Twenty-five years ago, the National Institutes of Health (NIH) Revitalization Act of 1993 mandated the inclusion of women in clinical research (1), following decades of misconceptions surrounding women’s health and reversing previous guidelines preventing women of childbearing age from participating in early-stage research (2). Many of us held tight to the belief that this requirement would usher in a new era of discovery where consideration of the female sex would become routine experimental practice both in the clinical and basic sciences. Yet today, 25 years later, women remain underrepresented as research subjects in the design and development of novel therapeutics and technologies (3–6). Moreover, when women are included in NIH-funded clinical research, there is often no attempt to desegregate or analyze data by sex or gender, hindering reproducibility and limiting the potential for sex-specific discoveries and our knowledge about the influences of sex or gender on health and disease (7).
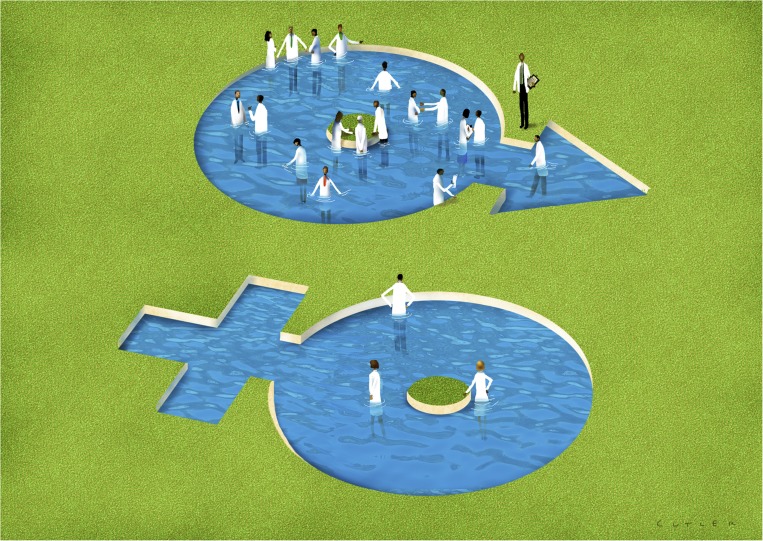
Our survey results suggest many study section members do not think sex is an important part of experimental design, sentiments that likely extend to the broader research community. Image credit: David Cutler (artist).
Survey data we’ve collected imply a further problem. Our results suggest that nearly one-third of NIH study section members do not think it is important to consider biological sex as part of experimental design. This indicates that, although in the minority, the “gate-keepers” of federal funding do not recognize the importance of sex-based research, and these sentiments likely extend to the broader research community.
Sex Versus Gender
To fully understand the implications of sex and gender, it’s important to outline their difference. Sex is a biological attribute of cells or organisms, defined by genetics, physiology, anatomy, and the hormonal milieu. In the context of clinical studies, male physiology differs from female physiology not only in the reproductive tract but in the biology of every organ system. Clinical studies that include both men and women but do not analyze data accordingly ignore the existence of potential sex differences (8). Gender, however, is a social construct applicable to humans, which defines the appearance, actions, thoughts, and behaviors associated with the male or female sex and varies depending on the cultural context. Only human clinical research studies can analyze and report data by both biological sex and self-reported gender. This is important because gender plays a role in the psychosocial and epidemiological determinants of health (8, 9).
Equally relevant to clinical research and human health are the developments and discoveries that take place in basic science laboratories using cells and model organisms. Unfortunately, the issue of female animals and cells was not considered in 1993, and today the paucity of the female sex in clinical research is paralleled in the basic sciences where the sex of animals and cells have largely been excluded from study or unanalyzed when included (3, 10–12).
To address this gap, the NIH implemented a policy in 2016 that asks investigators to “consider” sex as a biological variable (SABV) within fundamental research in experimental design, analyses, and reporting (13). Unlike the NIH Revitalization Act, the 2016 SABV policy was not a formal mandate but rather a strongly worded suggestion where compliance is tied to grant scoring and ultimately funding outcomes. As proponents of sex- and gender-inclusive research, we were reluctant to wait for another 25-years to determine the impact of this new policy statement on basic science practice and outcomes, and so we set out to examine the implementation and acceptance of the SABV policy by the biomedical research community in the 2 years since its enactment. Our data suggest that although attitudes toward the SABV policy are generally favorable, biological sex may play a role in how the policy is perceived (14). We also identified variability in how the policy is evaluated and scored, leaving behind concern for its ability to advance rigor and reproducibility in the biomedical sciences (14).
A Policy Evaluation
To evaluate the immediate reception of the SABV policy, we chose to survey NIH study section members who serve not only as representative members of the biomedical research community but as policy adjudicators with firsthand knowledge of compliance (14). Our study, which spanned two cohorts of study section members in 2016 and 2017, revealed that study section members attitudes toward the policy became more favorable over time and the number of grant applications that appropriately consider SABV have increased as well. Yet, when provided with the opportunity to leave an open-ended response, study section members left more colorful commentary, deriding the policy as “nonsense,” and a “waste of time.” At best, we can presume that these negative sentiments toward the policy derive from a lack of awareness or knowledge about the influences of biological sex. At worst, they may be tied to bias and the belief that females are not relevant experimental subjects.
If we cannot change the minds and experimental methods of seasoned investigators, it may fall upon the next generation of scientists to conduct their research in an unbiased and scientifically sound manner.
Perhaps even more worrisome was the notion that, although some study section members took the policy seriously, others indicated that the consideration of SABV was a “non-scoring factor,” essentially neutering the true intent of the policy. These negative statements were balanced by those that deemed the policy “a simple and needed criterion” that will “greatly improve scientific rigor and reproducibility, [and] hence should be promoted.” The contrast in these comments represents a divide in the way we as researchers see our role in the inclusion of fundamental variables such as sex. We did not ask study section members if they felt it was important to consider other relevant biological variables, such as age or weight. But the data indicate that there is something quite bothersome to the research community about the use of “sex” as a normal, reportable element in scientific reports.
The NIH SABV policy sets the minimum of “consideration” of sex as a variable in research studies. It does not make an edict that all studies must include equal numbers of male or female subjects or evaluate data with sex as an independent variable; it simply indicates that sex should be considered when developing biological studies. We hypothesized that women may be more supportive of the NIH SABV policy based on personal knowledge or awareness surrounding the impact of sex on health and disease. And we found that to be the case in 2017 (14).
Female study section members were more likely to think it was important to consider SABV and that it would improve rigor and reproducibility compared with their male peers. Similarly, Nielsen et al. (15) found that female researchers were more likely to analyze data by sex and gender. Such results suggest that women ascribe value to sex- and gender-inclusive research, be it on a conscious or unconscious level. The irony, of course, is that women are underrepresented throughout the scientific and engineering workforce (16, 17). Hence, although it may seem like apples and oranges, the number of female researchers and the application of SABV in scientific studies are likely intertwined, and it may take time to achieve parity on both fronts. As more women enter and advance in the biomedical research workforce, we anticipate a concurrent increase in research that examines or evaluates the influences of sex and gender.
How, as a research community, can we move forward to ensure that sex and gender inclusion are taken seriously at the fundamental and clinical ends of the knowledge/drug development pipeline? There have been editorials and opinion pieces calling for the equitable use and evaluation of both sexes in biological research (18–22), journals requiring sex- and gender-based reporting (23, 24), and review articles providing guidance on how to include and consider sex and gender appropriately (25, 26). Yet, we are still falling short and failing to include females at all stages of the biomedical research pipeline (3–6) and, therefore, failing all of us in the advances that science and medicine have on our lives (20).
If we cannot change the minds and experimental methods of seasoned investigators, it may fall upon the next generation of scientists to conduct their research in an unbiased and scientifically sound manner. It would be beneficial for trainees to gain exposure to sex- and gender-inclusive research techniques, either through formalized coursework or incorporated into qualifying examinations or thesis evaluations. This may be possible through existing Responsible Conduct of Research modules that are already required in graduate education. Moreover, institutions can support sex- and gender-inclusive research practices by including relevant questions or requirements within Institutional Review Board or Animal Care and Use Committee applications. This would not be intrusive and may, in fact, provide additional metadata as to how sex and gender are incorporated into experimental design.
Notably, the SABV policy was not intended simply to bring parity in basic science; it was to ensure that fundamental discoveries had the advantage of an entirely new way of looking at biology that can be informative. It is an on-road to exciting, novel discoveries. The fact that this new way of working also promises to make our drug development pipeline better structured toward successful outcomes for men and women is a secondary objective but one that we can all cheer.
Footnotes
The authors declare no conflict of interest.
Any opinions, findings, conclusions, or recommendations expressed in this work are those of the authors and have not been endorsed by the National Academy of Sciences.
References
- 1.National Institutes of Health NIH guidelines on the inclusion of women and minorities as subjects in clinical research. Fed Regist. 1994;59:14508–14513. [Google Scholar]
- 2.Food and Drug Administration . General Considerations for the Clinical Evaluation of Drugs. US Department of Health, Education, and Welfare; Rockville, MD: 1977. [Google Scholar]
- 3.Beery AK, Zucker I. Sex bias in neuroscience and biomedical research. Neurosci Biobehav Rev. 2011;35:565–572. doi: 10.1016/j.neubiorev.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poon R, et al. Participation of women and sex analyses in late-phase clinical trials of new molecular entity drugs and biologics approved by the FDA in 2007-2009. J Womens Health (Larchmt) 2013;22:604–616. doi: 10.1089/jwh.2012.3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinnow E, Herz N, Loyo-Berrios N, Tarver M. Enrollment and monitoring of women in post-approval studies for medical devices mandated by the Food and Drug Administration. J Womens Health (Larchmt) 2014;23:218–223. doi: 10.1089/jwh.2013.4343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoon DY, et al. Sex bias exists in basic science and translational surgical research. Surgery. 2014;156:508–516. doi: 10.1016/j.surg.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Geller SE, et al. The more things change, the more they stay the same: A study to evaluate compliance with inclusion and assessment of women and minorities in randomized controlled trials. Acad Med. 2018;93:630–635. doi: 10.1097/ACM.0000000000002027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clayton JA, Tannenbaum C. Reporting sex, gender, or both in clinical research? JAMA. 2016;316:1863–1864. doi: 10.1001/jama.2016.16405. [DOI] [PubMed] [Google Scholar]
- 9.Vlassoff C. Gender differences in determinants and consequences of health and illness. J Health Popul Nutr. 2007;25:47–61. [PMC free article] [PubMed] [Google Scholar]
- 10.Mansukhani NA, et al. Determining if sex bias exists in human surgical clinical research. JAMA Surg. 2016;151:1022–1030. doi: 10.1001/jamasurg.2016.2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Potluri T, Engle K, Fink AL, Vom Steeg LG, Klein SL. Sex reporting in preclinical microbiological and immunological research. MBio. 2017;8:e01868-17. doi: 10.1128/mBio.01868-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kong BY, Haugh IM, Schlosser BJ, Getsios S, Paller AS. Mind the gap: Sex bias in basic skin research. J Invest Dermatol. 2016;136:12–14. doi: 10.1038/JID.2015.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Institutes of Health 2015 Consideration of sex as a biological variable in NIH-funded research. Available at https://grants.nih.gov/grants/guide/notice-files/not-od-15-102.html. Accessed March 1, 2019.
- 14.Woitowich NC, Woodruff TK. Implementation of the NIH sex-inclusion policy: Attitudes and opinions of study section members. J Womens Health (Larchmt) 2019;28:9–16. doi: 10.1089/jwh.2018.7396. [DOI] [PubMed] [Google Scholar]
- 15.Nielsen MW, Andersen JP, Schiebinger L, Schneider JW. One and a half million medical papers reveal a link between author gender and attention to gender and sex analysis. Nat Hum Behav. 2017;1:791–796. doi: 10.1038/s41562-017-0235-x. [DOI] [PubMed] [Google Scholar]
- 16.National Science Foundation 2015 Women, minorities, and persons with disabilities in science and engineering. Available at https://www.nsf.gov/statistics/2017/nsf17310/data.cfm.
- 17.Zeng XH, et al. Differences in collaboration patterns across discipline, career stage, and gender. PLoS Biol. 2016;14:e1002573. doi: 10.1371/journal.pbio.1002573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim AM, Tingen CM, Woodruff TK. Sex bias in trials and treatment must end. Nature. 2010;465:688–689. doi: 10.1038/465688a. [DOI] [PubMed] [Google Scholar]
- 19.Woodruff TK. Sex, equity, and science. Proc Natl Acad Sci USA. 2014;111:5063–5064. doi: 10.1073/pnas.1404203111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klein SL, et al. Opinion: Sex inclusion in basic research drives discovery. Proc Natl Acad Sci USA. 2015;112:5257–5258. doi: 10.1073/pnas.1502843112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mazure CM, Jones DP. Twenty years and still counting: including women as participants and studying sex and gender in biomedical research. BMC Womens Health. 2015;15:94. doi: 10.1186/s12905-015-0251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shansky RM, Woolley CS. Considering sex as a biological variable will be valuable for neuroscience research. J Neurosci. 2016;36:11817–11822. doi: 10.1523/JNEUROSCI.1390-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hankivsky O, Springer KW, Hunting G. Beyond sex and gender difference in funding and reporting of health research. Res Integr Peer Rev. 2018;3:6. doi: 10.1186/s41073-018-0050-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prager EM. Addressing sex as a biological variable. J Neurosci Res. 2017;95:11. doi: 10.1002/jnr.23979. [DOI] [PubMed] [Google Scholar]
- 25.Clayton JA. Studying both sexes: A guiding principle for biomedicine. FASEB J. 2016;30:519–524. doi: 10.1096/fj.15-279554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tannenbaum C, Schwarz JM, Clayton JA, de Vries GJ, Sullivan C. Evaluating sex as a biological variable in preclinical research: The devil in the details. Biol Sex Differ. 2016;7:13. doi: 10.1186/s13293-016-0066-x. [DOI] [PMC free article] [PubMed] [Google Scholar]