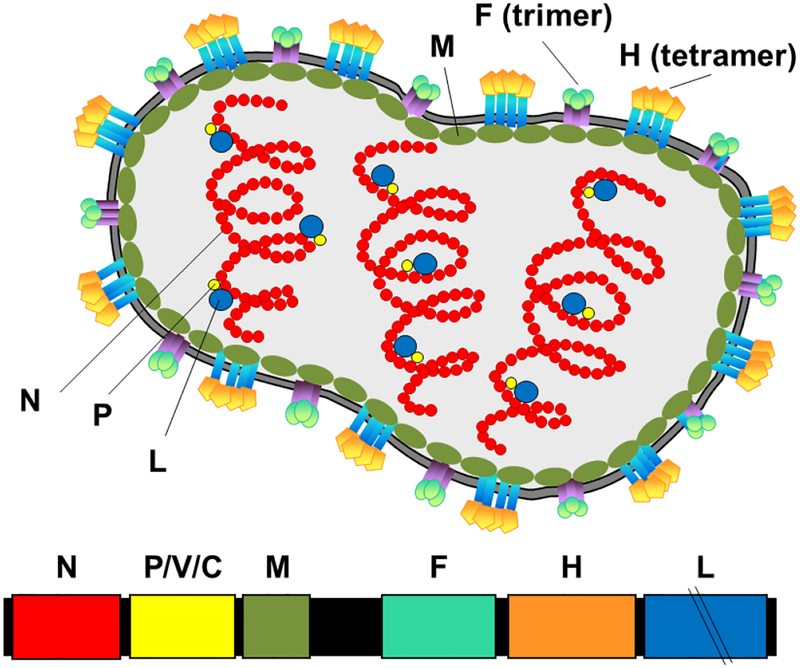
MeV is a negative strand RNA virus of the genus Morbillivirus in the family Paramyxoviridae (Lamb and Parks, 2013), which includes deadly emerging viruses like Hendra virus, Nipah virus, and prevalent human pathogens like mumps virus and the parainfluenza viruses. The particles of all these viruses have similar pleomorphic morphologies and may contain more than one genome (Rager et al., 2002) (Fig. 1, top). All the morbillivirus genomes are organized into six contiguous, non-overlapping transcription units separated by three non-transcribed nucleotides and coding for eight viral proteins in the order (positive strand): 5’-N-P/V/C-M-F-H-L-3’ (Fig. 1, bottom).
Figure 1. Diagram of a MeV particle (top) and of the viral RNA genome (bottom).
The particle is drawn with its six main components: the nucleocapsid (N) that covers the genomic RNA and interacts with the phosphoprotein (P), and polymerase (large, L), forming the ribonucleocapsid complex; the fusion (F) and hemagglutinin (H) proteins forming the membrane fusion apparatus; and the matrix (M) protein controlling particle assembly as well as transcription and membrane fusion. Particles contain multiple encapsidated genomes, of which three are drawn schematically. On the genome (shown here as positive strand, bottom), the coding regions of the proteins are color-coded, non-coding regions are black. The P gene codes also for the V and C proteins (see Fig. 3 for details).
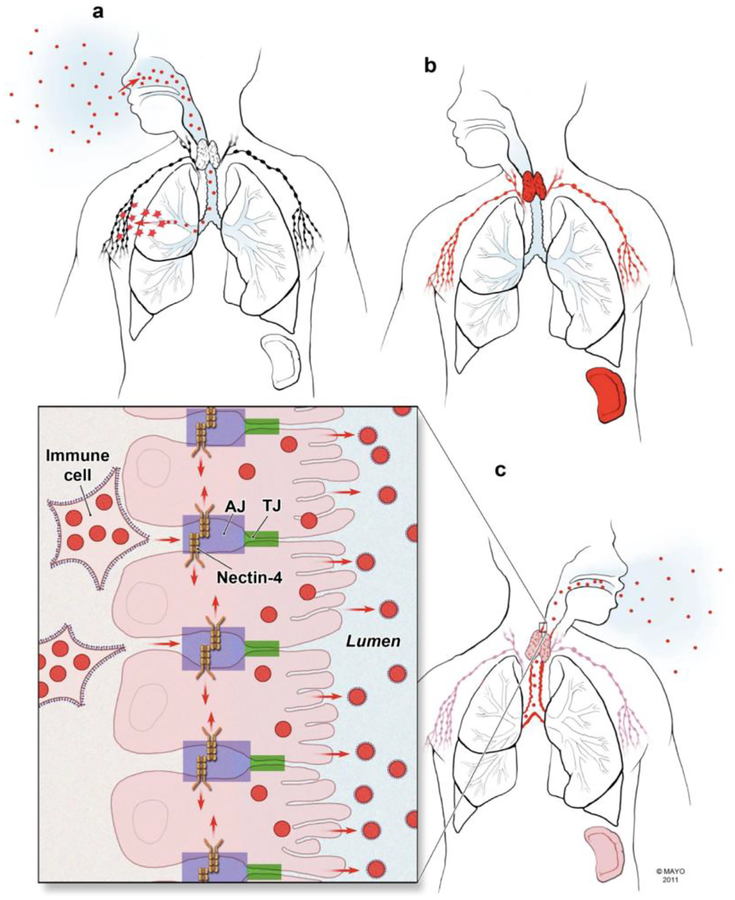
Interactions of the viral glycoproteins with cellular receptors determine the tropism of MeV and the other morbilliviruses. Since these viruses sequentially utilize two receptors to enter different tissue niches, they are considered dual-tropic (Takeda et al., 2011). After contagion the signaling lymphocytic activation molecule (SLAM) mediates virus entry (Tatsuo et al., 2000): SLAM-expressing alveolar macrophages and dendritic cells ferry the infection through the respiratory epithelium and spread it to lymphoid tissue (Ferreira et al., 2009; Ludlow et al., 2015) (Fig. 2a). The extensive spread of MeV and other morbilliviruses in immune tissues accounts for immunosuppression (Leonard et al., 2010; von Messling et al., 2006).
Figure 2. The MeV infectious cycle (Muehlebach et al., 2011).
The lymphatic phase of infection is shown in (a and b); the epithelial phase is shown in (c and inset). Infectious viral particles are shown as red spheres; viral glycoproteins as small spikes on extracellular viruses and infected immune cells (inset). Infected cells and organs are red at the peak of infection, or pink after the peak. a, MeV enters the airways and infects macrophages and dendritic cells, which ferry the infection to the regional lymph nodes. b, MeV infects the local lymph nodes and the infection spreads rapidly to the primary lymphatic organs (red). c, infection spreads to epithelia. Inset: MeV enters the airway epithelium carried from an infected immune cell that expresses the viral glycoproteins on its plasma membrane. The viral hemagglutinin binds to nectin-4 (orange) in the adherens junction (AJ, blue rectangle), which is located basolateral to the tight junction (TJ, green rectangle). Infection spreads laterally via AJ (red arrows). Epithelial cells express viral glycoproteins in their membranes (not shown).
In the second phase of infection, immune cells deliver morbilliviruses to upper airways epithelial cells that express nectin-4 (Frenzke et al., 2013; Sawatsky et al., 2012; Singh et al., 2016). Nectin-4, a component of the adherens junction, is expressed preferentially in the trachea, and morbillivirus replication at this location accounts for extremely efficient contagion (Muehlebach et al., 2011; Sawatsky et al., 2012).
MeV is the most contagious human respiratory virus (Mateo et al., 2014; Monto, 1999). Its basic reproductive number is often cited as 12–18, which means that each person with measles would, on average, infect 12–18 other people in a totally susceptible population (Guerra et al., 2017). In specific cases individual patients can infect more than 200 new patients (Christensen et al., 1953). Thus, even if the enveloped MeV particles are large and relatively unstable, they are very effective in transmitting infection.
We review here data indicating that MeV particles contain multiple genomes and that MeV spread in well-differentiated primary human airway epithelia relies on the transmission of genome populations. Moreover, adaptation studies indicate that distict quasispecies are selected in different cellular environments. Thus, en bloc genome transmission and genome diversity can be instrumental for MeV spread and pathogenesis.
2. GENOME DIVERSITY OF MeV AND OTHER RNA VIRUSES
MeV genomes, as those of all other RNA viruses, are quasispecies, mutant distributions (also termed mutant swarms or mutant clouds) that are generated upon the replication of RNA viruses in infected cells and organisms (Andino and Domingo, 2015). Genetic diversity allows virus populations to rapidly adapt in dynamic environments, and to develop resistance to antibodies and antiviral drugs (Lauring and Andino, 2010). Next generation sequencing, which greatly expands the capacity to examine the composition of viral quasispecies in infected cells and host organisms, is beginning to reveal the mechanisms driving mutant spectra adaptation during viral infections, including those of human immunodeficiency virus (HIV) and hepatitis C virus (HCV) (Ansari et al., 2017; Cuevas et al., 2015). These two viruses cause organ- or tissue-specific diseases: HCV causes liver disease, and HIV immunosuppression. Secondary infections of other organs occur but have minor effects on pathogenesis, and are irrelevant for spread to the next host. By contrast, MeV and the other morbilliviruses have to replicate sequentially in two different but equally relevant tissue niches before spreading to the next host. The sequential, dual-tropic nature of the MeV infectious cycle (Takeda et al., 2011) promotes it to an ideal system to characterize potential tissue adaptation of RNA virus genome populations.
Genomic diversity of RNA virus populations is due mainly to the intrinsic error rate of the viral polymerase (Borderia et al., 2016). The mutation rate of the MeV polymerase was estimated to 0.9 × 10−4 per base per replication (Schrag et al., 1999), or lower (Zhang et al., 2013). Our early analyses of MeV infections of permissive cell lines estimated a few positions per genome intra-population variability (Cattaneo et al., 1988). We also documented higher levels of MeV genome diversity in brains of patients who died with subacute sclerosing panencephalitis (SSPE), a rare but always lethal disease that can develop 5–10 years after acute MeV infection (Bellini et al., 2005).
Remarkably, a significant fraction of the changes in MeV RNA from the brains of SSPE patients were accounted by large clusters of biased transitions (U-to-C or A-to-G, depending on the polarity of the strand analyzed), an unprecedented finding when these studies were published (Cattaneo et al., 1988). Shortly thereafter, it was proposed that that the newly discovered cellular enzyme adenosine deaminase acting on RNA 1 (ADAR1) (Bass and Weintraub, 1988; Wagner et al., 1989), which converts adenosine residues to inosine in double-stranded RNA, may cause these A-to-I hypermutation events (Bass et al., 1989). Subsequently, similar A-to-I editing events were detected in several other RNA virus genomes (Cattaneo, 1994), including the Chinese MeV vaccine strain Shanghai-191 (Rota et al., 1994).
The advent of massive parallel genome-wide sequencing then revealed that many cellular RNAs are frequently edited (Li et al., 2009), not only in mammals but also across all orders of metazoans (Nishikura, 2016; Yablonovitch et al., 2017). Sequencing studies also demonstrated that extensive ADAR1 editing occurs frequently in defective-interfering MeV RNA genomes, and also in standard MeV genomes (Pfaller et al., 2015; Pfaller et al., 2014; Suspene et al., 2011). Very recently, it was formally demonstrated that ADAR1 accounts for MeV genome editing (Pfaller et al., 2018) and provides a mechanism that shields immunostimulatory defective-interfering RNAs from recognition by the innate immune system.
Another family of cellular enzymes edits viral and cellular nucleic acids: the APOBEC cytidine deaminase enzymes introduce C-to-U or C-toT changes, respectively, in RNA or DNA templates (Chen et al., 2017; Harris and Dudley, 2015). The APOBEC family member 3G restricts HIV and other Retroviridae through this mutagenic process (Harris et al., 2003; Zhang et al., 2003). Interestingly, MeV and two other negative strand RNA viruses are also sensitive to APOBEC3G inhibition, but specific C-to-U hypermutation events were not detected (Fehrholz et al., 2012).
Altogether, these observations indicate that both the intrinsic error rate of the MeV polymerase, and sometimes A-to-I mutations introduced by ADAR1, can contribute to MeV quasispecies diversity, while APOBEC3G may not.
3. THE MeV INFECTIOUS UNIT: MORE THAN ONE GENOME
A fundamental concept in virus research is that genomes are packaged into particles for spread in the extracellular milieu. In most viruses, individual genomes are packaged. However, the pleomorphic particles of MeV and the other members of the Paramyxoviridae family often incorporate more than one genome, as deduced initially from particle sedimentation and ultraviolet inactivation studies (Dahlberg and Simon, 1969; Hosaka et al., 1966).
A second characteristic of MeV biology consistent with the complex nature of the MeV infectious “unit” is the cell-associated nature of infections. In cultivated cells, MeV particles accumulate below the plasma membrane (Bohn et al., 1983) and the ratio of intracellular to secreted infectivity is about 10:1 (Cathomen et al., 1998). In monolayers of most immortalized cell lines, MeV infections spread mainly through fusion of an infected cell with recipient cells expressing an appropriate receptor (Navaratnarajah et al., 2009). Receptors on recipient cells trigger the viral membrane fusion apparatus expressed on the surface of infected cells to form fusion pores; pore expansion then results in coalescence of plasma membranes, and formation of large multinucleated syncytia. This mechanism promotes the spread of progressively larger genome populations, without selection for individual genomes. From this vantage point, the MeV infectious “unit” appears to be highly complex and diverse.
Genetic analyses of MeV infections have provided independent evidence of multi-genome MeV transmission (Rager et al., 2002; Shirogane et al., 2012). In a study originally aimed at re-targeting MeV entry, Rager et al. unexpectedly characterized a stable MeV mutant, which spread depends on the simultaneous packaging of two types of genomes, one of which arose fortuitously. Each genome is defective for one function, namely either cell attachment or polymerase, but the two genomes complement each other. Importantly, the infection kinetics of this two-genomes mutant indicated that packaging of multiple genomes does not negatively affect growth. It was also shown that polyploid particles are produced in standard infections at no expense to infectivity (Rager et al., 2002).
Another example of multi-genome MeV transmission (Shirogane et al., 2012) is discussed in more detail in another contribution to this special issue of Virus Research. In brief, Shirogane et al. observed that a non-fusogenic recombinant MeV can evolve into mutant viruses which regain the ability to induce membrane fusion. Unexpectedly, the spread of one of these mutant MeV was dependent on the simultaneous packaging of two types of genomes, one encoding the wild-type F protein, the other a mutant version with a single amino-acid substitution. Neither the wild-type, nor the mutant F protein mediated membrane fusion by themselves, but together they exhibited enhanced fusion activity through hetero-oligomer formation (Shirogane et al., 2012). Thus, biochemical studies of viral particles, analyses of MeV cell biology, and genetic studies are all consistent with the hypothesis that, at least in stable cell lines, the “unit” that spreads MeV infection can be constituted by more than one genome.
4. MULTI-GENOME MeV TRANSMISSION IN PRIMARY HUMAN AIRWAY EPITHELIA (HAE) CULTURES
The observation that different MeV genome types can cooperate to allow virus spread in tissue culture prompted the question as to whether multi-genome transmission may promote MeV spread also in natural hosts. Animal studies of MeV pathogenesis are demanding because only certain primate species are good models (de Swart, 2009; Delpeut et al., 2017; McChesney et al., 1997). Nevertheless, it is clear that MeV infections remain largely cell-associated during spread in lymphatic tissue and peripheral blood mononuclear cells (PBMC) of humans and other primates. In PBMC of experimentally infected monkeys, or of infected humans, no free MeV is detected, and titers are measured by overlaying leukocytes onto SLAM-expressing cells (McChesney et al., 1997; van Binnendijk et al., 1994).
To begin addressing the question of multiple genome transmission in a relevant model tissue system, we have relied on well-differentiated primary HAE cultures. Previously, MeV infections have been studied extensively in monolayers of immortalized cell lines, where large multinucleated syncytia are formed after extensive cell fusion (Navaratnarajah et al., 2009).
In HAE cultures, formation of large syncytia is not observed. Instead, infectious centers form while tissue structures, including plasma membranes, remain intact and trans-epithelial resistance is maintained, indicating functional tissue integrity (Singh et al., 2015; Sinn et al., 2002). Infectious center formation without visible cell fusion is consistent with the existence of intercellular fusion pores, which may not expand much but are wide enough to allow the transfer of viral ribonucleocapsids, or partially assembled viral particles (Cifuentes-Munoz et al., 2018). Remarkably, presumably because of viral utilization of preserved apical cytoskeletal structures, infections spread to naïve cells within 2–4 hours, which is faster than the spread of other respiratory viruses in the same HAE culture system (Singh et al., 2015). Analogous intercellular pores may account for rapid epithelial spread of MeV genome populations during infections of natural hosts, implying that the intra-host infectious “unit” is highly complex and diverse.
5. CYCLICAL ADAPTATION OF MeV GENOMES TO LYMPHOID AND EPITHELIAL CELLS
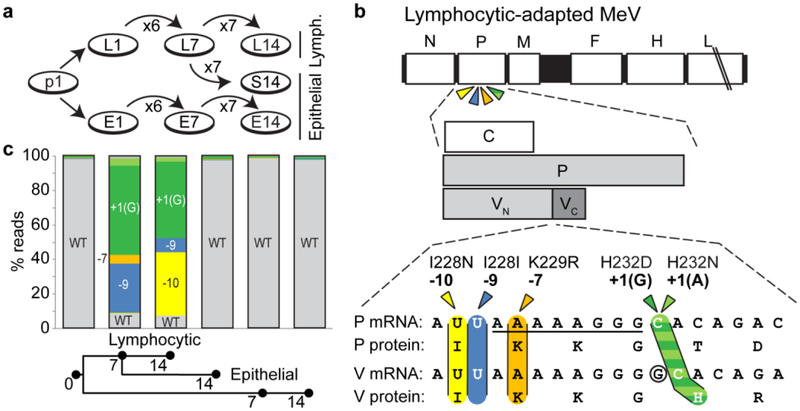
Inter-host adaptation of RNA viruses, for example of arboviruses to arthropods and vertebrates (Coffey et al., 2008; Weaver et al., 1999), or of influenza viruses to birds and mammals (Kuiken et al., 2006; Manz et al., 2013) are well characterized, but insights about genetic diversity and adaptation of viruses that replicate sequentially in two tissue niches of the same host are rare. The switch of MeV tropism from lymphatic tissues to epithelial cells provides an ideal experimental system to address the question of whether, and how, intra-host evolution occurs. To gain insights into the extent of MeV genome variability after growth in different tissues, we adapted MeV either to lymphoid (Granta-519) or epithelial (H358) human cells. We also passaged it consecutively in both cell lines (Donohue et al., 2019) (Fig. 3A). Since MeV passaged in these cell lines had different replication kinetics, we sought to investigate the underlying genetic mechanisms by performing deep-sequencing analyses.
Figure 3. Cyclical quasispecies re-equilibration.
(A) Strategy for adaptation of MeV to two cell types. The original inoculum (p1) was passaged 14 times on lymphoid cells (L1 to L14) or epithelial cells (E1 to E14). L7 was also passaged on epithelial cells seven times to generate S14. (B) P gene variants selected by adaptation to lymphoid cells. (Top) The MeV genome. Coding regions are shown as white boxes, non-coding regions are in black. Four nearby P gene variant positions are shown by colored arrows. (Center) Schematic of P gene coding regions. The P protein is translated from the first AUG start codon. The C protein is translated from the second AUG, on a different reading frame. V is generated from transcripts with an additional G inserted after the AAAAAGGG sequence AUG start codon (see bottom). V shares the first 231 amino acids with P (VN), but has a different C-terminal domain (VC). (Bottom) Sequence and position of the lymphoid variants. Variants are indicated by colored arrowheads, and their positions relative to the G insertion site (circled) are shown above the arrowheads. Amino acid sequences are shown below the nucleotide sequences. (C) Analysis of editing site-proximal variants across passage history. The y-axis shows the percentage reads with the indicated alleles. Alleles are colored as in panel B: wild type (WT, grey), −10 (yellow), −9 (blue), −7 (orange), +1(G) (dark green), and +1(A) (light green). The passage numbers analyzed are indicated on the horizontal axis, and the passage history is drawn schematically on the bottom.
As shown in Fig. 3B, lymphoid adaptation reproducibly resulted in accumulation of variants mapping within an 11-nucleotide sequence located in the middle of the phosphoprotein (P) gene. This sequence mediates polymerase slippage and addition of a pseudo-templated guanosine to the P mRNA (Cattaneo et al., 1989). This form of co-transcriptional RNA editing leads to the expression of an interferon antagonist, named V, in place of a polymerase cofactor, named P. Indeed, we found that lymphoid-adapted MeV produces minimal amounts of edited transcripts, and of V protein. In contrast, epithelial-adapted MeV produced similar levels of edited and non-edited transcripts, and of V and P proteins (Donohue et al., 2019). Importantly, adaptation is reversible: in epithelial cells V-competent MeV genomes rapidly out-compete the V-deficient variants (Fig. 3C). Thus, suboptimal variants in one environment may constitute a low frequency reservoir for adaptation to the other environment.
The mechanisms of this process, which was named cyclical genome re-equilibration, were further characterized by rescuing four recombinant MeV carrying individual editing site-proximal mutations. Three mutations interfered with RNA editing, resulting in almost exclusive P protein expression. The fourth preserved RNA editing and a standard P-to-V protein expression ratio (Donohue et al., 2019). However, it altered a histidine involved in Zn2+ binding, inactivating V function (Ramachandran and Horvath, 2010). Positive selection of this mutant suggests that inactivation of V protein function, rather than enhanced P protein expression, is key for adaptation to lymphoid cells. Thus, the lymphoid environment favors replication of V-deficient MeV, while the epithelial environment has the opposite effect, resulting in rapid and thorough cyclical quasispecies re-equilibration.
Adaptation by V-protein inactivation was characterized in two different lymphocytic cell lines (Donohue et al., 2019), but it remains to be established whether it occurs during infections of natural hosts. Analyses of the expression of the V and P proteins, or of P/V transcripts, in lymphoid cells from experimentally infected primates are not yet available, but G-insertion efficiency is reduced to 5–20% in MeV mRNA extracted from brain autopsy material of SSPE patients (Millar et al., 2016). This indicates that editing efficiency can vary in vivo, and could reflect quasispecies adaptation to the neural environment.
6. CONCLUSIONS AND PERSPECTIVES
MeV genomes, as those of all other RNA viruses, are quasispecies, or mutant distributions. MeV genomic diversity is due mainly to the intrinsic error rate of its polymerase, and also in part to editing by the cellular RNA-dependent adenosine deaminase ADAR1. Studies of viral particles, analyses of MeV cell biology, and genetic studies are all consistent with the hypothesis that, at least in stable cell lines, the “unit” that spreads MeV infection is constituted by more than one genome. Studies of MeV spread in well-differentiated HAE cultures suggest that also in this ex vivo system, MeV infections spread as a highly complex genome population.
We think that, even within natural hosts, MeV spread may rely on en bloc genome transmission, and that genomic diversity is instrumental for rapid dissemination and virulence. Interestingly, we have observed that the original epithelial-adapted genome sequence is conserved at low frequency in lymphoid cells, and is rapidly re-selected in epithelial cells. Thus, the compounded selective pressures for sequential adaptation to two different cell types within a host may account, at least in part, for the genetic stability of the dual-tropic morbilliviruses. Similar cyclical quasispecies re-equilibration processes may occur during natural infections with other dual-tropic RNA viruses. These include noroviruses, which infect epithelial and non-epithelial cell types (Wobus, 2018), and HIV, which infects T-cells and macrophages.
Highlights:
Measles virus is dual tropic: it replicates in lymphoid and epithelial cells
Measles virus quasispecies rapidly adapt to lymphoid and epithelial cells
In primary human epithelia measles virus spread relies on en bloc transmission
Genomic diversity appears instrumental for rapid virus dissemination within hosts
FUNDING:
This work was supported by National Institutes of Health grants R01 AI125747 and R01 AI128037 to RC.
Abbreviations:
- ADAR1
adenosine deaminase acting on RNA 1
- HAE
human airway epithelia
- HCV
hepatitis C virus
- HIV
human immunodeficiency virus
- MeV
measles virus
- PBMC
peripheral blood mononuclear cells
- SLAM
signaling lymphocytic activation molecule
- SSPE
subacute sclerosing panencephalitis
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Andino R and Domingo E (2015) Viral quasispecies. Virology 479–480, 46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansari MA, Pedergnana V, C LCI, Magri A, Von Delft A, Bonsall D, Chaturvedi N, Bartha I, Smith D, Nicholson G, McVean G, Trebes A, Piazza P, Fellay J, Cooke G, Foster GR, Hudson E, McLauchlan J, Simmonds P, Bowden R, Klenerman P, Barnes E and Spencer CCA (2017) Genome-to-genome analysis highlights the effect of the human innate and adaptive immune systems on the hepatitis C virus. Nat Genet 49(5), 666–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass BL and Weintraub H (1988) An unwinding activity that covalently modifies its double-stranded RNA substrate. Cell 55(6), 1089–98. [DOI] [PubMed] [Google Scholar]
- Bass BL, Weintraub H, Cattaneo R and Billeter MA (1989) Biased hypermutation of viral RNA genomes could be due to unwinding/modification of double-stranded RNA. Cell 56(3), 331. [DOI] [PubMed] [Google Scholar]
- Bellini WJ, Rota JS, Lowe LE, Katz RS, Dyken PR, Zaki SR, Shieh WJ and Rota PA (2005) Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. J Infect Dis 192(10), 1686–93. [DOI] [PubMed] [Google Scholar]
- Bohn W, Rutter G, Hohenberg H and Mannweiler K (1983) Inhibition of measles virus budding by phenothiazines. Virology 130(1), 44–55. [DOI] [PubMed] [Google Scholar]
- Borderia AV, Rozen-Gagnon K and Vignuzzi M (2016) Fidelity variants and RNA quasispecies. Curr Top Microbiol Immunol 392, 303–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cathomen T, Naim HY and Cattaneo R (1998) Measles viruses with altered envelope protein cytoplasmic tails gain cell fusion competence. J Virol 72(2), 1224–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaneo R (1994) Biased (A-->I) hypermutation of animal RNA virus genomes. Curr Opin Genet Dev 4(6), 895–900. [DOI] [PubMed] [Google Scholar]
- Cattaneo R, Kaelin K, Baczko K and Billeter MA (1989) Measles virus editing provides an additional cysteine-rich protein. Cell 56(5), 759–764. [DOI] [PubMed] [Google Scholar]
- Cattaneo R, Schmid A, Eschle D, Baczko K, ter Meulen V and Billeter MA (1988) Biased hypermutation and other genetic changes in defective measles viruses in human brain infections. Cell 55(2), 255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Qiu X, Zhang N, Wang Y, Wang M, Li D, Wang L and Du Y (2017) APOBEC-mediated genomic alterations link immunity and viral infection during human papillomavirus-driven cervical carcinogenesis. Biosci Trends 11(4), 383–388. [DOI] [PubMed] [Google Scholar]
- Christensen PE, Schmidt H, Jensen O, Bang HO, Andersen V and Jordal B (1953) An epidemic of measles in Southern Greenland, 1951. I. Measles in virgin soil. Acta Medica Scandinavica 144(4), 313–22. [DOI] [PubMed] [Google Scholar]
- Cifuentes-Munoz N, Dutch RE and Cattaneo R (2018) Direct cell-to-cell transmission of respiratory viruses: The fast lanes. PLoS Pathog 14(6), e1007015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey LL, Vasilakis N, Brault AC, Powers AM, Tripet F and Weaver SC (2008) Arbovirus evolution in vivo is constrained by host alternation. Proc Natl Acad Sci U.S.A. 105(19), 6970–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuevas JM, Geller R, Garijo R, Lopez-Aldeguer J and Sanjuan R (2015) Extremely high mutation rate of HIV-1 in vivo. PLoS Biol 13(9), e1002251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabbagh A, Patel MK, Dumolard L, Gacic-Dobo M, Mulders MN, Okwo-Bele JM, Kretsinger K, Papania MJ, Rota PA and Goodson JL (2017) Progress toward regional measles elimination - worldwide, 2000–2016. MMWR Morb Mortal Wkly Rep 66(42), 1148–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlberg JE and Simon EH (1969) Physical and genetic studies of Newcastle disease virus: evidence for multiploid particles. Virology 38(4), 666–78. [DOI] [PubMed] [Google Scholar]
- de Swart RL (2009) Measles studies in the macaque model. Curr Top Microbiol Immunol 330, 55–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delpeut S, Sawatsky B, Wong XX, Frenzke M, Cattaneo R and von Messling V (2017) Nectin-4 interactions govern measles virus virulence in a new model of pathogenesis, the squirrel monkey (Saimiri sciureus). J Virol 91(11), e02490–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue RC, Pfaller CK and Cattaneo R (2019) Cyclical adaptation of measles virus quasispecies to epithelial and lymphocytic cells: To V, or not to V. PLoS Pathog 15(2), e1007605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehrholz M, Kendl S, Prifert C, Weissbrich B, Lemon K, Rennick L, Duprex PW, Rima BK, Koning FA, Holmes RK, Malim MH and Schneider-Schaulies J (2012) The innate antiviral factor APOBEC3G targets replication of measles, mumps and respiratory syncytial viruses. J Gen Virol 93(Pt 3), 565–76. [DOI] [PubMed] [Google Scholar]
- Ferreira CSA, Frenzke M, Leonard VHJ, Welstead GG, Richardson CD and Cattaneo R (2009) Measles virus infection of alveolar macrophages and dendritic cells precedes spread to lymphatic organs in transgenic mice expressing human signaling lymphocytic activation molecule (SLAM, CD150). J Virol 84, 3033–3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenzke M, Sawatsky B, Wong XX, Delpeut S, Mateo M, Cattaneo R and von Messling V (2013) Nectin-4-dependent measles virus spread to the cynomolgus monkey tracheal epithelium: role of infected immune cells infiltrating the lamina propria. J Virol 87(5), 2526–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin DE (2013) Measles Virus In: Knipe DM and Howley PM (Eds), Fields Virology, 6th ed., pp. 1042–1069. Vol. 1. 2 vols. Lippincott Williams & Wilkins, Philadelphia. [Google Scholar]
- Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y and Crowcroft NS (2017) The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis 17(12), e420–e428. [DOI] [PubMed] [Google Scholar]
- Harris RS, Bishop KN, Sheehy AM, Craig HM, Petersen-Mahrt SK, Watt IN, Neuberger MS and Malim MH (2003) DNA deamination mediates innate immunity to retroviral infection. Cell 113(6), 803–9. [DOI] [PubMed] [Google Scholar]
- Harris RS and Dudley JP (2015) APOBECs and virus restriction. Virology 479–480, 131–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosaka Y, Kitano H and Ikeguchi S (1966) Studies on the pleomorphism of HVJ virons. Virology 29(2), 205–21. [DOI] [PubMed] [Google Scholar]
- Hotez PJ (2016) Texas and its measles epidemics. PLoS Med 13(10), e1002153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiken T, Holmes EC, McCauley J, Rimmelzwaan GF, Williams CS and Grenfell BT (2006) Host species barriers to influenza virus infections. Science 312(5772), 394–7. [DOI] [PubMed] [Google Scholar]
- Lamb RA and Parks G (2013) Paramyxoviridae In: Knipe DM and Howley PM (Eds), Fields Virology, pp. 957–995. Vol. 1. Lippincott Williams & Wilkins, Philadelphia. [Google Scholar]
- Lauring AS and Andino R (2010) Quasispecies theory and the behavior of RNA viruses. PLoS Pathog 6(7), e1001005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard VHJ, Hodge G, Reyes del Valle J, McChesney MB and Cattaneo R (2010) Signaling lymphocytic activation molecular (SLAM, CD150)-blind measles virus is attenuated and induces strong adaptive immune responses in rhesus monkeys. J Virol 84, 3280–3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li JB, Levanon EY, Yoon JK, Aach J, Xie B, Leproust E, Zhang K, Gao Y and Church GM (2009) Genome-wide identification of human RNA editing sites by parallel DNA capturing and sequencing. Science 324(5931), 1210–3. [DOI] [PubMed] [Google Scholar]
- Ludlow M, McQuaid S, Milner D, de Swart RL and Duprex WP (2015) Pathological consequences of systemic measles virus infection. J Pathol 235(2), 253–65. [DOI] [PubMed] [Google Scholar]
- Manz B, Schwemmle M and Brunotte L (2013) Adaptation of avian influenza A virus polymerase in mammals to overcome the host species barrier. J Virol 87(13), 7200–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateo M, Navaratnarajah CK and Cattaneo R (2014) Structural basis of efficient contagion: measles variations on a theme by parainfluenza viruses. Curr Opin Virol 5, 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McChesney MB, Miller CJ, Rota PA, Zhu YD, Antipa L, Lerche NW, Ahmed R and Bellini WJ (1997) Experimental measles. I. Pathogenesis in the normal and the immunized host. Virology 233(1), 74–84. [DOI] [PubMed] [Google Scholar]
- Millar EL, Rennick LJ, Weissbrich B, Schneider-Schaulies J, Duprex WP and Rima BK (2016) The phosphoprotein genes of measles viruses from subacute sclerosing panencephalitis cases encode functional as well as non-functional proteins and display reduced editing. Virus Res 211, 29–37. [DOI] [PubMed] [Google Scholar]
- Monto A (1999) Interrupting the transmission of respiratory tract infections: theory and practice. Clin Infect 28, 200–204. [DOI] [PubMed] [Google Scholar]
- Muehlebach MD, Mateo M, Sinn PL, Prufer S, Uhlig KM, Leonard VH, Navaratnarajah CK, Frenzke M, Wong XX, Sawatsky B, Ramachandran S, McCray PB Jr., Cichutek K, von Messling V, Lopez M and Cattaneo R (2011) Adherens junction protein nectin-4 is the epithelial receptor for measles virus. Nature 480(7378), 530–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navaratnarajah CK, Leonard VHJ and Cattaneo R (2009) Measles virus glycoprotein complex assembly, receptor attachment and cell entry. Curr Topics Microbiol Immunol 329, 59–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishikura K (2016) A-to-I editing of coding and non-coding RNAs by ADARs. Nat Rev Mol Cell Biol 17(2), 83–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaller CK, Donohue RC, Nersisyan S, Brodsky L and Cattaneo R (2018) Extensive editing of cellular and viral double-stranded RNA structures accounts for innate immunity suppression and the proviral activity of ADAR1p150. PLoS Biol 16(11), e2006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaller CK, Mastorakos GM, Matchett WE, Ma X, Samuel CE and Cattaneo R (2015) Measles virus defective interfering RNAs are generated frequently and early in the absence of C protein and can be destabilized by adenosine deaminase acting on RNA-1-like hypermutations. J Virol 89(15), 7735–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaller CK, Radeke MJ, Cattaneo R and Samuel CE (2014) Measles virus C protein impairs production of defective copyback double-stranded viral RNA and activation of protein kinase R. J Virol 88(1), 456–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rager M, Vongpunsawad S, Duprex WP and Cattaneo R (2002) Polyploid measles virus with hexameric genome length. EMBO J 21(10), 2364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran A and Horvath CM (2010) Dissociation of paramyxovirus interferon evasion activities: universal and virus-specific requirements for conserved V protein amino acids in MDA5 interference. J Virol 84(21), 11152–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rota JS, Wang ZD, Rota PA and Bellini WJ (1994) Comparison of sequences of the H, F, and N coding genes of measles virus vaccine strains. Virus Res 31(3), 317–330. [DOI] [PubMed] [Google Scholar]
- Sawatsky B, Wong XX, Hinkelmann S, Cattaneo R and von Messling V (2012) Canine distemper virus epithelial cell infection is required for clinical disease but not for immunosuppression. J Virol 86(7), 3658–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrag SJ, Rota PA and Bellini WJ (1999) Spontaneous mutation rate of measles virus: direct estimation based on mutations conferring monoclonal antibody resistance. J Virol 73(1), 51–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirogane Y, Watanabe S and Yanagi Y (2012) Cooperation between different RNA virus genomes produces a new phenotype. Nat Commun 3, 1235. [DOI] [PubMed] [Google Scholar]
- Singh BK, Hornick AL, Krishnamurthy S, Locke AC, Mendoza CA, Mateo M, Miller-Hunt CL, Cattaneo R and Sinn PL (2015) The Nectin-4/Afadin protein complex and intercellular membrane pores contribute to rapid spread of measles virus in primary human airway epithelia. J Virol 89(14), 7089–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh BK, Li N, Mark AC, Mateo M, Cattaneo R and Sinn PL (2016) Cell-to-cell contact and Nectin-4 govern spread of measles virus from primary human myeloid cells to primary human airway epithelial cells. J Virol 90(15), 6808–6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinn PL, Williams G, Vongpunsawad S, Cattaneo R and McCray PB Jr. (2002) Measles virus preferentially transduces the basolateral surface of well-differentiated human airway epithelia. J Virol 76(5), 2403–2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suspene R, Petit V, Puyraimond-Zemmour D, Aynaud MM, Henry M, Guetard D, Rusniok C, Wain-Hobson S and Vartanian JP (2011) Double-stranded RNA adenosine deaminase ADAR-1-induced hypermutated genomes among inactivated seasonal influenza and live attenuated measles virus vaccines. J Virol 85(5), 2458–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda M, Tahara M, Nagata N and Seki F (2011) Wild-type measles virus is intrinsically dual-tropic. Front Microbiol 2, 279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatsuo H, Ono N, Tanaka K and Yanagi Y (2000) SLAM (CDw150) is a cellular receptor for measles virus. Nature 406(6798), 893–897. [DOI] [PubMed] [Google Scholar]
- van Binnendijk RS, van der Heijden RW, van Amerongen G, UytdeHaag FG and Osterhaus AD (1994) Viral replication and development of specific immunity in macaques after infection with different measles virus strains. J Infect Dis 170(2), 443–8. [DOI] [PubMed] [Google Scholar]
- von Messling V, Svitek N and Cattaneo R (2006) Receptor (SLAM, CD150) recognition and the V protein sustain swift lymphocyte-based invasion of mucosal tissue and lymphatic organs by a morbillivirus. J Virol 80, 6084–6092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner RW, Smith JE, Cooperman BS and Nishikura K (1989) A double-stranded RNA unwinding activity introduces structural alterations by means of adenosine to inosine conversions in mammalian cells and Xenopus eggs. Proc Natl Acad Sci U.S.A. 86(8), 2647–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver SC, Brault AC, Kang W and Holland JJ (1999) Genetic and fitness changes accompanying adaptation of an arbovirus to vertebrate and invertebrate cells. J Virol 73(5), 4316–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wobus CE (2018) The dual tropism of Noroviruses. J Virol 92(16), e01010–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yablonovitch AL, Deng P, Jacobson D and Li JB (2017) The evolution and adaptation of A-to-I RNA editing. PLoS Genetic 28(13), e1007064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, Yang B, Pomerantz RJ, Zhang C, Arunachalam SC and Gao L (2003) The cytidine deaminase CEM15 induces hypermutation in newly synthesized HIV-1 DNA. Nature 424(6944), 94–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Rennick LJ, Duprex WP and Rima BK (2013) Determination of spontaneous mutation frequencies in measles virus under nonselective conditions. J Virol 87(5), 2686–92. [DOI] [PMC free article] [PubMed] [Google Scholar]