Abstract
Venous angiomas are relatively common lesions that occur in up to 3% of the general population. It is usually asymptomatic and discovered incidentally. We present a case of developmental venous anomaly mimicking thrombosed cerebral vein on nonenhanced computed tomography scan of the brain. A 48-year-old male patient medically free referred to our center for further management of high blood pressure. Because of the concern of thrombosed cerebral vein on computed tomography, further investigation with magnetic resonance venogram revealed a small network of veins in the region of the left internal cerebral vein with a picture of venous angioma. This case highlights such findings for the junior radiologist to consider additional investigations and avoid subsequent inadvertent treatment with anticoagulation.
Keywords: Cerebral Vascular malformations, Developmental Venous anomalies
Abbreviations: DVA, developmental venous anomalies; NECT, nonenhanced CT scan; MRI, magnetic resonance imaging; MRV, magnetic resonance venography
Introduction
Developmental venous anomalies (DVA) are one of the most common cerebral vascular malformations. They are present in up to 3% of the general population. The confluence of radially oriented veins into a single dilated venous channel is the defining characteristic of these lesions [1]. DVAs are considered congenital abnormalities of the venous vasculature of the brain. The hemodynamic imbalance which occurs due to the absence of superficial or deep venous collectors, results in compensatory drainage toward the deep venous system or pial venous system, respectively, through a collector's vein, and therefore should be considered an anatomical variation in the localized venous drainage pathway of the brain parenchyma [2]. These variations make it challengeable for a junior radiologist to diagnose it. We describe a case of asymptomatic DVA that mimicked thrombosed cerebral vein on nonenhanced CT scan (NECT).
Case presentation
A 48-year-old male patient medically free was complaining of a severe throbbing headache, referred from primary health care service due to high blood pressure (BP) (210/110 mm Hg). No blurring of vision, weakness, or loss of consciousness was mentioned. On physical examination, he was vitally stable apart from high BP, fully conscious and oriented with no abnormal neurogenic, thoracic or abdominal findings. Laboratory tests including complete blood count, basic metabolic panel, hepatic metabolic panel, and renal profile were normal.
Because of high BP, NECT brain was requested to exclude hemorrhage or minor stroke. The CT brain was seen by the ER specialist in charge and analyzed as normal. BP managed in the emergency department.
The on-call radiologist noticed a tubular hyperdense structure in the left para midline at the region of the left septal and internal cerebral veins (Fig. 1) and was worried about left internal cerebral vein thrombosis. The patient was admitted under medical service for observation and scheduled for MR venogram due to the suspicion of venous thrombosis.
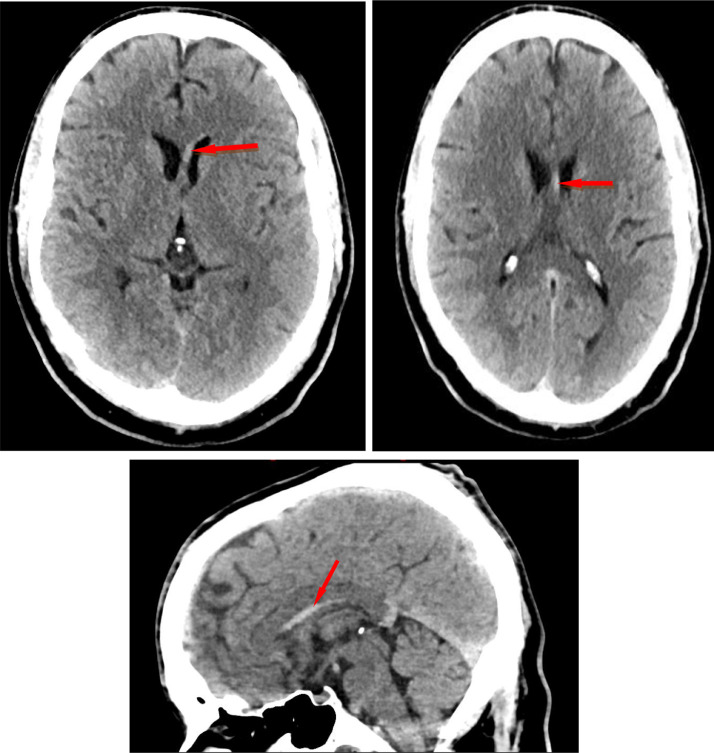
Fig. 1.
(a) Selected NECT axial images were showing a tubular hyperdense structure in the left para midline adjacent to the ventral horn of left ventricle (arrow). No parenchymal abnormalities were seen. (b) Selected sagittal reformat from the NECT brain showing a tubular hyperdense structure in the territory of the left internal cerebral vein (arrow).
MRI demonstrated a signal void tubular structure on conventional T1 and T2 WI in the region of the left internal cerebral vein with draining small left frontal lobe veins (Fig. 2). This structure was draining into the great cerebral vein (vein of Galen). No surrounding parenchyma changes were noted. magnetic resonance venography demonstrated this structure that was compatible with a DVA. Based on MRI findings and the absence of neurological manifestations, the patient was informed about the benign nature of his anomaly and was discharged home.
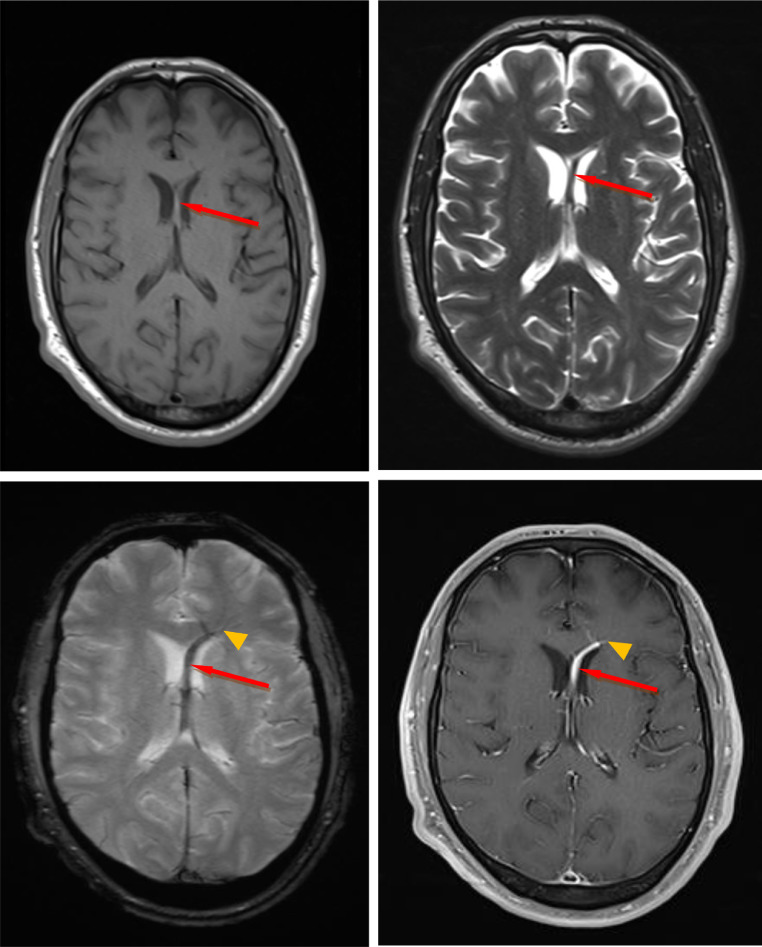
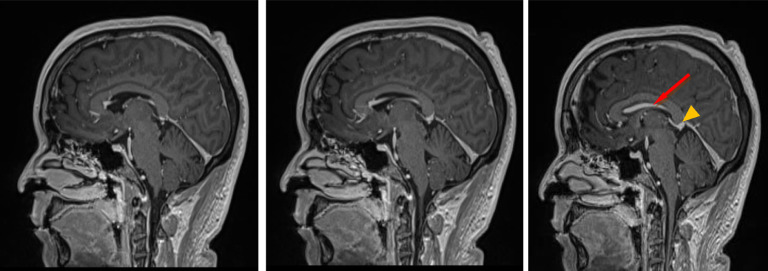
Fig. 2.
(a) Selected axial T1, T2, susceptibility, and contrast-enhanced T1 images show a small network of veins (arrowhead) in the left frontal deep white matter converging towards the left frontal horn and draining into the left anterior septal vein which extends posteriorly and drains into the left internal cerebral vein (arrow). (b) Selected sagittal images from T1-MR venogram of the brain showing dilated left internal cerebral vein (arrow) which drain into the great cerebral vein (arrowhead).
Discussion
DVAs also called venous angiomas are often asymptomatic and therefore are often found incidentally. The most frequent signs include headache, dizziness, seizure, and focal neurological deficits [3]. Before the advent of CT and MRI, DVAs were believed to be a rare cause of intracranial hemorrhage and seizures. With the extended use of MRI, DVAs are now more frequently discovered and are benign and asymptomatic [4]. They are not true vascular malformations and are thought to represent normal variations of parenchymal venous drainage [5]. DVA could potentially have unwanted consequences such as venous infarction and hemorrhage if surgically removed [2].
About one-third of DVA are located infratentorial commonly in the cerebellum while the remaining two-thirds are supratentorial; half are located in the frontal lobe [6]. Regarding the drainage pattern, DVAs more commonly drain superficially into the cortical veins 70%, but a deep venous drainage pattern can be evident in up to 20%. Both superficial and deep drainage were seen in 10% [2].
Regardless of the imaging modality employed, the diagnosis of a DVA relies on demonstrating typical caput medusae draining into a collecting vein [7]. On NECT scan of the brain, they are usually evident by the demonstration of slightly hyperdense blood compared to the normal brain parenchyma in addition to parenchymal abnormalities related to DVA such as calcification, hemorrhage, and atrophy. Signs of thrombosed DVA include marked hyperdensity of the collecting vein which warrants further investigation. CT venography visualizes the DVA as linear enhancing structures merging into a single enlarged draining vein [2]. Flow voids and phase-shift artifact are demonstrated on noncontrast T1 and T2-weighted MRI which produced by the collecting vein of a DVA and by the larger venous radicles of the caput medusae. MRI is superior to CT in demonstrating associated parenchymal abnormalities [7].
According to the widely acknowledged classification of cerebral vascular malformations, it is normal to differentiate between arteriovenous malformations, capillary telangiectasias, cavernomas, and venous angiomas. All 4 types of cerebral malformations can also be differentiated by distinct neuroradiological features that enable the radiologist to make an exact diagnosis without knowing the patient's history [6]. For example; DVAs lack an arterial component and have unaffected intervening neural parenchyma, which distinguishes these lesions from arteriovenous malformations [3].
Associations between DVAs and head and neck venous malformations have been reported. Up to 20% of patients with large cervicofacial venous malformations have DVAs [4].
Conclusion
The vast majority of DVAs cases follow a benign clinical course and do not require follow-up imaging studies or specific medical management. However, caution while interpreting the radiological images and further evaluation with venogram studies is needed due to possible complexity, thrombosed DVA, or even other associated vascular malformation could be present.
Footnotes
Financial support and sponsorship: None.
Conflicts of interest: The authors declare that they have no conflicts of interest.
References
- 1.Mooney M.A., Zabramski J.M. Developmental venous anomalies. Handb Clin Neurol. 2017;143:279–282. doi: 10.1016/B978-0-444-63640-9.00026-6. [DOI] [PubMed] [Google Scholar]
- 2.Nabavizadeh S.A., Mamourian A.C., Vossough A., Loevner L.A., Hurst R.. The many faces of cerebral developmental venous anomaly and its mimicks: spectrum of imaging findings. J Neuroiamging 2016;26(5):463–72. [DOI] [PubMed]
- 3.Parker B.J., Sabb B.J. Developmental venous anomaly complicated by cerebral venous infarction. Radiol Case Rep. 2007;2(4):48. doi: 10.2484/rcr.2007.v2i4.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aoki R., Srivatanakul K. Developmental venous anomaly: benign or not benign. Neurol Med-Chir. 2016;56(9):534–543. doi: 10.2176/nmc.ra.2016-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kroll H., Soares B.P., Saloner D., Dillon W.P., Wintermark M. Perfusion-CT of developmental venous anomalies: typical and atypical hemodynamic patterns. J Neuroradiol. 2010;37(4):239–242. doi: 10.1016/j.neurad.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Topper R., Jurgens E., Reul J., Thron A. Clinical significance of intracranial developmental venous anomalies. J Neurol Neurosurg Psychiatry. 1999;67(2):234–238. doi: 10.1136/jnnp.67.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruiz D.S., Yilmaz H., Gailloud P. Cerebral developmental venous anomalies: current concepts. Ann Neurol. 2009;66(3):271–283. doi: 10.1002/ana.21754. [DOI] [PubMed] [Google Scholar]