Abstract
Background
Having nurses take on tasks that are typically conducted by doctors (doctor‐nurse substitution, a form of 'task‐shifting') may help to address doctor shortages and reduce doctors' workload and human resource costs. A Cochrane Review of effectiveness studies suggested that nurse‐led care probably leads to similar healthcare outcomes as care delivered by doctors. This finding highlights the need to explore the factors that affect the implementation of strategies to substitute doctors with nurses in primary care. In our qualitative evidence synthesis (QES), we focused on studies of nurses taking on tasks that are typically conducted by doctors working in primary care, including substituting doctors with nurses or expanding nurses' roles.
Objectives
(1) To identify factors influencing implementation of interventions to substitute doctors with nurses in primary care. (2) To explore how our synthesis findings related to, and helped to explain, the findings of the Cochrane intervention review of the effectiveness of substituting doctors with nurses. (3) To identify hypotheses for subgroup analyses for future updates of the Cochrane intervention review.
Search methods
We searched CINAHL and PubMed, contacted experts in the field, scanned the reference lists of relevant studies and conducted forward citation searches for key articles in the Social Science Citation Index and Science Citation Index databases, and 'related article' searches in PubMed.
Selection criteria
We constructed a maximum variation sample (exploring variables such as country level of development, aspects of care covered and the types of participants) from studies that had collected and analysed qualitative data related to the factors influencing implementation of doctor‐nurse substitution and the expansion of nurses' tasks in community or primary care worldwide. We included perspectives of doctors, nurses, patients and their families/carers, policymakers, programme managers, other health workers and any others directly involved in or affected by the substitution. We excluded studies that collected data using qualitative methods but did not analyse the data qualitatively.
Data collection and analysis
We identified factors influencing implementation of doctor‐nurse substitution strategies using a framework thematic synthesis approach. Two review authors independently assessed the methodological strengths and limitations of included studies using a modified Critical Appraisal Skills Programme (CASP) tool. We assessed confidence in the evidence for the QES findings using the GRADE‐CERQual approach. We integrated our findings with the evidence from the effectiveness review of doctor‐nurse substitution using a matrix model. Finally, we identified hypotheses for subgroup analyses for updates of the review of effectiveness.
Main results
We included 66 studies (69 papers), 11 from low‐ or middle‐income countries and 55 from high‐income countries. These studies found several factors that appeared to influence the implementation of doctor‐nurse substitution strategies. The following factors were based on findings that we assessed as moderate or high confidence.
Patients in many studies knew little about nurses' roles and the difference between nurse‐led and doctor‐led care. They also had mixed views about the type of tasks that nurses should deliver. They preferred doctors when the tasks were more 'medical' but accepted nurses for preventive care and follow‐ups. Doctors in most studies also preferred that nurses performed only 'non‐medical' tasks. Nurses were comfortable with, and believed they were competent to deliver a wide range of tasks, but particularly emphasised tasks that were more health promotive/preventive in nature.
Patients in most studies thought that nurses were more easily accessible than doctors. Doctors and nurses also saw nurse‐doctor substitution and collaboration as a way of increasing people's access to care, and improving the quality and continuity of care.
Nurses thought that close doctor‐nurse relationships and doctor's trust in and acceptance of nurses was important for shaping their roles. But nurses working alone sometimes found it difficult to communicate with doctors.
Nurses felt they had gained new skills when taking on new tasks. But nurses wanted more and better training. They thought this would increase their skills, job satisfaction and motivation, and would make them more independent.
Nurses taking on doctors' tasks saw this as an opportunity to develop personally, to gain more respect and to improve the quality of care they could offer to patients. Better working conditions and financial incentives also motivated nurses to take on new tasks. Doctors valued collaborating with nurses when this reduced their own workload.
Doctors and nurses pointed to the importance of having access to resources, such as enough staff, equipment and supplies; good referral systems; experienced leaders; clear roles; and adequate training and supervision. But they often had problems with these issues. They also pointed to the huge number of documents they needed to complete when tasks were moved from doctors to nurses.
Authors' conclusions
Patients, doctors and nurses may accept the use of nurses to deliver services that are usually delivered by doctors. But this is likely to depend on the type of services. Nurses taking on extra tasks want respect and collaboration from doctors; as well as proper resources; good referral systems; experienced leaders; clear roles; and adequate incentives, training and supervision. However, these needs are not always met.
Plain language summary
What factors influence implementation of doctor‐nurse substitution strategies in primary care?
What was the aim of the review?
In this Cochrane Review of qualitative studies ('qualitative evidence synthesis'), we explored peoples' views and experiences of moving tasks from doctors to nurses in primary healthcare. We collected relevant studies on this topic and included 66 studies (69 papers).
This synthesis links to another Cochrane Review that assesses the effectiveness of moving tasks from doctors to nurses in primary care.
Key messages
Patients, doctors and nurses may accept the use of nurses to deliver services that are usually delivered by doctors. But this is likely to depend on the type of services. Nurses taking on extra tasks want respect and collaboration from doctors; proper resources; good referral systems; experienced leaders; clear roles; and adequate incentives, training and supervision. However, these needs are not always met.
What was studied in the review?
Many people do not get the healthcare they need because of a lack of healthcare workers where they live. Governments across the world are trying different solutions to address this problem. One possible solution is to move tasks from more‐specialised to less‐specialised health workers, for instance, moving certain tasks from doctors to nurses.
In this review, we looked for studies that explored how patients, nurses, doctors and others viewed and experienced these solutions, and what could influence their success.
What were the main results of the review?
We included 66 studies (69 papers) in our review, 11 from low‐ or middle‐income countries and 55 from high‐income countries. These studies found a number of factors that appear to influence the implementation of doctor‐nurse substitution strategies. The following factors are based on findings that we assessed as moderate or high confidence:
Patients in many studies knew little about nurses' roles and the difference between nurse‐led and doctor‐led care. They also had mixed views about the type of tasks that nurses should deliver. They preferred doctors when the tasks were more 'medical' but accepted nurses for preventive care and follow‐ups. Doctors in most studies also preferred that nurses performed only 'non‐medical' tasks. Nurses were comfortable with, and believed they were competent to deliver, a wide range of tasks, but particularly emphasised tasks that were more health promotive/preventive in nature.
Patients in most studies thought that nurses were more easily accessible than doctors. Doctors and nurses also saw nurse‐doctor substitution and collaboration as a way of increasing people's access to care, and improving the quality and continuity of care.
Nurses thought that close doctor‐nurse relationships and doctor's trust in and acceptance of nurses was important for shaping their roles. But nurses working alone sometimes found it difficult to communicate with doctors.
Nurses felt they had gained new skills when taking on new tasks. But nurses wanted more and better training. They thought this would increase their skills, job satisfaction and motivation, and would make them more independent.
Nurses taking on doctors' tasks saw this as an opportunity to develop personally, to gain more respect and to improve the quality of care they could offer to patients. Better working conditions and financial incentives also motivated nurses to take on new tasks. Doctors valued collaborating with nurses when this reduced their own workload.
Doctors and nurses pointed to the importance of having access to resources, such as enough staff, equipment and supplies; good referral systems; experienced leaders; clear roles; and adequate training and supervision. But they often had problems with these issues. They also pointed to the huge number of documents they needed to complete when tasks were moved from doctors to nurses.
How up‐to‐date was this review?
We searched for studies published before 28 June 2018.
Summary of findings
Summary of findings for the main comparison. Summary of qualitative findings.
| Summary of review finding | Studies contributing to the review finding | CERQual assessment of confidence in the evidence | Explanation of CERQual assessment |
| Type of task | |||
| Recipients of care had mixed views about the expansion of tasks undertaken by nurses. They preferred doctors when the tasks were more 'medical' in nature and they accepted nurses for preventive care and follow‐ups. | Bennett 2013; Boyle 2016; Branson 2008; Cheek 2002; Clendon 2001; Clendon 2003; Coker 2009; Courtenay 2010; Flowers 2008; Leipert 2011; Perry 2005; Rosemann 2006 | Moderate confidence | Due to minor concerns about methodological limitations and moderate concerns about relevance. |
| Doctors in most studies also preferred that nurses performed only non‐medical tasks. | Abbott 2013; Bailey 2006; Branson 2008; Coulter 2000; Georgeu 2012; Ivers 2011; Kraus 2017; Lindblad 2010; Lorch 2015; Marsden 2004; Rosemann 2006; Ross 2015; Stenner 2010; Stephen 2018; Twinn 1999; Voogdt‐Pruis 2011 | Moderate confidence | Due to minor concerns about methodological limitations and relevance; and moderate concerns about coherence |
| Nurses were comfortable with, and believed they were competent to deliver, a wide range of tasks, but particularly emphasised tasks that were more health promotive/preventive in nature. | Abbott 2013; Albers‐Heitner 2011; Bailey 2006; Carryer 2017; Dennis 2016; Francis 2013; Georgeu 2012; Hamel 2017; Hart 2012; Kraus 2017; Lindblad 2010; Peterson 2007; Stephen 2018 | Moderate confidence | Due to minor concerns about methodological limitations, adequacy and relevance |
| Accessibility and quality of care | |||
| Recipients in most studies believed that nurses were more easily accessible than doctors. | Basaleem 2009; Cheek 2002; Coker 2009; Fortin 2010; Georgeu 2012; Leipert 2011; Marsden 2004; Perry 2005; Ross 2015; Stenner 2011 | High confidence | — |
| Both doctors and nurses saw doctor‐nurse substitution and collaborative practice as a way of increasing quick access to care for certain tasks such as maternity care and prescriptions. | Kaasalainen 2013; Ljungbeck 2017; Lovink 2018; Perry 2005; Peterson 2007; Poghosyan 2017 | Moderate confidence | Due to minor concerns about methodological limitations and relevance; and moderate concerns about adequacy |
| Recipients of care in most studies were satisfied with nurses' social skills. Recipients' perceptions of nurses' technical skills were mixed. | Bennett 2013; Boyle 2016; Branson 2008; Coker 2009; Corneli 2008; Dennis 2016; Duane 2015; Fortin 2010; Friman 2011; Hart 2012; Leech 2007; Leipert 2011; Parfitt 2007; Peterson 2007; Ross 2015; Stenner 2011; Stephen 2018 | Very low confidence | Due to minor concerns about methodological limitations; and serious concerns about coherence |
| Health professionals, including doctors, nurses, policymakers and other healthcare providers, believed that doctor‐nurse substitution led to improvements in the quality of care. | Abbott 2013; Boyle 2016; Carryer 2017; Coulter 2000; Dierick‐van Daele 2010a; Kaasalainen 2013; Leipert 2011; Ljungbeck 2017; Lorch 2015; Marsden 2004; Nkhata 2016; Perry 2005; Rustagi 2015a; Stenner 2010 | Moderate confidence | Due to minor concerns about methodological limitations and coherence |
| Doctor‐nurse communication | |||
| A close doctor‐nurse relationship characterised by trust and mutual respect helped nurses to expand and develop their roles. | Burns 2009b; Francis 2013; Georgeu 2012; Hamel 2017; Lovink 2018; Mills 2008a; Peterson 2007; Poghosyan 2017; Schadewaldt 2016; Vetter‐Smith 2012; Voogdt‐Pruis 2011 | Moderate confidence | Due to moderate concerns about methodological limitations and minor concerns about relevance |
| Nurses might find it difficult to communicate effectively with colleagues in stand‐alone practices or vertical programmes of care. | Basaleem 2011; Broyles 2012; Flowers 2008; Rustagi 2015a; Walker 2015 | Moderate confidence | Due to moderate concerns about methodological limitations; and minor concerns about relevance and adequacy |
| Doctors' trust in and acceptance of nurses was a critical factor that shaped the extent of nursing practice. | Abbott 2013; Bailey 2006; Burns 2009b; Coulter 2000; Dennis 2016; Duane 2015; Francis 2013; Friman 2011; Georgeu 2012; Hamel 2017; James 2003; Kraus 2017; Leech 2007; Lindblad 2010; Mabelane 2016; Mills 2008a; Ross 2015; Stenner 2010 | Moderate confidence | Due to minor concerns about methodological limitations; and minor concerns about relevance |
| Financial issues might damage the relationship between doctors and nurses. | Coulter 2000; Lovink 2018; Mills 2008a; Peterson 2007; Poghosyan 2017; Ross 2015; Schadewaldt 2016 | Moderate confidence | Due to minor concerns about methodological limitations, coherence and adequacy; and moderate concern about relevance |
| Educational and training system | |||
| Nurses felt they had gained additional skills through task‐shifting. However, they believed that further training and education could increase their skills, job satisfaction and motivation; allow them to work more independently; and increase others' acceptance of their professional roles. | Albers‐Heitner 2011; Burns 2009b; Courtenay 2010; Dennis 2016; Duane 2015; Francis 2013; Friman 2011; Furin 2011; Hart 2012; Ivers 2011; Kassean 2005; Lindblad 2010; Maddox 2016; Mills 2008a; Mills 2008b; Mkhabela 2008; Rustagi 2015a; Stenner 2010; Stenner 2011 | Moderate confidence | Due to minor concerns about methodological limitations and relevance |
| Nurses had concerns about their training in terms of adequacy, equity and quality. | Broyles 2012; Drew 2002; Drew 2003; Francis 2013; Georgeu 2012; Hart 2012; Mabelane 2016; Maddox 2016; McKenna 2015; Nkhata 2016 | Moderate confidence | Due to minor concerns about methodological limitations and relevance |
| Awareness and understanding of the strategy | |||
| Recipients of care in many studies had limited knowledge about nurses' roles in primary care, nurse models of care, and any differences between nurse‐led and doctor‐led care. | Basaleem 2009; Branson 2008; Cheek 2002; Clendon 2001; Halcomb 2013; Leipert 2011; Lovink 2018 | Moderate confidence | Due to moderate concerns about relevance and methodological limitations |
| Continuity of care | |||
| Doctors in some studies felt that doctor‐nurse substitution improved the continuity of care and believed that recipients of care would prefer to see the same nurse rather than different doctors. | Marsden 2004; Ross 2015 | Moderate confidence | Due to moderate concerns about adequacy and relevance |
| Recipients of care in some studies were concerned over the continuity of care provided by nurses and felt insecure if they lost contact with their doctors. | Branson 2008; Fortin 2010; Georgeu 2012; Stephen 2018 | Low confidence | Due to minor concerns about methodological limitations, and moderate concerns about relevance and adequacy |
| Motivation and incentives | |||
| Internal motivators most frequently cited by nurses regarding task‐shifting were psychological (including personal development and being respected) and professional (improving the quality of care). | Albers‐Heitner 2011; Burns 2009b; Coulter 2000; Drew 2002; Drew 2003; Friman 2011; Furin 2011; Georgeu 2012; Hamel 2017; James 2003; Ljungbeck 2017; Petrova 2015; Ross 2015 | High confidence | — |
| Nurses believed that external motivators such as improved working conditions and financial incentives could act as an incentive to take on more responsibilities. | Flowers 2008; Francis 2013; Furin 2011; Hamel 2017; Hart 2012; Ljungbeck 2017; McKenna 2015; Mills 2008a; Nkhata 2016 | Moderate confidence | Due to moderate concerns about methodological limitations and minor concerns about relevance |
| Doctors valued the contribution of nurses in collaborative practices when this reduced their own workload. | Coulter 2000; Dierick‐van Daele 2010a; Drew 2002; Drew 2003; Georgeu 2012; Hamel 2017; Kaasalainen 2013; Ljungbeck 2017; Lorch 2015; Lovink 2018; Marsden 2004; Peterson 2007; Stenner 2010 | Moderate confidence | Due to minor concerns about methodological limitations and relevance; and moderate concerns about relevance and coherence |
| In settings where a proportion of doctors' revenues came from fee‐for‐service payments, doctors expressed negative reactions towards doctor‐nurse substitution. | Coulter 2000; Lorch 2015; Peterson 2007 | Low confidence | Due to minor concerns about methodological limitations; moderate concerns about adequacy and serious concerns about relevance |
| Resources (financial, infrastructures, facilities, and drugs and equipment) | |||
| A shortage of resources, including human resources, equipment and supplies, and lack of equity in how organisational resources were allocated, sometimes negatively impacted on the effective implementation of doctor‐nurse substitution strategies. | Abbott 2013; Basaleem 2009; Basaleem 2011; Coker 2009; Flowers 2008; Friman 2011; Leech 2007; Mabelane 2016; Mills 2008a; Mkhabela 2008; Nkhata 2016; Poghosyan 2017; Schadewaldt 2016; Vetter‐Smith 2012; Voogdt‐Pruis 2011; Walker 2004 | High confidence | — |
| Recipient of care flow processes and referrals | |||
| An appropriate referral system for recipients of care was important for the effective implementation of doctor‐nurse substitution strategies. | Basaleem 2011; Bennett 2013; Duane 2015; Lovink 2018 | Moderate confidence | Due to minor concerns about methodological limitations, relevance and adequacy |
| Management and leadership vision | |||
| Experienced leadership was a facilitator of smooth implementation of doctor‐nurse substitution strategies. | Burns 2009a; Leech 2007; Ljungbeck 2017; Mills 2008b; Petrova 2015; Poghosyan 2017 | High confidence | — |
| Nurses and recipients reported dissatisfaction with the huge number of documents and reports that needed to be completed in connection with doctor‐nurse substitution strategies. | Basaleem 2011; Flowers 2008; Georgeu 2012 | Moderate confidence | Due to minor concerns about methodological limitations and moderate concerns about adequacy |
| Doctor‐nurse professional boundaries and role clarity | |||
| Clear role definitions were critical in the successful implementation of doctor‐nurse substitution strategies. | Coulter 2000; Drew 2002; Drew 2003; Flowers 2008; Hamel 2017; Kraus 2017; Lindblad 2010; Lovink 2018; McKenna 2015; Mills 2008a; Peterson 2007; Poghosyan 2017; Schadewaldt 2016; Stephen 2018 | Moderate confidence | Due to minor concerns about methodological limitations and moderate concerns about relevance |
| Supervision | |||
| Where nurses were supervised by doctors, the quality of this supervision was central to the building of confidence in both partners. | Coulter 2000; Courtenay 2010; Drew 2002; Drew 2003; Kassean 2005; Kraus 2017; Lindblad 2010; Ljungbeck 2017; Mkhabela 2008 | Moderate confidence | Due to minor concerns about methodological limitations and adequacy |
| Nurses in LMIC settings appeared to lack effective supervision. | Basaleem 2011; Leech 2007 | Very low confidence | Due to serious concerns about adequacy |
aAdopted from the SURE Collaboration 2011; World Health Organization.
CERQual: Confidence in the Evidence from Reviews of Qualitative research; LMIC: low‐ to middle‐income country.
Background
Description of the topic
Most countries are facing a chronic shortage and maldistribution of health workers (Campbell 2013). It is acknowledged that human‐resource shortages in public healthcare systems play an important role in unsatisfactory health outcomes such as higher maternal mortality rates (Campbell 2013). The problem of human‐resource shortages is particularly challenging in low‐ and middle‐income countries (LMICs) in sub‐Saharan Africa, and in parts of Asia and the Americas. At the same time, the demand for health care is rising. There is a need to strengthen health systems and equip them with effective and efficient health service delivery strategies, as well as increase the coverage and reach of the effective services that are already in place (WHO 2008).
Governments worldwide are using several approaches to address this problem. One key approach is the moving of tasks from more specialised or highly‐trained to less specialised or less highly‐trained health workers, for instance by transferring certain tasks from doctors to nurses or midwives; sometimes referred to as 'task‐shifting' or 'optimising' (WHO 2004). By reorganising the health workforce in this way, policymakers hope to make more efficient use of the human resources already available (WHO 2012). One particular type of task‐shifting is the substitution of doctors by nurses. Doctor‐nurse substitution may help to address doctor shortages and reduce doctor workload.
Substitution is not a new strategy. For example, high‐income countries (HIC) such as Australia, the UK and the USA have extended nurses' tasks to include the prescription of routine medications (Cutliffe 2002; Hobson 2010; Stenner 2010). Also, a number of LMICs such as Ethiopia, Haiti, Malawi, Mozambique, Namibia, Rwanda, Uganda and Zambia are currently implementing this strategy to address the chronic shortage of health workers, particularly in the context of generalised HIV epidemics (Assan 2008; Freund 2015; Koenig 2004; Morris 2009).
One overview of systematic reviews considered the evidence for policy options for human resources, such as substitution or shifting tasks between different types of health workers, and assessed the effectiveness of these strategies in LMICs (Chopra 2008). Results showed that evidence from LMICs is sparse, and the studies are less rigorous than those from high‐income settings. The authors concluded that more reviews on the effects of policy options to improve human resources in such countries are needed.
Different arguments can be put forward to explain why doctor‐nurse substitution strategies are employed (e.g. Contandriopoulos 2015; Freund 2015; Kooienga 2015; Martinez‐Gonzalez 2014a; Newhouse 2011).
Substitution may reduce the cost of providing health care (as nurses are usually paid less than doctors), and hence may be more affordable for the health systems and users of care.
This is the main reason that policymakers may consider substituting doctors with nurses. Evidence on this is not clear‐cut (Dierick‐van Daele 2009; Hollinghurst 2006; Liu 2012). The Cochrane Library includes a review exploring the effectiveness of the substitution of general practitioners (family doctors) by nurses in primary care (Laurant 2018). This review suggested that nurse‐led care may make little or no difference to the cost of care compared to doctor‐led primary care (Laurant 2018). In another systematic review of substitution (task‐shifting) strategies for HIV care in Africa, the authors concluded that the delegation of tasks to nurses offered cost‐effective care to more patients than a doctor‐centred model (Callaghan 2010).
Substitution may improve access to primary care services as nurses may be available in settings where access to doctors is limited.
Substitution of doctors with nurses is one strategy for improving access. Nurses tend to provide more health advice (although an overall effect size could not be calculated), and are likely to achieve slightly higher levels of patient satisfaction compared to primary care doctors (Laurant 2018). Other reviews have also shown that nurses in advanced roles represent a substantial source of human capital for increasing access to (primary) care (Martinez‐Gonzalez 2014a; Martinez‐Gonzalez 2014b).
Substitution may enhance the quality of services provided in primary care. For example, patient education may be better when delivered by nurses.
Trained nurses can provide equal or potentially probably even better quality of care than primary care doctors and achieve equal or better health outcomes for patients (Laurant 2018; moderate‐certainty evidence (GRADE)).
Substitution may result in better retention of the nursing workforce by providing new clinical career pathways for experienced and higher educated nurses, further addressing nursing workforce shortages.
Deploying nurses as professional substitutes for doctors may improve retention among the nursing workforce (Kroezen 2015).
However, the potential relationships between the implementation of substitution strategies and health system objectives are not straightforward and might vary based on the setting and the organisation of care. The complexity of doctor‐nurse substitution and its interactions with the contextual factors in each setting has meant that it is difficult to explain why and how the intervention works, or does not work, in different settings. Substitution might also address equity concerns (for instance, by improving access to those most in need and most likely to benefit from care) without incurring additional costs. Furthermore, the long‐term cost‐effectiveness of a service might differ from short‐term outcomes, which are easier to assess.
Rashid 2010 conducted a systematic review exploring the benefits and limitations of the expansion of clinical tasks among nurses working in general practice in the UK. The focus of the review was to establish whether the findings of a previous Cochrane Review (Laurant 2005) were still relevant in the light of the more recent expansion of nurses' clinical tasks in the UK general practice setting. In this review, they integrated qualitative evidence from the UK with evidence on the effectiveness of doctor‐nurse substitution in primary care. The authors clustered the findings of this review under three themes: the impact on patients, on nurse competence, and on UK National Health Service policy. According to the findings, patients generally thought that all general practice nurses would be able to deal with simple conditions, but preferred to consult with a general practitioner if they thought it necessary. Indeed, there were concerns about nurses' knowledge base, particularly in diagnostics and therapeutics, and their levels of training and competence in tasks formerly undertaken by general practitioners. The review concluded that studies in this key area of healthcare policy were limited. As most of this limited evidence was from the UK, it was unclear to what extent these findings would apply to other settings.
Description of the intervention
In doctor‐nurse substitution strategies, nurses take on roles that were previously performed by doctors. The nature of the contribution that nurses substituting for doctors provide in clinical practice is complex and depends on several factors, including the setting, the tasks assigned to nurses, and the extent to which these tasks are accepted. Tasks can be supplementary to those performed by doctors or can be a substitution for doctors' tasks. This QES focused on tasks in which nurses substituted for doctors, meaning that they provided the same services as doctors (Laurant 2018).
Why is it important to do this synthesis?
The last decade have seen strong development in systematic review methodology for synthesising qualitative studies, including within Cochrane (Noyes 2009). The Cochrane Qualitative and Implementation Methods Group has identified around 500 such reviews; although very few of these are of direct relevance to policymakers making health workforce decisions in LMICs. It has been argued that in all countries, including resource‐poor countries, evidence‐informed decision‐making is essential (Chinnock 2005; Garner 1998; Oxman 2010). Policymakers need different types of evidence when choosing appropriate strategies. This includes reliable evidence about local context; but also global research evidence about the effectiveness of different strategies, and about potential factors influencing their implementation and success.
A QES can help in identifying factors influencing the success of substitution interventions, including the attitudes and experience of the health workers themselves; as well as those of other stakeholders (Harden 2004; Thomas 2008). The previous review on this issue conducted by Rashid was limited to UK studies only and covered a specific period of time (2004 to 2009) (Rashid 2010).
While the Cochrane intervention review on doctor‐nurse substitution concluded that the effectiveness of doctor‐nurse substitution strategies was promising (with certainty of the evidence (GRADE) moderate for mortality, patient health status, satisfaction and resource utilisation; and low for quality of life), the results of the included trials were heterogeneous (Laurant 2018). This finding is not unexpected given the complexity and variability of these types of interventions. In addition, the level of organisation and support associated with these trial interventions may have been higher than in real‐life settings. If these types of interventions are to be successfully implemented, we need a clearer understanding of the factors that influence their implementation, success and sustainability. Such factors may include the values and preferences of stakeholders and the feasibility and applicability of the intervention for particular settings and healthcare systems.
Objectives
To identify factors influencing the implementation of interventions to substitute doctors with nurses in primary care.
To explore how our synthesis findings related to, and helped to explain, the findings of the Cochrane intervention review of the effectiveness of substituting doctors with nurses
To identify hypotheses for subgroup analyses for future updates of the Cochrane intervention review
Methods
Criteria for considering studies for this synthesis
Types of studies
This was a systematic review of primary qualitative studies. We included primary studies that used qualitative study designs such as ethnography, phenomenology, case studies, grounded theory studies and qualitative process evaluations. We included studies that used both qualitative methods for data collection (e.g. focus group discussions, individual interviews, observation, diaries and document analysis) and qualitative methods for data analysis (e.g. thematic analysis, framework analysis and grounded theory). We excluded studies that collected data using qualitative methods but did not analyse the data qualitatively (e.g. open‐ended survey questions where the response data were analysed using descriptive statistics only).
We included studies regardless of whether or not they were conducted alongside studies of the effectiveness of the doctor‐nurse substitution (Laurant 2018). We included mixed methods studies when it was possible to extract the data derived and analysed using qualitative methods. We included studies irrespective of their publication status.
We did not exclude any studies based on our assessment of methodological limitations, but utilised this information to assess our confidence in the synthesis findings.
Topic of interest
We included studies that focused on the experiences and attitudes of stakeholders about doctor‐nurse substitution, nurses' role expansion and collaborative practice. Relevant stakeholders included nurses, doctors, patients and their families/carers, the general public, policymakers, programme managers, other health workers and any others directly involved in or affected by the substitution.
The phenomenon of interest was the substitution of doctors with nurses and the expansion of nurses' tasks in community or primary care worldwide. For the purposes of this QES, we used the same definition of substitution as in the Cochrane intervention review on this topic (i.e. as "the situation where task(s) formerly performed by one type of professional (i.e. a doctor) are transferred to a different type of professional (i.e. a nurse), usually with the intention of reducing cost or addressing workforce shortages" (Laurant 2018). We defined primary care as the first level of contact with formal health services (i.e. as those services that "provide first contact and ongoing care for patients with all types of health problems. This includes general practitioners, family doctors, paediatricians, general internists or geriatricians") (Laurant 2018). Primary care may have been delivered in the community or in a primary care facility (van Ginneken 2011; Wiley‐Exley 2007).
Search methods for identification of studies
Electronic searches
We searched the following electronic databases for eligible studies up to 18 June 2018.
CINAHL (EBSCOhost) (Appendix 1);
MEDLINE (OvidSP) (Appendix 1);
MEDLNE In‐Process & Other Non‐Index Citations (OvidSP).
Using guidelines developed by the Cochrane Qualitative and Implementation Methods Group for searching for qualitative evidence (Harris 2018), as well as a modified version of the search developed for the Laurant and colleagues intervention review on doctor‐nurse substitution (Laurant 2018), we developed search strategies for each database. Search strategies comprised of keywords and controlled vocabulary terms. Previous methodological work has demonstrated that the CINAHL database is the most important resource for qualitative evidence (Flemming 2007). Moreover, Flemming 2007 showed that for a specific review of qualitative evidence, all of the studies finally included in the review were identified in the CINAHL search. Therefore, we decided that instead of adding further databases to those listed above, we followed alternative routes to ensure the identification of relevant studies (see searching other resources below). We limited our searches to English for reasons of feasibility. We did not apply any date or geographic location limitations; and we searched all databases from inception to the date of search.
Searching other resources
In addition to our searches of the above‐mentioned databases, we conducted 'related article' searches in PubMed for all the studies included in the QES. We contacted experts in the field and scanned reference lists of relevant studies. We searched the reference lists of all the included studies and key references (i.e. relevant systematic reviews). We searched for any relevant papers that might have cited the included papers and key references (i.e. forwards citation search) in the ISI Web of Science (both the Science Citation Index and Social Science Citation Index) and Google Scholar. We also conducted individualised searches for qualitative studies that might have been linked to the studies included in the Cochrane doctor‐nurse substitution effectiveness review (Laurant 2005; Laurant 2018). This involved contacting the authors of the effectiveness studies; searching in PubMed for other articles published by the authors of the effectiveness studies and conducting 'related article' searches in PubMed for each study included in Laurant 2005 and Laurant 2018.
Data collection and analysis
Selection of studies
Two review authors independently assessed the titles and abstracts of the identified records to evaluate potential eligibility; we discarded those that were clearly irrelevant to the study topic. Two review authors independently retrieved and assessed the full text of all the potentially relevant papers using the review's inclusion criteria. At all stages, we resolved disagreements between the authors via discussion or, if required, by seeking a third review author's view. Where appropriate, we contacted the study authors for further information.
We included the Characteristics of excluded studies table from our synthesis and the main reasons for exclusion.
We included a PRISMA flow diagram to show our search results and the process of screening and selecting studies for inclusion (Figure 1).
1.
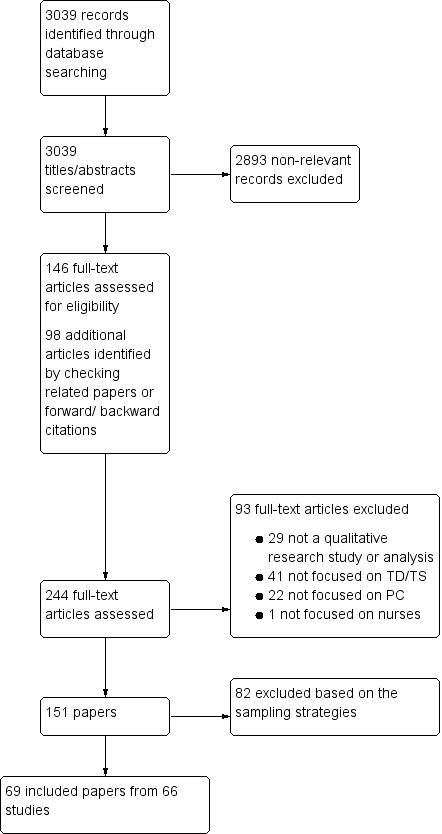
Study flow diagram. PC: primary care; TD: task development; TS: task‐shifting.
Sampling of studies
We did not use all of the studies that were eligible for inclusion when carrying out the synthesis of our QES as too great a number of studies can threaten the quality of data analysis (Glenton 2013). Instead, we aimed for a sample that was purposive rather than exhaustive, using an approach called maximum variation sampling with the aim of achieving the broadest possible variation within the eligible studies (Doyle 2003; Glenton 2013). We decided on two key sampling criteria that would enable us to capture rich data from all settings that would best answer our QES objectives. These became our sampling frame steps. First, we sampled all studies from LMIC settings, as most studies took place in HICs and we wanted to ensure that the synthesis included studies from all income settings. Second, we sampled studies according to the aspects of care covered and the types of interviewees in order to produce a sample with maximum variation. Finally, we examined the studies that remained after applying these first two steps and then further sampled studies with objectives that most closely matched our QES objectives. After applying this sampling approach, we included 69 papers for data extraction. The findings from these studies were the basis for the review findings. During the updating process, we used the same approach but complemented it with special attention to those studies that might help increase the confidence of the low or very low confidence review findings.
Data extraction and management
We collated records identified from different sources into one database using reference management software to remove duplicates.
We performed data extraction using a form designed specifically for this QES and based on the categories in the modified SURE (Supporting the Use of Research Evidence) framework for identifying factors affecting the implementation of a policy option (SURE Collaboration 2011) (see below). We also extracted information concerning the first author's name; year of publication; country of study; clinical area and setting of the study (primary health centre or community; rural/urban, etc.). We conducted a pilot trial of the data extraction form to check its adequacy, and made changes as necessary.
Data synthesis
We used the framework thematic synthesis approach to analyse and synthesise qualitative evidence (Booth 2015; Booth 2016). The Cochrane Qualitative Review Methods Group recommended the thematic synthesis (Noyes 2011), and may be particularly appropriate where evidence is likely to offer only a vague description and is likely to be largely descriptive as opposed to highly theorised or conceptual. In the framework approach, the thematic synthesis is guided by an a priori theoretical framework.
We followed the five stages of framework synthesis.
Familiarisation: three review authors occupied themselves with the included studies, with the aims and objectives of the QES in mind.
Identifying a thematic framework: rather than develop our own a priori framework after reading the included studies, we used an adapted version of the SURE framework as our framework of themes and categories (SURE Collaboration 2011). The SURE framework provided a comprehensive list of possible factors that could influence intervention implementation (Table 2).
Indexing: three review authors independently read and reread the selected studies and applied the SURE framework, moving between the data and the themes covered by the framework, but also searching for additional themes until all the studies had been reviewed. The review authors discussed the definitions and boundaries of each of the emerging themes. We then revised the SURE framework in line with the ideas and categories that emerged.
Charting: we developed the thematic synthesis further by rearranging data according to the appropriate part of the thematic framework to which they related, and formed charts. Our charts contained distilled summaries of evidence from different stakeholder perspectives and involved a high level of abstraction and synthesis.
Mapping and interpretation: using the charts, we then defined concepts, mapped the range and nature of phenomena, created typologies, and found associations between themes as a way of developing explanations for the findings. The process of mapping and interpretation was influenced by the original review objectives and by the themes that emerged from the data.
1. SURE framework for identifying factors affecting implementation of a policya.
| Level | Factors affecting implementation |
| Recipients of care | Knowledge and skills |
| Attitudes regarding programme acceptability, appropriateness and credibility | |
| Motivation to change or adopt new behaviour | |
| Providers of care | Knowledge and skills |
| Attitudes regarding program acceptability, appropriateness and credibility | |
| Motivation to change or adopt new behaviour | |
| Other stakeholders (including other healthcare providers, community health committees, community leaders, programme managers, donors, policymakers and opinion leaders) |
Knowledge and skills |
| Attitudes regarding program acceptability, appropriateness and credibility | |
| Motivation to change or adopt new behaviour | |
| Health system constraints | Accessibility of care |
| Financial resources | |
| Human resources | |
| Educational system | |
| Clinical supervision | |
| Internal communication | |
| External communication | |
| Allocation of authority | |
| Accountability | |
| Management or leadership, or both | |
| Information systems | |
| Facilities | |
| Patient flow processes | |
| Procurement and distribution systems | |
| Incentives | |
| Bureaucracy | |
| Relationship with norms and standards | |
| Social and political constraints | Ideology |
| Short‐term thinking | |
| Contracts | |
| Legislation or regulations | |
| Donor policies | |
| Influential people | |
| Corruption | |
| Political stability |
aAdopted from SURE Collaboration 2011.
Assessment of the methodological limitations in included studies
Two review authors (ES, AK) independently assessed methodological limitations for each study using an adaptation of the Critical Appraisal Skills Programme (CASP) quality assessment tool for qualitative studies (Appendix 2). We conducted a pilot with three included studies to assess the feasibility of the use of this tool and ensure integrity of the assessment. We included studies that met our inclusion criteria regardless of study quality. We resolved any disagreements by discussion or by involving a third review author (ES, AK, AR). Table 3 includes a summary of the assessment of methodological limitations of included studies.
2. Methodological limitations of included studies based on modified Critical Appraisal Skills Program (CASP) tool.
| Study ID | Was the context described? | Was the sampling strategy appropriate and described? | Was the data collection strategy appropriate and described? | Was the data analysis appropriate and described? | Were the findings supported by evidence? | Is there evidence of researcher reflexivity? | Have ethical issues been taken into consideration? | Overall assessment of methodological limitations |
| Abbott 2013 | Yes | Yes | Yes | No | Yes | Yes | Yes | Minor to moderate |
| Albers‐Heitner 2011 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Bailey 2006 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Minor |
| Basaleem 2009 | Yes | Yes | Yes | Yes | Yes | No | Yes | Minor to moderate |
| Basaleem 2011 | Yes | Yes | Yes | Yes | Yes | No | Yes | Minor to moderate |
| Bennett 2013 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Boyle 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Branson 2008 | Unclear | Unclear | Unclear | Unclear | No | No | No | Severe |
| Broyles 2012 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Burns 2009a | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Burns 2009b | Unclear | No | Unclear | Unclear | Yes | No | Unclear | Severe |
| Carryer 2017 | Yes | Yes | Yes | Unclear | Yes | No | Yes | Moderate |
| Cheek 2002 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Clendon 2001 | No | Unclear | No | No | Yes | No | Yes | Severe |
| Clendon 2003 | Yes | Unclear | Unclear | Unclear | Yes | No | Yes | Moderate to severe |
| Coker 2009 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Corneli 2008 | Yes | No | No | Yes | Yes | No | Yes | Moderate |
| Coulter 2000 | Unclear | No | Yes | Yes | Yes | No | No | Moderate to severe |
| Courtenay 2010 | Yes | No | Unclear | Yes | Yes | Unclear | Unclear | Moderate to severe |
| Dennis 2016 | No | No | Yes | Yes | Yes | Yes | Yes | Moderate |
| Dierick‐van Daele 2010a | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Minor |
| Drew 2002 | Yes | Unclear | Yes | Unclear | Yes | No | Unclear | Moderate to severe |
| Drew 2003 | Yes | Unclear | Yes | Unclear | Yes | No | Unclear | Moderate to severe |
| Duane 2015 | Unclear | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Flowers 2008 | Yes | Unclear | Yes | Unclear | No | No | Yes | Severe |
| Fortin 2010 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Francis 2013 | Yes | Yes | Yes | Yes | No | No | Unclear | Moderate |
| Friman 2011 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Furin 2011 | Yes | Unclear | Yes | Yes | Yes | Unclear | Yes | Minor to moderate |
| Georgeu 2012 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Hamel 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Minor to moderate |
| Hart 2012 | Yes | Yes | No | Yes | Yes | No | Yes | Moderate |
| Halcomb 2013 | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Ivers 2011 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Minor |
| James 2003 | Yes | Unclear | Yes | Yes | Yes | No | Yes | Moderate |
| Kaasalainen 2013 | No | Yes | Yes | Yes | Yes | Yes | Yes | Minor to moderate |
| Kassean 2005 | Yes | Yes | Unclear | Yes | Yes | No | Yes | Moderate |
| Kraus 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Leech 2007 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Leipert 2011 | Yes | Yes | Yes | Yes | Yes | No | Yes | Minor to moderate |
| Lindblad 2010 | Unclear | Unclear | Yes | Yes | Yes | No | Yes | Moderate |
| Ljungbeck 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Lorch 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Lovink 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Mabelane 2016 | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Maddox 2016 | Yes | Yes | Yes | Yes | Yes | No | Yes | Minor to moderate |
| Marsden 2004 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| McKenna 2015 | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Mills 2008a | No | Unclear | Unclear | Unclear | No | Yes | Yes | Severe |
| Mills 2008b | No | Unclear | Yes | No | Yes | Yes | Yes | Moderate to severe |
| Mkhabela 2008 | Yes | Yes | Yes | Yes | Yes | No | Yes | Minor to moderate |
| Nkhata 2016 | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Parfitt 2007 | Yes | Yes | Yes | Unclear | Yes | No | Yes | Moderate |
| Perry 2005 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Peterson 2007 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Minor |
| Petrova 2015 | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Poghosyan 2017 | No | Unclear | No | Yes | Yes | No | Yes | Severe |
| Rosemann 2006 | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Ross 2015 | Yes | Unclear | Yes | Unclear | Yes | Yes | Yes | Minor to moderate |
| Rustagi 2015a | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Schadewaldt 2016 | No | Yes | Unclear | Yes | Yes | No | Yes | Moderate to severe |
| Stenner 2010 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Stephen 2018 | No | No | Yes | Unclear | Yes | No | Yes | Severe |
| Stenner 2011 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Twinn 1999 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Vetter‐Smith 2012 | Yes | Yes | No | Yes | Yes | No | Yes | Moderate |
| Voogdt‐Pruis 2011 | No | No | Yes | Yes | Yes | Yes | Yes | Moderate |
| Walker 2004 | Yes | Yes | Yes | Unclear | Yes | No | No | Moderate to severe |
| Walker 2015 | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
Assessment of confidence in the synthesis findings
Two review authors (ES, AK) used the GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach to summarise our confidence in each finding (Lewin 2018a). CERQual assesses confidence in each review finding, based on the following four key components.
Methodological limitations of included studies: the extent to which there are concerns about the design or conduct of the primary studies that contributed evidence to an individual review finding (Munthe‐Kaas 2018).
Coherence of the review finding: an assessment of how clear and cogent the fit is between the data from the primary studies and a review finding that synthesises those data. By cogent, we mean well supported or compelling (Colvin 2018).
Adequacy of the data contributing to a review finding: an overall determination of the degree of richness and quantity of data supporting a review finding (Glenton 2018).
Relevance of the included studies to the review question: the extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context (perspective or population, the phenomenon of interest, setting) specified in the review question (Noyes 2018).
After assessing each of the four components, we made a judgement about the overall confidence in the review finding. We judged confidence as high, moderate, low or very low (Lewin 2018a). The final assessment was based on consensus among the review authors. All findings started as high confidence and were then graded down if there were important concerns regarding any of the CERQual components.
Summary of qualitative findings table
Our findings are presented in the Summary of Qualitative Findings tables (Lewin 2018b). These tables also provide our GRADE‐CERQual assessment of confidence in the review finding as well as an explanation of this assessment.
Linking the synthesised qualitative findings to a Cochrane intervention review
In the final stage of the analysis, we juxtaposed the key findings from this QES with those of the Cochrane intervention review of effectiveness (Laurant 2018) to form integrated matrices of evidence. The aim of linking the synthesised qualitative findings to the intervention review was to explore how the findings from our synthesis related to and helped to explain the findings of the related Cochrane intervention review. To do this, we used a matrix model similar to ones used previously by Candy 2011, Ames 2017, and Munabi‐Babigumira 2017. Our matrix explored whether the factors that were identified in our synthesis as important for implementing doctor‐nurse substitution strategies were reflected in the interventions evaluated in the studies in the related intervention review (Laurant 2018).
To create the matrix, we examined each of the synthesis findings that we assessed as high or moderate confidence. Within each of these findings, we identified factors identified by stakeholders as important for implementing doctor‐nurse substitution strategies. We then created 10 questions reflecting these factors and added them to a table. We then assessed whether there was a match between each of these questions and the intervention components or implementation approach from each trial, using 'yes', 'no' and 'unclear' answers. The questions are listed below.
Question 1: Is information being communicated to service users on the task/s that will be delivered by nurses rather than doctors, and about the roles that nurses will play in their care?
Question 2: Have efforts been made to increase doctors' trust in and acceptability of using nurses to substitute for doctors? For instance, have there been any attempts to reassure doctors that nurses have the necessary skills and training to take on the designated task/s? Does implementation of the specific task substitution reduce doctors' workloads? Does implementation of doctor‐nurse substitution for the specific tasks reduce doctors' workloads without leading to a reduction in their salary or other payments?
Question 3: Are processes in place that allow doctors and nurses to communicate effectively and provide feedback to one another concerning specific task‐shifting strategies?
Question 4: Can service users easily access the nurses who have been designated to deliver the specific substituted task/s?
Question 5: Have nurses received appropriate training and tailored feedback regarding the specific substituted task/s that they have been requested to deliver?
Question 6: Does the substituted task facilitate continuity of care for patients?
Question 7: Have attempts been made to ensure that factors affecting nurses' internal motivation (such as job satisfaction and independent work) and external motivation (such as improved working conditions and financial issues) are addressed?
Question 8: Are the necessary resources (financial, infrastructural, facilities, and drugs and equipment) available to nurses taking on new task/s?
Question 9: Have appropriate supervisory and monitoring arrangements been put in place for the specific substituted task/s?
Question 10: Are doctor/nurse role boundaries clearly defined for the specific substituted task/s?
Review author reflexivity
In keeping with quality standards for rigour in qualitative research, we considered our views and opinions on doctor‐nurse substitution as possible influences on the decisions made in the design and conduct of this QES, including the search strategy, inclusion decisions, synthesis and interpretation of the findings; and, in turn, on how the emerging results of the QES influenced our views and opinions. We were aware of our own positions (which included doctors who benefited from and nurses who had implemented substitution strategies). AR, ESh, AK, KhH, and SL have previously worked as public health specialists or clinicians in low‐ and middle‐income settings. ML is a professor of the organisation of health care and services, and is one of the experts on the substitution of care in the Netherlands. She is involved in MANP (Maine Association of Nonprofits) education at HAN University of Applied Sciences. The authors have multiple perspectives but generally all support the principles of doctor‐nurse substitution to improve access and outcomes in primary care and are of the view that substitution should be implemented where it has been shown to be effective for outcomes that are valued by patients and the public; and that implementation strategies should be sensitive to the needs and experiences of patients, nurses and doctors.
Results
Results of the search
We identified 3039 titles and abstracts (MEDLINE: 2259 and CINAHL: 780) published on or before 18 June 2018. We considered 244 full‐text papers for inclusion in this synthesis. We found 151 studies that met our inclusion criteria and purposively sampled 69 papers coming from 66 unique studies for inclusion in the synthesis (Figure 1). Two qualitative studies were conducted alongside or in relation to two of the 18 interventions reported in Laurant's review (Dierick‐van Daele 2010a; Voogdt‐Pruis 2011).
Included studies
Description of studies
Study participants
Participants mostly included recipients of care, nurses and doctors, although some studies also included clinical leaders, policymakers, physician assistants, pharmacists, managers and other health professionals.
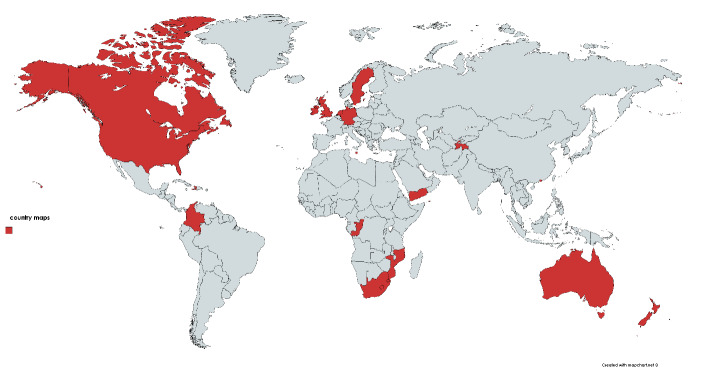
Settings
The sampled studies were conducted across 25 countries: nine countries in sub‐Saharan Africa, one in Asia, two in Oceania, seven in Europe, two in the Middle East and North Africa, two in North America and two in Latin America (Figure 2). Eleven of these studies were based in LMICs (Columbia, Congo, Haiti, Lesotho, Malawi, Mauritius, Mozambique, South Africa, Swaziland, Tajikistan, Uganda, Yemen, Zimbabwe) and 55 were based in HICs (Australia, Canada, Germany, Hong Kong, Malta, Netherland, New Zealand, Slovenia, Spain, Sweden, USA and UK).
2.
Geographical distribution of the sampled studies.
Types of interventions
The sampled studies dealt with the following tasks and healthcare areas within primary healthcare settings:
-
General practice
Nurse roles in primary health care and general practice (Albers‐Heitner 2011; Bailey 2006; Branson 2008; Cheek 2002; Coulter 2000; Duane 2015; Fortin 2010; Hamel 2017; Kraus 2017; Lindblad 2010; Marsden 2004; McKenna 2015; Mills 2008a; Mills 2008b; Perry 2005; Petrova 2015; Poghosyan 2017; Rosemann 2006; Schadewaldt 2016; Twinn 1999; Walker 2015).
-
Acute or chronic (or both) care
Anticipatory 'proactive care' (Bennett 2013).
Acute and chronic wound care (Friman 2011).
HIV/sexually transmitted disease/tuberculosis (TB) care (Abbott 2013; Corneli 2008; Georgeu 2012; Halcomb 2013; Ivers 2011; Mabelane 2016; Mkhabela 2008; Nkhata 2016; Rustagi 2015a).
Diabetes care (Boyle 2016; Kassean 2005; Vetter‐Smith 2012).
Chronic obstructive pulmonary disease (Dennis 2016).
Hypertension management (Stephen 2018).
Nurse prescribing (Courtenay 2010; Maddox 2016; Ross 2015; Stenner 2010; Stenner 2011).
Integration of nurses in long‐term care settings (Kaasalainen 2013).
-
Specific groups care
Child health care (Basaleem 2009; Basaleem 2011; Coker 2009; Flowers 2008; Leech 2007).
Healthcare for older people (Ljungbeck 2017; Lovink 2018).
Family health nursing (Parfitt 2007).
Maternity care (James 2003; Peterson 2007).
-
Setting‐oriented care
Nurse practitioner‐led clinics in primary school environments (Clendon 2001; Clendon 2003).
Advanced tasks in rural settings (Carryer 2017; Francis 2013; Leipert 2011).
-
Screening and preventive care
Alcohol screening, brief intervention and referral to treatment (Broyles 2012).
Screening young people for health risks and provide a brief intervention for detected risks (Hart 2012).
Chlamydia testing (Lorch 2015).
Cardiovascular prevention (Voogdt‐Pruis 2011).
-
Leadership
Clinical leadership of expert nurses (Burns 2009a; Burns 2009b).
Quality of the included qualitative studies
In general, there was relatively poor reporting of context, sampling, research methods and researcher reflexivity across the studies. All studies gave some description, even if very brief, about the participants, interventions, sampling, methods and analysis. All studies used an interview or focus group discussions, with seven studies using some type of observation along with the interviews (see Table 3).
Excluded studies
We excluded 93 full‐text articles for the following reasons (see Characteristics of excluded studies table):
29 were not qualitative research studies or analyses;
41 were not focused on task development/task‐shifting;
22 were not focused on primary care;
one was not focused on nurses.
Confidence in review findings
Out of 27 findings, we graded four as high confidence, 19 as moderate confidence and the remaining findings as low or very low confidence using the GRADE‐CERQual approach (see Table 1). Our explanation for each CERQual assessment is shown in Appendix 3.
Synthesis findings
In this section, we presented the categories identified in the data synthesis and the findings of the QES that corresponded to each category. Using the SURE framework, we developed 12 categories related to factors influencing implementation of doctor‐nurse substitution strategies that we could elicit data from included primary qualitative studies.
Type of task.
-
Accessibility and quality of care.
Ease of access.
Quality of access.
Doctor‐nurse communication.
Educational and training system.
Awareness and understanding of the strategy.
Continuity of care.
-
Motivation and incentives.
Nurses' motivation.
Doctors' motivation.
Resources (financial, infrastructures, facilities, and drugs and equipment).
Recipient of care flow processes and referrals.
Management and leadership vision.
Doctor‐nurse professional boundaries and role clarity.
Supervision.
Type of task
Recipients of care had mixed views about the expansion of tasks undertaken by nurses. They preferred doctors when the tasks were more 'medical' in nature but they accepted nurses for preventive care and follow‐ups (moderate confidence; finding #1;Appendix 3). Almost all recipients preferred having doctors rather than nurses as healthcare providers when the healthcare tasks undertaken were more 'medical' in nature, including tasks that involved invasive treatment, prescriptions, referral to other services (Cheek 2002), diagnosis of serious conditions or performing physical examinations (Cheek 2002; Coker 2009; Courtenay 2010). For instance, participants in one study conducted in the US did not perceive nurses as the preferred cadre for the provision of several child care services: "I just feel way more comfortable if the doctor checked everything" (Coker 2009). This preference for doctors was tied to recipients' uncertainty about nurses' ability to perform these types of tasks. Some recipients assumed that nurses would need to consult doctors in order to carry out these tasks (Rosemann 2006), and considered nurses to be complementary to doctors rather than replacing them for the services in question (Cheek 2002; Clendon 2001; Courtenay 2010). However, recipients' preferences varied in some cases by language and ethnic group (Coker 2009).
Recipients of care did accept the use of nurses for less 'medical' tasks, such as prevention and promotion activities, the monitoring of a condition after a diagnosis (Clendon 2003; Leipert 2011), chronic disease management (Branson 2008), public healthcare activities (Clendon 2001), and continuing to prescribe medication initiated by doctors (Branson 2008). Recipients referred to the following examples: screening (Cheek 2002), injections, wound care, taking measurements (blood pressure, weight, etc.), first aid, immunisation, counselling in schools (Boyle 2016; Cheek 2002; Clendon 2001; Perry 2005; Rosemann 2006), child growth and development monitoring (Flowers 2008), and arranging appointments with doctors (Bennett 2013). Some recipients felt that nurses delivered better care than doctors when they provided these types of services (Cheek 2002). The skills of the nurses were appreciated more by recipients in HICs (Clendon 2003; Leipert 2011): "Well, I only went to her once when she was offering free blood sugar tests, so I thought I would go and do that but I had lots and lots of conversations with her and a lot of respect for what she was doing …" (Clendon 2003).
Doctors in most studies also preferred that nurses perform only non‐medical tasks (moderate confidence; finding #2;Appendix 3). Doctors welcomed the transfer of certain tasks to nurses such as dealing with minor illness and chronic disease care (Abbott 2013; Branson 2008; Coulter 2000; Ivers 2011; Lindblad 2010; Stephen 2018; Twinn 1999), taking Pap smear samples (Coulter 2000), skin complaints and musculoskeletal problems (Branson 2008), prescribing/repeat prescribing (Branson 2008; Marsden 2004; Ross 2015; Stenner 2010), measurement of blood pressure (Bailey 2006) or height and weight (Twinn 1999), prevention consultation (Stephen 2018; Voogdt‐Pruis 2011), sexual health (Lorch 2015), routine primary care (Kraus 2017), and health promotion tasks (Bailey 2006). Some of these tasks are the same types of non‐medical tasks that recipients accepted from nurses (Branson 2008; Cheek 2002; Clendon 2001; Clendon 2003; Flowers 2008; Leipert 2011; Perry 2005; Rosemann 2006). Doctors believed that when nurses acted within the boundaries of what doctors believed to be appropriate, and could be counted on to consult and refer appropriately, nurses were judged to be safe/competent professionals (Bailey 2006; Ross 2015). In one HIC‐based study, doctors were not willing to shift tasks such as examination, diagnosis or therapy to nurses: "she can't assess what is good for the individual patient, and I don't think it's good if the task is handed down to the next level …" (Rosemann 2006). In one LMIC‐based study, doctors' attitudes were more mixed. Most doctors in this study supported decentralisation and nurse initiation of antiretroviral therapy. However, several doctors were uncertain about the ability of nurses to manage and appropriately refer more complex cases (Georgeu 2012).
Nurses were comfortable with, and believed they were competent to deliver a wide range of tasks, but particularly emphasised tasks that were more health promotive/preventive in nature (moderate confidence; finding #3;Appendix 3). Nurses believed that they could deliver different primary healthcare services such as health promotion and disease prevention practices (Bailey 2006; Kraus 2017; Stephen 2018); nutrition counselling, smoking cessation counselling, screening for family violence and abuse (Dennis 2016; Peterson 2007); improving patient access to primary care, their attention to social issues and education (Kraus 2017); assessing patients' situation and adjusting care plans (Hamel 2017); and sexual healthcare (Abbott 2013). Nurses in one study conducted in Australia also believed that they could have played a more prominent role in the preventive care of young people, and felt that having a linkage role with other agencies, schools and health professionals would provide more holistic care (Hart 2012).
One study conducted in South Africa reported that some nurses were comfortable with and enthusiastic about the opportunity to be involved more directly in providing HIV therapy (Georgeu 2012). Nurses in one study from Australia were also satisfied with having advanced roles in working with clients at risk of, or experiencing, cardiovascular disease assigned to them along with their own routine tasks (Francis 2013). However, this attitude was less common. In another study from New Zealand, nurses valued delivering tasks and procedures previously designated medical, as enabling them simply to provide care to a much wider range of patients (Carryer 2017).
Accessibility and quality of care
Ease of access
Recipients in most studies believed that nurses were more easily accessible than doctors (high confidence; finding #4;Appendix 3). Recipients of care perceived care delivered by nurses as having a number of advantages. Recipients in most studies saw nurse‐delivered care as easier to access than care from doctors (Basaleem 2009; Coker 2009; Fortin 2010; Georgeu 2012; Leipert 2011), with shorter waiting times (Cheek 2002), lower travel costs and less time spent (Georgeu 2012). They also described how it was quicker to obtain appointments (Marsden 2004; Perry 2005; Ross 2015; Stenner 2011), and easier to schedule visiting times (Coker 2009).
Both doctors and nurses saw doctor‐nurse substitution and collaborative practice as a way of increasing quick access to care for certain tasks such as maternity care and prescriptions (moderate confidence; finding #5;Appendix 3). Substitution strategies in both LMICs and HICs were seen by some doctors and nurses as beneficial because these strategies helped to improve access to care in settings that particularly needed this service (Kaasalainen 2013; Ljungbeck 2017; Lovink 2018; Perry 2005; Peterson 2007; Poghosyan 2017).
Quality of care
Recipients of care in most studies were satisfied with nurses' social skills. Recipients' perceptions of nurses' technical skills were mixed (very low confidence; finding #6;Appendix 3). Nurses appreciated the continuity of the nurse‐recipient relationship and the fact that these consultations were personal and interactive in nature (Friman 2011; Hart 2012; Parfitt 2007; Peterson 2007; Ross 2015). This made recipients feel cared for and was an indicator to them of a good‐quality service (Dennis 2016; Friman 2011; Stenner 2011). Recipients in some studies described how nurses listened more carefully to them, paid more attention and had time for their concerns (Bennett 2013; Boyle 2016; Coker 2009; Leipert 2011; Parfitt 2007; Ross 2015; Stenner 2011), used face‐to‐face interaction, and social contact (Ross 2015; Stenner 2011), had holistic approaches to care (Boyle 2016; Ross 2015; Stenner 2011), and allocated time to provide information and support (Boyle 2016; Duane 2015; Stephen 2018): "[She] took the time to listen to my concerns, answer my millions of questions … she didn't rush the appointment, my appointment took longer than it should have. It made me feel good, it made me feel comfortable, safe. It was about me." (Leipert 2011). Nurses' close, trusting and familiar relationships with recipients could encourage the recipients to become more involved in their treatment (Corneli 2008; Friman 2011; Leipert 2011; Ross 2015). Recipients in some studies also noted that nurses spoke to them at their own level and tended to use language that the recipients could understand and that was free of medical jargon. This led recipients to feel that they were able to develop 'collaborative partnerships' with nurses that were 'founded on trust and respect' (Ross 2015). However, in three studies conducted in HICs, recipients of care felt that it was easier to communicate with the doctor because they had known their doctor for longer (Branson 2008; Fortin 2010) or because they felt that nurses were too overworked to be able to increase the recipients' knowledge and skills (Leech 2007).
In addition to appreciating these social aspects of nurse‐delivered care, recipients in some studies also highlighted technical skills. In some HIC‐based studies, recipients were confident in the nurses' ability to prescribe and make treatment decisions (Bennett 2013; Stenner 2011). This confidence was gained partly through direct experience of benefiting from the nurses care, in particular where the nurses had identified problems missed by a doctor: "… and that explanation and everything was given to me by the Diabetic Nurse, not by the doctor or the Consultant" (Stenner 2011). However, in one study conducted in Africa, parents were dissatisfied with nursing practices related to infant developmental care and felt that these did not meet the desired standards. "They don't examine the babies. They only weigh them and that is most probably why most of our children's problems are not identified", "…if the queues are long, somewhere along the way these nurses get tired and they don't really give the kids a thorough attention." (Leech 2007).
Health professionals, including doctors, nurses, policymakers and other healthcare providers, believed that doctor‐nurse substitution led to improvements in the quality of care (high confidence; finding #7;Appendix 3). Similar to the viewpoints of recipients of care, health professionals in some studies believed that doctor‐nurse substitution led to improved quality of care by benefiting recipients with the social skills of nurses (Boyle 2016; Coulter 2000; Kaasalainen 2013; Lorch 2015; Marsden 2004; Rustagi 2015a; Stenner 2010), improved safety (due to nurses' abilities to put together several parts of a complex patient picture through their clinical competence, leadership and collaborative practice), more time to focus on each patient's situation as a whole (Ljungbeck 2017), and comprehensive person‐ and family‐centred care (Carryer 2017). Management staff in one study conducted in the UK noted that nurses had more time to spend with the recipients who often needed general advice and to have questions answered. The reception staff, in particular, relied on the expertise of the nurses, especially when the doctors were absent (Marsden 2004). In one study conducted in the Netherlands, a doctor stated: "It is crucial that the nurse has enough time to explore profound problems, this is quality of care." (Dierick‐van Daele 2010a). In some countries, the use of nurses to provide certain services was seen as a solution to recipient expectations (Abbott 2013; Coulter 2000; Leipert 2011; Marsden 2004; Perry 2005). For example, in one study from the US, nurse practitioners saw themselves as a solution to the shortage of female doctors providing obstetric care in a setting where women preferred female providers (Coulter 2000).
In one study based in three LMICs (Malawi, Uganda and Zimbabwe), nurses perceived that delivering new services had increased their workload and had several consequences. Some felt that the increase in workload has resulted in extending their working hours, leading to overcrowding in health facilities, in turn hindering the provision of quality care (Nkhata 2016).
Doctor‐nurse communication
A close doctor‐nurse relationship characterised by trust and mutual respect helped nurses to expand and develop their roles (moderate confidence; finding #8;Appendix 3). Professional trust, mutual respect and a close working relationship with doctors allowed nurses to develop their role. This was linked to feeling 'valued', 'trusted', 'appreciated' (Burns 2009b; Francis 2013; Georgeu 2012; Hamel 2017; Peterson 2007; Poghosyan 2017; Schadewaldt 2016), and 'empowered' (Burns 2009b; Lovink 2018): "I think the trust you receive from the GP is a facilitator, the space to act or not to act" (Lovink 2018). The doctor‐nurse relationship was seen as an enabler of role development and collaborative work by nurses (Hamel 2017; Mills 2008a; Peterson 2007; Vetter‐Smith 2012; Voogdt‐Pruis 2011). Nurses who did not have such a relationship with their doctor colleagues spoke of feeling 'totally unsupported' and 'powerless' (Burns 2009b).
Nurses working in stand‐alone practices or vertical programmes of care might find it difficult to communicate effectively with colleagues (moderate confidence; finding #9;Appendix 3). Nurses working in stand‐alone practices suggested that they might experience communication challenges with their colleagues due to infrequent contact and lack of channels for external contact such as sharing information by telephone, receiving feedback on referrals, exchanging printed information on services or sharing information on professional development opportunities (Broyles 2012; Flowers 2008; Walker 2015).
In LMICs, there was also limited collaboration between different vertical programmes of care (Basaleem 2011; Rustagi 2015a). Improving the communications between health workers (such as clearly defining the tasks of all cadres of health workers, encouraging broad participation in team meetings and ensuring a positive team dynamic) was valued by nurses in one study conducted in Mozambique (Rustagi 2015a).
Doctors' trust in and acceptance of nurses was a critical determinant shaping the extent of nursing practice (moderate confidence; finding #10;Appendix 3). The acceptance of nurses' programmes by doctors was critical to nurses' success (Coulter 2000; Dennis 2016; Duane 2015; Friman 2011; Georgeu 2012; Leech 2007; Stenner 2010). However, nurses believed that their practice might be limited by doctors' lack of understanding about the extent and quality of nurses' skills (Bailey 2006; Burns 2009b; Coulter 2000). When nurses and doctors worked closely together, nurses felt that the views of these doctors influenced their own professional nursing practice (Burns 2009b; Coulter 2000; Francis 2013). In one study performed in Australia, nurses looked for cause 'champions' (i.e. doctors) who were willing to advocate their roles as nurses and to assist them in establishing professional credibility (Mills 2008a). Some nurses in one study from Canada believed that the ideal shared practice would be one of mutual respect and reciprocity, but recognised that at present, there was neither mutual respect nor reciprocity (Bailey 2006).
Doctors' levels of trust in nurses' skills appeared to be influenced by the amount of time they spent working with nurses (Lindblad 2010), and how closely they worked together (Abbott 2013; Mabelane 2016). When there was a greater degree of collaboration between nurses and doctors, they viewed each other more as equals and partners within the care setting (Coulter 2000). Doctors appeared to value nurses more highly when they viewed them as professional equals (Burns 2009b; Coulter 2000; James 2003), and several doctors commented that the knowledge of nurse prescribers was equal to that of doctors (Ross 2015).
Financial issues might damage the relationship between doctors and nurses (low confidence; finding #11;Appendix 3). In some settings, when a task was conducted by a nurse, the practice received a lower payment than when the same task was conducted by a doctor. This resulted in imbalances in power between doctors with financial interests in the practice and nurses (Poghosyan 2017). However, conflicts of this type were not reported between salaried doctors (whose earnings were not linked to the remunerated value of the services) and nurses (Mills 2008a). Liability and insurance issues were also described as structural barriers to collaborative care (Lovink 2018). Doctors in some studies felt that being financially responsible for the actions of other members of the team was a barrier to collaborative practice, especially as there were differences in the level of insurance coverage of different team members (Peterson 2007). Doctors regarded fee‐for‐service payments as a barrier, and even a disincentive, to collaborative work (Coulter 2000; Peterson 2007; Ross 2015; Schadewaldt 2016).
Educational and training system
Nurses felt they had gained additional skills through task‐shifting. However, they believed that further training and education could increase their skills, job satisfaction and motivation, allowing them to work more independently and increase others' acceptance of their professional roles (moderate confidence; finding #12;Appendix 3). Nurses in some studies were aware of deficits in their knowledge and skills (Maddox 2016), and described the need for additional support and hands‐on training, particularly in the early days of expanding their roles (Mkhabela 2008; Stenner 2010). Nurses felt empowered and confident with their increased skills and knowledge (Dennis 2016). They considered continued and additional training and access to training updates as important (Burns 2009b; Courtenay 2010; Duane 2015; Francis 2013; Friman 2011; Furin 2011; Hart 2012; Kassean 2005; Maddox 2016; Rustagi 2015a; Stenner 2011), and believed that it could lead to several benefits. Training and education could influence their willingness to take on new tasks (Dennis 2016; Ivers 2011), and feelings of competence could enhance their job satisfaction and stimulate their motivation (Albers‐Heitner 2011). Further education was seen by nurses as an opportunity to work more independently (Friman 2011), take on more responsibility (Lindblad 2010), and develop personal competency, and was also seen as a career opportunity (Lindblad 2010). Finally, nurses regarded the knowledge and skills gained through task‐shifting as important for gaining acceptance from others of their professional roles (Mills 2008a; Mills 2008b).
Nurses had concerns about their training in terms of adequacy, equity and quality (moderate confidence; finding #13;Appendix 3). Nurses in some studies had concerns about the adequacy and quality of the training they undertook before extending or expanding their roles (Broyles 2012; Maddox 2016; McKenna 2015; Nkhata 2016). "Sometimes we are asked to test a mentally sick person and yet we have never learned on how to handle psychiatric patients –we are forced to do a quick job and give results. So we are denied chances [to take part] in most of the training and yet we meet different issues which need trained personnel to handle" (Nkhata 2016). In one study from the UK, concerns about the lack of specific training for advanced roles were raised as it was not clear what the current educational preparations were for training nurses (Drew 2002; Drew 2003). Access to appropriate education was a particular barrier identified by some nurses: "Expanding your prescribing may be difficult, not because of your knowledge of the drugs, but because there's no training at a good enough level for the other stuff, you know, how do you become competent to treat osteoporosis, there are no courses" (Maddox 2016). Where education was being offered, it was identified as more often being around specific clinical tasks and not necessarily building towards advanced practice (McKenna 2015). In one study conducted in Malawi, Uganda and Zimbabwe, a perception of unfair and inequitable access to training opportunities was also mentioned, especially by those in rural facilities and in lower level positions (Nkhata 2016).
Financial support and time release to attend training and education programmes were considered to be worthwhile investments by nurses in another study. The nurses stated a preference for short courses but also described a broad range of learning technologies that they could use (Francis 2013). One rural practice nurse felt that while training was a good idea, it would be difficult for many to attend: "Well, certainly for rural it would probably be much easier if it was a distance education component with, you know, perhaps some onsite visits to adolescent mental health areas" (Hart 2012). However, distance learning offered through digital technologies could be challenging for some nurses who were not computer literate (Mabelane 2016). In another study, staff raised other concerns regarding nurses' training. Here, they felt that trainers lacked direct clinical experience and perceived that trainers did not have sufficient time in their work schedule to travel regularly to sites to provide support (Georgeu 2012).
Awareness and understanding of the strategy
Recipients of care in many studies had limited knowledge about nurses' roles in primary care, nurse models of care, and any differences between nurse‐led and doctor‐led care (moderate confidence; finding #14;Appendix 3). Studies that assessed the recipients of care's awareness and understanding of the healthcare programmes offered by nurses noted that many recipients' knowledge of these services was limited (Basaleem 2009; Branson 2008; Cheek 2002; Clendon 2001; Halcomb 2013; Leipert 2011), and recipients and their families did not know what to expect from a nurse (Lovink 2018). In one study that involved expanding the services offered by public health nurses in schools, the authors noted that although the recipients of care were 'aware' of the service, they had little knowledge of the details of the strategies and the expansions of the nurses' roles. The authors concluded that there was a need to enhance public awareness about the roles and tasks the nurses were able to offer (Clendon 2001).
Continuity of care
Doctors in some studies felt that doctor‐nurse substitution improved the continuity of care and believed that recipients of care would prefer to see the same nurse rather than different doctors (moderate confidence; finding #15;Appendix 3). Doctors in some studies believed that recipients would prefer to see the same nurse rather than different doctors (Marsden 2004; Ross 2015): "I think the most important thing patients like is seeing somebody consistently and I think that if they were given a choice that they would probably prefer a non‐medical prescriber who is going to be there all the time as opposed to a rotational junior" (Ross 2015). In one study conducted in the UK, doctors described how nurse practitioners provided an opportunity for continuity of care and provided better services than locum or trainee doctors (Marsden 2004). Also, some doctors reported that prescribing rights enabled nurses to improve the continuity of recipients' care and to have longer consultations with recipients of care, and the opportunity of providing patient‐centred care (Marsden 2004).
Recipients of care in some studies were concerned over the continuity of care provided by nurses and felt insecure if they lost their contacts with their doctors (low confidence; finding #16;Appendix 3). Even where recipients of care were satisfied with the services the nurses offered, some recipients felt insecure if they lost their contacts with the doctors (Branson 2008; Fortin 2010; Georgeu 2012): and acknowledged that doctors continued involvement was important (Stephen 2018). "Of course I would feel more secure with my doctor than with the nurse! … You can meet with the nurse, but …replacing the appointment with, ah, with a nurse …I don't know!" (Fortin 2010), or "I feel quite sure that if there were any difficulties that she'd pass it on to the doctor" (Stephen 2018).
Motivation and incentives
Nurses' motivation
Internal motivators most frequently cited by nurses regarding task‐shifting were psychological (including personal development and being respected) and professional (improving the quality of care) (moderate confidence; finding #17;Appendix 3). When describing what motivated them to be involved in doctor‐nurse substitution strategies, nurses in most studies cited psychological factors including looking for new challenges and being respected (both by recipients and doctors) (Albers‐Heitner 2011; Burns 2009b; Coulter 2000; Drew 2002; Drew 2003; Friman 2011; James 2003; Ross 2015; Voogdt‐Pruis 2011).
Nurses in many studies also cited professional factors as motivators of the doctor‐nurse substitution strategies (Albers‐Heitner 2011; Furin 2011; Georgeu 2012; Ljungbeck 2017; Petrova 2015). These included a feeling of long‐term commitment to recipients (Georgeu 2012), helping recipients to get well (Albers‐Heitner 2011; Hamel 2017), and enhancing the professional role by providing more than only patient care (Albers‐Heitner 2011): "We see how our jobs affect people here and in other parts of Africa too. That helps get through the day. That and seeing people regain their health. It truly is a blessing to be part of" (Furin 2011).
Nurses believed that external motivators such as improved working conditions and financial incentives could act as an incentive to take on more responsibilities (moderate confidence; finding #18;Appendix 3). Studies mostly set in HICs reported that external motivators were important to nurses. Nurses described how working conditions that included lower levels of stress, flexible and shorter working hours in clinics (Flowers 2008), and the ability to send their families extra money from their salaries (Furin 2011), helped to improve job satisfaction and acted as an incentive to accept more responsibilities. Nurses raised the issue of continued funding of professional development as important for promoting advanced roles (Francis 2013; Hamel 2017). This included funding for scholarships and education as well as funds to provide for others to cover shifts while nurses were attending educational activities (McKenna 2015). Despite the readiness of nurses to provide care to patients, nurses recognised that there were remuneration issues that would need to be addressed to facilitate this care (Hart 2012; Ljungbeck 2017; Nkhata 2016). Another enabler to facilitating advanced roles raised by nurses was funding to support infrastructure in the form of nursing workspaces: "most of the advanced roles really need you to have a room of your own and practices don't have them. The nurses are frequently in treatment rooms or desks in corridors or funny places, so you do have to restructure your building" (McKenna 2015). In one study from Australia, nurses complained that organisational structures had impacted negatively on nurses' motivation surrounding task‐shifting. Nurses said that they were unable to disagree with doctors even when they wanted to. This was because they were paid and employed by the doctors and believed that such disagreements could threaten their job security (Mills 2008a).
Doctors' motivation
Doctors valued the contribution of nurses in collaborative practices when this reduced their own workload (moderate confidence; finding #19;Appendix 3). Many doctors both in HICs and LMICs believed that high workloads could lead to burnout for clinicians, and were satisfied with the collaborative practices that helped to reduce their workload (Coulter 2000; Dierick‐van Daele 2010a; Drew 2002; Drew 2003; Georgeu 2012; Hamel 2017; Ljungbeck 2017; Lorch 2015; Lovink 2018; Marsden 2004; Peterson 2007). Based on the views expressed by the doctors, the transfer of some of their tasks to nurses could give doctors more time to focus on other services that recipients require (Georgeu 2012). In turn, this could help to improve the likelihood of retaining doctors in practice, and therefore the likelihood of more doctors opting to provide speciality care (Georgeu 2012; Peterson 2007): "the nurses free us to deal with more complex cases" (Marsden 2004).
Doctors in some studies reported that the introduction of practice nurse services had not led to any change in their working hours (Marsden 2004; Stenner 2010), probably because of an already increasing demand for doctors' services (Marsden 2004). However, they were now seeing more new patients and patients with acute illnesses (Kaasalainen 2013); or were seeing a reduction in work disruption because nurses no longer needed to ask doctors to sign prescriptions (Stenner 2010).
In settings where a proportion of doctors'revenues came from fee‐for‐service payments, doctors expressed negative reactions towards doctor‐nurse substitution (low confidence; finding #20;Appendix 3). Financial concerns and negative reactions of doctors towards doctor‐nurse substitution strategies were raised regardless of whether the fee‐for‐service was paid directly by the user as an out‐of‐pocket payment or paid by third‐party payers. Doctors regarded fee‐for‐service payments as a barrier, and even a disincentive, to collaborative work (Coulter 2000; Peterson 2007). The organisational type and culture affected doctors' acceptance of the roles and tasks of nurses, although this acceptance varied between individuals (Coulter 2000; Lorch 2015).
Resources (financial, infrastructures, facilities, and drugs and equipment)
A shortage of resources, including human resources, equipment and supplies, and lack of equity in how organisational resources were allocated sometimes negatively impacted on the effective implementation of doctor‐nurse substitution strategies (high confidence; finding #21;Appendix 3). Studies mostly set in LMICs showed that a shortage of supplies and general resources was one factor preventing the effective implementation of doctor‐nurse substitution strategies (Basaleem 2009; Basaleem 2011; Mabelane 2016; Mkhabela 2008; Nkhata 2016; Schadewaldt 2016; Walker 2004). Nurses described how a shortage of resources such as equipment and medications added to the difficulty of the working environment. Other studies described a lack of human resources, drugs, and stationery; problems with telephone communication and limited workspace (Basaleem 2011; Mabelane 2016; Vetter‐Smith 2012; Voogdt‐Pruis 2011; Walker 2004). In one study from the US, lack of equity in resource allocation and unequal support were mentioned: "If you have a physician and NP [nurse practitioner] …practicing in a particular place …and the physician wants two rooms, and say there's three rooms, the physician's going to get two …there's no question the physician is going to get two" (Poghosyan 2017).
Nurses' limited access to medicines and equipment was also the main reason for recipients' dissatisfaction with nurse‐delivered care (Basaleem 2009; Basaleem 2011; Leech 2007): "[I] cannot remember when last one has, for instance, received a poster or a pamphlet, apparently there is no money for such things …" (Leech 2007). Nurses were faced with having to turn away recipients and ask them to return for their medication on another day. Other recipients were given medication for only one week at a time and had to return frequently to collect medication. There were also severe shortages in the procurement and distribution systems. Nurses in one study conducted in Yemen reported that the supplies of drugs were inadequate, although they were sure these drugs were present at the central level (Basaleem 2011).
Facility infrastructure such as electricity and water (Friman 2011; Mabelane 2016), and identification of appropriate geographical locations for the facilities were important factors in improving easy access (Coker 2009; Friman 2011). It was important for the nurse to have a private space for the provision of nursing care within the general practice; however, it was not always available (Abbott 2013; Basaleem 2011; Flowers 2008; Friman 2011; Mills 2008a).
Recipient of care flow processes and referrals
An appropriate referral system for recipients of care was important for the effective implementation of doctor‐nurse substitution strategies (moderate confidence; finding #22;Appendix 3). Nurses in some HIC‐based studies referred care recipients on to services within the same facility and in the wider community, and recipients and nurses appreciated this (Bennett 2013; Duane 2015): "From the start we didn't have a clue, yeah, so the nurse came in, she spoke to us about a lot of different services available to us. She sent out referrals for us for them to get in touch with us, which they have" (Duane 2015). This was also appreciated in one LMIC‐based study; however, dysfunctional referral systems and access barriers led to problems (Basaleem 2011).
In one study, nurses reported that they experienced problems if they wanted to liaise with a medical specialist at the hospital or refer a patient to the hospital because the medical specialists stated that they only wanted contact with doctors (Lovink 2018).
Management and leadership vision
Experienced leadership was a facilitator of smooth implementation of doctor‐nurse substitution strategies (moderate confidence; finding #23;Appendix 3). Doctor‐nurse substitution involves the transfer of power and responsibility between different disciplines. Leadership and management of these strategies, therefore, requires a certain level of experience and training (Burns 2009a; Ljungbeck 2017). A nurse from one study from Australia stated that: "There should be somebody that looks after, umbrellas, and the whole practice." (Mills 2008b). According to some nurses, without leadership and insight, effective doctor‐nurse substitution practice is extremely unlikely (Leech 2007).
There was agreement among nurses regarding the philosophy of working collaboratively with management to sustain cultural change and encourage team thinking and collaboration with managers (Burns 2009a; Mills 2008a; Petrova 2015): "… We are family here, a team … everybody helps each other, you know if we see that you're snowed under we will stop seeing patients and help you out and … if you see that we're in strife out there, just help out …" (Mills 2008b).
In one study conducted in the US, nurses perceived that administrators lacked sufficient knowledge about nurses scope of practice, which in some cases negatively impacted how the nurses role was viewed in teams. If administrators were familiar with nurse roles and competencies, they were more likely to support and advocate for these roles (Poghosyan 2017).
Nurses and recipients reported dissatisfaction with the huge number of documents and reports that needed to be completed in connection with doctor‐nurse substitution strategies (moderate confidence; finding #24;Appendix 3). Studies set in both HICs and LMICs reported that implementing doctor‐nurse substitution increased paperwork demands (Basaleem 2011; Flowers 2008; Georgeu 2012). Recipients of care did not like the long list of questions they had to answer when completing forms in order to access to the service. Also, the nurses did not seem to like it (Basaleem 2011; Flowers 2008; Georgeu 2012), and complained of too much paper‐work: "… Look what's happened …paperwork has overtaken client care and basic needs" (Flowers 2008). Basaleem 2011 reported dissatisfaction with the huge number of papers and reports that needed to be completed. One health provider explained: "sometimes we feel we can work better without IMCI [Integrated Management of Childhood Illness]. People in the central level insist on the reports as if it is the essence of IMCI. We are losing time and efforts in preparing reports, time which could be used in managing the child and educating the carer" (Basaleem 2011). Nurses said that paperwork demands in the health system as a whole were onerous; and had been increased by the substitution strategy (Georgeu 2012).
Doctor‐nurse professional boundaries and role clarity
Clear role definitions were critical in the successful implementation of doctor‐nurse substitution strategies (moderate confidence; finding #25;Appendix 3). Development of clear role definitions and descriptions was seen to be important by both nurses and doctors (Kraus 2017; Lindblad 2010; Lovink 2018; McKenna 2015; Poghosyan 2017; Schadewaldt 2016; Stephen 2018). Nurses believed that lack of awareness of the role boundaries might negatively affect practice (Peterson 2007). Limited data were available on the legal aspects of doctor‐nurse substitution. It seemed that in countries with legally defined referrals and supervisory requirements and clear lines of responsibilities for advanced roles for nurses (e.g. the UK and the USA), nurses had secure positions and established roles. The legal systems would identify the nurses' powers and limits of their ability for doing tasks, making referrals or supervisory requirement (Coulter 2000; Hamel 2017; Kraus 2017). One study conducted in an HIC noted that the support of general practitioners alongside the legal scope of nurses' practice resulted in nurses conducting independent assessment and planning of care for children (Drew 2002; Drew 2003).
In another HIC‐based study, an obstetrician stated that nurses and doctors struggled with each other to gain power in some labour and delivery units (Peterson 2007). Where the independence and authority of nurses was not established, this negatively affected their morale and potentially their practice (Flowers 2008; Mills 2008a).
Supervision
Where nurses were supervised by doctors, the quality of this supervision was central to the building of confidence in both partners (moderate confidence; finding #26;Appendix 3). Nurses were more likely to work in collaborative roles (Coulter 2000; Courtenay 2010; Ljungbeck 2017), follow doctors' orders (Kassean 2005; Kraus 2017), or work as 'lone providers' (Mkhabela 2008), and there were limited situations where nurses were actively supervised by doctors (Lindblad 2010). In environments with hierarchical relationships between doctors and nurses (i.e. one in which doctors acted as supervisors), supervision of doctors or the independency of nurses depended on the capacity and availability of doctors, the actual organisational settings and the legal framework informing nursing services (Coulter 2000; Drew 2002; Drew 2003). The scope of the nurse practitioner is clearly delineated in law in the UK. This allows nurses to act more independently with less supervision and support from doctors (Drew 2002; Drew 2003). The quality of supervision was central to the building of confidence in both partners (Lindblad 2010).
Nurses in LMIC settings appeared to lack effective supervision (very low confidence; finding #27;Appendix 3). While structures and procedures for clinical supervision were in place, nurses in LMICs felt that these did not always work effectively in practice and they were not provided with useful feedback (Basaleem 2011; Leech 2007). A nurse commented: "Yes, we usually meet with our assistant director. So, she does not say anything whether you must keep your good work or what, so that you do not know whether you are working fine …" (Leech 2007). The lack of effective supervision, together with inadequate communication and support, made some nurses feel that they were lone providers of care: "I don't know. It feels as if we are functioning alone, I mean without support. You must rely on your knowledge and take care to stay within, carry on according to the protocols" (Leech 2007).
Integrating the findings from this synthesis with the findings of the relevant Cochrane effectiveness review
One of our objectives was to integrate the findings of this QES with those of the relevant Cochrane intervention review of effectiveness, so as to enhance and extend understanding of how these complex interventions work and how context impacts implementation. However, our ability to fully integrate findings from this synthesis with the 18 trials in Laurant's intervention review was limited by several factors (Laurant 2018). First, only two of the qualitative studies were related to the trials and there were several differences between the contexts of the qualitative studies and the contexts of the trials. Second, although we attempted to create a maximum variation sample covering high‐, middle‐ and low‐income settings, the same level of variation was not seen in the corresponding intervention review of effectiveness, which included 18 trials, 17 of which were delivered in high‐income contexts. Third, by including a wide time span of qualitative evidence published between 1999 and 2018, it was challenging to determine the temporal nature of practice development and to identify if implementation factors identified in the late 1990s were still current in contemporary practice. These three factors meant that it was not clear if the contexts of the qualitative studies and interventions are sufficiently similar to attempt full data integration or draw meaningful conclusions. Fourth, our assessment of the trial interventions was reliant on the availability of detailed explanations in the trial reports, which typically are not required to meet CONSORT or TIDieR (Template for Intervention Description and Replication) reporting standards. Therefore, the lack of congruity between the qualitative evidence and the trial reports and other related outputs may be a trial reporting issue. Finally, the qualitative evidence synthesis may not have identified the full range of implementation factors and processes that may have influenced the implementation of the trial interventions.
Nonetheless, our synthesis identified several factors that appear to have influenced the implementation of doctor‐nurse substitution strategies. Table 4 compared the interventions and populations/contexts in the intervention review of effectiveness with our QES. The qualitative studies and trials differed with regard to which countries they were from. The qualitative studies also differed somewhat in the types of healthcare topics they were dealing with. Some topics were dealt with in both the studies and the trials (e.g. family healthcare, chronic disease care, HIV care). However, the qualitative studies also explored the use of nurses in several areas not covered by the trials, including child health care by nurses (Basaleem 2009; Basaleem 2011; Coker 2009; Flowers 2008; Leech 2007); anticipatory 'proactive care' (Bennett 2013); alcohol screening, brief intervention and referral to treatment (Broyles 2012); clinical leadership of expert nurses (Burns 2009a; Burns 2009b); establishing nurse practitioner‐led, family‐focused primary healthcare clinics based in a primary school environment (Clendon 2001; Clendon 2003); nurse prescribing (Courtenay 2010; Maddox 2016; Ross 2015; Stenner 2010; Stenner 2011); nurses taking on advanced skills in rural settings (Carryer 2017; Francis 2013; Leipert 2011); screening young people for health risks and provide a brief intervention for detected risks (Hart 2012); chlamydia testing (Lorch 2015); maternity care (Peterson 2007; James 2003); healthcare for older people (Ljungbeck 2017; Lovink 2018); hypertension management (Stephen 2018); and nurse‐delivered cardiovascular prevention at primary care level (Voogdt‐Pruis 2011).
3. Interventions, participants/context in the effectiveness review and comparison with the interventions in primary studies of our QES.
| Intervention categories | Effectiveness review | Similar Interventions in our QESa |
| Triage |
Intervention Nurse‐led computer‐supported telephone triageb Participants/country context patients, practices/UK |
N/A |
| Family healthcare |
Intervention Families allocated to nurse‐led primary carec Participants/country context patients, nurse, doctor/Canada |
Parfitt 2007 |
|
Intervention Families allocated to nursed Participants/country context patients, nurses, doctors/Canada | ||
| Nursing care after invasive procedures |
Intervention Patient care after gastric endoscopy allocated to nursee Participants/country context Patients, 1 nurse and unknown number of doctors/UK |
N/A |
| General practice/primary healthcare by nurses |
Intervention Patients allocated to nurse practitionersf Participants/country context Patients, GPs, nurse practitioners/Netherlands |
Albers‐Heitner 2011; Bailey 2006; Branson 2008; Cheek 2002; Coulter 2000; Duane 2015; Fortin 2010; Hamel 2017; Kraus 2017; Lindblad 2010; Marsden 2004; McKenna 2015; Mills 2008a; Mills 2008b; Perry 2005; Petrova 2015; Poghosyan 2017; Rosemann 2006; Schadewaldt 2016; Twinn 1999; Walker 2015 |
|
Intervention Patients allocated to nurse‐led primary careg Participants/country context Patients, nurses, doctors/USA | ||
|
Intervention Patients allocated to nurse‐led careh Participants/country context Patients, unknown numbers of nurses and doctors/USA | ||
|
Intervention Patients allocated to nurse‐led carei Participants/country context Patients, nurses, doctors/USA | ||
|
Intervention Patients allocated to nursej Participants/country context Patients, nurses, doctors/UK | ||
|
Intervention Patients allocated to nursek Participants/country context Patients, nurses, doctors/UK |
— | |
| Chronic diseases care |
Intervention Patients with T2DM allocated to nurse practitionersl Participants/country context Participants: patients, nurses, doctors/Netherlands |
Nurse consulting with patient diagnosed dementia (Drew 2002; Drew 2003); treating acute and chronic wound care by district nurses (Friman 2011); Integration of nurses in long‐term care settings (Kaasalainen 2013); nurses diabetes care in primary care (Boyle 2016; Dennis 2016; Kassean 2005; Vetter‐Smith 2012). |
|
Intervention Patients monitored by a nurse, later monitored by a rheumatologistm Participants/country context Patients, nurses, unknown number of rheumatologists/Sweden | ||
|
Intervention Patients with coronary heart disease allocated to nurse‐led follow‐upn Participants/country context Patients, unknown numbers of nurses and doctors/UK | ||
|
Intervention People with rheumatoid arthritis allocated to nurse‐led careo Participants/country context Patients, nurses, doctors (rheumatologists)/UK | ||
|
Intervention Patients at cardiovascular risk allocated to practice nursesp Participants/country context Patients, practice nurses, GPs/Netherlands | ||
| Same‐day care; out‐of‐hours callings |
Intervention Intervention: care delivered by nurses to patients asking for same‐day appointmentq Participants/country context Patients, GPs, nurses/Spain |
N/A |
|
Intervention Nurse call management during out‐of‐hoursr Participants/country context Patients, nurses, doctors/UK | ||
| HIV/sexually transmitted disease/TB care |
Intervention Patients with HIV allocated to nursess Participants/country context Patients, nurses, medical officers/South Africa |
Abbott 2013; Corneli 2008; Georgeu 2012; Halcomb 2013; Ivers 2011; Mabelane 2016; Mkhabela 2008; Nkhata 2016; Rustagi 2015a |
aOther QES interventions: child health care by nurses (Basaleem 2009; Basaleem 2011; Coker 2009; Flowers 2008; Leech 2007); anticipatory 'proactive care' (Bennett 2013); alcohol screening, brief intervention and referral to treatment (Broyles 2012); clinical leadership of expert nurses (Burns 2009a; Burns 2009b); establishing nurse practitioner‐led, family‐focused primary healthcare clinics based in a primary school environment (Clendon 2001; Clendon 2003); nurse prescribing (Courtenay 2010; Maddox 2016; Ross 2015; Stenner 2010; Stenner 2011); nurses taking on advanced skills in rural settings (Carryer 2017; Francis 2013; Leipert 2011); screening young people for health risks and providing a brief intervention for detected risks (Hart 2012); chlamydia testing (Lorch 2015); maternity care (James 2003; Peterson 2007); healthcare for older people (Ljungbeck 2017; Lovink 2018); hypertension management (Stephen 2018); and nurse‐delivered cardiovascular prevention at primary care level (Voogdt‐Pruis 2011).
bCampbell 2013; cChambers 1978; dSpitzer 1973; eChan 2009; fDierick‐van Daele 2010a; gHemani 1999; hLewis 1967; iMundinger 2000; jShum 2000; kVenning 2000; lHouweling 2011; mLarsson 2014; nMoher 2001; oNdosi 2014; pVoogdt‐Pruis 2010; qIglesias 2013; rLattimer 1998; sSanne 2010.
GP: general practitioner; N/A: not applicable; NP: nurse practitioner; QES: qualitative evidence synthesis; T2DM: type 2 diabetes mellitus.
In Table 5, we present our matrix model in which we mapped factors influencing the implementation of doctor‐nurse substitution strategies against the interventions in studies included in Laurant 2018. This matrix provides a useful overview of how the findings of this QES are reflected in the content of the interventions in the trials included in the related effectiveness review (Laurant 2018).
4. Mapping key questions regarding implementation factors identified in the QES onto the findings of relevant Cochrane effectiveness review (Laurant 2018).
| Intervention studies included in the Laurant 2018review | Key questions regarding implementation factors for nurse‐doctor substitutiona | |||||||||
|
1 Information shared with service users |
2 Increase doctors' trust in substitution |
3 Effective communication between nurses and doctors |
4 Service users can easily access nurses |
5 Nurses receive appropriate training |
6 Taskshifting facilitates continuity of care |
7 Factors motivating nurses addressed |
8 Necessary resources available |
9 Appropriate supervision in place |
10 Role boundaries defined clearly |
|
| Campbell 2013 | No | No | No | No | Yes | No | No | No | No | No |
| Chambers 1978 | No | No | No | No | Yes | No | No | No | No | No |
| Chan 2009 | No | No | No | No | No | No | No | No | No | Yes |
| Dierick‐van Daele 2009 | No | No | Yes | No | Yes | No | No | No | No | Yes |
| Hemani 1999 | No | No | No | No | No | No | No | No | No | Yes |
| Houweling 2011 | No | No | No | No | Yes | No | No | No | No | Yes |
| Iglesias 2013 | No | No | No | No | Yes | No | No | Yes | No | No |
| Larsson 2014 | No | No | No | Yes | Yes | No | No | No | No | Yes |
| Lattimer 1998 | No | No | No | No | Yes | No | No | Yes | No | Yes |
| Lewis 1967 | No | No | No | No | No | No | No | Yes | No | No |
| Moher 2001 | No | No | No | No | Yes | No | No | Yes | No | No |
| Mundinger 2000 | No | No | No | No | No | No | No | No | No | Yes |
| Ndosi 2014 | No | No | No | No | No | No | No | No | No | Yes |
| Sanne 2010 | No | No | No | No | Yes | No | No | No | No | No |
| Shum 2000 | No | No | No | No | No | No | No | No | No | Yes |
| Spitzer 1973 | Not available | Not available | Not available | Not available | Not available | Not available | Not available | Not available | Not available | Not available |
| Venning 2000 | No | No | No | No | No | No | No | No | No | No |
| Voogdt‐Pruis 2010 | No | No | Yes | No | No | No | No | No | No | No |
Campbell 2013: UK; intervention: nurse‐led computer‐supported telephone triage; participants: patients, practices.
Chambers 1978: Canada; intervention: families allocated to nurse‐led primary care; participants: patients, nurse, doctor.
Chan 2009: UK; intervention: patient care after gastric endoscopy allocated to nurse; participants: patients, 1 nurse and unknown number of doctors.
Dierick‐van Daele 2009: Netherlands; intervention: patients allocated to nurse practitioners; participants: patients, GPs, NPs.
Hemani 1999: USA; intervention: patients allocated to nurse‐led primary care; participants: patients, nurses, doctors.
Houweling 2011: Netherlands; intervention: patients with type 2 diabetes mellitus allocated to nurse practitioners; participants: patients, nurses, doctors.
Iglesias 2013: Spain; intervention: care delivered by nurses to patients asking same‐day appointment; participants: patients, GPs, nurses.
Larsson 2014: Sweden; intervention: patients monitored by a nurse, later monitored by a rheumatologist; participants: patients, nurses, unknown number of rheumatologists.
Lattimer 1998: UK; intervention: nurse call management during out‐of‐hours; participants: patients, nurses, doctors.
Lewis 1967: USA; intervention: patients allocated to nurse‐led care; participants: patients, unknown numbers of nurses and doctors.
Moher 2001: UK; intervention: patients with coronary heart disease allocated to nurse‐led follow‐up; participants: patients, unknown numbers of nurses and doctors.
Mundinger 2000: USA; intervention: patients allocated to nurse‐led care; participants: patients, nurses, doctors.
Ndosi 2014: UK; intervention: people with rheumatoid arthritis allocated to nurse‐led care; participants: patients, nurses, doctors (rheumatologists).
Sanne 2010: South Africa; intervention: patients with HIV allocated to nurses; participants: patients, nurses, medical officers.
Shum 2000: UK; intervention: patients allocated to nurse; participants: patients, nurses, doctors.
Spitzer 1973: Canada; intervention: families allocated to nurse; participants: patients, nurses, doctors.
Venning 2000: UK; intervention: patients allocated to nurse; participants: patients, nurses, doctors.
Voogdt‐Pruis 2010: Netherlands; intervention: patients at cardiovascular risk allocated to practice nurses; participants: patients, practice nurses, GPs.
aQuestion 1: Is information being communicated to service users on the task/s that will be delivered by nurses rather than doctors, and about the roles that nurses will play in their care?
Question 2: Have efforts been made to increase doctors' trust in and acceptability of using nurses to substitute for doctors? For instance, have there been any attempts to reassure doctors that nurses have the necessary skills and training to take on the designated task/s? Does implementation of the specific task substitution reduce doctors' workloads? Does implementation of doctor‐nurse substitution for the specific tasks reduce doctors' workloads without leading to a reduction in their salary or other payments?
Question 3: Are processes in place that allow doctors and nurses to communicate effectively and provide feedback to one another concerning specific task‐shifting strategies?
Question 4: Can service users easily access the nurses who have been designated to deliver the specific substituted task/s?
Question 5: Have nurses received appropriate training and tailored feedback regarding the specific substituted task/s that they have been requested to deliver?
Question 6: Does the substituted task facilitate continuity of care for patients?
Question 7: Have attempts been made to ensure that factors affecting nurses' internal motivation (such as job satisfaction and independent work) and external motivation (such as improved working conditions and financial issues) are addressed?
Question 8: Are the necessary resources (financial, infrastructural, facilities, and drugs and equipment) available to nurses taking on new task/s?
Question 9: Have appropriate supervisory and monitoring arrangements been put in place for the specific substituted task/s?
Question 10: Are doctor/nurse role boundaries clearly defined for the specific substituted task/s?
Our matrix indicated that few of the factors identified as important in our synthesis appeared to have been specifically taken account of in the 18 studies included in Laurant 2018. Interventions and implementation processes included in the Laurant 2018 review took account of between none to five of the factors our synthesis identified as influencing the implementation of doctor‐nurse substitution strategies. As the trials measured different outcomes among different populations, it was difficult to compare the effectiveness of the interventions with respect to whether they took account of more factors in their implementation process. It seemed that the strategies were implemented only within an available and present set of structural resources with no official plan to provide the rationale; and there were no attempts made to make extra efforts or support changes (such as changing doctors' attitudes, enhancing nurses' motivations, etc.) through the substitution strategy.
Nine of the intervention processes made attempts to ensure that nurses received training and tailored feedback regarding tasks they should deliver. Nine of the studies reported clearly defined professional boundaries and roles of both partners and used a supervision mechanism. Four studies attempted to provide adequate financial, infrastructural, facilities, drugs and equipment resources. Two studies considered effective communication and personal contacts between doctors and nurses. In one intervention, patients had the opportunity to contact the nurse during the 12‐month trial period. None of the trials reported information regarding the increasing doctors' trust in and acceptability of doctor‐nurses substitution among doctors; information that might be communicated to patients on the type of substituted tasks delivered by nurses; meeting nurses' internal and external motivations; ensuring the appropriateness of the supervisory and monitoring arrangements; and the impact of substituted tasks on continuity of care for patients.
Identifying hypotheses for future subgroup analysis
Our final objective was to identify hypotheses that could be used to design subgroup analyses of future updates of the intervention review of effectiveness. During the QES process, we identified 'setting' as a factor that might explain heterogeneity in the intervention review results (Laurant 2018). Table 6 showed the QES findings across country income levels. The LMIC‐based studies mainly dealt with tasks that were delivered by nurses or expanded for nurses on HIV/AIDS care, TB care, diabetes primary care and infant development care. In HICs, the aspects of the care covered were broader and included tasks such as cervical cancer screening, osteoarthritis care, mental health, prescription and wound care. Though country income level was not identified a priori, comparing these tasks between the country income levels can enable us to generate evidence that was directly relevant to LMICs, develop hypotheses on the applicability of studies from HICs to LMICs, and draw lessons from HICs for use in LMICs.
5. Review findings across country income levels.
| Findings |
HIC (No. of studies) |
LMIC (No. of studies) |
|
| 1 | Recipients of care had mixed views about the expansion of tasks undertaken by nurses. They preferred doctors when the tasks were more 'medical' in nature and they accepted nurses for preventive care and follow‐ups. | 12 | — |
| 2 | Doctors in most studies also preferred that nurses performed only non‐medical tasks. | 14 | 2 |
| 3 | Nurses were comfortable with, and believed they were competent to deliver, a wide range of tasks, but particularly tasks that were more health promotive/preventive in nature. | 12 | 1 |
| 4 | Recipients of care in most studies believed that nurses were more easily accessible than doctors. | 8 | 2 |
| 5 | Both doctors and nurses saw doctor‐nurse substitution and collaborative practice as a way of increasing quick access to care for certain tasks such as maternity care and prescriptions. | 6 | — |
| 6 | Recipients of care in most studies were satisfied with nurses' social skills. Recipients' perceptions of nurses' technical skills were mixed. | 14 | 3 |
| 7 | Health professionals, including doctors, nurses, policymakers and other healthcare providers, believed that doctor‐nurse substitution led to improvements in the quality of care. | 12 | 2 |
| 8 | A close doctor‐nurse relationship characterised by trust and mutual respect helped nurses to expand and develop their roles. | 9 | 2 |
| 9 | Nurses might find it difficult to communicate effectively with colleagues in stand‐alone practices or vertical programmes of care. | 3 | 2 |
| 10 | Doctors' trust in and acceptance of nurses was a critical factor that shaped the extent of nursing practice. | 15 | 3 |
| 11 | Financial issues might damage the relationship between doctors and nurses. | 6 | — |
| 12 | Nurses felt they had gained additional skills through task‐shifting. However, they believed that further training and education could increase their skills, job satisfaction and motivation; allow them to work more independently; and increase others' acceptance of their professional roles. | 14 | 5 |
| 13 | Nurses had concerns about their training in terms of adequacy, equity and quality. | 6 | 3 |
| 14 | Recipients of care in many studies had limited knowledge about nurses' roles in primary care, nurse models of care and any differences between nurse‐led and doctor‐led care. | 6 | 1 |
| 15 | Doctors in some studies felt that doctor‐nurse substitution improved the continuity of care and believed that recipients of care would prefer to see the same nurse rather than different doctors. | 2 | — |
| 16 | Recipients of care in some studies were concerned over the continuity of care provided by nurses and felt insecure if they lost contact with their doctors. | 3 | 1 |
| 17 | Internal motivations most frequently cited by nurses regarding task‐shifting were psychological (including personal development and being respected) and professional (improving the quality of care). | 11 | 2 |
| 18 | Nurses believed that external motivations such as improved working conditions and financial incentives could act as an incentive to take on more responsibilities. | 7 | 2 |
| 19 | Doctors valued the contribution of nurses in collaborative practices when this reduced their own workload. | 11 | 1 |
| 20 | In settings where a proportion of doctors' revenues came from fee‐for‐service payments, doctors expressed negative reactions towards doctor‐nurse substitution. | 3 | — |
| 21 | A shortage of resources, including human resources, equipment and supplies, and lack of equity in how organisational resources were allocated, sometimes negatively impacted on the effective implementation of doctor‐nurse substitution strategies. | 8 | 8 |
| 22 | An appropriate referral system for recipients of care was important for the effective implementation of doctor‐nurse substitution strategies. | 3 | 1 |
| 23 | Experienced leadership was a facilitator of smooth implementation of doctor‐nurse substitution strategies. | 5 | 1 |
| 24 | Nurses and recipients reported dissatisfaction with the huge number of documents and reports that needed to be completed in connection with doctor‐nurse substitution strategies. | 1 | 2 |
| 25 | Clear role definitions were critical in the successful implementation of doctor‐nurse substitution strategies. | 13 | — |
| 26 | Where nurses were supervised by doctors, the quality of this supervision was central to the building of confidence in both partners. | 6 | 2 |
| 27 | Nurses in LMIC settings appeared to lack effective supervision. | — | 2 |
HIC: high‐income country; LMIC: low‐ to middle‐income country.
Studies included in this QES were conducted across a wide period of time from very early in the timeline of practice development for doctor‐nurse substitution (2001) to present (2018), when there is a more general acceptance of doctor‐nurse substitution. The age of included studies should be considered for future subgroup analysis.
Laurant's review also showed that the nursing level was often unclear or varied between and even within studies and this should be addressed in trial and qualitative reports (Laurant 2018).
Discussion
Summary of main results
This synthesis included 66 primary qualitative studies (69 papers) from 25 countries. We have synthesised the views and experiences of different stakeholders involved in doctor‐nurse substitution strategies, and identified a number of factors influencing the successful implementation of doctor‐nurse substitution strategies.
Our QES showed that:
Experienced leadership facilitated the effective implementation of doctor‐nurse substitution strategies; however, a shortage of resources, including human resources, equipment and supplies, sometimes negatively impacted on the effective implementation of these strategies. Our QES also showed that recipients of care in most studies believed that nurses were more easily accessible than doctors; and nurses reported internal factors (i.e. psychological and professional ) and external factors (e.g. improved working conditions and financial incentives) that motivated them in delivering a wide range of tasks;
Recipients of care had mixed views about the expansion of tasks undertaken by nurses. They preferred doctors when the tasks were more 'medical' in nature and they accepted nurses for preventive care and follow‐up care. In many studies, recipients of care had limited knowledge of nurses' roles in primary care, of nurse models of care, and of any differences between nurse‐led and doctor‐led care;
Nurses were comfortable with, and believed they were competent to deliver, a wide range of tasks, but particularly emphasised tasks that were more health promotive / preventive in nature. However, nurses working in stand‐alone practices or vertical programmes of care sometimes found it difficult to communicate effectively with colleagues. Where nurses were supervised by doctors, the quality of this supervision was central to the building of confidence in both partners. Nurses had concerns about their training in terms of adequacy, equity and quality. They felt they had gained additional skills through task‐shifting. However, they believed that further training and education could increase their skills, job satisfaction and motivation, allowing them to work more independently and increase others' acceptance of their new professional roles. Nurses believed that external motivator such as improved working conditions and financial incentives could act as an incentive to take on more responsibilities. Nurses and recipients of care reported dissatisfaction with the huge number of documents and reports that needed to be completed in connection with doctor‐nurse substitution strategies;
Doctors in most studies preferred that nurses performed only non‐medical tasks. Doctors in some studies felt that doctor‐nurse substitution improved continuity of care and believed that recipients of care would prefer to see the same nurse rather than different doctors. Doctors valued the contribution of nurses in collaborative practices when this reduced their own workload. Both doctors and nurses saw doctor‐nurse substitution and collaborative practice as a way of increasing quick access to care in certain areas such as maternity care. Health professionals, including doctors, nurses, policymakers and other healthcare providers, believed that doctor‐nurse substitution led to improvements in the quality of care received by patients;
A close doctor‐nurse relationship characterised by trust and mutual respect helped nurses to expand and develop their roles. Doctors' trust in and acceptance of nurses was a critical factor that shaped the extent of nursing practice. However, the studies also showed that financial issues could damage relationships between doctors and nurses;
Clear role definitions and appropriate referral systems for recipients of care were critical to successfully implementing doctor‐nurse substitution strategies.
Summary of integrating the findings from this synthesis with the findings of relevant Cochrane effectiveness reviews
There were gaps in evidence and a mismatch between the contexts of the trials and of qualitative studies (Table 4). Our attempt to integrate the qualitative and effectiveness evidence is therefore partial and incomplete. Nonetheless, it does provide some high‐level and relevant insights that can inform decision‐making.
Our high‐level and limited comparison of the findings of the QES and the effectiveness review suggests that a limited number of the factors identified as important in our synthesis were specifically addressed when implementing the 18 interventions evaluated in the Laurant 2018 effectiveness review (Table 5). Specifically, interventions included in the Laurant 2018 review considered between none to five of our identified factors, including easy access of patients to nurses to deliver the specific substituted task; nurses' training and tailored feedback regarding the specific substituted tasks that they are requested to deliver; the availability of necessary resources (financial, infrastructural, facilities, drugs and equipment) for nurses taking on new tasks; defining clear boundaries and the new roles of both nurses and doctors; and effective communication and personal contacts between doctors and nurses.
Overall applicability and completeness of evidence
This QES is one of a series of reviews of qualitative research that aimed to inform the World Health Organization's "Recommendations for Optimizing Health Worker Roles to Improve Access to key Maternal and Newborn Health Interventions through Task Shifting" (OPTIMIZEMNH) (WHO 2012).
Our sampling strategy helped us to achieve variation in the settings, populations and forms of task‐shifting addressed in the included studies. Moreover, all studies we included explored issues raised by key stakeholders. All of the included studies made use of individual or group interviews and focus group discussions as their main method of data collection. Six studies used some form of observation alongside interviews.
Most studies included in our QES were from high‐income urban settings. However, the impacts of this on the overall completeness of the evidence is unclear. While the experiences and perceptions of doctor‐nurse substitution strategies are context‐ and programme‐specific, participants in studies from poorly resourced healthcare systems such as those in many LMICs seemed to have similar expectations and experiences around substitution strategies and their implementation.
Some primary studies included in this QES were undertaken a number of years ago, very early in the timeline of practice development for doctor‐nurse substitution. In many setttings, there is now more general acceptance of doctor‐nurse substitution; and many doctor‐nurse substitution strategies have become routine practice in HICs. In these settings, tasks have been assimilated by nurses and are no longer considered a form of substitution. This is particularly the case for advanced practice roles, such as diabetes nurse practitioners. Evidence from the early studies included in our QES suggested concerns about the lack of specific training for advanced practice roles. However, in HICs and some LMICs the postgraduate training of nurses has evolved significantly since the late 1990s to support the implementation of doctor‐nurse substitution strategies.
Our findings did not cover all areas of implementation. We used an adapted version of the SURE framework as an a priori framework of themes and categories (SURE Collaboration 2011). However, we did not identify data in relation to the 'social and political constraints' category of the framework, including with regard to ideology, short‐term thinking, contracts, legislation or regulations, donor policies, influential people, corruption, and political stability. This does not imply that these factors are not important, only that we did not identify studies addressing these topics. Moreover, comparing our findings with the list of key dimensions of implementation presented by Cargo and colleagues showed that some dimensions of implementation were not highlighted in our included studies (Cargo 2018). These dimensions included: 'recruitment' (specific information on procedures used to recruit or attract participants to the intervention); 'fidelity' (implementation integrity, adherence and extent to which a programme was implemented as intended); 'co‐intervention' (when interventions other than the treatment were applied differently to intervention groups); 'contamination' (unintentional delivery of the intervention to the control group or inadvertent failure to deliver the intervention to the experimental group); 'participant engagement' (participant's interaction with or receptivity to a programme); 'implementer engagement' (subjective staff attributes that influence programme delivery); and 'context' (social, built and political factors internal and external to the intervention environment) (Cargo 2018).
In assessing whether these findings are likely to be applicable to their setting, users of our findings may want to consider the following factors (adapted from Lavis 2009): firstly, users should consider whether the settings of the studies contributing to a review finding are similar to the setting in which the findings will be applied. Secondly, users should consider possible differences between the political, social and cultural contexts of the included studies and the contexts in which the findings will be applied. For instance, the extent to which people trust physicians and nurses to undertake medical procedures and nurses' independence in relation to practice. Thirdly, users should consider whether there are important differences in health system arrangements (e.g. the presence or absence of hierarchical relations between doctors and nurses; the extent to which the health system is organised to support nurse substitution through appropriate training, supportive supervision and monitoring and the provision of commodities) that may mean that the factors affecting the implementation of nurse‐doctor substitution in the setting of interest may be different to those in which the studies were conducted.
Doctor‐nurse substitution is often considered a challenging topic among health providers and professionals who may have discipline‐specific views and experiences. Future research on stakeholders' perspectives about substitution strategies should consider how participants perceive these issues, as this may influence their willingness to participate as well as their responses. In addition, for many of the included studies it was not possible to determine the backgrounds of the people recruiting study participants, especially recipients of care, or the backgrounds of those collecting data. This information is important as researchers' perspectives may influence the manner in which they collect, analyse and interpret data on this topic. For example, researchers with a nursing background may interpret data in a manner favourable to doctor‐nurse substitution. Very few studies, however, discussed researcher reflexivity in a meaningful way.
Confidence in the findings
The GRADE‐CERQual approach allowed us to assess the extent to which each review finding is a reasonable representation of the phenomenon of interest (Lewin 2015).Based on our CERQual assessments, the review includes four findings in which we have high confidence and 19 findings in which we have moderate confidence that the findings are a good representation of the phenomenon of interest. The review also includes four findings in which we have low or very low confidence. It was difficult to draw conclusions from these low and very low confidence findings. We have reported these assessments in Table 1.
For each of the primary studies that contributed evidence to an individual review finding, we attempted to assess any concerns regarding methodological limitations as part of our CERQual assessment for each finding. We assessed 15 studies to have 'moderate to severe' or 'severe' methodological limitations. The main reasons for downgrading for methodological limitations were poor sampling and poor methods reporting. In addition, few included studies discussed researcher reflexivity.
We downgraded findings because of concerns about relevance mainly when the setting or population of studies contributing to a finding was only partially relevant. Most studies in this review were from high‐income, urban settings. Our sampling strategy helped us to select studies that encompassed different forms of task‐shifting, including outright substitution (i.e. where doctors had been replaced by nurses); task development (i.e. where the formal roles of nurses had been expanded); and situations in which clinical tasks were assigned to nurses due to resource constraints or system inadequacies and inefficiencies that had resulted in such tasks not being covered by doctors.
We typically downgraded a finding for concerns about coherence when some of the data from the included studies contradicted the review finding or when it was not clear if some of the underlying data supported the review finding. Downgrading due to data adequacy mainly related to the limited number of studies and the thinness of the data contributing to many of the findings.
Agreements and disagreements with other studies or reviews
To our knowledge, this is the first QES to explore factors affecting the implementation of doctor‐nurse substitution globally. In recent years, other authors have also published systematic reviews of qualitative studies on task‐shifting in primary care, although these have focused on midwives globally (Colvin 2013), nurses in the UK (Rashid 2010), and lay health workers globally (Glenton 2013).
A QES conducted by Colvin and colleagues in 2013 (Colvin 2013) on barriers and facilitators to the successful implementation of task‐shifting to and from midwives included 37 studies. Most studies assessed the perspectives of midwives themselves, with few studies exploring the perspectives of health workers, supervisors, or the recipients of midwifery services. As in our review, the majority of included studies (26/37) were conducted in HIC settings. Task‐shifting emerged in several of the studies as something that often happened without an official plan or formal rationale in place. In these studies, lack of staff, poor access to care, poor outcomes, or unclear divisions of roles and responsibilities typically resulted in what one study described as 'ad hoc' forms of task‐shifting among health staff. In the Colvin review, a very large range of tasks was shifted downward and midwives, like the nurses in the studies included in our QES, often supported the intention behind many of these upskilling initiatives and derived job satisfaction from them. These forms of task‐shifting were accompanied by internal and external motivators such as promotion opportunities, a sense of achievement and clinical confidence, heightened job satisfaction from being able to help sicker or a greater number of people, improved overall practice and skills, and in some cases, improvements in quality and continuity of care. As in our review, the review of task‐shifting among midwives also showed that those trying to implement task‐shifting faced several challenges including poor clinical support and supervision, inadequate training, haphazard implementation of new programmes and working relationships, and insufficient educational preparation. In addition, the review on task‐shifting to and from midwives showed that lack of clarity regarding legal and regulatory issues could act as important barriers to successful task‐shifting.
The Colvin review also described how doctors often seemed unaware of the knowledge and skill sets of the midwives they worked with (Colvin 2013). Our QES also showed the importance of increasing doctors' trust in and acceptability of task substitution, and of assuring doctors that nurses have the necessary skills and training to take on new tasks. As in our QES, the midwife taskshifting review also highlighted how stakeholders saw task‐shifting initiatives as requiring some form of training, as well as follow‐up support and supervision, as part of implementation. Studies that assessed training programmes for new clinical knowledge and skills found that midwives generally had no problem absorbing new information and practicing new techniques. However, midwives expressed the greatest anxiety around tasks where they were expected to undertake complex new responsibilities with little substantive training. Whatever the initial education, experience or training, most of the studies addressing training argued that ongoing support and clinical supervision were also critical. This finding was also consistent with the findings of our QES.
Rashid 2010 explored the benefits and limitations of the expansion of clinical tasks among nurses working in general practice in the UK through an integrative review of eight studies. The evidence suggested that the increase in workload arising from a new general practitioner contract drove the changes in nurses' role. Increasing workload was also identified in our QES as one of doctors' motivators for accepting task shifting to nurses. Patients generally thought that all general practice nurses would be able to deal with simple conditions, but wanted to be able to consult with a general practitioner if they thought it necessary. Our QES showed also that recipients of care preferred doctors when the tasks were more 'medical' in nature and accepted nurses for preventive care and follow‐ups.
Another QES explored factors affecting the implementation of lay health worker programmes for maternal and child health and included 53 studies from multiple settings (Glenton 2013). In both this QES and our review, recipients of care were generally positive about task‐shifting. Another similarity to our findings was that most health professionals appreciated lay health workers' contributions to reducing their workload and also their communication skills and commitment. However, some health professionals thought that lay health workers added to their workload and feared a loss of authority. Although task‐shifting has the potential to free up the time of providers with higher levels of training, other work has shown that total productivity may be reduced if a limited demand exists for alternative uses of providers' skills (Janowitz 2012).
Our QES showed that nurses expressed the need for increased knowledge and skills, training, supervision and tailored feedback. It is evident that nurses must be adequately trained to act as substitutes for doctors (WHO 2008; WHO 2012). However, there is no agreement as to the level of training required for nurses to undertake the specific roles covered by this QES, and no consistency in the qualifications nurses must have to merit job titles such as 'nurse practitioner'. Rashid 2010 expressed concerns about nurses' knowledge base, particularly in diagnostics and therapeutics, and their levels of training and competence in roles formerly undertaken by general practitioners. There have been few studies in this key area of healthcare policy. There is a need for better training and support for nurses undertaking expanded roles and for patients' views to be better represented in this training. Lay health workers in Glenton 2013 also described insufficient, poor‐quality, irrelevant and inflexible training programmes, and called for more training in counselling and communication and in topics outside their current role, including common health problems and domestic problems.
Several studies have observed a successful expansion of the role of nurses in a wide range of health services (Laurant 2018; Maier 2016). The definition of roles and associated competency levels are seen as key elements in a successful task‐shifting strategy (WHO 2008), particularly in out‐of‐hours primary care where teams constantly change and team members are often unfamiliar with each other's competencies (van der Biezen 2017a). Other studies, however, have described significant variation across settings in the roles and work of practice nurses (Halcomb 2005). The views of stakeholders on substitution vary from extending nurses' roles to the complete substitution of doctors. While nurses often see substitution as a way of strengthening and expanding the role of the nurse, doctors often see substitution as a way of replacing and supporting doctors, and as a way of creating a bridge between doctors and nurses. In HICs, the degree to which nurses can work independently from doctors was seen to be linked to the legal and regulatory framework of nursing practice in these countries. Doctors agreed on the importance of boundaries of care to avoid confusion and disorder in the provision of care. There are several explanations for why a nurse's role might not be clear. First, as mentioned by Halcomb 2005, the scope of the practice nurse's work is defined through negotiation between doctor and nurse. Second, in many cases, the introduction of new roles such as expanded nurses' roles has occurred in response to perceived local needs rather than a central government plan, as emphasised by the WHO (WHO 2008). For example, doctor‐nurse substitution was used in the United States partly as a response to a lack of female doctors and a demand for female providers among recipients (Coulter 2000). This unintended expansion usually led to "an uncertain and ill‐defined role" (Halcomb 2005). Third, the lack of a nationally endorsed framework to harmonise these new roles with other aspects of health systems may be a source of confusion or conflict around interprofessional role boundaries. Other work has shown that role standardisation, long‐term political planning and support from professional associations are needed to support policymakers in implementing new skill mixes in primary care (van der Biezen 2017b).
The qualitative studies we examined provided little, and mostly indirect, evidence related to the topic of financial resources. However, studies undertaken in LMICs highlighted that a lack of financial resources was seen as a barrier to improving services (Basaleem 2011; Leech 2007; Mills 2008a). A successful task‐shifting strategy which decentralises and expands access to healthcare services at the community level is likely to increase the total number of health‐service users. Hence, task‐shifting should not be viewed as a way to save financial resources in the health sector. Furthermore, the effectiveness review conducted by Laurant 2018 reported that nurse‐led care may make little or no difference to the cost of care compared to doctor‐led primary care.
Authors' conclusions
Implications for practice
Doctor‐nurse substitution is a complex intervention that needs careful planning, implementation and ongoing supervision to ensure optimal impact. The following questions, derived from our findings, may help programme managers and other stakeholders when considering or implementing task‐shifting strategies.
Preparing nurses and doctors to implement task‐shifting
Have efforts been made to increase doctors' trust in and acceptability of using nurses to substitute for doctors? For instance, have there been any attempts to reassure doctors that nurses have the necessary skills and training to take on the designated task/s?
Are processes in place that allow doctors and nurses to communicate effectively and provide feedback to one another concerning specific task‐shifting strategies?
Are doctor/nurse role boundaries clearly defined for the specific substituted task/s?
Have nurses received appropriate training and tailored feedback regarding the specific substituted task/s that they have been requested to deliver?
Implementing doctor‐nurse substitution
Have appropriate leadership and management been put in place to implement doctor‐nurse substitution?
Have nursing documentation and record keeping with regard to task shifting been optimised and also kept to a minimum?
Have attempts been made to ensure that factors affecting nurses' internal motivation (such as job satisfaction and independent work) and external motivation (such as improved working conditions and financial issues) are addressed?
Have appropriate supervisory and monitoring arrangements been put in place for the specific substituted task/s?
Are the necessary resources (financial, infrastructural, facilities, and drugs and equipment) available to nurses taking on new task/s?
Is an appropriate patient referral system in place in relation to the specific substituted task/s?
Can service users easily access the nurses who have been designated to deliver the specific substituted task/s?
Supporting patients
Is information being communicated to service users on the task/s that will be delivered by nurses rather than doctors, and about the roles that nurses will play in their care?
Evaluating the shifting of tasks from doctors to nurses
Does the substituted task facilitate continuity of care for patients?
Does implementation of doctor‐nurse substitution for the specific tasks reduce doctors' workloads without leading to a reduction in their salary or other payments?
Implications for research
We identified a number of research implications from the findings of this QES:
There is a need for better reporting of context, sampling, methods and researcher reflexivity in qualitative studies of using nurses to substitute for doctors in primary care.
We assessed some of our review findings as low or very low confidence, and we suggest that these topics are explored further in future research. In addition, there were dimensions of the SURE framework (SURE Collaboration 2011) and of the framework for implementing interventions (Cargo 2018) for which we did not identify any evidence from the studies included in this QES. These areas should be addressed in future qualitative studies.
Although our maximum variation sample attempted to include studies reflecting a variety of country development levels, only 14 of the 66 included studies were from LMICs. In addition, all but one of the trials included in the linked effectiveness review were conducted in high‐income countries (Laurant 2018). Further qualitative studies in LMIC contexts are therefore needed to explore whether there are further important issues related to implementing doctor‐nurse substitution strategies in settings with more limited resources. Additional trials in LMICs might also help identify factors influencing substitution in different geographical contexts and these factors could then be further explored in qualitative studies.
The primary qualitative studies included in our QES mostly investigated the viewpoints of the recipients of care, nurses and doctors. Future studies should also explore the viewpoints of health service managers, policymakers, implementers and other health professionals.
Only two qualitative studies were conducted alongside or in relation to the 18 intervention trials included in the Laurant 2018 review, and these related to two of these trials. Conducting qualitative studies alongside intervention trials can optimise intervention procedures by offering insights into the conditions under which interventions are more effective, and understanding the issues that may emerge when implementing a substitution strategy (Lewin 2009).
Future trials should assess the effects of interventions on factors identified in this QES as influencing the implementation of doctor‐nurse substitution. These factors include the types of tasks delivered by nurses, effective communication and role boundaries between doctors and nurses, doctors' trust in and acceptance of nurses, training and education for nurses, knowledge and awareness of the strategy among recipients of care, what motivates and incentivises nurses and doctors, resources (financial, infrastructural, facilities, and drugs and equipment), care flow processes and referrals for recipients of care, supervision, and management and leadership vision.
What's new
| Date | Event | Description |
|---|---|---|
| 29 April 2019 | Amended | Edits to author affiliations |
History
Protocol first published: Issue 2, 2013 Review first published: Issue 4, 2019
| Date | Event | Description |
|---|---|---|
| 5 November 2015 | Amended | Protocol transferred to qualitative review template |
Acknowledgements
We thank the members of the Cochrane Effective Practice and Organisation of Care Group, and Cochrane Qualitative and Implementation Methods Group for their valuable input while conducting this QES. We would like to thank the following peer referees who provided comments to improve the review: Margaret Glogowska and Tanya Doherty. Our thanks also to Marit Johansen for help with developing and running the search strategies and Anne Lawson for copy‐editing the review.
The Norwegian Satellite of the EPOC Group receives funding from the Norwegian Agency for Development Cooperation (Norad), via the Norwegian Institute of Public Health to support review authors in the production of their reviews.
Appendices
Appendix 1. Search strategies
CINAHL 1981 ‐ present, EBSCOhost
| # | Query | Results |
| S47 | S42 OR S43 OR S44 OR S45 Limiters ‐ Exclude MEDLINE records |
816 |
| S46 | S42 OR S43 OR S44 OR S45 | 1909 |
| S45 | S4 AND S17 AND S40 AND S41 | 1041 |
| S44 | S17 AND S27 AND S41 | 705 |
| S43 | S8 AND S18 AND S41 | 158 |
| S42 | S4 AND S8 AND S17 AND S41 | 945 |
| S41 | ((TI interview or AB interview) or (MH "audiorecording" not MM "audiorecording") or (TI qualitative stud* or AB qualitative stud*) or (TI themes or AB themes)) | 145,291 |
| S40 | S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 | 187,956 |
| S39 | TI ( (role or competence or performance or skill or skills) N3 (nurse or nurses or midwife or midwives) ) OR AB ( (role or competence or performance or skill or skills) N3 (nurse or nurses or midwife or midwives) ) | 22,903 |
| S38 | (MH "Health Resource Utilization") | 11,590 |
| S37 | (MH "Health Care Delivery") | 29,107 |
| S36 | (MH "Outcome Assessment") | 23,739 |
| S35 | (MH "Task Performance and Analysis") | 7024 |
| S34 | (MH "Professional Competence") | 10,427 |
| S33 | (MH "Nursing Skills") | 3647 |
| S32 | (MH "Clinical Competence") | 23,761 |
| S31 | (MH "Professional Autonomy") | 3603 |
| S30 | (MH "Physician's Role") | 6409 |
| S29 | (MH "Nursing Role") | 43,785 |
| S28 | (MH "Professional Role") | 23,396 |
| S27 | S19 or S20 or S21 or S22 or S25 or S26 | 54,083 |
| S26 | TI ( "nurse led" or "nurse managed" or "nurse run" ) OR AB ( "nurse led" or "nurse managed" or "nurse run" ) | 3682 |
| S25 | S23 AND S24 | 4581 |
| S24 | TX ( nurse or nurses or midwife or midwives ) OR TX ( nurse or nurses or midwife or midwives ) | 588,988 |
| S23 | TI ( substitut* or delegat* or (task* N2 shift*) or (change* N2 role*) or (expand* N2 role*) or (extend* N2 role*) or (expand* N2 responsabilit*) or (extend* N2 responsabilit*) or (expand* N2 task*) or (extend* N2 task*) ) OR AB ( substitut* or delegat* or (task* N2 shift*) or (change* N2 role*) or (expand* N2 role*) or (extend* N2 role*) or (expand* N2 responsabilit*) or (extend* N2 responsabilit*) or (expand* N2 task*) or (extend* N2 task*) ) | 16,214 |
| S22 | (MH "Nursing Role") | 43,785 |
| S21 | (MH "Midwives+/MA/UT") | 243 |
| S20 | (MH "Nurses+/MA/UT") | 2523 |
| S19 | (MH "Delegation of Authority") | 1704 |
| S18 | (MH "Community Health Nursing+") | 24,795 |
| S17 | S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 | 158,850 |
| S16 | TI ( "primary care" or "primary healthcare" or "primary health care" or primary W0 practice* or general W0 practice* or family W0 practice* or outpatient* or "ambulatory care" or "community care" or community W0 health* or "community medicine" or "home care" ) OR AB ( "primary care" or "primary healthcare" or "primary health care" or primary W0 practice* or general W0 practice* or family W0 practice* or outpatient* or "ambulatory care" or "community care" or community W0 health* or "community medicine" or "home care" ) | 103,386 |
| S15 | (MH "Home Health Care") | 16,762 |
| S14 | (MH "Community Medicine") | 99 |
| S13 | (MH "Community Health Services") | 13,809 |
| S12 | (MH "Ambulatory Care Facilities+") | 10,215 |
| S11 | (MH "Ambulatory Care") | 7218 |
| S10 | (MH "Family Practice") | 13,008 |
| S9 | (MH "Primary Health Care") | 38,251 |
| S8 | S5 OR S6 OR S7 | 149,938 |
| S7 | TI ( physician* or doctor or doctors or (general W0 practitioner*) or GP or GPs or (family W0 practitioner*) or "conventional care" or "usual care" or "treatment as usual" ) OR AB ( physician* or doctor or doctors or (general W0 practitioner*) or GP or GPs or (family W0 practitioner*) or "conventional care" or "usual care" or "treatment as usual" ) | 123,714 |
| S6 | (MH "Physicians, Family") | 10,465 |
| S5 | (MH "Physicians") | 38,240 |
| S4 | S1 OR S2 OR S3 | 362,204 |
| S3 | TI ( nurse or nurses or midwife or midwives ) OR AB ( nurse or nurses or midwife or midwives ) | 264,006 |
| S2 | (MH "Midwives+") | 10,663 |
| S1 | (MH "Nurses+") | 179,744 |
MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, MEDLINE Daily and MEDLINE 1946 to Present, Ovid
| # | Searches | Results |
| 1 | exp Nurses/ | 82659 |
| 2 | Midwifery/ | 17897 |
| 3 | (nurse or nurses or midwife or midwives).ti,ab. | 248273 |
| 4 | or/1‐3 | 296988 |
| 5 | Physicians/ | 81464 |
| 6 | General Practitioners/ | 6204 |
| 7 | Physicians, Family/ | 15804 |
| 8 | Physicians, Primary Care/ | 2619 |
| 9 | (physician* or doctor or doctors or general practitioner* or GP* or family practitioner? or conventional care or usual care or treatment as usual).ti,ab. | 632579 |
| 10 | or/5‐9 | 671015 |
| 11 | Primary Health Care/ | 68186 |
| 12 | Family Practice/ | 63921 |
| 13 | Ambulatory Care/ | 40263 |
| 14 | exp Ambulatory Care Facilities/ | 51585 |
| 15 | Community Health Services/ | 29888 |
| 16 | Community Medicine/ | 1965 |
| 17 | Home Care Services/ | 31276 |
| 18 | (primary care or primary healthcare or primary health care or primary practice? or general practice? or family practice? or outpatient? or ambulatory care or community care or community health* or community medicine or home care).ti,ab. | 333934 |
| 19 | or/11‐18 | 481808 |
| 20 | Community Health Nursing/ | 19165 |
| 21 | Delegation, Professional/ | 542 |
| 22 | exp Nurses/ma, ut [Manpower, Utilization] | 1955 |
| 23 | Midwifery/ma, ut [Manpower, Utilization] | 368 |
| 24 | Nurse's Role/ | 38641 |
| 25 | (substitut* or delegat* or (task? adj2 shift*) or (cange* adj2 role?) or (expand* adj2 role?) or (extend* adj2 role?) or (expand* adj2 responsabilit*) or (extend* adj2 responsabilit*) or (expand* adj2 task?) or (extend* adj2 task?)).ti,ab. and (nurse or nurses or midwife or midwives).mp. | 3370 |
| 26 | (nurse led or nurse managed or nurse run).ti,ab. | 3649 |
| 27 | or/21‐26 | 47086 |
| 28 | Professional Role/ | 11570 |
| 29 | Professional Autonomy/ | 9186 |
| 30 | Professional Competence/ | 23011 |
| 31 | Clinical Competence/ | 82983 |
| 32 | "Task Performance and Analysis"/ | 28761 |
| 33 | "Outcome Assessment (Health Care)"/ | 63953 |
| 34 | Delivery of Health Care/ | 79784 |
| 35 | Health Resources/ma [Manpower] | 1 |
| 36 | ((role or competence or performance or skill?) adj3 (nurse or nurses or midwife or midwives)).ti,ab. | 14352 |
| 37 | or/28‐36 | 300099 |
| 38 | Qualitative Research/ | 39579 |
| 39 | qualitative.ti,ab. | 184990 |
| 40 | themes.ti,ab. | 53146 |
| 41 | or/38‐40 | 224816 |
| 42 | exp Animals/ | 21598221 |
| 43 | Humans/ | 17130236 |
| 44 | 42 not (42 and 43) | 4467985 |
| 45 | (review or meta analysis or news or comment or editorial).pt. or cochrane database of systematic reviews.jn. or comment on.cm. or (systematic review or literature review).ti. | 3655313 |
| 46 | 41 not (44 or 45) | 184651 |
| 47 | 4 and 10 and 19 and 46 | 1302 |
| 48 | 10 and 20 and 46 | 66 |
| 49 | 19 and 27 and 46 | 654 |
| 50 | 4 and 19 and 37 and 46 | 614 |
| 51 | or/47‐50 | 2032 |
Appendix 2. Questions included in the modified CASP
| 1 | Was the context described? |
| 2 | Was the sampling strategy appropriate and described? |
| 3 | Was the data collection strategy appropriate and described? |
| 4 | Was the data analysis appropriate and described? |
| 5 | Were the findings supported by evidence? |
| 6 | Is there evidence of researcher reflexivity? |
| 7 | Have ethical issues been taken into consideration? |
| 8 | Overall assessment of methodological limitations |
Appendix 3. CERQual evidence profiles
| Finding #1 | |
| Recipients of care had mixed views about the expansion of tasks undertaken by nurses. They preferred doctors when the tasks were more 'medical'in nature and they accepted nurses for preventive care and follow‐ups. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 5 studies did not report reflexivity; 1 study did not report ethical consideration; and a small number of studies did not report sampling strategy, data collection or data analysis methods. However, these may not have influenced the findings. |
| Coherence | No to very minor concerns. |
| Relevance | Moderate concerns, as data were drawn only from HICs. Data covered different types of care and various recipients of care in terms of socioeconomic status within the context. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and moderate concerns about relevance. |
| Contributing studies/setting | |
|
Oceania (5); Europe (5); North America (2) Bennett 2013: UK, primary care Boyle 2016: Australia, general practice Branson 2008: UK, primary care Cheek 2002: Australia, primary care Clendon 2001: New Zealand, school Clendon 2003: New Zealand, school Coker 2009: USA, primary care Courtenay 2010: UK, primary care Flowers 2008: Australia, child health nursing Leipert 2011: Canada, primary care Perry 2005: UK, personal medical services Rosemann 2006: Germany, clinic | |
| Finding #2 | |
| Doctors in most studies also preferred that nurses performed only non‐medical tasks. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 3 studies did not report reflexivity; 2 studies did not report ethical consideration; and 2 studies did not report sampling strategy. |
| Coherence | Moderate concerns because all studies welcomed the transfer of certain tasks to nurses, but only in 1 study doctors were not willing to shift tasks such as examination, diagnosis or therapy to nurses. Moreover, in LMICs, attitude among doctors was reported to be more mixed. |
| Relevance | Minor concerns because most data were from HICs and there were 2 studies from LMICs. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and relevance; and moderate concerns about coherence. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Asia (1); Oceania (3); Europe (7); North America (4) Abbott 2013: Australia, general practices Bailey 2006: Canada, primary care Branson 2008: UK, primary care Coulter 2000: USA, managed care organisation‐multispeciality group practices Georgeu 2012: South Africa, PHC clinic Ivers 2011: Haiti, rural communities Kraus 2017: USA, primary care Lindblad 2010: Sweden, primary health care Lorch 2015: Australia, chlamydia testing Marsden 2004: UK, practices Rosemann 2006: Germany, clinic Ross 2015: UK, mental health Stenner 2010: UK, primary care Stephen 2018: Australia, general practice Twinn 1999: Hong Kong, primary care‐teaching clinics Voogdt‐Pruis 2011: Netherlands, cardiovascular prevention | |
| Finding #3 | |
| Nurses were comfortable with, and believed they were competent to deliver, a wide range of tasks, but particularly tasks that were more health promotive/preventive in nature. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 1 study did not report data collection, 2 studies did not report data analysis and 5 studies did not report reflexivity. |
| Coherence | No or very minor concerns. |
| Relevance | Minor concerns, as most data were drawn from HICs; though data covered different types of care. |
| Adequacy | Minor concerns because data were from 4 regions. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations, adequacy and relevance. |
| Contributing studies/setting | |
|
North America (3); Oceania (6); Sub‐Saharan Africa (1); Europe (2) Abbott 2013: Australia, general practices Bailey 2006: Canada, primary care Carryer 2017: New Zealand, primary care Dennis 2016: Australia, primary care Georgeu 2012: South Africa, PHC clinic Francis 2013: Australia, general practice Hamel 2017: Slovenia and Spain, primary care Hart 2012: Australia, primary care Kraus 2017: USA, primary care Lindblad 2010: Sweden, primary health care Peterson 2007: Canada, primary care Stephen 2018: Australia, general practice | |
| Finding #4 | |
| Recipients of care in most studies believed that nurses were more easily accessible than doctors. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 2 studies did not report reflexivity; and in 1 study data sampling and data analysis were unclear. |
| Coherence | No or very minor concerns. |
| Relevance | No or very minor concerns. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| High confidence | — |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Middle East and North Africa (1); Oceania (1); Europe (4); North America (3) Basaleem 2009: Yemen, primary care Cheek 2002: Australia, primary care Coker 2009: USA, primary care Fortin 2010: Canada, primary care Georgeu 2012: South Africa, PHC clinic Leipert 2011: Canada, primary care Marsden 2004: UK, practices Perry 2005: UK, personal medical services Ross 2015: UK, mental health Stenner 2011: UK, primary care | |
| Finding #5 | |
| Both doctors and nurses saw doctor‐nurse substitution and collaborative practice as a way of increasing quick access to care for certain tasks such as maternity care and prescriptions. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 1 study did not describe the context and 1 study had unclear reporting of sampling criteria; 1 study did not report reflexivity. |
| Coherence | No or very minor concerns. |
| Relevance | Moderate concerns because only 2 regions were represented. In 6 studies, participants were nurses; and in 4 studies, they were doctors. |
| Adequacy | Minor concerns, as 6 studies reported this finding. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and relevance; and moderate concerns about adequacy. |
| Contributing studies/setting | |
|
Europe (3); North America (3) Kaasalainen 2013: Canada, long‐term care homes (primary care) Ljungbeck 2017: Sweden, municipal healthcare Lovink 2018: Netherlands, primary care Perry 2005: UK, personal medical services Peterson 2007: Canada, primary care Poghosyan 2017: USA, primary care | |
| Finding #6 | |
| Recipients of care in most studies were satisfied with nurses'social skills. Recipients'perceptions of nurses'technical skills were mixed. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because a few studies did not report sampling strategy, ethical considerations, data collection and reflexivity. |
| Coherence | Serious concerns because in most of the studies recipients of care were satisfied with the social skills of nurses; however, in 3 studies, the recipients felt that as they had known the doctor for longer, it was easier to communicate with the doctor; or nurses were described as being too overworked to be able to contribute to increasing the knowledge and skills of the healthcare recipients. Moreover, some recipients of care highlighted positive technical issues of accessibility. However in 1 study from South Africa, parents were dissatisfied with nursing practices related to infant developmental care and felt that these did not meet the desired standards. |
| Relevance | No or very minor concerns. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Low confidence | Due to minor concerns about methodological limitations; and serious concerns about coherence. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (2); Asia (1); Oceania (5); Europe (5); North America (4) Bennett 2013: UK, primary care Boyle 2016: Australia, general practice Branson 2008: UK, primary care Coker 2009: USA, primary care Corneli 2008: Congo, urban clinics Dennis 2016: Australia, primary care Duane 2015: Australia, Home Care Nursing Service and Aged Care Assessment Service Fortin 2010: Canada, primary care Friman 2011: Sweden, primary healthcare Hart 2012: Australia, primary care Leech 2007: South Africa, primary care Leipert 2011: Canada, primary care Parfitt 2007: Tajikistan, primary health clinic Peterson 2007: Canada, primary care Ross 2015: UK, mental health Stenner 2011: UK, primary care Stephen 2018: Australia, general practice | |
| Finding #7 | |
| Health professionals, including doctors, nurses, policymakers and other healthcare providers, believed that doctor‐nurse substitution led to improvements in the quality of care. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 1 study did not report reflexivity, ethical considerations and data analysis; 1 study did not report sampling strategies; 2 other studies did not report reflexivity. |
| Coherence | Minor concerns because in 1 study based in LMICs (Malawi, Uganda and Zimbabwe), nurses perceived that delivering new services had increased their workload that might hinder the provision of the quality of service. |
| Relevance | No or very minor concerns. In 9 studies, participants were nurses; in 9 studies, they were doctors; in 5 studies, they were other healthcare providers and in 4 studies, they were policymakers/managers. |
| Adequacy | No or very minor concerns, although data were relatively few, many studies from several regions reported this finding. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and coherence. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (2); Oceania (4); Europe ( 5); North America (3) Abbott 2013: Australia, general practices Boyle 2016: Australia, general practice Carryer 2017: New Zealand, primary care Coulter 2000: USA, managed care organisation‐multispeciality group practices Dierick‐van Daele 2010a: Netherland, general practice Kaasalainen 2013: Canada, long‐term care homes (primary care) Leipert 2011; Canada, primary care Ljungbeck 2017: Sweden, municipal healthcare Lorch 2015: Australia, chlamydia testing Marsden 2004: UK, practices Nkhata 2016: Malawi, Uganda and Zimbabwe, ART Perry 2005: UK, personal medical services Rustagi 2015a: Mozambique, N/A Stenner 2010: UK, primary care | |
| Finding #8 | |
| A close doctor‐nurse relationship characterised by trust and mutual respect helped nurses to expand and develop their roles. | |
| Assessment for each CERQual component | |
| Methodological limitations | Moderate concern because there were 3 studies with serious methodological limitations. |
| Coherence | No or very low concerns. |
| Relevance | Minor concerns because all but 2 studies were from HICs. Participants in 7 studies were nurses, in 3 studies were doctors, and in 4 studies were managers. |
| Adequacy | No or very low concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to moderate concerns about methodological limitations and minor concerns about relevance. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Oceania (3); Europe (4); North America (2); Latin America (1) Burns 2009b: UK, primary care trust Francis 2013: Australia, general practice Georgeu 2012: South Africa, PHC clinic Hamel 2017: Slovenia and Spain, primary care Mills 2008a: Australia, primary care Lovink 2018: Netherlands, primary care Peterson 2007: Canada, primary care Poghosyan 2017: USA, primary care Schadewaldt 2016: Australia, primary care Vetter‐Smith 2012: Columbia, diabetes care Voogdt‐Pruis 2011: Netherlands, cardiovascular prevention | |
| Finding #9 | |
| Nurses might find it difficult to communicate effectively with colleagues in stand‐alone practices or vertical programmes of care. | |
| Assessment for each CERQual component | |
| Methodological limitations | Mild concerns because 1/6 studies did not report data analysis and sampling and reflexivity; 3 other studies did not report reflexivity. |
| Coherence | No or very minor concern. |
| Relevance | Minor concerns because data were from only 4 regions. |
| Adequacy | Minor concerns due to few data. |
| Overall CERQual assessment | |
| Moderate confidence | Due to moderate concerns about methodological limitations; and minor concerns about relevance and adequacy. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Middle East and North Africa (1); Oceania (2); North America (1) Basaleem 2011: Yemen, primary care Broyles 2012: USA, alcohol screening Flowers 2008: Australia, child health nursing Rustagi 2015a: Mozambique, N/A Walker 2015: New Zealand, general practice | |
| Finding #10 | |
| Doctors' trust in and acceptance of nurses was a critical factor that shaped the extent of nursing practice. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 1/14 studies did not report ethical consideration; 7 studies did not report reflexivity; a few studies did not repot data sampling and analysis. |
| Coherence | No or very minor concerns. |
| Relevance | Minor concerns because data were from 4 regions. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations; and minor concerns about relevance. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (3); Oceania (5); Europe (6); North America (4) Abbott 2013: Australia, general practices Bailey 2006: Canada, primary care Burns 2009b: UK, primary care trust Coulter 2000: USA, managed care organisation‐multispeciality group practices Dennis 2016: Australia, primary care Duane 2015: Australia, Home Care Nursing Service and Aged Care Assessment Service Francis 2013: Australia, general practice Friman 2011: Sweden, primary healthcare Georgeu 2012: South Africa, PHC clinic Hamel 2017: Slovenia and Spain, primary care James 2003: USA, labour and birth units Leech 2007: South Africa, primary care Lindblad 2010: Sweden, primary care Kraus 2017: USA, primary care Mabelane 2016: South Africa, primary healthcare clinics Mills 2008a: Australia, primary care Ross 2015: UK, mental health Stenner 2010: UK, primary care | |
| Finding #11 | |
| Financial issues might damage the relationship between doctors and nurses. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because data sampling were not clear or reported in all but 2 studies; 3 studies did not report reflexivity and ethical considerations. |
| Coherence | Minor concerns because it was unclear whether the data match our finding. |
| Relevance | Moderate concerns because 3 regions were represented. Participants in 5 studies were nurses, in 3 study were doctors, and in 2 studies were managers. |
| Adequacy | Minor concerns due to relatively few data. |
| Overall CERQual assessment | |
| Moderate | Due to minor concerns about methodological limitations, coherence and adequacy; and moderate concern about relevance. |
| Contributing studies/setting | |
|
Oceania (2); North America (3); Europe (2) Coulter 2000: USA, managed care organisation‐multispeciality group practices Lovink 2018: Netherlands, primary care Mills 2008a: Australia, primary care Peterson 2007: Canada, primary care Poghosyan 2017: USA, primary care Ross 2015: UK, mental health Schadewaldt 2016: Australia, primary care | |
| Finding #12 | |
| Nurses felt they had gained additional skills through task‐shifting. However, they believed that further training and education could increase their skills, job satisfaction and motivation; allow them to work more independently; and increase others'acceptance of their professional roles. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 10/19 studies did not report reflexivity; 3 studies reported ethical considerations; some studies were unclear in data sampling, collection and analysis. |
| Coherence | No or very minor concerns. |
| Relevance | Minor concerns because data were from 4 regions. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and relevance. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (4); Oceania (6); Europe (8); North America (1) Albers‐Heitner 2011: Netherland, primary care Burns 2009b: UK, primary care trust Courtenay 2010: UK, primary care Dennis 2016: Australia, primary care Duane 2015: Australia, Home Care Nursing Service and Aged Care Assessment Service Francis 2013: Australia, general practice Friman 2011: Sweden, primary healthcare Furin 2011: Lesotho, rural setting Hart 2012: Australia, primary care Ivers 2011: Haiti, rural communities Kassean 2005: Mauritius, primary care Lindblad 2010: Sweden, primary care Maddox 2016: UK, community and primary care Mills 2008a: Australia, primary care Mills 2008b; Australia, primary care Mkhabela 2008: Swaziland, counselling and testing centres Rustagi 2015a: Mozambique, N/A Stenner 2010: UK, primary care Stenner 2011: UK, primary care | |
| Finding #13 | |
| Nurses had concerns about their training in terms of adequacy, equity and quality. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because ethical considerations were unclear in 2/9 studies; 5 studies did not report reflexivity; 1 study did not report data. |
| Coherence | No or very minor concerns. |
| Relevance | Minor concerns, as 4 regions were represented. |
| Adequacy | No or very minor concern. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and relevance. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (3); Oceania (3); Europe ( 2); North America (1) Broyles 2012: USA, alcohol screening Drew 2002, 2003: UK, primary care Francis 2013: Australia, general practice Georgeu 2012: South Africa, PHC clinic Hart 2012: Australia: primary care Maddox 2016: UK, community and primary care Mabelane 2016: South Africa, primary healthcare clinics McKenna 2015: Australia, general practice Nkhata 2016: Malawi, Uganda and Zimbabwe, ART | |
| Finding #14 | |
| Recipients of care in many studies had limited knowledge about nurses'roles in primary care, nurse models of care and any differences between nurse‐led and doctor‐led care. | |
| Assessment for each CERQual component | |
| Methodological limitations | Moderate concerns because 1 study did not provide sufficient evidence for findings; 5 studies did not report reflexivity; 1 study did not report data analysis; 1 study did not report data collection; 1 study did not report ethical considerations; and 2 studies did not described context. |
| Coherence | No or very minor concerns. |
| Relevance | Moderate concerns, as 4 regions were represented and majority of data are related to HIC. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to moderate concerns about relevance and methodological limitations. |
| Contributing studies/setting | |
|
Middle East and North Africa (1); Oceania (3); Europe (2); North America (1) Basaleem 2009: Yemen, primary care Branson 2008: UK, primary care Cheek 2002: Australia, primary care Clendon 2001: New Zealand, school Halcomb 2013: New Zealand, general practice Leipert 2011: Canada, primary care Lovink 2018: Netherlands, primary care | |
| Finding #15 | |
| Doctors in some studies felt that doctor‐nurse substitution improved the continuity of care and believed that recipients of care would prefer to see the same nurse rather than different doctors. | |
| Assessment for each CERQual component | |
| Methodological limitations | No or very minor concerns. |
| Coherence | No or very minor concerns. |
| Relevance | Moderate concerns because data are from only 1 region representing HICs. |
| Adequacy | Moderate concerns due to few studies. |
| Overall CERQual assessment | |
| Moderate confidence | Due to moderate concerns about adequacy and relevance. |
| Contributing studies/setting | |
|
Europe (2) Marsden 2004: UK, practices Ross 2015: UK, mental health | |
| Finding #16 | ||
| Recipients of care in some studies were concerned over the continuity of care provided by nurses and felt insecure if they lost contact with their doctors. | ||
| Assessment for each CERQual component | ||
| Methodological limitations | Minor concerns because 1 study did not report ethical considerations; 2 studies did not report reflexivity; and 1 study did not provide sufficient evidence for findings. However, these may not influence the findings. | |
| Coherence | No or very minor concerns. | |
| Relevance | Moderate concerns because only 4 regions were represented. | |
| Adequacy | Moderate concerns because data were from few studies. | |
| Overall CERQual assessment | ||
| Low confidence | Due to minor concerns about methodological limitations, and moderate concerns about relevance and adequacy. | |
| Contributing studies/setting | ||
|
Middle East and North Africa (1); Europe (1); North America (1); Oceania (1) Branson 2008: UK, primary care Fortin 2010: Canada, primary care Georgeu 2012: South Africa, primary care Stephen 2018: Australia, general practice | ||
| Finding #17 | |
| Internal motivations most frequently cited by nurses regarding task‐shifting were psychological (including personal development and being respected) and professional (improving the quality of care). | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concern because 1 study did not report ethical considerations; 2 studies did not report reflexivity; a few studies did not clearly report sampling strategy and data collection and analysis; and 1 study did not clearly report contextual description. |
| Coherence | No or very minor concerns. |
| Relevance | No or very minor concerns. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
|
High confidence |
— |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (2); Middle East and North Africa (1); Europe ( 9); North America (2) Albers‐Heitner 2011, Netherlands, primary care Burns 2009b: USA, primary care trust Coulter 2000: UK, managed care organisation/multispeciality group practices Drew 2002; UK, primary care Drew 2003: UK, primary care Friman 2011: Sweden, primary care Furin 2011: Lesotho, rural setting Georgeu 2012: South Africa, primary care Hamel 2017: Slovenia and Spain, primary care James 2003: USA, labour and birth units Ljungbeck 2017: Sweden, municipal healthcare Petrova 2015: Malta, primary care Ross 2015: UK, mental health Voogdt‐Pruis 2011: Netherlands, cardiovascular prevention | |
| Finding #18 | |
| Nurses believed that external motivations such as improved working conditions and financial incentives could act as an incentive to take on more responsibilities. | |
| Assessment for each CERQual component | |
| Methodological limitations | Moderate concerns because 3 studies did not provide sufficient evidence for findings; 6 studies did not report reflexivity; 1 study did not report data collection; and 3 studies did not describe context. |
| Coherence | No or very minor concerns. |
| Relevance | Minor concerns because 4 regions were represented. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to moderate concerns about methodological limitations and minor concerns about relevance. |
| Contributing studies/setting | |
|
Middle East and North Africa (1); Oceania (5); Europe (2); Sub‐Saharan Africa (1) Flowers 2008: Australia, child health nursing Francis 2013: Australia, general practice Furin 2011: Lesotho, rural setting Hamel 2017: Slovenia and Spain, primary care Hart 2012: Australia, primary care Ljungbeck 2017: Sweden, municipal healthcare McKenna 2015: Australia, general practice Mills 2008a: Australia, primary care Nkhata 2016: Malawi, Uganda and Zimbabwe, ART | |
| Finding #19 | |
| Doctors valued the contribution of nurses in collaborative practices when this reduced their own workload. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 4 studies did not report reflexivity; 1 study did not report ethical consideration. However, these may not have influenced the findings. |
| Coherence | Moderate concerns because most of studies stated that contribution of nurses in collaborative practices reduced doctors workloads, but in 2 study doctors reported that as a result of practice nurse services, their working hours had not changed. |
| Relevance | Minor concerns, as 4 regions were represented and majority of data are related to HIC. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and relevance; and moderate concerns about coherence. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Europe (7); North America (3); Oceania (1) Coulter 2000: USA, managed care organisation/multispeciality group practices Dierick‐van Daele 2010a: Netherland, general practice Drew 2002: UK, primary care Drew 2003: UK, primary care Georgeu 2012: South Africa, primary care Hamel 2017: Slovenia and Spain, primary care Kaasalainen 2013: Canada, primary care Ljungbeck 2017: Sweden, municipal healthcare Lorch 2015: Australia, chlamydia testing Lovink 2018: Netherlands, primary care Marsden 2004: UK, practices Peterson 2007: Canada, primary care Stenner 2010: UK, primary care | |
| Finding #20 | |
| In settings where a proportion of doctors'revenues came from fee‐for‐service payments, doctors expressed negative reactions towards doctor‐nurse substitution. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 1/2 studies did not report sampling strategy. |
| Coherence | No to very minor concerns. |
| Relevance | Serious concerns, as only 1 region was represented. |
| Adequacy | Moderate concerns, as only 3 studies with relatively few data reported this finding. |
| Overall CERQual assessment | |
| Low confidence | Due to minor concerns about methodological limitations; moderate concerns about adequacy; and serious concerns about relevance. |
| Contributing studies/setting | |
|
North America (2); Oceania (1) Coulter 2000: USA, managed care organisation/multispeciality group practices Lorch 2015: Australia, chlamydia testing Peterson 2007: Canada, primary care | |
| Finding #21 | |
| A shortage of resources, including human resources, equipment and supplies, and lack of equity in how organisational resources were allocated, sometimes negatively impacted on the effective implementation of doctor‐nurse substitution strategies. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 8 study did not report reflexivity; 1 study did not report data analysis; and 1 study did not report ethical considerations. |
| Coherence | No or very minor concerns. |
| Relevance | No or very minor concerns. Participants in 10 studies were nurses, in 2 studies were doctors, in 3 studies were recipient of care, in 3 studies were managers/leaders, and in 1 study were health workers. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| High confidence | — |
| Contributing studies/setting | |
|
Middle East and North Africa (2); Oceania (4); Europe (2); North America (2), Sub‐Saharan Africa (5); Latin America (1) Abbott 2013: Australia, general practices Basaleem 2009: Yemen, primary care Basaleem 2011: USA, primary care Coker 2009: Yemen, primary care Flowers 2008: Australia, child health nursing Friman 2011: Sweden, primary care Leech 2007: South Africa, primary care Mabelane 2016: South Africa, primary care Mills 2008a: Australia, primary care Mkhabela 2008: Swaziland, counselling and testing centres Nkhata 2016: Malawi, Uganda and Zimbabwe, ART Poghosyan 2017: USA, primary care Schadewaldt 2016: Australia, primary care Vetter‐Smith 2012: Columbia, diabetes care Voogdt‐Pruis 2011: Netherlands, cardiovascular prevention Walker 2004: South Africa, primary care | |
| Finding #22 | |
| An appropriate referral system for recipients of care was important for the effective implementation of doctor‐nurse substitution strategies. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 2 studies did not report reflexivity; this may not have influenced the findings. |
| Coherence | No or very minor concerns. |
| Relevance | Minor concerns, as 3 regions were represented, both HIC and LIMC. Participants in 4 studies were nurses, in 1 study were doctors, and in 2 studies were recipient of care. |
| Adequacy | Minor concerns because 4 studies supported this finding. |
| Overall CERQual assessment | |
| Moderate confidence | Minor concerns because 4 studies supported this finding. |
| Contributing studies/setting | |
|
Middle East and North Africa (1); Oceania (1); Europe (2) Basaleem 2011: Yemen, primary care Bennett 2013: UK, primary care Duane 2015: Australia, Home Care Nursing Service (HCNS) and Aged Care Assessment Service (ACAS) Lovink 2018: Netherlands, primary care | |
| Finding #23 | |
| Experienced leadership was a facilitator of smooth implementation of doctor‐nurse substitution strategies. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 2 studies did not report reflexivity; 1 study did not report data analysis; and 3 studies did not described context. |
| Coherence | No or very minor concerns. |
| Relevance | No or very minor concerns. Participants in 6 studies were nurses, in 1 study were doctors and in 2 studies were managers. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| High confidence | — |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Oceania (2); Middle East and North Africa (1); Europe (2); North America (1) Burns 2009a: UK, primary care Leech 2007: South Africa, primary care Ljungbeck 2017: Sweden, municipal healthcare Mills 2008a: Australia, primary care Mills 2008b: Australia, primary care Petrova 2015: Malta, primary care Poghosyan 2017: USA, primary care | |
| Finding #24 | |
| Nurses and recipients reported dissatisfaction with the huge number of documents and reports that needed to be completed in connection with doctor‐nurse substitution strategies. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 1 study did not provide sufficient evidence for findings and 2 studies did not report reflexivity. However, these may not have influenced the finding. |
| Coherence | No or very minor concerns. |
| Relevance | Minor concerns because only 3 regions are represented, both HIC and LIMC. |
| Adequacy | Moderate concern because data were from few studies. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations; and relevance and moderate concerns about adequacy. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Oceania (1); Middle East and North Africa (1) Basaleem 2011: Yemen, primary care Flowers 2008: Australia, primary care Georgeu 2012: South Africa, primary care | |
| Finding #25 | |
| Clear role definitions were critical in the successful implementation of doctor‐nurse substitution strategies. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 3/13 studies did not provide sufficient evidence for findings; 9 studies did not report reflexivity; 3 studies did not report ethical considerations; and 2 studies did not describe context. |
| Coherence | No or very minor concerns. |
| Relevance | Moderate concerns, as 3 HIC regions were represented. Participants in 10 studies were nurses, in 7 studies were doctors, and in 4 studies were managers. |
| Adequacy | No or very minor concerns. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and moderate concerns about relevance. |
| Contributing studies/setting | |
|
Oceania (5); Europe (4); North America (4) Coulter 2000: USA, managed care organisation/multispeciality group practices Drew 2002; UK, primary care Drew 2003: UK, primary care Flowers 2008: Australia, child health nursing Hamel 2017: Slovenia and Spain, primary care Kraus 2017: USA, primary care Lindblad 2010: Sweden, primary health care Lovink 2018: Netherlands, primary care McKenna 2015: Australia, general practice Mills 2008a: Australia, primary care Peterson 2007: Canada, primary care Poghosyan 2017: USA, primary care Schadewaldt 2016: Australia, primary care Stephen 2018: Australia, general practice | |
| Finding #26 | |
| Where nurses were supervised by doctors, the quality of this supervision was central to the building of confidence in both partners. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns because 2 studies did not report sampling strategy and this may not influence the findings. |
| Coherence | No or very minor concerns. |
| Relevance | No or very minor concerns. Participants in 6 studies were nurses, in 6 studies were doctors, in 1 study were recipients of care, and in 2 studies were managers. |
| Adequacy | Minor concerns, as 8 studies with relatively few data reported this finding. |
| Overall CERQual assessment | |
| Moderate confidence | Due to minor concerns about methodological limitations and adequacy. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (2); Asia (1); Europe (4); North America (2) Coulter 2000: USA, managed care organisation/multispeciality group practices Courtenay 2010: UK, primary care Drew 2002: UK, primary care Drew 2003: UK, primary care Kassean 2005: Mauritius, primary care Kraus 2017: USA, primary care Lindblad 2010: Sweden, primary health care Ljungbeck 2017: Sweden, municipal healthcare Mkhabela 2008: Swaziland, counselling and testing centres | |
| Finding #27 | |
| Nurses in LMIC settings appeared to lack effective supervision. | |
| Assessment for each CERQual component | |
| Methodological limitations | Minor concerns regarding methodological limitations due to 1 study did not report reflexivity. |
| Coherence | No or very minor concerns. |
| Relevance | No or very minor concerns. Participants in 2 studies were nurses, in 1 study were managers, and in 2 studies were other care providers. |
| Adequacy | Serious concerns due to data were from 2 studies with few data. |
| Overall CERQual assessment | |
| Very low confidence | Due to serious concerns about adequacy and minor concerns about methodological concerns. |
| Contributing studies/setting | |
|
Sub‐Saharan Africa (1); Middle East and North Africa (1) Basaleem 2011: Yemen, primary care Leech 2007: South Africa, primary care | |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abbott 2013.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | The role of PNs in sexual health care | |
| Notes |
Methodological assessment Context poorly described. Sampling strategy, data collection described and appropriate but data analysis described poorly. Evidence of reflexivity. Claims somewhat supported by the depth of the data. |
|
Albers‐Heitner 2011.
| Country | Netherlands | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of data. |
|
Bailey 2006.
| Country | Canada | |
| Macroeconomic status | HIC | |
| Aspects of care covered | FP/NP | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Basaleem 2009.
| Country | Yemen | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | IMCI | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Basaleem 2011.
| Country | Yemen | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | IMCI | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Bennett 2013.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Chronic depression | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Boyle 2016.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Diabetes (nurses in care team) | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims somewhat supported by the depth of the data. |
|
Branson 2008.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Skill mix in primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Broyles 2012.
| Country | USA | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Alcohol screening | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims supported by the depth of the data. |
|
Burns 2009a.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Leadership | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Burns 2009b.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Leadership | |
| Notes |
Methodological assessment Context poorly described. Sampling strategy, data collection and data analysis poorly described. Claims somewhat supported by the depth of the data. |
|
Carryer 2017.
| Country | New Zealand | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Advanced roles for nurses | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Cheek 2002.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Clendon 2001.
| Country | New Zealand | |
| Macroeconomic status | HIC | |
| Aspects of care covered | School | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis poorly described. Claims somewhat supported by the depth of the data. |
|
Clendon 2003.
| Country | New Zealand | |
| Macroeconomic status | HIC | |
| Aspects of care covered | School | |
| Notes |
Methodological assessment Context poorly described. Sampling strategy, data collection and data analysis poorly described. Claims somewhat supported by the depth of the data. |
|
Coker 2009.
| Country | USA | |
| Macroeconomic status | HIC, low SES | |
| Aspects of care covered | Well Child Care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Corneli 2008.
| Country | Congo | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | TB/HIV | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Coulter 2000.
| Country | USA | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Well women primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis poorly described. Claims somewhat supported by the depth of the data. |
|
Courtenay 2010.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Diabetes | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Dennis 2016.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | COPD | |
| Notes |
Methodological assessment Context and Sampling strategy did not describe, data collection and data analysis described and appropriate. Claims somewhat supported by the depth of the data. |
|
Dierick‐van Daele 2010a.
| Country | Netherland | |
| Macroeconomic status | HIC | |
| Aspects of care covered | General practices | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims somewhat supported by the depth of the data. |
|
Drew 2002.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Paediatric care | |
| Notes |
Methodological assessment Context described. Sampling strategy and data analysis described poorly. Data collection somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Drew 2003.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Paediatric care | |
| Notes |
Methodological assessment Context described. Sampling strategy and data analysis described poorly. Data collection somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Duane 2015.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Role of a clinical nurse consultant dementia specialist | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Flowers 2008.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | PBCs | |
| Notes |
Methodological assessment Context described. Sampling strategy data analysis poorly described. Data collection and somewhat described appropriate. Claims somewhat supported by the depth of the data. |
|
Fortin 2010.
| Country | Canada | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Patients with multimorbidity | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Francis 2013.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Advanced roles for nurses working in general practice | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Friman 2011.
| Country | Sweden | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Wound care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Furin 2011.
| Country | Lesotho | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | HIV/AIDS | |
| Notes |
Methodological assessment Context described. Sampling strategy described poorly. Data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Georgeu 2012.
| Country | South Africa | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | HIV/AIDS | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Halcomb 2013.
| Country | New Zealand | |
| Macroeconomic status | HIC | |
| Aspects of care covered | General practice | |
| Notes |
Methodological assessment Sampling strategy, data collection and data analysis described, reflexivity and context poorly described. Claims somewhat supported by the depth of the data. |
|
Hamel 2017.
| Country | Slovenia and Spain | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care collaboration of GPs and nurses | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims somewhat supported by the depth of the data. |
|
Hart 2012.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Preventive care for young people | |
| Notes |
Methodological assessment Context described. Data collection described poorly. Sampling strategy and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Ivers 2011.
| Country | Haiti | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | HIV | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
James 2003.
| Country | USA | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Labour | |
| Notes |
Methodological assessment Context described. Sampling strategy described poorly. Data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Kaasalainen 2013.
| Country | Canada | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Palliative care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Kassean 2005.
| Country | Mauritius | |
| Macroeconomic status | Upper middle income | |
| Aspects of care covered | Diabetes | |
| Notes |
Methodological assessment Context described. Data collection described poorly. Sampling strategy, and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Kraus 2017.
| Country | USA | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims somewhat supported by the depth of the data. |
|
Leech 2007.
| Country | South Africa | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | Infant development | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Leipert 2011.
| Country | Canada | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Lindblad 2010.
| Country | Sweden | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy described poorly. Data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data |
|
Ljungbeck 2017.
| Country | Sweden | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Frail elderly people | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims somewhat supported by the depth of the data. |
|
Lorch 2015.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Chlamydia testing | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims supported by the depth of the data. |
|
Lovink 2018.
| Country | Netherlands | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary healthcare for older people | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described and appropriate. Claims somewhat supported by the depth of the data. |
|
Mabelane 2016.
| Country | South Africa | |
| Macroeconomic status | HIC | |
| Aspects of care covered | HIV | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Maddox 2016.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | NMPs | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Marsden 2004.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
McKenna 2015.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | General practice | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Mills 2008a.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Cervical screening | |
| Notes |
Methodological assessment Context poorly described. Sampling strategy described poorly. Data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Mills 2008b.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Cervical screening | |
| Notes |
Methodological assessment Context poorly described. Sampling strategy and data analysis described poorly. Data collection or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Mkhabela 2008.
| Country | Swaziland | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | AIDS | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Nkhata 2016.
| Country | Malawi, Uganda and Zimbabwe | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | ART | |
| Notes |
Methodological assessment Context not described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Parfitt 2007.
| Country | Tajikistan | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | Family nurse | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection or somewhat described and appropriate. Data analysis described poorly. Claims somewhat supported by the depth of the data. |
|
Perry 2005.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Peterson 2007.
| Country | Canada | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Collaborative primary maternity care | |
| Notes |
Methodological assessment Context described. Sampling strategy described poorly. Data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Petrova 2015.
| Country | Malta | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Poghosyan 2017.
| Country | USA | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context, Sampling strategy and data collection described poorly. Data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Rosemann 2006.
| Country | Germany | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Osteoarthritis with another chronic condition | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Ross 2015.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Mental health | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Rustagi 2015a.
| Country | Mozambique | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | HIV | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Schadewaldt 2016.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context did not describe. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Stenner 2010.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Diabetes | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Stenner 2011.
| Country | UK | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Diabetes | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Stephen 2018.
| Country | Australia | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Hypertension management | |
| Notes |
Methodological assessment Context, sampling strategy and data analysis somewhat described. Data collection described and appropriate. Claims somewhat supported by the depth of the data. |
|
Twinn 1999.
| Country | Hong Kong | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Cervical screening | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Vetter‐Smith 2012.
| Country | Columbia | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | Diabetes | |
| Notes |
Methodological assessment Context described. Sampling strategy and data analysis described or somewhat described and appropriate. Method of data collection poorly described. Claims somewhat supported by the depth of the data. |
|
Voogdt‐Pruis 2011.
| Country | Netherland | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Cardiovascular prevention | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
Walker 2004.
| Country | South Africa | |
| Macroeconomic status | LMIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy and method of data collection described or somewhat described and appropriate. Data analysis poorly described. Claims somewhat supported by the depth of the data. |
|
Walker 2015.
| Country | New Zealand | |
| Macroeconomic status | HIC | |
| Aspects of care covered | Primary care | |
| Notes |
Methodological assessment Context described. Sampling strategy, data collection and data analysis described or somewhat described and appropriate. Claims somewhat supported by the depth of the data. |
|
ACAS: Aged Care Assessment Service; APN: advanced practice nurse; ART: antiretroviral therapy; ARV: antiretroviral; CHN: child health nurse; COPD: chronic obstructive pulmonary disease; DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; EN: enrolled nurse; FP: family physician; GP: general practitioner; GPN: general practice nurse; HCNS: Home Care Nursing Service; HIC: high‐income country; IMCI: Integrated Management of Childhood Illness; LMIC: low‐ and middle‐income country; LTC: long‐term care; N/A: not applicable; NCD: non‐communicable disease; NGO: non‐governmental organisation; NHS: National Health Service; NMC: nurse‐managed clinic; NMP: non‐medical prescriber; NP: nurse practitioner; NTP: National Tuberculosis Control Programme; PBC: pharmacy baby clinic; PCPA: primary care pharmacy associate; PCT: primary care trust; PDN: practice development nurse; PHC: primary health care; PHCNP: primary healthcare nurse practitioner; PHCT: primary healthcare team; PHN: public health nurse; PN: practice nurse; ProCEED: Pro‐active Care and its Evaluation for Enduring Depression; RN: registered nurse; SES: socioeconomic status; STI: sexually transmissible infection; T2DM: type 2 diabetes mellitus; TB: tuberculosis; UI: urinary incontinence; VCT: voluntary counselling and testing; WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abbott 2015 | Not focused on TD/TS. |
| Andersson 2015 | Not focused on TD/TS. |
| Andersson 2017 | Not focused on PC. |
| Bala 2012 | Not focused on PC. |
| Benton 2011 | Not focused on PC. |
| Bergman 2013 | Not a qualitative research study. |
| Bernstein 2017 | Not focused on TD/TS. |
| Blackstone 2017 | Not a qualitative research study. |
| Bowers 2017 | Not focused on TD/TS. |
| Bunn 2016 | Not a qualitative research study. |
| Cant 2011 | Not focused on PC. |
| Carlisle 2007 | Not focused on TD/TS. |
| Chan 2014 | Not focused on TD/TS. |
| Claesson 2015 | Not focused on TD/TS. |
| Creedon 2015 | Not a qualitative research study. |
| Dawson 2015 | Not a qualitative research study. |
| Dierick‐van Daele 2010b | Not a qualitative research study. |
| Dodd 2014 | Not focused on TD/TS. |
| Flynn 1974 | Not a qualitative research study. |
| Foster 2017 | Not focused on TD/TS. |
| Frolund 2015 | Not focused on PC. |
| Frost 2018 | Not focused on TD/TS. |
| Gosden 2015 | Not focused on PC. |
| Graves 2016 | Not focused on TD/TS. |
| Gray 2011 | Not focused on TD/TS. |
| Grohmann 2017 | Not focused on TD/TS. |
| Gucciardi 2016 | Not focused on TD/TS. |
| Hadi 2016 | Not focused on TD/TS. |
| Halcomb 2017 | Not focused on TD/TS. |
| Hall 2016 | Not focused on TD/TS. |
| Harrod 2016 | Not focused on TD/TS. |
| Hemani 1999 | Not a qualitative research study. |
| Hosie 2014 | Not focused on PC. |
| Ingram 2007 | Not focused on TD/TS. |
| Ismail 2013 | Not focused on PC. |
| Jackson 2017 | Not focused on TD/TS. |
| Jefferies 2011 | Not a qualitative research study. |
| Johansen 2018 | Not focused on PC. |
| Johansson‐Pajala 2016 | Not focused on TD/TS. |
| Jokiniemi 2015a | Not focused on TD/TS. |
| Jokiniemi 2015b | Not focused on PC. |
| Jolanki 2017 | Not focused on TD/TS. |
| Kaasalainen 2015 | Not focused on TD/TS. |
| Kennedy 2011 | Not focused on TD/TS. |
| Kennedy 2015 | Not focused on PC. |
| Kilpatrick 2012 | Not focused on PC. |
| Lattimer 2000 | Not a qualitative research study. |
| Lenz 2002 | Not a qualitative research study. |
| Lenz 2004 | Not a qualitative research study. |
| Lewis 1967 | Not a qualitative research study. |
| Li 2013 | Not focused on PC. |
| Lowe 2012 | Not a qualitative research study. |
| Lowen 2017 | Not focused on TD/TS. |
| Manski‐Nankervis 2014 | Not focused on TD/TS. |
| Mccarter 2016 | Not focused on PC. |
| McConnell 2013 | Not a qualitative research study. |
| Mcinnes 2017 | Not focused on TD/TS. |
| McIntosh 1997 | Not a qualitative research study. |
| Mendenhall 2014 | Not focused on TD/TS. |
| Moore 1997 | Not a qualitative research study. |
| Mothiba 2016 | Not focused on TD/TS. |
| Mwebe 2017 | Not focused on TD/TS. |
| Nieminen 2011 | Not focused on TD/TS. |
| Nikbakht‐Van De Sande 2014 | Not focused on PC. |
| Nissanholtz‐Gannot 2017 | Not focused on TD/TS. |
| Nover 2013 | Not focused on TD/TS. |
| O'Rourke 2016 | Not focused on TD/TS. |
| Paul 2014 | Not focused on nurses. |
| Pype 2015 | Not focused on TD/TS. |
| Risa 2015 | Not focused on PC. |
| Robb 2011 | Not focused on PC. |
| Robinson 2012 | Not focused on TD/TS. |
| Robinson 2013 | Not focused on TD/TS. |
| Rowbotham 2012 | Not focused on TD/TS. |
| Rustagi 2015b | Not a qualitative research study. |
| Santina de Araujo 2016 | Not focused on TD/TS. |
| Sibley 2011 | Not focused on TD/TS. |
| Sox 2000 | Not a qualitative research study. |
| Spitzer 1973 | Not a qualitative research study. |
| Spitzer 1976a | Not a qualitative research study. |
| Spitzer 1976b | Not a qualitative research study. |
| Stein 1974 | Not a qualitative research study. |
| Supper 2015 | Not a qualitative research study. |
| Sweeny 1973 | Not a qualitative research study. |
| Tariman 2016 | Not focused on PC. |
| Toso 2016 | Not a qualitative analysis. |
| Tracy 2016 | Not focused on PC. |
| Vallerand 2011 | Not a qualitative research study. |
| Vogelsmeier 2017 | Not focused on TD/TS. |
| Wand 2016 | Not focused on PC. |
| Wilkinson 2014 | Not a qualitative research study. |
| Wilkinson 2016 | Not focused on TD/TS. |
| Williamson 2015 | Not focused on PC. |
| Wilson 2015 | Not focused on TD/TS. |
PC: primary care; TD: task development; TS: task‐shifting.
Contributions of authors
AR, JN, CG, SL, CC, ESh, AK and ML devised this synthesis.
ESh, AK, AR and KhH led the development of this synthesis with input from JN, CG, SL, CC and ML.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Alliance for Health Policy and Systems Research, Implementation Research Platform, Switzerland.
We received funding from the Alliance for Health Policy and Systems Research, Implementation Research Platform: WHO‐AHPSR grant 2011/139555‐1.
Declarations of interest
AK: none.
ES: none.
AR: AR is an editor for the Cochrane EPOC Group.
KhH: none.
CG: CG is an editor for the Cochrane EPOC Group.
JN: none.
SL: SL is the Joint Co‐ordinating Editor of the Cochrane EPOC Group.
ML: none.
CC: none.
Edited (no change to conclusions)
References
References to studies included in this review
Abbott 2013 {published data only}
- Abbott P, Dadich A, Hosseinzadeh H, Kang M, Hu W, Bourne C, et al. Practice nurses and sexual health care: enhancing team care within general practice. Australian Family Physician 2013;42:729. [PubMed] [Google Scholar]
Albers‐Heitner 2011 {published data only}
- Albers‐Heitner C, Lagro‐Janssen A, Venema P, Berghmans L, Winkens R, Jonge A, et al. Experiences and attitudes of nurse specialists in primary care regarding their role in care for patients with urinary incontinence. Scandinavian Journal of Caring Sciences 2011;25(2):303‐10. [DOI] [PubMed] [Google Scholar]
Bailey 2006 {published data only}
- Bailey P, Jones L, Way D. Family physician/nurse practitioner: stories of collaboration. Journal of Advanced Nursing 2006;53(4):381‐91. [DOI] [PubMed] [Google Scholar]
Basaleem 2009 {published data only}
- Basaleem HO, Amin RM. Qualitative study on the Community Perception of the Integrated Management of Childhood Illness (IMCI) Implementation in Lahej, Yemen. Sultan Qaboos University Medical Journal 2009;9(1):42. [PMC free article] [PubMed] [Google Scholar]
Basaleem 2011 {published data only}
- Basaleem H, Amin R. Integrated management of childhood illness in Lahej, Yemen: a qualitative analysis from the perspective of health providers. Eastern Mediterranean Health Journal 2011;17(2):101. [PubMed] [Google Scholar]
Bennett 2013 {published data only}
- Bennett M, Walters K, Drennan V, Buszewicz M. Structured pro‐active care for chronic depression by practice nurses in primary care: a qualitative evaluation. PloS One 2013;8(9):e75810. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyle 2016 {published data only}
- Boyle E, Saunders R, Drury V. A qualitative study of patient experiences of type 2 diabetes care delivered comparatively by general practice nurses and medical practitioners. Journal of Clinical Nursing 2016;25(13‐14):1977‐86. [DOI] [PubMed] [Google Scholar]
Branson 2008 {published data only}
- Branson C, Badger B. Skill mix in general practice. Primary Health Care London 2008;18(1):35. [Google Scholar]
Broyles 2012 {published data only}
- Broyles LM, Rodriguez KL, Kraemer KL, Sevick MA, Price PA, Gordon AJ. A qualitative study of anticipated barriers and facilitators to the implementation of nurse‐delivered alcohol screening, brief intervention, and referral to treatment for hospitalized patients in a Veterans Affairs medical center. Addiction Science & Clinical Practice 2012;7(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns 2009a {published data only}
- Burns D. Clinical leadership for general practice nurses, part 1: perceived needs. Practice Nursing 2009;20(9):466‐9. [Google Scholar]
Burns 2009b {published data only}
- Burns D. Clinical leadership for general practice nurses, 2: facilitating factors. Practice Nursing 2009;20(10):519‐23. [Google Scholar]
Carryer 2017 {published data only}
- Carryer J, Adams S. Nurse practitioners as a solution to transformative and sustainable health services in primary health care: a qualitative exploratory study. Collegian (Royal College of Nursing, Australia) 2017;24(6):525‐31. [Google Scholar]
Cheek 2002 {published data only}
- Cheek J, Price MK, Dawson AP, Mott K, Beilby J. Consumer perceptions of nursing and nurses in general practice. A report to the General Practice Branch. Centre for Research into Nursing and Health Care, Adelaide: University of South Australia 2002.
Clendon 2001 {published data only}
- Clendon J, White G. The feasibility of a nurse practitioner‐led primary health care clinic in a school setting: a community needs analysis. Journal of Advanced Nursing 2001;34(2):171‐8. [DOI] [PubMed] [Google Scholar]
Clendon 2003 {published data only}
- Clendon JM. Nurse‐managed clinics: issues in evaluation. Journal of Advanced Nursing 2003;44(6):558‐65. [DOI] [PubMed] [Google Scholar]
Coker 2009 {published data only}
- Coker TR, Chung PJ, Cowgill BO, Chen L, Rodriguez MA. Low‐income parents' views on the redesign of well‐child care. Pediatrics 2009;124(1):194‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Corneli 2008 {published data only}
- Corneli A, Jarrett N, Sabue M, Duvall S, Bahati E, Behets F, et al. Patient and provider perspectives on implementation models of HIV counseling and testing for patients with TB. International Journal of Tuberculosis and Lung Disease 2008;12(3):S79‐S84. [PubMed] [Google Scholar]
Coulter 2000 {published data only}
- Coulter I, Jacobson P, Parker LE. Sharing the mantle of primary female care: physicians, nurse practitioners, and physician assistants. Journal of the American Medical Women's Association (1972) 2000;55(2):100‐3. [PubMed] [Google Scholar]
Courtenay 2010 {published data only}
- Courtenay M, Stenner K, Carey N. The views of patients with diabetes about nurse prescribing. Diabetic Medicine 2010;27(9):1049‐54. [DOI] [PubMed] [Google Scholar]
Dennis 2016 {published data only}
- Dennis S, Reddee HK, Middleton S, Hasan I, Hermiz O, Phillips R, et al. Barriers and outcomes of an evidence‐based approach to diagnosis and management of chronic obstructive pulmonary disease (COPD) in Australia: a qualitative study. Family Practice 2016;34(4):485‐90. [DOI] [PubMed] [Google Scholar]
Dierick‐van Daele 2010a {published data only}
- Dierick‐van Daele AT, Spreeuwenberg C, Derckx EW, Leeuwen Y, Toemen T, Legius M, et al. The value of nurse practitioners in Dutch general practices. Quality in Primary Care 2010;18(4):231‐41. [PubMed] [Google Scholar]
Drew 2002 {published data only}
- Drew J, Nathan D, Hall D. Role of a paediatric nurse in primary care 1: research issues. British Journal of Nursing 2002;11(22):1452‐60. [DOI] [PubMed] [Google Scholar]
Drew 2003 {published data only}
- Drew J, Nathan D, Hall D. Role of a paediatric nurse in primary care 2: research findings. British Journal of Nursing 2003;12(1):34‐42. [DOI] [PubMed] [Google Scholar]
Duane 2015 {published data only}
- Duane FM, Goeman DP, Beanland CJ, Koch SH. The role of a clinical nurse consultant dementia specialist: a qualitative evaluation. Dementia (London) 2015;14(4):436‐49. [DOI] [PubMed] [Google Scholar]
Flowers 2008 {published data only}
- Flowers K. An exploration of child health nursing practice in pharmacy baby clinics. Neonatal Paediatric and Child Health Nursing 2008;11(2):18. [Google Scholar]
Fortin 2010 {published data only}
- Fortin M, Hudon C, Gallagher F, Ntetu AL, Maltais D, Soubhi H. Nurses joining family doctors in primary care practices: perceptions of patients with multimorbidity. BMC Family Practice 2010;11:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Francis 2013 {published data only}
- Francis K, Anderson J, Mills N, Hobbs T, Fitzgerald M. Advanced roles for nurses working in general practice: a study of barriers and enablers for nurses in rural Australia. Clinical Nursing Studies 2013;1(4):45. [Google Scholar]
Friman 2011 {published data only}
- Friman A, Klang B, Ebbeskog B. Wound care by district nurses at primary healthcare centres: a challenging task without authority or resources. Scandinavian Journal of Caring Sciences 2011;25(3):426‐34. [DOI] [PubMed] [Google Scholar]
Furin 2011 {published data only}
- Furin J. The role of traditional healers in community‐based HIV care in rural Lesotho. Journal of Community Health 2011;36(5):849‐56. [DOI] [PubMed] [Google Scholar]
Georgeu 2012 {published data only}
- Georgeu D, Colvin CJ, Lewin S, Fairall L, Bachmann MO, Uebel K, et al. Implementing nurse‐initiated and managed antiretroviral treatment (NIMART) in South Africa: a qualitative process evaluation of the STRETCH trial. Implementation Science 2012;7:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Halcomb 2013 {published data only}
- Halcomb EJ, Peters K, Davies D. A qualitative evaluation of New Zealand consumers perceptions of general practice nurses. BMC Family Practice 2013;14:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamel 2017 {published data only}
- Hamel K, Vossing C. The collaboration of general practitioners and nurses in primary care: a comparative analysis of concepts and practices in Slovenia and Spain. Primary Health Care Research & Development 2017;18(5):492‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hart 2012 {published data only}
- Hart C, Parker R, Patterson E, Hegarty K, Sanci LA. Potential roles for practice nurses in preventive care for young people ‐ a qualitative study. Australian Family Physician 2012;41(8):618‐21. [PubMed] [Google Scholar]
Ivers 2011 {published data only}
- Ivers LC, Jerome JG, Cullen KA, Lambert W, Celletti F, Samb B. Task‐shifting in HIV care: a case study of nurse‐centered community‐based care in Rural Haiti. PloS One 2011;6(5):e19276. [DOI] [PMC free article] [PubMed] [Google Scholar]
James 2003 {published data only}
- James DC, Simpson KR, Knox GE. How do expert labor nurses view their role?. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2003;32(6):814‐23. [DOI] [PubMed] [Google Scholar]
Kaasalainen 2013 {published data only}
- Kaasalainen S, Ploeg J, McAiney C, Schindel Martin L, Donald F, Martin‐Misener R, et al. Role of the nurse practitioner in providing palliative care in long‐term care homes. International Journal of Palliative Nursing 2013;19(10):477‐85. [DOI] [PubMed] [Google Scholar]
Kassean 2005 {published data only}
- Kassean H. Nurses' perceptions of their role in caring for diabetic patients at the primary care level: a case study from Mauritius. Journal of Health Management 2005;7(2):207‐17. [Google Scholar]
Kraus 2017 {published data only}
- Kraus E, Dubois JM. Knowing your limits: a qualitative study of physician and nurse practitioner perspectives on NP independence in primary care. Journal of General Internal Medicine 2017;32(3):284‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leech 2007 {published data only}
- Leech R, Wyk N, Uys C. The management of infant developmental needs by community nurses – part 1: description of the responsibilities of community nurses with regard to the management of infant developmental needs. Curationis 2007;30:91‐103. [DOI] [PubMed] [Google Scholar]
Leipert 2011 {published data only}
- Leipert BD, Delaney JW, Forbes D, Forchuk C. Canadian rural women's experiences with rural primary health care nurse practitioners. Online Journal of Rural Nursing and Health Care 2011;11(1):37‐53. [Google Scholar]
Lindblad 2010 {published data only}
- Lindblad E, Hallman EB, Gillsjo C, Lindblad U, Fagerstrom L. Experiences of the new role of advanced practice nurses in Swedish primary health care – a qualitative study. International Journal of Nursing Practice 2010;16(1):69‐74. [DOI] [PubMed] [Google Scholar]
Ljungbeck 2017 {published data only}
- Ljungbeck B, Forss KS. Advanced nurse practitioners in municipal healthcare as a way to meet the growing healthcare needs of the frail elderly: a qualitative interview study with managers, doctors and specialist nurses. BMC Nursing 2017;16(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorch 2015 {published data only}
- Lorch R, Hocking J, Guy R, Vaisey A, Wood A, Donovan B, et al. Do Australian general practitioners believe practice nurses can take a role in chlamydia testing? A qualitative study of attitudes and opinions. BMC Infectious Diseases 2015;15:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lovink 2018 {published data only}
- Lovink MH, Vught AJ, Persoon A, Schoonhoven L, Koopmans RT, Laurant MG. Skill mix change between general practitioners, nurse practitioners, physician assistants and nurses in primary healthcare for older people: a qualitative study. BMC Family Practice 2018;19(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mabelane 2016 {published data only}
- Mabelane T, Marincowitz GJ, Ogunbanjo GA, Govender I. Factors affecting the implementation of nurse‐initiated antiretroviral treatment in primary health care clinics of Limpopo Province, South Africa. South African Family Practice 2016;58:9‐12. [Google Scholar]
Maddox 2016 {published data only}
- Maddox C, Halsall D, Hall J, Tully MP. Factors influencing nurse and pharmacist willingness to take or not take responsibility for non‐medical prescribing. Research in Social & Administrative Pharmacy : RSAP 2016;12(1):41‐55. [DOI] [PubMed] [Google Scholar]
Marsden 2004 {published data only}
- Marsden J, Street C. A primary health care team's views of the nurse practitioner role in primary care. Primary Health Care Research & Development 2004;5(1):17‐27. [Google Scholar]
McKenna 2015 {published data only}
- McKenna L, Halcomb E, Lane R, Zwar N, Russell G. An investigation of barriers and enablers to advanced nursing roles in Australian general practice. Collegian 2015;22(2):183‐9. [DOI] [PubMed] [Google Scholar]
Mills 2008a {published data only}
- Mills J, Fitzgerald M. The changing role of practice nurses in Australia: an action research study. Australian Journal of Advanced Nursing 2008;26(1):16. [Google Scholar]
Mills 2008b {published data only}
- Mills J, Fitzgerald M. Renegotiating roles as part of developing collaborative practice: Australian nurses in general practice and cervical screening. Journal of Multidisciplinary Healthcare 2008;1:35‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mkhabela 2008 {published data only}
- Mkhabela MP, Mavundla TR, Sukati NA. Experiences of nurses working in voluntary counseling and testing services in Swaziland. Journal of the Association of Nurses in AIDS Care 2008;19(6):470‐9. [DOI] [PubMed] [Google Scholar]
Nkhata 2016 {published data only}
- Nkhata MJ, Muzambi M, Ford D, Chan AK, Abongomera G, Namata H, et al. Shifting human resources for health in the context of ART provision: qualitative and quantitative findings from the Lablite baseline study. BMC Health Services Research 2016;16(1):660. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parfitt 2007 {published data only}
- Parfitt BA, Cornish F. Implementing family health nursing in Tajikistan: from policy to practice in primary health care reform. Social Science & Medicine 2007;65(8):1720‐9. [DOI] [PubMed] [Google Scholar]
Perry 2005 {published data only}
- Perry C, Thurston M, Killey M, Miller J. The nurse practitioner in primary care: alleviating problems of access?. British Journal of Nursing 2005;14(5):255‐9. [DOI] [PubMed] [Google Scholar]
Peterson 2007 {published data only}
- Peterson WE, Medves JM, Davies BL, Graham ID. Multidisciplinary collaborative maternity care in Canada: easier said than done. Journal of Obstetrics and Gynaecology Canada : JOGC = Journal d'Obstétrique et Gynécologie du Canada : JOGC 2007;29(11):880‐6. [DOI] [PubMed] [Google Scholar]
Petrova 2015 {published data only}
- Petrova E, Camilleri M. The role of practice development nurses in Malta. Nursing Standard 2015;30(4):40‐8. [DOI] [PubMed] [Google Scholar]
Poghosyan 2017 {published data only}
- Poghosyan L, Norful AA, Martsoif GR. Primary care nurse practitioner practice characteristics: barriers and opportunities for interprofessional teamwork. Journal of Ambulatory Care Management 2017;40(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosemann 2006 {published data only}
- Rosemann T, Joest K, Körner T, Schaefert R, Heiderhoff M, Szecsenyi J. How can the practice nurse be more involved in the care of the chronically ill? The perspectives of GPs, patients and practice nurses. BMC Family Practice 2006;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ross 2015 {published data only}
- Ross JD. Mental health nurse prescribing: the emerging impact. Journal of Psychiatric and Mental Health Nursing 2015;22(7):529‐42. [DOI] [PubMed] [Google Scholar]
Rustagi 2015a {published data only}
- Rustagi AS, Manjate RM, Gloyd S, John‐Stewart G, Micek M, Gimbel S, et al. Perspectives of key stakeholders regarding task shifting of care for HIV patients in Mozambique: a qualitative interview‐based study with Ministry of Health leaders, clinicians, and donors. Human Resources for Health 2015;13:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schadewaldt 2016 {published data only}
- Schadewaldt V, Mclnnes E, Hiller JE, Gardner A. Experiences of nurse practitioners and medical practitioners working in collaborative practice models in primary healthcare in Australia – a multiple case study using mixed methods. BMC Family Practice 2016;17(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stenner 2010 {published data only}
- Stenner K, Carey N, Courtenay M. Implementing nurse prescribing: a case study in diabetes. Journal of Advanced Nursing 2010;66(3):522‐31. [DOI] [PubMed] [Google Scholar]
Stenner 2011 {published data only}
- Stenner KL, Courtenay M, Carey N. Consultations between nurse prescribers and patients with diabetes in primary care: a qualitative study of patient views. International Journal of Nursing Studies 2011;48(1):37‐46. [DOI] [PubMed] [Google Scholar]
Stephen 2018 {published data only}
- Stephen CM, Hermiz OS, Halcomb EJ, Mclnnes S, Zwar N. Feasibility and acceptability of a nurse‐led hypertension management intervention in general practice. Collegian (Royal College of Nursing, Australia) 2018;25(1):33‐8. [Google Scholar]
Twinn 1999 {published data only}
- Twinn S, Cheng F. A case study of the effectiveness of nurse‐led screening programmes for cervical cancer among Hong Kong Chinese women. Journal of Advanced Nursing 1999;29(5):1089‐96. [DOI] [PubMed] [Google Scholar]
Vetter‐Smith 2012 {published data only}
- Vetter‐Smith M, Lemaster J, Olsberg J, Kruse R, Day T, Mehr D. Providing diabetes self‐management support in rural primary care clinics with nurse partners. Western Journal of Nursing Research 2012;34(8):1023‐42. [DOI] [PubMed] [Google Scholar]
Voogdt‐Pruis 2011 {published data only}
- Voogdt‐Pruis HR, Beusmans GH, Gorgels AP, Ree JW. Experiences of doctors and nurses implementing nurse‐delivered cardiovascular prevention in primary care: a qualitative study. Journal of Advanced Nursing 2011;67(8):1758‐66. [DOI] [PubMed] [Google Scholar]
Walker 2004 {published data only}
- Walker L, Gilson L. 'We are bitter but we are satisfied': nurses as street‐level bureaucrats in South Africa. Social Science & Medicine 2004;59(6):1251‐61. [DOI] [PubMed] [Google Scholar]
Walker 2015 {published data only}
- Walker L, Clendon J, Nelson K. Nursing roles and responsibilities in general practice: three case studies. Journal of Primary Health Care 2015;7(3):236‐43. [PubMed] [Google Scholar]
References to studies excluded from this review
Abbott 2015 {published data only}
- Abbott AA, Fuji KT, Galt KA. A qualitative case study exploring nurse engagement with electronic health records and E‐prescribing. Western Journal of Nursing Research 2015;37(7):935‐51. [DOI] [PubMed] [Google Scholar]
Andersson 2015 {published data only}
- Andersson EK, Sjostrom‐Strand A, Willman A, Borglin G. Registered nurses views of caring in coronary care – a deductive and inductive content analysis. Journal of Clinical Nursing 2015;24(23‐24):3481‐93. [DOI] [PubMed] [Google Scholar]
Andersson 2017 {published data only}
- Andersson H, Lindholm M, Pettersson M, Jonasson LL. Nurses' competencies in home healthcare: an interview study. BMC Nursing 2017;16:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bala 2012 {published data only}
- Bala SV, Samuelson K, Hagell P, Svensson B, Fridlund B, Hesselgard K. The experience of care at nurse‐led rheumatology clinics. Musculoskeletal Care 2012;10(4):202‐11. [DOI] [PubMed] [Google Scholar]
Benton 2011 {published data only}
- Benton B, Norton C, Lindsay JO, Dolan S, Andreyev HJ. Can nurses manage gastrointestinal symptoms arising from pelvic radiation disease?. Clinical Oncology (Royal College of Radiologists (Great Britain)) 2011;23(8):538‐51. [DOI] [PubMed] [Google Scholar]
Bergman 2013 {published data only}
- Bergman K, Perhed U, Eriksson I, Lindblad U, Fagerstrom L. Patients' satisfaction with the care offered by advanced practice nurses: a new role in Swedish primary care. International Journal of Nursing Practice 2013;19(3):326‐33. [DOI] [PubMed] [Google Scholar]
Bernstein 2017 {published data only}
- Bernstein J, Gebel C, Vargas C, Geltman P, Walter A, Garcia R, et al. Listening to paediatric primary care nurses: a qualitative study of the potential for interprofessional oral health practice in six federally qualified health centres in Massachusetts and Maryland. BMJ Open 2017;7(3):e014124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blackstone 2017 {published data only}
- Blackstone S, Iwelunmor J, Plange‐Rhule J, Gyamfi J, Quakyi NK, Ntim M, et al. Sustaining nurse‐led task‐shifting strategies for hypertension control: a concept mapping study to inform evidence‐based practice. Worldviews on Evidence‐Based Nursing 2017;14(5):350‐7. [DOI] [PubMed] [Google Scholar]
Bowers 2017 {published data only}
- Bowers B, Redsell SA. A qualitative study of community nurses' decision‐making around the anticipatory prescribing of end‐of‐life medications. Journal of Advanced Nursing 2017;73(10):2385‐94. [DOI] [PubMed] [Google Scholar]
Bunn 2016 {published data only}
- Bunn F, Goodman C, Pinkney E, Drennan VM. Specialist nursing and community support for the carers of people with dementia living at home: an evidence synthesis. Health & Social Care in the Community 2016;24(1):48‐67. [DOI] [PubMed] [Google Scholar]
Cant 2011 {published data only}
- Cant R, Birks M, Porter J, Jacob E, Cooper S. Developing advanced rural nursing practice: a whole new scope of responsibility. Collegian 2011;18(4):177‐82. [DOI] [PubMed] [Google Scholar]
Carlisle 2007 {published data only}
- Carlisle J, Lawton J, Goyder E, Peters J, Lacey EA. The role of healthcare assistants in screening for diabetes: a qualitative study. Quality in Primary Care 2007;15:77‐83. [Google Scholar]
Chan 2014 {published data only}
- Chan DS, Lee DT, Chair SY, Fung SY, Chan EL, Chan CW. A qualitative study on the roles and responsibilities of nurse consultants in Hong Kong. International Journal of Nursing Practice 2014;20(5):475‐81. [DOI] [PubMed] [Google Scholar]
Claesson 2015 {published data only}
- Claesson A, Toth‐Pal E, Piispanen P, Salminen H. District nurses' perceptions of osteoporosis management: a qualitative study. Osteoporosis International 2015;26(7):1911‐8. [DOI] [PubMed] [Google Scholar]
Creedon 2015 {published data only}
- Creedon R, Byrne S, Kennedy J, McCarthy S. The impact of nurse prescribing on the clinical setting. British Journal of Nursing 2015;24(17):878‐85. [DOI] [PubMed] [Google Scholar]
Dawson 2015 {published data only}
- Dawson AJ, Nkowane AM, Whelan A. Approaches to improving the contribution of the nursing and midwifery workforce to increasing universal access to primary health care for vulnerable populations: a systematic review. Human Resources for Health 2015;13:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dierick‐van Daele 2010b {published data only}
- Dierick‐van Daele AT, Steuten LM, Metsemakers JF, Derckx EW, Spreeuwenberg C, Vrijhoef HJ. Economic evaluation of nurse practitioners versus GPs in treating common conditions. British Journal of General Practice 2010;60(570):e28‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dodd 2014 {published data only}
- Dodd E, Cheston R, Fear T, Brown E, Fox C, Morley C, et al. An evaluation of primary care led dementia diagnostic services in Bristol. BMC Health Services Research 2014;14:592. [DOI] [PMC free article] [PubMed] [Google Scholar]
Flynn 1974 {published data only}
- Flynn BC. The effectiveness of nurse clinicians' service delivery. American Journal of Public Health 1974;64(6):604‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2017 {published data only}
- Foster AA, Goma FM, Shamian J, Moore C, Kabinga‐Makukula M, Chizuni NL, et al. A formative assessment of nurses' leadership role in Zambia's community health system. World Health & Population 2017;17(3):55‐68. [DOI] [PubMed] [Google Scholar]
Frolund 2015 {published data only}
- Frolund JC, Primdahl J. Patients' experiences of nurse‐led screening for cardiovascular risk in rheumatoid arthritis. Musculoskeletal Care 2015;13(4):236‐47. [DOI] [PubMed] [Google Scholar]
Frost 2018 {published data only}
- Frost J, Currie MJ, Cruickshank M, Northam H. Using the lens of enablement to explore patients' experiences of nurse practitioner care in the primary health care setting. Collegian (Royal College of Nursing, Australia) 2018;25(2):193‐9. [Google Scholar]
Gosden 2015 {published data only}
- Gosden CA, Barnard K, Williams DR, Tinati T, Turner B, Holt RI. A decade in diabetes specialist services, 2000 to 2011, in England: the views of consultant diabetologists and diabetes specialist nurses amidst persistent healthcare delivery change. Diabetic Medicine 2015;32(12):1662‐6. [DOI] [PubMed] [Google Scholar]
Graves 2016 {published data only}
- Graves H, Garrett C, Amiel SA, Ismail K, Winkley K. Psychological skills training to support diabetes self‐management: qualitative assessment of nurses' experiences. Primary Care Diabetes 2016;10(5):376‐82. [DOI] [PubMed] [Google Scholar]
Gray 2011 {published data only}
- Gray C, Hogg R, Kennedy C. Professional boundary work in the face of change to generalist working in community nursing in Scotland. Journal of Advanced Nursing 2011;67(8):1695‐704. [DOI] [PubMed] [Google Scholar]
Grohmann 2017 {published data only}
- Grohmann B, Espin S, Gucciardi E. Patients' experiences of diabetes education teams integrated into primary care. Canadian Family Physician Medecin de Famille Canadien 2017;63(2):e128‐e36. [PMC free article] [PubMed] [Google Scholar]
Gucciardi 2016 {published data only}
- Gucciardi E, Espin S, Morganti A, Dorado L. Exploring interprofessional collaboration during the integration of diabetes teams into primary care. BMC Family Practice 2016;17:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hadi 2016 {published data only}
- Hadi MA, Alldred DP, Briggs M, Marczewski K, Cioss SJ. Effectiveness of a community based nurse‐pharmacist managed pain clinic: a mixed‐methods study. International Journal of Nursing Studies 2016;53:219‐27. [DOI] [PubMed] [Google Scholar]
Halcomb 2017 {published data only}
- Halcomb E, Stephens M, Bryce J, Foley E, Ashley C. The development of professional practice standards for Australian general practice nurses. Journal of Advanced Nursing 2017;73(8):1958‐69. [DOI] [PubMed] [Google Scholar]
Hall 2016 {published data only}
- Hall J. Nurse Practitioners' Perceptions of their Role and Value in UK General Practice [Doctoral thesis]. Sheffield (UK): Sheffield Hallam University, 2016. [Google Scholar]
Harrod 2016 {published data only}
- Harrod M, Weston LE, Robinson C, Tremblay A, Greenstone CL, Forman J. "It goes beyond good camaraderie": a qualitative study of the process of becoming an interprofessional healthcare "teamlet". Journal of Interprofessional Care 2016;30(3):295‐300. [DOI] [PubMed] [Google Scholar]
Hemani 1999 {published data only}
- Hemani A, Rastegar DA, Hill C, al‐Ibrahim MS. A comparison of resource utilization in nurse practitioners and physicians. Effective Clinical Practice 1999;2(6):258‐65. [PubMed] [Google Scholar]
Hosie 2014 {published data only}
- Hosie A, Agar M, Lobb E, Davidson PM, Phillips J. Palliative care nurses' recognition and assessment of patients with delirium symptoms: a qualitative study using critical incident technique. International Journal of Nursing Studies 2014;51(10):1353‐65. [DOI] [PubMed] [Google Scholar]
Ingram 2007 {published data only}
- Ingram J, Salmon D. No worries! Young people's experiences of nurse‐led drop‐in sexual health services in South West England. Journal of Research in Nursing 2007;12(4):305‐15. [Google Scholar]
Ismail 2013 {published data only}
- Ismail H, Lewin RJ. The role of a new arrhythmia specialist nurse in providing support to patients and caregivers. European Journal of Cardiovascular Nursing 2013;12(2):177‐83. [DOI] [PubMed] [Google Scholar]
Jackson 2017 {published data only}
- Jackson B, Marshall M, Schofield S. Barriers and facilitators to integration of physician associates into the general practice workforce: a grounded theory approach. British Journal of General Practice 2017;67(664):e785‐e91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jefferies 2011 {published data only}
- Jefferies D, Johnson M, Ravens J. Nurturing and nourishing: the nurses' role in nutritional care. Journal of Clinical Nursing 2011;20(3‐4):317‐30. [DOI] [PubMed] [Google Scholar]
Johansen 2018 {published data only}
- Johansen ML, Ervik B. Teamwork in primary palliative care: general practitioners' and specialised oncology nurses' complementary competencies. BMC Health Services Research 2018;18(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johansson‐Pajala 2016 {published data only}
- Johansson‐Pajala RM, Jorsater Blomgren K, Bastholm‐Rahmner P, Fastbom J, Martin L. Nurses in municipal care of the elderly act as pharmacovigilant intermediaries: a qualitative study of medication management. Scandinavian Journal of Primary Health Care 2016;34(1):37‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jokiniemi 2015a {published data only}
- Jokiniemi K, Haatainen K, Meretoja R, Pietila AM. The future of the clinical nurse specialist role in Finland. Journal of Nursing Scholarship 2015;47(1):78‐86. [DOI] [PubMed] [Google Scholar]
Jokiniemi 2015b {published data only}
- Jokiniemi K, Haatainen K, Pietila AM. From challenges to advanced practice registered nursing role development: qualitative interview study. International Journal of Nursing Practice 2015;21(6):896‐903. [DOI] [PubMed] [Google Scholar]
Jolanki 2017 {published data only}
- Jolanki O, Tynkkynen L‐K, Sinervo T. Professionals' views on integrated care. Journal of Integrated Care 2017;25(4):247‐55. [Google Scholar]
Kaasalainen 2015 {published data only}
- Kaasalainen S, Papaioannou A, Burgess J, Horst ML. Exploring the nurse practitioner role in managing fractures in long‐term care. Clinical Nursing Research 2015;24(6):567‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kennedy 2011 {published data only}
- Kennedy C, Harbison J, Mahoney C, Jarvis A, Veitch L. Investigating the contribution of community nurses to anticipatory care: a qualitative exploratory study. Journal of Advanced Nursing 2011;67(7):1558‐67. [DOI] [PubMed] [Google Scholar]
Kennedy 2015 {published data only}
- Kennedy C, Brooks Young P, Nicol J, Campbell K, Gray Brunton C. Fluid role boundaries: exploring the contribution of the advanced nurse practitioner to multi‐professional palliative care. Journal of Clinical Nursing 2015;24(21‐22):3296‐305. [DOI] [PubMed] [Google Scholar]
Kilpatrick 2012 {published data only}
- Kilpatrick K, Lavoie‐Tremblay M, Ritchie JA, Lamothe L, Doran D, Rochefort C. How are acute care nurse practitioners enacting their roles in healthcare teams? A descriptive multiple‐case study. International Journal of Nursing Studies 2012;49(7):850‐62. [DOI] [PubMed] [Google Scholar]
Lattimer 2000 {published data only}
- Lattimer V, Sassi F, George S, Moore M, Turnbull J, Mullee M, et al. Cost analysis of nurse telephone consultation in out of hours primary care: evidence from a randomised controlled trial. BMJ 2000;320(7241):1053‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lenz 2002 {published data only}
- Lenz ER, Mundinger MO, Hopkins SC, Lin SX, Smolowitz JL. Diabetes care processes and outcomes in patients treated by nurse practitioners or physicians. Diabetes Educator 2002;28(4):590‐8. [DOI] [PubMed] [Google Scholar]
Lenz 2004 {published data only}
- Lenz ER, Mundinger MO, Kane RL, Hopkins SC, Lin SX. Primary care outcomes in patients treated by nurse practitioners or physicians: two‐year follow‐up. Medical Care Research and Review : MCRR 2004;61(3):332‐51. [DOI] [PubMed] [Google Scholar]
Lewis 1967 {published data only}
- Lewis CE, Resnik BA. Nurse clinics and progressive ambulatory patient care. New England Journal of Medicine 1967;277(23):1236‐41. [DOI] [PubMed] [Google Scholar]
Li 2013 {published data only}
- Li J, Westbrook J, Callen J, Georgiou A, Braithwaite J. The impact of nurse practitioners on care delivery in the emergency department: a multiple perspectives qualitative study. BMC Health Services Research 2013;13:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowe 2012 {published data only}
- Lowe G, Plummer V, O'Brien AP, Boyd L. Time to clarify – the value of advanced practice nursing roles in health care. Journal of Advanced Nursing 2012;68(3):677‐85. [DOI] [PubMed] [Google Scholar]
Lowen 2017 {published data only}
- Lowen IM, Peres AM, Ros CD, Polineto P, Faoro NT. Innovation in nursing health care practice: expansion of access in primary health care. Revista Brasileira de Enfermagem 2017;70(5):898‐903. [DOI] [PubMed] [Google Scholar]
Manski‐Nankervis 2014 {published data only}
- Manski‐Nankervis JA, Furler J, Blackberry I, Young D, O'Neal D, Patterson E. Roles and relationships between health professionals involved in insulin initiation for people with type 2 diabetes in the general practice setting: a qualitative study drawing on relational coordination theory. BMC Family Practice 2014;15:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mccarter 2016 {published data only}
- Mccarter SP, Tariman JD, Spawn N, Mehmeti E, Bishop‐Royse J, Garcia I, et al. Barriers and promoters to participation in the era of shared treatment decision‐making. Western Journal of Nursing Research 2016;38(10):1282‐97. [DOI] [PubMed] [Google Scholar]
McConnell 2013 {published data only}
- McConnell D, Slevin OD, McIlfatrick SJ. Emergency nurse practitioners' perceptions of their role and scope of practice: is it advanced practice?. International Emergency Nursing 2013;21(2):76‐83. [DOI] [PubMed] [Google Scholar]
Mcinnes 2017 {published data only}
- Mcinnes S, Peters K, Bonney A, Halcomb E. Understanding collaboration in general practice: a qualitative study. Family Practice 2017;34(5):621‐6. [DOI] [PubMed] [Google Scholar]
McIntosh 1997 {published data only}
- Mcintosh M, Leigh G, Baldwin N, Marmulak J. Reducing alcohol consumption. Comparing three brief methods in family practice. Canadian Family Physician 1997;43:1959‐62. [PMC free article] [PubMed] [Google Scholar]
Mendenhall 2014 {published data only}
- Mendenhall E, Silva MJ, Hanlon C, Petersen I, Shidhaye R, Jordans M, et al. Acceptability and feasibility of using non‐specialist health workers to deliver mental health care: stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Social Science & Medicine 2014;118:33‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 1997 {published data only}
- Moore M. Nurse telephone triage in out of hour's primary care: a pilot study. BMJ 1997;314:198‐9. [PMC free article] [PubMed] [Google Scholar]
Mothiba 2016 {published data only}
- Mothiba TM, Tladi FM. Challenges faced by professional nurses when implementing the Expanded Programme on Immunisation at rural clinics in Capricorn District, Limpopo. African Journal of Primary Health Care & Family Medicine 2016;8(2):e1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mwebe 2017 {published data only}
- Mwebe H. Physical health monitoring in mental health settings: a study exploring mental health nurses' views of their role. Journal of Clinical Nursing 2017;26(19‐20):3067‐78. [DOI] [PubMed] [Google Scholar]
Nieminen 2011 {published data only}
- Nieminen AL, Mannevaara B, Fagerstrom L. Advanced practice nurses' scope of practice: a qualitative study of advanced clinical competencies. Scandinavian Journal of Caring Sciences 2011;25(4):661‐70. [DOI] [PubMed] [Google Scholar]
Nikbakht‐Van De Sande 2014 {published data only}
- Nikbakht‐Van De Sande CV, Braat C, Visser AP, Delnoij D, Staa A. Why a carefully designed, nurse‐led intervention failed to meet expectations: the case of the care programme for palliative radiotherapy. European Journal Of Oncology Nursing 2014;18:151‐58. [DOI] [PubMed] [Google Scholar]
Nissanholtz‐Gannot 2017 {published data only}
- Nissanholtz‐Gannot R, Rosen B, Hirschfeld M. The changing roles of community nurses: the case of health plan nurses in Israel. Israel Journal of Health Policy Research 2017;6(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nover 2013 {published data only}
- Nover CH. Mental health in primary care: perceptions of augmented care for individuals with serious mental illness. Social Work in Health Care 2013;52(7):656‐68. [DOI] [PubMed] [Google Scholar]
O'Rourke 2016 {published data only}
- O'Rourke T, Higuchi KS, Hogg W. Stakeholder participation in system change: a new conceptual model. Worldviews on Evidence‐Based Nursing 2016;13(4):261‐9. [DOI] [PubMed] [Google Scholar]
Paul 2014 {published data only}
- Paul M, Gemzell‐Danielsson K, Kiggundu C, Namugenyi R, Klingberg‐Allvin M. Barriers and facilitators in the provision of post‐abortion care at district level in central Uganda – a qualitative study focusing on task sharing between physicians and midwives. BMC Health Services Research 2014;14:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pype 2015 {published data only}
- Pype P, Mertens F, Wens J, Stes A, Eynden B, Deveugele M. Preparing palliative home care nurses to act as facilitators for physicians' learning: evaluation of a training programme. Palliative Medicine 2015;29(5):458‐63. [DOI] [PubMed] [Google Scholar]
Risa 2015 {published data only}
- Risa CF, Friberg F, Liden E. Norwegian nurse‐midwives' perspectives on the provision of antenatal diabetes care in an outpatient setting: a qualitative study. Women and Birth 2015;28(2):e1‐6. [DOI] [PubMed] [Google Scholar]
Robb 2011 {published data only}
- Robb KA, Smith SG, Power E, Kralj‐Hans I, Vance M, Wardle J, et al. Nurses' experiences of a colorectal cancer screening pilot. British Journal of Nursing 2011;20(4):210, 2, 4 passim. [DOI] [PubMed] [Google Scholar]
Robinson 2012 {published data only}
- Robinson S, Kellett S, King I, Keating V. Role transition from mental health nurse to IAPT high intensity psychological therapist. Behavioural and Cognitive Psychotherapy 2012;40(3):351‐66. [DOI] [PubMed] [Google Scholar]
Robinson 2013 {published data only}
- Robinson A, Denney‐Wilson E, Laws R, Harris M. Child obesity prevention in primary health care: investigating practice nurse roles, attitudes and current practices. Journal of Paediatrics and Child Health 2013;49(4):E294‐9. [DOI] [PubMed] [Google Scholar]
Rowbotham 2012 {published data only}
- Rowbotham S, Chisholm A, Moschogianis S, Chew‐Graham C, Cordingley L, Wearden A, et al. Challenges to nurse prescribers of a no‐antibiotic prescribing strategy for managing self‐limiting respiratory tract infections. Journal of Advanced Nursing 2012;68(12):2622‐32. [DOI] [PubMed] [Google Scholar]
Rustagi 2015b {published data only}
- Rustagi AS, Manjate RM, Gloyd S, John‐Stewart G, Micek M, Gimbel S, et al. Perspectives of key stakeholders regarding task shifting of care for HIV patients in Mozambique: a qualitative interview‐based study with Ministry of Health leaders, clinicians, and donors. Human Resources for Health 2015;13:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Santina de Araujo 2016 {published data only}
- Santina de Araujo M, Oliveira Sales LK, Araujo MG, Forte de Morais I, Roaado de Morais FR, Nogueira Valenca C. Difficulties faced by nurses to develop direct actions to adolescents in primary care. Revista de Enfermagem 2016;10:4219‐25. [Google Scholar]
Sibley 2011 {published data only}
- Sibley A, Latter S, Richard C, Lussier MT, Roberge D, Skinner TC, et al. Medication discussion between nurse prescribers and people with diabetes: an analysis of content and participation using MEDICODE. Journal of Advanced Nursing 2011;67(11):2323‐36. [DOI] [PubMed] [Google Scholar]
Sox 2000 {published data only}
- Sox HC. Independent primary care practice by nurse practitioners. JAMA 2000;283(1):106‐8. [DOI] [PubMed] [Google Scholar]
Spitzer 1973 {published data only}
- Spitzer WO, Kergin DJ. Nurse practitioners in primary care I. The McMaster University educational program. Canadian Medical Association Journal 1973;108(8):991‐5. [PMC free article] [PubMed] [Google Scholar]
Spitzer 1976a {published data only}
- Spitzer W, Roberts R, Delmore T. Nurse practitioners in primary care. V. Development of the utilization and financial index to measure effects of their deployment. Canadian Medical Association Journal 1976;114:1099‐102. [PMC free article] [PubMed] [Google Scholar]
Spitzer 1976b {published data only}
- Spitzer WO, Roberts R, Delmore T. Nurse practitioners in primary care. Vi. Assessment of their deployment with the utilization and financial index. Canadian Medical Association Journal 1976;114(12):1103‐8. [PMC free article] [PubMed] [Google Scholar]
Stein 1974 {published data only}
- Stein GH. The use of a nurse practitioner in the management of patients with diabetes mellitus. Medical Care 1974;12(10):885‐90. [DOI] [PubMed] [Google Scholar]
Supper 2015 {published data only}
- Supper I, Catala O, Lustman M, Chemla C, Bourgueil Y, Letrilliart L. Interprofessional collaboration in primary health care: a review of facilitators and barriers perceived by involved actors. Journal of Public Health (Oxford, England) 2015;37(4):716‐27. [DOI] [PubMed] [Google Scholar]
Sweeny 1973 {published data only}
- Sweeny GP, Hay WI. The Burlington experience: a study of nurse practitioners in family practice. Canadian Family Physician Medecin de Famille Canadien 1973;19(9):101‐10. [PMC free article] [PubMed] [Google Scholar]
Tariman 2016 {published data only}
- Tariman JD, Mehmeti E, Spawn N, Mccarter SP, Bishop‐Royse J, Garcia I, et al. Oncology nursing and shared decision making for cancer treatment. Clinical Journal of Oncology Nursing 2016;20(5):560‐3. [DOI] [PubMed] [Google Scholar]
Toso 2016 {published data only}
- Toso BR, FilIppon J, Giovanella L. Nurses' performance on primary care in the National Health Service in England. Revista Brasileira de Enfermagem 2016;69(1):169‐77. [DOI] [PubMed] [Google Scholar]
Tracy 2016 {published data only}
- Tracy M, Mcdivitt K, Ryan M, Tomlinson J, Brotto LA. Feasibility of a sexual health clinic within cancer care: a pilot study using qualitative methods. Cancer Nursing 2016;39(4):E32‐42. [DOI] [PubMed] [Google Scholar]
Vallerand 2011 {published data only}
- Vallerand AH, Musto S, Polomano RC. Nursing's role in cancer pain management. Current Pain and Headache Reports 2011;15(4):250‐62. [DOI] [PubMed] [Google Scholar]
Vogelsmeier 2017 {published data only}
- Vogelsmeier A, Anderson RA, Anbari A, Ganong L, Farag A, Niemeyer M. A qualitative study describing nursing home nurses sensemaking to detect medication order discrepancies. BMC Health Services Research 2017;17(1):531. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wand 2016 {published data only}
- Wand T, D'Abrew N, Acret L, White K. Evaluating a new model of nurse‐led emergency department mental health care in Australia; perspectives of key informants. International Emergency Nursing 2016;24:16‐21. [DOI] [PubMed] [Google Scholar]
Wilkinson 2014 {published data only}
- Wilkinson J, Carryer J, Adams J. Evaluation of a diabetes nurse specialist prescribing project. Journal of Clinical Nursing 2014;23(15‐16):2355‐65. [DOI] [PubMed] [Google Scholar]
Wilkinson 2016 {published data only}
- Wilkinson M, Whitehead L, Crowe M. Nurses perspectives on long‐term condition self‐management: a qualitative study. Journal of Clinical Nursing 2016;25(1‐2):240‐6. [DOI] [PubMed] [Google Scholar]
Williamson 2015 {published data only}
- Williamson S, Chalmers K, Beaver K. Patient experiences of nurse‐led telephone follow‐up following treatment for colorectal cancer. European Journal of Oncology Nursing 2015;19(3):237‐43. [DOI] [PubMed] [Google Scholar]
Wilson 2015 {published data only}
- Wilson E, Morbey H, Brown J, Payne S, Seale C, Seymour J. Administering anticipatory medications in end‐of‐life care: a qualitative study of nursing practice in the community and in nursing homes. Palliative Medicine 2015;29(1):60‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Ames 2017
- Ames HMR, Glenton C, Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database of Systematic Reviews 2017, Issue 2. [DOI: 10.1002/14651858.CD011787.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Assan 2008
- Assan A, Mudender F, Brentlinger P, Vallejo J, Bacon O, Martinez P, et al. Task‐shifting in Mozambique: evaluating antiretroviral therapy as newly implemented by mid‐level health professionals. AIDS 2008 – XVII International AIDS Conference; 2008 Aug 3–8; Mexico City (Mexico); Abstract MOPE0790.
Booth 2015
- Booth A, Carroll C. How to build up the actionable knowledge base: the role of 'best fit' framework synthesis for studies of improvement in healthcare. BMJ Quality & Safety 2015;24(11):700‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Booth 2016
- Booth A, Sutton A, Papaioannou D. Systematic Approaches to a Successful Literature Review. 2nd Edition. New York (NY): Sage, 2016. [Google Scholar]
Callaghan 2010
- Callaghan M, Ford N, Schneider H. A systematic review of task‐shifting for HIV treatment and care in Africa. Human Resources for Health 2010;8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2013
- Campbell J, Dussault G, Buchan J, Pozo‐Martin F, Arias MG, Leone C. World Health Organisation. A universal truth: no health without a workforce. Third Global Forum on Human Resources for Health, Recife, Brazil, 2013. www.whoint/workforcealliance/knowledge/resources/GHWA_AUniversalTruthReport pdf (accessed 20 March 2015).
Candy 2011
- Candy B, King M, Jones L, Oliver S. Using qualitative synthesis to explore heterogeneity of complex interventions. BMC Medical Research Methodology 2011;11:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cargo 2018
- Cargo M, Harris J, Pantoja T, Booth A, Harden A, Hannes K, et al. Cochrane Qualitative and Implementation Methods Group guidance paper 4: methods for assessing evidence on intervention implementation. Journal of Clinical Epidemiology 2018;97:59‐69. [DOI] [PubMed] [Google Scholar]
Chambers 1978
- Chambers LW, West AE. St John's randomized trial of the family practice nurse: health outcomes of patients. International Journal of Epidemiology 1978;7(2):153‐61. [DOI] [PubMed] [Google Scholar]
Chan 2009
- Chan D, Harris S, Roderick P, Brown D, Patel P. A randomised controlled trial of structured nurse‐led outpatient clinic follow‐up for dyspeptic patients after direct access gastroscopy. BMC Gastroenterology 2009;9:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chinnock 2005
- Chinnock P, Siegfried N, Clarke M. Is evidence‐based medicine relevant to the developing world?. PLoS Medicine 2005;2(5):e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chopra 2008
- Chopra M, Munro S, Lavis JN, Vist G, Bennett S. Effects of policy options for human resources for health: an analysis of systematic reviews. Lancet 2008;371:629‐30. [DOI] [PubMed] [Google Scholar]
Colvin 2013
- Colvin CJ, Heer J, Winterton L, Mellenkamp M, Glenton C, Noyes J, et al. A systematic review of qualitative evidence on barriers and facilitators to the implementation of task‐shifting in midwifery services. Midwifery 2013;29(10):1211‐21. [DOI] [PubMed] [Google Scholar]
Colvin 2018
- Colvin CJ, Garside R, Wainwright M, Munthe‐Kaas H, Glenton C, Bohren MA, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings – paper 4: how to assess coherence. Implementation Science 2018;13(Suppl 1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Contandriopoulos 2015
- Contandriopoulos D, Brousselle A, Dubois CA, Perroux M, Beaulieu MD, Brault I, et al. A process‐based framework to guide nurse practitioners integration into primary healthcare teams: results from a logic analysis. BMC Health Services Research 2015;15:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cutliffe 2002
- Cutliffe JR. The beguiling effects of nurse‐prescribing in mental health nursing: re‐examining the debate. Journal of Psychiatric and Mental Health Nursing 2002;9(3):369‐75. [PubMed] [Google Scholar]
Dierick‐van Daele 2009
- Dierick‐van Daele AT, Metsemakers JF, Derckx EW, Spreeuwenberg C, Vrijhoef HJ. Nurse practitioners substituting for general practitioners: randomized controlled trial. Journal of Advanced Nursing 2009;65(2):391‐401. [DOI] [PubMed] [Google Scholar]
Doyle 2003
- Doyle LH. Synthesis through meta‐ethnography: paradoxes, enhancements, and possibilities. Qualitative Research 2003;3(3):321‐44. [Google Scholar]
Flemming 2007
- Flemming K, Briggs M. Electronic searching to locate qualitative research: evaluation of three strategies. Journal of Advanced Nursing 2007;57(1):95‐100. [DOI] [PubMed] [Google Scholar]
Freund 2015
- Freund T, Everett C, Griffiths P, Hudon C, Naccarella L, Laurant M. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world?. International Journal of Nursing Studies 2015;52(3):727‐43. [DOI] [PubMed] [Google Scholar]
Garner 1998
- Garner P, Kale R, Dickson R, Dans T, Salinas R. Implementing research findings in developing countries. BMJ 1998;317:531‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glenton 2013
- Glenton C, Colvin C, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD010414.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glenton 2018
- Glenton C, Carlsen B, Lewin S, Munthe‐Kaas H, Colvin CJ, Tuncalp O, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings‐paper 5: how to assess adequacy of data. Implementation Science 2018;13(Suppl 1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Halcomb 2005
- Halcomb E, Davidson P, Daly J, Griffiths R, Yallop J, Tofler G. Nursing in Australian general practice: directions and perspectives. Australian Health Review 2005;29:156‐66. [DOI] [PubMed] [Google Scholar]
Harden 2004
- Harden A, Garcia J, Oliver S, Rees R, Shepherd J, Brunton G, et al. Applying systematic review methods to studies of people's views: an example from public health research. Journal of Epidemiology and Community Health 2004;58(9):794‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harris 2018
- Harris JL, Booth A, Cargo M, Hannes K, Harden A, Flemming K, et al. Cochrane Qualitative and Implementation Methods Group guidance series‐paper 2: methods for question formulation, searching, and protocol development for qualitative evidence synthesis. Clinical Epidemiology 2018;97:39‐48. [DOI: 10.1016/j.jclinepi.2017.10.023] [DOI] [PubMed] [Google Scholar]
Hobson 2010
- Hobson RJ, Scott J, Sutton J. Pharmacists and nurses as independent prescribers: exploring the patient's perspective. Family Practice 2010;27(1):110‐20. [DOI] [PubMed] [Google Scholar]
Hollinghurst 2006
- Hollinghurst S, Horrocks S, Anderson E, Salisbury C. Comparing the cost of nurse practitioners and GPs in primary care: modelling economic data from randomised trials. British Journal of General Practice 2006;56:530‐5. [PMC free article] [PubMed] [Google Scholar]
Houweling 2011
- Houweling ST, Kleefstra N, Hateren KJ, Groenier KH, Meyboomde Jong B, Bilo HJ. Can diabetes management be safely transferred to practice nurses in a primary care setting? A randomised controlled trial. Journal of Clinical Nursing 2011;20:1264‐72. [DOI] [PubMed] [Google Scholar]
Iglesias 2013
- Iglesias B, Ramos F, Serrano B, Fàbregas M, Sánchez C, Garcíam J, et al. A randomized controlled trial of nurses vs. doctors in the resolution of acute disease of low complexity in primary care. Journal of Advanced Nursing 2013;69(11):2446‐57. [DOI] [PubMed] [Google Scholar]
Janowitz 2012
- Janowitz B, Stanback J, Boyer B. Task sharing in family planning. Stud Fam Plann 2012;41(1):57‐62. [DOI] [PubMed] [Google Scholar]
Koenig 2004
- Koenig SP, Leandre F, Farmer P. Scaling up HIV treatment programmes in resource‐limited settings: the rural Haiti experience. AIDS 2004;18(Suppl 3):S21‐5. [DOI] [PubMed] [Google Scholar]
Kooienga 2015
- Kooienga SA, Carryer JB. Globalization and advancing primary health care nurse practitioner practice. Journal for Nurse Practitioners 2015;11(8):804‐11. [Google Scholar]
Kroezen 2015
- Kroezen M, Dussault G, Craveiro I, Dieleman M, Jansen C, Buchan J, et al. Recruitment and retention of health professionals across Europe: a literature review and multiple case study research. Health Policy 2015;119(12):1517‐28. [DOI] [PubMed] [Google Scholar]
Larsson 2014
- Larsson I, Fridlund B, Arvidsson B, Teleman A, Bergman S. Randomized controlled trial of a nurse‐led rheumatology clinic for monitoring biological therapy. Journal of Advanced Nursing 2013;70(1):164‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lattimer 1998
- Lattimer V, George S, Thompson F, Thomas E, Mulle M, Turnbull J, et al. South Wiltshire Out of Hours Project (SWOOP) Group. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. BMJ 1998;317:1054‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laurant 2005
- Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD001271.pub2] [DOI] [PubMed] [Google Scholar]
Laurant 2018
- Laurant M, Biezen M, Wijers N, Watananirun K, Kontopantelis E, Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database of Systematic Reviews 2018, Issue 7. [DOI: 10.1002/14651858.CD001271.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lavis 2009
- Lavis JN, Oxman AD, Souza NM, Lewin S, Gruen RL, Fretheim A. SUPPORT Tools for evidence‐informed health Policymaking(STP): 9. Assessing the applicability of the findings of a systematic review. Health Research Policy and Systems 2009;7(Suppl 1):9. [DOI: 10.1186/1478-4505-7-S1-S9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2009
- Lewin S, Glenton C, Oxman AD. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: methodological study. BMJ 2009;339(b3496). [DOI: 10.1136/bmj.b3496] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2015
- Lewin S, Glenton C, Munthe‐Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE‐CERQual). PLoS Medicine 2015;12(10):e1001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2018a
- Lewin S, Both A, Glenton C, Munthe‐Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings: introduction to the series. Implementation Science 2018;13 (Suppl 1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2018b
- Lewin S, Bohren M, Rashidian A, Munthe‐Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings‐paper 2: how to make an overall CERQual assessment of confidence and create a Summary of Qualitative Findings table. Implementation Science 2018;13(Suppl 1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2012
- Liu N, D'Aunno T. The productivity and cost efficiency of models for involving nurse practitioners in primary care: a perspective from queuing analysis. Health Services Research 2012;47(2):594‐613. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maier 2016
- Maier CB, Aiken LH. Task shifting from physicians to nurses in primary care in 39 countries: a cross‐country comparative study. European Journal of Public Health 2016;26(6):927‐34. [DOI] [PubMed] [Google Scholar]
Martinez‐Gonzalez 2014a
- Martinez‐Gonzalez NA, Tandjung R, Djalali S, Huber‐Geismann F, Markun S, Rosemann T. Effects of physician‐nurse substitution on clinical parameters: a systematic review and meta‐analysis. PloS One 2014;9(2):e89181. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martinez‐Gonzalez 2014b
- Martinez‐Gonzalez NA, Djalali S, Tandjung R, Huber‐Geismann F, Markun S, Wensing M, et al. Substitution of physicians by nurses in primary care: a systematic review and meta‐analysis. BMC Health Services Research 2014;14:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2001
- Moher M, Yudkin P, Wright L, Turner R, Fuller A, Schofield T, et al. for the Assessment of Implementation Strategies (ASSIST) Trial Collaborative Group. Cluster randomised controlled trial to compare three methods of promoting secondary prevention of coronary heart disease in primary care. BMJ 2001;322:1338‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2009
- Morris MB, Chapuli B, Chi B, Mwango A, Chi HF, Mwanza J, et al. Use of task‐shifting to rapidly scale‐up HIV treatment services: experiences from Lusaka, Zambia. BMC Health Services Research 2009;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Munabi‐Babigumira 2017
- Munabi‐Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low‐ and middle‐income countries: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2017, Issue 11. [DOI: 10.1002/14651858.CD011558.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mundinger 2000
- Mundinger MO, Kane Rl, Lenz ER, Totten AM, Tsji WY, Cleary PD, et al. Primary care outcomes in patients treated by nurse practitioners or physicians. A randomized trial. JAMA 2000;283(1):59‐68. [DOI] [PubMed] [Google Scholar]
Munthe‐Kaas 2018
- Munthe‐Kaas H, Bohren MA, Glenton C, Lewin S, Noyes J, Tuncalp O, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings‐paper 3: how to assess methodological limitations. Implementation Science 2018;13(Suppl 1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ndosi 2014
- Ndosi M, Lewis M, Hale C, Quinn H, Ryan S, Emery P, et al. The outcome and cost‐effectiveness of nurse‐led care in people with rheumatoid arthritis: a multicentre randomised controlled trial. Annals of the Rheumatic Diseases 2014;73:1975‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Newhouse 2011
- Newhouse RP, Stanik‐Hutt J, White KM, Johantgen M, Bass EB, Zangaro G, et al. Advanced practice nurse outcomes: 1990‐2008: a systematic review. Nursing Economics 2011;29(5):1‐22. [PubMed] [Google Scholar]
Noyes 2009
- Noyes J, Popay J, Pearson A, Hannes K, Booth A. Chapter 20: qualitative research and Cochrane reviews. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 (updated September 2009). Chichester (UK): John Wiley & Sons, 2009. [Google Scholar]
Noyes 2011
- Noyes J, Lewin S. Chapter 6: Supplemental guidance on selecting a method of qualitative evidence synthesis, and Integrating qualitative evidence with Cochrane intervention reviews. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions Version 1 (updated August 2011). Chichester (UK): Cochrane Collaboration Qualitative Methods Group, 2011. [Google Scholar]
Noyes 2018
- Noyes J, Booth A, Lewin S, Carlsen B, Glenton C, Colvin CJ, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings‐paper 6: how to assess relevance of the data. Implementation Science 2018;13(Suppl 1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oxman 2010
- Oxman AD, Bjorndal A, Becerra‐Posada F, Gibson M, Block MA, Haines A, et al. A framework for mandatory impact evaluation to ensure well informed public policy decisions. Lancet 2010;375:427‐31. [DOI] [PubMed] [Google Scholar]
Rashid 2010
- Rashid C. Benefits and limitations of nurses taking on aspects of the clinical role of doctors in primary care: integrative literature review. Journal of Advanced Nursing 2010;66(8):1658‐70. [DOI] [PubMed] [Google Scholar]
Sanne 2010
- Sanne I, Orrell C, Fox MP, Conradie F, Ive P, Zeinecker J, et al. CIPRA‐SA Study Team. Nurse versus doctor management of HIV‐infected patients receiving antiretroviral therapy (CIPRA‐SA): a randomised non‐inferiority trial. Lancet 2010;376(9734):33‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shum 2000
- Shum C, Humphreys A, Wheeler D, Cochrane MA, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: multicentre randomised controlled trial. BMJ 2000;320:1038‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
SURE Collaboration 2011
- SURE Collaboration. SURE guides for preparing and using evidence‐based policy briefs: 5. Identifying and addressing barriers to implementing policy options. Version 2.1 (updated November 2011). Available from www.who.int/evidence/sure/guides.
Thomas 2008
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology 2008;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
van der Biezen 2017a
- Biezen M, Wensing M, Poghosyan L, Burgt R, Laurant M. Collaboration in teams with nurse practitioners and general practitioners during out‐of‐hours and implications for patient care; a qualitative study. BMC Health Services Research 2017;17:589. [DOI] [PMC free article] [PubMed] [Google Scholar]
van der Biezen 2017b
- Biezen M, Derckx E, Wensing M, Laurant M. Factors influencing decision of general practitioners and managers to train and employ a nurse practitioner or physician assistant in primary care: a qualitative study. BMC Family Practice 2017;18:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Ginneken 2011
- Ginneken N, Tharyan P, Lewin S, Rao GN, Romeo R, Patel V. Non‐specialist health worker interventions for mental health care in low‐ and middle‐income countries. Cochrane Database of Systematic Reviews 2011, Issue 5. [DOI: 10.1002/14651858.CD009149] [DOI] [PMC free article] [PubMed] [Google Scholar]
Venning 2000
- Venning P, Durie A, Roland M, Roberts C, Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ 2000;320:1048‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Voogdt‐Pruis 2010
- Voogdt‐Pruis H, Beusmans G, Gorgels A, Ree J. Adherence to a guideline on cardiovascular prevention: a comparison between general practitioners and practice nurses. International Journal of Nursing Studies 2010;48(7):798‐807. [DOI] [PubMed] [Google Scholar]
WHO 2004
- World Health Organization. Making Pregnancy Safer: the Critical Role of the Skilled Birth Attendant – a Joint Statement by WHO, ICM and FIGO. Geneva: World Health Organization, 2004. [Google Scholar]
WHO 2008
- World Health Organization. Task Shifting: Rational Redistribution of Tasks Among Health Workforce Teams: Global Recommendations and Guidelines. Geneva: World Health Organization, 2008. [Google Scholar]
WHO 2012
- World Health Organization. WHO Recommendations: Optimizing Health Worker Roles to Improve Access to Key Maternal and Newborn Health Interventions Through Task Shifting – OPTIMIZEMNH. Geneva: World Health Organization, 2012. [PubMed] [Google Scholar]
Wiley‐Exley 2007
- Wiley‐Exley E. Evaluations of community mental health care in low‐ and middle‐income countries: a 10‐year review of the literature. Social Science & Medicine 2007;64(6):1231‐41. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Rashidian 2013
- Rashidian A, Shakibazadeh E, Karimi‐Shahanjarini A, Glenton C, Noyes J, Lewin S, Colvin C, Laurant M. Barriers and facilitators to the implementation of doctor‐nurse substitution strategies in primary care: qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2013, Issue 2. [DOI: 10.1002/14651858.CD010412] [DOI] [PMC free article] [PubMed] [Google Scholar]