Abstract
Purpose:
This longitudinal study sought to examine the reciprocal relationship between spirituality and physical health status among breast cancer survivors.
Methods:
Breast cancer survivors (N=634) completed baseline assessments (T1) within 8 months of breast cancer diagnosis and 12 (T2) and 18 months (T3) after their baseline assessment. Spirituality was assessed by the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) scale which consists of 3 subscales: meaning, peace, and faith. Physical health status was measured with the SF-36 Physical Component Summary (PCS). A cross-lagged structural equation model (SEM) was used to analyze the three-wave data to examine the reciprocal relationships between the observed variable, PCS, and the 3 subscales of the FACIT-Sp, treated as latent variables.
Results:
The cross-lagged SEM yielded an adequate fit to the data: RMSEA = .036, CFI = 0.97, TLI = 0.96. After controlling for relevant sociodemographic and cancer-related variables, only higher PCS at T2 predicted greater meaning at T3. PCS at T1 did not predict meaning at T2 and the reciprocal relationship of meaning predicting PCS was not significant. Neither peace nor faith was reciprocally related to PCS.
Conclusions:
Results provide evidence of a unidirectional relationship between self-reported physical health status and subsequent meaning among breast cancer survivors during the period of early to later survivorship. Additional studies are needed that examine the longitudinal and directional relationships between spirituality and physical health among diverse samples of cancer survivors.
Keywords: Spirituality, Physical Health, Breast Cancer Survivors, Longitudinal
A growing body of research supports a positive relationship between religion and/or spirituality and physical health in the general population [1,2], as well as among patients facing a serious illness such as cancer [3,4]. Religion and spirituality are both considered multidimensional with the degree of distinction and overlap continually debated [2,3,5,6]. A full discussion of the distinctions goes beyond the scope of this manuscript, but there are several outstanding articles on this topic for further reference [2,5]. For health researchers, religion often refers to the involvement in institutional practices of a particular group while spirituality has been defined to include dimensions regarding a personal search for meaning and purpose, connection with the transcendent or sacred, and the experiences associated with that connection [7,8]. Increasingly, individuals in the United States describe themselves as spiritual but not religious, with the percentage of Americans describing themselves as such increasing from 19% in 2012 to 27% in 2017 according to a recent Pew Research Center survey [9].
For the purpose of this study, we focus on the relationship between spirituality, as measured by the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) scale, and self-reported physical health. The FACIT-Sp was specifically developed to capture spirituality independent of a specific set of religious beliefs and behaviors [8]. As such, this measure was developed to be non-faith specific and to be used with chronic illness populations. The original validation study of the FACIT-Sp found two subscales reflecting meaning/peace and faith dimensions of spirituality [8].
Cross-sectional studies in cancer survivors have found a positive association between overall spirituality using the FACIT-Sp and better self-reported health [10–12]. A meta-analysis of studies of religion/spirituality more broadly also supports these findings and this relationship [14] When examining the meaning/peace subscale, many studies find a positive association with physical health [11,13,14]. On the other hand, the faith subscale generally has not been found to be associated with physical health [11,14].
More recent psychometric studies have suggested that the meaning/peace subscale of the FACIT-Sp is best captured by two separate subscales, with meaning representing a cognitive aspect of spirituality and peace representing an affective component [15–18]. These studies have generally found that the 3-factor solution is more informative and differentially related to outcomes than the 2-factor solution. For example, in one study, peace was most prominently associated with the functional and emotional well-being subscales of the Functional Assessment of Cancer Therapy-General (FACT-G) quality of life measure, while meaning was highly associated with functional and social well-being [18]. In studies that have examined meaning and peace separately in relation to physical health, either both subscales have been found to be related to physical health [19] or only meaning is found to be related [15,16].
The current literature on spirituality and physical health has a number of limitations. In particular, there is a dearth of longitudinal studies and studies examining the directionality of relationships. Less than 10% of the studies cited in the meta-analysis were longitudinal [4]. Cross-sectional studies generally assume that greater spirituality leads to better physical health, yet the direction of this relationship may be more complex. Physical health may impact spirituality, just as spirituality may impact physical health [4]. A better understanding of the direction of this relationship may provide insight for future research and interventions.
The present study addresses these gaps in the current literature by using longitudinal data to examine the reciprocity of this relationship. Specifically, in a sample of breast cancer survivors, we use a 3-wave cross-lagged structural equation model (SEM) to examine the reciprocal relationships between subscales of spirituality (meaning, peace, faith) measured by the FACIT-Sp and self-reported physical health status, as measured by the SF-36 Physical Component Summary (PCS). Structural equation modeling allows for variables to be simultaneously included in a model to test the direction of relationships. Based on previous research, we hypothesized that the relationship would be bi-directional for meaning and peace (i.e., that is meaning and peace would predict subsequent physical health status and vice versa) and there would be no relationship between faith and physical health status.
Methods
Study Population and Procedure
This is a secondary analysis of a longitudinal study that examined age-related differences in adjustment to breast cancer. The study design has been previously described [20]. Participants were recruited within 8 months of their breast cancer diagnosis from Memorial Sloan Kettering Cancer Center and the University of Texas-Southwestern Center for Breast Care between 2002–2006 and followed until 2008. Eligibility criteria included a first-time diagnosis of stage I-III breast cancer, age > 18 years old, and ability to read and write English. Participants completed baseline questionnaires at time of recruitment and follow-up questionnaires 6, 12, and 18 months after completion of their baseline questionnaire. After completion of primary treatment, chart reviews were conducted to obtain cancer treatment information. All sites had approval from their Institutional Review Boards. Informed consent was provided by all study participants.
The current analyses used data from the baseline (T1; 0–8 months post-diagnosis), 12 month (T2; 12–20 months post-diagnosis), and 18 month (T3; 18–26 months post-diagnosis) assessments. The 6-month assessment was not included because many women were still in active treatment at this time and we wanted to avoid overlap with active treatment at T1.
Measures
Spirituality was assessed using the 12-item Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) scale [8]. Participants rated the extent to which they experienced aspects of spiritual well-being in the past 7 days (0 = not at all; 4 = very much). This measure yields three subscales: meaning (e.g., “I felt a sense of purpose in my life” and “I had a reason for living”), peace (e.g., “I felt a sense of harmony with myself” and “I felt peaceful”), and faith (e.g., “I found strength in my faith or spiritual beliefs” and “My illness strengthened my faith or spiritual beliefs”) [16]. Each subscale contains four items that are summed to provide a total score that ranges from 0 to 16, with higher scores indicating higher spirituality.
Physical Health Status was measured by the Physical Component Summary (PCS) from the Medical Outcomes Study Short Form- 36 item version (SF-36) [21]. The SF-36 is a generic measure of health-related quality of life yielding eight subscales and two summary scores: the Physical Component Summary (PCS) and Mental Component Summary (MCS). Higher scores indicate better physical health status.
Sociodemographic and Cancer-Related Characteristics as Covariates: age at baseline (continuous), race (white/not white), married/partnered (yes/no), number of self-reported comorbidities at baseline (0, 1–2, 3+), stage at diagnosis (I, II or III), mastectomy (vs. lumpectomy only), chemotherapy (yes/no), and radiation (yes/no).
Statistical Analyses
Descriptive statistics were calculated to summarize the demographic and cancer-related characteristics of the sample. Bivariate correlations were conducted between the three subscales of the FACIT-Sp and the PCS.
Measurement Model.
Confirmatory factor analysis (CFA) was conducted to test the measurement model and examine the relationship between indicators and latent constructs and to test measurement invariance [22]. We used three latent constructs (meaning, peace, and faith); the four items of the FACIT-Sp that make up each scale at each assessment were used as indicators. For easier interpretation, negatively worded items were reverse-scored. First, a full model was specified in which: a) the residuals were correlated between indicators that were repeated at each assessment, b) all factor loadings were free to vary, and c) all latent variables were allowed to be correlated. Subsequently, all parameters of the same indicator were constrained to be equal across time to test for measurement invariance [22].
Cross-Lagged Model.
A three-wave cross-lagged SEM model was tested to examine the reciprocal relationships between the PCS and each subscale of the FACIT-Sp. In this model, there were three latent variables (meaning, peace, faith) and one manifest variable (PCS). The PCS was calculated using weighted items and, therefore, maintained as a manifest variable. For this model, each variable at T2 is predicted by itself at T1 (autoregressive path) and each T3 variable is predicted by itself at T2. The autoregressive path represents the stability of the variable over time, or the stability of individual differences from one timepoint to the next [23]. Additionally, each latent variable at time t predicts PCS at time t+1, and PCS at time t predicts each latent variable at time t+1 (crossed-lagged path). This cross-lagged path represents the effect of one variable on the other, controlling for the prior level of the variable being predicted The paths in the cross-lagged model were not constrained to be equal across assessments because the actual time intervals varied between assessments. Age at baseline, cancer stage, time since diagnosis at baseline, radiation therapy ever (yes/no), chemotherapy ever (yes/no), type of surgery (lumpectomy only/mastectomy), race (white/non-white), and number of comorbidities (0, 1–2, or 3+) were included as covariates in the model.
SPSS 24 was used for descriptive statistics and bivariate correlations. CFA and SEM analyses were conducted using Mplus 7.4 with full information maximum likelihood used as the method for handling missing data [24]. The model data fit were evaluated using multiple fit indices including: chi-square goodness of fit statistic, the comparative fit index (CFI; greater than .95 considered acceptable), the Tucker-Lewis Index (TLI; greater than .95 considered acceptable), and the root mean square of approximation (RMSEA; less than .06 considered acceptable) [25]. Chi-square tests were computed when comparing models, but the chi-square goodness of fit statistics was not used as a fit criterion, as with large sample sizes it rejects the model even with good model fit [26].
Results
Sample Characteristics
Of a total of 653 study participants, 634 breast cancer survivors met the criteria for these analyses. Analyses excluded women who were in active treatment at T2 or T3 (n=13), women who did not receive any type of breast surgery (n=1), and women with missing data on covariates (n = 5). Characteristics of the analytic sample are shown in Table 1. Women were predominately Caucasian (90%), married/partnered (72%), and had at least a college education (63%). The mean age was 55.5 years (SD = 12.5; range = 25–97). The majority were diagnosed with stage I breast cancer (52%), had a lumpectomy only (64%), received adjuvant radiation therapy (72%), and received chemotherapy (66%). The mean time since breast cancer diagnosis at T1 was 4.5 months.
Table 1.
Participant Characteristics (N=634)
| Characteristic | Number (%) | M (SD) |
|---|---|---|
| Age (years) | 55.5 (12.6) | |
| Race (White) | 568 (90) | |
| College graduate (yes) | 396 (63) | |
| Household Income | ||
| <$20,000 | 44 (7) | |
| $20,000–$49,999 | 109 (17) | |
| $50,000–$100,000 | 193 (31) | |
| >$100,000 | 268 (42) | |
| Married/partner (yes) | 454 (72) | |
| Time since diagnosis (months, | 4.5 (1.3) | |
| Cancer Stage | ||
| I | 332 (52) | |
| II | 252 (40) | |
| III | 50 (8) | |
| Chemotherapy (yes) | 420 (66) | |
| Radiation Therapy (yes) | 458 (72) | |
| Mastectomy (vs. lumpectomy) | 226 (36) | |
| Number of Comorbid Conditions | ||
| 0 | 236 (37) | |
| 1–2 | 289 (46) | |
| 3+ | 109 (17) |
PCS and Spirituality over Time
Table 2 provides the means and standard deviations of the PCS and FACIT-Sp subscale scores over time. The scores of the FACIT-Sp subscales at all assessments fall within one standard deviation of the reference sample of breast cancer survivors 2–10 years post-diagnosis [27] Bivariate correlations between PCS and spirituality subscales showed that both meaning and peace were significantly correlated with PCS cross-sectionally and longitudinally (Table 3). The correlations were somewhat higher for meaning (r = .15–.26) than peace (r = .12–.20). Correlations between faith and PCS were very low (and non-significant) across all assessments.
Table 2.
Mean SF-36 PCS and FACIT-Sp subscale scores at each timepoint
| T1 | T2 | T3 | |
|---|---|---|---|
| SF-36 PCS | 45.04 (9.74) n = 634 |
49.30 (9.24) n = 571 |
49.85 (9.60) n = 545 |
| Meaning | 13.25 (2.91) n = 626 |
13.18 (2.95) n=574 |
13.20 (2.87) n=548 |
| Peace | 10.55 (3.84) n = 626 |
10.76 (3.81) n = 574 |
10.83 (3.77) n = 548 |
| Faith | 9.79 (4.88) n = 618 |
9.29 (5.01) n = 568 |
9.40 (4.95) n = 544 |
Table 3.
Bivariate Correlations Between the SF-36 PCS and FACIT-Sp Subscales
| PCS T1 | PCS T2 | PCS T3 | |
|---|---|---|---|
| Meaning T1 | .26** | .15** | .15** |
| Meaning T2 | .22** | .23** | .21** |
| Meaning T3 | .18** | .22** | .19** |
| Peace T1 | .20** | .12** | .12** |
| Peace T2 | .13** | .14** | .15** |
| Peace T3 | .16** | .13** | .13** |
| Faith T1 | −.03 | −.05 | −.04 |
| Faith T2 | −.05 | −.06 | −.07 |
| Faith T3 | −.02 | −.05 | −.05 |
p <.01
Measurement Model
Results for the CFA are provided in Table 4. The initial measurement model fit the data well (χ2 (522) = 1256.66; p < 0.001; CFI = 0.96, TLI = 0.95; RMSEA = .047; Model 1). However, because analyses suggested that changes to the model would improve model fit, we ran subsequent models. First, the error covariances for two similarly worded items (“I found comfort in my faith or spiritual beliefs” and “I found strength in my faith or spiritual beliefs.”) were allowed to correlate with each other within all 3 assessments (Model 2). Second, the error covariances for the two negatively worded items (“I had trouble feeling peace of mind” and “My life lacked meaning and purpose”) were allowed to correlate within all 3 assessments (Model 3). Finally, we also allowed the error covariances for two items (“I felt peaceful” and “I had trouble feeling peace of mind”) to correlate, as they have similar, though reversed, wording (Model 4). In a CFA on the FACIT-Sp, Canada and colleagues also found that making the adjustments in Models 3 and 4 led to improved model fit [16]. After these adjustments, the factor loadings were constrained as equal across time (Model 5). The parameter-constrained model also fit the data well (χ2 (531) = 978.93; p < 0.001; CFI = 0.98, TLI = 0.97; RMSEA = .036). The changes in fit indices from constraining the factor loadings were negligible, and the change in χ2 was also not statistically significant (Δ χ2 = 19.39, Δdf = 18, p = 0.37), supporting invariance of measurement over time.
Table 4.
Results of confirmatory factor analyses of the FACIT-Sp
| Model | χ2 | df | Δχ2 | Δdf | p | TLI | CFI | RMSEA | |
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Longitudinal CFA configural model |
1256.66 | 522 | .95 | .96 | .047 | |||
| Model 2 | Adjusted model 1 with correlated error covariances for similarly worded items |
1140.00 | 519 | 116.66 | 3 | <.001 | .96 | .97 | .043 |
| Model 3 | Adjusted model 2 with correlated error covariances for reverse-scored items |
1038.61 | 516 | 101.39 | 3 | <.001 | .97 | .97 | .040 |
| Model 4 | Adjusted model 3 with correlated error covariances for similar, but reversed, worded items |
959.54 | 513 | 79.07 | 3 | <.001 | .97 | .98 | .037 |
| Model 5 | Adjusted model 4 with factor loadings held constant across time |
978.93 | 531 | 19.39 | 18 | 0.37 | .97 | .98 | .036 |
Cross-Lagged Model
The cross-lagged model examined the reciprocal relationship between the three latent variables of spirituality (meaning, peace, and faith) and PCS. The autoregressive effects of each variable over time were also examined (Figure 1). The cross-lagged model fit the data well: (χ2 (856) = 1541.31; p < 0.001; CFI = 0.97, TLI = 0.96; RMSEA = .036).
Fig 1.
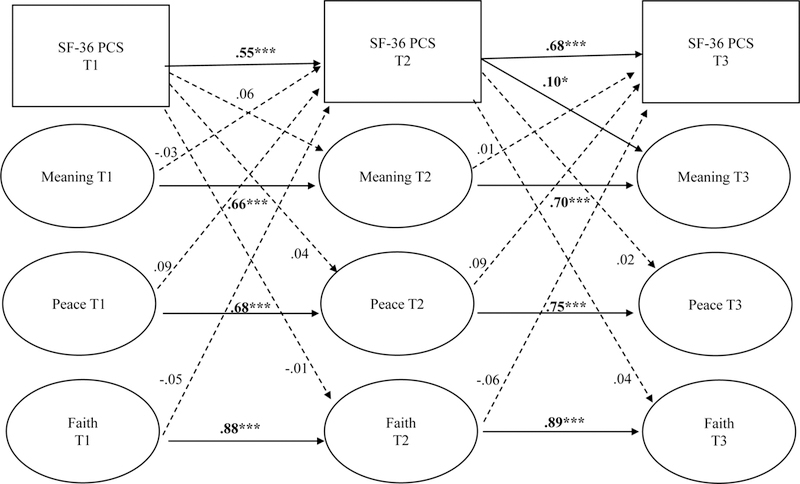
Cross-lagged structural equation model of the FACIT-Sp subscales (meaning, peace, and faith) and SF-36 PCS. Path coefficients are standardized. All models controlled for age, race, chemotherapy, time since diagnosis, radiation, surgery type, stage, and comorbidity. Dotted lines indicate non-significant paths, while solid lines represent significant paths. For clarity, indicators of the latent variables, error covariances, covariates, and cross-sectional associations are not depicted on the diagram. *p <.05; ***p < 0.001.
The autoregressive paths from prior to subsequent PCS were significant for all assessments (standardized β = .55 for the path from T1 to T2 and .68 for the path from T2 to T3), indicating that individuals’ relative standings on the variable changed little over time. The stability effect over both timepoints for meaning (standardized β = .66 and .70), peace (standardized β = .68 and .75), and faith (standardized β= .88 and .89) were also significant. For all variables, the stability effect was larger between T2 to T3, which spanned only 6 months, than from T1 to T2, which spanned 12 months.
The path from T2 PCS to T3 meaning was the only statistically significant cross-lagged effect (standardized β = .10, p < .05), suggesting that higher PCS at T2 predicted greater meaning at T3. This cross-lagged path was not significant from T1 to T2. The reverse (i.e., meaning predicting subsequent PCS) was not significant from either T1 to T2 or T2 to T3. Neither peace nor faith was reciprocally associated with PCS at any timepoint.
Discussion
To our knowledge, this is the first study to examine the cross-lagged association between self-reported physical health status and spirituality in cancer survivors. Study results found that better physical health status post-treatment was associated with subsequently higher meaning in the cross-lagged model. This finding is consistent with a prior study that found that breast cancer survivors at 18 months post-diagnosis who had poorer physical functioning experienced less meaning in life 6 months later [28], but extends these findings by examining the reciprocal relationship. Contrary to our hypothesis, greater meaning did not predict better subsequent physical health status. This is somewhat surprising given that the literature often assumes that greater spirituality predicts better health. Although meaning at one assessment was related to subsequent PCS in bivariate correlations, this relationship became non-significant in the cross-lagged model. A cross-lagged model in which one variable predicts another at a later time point controlling for the prior level of the outcome variable offers a more stringent analysis than bivariate correlations.
It is worth pointing out that PCS predicted meaning only from T2 to T3, and not from T1 to T2, a time period closer to diagnosis and active treatment. There are at least two possible explanations for this finding. One explanation for these findings may have to do with the shorter time period between T2 and T3 (6 months) than T1 and T2 (12 months). It is possible that a shorter time period allows for greater predictive ability between variables. Another possible explanation is that the relationship between physical health status and meaning may vary by time since diagnosis. Specifically, closer to diagnosis and active treatment, a person’s ability to find meaning may be less strongly related to physical health than to other factors such as personal resources (e.g., social support, resilience), whereas further from diagnosis physical health may become more relevant for experiencing meaning in life. Future studies might examine the role of personal resources in finding meaning when diagnosed with cancer.
Despite the longitudinal correlations between peace and PCS, contrary to our hypothesis, peace was not related longitudinally to PCS in the cross-lagged model. Peace is often considered an affective component of spirituality and is highly associated with emotional well-being [12], so much so that many critics consider them to be tautological [29]. Although peace was associated with PCS in bivariate correlations, peace may not be strongly associated with one’s physical health status longitudinally when the other subscales of spirituality are considered in the model. This is consistent with other studies that found when meaning, peace, and faith are in the same model together, the peace subscale was not related to physical health [16]. Our findings provide further evidence of the value of separating the meaning and peace subscales when using the FACIT-Sp, as they were each differentially related to PCS.
The finding that faith, often considered to be the component of spirituality most associated with religiousness [8,14], was not related to PCS in either bivariate correlations or the cross-lagged model supports our hypothesis and is consistent with cross-sectional studies [11,14,16]. Although faith may be an important part of a person’s values and attitudes towards life and can help provide a framework through which people create meaning out of their stressful life experiences [30], this aspect of spirituality was, , unrelated to how participants in our sample reported their physical health.
Strengths of the study include the longitudinal design with repeated measurements of spirituality and self-reported physical health, thus providing the opportunity to examine reciprocal relationships using a comprehensive statistical method. This study also used a large sample of participants who completed the most common measure of spirituality used in the psycho-oncology literature [27], which helps to contextualize our findings in the larger literature of spirituality and health. This study also has several limitations. The sample was fairly homogenous, as women were predominantly White and well-educated. Previous studies have shown that spirituality tends to be higher among ethnic minorities [31], thus limiting the generalizability of findings to a more diverse population. Second, although our analyses provided insights into temporal relationships, as an observational study, we cannot make conclusions regarding causality. In addition, as previously pointed out, the time interval between T1 and T2 was longer (12 months) than that between T2 and T3 (6 months), which may have been a factor in not finding significant paths between T1 and T2.
This study suggests several directions for future research. First, future studies might examine these reciprocal relationships in a more diverse cohort of cancer patients. Future research should also test whether these findings hold for other cancer types and for patients with advanced cancer, particularly near end-of-life where spirituality may be particularly relevant. Results also support the value of the 3-factor approach to the FACIT-Sp in future studies. Finally, intervention studies designed to improve physical health may consider including meaning in life as a secondary outcome to better determine whether there is a causal relationship between physical health and meaning to further elucidate the relationship.
Our findings provide preliminary support that greater self-reported physical health status is related to subsequent greater meaning in life rather than meaning being associated with subsequent physical health, as often assumed. Furthermore, physical health is not reciprocally related to a sense of peace or faith among breast cancer survivors. Future studies are needed that further elucidate the relationship between spirituality and physical health longitudinally.
Acknowledgments
Funding: National Cancer Institute R25 CA122061, Department of Defense grant DAMD17-01-1-0447, and the National Center for Advancing Translational Sciences UL1 TR001420-01
Footnotes
Ethical approval: “All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Conflict of Interest: The authors declare that they have no conflicts of interest to report.
References
- 1.Koenig HG (2015) Religion, spirituality, and health: a review and update. Adv Mind Body Med 29 (3):19–26 [PubMed] [Google Scholar]
- 2.Miller WR, Thoresen CE (2003) Spirituality, religion, and health. An emerging research field. Am Psychol 58 (1):24–35 [DOI] [PubMed] [Google Scholar]
- 3.Park CL, Masters KS, Salsman JM, Wachholtz A, Clements AD, Salmoirago-Blotcher E, Trevino K, Wischenka DM (2017) Advancing our understanding of religion and spirituality in the context of behavioral medicine. J Behav Med 40 (1):39–51. doi: 10.1007/s10865-016-9755-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jim HS, Pustejovsky JE, Park CL, Danhauer SC, Sherman AC, Fitchett G, Merluzzi TV, Munoz AR, George L, Snyder MA, Salsman JM (2015) Religion, spirituality, and physical health in cancer patients: A meta-analysis. Cancer 121 (21):3760–3768. doi: 10.1002/cncr.29353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oman D (2013) Defining Religion and Spirituality. In: Paloutzian R, Park C (eds) Handbook of the psychology of religion and spirituality 2nd edn. Guilford Press, New York, NY, pp 23–47 [Google Scholar]
- 6.Salsman JM, Fitchett G, Merluzzi TV, Sherman AC, Park CL (2015) Religion, spirituality, and health outcomes in cancer: A case for a meta-analytic investigation. Cancer 121 (21):3754–3759. doi: 10.1002/cncr.29349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puchalski C, Ferrell B, Virani R, Otis-Green S, Baird P, Bull J, Chochinov H, Handzo G, Nelson-Becker H, Prince-Paul M, Pugliese K, Sulmasy D (2009) Improving the quality of spiritual care as a dimension of palliative care: the report of the Consensus Conference. J Palliat Med 12 (10):885–904. doi: 10.1089/jpm.2009.0142 [DOI] [PubMed] [Google Scholar]
- 8.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D (2002) Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (, FACIT-Sp). Ann Behav Med 24 (1):49–58 [DOI] [PubMed] [Google Scholar]
- 9.Lipka MGecewicz C (2017) More Americans now say they’re spiritual but not religious. Pew Research Center http://www.pewresearch.org/fact-tank/2017/09/06/more-americans-now-say-theyre-spiritual-but-not-religious/. Accessed June 19 2018
- 10.Whitford HS, Olver IN, Peterson MJ (2008) Spirituality as a core domain in the assessment of quality of life in oncology. Psychooncology 17 (11):1121–1128. doi: 10.1002/pon.1322 [DOI] [PubMed] [Google Scholar]
- 11.Krupski TL, Kwan L, Fink A, Sonn GA, Maliski S, Litwin MS (2006) Spirituality influences health related quality of life in men with prostate cancer. Psychooncology 15 (2):121–131. doi: 10.1002/pon.929 [DOI] [PubMed] [Google Scholar]
- 12.Bai M, Lazenby M (2015) A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med 18 (3):286–298. doi: 10.1089/jpm.2014.0189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salsman JM, Yost KJ, West DW, Cella D (2011) Spiritual well-being and health-related quality of life in colorectal cancer: a multi-site examination of the role of personal meaning. Support Care Cancer 19 (6):757–764. doi: 10.1007/s00520-010-0871-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edmondson D, Park CL, Blank TO, Fenster JR, Mills MA (2008) Deconstructing spiritual well-being: existential well-being and HRQOL in cancer survivors. Psychooncology 17 (2):161–169 doi: 10.1002/pon.1197 [DOI] [PubMed] [Google Scholar]
- 15.Bai M, Dixon JK (2014) Exploratory factor analysis of the 12-item Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale in people newly diagnosed with advanced cancer. J Nurs Meas 22 (3):404–420 [DOI] [PubMed] [Google Scholar]
- 16.Canada AL, Murphy PE, Fitchett G, Peterman AH, Schover LR (2008) A 3-factor model for the FACIT-Sp. Psychooncology 17 (9):908–916. doi: 10.1002/pon.1307 [DOI] [PubMed] [Google Scholar]
- 17.Peterman AH, Reeve CL, Winford EC, Cotton S, Salsman JM, McQuellon R, Tsevat J, Campbell C (2014) Measuring meaning and peace with the FACIT-spiritual well-being scale: distinction without a difference? Psychol Assess 26 (1):127–137. doi: 10.1037/a0034805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whitford HS, Olver IN (2012) The multidimensionality of spiritual wellbeing: peace, meaning, and faith and their association with quality of life and coping in oncology. Psychooncology 21 (6):602–610. doi: 10.1002/pon.1937 [DOI] [PubMed] [Google Scholar]
- 19.Murphy PE, Canada AL, Fitchett G, Stein K, Portier K, Crammer C, Peterman AH (2010) An examination of the 3-factor model and structural invariance across racial/ethnic groups for the FACIT-Sp: a report from the American Cancer Society’s Study of Cancer Survivors-II (SCS-II). Psychooncology 19 (3):264–272. doi: 10.1002/pon.1559 [DOI] [PubMed] [Google Scholar]
- 20.Avis NE, Levine B, Naughton MJ, Case LD, Naftalis E, Van Zee KJ (2013) Age-related longitudinal changes in depressive symptoms following breast cancer diagnosis and treatment. Breast Cancer Res Treat 139 (1):199–206. doi: 10.1007/s10549-013-2513-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ware JE, Kosinski M, Keller SD (1994) SF-36 Physical and Mental Health Summary Scales: A User’s Manual. The Health Institute, Boston, MA [Google Scholar]
- 22.Little TD (2013) The Longitudinal CFA Model. In: Longitudinal Structural Equation Modeling. Guildford Publications, New York, NY, pp 137–159 [Google Scholar]
- 23.Selig JP, Little TD (2012) Autoregressive and cross-lagged panel analyis for longitudinal data. In: Laursen B, Little TD, Card NA (eds) Handbook of Developmental Research Methods The Guilford Press, New York, NY, pp 265–278 [Google Scholar]
- 24.Muthén L, Muthén B (2012) Mplus user’s guide Muthén & Muthén Los Angeles, CA [Google Scholar]
- 25.Hu LT, Bentler PM (1999) Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives. Struct Equ Modeling 6 (1):1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- 26.Bentler PM, Bonett DG (1980) Significance Tests and Goodness of Fit in the Analysis of Covariance-Structures. Psychol Bull 88 (3):588–606. doi: 10.1037/0033-2909.88.3.588 [DOI] [Google Scholar]
- 27.Munoz AR, Salsman JM, Stein KD, Cella D (2015) Reference values of the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being: a report from the American Cancer Society’s studies of cancer survivors. Cancer 121 (11):1838–1844. doi: 10.1002/cncr.29286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jim HS, Andersen BL (2007) Meaning in life mediates the relationship between social and physical functioning and distress in cancer survivors. Br J Health Psychol 12 (Pt 3):363–381. doi: 10.1348/135910706X128278 [DOI] [PubMed] [Google Scholar]
- 29.Visser A, Garssen B, Vingerhoets A (2010) Spirituality and well-being in cancer patients: a review. Psychooncology 19 (6):565–572. doi: 10.1002/pon.1626 [DOI] [PubMed] [Google Scholar]
- 30.Park CL (2005) Religion as a meaning-making framework in coping with life stress. Journal of Social Issues 61 (4):707–729. doi: 10.1111/j.1540-4560.2005.00428.x [DOI] [Google Scholar]
- 31.Canada AL, Fitchett G, Murphy PE, Stein K, Portier K, Crammer C, Peterman AH (2013) Racial/ethnic differences in spiritual well-being among cancer survivors. J Behav Med 36 (5):441–453. doi: 10.1007/s10865-012-9439-8 [DOI] [PubMed] [Google Scholar]


