Abstract
Objectives:
To determine if levels of neighbourhood poverty and neighbourhood antisocial behaviour modify associations between household poverty and child and youth mental health problems.
Methods:
Data come from the 2014 Ontario Child Health Study—a provincially representative survey of 6537 families with 10,802 four- to 17-year-olds. Multivariate multilevel modelling was used to test if neighbourhood poverty and antisocial behaviour interact with household poverty to modify associations with children’s externalizing and internalizing problems based on parent assessments of children (4- to 17-year-olds) and self-assessments of youth (12- to 17-year-olds).
Results:
Based on parent assessments, neighbourhood poverty, and antisocial behaviour modified associations between household poverty and children’s mental health problems. Among children living in households below the poverty line, levels of mental health problems were 1) lower when living in neighbourhoods with higher concentrations of poverty and 2) higher when living in neighbourhoods with more antisocial behaviour. These associations were stronger for externalizing versus internalizing problems when conditional on antisocial behaviour and generalized only to youth-assessed externalizing problems.
Conclusion:
The lower levels of externalizing problems reported among children living in poor households in low-income neighbourhoods identify potential challenges with integrating poorer households into more affluent neighbourhoods. More important, children living in poor households located in neighbourhoods exhibiting more antisocial behaviour are at dramatically higher risk for mental health problems. Reducing levels of neighbourhood antisocial behaviour could have large mental health benefits, particularly among poor children.
Keywords: child, youth, mental disorder, Ontario, neighbourhood effects, poverty, antisocial behaviour
Abstract
Objectifs :
Déterminer si les niveaux de pauvreté du quartier et du comportement antisocial du quartier modifient les associations entre la pauvreté des ménages et les problèmes de santé mentale des enfants et des adolescents.
Méthode :
Les données proviennent de l’Étude sur la santé des jeunes Ontariens 2014, une étude représentative à l’échelle provinciale de 6 537 familles comptant 10 802 enfants et adolescents de 4 à 17 ans. Une modélisation multivariée à plusieurs niveaux a été utilisée pour vérifier si la pauvreté et le comportement antisocial du quartier interagissent avec la pauvreté des ménages pour modifier les associations avec les problèmes d’externalisation et d’internalisation des enfants, selon les évaluations des enfants par les parents (pour les 4 à 17 ans) et les auto-évaluations des adolescents (les 12 à 17 ans).
Résultats :
Selon les évaluations des parents, la pauvreté et le comportement antisocial du quartier modifiaient les associations entre la pauvreté des ménages et les problèmes de santé mentale des enfants. Chez les enfants vivant dans un ménage sous le seuil de la pauvreté, les niveaux des problèmes de santé mentale étaient (1) plus faibles quand ils vivaient dans des quartiers à plus fortes concentrations de pauvreté et (2) plus élevés quand ils vivaient dans des quartiers où le comportement était plus antisocial. Ces associations étaient plus marquées pour les problèmes d’externalisation plutôt que d’internalisation, lorsqu’elles étaient tributaires du comportement antisocial et qu’elles n’étaient généralisées qu’aux problèmes d’externalisation auto-évalués par les adolescents.
Conclusion :
Les faibles niveaux des problèmes d’externalisation déclarés chez les enfants vivant dans des ménages pauvres dans des quartiers à faible revenu posent des problèmes potentiels quant à l’intégration des ménages pauvres dans des quartiers plus aisés. À plus forte raison, les enfants vivant dans des ménages pauvres situés dans des quartiers affichant un comportement plus antisocial sont à risque radicalement plus élevé de problèmes de santé mentale. Réduire les niveaux de comportement antisocial d’un quartier pourrait avoir d’importants bénéfices de santé mentale, particulièrement chez les enfants pauvres.
Levels of child (4- to 17-year-olds) and youth (12- to 17-year-olds) mental health problems are high in Ontario1 and have increased among 4- to 11-year-olds from 30 years ago,2 reflecting secular trends observed in many countries.3,4 The resources available to identify and treat children with mental health problems case-by-case are too limited to alter children’s mental health in the general population. Prevention initiatives aimed at all children (universal programs) or groups of children at elevated risk for mental health problems (targeted programs) complement treatment efforts by attempting to reduce the number of children in need of specialized services.5 Preventing the adverse health effects of exposure to poverty on children depends on identifying variables associated with individual children, their families, or neighbourhoods, which can be manipulated to maintain or improve child health.
The positive association between poverty and children’s mental health problems is highly variable, with odds ratios ranging from 1.18 to 3.34.6 In the 2014 Ontario Child Health Study (OCHS), the association between household poverty and one or more mental disorders was weak,1 reflecting a possible attenuation of the poverty gradient between the 1983 and 2014 OCHS.2 This led us to examine if the relationship between household poverty and children’s mental health problems might be modified in the presence of 2 neighbourhood variables—neighbourhood poverty and antisocial behaviour. The hypothesis is that the disadvantages associated with these 2 neighbourhood characteristics will interact with the psychosocial vulnerabilities associated with household poverty to modify its association with children’s mental health problems. The hypotheses linking these neighbourhood characteristics with household poverty are situated in stress-process theory7 and the recognition that neighbourhoods provide important contexts for how the stress process unfolds.8
Neighbourhood Poverty
The joint effects of neighbourhood and household poverty are subject to debate. Theories of relative disadvantage9,10 predict that living alongside more affluent neighbours will have adverse effects on the health and functioning of children in poor households through psychosocial pathways (e.g., unfavourable social comparisons, threats to self-esteem and social status, marginalization, inability to compete for resources). These adverse effects, attributable to income inequality in neighbourhoods, have been identified recently in boys11 and boys and girls.12
Theories of compound disadvantage9 predict that the absence of social networks and institutional resources associated with poor neighbourhoods13 will magnify the disadvantages for children living in poor households. This prediction is supported historically by studies in Europe and North America and is responsible for policies and programs aimed at increasing neighbourhood socioeconomic heterogeneity or “social mix.”14 A singular influence on these policies and programs has been Wilson’s 1987 book, The Truly Disadvantaged.15 Wilson raised concern about compound disadvantage associated with selected housing projects and neighbourhoods in the United States that were characterized by intense poverty, inadequate housing, criminality, social isolation, and the absence of institutional resources. In the general population, this portrait of disadvantage will apply to some but not all neighbourhoods characterized as economically poor. This leaves open questions about the effects of relative versus compound disadvantage when household and neighbourhood poverty are examined in the general population.
Neighbourhood Antisocial Behaviour
Neighbourhood poverty is associated with a number of other neighbourhood characteristics linked with children’s mental health problems, including ethnic heterogeneity, residential instability, and violence.16–18 Based on available evidence, it is arguable that the personal experience of household members with neighbourhood antisocial behaviour (e.g., being subject to personal insult, violence, or theft) or simply living in neighbourhoods with high levels of antisocial behaviour could be a potent variable in the mix of neighbourhood influences on children’s mental health.19 Exposure to neighbourhood antisocial behaviour could 1) have indirect effects on children’s mental health mediated through maladaptive parent and family processes20; 2) have direct adverse effects on children’s mental health induced by fear, stress, and enduring concerns for safety21; or 3) create a normative behavioural context that contributes to maladaptive social learning and affiliation with deviant peers.20
A number of studies have examined the moderating effects of neighbourhood characteristics on associations between family variables and children’s mental health. Few, if any, have considered the interaction between neighbourhood antisocial behaviour and household poverty.22 Two studies reported that neighbourhood adversity (physical/social disorder, fear of retaliation/victimization, dangerousness) intensified the positive association between family adversity (multiple social/economic characteristics) and children’s emotional and behavioural problems.23,24 The implications were that levels of neighbourhood antisocial behaviour could modify the association between household poverty and children’s mental health problems.
Indicators of socioeconomic disadvantage are believed to exhibit general rather than specific associations with different child psychiatric disorders.25 Although it is rare for studies to conduct formal empirical tests of these differences, a recent investigation reported stronger associations between poverty and externalizing versus internalizing problems.26 This led us to predict that interactions between household poverty and the 2 neighbourhood variables being studied will be stronger for externalizing versus internalizing problems. Evidence of substantial disagreement among informant assessments of children’s mental health problems27 led us to test if the results based on parent assessments extended to youth assessments. Although there is no convincing theoretical or empirical basis to expect differential effects for boys versus girls, we conducted post hoc tests because it is an important question.
The objectives of this study were to determine if neighbourhood poverty and antisocial behaviour modify associations between household poverty and children’s mental health problems. The study addresses 3 questions: Q1) Do neighbourhood poverty and antisocial behaviour modify associations between household poverty and children’s externalizing or internalizing problems? Q2) Are the observed interactions stronger for externalizing versus internalizing problems? and Q3) Are the results for parent-rated externalizing and internalizing problems of children generalizable to youth ratings?
Methods
The 2014 OCHS was a province-wide, cross-sectional, epidemiologic study of child health and mental disorder. A probability sample of 6,537 households (50.8% response) with 10,802 four- to 17-year-olds participated. The sampling frame was the 2014 Canadian Child Tax Benefit file. Households were selected based on a complex 3-stage survey design that involved cluster sampling of residential areas and stratification by residency (urban, rural) and income (areas and households cross-classified by 3 levels of income: <20th, 20th to 80th, and >80th percentiles). Detailed accounts of the survey design, content, training, and data collection are available elsewhere.28,29
Concepts and Measures
Externalizing and internalizing problems
The dependent variables were dimensional measures of children’s mental health problems defined as externalizing and internalizing problems assessed by the person most knowledgeable (PMK) (87% mothers) and youth aged 12 to 17 years completing the OCHS Emotional Behavioural Scales (OCHS-EBS). The OCHS-EBS are dimensional measures of selected DSM-5 disorders that we grouped to measure externalizing problems (attention-deficit hyperactivity disorder, oppositional-defiant disorder, and conduct disorder—25 items) and internalizing problems (major depressive disorder, generalized anxiety disorder, separation anxiety disorder, and social anxiety disorder—27 items). The OCHS-EBS were presented in a self-administered checklist questionnaire with response options of 0 = never or not true, 1 = sometimes or somewhat true, and 2 = often or very true. Items were summed to generate scale scores. The internal consistency and test-retest reliabilities of the scales exceed 0.80 for the externalizing and internalizing scales completed by the PMK or youth. Detailed information on the evolution, development, and psychometric properties of the scales is available.30,31
Control variables
Household information was collected from the PMK based on standard questions developed by Statistics Canada for the Census and population surveys. At the child and family levels, the variables include child age in years, sex (0 = female; 1 = male), residency (0 = large urban; 1 = small-medium urban or rural), years living in the neighbourhood, highest level of education attained by either parent (grouped from 1 = grade 8 or lower to 9 = university degree above the Bachelor level) and treated as a continuous measure, and family immigrant status (0 = parent(s) born in Canada; 1 = one or both parents born outside Canada). Neighbourhoods are represented by census tracts or dissemination areas. Percentage of individuals born outside of Canada was measured based on the 2011 Census.
Poverty
Household poverty was measured as household income below the low-income measure (LIM) (0 = >LIM; 1 = ≤LIM) and neighbourhood poverty, as the percentage of households below the LIM based on the 2011 Census.
Antisocial behaviour
Antisocial behaviour is a cumulative risk variable represented by a count of positive responses provided by the PMK to 4 questions. The questions all begin with: “While you have lived in this neighbourhood…”; they ask about the personal experience of any household member to 1) assault, 2) repeated verbal insult or disrespect, 3) theft from household property, or 4) household break-in. PMKs were able to check “not applicable” to these questions, which we treated as missing: 0 missing (81.3%), 1 (10.0%), 2 (1.5%), 3 (0.6%), and 4 (6.7%). If at least 1 item was checked, the remaining items were imputed based on the nonmissing antisocial items and 10 other Census-derived and study variables (e.g., Census: large urban, small urban, rural; interviewer: neighbourhood problems; PMK ratings: neighbourhood safety for children). Positive responses were summed to form a count from 0 to 4. Test-retest reliability was r = 0.72. To obtain a neighbourhood measure of antisocial behaviour, the PMK scale scores were aggregated to the neighbourhood level and averaged.
Analysis
Data were analyzed using multivariate multilevel regression in which variability in each outcome is explained by an overall average (intercept), a set of predictor variables (fixed effects), and 3 residual terms (random effects). The residual term quantified unexplained variation between children within families (level 1), between families within neighbourhoods (level 2), and between neighbourhoods (level 3). Statistics Canada sampling weights based on the probability of being selected and participating in the study were applied separately to children (level 1) to represent the probability of each child being selected within a specific household and to households (level 2) to represent the joint probability of each household and area being selected. The regression models in the analyses were estimated using full information maximum likelihood (FIML) with robust standard errors in MPlus 7.032.32,33 FIML estimates parameters on the basis of the available complete data as well as the implied values of the missing data given the observed data. Study participants with 1 or more missed responses (1043 of 10,802 parents and 676 of 4428 youth) versus complete responses differed on residency in urban areas (8.6% versus 5.8%), household poverty (9.6% versus 5.9%), and exposure to neighbourhood antisocial behaviour (0.28 versus 0.49). To evaluate the impact of missed responses, comparator models were implemented based on complete case analysis for parent (n = 9759) and youth (n = 3752) assessed problems.
The following variables were grand-mean centred (rescaled so their mean values were 0): child age in years, parental education, household member’s experience of neighbourhood antisocial behaviour, neighbourhood poverty, percentage of individuals born outside Canada, and average levels of neighbourhood antisocial behaviour. Centering facilitated the interpretation of main effects that comprise the interaction terms and the intercept.
To answer Q1, we tested for cross-level interactions between household poverty, neighbourhood poverty, and average levels of neighbourhood antisocial behaviour. The model included the control variables as well as household poverty, household member’s experience of neighbourhood antisocial behaviour, neighbourhood poverty, and average levels of neighbourhood antisocial behaviour. To answer Q2, we used the Wald χ2 to test for statistically significant differences in the cross-level interactions involving children’s externalizing and internalizing problems. To answer Q3, we repeated the analyses for youth ratings of externalizing and internalizing problems. Because specific hypotheses are being tested in the analyses, nominal P values are not vulnerable to inflation by multiple testing.
Results
Table 1 shows the sample characteristics. There are several large, statistically significant differences between families in households below and above the LIM. For example, in households below the LIM, there were higher levels of parent-reported externalizing problems (6.4 versus 5.5), lower levels of parental education (6.0 versus 7.0), and a higher percentage of immigrant families (58.2% versus 41.7%). As expected, a higher percentage of households below the LIM was located in areas with higher percentages of other households below the LIM (17.0% versus 12.3%).
Table 1.
Sample Characteristics.
| Characteristic | n | Families in Households above the LIM | Families in Households below the LIM | Total | F Statistic (P Value) |
|---|---|---|---|---|---|
| Children/youth | |||||
| Male, % (SE) | 10,802 | 51.4 (1.03) | 51.7 (1.39) | 51.3 (0.87) | 0.02 (0.882) |
| Age in years, mean (SE) | 10,802 | 10.7 (0.08) | 10.5 (0.11) | 10.6 (0.07) | 1.94 (0.164) |
| Parent report: externalizing problems, mean (SE) | 10,643 | 5.5 (0.12) | 6.4 (0.19) | 5.6 (0.11) | 15.6 (<0.001) |
| Parent report: internalizing problems, mean (SE) | 10,614 | 5.7 (0.14) | 6.2 (0.20) | 5.7 (0.11) | 4.66 (0.031) |
| Youth report: externalizing problems, mean (SE) | 3981 | 6.8 (0.19) | 6.9 (0.27) | 6.8 (0.16) | 0.05 (0.819) |
| Youth report: internalizing problems, mean (SE) | 3972 | 11.3 (0.33) | 10.7 (0.42) | 11.1 (0.28) | 1.25 (0.263) |
| Households | |||||
| Children, mean (SE) | 6537 | 1.6 (0.02) | 1.7 (0.03) | 1.6 (0.01) | 14.43 (0.001) |
| Households below LIM, % (SE) | 6386 | 17.6 (0.65) | |||
| Highest level of parent education, mean (SE) | 6264 | 7.0 (0.04) | 6.0 (0.07) | 6.8 (0.04) | 134.7 (<0.001) |
| One or both parents born outside Canada, % (SE) | 6371 | 41.7 (1.29) | 58.2 (1.81) | 44.6 (1.11) | 53.1 (<0.001) |
| Exposure to antisocial behaviour, mean (SE) | 6537 | 0.44 (0.02) | 0.48 (0.03) | 0.44 (0.02) | 1.31 (0.252) |
| Years living in neighbourhood, mean (SE) | 6537 | 10.1 (0.20) | 8.3 (0.31) | 9.8 (0.17) | 22.8 (<0.001) |
| Neighbourhood areas | |||||
| Households below LIM, % (SE) | 484 | 12.3 (0.01) | 17.0 (0.02) | 13.3 (0.01) | 206.04 (<0.001) |
| Small-medium urban or rural residency, % (SE) | 484 | 30.3 (0.04) | 22.4 (0.09) | 28.6 (0.04) | 31.83 (<0.001) |
| Individuals born outside Canada, % (SE) | 484 | 28.3 (0.02) | 33.6 (0.05) | 29.4 (0.02) | 55.65 (<0.001) |
| Levels of antisocial behaviour, mean (SE) | 484 | 0.48 (0.00) | 0.49 (0.00) | 0.48 (0.00) | 0.68 (0.411) |
LIM, low-income measure.
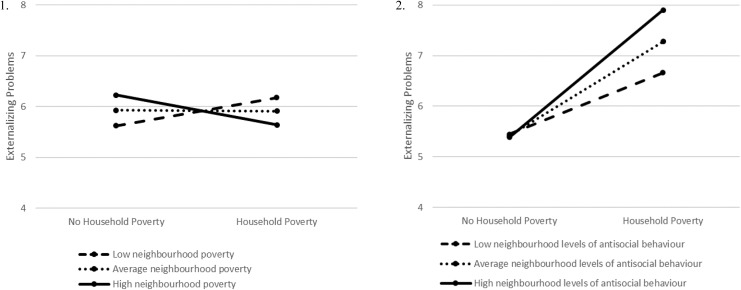
Table 2 shows the multivariate multilevel model results for parent- and youth-assessed externalizing and internalizing problems. Household member’s experience of neighbourhood antisocial behaviour exhibits strong, statistically significant associations with parent-assessed externalizing (1.17) and internalizing (0.84) problems. The main effect associations between households below the LIM and externalizing (0.86) and internalizing (0.88) problems do not reach statistical significance (0.05 < P < 0.10). However, this variable is involved in significant cross-level interactions. Levels of externalizing (–0.66) and internalizing (–0.54) problems are lower among children living in households below the LIM located in neighbourhoods with higher rates of poverty. At the same time, levels of externalizing (2.09) problems are higher among children living in households below the LIM located in neighbourhoods with elevated levels of antisocial behaviour. At the neighbourhood level, neighbourhood poverty exhibits positive, statistically significant associations with externalizing (0.35) and internalizing (0.34) problems. Because household poverty is controlled in the model, these coefficients apply to children living in households above the LIM. Accordingly, levels of externalizing and internalizing problems among children in more affluent households are higher when residing in poorer neighbourhoods. These interactions are illustrated for externalizing behaviour in Figure 1 and address Q1.
Table 2.
Fixed-Effects and Random-Effects Variance Components for Multivariate Multilevel Models of Parent and Youth Externalizing and Internalizing Problems.a
| Parent (n = 10,802) | Youth (n = 4428) | |||
|---|---|---|---|---|
| Externalizing | Internalizing | Externalizing | Internalizing | |
| Fixed effects | ||||
| Intercept | 5.46 (0.48) * | 6.01 (0.54) *D | 7.26 (0.62) * | 12.94 (1.03) *D |
| Level 1: Children/youth | ||||
| Male | 1.56 (0.15) * | –0.05 (0.15) D | 0.43 (0.23) | –3.37 (0.38) *D |
| Age | –0.07 (0.02) * | 0.12 (0.02) *D | 0.21 (0.07) * | 0.26 (0.11) * |
| Level 2: HHLDs | ||||
| Years living in neighbourhood | –0.04 (0.01) * | –0.04 (0.01) * | –0.03 (0.02) | –0.05 (0.03) * |
| Highest education level | –0.06 (0.06) | 0.01 (0.06) D | –0.08 (0.07) | 0.10 (0.12) D |
| One or both parents born outside Canada | –0.95 (0.24) * | –0.77 (0.24) * | –0.80 (0.28) * | –0.95 (0.48) * |
| HHLDs below LIM | 0.86 (0.46) | 0.88 (0.48) | 0.07 (0.48) | –0.23 (0.74) |
| Exposure to antisocial behaviour | 1.17 (0.16) * | 0.84 (0.16) *D | 0.65 (0.19) * | 0.32 (0.28) D |
| Level 3: Neighbourhoods | ||||
| Small-medium urban or rural | 0.19 (0.28) | 0.12 (0.32) | 0.47 (0.41) | –0.02 (0.64) |
| Percentage of individuals born outside Canada | –0.19 (0.08) * | –0.27 (0.08) * | –0.11 (0.12) | –0.37 (0.18) * |
| Percentage of HHLDs below LIM | 0.35 (0.14) * | 0.34 (0.15) * | 0.29 (0.22) | 0.28 (0.33) |
| Levels of antisocial behaviour | –0.09 (0.43) | –0.31 (0.45) | –0.27 (0.55) | –0.02 (0.97) |
| Cross-level interactions | ||||
| HHLD poverty × neighbourhood poverty | –0.66 (0.21) * | –0.54 (0.20) * | –0.41 (0.24) | –0.24 (0.35) |
| HHLD poverty × neighbourhood antisocial behaviour | 2.09 (0.73) * | 1.32 (0.75) D | 1.78 (0.76) * | 1.82 (1.36) |
| Random effects | ||||
| Level 1: children/youth | 21.67 (1.22) * | 21.38 (1.13) * | 26.07 (0.88) * | 64.04 (1.92) *D |
| Level 2: households | 13.70 (1.23) * | 16.65 (1.30) *D | 3.16 (0.63) * | 7.57 (1.25) *D |
| Level 3: neighbourhoods | 1.96 (0.31) * | 2.38 (0.44) * | 3.46 (0.70) * | 9.34 (1.65) *D |
| AIC | 237,323.543 | 108,156.287 | ||
| Sample size adjusted BIC | 237,160.748 | 107,992.401 | ||
| Parent (n = 9759) | Youth (n = 3752) | |||
| Cross-level interactions (complete case analysis) | ||||
| HHLD poverty × neighbourhood poverty | –0.62 (0.22) * | –0.41 (0.21) * | –0.53 (0.28) | –0.05 (0.44) |
| HHLD poverty × neighbourhood antisocial behaviour | 2.82 (0.78) * | 1.75 (0.77) * | 2.33 (0.86) * | 1.71 (1.65) |
AIC, Akaike information criterion model fit statistic; BIC, Bayesian information criterion model fit statistic; HHLD, household; LIM, low-income measure.
aThe letter “D” identifies coefficients that differ in their associations with externalizing versus internalizing problems at P < 0.05.
*Significant at P < 0.05.
Figure 1.
Graph 1 shows the interaction between household poverty, neighbourhood poverty, and externalizing problems. Graph 2 shows the interaction between household poverty, levels of neighbourhood antisocial behaviour, and externalizing problems.
In Table 2, the strength of association between household member’s experience of neighbourhood antisocial behaviour and parent-assessed children’s mental health problems is stronger for externalizing (1.17) versus internalizing (0.84) problems, as is the cross-level interaction between household poverty and neighbourhood levels of antisocial behaviour (2.09 versus 1.32), addressing Q2.
The results associated with parent assessments in Table 2 are replicated partially for youth-assessed externalizing problems, addressing Q3. The association between household member’s exposure to neighbourhood antisocial behaviour is statistically significant and stronger for youth-assessed externalizing (0.65) versus internalizing (0.32) problems. The cross-level interaction involving households below the LIM, neighbourhood exposure to antisocial behaviour, and youth externalizing (1.78) problems is consistent with the parent. Post hoc statistical tests revealed no male-female differences in the cross-level interactions involving household poverty and the 2 neighbourhood variables.
Using complete case analysis would have produced similar results. This is illustrated by the cross-level interactions reported at the bottom of Table 2. In general, the coefficients and their standard errors for complete case analysis were slightly larger than the estimates generated using FIML. The difference was large enough in the complete case analysis to render significant the cross-level interaction between household poverty, neighbourhood antisocial behaviour, and parent-reported internalizing problems (1.75).
Discussion
This study indicates that neighbourhood poverty and neighbourhood antisocial behaviour modify the associations between household poverty and children’s externalizing problems—an effect that generalizes to youth self-assessments. However, these effects run in opposite directions. In neighbourhoods with higher concentrations of poverty, children living in households below the LIM exhibit lower levels of children’s mental health problems while children living in households above the LIM exhibit higher levels of mental health problems. Consistent with theories of relative disadvantage, this pattern of response indicates generally that person-context fit may have mental health implications for children in households classified below or above the LIM. These findings align with Wilkinson’s theory that income inequality or relative income differences among people contribute to negative psychosocial processes adversely affecting everyone, not just those experiencing income disadvantage.
In contrast, the main effect for household member’s experience of neighbourhood antisocial behaviour exhibits a strong statistically significant positive association with children’s externalizing problems, indicating that externalizing problems are elevated among all children exposed to neighbourhood antisocial behaviour. Moreover, the cross-level interaction between neighbourhood antisocial behaviour and household poverty indicates that children living in households below the LIM exhibit substantially higher levels of externalizing problems in the presence of high levels of neighbourhood antisocial behaviour.
Income Poverty and Person-Context Fit
Since the 1970s, housing policies in Canada have attempted to address the adverse effects of poverty by providing lower-income families with the opportunity to live in communities with households of greater economic means.34 Such communities are expected to provide positive role models, supportive networks, safe environments, and institutional resources that will benefit new residents with less income. Our study, consistent with recent reports,11,12 suggests that socioeconomic mix may have adverse effects on the mental health of children from both poor and nonpoor families. In other words, children in poor households are at lower risk living in poorer neighbourhoods (or higher risk living in more affluent neighbourhoods) while the reverse is true for children in more affluent households. Achieving the benefits of socioeconomic mix may require additional strategies aimed at social integration to overcome differences in the attitudes, behaviour, and personal resources of families with different economic backgrounds.
The advantages and challenges of person-context fit are not restricted to the income characteristics of residents. For example, the psychosocial advantages associated with good person-context fit are a lesson well learned from studies of neighbourhood settlement practices among immigrants to Canada.35 Levels of mental health problems among immigrant children decrease as the neighbourhood immigrant concentration increases, in contrast to nonimmigrant children whose levels of mental health problems increase. In Canada, little is known empirically about the precise social mechanisms underlying good person-context fit and the types of interventions that support healthy adjustment and acceptance in communities. Furthermore, there may be optimal levels of social mix or thresholds in the composition of neighbourhoods (e.g., the percent concentration of immigrant families or families with high or low income) where positive social engagement gives way to forces of social segregation. We need to address these important research questions if the ideals of socioeconomic mix are to be realized.
Income Poverty and Neighbourhood Levels of Antisocial Behaviour
Household exposure to concentrated poverty is substantially lower in Canada compared to the United States because of less income segregation, lower crime intensity, and the increased presence of poor but high-functioning immigrants.36 As a result, neighbourhoods characterized as poor vary substantially in their ability to support healthy development. However, as indicated in our study, specific neighbourhood variables can modify associations between household poverty and children’s mental health. Neighbourhood antisocial behaviour is one such variable. In neighbourhoods characterized by high levels of antisocial behaviour, there is a very large extra burden for children in households classified as poor as these children are also at much higher risk for externalizing problems.
Our measure of antisocial behaviour includes indicators of criminal behaviour (assault) and incivility (verbal insult). Personal safety and security are basic human needs that can be met through a variety of initiatives and programs. For example, the City of Toronto, concerned in 2005 about the negative impact of increasing income segregation and concentrated disadvantage in neighbourhoods, published a policy document called Toronto 2020.37 Included among the many strategies to address these concerns is a commitment to “Make our neighbourhoods safer.”
If we want to improve the mental health of children, our study suggests that reducing antisocial behaviour in neighbourhoods should be extremely high on the policy agenda, particularly those living in households below the poverty line.
There are 2 primary limitations of this study: 1) the cross-sectional design, which provides no perspective on the temporal relationships among the variables investigated, and 2) the self-selection of families into neighbourhoods. The latter has triggered substantial debate over the correct way to distinguish between contextual and compositional effects.38 We have taken the view that children are born without choice into “inceptive environments,”39 which are family and neighbourhood contexts that often persist over the early life course and may modify each other in ways supportive or unsupportive to child mental health. The strength of this study lies in its large-scale use of cluster sampling to facilitate the examination of contextual influences and the stratification of neighbourhoods and households by income to better represent income heterogeneity among families and neighbourhoods in the population.
Conclusion
The study has shown that externalizing behaviour problems are lower among children living in neighbourhoods where family incomes are similar. This suggests some mental health benefits associated with good person-context fit. We also found that exposure of household members to antisocial behaviour is associated strongly with children’s mental health problems, irrespective of household income. However, there is a very large extra mental health burden for children in households classified as poor when located in neighbourhoods with high levels of antisocial behaviour. Reducing exposure to antisocial behaviour in neighbourhoods is important for all children and could yield special benefits for children living in households below the poverty line.
Acknowledgements
The authors would like to thank Dr. James Carpenter and Dr. Paul Allison for advice regarding handling missing data and Nancy Pyette for technical assistance with editing and proofreading the manuscript.
Data Access: Data access available through Statistics Canada Research Data Centres.
Declaration of Conflicting Interests: The primary authors (MB, KG, LD, LW, and JC) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by research operating grant 125941 from the Canadian Institutes of Health Research (CIHR), Health Services Research Grant 8-42298 from the Ontario Ministry of Health and Long-Term Care (MOHLTC), and funding from MOHLTC, the Ontario Ministry of Children and Youth Services, and the Ontario Ministry of Education. Dr. Boyle was supported by CIHR Canada Research Chair in the Social Determinants of Child Health and Dr. Georgiades by the David R. (Dan) Offord Chair in Child Studies.
ORCID iD: Laura Duncan, MA  https://orcid.org/0000-0001-7120-6629
https://orcid.org/0000-0001-7120-6629
References
- 1. Georgiades K, Duncan L, Wang L, et al. Six-month prevalence of mental disorders and service contacts among children and youth in Ontario: evidence from the 2014 Ontario Child Health Study. Can J Psychiatry. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Comeau J, Georgiades K, Wang L, et al. Changes in the prevalence of child mental disorders and perceived need for professional help between 1983 and 2014: evidence from the Ontario Child Health Study. Can J Psychiatry. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bor W, Dean AJ, Najman J, et al. Are child and adolescent mental health problems increasing in the 21st century? A systematic review. Aust N Z J Psychiatry. 2014;48(7):606–616. [DOI] [PubMed] [Google Scholar]
- 4. Collishaw S, Goodman R, Ford T, et al. How far are associations between child, family and community factors and child psychopathology informant-specific and informant-general? J Child Psychol Psychiatry. 2009;50(5):571–580. [DOI] [PubMed] [Google Scholar]
- 5. Waddell C, McEwan K, Shepherd CA, et al. A public health strategy to improve the mental health of Canadian children. Can J Psychiatry. 2005;50(4):226–233. [DOI] [PubMed] [Google Scholar]
- 6. Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. [DOI] [PubMed] [Google Scholar]
- 7. Pearlin LI, Lieberman M, Menaghan E, et al. The stress process. J Health Soc Behav. 1981;22(4):337–356. [PubMed] [Google Scholar]
- 8. Aneshensel CS. Neighborhood as a social context of the stress process In: Avison WR, Aneshensel CS, Schieman S, Wheaton B, eds. Advances in the Conceptualization of the Stress Process: Essays in Honor of Leonard I. Pearlin. New York (NY): Springer; 2010:35–52. [Google Scholar]
- 9. Jencks C, Mayer S. The social consequences of growing up in a poor neighborhood In: Lynn LE, McGeary MFH, eds. Inner-City Poverty in the United States. Washington (DC): National Academies Press; 1990:111–186. [Google Scholar]
- 10. Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago (IL): University of Chicago Press; 1987. [Google Scholar]
- 11. Odgers CL, Donley S, Caspi A, et al. Living alongside more affluent neighbors predicts greater involvement in antisocial behavior among low-income boys. J Child Psychol Psychiatry. 2015;56(1):1055–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sorhagen NS, Wurster TJ. Income within context: relative income matters for adolescent social satisfaction and mental health. J Child Psychol Psychiatry. 2017;58(6):736–743. [DOI] [PubMed] [Google Scholar]
- 13. Bailey N, Besemer K, Bramley G, et al. How neighbourhood social mix shapes access to resources from social networks and from services. Hous Stud. 2015;30(2):295–314. [Google Scholar]
- 14. Galster GC, Friedrichs J. The dialectic of neighborhood social mix: editors’ introduction to the special issue. Hous Stud. 2015;30(2):175–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wilkinson RG. Socioeconomic determinants of health: health inequalities: relative or absolute material standards? BMJ. 1997;314(7080):591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chang LY, Wang MY, Tsai PS. Neighborhood disadvantage and physical aggression in children and adolescents: a systematic review and meta-analysis of multilevel studies. Aggress Behav. 2016;42(5):441–454. [DOI] [PubMed] [Google Scholar]
- 17. Ingoldsby EM, Shaw DS. Neighborhood contextual factors and early-starting antisocial pathways. Clin Child Fam Psychol Rev. 2002;5(1):21–55. [DOI] [PubMed] [Google Scholar]
- 18. Sellström E, Bremberg S. The significance of neighbourhood context to child and adolescent health and well-being: a systematic review of multilevel studies. Scan J Public Health. 2006;34(5):544–554. [DOI] [PubMed] [Google Scholar]
- 19. Jennings WG, Perez NM, Reingle Gonzalez JM. Conduct disorder and neighborhood effects. Ann Rev Clin Psychol. 2018;14:317–341. [DOI] [PubMed] [Google Scholar]
- 20. Levanthal T, Dupere V, Shuey EA. Children in neighborhoods In: Lerner RM, Liben LS, Mueller U, eds. Handbook of Child Psychology and Developmental Science. 7th ed Hoboken (NJ): John Wiley; 2015:493–533. [Google Scholar]
- 21. Gershoff ET, Benner AD. Neighborhood and school contexts in the lives of children In: Gershoff ET, Mistry R, Crosby DA, eds. Societal Contexts of Child Development: Pathways of Influence and Implications for Practice and Policy. Oxford (UK): Oxford University Press; 2014:141–155. [Google Scholar]
- 22. Minh A, Muhajarine N, Janus M, et al. A review of neighborhood effects and early child development: how, where, and for whom, do neighborhoods matter? Health Place. 2017;46:155–174. [DOI] [PubMed] [Google Scholar]
- 23. Callahan KL, Scaramella LV, Laird RD, et al. Neighborhood disadvantage as a moderator of the association between harsh parenting and toddler aged children’s internalizing and externalizing problems. J Fam Psychol. 2011;25(1):68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lima J, Caughy M, Nettles SM, et al. Effects of cumulative risk on behavioral and psychological well-being in first grade: moderation by neighborhood context. Soc Sci Med. 2010;71(8):1447–1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shanahan L, Copeland W, Costello EJ, et al. Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. J Child Psychol Psychiatry. 2008;49(1):34–42. [DOI] [PubMed] [Google Scholar]
- 26. Comeau J, Boyle MH. Patterns of poverty exposure and children’s trajectories of externalizing and internalizing behaviors. SSM Popul Health. 2018;4:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol Bull. 2005;131(4):483–509. [DOI] [PubMed] [Google Scholar]
- 28. Boyle MH, Georgiades K, Duncan L, et al. The 2014 Ontario Child Health Study—Methodology. Can J Psychiatry. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Statistics Canada. Microdata User Guide 2014 Ontario Child Health Study. Ottawa (ON): Special Surveys Division; 2017. [Google Scholar]
- 30. Boyle MH, Duncan L, Georgiades K, et al. The 2014 Ontario Child Health Study Emotional Behavioural Scales (OCHS-EBS) part II: psychometric adequacy for categorical measurement of selected DSM-5 disorders. Can J Psychiatry. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Duncan L, Georgiades K, Wang L, et al. The 2014 Ontario Child Health Study Emotional Behavioural Scales (OCHS-EBS) part I: a checklist for dimensional measurement of selected DSM-5 disorders. Can J Psychiatry. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Muthén LK, Muthén BO. Mplus User’s Guide. 6th ed Los Angeles (CA): Muthén & Muthén; 2016. [Google Scholar]
- 33. Asparouhov T, Muthén B. Computationally efficient estimation of multilevel high dimensional latent variable models. In: Proceedings of the Joint Statistical Meeting: Section on Statistics in Epidemiology: 2007 Aug 29-30; Salt Lake City (UT); p. 2531–2535. [Google Scholar]
- 34. Ley D. Social mixing and the historical geography of gentrification, In: Bridge G, Butler T, Lees L, eds. Mixed Communities: Gentrification by Stealth? Bristol (UK): Policy Press; 2011:53–68. [Google Scholar]
- 35. Georgiades K, Boyle MH, Duku E. Contextual influences on children’s mental health and school performance: the moderating effects of family immigrant status. Child Dev. 2007;78(5):1572–1591. [DOI] [PubMed] [Google Scholar]
- 36. Oreopoulos P. Neighbourhood effects in Canada: a critique. Can Public Policy. 2008;34(2):237–258. [Google Scholar]
- 37. City of Toronto. Toronto strong neighbourhoods strategy 2020: action plan. Toronto, 2012. [cited 2018 Jul. 27]. Available from: https://www.toronto.ca/city-government/data-research-maps/research-reports/social-reports. [Google Scholar]
- 38. Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55(1):125–139. [DOI] [PubMed] [Google Scholar]
- 39. Glass TA, Bilal U. Are neighborhoods causal? Complications arising from the ‘stickiness’ of ZNA. Soc Sci Med. 2016;166:244–253. [DOI] [PubMed] [Google Scholar]