Abstract
This article examines the impacts of public health insurance on the health of adults through use of data from the China Health and Nutrition Survey. We use the endogenous treatment effects model to infer the causal effects of public health insurance on health. We find that public health insurance significantly improves the physical and mental health status of health insurance beneficiaries after controlling for other covariates. Among the 2 types of voluntary public health insurance, the Urban Resident Basic Medical Insurance has the greater impact in improving health than the New Cooperative Medical Scheme. Moreover, the health effect appears to be stronger for middle-aged individuals, the elderly, and those with lower incomes than for their counterparts. The positive health effects may result from few channels, including the increase of health care utilization, the improvement of health-related behaviors, and the fact that individuals with public health insurance are more likely to use higher level care providers. This study provides implications on reforming China’s health care system.
Keywords: public health insurance, health, urban and rural adults, treatment effects model, China
What do we already know about this topic?
There are some studies about evaluating the health impact of public health insurance, but most are mainly focus only on the urban or only the rural people at one time; therefore, the results may be biased, decentralized and can hardly represent the overall China’s situation.
How does your research contribute to the field?
We evaluate the effects of public health insurance schemes on health outcomes for the urban and rural residents, using the national representative survey data from Chinese Health and Nutrition Survey during 2004 to 2015; we also investigate the heterogeneity among different age and income groups, and explore the mechanisms by which health insurance may impact health.
What are your research’s implications towards theory, practice, or policy?
This study provides implications on reforming China’s health care system and its public health insurance policies.
Introduction
Improving health and well-being of the population is often cited as the main goal of health care systems.1 China has conducted a series of public health insurance (PHI) reforms as the primary health policy over the past 2 decades, with the goal of health improvement for all. These ambitious PHI reforms consist of 3 key programs: the Urban Employee Basic Medical Insurance (UEBMI) for urban employees, the Urban Resident Basic Medical Insurance (URBMI) for unemployed urban residents, and the New Cooperative Medical Scheme (NCMS) for rural residents. We focus on the last 2 government-run voluntary schemes in this article.
The URBMI was launched in 2007 to provide health protection for urban residents not covered by the government-run mandatory UEBMI, including young children, students, the elderly, and other urban residents. It is financed by central and local government subsidies and individual contributions at the city level. The government subsidies vary by city, but the central government required a minimum total government subsidies: 40 RMB per capita in 2007, which was raised to 380 RMB in 2015. Specifically, the average premiums for adults were 236 RMB in 2007and 560 RMB in 2015. The NCMS was established in 2003 for the population in rural areas. It is financed by household premiums and subsidies shared by central and local governments at the country level. To participate in the NCMS, every person in the household has to pay 10 RMB, and governments supplement minimum 20 RMB in 2003. Due to budget constraint, the URBMI and NCMS were intended to mainly cover inpatient services and limited outpatient services,2,3 but the benefits package has become more generous, with more subsidies added to the program.4 Also, these 2 programs were expanded rapidly. Figure 1 shows the trend of PHI coverage in urban and rural China from 2004 to 2015. The enrollment rates of URBMI and NCMS were high and increased throughout the period. The enrollment rates under the URBMI were 81.38%, 93.68%, and 94.01% in 2009, 2011, and 2015, respectively, while equivalent figures for the NCMS were 71.72%, 80.70%, 94.00%, 97.50%, and 98.80% in 2004, 2006, 2009, 2011, and 2015, respectively, almost reaching the goal of universal health insurance coverage.
Figure 1.
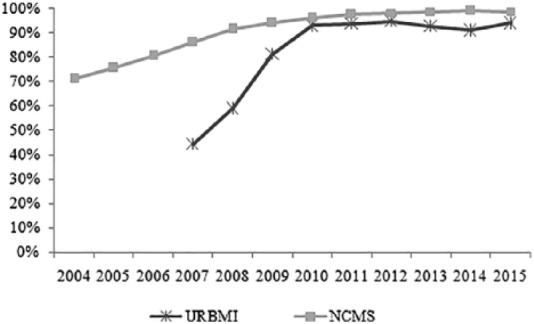
The health insurance coverage of the URBMI and NCMS.
Source. The National Bureau of Statistics (2005-2016), and the Statistical Bulletin on the Development of Health Care in China (2004-2015). URBMI = Urban Resident Basic Medical Insurance; NCMS = New Cooperative Medical Scheme.
In principle, expanding universal health insurance coverage has the potential to improve population health, by enhancing the financial access to care and increasing health service utilization. However, health insurance may not get notable health gains for various reasons, say, if the insurance benefits package is not enough for enrollees to get effective access to needed care,5 or if the moral hazard discounts the insurance health promotion. Therefore, it remains an empirical question to test whether universal insurance schemes lead to better health. Also, health insurance may result in moral hazard that lead to health resources waste because it provides health care access for lower marginal cost. Thus, whether health insurance promotes health becomes the key to measuring whether the health care utilization is effective demand or overconsumption.6 Moreover, such performance evaluations may inform the development of the Healthy China Strategy, which is one of China’s main policy goals over the next 3 decades.
The literature analyzing the effect of health insurance on health in developing countries is scare, but the studies are growing,7 including on Brazil,8 Vietnam,9 and Mexico.10 However, there is limited studies examining the causal health impact of China’s health insurance reforms and show mixed results. Several recent studies evaluated the effect of the NCMS on health and demonstrated that the NCMS significantly improved self-reported health for rural residents,11,12 while other studies did not found such effects.13,14 Even fewer researchers examined the URBMI in China, among which 2 studies are exceptions. Pan et al6 showed that URBMI beneficiaries experienced statistically better self-reported health than the uninsured among all urban residents, while the other research found that the URBMI scheme had no significant effect on health of all urban residents.15 Most studies focus only on the urban or only the rural people at one time. In this article, we infer the causal effect of PHI coverage on health for urban and rural population together.
In this article, using a national representative survey data from 5 waves of the China Health and Nutrition Survey (CHNS), we evaluate the health effects of PHI directly in China. Our article contributes to the existing literature in some aspects. First, this article focuses on the urban and rural adults at one time, and offers a comprehensive assessment of the impact of PHI on a wide range health dimensions, including physical and mental health as well as objective and subjective measures. Second, the study explores the heterogeneity effects with different socioeconomic status, the potential disparity in the health effects associated with different PHI schemes, and the mechanisms by which health insurance may impact health. Third, we pay close attention to various statistical issues, particularly the potential endogeneity of PHI coverage and health by using the endogenous treatment effects model (TEM) with regional and time fixed effects. The magnitude of the dataset used also reduces concern about potential selection biases. In sum, by combining a solid empirical framework with longitudinal data, this study can offer additional empirical evidence on the health effect of PHI in China that has drawn attention to its health care reforms.
The rest of this article proceeds as follows: “Materials and Methods” section describes the study data, while the empirical strategy employed is outlined in “Results” section. “Discussion” section presents the empirical findings, and “Conclusion” section offers a discussion and brief set of conclusions.
Materials and Methods
Data
This study uses data from the CHNS, a longitudinal survey provided by the Carolina Population Center at the University of North Carolina and the National Institute at the Chinese Center for Disease Control and Prevention. Ten waves of this survey have been conducted since 1989 on 30 000 individuals in 7200 households in 15 provinces and municipal cities that differ considerably in their geography, economic development, public resources, and health indicators through use of a multistage, random cluster design. The response rate to the survey has been consistently high, exceeding 80%.16
The CHNS contains detailed information on individual and household demographics, health status, access to health insurance, health service use, and socioeconomic status. We used data from the last 5 waves of the CHNS, ie, 2004, 2006, 2009, 2011, and 2015, as the CHNS did not ask the respondents report their NCMS before 2004. The longitudinal survey data and the timeline of the implementation of the NCMS and URBMI allow us to better control for unobservable and possible selection bias,17 which is especially important in the context of a health insurance plan with voluntary enrollment.18 We focus on adults, so we exclude children younger than 18 years. The sample was further limited to individuals who had either no insurance at all or one of the following 2 main forms of PHI: URBMI or NCMS. Consequently, individuals were excluded if they had UEBMI (8367 individuals), commercial health insurance (2781 individuals), free medical insurance (8632 individuals), or other types of insurance (170 individuals). After excluding observations with missing values, our analysis sample included 18 155 respondents in total, with 2412, 2818, 4062, 4204, and 4659 individuals from the 2004, 2006, 2009, 2011, and 2015 surveys, respectively.
Variables and Measures
The main dependent variables used in our analyses were comprised of various health outcome measures, including physical and mental health, as well as objective and subjective measures. First, as a proxy for health condition, we used chronic diseases to indicate objective physical health.19 We defined a dichotomous variable chronic disease, which was available for all 5 waves of the CHNS. It was coded as 1 if the respondent was not diagnosed with hypertension, diabetes, myocardial infarction, stroke or asthma, and 0 otherwise. Second, we used self-reported health that captures overall subjective health, associated with changes in functional ability in daily life,20 and is a powerful predictor of mortality and morbidity.21 We created a binary variable self-reported good health that was coded as 1 if a respondent reported being in very good or excellent health and zero otherwise. Finally, we also measured health status with self-rated life satisfaction to check the effect of health insurance on mental health. We created a binary variable equals 1 if respondents rated their life satisfaction as very good, good, or OK, and zero otherwise. Focused on individuals’ judgment of happiness and life satisfaction as a whole, self-rated life satisfaction is the important subjective health, which is conceptualized as indicators of mental health.22,23
The key independent variable used in the analysis was whether the respondent enrolled in the PHI—URBMI or NCMS. We also used various covariates to control for demographic and socioeconomic characteristics that may independently impact either objective or subjective measures of health status. Demographic characteristics included age, sex, marital status, household size, and the socioeconomic variables including education levels, occupation (1 = professional/technical worker or manager), residential area, and household income, which is inflated to Chinese RMB in 2015. We also controlled for the participants’ health behaviors, including smoking and drinking status that may affect health status.
Descriptive Statistics
Table 1 presents the descriptive statistics of variables stratified by PHI status. The URBMI covered about 40.93% target urban residents in 2009, while the coverage increased to 54.57% in 2015. The share of rural adults with NCMS increased from 49.07% in 2004 to 62.97% in 2015. According to standard t tests, there was significant difference in health between the nonenrollees and enrollees. People covered by PHI have a significantly higher probability of having no diagnosed chronic diseases, higher self-assessed health status, and higher self-assessed life satisfaction. Those with insurance are slightly older, more educated, have a slightly bigger household size, higher income, and are more likely to smoke, live in urban areas, and work as professional workers, technical workers, or as managers when compared with those without insurance.
Table 1.
Descriptive Statistics by PHI.
| Variables | Full sample |
No PHI |
PHI |
Significance | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Chronic diseases (1 = no) | 0.236 | 0.308 | 0.223 | 0.305 | 0.274 | 0.301 | |
| Self-assessed good health (1 = yes) | 0.662 | 0.130 | 0.647 | 0.129 | 0.706 | 0.139 | *** |
| Self-rated life satisfaction (1 = good) | 0.509 | 0.110 | 0.501 | 0.213 | 0.562 | 0.226 | ** |
| Age groups | |||||||
| 18-24 | 0.041 | 0.192 | 0.046 | 0.187 | 0.031 | 0.200 | |
| 25-34 | 0.144 | 0.350 | 0.205 | 0.400 | 0.139 | 0.348 | *** |
| 35-44 | 0.277 | 0.451 | 0.311 | 0.465 | 0.274 | 0.443 | ** |
| 45-54 | 0.286 | 0.453 | 0.316 | 0.460 | 0.283 | 0.457 | ** |
| 55-64 | 0.189 | 0.392 | 0.108 | 0.314 | 0.196 | 0.392 | *** |
| 65+a | 0.064 | 0.240 | 0.025 | 0.156 | 0.067 | 0.258 | *** |
| Male | 0.546 | 0.497 | 0.532 | 0.500 | 0.548 | 0.492 | |
| Married | 0.890 | 0.321 | 0.883 | 0.324 | 0.892 | 0.315 | |
| Education levels | |||||||
| Primary school or lessa | 0.352 | 0.477 | 0.364 | 0.480 | 0.183 | 0.387 | *** |
| Middle school | 0.341 | 0.475 | 0.351 | 0.477 | 0.256 | 0.437 | *** |
| High school | 0.214 | 0.409 | 0.198 | 0.398 | 0.387 | 0.487 | *** |
| College or more | 0.093 | 0.291 | 0.086 | 0.281 | 0.174 | 0.379 | *** |
| Occupation | 0.231 | 0.009 | 0.170 | 0.376 | 0.553 | 0.497 | *** |
| Urban resident | 0.294 | 0.450 | 0.258 | 0.498 | 0.550 | 0.437 | *** |
| Cohabitants | 3.794 | 1.525 | 3.587 | 1.368 | 3.812 | 1.536 | *** |
| Log (income) | 9.010 | 1.277 | 8.995 | 1.304 | 9.181 | 0.895 | *** |
| Smoke | 0.361 | 0.480 | 0.358 | 0.480 | 0.361 | 0.480 | |
| Drink | 0.406 | 0.491 | 0.424 | 0.494 | 0.405 | 0.491 | |
| Activity | 0.099 | 0.286 | 0.166 | 0.372 | 0.083 | 0.276 | *** |
Note. PHI = public health insurance.
Refers the omitted reference category.
P < .1. **P < .05. ***P < .01.
Methods
The purpose of this study is to assess the impact of PHI on health status. Due to the voluntary nature of enrollment with UEBMI and NCMS, those enrolled and those not enrolled may differ in both observed and unobserved characteristics, which could lead to potential sample selection bias.17 Also, reverse causality, wherein health status influences the decision to enrollment in PHI, rather than the other way around, is the other potential source of endogeneity. Hence, the direct effect of PHI is difficult to sign a priori. We need to use an innovative statistical approach to address these methodological challenges.
In this article, we employed the endogenous TEM to identify the potential self-selection bias and to address concerns over potential endogeneity.24-26 Within this framework, we have a treatment equation and an outcome equation, whereby the treatment and outcome variables are dichotomous. The outcome equation describing health status may be expressed as follows:
| (1) |
In equation 1, Hit is the outcome variable, ie, objective and subjective health status for individual i at time t. represents a set of observable covariates. εit is an idiosyncratic error term. The coefficient α1 of PHIit is our primary interest, ie, the effect of the PHI on health status. We also control the regional and time factors with a vector of dummy variables. The regional dummy variables refer to the different cities and countries in different provinces.
PHIit is the treatment variable representing PHI enrollment defined in treatment equation as follows:
| (2) |
where PHIit = 1 denotes enrollment in PHI, otherwise PHIit = 0; Zit is an instrument used to model the treatment assignment process. The error terms εi and ui are bivariate normal with mean zero. Both Zit and are assumed to be exogenous and unrelated to the error terms.
In line with the existing literature on health insurance, we instrumented enrollment in PHI with PHI implementation duration in each city/country at time t18 and the city/ country-level PHI subsidies.6 The PHI duration is the time variation of the PHI implementation in each area at time t, which is measured by a continuous variable with a range from 0 to 12. The PHI subsidies are the ratio of the government subsidy to the total premium. There are several illustrations for our instruments’ validity. First, in most cases, registered residents are only eligible for the program in the pilot cities/countries. Also, individuals are more likely to participate in PHI if the fraction of government subsidies is larger. Therefore, individual enrollment status should be highly correlated with the PHI implementation duration and the subsidies fraction. Second, the pilot cities or countries were mainly selected by the provincial governments; the local governments only implemented the PHI with the central government’s issued policy guidelines. Meanwhile, the government set the subsidies and premium levels. It is reasonable to assume that the PHI implementation duration and the subsidies are exogenous to individual health status.
In Table 2, we report the results related to the selection equation in columns 1, 3, and 5. As expected, the PHI implementation duration and PHI subsidies at city/country level were found to significantly increase the probability that individuals would have PHI, indicating strong predictive power. We also conduct 2 empirical tests to show the validity of our instruments. In the weak identification test, the F statistics are greater than 10, indicating the PHI implementation timing and subsidies are highly correlated with PHI enrollment. The overidentification test—Hansen statistic—is not significant, which shows that the instruments are exogenous, ie, the 2 instruments should satisfy the valid instrument conditions.
Table 2.
The Effect of PHI on Different Health Outcome.
| Chronic disease (1 = no) |
Self-reported good health (1 = yes) |
Self-rated life satisfaction (1 = good) |
||||
|---|---|---|---|---|---|---|
| Treatment equation | Outcome equation | Treatment equation | Outcome equation | Treatment equation | Outcome equation | |
| PHI | 0.228***
(0.018) |
0.196***
(0.045) |
0.293***
(0.060) |
|||
| Age | ||||||
| 18-24 | −0.351***
(0.054) |
0.056***
(0.010) |
−0.211 (0.130) |
0.034 (0.021) |
−0.380***
(0.055) |
0.124***
(0.023) |
| 25-34 | −0.306***
(0.040) |
0.039***
(0.009) |
−0.520***
(0.102) |
0.002 (0.017) |
−0.310***
(0.042) |
0.008 (0.020) |
| 35-44 | −0.063 (0.040) |
0.041***
(0.008) |
−0.342***
(0.010) |
−0.033**
(0.016) |
−0.093**
(0.040) |
0.017 (0.019) |
| 45-54 | 0.121***
(0.039) |
0.021**
(0.010) |
−0.320***
(0.095) |
−0.063***
(0.017) |
0.121***
(0.039) |
−0.024 (0.018) |
| 55-64 | 0.235***
(0.046) |
−0.032**
(0.009) |
−0.225**
(0.103) |
−0.058***
(0.019) |
0.229***
(0.041) |
−0.017 (0.018) |
| Male | −0.050***
(0.016) |
0.001 (0.006) |
0.021 (0.037) |
0.008 (0.011) |
−0.060***
(0.016) |
0.028**
(0.012) |
| Married | 0.027 (0.036) |
0.009 (0.006) |
0.083 (0.068) |
−0.001 (0.012) |
0.014 (0.031) |
−0.011 (0.015) |
| Middle school | 0.013 (0.021) |
−0.019***
(0.007) |
0.045***
(0.005) |
0.003 (0.013) |
0.021 (0.024) |
0.042***
(0.015) |
| High school | 0.049***
(0.002) |
−0.023***
(0.008) |
0.012***
(0.003) |
0.019 (0.015) |
0.476***
(0.025) |
0.078***
(0.017) |
| College or more | 0.192***
(0.030) |
−0.011 (0.011) |
0.080***
(0.002) |
0.027 (0.023) |
0.239***
(0.031) |
0.155***
(0.022) |
| Occupation | 0.026***
(0.007) |
0.024***
(0.008) |
0.021**
(0.009) |
0.021 (0.017) |
0.034***
(0.008) |
0.040**
(0.017) |
| Urban resident | 0.027**
(0.005) |
−0.057***
(0.006) |
0.084***
(0.004) |
−0.106**
(0.012) |
0.010 (0.013) |
−0.022*
(0.013) |
| Cohabitants | −0.014***
(0.001) |
0.005**
(0.002) |
0.003 (0.006) |
0.001 (0.004) |
−0.014***
(0.004) |
−0.013***
(0.005) |
| Log (income) | 0.072***
(0.001) |
−0.007***
(0.002) |
0.078***
(0.019) |
0.007 (0.005) |
0.046***
(0.015) |
0.006 (0.005) |
| PHI duration | 0.017***
(0.004) |
— — |
0.011**
(0.004) |
— — |
0.004**
(0.002) |
— — |
| PHI subsidies | 0.026*
(0.011) |
— — |
0.020*
(0.009) |
— — |
0.012*
(0.005) |
— — |
| Smoke | — — |
−0.019**
(0.007) |
— — |
−0.024*
(0.014) |
— — |
−0.062***
(0.015) |
| Drink | — — |
−0.018**
(0.006) |
— — |
−0.014 (0.013) |
— — |
−0.006 (0.014) |
| Regional dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| Wave dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| Wald test | 309.44*** (P = .000) | 25.78*** (P = .000) | 18.03*** (P = .000) | |||
| Observations | 18 155 | 9889 | 12 925 | |||
Note. Clustered-robust standard errors are in parentheses. PHI = public health insurance.
P < .1. **P < .05. ***P < .01.
We estimated equations 1 and 2 with the maximum likelihood approach and reported the marginal treatment effect with standard error clustered at the city or country level.27 Also, the testing of endogeneity was carried out through use of the Wald test. If the null hypothesis of ρ = 0 were rejected, then there would be an endogeneity issue; we should use the TEM to deal with this issue.
Results
Health Effects of PHI
Table 2 reports estimates of the endogenous TEM. We presented the effect of PHI on health for the 3 outcome measures in outcome equations (Table 2, column 2, 4, 6). The Wald test of ρ = 0 was statistically significant in most regressions, indicating that addressing the issue of endogeneity was of critical importance to infer the causal effect of PHI on health outcomes. The TEM model indicated that PHI coverage had a significant and positive effect on physical and mental health. For the insured, there is a 22.8% higher probability of having no diagnosed chronic disease, self-reported good health status is 19.6% greater, and self-rated good life satisfaction is 29.3% greater than the uninsured.
We further assessed how sensitive our findings are to alternative specifications. First, we used a sample bounding procedure to restrict the data from 2004 and 2009 to reestimate our model, which can exclude the effect of the URBMI and NCMS integration when we analyze the health effect of PHI, as the government began to integrate the URBMI and NCMS at the end of 2010. The results were reported in columns 1 to 3 of Table 3, which was consistent with the main results presented in Table 2. We can conclude that the integration of the URBMI and NCMS has no significant effect on our analysis. We also examined whether the health effect was robust by using the 2-stage residual inclusion (2SRI). The 2SRI is one of the instrumental variable methods to correct for endogeneity bias, which provides consistent estimates in nonlinear models.28,29 The columns 4 to 6 showed that PHI significantly improved health. The robust checks reported in Table 3 provide supporting evidence of the robustness of our main results.
Table 3.
Robustness Checks for the Health Effects of Public Health Insurance.
| Sample bounding |
Two-stage residual inclusion |
|||||
|---|---|---|---|---|---|---|
| Chronic disease (1 = no) | Self-reported good health (1 = yes) | Self-rated life satisfaction (1 = good) | Chronic disease (1 = no) | Self-reported good health (1 = yes) | Self-rated life satisfaction (1 = good) | |
| Public health insurance | 0.305***
(0.026) |
0.234***
(0.057) |
0.352***
(0.127) |
0.301***
(0.025) |
0.289***
(0.065) |
0.106*
(0.055) |
| Wald test | 121.27***
(P = .000) |
22.92***
(P = .000) |
5.89**
(P = .015) |
571.80***
(P = .000) |
128.73***
(P = .000) |
90.53**
(P = .012) |
| Observations | 9292 | 5230 | 4062 | 18 155 | 9889 | 12 925 |
Note. Clustered-robust standard errors are in parentheses.
P < .1. **P < .05. ***P < .01.
Health Effects of Different PHI Schemes
In addition to the general effect of PHI coverage on various health outcomes, we also examined how different types of PHI coverage (eg, URBMI and NCMS) impacted health outcomes in 3 separate regressions (see Table 4); this may arise through the different ways in which each type of insurance is designed and implemented. We found that people covered by URBMI were significantly more likely to have no chronic disease, report good health, and life satisfaction than those with NCMS coverage. These results suggest that URBMI coverage had a greater effect in improving health status than that associated with NCMS.
Table 4.
The Health Effects of URBMI and NCMS.
| Chronic disease (1 = no) |
Self-reported good health (1 = yes) |
Self-rated life satisfaction (1 = good) |
||||
|---|---|---|---|---|---|---|
| URBMI | NCMS | URBMI | NCMS | URBMI | NCMS | |
| Public health insurance | 0.279***
(0.026) |
0.201***
(0.006) |
0.251***
(0.073) |
0.178***
(0.018) |
0.349***
(0.027) |
0.189***
(0.016) |
| Wald test | 90.63***
(P = .000) |
88.46***
(P = .000) |
15.27***
(P = .000) |
25.39***
(P = .000) |
2.97*
(P = .081) |
39.17**
(P = .000) |
| Observations | 12 925 | 18 155 | 4659 | 9889 | 12 925 | 12 925 |
Note. We also controlled other demographic and socioeconomic variables. Clustered-robust standard errors are in parentheses. URBMI = Urban Resident Basic Medical Insurance; NCMS = New Cooperative Medical Scheme.
P < .1. **P < .05. ***P < .01.
This finding may be associated with the design of each insurance scheme and the manner in which each scheme was implemented. The URBMI covers all inpatient services and restricts outpatient service coverage to chronic or catastrophic diseases. In contrast, the NCMS does not cover any of the costs of outpatient care. In addition, reimbursement levels and the coverage ceilings are low under the NCMS compared with the URBMI, while the deductibles and coinsurance rates are higher for the NCMS relative to the URBMI. When the URBMI and NCMS were initially implemented, government regulations specified the deductibles as 659 yuan per capita for expenses in a general hospital under the URBMI and 1500 yuan per capita under the NCMS. Differences in reimbursement rates, ceilings, and deductibles also varied between cities and counties due to regional variation in subsidies and premiums. According to the calculation in our sample, the average reimbursement rate for inpatient care in 2009, 2011, and 2015 were 30.2%, 80.5%, and 85.7%, respectively, under the URBMI, while equivalent figures for the NCMS were 30.1%, 43.5%, and 55.8%. These differences in lower deductibles, higher reimbursement rates, and broader coverage make residents covered by URBMI more likely to use both inpatient and outpatient services than those covered by NCMS. Moreover, residents with URBMI coverage are more likely to seek care from higher level hospitals than those covered with NCMS.30 These factors may account for the greater impact of URBMI coverage on health status than the effect of NCMS.
Heterogeneous Effects
In this section, we further analyzed whether PHI had heterogeneous effects by age and income (see Figure 2). We divided the sample into 3 groups to assess potential differential effects for younger adults (18-45 years old), middle-aged adults (46-59 years old), and the elderly (60 years and above). We also classified the sample by household income: below the 25th percentile, between the 25th and 75th percentiles, and above the 75th percentile. We found evidence of heterogeneous effects by age and income. The health effect of PHI was stronger for both middle-aged and elderly individuals. Also, PHI benefits disadvantaged groups with low income more. The PHI significantly increased the probability of having no chronic diseases, reporting good health, and good life satisfaction by 28.9%, 27.2%, and 23.9%, respectively, for the low-income group. The medium-income group also benefited from participating in PHI, but the beneficial effects of insurance were insignificant for the high-income group. These findings could be explained by the reasons that poor PHI participants have more significant increase in health care utilization,12 and poor enrollees are more likely to feel relieved of a medical financial burden.2
Figure 2.
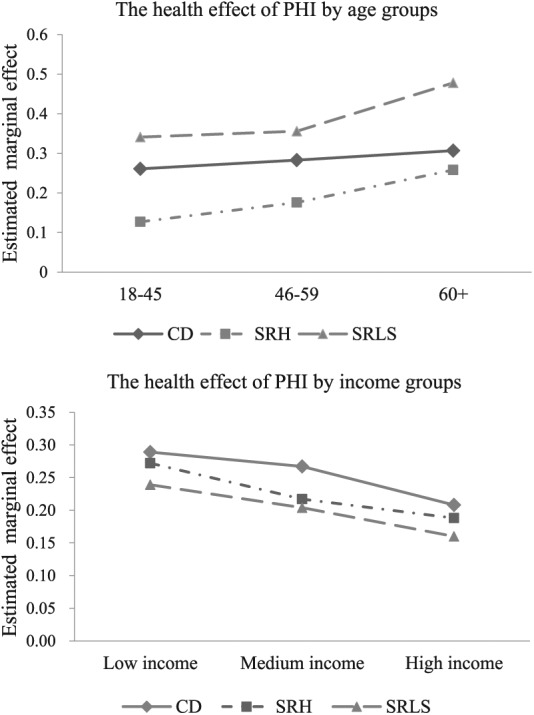
The effect of PHI on health by age groups and income groups.
Note. PHI = public health insurance; CD = chronic disease (1 = no); SRH = self-reported good health (1 = yes); SRLS = self-rated life satisfaction (1 = good).
Mechanisms Discussion
The possible channels through which PHI impacts health status are important to explore. There is evidence of several mechanisms through which health insurance could improve objective and subjective health, including increasing health service utilization, improving health-related behaviors, and reducing financial risk which could reduce individual stress and positively affect health.31-34 In this section, we discuss 4 potential mechanisms: a general increase in health care use, modified health-related behaviors, an increase in the use of preventive health services, and financial protection.
For health care utilization used in our work, we had indicators for whether individuals used formal care in last month (outpatient or inpatient care), indicators for the choice of formal care providers, and the length of stay for inpatient hospital care. The results indicated that PHI was associated with a significant increase in the use of formal medical services, including both outpatient care and inpatient care; extended inpatient hospital days; and raised the probability of seeking care in a county hospital or higher level (see Panel A, Table 5). There was also evidence that people with PHI were more likely to be physically active and receive preventive health services (see Panels B and C, Table 5). We found that PHI reduced the out-of-pocket (OOP) share, but there was no significant decline in the proportion of OOP expenditures in household net expenditures, and the financial protection of PHI was still limited. The findings support the view that health care utilization, the use of preventive health services, and health-improving behaviors are enhanced in the presence of PHI, which in turn highlight possible mechanisms through which health outcomes are improved with insurance.
Table 5.
The Potential Mechanism of the Effect of PHI on Health.
| Dependent variables | PHI | ρ | Observations |
|---|---|---|---|
| Panel A: Health care utilization | |||
| (1) Any formal medical care (1 = yes) | 0.145***
(0.024) |
0.244***
(0.041) |
18 155 |
| (2) Hospital level (1 = county or city hospitals) | 0.166**
(0.073) |
−0.082***
(0.025) |
7018 |
| (3) Length of stay in hospital (days) | 0.085**
(0.041) |
0.054***
(0.011) |
3806 |
| Panel B: Health-related behaviors | |||
| (4) Physically active (1 = yes) | 0.049*
(0.025) |
−0.074 (0.050) |
18 155 |
| (5) Any preventive examination (1 = yes) | 0.137***
(0.008) |
−0.431***
(0.025) |
11 251 |
| Panel C: Financial protection | |||
| (6) OOP share of total expenditures (0-1) | −0.071*
(0.038) |
−0.245***
(0.035) |
9527 |
| (7) Proportion of OOP expenditures in household net expenditures (0-1) | −0.053 (0.059) |
−0.073***
(0.025) |
9527 |
Note. We also controlled other demographic and socioeconomic variables. Clustered-robust standard errors are in parentheses. PHI = public health insurance; OOP = out-of-pocket.
P < .1. **P < .05. ***P < .01.
Discussion
Expansion of PHI is a popular public policy issue in China. The Chinese government has embarked on several efforts to launch several different PHI programs for various populations, but all with the twin objectives of offering universal health coverage and improving population health. Despite this rapid expansion, the insurance programs in China are generally less generous, which may have limited their impact on health. Our study contributes to the existing literature by assessing the physical and the mental health effects of PHI among adults in Chinese comprehensively. Furthermore, we employed the endogenous treatment effects strategy to control for the endogeneity with the national data, which can offer a clearer (and potentially less biased) picture of the causal effect of PHI on health outcomes.
We found that people covered by PHI reported higher health status. The PHI enrollment has reduced the likelihood of having acute or chronic diseases, and increased in the likelihood of reporting good health and good life satisfaction. Among individuals with PHI, the URBMI scheme was found to have the greater effect in improving health than the NCMS scheme. This indicates that although PHI improved health outcomes, there are large differences in the impacts on health outcomes between different schemes.
Using comprehensive data including all age and income groups under different insurance coverages, we also investigated heterogeneous effects of PHI. The results revealed that the health benefits from insurance appeared to be stronger for both the middle-aged and the elderly as well as for those with lower incomes than for their counterparts. Our findings are consistent with previous international literature on the health effects of PHI.6,12,32,35 The positive health effects result from few channels, including the increase of health care and preventive health services utilization, the improvement of health-related behaviors, and the fact that individuals with PHI are more likely to use higher level care providers. These findings are also consistent with existing literature.36
These empirical findings presented in this study reinforce our understanding of the role of PHI as an integral component in the implementation of the Healthy China Strategy. Expanding health insurance coverage and improving health benefits have significant beneficial consequences for the welfare of all citizens, which is essential for a well-functioning social security and health care system. China has built universal health insurance coverage, but still need a long way to transform such coverage into cost-effective services. The results indicate that although the PHI has improved health of the Chinese people, challenges still remain. Rural residuals are in a disadvantaged situation because of the less generosity of their health insurance. This is largely due to the 2-step strategy of the health reform. As crucial steps toward the unification of basic PHI, the next steps of health reform should target on the integration of URBMI and NCMS, and fully implement the nationwide unified PHI system for urban and rural residents, to reduce the imbalance between people with different health schemes and with different social economic status.
It must be acknowledged that this study is subject to several limitations. First, the variables included in this study may be subject to measurement error as the data were based on self-reported information. However, these concerns may be reduced as the CHNS has been in place for several years and was designed by leading national and international authorities. Second, some unobservable factors may impact our estimates, but we tried to minimize this potential by controlling for as many potentially confounding variables as possible. Further research promises to be fruitful in the further.
Conclusion
This panel data study explored the causal effect of PHI on health status in the largest and most populated developing country, China. We found that PHI coverage is associated with better health. The study indicates that there is difference in health effect between different PHI programs: The health effect of the URBMI scheme was greater than the NCMS scheme. Meanwhile, the heterogeneous analysis reveals that PHI improved health more for the middle-aged and the elderly as well as for those with lower incomes. The findings could be useful in implementing the integration of different PHI in different provinces to reduce the imbalance between people with different health schemes and with different social economic status.
Acknowledgments
This research uses data from China Health and Nutrition Survey (CHNS). We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924, T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700), and the NIH Fogarty International Center (D43 TW009077, D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009, and Beijing Municipal Center for Disease Prevention and Control since 2011. We would also like to thank Dr Xinliang Yu who provided invaluable comments and suggestions for this article.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Natural Science Fund of China (No. 71804090), the National Social Science Fund of China (No. 15BJY007; No. 16CRK005), the Humanity and Social Science Project of the Ministry Education of China (No. 16YJC630070; No. 17YJCZH201), the Social Science Fund of Shandong Province (No. 18DSHJ04; No. 18BJJJ08), the Fostering Project of Dominant Discipline and Talent Team of Shandong Province Higher Education Institutions (No. 1716009).
ORCID iD: Hongli Fan  https://orcid.org/0000-0001-8675-2438
https://orcid.org/0000-0001-8675-2438
References
- 1. World Health Organization. Research for Universal Health Coverage. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 2. Lin W, Liu GG, Chen G. The Urban Resident Basic Medical Insurance: a landmark reform towards universal coverage in China. Health Econ. 2009;18(suppl 2):S83-S96. [DOI] [PubMed] [Google Scholar]
- 3. Wagstaff A, Lindelow M, Jun G, Ling X, Juncheng Q. Extending health insurance to the rural population: an impact evaluation of China’s New Cooperative Medical Scheme. J Health Econ. 2009;28(1):1-19. [DOI] [PubMed] [Google Scholar]
- 4. Li C, Yu X, Yu M. The comparative analysis of Urban Resident Basic Medical Insurance schemes of four cities in Eastern and Western China. Chin J Health Econ. 2010;29:12-13. [Google Scholar]
- 5. Yip W, Hsiao WC, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China’s huge and complex health-care reforms. Lancet. 2012;379(9818):833-842. [DOI] [PubMed] [Google Scholar]
- 6. Pan J, Lei XY, Liu GG. Health insurance and health status: exploring the causal effect from a policy intervention. Health Econ. 2016;25:1389-1402. [DOI] [PubMed] [Google Scholar]
- 7. Escobar ML, Griffin CC, Shaw RP. The Impact of Health Insurance in Low- and Middle-income Countries. Washington, DC: Brookings Institution Press; 2011. [Google Scholar]
- 8. Nyman J, Barleen N. The Effect of Supplemental Private Health Insurance on Health Care Purchases, Health, and Welfare in Brazil. Minneapolis: University of Minnesota; 2005. [Google Scholar]
- 9. Wagstaff A, Pradhan M. Health Insurance Impacts on Health and Nonmedical Consumption in Developing Countries. Washington, DC: The World Bank; 2005. [Google Scholar]
- 10. King G, Gakidou E, Imai K, et al. Public policy for the poor? a randomized assessment of the Mexican universal health insurance program. Lancet. 2009;373(9673):1447-1454. [DOI] [PubMed] [Google Scholar]
- 11. Wu C, Shen S. The health impact of China’s New Cooperative Medical Scheme. Chin Insurance Res. 2010;6:60-68. [Google Scholar]
- 12. Cheng LG, Zhang Y. The New Rural Cooperative Medical Scheme: financial protection or health improvement. Chin J Econ Res. 2012;1:120-133. [Google Scholar]
- 13. Lei X, Lin W. The New Cooperative Medical Scheme in rural China: does more coverage mean more service and better health? Health Econ. 2009;18(suppl 2):S25-S46. [DOI] [PubMed] [Google Scholar]
- 14. Chen Y, Jin GZ. Does health insurance coverage lead to better health and educational outcomes? evidence from rural China. J Health Econ. 2012;31:1-14. [DOI] [PubMed] [Google Scholar]
- 15. Hu HW, Liu GE. Impact of Urban Resident Basic Medical Insurance on national health: effect evaluation and evidence of mechanism. Chin J South Econ. 2012;10:186-199. [Google Scholar]
- 16. Popkin BM, Du SF, Zhai FY, Zhang B. Cohort profile: the China Health and Nutrition Survey—Monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. 2010;39(6):1435-1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Heckman JJ. Varieties of selection bias. American Econ Rev. 1990;80(2):313-318. [Google Scholar]
- 18. Liu H, Zhao Z. Does health insurance matter? evidence from China’s Urban Resident Basic Medical Insurance. J Comparative Econ. 2014;42:1007-1020. [Google Scholar]
- 19. Jeon B, Kwon S. Effect of private health insurance on health care utilization in a universal public insurance system: a case of south Korea. Health Policy. 2013;113:69-76. [DOI] [PubMed] [Google Scholar]
- 20. Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci. 1995;50(6):S344-S153. [DOI] [PubMed] [Google Scholar]
- 21. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21-37. [PubMed] [Google Scholar]
- 22. Headey BW, Kelley J, Wearing AJ. Dimensions of mental health: life satisfaction, positive affect, anxiety, and depression. Soc Indic Res. 1993;29:63-82. [Google Scholar]
- 23. Keyes CLM. Subjective well-being in mental health and human development research worldwide: an introduction. Soc Indic Res. 2006;77:1-10. [Google Scholar]
- 24. Cameron A, Trivedi P. Microeconometrics: Methods and Applications. New York, NY: Cambridge University Press; 2005. [Google Scholar]
- 25. Imbens G, Wooldridge J. Recent developments in the econometrics of program evaluation. J Econ Literature. 2009;47(1):5-86. [Google Scholar]
- 26. Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. 2nd ed. Cambridge, MA: MIT Press; 2010. [Google Scholar]
- 27. Aakvik A, Heckman JJ, Vytlacil EJ. Treatment effects for discrete outcomes when responses to treatment vary among observationally identical persons: an application to Norwegian vocational rehabilitation programs. J Econometrics. 2005;125(12):15-51. [Google Scholar]
- 28. Gibson TB, Mark TL, Axelsen K, Baser O, Rublee DA, McGuigan KA. Impact of statin copayments on adherence and medical care utilization and expenditures. Am J Manag Care. 2006;12:SP11-SP19. [PubMed] [Google Scholar]
- 29. Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling. J Health Econ. 2008;27:531-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhang CC, Lei XY, Strauss J, Zhao Y. Health insurance and health care among the mid-aged and older Chinese: evidence from the national baseline survey of CHARLS. Health Econ. 2017;26:431-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bhattacharya J, Goldman D, Sood N. The link between public and private insurance and HIV-related mortality. J Health Econ. 2003;22:1105-1122. [DOI] [PubMed] [Google Scholar]
- 32. Finkelstein A, Taubman S, Wright B, et al. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057-1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bai C, Wu B. Health insurance and consumption: evidence from China’s New Cooperative Medical Scheme. J Comp Econ. 2014;42(2):450-469. [Google Scholar]
- 34. Barnes K, Mukherji A, Mullen P, Sood N. Financial risk protection from social health insurance. J Health Econ. 2017;55:14-29. [DOI] [PubMed] [Google Scholar]
- 35. Huang F, Wu CJ. Estimating the effects of public health insurance on mortality of the elderly in urban China. Chin Nankai Econ Res. 2009;6:126-137. [Google Scholar]
- 36. Wagstaff A, Lindelow M. Can insurance increase financial risk? the curious case of health insurance in China. J Health Econ. 2008;27(4):990-1005. [DOI] [PubMed] [Google Scholar]


