Abstract
Purpose
Aseptic loosening (AL) has been reported to be one of the most frequent complications in Total Knee Arthroplasty (TKA) and Total Hip Arthroplasty (THA). The aim of this study was to identify the effects of gender, current tobacco use and BMI on the incidence of AL and implant survival time in THA and TKA.
Methods
Between July 2012 and December 2016 all patients that were diagnosed with an AL of a primary THA or primary TKA and underwent revision surgery at a single institution were retrospectively reviewed for this study. For each patient gender, current tobacco use, BMI, and implant survival time were obtained from the medical records.
Results
202 patients with 85 THA and 117 TKA were included in this study. There was no impact of the gender on implant survival times (p > 0.05) in THA and TKA. In the TKA group current tobacco use was associated with a significant shorter implant survival time (p < 0.05). For THA and TKA with cemented stem fixation a significant increase of AL was seen in overweight compared to normal weight patients (p < 0.05) and in obese compared to normal weight patients (p < 0.05).
Conclusion
The results demonstrate that current tobacco use and elevated BMI are associated with increased rates of AL in TKA. Also, in THA with cemented stem fixation an elevated BMI is associated with an increased incidence of AL.
Keywords: aseptic loosening, Hip, Knee, Arthroplasty
1. Introduction
Aseptic loosening (AL) remains one of the most frequent modes of failure in Total Knee Arthroplasty (31%–44%) and Total Hip Arthroplasty (55%).1, 2, 3 Various theories for the emergence of AL have been proposed and obesity has been described as an important factor influencing the outcome after Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA).4, 5, 6 Within various definitions of obesity the Body Mass index (BMI) is one of the most frequently used measures. The influence of an elevated BMI on AL in THA and TKA has been discussed controversially in literature. Some authors have reported an elevated BMI as a predictor of AL in THA and TKA.4,7,8 However, in several studies no association between obesity and AL of THA and TKA was seen.6,9 In summary, there is insufficient evidence on the effects of an elevated BMI on AL in THA and TKA.7
The influence of gender on the outcome after THA and TKA, as well as the implant survival time is still unclear. Some authors reported higher failure rates after THA in men compared to women,10 other authors found no differences between woman and men.11 Also, tobacco use is considered as a risk factor for AL in THA and TKA. However, the influence of tobacco use on the survival time of TKA and THA remains subject of controversial discussion.12,13
Aim of this study is to evaluate the influence of gender, current tobacco use and BMI on incidence of AL and on implant survival time in THA and TKA.
1.1. Patients and methods
All patients undergoing revision surgery due to an AL of a primary THA or primary TKA between July 2012 and December 2016 were included in this study. The appropriate ethics committee approved this retrospective study.
. The diagnosis of AL was suspected in cases with a periimplant lucency of greater than 2 mm14 in serial anteroposterior and lateral radiographs in absence of local or systemic signs of an infection. Diagnosis was confirmed by the serologic parameter CRP within normal limits in combination with a negative result of a microbiologic testing of a synovial fluid aspiration according to Schiffner et al.15 These tests were performed in all patients. To allow a retrospective control of the diagnosis soft tissue samples were obtained in all cases during the revision surgery and were subjected to a microbiological analysis. In none of the patients diagnosed with implant loosening bacterial growth was detected in these soft tissue samples. For each patient included the following data were collected from the medical record: gender, age, BMI, current smoking, and implant survival time. The BMI was calculated for each patient and according to the World Health Organisation (WHO) patients were categorized into three groups: normal (BMI 19–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese (BMI > 30 kg/m2). Implant survival time was defined as time between the primary arthroplasty and the date of revision surgery for AL. Also, the type of fixation was grouped into cemented and non-cemented fixation for all cases.
For statistical analysis Kruskal-Wallis non-parametric test followed by the post-hoc Dunn's test and the chi-squared test was used to compare categorical variables using SPSS software pack (version 23, IBM, New York, USA). P value < 0.05 was considered for statistic significance.
2. Results
In this study 202 patients were included. This group consisted of 85 with a THA and 117 patients with a TKA. Of the 85 patients included with a THA 39 stems were implanted cemented (12 normal weight, 14 overweight, 13 obese) and 46 stems with non-cemented (16 normal weight, 19 overweight, 11 obese) stem fixation. The demographic data are displayed in Table 1. All cups were implanted uncemented. All TKA were implanted in a cemented fixation technique.
Table 1.
Demographic data.
| TKA | THA | |
|---|---|---|
| n | 117 | 85 |
| age (years) | 72,5 ± 8.8 | 75.3 ± 8.1 |
| 🛇BMI (kg/m2) | 25.9 ± 3.1 | 25.9 ± 3.1 |
| woman | 80 | 47 |
| men | 37 | 38 |
| Current smokers | 74 | 50 |
| whitebloodcells (synovialfluid) | 1313 (range 100-2308) | 1900 (range 208-2884) |
There were no significant gender associated differences in implant survival time (p > 0.05) in THA as well as TKA groups. Furthermore, no significant difference in the mean BMI between women and men in the THA and TKA groups (p > 0.05) could be observed. Current tobacco use in TKA group was associated with significantly shorter implant survival time (Table 2., p < 0.05). In the THA group no difference in implant survival time between current smokers and non-smokers was seen (p > 0.05).
Table 2.
Survival time THA and TKA (years ± SD).
| survival time TKA | survival time THA | |
|---|---|---|
| current smoker | 9.3 ± 1.1 | 13.6 ± 3.5 |
| none smoker | 14.2 ± 2.1 | 14.1 ± 4.3 |
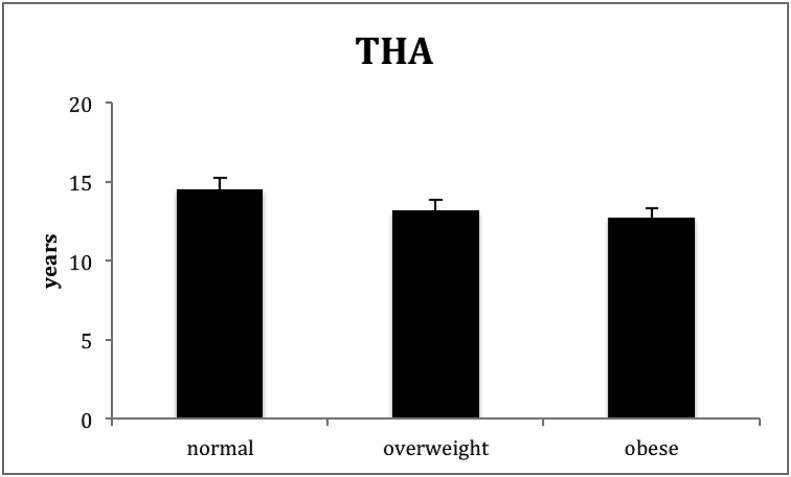
The mean survival time in the TKA group was 12.2 (±3.2) and 13.8 years (±3.6).in THA group. Cemented THA had a mean survival time of 13.1 (±2.4),and 14,5 (±3.2) years for uncemented THA. The THA overall survival time subdivided by the BMI groups is shown in Fig. 1. There was no significant difference between normal group, overweight group, and obese group (p > 0.05).
Fig. 1.
Mean survival time THA (Years).
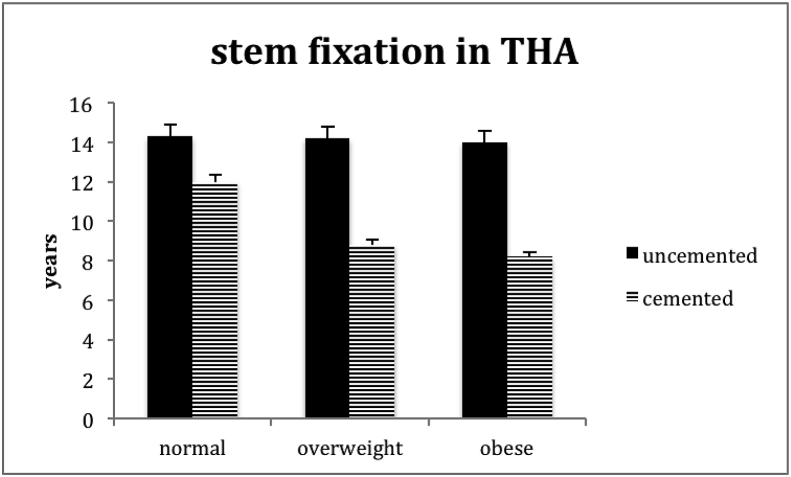
A further evaluation according to the stem fixation type of THA and survival time was carried out (Fig. 2). In the uncemented group (n = 46) no difference in survival time between the BMI groups was seen (p > 0.05). However, there were significant differences for the survival times of cemented THA according to the BMI group with a significant decrease of survival times with higher BMI. Overweight and obese group had significant shorter implant survival times compared to the adjacent lower BMI group (p < 0.05).
Fig. 2.
Stem fixation type and mean survival time THA (Years).
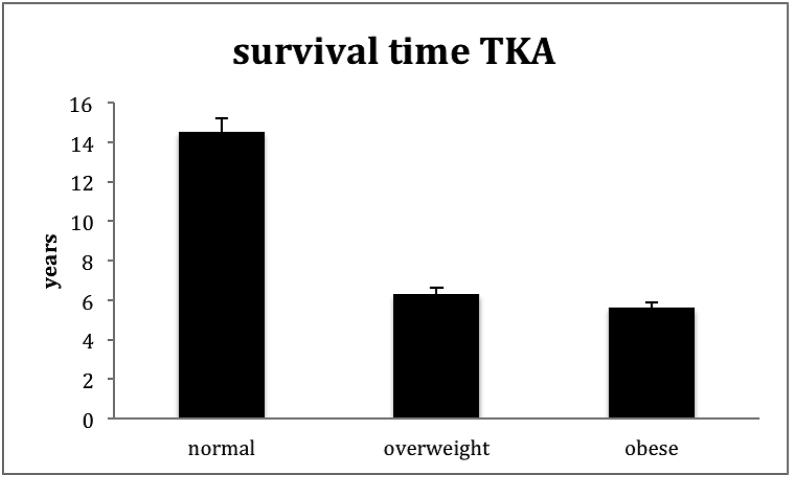
Within the TKA group a significant difference in implant survival time between normal weight versus overweight and normal weight versus obese (p < 0.05) was observed for AL (Fig. 3).
Fig. 3.
Mean survival time TKA (Years).
3. Discussion
Various host factors that may influence the incidence of AL have been reported.6 In this study the influence of gender, tobacco use, and BMI on the incidence of AL and on implant survival time after THA and TKA have been analyzed.
Within the limitations of this study no significant gender associated differences in implant survival time (p > 0.05) could be observed for THA as well as TKA. This finding is subject of controversial discussion within the available literature. In a systematic review Cherian et al.6 reported no relationship between gender and AL in TKA, however in THA male gender was associated with an increased risk of AL. With a mean follow-up of 3.0 years Inacio et al.16 stated significantly higher risk of AL following THA in women compared to men. However, in a prospective study with a mean follow up of 11.3 years Kostamo et al.11 found no significant differences in the incidence of AL and implant survivorship in THA between men and woman. These controversial results may be a result of different follow-up-times and inhomogeneous study designs. In contrast to most other studies, in the current study all THA and TKA patients were undergoing the same diagnostic algorithm for AL according to Schiffner et al.15
The impact of tobacco use on the incidence of AL and implant survival time is discussed controversially in literature. Meldrum et al.17 reported a significantly higher rate of component revision with shorter survival time in THA in smokers. Bedard et al.12 demonstrated that smoking significantly increases the risk of infection and reoperation after TKA. In our study current tobacco use was associated with a significantly shorter implant survival time after TKA. However, in the THA group no association was seen between current smoking and survival time. These results are in line with Khan et al.13 They found no differences in the revision rates of THA between none smokers, current smokers and former smokers. These results are contradictory. Nevertheless, based on these results current smoking seems to represent a risk factor for shorter implant survival time after TKA. This correlation was not seen for THA. In this study no information on former tobacco use was available. Further studies are needed to determine effects of former and current smoking habits to AL in THA and TKA.
The impact of obesity on the complication rates of THA and TKA is subject of controversial debate in current literature.5,7 Wagner et al.7 evaluated the influence of BMI on reoperation and complication rate after TKA and found a strong association between BMI and the risk of AL. Compared to patients with normal weight obese patients showed a significantly increased risk for AL of TKA. In a meta-analysis Kerkhoffs et al.18 demonstrated an increased implant revision rate of TKA in obese patients. However, other authors6,9,19 did not observe an influence of obesity on the incidence of AL in TKA. Even though the mechanical load increases with an elevated body weight, a lower activity levels in obese patient could account for the missing impact of BMI on AL in these studies.4 In this study we observed a significant difference in the implant survival times of TKA between normal weight, overweight, and obese patients.
Various studies evaluated the impact of obesity on complication rate following THA.5,6,20 In this study no significant impact of BMI on the incidence of AL in THA was observed. The results are in accordance with Andrew et al.5 who reported no significant difference in incidence of AL between normal weight and obese patients at a five-year follow up. In a systematic review carried out by Cherian et al.6 obesity was not associated with an increased risk of AL in THA. However, one major limitation of these studies represents the short follow-up time. With a follow-up of 10 years Munger et al.8 described a significant correlation between BMI and aseptic stem loosening in THA. In the current study the mean time to AL observed was 13.8 (±3.6) years. Overall, long follow-up times seem to be desirable to detect AL in cohorts of patients with THA. as demonstrated in our study. Due to the design of the current study the individual implant survival rate can be determined precisely.
In this study a significant impact of BMI on implant survival time was seen for cemented THA. In this group with increasing BMI the implant survival rate decreased significantly (p < 0.05). This effect was not present in uncemented THA. These findings suggest that the type of stem fixation plays an important role in patients with an elevated BMI. These results are in accordance with the findings by Melloh et al.,21 who presented an increase in the risk of AL of cemented hip stems by 3% for each additional unit of BMI. On the contrary, the current study demonstrated no significant impact of BMI on AL in uncemented THA. In accordance to these findings Stihsen et al.22 showed that a high BMI does not trigger progressive cementless stem migration.
This study has some limitations, such as its retrospective design and relatively low sample size. Also, due to the design there are no information about further comorbidity of the patients and the level of physical activities. The study did not adjust for differences in implant designs in THA and TKA.
Our results support the assumption that a high BMI and current tobacco use are associated with an increased risk for AL and shorter implant survival time in TKA. For THA no significant correlation was found between current tobacco use or BMI and incidence of AL or implant survival time. However, in cemented stem fixation of THA a high BMI significantly increases the risk of aseptic stem loosening. Further studies including larger numbers of patients, a prospective study design, longer follow up times, and adjustment for different implant designs of THA and TKA are needed to support these results.
4. Conclusion
The results demonstrate that current tobacco use and elevated BMI are related to increased rates of AL in TKA. Also, THA with cemented stem fixation and elevated BMI is associated with an increased incidence of AL.
Conflicts of interest
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgment
This study was not supported.
References
- 1.Sadoghi P. Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty. 2013;28(8):1329–1332. doi: 10.1016/j.arth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 2.Robertsson O. The Swedish Knee Arthroplasty Register 1975-1997: an update with special emphasis on 41,223 knees operated on in 1988-1997. Acta Orthop Scand. 2001;72(5):503–513. doi: 10.1080/000164701753532853. [DOI] [PubMed] [Google Scholar]
- 3.Khan M. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint Lett J. 2016;98-B(1 Suppl A):105–112. doi: 10.1302/0301-620X.98B1.36293. [DOI] [PubMed] [Google Scholar]
- 4.Foran J.R. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004;19(7):817–824. doi: 10.1016/j.arth.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 5.Andrew J.G. Obesity in total hip replacement. J Bone Joint Surg Br. 2008;90(4):424–429. doi: 10.1302/0301-620X.90B4.20522. [DOI] [PubMed] [Google Scholar]
- 6.Cherian J.J. What host factors affect aseptic loosening after THA and TKA? Clin Orthop Relat Res. 2015;473(8):2700–2709. doi: 10.1007/s11999-015-4220-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagner E.R. Effect of body mass index on reoperation and complications after total knee arthroplasty. J Bone Joint Surg Am. 2016;98(24):2052–2060. doi: 10.2106/JBJS.16.00093. [DOI] [PubMed] [Google Scholar]
- 8.Munger P. Patient-related risk factors leading to aseptic stem loosening in total hip arthroplasty: a case-control study of 5,035 patients. Acta Orthop. 2006;77(4):567–574. doi: 10.1080/17453670610012629. [DOI] [PubMed] [Google Scholar]
- 9.Griffin F.M. Total knee arthroplasty in patients who were obese with 10 years followup. Clin Orthop Relat Res. 1998;(356):28–33. doi: 10.1097/00003086-199811000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Roder C. Obesity, age, sex, diagnosis, and fixation mode differently affect early cup failure in total hip arthroplasty: a matched case-control study of 4420 patients. J Bone Joint Surg Am. 2010;92(10):1954–1963. doi: 10.2106/JBJS.F.01184. [DOI] [PubMed] [Google Scholar]
- 11.Kostamo T. No difference in gender-specific hip replacement outcomes. Clin Orthop Relat Res. 2009;467(1):135–140. doi: 10.1007/s11999-008-0466-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bedard N.A. What is the impact of smoking on revision total knee arthroplasty? J Arthroplasty. 2018;33(7S):S172–S176. doi: 10.1016/j.arth.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Khan L.A. The complication rate and medium-term functional outcome after total hip replacement in smokers. Hip Int. 2009;19(1):47–51. doi: 10.1177/112070000901900109. [DOI] [PubMed] [Google Scholar]
- 14.Greiner B., Braun M., Becker W. Value of the plain roentgen image and arthrography in diagnosis of loosening of cemented hip endoprostheses. Z Orthop Ihre Grenzgeb. 1997;135(4):292–296. doi: 10.1055/s-2008-1039391. [DOI] [PubMed] [Google Scholar]
- 15.Schiffner E. Normal CRP and WBC values in total hip arthroplasty (THA) with signs of loosening. Do we need a joint aspiration? J Clin Orthop Trauma. 2018 doi: 10.1016/j.jcot.2018.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inacio M.C. Sex and risk of hip implant failure: assessing total hip arthroplasty outcomes in the United States. JAMA Intern Med. 2013;173(6):435–441. doi: 10.1001/jamainternmed.2013.3271. [DOI] [PubMed] [Google Scholar]
- 17.Meldrum R.D. Does smoking affect implant survivorship in total hip arthroplasty? A preliminary retrospective case series. Iowa Orthop J. 2005;25:17–24. [PMC free article] [PubMed] [Google Scholar]
- 18.Kerkhoffs G.M. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am. 2012;94(20):1839–1844. doi: 10.2106/JBJS.K.00820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naziri Q. Bariatric orthopaedics: total knee arthroplasty in super-obese patients (BMI > 50 kg/m2). Survivorship and complications. Clin Orthop Relat Res. 2013;471(11):3523–3530. doi: 10.1007/s11999-013-3154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibrahim T. No influence of body mass index on early outcome following total hip arthroplasty. Int Orthop. 2005;29(6):359–361. doi: 10.1007/s00264-005-0012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Melloh M. Predictors of early stem loosening after total hip arthroplasty: a case-control study. J Orthop Surg. 2011;19(3):269–273. doi: 10.1177/230949901101900301. [DOI] [PubMed] [Google Scholar]
- 22.Stihsen C. Subsidence of a cementless femoral component influenced by body weight and body mass index. Int Orthop. 2012;36(5):941–947. doi: 10.1007/s00264-011-1360-1. [DOI] [PMC free article] [PubMed] [Google Scholar]