Abstract
Aggressive angiomyxoma is a rare tumour that frequently involves the perineal region with a high risk of local recurrence. This is a case report of a 24-year-old female patient with a genital prolapse. We performed a surgical treatment. Histological examination found an aggressive angiomyxoma. The tumour recurred 1 year after surgery. Long-term follow-up is necessary.
Keywords: Gynaecology, surgery, radiology, angiomyxoma, rectocele
Background/Introduction
First reported in 1983, aggressive angiomyxoma is a rare, slow growing mesenchymal tumour which is more often found in the pelvis or perineum areas.1 Very few extra-genital lesions have been reported.2 Its diagnosis remains difficult due to its non-specific clinical and radiological aspects. The risk involved is local recurrence; however, its peripheral extension remains exceptional.3 We describe a case of aggressive angiomyxoma, mimicking a genital prolapse in a young female patient.
Case report
We present the case of a female patient aged 24 years, with no particular past medical history noted and has never been pregnant. She presented with a perineal swelling in a standard gynaecology consultation. Physical examination showed signs of genital prolapse of ‘rectocele’ type. No other clinical signs or cutaneous lesions were noticed. The patient had an abdominal ultrasound scan with a pelvic magnetic resonance imaging (MRI) that showed a mass of the rectovaginal septum spread over 7 cm descending through the vagina while straining (Figure 1). The lesion was in hyposignal on T1 and T2 sequences.
Figure 1.
(a) Sagittal and (b) axial T2-weighted images. Slight enhancement in (c) sagittal and (d) axial MRI with contrast and FAT SAT. (e) During straining.
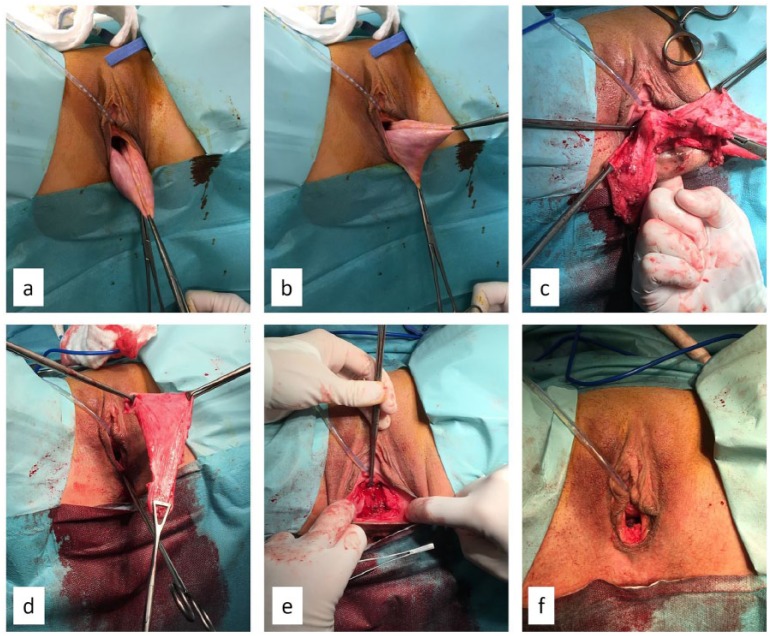
The patient accepted a surgical procedure. During the procedure, it was noticed that a tissular growth had developed at the cost of the vagina and had taken the appearance of a rectocele. Complete excision was done (Figure 2). The final histological analysis found an aggressive angiomyxoma with no trace of malignancy. The immunohistochemistry examination showed the positivity of the hormonal receptors (progesterone and oestrogens), the desmin and the actin-based smooth muscular cells of the CD34 and the negativity of the protein S100.
Figure 2.
Surgical procedure: (a and b) perineal mass seeming to be a rectocele, (c) posterior colpotomy, (d) resection by rectal shaving, (e) supplementary colpectomy and (f) final view.
Unfortunately, a relapse was noted at 1 year of follow-up for which a second surgery was attempted (Figure 3).
Figure 3.
(a and b) Normal MRI after 6 months and (c and d) recurrence after 1 year.
Discussion
Aggressive angiomyxoma is a rare tumour which is, most of the time, to be found in women of reproductive age with a peak incidence around the age of 40 years.3 The female/male ratio is 6:1.3 Clinically, it is seen as an asymptomatic or multisymptomatic growth found in the majority of cases in the pelvic-perineal region and genital tract.
Radiologically, it is a well-defined soft tissue tumour which displaces the organs around it rather than infiltrating them.4 Ultrasonography confirms the lesions to be cystic or hypoechogenic.1 Computed tomography (CT) scan is non-specific as it shows a hypodense lesion resembling a cyst. The MRI shows that the tumour is hypointense on T1-weighted (or isointense T1) and hyperintense on T2-weighted. After an intravenous injection of gadolinium, the lesion takes on a specific laminated appearance.4,5
Histologically, aggressive angiomyxoma is like a non-encased, but well-defined, macroscopic gelatinous tumour. A microscopic analysis of this tumour reveals a compound of randomized fusiform star-like orientated cells at the heart of a monocyte extracellular matrix containing numerous fibroblasts, myofibroblasts and veins. The immunohistochemistry analysis showed that the angioma has been found to be positive for vimentin, desmin, actin and the CD34 (implied in the endothelial differential) and negative for S100 protein (marker for Schwann cells, chondrocytes, adipocytes, and melanocytes cells) and also CD68 (marker for histiocytic cells). The oestrogen and progesterone receptors are often shown.6 These characteristics are non-specific; nevertheless, they help with the diagnosis of aggressive angiomyxoma.
Surgical excision is the gold standard in the treatment of this pathology and allows histological analysis.6 Other therapies have been tried as stated in literature such as hormonotherapy, chemotherapy or even embolization, however, without any noticeable efficacy.2,3 Rhomberg et al.7 have reported that adjuvant radiotherapy controlled the spread of the disease in a female patient who had a fourth recurrence of her tumour.
Morbidity and mortality of the aggressive angiomyxoma, is above all, linked to its localisation. In the majority of cases, it has a good prognosis.8 No more than two cases of metastases have been described in the literature.8 The main problem with this disease is the high risk of local recurrence. In a retrospective study by Chan et al., 73 cases of aggressive angiomyxoma were examined and treated by surgical resection with a rate of recurrence being reported at 47% of which a total of 73% occurred in the 3 years following surgery.9 Furthermore, no significant differences between the recurrence rates between positive margin resections and healthy margins of resection were reported. Incomplete resection may be acceptable in the treatment of aggressive angiomyxoma.
Conclusion
This case report reveals the difficulty of diagnosis in aggressive angiomyxoma which is a very rare tumour. This tumour should be considered in the case of a pelvic or perineal mass which is unexplained by the patient’s past medical history, is paucisymptomatic and has a whorled pattern on MRI after gadolinium. Patients should be warned of the high risk of recurrence and the necessity of long-term follow-up after surgical removal.
Footnotes
Authors’ note: Jean-Philippe Lucot is now affiliated with Lille Catholic Hospitals, Department of Gynecology Obstetrics, Lille Catholic University, Lille, France.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Informed consent was obtained to publish the patient information and images.
ORCID iD: Clémence Raptin  https://orcid.org/0000-0002-5953-7924
https://orcid.org/0000-0002-5953-7924
References
- 1. Umranikar S, Ubee S, Williams G. Aggressive angiomyxoma of the perineum: a rare presentation in a male with 4 years follow up. J Surg Case Rep 2017; 2017(8): rjx086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang Z, Liu Y, Yang L, et al. Maxillary aggressive angiomyxoma showing ineffective to radiotherapy: a rare case report and review of literature. Int J Clin Exp Pathol 2015; 8(1): 1063–1067. [PMC free article] [PubMed] [Google Scholar]
- 3. Sutton BJ, Laudadio J. Aggressive angiomyxoma. Arch Pathol Lab Med 2012; 136(2): 217–221. [DOI] [PubMed] [Google Scholar]
- 4. Brunelle S, Bertucci F, Chetaille B, et al. Aggressive angiomyxoma with diffusion-weighted magnetic resonance imaging and dynamic contrast enhancement: a case report and review of the literature. Case Rep Oncol 2013; 6(2): 373–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Surabhi VR, Garg N, Frumovitz M, et al. Aggressive angiomyxomas: a comprehensive imaging review with clinical and histopathologic correlation. AJR Am J Roentgenol 2014; 202(6): 1171–1178. [DOI] [PubMed] [Google Scholar]
- 6. Miguez Gonzalez J, Dominguez Oronoz R, Lozano Arranz P, et al. Aggressive angiomyxoma: imaging findings in 3 cases with clinicopathological correlation and review of the literature. J Comput Assist Tomogr 2015; 39(6): 914–921. [DOI] [PubMed] [Google Scholar]
- 7. Rhomberg W, Jasarevic Z, Alton R, et al. Aggressive angiomyxoma: irradiation for recurrent disease. Strahlenther Onkol 2000; 176(7): 324–326. [DOI] [PubMed] [Google Scholar]
- 8. Blandamura S, Cruz J, Faure Vergara L, et al. Aggressive angiomyxoma: a second case of metastasis with patient’s death. Hum Pathol 2003; 34(10): 1072–1074. [DOI] [PubMed] [Google Scholar]
- 9. Chan YM, Hon E, Ngai SW, et al. Aggressive angiomyxoma in females: is radical resection the only option. Acta Obstet Gynecol Scand 2000; 79(3): 216–220. [PubMed] [Google Scholar]