Abstract
Diabetic retinopathy (DR) is a microvascular disease of the retina and the leading cause of visual disability in diabetic patients. Genetic factors have shown to play a pivotal role in DR onset, and several candidate genes have been associated with its progression. A literature search was performed to identify the genes known to be associated with DR through linkage analysis, candidate gene association, and genome-wide association studies (GWAS). A further literature search was performed to discover their potential connection with various biological pathways. A total of 65 genes were found and several of these genes belong to major signaling pathways known to play a significant role in DR, including systemic inflammation, angiogenesis, and neurogenesis. A comprehensive analysis presented in this review will be helpful in unraveling the role of genetics in the pathogenesis of DR.
Background
Diabetic retinopathy (DR) is one of the major microvascular complications of diabetes [1]. According to its severity, DR can be classified into non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). Hallmarks of NPDR include microaneurysms, hard exudates, cotton wool spots, intra-retinal micro-vascular abnormalities, and venous beading [2]. This condition can either remain stable or progressively develop into PDR which is characterized by neovascularization, pre-retinal hemorrhage, and vitreous hemorrhage [3]. The precise mechanisms underlying DR etiology have not been fully elucidated, and consequently, the currently available therapies are insufficient to reverse or prevent diabetic complications of the eye [1, 4–6]. Several genetic studies including linkage analysis, candidate gene association, and genome-wide association studies (GWAS) have identified a total of 65 genes associated with DR (Fig. 1). Most of the genes associated with DR have been identified through candidate gene-based association studies and GWAS (Table 1) [7–19].
Fig. 1.
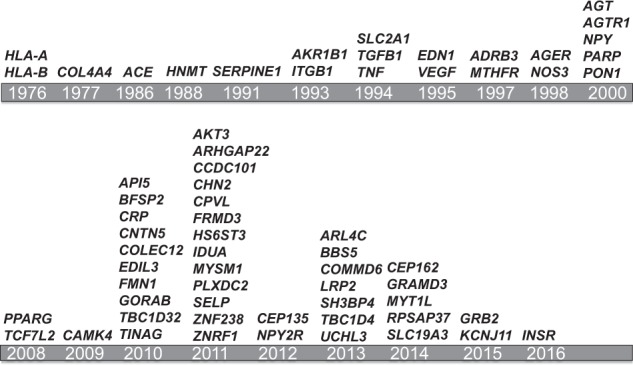
Chronological list of genes associated with diabetic retinopathy. A comprehensive search of published literature was performed to generate a list of all the genes associated with diabetic retinopathy. Before 2007, most of the genes were discovered using linkage analysis or candidate gene approach. After 2007, the evolution of genome wide association studies (GWAS) led to the discovery of a large number of genes
Table 1.
List of genes associated with diabetic retinopathy
| Chr | Nearby genes | SNPs (top signal) | p value | OR | Type of diabetes | Subjects (n) | Type of DR | Country | Year | Reference |
|---|---|---|---|---|---|---|---|---|---|---|
| 1p5.89 | MYSM1 | rs2811893 | 3.1 × 10−7 | 1.5 | T2D | 174 patients, 575 controls | PDR, NPDR | Taiwan | 2011 | [67 GWAS] |
| 1q23.2 | CRP | rs2808629 | 6.0 × 10-3 | 1.3 | T2D | 618 patients, 400 controls | PDR, NPDR | China | 2015 | [68] |
| 1q24.2 | SELP | rs6128 | 1.0 × 10−4 | 0.43 | T2D | 6639 patients, 4047 controls | PDR | International | 2011 | [11] |
| 1q24.2 | GORAB | rs6427247 | 3.3 × 10−2 | 1.37 | T2D | 819 patients, 1153 controls | PDR, NPDR | China | 2015 | [62] |
| 4.6 × 10−4 | 2.17 | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] | |||
| 1q44 | AKT3, ZBTB18 | rs476141 | 1.2 × 10−7 | 1.37 | T1D | 973 patients, 1856 controls | PDR | USA | 2011 | [61 GWAS] |
| 2p25.3 | MYT1L | rs10199521 | 2.2 × 10−2 | 1.25 | T2D | 309 patients, 1490 controls | PDR | China | 2016 | [69] |
| 2q31.1 | LRP2, BBS5 | rs1399634 | 2.0 × 10−6 | 1.50 | T2D | 437 patients, 570 controls | PDR, NPDR | China | 2013 | [25 GWAS] |
| 2q36.3 | SLC19A3 | rs6713116 | 3.2 × 10−6 | 0.41 | T1D | 1,566 patients, 218 controls | NPDR | Finland | 2016 | [70 GWAS] |
| 2q37.2 | ARL4C, SH3BP4 | rs2380261 | 2.1 × 10−6 | 1.50 | T2D | 437 patients, 570 controls | PDR, NPDR | China | 2013 | [25 GWAS] |
| 3p25 | PPARG | rs1801282 | 9.7 × 10−3 | 0.73 | T1D | 518 patients, 1389 controls | PDR, NPDR | USA-Canada | 2015 | [19] |
| 3q22.1 | BFSP2 | rs1197310 | 3.4 × 10−4 | 2.25 | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| 4p16.3 | IDUA | rs6856425 | 2.1 × 10−5 | 2.88 | T2D | 969 patients, 1789 controls | PDR | International | 2011 | [11] |
| 4q32.1 | NPY2R | rs1902491 | 2.8 × 10−5 | - | T1D | 208 patients, 261 controls | PDR | USA | 2012 | [21] |
| 4q12 | CEP135 | rs4865047 | 2.1 × 10−5 | - | T1D | 208 patients, 261 controls | PDR | USA | 2012 | [21] |
| 5q9.35 | KIAA0825 | rs17376456 | 3.0 × 10−15 | 3.63 | T2D | 174 patients, 575 controls | PDR, NPDR | Taiwan | 2011 | [67 GWAS] |
| 5q14 | EDIL3 | rs1445754 | 3.4 × 10−4 | 0.37 | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| 5q21 | CAMK4 | rs2300782 | 6.0 × 10−5 | 2.64 | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| 5q23.3 | RPSAP37,GRAMD3 | rs1073203 | 2.7 × 10−2 | 1.4 | T1D, T2D | 163 patients, 300 controls | PDR, NPDR | Australia | 2014 | [71] |
| 6p11-12 | TINAG | rs6909083 | 1.8 × 10−5 | - | TD2 | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| 6q14.3 | CEP162 | rs9362054 | 1.4 × 10−7 | 1.36 | T2D | 837 patients, 1149 controls | NPDR | Japan | 2014 | [72 GWAS] |
| 6q22 | TBC1D32 | rs17083119 | 2.8 × 10−5 | - | TD2 | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| 7p15.1 | CPVL, CHN2 | rs39059 | 3 × 10−4 | 1.29 | T2D | 805 patients, 1017 controls | PDR, NPDR | China | 2011 | [73] |
| 9p21.33 | FRMD3 | rs10868025 | 3.4 × 10−2 | 0.83 | T2D | 618 patients, 280 controls | PDR, NPDR | China | 2011 | [73] |
| 10p4.93 | ARHGAP22 | rs4838605 | 1.9 × 10−9 | 1.65 | T2D | 174 patients, 575 controls | PDR, NPDR | Taiwan | 2011 | [67 GWAS] |
| 10p2.06 | PLXDC2 | rs12219125 | 7.2 × 10−3 | 1.40 | T1D | 518 patients, 1389 controls | PDR, NPDR | USA- Canada | 2015 | [19] |
| 9.3 × 10−9 | 1.67 | T2D | 174 patients, 575 controls | PDR, NPDR | Taiwan | 2011 | [67 GWAS] | |||
| 10q25.3 | TCF7L2 | rs7903146 | 4.0 × 10−4 | 1.77 | T2D | 154 patients, 171 controls | PDR | Italy | 2013 | [43] |
| 11p12 | API5 | rs899036 | 5.0 × 10−4 | 0.34 | T2D | 819 patients, 1153 controls | PDR, NPDR | China | 2015 | [62] |
| rs899036 | 2.5 × 10−4 | 0.32 | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] | ||
| 11p15.1 | KCNJ11 | rs5219 | 1.0 × 10−3 | 1.61 | T2D | 105 patients, 475 controls | NPDR | China | 2015 | [23] |
| 11q22.1 | CNTN5 | rs10501943 | 2.5 × 10−4 | 3.04 | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| 13q9.57 | HS6ST3 | rs2038823 | 4.7 × 10−11 | 2.33 | T2D | 174 patients, 575 controls | PDR, NPDR | Taiwan | 2011 | [67 GWAS] |
| 13q22.2 | TBC1D4 | rs9565164 | 1.3 × 10−7 | 1.70 | T2D | 437 patients, 570 controls | PDR, NPDR | China | 2013 | [25 GWAS] |
| 15q13 | FMN1 | rs11635920 | 7.2 × 10−5 | - | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| 16p28.5 | CCDC101 | rs10521145 | 3.4 × 10−6 | 0.58 | T1D | 281 patients, 1715 controls | PDR | USA | 2011 | [61 GWAS] |
| 16q22.3 | ZNRF1 | rs17684886 | 3.9 × 10−3 | 0.81 | T2D | 819 patients, 1153 controls | PDR, NPDR | China | 2015 | [62] |
| 17q25.1 | GRB2 | rs9896052 | 4.2 × 10−8 | - | T1D, T2D | 1175 patients, 1319 controls | PDR, NPDR | Australia-India | 2015 | [74] |
| 18p11.2 | COLEC12 | rs599019 | 4.1 × 10−4 | 0.15 | T2D | 103 patients, 183 controls | PDR, NPDR | USA-Mexico | 2010 | [36 GWAS] |
| rs599019 | 1.2 × 10−2 | 0.84 | T2D | 819 patients, 1153 controls | PDR, NPDR | China | 2015 | [62] | ||
| 19p13.2 | INSR | rs2115386 | 1.1 ×10−4 | 1.44 | T2D | 309 patients, 1490 controls | PDR | China | 2016 | [69] |
| rs2115386 | 9.1×10−4 | 1.28 | T2D | 567 patients, 1490 controls | NPDR | China | 2016 | [69] |
To improve our understanding of the functional role of these genetic factors in DR pathogenesis, we mapped these genes to biological processes and pathways. Our analyses revealed that majority of these genes belong to various biological pathways known to have a significant contribution to the DR pathology including insulin signaling, angiogenesis (HIF-1 signaling, regulation of blood vessel size, VEGF signaling), inflammation (IL-6 signaling, leukocyte adhesion, TGF-β and TNF signaling), lipid metabolic process, neurogenesis (neural cells differentiation, neurotrophin signaling), protein kinase signaling (Jak-STAT, PI3K-Akt, MAPK, Ras and mTOR signaling) and regulation of endothelial cell / leukocytes interaction (cell adhesion molecules, cell migration) (Table 2).
Table 2.
Candidate genes and important signaling pathways associated with diabetic retinopathy
| Signaling pathways | Candidate genes |
|---|---|
| Insulin signaling | AKT3,GRB2,SLC2A1,KCNJ11,TBC1D4,CEP135,UCHL3, HNMT, INSR |
| Angiogenesis | EDIL3,NOS3,SERPINE1,PLXDC2 |
| Blood vessel development | ACE,AGT,EDN1,NOS3,SELP,TCF7L2 |
| HIF-1 signaling | AKT3,EDN1, SLC2A1,NOS3,SERPINE1,VEGFA |
| Patterning of blood vessels | EDN1,VEGFA, GRAMD3 |
| Regulation of blood vessel size | ADRB3,AGT,AGTR1,EDN1,NOS3 |
| Response to hypoxia | ACE,EDN1, MTHFR,NOS3,TGFB1 |
| VEGF signaling | AKT3,GRB2,NOS3,VEGFA |
| Inflammation: | |
| IL-6 signaling | AKT3,GRB2,ICAM1, CRP |
| Leukocyte adhesion | ICAM1,ITGB1,SELP,TNF, |
| NF-kappa B activation | AGT,ICAM1,PARP1,TGFB1,TNF |
| NF-kappa B inhibition | COMMD6 |
| TGF-beta signaling | TGFB1,TNF |
| TNF signaling | AKT3,EDN1,ICAM1,PARP1,TNF |
| Lipid metabolic process | LRP2,PON1,ARL4C,COLEC12 |
| Neurogenesis: | |
| Apoptotic process | API5,GORAB |
| Neural cells differentiation | ZBTB18,ZNRF1 |
| Neuroactive ligand-receptor interaction | ADRB3,AGTR,NPY,NPY2R |
| Neurotrophin signaling | AKT3,CAMK4,GRB2 |
| Jak-STAT signaling | AKT3, GRB2 |
| PI3K-Akt signaling | AKT3,COL4A4, GRB2,ITGB1,NOS3,VEGFA |
| Protein kinase cascade | ADRB3,AGT,EDN1, TGFB1,TNF |
| MAPK signaling | AKT3,GRB2,TGFB1,TNF |
| Ras signaling | AKT3,GRB2,VEGFA |
| mTOR signaling | AKT3,TNF,VEGFA |
| Regulation of endothelial cell / leukocytes interaction | |
| Cell adhesion molecules (CAMs) | FMN1,ICAM1,ITGB1, SELP, COL4A4,ITGB1 |
| ECM-receptor interaction | ACE,AGT,NOS3,TGFB1 |
| Regulation of endothelial cell migration | AGT,EDN1,TGFB1 |
| Regulation of cellular localization | AGT,EDN1,KCNJ11,TCF7L2,TGFB1,TNF |
| Regulation of cell migration | ACE,AGT,EDN1,ICAM1,ITGB1,NOS3,SELP,TGFB1 |
Insulin signaling
A total of 9 genes (AKT3, GRB2, SLC2A1, KCNJ11, TBC1D4, CEP135, UCHL3, INSR, and HNMT) were mapped to insulin signaling pathway. Insulin activates the insulin receptor (INSR) tyrosine kinase which phosphorylates numerous signaling partners. In the retina, disrupted INSR signaling has been shown to produce cellular dysfunction [20]. Among the INSR phosphorylated signaling partners, the activation of the AKT3/PKB and the PKCζ cascade regulates diverse biochemical responses including glycogen synthesis, protein synthesis, and autophagy. One such biochemical response is mediated by GRB2 activation, which forms a stable complex with phosphorylated insulin receptor substrate (IRS-1) and the SH2 domain-containing oncogenic protein, SHC. CEP135 (Centrosomal protein 135kDa), expressed in the retina, encodes a centrosomal protein required for centriole-centriole cohesion during the interphase of the cell cycle [21]. CEP135 interacts with SMAD9, a critical component in the TGF-β signaling pathway which is also upregulated in diabetes and diabetic retinopathy [21]. KCNJ11 (Potassium voltage-gated channel subfamily J member 11) encodes for a potassium channel controlled by G-proteins and was found to be associated with the sulfonylurea receptor. The common variant of KCNJ11 (rs5219) has a strong association with DR [22, 23]. SLC2A1 (Solute carrier family 2, member 1 also known as GLUT1) is expressed in endothelial and epithelial barriers including the retinal capillary endothelium, retinal pigment epithelium, and the basal cells of the corneal epithelium in the eye [24]. SLC2A1 is an important target for DR as it is the only glucose transporter between the blood and retina [24]. The knockdown by intraocular injections of a pool of siRNAs directed against SLC2A1 mRNA significantly reduced retinal glucose levels in diabetic mice. TBC1D4 (TBC1 domain family, member 4) is known to play a role in insulin signaling in the retina and DR pathogenesis [25]. UCHL3 (Ubiquitin carboxyl-terminal esterase L3) is a deubiquitinating enzyme playing a role in the maintenance of ubiquitin levels within the cell through processing of ubiquitin precursors and ubiquitinated proteins. Several studies have shown the role of UCHL3 in insulin signaling and retinal maintenance in stress conditions [26, 27].
Angiogenesis
The crucial role of angiogenesis in DR has been recognized since 1985 when Rand et al. reported how changes in retinal venular caliber could predict vision loss [28]. VEGF is a heparin-binding homodimeric glycoprotein that acts via endothelial-specific receptor tyrosine kinases, among which VEGFR2 is the main VEGF receptor regulating angiogenesis. VEGF is one of the targets of the HIF (Hypoxia-Inducible Factor), a basic helix-loop-helix transcription factor that regulates the response to hypoxia. HIF induces expression of proteins controlling glucose metabolism, cell proliferation, vascularization, and blood vessel development such as SELP (P-selectin), EDN1 (Endothelin 1), LDHA (Lactate dehydrogenase-A), TGFβ1, and b-FGF (basic fibroblast growth factor) [29]. VEGF was amongst the first factors known to regulate retinal neovascularization and blood-retinal barrier (BRB) breakdown in DR [30]. The absence of the SLC2A1 carrier in neovascular tissue of PDR is a sign of the loss of glucose selective permeability [31] and GRB2 participates in the MAPK pathway via Ras in response to vascular endothelial growth factor signaling [32].
ACE, AGT and AGTR belong to the renin-angiotensin system, a crucial pathway which regulates blood pressure. The production of Ang II within the retina leads to a series of hemodynamic and growth promoting effects that trigger DR development [33]. Ang-II induces capillary growth, vascular permeability, and an increase in oxidative stress via stimulation of growth factors such as TGF-β, VEGF, and PDGF [34]. Furthermore, the increase of Ang-II has been shown in diabetic patients, particularly with microangiopathy and microvascular damage [35]. EDIL3 (EGF-like repeats and discoidin domains 3) encodes for an integrin ligand which plays an important role in mediating angiogenesis and vessel wall remodeling. It also influences retinal endothelial cell behavior [36]. The EDN1 (Endothelin 1) gene encodes a protein that is primarily produced in vascular endothelium, vascular smooth muscle cells, macrophages, leukocytes, cardiomyocytes, and fibroblasts [37]. Endothelin 1 plays a pivotal role in endothelial dysfunction, one of the significant elements in the pathogenesis of DR [38]. Studies have shown high EDN1 expression in vascular and extravascular sites in the retina and its contribution to abnormal retinal hemodynamics in DR [39].
Endothelial nitric oxide synthase (eNOS) plays an essential role in maintaining vascular homeostasis. Deficiency in eNOS expression coupled with concomitant activation of inducible nitric oxide synthase (iNOS) triggers highly reactive nitrogen species (RNS) formation, thus, leading to oxidative stress and accelerated retinopathy [40]. PLXDC2 (Plexin domain-containing protein 2), also known as TEM7R (tumor endothelial marker seven-related protein), has been implicated in neurogenesis and angiogenesis [19, 41]. PDR results in part from the formation of fibrovascular membranes (FVMs) in the posterior fundus. Tumor endothelial marker 7 (TEM7) is a protein that is highly expressed in the endothelial cells of tumors. TEM7 has been shown to play a significant role in the proliferation and maintenance of neovascular endothelial cells in the FVMs [42]. TCF7L2 (Transcription factor 7-like 2) participates in the WNT signaling pathway and regulates MYC expression by binding to its promoter in a sequence-specific manner [43]. ARHGAP22 encodes a Rho family GTPase protein, which is a component in the regulation of endothelial cell capillary tube development during angiogenesis [44]. Similar to PLXDC2, ARHGAP22 has been implicated in PDR and is involved in endothelial cell angiogenesis.
Inflammation
Eleven genes associated with DR (CRP, AKT3, GRB2, ICAM1, ITGB1, SELP, TNF, AGT, PARP1, COMMD6, and EDN1) were mapped to pathways involved in inflammation. Several studies have shown that patients exhibit higher blood levels of inflammatory markers such as C-reactive protein (CRP), interleukin-6 (IL-6), transforming growth factor (TGF-β), tumor necrosis factor-alpha (TNF-α) [27], cyclooxygenase-2 (COX-2), and interleukin-1 (IL-1) [45, 46]. Moreover, soluble TNF-receptor levels have been associated with an increased risk of severe DR [25]. IL-6 is a cytokine that provokes a broad range of cellular and physiological responses including the immune response, inflammation, hematopoiesis, and oncogenesis by regulating cell growth, gene activation, proliferation, survival, and differentiation. AKT3, CRP, ICAM1 and GRB2 are known to be involved in the IL-6 signaling. AKT3, a member of the AKT (or PKB) serine/threonine-protein kinase family, regulates many processes including metabolism, proliferation, cell survival, growth and angiogenesis. In particular, AKT3 has been shown to be stimulated by platelet-derived growth factor (PDGF), insulin, and insulin-like growth factor 1 (IGF1), both implicated in proliferative retinopathy [21, 47]. The GRB2 gene codes for an adapter protein that is involved in the Ras-mediated pathway which leads to the activation of transcription factors such as EIK1 and NF-IL-6 (C/EBP-Beta). Burton et al. [32]. recently described GRB2 as a promising candidate for DR susceptibility because increase of this protein in mouse retina was correlated to retinal stress leading to DR. Also, GRB2 protein is expressed in all layers of the human retina. The COMMD6 (COMM domain containing 6) gene belongs to a family of NF-kB inhibiting proteins characterized by the presence of a COMM domain and down-regulates TNF-induced NF-kB activation [48]. PARP1 (poly(ADP-ribose) polymerase), a DNA repair enzyme activated by oxidative damage, mediates the hyperglycemia-induced activation of NF-kB, pro-inflammatory molecules, cytokines, and iNOS. Its overexpression leading to a depletion of ATP, NAD+ and NADH [49]. The loss of these cofactors cause an impairment in glycolysis and mitochondrial respiration that affect cellular viability. The TNF gene encodes for a pro-inflammatory cytokine which is member of the tumor necrosis factor superfamily. Studies have described the involvement of TNF-α in diabetic retinal microvascular damage and drugs that target TNF-α have been shown to reduce leukostasis, retinal vascular leakage, and retinal cell death in animal models [50] . TGF-β, a cytokine implicated in multiple cellular functions including proliferation, differentiation, adhesion, and migration, has been shown to be involved in the basement membrane thickening and matrix accumulation in the blood vessels [51]. The gene expression profile of retinal vessels isolated from streptozotocin- treated rats revealed an increased expression in 20 genes of the TGF-β signaling pathways [52]. ICAM1, ITGB1 and SELP are particularly important in leukocyte adhesion, one of the earliest signs of retinal complications. ICAM1 (Intercellular adhesion molecule 1 or CD18) is a member of the ICAM proteins that act as ligands for the leukocyte adhesion protein, LFA-1. This gene encodes for a cell surface glycoprotein, typically on endothelial cells, whose expression is induced by increased levels of VEGF. Specific inhibition of ICAM1 in diabetic animals leads to reduction of leukostasis and BRB breakdown [53]. The ITGB1 (Integrin, beta 1) belongs to the integrins family and plays a pivotal role in PDR and proliferative vitreo-retinopathy due to its contribution to the terminal event of tractional retinal detachment [54].
Neurogenesis
Several DR associated genes (API5, GORAB, ZBTB18, ZNRF1, ADRB3, AGTR, NPY, NPY2R, AKT3, CAMK4, and GRB2) belong to the neurological processes. Despite the retina’s peripheral localization, it is actually part of the central nervous system. DR is a multifactorial disease involving not only the vasculature, but also the neurons and glia and studies have suggested that neuronal changes in the retina may occur before vascular alterations [55, 56]. There is sufficient evidence of neurodegenerative changes in DR including increased apoptosis of ganglion cells, glial cell reactivity, microglial activation, and altered glutamate metabolism [57].
Neurotrophins (NTs) are a family of growth factors that mediate the growth, differentiation, and survival of developing neurons. A significant increase was observed in the expression of NT-3 and NT-4 in vitreous samples from PDR patients compared to non-diabetic controls [58]. Interestingly, AKT3 and GRB2 have been shown to participate in NT signaling. API5 (Apoptosis inhibitor 5) is an anti-apoptotic factor which acts as a suppressor of the transcription factor E2F1 which induces apoptosis and also interacts with, and negatively regulates, Acinus, a nuclear factor involved in apoptotic DNA fragmentation. CAMK4 (Calcium/calmodulin-dependent protein kinase IV) acts in the calcium-triggered CaMKK-CaMK4 signaling cascade. This kinase is expressed in the brain, spleen, thymus, and regulates the activity of several transcription factors implicated in the immune response, inflammation, and memory consolidation [59]. Neuropeptide Y (NPY) and its receptor (NPY2R) play a pivotal role in the central nervous system regulating many physiological processes. The Leu7Pro (codon 7) polymorphism in NPY was identified as a risk factor for DR development in a well-characterized cohort of patients with Type 2 diabetes [16]. ZBTB18 (Zinc finger and BTB domain containing 18) encodes a C2H2-type zinc finger protein which acts as a transcriptional repressor of key pro-neurogenic genes such as Neurogenin2 and NeuroD1[60]. ZBTB18 is also involved in various developmental processes such as myogenesis and other aspects of brain development [61]. ZNRF1 (Zinc and ring finger 1, E3 ubiquitin protein ligase) is an E3 ubiquitin-protein ligase that mediates the ubiquitination of AKT1 and glutamate-ammonia ligase (GLUL), playing a role in neuronal cell differentiation. ZNRF1 regulates neurodegeneration, maintenance of neuronal transmission, plasticity, and Schwann cell differentiation in DR [62].
Regulation of endothelial cell / leukocytes interaction
An important cause of damage in the vascular endothelium in DR is leukocyte activation and migration that is mediated by the specific adhesion molecules expressed on the cell surface of leukocytes and the endothelium. A significant correlation between the number of leukocytes accumulated within the vessel and capillary damage in the retina has been identified in post-mortem DR patients [63]. Moreover, pre-clinical animal studies of early DR have also highlighted the disruption of the retinal endothelium caused by adhering leukocytes and the subsequent increase of the vascular permeability [64]. Thirteen genes (ACE, AGT, COL4A4, EDN1, FMN1, ICAM1, ITGB1, KCNJ11, NOS3, SELP, TCF7L2, TGFB1, TNF) were mapped to this pathway. ICAM1, EDN1, and SELP are important markers of endothelial dysfunction that have been linked with the development of DR [65]. ICAM-1 level increases in the diabetic retina, even in the early stages of DR. Endothelial complications in DR are dramatically reduced in animals treated with anti-ICAM-1 antibodies [64]. EDN-1 is known to be a potent vasoconstrictor molecule, implicated in the disruption of retinal hemodynamics and DR progression [39]. COL4A4 (Collagen, type IV, alpha 4) encodes one of the six subunits of type IV collagen, the major structural component of basement membranes and modification of collagen metabolism in the basement membrane is associated with DR [66]. FMN1 (Formin 1) is involved in cell adhesion and morphogenesis [36].
Conclusions
In this review, we compiled a comprehensive list of genetic factors associated with DR. Further analyses revealed the biological functions of these genes in DR pathogenesis. The identification of genetic factors and their contribution to DR etiology will allow for tailored pharmacogenomics approaches for the treatment of DR.
Summary
Diabetic retinopathy (DR) is a microvascular disease of the retina and the leading cause of visual disability in diabetic patients.
Genetic factors have shown to play a pivotal role in DR onset, and several candidate genes have been associated with its progression.
This review presents an insight into genes associated with DR and their role in various biological functions and signaling pathways.
Acknowledgements
This research was supported by an NIH/NEI grant to Shruti Sharma at the Augusta University (5R01-EY026936).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stitt Alan W, Lois N, Medina Reinhold J, Adamson P, Curtis Timothy M. Advances in our understanding of diabetic retinopathy. Clin Sci. 2013;125:1–17. doi: 10.1042/CS20120588. [DOI] [PubMed] [Google Scholar]
- 2.Aiello LM. Perspectives on diabetic retinopathy. Am J Ophthalmol. 2003;136:122–35. doi: 10.1016/S0002-9394(03)00219-8. [DOI] [PubMed] [Google Scholar]
- 3.Hietala K, Forsblom C, Summanen P, Groop PH. Heritability of proliferative diabetic retinopathy. Diabetes. 2008;57:2176–80. doi: 10.2337/db07-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stitt AW, Curtis TM, Chen M, Medina RJ, McKay GJ, Jenkins A, et al. The progress in understanding and treatment of diabetic retinopathy. Prog Retin Eye Res. 2016;51:156–86. doi: 10.1016/j.preteyeres.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Osaadon P, Fagan XJ, Lifshitz T, Levy J. A review of anti-VEGF agents for proliferative diabetic retinopathy. Eye. 2014;28:510–20. doi: 10.1038/eye.2014.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheung N, Wong IY, Wong TY. Ocular Anti-VEGF therapy for diabetic retinopathy: overview of clinical efficacy and evolving applications. Diabetes Care. 2014;37:900–5. doi: 10.2337/dc13-1990. [DOI] [PubMed] [Google Scholar]
- 7.Safi SZ, Qvist R, Kumar S, Batumalaie K, Ismail ISB. Molecular mechanisms of diabetic retinopathy, general preventive strategies, and novel therapeutic targets. Biomed Res Int. 2014;2014:801269. doi: 10.1155/2014/801269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab. 2013;17:20–33. doi: 10.1016/j.cmet.2012.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abhary S, Hewitt AW, Burdon KP, Craig JE. A systematic meta-analysis of genetic association studies for diabetic retinopathy. Diabetes. 2009;58:2137–47. doi: 10.2337/db09-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liew G, Klein R, Wong TY. The role of genetics in susceptibility to diabetic retinopathy. Int Ophthalmol Clin. 2009;49:35–52. doi: 10.1097/IIO.0b013e31819fd5d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sobrin L, Green T, Sim X, Jensen RA, Tai ES, Tay WT, et al. Candidate gene association study for diabetic retinopathy in persons with type 2 diabetes: the candidate gene association resource (CARe) Invest Ophthalmol & Vis Sci. 2011;52:7593–602. doi: 10.1167/iovs.11-7510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ng DPK. Human genetics of diabetic retinopathy: current perspectives. J Ophthalmol. 2010;2010:172593. doi: 10.1155/2010/172593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falck AAK, Knip JM, Ilonen JS, Laatikainen LT. Genetic markers in early diabetic retinopathy of adolescents with type i diabetes. J Diabetes Complicat. 1997;11:203–7. doi: 10.1016/S1056-8727(96)00051-7. [DOI] [PubMed] [Google Scholar]
- 14.Hawrami K, Hitman GA, Rema M, Snehalatha C, Viswanathan M, Ramachandran A, et al. An association in non-insulin-dependent diabetes mellitus subjects between susceptibility to retinopathy and tumor necrosis factor polymorphism. Hum Immunol. 1996;46:49–54. doi: 10.1016/0198-8859(95)00177-8. [DOI] [PubMed] [Google Scholar]
- 15.Sakane N, Yoshida T, Yoshioka K, Nakamura Y, Umekawa T, Kogure A, et al. 3-Adrenoreceptor gene polymorphism: a newly identified risk factor for proliferative retinopathy in NIDDM Patients. Diabetes. 1997;46:1633–6. doi: 10.2337/diacare.46.10.1633. [DOI] [PubMed] [Google Scholar]
- 16.Niskanen L, Voutilainen-Kaunisto R, Teräsvirta M, Karvonen MK, Valve R, Pesonen U, et al. Leucine 7 to proline 7 polymorphism in the neuropeptide y gene is associated with retinopathy in Type 2 diabetes. Exp Clin Endocrinol Diabetes. 2000;108:235–6. doi: 10.1055/s-2000-7748. [DOI] [PubMed] [Google Scholar]
- 17.Kao YL, Donaghue K, Chan A, Knight J, Silink M. A variant of paraoxonase (PON1) gene is associated with diabetic retinopathy in IDDM. J Clin Endocrinol & Metab. 1998;83:2589–92. doi: 10.1210/jcem.83.7.5096. [DOI] [PubMed] [Google Scholar]
- 18.Alcolado JC, Baroni MG, Li SR, Galton DJ. Genetic variation around the collagen IV 1a gene locus and proliferative retinopathy in type 2 diabetes mellitus. Hum Hered. 1993;43:126–30. doi: 10.1159/000154129. [DOI] [PubMed] [Google Scholar]
- 19.Hosseini SM, Boright AP, Sun L, Canty AJ, Bull SB, Klein BEK, et al. The association of previously reported polymorphisms for microvascular complications in a meta-analysis of diabetic retinopathy. Hum Genet. 2015;134:247–57. doi: 10.1007/s00439-014-1517-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reiter CEN, Gardner TW. Functions of insulin and insulin receptor signaling in retina: possible implications for diabetic retinopathy. Prog Retin Eye Res. 2003;22:545–62. doi: 10.1016/S1350-9462(03)00035-1. [DOI] [PubMed] [Google Scholar]
- 21.Grassi MA, Tikhomirov A, Ramalingam S, Lee KE, Hosseini SM, Klein BEK, et al. Replication analysis for severe diabetic retinopathy. Invest Ophthalmol & Vis Sci. 2012;53:2377–81. doi: 10.1167/iovs.11-8068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koo BK, Cho YM, Park BL, Cheong HS, Shin HD, Jang HC, et al. Polymorphisms of KCNJ11 (Kir6.2 gene) are associated with Type 2 diabetes and hypertension in the Korean population. Diabet Med. 2007;24:178–86. doi: 10.1111/j.1464-5491.2006.02050.x. [DOI] [PubMed] [Google Scholar]
- 23.Liu NJ, Wu HH, Li YL, Yang Z, Tao XM, Du YP, et al. An analysis of the association between a polymorphism of KCNJ11 and diabetic retinopathy in a Chinese Han population. Eur J Med Res. 2015;20:3. doi: 10.1186/s40001-014-0075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu L, Seidel CP, Iwase T, Stevens RK, Gong YY, Wang X, et al. Suppression of GLUT1; a new strategy to prevent diabetic complications. J Cell Physiol. 2013;228:251–7. doi: 10.1002/jcp.24133. [DOI] [PubMed] [Google Scholar]
- 25.Sheu WHH, Kuo JZ, Lee IT, Hung YJ, Lee WJ, Tsai HY, et al. Genome-wide association study in a Chinese population with diabetic retinopathy. Hum Mol Genet. 2013;22:3165–73. doi: 10.1093/hmg/ddt161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suzuki M, Setsuie R, Wada K. Ubiquitin carboxyl-terminal hydrolase l3 promotes insulin signaling and adipogenesis. Endocrinology. 2009;150:5230–9. doi: 10.1210/en.2009-0332. [DOI] [PubMed] [Google Scholar]
- 27.Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Investig. 2006;116:1793–801. doi: 10.1172/JCI29069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rand LI, Krolewski AS, Aiello LM, Warram JH, Baker RS, Maki T. Multiple factors in the prediction of risk of proliferative diabetic retinopathy. New Engl J Med. 1985;313:1433–8. doi: 10.1056/NEJM198512053132302. [DOI] [PubMed] [Google Scholar]
- 29.Ziello JE, Jovin IS, Huang Y. Hypoxia-inducible factor (hif)-1 regulatory pathway and its potential for therapeutic intervention in malignancy and ischemia. Yale J Biol Med. 2007;80:51–60. [PMC free article] [PubMed] [Google Scholar]
- 30.Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. New Engl J Med. 1994;331:1480–7. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 31.Kumagai AK, Glasgow BJ, Pardridge WM. GLUT1 glucose transporter expression in the diabetic and nondiabetic human eye. Invest Ophthalmol & Vis Sci. 1994;35:2887–94. [PubMed] [Google Scholar]
- 32.Burdon Kathryn P., Fogarty Rhys D., Shen Weiyong, Abhary Sotoodeh, Kaidonis Georgia, Appukuttan Binoy, Hewitt Alex W., Sharma Shiwani, Daniell Mark, Essex Rohan W., Chang John H., Klebe Sonja, Lake Stewart R., Pal Bishwanath, Jenkins Alicia, Govindarjan Gowthaman, Sundaresan Periasamy, Lamoureux Ecosse L., Ramasamy Kim, Pefkianaki Maria, Hykin Philip G., Petrovsky Nikolai, Brown Matthew A., Gillies Mark C., Craig Jamie E. Genome-wide association study for sight-threatening diabetic retinopathy reveals association with genetic variation near the GRB2 gene. Diabetologia. 2015;58(10):2288–2297. doi: 10.1007/s00125-015-3697-2. [DOI] [PubMed] [Google Scholar]
- 33.Marin Garcia PJ, Marin-Castaño ME. Angiotensin II-related hypertension and eye diseases. World J Cardiol. 2014;6:968–84. doi: 10.4330/wjc.v6.i9.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Funatsu H, Yamashita H. Pathogenesis of diabetic retinopathy and the renin-angiotensin system. Ophthalmic Physiol Opt. 2003;23:495–501. doi: 10.1046/j.1475-1313.2003.00134.x. [DOI] [PubMed] [Google Scholar]
- 35.Toop MJ, Dallinger KJC, Jennings PE, Barnett AH. Angiotensin-Converting Enzyme (ACE): relationship to insulin-dependent diabetes and microangiopathy. Diabet Med. 1986;3:455–7. doi: 10.1111/j.1464-5491.1986.tb00790.x. [DOI] [PubMed] [Google Scholar]
- 36.Fu YP, Hallman DM, Gonzalez VH, Klein BEK, Klein R, Hayes MG, et al. Identification of diabetic retinopathy genes through a genome-wide association study among Mexican-Americans from Starr County, Texas. J Ophthalmol. 2010;2010:861291. doi: 10.1155/2010/861291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Freeman BD, Machado FS, Tanowitz HB, Desruisseaux MS. Endothelin-1 and its role in the pathogenesis of infectious diseases. Life Sci. 2014;118:110–9. doi: 10.1016/j.lfs.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rask-Madsen C, King GL. Mechanisms of Disease: endothelial dysfunction in insulin resistance and diabetes. Nat Clin Pract End Met. 2007;3:46–56. doi: 10.1038/ncpendmet0366. [DOI] [PubMed] [Google Scholar]
- 39.Kalani M. The importance of endothelin-1 for microvascular dysfunction in diabetes. Vasc Health Risk Manag. 2008;4:1061–8. doi: 10.2147/VHRM.S3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Montufar-Solis D, Garza T, Vigneswaran N, Klein JR. Soluble gp130 promotes intestinal epithelial hyperplasia during reovirus infection. Int J Exp Pathol. 2010;91:276–80. doi: 10.1111/j.1365-2613.2010.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller-Delaney SFC, Lieberam I, Murphy P, Mitchell KJ. Plxdc2 is a mitogen for neural progenitors. PLoS ONE. 2011;6:e14565. doi: 10.1371/journal.pone.0014565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yamaji Y, Yoshida S, Ishikawa K, Sengoku A, Sato K, Yoshida A, et al. TEM7 (PLXDC1) in neovascular endothelial cells of fibrovascular membranes from patients with proliferative diabetic retinopathy. Invest Ophthalmol & Vis Sci. 2008;49:3151–7. doi: 10.1167/iovs.07-1249. [DOI] [PubMed] [Google Scholar]
- 43.Ciccacci C, Di Fusco D, Cacciotti L, Morganti R, D’Amato C, Novelli G, et al. TCF7L2 gene polymorphisms and type 2 diabetes: association with diabetic retinopathy and cardiovascular autonomic neuropathy. Acta Diabetol. 2013;50:789–99. doi: 10.1007/s00592-012-0418-x. [DOI] [PubMed] [Google Scholar]
- 44.Katoh M, Katoh M. Identification and characterization of ARHGAP24 and ARHGAP25 genes in silico. Int J Mol Med. 2004;14:333–8. [PubMed] [Google Scholar]
- 45.JOUSSEN ANTONIA M., POULAKI VASSILIKI, LE MINH LY, KOIZUMI KAN, ESSER CHRISTINA, JANICKI HANNA, SCHRAERMEYER ULRICH, KOCIOK NORBERT, FAUSER SASCHA, KIRCHHOF BERND, KERN TIMOTHY S., ADAMIS ANTHONY P. A central role for inflammation in the pathogenesis of diabetic retinopathy. The FASEB Journal. 2004;18(12):1450–1452. doi: 10.1096/fj.03-1476fje. [DOI] [PubMed] [Google Scholar]
- 46.Kern TS. Contributions of inflammatory processes to the development of the early stages of diabetic retinopathy. Exp Diabetes Res. 2007;2007:95103. doi: 10.1155/2007/95103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sandirasegarane L, Kester M. Enhanced stimulation of Akt-3/protein kinase b-γ in human aortic smooth muscle cells. Biochem Biophys Res Commun. 2001;283:158–63. doi: 10.1006/bbrc.2001.4739. [DOI] [PubMed] [Google Scholar]
- 48.de Bie P, van de Sluis B, Burstein E, Duran Karen J, Berger R, Duckett Colin S, et al. Characterization of COMMD protein–protein interactions in NF-κB signalling. Biochem J. 2006;398(Pt 1):63–71. doi: 10.1042/BJ20051664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garcia Soriano F, Virag L, Jagtap P, Szabo E, Mabley JG, Liaudet L, et al. Diabetic endothelial dysfunction: the role of poly(ADP-ribose) polymerase activation. Nat Med. 2001;7:108–13. doi: 10.1038/83241. [DOI] [PubMed] [Google Scholar]
- 50.Joussen AM, Doehmen S, Le ML, Koizumi K, Radetzky S, Krohne TU, et al. TNF-α mediated apoptosis plays an important role in the development of early diabetic retinopathy and long-term histopathological alterations. Mol Vis. 2009;15:1418–28. [PMC free article] [PubMed] [Google Scholar]
- 51.LEASK A, ABRAHAM DJ. TGF-β signaling and the fibrotic response. FASEB J. 2004;18:816–27. doi: 10.1096/fj.03-1273rev. [DOI] [PubMed] [Google Scholar]
- 52.Gerhardinger C, Dagher Z, Sebastiani P, Park YS, Lorenzi M. The transforming growth factor-β pathway is a common target of drugs that prevent experimental diabetic retinopathy. Diabetes. 2009;58:1659–67. doi: 10.2337/db08-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Joussen AM, Murata T, Tsujikawa A, Kirchhof B, Bursell SE, Adamis AP. Leukocyte-mediated endothelial cell injury and death in the diabetic retina. Am J Pathol. 2001;158:147–52. doi: 10.1016/S0002-9440(10)63952-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kupper TS, Ferguson TA. A potential pathophysiologic role for alpha 2 beta 1 integrin in human eye diseases involving vitreoretinal traction. FASEB J. 1993;7:1401–6. doi: 10.1096/fasebj.7.14.8224612. [DOI] [PubMed] [Google Scholar]
- 55.Kadłubowska J, Malaguarnera L, Wąż P, Zorena K. Neurodegeneration and neuroinflammation in diabetic retinopathy: potential approaches to delay neuronal loss. Curr Neuropharmacol. 2016;14:831–9. doi: 10.2174/1570159X14666160614095559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bloodworth JM., Jr. Diabetic retinopathy. Diabetes. 1962;11:1–22. [PubMed] [Google Scholar]
- 57.Whitmire W, Al-Gayyar MMH, Abdelsaid M, Yousufzai BK, El-Remessy AB. Alteration of growth factors and neuronal death in diabetic retinopathy: what we have learned so far. Mol Vis. 2011;17:300–8. [PMC free article] [PubMed] [Google Scholar]
- 58.Abu El-Asrar AM, Mohammad G, De Hertogh G, Nawaz MI, Van Den Eynde K, Siddiquei MM, et al. Neurotrophins and neurotrophin receptors in proliferative diabetic retinopathy. PLoS ONE. 2013;8:e65472. doi: 10.1371/journal.pone.0065472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ban N, Yamada Y, Someya Y, Ihara Y, Adachi T, Kubota A, et al. Activating transcription factor-2 is a positive regulator in CaM kinase IV-induced human insulin gene expression. Diabetes. 2000;49:1142–8. doi: 10.2337/diabetes.49.7.1142. [DOI] [PubMed] [Google Scholar]
- 60.Xiang C, Baubet V, Pal S, Holderbaum L, Tatard V, Jiang P, et al. RP58/ZNF238 directly modulates proneurogenic gene levels and is required for neuronal differentiation and brain expansion. Cell Death Differ. 2011;19:692. doi: 10.1038/cdd.2011.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Grassi MA, Tikhomirov A, Ramalingam S, Below JE, Cox NJ, Nicolae DL. Genome-wide meta-analysis for severe diabetic retinopathy. Hum Mol Genet. 2011;20:2472–81. doi: 10.1093/hmg/ddr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Peng D, Wang J, Zhang R, Jiang F, Tang S, Chen M, et al. Common variants in or near ZNRF1, COLEC12, SCYL1BP1 and API5 are associated with diabetic retinopathy in Chinese patients with type 2 diabetes. Diabetologia. 2015;58:1231–8. doi: 10.1007/s00125-015-3569-9. [DOI] [PubMed] [Google Scholar]
- 63.McLeod DS, Lefer DJ, Merges C, Lutty GA. Enhanced expression of intracellular adhesion molecule-1 and P-selectin in the diabetic human retina and choroid. Am J Pathol. 1995;147:642–53. [PMC free article] [PubMed] [Google Scholar]
- 64.Miyamoto K, Khosrof S, Bursell SE, Rohan R, Murata T, Clermont AC, et al. Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proc Natl Acad Sci. 1999;96:10836–41. doi: 10.1073/pnas.96.19.10836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.van den Oever IAM, Raterman HG, Nurmohamed MT, Simsek S. Endothelial dysfunction, inflammation, and apoptosis in diabetes mellitus. Mediat Inflamm. 2010;2010:15. doi: 10.1155/2010/792393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roux E, Cherbit G, Regnault F. Collagen-induced platelet aggregation and collagen glycosyl-transferase activity in diabetic patients. Thromb Res. 1977;11:847–58. doi: 10.1016/0049-3848(77)90113-X. [DOI] [PubMed] [Google Scholar]
- 67.Huang YC, Lin JM, Lin HJ, Chen CC, Chen SY, Tsai CH, et al. Genome-wide association study of diabetic retinopathy in a Taiwanese population. Ophthalmology. 2011;118:642–8. doi: 10.1016/j.ophtha.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 68.Peng D, Wang J, Zhang R, Tang S, Jiang F, Chen M, et al. C-reactive protein genetic variant is associated with diabetic retinopathy in Chinese patients with type 2 diabetes. BMC Endocr Disord. 2015;15:8. doi: 10.1186/s12902-015-0006-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cheung CY, Hui EY, Lee CH, Kwok KH, Gangwani RA, Li KK, et al. Impact of genetic loci identified in genome-wide association studies on diabetic retinopathy in chinese patients with type 2 diabetes. Invest Ophthalmol Vis Sci. 2016;57:5518–24. doi: 10.1167/iovs.16-20094. [DOI] [PubMed] [Google Scholar]
- 70.Porta M, Toppila I, Sandholm N, Hosseini SM, Forsblom C, Hietala K, et al. Variation in SLC19A3 and protection from microvascular damage in type 1 diabetes. Diabetes. 2016;65:1022–30. doi: 10.2337/db15-1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McAuley AK, Wang JJ, Dirani M, Connell PP, Lamoureux E, Hewitt AW. Replication of genetic loci implicated in diabetic retinopathygenetic loci implicated in diabetic retinopathy. Invest Ophthalmol Vis Sci. 2014;55:1666–71. doi: 10.1167/iovs.13-13559. [DOI] [PubMed] [Google Scholar]
- 72.Awata T, Yamashita H, Kurihara S, Morita-Ohkubo T, Miyashita Y, Katayama S, et al. A genome-wide association study for diabetic retinopathy in a japanese population: potential association with a long intergenic non-coding RNA. PLoS ONE. 2014;9:e111715. doi: 10.1371/journal.pone.0111715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hu C, Zhang R, Yu W, Wang J, Wang C, Pang C, et al. CPVL/CHN2 genetic variant is associated with diabetic retinopathy in Chinese type 2 diabetic patients. Diabetes. 2011;60:3085–9. doi: 10.2337/db11-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Burdon KP, Fogarty RD, Shen W, Abhary S, Kaidonis G, Appukuttan B, et al. Genome-wide association study for sight-threatening diabetic retinopathy reveals association with genetic variation near the GRB2 gene. Diabetologia. 2015;58:2288–97. doi: 10.1007/s00125-015-3697-2. [DOI] [PubMed] [Google Scholar]


