Abstract
Medical professionals are expected to prioritize patient interests and most patients trust physicians to act in their best interest. But a single patient is never a physician’s sole concern. The competing interests of other patients, clinicians, family members, hospital administrators, regulators, insurers, and trainees are omnipresent. While prioritizing patient interests is always a struggle, it is especially challenging and important in the ICU setting where most patients lack the ability to advocate for themselves or seek alternative sources of care. This review explores factors that increase the risk, or the perception, that an ICU physician will reason, recommend, or act in a way that is not in their patient’s best interest, and discusses steps that could help minimize the impact of these factors on patient care.
Keywords: Critical Care, Patient-Centered Care, Research Design, Clinical Studies as Topic, Conflict of interest
Despite often meeting for the first time at admission, most hospitalized patients trust clinicians with their lives. In the intensive care unit (ICU) this trust is born of necessity – after all, most ICU patients are not stable enough to seek care elsewhere. However, it is naïve for clinicians to assume patient trust is invulnerable or entirely rational, especially as public trust in scientific, political, religious, and media institutions falters in some parts of the world.[1–3]
Trust is the belief that another person or entity will act in our best interest.[4, 5] Public trust in the medical profession stems in part from policies instructing healthcare providers to prioritize patient interests above other interests. For example, the American Medical Association (AMA) states in its Code of Medical Ethics[6] that “physicians’ ethical responsibility [is] to place patients’ welfare above the physician’s own self-interest” (Opinion 1.1.1). As a result, unless they belong to a population that has historically been harmed by medical professionals,[7–9] patients and their families rarely question clinician motives. But while patient welfare, or well-being, is a clinician’s primary interest, competing interests are ubiquitous.[10] Managing the competing interests of other patients, clinicians, hospital administrators, trainees, and one’s own implicit biases has become so routine that we often forget this balancing act is ever-present and yet generally invisible to patients.
Interests that influence physician decision-making and compete with patient well-being generate conflicts of interest,[11, 12] defined as “circumstances that create a risk that professional judgments or actions regarding a primary interest will be unduly influenced by a secondary interest.”[13] (Figure 1) What constitutes “undue” influence, and therefore a conflict of interest, is subjective and context specific. Similarly, well-being encompasses how a patient thinks and feels about his or her life, and is patient-specific.[14] Competing interests alone do not necessarily constitute an ethical problem or result in harm to patients, but they do produce conditions that increases the risk of harm to patients.[12] The seriousness of the harm that can result when a conflict of interest impacts a decision about the care of a critically ill patient creates a special obligation for intensivists to develop both a high degree of situational and self-awareness and the courage to name and discuss the competing interests they continually work to manage.
Figure 1:
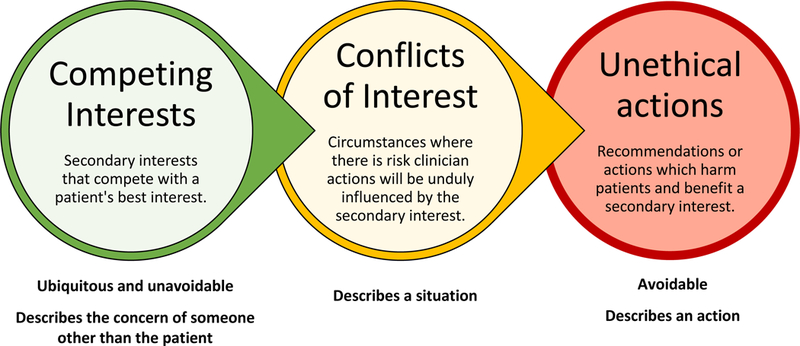
Conceptual model
Ideally, conflicts of interest should be prevented through policies and practices that align clinician and patient interests. This idea underlies the recent formation of accountable care organizations (ACOs) in the United States as part of the Affordable Care Act.[15] Physicians participating in ACOs make more money if they keep patients healthy, rather than if they provide more treatments. Similarly, the organization of some novel healthcare financing systems in Europe intends to strengthen patient-specific decision-making.[16] When secondary competing interests cannot be eliminated, the risk that they will influence a physician’s judgement should be minimized via procedures that allow decisions to be periodically reviewed for evidence of undue influence. Conflicts of interest are ubiquitous throughout medicine, but the potential consequences for critically ill patients who generally lack the ability to advocate for themselves or seek care elsewhere, makes it important to explicitly address this issue in the ICU setting.
Here, we explore factors that increase the risk, or the perception, that an ICU physician will reason, recommend, or act in a way that might be construed as not in their patient’s best interest.[17] Our goal is not to dishonor or cast doubt on prior decisions. Rather, we hope that naming the many parties with a stake in these decisions and the pervasive competing interests will illustrate both the ethical challenges intensivists are routinely expected to navigate and the vast faith patients and families place in the integrity of critical care professionals. Understanding, exploring, and explicitly addressing competing interests provides an opportunity to minimize the impact of these interests on patient care, thereby potentially preventing avoidable harm.
Interests of other ICU Patients and Patients Being Considered for ICU Admission
Resources such as operating rooms, equipment, and physicians’ or other clinicians’ time and attention are finite. So while patient well-being is an intensivist’s first priority, not every patient can be first. When multiple ICU patients stand to benefit from a limited resource, intensivists decide which patients to treat first.[18] (Table 1) These decisions constitute a form of triage in which priority is generally given to patients who are most likely to benefit or are at the greatest risk of death. Managing the competing interests of admitted patients is generally not recognized as an ethical problem unless ethically irrelevant factors such as patient race, gender, religion, political preferences, citizenship status, ability to pay for care, celebrity status, personal relationships with hospital personnel, or sexual orientation influence decisions.[19, 20] But because ICU patients are unaware of other patients’ needs, how patients are prioritized is not transparent, and in the context of promotional campaigns that stress the philosophy of patient-centered care, waiting for care or attention is sometimes surprising or confusing for patients and their families.
Table 1:
How the Interests of Other Patients, Family Members, and Trainees Compete or Conflict with Patient Interests
| Interested party | How a patient’s care could be affected |
|---|---|
| Other ICU patients | When multiple patients need a procedure or intervention requiring a particular clinician or piece of equipment, some patient are forced to wait. Example: There are more patients requiring CVVHD than CVVHD units available in the hospital. |
| Patients outside the hospital | When the ICU is full, patients for whom an additional day of ICU-level care is optimal may be downgraded to make an ICU bed available for a patient seeking ICU admission. |
| ICU families | Families may gain financially from hastening (inheritance) or delaying (disability benefits) a patient’s death. When family members do not support a patient’s informed decision to forgo life support, therapies are initiated or continued to assuage family members. |
| Medical trainees | Critical care fellows, who are not the most experienced clinicians available, must practice certain procedures a pre-determined number of times to demonstrate proficiency. Example: Choosing to perform a bronchoscopy for a patient with community-acquired pneumonia when either a bronchoscopy or an endotracheal aspirate is appropriate and fellows need to practice bronchoscopy. |
Abbreviations: CVVHD, Continuous veno-venous hemodialysis; ICU, Intensive Care Unit
The rationales supporting decisions about which patients to admit to an ICU differ across countries,[21] are generally not communicated to patients,[22, 23] and can impact the care of existing ICU patients. This is most likely to happen in busy hospitals where ICU beds are a scarce resource. In these circumstances, patients who can safely be treated outside the ICU may be discharged or moved to a lower-intensity level of care, even though another day of higher-intensity ICU-level care may be in that patient’s best interest. This situation differs from decisions about which ICU patient to treat first because the intensivist has entered into a patient-physician relationship with the current ICU patient, but not usually with the person seeking hospital or ICU admission. Triage dilemmas are further complicated in rural hospitals where the nearest comparable ICU may be many miles away. In urban centers with multiple tertiary care centers, intensivists arguably have less obligation to admit patients if they believe existing ICU patient may be adversely affected.
Interests of Family Members
Patient’s family members are usually assumed to advocate for their loved one’s best interests. But a patient’s death can have major financial ramifications for families that motivate decisions. For example, when a recipient of disability benefits dies in the U.S., the Social Security Administration generally reduces or stops issuing payments. If the patient’s family is financially dependent on these disability payments, death becomes a harbinger of destitution. Conversely, family members of patients with substantial wealth or a generous life insurance policy stand to benefit financially from a patient’s death.
When patients decide to forgo or end treatment, some family members are unable to accept the decision. In this situation, patients may acquiesce to another round of chemotherapy or a few more weeks of mechanical ventilation to give their loved ones time to accept their prognosis. But other patients are adamantly opposed to additional treatment. Even when a patient has been unwavering and has legally documented their preferences, a power differential remains between terminally ill patients and their families. This imbalance stems from the fact that patients with critical illness often lose the ability to communicate or advocate for themselves. Clinicians know such patients are unlikely to regain sufficient strength to create bad publicity for the hospital or file a lawsuit for assault, battery, or inadequate informed consent.[24] In contrast, distraught or aggrieved family members may register complaints with the hospital’s office of patient-relations, post scathing reviews online, file a wrongful death lawsuit, or even threaten physical violence. Even intensivists who believe a patient’s decision to decline interventions is in that patient’s best interest sometimes acquiesce to insistent family members in the U.S., although this is illegal in some European countries.[25] Recognizing when families constitute a competing interest to patient well-being offers the opportunity to strive for more informed and ethical decision-making in these taxing situations.
Interests of Medical Trainees
For teaching hospitals, medical education remains a core component of the tripartite mission. However, most patients do not understand the gradations of training within members of the medical team, and they are rarely asked to consent to involving physician trainees in their care. Teaching hospitals offer access to state of the art technology and renowned clinicians. Many teaching hospitals in the U.S. also offer non-teaching services for patients who do not want to be treated by trainees.[26] Outside these non-teaching wards, faculty in teaching hospitals attempt to ensure patients receive appropriate care from the most capable physician while also ensuring their trainees receive appropriate experience in directly caring for patients. If this balance is not appropriately achieved, unnecessary interventions may be performed primarily for “medical education” rather than the benefit of the patient, or procedures may result in complications that would not have occurred if performed by a more experienced physician. Explicitly naming these competing interests with trainees should be a routine part of medical education.
Interests of Physicians
In both Europe and the United States some intensivists work on a fee-for-service contract under which performing more procedures leads to more financial compensation. When intensivists in the United States (U.S.) are salaried, clinical work quotas defined by relative value units (RVUs) are common. (Table 2) A payment formula for every test and procedure covered by the U.S. Medicare system has an associated number of RVUs for physician work.[27] Many U.S. intensivists must bill for services associated with sufficient RVUs to fulfill their contract, and performing more than the minimum quota may result in a financial bonus. Under this system, performing tests and procedures remains in a physician’s financial interest.
Table 2:
How Physician Interests Compete with ICU Patient Interests
| Secondary interest | How a patient’s care could be affected |
|---|---|
| Work quotas | Intensivist salaries may require billing patients for a minimum number of relative value units (RVUs) creating an incentive to perform tests and procedures. |
| Legal risk | Diagnostic tests or imaging may be ordered out of concern about malpractice litigation. After an error, fear of a wrongful death suit may drive life-prolonging treatment. |
| Study recruitment or outcome | Intensivists who are also clinical investigators have an interest in enrolling eligible patients in studies to meet recruitment targets and in study results. Example: If a patient is enrolled in a study with a primary outcome of extubation failure, intensivists may attempt to delay re-intubation with additional breathing treatments or non-invasive ventilation, but while a similar patient not enrolled in the study is reintubated earlier. |
| Conflict avoidance | Patients and their family experience high emotional distress, often expressed as sadness or anger when a poor prognosis is disclosed. Disclosure of prognosis is delayed to avoid witnessing and responding to this reaction. |
| Maintaining team relations | Treatment decisions prioritize work flow rather than patient welfare. Example: A Foley catheter remain in place for a patient to increase ease of nursing care. |
| Avoiding bureaucracy | Intensivists may be less likely to prescribe therapies requiring an approval process. Example: An intensivists waits until 22:01 to place an order for an antibiotic to avoid the additional forms and phone calls required for antibiotic approval when antibiotic stewards are on-duty. |
| Curiosity | Desire to understand the pathophysiology of disease may influence diagnostic testing or imaging decisions even if results aren’t expected to impact patient care. |
| Fame | Unusual treatments are more likely to garner positive media attention than the standard of care. |
| Religious belief | Intensivists who adhere to a religious tradition that condemns withdrawing life support may avoid discussing this option with patients or family members who are requesting evaluation of the goals of care. |
| Financial gain | Intensivists may preferentially prescribe or utilize products from companies they have invested in or that provide financial support through grants or honoraria. |
In some countries where physicians receive modest government salaries, patients and families have traditionally provided physician bonuses or given expensive gifts.[28] While some physicians in the former Soviet Republics view these “irregular payments” as an acceptable way for patients to express gratitude for good care and augment under-funded healthcare systems, others describe the system as medical bribery.[29, 30] The difference between accepting unregulated payments from patients and illegal payments is also easily muddled. In these environments it is perhaps unsurprising then, that writing prescriptions in return for illegal bribes from pharmaceutical companies remains a problem.[31, 32]
An intensivist, like any other clinician, may also consider his or her legal risk when developing a care plan. Most U.S. physicians are involved in a malpractice claim at some point in their career.[33] In response, physicians order tests and procedures, or avoid high-risk patients or procedures, out of fear of malpractice litigation. This practice is referred to as “defensive medicine”.[34] The degree to which concern about legal risk impacts physician decisions is challenging to measure, but U.S. hospitalists reported that 28% of their orders were at least partially defensive in a 2008 study.[35] After a life-threatening medical error has occurred, providers have a strong interest in avoiding being charged with a wrongful death which is likely to influence decisions about the continued use of life-sustaining (or death-prolonging) therapies.
Intensivists conducting clinical research have a strong interest in enrolling patients in their studies. Enrolling ICU patients is difficult because most patients can’t consent, and family members who can provide surrogate consent may be difficult to contact.[36] As a result, slow recruitment is the most frequent reason that randomized clinical trials are stopped prematurely in critical care.[37] Discontinuing a trial due to slow recruitment can have important professional consequences. Sponsors may be less likely to fund future trials proposed by the investigator, the ICU may be viewed as a less-desirable partner in future multi-site trials, and an academic clinical investigator’s prospects for professional advancement dim. Therefore, if a patient must receive a particular treatment or intervention to be eligible for a trial, the prospect of being able to recruit the patient can create an incentive for treatment. While Institutional Review Boards (IRBs) provide oversite of how trials are advertised and consent is obtained, they generally do not have the ability to monitor whether triage or treatment decisions are being made to increase the number of potentially eligible patients. The research practices and elements of informed consent required by IRBs also vary considerably across institutions.[38, 39] Additionally, when trials are not blinded, desire to demonstrate the intervention’s effectiveness may impact treatment decisions. For example, prior research has suggested that there is a higher threshold for initiating Do Not Resuscitate (DNR) orders for ICU patients enrolled in clinical trials.[40]
Maintaining interpersonal relationships with patients, patients’ family members, colleagues and administrators is also in a physician’s interest. Patients and their families understandably have strong emotional reactions when a poor prognosis is disclosed, and witnessing their distress or anger is uncomfortable. When physicians are busy or unprepared to respond to these emotions, the desire to maintain a cordial relationship with a patient or their family may influence decisions about when to disclose prognosis and inform patients of the option to prioritize comfort rather than longevity.[41] Maintaining relationships with colleagues in nursing is also a consideration. For example, removing urinary catheters or peripheral intravenous access as soon as possible is generally in the best interest of patients because this decreases the risk of infection. But removing these interventions also creates more work for busy bedside nurses who already struggle with high rates of burnout and moral distress.[42] Finally, hospitals sometimes require administrative approval before prescribing or performing certain therapies. When the process for requesting approval is burdensome, bureaucratic, or contentious this creates an incentive for intensivists to seek alternatives, rather than advocate for the therapy they believe is in the patient’s best interest.
Physician curiosity or desire for recognition can also compete with patient interests. A desire to understand the complex pathophysiology underlying illness draws many physicians into the profession. Understandably, these physicians may desire to perform tests and imaging on patients representing unusual cases, even when the results of testing are not expected to impact treatment decisions and are associated with risks. Of course, some patients and family members share this curiosity and are happy to undergo testing in pursuit of a diagnosis even when it is unlikely to impact treatment. But for critically ill patients who prioritize comfort and time outside the hospital, this testing for the sake of discovery can be burdensome. Unusual cases and treatments can also draw significant media attention. For example, an unorthodox sepsis treatment combining hydrocortisone, vitamin C, and thiamine[43] has generated substantial media attention[44, 45], celebrity for investigators, and funding for a multi-center randomized clinical trial.
Finally, a clinician’s religious belief has been described as a competing interest in medicine.[46] Currently, most religious institutions condemn physician-assisted death despite its being legal in 7 European Countries and 7 U.S. states.[47, 48] Most ICU patients are too ill to complete the steps required to obtain approval for physician-assisted death, but opposition to the practice can influence a physician’s feelings about other practices including palliative sedation and withdrawal of mechanical ventilation. With the exceptions of Sweden, Finland, and Iceland,[49] most countries, professional societies,[50] and hospitals have conscientious objection policies permitting clinicians who object to professionally contested interventions on religious grounds to avoid directly participating in those interventions as long as they provide accurate information and a timely referral to a colleague who will perform the intervention.[51]
Interests of Hospitals
The interests and concerns of hospital boards and administrators may differ from those of both clinicians and patients. Administrators are responsible for ensuring a hospital remains financially solvent and for advancing the mission of the institution, which may focus exclusively on providing medical care for a local population, or balancing patient care, teaching, and research. Depending on the environment, hospital administrators may also feel compelled to consider the interests of the national healthcare system, regulators, political leaders, local employers, insurers, or hospital board members and this can produce actions that would be in conflict with patients’ interests.
The primary interest of any hospital is to continue existing and pursuing its mission. To achieve this, the organization must have sufficient funds to continue operating. Which patients are most advantageous to admit and what treatments are beneficial to offer from a hospital perspective depends on how the hospital is compensated for services. (Table 3) In a capitated system where a fixed amount of money is provided per patient, or to care for a population within a given timeframe, it is in a hospital’s interest to avoid admitting costly patients or providing costly treatments. In contrast, a fee-for-service payment model incentivizes admitting as many patients as possible and performing costly procedures. In countries where hospital revenue depends on patients’ ability to pay, or the price charged for care depends on a patient’s insurance status, it is in a hospital’s interest to admit wealthy or well-insured patients. Administrators often seek to shield providers from these considerations to avoid creating obvious conflicts of interest that could compromise patient care. But observational data and qualitative interviews suggest this shielding may be incomplete. For example, Germany physicians reported feeling increasing pressure to consider their hospitals’ economic interests when making clinical decisions.[52] Similarly, a recent analysis found most patients who received ECMO for Acute Respiratory Distress Syndrome (ARDS) – an unproven but profitable intervention for hospitals[53] – did not first have a trial of prone positioning which is considered a proven intervention for ARDS but is generally not billable.[54]
Table 3:
How Institutional Interests Compete with ICU Patient Interests
| Secondary interest | How a patient’s care could be affected |
|---|---|
| Hospital Revenue | Hospitals with capitated payment models have an incentive to avoid costly treatments and avoid admitting costly patients. |
| Hospitals with fee-for-service payment models have an incentive to perform more costly procedures and admit as many patients as possible. | |
| In health systems where hospital revenue depends on patients’ ability to pay or their insurer, there is a strong incentive to admit patients with health insurance or the ability to directly pay full price. | |
| Hospital Reputation | Questions on a publicly-available patient satisfaction survey, which can effect hospital reputation and/or reimbursement, often ask about pain management and satisfaction with clinician communication creating incentives for physicians to treat pain aggressively and avoid discussing topics patients and families do not want to hear about. |
| Program Reputation | Organ transplant programs in the U.S. are publicly evaluated on volume and on the number of patients alive with a functioning transplanted organ 1 year after transplant. Because people waiting for an organ may choose the transplant center where they wish to be wait-listed, using life-prolonging therapy for at least 1 year after transplant is in the best interest of the transplant program. |
| Ensuring ICU beds are full | In some areas, there is pressure to keep ICU beds full to ensure adequate ICU reimbursement and several empty beds might incentivize admitting an elderly patient with multi-morbidity to the ICU when that might not be in the patient’s best interest. |
Hospital administrators must also concern themselves with a hospital’s reputation as assessed by quality metrics, rankings, and public opinion. One of the most common quality metrics in the U.S. is the 30-day mortality rate.[55] However this metric does not take patient preferences into account, creating an incentive to continue life-prolonging treatments in patients with poor prognoses who wish to withdraw life support before 30 days post-operatively.[56] This conflict is even more pronounced in transplant patients. Organ transplant programs are evaluated on the number of patients alive with a functioning transplanted organ at specific time intervals after transplant. One-year survival is publicly reported for all programs in the U.S., and people who need an organ may choose the transplant center where they wish to be waitlisted. Thus even when a transplant recipient becomes ICU-dependent and wishes to withdraw life support, U.S. transplant programs have an interest in ensuring the patient remains alive for 1 year.
Finally, hospital reputation and reimbursement may be impacted by measures of patient satisfaction. Such measures are designed to elevate the importance of patient experience which is laudable and an important outcome in its own right.[57] But high satisfaction scores are also associated with greater prescription drug expenditures and higher mortality rates,[58] causing some to worry these metrics encourage inappropriate prescribing of drugs with high abuse potential including opioids.[59] Satisfaction scores also create a disincentive for physicians to confront patients about dangerous behaviors like drug and alcohol abuse, or to share bad news about prognosis, with some physicians reportedly foregoing these conversations as a result.[60]
The Role of Cognitive Biases
Cognitive biases are automatic psychological mechanisms that short-cut deliberate reasoning. While this may be helpful for decision-making under uncertainty, cognitive biases may aggravate competing or conflicting interests. For instance, reciprocity bias is a sense of obligation and can be triggered by presents or financial payments. Wish bias and confirmation bias lead to selective uptake of information, while commitment and consistency bias restrict our willingness to change our behavior even in the face of new evidence. Implicit bias, any form of cognitive bias about which we have no conscious awareness, may be particularly difficult to address.[20, 61, 62] Some of the more common biases, such as overconfidence and tolerance to risk and uncertainty, may make it more difficult for clinicians to accurately assess the degree to which a competing interest exists or it’s potential for harm. Explicit exploration of how these biases interact with or exacerbate the challenge of preventing competing interests from exerting undue influence on patient care can become part of routine clinical care in an environment that is supportive of such exploration. Interactions with the pharmaceutical and device manufacturers in particular may give rise to cognitive biases regarding use of relevant pharmaceuticals and devices.[63, 64] Physicians should actively avoid, and be protected from, exposure to direct and indirect marketing efforts of drug and device manufacturers.
Recommendations
Competing interests in the ICU setting will always exist to varying extents. No clinician can, or should, focus solely on the well-being of one patient without concern for other patients, colleagues, or themselves. But to continue enjoying high levels of public trust, particularly about the use, withholding, and withdrawal of life-support technologies, professional societies should demonstrate commitment to ensuring competing interests do not unduly influence physician judgement, or harm patients. The two primary ways to address conflicts of interest are avoidance and disclosure.[17] A comprehensive approach to conflicts of interest depends on a combination of both avoidance and disclosure and implementation of this approach must be adapted to the specific circumstances (Figure 2).
Figure 2:
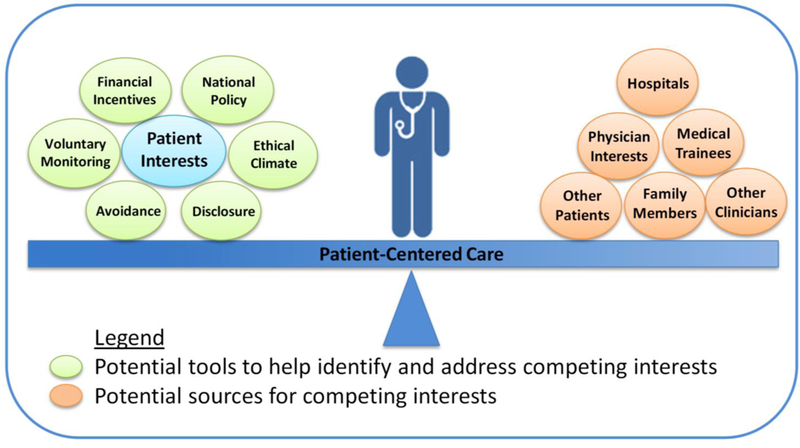
Potential role of competing interests in preventing the attainment of patient-centered care and potential tools to address competing interests
Although routinely mandated in many healthcare settings, the limitations of disclosure are well documented.[65] Asking clinicians to disclose potential conflicts of interest to patients in the ICU setting is often impractical and inappropriate for multiple reasons. First, it places the onus of responsibility on individual clinicians to determine whether they are unduly influenced by a competing interest. This level of objective self-assessment is often not feasible. Social science research has demonstrated that even motivated individuals are unable to remain objective about conflicts of interest because self-serving bias is unintentional.[66] Second, patients and their families struggle to understand the benefits and drawbacks of medical procedures[67] and billing under normal circumstances, and are even less likely to understand complex professional and financial relationships in the midst of critical illness.[68] Third, most ICU patients are involuntary consumers. Unlike patients seeking elective procedures or an outpatient provider, they cannot choose their provider or decide to transfer to another institution or another physician after learning of a conflict of interest. Finally, disclosure can have adverse and paradoxical unintended consequences. Specifically, disclosure makes some people feel they have moral license to act in their own best interest.[69, 70] In addition, disclosure of immutable competing interests may serve to erode patient or family member trust in clinicians and thereby make shared medical decision-making more difficult without providing benefit.
Determining whether competing interests have undue influence requires explicit exploration of the competing interests and influences as well as data to support this exploration.[71] Ideally, empiric evidence should inform decisions about when secondary interests are adversely impacting patient care and need to be eliminated or disclosed. In some circumstances, hospitals may be able to monitor themselves, essentially creating a transparent quality improvement program for monitoring and mitigating conflicts of interest. For example, data on ethics committee consultations regarding disagreements on whether to offer cardiopulmonary resuscitation in the event of cardiac arrest at one hospital found that patients who were not offered CPR were more than three times as likely to be critically ill, but there was no association between the committee’s recommendation and patient age, race, or functional status at admission.[72] These findings are reassuring for patients, demonstrate the hospital’s commitment to ethical practice, reduce the likelihood that biases are permitted to influence decisions, and provide a strong defense against accusations of discrimination. Similarly, Institutional Review Boards and the Scientific Registry of Transplant Recipients monitoring programs could require data on the timing and results of DNR decisions in patients enrolled in trials or receiving organs to safeguard patients from inappropriate pressure.
Exploring and addressing competing and conflicting interests should be an activity supported by the entire ICU team and not be the sole responsibility of individual clinicians. The ethical decision-making climate of an ICU can either support or detract from such exploration. Ethical climate, defined as “individual perceptions of the organization that influences attitudes and behavior and serves as a reference for employee behavior”,[73] should be recognized as an important characteristic of the quality of ICU care that will influence the ability of clinicians to explore and address competing interests. A recent study describes the development and validation of the Ethical Decision-Making Climate Questionnaire (EDMCQ).[74, 75] This tool provides the opportunity to develop and evaluate interventions that improve an ICU’s ethical climate to facilitate ethical decision-making. Importantly, a clinician’s decisions, and the competing interests for those decisions, do not operate in a vacuum, but are instead embedded in a cultural milieu influenced by national policy, financial incentives, resource pressures, patient and family factors, and institutional leadership. A recent qualitative study found that an ICU’s ethical priorities influenced the way physicians conceptualized autonomy and beneficence, which consequently influenced communication practices surrounding resuscitation decision-making.[76] The study also revealed the importance of institutional cultural norms that contributed to inappropriately aggressive care at the end of life.[77] Other studies also highlight the understanding these institutional and ethical norms as an important step to mitigate decisions that are not in the patient’s best interests.[78, 79]
When there are concerns about institutional conflicts of interest, an independent organization, similar to a consumer protection or watch-dog group could be engaged to perform this monitoring function. Admittedly, hospitals are unlikely to embrace the idea of voluntary data-sharing with a monitoring group. But proactive, voluntary monitoring programs developed with buy-in from hospitals are more likely to set achievable standards than programs created in response to adverse events. As it stands, the task of explaining to the public how competing interests impact their medical care has thus far fallen to journalists. More often than not, these explanations have not been flattering.[80–83] As public trust in political, financial, and criminal justice systems wavers, the medical community would be wise to demonstrate its commitment to a primary goal of protecting patient welfare.
Acknowledgements
The authors wish to thank Medical Librarian Carrie Price, MLS for her assistance.
Footnotes
Conflicts of interest: The authors declare that no conflict of interest exists.
References
- 1.Gauchat G (2012) Politicization of Science in the Public Sphere: A Study of Public Trust in the United States, 1974 to 2010. Am Sociol Rev 77:167–187 . doi: 10.1177/0003122412438225 [DOI] [Google Scholar]
- 2.Malone C (2016) Americans Don’t Trust Their Institutions Anymore In: FiveThirtyEight; https://fivethirtyeight.com/features/americans-dont-trust-their-institutions-anymore/. Accessed 18 Apr 2018 [Google Scholar]
- 3.Funk C (2017) Mixed Messages about Public Trust in Science In: Pew Res. Cent. Internet Sci. Tech; http://www.pewinternet.org/2017/12/08/mixed-messages-about-public-trust-in-science/. Accessed 18 Apr 2018 [Google Scholar]
- 4.Cook K (2003) Trust in Society Russell Sage Foundation, New York, NY [Google Scholar]
- 5.Hardin R (2004) Trust and Trustworthiness Russell Sage Foundation, New York [Google Scholar]
- 6.AMA Council on Ethical and Judicial Affairs (2016) AMA Code of Medical Ethics American Medical Association, Chicago [Google Scholar]
- 7.Gamble VN (1997) Under the shadow of Tuskegee: African Americans and health care. Am J Public Health 87:1773–1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones DS (2002) The Health Care Experiments at Many Farms: The Navajo, Tuberculosis, and the Limits of Modern Medicine, 1952–1962. Bull Hist Med 76:749–790 . doi: 10.1353/bhm.2002.0186 [DOI] [PubMed] [Google Scholar]
- 9.Stern AM (2005) Sterilized in the Name of Public Health: Race, Immigration, and Reproductive Control in Modern California. Am J Public Health 95:1128–1138 . doi: 10.2105/AJPH.2004.041608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stell LK (2004) Two cheers for physicians’ conflicts of interest. Mt Sinai J Med N Y 71:236–242 [PubMed] [Google Scholar]
- 11.Schünemann HJ, Osborne M, Moss J, et al. (2009) An official American Thoracic Society Policy statement: managing conflict of interest in professional societies. Am J Respir Crit Care Med 180:564–580 . doi: 10.1164/rccm.200901-0126ST [DOI] [PubMed] [Google Scholar]
- 12.McCoy MS, Emanuel EJ (2017) Why There Are No “Potential” Conflicts of Interest. JAMA 317:1721–1722 . doi: 10.1001/jama.2017.2308 [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine (US) Committee on Conflict of Interest in Medical Research, Education, and Practice (2009) Conflict of Interest in Medical Research, Education, and Practice National Academies Press (US), Washington (DC) [PubMed] [Google Scholar]
- 14.Diener E, Scollon CN, Lucas RE (2009) The evolving concept of subjective well-being: The multifaceted nature of happiness. In: Assessing well-being: The collected works of Ed Diener Springer Science + Business Media, New York, NY, US, pp 67–100 [Google Scholar]
- 15.McClellan M, McKethan AN, Lewis JL, et al. (2010) A national strategy to put accountable care into practice. Health Aff Proj Hope 29:982–990 . doi: 10.1377/hlthaff.2010.0194 [DOI] [PubMed] [Google Scholar]
- 16.Pimperl A, Schulte T, Mühlbacher A, et al. (2017) Evaluating the Impact of an Accountable Care Organization on Population Health: The Quasi-Experimental Design of the German Gesundes Kinzigtal. Popul Health Manag 20:239–248 . doi: 10.1089/pop.2016.0036 [DOI] [PubMed] [Google Scholar]
- 17.Tonelli MR (2007) Conflict of Interest in Clinical Practice. CHEST 132:664–670 . doi: 10.1378/chest.07-0315 [DOI] [PubMed] [Google Scholar]
- 18.Evans S, Darvall J, Gorelik A, Bellomo R (2018) Influence of ward round order on critically ill patient outcomes. J Crit Care 45:110–113 . doi: 10.1016/j.jcrc.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 19.Stepanikova I (2012) Racial-ethnic biases, time pressure, and medical decisions. J Health Soc Behav 53:329–343 . doi: 10.1177/0022146512445807 [DOI] [PubMed] [Google Scholar]
- 20.FitzGerald C, Hurst S (2017) Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics 18: . doi: 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evans TW, Nava S, Mata GV, et al. (2011) Critical care rationing: international comparisons. Chest 140:1618–1624 . doi: 10.1378/chest.11-0957 [DOI] [PubMed] [Google Scholar]
- 22.Mielke J, Martin DK, Singer PA (2003) Priority setting in a hospital critical care unit: qualitative case study. Crit Care Med 31:2764–2768 . doi: 10.1097/01.CCM.0000098440.74735.DE [DOI] [PubMed] [Google Scholar]
- 23.Cooper AB, Joglekar AS, Gibson J, et al. (2005) Communication of bed allocation decisions in a critical care unit and accountability for reasonableness. BMC Health Serv Res 5:67 . doi: 10.1186/1472-6963-5-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pope T (2017) Legal Briefing: New Penalties for Disregarding Advance Directives and Do-Not-Resuscitate Orders. J Clin Ethics Spring:74–81 [PubMed] [Google Scholar]
- 25.Abadir PM, Finucane TE, McNabney MK (2011) When doctors and daughters disagree: twenty-two days and two blinks of an eye. J Am Geriatr Soc 59:2337–2340 . doi: 10.1111/j.1532-5415.2011.03700.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reilly BM (2014) Don’t Learn on Me — Are Teaching Hospitals Patient-Centered? N Engl J Med 371:293–295 . doi: 10.1056/NEJMp1405709 [DOI] [PubMed] [Google Scholar]
- 27.Laugesen MJ (2014) The Resource-Based Relative Value Scale and Physician Reimbursement Policy. Chest 146:1413–1419 . doi: 10.1378/chest.13-2367 [DOI] [PubMed] [Google Scholar]
- 28.Holt E (2015) Slovak bribery case sparks wider debate in eastern Europe. The Lancet 385:2242 . doi: 10.1016/S0140-6736(15)61051-0 [DOI] [PubMed] [Google Scholar]
- 29.Kakuk P, Domján A (2013) Healthcare Financing and Conflict of Interests in Hungary: The System of Irregular Payments and its Challenges to the Integrity of Healthcare Ethics. Camb Q Healthc Ethics 22:263–270 . doi: 10.1017/S0963180113000078 [DOI] [PubMed] [Google Scholar]
- 30.Manea T (2015) Medical Bribery and the Ethics of Trust: The Romanian Case. J Med Philos 40:26–43 [DOI] [PubMed] [Google Scholar]
- 31.Burashnikova IS, Ziganshin AU, Ziganshina LE (2008) Attitudes to pharmaceutical promotion techniques among healthcare professionals in the Republic of Tatarstan, Russia. Int J Risk Saf Med 20:57–71 . doi: 10.3233/JRS-2008-0425 [DOI] [Google Scholar]
- 32.Jofre S (2014) GSK faces accusations of bribing doctors in Poland. BMJ 348:g2768 . doi: 10.1136/bmj.g2768 [DOI] [PubMed] [Google Scholar]
- 33.Jena AB, Seabury S, Lakdawalla D, Chandra A (2011) Malpractice risk according to physician specialty. N Engl J Med 365:629–636 . doi: 10.1056/NEJMsa1012370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mello MM, Chandra A, Gawande AA, Studdert DM (2010) National Costs Of The Medical Liability System. Health Aff Proj Hope 29:1569–1577 . doi: 10.1377/hlthaff.2009.0807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rothberg MB, Class J, Bishop TF, et al. (2014) The Cost of Defensive Medicine on 3 Hospital Medicine Services. JAMA Intern Med 174:1867–1868 . doi: 10.1001/jamainternmed.2014.4649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burns KEA, Zubrinich C, Tan W, et al. (2013) Research Recruitment Practices and Critically Ill Patients. Am J Respir Crit Care Med 187:1212–1218 . doi: 10.1164/rccm.201208-1537OC [DOI] [PubMed] [Google Scholar]
- 37.Schandelmaier S, von Elm E, You JJ, et al. (2016) Premature Discontinuation of Randomized Trials in Critical and Emergency Care: A Retrospective Cohort Study. Crit Care Med 44:130–137 . doi: 10.1097/CCM.0000000000001369 [DOI] [PubMed] [Google Scholar]
- 38.Silverman H, Hull SC, Sugarman J (2001) Variability among institutional review boards’ decisions within the context of a multicenter trial. Crit Care Med 29:235–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khan MA, Barratt MS, Krugman SD, et al. (2014) Variability of the institutional review board process within a national research network. Clin Pediatr (Phila) 53:556–560 . doi: 10.1177/0009922814527504 [DOI] [PubMed] [Google Scholar]
- 40.Mehter HM, Wiener RS, Walkey AJ (2014) “Do Not Resuscitate” Decisions in Acute Respiratory Distress Syndrome: A Secondary Analysis of Clinical Trial Data. Ann Am Thorac Soc 11:1592–1596 . doi: 10.1513/AnnalsATS.201406-244BC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Darmon M, Ducos G, Coquet I, et al. (2016) Formal Academic Training on Ethics May Address Junior Physicians’ Needs. Chest 150:180–187 . doi: 10.1016/j.chest.2016.02.651 [DOI] [PubMed] [Google Scholar]
- 42.Rushton CH, Batcheller J, Schroeder K, Donohue P (2015) Burnout and Resilience Among Nurses Practicing in High-Intensity Settings. Am J Crit Care 24:412–420 . doi: 10.4037/ajcc2015291 [DOI] [PubMed] [Google Scholar]
- 43.Marik PE, Khangoora V, Rivera R, et al. (2017) Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study. CHEST 151:1229–1238 . doi: 10.1016/j.chest.2016.11.036 [DOI] [PubMed] [Google Scholar]
- 44.Simpson E A Norfolk doctor found a treatment for sepsis. Now he’s trying to get the ICU world to listen In: Virginian-Pilot; http://pilotonline.com/news/local/health/article_7a3063e5-24cf-56c1-b25c-142731604196.html. Accessed 23 Apr 2018 [Google Scholar]
- 45.Did An IV Cocktail Of Vitamins And Drugs Save This Lumberjack From Sepsis? In: NPR; org. https://www.npr.org/sections/health-shots/2018/02/21/583845485/did-an-iv-cocktail-of-vitamins-and-drugs-save-this-lumberjack-from-sepsis. Accessed 23 Apr 2018 [Google Scholar]
- 46.Smith R, Blazeby J (2018) Why religious belief should be declared as a competing interest. BMJ 361:k1456 . doi: 10.1136/bmj.k1456 [DOI] [Google Scholar]
- 47.Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, Cohen J (2016) Attitudes and practices of euthanasia and physician-assisted suicide in the united states, canada, and europe. JAMA 316:79–90 . doi: 10.1001/jama.2016.8499 [DOI] [PubMed] [Google Scholar]
- 48.Pope T (2018) Legal History of Medical Aid in Dying: Physician Assisted Death in U.S. Courts and Legislatures. N M Law Rev 48:267 [Google Scholar]
- 49.Fiala C, Gemzell Danielsson K, Heikinheimo O, et al. (2016) Yes we can! Successful examples of disallowing “conscientious objection” in reproductive health care. Eur J Contracept Reprod Health Care Off J Eur Soc Contracept 21:201–206 . doi: 10.3109/13625187.2016.1138458 [DOI] [PubMed] [Google Scholar]
- 50.Lewis-Newby M, Wicclair M, Pope T, et al. (2015) An official American Thoracic Society policy statement: managing conscientious objections in intensive care medicine. Am J Respir Crit Care Med 191:219–227 . doi: 10.1164/rccm.201410-1916ST [DOI] [PubMed] [Google Scholar]
- 51.Stahl RY, Emanuel EJ (2017) Physicians, Not Conscripts — Conscientious Objection in Health Care. N Engl J Med 376:1380–1385 . doi: 10.1056/NEJMsb1612472 [DOI] [PubMed] [Google Scholar]
- 52.Wehkamp K-H, Naegler H (2017) The Commercialization of Patient-Related Decision Making in Hospitals. Dtsch Arzteblatt Int 114:797–804 . doi: 10.3238/arztebl.2017.0797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blum JM, Lynch WR, Coopersmith CM (2015) Clinical and Billing Review of Extracorporeal Membrane Oxygenation. Chest 147:1697–1703 . doi: 10.1378/chest.14-2954 [DOI] [PubMed] [Google Scholar]
- 54.Li X, Scales DC, Kavanagh BP (2018) Unproven and Expensive before Proven and Cheap: Extracorporeal Membrane Oxygenation versus Prone Position in Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med 197:991–993 . doi: 10.1164/rccm.201711-2216CP [DOI] [PubMed] [Google Scholar]
- 55.Schwarze ML, Brasel KJ, Mosenthal AC (2014) Beyond 30-day mortality: aligning surgical quality with outcomes that patients value. JAMA Surg 149:631–632 . doi: 10.1001/jamasurg.2013.5143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Walkey AJ, Barnato AE, Wiener RS, Nallamothu BK (2017) Accounting for Patient Preferences Regarding Life-Sustaining Treatment in Evaluations of Medical Effectiveness and Quality. Am J Respir Crit Care Med 196:958–963 . doi: 10.1164/rccm.201701-0165CP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nash IS (2015) Why Physicians Hate “Patient Satisfaction” but Shouldn’t. Ann Intern Med 163:792 . doi: 10.7326/M15-1087 [DOI] [PubMed] [Google Scholar]
- 58.Fenton JJ, Jerant AF, Bertakis KD, Franks P (2012) The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med 172:405–411 . doi: 10.1001/archinternmed.2011.1662 [DOI] [PubMed] [Google Scholar]
- 59.Zgierska A, Miller M, Rabago D (2012) Patient Satisfaction, Prescription Drug Abuse, and Potential Unintended Consequences. JAMA 307:1377–1378 . doi: 10.1001/jama.2012.419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Johnston C (2013) Patient satisfaction and its discontents. JAMA Intern Med 173:2025–2026 . doi: 10.1001/jamainternmed.2013.11356 [DOI] [PubMed] [Google Scholar]
- 61.Blumenthal-Barby JS, Krieger H (2015) Cognitive Biases and Heuristics in Medical Decision Making: A Critical Review Using a Systematic Search Strategy. Med Decis Making 35:539–557 . doi: 10.1177/0272989X14547740 [DOI] [PubMed] [Google Scholar]
- 62.Saposnik G, Redelmeier D, Ruff CC, Tobler PN (2016) Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak 16:138 . doi: 10.1186/s12911-016-0377-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hartog CS, Skupin H, Natanson C, et al. (2012) Systematic analysis of hydroxyethyl starch (HES) reviews: proliferation of low-quality reviews overwhelms the results of well-performed meta-analyses. Intensive Care Med 38:1258–1271 . doi: 10.1007/s00134-012-2614-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wood SF, Podrasky J, McMonagle MA, et al. (2017) Influence of pharmaceutical marketing on Medicare prescriptions in the District of Columbia. PloS One 12:e0186060 . doi: 10.1371/journal.pone.0186060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rodwin MA (1989) Physicians’ Conflicts of Interest. N Engl J Med 321:1405–1408 . doi: 10.1056/NEJM198911163212010 [DOI] [PubMed] [Google Scholar]
- 66.Dana J, Loewenstein G (2003) A Social Science Perspective on Gifts to Physicians From Industry. JAMA 290:252–255 . doi: 10.1001/jama.290.2.252 [DOI] [PubMed] [Google Scholar]
- 67.Wegwarth O, Gigerenzer G (2018) The Barrier to Informed Choice in Cancer Screening: Statistical Illiteracy in Physicians and Patients. Recent Results Cancer Res Fortschritte Krebsforsch Progres Dans Rech Sur Cancer 210:207–221 . doi: 10.1007/978-3-319-64310-6_13 [DOI] [PubMed] [Google Scholar]
- 68.Netzer G, Sullivan DR (2014) Recognizing, naming, and measuring a family intensive care unit syndrome. Ann Am Thorac Soc 11:435–441 . doi: 10.1513/AnnalsATS.201309-308OT [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cain DM, Loewenstein G, Moore DA (2005) The Dirt on Coming Clean: Perverse Effects of Disclosing Conflicts of Interest. J Leg Stud 34:1–25 . doi: 10.1086/426699 [DOI] [Google Scholar]
- 70.Loewenstein G, Sah S, Cain DM (2012) The Unintended Consequences of Conflict of Interest Disclosure. JAMA 307:669–670 . doi: 10.1001/jama.2012.154 [DOI] [PubMed] [Google Scholar]
- 71.Lo B (2012) The Future of Conflicts of Interest: A Call for Professional Standards. J Law Med Ethics 40:441–451 . doi: 10.1111/j.1748-720X.2012.00677.x [DOI] [PubMed] [Google Scholar]
- 72.Courtwright AM, Brackett S, Cadge W, et al. (2015) Experience with a hospital policy on not offering cardiopulmonary resuscitation when believed more harmful than beneficial. J Crit Care 30:173–177 . doi: 10.1016/j.jcrc.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 73.Olson LL (1998) Hospital nurses’ perceptions of the ethical climate of their work setting. Image-- J Nurs Scholarsh 30:345–349 [DOI] [PubMed] [Google Scholar]
- 74.Van den Bulcke B, Piers R, Jensen HI, et al. (2018) Ethical decision-making climate in the ICU: theoretical framework and validation of a self-assessment tool. BMJ Qual Saf doi: 10.1136/bmjqs-2017-007390 [DOI] [PubMed] [Google Scholar]
- 75.Benoit DD, Jensen HI, Malmgren J, et al. (2018) Outcome in patients perceived as receiving excessive care across different ethical climates: a prospective study in 68 intensive care units in Europe and the USA. Intensive Care Med 1–11 . doi: 10.1007/s00134-018-5231-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dzeng E, Colaianni A, Roland M, et al. (2015) Influence of institutional culture and policies on do-not-resuscitate decision making at the end of life. JAMA Intern Med 175:812–819 . doi: 10.1001/jamainternmed.2015.0295 [DOI] [PubMed] [Google Scholar]
- 77.Dzeng E, Dohan D, Curtis JR, et al. (2018) Homing in on the Social: System-Level Influences on Overly Aggressive Treatments at the End of Life. J Pain Symptom Manage 55:282–289.e1 . doi: 10.1016/j.jpainsymman.2017.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Barnato AE, Tate JA, Rodriguez KL, et al. (2012) Norms of decision making in the ICU: a case study of two academic medical centers at the extremes of end-of-life treatment intensity. Intensive Care Med 38:1886–1896 . doi: 10.1007/s00134-012-2661-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kelley AS, Bollens-Lund E, Covinsky KE, et al. (2017) Prospective Identification of Patients at Risk for Unwarranted Variation in Treatment. J Palliat Med 21:44–54 . doi: 10.1089/jpm.2017.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fields/ProPublica R (2010) “God Help You. You’re on Dialysis” The Atlantic [Google Scholar]
- 81.Rivière P (2003) Case notes on corruption Monde Dipl. [Google Scholar]
- 82.Creswell J, Abelson R, Sanger-Katz M (2017) The Company Behind Many Surprise Emergency Room Bills N. Y. Times [Google Scholar]
- 83.Ornstein C, Hixenbaugh M (2018) At St. Luke’s in Houston, Patients Suffer as a Renowned Heart Transplant Program Loses Its Luster In: ProPublica; https://www.propublica.org/article/baylor-st-lukes-medical-center-heart-transplants-houston-texas-patients-suffer. Accessed 16 May 2018 [Google Scholar]


