Abstract
Overview
As chronic disease and comorbidities increase, so does the complexity of patient care.
This complexity requires interdisciplinary care teams and multifactor interventions to ensure that patients get the most efficient care. Patient navigators—defined as individuals who help patients move through the complex care continuum—can improve access to care and patient engagement, which can translate into better outcomes. Health information technology (health IT) can support timely communication and information sharing for patient navigators and the providers with whom they interact to better coordinate care. We explored the health IT that patient navigators used, how they used it, and their health IT needs in community-based interventions.
Methods
We analyzed three years of qualitative program evaluation data captured though progress reports, site visits, and telephone interviews as part of a larger evaluation of community-based demonstration projects. We used inductive analysis to identify preliminary themes to develop a codebook. Using QSR International's NVivo qualitative analysis software (version 11.0), we then used the preliminary themes in a second round of independent coding. We identified themes relevant to navigators and to barriers and facilitators for health IT. Coders achieved a final kappa of 0.8, suggesting excellent interrater reliability.
Results
Navigators used various types of health IT (e.g., health information exchanges, electronic health records, short message service) to capture and share information with the rest of the care team. Navigators used technology to document patient information, track services, and schedule appointments for patients; however, some respondents reported challenges with systems that were not integrated. Navigators must learn to use health IT systems of varying complexity to complete their job duties.
Discussion
Health IT can improve workflow by facilitating task organization and communication with the care team. Ultimately, integrating the health IT systems used by navigators with those used by other care team members was most beneficial. Because of the various types of health IT used, patient navigators should receive training to ensure that they have the technical skills to use these systems efficiently and reduce duplication of effort.
Conclusion
Managing the care of patients with chronic disease requires comprehensive care teams, which can include patient navigators. Integrating navigators' documentation into other health IT systems can keep providers updated on information while patients are outside of the providers' care. With the growth of health IT use in recent years, technical skills are becoming increasingly important. These findings can help leaders who are planning complex health interventions involving navigators to ensure that technology is used efficiently to support coordination and allow navigators to reach more patients.
Keywords: navigator, health information technology (health IT), workflow, care coordination
Introduction and Background
Chronic diseases and comorbidities result in patients who are medically complex. These patients have a variety of needs and are seen by multiple providers, which increases the need for coordination and communication across providers. The number of Americans with chronic diseases, such as diabetes, has greatly increased in recent years.1 Additionally, the prevalence of people who experience multiple chronic conditions is also increasing.2 Chronic diseases affect low-income and minority populations disproportionately.3 These populations face significant challenges related to care management and patient engagement. Chronic diseases and associated conditions require multiple providers, an interdisciplinary care team,4 and multifactor health interventions.5 These factors point to the need for patient navigators to help these patients and to coordinate their care across members of the care team.
The role of patient navigators is to connect patients and their care team. Navigators can be nurses, social workers, laypeople trained in navigation, or certified community health workers. Regardless of professional background, they help patients overcome barriers to accessing, receiving, and engaging with their care. In addition, they can contribute to improved outcomes by facilitating coordination of care.6 Patient navigators help patients move through the care continuum to receive the medical services they need.7
The use of patient navigators spans care types (e.g., primary versus specialty care) and care settings (e.g., primary care, acute care, and long-term and post-acute care). Patient navigators have been used in specialty settings, such as to help cancer patients manage and overcome determinants of disparities in care (i.e., lack of health insurance, transportation, and patient education).8
The benefit of navigators for improving health outcomes and reducing disparities is widespread. They have helped achieve improvements in medication adherence, clinical outcomes, and attendance at appointments among chronic disease patients in primary and specialty care settings.9 Navigators contributed to improvements in breast and cervical cancer screening rates among Korean-American women10 and in delivering effective depression treatment for elderly patients.11 Among inner-city minority women, navigators helped improve timely diagnostic follow-up rates for those with potential breast cancer.12 Frequent communication among navigators, specialists, and other providers on behalf of the patients helped achieve this timely follow-up.
Patient navigators have become more involved in healthcare teams and community health interventions. As patient complexity increases, so does the number of stakeholders with whom the navigators must communicate. Time sensitivity, care sequencing, and workflow concerns mean that communication with care teams and patients must occur in a timely manner. Health information technology (health IT) can support information sharing between providers, navigators, and patients to better coordinate care. Health IT adoption has continued to grow among hospitals and ambulatory physicians, increasing at least 50 percent in recent years among hospitals and office-based physicians.13, 14
The benefits of patient navigation are predicated on being able to access information and also share it with care providers and patients to support coordination. To that end, health IT has been used to support navigator activities in several areas. Examples of health IT to support navigator activities include self-management for diabetes,15 online portals to connect patients to primary and specialty care services,16 and improvement of access to primary care.17 These studies demonstrate examples of health IT use by navigators. However, they often involve a single type of technology use in a single organization. Bidirectional information sharing (in which data can flow from existing health IT systems to navigators to support their interventions, and information on the status and outcomes of those interventions flows back to the rest of the care team) can facilitate navigators' integration into care teams. Further information across technology types and uses is needed to more fully understand navigators' needs and their use of health IT.
Because of the need for more research to understand navigators' use of health IT and the implications for health IT design and implementation, we sought to answer the following research questions:
How do patient navigators use health IT?
How can health IT be tailored to better meet the needs of patient navigators?
Do navigators need different skills for health IT systems?
Methods
The authors conducted an evaluation of the 24 Health Care Innovation Award recipients funded under the Community Resource Planning, Prevention, and Monitoring Models initiative between 2014 and 2017.18, 19 The Centers for Medicare and Medicaid Services awarded grants under this program to support implementation of community-based programs designed to enhance the quality of healthcare, improve health outcomes, and reduce the cost of providing care to Medicare, Medicaid, and Children's Health Insurance Program beneficiaries.
Awardees represented a variety of organizational types, including hospitals, community health centers, specialty care providers, universities, nonprofits, health plans, and health technology firms. Programs varied and included healthcare transformation through health IT and care coordination, information exchange, care delivery, and health promotion and education. The term patient navigator applies to the roles the awardees assigned or created to assist patients in overcoming barriers to care, particularly for complex cases. This analysis examines the six awardees that developed interventions involving health IT and navigators.20, 21 The awardees in this subset and their organizational types are listed in Table 1.
Table 1.
Health Care Innovation Award Community Resource Planning Awardees with Navigators as a Key Component of the Innovation
| Awardee | Organizational Type | Location |
|---|---|---|
| Bronx RHIO | Regional health information organization | New York, NY |
| Curators of the University of Missouri | Academic medical center | Columbia, MO |
| Finity Communications | Technology vendor | Portland, OR |
| Mary's Center for Maternal and Child Care | Federally qualified health center | Washington, DC |
| University of Chicago | Academic medical center | Chicago, IL |
| University of Miami | Academic medical center | Miami, FL |
Source: Centers for Medicare and Medicaid Services. “Health Care Innovation Awards.” 2014. Available at https://innovation.cms.gov/initiatives/Health-Care-Innovation-Awards/
The authors collected and analyzed program data over the course of three years. Documentary data provided by the awardees consisted of progress reports that the awardees prepared quarterly. The reports included updates on implementation activities and the results of the awardees' internal evaluation processes. To supplement this reporting and obtain perspectives from awardees, the authors conducted site visits and telephone interviews. These interviews were conducted with various members of the awardee teams, including administrators, patient navigators, and providers. The research team developed semistructured interview guides tailored to each role to more fully understand program design, implementation progress, partnerships, organizational resources and capacity, workforce development, and lessons learned.
Using an inductive analytic approach to elicit themes from the collected data, the research team independently reviewed a sample of the data and identified preliminary themes to develop a codebook. Using QSR International's NVivo qualitative analysis software (version 11.0), we then used the preliminary themes in a second round of independent coding. Ambiguous passages were flagged and discussed within the group or adjudicated by a third reader to refine the codebook. To ensure consistency in coding, approximately 40 percent of the qualitative text was double-coded and then adjudicated by a third reader. Coders achieved a final kappa of 0.8, suggesting excellent interrater reliability.22
Results
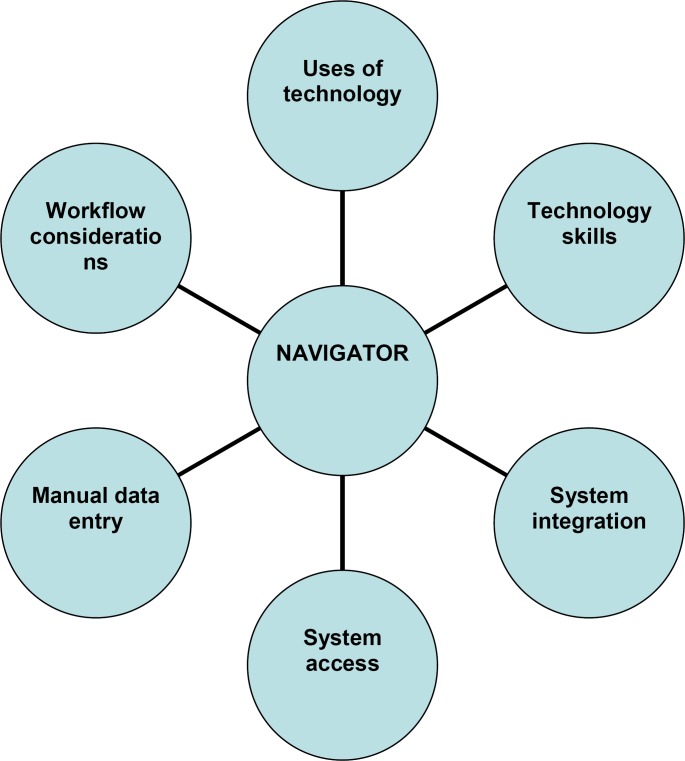
The educational backgrounds and roles of the patient navigators varied across awardees, with subsequent variation in responsibilities. The navigators included nurse navigators, community health workers, peer health mentors, and community lay workers trained by the awardee. The role of the navigators influenced how their use of technology, their workflow, their system access, and the integration of their role with the rest of the team and other systems. These and other concepts that influence how navigators interact with technology are illustrated in Figure 1.
Figure 1.
Factors Influencing Navigators' Interaction with Technology
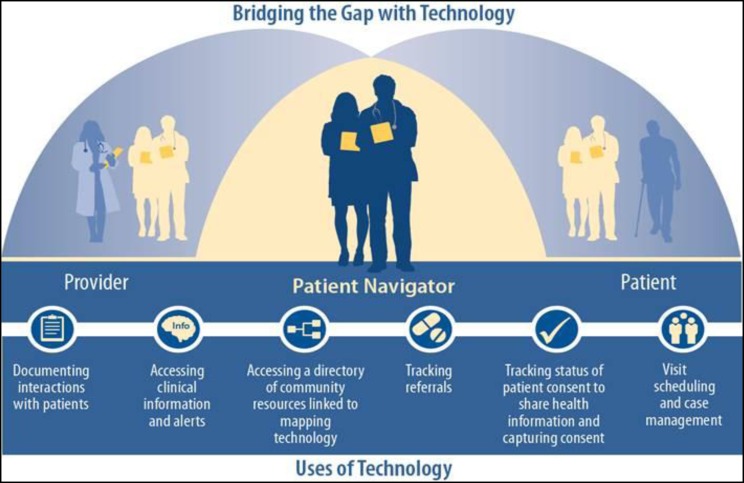
Uses of Technology
Navigators consistently used health IT to help patients access and use healthcare. As one awardee leader said about navigators, “[They] are a new type of community health worker with hyper-local, expert knowledge about places in the community where individuals can get goods and services to manage their health and who uses information technology to collate, manage and search this information.” While use of technology was consistent, the ways in which technology was used and the types of tools used varied, as shown in Figure 2. Technology uses included documentation, patient tracking, and appointment scheduling.
Figure 2.
Navigators' Various Uses of Technology. Source: Addendum to Centers for Medicare and Medicaid Services. Evaluation of the Health Care Innovation Awards: Community Resource Planning, Prevention, and Monitoring: Third Annual Report. 2017. Available at https://downloads.cms.gov/files/cmmi/hcia-crppm-thirdannrptaddendum.pdf.
Workflow
Technology use influenced the workflows of both the navigators and the rest of the care team. Integrating navigator documentation into electronic health records (EHRs) required fewer workflow accommodations from the rest of the care team than when separate systems were used. Separate systems may also have necessitated manual double data entry. Navigators who worked in the field also had some difficulties accessing necessary patient information. Discussion of these issues follows.
Importance of Integrated Systems
Awardees used EHRs, messaging, and health information exchange (HIE) to share information captured by navigators with the rest of the care team. For three awardees, sharing health information was a key component of the navigators' work. The rest of the care team could review data captured by navigators receive updates outside of the visit. As one administrator indicated, “The HIE part has always been viewed as essential to the CHWs' [community health workers'] work. The CHWs can go out and meet with these people and manage them on an individual basis but it is bringing in the HIE that allows that massive flow of data in both directions… . When the clinics can share all the information with the CHWs and see the information of what CHWs have been doing we can begin to really look at population health.”
This same awardee developed a navigator case management system integrated with providers' EHRs via HIE. Another awardee expressed the desire for more efficient workflow and input, stating, “CHWs should just be able to press the right button in the EMR [electronic medical record] without requiring them to write anything. We should have data templates that flow from one check box to the next. I want the CHWs to check off what they did for the patient, whether it's education, or medication, which then flows into more specific information.” Awardees expressed that lack of integration made it difficult for navigators to interact with other team members.
Manual Data Entry
Three awardees indicated that navigators had to document the same information from their patient interactions in different systems. Awardees used separate systems to support communication and capture encounter data. For example, one provider stated, “Now we have access to the information they gather in the homes. They are gathering the information on paper and then they are inputting the information into the [reporting system] and the EHR. We only have [access to] information in the EHR, so the CHWs are doing double work. If they have to do double work, they [must] see fewer patients.”
Another awardee reported that navigators had to first document information on paper and then manually enter the data into an electronic version of the paper form because of lack of internet access in the field. Although the electronic system was reportedly easy to use, the system did not initially accommodate navigators' need because it was initially designed for the supervisors to use. Documenting in multiple places created inconsistencies in the data, such as the number of home visits completed. Over time, the navigators worked with the program manager and developers to refine the system and workflow, but the issue of dual entry remained.
Lack of Access to Systems in the Field
Two awardees reported issues with access to patient information. Some navigators in these innovations did not have access to patient information while on home visits. This limitation meant that navigators had to manually look up information beforehand and also had to enter data about the visit later. To illustrate this, one navigator stated, “Having a [t]ablet would be really useful. I need something I could take with me to the home, because sometimes I end up taking triple documentation to the home. Documentation can take up your day. We have the paper documentation which we have to put in the registry and then EHR. I don't always remember everything. If it had EHR and reporting system, we could at least do one, or download it and upload it when we get into the office. The data input becomes overkill and the patients have to see us with our bags [overflowing with] papers.”
Technology Skills of Navigators
In many cases, the navigator was a new role for awardees. Thus, the job descriptions, required skills, and responsibilities were adjusted as the role was refined. This changing nature of the role was reflected in hiring. Initially, awardees did not prioritize technical literacy and skills in hiring. Instead they prioritized skills related to being proactive and outgoing. However, as the role evolved and technology became a large part, technical skills were added to job descriptions and hiring processes. In one innovation, CHWs used a dedicated case management system that linked to the EHR system. Training and support were required to ensure timely and accurate recordkeeping, and those with technical skills at baseline were more successful. Another awardee reported that navigators needed technical skills to use the clinic's EHR system, and a third awardee trained navigators to use short message service (SMS) to complement their HIE for patient outreach. This awardee trained their navigators to respond to messages and developed a workflow for documenting SMS interactions.
One awardee said, “The CHWs need to know a lot to do their jobs, operating a computer, accessing EMR in the field; they carry electronic signature devices, edit or load all demographic information into the patient record, perform intake interviews, schedule the initial clinical visit.”
Discussion
We found that integration of systems, workflows, roles, and responsibilities was a key driver of efficiency. When systems and processes were not integrated, challenges such as dual data entry, lack of access, and lack of care team integration were more likely. In addition, we found that technology acceptance and literacy was a significant part of the navigator role.
Use Health IT to Create Workflow Efficiencies for Navigators
Health IT that is integrated with EHRs and with clinical and administrative processes can improve workflow and alleviate some of the challenges cited by the awardees. As indicated in Figure 2, navigators used health IT for a variety of functions. The specific technology varied, but integration of these functions with other health IT systems and care team activities was a key factor in workflow and clinical efficiencies for the awardees.
Improvements are realized by facilitating task organization and by communicating with the care team.23 Organizing tasks helps navigators maximize their productivity.24 By improving efficiency in task management, navigators can provide more services, ultimately providing more opportunities to improve outcomes. This finding aligns with previous research showing that CHWs used EHRs to communicate with providers, make appointments, and track patients.25
In sum, leaders and planners who are developing community health interventions for patients should consider integrating the navigators' health IT systems (e.g., electronic notes, care management systems) to facilitate the following:
Access to the EHRs used by the rest of the care team,
• Management and documentation of interactions with patients, and
Communication with the care team.
Engage Navigators in Health IT Design
This study points to the need to design roles and systems in tandem. The awardees either were new to having navigators or were using them in a different way. Therefore, the navigators' roles, responsibilities, information needs, and documentation processes were also new. In addition, navigators were implemented in tandem with an increased focus on a team-based approach. This situation indicates the need to engage both the navigator and associated team members when health IT systems and related processes are designed.
When specific functionalities for documentation and information sharing are not fully considered, some navigators may need to rely on workarounds like dual data entry—a common workaround to overcome interoperability challenges—to ensure that their documentation populates the necessary systems.26 Several awardees in our study reported challenges with inefficiencies such as dual data entry; however, only two awardees reported regularly engaging their navigators to design and refine systems.
Seeking and using feedback from navigators when developing health IT systems that they will use helps ensure that they will have the right tools to support their activities. Functionality and tools include specific electronic forms, note-taking templates, and tracking systems. Obtaining users' input can help refine health IT systems, making them more useful for end users.27 For example, in the development of a diabetes web application for CHWs, CHWs regularly met with vendors and other care team members to provide feedback on their tracking forms and reports.28 Additionally, as a result of CHWs' feedback after the study, the vendor added a “free note” to the system to allow CHWs to document notes from unscheduled calls, helping refine the system. Consistent with this evidence, in our current study, one awardee's navigators reported working with their technical team to improve the electronic forms they used for documentation as the intervention progressed.
Not only should health system leaders seek to integrate navigators' health IT tools into existing systems, but they should also involve navigators in the development process.
Incorporate Technical Skills into Hiring and Training of Navigators
Although navigators are not traditionally considered a technical role, those serving in this position need to have technical skills and awareness. The necessary technical skills included familiarity and comfort with a variety of software systems, the ability to run reports, and the ability to use different hardware systems (e.g., tablet, laptop). In our study, although awardees noted that navigators should be self-starting, gregarious, and outgoing in care settings, those skills alone did not assist in documentation using the systems. Patient navigator training programs often omit training on technology systems.29–31 Thus, awardees in the current study often reported refining their hiring processes after identifying the specific skill set and personality traits needed for productivity and efficiency. In addition, they reported the importance of considering technology along with roles and responsibilities when developing job descriptions and associated training.
Certification and training programs for navigators should incorporate health IT education so that they can combine technical skills with their existing skill set. Intervention planners can also include health IT experience as a desired trait in job postings.
Limitations
We were able to obtain feedback directly from innovation leaders, clinicians, and navigators themselves about their technology use and workflow. The study also examined diverse organizational types. We obtained specific feedback on how health IT affected navigators' workflow and how they worked with other stakeholders on the care team to refine processes and the technology itself. Although we were able to obtain this valuable feedback, we had only a limited number of awardees, all with different interventions. These limitations make our findings less generalizable to other interventions. Future studies should compare interventions that use a combination of navigators and technology with those that use solely navigators. This research would help to determine whether health IT is a driver of efficiency and outcomes for navigators.
Conclusions
Managing the care of complex patients requires comprehensive care teams. Adding patient navigators to extend organizational capacity and improve coordination increases the need for seamless information exchange. Information flow ensures that the entire care team has a comprehensive picture of the patient's status. Thus, it is important to consider navigators' technology needs and how navigators will interact with the technology. Ideally, health IT solutions should be integrated, functional, and easy to use. To coincide with the growth of health IT use in recent years, technical skills are becoming increasingly important for navigators. These findings can help leaders who are planning community health interventions involving navigators to ensure that technology is used in the most efficient manner. These efficiencies can create a more integrated team and allow navigators to reach more patients, ultimately increasing the amount of services that vulnerable patients receive.
Research Disclaimer
This publication was made possible by Contract Number HHSM-500-2010-00021I from the US Department of Health and Human Services, Centers for Medicare and Medicaid Services. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the US Department of Health and Human Services or any of its agencies.
Contributor Information
Saira Haque, RTI International in Research Triangle Park, NC..
Shellery Ebron, RTI International in Research Triangle Park, NC..
Bob Bailey, RTI International in Research Triangle Park, NC..
Barry Blumenfeld, RTI International in Research Triangle Park, NC..
Notes
- 1.Centers for Disease Control and Prevention Diabetes Report Card 2014. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services. 2015 [Google Scholar]
- 2.Vogeli C., Shields A., Lee T., Gibson T., Marder W., Weiss K., Blumenthal D. “Multiple Chronic Conditions: Prevalence, Health Consequences, and Implications for Quality, Care Management and Costs.”. Journal of General Internal Medicine. 2007;22(suppl. 3):391–95. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services Office of Disease Prevention and Health Promotion Healthy People 2020. “Disparities.” 2017. Available at https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities [Google Scholar]
- 4.Bodenheimer T., Chen E., Bennett H. “Confronting the Growing Burden of Chronic Disease: Can the U.S. Health Care Workforce Do the Job?”. Health Affairs. 2009;28(no. 1):64–74. doi: 10.1377/hlthaff.28.1.64. [DOI] [PubMed] [Google Scholar]
- 5.Bauer U., Briss P., Goodman R., Bowman B. “Prevention of Chronic Disease in the 21st Century: Elimination of the Leading Preventable Causes of Premature Death and Disability in the USA.”. Lancet. 2014;384:45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 6.Powell R., Doty A., Casten R., Rovner B., Rising K. “A Qualitative Analysis of Interprofessional Healthcare Team Members' Perceptions of Patient Barriers to Healthcare Engagement.”. BMC Health Services Research. 2016;16(no. 493):1–10. doi: 10.1186/s12913-016-1751-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freeman H., Rodriguez R. “History and Principles of Patient Navigation.”. Cancer. 2011;117(suppl. 15):3537–40. doi: 10.1002/cncr.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wells K., Battaglia T., Dudley D., Garcia R., Greene A., Calhoun E., S. Mandelblatt J., D. Paskett E., C. Raich P., the Patient Navigation Research Program “Patient Navigation: State of the Art, or Is It Science?”. Cancer. 2008;113(no. 8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ursua, A. R., E. Aguilar D., C. Wyatt L., Katigbak C., S. Islam N., D. Tandon S., R. Nur P., Van Devanter N., J. Rey M., Trinh-Shevrin C. “A Community Health Worker Intervention to Improve Management of Hypertension among Filipino Americans in New York and New Jersey: A Pilot Study.”. Ethnicity & Disease. 2014;24(no. 1):67–76. [PMC free article] [PubMed] [Google Scholar]
- 10.Han H., Song Y., Kim M., Hedlin H., Kim K., Lee H., Roter D. “Breast and Cervical Cancer Screening Literacy among Korean American Women: A Community Health Worker-led Intervention.”. American Journal of Public Health. 2017;107(no. 1):159–65. doi: 10.2105/AJPH.2016.303522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joo J., Hwang S., Abu H., Gallo J. “An Innovative Model of Depression Care Delivery: Peer Mentors in Collaboration with a Mental Health Professional to Relieve Depression in Older Adults.”. American Geriatric Psychiatry. 2016;24(no. 5):407–16. doi: 10.1016/j.jagp.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Battaglia, A. T., Roloff K., A. Posner M., M K., Freund “Improving Follow-up to Abnormal Breast Cancer Screening in an Urban Population.”. Cancer. 2007;109:359–67. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 13.Charles D., Gabriel M., Furukawa M. Adoption of Electronic Health Record Systems among U.S. Non-federal Acute Care Hospitals: 2008–2013. Washington, DC: Office of the National Coordinator for Health Information Technology; 2014. [Google Scholar]
- 14.Hsiao C.-J., Hing E. Use and Characteristics of Electronic Health Record Systems among Office-based Physician Practices: United States, 2001–2013. 2014 NCHS Data Brief No. 143. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- 15.Lopez L., Grant R. “Closing the Gap: Eliminating Health Care Disparities among Latinos with Diabetes Using Health Information Technology Tools and Patient Navigators.”. Journal of Diabetes Science and Technology. 2012;6(no. 1):169–76. doi: 10.1177/193229681200600121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Highfield L., Ottenweller C., Pfanz A., Hanks J. “Interactive Web-based Portals to Improve Patient Navigation and Connect Patients with Primary Care and Specialty Services in Underserved Communities.”. Perspectives in Health Information Management. (Spring 2014). [PMC free article] [PubMed] [Google Scholar]
- 17.Peart A., Lewis V., Brown T., Russell G. “Patient Navigators Facilitating Access to Primary Care: A Scoping Review.”. BMJ Open. 2018;8:e019252. doi: 10.1136/bmjopen-2017-019252. doi:10.1136/bmjopen-2017-019252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare and Medicaid Services “Health Care Innovation Awards.”. 2014 Available at https://innovation.cms.gov/initiatives/Health-Care-Innovation-Awards/ [Google Scholar]
- 19.Centers for Medicare and Medicaid Services Evaluation of the Health Care Innovation Awards: Community Resource Planning, Prevention, and Monitoring: Third Annual Report. 2017 Available at https://downloads.cms.gov/files/cmmi/hcia-communityrppm-thirdannualrpt.pdf. [Google Scholar]
- 20.Ibid
- 21.Centers for Medicare and Medicaid Services “Health Care Innovation Awards.” [Google Scholar]
- 22.QSR International The Kappa Statistic in Reliability Studies: Use, Interpretation, and Sample Size Requirements”. Physical Therapy. 2005 doi:10.1093/ptj/85.3.257. ISSN 1538-6724. [PubMed] [Google Scholar]
- 23.Cain C., Haque S. Rockville, MD: Agency for Healthcare Research and Quality; 2008. “Organizational Workflow and Its Impact on Work Quality.” In R. G. Hughes (Editor), Patient Safety and Quality: An Evidence-Based Handbook for Nurses. pp. 217–44. [PubMed] [Google Scholar]
- 24.Jaskiewicz W., Tulenko K. “Increasing Community Health Worker Productivity and Effectiveness: A Review of the Influence of the Work Environment.”. Human Resources for Health. 2012;10(no. 38):1–10. doi: 10.1186/1478-4491-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allen, G. C., Escoffery C., Satsangi A., N J., Brownstein “Strategies to Improve the Integration of Community Health Workers into Health Care Teams: ‘A Little Fish in a Big Pond.’”. Preventing Chronic Disease. 2015;12:E154. doi: 10.5888/pcd12.150199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cifuentes M., Davis M., Fernald D., Gunn R., Dickinson P., J. Cohen D. “Electronic Health Record Challenges, Workarounds, and Solutions Observed in Practices Integrating Behavioral Health and Primary Care.”. Journal of the American Board of Family Medicine. 2015;28(suppl. 1):S63–S72. doi: 10.3122/jabfm.2015.S1.150133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cain C., Haque S. “Organizational Workflow and Its Impact on Work Quality.”. [PubMed] [Google Scholar]
- 28.Cherrington A., Agne A., Lampkin Y., Birl A., Shelton T., Guzman A., Willig J. “Diabetes Connect: Developing a Mobile Health Intervention to Link Diabetes Community Health Workers with Primary Care.”. Journal of Ambulatory Care Management. 2015;38(no. 4):333–45. doi: 10.1097/JAC.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shelton R., Thompson H., Jandorf L., Varela A., Oliveri B., Villagra C., B. Valdimarsdottir H., Redd W. “Training Experiences of Lay and Professional Patient Navigators for Colorectal Cancer Screening.”. Journal of Cancer Education. 2011;26(no. 2):277–84. doi: 10.1007/s13187-010-0185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jean-Pierre P., Hendren S., Loader S., Rousseau S., Schwartzbauer B., Sanders M., Carroll J., Epstein R. “Understanding Processes of Patient Navigation to Reduce Disparities in Cancer Care: Perspectives of Trained Navigators from the Field.”. Journal of Cancer Education. 2011;26(no. 1):111–20. doi: 10.1007/s13187-010-0122-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DeGroff A., Coa K., Morrissey K., Rohan E., Slotman B. “Key Considerations in Designing a Patient Navigation Program for Colorectal Cancer Screening.”. Health Promotion Practice. 2014;15(no. 4):483–95. doi: 10.1177/1524839913513587. [DOI] [PMC free article] [PubMed] [Google Scholar]