Abstract
Background
In low resources settings, especially during periods of turmoil, asthma care becomes emergency-oriented, and adherence to international asthma management guidelines such as long-term inhaled corticosteroids (ICS) prescription is limited. The role of education for inhaler technique to guarantee treatment efficacy is neglected and follow up is hampered by war-related displacement. In Syria, asthma care is not included in primary care, and frequently, internal medicine general hospital outpatient clinics are the first contact. The main objective of our study was to evaluate the adequacy of prescription of controller medications (ICS/LABA) by residents on initial contact with patients, and the effect of regular onsite personalized supervision and coaching by a trainer pulmonologist on improving their practice. The second objective was to evaluate the efficacy of mobile training for inhaler technique, and asthma mobile follow up.
Methods
We developed an audit form to assess initial prescription of ICS/LABA by residents. Filled forms were reviewed by a trainer pulmonologist for compliance with international guidelines. When discrepancies were noted, onsite training was provided. Auditing of new presenting asthma patients is continual to evaluate improvement of initial prescription by the same residents. In parallel, video-mobile education of patients for inhaler technique, and mobile interviewing follow up were tested.
Results
Implementation of these strategies resulted in improved adherence of residents to ICS dosing guidelines (P=0.002), optimal inhaler technique by patients, and efficacy of mobile follow up.
Conclusions
WHO programs for CRD in developing countries, especially in regions of conflict and war, should include auditing of care by residents with onsite coaching by trainer pulmonologists, and mobile education for technology of inhaler and patient follow up.
Keywords: Asthma audit, case management supervision, mobile-health, inhaler technique, Global Alliance against Chronic Respiratory Diseases (GARD), World Health Organization (WHO)
Introduction
Adherence to international asthma management guidelines is suboptimal even in developed countries (1,2). In low resources settings, especially in areas of armed conflict and war like Syria, clinical care is more difficult with most asthma patients receiving only initial care without routine follow up, and future care delivered in urgent and emergency settings. This is due to poverty and war related migration and displacement (3). A survey of asthma in shelters in Syria in 2017 showed the same (4). The World Health Organization Eastern Mediterranean Regional Office (WHO-EMRO) believes similar conditions exist outside the shelters with internally displaced individuals, and patients in besieged zones (5). According to the Director General of EMRO, every month, more than 30,000 people need treatment for injuries, and people with chronic diseases are dying of complications (5). Many health care primary care centers of the Ministry of Health (MOH) have been destroyed, closed, or lack health care workers due to migration (5,6). Consequently, general public hospital outpatient internal medicine clinics are the first contact for care for the much-deprived people (6,7).
Health systems in Syria have been weakened by sustained armed conflict. These systems are not multisectoral, and asthma management is not routinely addressed in MOH-WHO primary care centers. Furthermore, there is a weak referral system to secondary care, or to asthma specialists (6). The majority of asthma patients refer themselves to free clinics in secondary care public hospitals, a practice which has been amplified by the economic shortages of the war.
In 2016, upon the recommended of the multicenter national Global Alliance against Chronic Respiratory Diseases (GARD-WHO) survey (8), the WHO country office in Syria published the “Technical guide for management of chronic respiratory diseases in primary care, emergency rooms and general medicine outpatient clinics in public hospitals” as hard copy and on the MOH website. This publication includes guidelines and technical guide for asthma care, based on the Global Initiative for Asthma (GINA) Stepwise approach for asthma management. The guidelines stipulate initial prescription of controllers after assessment of level of control (symptom control and future risk), adapted to local capacities (1,9). Although this guide was distributed to physicians in primary care health centers and to residents in outpatient clinics of secondary care general hospitals, it is not clear to what degree health care providers in Syria are aware of these recommendations. Medical knowledge about asthma and its management by residents has not, to our knowledge, been systematically addressed in outpatient clinics. To attempt to gain this information, we proposed an intervention with three components. First, audits conducted to evaluate adequacy of prescribing of ICS with or without LABA by residents when patients first present to the outpatient clinic. Second, audits are repeated in the same health care setting to highlight the effect of supervision and coaching by a trainer pulmonologist on asthma management when initial prescription patterns by the resident are deemed inadequate. Third, utilization of mobile devices for initial education of patients on how to use inhaler was measured and reported. We used mobile video to provide training for inhaler technique during the first week after initiating ICS therapy, taking as reference the National Assessment of Educational Progress (NAEP) program video (10). This study also included monthly face to face or mobile follow up, for three months, to assess adherence and subsequently control.
Although this is a pilot observational feasibility study with a limited number of patients and of residents, our results will shed light on the effectiveness of onsite personalized supervision of residents on improving initial prescription of ICS with or without LABA by residents, and the effectiveness of mobile video training for inhaler technique.
Methods
Data collection: inclusion criteria
All asthma patients presenting for the first time to the outpatient clinic of internal medicine in a crowded general hospital in Damascus (Damascus Hospital) between April and May 2018 were included in the study. Patients were either previously physician diagnosed as having asthma, or presented with asthma like symptoms and diagnosed for the first time as asthmatics in the clinic. This hospital is accredited by the MOH to train residents with exclusive clinical responsibilities and no other academic or research tasks. Although asthma management is not yet included in WHO-MOH programs for health centers for primary care at the time of the survey, these free clinics recruit self-referred asthma patients from deprived poor areas, as first contact, or receive patients referred from emergency room in the same hospital. Fifteen residents were involved in this pilot study.
Data collection tools
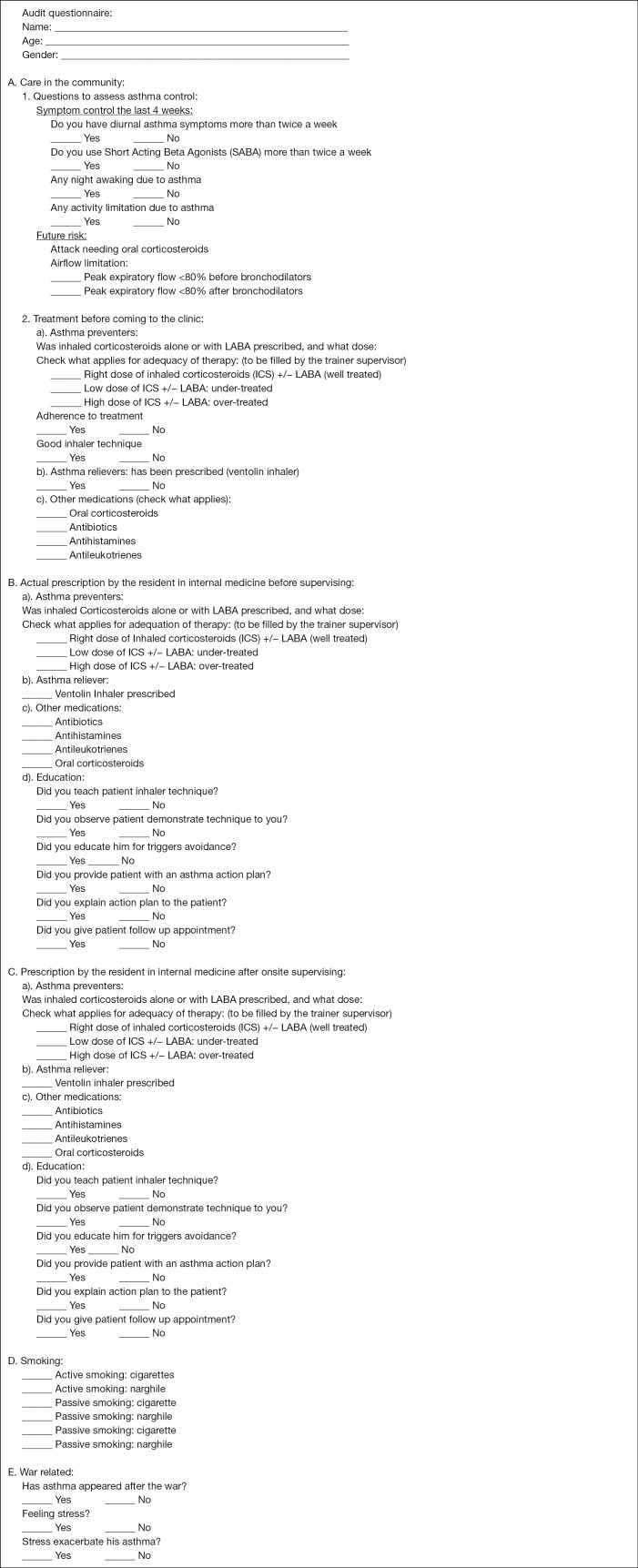
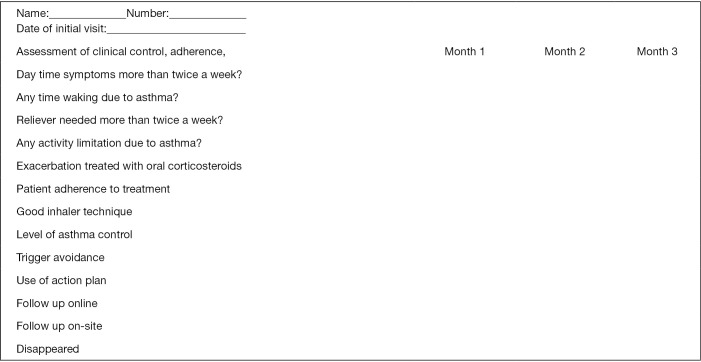
We introduced two audits: the asthma care audit form (Figure S1), and the follow up audit form (Figure S2).
Figure S1.
The audit form for initial visit.
Figure S2.
Follow up audit.
The asthma care audit was designed to evaluate care when patients first present to the clinic. This data collection tool included three primary features: auditing care, providing supervision and training onsite taking as reference our technical guide, and evaluation of the impact of training on improving resident adherence to guidelines.
The asthma care audit form (Figure S1): this was prepared based on GINA criteria for asthma control to initiate a stepwise therapeutic approach. It included:
❖ Documentation of asthma control level (well controlled, partly controlled, and uncontrolled) at presentation:
⬥ Questions to assess symptom control;
⬥ Identification of future risk for exacerbation;
⬥ Documentation of peak expiratory flow measurements.
❖ List of pre-visit prescriptions of preventers;
❖ List of pre-visit use of non-useful therapies like antibiotics;
❖ Investigating the adequacy of the patient inhaler technique at presentation;
❖ Stepwise approach for initiating preventive treatment with inhaled corticosteroids (ICS), alone or ICS with long acting β2 agonists (ICS/LABA) by the resident:
⬥ Right dose when the initial prescription is adequate. e.g.: step 2 if partly controlled, and 3 if uncontrolled, in this case the patient is well treated;
⬥ The initial dose is lower than requested for the level of control: e.g.: step 2 for uncontrolled, or non-treatment in spite of future risk or/and the patient is only partly controlled, in this case the patient is under-treated;
⬥ The initial dose is higher than requested for the level of control, e.g.: step 3 for partly controlled, in this case the patient is over-treated.
❖ Education of patients: updated inhaler technique instruction using pressurized meter dose inhaler (pMDI), and triggers avoidance by the resident;
❖ Documentation of distribution of asthma self-management plan by the resident.
❖ List of war and stress factors which affect health;
❖ Active and passive smoking of cigarette or waterpipe.
Two groups were audited
Group one
Included forty-five [45] previously diagnosed asthma patients presenting to the outpatient clinic for the first time. We audited their care in the community before coming to hospital. We also audited clinic management including initial prescription of preventers and other medications, and initial education of patients by internal medicine residents. A trainer pulmonologist reviewed filled audit forms and whenever a teachable moment arose, provided onsite teaching to residents to correct any deficiencies and promote patient education.
Group two
Included forty-five [45] patients presenting to the outpatient clinic and managed by the same practitioner after case teaching training by supervisor.
To conclude, we have two groups: group one consists of patients presenting from the community to the clinic and managed by the resident before supervision by the trainer, and group two of patients consequently presenting to the clinic and treated by the residents after coaching and supervision to measure the impact of supervision.
In parallel, we instituted a program of two components to communicate with asthma patients via mobile devices.
First, an educational video on optimal inhaler technique was sent to patients during the first week after initiating ICS therapy at the first presentation visit. We believe that, good technique is gold standard, and we supposed that we cannot evaluate outcomes of treatment if inhaler technique is inadequate.
Second, monthly follow up for three month (follow up audit form: Figure S2): a second component of our program is monthly follow up to asses adherence and subsequent control either by onsite evaluation by the resident when the patient was able to return, or by mobile interview when follow up was impossible due to displacement.
Our current paper will focus on auditing, impact of supervision, and evaluation of the efficacy of use of mobile video to provide training for inhaler technique during the week following the initial prescription, taking as reference the NAEP program video (10).
Statistical analysis
Descriptive statistics using means (standard deviations) for continuous data and frequencies (%) for categorical data were calculated. The chi-square test was used to compare percentages between the two groups before supervision of the resident practitioner and then after supervision. The t-test was used to compare differences between continuous variables. All analyses were completed using the Statistical Package for the Social Sciences (SPSS) version 18 (IBM Corporation). P<0.05 was considered statistically significant.
Ethics review
Ethical approval was secured from hospital institutional board, and patient consent forms were collected. Physicians accepted to participate.
Results
Table 1 lists the initial characteristics of patients, their level of control and how they were managed in the community before seeking care in this outpatient clinic. A total of 90 asthmatics in two groups were analyzed. Group one represents patients presenting to the outpatient clinic and managed by the residents before this resident being supervised by a trainer pulmonologist, and group two represents patients presenting to the outpatient clinic and managed by the same practitioner after case teaching training by supervisor. No significant differences in community management before coming to the hospital were noted between the two groups. Our data show that patients seeking asthma care at Damascus General Hospital were inadequately managed in the community according to guidelines, and were partially or totally uncontrolled. Only 7 of 90 patients had ICS alone or with LABA prescribed in adequate doses. Many patients were receiving non-useful drugs like antihistamines, antibiotics, and leukotriene modifiers as first line prescription. Education for trigger avoidance or inhaler technique was absent.
Table 1. Characteristics of subjects presenting to the clinic from the community.
| Characteristics | Group one: will be treated before supervising, n (%) | Group two: will be treated after supervising, n (%) | P value |
|---|---|---|---|
| Age (years), m ± SD | 35.6±18.5 | 34.6±16.3 | 0.77 |
| Gender | |||
| F | 24 (53.33) | 26 (57.78) | 0.671 |
| M | 21 (46.67) | 19 (42.22) | |
| Level of asthma control | |||
| Uncontrolled | 29 (64.44) | 24 (53.33) | 0.236 |
| Partly controlled | 8 (17.78) | 6 (13.33) | |
| Well controlled | 8 (17.78) | 15 (33.33) | |
| Adequacy of therapy: was he treated with the right dose of ICS +/− LABA | |||
| Over treated | 13 (28.89) | 18 (40.00) | 0.53 |
| Undertreated | 28 (62.22) | 24 (53.33) | |
| Well treated | 4 (8.89) | 3 (6.67) | |
| Adherence | 3 (6.67) | 4 (8.89) | 0.694 |
| Prescription of oral corticosteroids | 8 (17.78) | 6 (13.33) | 0.56 |
| Good inhaler technique | 4 (8.89) | 8 (17.78) | 0.215 |
| Ventolin as needed | 25 (55.56) | 30 (66.67) | 0.28 |
| Antibiotics prescription | 2 (4.44) | 2 (4.44) | 1 |
| Antihistamine prescription | 6 (13.33) | 8 (17.78) | 0.561 |
| Antileukotrienes prescriptions | 4 (8.89) | 4 (8.89) | 1 |
| Peak flow percent predicted before bronchodilators (%), m ± SD | 59±0.15 | 61±0.15 | 0.37 |
| Peak flow percent predicted after bronchodilators (%), m ± SD | 71±0.16 | 76±0.13 | 0.12 |
| Cigarette smoker | 13 (28.89) | 12 (26.67) | 0.814 |
| Narghile smoker | 5 (11.11) | 7 (15.56) | 0.535 |
| Passive smoker cigarette | 9 (20.00) | 5 (11.11) | 0.203 |
| Passive smoker narghile | 6 (13.33) | 4 (8.89) | 0.555 |
| Asthma appeared after the war | 29 (64.44) | 32 (71.11) | 0.499 |
| Stress feeling | 37 (82.22) | 32 (71.11) | 0.215 |
| Asthma exaggerated by stress | 37 (82.22) | 39 (86.67) | 0.561 |
ICS, inhaled corticosteroid.
Table 2 is a comparative analysis of initial controller treatment prescribed and initial patient education by residents for group one and group two of patients, showing that prescription of adequate dose of ICS alone or with LABA improved significantly in Group two and there was a reduction of use of non-useful drugs (P=0.002).
Table 2. Importance of supervising in management of asthma by residents in the two groups:
| Variable | Without supervising, n (%) | With supervising, n (%) | P value |
|---|---|---|---|
| Adequacy of initial prescription: was he treated with the right dose of ICS +/− LABA | |||
| Over treated | 9 (20.00) | 4 (8.89) | 0.002 |
| Undertreated | 16 (35.56) | 5 (11.11) | |
| Well treated | 7 (15.56) | 36 (80.00) | |
| Oral corticosteroids now by resident | 12 (26.67) | 7 (15.56) | 0.197 |
| Antileukotrienes now by resident | 20 (44.44) | 2 (4.44) | 0.0001 |
| Antihistamine now by resident | 15 (33.33) | 2 (4.44) | 0.0001 |
| Antibiotic now by resident | 12 (26.67) | 2 (4.44) | 0.004 |
| Ventolin spray now by resident | 43 (95.56) | 45 (100.00) | 0.153 |
| Education for triggers avoidance | 29 (64.44) | 43 (95.56) | 0.0001 |
| You educated him for how to use inhaler | 45 (100.00) | 45 (100.00) | |
| You gave him asthma self-management plan | 45 (100.00) | 45 (100.00) |
ICS, inhaled corticosteroid.
Use of mobile devices
Implementation of mobile training one week after the initial visit resulted in all patients except one using the inhalers correctly. This was partly due to the distributed video training material, and to mobile case by case supervision by the resident of videos produced by the patient on how to use inhaler until a good technique is achieved, e.g., the videos attached of a woman: video with bad technique of inhaler before training (Figure 1), then good technique after training (Figure 2).
Figure 1.

Bad technique (11). Available online: http://www.asvide.com/article/view/30794
Figure 2.

Right technique of inhaler after mobile training (12). Available online: http://www.asvide.com/article/view/30795
Table 3 represents data after three months of follow up. Forty-four [44] patients were lost to follow up, 28 were followed only by mobile interview and were well controlled. Sixteen [16] were followed regularly in the clinic, among them 14 were well controlled. Twenty-two [22] patients were followed up by a combination of clinic visit and mobile follow up (when clinic visit was impossible). Twenty [20] were controlled. We observed that mobile follow up was at least as effective as on-site follow up (P=0.19).
Table 3. Mobile and/or onsite follow up.
| Method of follow up | Controlled asthma after 3 months | P value | |
|---|---|---|---|
| No | Yes | ||
| Online | Zero | 28 | 0.19 |
| Mobile and onsite | 2 | 20 (one uncontrolled for non-adherence, the second needs higher step) | |
| Onsite only | 2 | 14 (one uncontrolled because exacerbation by infection, the second is non-treated rhino-sinusitis) | |
| Disappeared | 44 | ||
Correction of initial prescription was done onsite or online. Online follow up was not inferior to on site follow up for gaining control and adherence. P=0.19.
Discussion
Several studies have shown that although management guidelines and programs are available in developing counties and in areas of conflict, implementation at country level is weak (1,2,8,9,13). Weakness of health systems and lack of medical education at primary and secondary level of care hampers asthma management even if essential supplies are available (1,5,13). These findings have been documented in several developing countries (1,13) and also in areas of armed conflict countries such Syria in the Eastern Mediterranean Region (2,4).
The healthcare system in Syria has been challenged during the war. Many primary care health centers went out of service (2,4,5,6) negatively impacting initial and follow up care of asthma patients. Most asthma care is now provided in Internal Medicine outpatient hospital clinics staffed by residents in training. It is not clear to what degree these residents are familiar with and implement established asthma management guidelines. By auditing the care provided by residents, we were able to evaluate adequacy of initial prescription of controller medications. We were also able to assess adequacy of education of patients in asthma care, trigger avoidance, use of unnecessary medications, and inhaler technique. When gaps were noted, the use of onsite supervision by a trainer pulmonologist resulted in improvement in all parameters.
It is important to note that trainers were asked to use our “National Technical guide based on GINA” as reference. In this guide, initial prescription of daily controllers is followed by an escalating step wise approach based on GINA presenting symptoms and future risks (1).
This short term, single center, feasibility pilot study adds to the scientific body of knowledge in three ways. First, it shows that implementation of an auditing step in International Management Guidelines identified deficiencies in knowledge and practice among general practitioners and residents. Second, it further revealed that the International Management Guidelines can be strengthened by adding onsite resident supervision and onsite personalized case teaching. Our study establishes the role of onsite supervision of residents by pulmonary experts as a key factor in improving asthma treatment especially the initial prescription of controller medications. Finally, the study established the role of mobile devices in allowing effective communication with patients to help them master good inhaler technique. This was accomplished through video exchange during the first week after initiating long term treatment, and through monthly follow up mobile interactions especially when patients were unable to return to clinic in zones of conflict.
The development and implementation of the various WHO programs to address non-communicable diseases, especially chronic respiratory disorders, has been instrumental in improving respiratory care in many nations. The two main WHO programs are the Practical Approach to Lung Health (PAL) (14) and the Package of Essential Non-communicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings (15). These programs helped manage chronic diseases and identified areas where protocols and training of these programs could be adjusted to meet the needs of some developing nations. One of the strengths of these programs is the inclusion of auditing mechanisms to ensure compliance with guidelines, regular supervision to insure that different components of the program are running well, and referral to secondary care district hospitals when needed. These programs, however, were launched before the war, onsite supervision and onsite case teaching by the trainer of general practitioners at primary or secondary care outpatient clinics in hospitals was not prioritized, but rather initial training workshops for physicians who will manage to launch the program. As we said The internal armed conflict resulted on poverty and economic shortage, internal displacement to shelters and difficulty of patients transportation (2,4,5). In such situation we proved that adding onsite supervision and onsite personalized teaching of residents for inadequately managed cases will improve care.
PAL and PEN were introduced in Syria in 2004 and 2009, respectively. Initial workshops to train the trainers were achieved by WHO headquarter and regional program officer but implementation was not sustainable, non-scaling up (14-16), due, in our opinion, to a weak health system, lack of defined criteria for intersectoral collaboration between the directorate of NCD and the directorate or Primary care in MOH, and lack of multisectoral collaboration. Specifically, academic experts were appointed for the national group, but they were not given any supervisory or organizational role. Multisectoral collaboration and improving medical knowledge are recommended in the WHO action plan 2013–2020 for NCD (17).
A third WHO program is the Global Alliance against Chronic Respiratory diseases GARD-WHO which contributes to WHO’s global work to prevent and control chronic respiratory diseases especially at country level (13). GARD work in Syria has been successfully intersectoral and multisectoral, and academics are highly involved. This resulted in the elaboration of “Technical guide for management of Chronic Respiratory Diseases in Primary Care. Emergency and General Medicine Outpatients Clinics in Public Hospitals”. This guide included national algorithms, guidelines, essentially based on GINA for asthma, and audits for care before and after supervision and coaching of practice for asthma and COPD at primary care, and first referral level. A case management approach with onsite discussion between the supervisor pulmonologist and the physician was recommended. Audits for follow up were also included in our guide. Our survey used these audits.
The originality of our study is that after initial auditing of asthma care in the community and during initial encounter with the resident practitioner, we provided teaching on case by case basis when error in following guidelines were noted. Our preliminary results show that by auditing after onsite case teaching, there is quick improvement of knowledge as demonstrated by adequate prescription of ICS alone or with LABA, and practically no prescription of non-useful drugs (Tables 1,2).
The originality of our study also relates to the use of mobile devices in follow up and ensuring adequate inhaler technique performed by mobile video taking as reference the NAEP program (10). Onsite checking and teaching for inhaler technique once during the first initial visit proved insufficient and mobile video exchange was a good solution. This was a successful approach to manage poor patients displaced by war who were unable to come back to clinic for further follow-up.
We are not the first to use mobile health for asthma in the medical literature, but the first to introduce mobile videos to train in inhaler technique. Xiao et al. conducted a systematic review and meta-analysis of relevant studies in 2018 and demonstrated that mobile interventions compared to routine care improved level of asthma control and adherence to treatment, and reduced exacerbation rate (18). Similarly, MacDonell et al. in an NHLBI funded pilot study of African American adolescent minorities (20–29 old), found that the use of computer and mobile devices to provide information sessions and regular personalized messages were more efficient in changing behavior moving to adherence than face to face contact (19). The investigators, however, did not introduce video mobile inhaler technique teaching.
Our survey has this add on value of the efficacy of video-mobile for inhaler technique. The ERS-International Society for Aerosols in Medicine task force reported that: the benefice of using inhaler medication depends on the dose that is deposited into the lung. This dose is dependent on correct use of inhalers (20). Our study includes the following two limitations. We evaluated only a small number of residents and the study was conducted in a single center. This could limit the external validity of the study.
Conclusions
The GARD-WHO survey on asthma prevalence and risk factors in Syria revealed gaps in asthma management (8). Only a few patients were receiving ICS, asthma education was absent, and follow up was limited. We elaborated on the Technical Guide for Management of Chronic Respiratory Diseases in Primary Care, the Emergency and General Medicine Outpatients Clinics in Public Hospitals. The guide was published by WHO country office and is available at MOH website.
We audited asthma care in patients presenting to the outpatient clinic of a General Hospital in Damascus and identified inadequate prescription of ICS by residents and bad inhaler technique by patients. Next, we assessed resident knowledge and management before and after supervision by a pulmonologist trainer from the same hospital. Our results showed improvement of asthma care after supervision and onsite clinical case-based teaching, especially for adequate prescribed dose of ICS P=0.002. Equally we demonstrated that Mobile video training for inhaler technique was very successful. We also observed that mobile interview for follow up was promising. Although our study is a feasibility short term study, we were successful in coping with turmoil, poverty, shortage of medical work force, and difficulty of transportation.
We recommend WHO programs for CRD to include these practical items: auditing, onsite supervision, and mobile communication with patients.
Acknowledgements
We are grateful for Dr. Hala Rifai and Dr. AbdulRahman Dakkak for their continual help as trainers pulmonologists from Damascus Hospital. And for the Director of Damascus Hospital who hosted the pilot survey.
Ethical Statement: Ethical approval was secured from hospital institutional board, and patient consent forms were collected.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Available online: www.ginasthma.org
- 2.Boulet LP. War-time Asthma: Lessons from Syria. J Thorac Dis 2017;9:3412-4. 10.21037/jtd.2017.08.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Eastern Mediterranean Region. Annual report of the Regional Director 2015. The work of WHO in the Eastern Mediterranean Region. Noncommunicable Diseases: Regional framework for action. Published 2016. Retrieved on March 4, 2018. Available online: http://applications.emro.who.int/docs/RD_Annual_Rep_2016_Noncommunicable_Diseases_19004_EN.pdf?ua=1&ua=1
- 4.Mohammad Y, Rafea S, Latifeh Y, et al. Uncontrolled and under-diagnosed asthma in a Damascus shelter during the Syrian Crisis. J Thorac Dis 2017;9:3415-24. 10.21037/jtd.2017.08.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devi S. Syria's health crisis: 5 years on. Lancet 2016;387:1042-3. 10.1016/S0140-6736(16)00690-5 [DOI] [PubMed] [Google Scholar]
- 6.Mohammad Y, Dubaybo B. Managing Bronchial Asthma in Underprivileged Communities. In: Pereira C. editor. Asthma. Rijeka, Croatia: Intech, 2016. [Google Scholar]
- 7.Mohammad Y. Managing Bronchial Asthma in Primary Health Care (PHC) in Syria as Example of Middle Income Developing Country: An Expert Opinion. EC Pulmonology and Respiratory Medicine 2015:S1-5.
- 8.Mohammad Y, Shaaban R, Yassine F, et al. Executive summary of the multicenter survey on the prevalence and risk factors of chronic respiratory diseases in patients presenting to primary care centers and emergency rooms in Syria. J Thorac Dis 2012,4:203-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prevention and Control of Noncommunicable Diseases: Guidelines for primary health care in low-resource settings. Geneva: World Health Organization, 2012. [PubMed] [Google Scholar]
- 10.National Asthma Education and Prevention Program National asthma education and prevention program.expert panel report: Guidelines for the Diagnosis and management of asthma update on selected topics-2002. J Allergy Clin Immunol 2002;110:S141-219. [PubMed] [Google Scholar]
- 11.Mohammad Y, Shaaban R, Salman HA, et al. Bad technique. Asvide 2019;6:084. Available online: http://www.asvide.com/article/view/30794
- 12.Mohammad Y, Shaaban R, Salman HA, et al. Right technique of inhaler after mobile training. Asvide 2019;6:085. Available online: http://www.asvide.com/article/view/30795
- 13.Khaltaev N. GARD, new way to battle with Chronic Respiratory Diseases, from disease oriented programmes to global partnership. J Thorac Dis 2017,9:4676-89. 10.21037/jtd.2017.11.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamzaoui A, Ottmani S. Practical Approach to Lung Health: Lung health for every one? European Respiratory Update. Eur Respir Rev 2012;21:186-95. 10.1183/09059180.00002612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Package of essential noncommunicable (PEN) disease interventions for primary health care in low-resourced settings. Geneva, World Health Organization, 2010. Available online: http://www.who.int/ nmh/publications/essential_ncd_interventions_lr_settings.pdf
- 16.Me'emary F, Ottmani SE, Pio A, et al. Results of the feasibility test of the Practical Approach to Lung Health in the Syrian Arab Republic. East Mediterr Health J 2009;15:504-15. 10.26719/2009.15.3.504 [DOI] [PubMed] [Google Scholar]
- 17.Global action plan for the prevention and control of noncommunicable diseases 2013-2020. World Health Organization. ISBN 978 92 4 150623 6 (NLM classification: WT 500).
- 18.Xiao Q, Wang J, Chiang V, et al. Effectiveness of mHealth Interventions for Asthma Self-Management: A Systematic Review and Meta-Analysis Stud Health Technol Inform 2018;250:144-5. [PubMed] [Google Scholar]
- 19.MacDonell K, Naar S, Gibson-Scipio W, et al. Technology Intervention for African American Emerging Adults With Asthma. JMIR Res Protoc 2018;7:e98. 10.2196/resprot.8872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laube BL, Janssens HM, de Jongh FH, et al. What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J 2011;37:1308-31. 10.1183/09031936.00166410 [DOI] [PubMed] [Google Scholar]