Abstract
Introduction:
Seborrheic dermatitis (SD) is a chronic-recidive inflammatory skin disorder with predilection in areas rich of sebaceous gland. The most common clinical manifestations are pruritus and scales. Although SD can be diagnosed without special tools, other examinations may be needed to determine additional specific therapy. Trichoscopy is one of the noninvasive tools which can help to diagnose SD as it can provide the microstructure view of the scalp.
Materials and Methods:
This descriptive study was conducted to explore the trichoscopic features of SD and its characteristics. There were 96 SD patients enrolled in this study. The scalp was divided into four areas, and each area was scored based on Seborrheic Area Severity Index, comprising erythema, desquamation, number of papules, and percentage of lesion area. The most severe area was examined with a trichoscopy to observe the characteristics of hair and scalp. The association between trichoscopic findings and SD severity was analyzed with Fisher's exact test.
Results:
Overall, the participants were 36% males and 64% females with the mean age of 30 (13–70) years old. Based on the trichoscopic examination, the most common findings were thick hair shafts (72%), white scales (69%), arborizing thin vessels (38%), yellowish area (36%), and structureless red area (19%). These findings were not significantly different between mild and moderate SD (P > 0.05).
Conclusion:
Considering the merits and demerits of trichoscopic examination, it can be helpful to aid the diagnosis of SD. Further studies in Asian population with greater sample size are needed to demonstrate more significant result.
Key words: Diagnostic tools, scalp, seborrheic dermatitis, seborrheic dermatitis area severity index, trichoscopy
INTRODUCTION
Seborrheic dermatitis (SD) is an inflammatory skin disorder characterized by chronic, recidive, which is located in the predilection areas rich of sebaceous glands, such as the scalp, face, and chest.[1] It is reported to have occurred in 1%–5% of population globally. In Asia, the prevalence of SD was reported between 2.7% and 26.5% in participants with age of 12–20 years old.[2]
Manifestation of this disorder varies from mild to severe. Mild SD on the scalp is characterized by dry scales distributed from anterior to posterior scalp without sign of inflammation. Severe seborrheic dermatitis is characterized by greasy and yellowish scales, also erythematous plaque with diffuse border. The plaque's size varies from small to large and can be solitary or multiple, also several plaques may become confluent. Clinical manifestation also varies depending on patient's age. Subjective complaint is mostly pruritus.[1,3]
In most cases, SD is diagnosed without the need of special tools, but other examinations which can interpret the etiopathogenesis and epidemiology may be needed to determine additional specific therapy. Furthermore, SD on the scalp is sometimes difficult to be differentiated from other skin disorders on the scalp such as fungal infection.[4] Trichoscopy is one of the noninvasive tools that can help to diagnose SD, as it gives a view of color and microstructure of epidermis, dermoepidermal junction, and dermal papillae. Formerly, dermoscopy is used to detect malignancy in skin neoplasm, but nowadays, it is also used to diagnose inflammation disorders, such as psoriasis, lichen planus, scabies, and tinea nigra.[5,6] A research is conducted to get the trichoscopic view of mild, moderate, and severe SD.
MATERIALS AND METHODS
This descriptive research's aim is to study the clinical manifestation and trichoscopic findings of mild, moderate, and severe SD. This study was approved by the ethics committee of the Faculty of Medicine, Universitas Indonesia. Before initiating the study, the patients were required to give written consent. Patients who meet the inclusion criteria were eligible for the study. The inclusion criteria were agreed to become the patient of study, aged 12–70 years old with mild-to-severe SD and agreed to be taken pictures of the face and scalp. There were no any exclusion criteria. This study enrolled 96 patients, who were diagnosed and classified by dermatologists in the Department of Dermatology and Dermatology, Dr. Cipto Mangunkusumo General Hospital, Jakarta. The dermatologists, who were also the investigators, arranged a mini workshop to achieve a uniform perception about how to use trichoscope and how to assess the trichoscopic view based on the criteria. The scalp was divided into four areas, which are left anterior, right anterior, left posterior, and right posterior. Each area was examined and scored based on Seborrheic Dermatitis Area Severity Index (SDASI). SDASI is measured by multiplying the lesion area by the score of erythema, desquamation, and number of papule per scalp quadrant. Erythema, desquamation, and number of papules were ranked 0 for none, 1 for mild, 2 for moderate, and 3 for severe. Lesion area was ranked from 0 for none, 1 for under 25%, 2 for 25%–50%, 3 for 50%–75%, and 4 for 75%–100%. The average score of SDASI in each area will give an information on the severity of SD. Ranges of scores are 1–9 for mild, 10–26 for moderate, and ≥27 for severe SD.[7]
The most severe segment of each area was examined with trichoscopy to observe the characteristics of hair shafts, blood vessels, total number of hair from an ostium, dots, perifollicular white scales, perifollicular pigmentation, perifollicular red areas, scales, discharge, and other features, such as yellowish areas, structureless red areas, featureless area, and honeycomb pigment pattern. Former studies stated that thin arborizing vessels, yellowish scale, and featureless area were the characteristic findings in SD.[5] Dermlite® DL4 Trichoscopy and Sony® Cybershot DSC-W310 camera (12.1 MP) were used for this study. It was a handheld trichoscopy which gave an object view up to ×10. Low magnification was ideal to examine the scalp area. This type of trichoscopy did not require lens or other specific tools to be used.
RESULTS
The participants in this study comprised 35 males and 61 females with the median age of 30 (31–70) years old. Within the participants, 86 participants were diagnosed with mild SD and 10 participants were diagnosed with moderate SD, and the details of the participants' characteristics are shown in Table 1.
Table 1.
Baseline demographic characteristics
| Characteristics | Data |
|---|---|
| Gender, n (%) | |
| Male | 35 (36) |
| Female | 61 (64) |
| Hypertension grade, n (%) | |
| Normal | 61 (64) |
| Prehypertension | 29 (30) |
| Stage I hypertension | 5 (5) |
| Stage II hypertension | 1 (1) |
| Age (years), median (minimum-maximum) | 30 (13-70) |
| BMI, median (minimum-maximum) | 24 (16-41) |
BMI – Body mass index
The scalp was divided into four areas. Thirty-five participants demonstrated that area 1 (left anterior area) had the most severe characteristics. The most common findings in the participants were white scales, thick hair shafts, arborizing thin vessels, and yellowish area. These findings are shown in Tables 2 and 3.
Table 2.
Clinical characteristics of the subjects' scalp
| Characteristics | n (%) |
|---|---|
| Scalp area | |
| 1 | 35 (36) |
| 2 | 27 (28) |
| 3 | 13 (14) |
| 4 | 21 (22) |
| Dots | |
| Yellow | 3 (3) |
| White | 14 (15) |
| None | 79 (82) |
| Perifollicular | |
| White scale | 89 (93) |
| Pigmentation | 1 (1) |
| Red areas | 2 (2) |
| None | 4 (4) |
| Scale | |
| Yes | 95 (99) |
| None | 1 (1) |
| Scale | |
| Yellow | 30 (31) |
| White | 66 (69) |
| Discharge | |
| Yes | 4 (4) |
| None | 92 (96) |
| Blood vessels | |
| Dotted | 14 (15) |
| Linear | 3 (3) |
| Comma | 9 (9) |
| Atypical | 2 (2) |
| Arborizing thin | 36 (38) |
| Glomerular | 0 |
| None | 48 (50) |
| Other features | |
| Yellowish area | 35 (36) |
| Structureless red area | 18 (19) |
| Featureless red area | 6 (6) |
| Honeycomb pattern | 17 (18) |
| None | 31 (32) |
Table 3.
Clinical characteristics of the subjects' hair
| Characteristics | n (%) |
|---|---|
| Hair shafts | |
| Thick | 69 (72) |
| Thin | 51 (53) |
| Broken | 1 (1) |
| Hidden | 0 |
| Comma | 1 (1) |
| Normal | 32 (33) |
| Hair shaft(s) per follicle | |
| 1 | 69 (72) |
| 2 | 87 (91) |
| 3 | 24 (25) |
| ≥4 | 0 |
The association between the trichoscopic findings and SD severity was analyzed with Fisher's exact test. From this analysis, the trichoscopic findings were not significantly different between mild SD and moderate SD (P > 0.05). The analysis results are shown in Table 4.
Table 4.
Association between scalp characteristics and standard deviation severity
| Characteristics | Mild SD (%) | Moderate SD (%) | Total | P |
|---|---|---|---|---|
| Scalp area | ||||
| 1 | 33 (94) | 2 (6) | 35 | |
| 2 | 22 (81) | 5 (19) | 27 | |
| 3 | 13 (100) | 0 | 13 | |
| 4 | 18 (86) | 3 (14) | 21 | |
| Dots | ||||
| Yellow | 2 (67) | 1 (33) | 3 | |
| White | 14 (100) | 0 | 14 | |
| None | 70 (89) | 9 (11) | 79 | |
| Perifollicular | ||||
| White scale | 79 (89) | 10 (11) | 89 | |
| Pigmentation | 1 (100) | 0 | 1 | |
| Red areas | 2 (100) | 0 | 2 | |
| None | 4 (100) | 0 | 4 | |
| Scale | ||||
| Yes | 85 (89) | 10 (11) | 95 | 1.000 |
| None | 1 (100) | 0 | 1 | |
| Scale | ||||
| Yellow | 24 (80) | 6 (20) | 30 | 0.066 |
| White | 62 (94) | 4 (6) | 66 | |
| Discharge | ||||
| Yes | 3 (75) | 1 (25) | 4 | 0.361 |
| None | 83 (90) | 9 (10) | 92 | |
| Hair shafts | ||||
| Thick hair shafts | ||||
| Yes | 60 (87) | 9 (13) | 69 | 0.274 |
| None | 26 (96) | 1 (4) | 27 | |
| Thin hair shafts | ||||
| Yes | 45 (88) | 6 (12) | 51 | 0.746 |
| None | 41 (91) | 4 (9) | 45 | |
| Broken hair shafts | ||||
| Yes | 1 (100) | 0 | 1 | 1.000 |
| None | 85 (89) | 10 (11) | 95 | |
| Hidden hair | ||||
| Yes | 0 | 0 | 0 | N/A |
| None | 86 (90) | 10 (10) | 96 | |
| Comma hair | ||||
| Yes | 1 (100) | 0 (0) | 1 | 1.000 |
| None | 85 (89) | 10 (11) | 95 | |
| Normal hair | ||||
| Yes | 30 (94) | 2 (6) | 32 | 0.488 |
| None | 56 (88) | 8 (13) | 64 | |
| Blood vessels | ||||
| Dotted vessels | ||||
| Yes | 12 (86) | 2 (14) | 14 | 0.636 |
| None | 74 (90) | 8 (10) | 82 | |
| Linear vessels | ||||
| Yes | 3 (100) | 0 | 3 | 1.000 |
| None | 83 (89) | 10 (11) | 93 | |
| Comma vessels | ||||
| Yes | 9 (100) | 0 | 9 | 0.591 |
| None | 77 (89) | 10 (11) | 87 | |
| Atypical vessels | ||||
| Yes | 2 (100) | 0 | 2 | 1.000 |
| None | 84 (89) | 10 (11) | 94 | |
| Arborizing thin vessels | ||||
| Yes | 33 (92) | 3 (8) | 36 | 0.739 |
| None | 53 (88) | 7 (12) | 60 | |
| Glomerular vessels | ||||
| Yes | 0 | 0 | 0 | N/A |
| None | 86 (90) | 10 (10) | 96 | |
| No blood vessels | ||||
| Yes | 43 (90) | 5 (10) | 48 | 1.000 |
| None | 43 (90) | 5 (10) | 48 | |
| Hair shaft(s) per follicle | ||||
| One hair shaft per follicle | ||||
| Yes | 63 (91) | 6 (9) | 69 | 0.460 |
| None | 23 (85) | 4 (15) | 27 | |
| Two hair shafts per follicle | ||||
| Yes | 79 (91) | 8 (9) | 87 | 0.236 |
| None | 7 (78) | 2 (22) | 9 | |
| Three hair shafts per follicle | ||||
| Yes | 21 (88) | 3 (13) | 24 | 0.707 |
| None | 65 (90) | 7 (10) | 72 | |
| Four hair shafts per follicle | ||||
| Yes | 0 | 0 | 0 | N/A |
| None | 86 (90) | 10 (10) | 96 | |
| Other features | ||||
| Yellow area | ||||
| Yes | 30 (86) | 5 (14) | 35 | 0.489 |
| None | 56 (92) | 5 (8) | 61 | |
| Red area | ||||
| Yes | 14 (78) | 4 (22) | 18 | 0.088 |
| None | 72 (92) | 6 (8) | 78 | |
| Featureless area | ||||
| Yes | 6 (100) | 0 | 6 | 1.000 |
| None | 80 (89) | 10 (11) | 90 | |
| Honeycomb pattern | ||||
| Yes | 16 (94) | 1 (6) | 17 | 0.685 |
| None | 70 (89) | 9 (11) | 79 | |
| No other features | ||||
| Yes | 29 (94) | 2 (6) | 31 | 0.492 |
| None | 57 (88) | 8 (12) | 65 |
Analysis with Fisher’s exact test. N/A – Not available; SD – Standard deviation
DISCUSSION
SD is one of the most common skin disorders in Asia, which affects mostly in infancy and mid-adulthood.[2] Our study demonstrated participants with median age 30 (13–70) years, which is consistent with the theory of SD in mid-adulthood. Similar characteristic was demonstrated by Araya et al., whose study's participants had the mean age of 41.9 (18–89) years.[8] Borda et al. suggested that SD is probably associated with sex hormones, for instance, androgen since it was commonly found in men.[1] Our study was inconsistent with this gender predilection since our participants were mostly female (64%). However, Araya et al. demonstrated similar characteristics with 56.6% female participants.[1] We suspected this due to excessive use of hair products by female patients, use of scarf covering their hair, and long hair, which contributed to hair moisture. Furthermore, male patients seldom seek treatment and tend to ignore their symptoms.
Errichetti et al. described arborizing vessels, yellowish scales, structureless areas, honeycomb pigment, and comma vessels as characteristic findings for SD.[9] This was consistent with our study, in which arborizing thin vessels (38%) were the most common type of vessels found. However, white scales (66%), which are specific findings for scalp psoriasis, were also found more than yellow scales (31%). Both structureless areas (19%) and honeycomb pattern (19%) were found in our study, even though both findings were not the majority. This might be explained by the domination of mild SD participants; therefore, the clinical manifestations of the SD were not specific enough. Furthermore, we only examined the most severe segment of each area, thus this might not be representative for all findings on the scalp.
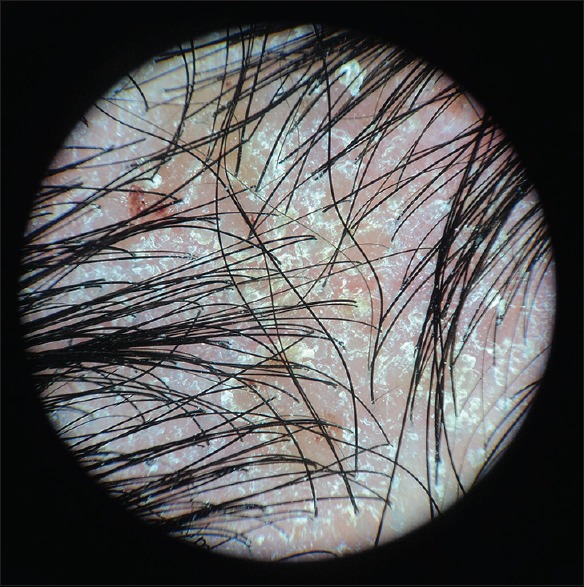
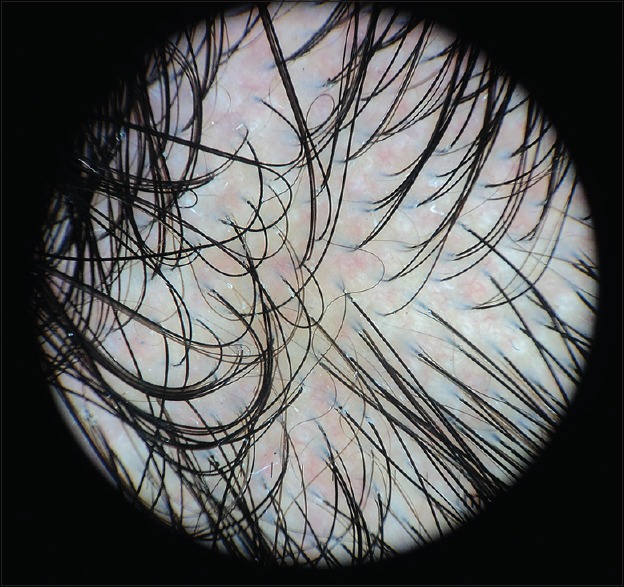
Our study demonstrated area 2 as the most common area with moderate SD (19%) [Figure 1], while area 3 is accounted for only mild SD (100%). The most common findings were perifollicular white scale (93%), thick hair shaft (72%), white scale (69%), arborizing thin vessels (38%), yellow area (36%), and white dots (15%) [Figures 2-5]. Our study found no significant differences between these findings in mild and moderate SD is often found in areas rich of sebaceous glands. Sebum is mostly secreted on the scalp which became the area for examination in this study. Sebum secretion is demonstrated as yellow area on the scalp.[1] However, the yellow area was not the most common finding in this study probably because most of the patients were diagnosed with mild SD or dandruff which often presented as white-to-yellowish area.
Figure 1.

Clinical manifestations of moderate seborrheic dermatitis
Figure 2.

Trichoscopic findings in mild seborrheic dermatitis
Figure 5.
Trichoscopic findings in moderate seborrheic dermatitis with prominent blood vessels and yellowish scales
Figure 3.
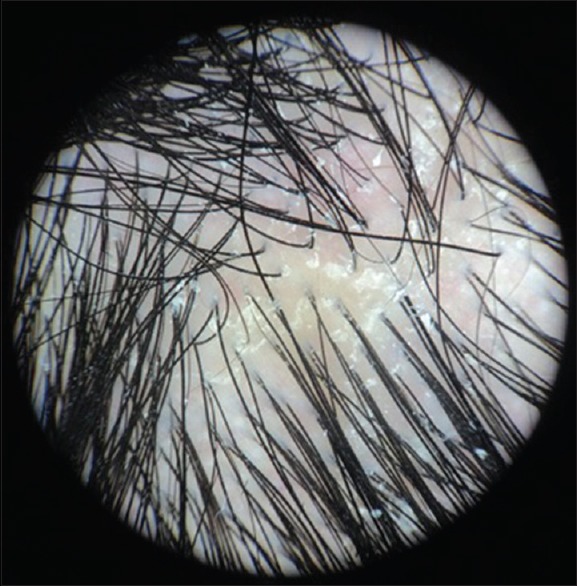
Trichoscopic findings in moderate seborrheic dermatitis with white scales and yellowish area
Figure 4.
Trichoscopic findings in mild seborrheic dermatitis with prominent arborizing blood vessels
A study by Kibar et al., which compared SD with nonscarring alopecia and psoriasis, showed that the most common findings in SD were arborizing red lines, hidden hair, and perifollicular white scale. It also demonstrated that atypical red vessels, comma vessels, structureless red areas, twisted red loops, perifollicular pigmentation, signet ring vessels, and hidden hair findings in SD were significantly different with nonscarring alopecia and psoriasis (P < 0.05). Despite being the most common findings, arborizing red lines and perifollicular white scale findings in SD only showed significant differences with nonscarring alopecia (P < 0.001). Kibar et al. also concluded that signet ring vessel and hidden hair were considered as specific signs for SD and psoriasis. However, there are relatively few presences of these two signs, and they are more commonly found in psoriasis.[10] These two signs were not found in this study, and it seems that no other studies have explained nor demonstrated these findings as characteristics of SD.
Kim et al. demonstrated similar result with Kibar et al. They compared scalp and SD, which found atypical red vessels, arborizing vessels, and featureless area as the most common findings in SD arborizing vessels, atypical red vessels, featureless area, glomerular vessel, red dots, and globules, as well as twisted red loops findings were found to be significantly different between SD and psoriasis.[11] This suggests that these findings as also found in our study can be used to differentiate SD with other disease, such as nonscarring alopecia and psoriasis. However, these findings cannot differentiate mild and moderate SD.
From our study, trichoscopy is proven to be a noninvasive, cost-effective, and useful diagnostic method for physicians. Despite commonly used for diagnosing malignancy, trichoscopy demonstrated its usefulness in aiding the diagnosis of other skin disorders, such as SD. Since the characteristics were not found to be significantly different in mild and moderate SD, it should not be the gold standard for diagnosis but only used for supporting diagnosis. Limitations in our study were the disproportional SD severity within the participants and only one area examined.
CONCLUSION
Considering the merits and demerits of trichoscopy, it may be helpful in aiding the diagnosis of SD. Further studies regarding trichoscopy use in SD, especially in the Asian population and with greater sample size, are needed to demonstrate more significant result.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Borda LJ, Wikramanayake TC. Seborrheic dermatitis and dandruff: A comprehensive review. J Clin Investig Dermatol. 2015;3:1–22. doi: 10.13188/2373-1044.1000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheong WK, Yeung CK, Torsekar RG, Suh DH, Ungpakorn R, Widaty S, et al. Treatment of seborrhoeic dermatitis in Asia: A consensus guide. Skin Appendage Disord. 2016;1:187–96. doi: 10.1159/000444682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berk T, Scheinfeld N. Seborrheic dermatitis. P T. 2010;35:348–52. [PMC free article] [PubMed] [Google Scholar]
- 4.Clark GW, Pope SM, Jaboori KA. Diagnosis and treatment of seborrheic dermatitis. Am Fam Physician. 2015;91:185–90. [PubMed] [Google Scholar]
- 5.Tosti A, Torres F. Dermoscopy in the diagnosis of hair and scalp disorders. Actas Dermosifiliogr. 2009;100(Suppl 1):114–9. doi: 10.1016/s0001-7310(09)73176-x. [DOI] [PubMed] [Google Scholar]
- 6.Lallas A, Giacomel J, Argenziano G, García-García B, González-Fernández D, Zalaudek I, et al. Dermoscopy in general dermatology: Practical tips for the clinician. Br J Dermatol. 2014;170:514–26. doi: 10.1111/bjd.12685. [DOI] [PubMed] [Google Scholar]
- 7.Agustin T, Widaty S, Rahmayunita G, Astriningrum R, Miranda E, Pusponegoro EH. Clinical Study of Antidandruff Shampoo on Patients with Dandruff and Mild Scalp Seborrheic Dermatitis. Jakarta: University Indonesia; 2018. In press. [Google Scholar]
- 8.Araya M, Kulthanan K, Jiamton S. Clinical characteristics and quality of life of seborrheic dermatitis patients in a tropical country. Indian J Dermatol. 2015;60:519. doi: 10.4103/0019-5154.164410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Errichetti E, Stinco G. Dermoscopy in general dermatology: A practical overview. Dermatol Ther (Heidelb) 2016;6:471–507. doi: 10.1007/s13555-016-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kibar M, Aktan Ş, Bilgin M. Dermoscopic findings in scalp psoriasis and seborrheic dermatitis; two new signs; signet ring vessel and hidden hair. Indian J Dermatol. 2015;60:41–5. doi: 10.4103/0019-5154.147786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim GW, Jung HJ, Ko HC, Kim MB, Lee WJ, Lee SJ, et al. Dermoscopy can be useful in differentiating scalp psoriasis from seborrhoeic dermatitis. Br J Dermatol. 2011;164:652–6. doi: 10.1111/j.1365-2133.2010.10180.x. [DOI] [PubMed] [Google Scholar]


