Abstract
In many countries including Japan, the status of emerging antimicrobial resistance among Serratia spp. and Citrobacter spp. in companion animals remains unknown because these genera are rarely isolated from animals. In this study, 30 Serratia spp. and 23 Citrobacter spp. isolates from companion animals underwent susceptibility testing for 10 antimicrobials. Phenotypic and genetic approaches were used to identify the mechanisms of extended-spectrum cephalosporins (ESC). Subsequently, ESC-resistant Citrobacter spp. strains underwent multilocus sequence typing and pulsed-field gel electrophoresis (PFGE). A significantly higher rate (34.8%) of ESC resistance was observed in Citrobacter spp. isolates than in Serratia spp. isolates (0%). ESC resistance was detected in five C. freundii strains, two C. portucalensis strains, and one C. koseri strain. All of the ESC-resistant Citrobacter spp. strains harbored CMY-type and/or DHA-type AmpC β-lactamases. Three C. freundii strains harbored the CTX-M-3-type extended-spectrum β-lactamases. Notably, the three blaCTX-3-producing and two blaCMY-117-bearing C. freundii strains (obtained from different patients in one hospital) had the same sequence type (ST156 and ST18, respectively) and similar PFGE profiles. We believe that ESC-resistant Citrobacter spp. are important nosocomial pathogens in veterinary medicine. Therefore, infection control in animal hospitals is essential to prevent dissemination of these resistant pathogens.
Keywords: Serratia spp., Citrobacter spp., companion animals, extended-spectrum cephalosporin resistance, nosocomial dissemination
1. Introduction
The genera of Serratia and Citrobacter, belonging to the Enterobacteriaceae family, are opportunistic nosocomial pathogens and cause a wide spectrum of human infections [1,2]. In companion animals, these genera are also rarely associated with infections such as pneumonitis, urinary tract infection, myocarditis, septicemia, and intravenous catheter site infection [3]. The Citrobacter genus previously comprised 11 species [4], but recently, two new species (i.e., C. pasteurii and C. portucalensis) have been proposed [5,6]. Serratia marcescens and Citrobacter freundii are the most important species in each genus, medically speaking [7,8]. However, the species distribution in these genera has not yet been elucidated in veterinary medicine.
The emergence of multidrug resistance—notably, resistance to extended-spectrum cephalosporins (ESC)—among Serratia spp. and Citrobacter spp. is a worldwide concern to human medicine [1]. Together with Pseudomonas spp., Acinetobacter spp., and Enterobacter spp., these genera are hospital-acquired Gram-negative bacilli which can easily develop antimicrobial resistance and are often grouped as the SPACE organisms [9]. ESC resistance in these bacteria is usually caused by overproduction of AmpC β-lactamases, secondary to the derepression of a chromosomal gene or acquisition of a transferable AmpC β-lactamase [9]. Additionally, extended-spectrum β-lactamases (ESBLs) and carbapenemases have been identified in Serratia spp. and Citrobacter spp. [1,10], which exacerbates ESC resistance. However, in many countries including Japan, the status of emerging antimicrobial resistance among Serratia spp. and Citrobacter spp. in companion animals remains unknown.
Therefore, we performed an epidemiological investigation of the predominance of antimicrobial resistance and provide molecular characterization of ESC resistance among Serratia spp. and Citrobacter spp. isolates recovered from clinical specimens of dogs and cats in Japan.
2. Materials and Methods
We evaluated a total of 53 clinical isolates including 30 Serratia spp. and 23 Citrobacter spp. isolates collected from dogs (n = 36) and cats (n = 17) housed by different owners who visited veterinary hospitals between 2012 and 2016. Table S1 shows the details of the isolates used in this study, including the specific locations of hospitals and isolation sites. Specimens were isolated using sterile cotton swabs from various anatomical sites, identified as sites of bacterial infection by many clinical veterinarians in 15 prefectures in Japan and submitted to Tottori University and Sanritsu Zelkova Laboratory for analysis. All confirmed isolates were stored at −80 °C in 10% skim milk.
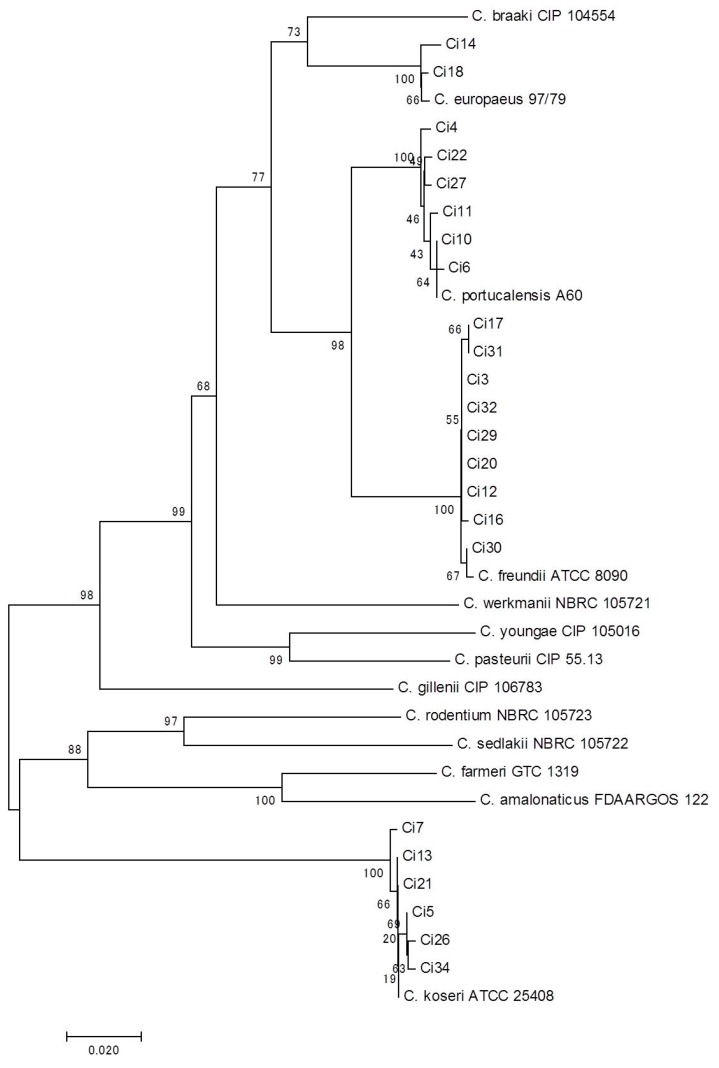
Bacterial species identification was determined based on growth conditions on CHROMagar orientation medium (Nippon Becton Dickinson and Company, Ltd., Tokyo, Japan) and by using the API 20E kit (SYSMEX bioMérieux Co., Ltd., Tokyo, Japan), MicroScan WalkAway (Beckman Coulter, Inc., Tokyo, Japan), and MALDI-TOF MS with a Bruker MALDI Biotyper system (Bruker Daltonik, Bremen, Germany). Additionally, the species of Citrobacter spp. isolates were confirmed based on the phylogeny of the recN (DNA repair protein) gene, as described previously [11]. Briefly, PCR amplification and further sequencing of recN genes were performed. Then, we constructed a phylogenetic tree based on the recN sequences of our strains and type strains of each species using MEGA version 7.0.18 [12] using the neighbor-joining (NJ) method [13]. The genetic distance among these strains was calculated using the Kimura two-parameter model [14].
We determined the susceptibilities of these bacterial species to amoxicillin–clavulanic acid (ACV, Sigma-Aldrich Co. LLC., Tokyo, Japan), cephalothin (CPL, Sigma-Aldrich), cefmetazole (CMZ, Sigma-Aldrich), cefotaxime (CTX, Wako Pure Chemical Industries, Ltd., Osaka, Japan), meropenem (Wako Pure Chemical), tetracycline (TET, Wako Pure Chemical), amikacin (Sigma-Aldrich), chloramphenicol (CHL, Wako Pure Chemical), trimethoprim/sulfamethoxazole (TMS, Wako Pure Chemical), and ciprofloxacin (CIP, Wako Pure Chemical). We used the agar dilution method to perform susceptibility testing in accordance with the Clinical and Laboratory Standards Institute (CLSI) guidelines [15]. The susceptibility results were interpreted in relation to the CLSI guideline criteria [16]. Escherichia coli ATCC 25922 was used as a control strain. ESC-resistant (i.e., minimum inhibitory concentration (MIC) for CTX of ≥ 4 µg/mL) strains were screened for ESBLs using the double-disc synergy test with CTX, ceftazidime, cefepime, and ACV disks on Mueller–Hinton agar plates with or without 200 µg/mL cloxacillin [17]. Additionally, ESC-resistant isolates without the synergistic effect of clavulanate and with inhibition zones enhanced by cloxacillin were classified as organisms overexpressing AmpC β-lactamase [18].
All ESC-resistant strains were screened for class A β-lactamase genes (i.e., blaTEM and blaSHV) and acquired AmpC β-lactamase (qAmpC) genes (i.e., the ACC, FOX, MOX, DHA, CIT, and EBC groups) on PCR as previously described [19,20]. The amplified products underwent bidirectional sequencing using specific primers [19,21]. In ESBL-positive strains, multiplex PCR was used to detect the CTX-M-type β-lactamase genes [22]. For the positive isolates, genes were amplified and sequenced to distinguish CTX-M subtypes using group-specific PCR primers [19]. A previous conjugation experiment [23] with slight modifications confirmed the transferability of ESBL genes. The E. coli DH5α strain (Thermo Fisher Scientific K.K., Tokyo, Japan) was used as a recipient, and transconjugants were selected on DHL-agar containing rifampicin (50 µg/mL) and CTX (2 µg/mL).
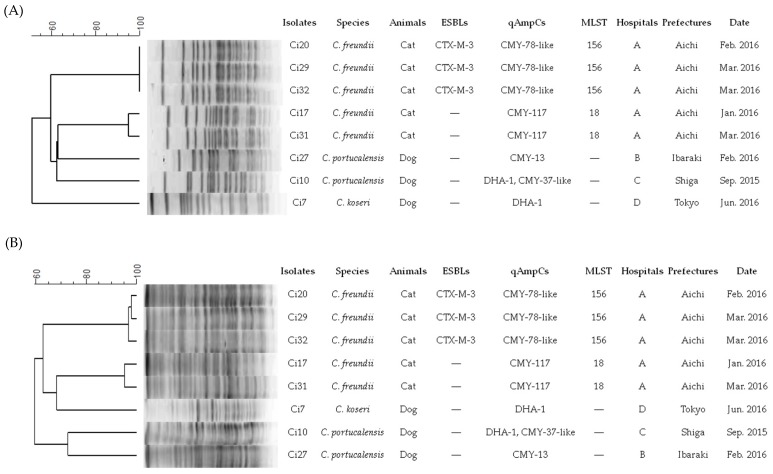
Pulsed-field gel electrophoresis (PFGE) was conducted on ESC-resistant C. freundii strains as previously described [2,24]. Bacterial DNA was digested with XbaI and SfiI and electrophoresed using CHEF-DR II (Bio-Rad Laboratories, Richmond, CA, USA). Then, PFGE profiles were digitized for analysis using GelCompar II (Applied Maths, Inc., Austin, TX, USA). Finally, multilocus sequence typing (MLST) with seven genes (i.e., aspC, clpX, fadD, mdh, arcA, dnaG, and lysP) was performed as previously described [25]. A new sequence type (ST) was submitted to the MLST website and new ST numbers were assigned.
3. Results and Discussion
Few studies have reported the species distribution and prevalence of antimicrobial resistance in the overall population of Serratia spp. and Citrobacter spp. clinical isolates from companion animals. The bacterial species of our collection were identified by several conventional methods and finally determined by MALDI-TOF MS (in Serratia spp.) and recN phylogeny (in Citrobacter spp.). We classified 30 Serratia spp. isolates into S. marcescens (n = 26), S. liquefaciens (n = 2), S. fonticola (n = 1), and S. ureilytica (n = 1); therefore, S. marcescens is most likely the major species of the genus in companion animals and in human medicine [4]. We conclusively determined 23 Citrobacter spp. isolates based on recN phylogeny as follows: C. freundii (n = 9), C. koseri (n = 6), C. portucalensis (n = 6), and C. europaeus (n = 2) (Figure 1). To the best of our knowledge, this is the first report on the isolation of C. portucalensis and C. europaeus strains from animals, although these species have been rarely reported in humans [26,27]. These findings imply the prevalence of several Citrobacter species in companion animals, in addition to C. freundii. We also found discrepancies in bacterial species between conventional phenotypic methods and the more reliable methods (i.e., MALDI TOF-MS and recN phylogeny) in several strains (Table S1); this suggests that phenotypic methods are limited in their ability to identify species of Serratia spp. and Citrobacter spp.
Figure 1.
Neighbor-joining tree based on recN gene sequences from our data collection and type strains of Citrobacter species. Genetic distances were constructed using Kimura’s two-parameter method. Bootstrap values obtained after 1000 replicates are given at the nodes [11]. The corresponding GenBank/Patric accession numbers of type strains refer to the previous report by Ribeiro et al. [6].
Table 1 shows the MIC distribution of the 10 tested antimicrobials in both genera. There were significant differences in overall resistance rates to six antimicrobials: Serratia spp. isolates exhibited higher rates of resistance to CPL (100%) and TET (86.7%), compared to the Citrobacter spp. isolates which exhibited higher rates of resistance to CTX (34.8%), CIP (26.1%), and TMS (17.4%). Previous work demonstrated higher rates of resistance to ACV (93.3%), CMZ (93.3%), CHL (46.7%), and CIP (43.3%) in Enterobacter spp. isolates from companion animals in Japan during 2003–2015 [28]. On the other hand, moderate rates of resistance to CIP (20.5% and 11.9%) were validated in Pseudomonas spp. and Acinetobacter spp. isolates from companion animals in Japan during the periods of 2003–2010 and 2012–2016, respectively [29,30], suggesting that SPACE organisms from companion animals have different antimicrobial resistance profiles by genus.
Table 1.
Minimum inhibitory concentration (MIC) distribution and resistance rates among Serratia spp. and Citrobacter spp. isolates from dogs and cats.
| Agents | Genera (No. of Isolates) | MIC (µg/mL) | No. of Resistance (%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤0.031 | 0.063 | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | 32 | 64 | 128 | 256 | >256 | |||
| CPL | Serratia (30) | 30 | 30 (100) * | ||||||||||||||
| Citrobacter (23) | 2 | 2 | 1 | 1 | 4 | 2 | 1 | 10 | 18 (78.3) | ||||||||
| CMZ | Serratia (30) | 2 | 9 | 10 | 5 | 4 | 4 (13.3) | ||||||||||
| Citrobacter (23) | 1 | 3 | 1 | 1 | 5 | 5 | 6 | 1 | 7 (30.4) | ||||||||
| CTX | Serratia (30) | 2 | 14 | 13 | 1 | 0 (0.0) | |||||||||||
| Citrobacter (23) | 3 | 6 | 6 | 1 | 1 | 1 | 2 | 1 | 2 | 8 (34.8) * | |||||||
| MPM | Serratia (30) | 4 | 25 | 1 | 0 (0.0) | ||||||||||||
| Citrobacter (23) | 19 | 3 | 1 | 0 (0.0) | |||||||||||||
| TET | Serratia (30) | 1 | 1 | 2 | 7 | 14 | 5 | 26 (86.7) * | |||||||||
| Citrobacter (23) | 1 | 15 | 1 | 2 | 1 | 1 | 2 | 4 (17.4) | |||||||||
| AMK | Serratia (30) | 4 | 3 | 20 | 3 | 0 (0.0) | |||||||||||
| Citrobacter (23) | 2 | 5 | 13 | 2 | 1 | 0 (0.0) | |||||||||||
| CHL | Serratia (30) | 2 | 14 | 10 | 2 | 1 | 1 | 4 (13.3) | |||||||||
| Citrobacter (23) | 17 | 4 | 1 | 1 | 2 (8.7) | ||||||||||||
| CIP | Serratia (30) | 4 | 4 | 16 | 4 | 1 | 1 | 0 (0.0) | |||||||||
| Citrobacter (23) | 6 | 2 | 2 | 3 | 1 | 1 | 2 | 2 | 3 | 1 | 6 (26.1) * | ||||||
| 0.125/0.063 | 0.25/0.125 | 0.5/0.25 | 1/0.5 | 2/1 | 4/2 | 8/4 | 8/16 | 32/16 | 64/32 | 128/64 | 256/128 | >256/128 | |||||
| ACV | Serratia (30) | 1 | 3 | 1 | 2 | 15 | 8 | 25 (83.3) | |||||||||
| Citrobacter (23) | 3 | 2 | 4 | 5 | 9 | 14 (60.9) | |||||||||||
| ≤0.03/0.59 | 0.06/1.19 | 0.13/2.38 | 0.25/4.75 | 0.5/9.5 | 1/19 | 2/38 | 4/76 | 8/152 | 16/304 | 32/608 | 64/1216 | >64/1216 | |||||
| TMS | Serratia (30) | 4 | 5 | 18 | 3 | 0 (0.0) | |||||||||||
| Citrobacter (23) | 9 | 5 | 1 | 2 | 1 | 1 | 1 | 3 | 4 (17.4) * | ||||||||
CPL, cephalothin; CMZ, cefmetazole; CTX, cefotaxime; MPM, meropenem; TET, tetracycline; AMK, amikacin; CHL, chloramphenicol; CIP, ciprofloxacin; ACV, amoxicillin–clavulanic acid; TMS, trimethoprim–sulfamethoxazole. Vertical lines indicate breakpoints of each drug according to the Clinical and Laboratory Standards Institute guideline [10]. * Significant differences in resistance rates between Serratia spp. and Citrobacter spp. (p < 0.05).
ESC resistance was identified in none of the Serratia spp. isolates and in 8 of 23 Citrobacter spp. isolates, namely, C. freundii (n = 5), C. portucalensis (n = 2), and C. koseri (n = 1) (Table 2). All ESC-resistant isolates had an MIC for MPM of ≤ 0.125 µg/mL, indicating that these isolates were negative for carbapenemase [31]. Of these ESC-resistant Citrobacter spp. strains, the three C. freundii strains harbored nontransferable blaCTX-M-3, which has previously been detected in Enterobacteriaceae in companion animals in Japan [28,32,33], as well as in France [34], South Korea [35], and China [36]. To the best of our knowledge, ours is the first report to detect blaCTX-M-3 among Citrobacter spp. isolates from companion animals, although Ewers et al. previously reported C. freundii isolates producing blaCTX-M-1 or blaSHV-12 in European countries [37]. The present study demonstrated ESBLs in 3 of 23 (13.0%) Citrobacter spp. isolates, comparable to previous work in companion animals in European countries (9/77, 11.7%) [37]. On the other hand, Kanamori et al. [2] previously detected ESBLs in 67 of 348 (19.3%) human isolates in Japan, but no evidence of blaCTX-M-3. Hence, it is likely that different types of ESBLs are prevalent in Citrobacter spp. isolates between companion animals and humans in Japan.
Table 2.
Characterization of eight extended-spectrum cephalosporin (ESC)-resistant Citrobacter spp. strains from dogs and cats.
| Strain | Year | Host | Origin | ST | AmpC Overexpression | ESBLs | qAmpCs | Other β-lactamases | MIC (μg/mL)b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACV | CPL | CMZ | CTX | MPM | TET | CHL | AMK | CIP | TMS | |||||||||
| C. freundii (n = 5) | ||||||||||||||||||
| Ci17 | 2016 | Cat | Urine | 18 | + | CMY-117 | TEM-1 | 64/32 | >256 | 64 | 32 | 0.063 | 1 | 16 | 2 | 8 | 8/152 | |
| Ci20 | 2016 | Cat | Urine | 156 * | - | CTX-M-3 | CMY-78-like | TEM-1 | 16/8 | >256 | 16 | 256 | 0.031 | 1 | 8 | 4 | 2 | 0.06/1.19 |
| Ci29 | 2016 | Cat | Urine | 156 * | - | CTX-M-3 | CMY-78-like | TEM-1 | 16/8 | >256 | 8 | >256 | 0.031 | 4 | 16 | 2 | 4 | 0.25/4.75 |
| Ci31 | 2016 | Cat | Urine | 18 | + | CMY-117 | 64/32 | >256 | 64 | 16 | 0.063 | 128 | 8 | 1 | 8 | >64/1216 | ||
| Ci32 | 2016 | Cat | Urine | 156 * | - | CTX-M-3 | CMY-78-like | TEM-1 | 32/16 | >256 | 16 | >256 | 0.031 | 32 | 16 | 8 | 8 | 2/38 |
| C. portucalensis (n = 2) | ||||||||||||||||||
| Ci10 | 2015 | Dog | Urine | NA | + | DHA-1, CMY-37-like |
64/32 | >256 | 64 | 8 | 0.125 | 128 | 128 | 2 | 16 | >64/1216 | ||
| Ci27 | 2016 | Dog | Nasal | NA | + | CMY-13 | 64/32 | >256 | 128 | 32 | 0.063 | 1 | 8 | 4 | 4 | ≤0.03/0.59 | ||
| C. koseri (n = 1) | ||||||||||||||||||
| Ci7 | 2015 | Dog | Urine | NA | NA | DHA-1 | 64/32 | >256 | 64 | 4 | 0.015 | 1 | 8 | 1 | 0.25 | 0.5/9.5 | ||
NA, Not applicable. * ST156 was firstly identified in this study. ACV, amoxicillin–clavulanic acid; CPL, cephalothin; CMZ, cefmetazole; CTX, cefotaxime; MPM, meropenem; TET, tetracycline; CHL. Chloramphenicol; AMK, amikacin; CIP, ciprofloxacin; TMS, trimethoprim–sulfamethoxazole.
We also found a prevalence of AmpC β-lactamases among eight ESC-resistant Citrobacter spp. strains. Of the qAmpC genes, CMY-family β-lactamases (previously reported in Citrobacter spp., accession numbers: NG_048788, NG_048875, NG_048832, and NZ_QRJT01000009) were detected in seven strains: five C. freundii and two C. portucalensis strains. On the other hand, blaDHA-1 was identified in one C. portucalensis and one C. koseri strain, as well as the other Gram-negative bacteria from companion animals [28,33,38]. In addition, each of the two strains of C. freundii and C. portucalensis were chromosomal AmpC hyperproducers, which can confer resistance to cephalosporins, including later-generation compounds and some penicillins [39,40]. Our data indicate that these AmpC-mediated resistance mechanisms, as well as ESBLs, play a role in the prevalence of ESC-resistant Citrobacter spp. strains in companion animals.
In the present study, we conducted MLST analysis for C. freundii isolates from animals for the first time. The three blaCTX-M-3-producing C. freundii strains (strains Ci20, Ci29, and Ci32) were assigned to ST156, which was the first ST identified in our study (Table 2). Additional analysis revealed a similar or identical antimicrobial susceptibility profiles and PFGE profiles of XbaI- and SfiI-digested genomic DNA among the three strains (Figure 2). In addition, the two CMY-117-bearing C. freundii strains (strains Ci17 and Ci31) were assigned to ST18, which was the previously identified ST in human-origin carbapenemase-producing C. freundii in Denmark [41], Spain [42], and Czech Republic [43], and had almost indistinguishable PFGE profiles. These ESC-resistant C. freundii strains were acquired from different animals in the same hospital, suggesting nosocomial infections. Similar findings have been observed in other ESBL-producing bacteria [28,33,38]. Therefore, infection control in hospitals is essential in preventing the dissemination of ESC-resistant Citrobacter spp. isolates among companion animals.
Figure 2.
Pulsed-field gel electrophoresis (PFGE) profiles of eight ESC-producing Citrobacter strains digested with XbaI (A) and SfiI (B).
4. Conclusions
In conclusion, we described antimicrobial resistance, particularly ESC resistance, among Serratia spp. and Citrobacter spp. strains isolated from companion animals in Japan and established differences in the prevalence of antimicrobial resistance between those isolates. Moreover, we are the first to identify nosocomial dissemination of ESC-resistant C. freundii strains producing ESBLs or qAmpCs in companion animals. Although Citrobacter spp. are only rarely isolated from companion animals, these bacteria deserve continuous surveillance to determine the true risk of their antimicrobial resistance in veterinary and human medicine.
Acknowledgments
The authors are grateful to Miss Akane Kawahara for constructing the dendrograms of PFGE. The authors would like to thank Enago (www.enago.jp) for the English language review.
Supplementary Materials
The following are available online at https://www.mdpi.com/2076-2607/7/3/64/s1, Table S1: The details of Serratia spp. and Citrobacter spp. isolates used in this study.
Author Contributions
Conceptualization, K.H.; methodology, K.H., T.S., H.O. and Y.T.; formal analysis, K.H.; investigation, K.H., T.S., and H.O.; resources, Y.K., T.M., and Y.T.; data curation, K.H.; writing—original draft preparation, K.H.; writing—review and editing, H.O., T.M., and Y.T.; visualization, K.H.; project administration, K.H.; funding acquisition, K.H.
Funding
This research was funded by JSPS KAKENHI Grant Number 16K18804 (Japan Society for the Promotion of Science: https://www.jsps.go.jp/j-grantsinaid/]).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- 1.Choi S.H., Lee J.E., Park S.J., Kim M.N., Choo E.J., Kwak Y.G., Jeong J.Y., Woo J.H., Kim N.J., Kim Y.S. Prevalence, microbiology, and clinical characteristics of extended-spectrum β-lactamase-producing Enterobacter spp., Serratia marcescens, Citrobacter freundii, and Morganella morganii in Korea. Eur. J. Clin. Microbiol. Infect. Dis. 2007;26:557–561. doi: 10.1007/s10096-007-0308-2. [DOI] [PubMed] [Google Scholar]
- 2.Kanamori H., Yano H., Hirakata Y., Endo S., Arai K., Ogawa M., Shimojima M., Aiyagi T., Hatta M., Yamada M., et al. High prevalence of extended-spectrum β-lactamases and qnr determinants in Citrobacter species from Japan: dissemination of CTX-M-2. J. Antimicrob. Chemother. 2011;66:2255–2262. doi: 10.1093/jac/dkr283. [DOI] [PubMed] [Google Scholar]
- 3.Wiebe V.J. Drug Therapy for Infectious Diseases of the Dog and Cat. Wiley Blackwell; Ames, IA, USA: 2015. pp. 49–108. [Google Scholar]
- 4.Brenner D.J., O’Hara C.M., Grimont P.A.D., Janda J.M., Falsen E., Aldova E., Ageron E., Schindler J., Abbott S.L., Steigerwalt A.G. Biochemical identification of Citrobacter species defined by DNA hybridization and description of Citrobacter gillenii sp. nov. (formerly Citrobacter Genomospecies 10) and Citrobacter murliniae sp. nov. (Formerly Citrobacter Genomospecies 11) J. Clin. Microbiol. 1999;37:2619–2624. doi: 10.1128/jcm.37.8.2619-2624.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clermont D., Motreff L., Passet V., Fernandez J.C., Bizet C., Brisse S. Multilocus sequence analysis of the genus Citrobacter and description of Citrobacter pasteurii sp. nov. Int. J. Syst. Evol. Microbiol. 2015;65:1486–1490. doi: 10.1099/ijs.0.000122. [DOI] [PubMed] [Google Scholar]
- 6.Ribeiro T.G., Gonçalves B.R., da Silva M.S., Novais Â., Machado E., Carriço J.A., Peixe L. Citrobacter portucalensis sp. nov., isolated from an aquatic sample. Int. J. Syst. Evol. Microbiol. 2017;67:3513–3517. doi: 10.1099/ijsem.0.002154. [DOI] [PubMed] [Google Scholar]
- 7.Samonis G., Karageorgopoulos D.E., Kofteridis D.P., Matthaiou D.K., Sidiropoulou V., Maraki S., Falagas M.E. Citrobacter infections in a general hospital: characteristics and outcomes. Eur. J. Clin. Microbiol. Infect. Dis. 2009;28:61–68. doi: 10.1007/s10096-008-0598-z. [DOI] [PubMed] [Google Scholar]
- 8.Samonis G., Vouloumanou E.K., Christofaki M., Dimopoulou D., Maraki S., Triantafyllow E., Kofteridis D.P., Falagas M.E. Serratia infections in a general hospital: characteristics and outcomes. Eur. J. Clin. Microbiol. Infect. Dis. 2011;30:653–660. doi: 10.1007/s10096-010-1135-4. [DOI] [PubMed] [Google Scholar]
- 9.MacDougall C. Beyond susceptible and resistant, Part I: Treatment of infections due to gram-negative organisms with inducible β-lactamases. J. Pediatr. Phrmacol. Ther. 2011;16:23–30. [PMC free article] [PubMed] [Google Scholar]
- 10.Deshpande L.M., Jones R.N., Fritsche T.R., Sader H.S. Occurrence and characterization of carbapenemase-producing Enterobacteriaceae: report from the SENTRY antimicrobial surveillance program (2000–2004) Microb. Drug Resist. 2006;12:223–230. doi: 10.1089/mdr.2006.12.223. [DOI] [PubMed] [Google Scholar]
- 11.Ribeiro T.G., Novais Å., Branquinho R., Machado E., Peixe L. Phylogeny and comparative genomics unveil independent diversification trajectories of qnrB and genetic platforms within particular Citrobacter species. Antimicrob. Agents Chemother. 2015;59:5951–5958. doi: 10.1128/AAC.00027-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tamura K., Peterson D., Peterson N., Stecher G., Nei M., Kumar S. MEGA5: Molecular Evolutionary Genetics Analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol. Biol. Evol. 2011;28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saitou N., Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol. Boil. Evol. 1987;4:406–425. doi: 10.1093/oxfordjournals.molbev.a040454. [DOI] [PubMed] [Google Scholar]
- 14.Kimura M. A simple method for estimating evolutionary rate of base substitutions through comparative studies of nucleotide sequences. J. Mol. Evol. 1980;16:111–120. doi: 10.1007/BF01731581. [DOI] [PubMed] [Google Scholar]
- 15.Clinical and Laboratory Standards Institute . Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals. Approved Standard-Fourth Edition. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2013. CLSI Document VET01-A4. [Google Scholar]
- 16.Clinical and Laboratory Standards Institute . Performance Standards for Antimicrobial Susceptibility Testing; Twntieth Informational Supplement. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2010. CLSI document M100-S20. [Google Scholar]
- 17.EUCAST EUCAST Guidelines for Detection of Resistance Mechanisms and Specific Resistances of Clinical and/or Epidemiological Importance. [(accessed on 27 September 2017)]; Available online: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Resistance_mechanisms/EUCAST_detection_of_resistance_mechanisms_v1.0_20131211.pdf.
- 18.Izdebski R., Baraniak A., Herda M., Fiett J., Bonten M.J., Carmeli Y., Goossens H., Hryniewicz W., Brun-Buisson C., Gniadkowski M. MOSAR WP2, WP3 and WP5 Study Groups. MLST reveals potentially high-risk international clones of Enterobacter cloacae. J. Antimicrob. Chemother. 2015;70:48–56. doi: 10.1093/jac/dku359. [DOI] [PubMed] [Google Scholar]
- 19.Kojima A., Ishii Y., Ishihara K., Esaki H., Asai T., Oda C., Tamura Y., Takahashi T., Yamaguchi K. Extended-spectrum-β-lactamase-producing Escherichia coli strains isolated from farm animals from 1999 to 2002: report from the Japanese Veterinary Antimicrobial Resistance Monitoring Program. Antimicrob. Agents Chemother. 2005;49:3533–3537. doi: 10.1128/AAC.49.8.3533-3537.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pérez-Pérez F.J., Hanson N.D. Detection of plasmid-mediated AmpC β-lactamase genes in clinical isolates by using multiplex-PCR. J. Clin. Microbiol. 2002;40:2153–2162. doi: 10.1128/JCM.40.6.2153-2162.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yan J.J., Ko W.C., Jung Y.C., Chuang C.L., Wu J.J. Emergence of Klebsiella pneumoniae isolates producing inducible DHA-1 β-lactamase in a university hospital in Taiwan. J. Clin. Microbiol. 2002;40:3121–3126. doi: 10.1128/JCM.40.9.3121-3126.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu L., Ensor V., Gossain S., Nye K., Hawkey P. Rapid and simple detection of blaCTX-M genes by multiplex PCR assay. J. Med. Microbiol. 2007;54:1183–1187. doi: 10.1099/jmm.0.46160-0. [DOI] [PubMed] [Google Scholar]
- 23.Usui M., Hiki M., Murakami K., Ozawa M., Nagai H., Asai T. Evaluation of transferability of R-plasmid in bacteriocin-producing donors to bacteriocin-resistant recipients. Jpn. J. Infect. Dis. 2012;65:252–255. doi: 10.7883/yoken.65.252. [DOI] [PubMed] [Google Scholar]
- 24.Ozaki H., Matsuoka Y., Nakagawa E., Murase T. Characteristics of Escherichia coli isolated from broiler chickens with colibacillosis in commercial farms from a common hatchery. Poult. Sci. 2017;96:3717–3724. doi: 10.3382/ps/pex167. [DOI] [PubMed] [Google Scholar]
- 25.Liu L., Lan R., Liu L., Wang Y., Zhang Y., Wang Y., Xu J. Antimicrobial resistance and cytotoxicity of Citrobacter spp. in Maanshan Anhui Province, China. Front. Microbiol. 2017;8:1357. doi: 10.3389/fmicb.2017.01357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giani T., Sennati S., Antonelli A., Di Pilato V., di Maggio T., Mantella A., Niccolai C., Spinicci M., Monasterio J., Castellanos P., et al. High prevalence of carriage of mcr-1-positive enteric bacteria among healthy children from rural communities in the Chaco region, Bolivia, September to October 2016. Eur. Surveill. 2018;23 doi: 10.2807/1560-7917.ES.2018.23.45.1800115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang J., Ding H., Shi Y., Zhao Y., Hu X., Ren J., Huang G., Wu R., Zhao Z. Further spread of a blaKPC-harboring untypeable plasmid in Enterobacteriaceae in China. Front. Microbiol. 2018;9:1938. doi: 10.3389/fmicb.2018.01938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harada K., Shimizu T., Mukai Y., Kuwajima K., Sato T., Kajino A., Usui M., Tamura Y., Kimura Y., Miyamoto T., et al. Phenotypic and molecular characterization of antimicrobial resistance in Enterobacter spp. isolates from companion animals in Japan. PLoS ONE. 2017;12:e0174178. doi: 10.1371/journal.pone.0174178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harada K., Arima S., Niina A., Kataoka Y., Takahashi T. Characterization of Pseudomonas aeruginosa isolates from dogs and cats in Japan: current status of antimicrobial resistance and prevailing resistance mechanisms. Microbiol. Immunol. 2012;56:123–127. doi: 10.1111/j.1348-0421.2011.00416.x. [DOI] [PubMed] [Google Scholar]
- 30.Kimura Y., Harada K., Shimizu T., Sato T., Kajino A., Usui M., Tamura Y., Tsuyuki Y., Miyamoto T., Ohki A., et al. Species distribution, virulence factors, and antimicrobial resistance of Acinetobacter spp. isolates from dogs and cats: a preliminary study. Microbiol. Immunol. 2018;62:462–466. doi: 10.1111/1348-0421.12601. [DOI] [PubMed] [Google Scholar]
- 31.Hrabák J., Chudáčková E., Papagiannitsis C.C. Detection of carbapenemases in Enterobacteriaceae: a challenge for diagnostic microbiological laboratories. Clin. Microbiol. Infect. 2014;20:839–853. doi: 10.1111/1469-0691.12678. [DOI] [PubMed] [Google Scholar]
- 32.Shimizu T., Harada K., Tsuyuki Y., Kimura Y., Miyamoto T., Hatoya S., Hikasa Y. In vitro efficacy of 16 antimicrobial drugs against a large collection of β-lactamase-producing isolates of extraintestinal pathogenic Escherichia coli from dogs and cats. J. Med. Microbiol. 2017;66:1085–1091. doi: 10.1099/jmm.0.000535. [DOI] [PubMed] [Google Scholar]
- 33.Harada K., Shimizu T., Mukai Y., Kuwajima K., Sato T., Usui M., Tamura Y., Kimura Y., Miyamoto T., Tsuyuki Y., et al. Phenotypic and molecular characterization of antimicrobial resistance in Klebsiella spp. isolates from companion animals in Japan: clonal dissemination of multidrug-resistant extended-spectrum β-lactamase-producing Klebsiella pneumoniae. Front. Microbiol. 2016;7:1021. doi: 10.3389/fmicb.2016.01021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ewers C., Stamm I., Pfeifer Y., Wieler L.H., Kopp P.A., Schønning K., Prenger-Berninghoff E., Scheufen S., Stolle I., Günther S., et al. Clonal spread of highly successful ST15-CTX-M-15 Klebsiella pneumoniae in companion animals and horses. J. Antimicrob. Chemother. 2014;69:2676–2680. doi: 10.1093/jac/dku217. [DOI] [PubMed] [Google Scholar]
- 35.Tamang M.D., Nam H.M., Jang G.C., Kim S.R., Chae M.H., Jung S.C., Byun J.W., Park Y.H., Lim S.K. Molecular characterization of extended-spectrum-β-lactamase-producing and plasmid-mediated AmpC β-Lactamase-producing Escherichia coli isolated from stray dogs in South Korea. Antimicrob. Agents Chemother. 2012;56:2705–2712. doi: 10.1128/AAC.05598-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sun Y., Zeng Z., Chen S., Ma J., He L., Liu Y., Deng Y., Lei T., Zhao J., Liu J.H. High prevalence of blaCTX-M extended-spectrum β-lactamase genes in Escherichia coli isolates from pets and emergence of CTX-M-64 in China. Clin. Microbiol. Infect. 2010;16:1475–1481. doi: 10.1111/j.1469-0691.2010.03127.x. [DOI] [PubMed] [Google Scholar]
- 37.Ewers C., Bethe A., Wieler L.H., Guenther S., Stamm I., Kopp P.A., Grobbel M. Companion animals: a relevant source of extended-spectrum β-lactamase-producing fluoroquinolone-resistant Citrobacter freundii. Int. J. Antimicrob. Agents. 2011;37:86–87. doi: 10.1016/j.ijantimicag.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 38.Harada K., Nakai Y., Kataoka Y. Mechanisms of resistance to cephalosporin and emergence of O25b-ST131 clone harboring CTX-M-27 β-lactamase in extraintestinal pathogenic Escherichia coli from dogs and cats in Japan. Microbiol. Immunol. 2012;56:480–485. doi: 10.1111/j.1348-0421.2012.00463.x. [DOI] [PubMed] [Google Scholar]
- 39.Avison M.B., Underwood S., Okazaki A., Walsh T.R., Bennett P.M. Analysis of AmpC β-lactamase expression and sequence in biochemically atypical ceftazidime-resistant Enterobacteriaceae from paediatric patients. J. Antimicrob. Chemother. 2004;53:584–591. doi: 10.1093/jac/dkh151. [DOI] [PubMed] [Google Scholar]
- 40.Jacoby G.A. AmpC β-lactamases. Clin. Microbiol. Rev. 2009;22:161–182. doi: 10.1128/CMR.00036-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hammerum A.M., Hansen F., Nielsen H.L., Jakobsen L., Stegger M., Andersen P.S., Jensen P., Nielsen T.K., Hansen L.H., Hasman H., et al. Use of WGS data for investigation of a long-term NDM-1-producing Citrobacter freundii outbreak and secondary in vivo spread of blaNDM-1 to Escherichia coli, Klebsiella pneumoniae and Klebsiella oxytoca. J. Antimicrob. Chemother. 2016;71:3117–3124. doi: 10.1093/jac/dkw289. [DOI] [PubMed] [Google Scholar]
- 42.Villa J., Arana D.M., Viedma E., Perez-Montarelo D., Chaves F. Characterization of mobile genetic elements carrying VIM-1 and KPC-2 carbapenemases in Citrobacter freundii isolates in Madrid. Int. J. Med. Microbiol. 2017;307:340–345. doi: 10.1016/j.ijmm.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 43.Kukla R., Chudejova K., Papagiannitsis C.C., Medvecky M., Habalova K., Hobzova L., Bolehovska R., Pliskova L., Hrabak J., Zemlickova H. Characterization of KPC-encoding plasmids from Enterobacteriaceae isolated in a Czech Hospital. Antimicrob Agents Chemother. 2018;62 doi: 10.1128/AAC.02152-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.