Abstract
Background
Diabetic ketoacidosis (DKA) is a metabolic catastrophe which could occur in any type of diabetes. Even when fundamental key points of DKA treatment had been followed, some differences exist in treatment protocols in each physician, highlighting the need to assess adherence to DKA guideline.
Aim
This study aimed to examine trend of hospitalized DKA patients and outcomes of treatment over a decade at Theptarin Hospital, a multi-discipline based diabetes center in Thailand.
Method
A retrospective study of DKA episodes admitted over a 14-year period (2005–2018) was done. Clinical characteristics, laboratory data, type of diabetes, severity of DKA were collected and analyzed.
Results
A total of 94 DKA episodes occurred in 81 diabetic patients (females 61.5%, mean age 47.4 ± 20.4 years, T1DM 41.5%, T2DM 50.0%, Ketosis-prone diabetes 8.5%, baseline A1C 10.8 ± 3.0%). While infection was the common precipitating factor in T2DM, omission of insulin was the usual precipitating factor in T1DM. During ongoing management, 26.6% of patients developed hypokalemia and supplementation was not prescribed as per protocol in this group of patients. Almost 13% of patients experienced hypoglycemia in the first 24 h. Median time to resolution of DKA was 8.5 h. Four T2DM patients expired from the precipitating cause of DKA which accounted for mortality rate at 4.3% in our study.
Conclusions
Inadequate metabolic monitoring and iatrogenic hypoglycemia remain areas of concern for DKA management. Occurrence of hypokalemia was related to poor adherence to protocol guidance on potassium supplementation. A strengthened educational program for nursing and medical staffs should be emphasized.
Keywords: Diabetic ketoacidosis (DKA), Outcomes, Adult, Ketosis-prone diabetes mellitus (KPDM), Thailand
Introduction
Diabetic ketoacidosis (DKA) is the most serious hyperglycemic condition which could develop in any type of diabetes mellitus [1], [2]. Several epidemiological studies have reported that hospitalizations for DKA have increased worldwide in both type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) [3], [4], [5]. While inpatient mortality rates for DKA are generally very low (<5%) in most developed countries [4], [6], they are still high in developing countries from mismanagement or unaddressed precipitating factors [7], [8]. Previous studies in the last decade from Thailand reported the DKA mortality rate varied from 5 to 10% which was higher than observed mortality rates from Western countries [9], [10], [11]. Not only concomitant life-threatening illnesses of patients but also the problem in adhering to DKA guideline from treating physicians might contribute to higher mortality observed in Thai patients. Protocol for management of adult patients with DKA has been available from American Diabetes Association (ADA) and adopted worldwide since 2001. It was updated several times to improve patient safety and educational experience [12], [13], [14]. According to a previous study [6], the use of standardized written DKA guideline resulted in a mortality rate <2%, however; quality assurance standards for guideline adherence needed periodic assessment to obtain the best outcome and reduce readmission rates of DKA.
In the past two decades, an increasingly recognized new entity called ‘ketosis-prone diabetes mellitus’ (KPDM) might be an additional contributing factor in increased rate of DKA in some specific geographic locations [15], [16], [17]. This spectrum of atypical diabetes had been previously studied in Thai patients with results consistent with other studies from African-American population [18]. Most KPDM patients recovered from glucose toxicity and could be withdrawn from insulin treatment within 3–6 months after the episode of DKA. Therefore, managing acute complications such as DKA deserves more attention in aspects of diagnosis type of diabetes and long-term treatments. While studies focused on DKA trends in children were well-documented, temporal trends of DKA in adult is limited especially in Asian population. According to the recent national survey of DKA in the United Kingdom (UK), adult patients with T1DM had higher readmission rate than adults with T2DM but were more likely to be discharged within 2 days [19]. It is interesting to observe that one-third of adult patients with T1DM had at least one episode of DKA in the preceding year. Whether these differences will be observed in Asian patients is unknown. The data from the UK indicated that non-compliance to insulin treatment and infection are still two of the most common precipitating factors for DKA.
The available studies in Thailand were scarce but consistently showed inadequate metabolic monitoring and development of hypokalemia in almost half of treated patients [9], [10], [11]. Therefore, management of DKA is still an area of concern and factors-related to poor adherence to protocol guidance should be addressed to improve outcomes of DKA management. Clinical audits could lead to quality improvement and achieve desired processes and outcomes through changing healthcare provider behavior and organization strategies. This retrospective study aimed to examine secular trend of hospitalized DKA patients and outcomes of treatment over a decade at Theptarin Hospital, a multi-discipline based diabetes center in Bangkok.
Materials and methods
A 14-year (2005–2018) retrospective audit of hospitalized DKA patients at Theptarin Hospital, a specialized endocrine center in Bangkok, was performed. We included all DKA admissions for analyses. The diagnosis of DKA was verified based on standard clinical and laboratory criteria from ADA. The severity of DKA was classified as mild, moderate, or severe based on the mental status and severity of metabolic acidosis. Euglycemic DKA was defined as DKA without marked hyperglycemia (plasma glucose ≤ 250 mg/dL) and the presence of ketonemia. The diagnosis of KPDM was suspected if DKA occurred without obvious precipitating cause in newly diagnosed diabetes or unclassified type of diabetes. KPDM is one of the groups of atypical diabetes which is distinguished from typical known case of T2DM based on the occurrence of unprovoked DKA as an initial presentation of diabetes. After resolution of DKA, some patients of KPDM might be classified as T2DM later after clinical course and laboratory follow-up. The results of mixed meal tolerance test (MMTT) and pancreatic auto-antibodies were collected if available. KPDM was classified by “Aβ classification” [20] which depended on the presence or absence of pancreatic autoantibodies (A) and reserved beta cell function (β). Hypoglycamia was defined as blood glucose of < 70 mg/dL. Resolution of DKA was defined as pH > 7.3, bicarbonate > 15 mmol/L, and blood ketone level < 0.6 mmol/L. Each DKA episode was audited as a discrete event. Clinical data, precipitating factors for DKA, laboratory data on arrival, treatment details, length of hospital stays and mortality rate were collected and analyzed.
This retrospective study was approved by the Institutional Review Board of Theptarin Hospital (Certificate of Approval No. 04/2017).
Statistical analysis
Continuous variables are presented as mean (SD) and categorical variables are presented as proportions. Characteristics of patients in each type of diabetes were compared using unpaired t-test for continuous variables and Chi-square test for categorical variables. The level of significance was set at 0.05. All statistical analyses were conducted using the Statistical Package for the Social Sciences (version 22.0; SPSS, Chicago, IL, USA).
Results
Characteristics of patients and annual incidence of hospitalized DKA patients
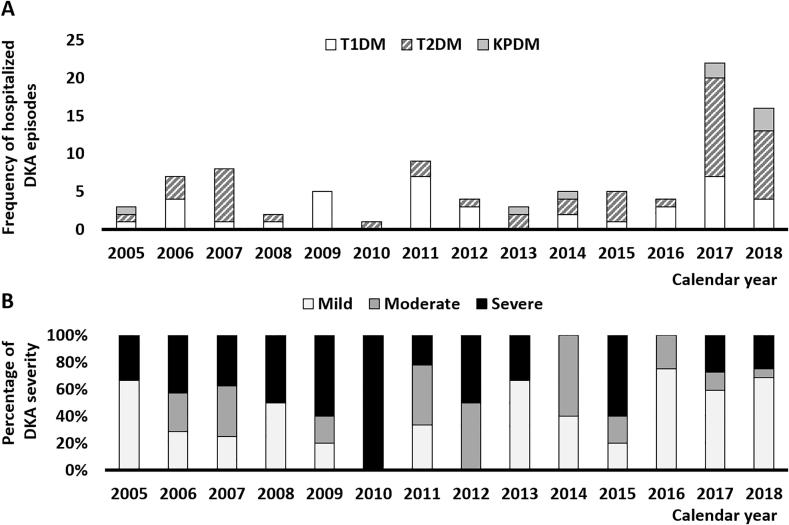
During the study period (2005–2018), there were 94 DKA episodes in 81 patients (females 61.5%, mean age 47.4 ± 20.4 years, T1DM 41.5%, T2DM 50.0%, Ketosis-prone diabetes 8.5%, baseline A1C 10.8 ± 3.0%) at Theptarin Hospital. According to criteria for severity of DKA from ADA, 45.7% of our hospitalized DKA episodes were classified as mild DKA, 22.3% as moderate DKA, and 31.9% as severe DKA. As shown in Fig. 1, hospitalization from DKA in 2005–2016 was on average 4–6 admissions per year with moderate to severe DKA in most patients. However, admissions due to mild DKA from concomitant illnesses or non-compliance to insulin treatment surged remarkably from 2017 due to the availability of point-of-care testing (POCT) of beta-hydroxybutyrate as a rapid measurement of serum ketone. Euglycemic DKA was found in 6 episodes (6.4% of admissions) from 6 patients during the past 14 years with sodium-glucose cotransporter-2 inhibitors (SGLT2i)-associated DKA was accounted in 2 patients. In patients who had recurrent DKA during study period (11.1% of all patients), recurrent DKA varied from 2 to 7 episodes. There were no any differences in type of diabetes, age, duration of diabetes, and severity of DKA when compared between patients who had only single DKA episode and patients who had recurrent DKA. Insulin withdrawal was the most common causes of recurrent DKA in both T1DM and T2DM patients.
Fig. 1.
A) Trend of hospitalization from DKA (2005–2018) divided by type of diabetes B) Trend of hospitalization from DKA (2005–2018) divided by severity of DKA.
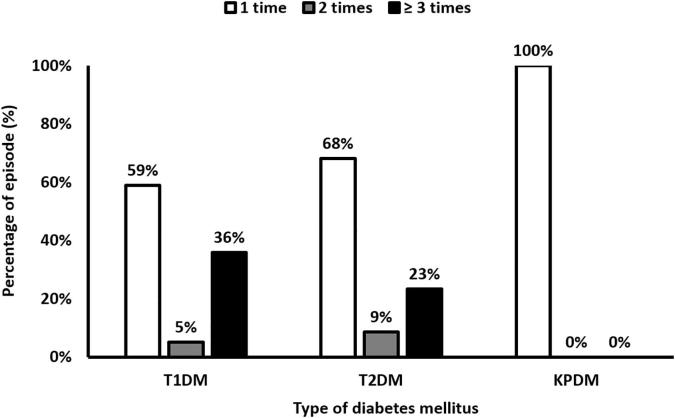
DKA was first diagnosed at emergency room in 47.9% of episodes, outpatients in 39.4% of episodes, and others in 12.7% of episodes. It is noteworthy that 5.3% of hospitalized DKA was initially misdiagnosed as uncomplicated hyperglycemia and admitted to general ward before transferring to ICU later. The details of clinical characteristics and laboratory data on arrival were summarized according to the type of diabetes in Table 1. While omission of insulin was the most common precipitating factor of DKA in T1DM (59.0% of DKA episodes), sepsis was the most common precipitating factor of DKA in T2DM (57.4% of DKA episodes). The three most common sites of infection leading to sepsis are gastrointestinal infections (40%), urinary tract infections (22%), and pulmonary infections (15%). Frequency of DKA episode in each type of diabetes was showed in Fig. 2. There were 8 episodes which DKA and hyperosmolar hyperglycemic state (HHS) co-existed during the same episode (7 patients with T2DM and 1 patient with T1DM). No mortality case was found in these patients who developed co-occurrence of DKA and HHS.
Table 1.
Details of clinical characteristics, laboratory data in studied DKA episodes.
| Total DKA (N = 94) | Type 1 DM (N = 39) | Type 2 DM (N = 47) | KPDM (N = 8) | p-value | |
|---|---|---|---|---|---|
| Age (years) | 47.4 ± 20.4 | 32.6 ± 16.0 | 61.3 ± 14.6 | 37.6 ± 10.6 | <0.001 |
| %Female | 53 (56%) | 31 (79%) | 18 (38%) | 4 (50%) | 0.001 |
| Duration of DM (years) | 11.6 ± 10.2 | 10.0 ± 8.9 | 15.0 ± 10.5 | 0.6 ± 1.2 | <0.001 |
| BMI (kg/m2) | 22.9 ± 3.9 | 22.1 ± 3.9 | 23.2 ± 3.6 | 25.4 ± 4.8 | 0.078 |
| Length of stay (days)* | 3 (2–5) | 3 (2–3) | 4 (2–7) | 3 (2–5) | 0.021 |
| Plasma glucose (mg/dL) | 511 ± 200 | 481 ± 184 | 540 ± 215 | 485 ± 176 | 0.366 |
| A1C (%NGSP) | 10.8 ± 3.1 | 10.9 ± 3.1 | 10.7 ± 3.2 | 10.6 ± 2.8 | 0.954 |
| Plasma HCO3 (mEq/L) | 14.3 ± 6.1 | 13.3 ± 6.1 | 14.4 ± 6.1 | 18.1 ± 4.6 | 0.118 |
| Serum ketone (mmol/L) | 4.1 ± 2.4 | 4.3 ± 1.5 | 4.1 ± 3.2 | 3.5 ± 2.0 | 0.756 |
| Precipitating factors* | |||||
| -Infection | 31 (33%) | 4 (10%) | 27 (57%) | 0 (0%) | <0.001 |
| -Insulin omission | 34 (35%) | 23 (59%) | 11 (23%) | 0 (0%) | |
| -Drug-induced | 3 (5%) | 1 (3%) | 2 (4%) | 0 (0%) | |
| -Newly diagnosed | 21 (22%) | 6 (15%) | 7 (15%) | 8 (100%) | |
| -Others | 5 (5%) | 5 (13%) | 0 (0%) | 0 (0%) | |
| Time to DKA resolution (hours)** | 8.5 (6–15) | 9.0 (7–16) | 8.5 (5–16) | 8.5 (6–15) | 0.403 |
*Data were presented with median and IQR in parenthesis.
Fig. 2.
Frequency of DKA episode in each type of diabetes during study period (2005–2018).
Treatment details in management of DKA
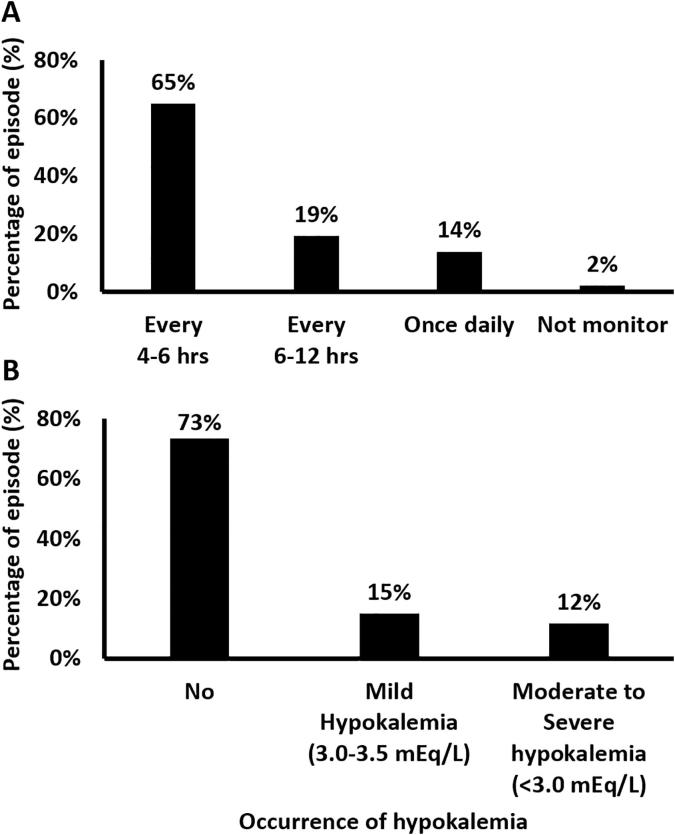
After admission, 54.2% of DKA episodes were treated by endocrinologists and 45.8% were treated by general internists or on-call physicians. During ongoing management, 26.6% of patients developed hypokalemia and supplementation was not prescribed as per protocol in those patients. Adequate electrolyte monitoring at the interval of 4–6 h was documented in 64.9% of all DKA episodes. When analyzed the occurrence of hypokalemia according to treating physicians, the rate of hypokalemia were not different between endocrinologists and general internists (27.4% versus 25.6%, p-value 0.324). The details of the occurrence of hypokalemia after DKA treatments were showed in Fig. 3. The severity of hypokalemia ranged from 2.3 to 3.5 mEq/L. No patients were dead from hypokalemia. Almost 13% of patients experienced hypoglycemia in the first 24 h. Subcutaneous insulin treatments were given in 14.9% of episodes which mild DKA episodes were a majority of patients who had been treated with this route of insulin. However, 3 of 30 severe DKA patients received subcutaneous treatment of insulin inappropriately and then resulted in rebound hypoglycemia within 24 h of treatments. Intravenous bicarbonate was prescribed in only 2 patients during DKA episodes due to severe acidosis from sepsis. None of the patient received intravenous phosphate during management of DKA. Median time to resolution of DKA was 8.5 h.
Fig. 3.
A) Process of cares and B) Outcomes in electrolytes monitoring during management of DKA episodes.
Outcomes of DKA treatments
Median length of stay was 3 days and 76.3% of patients were discharge within 5 days after admission. Four T2DM patients expired from the precipitating cause of DKA (3 cases with sepsis and 1 case with extensive myocardial infarction) which accounted for mortality rate at 4.3% in our study. No death due to complications from DKA management was found. After discharge, only 48% of patients were still in regular follow-up at the end of 2018 and 20% of hospitalized DKA patients were lost to follow-up immediately after discharge. All KPDM patients (N = 8) were classified as A-β + Ketosis-prone diabetes according to results of MMTT and pancreatic auto-antibodies after resolution of DKA. Insulin treatment could be stopped successfully in all cases of KPDM within 3 months after discharge.
Discussions
The number of patients presented with DKA to hospital has been rising steadily in the US and many countries [21], [22]. The reason for these rising trends might come from early identification of DKA by using rapid plasma ketone measurement and also emerging entities such as KPDM, drug-associated DKA, etc [23]. Our study highlights the importance of prompt diagnosis and urgent multifaceted DKA treatment to avoid the risk of fatal outcome. Inadequate metabolic monitoring and iatrogenic hypoglycemia remain areas of concern for DKA management. Occurrence of hypokalemia was related to poor adherence to protocol guidance on potassium supplementation. A strengthened educational program for medical staffs should focus on metabolic monitoring and improved patient contact after discharge from the hospital. Our results also present changes in the severity of DKA toward mild DKA after the introduction of POCT ketone testing and increased a high index of suspicion for DKA in patients at risk. Therefore, local DKA guideline needs to adapt and evolve in response to the heterogeneity of DKA patients. The next challenge is to implement this guideline consistently and periodally update guideline with structured order sets to improve quality of DKA treatment. Endocrinologists and/or internists who experienced in DKA management should be involved and regular review outcomes of treatments in each DKA episodes in order to improve the current status of DKA outcomes.
Managing DKA deserves more attention from general physicians and diabetes specialist teams. Despite the advancement in diabetes treatments and technology in the last decade, the mortality rate from DKA remained relatively high at about 5% in Thailand [9], [10], [11]. There are two accepted international DKA guideline from the US [14] and the UK [24]. While ADA recommended a classification of severity of DKA and advocated that mild DKA could be treated with subcutaneous rapid-acting insulin analogs treatment and may not be necessary to hospitalization, the UK DKA guideline focused on the presence of ketonemia in the setting of patients with diabetes as a requirement diagnosis of DKA [25]. Based on our previous experiences and the result of this retrospective study, both the US and the UK guidelines should be adapted and incorporated into the current changing trends toward mild DKA cases. In the era of widespread uses of SGLT2i from proven cardiovascular benefits, bedside ketone testings are required to make a diagnosis of euglycemic DKA and those selected patients might be treated and discharged from the emergency room [26], [27], [28]. Differences in healthcare systems play a vital role in choosing the US, the UK, or adapted versions of both guidelines to be implemented in each hospital. Timely review of key metabolic parameters such as volume status, intravenous insulin therapy, electrolyte and glucose monitoring are the universal multifaceted DKA treatment in every guideline. However, audited data always highlight some differences on treatment protocols in each physician so periodic evaluation should be implemented to assess adherence to DKA guideline [29], [30].
The recognition of KPDM underscores the importance of accurate diagnosis and classification of these patients utilizing the Aβ scheme (‘A’ for autoantibody status and ‘ß’ for beta cell functional reserve) as revealed in the minority of newly diagnosed patients who presented with DKA as their first presentation of diabetes [31]. Accurate classification is necessary to guide clinicians whether KPDM patients need to continue lifelong insulin treatment. Future longitudinal studies should focus on this atypical diabetes which could explain the increased rate of DKA hospitalization worldwide. Most DKA readmission especially in KPDM patients are preventable through implementing structured educational programs emphasizing the importance of treatment adherence and improving sick day management [32], [33]. From our study, recurrent DKA episodes which occurred in both T1DM and T2DM patients accounted for 20% of hospitalizations during the study period. Intervention strategies targeting these patients should be developed to prevent recurrent admission from DKA.
In light of trend toward greater cases of mild DKA, there might be increased opportunity to treat some DKA cases in the emergency room or short-term observation ward with subcutaneous insulin treatment [34], [35], [36], [37]. Further prospective studies are warranted for the feasibility and safety of this novel treatment in the setting of Asian patients. We acknowledged that our study had several important limitations from the inherent nature of retrospective study from a single tertiary diabetes center. However, the present findings of this study highlight the need for ongoing quality improvement for DKA management especially timely glucose and metabolic derangement monitoring during DKA treatment. Many physicians and nurses might not be familiar with DKA in adult patients. Therefore, written or computerized up-to-date protocol that involved all stakeholders in treatment of DKA should be available in every hospital. In-hospital education with a multi-disciplinary diabetes care team should be provided for all patients to avoid recurrent DKA. Further research is necessary to alleviate an upward trend of DKA globally. A unifying diagnostic and treatment protocol for DKA should be developed to guide physicians for successful DKA management.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Acknowledgments
Acknowledgments
The authors wish to thank Dr. Tinapa Himathongkam for her English editing and the staffs of Theptarin Hospital for all their supports and helps. Parts of this manuscript had previously been presented as a poster at the 19th ASEAN Federation of Endocrine Societies Congress (AFES) meeting, Yangon, Myanmar, 9–12 November 2017.
Funding
No source of funding was applied in this retrospective study.
Authors’ contributions
TY, PP, and CP performed the data collection, statistical analyses, interpreted the data and drafted the manuscript. CA, NS, WE, and KS contributed to interpretation of the data and revised the manuscript critically before submission. KS and HT made substantial contributions to the discussion of results. All authors read and approved the final manuscript.
Consent for publication
Not applicable.
Ethical approval and consent to participant
This retrospective study is approved by the Ethics board committee of Theptarin Hospital (No.04/2017). No inform consent to participant was required as a retrospective study.
References
- 1.Umpierrez G., Korytkowski M. Diabetic emergencies-ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endocrinol. 2016;12:222–232. doi: 10.1038/nrendo.2016.15. [DOI] [PubMed] [Google Scholar]
- 2.Nyenwe E.A., Kitabchi A.E. The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management. Metabolism. 2016;65:507–521. doi: 10.1016/j.metabol.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Zhong V.W., Juhaeri J., Mayer-Davis E.J. Trends in hospital admission for diabetic ketoacidosis in adults with type 1 and type 2 diabetes in England, 1998–2013: a retrospective cohort study. Diabetes Care. 2018;41:1870–1877. doi: 10.2337/dc17-1583. [DOI] [PubMed] [Google Scholar]
- 4.Benoit S.R., Zhang Y., Geiss L.S., Gregg E.W., Albright A. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality - United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2018;67:362–365. doi: 10.15585/mmwr.mm6712a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ko S.H., Lee W.Y., Lee J.H., Kwon H.S., Lee J.M., Kim S.R. Clinical characteristics of diabetic ketoacidosis in Korea over the past two decades. Diabet Med. 2005;22:466–469. doi: 10.1111/j.1464-5491.2005.01450.x. [DOI] [PubMed] [Google Scholar]
- 6.Kitabchi A.E., Umpierrez G.E., Fisher J.N., Murphy M.B., Stentz F.B. Thirty years of personal experience in hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. J Clin Endocrinol Metab. 2008;93:1541–1552. doi: 10.1210/jc.2007-2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jabbar A., Farooqui K., Habib A., Islam N., Haque N., Akhter J. Clinical characteristics and outcomes of diabetic ketoacidosis in Pakistani adults with Type 2 diabetes mellitus. Diabet Med. 2004;21:920–923. doi: 10.1111/j.1464-5491.2004.01249.x. [DOI] [PubMed] [Google Scholar]
- 8.Basavanthappa S.P., Pejaver R., Raghavendra K., Srinivasa V., Suresh Babu M.T. Clinical profile and outcome of diabetic ketoacidosis in a tertiary care hospital in South India. Int J Contemp Pediatr. 2015;2:29–31. [Google Scholar]
- 9.Thewjitcharoen Y., Sunthornyothin S. Clinical characteristics of diabetic ketoacidosis in newly diagnosed adult patients. Diabetes Res Clin Prac. 2010;90:e43–e45. doi: 10.1016/j.diabres.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Anthanont P., Khawcharoenporn T., Tharavanij T. Incidences and outcomes of hyperglycemic crises: a 5-year study in a tertiary care center in Thailand. J Med Assoc Thai. 2012;95:995–1002. [PubMed] [Google Scholar]
- 11.Vijara V., Polamuang W. Hyperglycemic Crisis in Prapokklao Hospital. J Prapokklao Hosp Clin Med Educat Center. 2013;30:133–145. [Google Scholar]
- 12.American Diabetes Association Hyperglycemic crises in patients with diabetes mellitus. Diabetes Care. 2001;24:154–161. doi: 10.2337/diacare.24.1.154. [DOI] [PubMed] [Google Scholar]
- 13.Kitabchi A.E., Umpierrez G.E., Murphy M.B., Kreisberg R.A. Hyperglycemic crises in adult patients with diabetes: a consensus statement. Diabetes Care. 2006;29:2739–2748. doi: 10.2337/dc06-9916. [DOI] [PubMed] [Google Scholar]
- 14.Kitabchi A.E., Umpierrez G.E., Miles J.M., Fisher J.N. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32:1335–1343. doi: 10.2337/dc09-9032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banerji M.A., Chaiken R.L., Huey H., Tuomi T., Norin A.J., Mackay I.R. GAD antibody negative NIDDM in adult black subjects with diabetic ketoacidosis and increased frequency of human leukocyte antigen DR3 and DR4. Flatbush diabetes. Diabetes. 1994;43:741–745. doi: 10.2337/diab.43.6.741. [DOI] [PubMed] [Google Scholar]
- 16.Umpierrez G.E., Casals M.M., Gebhart S.P., Mixon P.S., Clark W.S., Phillips L.S. Diabetic ketoacidosis in obese African-Americans. Diabetes. 1995;44:790–795. doi: 10.2337/diab.44.7.790. [DOI] [PubMed] [Google Scholar]
- 17.Balasubramanyam A., Nalini R., Hampe C.S., Maldonado M. Syndrome of ketosis-prone diabetes mellitus. Endocr Rev. 2008;29:292–302. doi: 10.1210/er.2007-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thewjitcharoen Y., Sunthornyothin S. Clinical Characteristics and Long term Follow up of Ketosis prone Diabetes in Thai Patients. Exp Clin Endocrinol Diabetes. 2014;122:303–307. doi: 10.1055/s-0034-1371812. [DOI] [PubMed] [Google Scholar]
- 19.Crasto W., Htike Z.Z., Turner L., Higgins K. Management of diabetic ketoacidosis following implementation of the JBDS guidelines: Where are we and where should we go? Br J Diabetes Vasc Dis. 2015;15:11–16. [Google Scholar]
- 20.Maldonado M., Hampe C.S., Gaur L.K., D'Amico S., Iyer D., Hammerle L.P. Ketosis-prone diabetes: dissection of a heterogeneous syndrome using an immunogenetic and beta-cell functional classifi cation, prospective analysis, and clinical outcomes. J Clin Endocrinol Metab. 2003;88:5090–5098. doi: 10.1210/jc.2003-030180. [DOI] [PubMed] [Google Scholar]
- 21.Desai D., Mehta D., Mathias P., Menon G., Schubart U.K. Health Care Utilization and Burden of Diabetic Ketoacidosis in the U.S. Over the Past Decade: A Nationwide Analysis. Diabetes Care. 2018;41:1631–1638. doi: 10.2337/dc17-1379. [DOI] [PubMed] [Google Scholar]
- 22.Xu Y., Bai J., Wang G., Zhong S., Su X., Huang Z. Clinical profile of diabetic ketoacidosis in tertiary hospitals in China: a multicentre, clinic-based study. Diabet Med. 2016;33:261–268. doi: 10.1111/dme.12820. [DOI] [PubMed] [Google Scholar]
- 23.Vellanki P., Umpierrez G.E. Increasing Hospitalizations for DKA: A Need for Prevention Programs. Diabetes Care. 2018;41:1839–1841. doi: 10.2337/dci18-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Savage M.W., Dhatariya K.K., Kilvert A., Rayman G., Rees J.A., Courtney C.H. Joint British Diabetes Societies guideline for the management of diabetic ketoacidosis. Diabetic Med. 2011;28:508–515. doi: 10.1111/j.1464-5491.2011.03246.x. [DOI] [PubMed] [Google Scholar]
- 25.Dhatariya K., Vellanki P. Treatment of Diabetic Ketoacidosis (DKA)/Hyperglycemic Hyperosmolar State (HHS): Novel Advances in the Management of Hyperglycemic Crises (UK Versus USA) Curr Diab Rep. 2017;17:33. doi: 10.1007/s11892-017-0857-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhatariya K. Blood ketones—measurement, interpretation, limitations and utility in the management of diabetic ketoacidosis. Rev Diabet Stud 2016 Winter;13:217–25. [DOI] [PMC free article] [PubMed]
- 27.Thewjitcharoen Y., Wanothayaroj E., Tammawiwat C., Malidaeng A., Yenseung N., Nakasatien S. A single center retrospective analysis of SGLT2i-associated diabetic ketoacidosis in Bangkok: The role of point-of-care blood ketone testing. J Clin Transl Endocrinol Case Rep. 2018;10:8–10. [Google Scholar]
- 28.Jeon JY, Kim SK, Kim KS, Song SO, Yun JS, Kim BY, et al. Clinical characteristics of diabetic ketoacidosis in users and non-users of SGLT2 inhibitors. Diabetes Metab 2019 Jan 9. pii: S1262-3636(19)30001-1. [Epub ahead of print]. [DOI] [PubMed]
- 29.Dhatariya K.K., Nunney I., Higgins K., Sampson M.J., Iceton G. A national survey of the management of diabetic ketoacidosis in the UK in 2014. Diabetic Med. 2016;33:252–260. doi: 10.1111/dme.12875. [DOI] [PubMed] [Google Scholar]
- 30.Wong B., Cheng A., Yu C., Goguen J. Examining the “Killer K” of Diabetic Ketoacidosis at a Tertiary Care Hospital: An Exploratory Study. Can J Diabetes. 2016;40:204–209. doi: 10.1016/j.jcjd.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 31.Gaba R., Mehta P., Balasubramanyam A. Evaluation and management of ketosis-prone diabetes. Expert Rev Endocrinol Metab. 2019;14:43–48. doi: 10.1080/17446651.2019.1561270. [DOI] [PubMed] [Google Scholar]
- 32.Randall L., Begovic J., Hudson M., Smiley D., Peng L., Pitre N. Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Diabetes Care. 2011;34:1891–1896. doi: 10.2337/dc11-0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mays J.A., Jackson K.L., Derby T.A., Behrens J.J., Goel S., Molitch M.E. An evaluation of recurrent diabetic ketoacidosis, fragmentation of care, and mortality across Chicago, Illinois. Diabetes Care. 2016;39:1671–1676. doi: 10.2337/dc16-0668. [DOI] [PubMed] [Google Scholar]
- 34.Andrade-Castellanos C.A., Colunga-Lozano L.E., Delgado-Figueroa N., Gonzalez-Padilla D.A. Subcutaneous rapid-acting insulin analogues for diabetic ketoacidosis. Cochrane Database Syst Rev. 2016;1:CD011281. doi: 10.1002/14651858.CD011281.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ullal J., McFarland R., Bachand M., Aloi J. Use of a Computer-Based Insulin Infusion Algorithm to Treat Diabetic Ketoacidosis in the Emergency Department. Diabetes Technol Ther. 2016;18:100–103. doi: 10.1089/dia.2015.0215. [DOI] [PubMed] [Google Scholar]
- 36.Fernando S.M., Bagshaw S.M., Rochwerg B., McIsaac D.I., Thavorn K., Forster A.J. Comparison of outcomes and costs between adult diabetic ketoacidosis patients admitted to the ICU and step-down unit. J Crit Care. 2018;50:257–261. doi: 10.1016/j.jcrc.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 37.Mohamed M, Assal A, Boyle L, Kwok E, DeSousa F, Karovitch A, Malcolm J. Development and Implementation of a Diabetic Ketoacidosis Protocol for Adults With Type 1 and Type 2 Diabetes at a Tertiary Care Multicampus Hospital. Can J Diabetes 2018 Aug 16. pii: S1499-2671(18)30108-4. [Epub ahead of print]. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.