Abstract
The prevalence of obesity in children/adolescents has increased worldwide during the past 30 years, becoming a significant public health concern; prevention, and management of pediatric obesity onset is one of the most critical public health goals for both industrialized and developing countries. Pediatric obesity has been identified as a risk factor for various psychopathologies, including eating disorders (ED). Although it has been demonstrated that a comprehensive multidisciplinary treatment (MT), with small steps and practical approaches to lifestyle change, can be an effective treatment for children and adolescents with obesity, to the best of our knowledge, this is the first systematic review investigating the effect of MT on the development, progression or decrease of ED symptoms (EDS) in this target population. PubMed and Web of Science databases were searched (last search on 18 February 2019) according to a predetermined search strategy, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines and Statement. Original studies published in English examining the effect of MT on pediatric overweight/obesity, paying particularly attention at the development of EDS, were eligible for inclusion. Seven hundred and forty-four records have been identified; nine articles with study quality ranging from weak to moderate have been included. MTs were heterogeneous in nature including length, number, frequency and type of sessions, parent-involvement and use of technology, besides several psychometric questionnaires were used to screen for EDS, since there are no standardized criteria. In 3 studies there was a significant decrease in external and emotional eating and in four studies a significant increase in restraint eating post MT. Two studies found a significant decrease of binge eating symptoms and other two studies showed an improvement of self-perception, weight, and shape concern. A statistical significant decrease in BMI, BMIz, BMISDS, and adjusted BMI was observed after all MTs, except one. A narrative summary of the evidences reported highlighted the positive impact of MT on the EDS. Moreover, since weight loss post MTs was not necessarily related to EDS, clinicians should also look for the presence of EDS and treat them accordingly.
Keywords: pediatric obesity, eating disorders, multidisciplinary treatment, obesity prevention, obesity management
Introduction
Pediatric obesity is one of the greatest health challenges of the Twenty-first century (1). Prevalence of overweight or obesity in infants and young children (0–5 years) has increased globally and rapidly over time from 32 million in 1990 to 41 million in 2016 (2). In the United States, more than 10% of infants or toddlers and more than 17% of children and teens are affected by obesity while in Europe (3), 19–49 and 18–43% respectively of boys and girls are affected by either overweight or obesity (4). If the current rates keep on rising, the number of infants and young children with overweight or obesity will reach 70 million by 2025 (2). In addition, evidence show that at least 25–50% of children and adolescents defined as having a healthy Body Mass Index (BMI)-for-age have excessive body fat and this may indicate a dangerous underestimation of “obesity” comorbidities risk (5–7). Indeed, childhood and adolescent obesity is associated with a number of negative health sequelae, including hypertension, hyperlipidemia, respiratory problems, endocrine consequences, orthopedic complications, which contribute to a significant decrease in quality of life and life expectancy (8).
Recently, the Childhood Obesity Task Force (COTF) of the European Association for the Study of Obesity (EASO) classified obesity as not just a health risk but as a chronic disease in children and adolescents, in order to develop tailored interventions and health policies to prevent and treat obesity at both public and individual level (1).
Furthermore, there is increasing evidence that childhood-onset obesity is not only a risk factor for metabolic complications in adulthood, but also associated with an increased risk of developing eating disorders (EDs) during adolescence (9–13).
Children with obesity or overweight experience psychosocial distress that significantly affects their quality of life and well-being, so mental health of these children has also gained the attention of researchers and clinicians (11, 14–16).
Additionally, pediatric obesity has been identified as a risk factor for psychopathology, that may manifest itself through eating disorder symptoms (EDS) like excessive shape and weight concerns, body image dissatisfaction, dieting, and other unhealthy weight control methods, or binge eating (17, 18), sneaking, hiding or hoarding food, eating in the absence of hunger and inhibition or embarrassment when eating in front of others (19).
ED symptoms do not always correspond in severity or specificity to full-syndrome ED (20); they encompass a broad array of dimensional maladaptive cognitions and behaviors relating to eating and weight, that are found across the range of full syndrome ED diagnoses as well as in subsyndromal variants (21). This is probably why they are continuously underdiagnosed by pediatric professionals, although they are more common than metabolic disorders in childhood and adolescence and are associated with high morbidity and mortality (20). Overweight adolescents have a 2 1/2 to 5 times higher risk of developing eating disorders than teens whose weight is in the healthy range (21, 22).
Prevention and management of obesity onset is one of the most critical public health goals, and childhood represents the ideal time for lifestyle intervention, throughout multidisciplinary treatment (MT), as lifestyle habits in youth are not yet ingrained (23, 24). In fact, evidences show that behavioral lifestyle interventions are effective for weight loss in most children and adolescents (25). Success in treatment of childhood obesity requires a multifaceted approach to nutrition patterns and physical activity, with particular attention paid to the family and other environmental factors that may significantly affect outcomes (26).
The 2016 WHO Commission on Ending Childhood Obesity report, recommended “family-based, multicomponent, lifestyle weight management services for children and young people who are obese” as part of the universal child and adolescent health care (2). There is no specific definition of “multidisciplinary treatment” (MT), but some authoritative sources [WHO (2); Endocrine Society (27)] underlined it should include some common components such as nutrition and physical activity, besides family counseling and psychosocial support.
The multidisciplinary approach should also include health professionals such as physicians, dieticians, health coaches, and psychologists or other mental health care providers able to offer behavioral counseling (28, 29). Working in teams allows for modification of assessment and treatment providing effective integral interventions in the management of childhood obesity.
Multidisciplinary treatments (MTs) have proven beneficial and effective in combating obesity reducing body mass index (BMI) as well as the risk of future comorbidities (30–32).
Treatment of overweight and obesity mainly aims at achieving weight loss and BMI reduction, fat mass decrease, risk factors for metabolic syndrome decline and increased health-related quality of life (33, 34). However, despite weight reduction is a common and legitimate outcome to pursue, psychosocial contributors to eating behaviors not be neglected (35–37).
Objectives
Since the effects of MT on eating behavior in children with overweight/obesity are largely unknown, in this systematic review, we attempted to address the question: is multidisciplinary treatment effective on eating disorder symptoms in children with obesity?
This systematic review has been conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines recommending to present a full electronic search strategy for at least 1 major database (38).
Methods
Data and Search Strategy
Two electronic databases (PubMed and Web of Science) were searched from 2008 to 2019 using the following structured search strings: childhood obesity OR childhood overweight OR pediatric obesity OR pediatric overweight OR obesity in children OR overweight in children OR multidisciplinary treatment* OR multidisciplinary approach* OR multidisciplinary intervention* OR multidisciplinary program*, combined to eating behavior* OR binge eating OR sneaking food* OR hiding food*OR hoarding food* OR reward OR overeating.
Eligibility Criteria
All studies were assessed according to the following inclusion and exclusion criteria summarized below:
Participants
Eligible participants were children with overweight/obesity (as defined in the selected studies), age ranging from 6 to 18 years at the beginning of MT. Participants with pre-existing disease or organic cause for obesity and on medications that could affect weight were excluded.
Intervention
MT was defined as an approach covering lifestyle intervention on nutrition and healthy behavior dietary patterns and/or physical activity. According to this, we selected only studies that included MTs considering also EDS.
Assessment of EDS was obtained through a variety of different psychometric tests: DEBQ (Dutch Eating Behavior Questionnaire) (39), ChEDE (Child Eating Disorder Examination) (40), YEDE-Q (Youth Eating Disorder Examination Questionnaire) (41, 42), CEBQ (Children Eating Behavior Questionnaire) (43), TEFQ (Three-Factor Eating Questionnaire) (44), BES (Binge Eating Scale) (45), BITE (Bulimic Investigatory Test, Edinburgh) (46), EDI—II (Eating Disorder Inventory) (47), EES-C (Emotional Eating Scale for Children and Adolescents) (48), QWEP (Questionnaire on Weight and Eating Patterns) (49), EI (Eating Inventory) (50).
Comparison
Different study designs (i.e., randomized controlled-trials, case–control studies and pre–post uncontrolled studies with no comparison group) were included in this review.
Outcome
The outcome of this systematic review was to evaluate for the first time MT impact on EDS in children affected by overweight/obesity.
We also evaluated weight reduction and/or fluctuations, expressed as Body Mass Index (BMI), BMI z score (BMIz), BMI Standard Deviation Score (BMISDS) as a possible confounding factor.
Exclusion Criteria
The comprehensive search strategy inadvertently retrieved studies that were unrelated to the aim of this systematic review and were subsequently excluded. Narrative reviews, systematic reviews and case reports were excluded, as well as case series, descriptive studies, letters, comments, articles that did not correspond to the objective of this review or had no full-text accessible in English.
Selection Process
Titles and abstracts were screened by two authors (Di Napoli Ilaria, Porri Debora) for inclusion. Reference lists of primary articles and related reviews were checked to identify any other study appropriate for inclusion. Studies assessed as eligible, potentially eligible or unclear, were retrieved in full text whenever available. Any uncertainty concerning the inclusion of specific studies was resolved by discussing with a third author (De Giuseppe Rachele). Last search date 18/02/2019.
Data Extraction
Study's characteristics (e.g., multidisciplinary treatment, participants, aim, outcome of interest, and study design) were extracted into standardized tables. Data items extracted were used to investigate the effect of MT on EDS in children affected by overweight/obesity.
Data Synthesis
Due to the heterogeneity of study population characteristics and MTs features (such as length of the treatment, outcomes measured, and timing of assessment), we were not able to perform a meta-analysis. However, we conducted a narrative summary of the findings.
Quality Assessment and Risk of Bias
Study quality was assessed in duplicate using a designed appraisal tool, the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies, a useful tool for systematic reviews, which evaluates randomized and non-randomized intervention studies (51).
Individual component quality rankings, including the risk of bias measures are included in the Supplementary Table 1.
Component and overall quality ratings were scored as “strong,” “moderate” or “weak” according to instructions accompanying the tool (52, 53).
Results
Overview of Studies
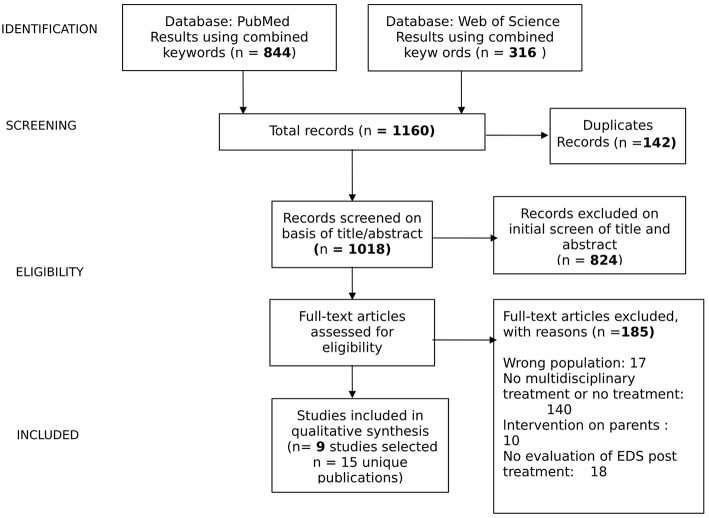
A flowchart summarizing the study selection procedure is presented in Figure 1.
Figure 1.
Studies selection.
Electronic searches returned 1,160 records. Duplicates (n = 142) were firstly removed. Secondly, 194 studies were retained after screening the titles and abstract. Finally, 170 studies were further excluded after reading throughout full texts. Of the 184 excluded records, 17 referred on a wrong population, in 140 MT was not considered, in 10 was considered an intervention on parents and in 18 were not evaluated EDS post MT. Only 9 eligible studies met the inclusion criteria and were included in this review.
Data abstraction revealed 6 programs that had multiple publications either protocols, additional cohorts, further follow-up time-points or different outcome measures/other secondary analysis (see references in Supplementary Table 1). Hence, studies were grouped by program cohort for reporting and analysis. Disagreements were resolved via discussion.
Study Characteristics
Characteristics of selected studies are reported in Table 1. All studies have been published between 2008 and 2019.
Table 1.
Characteristics of selected studies.
| References | Study design | Quality score | Simple size | Age | Questionnaire |
|---|---|---|---|---|---|
| Cohen et al. (54) | Randomized Controlled Trial | moderate | 78 | 6–8 year old | CEBQ(43) |
| Balantekin et al. (55) | Interrupted time series without comparison group | moderate | 241 | 7–11 years old | ChEDE (40) YEDE-Q (41, 42) |
| Halberstadt et al. (56) | Interrupted time series without comparison group | weak | 120 | 8–19 years old | DEBQ (39) |
| Adam et al. (57) | Interrupted time series without comparison group | weak | 604 | 10 – 15 years old | TFEQ (44) |
| Raimunda Damaso et al. (58) | Interrupted time series without comparison group | moderate | 97 | 15−19 years old. | BES (45) BITE (46) |
| De Niet et al. (59) | Randomized Controlled Trial | moderate | 144 | 8–12 years old. | DEBQ (39) |
| Bishop-Gilyard et al. (60) | Randomized double blinded placebo–controlled trial | moderate | 82 | 13–17 years old | QWEP (49) EI (50) |
| Goossens et al. (61) | Interrupted time series without comparison group | weak | 108 | 10–17 years old | ChEDE (40) |
| Sarvestani et al. (62) | Non Randomized Controlled Trial | moderate | 60 | 11-15 years old. | DEBQ (39) |
Four studies were conducted in Europe (56, 57, 59, 61), two studies took place in US (55, 60) while one study was conducted in Canada (54), one study was conducted in Brazil (58), and one in Iran (62).
The programs were evaluated as controlled trials (n = 4) (54, 59, 60, 62) both randomized (n = 3) (54, 59, 60) and non-randomized (n = 1) (62), and as interrupted time series without comparison group (n = 5) (55–58, 61).
Study quality was assessed to be weak for three studies (56, 57, 61); moderate for six (54, 55, 58–60, 62). Eight studies (54–57, 59–62) were rated as being weak for selection bias as they involved self-referrals from community advertisements and public service announcements, as is commonplace for community interventions, and thus participants were not randomly selected from the eligible population.
The sample size ranged from 60 to 504 children and adolescents while age of participants ranged from 7 to 18 years old.
In all studies, selected multidisciplinary treatment of pediatric obesity was provided. MTs were heterogeneous in nature, including length, number, frequency and type of sessions, parent-involvement and technology involvement.
Among selected studies, eight of them (54–57, 59–62) required either active and frequent participation of at least one parent/caregiver during MT or a “family-based intervention.”
As regards the characteristics of the various MT approaches, all treatments (54–62) included either advice on healthy nutritional habits or advice on physical activity and healthy lifestyle.
Particularly, in one study (54), besides nutritional and lifestyle advice, both dietary treatment and structured physical activity were performed, while in other three studies (58, 61, 62) besides lifestyle advice, MT included the prescription of structured physical activity sessions, under the supervision of a skilled trainer.
Additionally, four studies (56, 57, 60, 61) combined an inpatient multidisciplinary program, ranging from 6 weeks to 10 months, with a strict control of children's daily dietary intake and lifestyle habits. De Niet et al. (59), evaluated the effect of Short Message Service (SMS) maintenance treatment (SMSMT) by means of smart devices.
Finally, only one study reported the use of medications (e.g., sibutramine) during MT (60).
Concerning psychological aspects in MT, all studies selected in this review (54–62) included support group therapy, with exception of Adam's (57) study for which we were not able to establish it since the protocol, described previously elsewhere, was written in German. Only Raimunda Damaso et al. (58) included also individual therapy in MT.
All MT approaches (54–62) included cognitive behavioral therapy (CBT), with parents' involvement promoting parent-child interaction patterns change toward a supporting relationship, instead of a parental controlling behavior, giving positive feedback and reinforcement. Three (56, 59, 61) of these nine studies analyzed also the psychosocial consequences of obesity and the relationships of children with their peers. Considering the duration of the various MT approaches, except one study (55) that did not state MT length, we reported different lengths of treatments ranging from 16 weeks (62) to 12 months (54, 56–60). As for follow ups three studies (56, 57, 61) reported follow ups ranging from 12 to 60 months post MT.
Outcome
The focus of this review was to evaluate MT outcome on ED symptoms in children affected by overweight/obesity (Table 4).
Different questionnaires have been used (Table 2) and administered at baseline, at the end of MT and during follow-up for ED symptoms screening in children and adolescents, since the lack of a standardized method.
Table 2.
Description of questionnaires used in the different selected studies to assess ED symptoms.
| References | Variables assessed | Questionnaires |
|---|---|---|
| Cohen et al. (54) | Items aimed at investigating:
|
CEBQ (43) Children Eating Behaviour Questionnaire |
| Balantekin et al. (55) Goossens et al. (61) |
Items aimed at investigating four major areas of eating disorder psychopathology: restraint, eating, shape, and weight concerns. | ChEDE (40) Child Eating Disorder Examination |
| Balantekin et al. (55) | Adaption of ChEDE for adolescents. | YEDEQ (41, 42) Youth Eating Disorder Examination Questionnaire |
| Halberstadt et al. (56) De Niet et al. (59) Sarvestani et al. (62) |
Items aimed at investigating: external eating, emotional eating and restrained eating. | DEBQ (39) Dutch Eating Behaviour Questionnaire |
| Adam et al. (57) | Items aimed at evaluating: disinhibition, cognitive control, flexible control and rigid control. | TFEQ(44) Three-Factor Eating Questionnaire |
| Raimunda Dâmaso et al. (58) | Items aimed at evaluating Bulimia symptoms. | BITE (46) Bulimic Investigatory Test, Edinburgh |
| Raimunda Damask et al. (58) | Items aimed at describing both behavioral manifestations and feeling/cognitions surrounding a binge episode and cognitive phenomena thought to be related to binge eating. | BES (45) Binge Eating Scale |
| Bishop-Gillard et al. (60) | Items aimed at measuring the ability to control food intake, loss of control over eating, and reported hunger | EI (50) Eating Inventory |
| Bishop-Gillard et al. (60) | Items aimed at measuring the BED diagnostic criteria. | QWEP(49) Questionnaire on Weight and Eating Patterns |
| Goossens et al. (61) | Items aimed at assessing both eating attitudes and related ego dysfunction characteristics. For the purpose of this study, nag eating attitudes (i.e., drive for thinness, bulimia, and body dissatisfaction) were evaluated | EDI-II (47) Eating Disorder Inventory |
MT features as sessions, length, follow-up, focus, prescriptions, target, and parental involvement are described in Table 3 while the outcome of selected studies is reported in Table 4.
Table 3.
Description of studies' multidisciplinary treatments.
| References | Multidisciplinary treatment | Sessions | Length | Follow-up | Focus | Diet or physical activity prescribed by a specialist | Inpatient period | Parents involved |
|---|---|---|---|---|---|---|---|---|
| Cohen et al. (54) | Based on Canadian diet and physical activity guidelines. Children were randomized into 3 groups: – Control (Ctrl; no intervention) – Standard treatment (StnTx: 2 servings milk and alternatives/day (d), 3x/week. weight bearing physical activity) – Modified treatment (ModTx: 4 servings milk and alternatives/day; daily weight bearing physical activity). Ctrl received counseling after 12 months |
StnTx and ModTx participated in 6 sessions, which were held at the end of each month for the first 5-months of the study, then a final “relapse prevention” session at the end of the 8th month. Ctrl group received the interventions after the end of the study. | 12 months | NO | – Physical activity – Nutrition – Eating behavior – Parenting skills |
YES (diet, structured physical activity) | NO | YES |
| Balantekin et al. (55) | Family-based behavioral weight loss treatment | 16 session of family-based behavioral treatment. | Not specified | NO | –Nutrition, – Physical activity, – Eating behavior – Parenting skills |
NO | NO | YES |
| Halberstadt et al. (56) | Combined multidisciplinary lifestyle intervention. Two months or 6 months period of inpatient treatment during weekdays requiring active and frequent participation of the parents/caregivers. |
The MT had a period of inpatient treatment during weekdays of either 2 months and biweekly return visits of 2 days during the next 4 months or 6 months, followed by 6 monthly return visits of 2 days | 12 months | 12 months | – Nutrition, – Physical activity – Eating behavior – Parenting skills |
NO | YES | YES |
| Adam et al. (57) | The DAK program, designed for one year with an initial multidisciplinary inpatient treatment followed by an outpatient family based treatment. | The details of MT was previously published elsewhere. The protocol was written in Germany (see Supplementary Table 1) | 12 months | 48 months | –Nutrition, – Physical activity – Eating behavior – Parenting skills |
YES (diet and structured physical activity) | YES | YES |
| Raimunda Damaso et al. (58) | Multidisciplinary treatment with the supervision of an exercise physiologist | Once a week, the adolescents had classes on topics related to improved food consumption. Adolescents underwent therapy support group weekly Adolescents were involved in structured session of physical activity three times a week. |
12 months | NO | – Physical activity – Nutrition – Eating behavior |
YES (structured physical activity) | NO | NO |
| De Niet et al. (59) | SMS maintenance treatment (SMSMT) program After the first 3 months of treatment where children and parents were involved into educational session group, participants were randomly assigned to: – Intervention group, receiving SMSMT for 9 months, or to – Control group (no SMSMT) |
1 intake session; 8 children sessions; 3 parent sessions; for 3 months. |
12 months | NO | – Physical activity – Nutrition – Eating behavior – Technology involvement – Parenting skills |
NO | NO | YES |
| Bishop-Gilyard et al. (60) | Participants attending at a family based behavioral weight loss program were randomly assigned to: –Intervention group (sibutramine 15 mg/d) or to – Control group received placebo. |
The treatment was structured into 2 phases.Phase 1: Both intervention and control group attended a behavioral counseling for 4 months followed by bi-weekly visits for an additional 2 months. Parents were instructed in methods of supporting their children. Phase 2: After the initial 6 months all participant received sibutramine for 6 months. |
12 months | NO | – Physical activity – Nutrition – Eating behavior – Parenting skills |
YES (diet) | NO | YES |
| Goossens et al. (61) | Inpatient non-diet healthy lifestyle program. | Each child received 4 hours of individual guided exercises. All children had facilities to take part in exercise programs for at least 14 hours per week. All children received a 12-week cognitive behavioral treatment. |
10 months | 60 moths | – Physical activity – Nutrition – Eating behavior – Parenting skills |
YES (structured physical activity) | YES | YES |
| Sarvestani et al. (62) | Participants were randomized into: – Intervention group receiving lifestyle counseling and structured sessions of physical activity – Control group attended only three sessions of the same treatment. |
Four-hour structured sessions of physical activity were held weekly for 16 weeks; each session involved 2 hours of behavior modification or dietary instruction and 2 hours of yoga therapy. | 4 months | NO | – Physical activity – Nutrition – Eating behavior – Parenting skills |
YES (structured physical activity) | NO | YES |
Table 4.
Outcome of selected studies.
| References | Outcome |
|---|---|
| Cohen et al. (54) | StnTx: - Food Approach ↓** - Food Avoidance not significantly change - BMIz ↓* ModTx: - Food Approach ↓ - Food Avoidance not significantly change - BMIz ↓ Ctrl: - Food Approach ↔ - Food Avoidance not significantly change - BMIz ↔* |
| Balantekin et al. (55) | Entire sample: - Weight concern ↓** - Shape concern no significant change - LOC no significant change - BMIz↓*** HIGH and SWC (compared with LOW): - Weight concern ↓*** - Shape concern ↓*** |
| Halberstadt et al. (56) | Girls: - Restraint eating ↑** - External eating↓ Boys: - Emotional eating ↓* - External eating ↓** Entire sample: BMISDS ↓*** |
| Adam et al. (57) | - Cognitive control/Restrained eating ↑*** - Flexible control ↑*** - Disinhibition ↓*** - Rigid control ↓(at 24 months and at 48 months)*** - BMISDS ↓*** |
| Raimunda Damaso et al. (58) | - Percentage of adolescents with binge eating symptoms ↓*** - BMI ↓*** |
| De Niet et al. (59) | - Emotional eating ↓* - External eating ↓* - BMISDS ↓*** |
| Bishop-Gilyard et al. (60) | - Percentage of adolescents with binge eating symptoms ↓** - Hunger ↓*** - Disinhibition ↓*** - Cognitive restraint ↑*** - BMI ↓ |
| Goossens et al. (61) | - OBE ↔ - Restraint ↔ - Weight concern ↔ - Shape concern ↔ - SBE ↓ - Eating Concern ↓** - Drive for Thinness ↓** - Bulimia ↓** - Body Dissatisfaction ↓** - adjusted BMI ↓*** |
| Sarvestani et al. (62) | - Emotional eating ↓* - Restraint eating ↑* - External eating ↓* - BMI ↓* |
SBE, subjective binge eating episodes; OBE, objective binge eating episodes; LOC, loss of control; HIGH, high probability to develop ED pathology group; SWC, shape and weight concern group; LOW, Low probability to develop ED pathology group; BMIz, BMI z score; BMISDS, BMI Standard Deviation Score; ↓ decrease; ↔ remain stable; ↑ increased.
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001.
Additionally, we evaluated BMI fluctuations, expressed as BMI, BMIz, BMISD, or adjusted BMI, as a possible confounding factor, at end of treatment (MT) (54–62) and during follow-up period (56–58, 61) (Table 4).
Raimunda Damaso et al. (58) identified symptoms of binge eating and bulimia at baseline in 6% of their sample of adolescents with obesity, by means of BES and BITE questionnaires; at 12 months' follow up, the percentage of adolescents with binge eating symptoms had significantly decreased (2%) (Table 4).
Similarly, Bishop-Gilyard et al. (60) assessed symptoms of binge eating in adolescents affected by obesity by QWEP and EI questionnaires (Table 2), complemented by an interview to estimate the amount of food consumed during binging episodes and evaluate loss of control. The Authors (60) reported at baseline binge eating symptoms in 24% of participants with a significant decrease after 6 and 12-months' post MT, respectively 8 and 3%. Moreover, hunger and disinhibition significantly dropped, while cognitive restraint significantly increased over time (Table 4).
Concerning BMI reduction/fluctuation, the authors (60) also noticed that adolescents with obesity and binge eating episodes lost the same amount of weight as those without these episodes.
Besides binge eating, other eating disordered symptoms were identified by means of several others questionnaires as described in Table 2.
Choen et al. (54) conducted an RCT aimed at examining changes in EDS by means of CEBQ (Table 2) in children with overweight and obesity participating in a 12 months-MT protocol, based on a family-centered lifestyle intervention, according to Canadian dietary and physical activity guidelines. As shown in Table 3, the subjects were divided into three groups: control (Ctrl), standard (StnTx) and modified (ModTx) treatment. The StnTx and the ModTx attended 6 sessions plus a final of “prevention of relapse” session at the end the eighth month MT (Table 3) while the Ctrl group received the same session but at the end of 12 months of the study. CEBQ scores were then categorized as either Food Approach or Food Avoidance (Table 2), meaning for Food Approach food responsiveness, enjoyment of food, emotional overeating, and desire to drink scoring and for Food Avoidance slowness in eating, food fussiness, satiety responsiveness, and emotional under-eating scoring. Food Approach resulted significantly decreased only in the StnTx group and not in the ModTx group when compared to Ctrl group. Food Avoidance did not significantly change among groups (Table 4). Notably, this is the only study that used a parent-completed questionnaire (CEBQ).
Adam et al. (57) evaluated four parameters of EDS (disinhibition, cognitive control/restrained eating, flexible control, rigid control), by means of TFEQ questionnaire (Table 2) at baseline, at the end of MT and 24 and 48 months post treatment (MT). The Authors reported that cognitive control/restrained eating, flexible control, and disinhibition improved significantly at the end of MT as well as 24 and 48 months post MT, when compared to the baseline; rigid control improved but reached the significance only 24 and 48 months post MT (Table 4).
Goossens et al. (61) and Balantekin et al. (55) assessed different aspects such as restraint, eating, shape, weight concerns and loss of control (LC) overeating identified as objective binge eating (OBE) and subjective binge eating (SBE) on adolescents and children with overweight/obesity by using ChEDE, as described in Table 2. Balantekin et al. (55) used YEDE-Q (a version of ChEDE adapted for adolescent population) and EES-C to rate children desire to eat facing emotions; Goossens et al. (61) additionally used EDI-II (Table 2) aimed at assessing both eating attitudes and related ego dysfunction characteristics (such as drive for thinness, bulimia, and body dissatisfaction).
Previous findings (63) hypothesized that EDS in youngsters with overweight, would remain stable or decrease over a certain period post MT. Similarly, Goossens et al. (61) investigated the stability of EDS in youngsters at 60 months post MT, reporting that some ED symptoms (like OBE, Restraint, Weight, and Shape Concerns) remained stable, while others decreased (like SBE, Eating Concern, Drive for Thinness, Bulimia, and Body Dissatisfaction) (Table 4).
Balantekin et al. (55) quantified each different aspect (restraint, eating, weight and shape concerns and loss control) investigated through ChEDE questionnaire (Table 2), identifying at baseline 4 different EDS patterns: (i) LOW (subjects with a very low probability to develop ED); (ii) SWC (subjects with a high probability to develop shape and weight concerns); (iii) OLOC (subjects at risk of loss of control eating); (iv) HIGH (subjects with a high probability to develop ED). The Authors (55) reported that after 16 MT sessions (Table 4), there was a significant decrease in weight concern from baseline to post treatment for the entire sample, with a significant time-by-group interaction. Compared with LOW children, HIGH, and SWC ones reported significantly greater reductions in weight concern; no differences were detected between children in LOW and OLOC and no significant change in shape concern from baseline to post treatment was observed for the entire sample. However, there was a significant time-by-group interaction; in fact, compared to LOW children, the HIGH, and SWC ones experienced a significantly greater reduction in shape concern. No significant change in the number of LOC eating episodes nor in the time-by-group interaction was found for the entire sample (Table 4). Interestingly, although the significant reduction in BMIz and weight concern after the MT in the whole study sample, Balantekin et al. (55) reported a lower decrease in BMIz in HIGH and SWC group when compared to LOW group. Moreover, shape and weight concern in HIGH group was not significantly related to BMIz reduction (55).
Finally, three studies (56, 59, 62) used DEBQ questionnaire (Table 2), in order to evaluate external, emotional and restrained eating in children and/or adolescent with overweight/obesity post MT.
Particularly, a RCT performed by de Niet et al. (59) and a non-RCT performed by Sarvestani et al. (62) reported a significant reduction in the emotional eating after 12 months and 6 months' MT, respectively (Table 4). Sarvestani et al. (62) also observed a significant increase in restraint eating (Table 4).
Similarly, Halberstadt et al. (56) in an interrupted time series with no control group study, noticed a significant increase of restraint eating in girls and, in agreement with others (62), a significant decrease in emotional eating but only in boys (Table 4).
The authors (56) also reported a significant reduction of BMI and BMISDS post MT that was maintained during follow-up. However, a slight increase in BMI and BMISDS occurred after 12 months, showing that weight re-gain influenced significantly the increase of restraint and external eating post MT, only in girls.
Concerning external eating, all studies (56, 59, 62) reported a significant decrease after MT (Table 4).
Discussion
Multidisciplinary treatment for children/adolescents with overweight and obesity should focus on diet and healthy eating habits, physical activity, and family coping strategies (64, 65).
Assessment and treatment of childhood obesity and associated medical conditions, including psychological consequences, should be ensured.
It is well known that psychological distress and risk for eating disorders in pediatric population with a history of obesity are frequent (19); however classifying eating disorders in youth is challenging (66).
During childhood, eating disorders often present with atypical or sub-threshold criteria. This is particularly true for Binge Eating, one of the most common ED symptom associated with childhood obesity (19). Despite binge eating symptoms in children with obesity are common, the diagnosis of binge eating disorder (BED) in youth is rare (67–69); compulsive eating and stereotypical disordered eating behaviors such as hiding food, eating in secret, purging, exercising excessively, can be frequently observed (20).
Previous research showed an association between pediatric obesity and EDS, such as dietary restraint, self-dieting, and body image dissatisfaction (70). Moreover, results confirmed by Boutelle et al. (71) suggested that external eating, satiety sensitivity, eating in the absence of hunger, loss of control eating, and emotional eating were related to adiposity and excessive weight gain in children.
Assessment and management of EDS caused by or consequent to excessive weight gain are not always contemplated with due caution; however, pediatric obesity should be considered a significant risk factor for the development of eating disorders during adolescence and childhood (17).
Although multidisciplinary treatments are well supported by the literature in their effectiveness to reduce BMI and risk of future co-morbidities (30–32), to the best of our knowledge the effect of MT on the development, progression or reduction of EDS in children/adolescents with overweight/obesity has never been evaluated.
In our systematic review, the first aim was to evaluate the effectiveness of MT on EDS in children with obesity.
Concerning MT efficacy on dietary restraint, results (56, 57, 60, 62) presented are conflict.
Adam et al. (57) found a significant decrease of dietary restraint after MT; they also reported a significant reduction of flexible control, a typical behavior characterized by a graduated “more or less” approach to eating and weight control, which is considered a permanent behavior (57).
These effects were also maintained during the whole follow-up period (57) and can reflect a success of MT since dietary restraint is often considered a determinant of overeating and a precursor of EDS (72). In fact, as previously demonstrated by Stice et al. (73) in a 60 months prospective study on 496 adolescent girls, children and adolescents with higher dietary restraint scores appeared to have an increased risk of developing obesity later on.
On the contrary, other findings (56, 60, 62) described in our systematic review, reported that children or adolescents with obesity, especially girls (56) showed a significant increase in dietary restraint after MT.
However, in the light of what has been described above, it is also important to note that while dietary restraint is often conceptualized as maladaptive for individuals with ED, in the context of obesity, a moderate degree of dietary restraint may be beneficial in facilitating weight loss, improving physical health and maintaining weight control after treatment (74).
It should be noted that dietary restraint scales measure the intention to eat less rather than the real energy intake restriction (75); although some people may develop an intention to restrict their food intake, this intention is not always translated into action (73, 75). Planning, maintenance self-efficacy and action control are suggested to be important variables that may explain the gap between intention and behavior; subjects showing higher food restriction intention are more vulnerable to future eating disorders and weight gain (76).
Similarly, self-dieting is common among adolescents but it is not always a harmless behavior (17, 77). In fact, if self-dieting is not supervised or controlled, may lead to negative emotions that increase the risk of binge eating and use of inappropriate compensatory behaviors (17, 78).
Additionally, binge eating is a cognitive and behavioral process that is particularly important in the context of obesity (74), as recently demonstrated by a meta-analysis (79) binge eating symptoms are prevalent in more than one quarter of children and adolescents with overweight and obesity (19, 79).
Goossens and Bishop-Gilyard (60, 61) found a significant decrease in binge eating symptoms in adolescents post MT, confirming the importance of a structured MT rather than self-made -diets. They also distinguished between OBE, with the onset of LC over eating a larger amount of food that other people would not do, and SBE, with the onset of LC over eating a subjective large amount of food, that other people would not quantify as unambiguously large (61). The authors (61) reported a decrease of SBE after MT while OBE did not change (Table 4). This may occur since SBE seems quite common in youngsters, and its association with obesity and psychological impairment has already been demonstrated (80) while OBE is more common in adults (80).
Moreover, children and adolescents with obesity can develop body dissatisfaction which is linked to unhealthy weight control behaviors, binge eating, and lower physical activity levels (81); in addition, children and adolescents with obesity or overweight may experience weight stigma that exacerbates weight gain and creates additional barriers to healthy behavioral changes (82).
However, concern for body image, which is central to adolescents' overall sense of self-esteem, can play a dual role according to personal and environmental interactions (83, 84). In fact, it may exert negative or positive feedback, respectively, pushing toward dieting and triggering overeating or acting as a motivational driver toward healthier eating and lifestyle behaviors (83, 84). Studies reported in our systematic review (55, 61) assessed concern for body image throughout different questionnaires, investigating self-perceptions, weight, and shape concern. Only Balantekin et al. (55) and Goossens et al. (61) showed an improvement of self-perception, weight and shape concern, post MT.
Among the EDS, emotional and external eating can be considered behaviors related to overeating. Emotional eating means eating in response to emotional states, such as hunger, fear or anxiety, while external eating identifies eating in response to environmental food stimuli, such as sight and smell of food, regardless of hunger, and satiety stimuli (85).
Moreover, disinhibition leads to increase food intake and overeating if exposed to emotional stimuli (57).
Studies described in our systematic review (56, 57, 59, 62) showed that MT had a positive impact on external eating, disinhibition of control and emotional eating. Many authors (56, 57, 59, 62) concluded by agreeing that MT could influence eating behavior and that children/adolescents with overweight/obesity undergoing MT learned to react to emotional stress and external stimuli.
In this systematic review, we also investigated the weight and/or BMI reduction/fluctuation, as possible confounding factor.
A statistically significant decrease in BMI was observed in all MT approaches (54–62) except for Bishop-Gilyard et al. (60) where the decrease did not reach the significance.
Some authors (55, 56, 60) also analyzed the relation between EDS, such as weight and shape concern (55), binge eating episodes (60), dietary restraint, and external eating (56) and BMI reduction and/or fluctuation post MT.
Balantekin et al. (55) reported that BMIz was not strictly related to weight and shape concern improvement. In fact, although the authors (55) described a significant reduction in BMIz and weight concern post MT in the whole study sample. They reported a lower reduction in BMIz in subjects with a high probability to develop ED and in subjects with a greater likelihood of developing weight and shape concerns, when compared to subjects with a low risk of ED. Moreover, shape and weight concern in subjects with at high risk of ED was not significantly related to BMIz reduction (55).
Bishop-Gilyard et al. (60) revealed that adolescents with obesity and binge eating episodes lost the same amount of weight as those without binge.
Halberstadt et al. (56) described a BMI re-gain impact on EDS, showing that weight re-gain affected the increase of restraint and external eating post MT, only in girls.
Therefore, given the small numbers of the studies mentioned above (55, 56, 60), we could only hypothesize that weight status and EDS improvement after MT were independent factors.
Notably, all selected studies (54–62) provided MT approaches including CBT and eight of them (54–61) considered either active and frequent participation of the parents/caregivers during MT or “family-centered” approaches.
Multiple organizations, including the American Dietetic Association, the American Academy of Pediatricians, and the National Academy of Medicine, support family-based treatments, encouraging healthy nutrition and parent education/modeling (86, 87). Nowadays, supporting parents to improve their skills regarding healthy child growth is considered an important public health goal (65, 88). In fact, it is well known (89) that parents impact child's behaviors throughout home environmental influence. For instance, parenting practices and lifestyle such as eating pattern, provision of nutritious food, physical activity reinforcement, and counteracting sedentary behaviors could influence children eating behavior. On the other hand, family-based interventions are an effective method, positively impacting pediatric obesity treatment outcome and improving the probability for children and adolescents to be adherent and successful once engaged in a weight loss program (90, 91).
Strength and Limitations
The strength of this systematic review includes the development of a comprehensive search strategy applied, for the first time, on the effect of MT on the development and/or progress of EDS in children with overweight/obesity.
The assessment of risk of BIAS reported that the quality of the included studies was variable. Weak studies were included in this review and study quality was generally limited by participants selection (see Table S1, column “selection bias”). In fact, participants were no more likely to be representative of the target population, according to the tool that was used in this systematic review (51–53); in the selected studies, participants are often referred from a clinic or self-recruited via fliers, newspapers, television, radio, referrals from schools and community providers.
Another limit is that MTs were largely heterogeneous in length, period of discharge of patient, frequency and intensity of sessions, parents' involvement. Finally, quite a number of behavioral and psychosocial variables were assessed, by means of different validated questionnaires.
Conclusions
Evidence showed that comprehensive MTs for children and adolescents with obesity reduce BMI and risk of future co-morbidities.
Although obesity and ED have traditionally been conceptualized as separate conditions, EDS in the pediatric population, with a history of obesity, are not unusual. Overweight and obesity in childhood and adolescence significantly increase the risk for ED development.
Results from this systematic review highlighted, for the first time, the positive short- and long-term impact of MTs on ED symptoms, which are not always associated to BMI reduction in children. Therefore, awareness amongst clinicians who treat children and adolescents with overweight and obesity should be raised so that EDS could be identified and treated accordingly.
Author Contributions
RD, ID, and DP designed the search strategy. ID and DP screened studies for inclusion. RD resolved any uncertainty concerning the inclusion of specific studies. All authors analyzed results and drafted the manuscript. HC approved the manuscript. All authors are in agreement with the manuscript and declare that the content has not been published elsewhere.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2019.00123/full#supplementary-material
References
- 1.Farpour-Lambert NJ, Baker JL, Hassapidou M, Holm JC, Nowicka P, O'Malley G, et al. Childhood obesity is a chronic disease demanding specific health care–a position statement from the Childhood Obesity Task Force (COTF) of the European Association for the Study of Obesity (EASO). Obes Facts. (2015) 8:342–9. 10.1159/000441483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Commission on Ending Childhood Obesity. Report of the Commission on Ending Childhood Obesity. Geneva: World Health Organization; (2016). [Google Scholar]
- 3.Wijnhoven TM, van Raaij JM, Spinelli A, Starc G, Hassapidou M, Spiroski I, et al. WHO European Childhood Obesity Surveillance Initiative: body mass index and level of overweight among 6-9-year-old children from school year 2007/2008 to school year 2009/2010. BMC Public Health. (2014) 14:806. 10.1186/1471-2458-14-806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden C, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. (2016) 315:2292–9. 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huxley R, Mendis S, Zheleznyakov E, Reddy S, Chan J. Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk—a review of the literature. Eur J Clin Nutr. (2010) 64:16–22. 10.1038/ejcn.2009.68 [DOI] [PubMed] [Google Scholar]
- 6.NCD Risk Factor Collaboration (NCD-RisC) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. (2016) 387:1377–96. 10.1016/S0140-6736(16)30054-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. (2017) 390:2627–42. 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rendón-Macías ME, Rosas-Vargas H, Villasís-Keever MÁ, Pérez-García C. Children's perception on obesity and quality of life: a Mexican survey. BMC Pediatr. (2014) 14:131. 10.1186/1471-2431-14-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Micali N, Solmi F, Horton NJ, Crosby RD, Eddy KT, Calzo JP, et al. Adolescent eating disorders predict psychiatric, high-risk behaviors and weight outcomes in young adulthood. J Am Acad Child Adolesc Psychiatry. (2015) 54:652–9. 10.1016/j.jaac.2015.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rancourt D, McCullough MB. Overlap in eating disorders and obesity in adolescence. Curr Diab Rep. (2015) 15:78. 10.1007/s11892-015-0645-y [DOI] [PubMed] [Google Scholar]
- 11.Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Family Med Prim Care. (2015) 4:187–92. 10.4103/2249-4863.154628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sim LA, Lebow J, Billings M. Eating disorders in adolescents with a history of obesity. Pediatrics. (2013) 132:e1026–30. 10.1542/peds.2012-3940 [DOI] [PubMed] [Google Scholar]
- 13.Villarejo C, Fernández-Aranda F, Jiménez-Murcia S, Peñas-Lledó E, Granero R, Penelo E, et al. Lifetime obesity in patients with eating disorders: increasing prevalence, clinical and personality correlates. Eur Eat Disorders Rev. (2012) 20:250–4. 10.1002/erv.2166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sagar R, Gupta T. Psychological aspects of obesity in children and adolescents. Indian J Pediatr. (2018) 85:554–9. 10.1007/s12098-017-2539-2 [DOI] [PubMed] [Google Scholar]
- 15.Nieman P, Leblanc CM, Canadian Paediatric Society Healthy Active Living and Sports Medicine Committee . Psychosocial aspects of child and adolescent obesity. Paediatr Child Health. (2012) 17:205–6. 10.1093/pch/17.4.205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rankin J, Matthews L, Cobley S, Han A, Sanders R, Wiltshire HD, et al. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolesc Health Med Ther. (2016) 7:125–46. 10.2147/AHMT.S101631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cena H, Stanford FC, Ochner L, Fonte ML, Biino G, De Giuseppe R, et al. Association of a history of childhood-onset obesity and dieting with eating disorders. Eat Disord. (2017) 25:216–29. 10.1080/10640266.2017.1279905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldschmidt AB, Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Yanovski SZ, et al. Subtyping children and adolescents with loss of control eating by negative affect and dietary restraint. Behav Res Ther. (2008) 46:777–87. 10.1016/j.brat.2008.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiechtner L, Fonte ML, Castro I, Gerber M, Horan C, Sharifi M, et al. Determinants of binge eating symptoms in children with overweight/obesity. Child Obes. (2018) 14:510–7. 10.1089/chi.2017.0311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics. (2014) 34:582–92. 10.1542/peds.2014-0194 [DOI] [PubMed] [Google Scholar]
- 21.Evans EH, Adamson AJ, Basterfield L, Le Couteur A, Reilly JK, Reilly JJ, et al. Risk factors for eating disorder symptoms at 12 years of age: a 6-year longitudinal cohort study. Appetite. (2016) 108:12–20. 10.1016/j.appet.2016.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Veses AM, Martínez-Gómez D, Gómez-Martínez S, Vicente-Rodriguez G, Castillo R, Ortega FB, et al. AFINOS study groups. physical fitness, overweight and the risk of eating disorders in adolescents. The AVENA and AFINOS studies. Pediatr Obes. (2014) 9:1–9. 10.1111/j.2047-6310.2012.00138.x [DOI] [PubMed] [Google Scholar]
- 23.WHO Population-Based Approaches to Childhood Obesity Prevention. Geneva: World Health Organization; (2012). [Google Scholar]
- 24.Pandita A, Sharma D, Pandita D, Pawar S, Tariq M, Kaul A. Childhood obesity: prevention is better than cure. Diabetes Metab Syndr Obes. (2016) 9:83–9. 10.2147/DMSO.S90783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. (2009) CD001872 10.1002/14651858.CD001872 [DOI] [PubMed] [Google Scholar]
- 26.Ross MM, Kolbash S, Cohen GM, Skelton JA. Multidisciplinary treatment of pediatric obesity: nutrition evaluation and management. Nutr Clin Pract. (2010) 25:327–34. 10.1177/0884533610373771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Styne DM, Arslanian SA, Connor EL, Sadaf Farooqi I, Murad MH, Silverstein JH, et al. Pediatric obesity—assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. (2017) 102:709–57 10.1210/jc.2017-00561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spear BA, Barlow SE, Ervin C, Ludwig DS, Saelens BE, Schetzina KE, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. (2007) 120(Suppl. 4):254–88. 10.1542/peds.2007-2329F [DOI] [PubMed] [Google Scholar]
- 29.Kelly KP, Kirschenbaum DS. Immersion treatment of childhood and adolescent obesity: the first review of a promising intervention. Obes Rev. (2011) 12:37–49. 10.1111/j.1467-789X.2009.00710.x [DOI] [PubMed] [Google Scholar]
- 30.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. (2007) 120:S164–92. 10.1542/peds.2007-2329C [DOI] [PubMed] [Google Scholar]
- 31.Mameli C, Krakauer JC, Krakauer NY, Bosetti A, Ferrari CM, Schneider L, et al. Effects of a multidisciplinary weight loss intervention in overweight and obese children and adolescents: 11 years of experience. PLoS ONE. (2017) 12:e0181095. 10.1371/journal.pone.0181095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moores CJ, Bell LK, Miller J, Damarell RA, Matwiejczyk L, Miller MD. A systematic review of community-based interventions for the treatment of adolescents with overweight and obesity. Obes Rev. (2017) 19:698–715. 10.1111/obr.12660 [DOI] [PubMed] [Google Scholar]
- 33.Bianchini JA, da Silva DF, Nardo CC, Carolino ID, Hernandes F, Nardo N, Jr. Multidisciplinary therapy reduces risk factors for metabolic syndrome in obese adolescents. Eur J Pediatr. (2013) 172:215–21. 10.1007/s00431-012-1865-7. [DOI] [PubMed] [Google Scholar]
- 34.Carriere C, Cabaussel C, Bader C, Barberger-Gateau P, Thibault BH. Multidisciplinary care management has a positive effect on paediatric obesity and social and individual factors are associated with better outcomes Acta Pædiatr. (2016) 105:e536–42. 10.1111/apa.13560 [DOI] [PubMed] [Google Scholar]
- 35.Coles N, Birken C, Hamilton J. Emerging treatments for severe obesity in children and adolescents. BMJ. (2016) 354:i4116. 10.1136/bmj.i4116 [DOI] [PubMed] [Google Scholar]
- 36.EUFIC Childhood Obesity Review. European Food Information Council; (2017). [Google Scholar]
- 37.Reinehr T. Lifestyle intervention in childhood obesity: changes and challenges. Nat Rev Endocrinol. (2013) 9:607–14. 10.1038/nrendo.2013.149 [DOI] [PubMed] [Google Scholar]
- 38.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and metanalyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Strien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional and external eating behavior. Int J Eat Disord. (1986) 5:295–315. [DOI] [Google Scholar]
- 40.Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the eating disorder examination with children: a pilot study. Int J Eat Disord. (1996) 19:391–7. [DOI] [PubMed] [Google Scholar]
- 41.Goldschmidt AB, Doyle AC, Wilfley DE. Assessment of binge eating in overweight youth using a questionnaire version of the child eating disorder examination with instructions. Int J Eat Disord. (2007) 40:460–7. 10.1002/eat.20387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. (1994) 16:363–70. [DOI] [PubMed] [Google Scholar]
- 43.Guthrie CA, Sanderson S, Rapoport L. Development of the childrens' eating behaviour questionnaire. J Child Psychol Psychiatr. (2001) 42:963–70. 10.1111/1469-7610.00792 [DOI] [PubMed] [Google Scholar]
- 44.Pudel V, Westenhoefer J. Fragebogen zum Eßverhalten. Göttingen: Hogrefe: Verlag für Psychologie (1989). [Google Scholar]
- 45.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among 340 obese persons. Addict Behav. (1982) 7:47–55. 10.1016/0306-4603(82)90024-7 [DOI] [PubMed] [Google Scholar]
- 46.Henderson M, Freeman CP. A self-rating scale for bulimia. The 'BITE'. Br J Psychiatry. (1987) 150:18–24. 10.1192/bjp.150.1.18 [DOI] [PubMed] [Google Scholar]
- 47.Garner D. EDI-2: Eating Disorder Inventory-II. Professional Manual. Odessa, FL: Psychological Assessment Resources; (1991). [Google Scholar]
- 48.Tanofsky-Kraff M, Theim KR, Yanovski SZ, et al. Validation of the emotional eating scale adapted for use in children and adolescents (EES-C). Int J Eat Disord. (2007) 40:232–40. 10.1002/eat.20362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Spitzer RL, Devlin M, Walsh BT, Hasin D, Wing R, Marcus M, et al. Binge eating disorder: a multisite field trial of the diagnostic criteria. Int J Eat Disord. (1992) 11:191–203. [DOI] [Google Scholar]
- 50.Stunkard AJ, Messick S. Eating Inventory Manual. San Antonio, TX: Psychological Corporation; (1988). [Google Scholar]
- 51.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. (2004) 1:176–84. 10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- 52.Effective Public Health Practice Project Quality Assessment Tool For Quantitative Studies. Hamilton: Effective Public Health Practice Project; (1998). [Google Scholar]
- 53.Effective Public Health Practice Project Dictionary for the Effective Public Health Practice Project Quality Assessment Tool For Quantitative Studies. (Accessed October, 2008).(Corresponding article of interest: Thomas, B.H., Ciliska, D., Dobbins, M., and Micucci, S. (2004). A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews on Evidence-Based Nursing, 1(3), 176-184). [DOI] [PubMed] [Google Scholar]
- 54.Cohen TR, Hazell TJ, Vanstone CA, Rodd C, Weiler HA. Changes in eating behavior and plasma leptin in children with obesity participating in a family-centered lifestyle intervention. Appetite. (2018) 125:81–9. 10.1016/j.appet.2018.01.017 [DOI] [PubMed] [Google Scholar]
- 55.Balantekin KN, Hayes JF, Sheinbein DH, Kolko RP, Stein RI, Saelens BE, et al. Patterns of eating disorder pathology are associated with weight change in family-based behavioral obesity treatment. Obesity (Silver Spring). (2017) 25:2115–22. 10.1002/oby.22028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Halberstadt J, van Strien T, de Vet E, Eekhout I, Braet C, Jacob C, et al. The association of eating styles with weight change after an intensive combined lifestyle intervention for children and adolescents with severe obesity. Appetite. (2016) 99:82–90. 10.1016/j.appet.2015.12.032 [DOI] [PubMed] [Google Scholar]
- 57.Adam S, Westenhoefer J, Rudolphi B, Kraaibeek HK. Three- and five-year follow-up of a combined inpatient-outpatient treatment of obese children and adolescents. Int J Pediatr. (2013) 2013:856743. 10.1155/2013/856743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Raimunda Dâmaso A, de Piano A, da Silveira Campos RM, Corgosinho FC, Siegfried W, Caranti DA, et al. Multidisciplinary approach to the treatment of obese adolescents: effects on cardiovascular risk factors, inflammatory profile, and neuroendocrine regulation of energy balance. Int J Endocrinol. (2013) 2013:541032 10.1155/2013/541032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.De Niet J, Timman R, Bauer S, van den Akke E, Buijks H, de Klerk C, et al. Effect of a short message service maintenance treatment on body mass index and psychological well-being in overweight and obese children: a randomized controlled trial. Pediatr Obes. (2012) 7:205–19. 10.1111/j.2047-6310.2012.00048.x [DOI] [PubMed] [Google Scholar]
- 60.Bishop-Gilyard CT, Berkowitz RI, Wadden TA, Gehrman CA, Cronquist JL, Moore RH. Weight reduction in obese adolescents with and without binge eating. Obesity (Silver Spring). (2011) 19:982–7. 10.1038/oby.2010.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Goossens L, Braet C, Verbeken S, Veerle Decaluwe MA, Bosmans G. Long-term outcome of pediatric eating pathology and predictors for the onset of loss of control over eating following weight-loss treatment. Int J Eat Disord. (2011) 44:397–405. 10.1002/eat.20848 [DOI] [PubMed] [Google Scholar]
- 62.Sarvestani RS, Jamalfard MH, Kargar M, Kaveh MH, Tabatabaee HR. Effect of dietary behaviour modification on anthropometric indices and eating behaviour in obese adolescent girls. J Adv Nurs. (2009) 65:1670–5. 10.1111/j.1365-2648.2009.05029.x [DOI] [PubMed] [Google Scholar]
- 63.Braet C. Patient characteristics as predictors of weight loss after an obesity treatment for children. Obesity. (2006) 14:148–55. 10.1038/oby.2006.18 [DOI] [PubMed] [Google Scholar]
- 64.NICE Weight Management: Lifestyle Services for Overweight or Obese Children and Young People. Nice (2013). Available online at: https://www.nice.org.uk/guidance/ph47
- 65.NICE . Obesity in Children and Young People: Prevention and Lifestyle Weight Management Programmes. Nice (2015). Available online at: https://www.nice.org.uk/guidance/qs94
- 66.Goldschmidt AB, Crosby RD, Cao L, Moessner M, Forbush KT, Accurso EC, et al. Network analysis of pediatric eating disorder symptoms in a treatment-seeking, transdiagnostic sample. J Abnorm Psychol. (2018) 127:251–64. 10.1037/abn0000327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lewer M, Bauer A, Hartmann AS, Vocks S. Different facets of body image disturbance in binge eating disorder: a review. Nutrients. (2017) 9:E1294. 10.3390/nu9121294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Glasofer DR, Tanofsky-Kraff M, Eddy KT, Yanovsky SZ, Theim KR, Mirch MC, et al. Binge eating in overweight treatment-seeking adolescents. J Pediatr Psychol. (2007) 32:95–105. 10.1093/jpepsy/jsl012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus M.D. Overeating among seriously overweight children seeking treatment: results of the children's eating disorder examination. Int J Eat Disord. (2006) 39:135–40. 10.1002/eat.20218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vander Wal JS, Thelen MH. Eating and body image concerns among obese and average-weight children. Addict Behav. (2000) 25:775–8. 10.1016/S0306-4603(00)00061-7 [DOI] [PubMed] [Google Scholar]
- 71.Boutelle KN, Peterson CB, Crosby RB, Rydell SA, Zucker N, Harnack L. Overeating phenotypes in overweight and obese children. Appetite. (2014) 76:95–100. 10.1016/j.appet.2014.01.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jansen A, Nederkoorn C, van Baak L, Keirse C, Guerrieri R, Havermans R. High-restrained eaters only overeat when they are also impulsive. Behav Res Ther. (2009) 47:105e110. 10.1016/j.brat.2008.10.016 [DOI] [PubMed] [Google Scholar]
- 73.Stice E, Presnell K, Shaw H, Rohde P. Psychological and behavioral risk factors for obesity onset in adolescent girls: a prospective study. J Consult Clin Psychol. (2005) 73:195–202. 10.1037/0022-006X.73.2.195 [DOI] [PubMed] [Google Scholar]
- 74.Smith KE, Mason TB, Crosbya RD, Engela SG, Crowd SJ, Wonderlicha SA, et al. State and trait positive and negative affectivity in relation to restraint intention and binge eating among adults with obesity. Appetite. (2018) 120:327–34. 10.1016/j.appet.2017.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stice E, Sysko R, Roberto CA, Allison S. Are dietary restraint scales valid measures of dietary restriction? Additional objective behavioral and biological data suggest not. Appetite. (2010) 54:331–9. 10.1016/j.appet.2009.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Larsen JK, van Strien T, Eisinga R, Herman CP, Engels RC. Dietary restraint: intention vs behaviour restrict food intake. Appetite. (2007) 49:100–8 10.1016/j.appet.2006.12.005 [DOI] [PubMed] [Google Scholar]
- 77.Neumark-Sztainer D, Wall M, Story M, Standish A. Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. J Adolesc Health. (2012) 50:80–6. 10.1016/j.jadohealth.2011.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: findings from a 10-year longitudinal study. J Am Diet Assoc. (2011) 111:1004–11. 10.1016/j.jada.2011.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.He J, Cai Z, Fan X. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: an exploratory meta-analysis. Int J Eat Disord. (2017) 50:91–103. 10.1002/eat.22661 [DOI] [PubMed] [Google Scholar]
- 80.Tanofsky-Kraff M, Marcus M, Yanovski S, Yanovski J. Loss of control eating disorder in children age 12 years and younger: proposed research criteria. Eat Behav. (2008) 9:360–5. 10.1016/j.eatbeh.2008.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Calzo JP, Sonneville KR, Haines J, Blood EA, Field AE, Austin SB. The development of association among body mass index, body dissatisfaction, and weight and shape concern in adolescent boys and girls. J Adolesc Health. (2012) 51:517–23. 10.1016/j.jadohealth.2012.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pont SJ, Puhl R, Cook SR, Slusser W. Stigma experienced by children and adolescents with obesity. Pediatrics. (2017) 140:e20173034. 10.1542/peds.2017-3034 [DOI] [PubMed] [Google Scholar]
- 83.Heinberg Joel LJ, Thompson K, Matzon JL. Body image dissatisfaction as a motivator for healthy lifestyle change: is some distress beneficial? In: Striegel-Moore RH, Smolak L, editors. Eating Disorders: Innovative Directions in Research and Practice. Washington, DC: American Psychological Association; (2001), 215–232. 10.1037/10403-011 [DOI] [Google Scholar]
- 84.Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res. (2006) 21:770–82. 10.1093/her/cyl094 [DOI] [PubMed] [Google Scholar]
- 85.Cebolla A, Barrada JR, van Strien T, Oliver E, Baños R. Validation of the Dutch Eating Behavior Questionnaire (DEBQ) in a sample of Spanish women. Appetite. (2014) 73:58–64. 10.1016/j.appet.2013.10.014 [DOI] [PubMed] [Google Scholar]
- 86.Daniels SR, Hassink SG, Committee On Nutrition . The role of the pediatrician in primary prevention of obesity. Pediatrics. (2015) 136:e275–92. 10.1542/peds.2015-1558 [DOI] [PubMed] [Google Scholar]
- 87.Dietz WH, Belay B, Bradley D, Kahan S, Muth ND, Sanchez E, et al. A Model Framework that Integrates Community and Clinical Systems for the Prevention and Management of Obesity and Other Chronic Diseases. Washington, DC: National Academy of Medicine; (2017). [Google Scholar]
- 88.Armstrong-Heimsoth A, Johnson M, McCulley A, Basinger M, Maki K. Davison A consumer health literacy program empowering parents to find quality health information online. J Consum Health Internet. (2017) 21:111–24. 10.1080/15398285.2017.1308191 [DOI] [Google Scholar]
- 89.Ash T, Agaronov A, Young T, Aftosmes-Tobio A, Davison KK. Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis. Int J Behav Nutr Phys Act. (2017) 14:113. 10.1186/s12966-017-0571-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gentile N, Kaufman TK, Maxson J, Klein DM, Merten S, Price M, et al. The effectiveness of a family-centered childhood obesity intervention at the YMCA: a pilot study. J Community Med Health Educ. (2018) 8:591. 10.4172/2161-0711.1000591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Brotman LM, Dawson-McClure S, Huang KY, Theise R, Kamboukos D, Wang J, et al. Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics. (2012) 129:e621–8. 10.1542/peds.2011-1568 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.