Abstract
Background
Automated telephone communication systems (ATCS) can deliver voice messages and collect health‐related information from patients using either their telephone's touch‐tone keypad or voice recognition software. ATCS can supplement or replace telephone contact between health professionals and patients. There are four different types of ATCS: unidirectional (one‐way, non‐interactive voice communication), interactive voice response (IVR) systems, ATCS with additional functions such as access to an expert to request advice (ATCS Plus) and multimodal ATCS, where the calls are delivered as part of a multicomponent intervention.
Objectives
To assess the effects of ATCS for preventing disease and managing long‐term conditions on behavioural change, clinical, process, cognitive, patient‐centred and adverse outcomes.
Search methods
We searched 10 electronic databases (the Cochrane Central Register of Controlled Trials; MEDLINE; Embase; PsycINFO; CINAHL; Global Health; WHOLIS; LILACS; Web of Science; and ASSIA); three grey literature sources (Dissertation Abstracts, Index to Theses, Australasian Digital Theses); and two trial registries (www.controlled‐trials.com; www.clinicaltrials.gov) for papers published between 1980 and June 2015.
Selection criteria
Randomised, cluster‐ and quasi‐randomised trials, interrupted time series and controlled before‐and‐after studies comparing ATCS interventions, with any control or another ATCS type were eligible for inclusion. Studies in all settings, for all consumers/carers, in any preventive healthcare or long term condition management role were eligible.
Data collection and analysis
We used standard Cochrane methods to select and extract data and to appraise eligible studies.
Main results
We included 132 trials (N = 4,669,689). Studies spanned across several clinical areas, assessing many comparisons based on evaluation of different ATCS types and variable comparison groups. Forty‐one studies evaluated ATCS for delivering preventive healthcare, 84 for managing long‐term conditions, and seven studies for appointment reminders. We downgraded our certainty in the evidence primarily because of the risk of bias for many outcomes. We judged the risk of bias arising from allocation processes to be low for just over half the studies and unclear for the remainder. We considered most studies to be at unclear risk of performance or detection bias due to blinding, while only 16% of studies were at low risk. We generally judged the risk of bias due to missing data and selective outcome reporting to be unclear.
For preventive healthcare, ATCS (ATCS Plus, IVR, unidirectional) probably increase immunisation uptake in children (risk ratio (RR) 1.25, 95% confidence interval (CI) 1.18 to 1.32; 5 studies, N = 10,454; moderate certainty) and to a lesser extent in adolescents (RR 1.06, 95% CI 1.02 to 1.11; 2 studies, N = 5725; moderate certainty). The effects of ATCS in adults are unclear (RR 2.18, 95% CI 0.53 to 9.02; 2 studies, N = 1743; very low certainty).
For screening, multimodal ATCS increase uptake of screening for breast cancer (RR 2.17, 95% CI 1.55 to 3.04; 2 studies, N = 462; high certainty) and colorectal cancer (CRC) (RR 2.19, 95% CI 1.88 to 2.55; 3 studies, N = 1013; high certainty) versus usual care. It may also increase osteoporosis screening. ATCS Plus interventions probably slightly increase cervical cancer screening (moderate certainty), but effects on osteoporosis screening are uncertain. IVR systems probably increase CRC screening at 6 months (RR 1.36, 95% CI 1.25 to 1.48; 2 studies, N = 16,915; moderate certainty) but not at 9 to 12 months, with probably little or no effect of IVR (RR 1.05, 95% CI 0.99, 1.11; 2 studies, 2599 participants; moderate certainty) or unidirectional ATCS on breast cancer screening.
Appointment reminders delivered through IVR or unidirectional ATCS may improve attendance rates compared with no calls (low certainty). For long‐term management, medication or laboratory test adherence provided the most general evidence across conditions (25 studies, data not combined). Multimodal ATCS versus usual care showed conflicting effects (positive and uncertain) on medication adherence. ATCS Plus probably slightly (versus control; moderate certainty) or probably (versus usual care; moderate certainty) improves medication adherence but may have little effect on adherence to tests (versus control). IVR probably slightly improves medication adherence versus control (moderate certainty). Compared with usual care, IVR probably improves test adherence and slightly increases medication adherence up to six months but has little or no effect at longer time points (moderate certainty). Unidirectional ATCS, compared with control, may have little effect or slightly improve medication adherence (low certainty). The evidence suggested little or no consistent effect of any ATCS type on clinical outcomes (blood pressure control, blood lipids, asthma control, therapeutic coverage) related to adherence, but only a small number of studies contributed clinical outcome data.
The above results focus on areas with the most general findings across conditions. In condition‐specific areas, the effects of ATCS varied, including by the type of ATCS intervention in use.
Multimodal ATCS probably decrease both cancer pain and chronic pain as well as depression (moderate certainty), but other ATCS types were less effective. Depending on the type of intervention, ATCS may have small effects on outcomes for physical activity, weight management, alcohol consumption, and diabetes mellitus. ATCS have little or no effect on outcomes related to heart failure, hypertension, mental health or smoking cessation, and there is insufficient evidence to determine their effects for preventing alcohol/substance misuse or managing illicit drug addiction, asthma, chronic obstructive pulmonary disease, HIV/AIDS, hypercholesterolaemia, obstructive sleep apnoea, spinal cord dysfunction or psychological stress in carers.
Only four trials (3%) reported adverse events, and it was unclear whether these were related to the interventions.
Authors' conclusions
ATCS interventions can change patients' health behaviours, improve clinical outcomes and increase healthcare uptake with positive effects in several important areas including immunisation, screening, appointment attendance, and adherence to medications or tests. The decision to integrate ATCS interventions in routine healthcare delivery should reflect variations in the certainty of the evidence available and the size of effects across different conditions, together with the varied nature of ATCS interventions assessed. Future research should investigate both the content of ATCS interventions and the mode of delivery; users' experiences, particularly with regard to acceptability; and clarify which ATCS types are most effective and cost‐effective.
Plain language summary
Automated telephone communication systems for preventing disease and managing long‐term conditions
Background
Automated telephone communication systems (ATCS) send voice messages and collect health information from people using their telephone's touch‐tone keypad or voice recognition software. This could replace or supplement telephone contact between health professionals and patients. There are several types of ATCS: one‐way voice messages to patients (unidirectional), interactive voice response (IVR) systems, those with added functions like referral to advice (ATCS Plus), or those where ATCS are part of a complex intervention (multimodal).
Review question
This review assessed the effectiveness of ATCS for preventing disease and managing long‐term conditions.
Results
We found 132 trials with over 4 million participants across preventive healthcare areas and for the management of long‐term conditions.
Studies compared ATCS types in many ways.
Some studies reported findings across diseases. For prevention, ATCS probably increase immunisation uptake in children, and slightly in adolescents, but in adults effects are uncertain. Also for prevention, multimodal ATCS increase numbers of people screened for breast or colorectal cancers, and may increase osteoporosis screening. ATCS Plus probably slightly increases attendance for cervical cancer screening, with uncertain effects on osteoporosis screening. IVR probably increases the numbers screened for colorectal cancer up to six months, with little effect on breast cancer screening.
ATCS (unidirectional or IVR) may improve appointment attendance, key to both preventing and managing disease.
For long‐term management, multimodal ATCS had inconsistent effects on medication adherence. ATCS Plus probably improves medication adherence versus usual care. Compared with control, ATCS Plus and IVR probably slightly improve adherence, while unidirectional ATCS may have little, or slightly positive, effects. No intervention consistently improved clinical outcomes. IVR probably improves test adherence, but ATCS Plus may have little effect.
ATCS were also used in specific conditions. Effects varied by condition and ATCS type. Multimodal ATCS, but not other ATCS types, probably decrease cancer pain and chronic pain. Outcomes may improve to a small degree when ATCS are applied to physical activity, weight management, alcohol use and diabetes.However, there is little or no effect in heart failure, hypertension, mental health or quitting smoking. In several areas (alcohol/substance misuse, addiction, asthma, chronic obstructive pulmonary disease, HIV/AIDS, high cholesterol, obstructive sleep apnoea, spinal cord dysfunction, carers' psychological stress), there is not enough evidence to tell what effects ATCS have.
Only four trials reported adverse events. Our certainty in the evidence varied (high to very low), and was often lowered because of study limitations, meaning that further research may change some findings.
Conclusion
ATCS may be promising for changing certain health behaviours, improving health outcomes and increasing healthcare uptake.
Summary of findings
Background
Description of the condition
The demand for information and communication technology applications in healthcare settings is increasing, driven by an interest in facilitating active participation of consumers in managing their own health as well as by the need to develop platforms that have greater reach and are also more cost‐effective than traditional approaches. Automated telephone communication systems (ATCS) are applications that have been used to deliver both preventive healthcare programmes as well as services to manage long‐term conditions.
The range of ATCS interventions included in this review encompasses the following.
Unidirectional ATCS. This is the non‐interactive form, which enables one‐way, non‐interactive voice communication.
Interactive ATCS. These are systems that enable two‐way real‐time communication. The most common form of this is the interactive voice response system or IVR, which might be used, for example, to provide automated tailored feedback based on the monitoring of an individual's progress.
ATCS Plus. These are also interactive ATCS systems, but they are more complex and include additional functions, such as access to an advisor to ask questions.
Additionally, this review includes several multimodal/complex ATCS interventions, defined as any type of ATCS (unidirectional, IVR or ATCS Plus) delivered as part of a complex, multimodal package, such as symptom monitoring by a health professional plus automated monitoring via IVR plus provision of medications.
Primary preventive healthcare
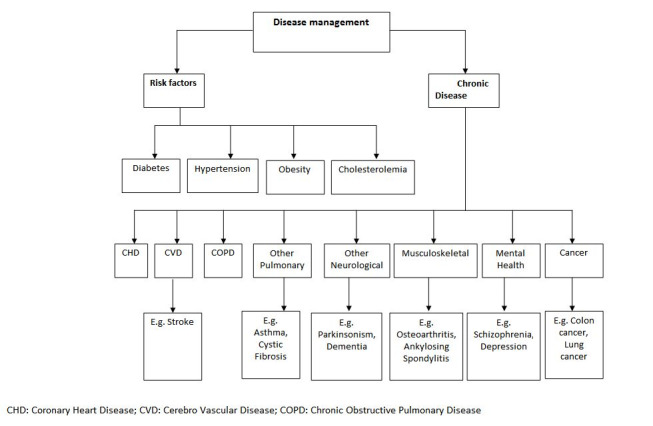
Primary preventive healthcare focuses on keeping people well, preventing disease and injury, and educating people about adopting healthier behaviours (Family Health Teams 2006). There are two types of primary prevention strategies: health promotion and disease prevention (Figure 1).
1.
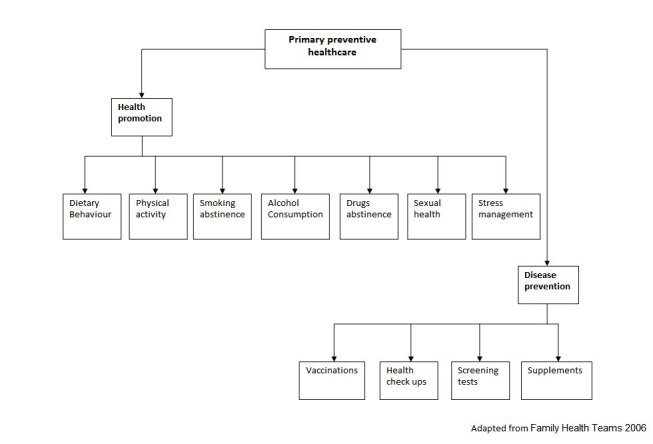
Primary preventive healthcare
A major challenge for healthcare systems is to deliver preventive services that systematically target the factors that contribute to ill health (Gullotta 2014). In the prevention of diabetes mellitus, for example, a combination of cognitive, physiological, and behavioural factors (such as lack of knowledge around risk factors, lack of physical activity and unhealthy diet) may contribute to the development of the condition. An effective preventive strategy would therefore need to take an integrative approach and target each of the influencing factors (Figure 2).
2.
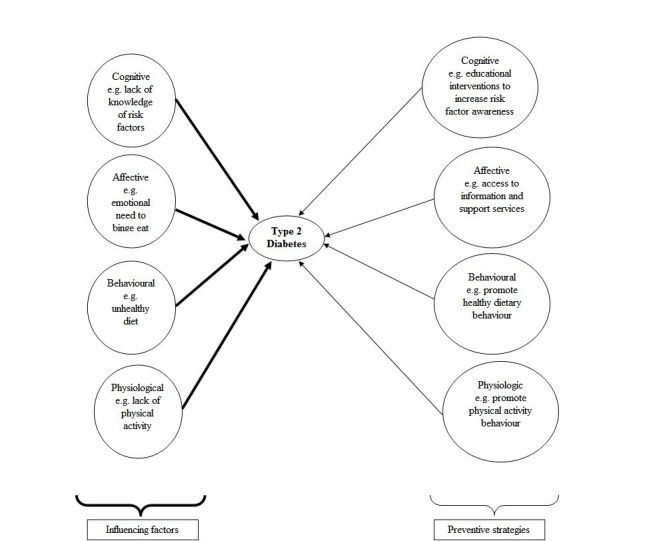
Influencing factors and preventive strategies in type 2 diabetes
One possible method of communicating preventive activities to the population is via information and communication technology (ICT) (Baranowski 2012; Haluza 2015).
Management of long‐term conditions
Long‐term conditions such as cardiovascular diseases, cancer, diabetes and chronic lung diseases are the leading causes of death globally (O'Dowd 2014). People with long‐term conditions face challenges such as dealing with complex symptoms, medication regimens, disability, and lifestyle adjustments (Carolan 2014; Demain 2015).
Effective chronic disease management programmes bring together relevant information systems with continuous follow‐up and targeted management, incorporating ICT to provide accessible and convenient educational information as well as self‐management tools for people with long‐term conditions (Galdas 2015).
ICT for primary prevention and management of long‐term conditions
Consumers increasingly use ICT for health in a myriad of ways, such as accessing medical records through web portals; communicating online with others, one‐on‐one or in a virtual community (Sawmynaden 2012); surfing the Internet to find information about health and health services; and transmitting health data or communicate messages using the web or the telephone (Pappas 2011).
There is some evidence that tools such as ATCS can successfully deliver health information to consumers, which facilitates health promotion (Cohen‐Cline 2014; Oake 2009b), enables active participation of consumers in managing their own care, and facilitates epidemiological and public health research by using collected patient data (Hendren 2014; Maheu 2001).
ICT can also support the delivery and administration of disease management programmes. There is evidence that ATCS can successfully deliver health information to patients for the management of long‐term conditions (Derose 2009; Derose 2013).
Description of the intervention
ATCS incorporate a specialised computer technology platform to deliver voice messages and collect information from consumers using either touch‐tone telephone keypads or voice recognition software (Piette 2012c). There are three types of ATCS.
Unidirectional ATCS enable one‐way, non‐interactive voice communication. This might include interventions such as automated reminder calls to take medication or perform other actions.
Interactive ATCS (e.g. IVR systems) enable two‐way real‐time communication, for example asking questions and receiving responses and individualised interventions (Reidel 2008; Rose 2015). Different studies have tested interactive ATCS for managing diabetes (Katalenich 2015; Khanna 2014), heart failure (Chaudhry 2010; Krum 2013), coronary heart disease (Reid 2007), and asthma (Bender 2010). They have also been used in health promotion initiatives, focusing on dietary behaviour (Delichatsios 2001; Wright 2014), physical activity (David 2012; Pinto 2002), and substance use (Aharonovich 2012).
ATCS Plus interventions are also interactive systems but include additional functions.
Advanced communicative functions including access to an advisor to request advice (e.g. 'ask the expert' function), scheduled contact with an advisor (e.g. telephone or face‐to‐face meetings), and peer‐to‐peer access (e.g. buddy systems).
Supplementary functions including automated, non‐voice communication (e.g. email or short messaging service (SMS)) (Webb 2010).
In this review, we also include several multimodal/complex ATCS interventions. These are more complex packages of care than ATCS Plus interventions and can include any type of ATCS (unidirectional, IVR or ATCS Plus) delivered as part of a complex, multimodal package, such as symptom monitoring by a health professional plus automated IVR monitoring plus provision of medications.
How the intervention might work
ATCS is a mode of communication that can replace or supplement some of the human‐to‐human telephone communication with a computer‐to‐human communication (Lieberman 2012; McCorkle 2011).
There is recognition that ATCS – like all other health interventions – should be underpinned by appropriate theoretical models (Krupinski 2006; Puskin 2010). These include the transtheoretical model (Prochaska 1984); theory of planned behaviour (Ajzen 1985); the health belief model (Rosenstock 1974); social cognitive theory (Bandura 2001); and self‐regulation theory (Leventhal 1984). Self‐management or preventive skills can be developed using any of these models (Barlow 2002).
There is evidence to suggest that behaviour change interventions underpinned by a theory can significantly enhance health behaviours (Fisher 2007; Gourlan 2015; Michie 2009; Webb 2010). Figure 3 shows a conceptual framework on how theories can influence health behaviour and illustrates how ATCS are used in preventive healthcare.
3.
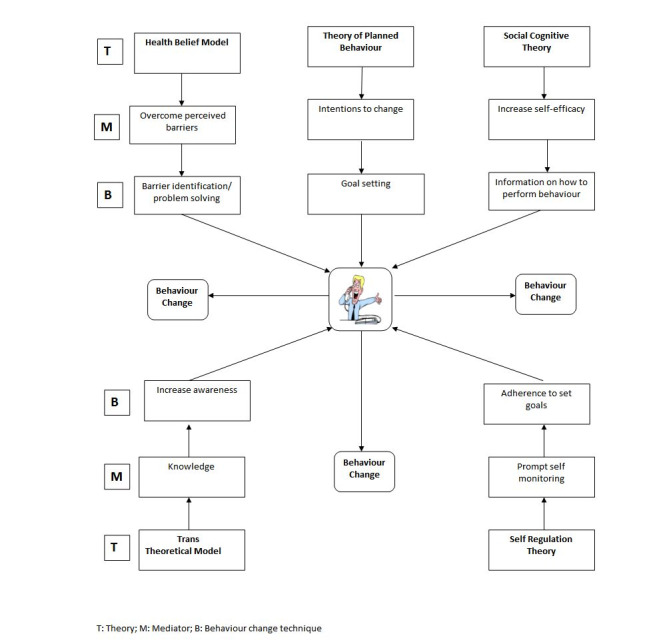
Conceptual framework of ATCS in preventive healthcare
Social cognition models assume that any health outcome is the consequence of the complex interaction between social, environmental, economic, psychological and biomedical factors (Edelman 2000; Jekauc 2015; Kelly 2009). These models focus on key concepts, such as self‐efficacy and attitudes to influence behaviour, which in turn can lead to behaviour change (Hardeman 2005; Michie 2010; Vo 2015).
Healthcare interventions delivered through disease management programmes, such as those underpinned by the chronic care model, have produced improved consumer care and health outcomes (Gee 2015; Lee 2011; Piatt 2006; Schillinger 2009). According to the chronic care model, management of long‐term conditions requires an interaction between a prepared, proactive team of practitioners and an informed, engaged consumer (Gammon 2015; Wagner 2002). This can be achieved through the interplay between elements such as self‐management support, delivery system design, decision support, and clinical information systems (Webb 2006). Figure 4 describes a framework illustrating how ATCS might work in the management of long‐term conditions using the chronic care model, by educating, monitoring, and coaching patients.
4.
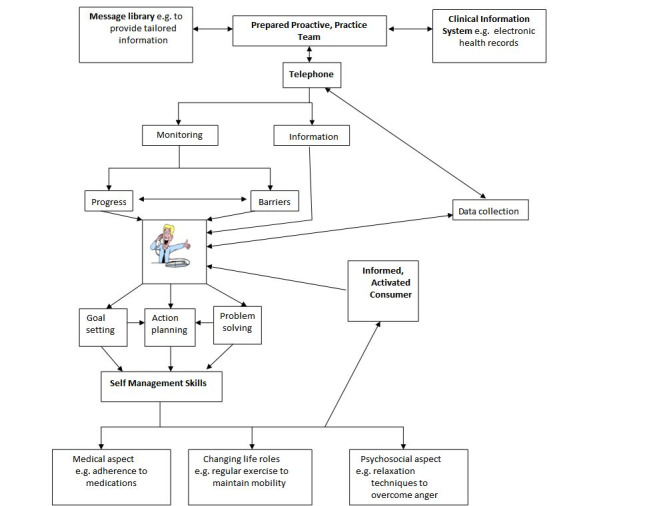
Conceptual framework of ATCS in the management of long‐term conditions
The importance of verbal communication is a complex psycholinguistic, cognitive‐emotional, and educational process that involves the transfer of information between a source (or sender) and a destination (or receiver); it largely depends on the topic/perspective of communication, perceived efficacy of communication, a person's mastery in encoding and understanding the semantic meaning decoded in verbal messages, and communicative intentions. However, other variables such as accent, voice tone, speech rate, and background noise also need to be taken into account when evaluating ATCS (Krauss 2001).
Advantages of automated telephone communication systems
ATCS as a data collection tools have a number of advantages over traditional face‐to‐face consultation (Rosen 2015). These include convenience, simplicity, anonymity, and low cost (Lee 2003; Piette 2012c). ATCS can provide access to health care 24 hours a day, seven days a week, along with immediate feedback to the consumer (Hall 2000; Schroder 2009). Both patients and healthcare professionals using ATCS have reported a high degree of user satisfaction, indicating that it is user‐friendly and convenient (Abu‐Hasaballah 2007).
ATCS technology can facilitate access to difficult‐to‐reach populations (e.g. people from a lower socioeconomic background) as ATCS require access only to a telephone (private or public) (Schroder 2009). Different authors have found ATCS to be acceptable to low‐literacy populations (Glasgow 2004; Piette 2007; Piette 2012c), and others have confirmed these findings in frail elderly patients (Mundt 2001). Unlike face‐to‐face interaction, which can elicit socially desirable responses, leading to under‐reporting of stigmatising behaviours and over‐reporting of socially desirable behaviours, ATCS have been found to elicit better self‐reporting of sensitive issues (e.g. substance misuse, alcohol use and sexual history) and reduce self‐reporting bias (Schroder 2009). They also have the potential to reduce healthcare delivery costs (Phillips 2015; Szilagyi 2013).
Disadvantages of automated telephone communication systems
Programming of ATCS involves investment in software and hardware, for example to enable multiple simultaneous calls and the development of a voice script appropriate for the target population and the topic of investigation (Piette 2007; Schroder 2009). ATCS may also present difficulties with the provision of immediate participant support. Should questions arise during the interview (Schroder 2009), ATCS cannot capture, interpret, or respond to the users' non‐verbal responses (Williams 2001). Individuals with physical disabilities (e.g. severe loss of hearing or speech) may have difficulty with ATCS (Mundt 2001). Others may simply have a strong preference for interactions with humans rather than with automated voice messages (Mahoney 2003). In addition, for individuals targeted by several ATCS‐based interventions, ATCS could lead to information overload and outright rejection of the interventions. Finally, protection of individually identifiable health information could be a challenge.
Why it is important to do this review
Existing reviews found evidence of effectiveness of ATCS in preventive healthcare and management of long‐term conditions (Krishna 2002; Lieberman 2012; Oake 2009b). However, none of those was conclusive, nor did they explore the theoretical basis or the mechanism of action of the intervention. The present review fills this gap by investigating the effects of interventions based on theoretical constructs and by exploring the behaviour change techniques implemented in the intervention (Abraham 2008; Michie 2011).
In addition, it is not clear which types of ATCS are most effective for prevention or management of long‐term conditions, in what setting, or for which conditions. This review aims to explore different interfaces of ATCS programme design and layout that may be used for diverse population groups (considering factors such as age, socioeconomic status, preferred language, and literacy) (Car 2004; Pappas 2011). Numerous randomised controlled trials (RCTs) evaluating the effectiveness of ATCS have recently been published.
A new systematic review is thus needed to critically assess the available evidence and to guide the implementation of ATCS in preventive healthcare and management of long‐term conditions.
Objectives
To assess the effects of ATCS for preventing disease and managing long‐term conditions on behavioural change, clinical, process, cognitive, patient‐centred and adverse outcomes.
Specific secondary objectives include:
determining which type of ATCS is most effective for preventive healthcare and management of long‐term conditions;
exploring which components of the interventional design contribute to positive consumer behavioural change;
exploring the behaviour change techniques and theoretical models underpinning the ATCS interventions.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs, cluster RCTs, quasi‐RCTs, interrupted time series (ITS) and controlled before‐and‐after (CBA) studies.
We included CBA and ITS studies because they are often used to draw conclusions about 'promising interventions' ready for trial when RCTs may be too expensive or simply impractical or where there are insufficient RCTs on a particular type of intervention (Centre for Reviews and Dissemination 2008; Higgins 2011; Jackson 2005). Interrupted time series designs can address cyclical trends (i.e. the outcome may be increasing or decreasing over time such as seasonal or other cyclical observations). To be considered for inclusion, these studies must have met the criteria specified by the Cochrane Effective Practice and Organisation of Care Review Group (EPOC) (Ryan 2009). For CBA designs, the timing of data collection for the control and intervention groups had to have been the same, there must have been at least two intervention sites and two control sites, and both groups would have been comparable on key characteristics related to demographics and intervention context. For ITS designs, the studies had to use a clearly defined point in time when the intervention occurred and at least three data points before and three after the intervention.
Types of participants
We included consumers, including carers, who received ATCS for prevention or management of long‐term conditions, regardless of age, sex, education, marital status, employment status, or income.
For management of long‐term conditions, we included consumers who had one or more concurrent long‐term conditions (i.e. multimorbidity).
We included consumers in all settings.
Types of interventions
The ATCS interventions included in this review included the following.
Unidirectional ATCS: non‐interactive ATCS enabling one‐way voice communication.
Interactive ATCS: systems that enable two‐way, real‐time communication, such as interactive voice response systems or IVR.
ATCS Plus: interactive ATCS systems including additional functions.
The review also included several multimodal/complex ATCS interventions, defined as any type of ATCS (unidirectional, IVR or ATCS Plus) delivered as part of a complex, multimodal package.
We included studies that evaluated either unidirectional ATCS or interactive ATCS. We also included studies that compared ATCS interventions (e.g. unidirectional ATCS versus interactive ATCS and/or ATCS Plus) to compare the effects of different intervention designs on preventive healthcare or management of long‐term conditions.
Interactive ATCS had an automated function such as automated tailored feedback based on individual progress monitoring (e.g. comparison to norms or goals, reinforcing messages, coping messages, and automated follow‐up messages). Although our protocol (Cash‐Gibson 2012) indicated that we would include ATCS Plus interventions only if the study explicitly reported that the effects of the intervention could be attributed to the ATCS component, in the review we included all types of ATCS Plus interventions as, in a complex intervention such as this, it would be impossible to attribute the intervention effect to one of the intervention components. We also included studies that delivered any type of ATCS (unidirectional, IVR, or ATCS Plus) as part of a complex, multimodal (package) intervention.
The interventions were delivered for one or more types of prevention or one or more types of management for long‐term conditions, as illustrated in Figure 1 and Figure 5, respectively.
5.
Management of long‐term conditions
We excluded studies in which interventions:
targeted health professionals or teachers for educational purposes;
were exclusively for the purpose of electronic history‐taking or data collection or risk assessment with no health promotion or interactive elements;
involved only a non‐ATCS component such as face‐to‐face communication or written communication;
were web‐based interventions that were accessed via a mobile phone.
Comparisons were made against various controls or standard or enhanced forms of usual care (i.e. no ATCS intervention). We also included comparisons of one type of ATCS against another, or the same type of ATCS that was delivered via different delivery modes (e.g. landline telephone versus mobile phone).
As part of this review, we piloted and applied the intervention Complexity Assessment Tool for Systematic Reviews version 1 (iCAT_SR) for assessing complex, multimodal interventions and reported results narratively/qualitatively (Lewin 2015).
Types of outcome measures
Primary outcomes
Primary outcomes consisted of health behaviour and clinical outcomes (defined below). For each study, we included all relevant primary outcomes, as these are likely to be most meaningful to clinicians, consumers, the general public, administrators and policymakers (Chandler 2013). Given the wide spread of the included studies and the fact that this review represents the first attempt to systematically assess all relevant evidence on broadly defined ATCS interventions, we felt that it was important to capture and report as much relevant information on outcomes and effects of interventions as possible, in order to assist with comprehensively mapping where the evidence lies and how it has been assessed. In future updates to this review, we may consider modifying this approach to focus on a smaller number and range of outcomes if this is likely to improve the clarity and meaningfulness of the collected data.
We reported the following outcomes in 'Summaries of findings' tables.
1. Health behaviour outcomes (category)
Changes in health‐enhancing behaviour (e.g. physical activity, adherence to medications/uptake of recommended laboratory or other testing)
Risk‐taking behaviour (e.g. tobacco consumption)
This outcome was either self‐reported or collected using a validated questionnaire that was either self‐administered or completed in an interview. In studies that measured the same outcome using both a self‐reported measure and an objective measure, we used the objective measure. For example, if a study on physical activity measured Metabolic Equivalent of Task (MET) scores using a self‐reported, seven‐day physical activity recall as well as a pedometer, we used the score obtained from the (objective) pedometer.
2. Clinical outcomes (category)
Physiological measures (e.g. blood pressure)
Blood biochemistry (e.g. glucose levels)
Secondary outcomes
For each study, we selected all relevant secondary outcomes as these were also meaningful for the various stakeholders.
1. Process outcomes (category)
Change in acceptability of service (e.g. consumer accessibility and usability of the interventions to apply information and support supplied through ATCS)
Satisfaction (e.g. patient and carer satisfaction with the intervention)
Cost‐effectiveness
2. Cognitive outcomes (category)
Changes in knowledge (i.e. accurate risk knowledge and perception)
Attitude and intention to change
Self‐efficacy (i.e. a person's belief in their capacity to carry out a specific action)
3. Patient‐centred outcomes (category)
Quality of life
4. Adverse outcomes
Unintended adverse events attributable to the intervention
Search methods for identification of studies
Electronic searches
We searched the following electronic databases.
The Cochrane Central Register of Controlled Trials (CENTRAL; 2015; Issue 5) in the Cochrane Library (searched 12 May 2015);
MEDLINE OvidSP (1980 to 12 May 2015);
Embase OvidSP (1980 to 12 May 2015);
PsycINFO OvidSP (1980 to 12 May 2015);
CINAHL EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1980 to 12 June 2015);
Web of Science (1980 to 19 May 2015);
GlobalHealth EBSCOhost (1980 to 16 June 2015);
WHOLIS (1980 to 17 June 2015);
LILACS (1982 to 17 June 2015); and
ASSIA ProQuest (Applied Social Sciences Index and Abstracts; 1987 to 20 May 2015).
We detail the search strategies for each database in respective appendices: CENTRAL (Appendix 1), MEDLINE (Appendix 2), Embase (Appendix 3), PsycINFO (Appendix 4), CINAHL (Appendix 5), Web of Science (Appendix 6), Global Health (Appendix 7), and WHOLIS (Appendix 8). We also present the list of keywords used in trial registers (Appendix 9) and grey literature (Appendix 10).
We searched most databases from 1980 onwards because we expected that any prior evidence would have been incorporated into subsequent research, and because technology has advanced dramatically over the last thirty years, so integration of older research should be interpreted only in light of new findings. We tailored search strategies to each database and reported them in the review. There were no language restrictions.
Searching other resources
We searched grey literature (Dissertation Abstracts, Index to Theses, Australasian Digital Theses). We contacted experts in the field and authors of included studies for advice as to other relevant studies. We searched reference lists of relevant studies, including all included studies and previously published reviews. We also searched online trial registers (e.g. Current Controlled Trials, www.controlled‐trials.com; www.clinicaltrials.gov) for ongoing and recently completed studies.
Data collection and analysis
Selection of studies
We merged search results across databases using (EndNote 2015) reference management software and removed duplicate records. Following de‐duplication, two authors (PP, NM) independently examined titles and abstracts of records retrieved from the search. We retrieved the full text of the potentially relevant studies and assessed their eligibility according to the inclusion criteria. We linked multiple reports of the same study in order to determine whether the study was eligible for inclusion. Two authors independently performed both the initial screening and the full text screening. Authors corresponded with each other to make final decisions on study inclusion and resolved disagreement about study eligibility through discussion with a third review author (JC). We describe excluded studies, with reasons for exclusion, in Characteristics of excluded studies. We used an adapted PRISMA flow chart to describe the study selection process Figure 6 (Higgins 2011).
6.
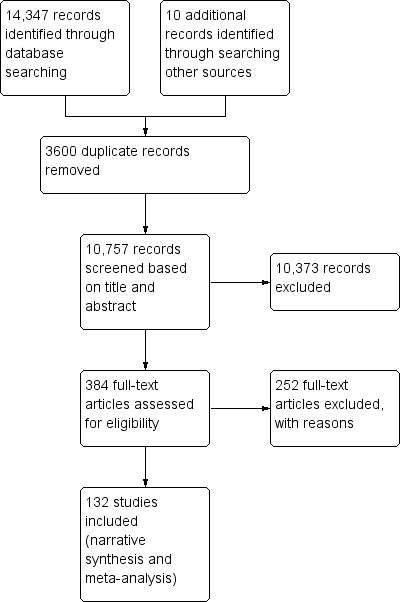
Study flow diagram
Data extraction and management
Two authors (PP, NM) independently extracted relevant characteristics related to participants, intervention, comparators, outcome measures, and results (effectiveness of the interventions) from all the included studies using a standard data collection form; any disagreements were resolved by discussion. We sought relevant missing information on the trial, particularly information required to judge the risk of bias, from the original author(s) of the article. One author (PP) transferred all the data from the extraction form into the Review Manager (RevMan) software while another author (NM) confirmed the accuracy of the transferred data (RevMan 2014).
Assessment of risk of bias in included studies
We included all studies meeting the inclusion criteria regardless of the outcome of the assessment of risk of bias. We assessed and reported on the methodological risk of bias of included studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions and Cochrane Consumers and Communication guidelines (Higgins 2011; Ryan 2011), which recommend explicitly reporting the following individual elements for RCTs: random sequence generation; allocation concealment; blinding (participants, personnel); blinding (outcome assessment); completeness of outcome data (attrition bias), selective outcome reporting (relevant outcomes reported); other sources of bias (baseline imbalances). For cluster RCTs, we also assessed and reported the risk of bias associated with an additional domain: selective recruitment of cluster participants. We referred to Cochrane Consumers and Communication guidelines to narratively describe the results of risk of bias for each domain for all included studies (Ryan 2011). We reported our assessment of risk of bias for each domain and included study, with a descriptive summary/synthesis of our judgments. In all cases, two authors (PP, NM) independently assessed the risk of bias of included studies, resolving any disagreements by discussion and consensus. We also contacted several study authors for additional information about the included study or for clarification of the study's methods. We incorporated the results of the risk of bias assessment into GRADE assessments and the review itself through standard tables together with systematic and descriptive summary, leading to an overall assessment of the risk of bias of included studies and a judgment about the internal validity of the review's results.
Measures of treatment effect
For dichotomous data, we reported risk ratios (RR), odds ratios (OR), or hazard ratios (HR), as well as their 95% confidence intervals (CI) and P values. For continuous data we reported mean values and standard deviations (SD) of the outcomes in each intervention group along with the number of participants and P values (Table 13).
1. Results.
| Dichotomous outcomes | ||||||||||
| Primary outcome | Study ID | Timing of outcome assessment (months) | Intervention group | Comparator group | Between group difference | Notes | ||||
| Observed (n) | Total (N) | Observed (n) | Total (N) | P value | Effect estimate (OR/RR/HR) | 95% CI | ||||
| IMMUNISATIONS | ||||||||||
| Immunisation uptake | Dini 2000 | 24 | 107 | 189 | 87 | 186 | — | 1.21 | 0.99 to 1.47 | — |
| Franzini 2000 | * | 270 | 314 | 273 | 429 | — | — | — | — | |
| Hess 2013 | 3 | 146 | 5599 | 46 | 6383 | < 0.001 | 3.69 | 2.64 to 5.15 | Cluster RCT unadjusted for clustering. Approximate sample size calculations gave the following adjusted values: intervention 20/791; control 6/902; see Appendix 14 for calculations | |
| Lieu 1998 | 4 | 89 | 167 | 70 | 162 | 0.11 | — | 29.0 to 43.8 | CIs for % values and for IVR alone; P value from Chi2 | |
| Linkins 1994 | 1 | 1684 | 4636 | 955 | 3366 | < 0.01 | 1.28 | 1.20 to 1.37 | — | |
| LeBaron 2004 | 13 | 305 | 763 | 259 | 763 | < 0.05 | — | — | — | |
| Nassar 2014 | 2 | 3 | 26 | 3 | 24 | — | — | — | — | |
| Stehr‐Green 1993 | 1 | 46 | 112 | 41 | 110 | — | 1.07 | 0.78 to 1.46 | — | |
| Szilagyi 2006 | 18 | 928 | 1496 | 873 | 1510 | 0.02 | — | — | — | |
| Szilagyi 2013 | 12 | 748 | 1423 | 651 | 1296 | < 0.05 | 1.3 | 1.0 to 1.7 | — | |
| SCREENING | ||||||||||
| Screening rate | Baker 2014 | 6 | 191 | 225 | 90 | 225 | < 0.001 | — | — | — |
| Cohen‐Cline 2014 | 6 | 801 | 8005 | 234 | 3005 | 0.0012 | 1.32 | 1.14 to 1.52 | ||
| Corkrey 2005 | 3 | — | 45,303 | — | 30,229 | — | — | 1.28 to 1.42a 0.11 to 0.17b |
aWomen aged 50‐69 years bWomen aged 20‐49 years |
|
| DeFrank 2009 | 10 to 14 | 960 | 1355 | 574 | 847 | 0.014 | 1.32 | 1.06 to 1.64 | — | |
| Fiscella 2011 | 12 | 55a 47b |
134a 163b |
23a 16b |
137a 160b |
— | 3.44a 3.70b |
1.91 to 6.19a 1.93 to 7.09b |
aBreast cancer screening; bColorectal cancer screening |
|
| Fortuna 2014 | 12 | 36a 24b |
158a 157b |
28a 19b |
157a 156b |
> 0.05 | 1.4a 1.3b |
0.8 to 2.4a 0.7 to 2.5b |
aBreast cancer screening; bColorectal cancer screening (both crude estimates) |
|
| Hendren 2014 | 12 | 30a 43b |
101a 114b |
15a 21b |
90a 126b |
0.034a 0.0002b |
1.96a 3.22b |
0.87 to 4.39a 1.65 to 6.30b |
aBreast cancer screening; bColorectal cancer screening |
|
| Heyworth 2014 | 12 | 385 | 1565 | 290 | 1558 | < 0.001 | — | — | ||
| Mosen 2010 | 6 | 662 | 2943 | 474 | 2962 | < 0.001 | 1.31 | 1.10 to 1.56 | — | |
| Phillips 2015 | 9 | 19a 33b |
90a 198b |
17a 27b |
88a 199b |
— | — | — |
aBreast cancer screening; bColorectal cancer screening |
|
| Simon 2010a | 12 | 3192 | 10,432 | 3194 | 10,506 | 0.76 | 1.01 | 0.94 to 1.07 | In the adjusted model | |
| Solomon 2007 | 10 | 144 | 997 | 97 | 976 | 0.006 | 1.52 | 1.13 to 2.05 | In the adjusted model | |
| APPOINTMENT REMINDERS | ||||||||||
| Reducing non‐attendance rates | Dini 1995 | 1 | 144 | 277 | 78 | 240 | < 0.05 | 1.60 | 1.29 to 1.98 | — |
| Griffin 2011 | 1.5 | 333a 169b |
794a 411b |
324a 164b |
790a 409b |
> 0.05 | — | −6 to 5a −8 to 7b |
aColonoscopy bFlexible sigmoidoscopy |
|
| Maxwell 2001 | 2 | 347 | 700 | 322 | 670 | > 0.05 | — | — | — | |
| Parikh 2010 | 4 | 2662 | 3219 | 2576 | 3350 | < 0.001 | 1.52 | 1.34 to 1.71 | — | |
| Reekie 1998 | 1.5 | 473 | 500 | 453 | 500 | < 0.001 | 3.41 | 1.87 to 6.20 | — | |
| Tanke 1994 | 6 | 257 | 407 | 235 | 456 | < 0.01 | 1.50 | — | — | |
| Tanke 1997 | 3 days | 652 | 701 | 617 | 701 | < 0.05 | 1.71 | — | — | |
| ADHERENCE | ||||||||||
| Adherence to medications/laboratory tests | Bender 2010 | 2.5 | 16 | 25 | 12 | 25 | 0.003 | — | — | — |
| Derose 2009 | 3 | 453 | 2199 | 298 | 1550 | 0.31 | 1.09 | 0.92 to 1.28 | At 8 weeks differences were not significant (P = 0.23) | |
| Feldstein 2006 | 25 days | 177 | 267 | 53 | 237 | < 0.001 | 4.1 | 3.0 to 5.6 | — | |
| Friedman 1996 | 6 | 24 | 133 | 16 | 134 | 0.03 | — | — | — | |
| Glanz 2012 | 12 | 47 | 157 | 42 | 155 | > 0.05 | — | — | — | |
| Green 2011 | 2 weeks | 1180 | 4124 | 958 | 4182 | < 0.001 | — | — | — | |
| Ho 2014 | 12 | 109 | 122 | 88 | 119 | 0.003 | — | — | — | |
| Lim 2013 | 5 | 29 | 38 | 34 | 42 | 0.233 | — | — | After the mid‐study visit | |
| Migneault 2012 | 12 | — | 169 | — | 168 | 0.19 | — | — | — | |
| Mu 2013 | 1 | 1096975 | 4153634 | 18395 | 84187 | < 0.001 | — | — | — | |
| Patel 2007 | 3 to 6 | 3362 | 6833 | 1865 | 4172 | — | — | — | ||
| Reynolds 2011 | 2 weeks | 4318 | 15,356 | 3309 | 15,254 | < 0.001 | — | — | — | |
| Sherrard 2009 | 6 | 70 | 137 | 55 | 143 | 0.041 | 0.60 | 0.37 to 0.96 | Primary composite outcome of adherence and adverse effects (emergency room visit and hospitalisation) | |
| Simon 2010b | 12 | — | 600 | — | 600 | — | 0.93 | 0.71 to 1.22 | — | |
| Stacy 2009 | 6 | 178 | 253 | 148 | 244 | < 0.05 | 1.54 | 1.13 to 2.10 | — | |
| Vollmer 2011 | 18 | — | 3171 | — | 3260 | 0.002 | — | 0.01 to 0.03 | P value and CIs for Δ change | |
| Vollmer 2014 | 12 | — | 7247 | — | 7255 | 0.022 | — | 0.011 to 0.034 | P value and CIs for Δ change | |
| HEART FAILURE | ||||||||||
| Heart failure hospitalisation | Capomolla 2004 | 10 ± 6 (median 11) | 17 | 67 | 58 | 66 | < 0.05 | — | — | — |
| Kurtz 2011 | 12 | 4 | 32 | 17 | 50 | < 0.05 | — | — | This was a cluster outcome: "cardiovascular deaths and hospitalisations‐ which ever event occurred first" | |
| All‐cause mortality | Capomolla 2004 | 10 ± 6 (median 11 ) | 5 | 67 | 7 | 66 | > 0.05 | — | — | — |
| Chaudhry 2010 | 6 | 92 | 826 | 94 | 827 | 0.86 | 0.97 | 0.73 to 1.30 | Death or readmission | |
| Krum 2013 | 12 | 17 | 170 | 16 | 209 | 0.439 | 1.36 | 0.63 to 2.93 | — | |
| Cardiac mortality | Capomolla 2004 | 10 ± 6 (median 11) | 2 | 67 | 6 | 66 | > 0.05 | — | — | — |
| Kurtz 2011 | 12 | 3 | 32 | 5 | 50 | > 0.05 | — | — | Cluster outcome: "cardiovascular deaths and hospitalisations‐ which ever event occurred first" | |
| SMOKING | ||||||||||
| Smoking abstinence | Brendryen 2008 | 12 | 74 | 197 | 48 | 199 | 0.02 | 1.91 | 1.12 to 3.26 | — |
| Ershoff 1999 | 9 | 20 | 120 | 25 | 111 | — | — | — | — | |
| McNaughton 2013 | 12 | 12 | 23 | 14 | 21 | 0.33 | — | — | — | |
| Regan 2011 | 3 | 105 | 361 | 95 | 364 | 1.13 | 0.90 to 1.41 | — | ||
| Reid 2007 | 12 | 23 | 50 | 17 | 49 | 0.25 | 1.60 | 0.71 to 3.60 | — | |
| Rigotti 2014 | 6 | 51 | 198 | 30 | 199 | 0.009 | 1.71 | 1.14 to 2.56 | — | |
| Velicer 2006 | 30 | 75 | 500 | 65 | 523 | — | — | — | For 6 month prolonged abstinence | |
| Continous outcomes | ||||||||||
| Primary outcome | study ID | Timing of outcome assessment (months) | Intervention group | Comparator group | Between‐group difference | Notes | ||||
| Mean |
Standard deviation of change (SD) or SD |
Mean | Standard deviation of change (SD) or SD | Change | Confidence intervals | P values | ||||
| ALCOHOL CONSUMPTION | ||||||||||
| Drinks per drinking day | Hasin 2013 | 2 | 3.5 | 1.8 | 4.7 | 3.2 | 1.38 | 1.12 to 1.70 | < 0.01 | CIs are for the effect size |
| Rose 2015 | 2 | 4 | 0.4 | 4.3 | 0.4 | — | — | 0.45 | — | |
| CANCER | ||||||||||
| Symptom severity | Cleeland 2011 | 1 | — | — | — | — | — | — | — | Effect size: intervention = 0.75; control = 0.68 |
| Mooney 2014 | 1.5 | 5.76 to 7.36 (range) | — | 5.55 to 7.44 (range) | — | 0.06 | — | 0.58 | — | |
| Sikorskii 2007 | 2.5 | 20.73 | — | 20.80 | — | — | — | > 0.05 | Effect size: intervention = 0.59; control = 0.56 | |
| Spoelstra 2013 | 2.5 | 11.6 | — | 11.0 | — | — | — | 0.02 | — | |
| DIABETES | ||||||||||
| Glycated haemoglobin (%) | Graziano 2009 | 3 | 7.87 | 1.09 | 7.82 | 1.14 | — | — | 0.89 | — |
| Katalenich 2015 | 6 | 8.10 | 7.90 | — | — | — | > 0.05 | Median values | ||
| Khanna 2014 | 3 | 9.1 | 1.9 | 8.6 | 1.3 | — | — | 0.41 | — | |
| Kim 2014 | 12 | 9.0 | 2 | 9.9 | 2.2 | — | — | 0.02 | — | |
| Lorig 2008 | 6 | 7.0 | 1.4 | 7.3 | 1.5 | — | — | 0.04 | — | |
| Piette 2001 | 12 | 8.1 | 1.15 | 8.2 | 1.18 | — | — | 0.3 | — | |
| Schillinger 2009 | 12 | 8.7 | 1.9 | 9.0 | 2.2 | 0.1 | 0.5 to 0.4 | 0.8 | — | |
| Williams 2012 | 6 | 7.9 | 1.2 | 8.7 | 1.8 | 0.91 | 0.86 to 0.93 | 0.002 | — | |
| Serum blood glucose (mg/dL) | Piette 2001 | 12 | 180 | 9 | 172 | 10 | — | — | 0.6 | — |
| Homko 2012 | 26 | 107.4 | 12.9 | 109.7 | 16.5 | — | — | 0.44 | — | |
| Self‐monitoring of blood glucose | Graziano 2009 | 3 | 1.9 | 1.07 | 1.3 | 0.75 | — | — | < 0.001 | — |
| Lorig 2008 | 6 | 0.05 | 0.387 | 0.08 | 0.365 | — | — | 0.457 | — | |
| Piette 2001 | 12 | 4.6 | 0.1 | 4.4 | 0.1 | — | — | 0.05 | — | |
| Schillinger 2009 | 12 | 4.3 | 2.6 | 3.3 | 2.9 | 0.8 | 0.1 to 1.5 | 0.03 | — | |
| Self‐monitoring of diabetic foot | Piette 2001 | 12 | 4.6 | 0.1 | 4.4 | 0.1 | — | — | — | — |
| Schillinger 2009 | 12 | 5.1 | 1.4 | 4.6 | 1.7 | 0.6 | 0.2 to1.0 | 0.002 | — | |
| HYPERTENSION | ||||||||||
| Systolic Blood Pressure (mm Hg) | Dedier 2014 | 3 | 136.4 | 83.5 | 138.9 | 81.5 | — | — | > 0.05 | — |
| Goulis 2004 | 6 | 123.8 | 14.2 | 128.6 | 19.4 | — | — | > 0.05 | — | |
| Friedman 1996 | 6 | 158 | * | 160.2 | * | −1.8 | — | 0.20 | — | |
| Harrison 2013 | 1 | 141.2 | 15.1 | 143.1 | 14.6 | — | < 0.001 | — | ||
| Magid 2011 | 6 | 137.4 | 19.4 | 136.7 | 17.0 | −0.7 | — | 0.006 | — | |
| Piette 2012 | 6 weeks | 142.5 | 2.3 | 143.6 | 2.4 | −4.2 | −9.1 to 0.7 | 0.09 | — | |
| Diastolic Blood Pressure (mm Hg) | Friedman 1996 | 6 | 80.9 | — | 83.2 | — | — | — | 0.02 | — |
| Goulis 2004 | 6 | 74.6 | 8.5 | 79.5 | 14.0 | — | — | > 0.05 | — | |
| Harrison 2013 | 1 | 80.3 | 12.6 | 81.3 | 12.5 | — | — | < 0.001 | — | |
| Magid 2011 | 6 | 82.9 | 12.9 | 81.1 | 11.7 | −2.3 | −4.9 to −0.2 | 0.07 | — | |
| OBSTRUCTIVE SLEEP APNOEA SYNDROME (OSAS) | ||||||||||
| Continuous positive airway pressure (CPAP) use | DeMolles 2004 | 2 | 4.4 | — | 2.9 | — | — | — | 0.076 | — |
| Sparrow 2010 | 12 | — | — | — | — | — | 1.18 to 2.48 | 0.004 | — | |
| WEIGHT MANAGEMENT | ||||||||||
| BMI in adults | Bennett 2012 | 18 | 36.54 | 2.01 | 36.84 | 1.90 | −0.35 | −0.75 to 0.06 | — | — |
| Bennett 2013 | 18 | 29.8 | 1.90 | 30.3 | 1.93 | −0.6 | −1.2 to −0.1 | 0.03 | — | |
| Goulis 2004 | 6 | 33.7 | 5.2 | 37.2 | 8.7 | — | — | 0.06 | — | |
| BMI‐z scores in children | Estabrooks 2009 | 12 | 1.95 | 0.04 | 1.98 | 0.03 | — | — | > 0.05 | — |
| Wright 2013 | 3 | 1.9 | 0.28 | 1.9 | 0.3 | −0.03 | — | 0.48 | — | |
Analyses limited to primary outcomes from at least 2 studies from the same category.
Unit of analysis issues
When a study had more than one active treatment arm, we labelled the study arms as 'a', 'b' and so on. If more than one intervention arm was relevant for a single comparison, we compared the relevant ATCS arm with the least active control arm to avoid double‐counting of data. We listed the arms that were not used for comparison in the 'Notes' section of the Characteristics of included studies tables.
In cluster RCTs, we checked for unit of analysis errors. If we identified any and sufficient information was available, we re‐analysed the data using the appropriate unit of analysis, taking account of the intracluster correlation coefficients (ICC). We planned to impute estimates of the ICC using external sources. Where it was not possible to obtain sufficient information to reanalyse the data, we annotated the study 'unit of analysis error' and used this when interpreting the results of that study (where failure to adjust for clustering may lead to overly precise effect estimates) (Higgins 2011; Ukoumunne 1999).
Dealing with missing data
We conducted an intention‐to‐treat analysis, including all participants who were randomised to either the ATCS group or comparator, regardless of losses to follow‐up and withdrawals (Higgins 2011). Wherever possible, we attempted to obtain missing data (e.g. number of participants in each group, outcomes and summary statistics) from the original author(s). For dichotomous outcomes, data imputed case analysis can be used to fill in missing values. This strategy imputes missing data according to reasons for 'missingness' and essentially averages over several of the specific imputation strategies (Higgins 2008). When SDs of continuous outcome data were missing, we calculated them from other statistics, such as 95% CIs, standard errors, or P values. If these were unavailable, we planned to contact the authors or impute the standard deviations from other similar studies (Higgins 2008).
Assessment of heterogeneity
Where we considered studies to be sufficiently similar (based on consideration of populations, interventions, comparators, outcome measures and primary endpoints) to allow pooling of data using meta‐analysis, we assessed the degree of heterogeneity by visual inspection of forest plots and by examining the Chi2 test for heterogeneity. We quantified heterogeneity using the I2 statistic. We considered an I2 value of 50% or more to represent substantial levels of heterogeneity, but we also interpreted this value in light of the size and direction of effects and the strength of the evidence for heterogeneity, based on the P value from the Chi2 test (Higgins 2011). Where substantial heterogeneity was present in pooled effect estimates, we had planned to explore the reasons for variability by conducting subgroup analyses. However, there was not a sufficient number of studies in pooled analyses to enable performance of subgroup analysis. Where we detected substantial clinical, methodological, or statistical heterogeneity across included studies, we did not report pooled results from meta‐analysis but instead used a narrative approach to data synthesis. In this event we attempted to explore possible clinical or methodological reasons for this lack of homogeneity by grouping studies that were similar in terms of populations, interventions, comparators, outcome measures and primary endpoints to explore differences in intervention effects.
Assessment of reporting biases
We assessed reporting bias qualitatively based on the characteristics of the included studies (e.g. if only small studies that indicate positive findings were identified for inclusion). Where quantitative meta‐analysis included at least 10 studies, we had planned to construct a funnel plot to investigate small study effects, as this may indicate the presence of publication bias. We also planned to formally test for funnel plot asymmetry, with the choice of test made based on advice in Higgins 2011, and bearing in mind that there may be several reasons for funnel plot asymmetry when interpreting the results (Egger 1997). However, there were not enough studies in any of the pooled analyses to allow formal assessment of reporting biases.
Data synthesis
Our decisions on whether to perform meta‐analysis were based on an assessment of whether participants, interventions, comparisons, and outcomes were sufficiently similar to ensure a clinically meaningful result. For studies that were included in meta‐analysis, we used a random‐effects model. For studies that assessed the same continuous outcome measures, we estimated mean differences (for studies using the same scale) and standardised mean differences (for differences in scale) between groups, along with 95% CIs. We displayed the results of the meta‐analysis in a forest plot that provided effect estimates and 95% CIs for each individual study as well as a pooled effect estimate and 95% CI. We performed meta‐analysis using RevMan 2014. We adhered to the statistical guidelines described in Higgins 2011.
We used a systematic approach to the description of results from pooled data and to narratively describe results. This approach was based on the following process.
Two authors (PP, RR) assessed the size of the effect and jointly rated it as an important, less important, or not important.
Two authors (PP, RR) assessed the quality of the evidence using GRADE criteria (Schünemann 2011). According to these guidelines, we assessed all primary and secondary outcomes reported in the review and assigned a rating of high, moderate, low, or very low certainty.
We reported results and then adopted the standardised wording developed for writing Plain Language Summaries in Cochrane reviews (Glenton 2010); see Appendix 12. We used this wording to synthesise all of the results of the review, irrespective of whether we meta‐analysed or narratively reported the data.
For all the included studies we used the following steps to describe the studies as described by Rodgers 2009.
Developed a preliminary synthesis by grouping the included studies by the type of prevention or long‐term condition and intervention.
Described the inclusion criteria (especially participants, interventions, comparators, and outcome elements) along with the reported findings for each of the included studies.
Included an additional table to describe the intervention components including: the type of ATCS; content delivery; intervention content; behaviour change theories; behaviour change techniques (Michie 2011); instructions on how to use the system (yes/no); call initiation (participants/interventionist/either); telephone keypad for response (yes/no); toll free number (yes/no); duration of intervention; duration of call; frequency, intensity; speakers features; and security arrangement.
Used the summary of quality of the evidence, assessed using the GRADE tool, to judge the robustness of the evidence; and adapted standardised wording based on the size of effects and the strength (quality) of the evidence to consistently describe results.
Subgroup analysis and investigation of heterogeneity
We considered performing subgroup analyses depending on the types of preventive intervention (Figure 1), long‐term condition being managed (Figure 5), and other relevant factors that may have influenced the results.
Type of ATCS (unidirectional, IVR or ATCS Plus, multimodal).
Type of preventive intervention;
Type of long‐term condition.
Language (for studies in languages other than English).
Country's income level (for studies undertaken in 'high‐income countries', 'middle‐income countries', or 'low‐income countries' as defined by the World Bank's income level data (World Bank 2012)).
Source of funding (industry versus other).
Theoretical models (where applicable, we separated included studies depending on the type of theoretical model used to inform the design of the intervention).
If at least 10 studies had been available for a particular outcome and if feasible, we would have performed a meta‐regression. This was to be undertaken using Stata Software with the metareg command, including trial characteristics as covariates. However, we did not identify a sufficient number of studies within review comparisons to allow performance of subgroup analyses.
Sensitivity analysis
We planned to perform sensitivity analyses to investigate the robustness of the results, including assessing the effects of:
including only studies with low risk of bias in the selection bias domain in analysis (i.e. sequence generation and allocation concealment);
including only studies with low risk of bias in the attrition bias domain in analysis (i.e. incomplete outcome data);
using a fixed‐effect model of analysis for all the studies;
using a fixed‐effect model for analysis of studies with low risk of bias in the selection bias domain; and
using a fixed‐effect model for analysis of studies with low risk of bias in the attrition bias domain.
Again, we did not identify a sufficient number of studies within review comparisons to enable performance of sensitivity analyses.
Summary of findings tables
We prepared 'Summary of findings' tables to present the results for each of the major primary outcomes, based on meta‐analysis or narrative synthesis. We converted results into absolute effects when possible and provided a source and rationale for each assumed risk cited in the table(s) when presented. Two authors independently (PP, RR) assessed the overall quality of the evidence as implemented and described in the GRADEprofiler (GRADEpro 2016) software and chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011). We considered the following criteria to assess the quality of the evidence: limitations of studies (risk of bias), inconsistency of results, indirectness of the evidence, imprecision and publication bias, downgrading the quality where appropriate. We did this for all primary and secondary outcomes reported in the review.
As there were many prevention and long‐term management areas and comparisons included in this review, two authors (PP, RR) made the decision to limit the number of 'Summary of findings' tables presented. We examined the prevention and long‐term management areas covered by the review, assessed the numbers of studies contributing data to each of these areas, and determined the direction of results for each area (positive, negative or inconclusive). We then made the decision to report in 'Summary of findings' tables only those areas of prevention and/or long‐term management where four or more studies contributed data.
We also determined that in the review, we would represent both comparisons presented and those not presented in 'Summary of findings' tables, describing results that were positive, negative, or inconclusive.
We took this approach in order to be confident that we were not selectively reporting and presenting positive results (those in favour of the intervention) over negative or inconclusive results.
As the included studies covered a very large range of preventive care and long‐term management decisions, we also made the pragmatic decision not to report only a single comparison in each 'Summary of findings' table. Instead we chose to present all the main results for primary outcomes within a given preventive healthcare/long‐term management area, irrespective of the comparisons being made. We clearly identified the different comparisons in each case within each 'Summary of findings' table. The reasons for doing so were as follows.
Reporting by different disease/prevention areas together (i.e. by comparison) would have resulted in significant clinical heterogeneity, as the populations and the likely effects of interventions on targeted behaviours and clinical outcomes varied considerably.
Given the above point, if we had further split tables by comparisons, it would have most likely meant creation and reporting of more than 30 tables, many with sparse data that would not be informative to most users or readers of this review.
We have otherwise not deviated from the advice on preparing 'Summary of findings' tables outlined in Schünemann 2011.
Involvement of non‐governmental organisations (NGOs) that represent a range of potential user groups was an important part of the project development. We contacted NGOs such as the Diabetes Research Network and requested one of the members (AM) to guide us in the review process, particularly in considering outcomes of interest to users and methods of disseminating results to user communities. The protocol was peer reviewed by at least one consumer, as part of the Cochrane Consumers and Communication Group's standard editorial process.
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies for more details about individual studies.
Additional tables also contain supplementary information: Table 14 presents further information on participants of included studies, Table 15 reports details of the interventions assessed, and Table 16 presents an assessment of intervention complexity for studies evaluating the effects of highly complex (i.e. multimodal) ATCS interventions.
2. Participants.
| Study ID | Study typea | Study subtypeb | Country | Sample size | Mean age (years unless stated otherwise) | Male (%) | Female (%) | Ethnicityc | Duration of condition | Comorbidities, medication | Incentives for participation | Incentives |
| Tucker 2012 | P | Alcohol misuse | USA | 187 | 45 | 63 | 37 | White ‐ 54% Other ‐ 46% |
— | — | Yes | Visa gift cards or checks (USD 50 per in‐person interview, USD 15 per phone interview). IG participants received USD 0.50 minimum for each daily call and USD 1.00 after seven consecutive calls |
| Franzini 2000 | P | I | USA | 1138 | — | — | — | — | — | — | — | — |
| Hess 2013 | P | I | USA | 11,982 | 72 | — | — | — | — | — | — | — |
| Dini 2000 | P | I | USA | 1227 | 2‐3 months | — | — | — | — | — | — | — |
| LeBaron 2004 | P | I | USA | 3050 | 9 monthsd | 49 | 51 | Black ‐ 76% Hispanic ‐ 14% White ‐ 7% Other – 3% |
— | — | — | — |
| Lieu 1998 | P | I | USA | 752 | 20 months | — | — | — | — | — | — | — |
| Linkins 1994 | P | I | USA | 8002 | — | 51 | 49 | Black ‐ 50% White ‐ 45% Other – 5% |
— | — | — | — |
| Nassar 2014 | P | I | USA | 50 | 24 | 0 | 100 | Black ‐ 86% White ‐ 14% |
— | — | Yes | USD 35 per month to help pay for cell phone service or a free, unlimited minutes cell phone until 6 weeks postpartum |
| Stehr‐Green 1993 | P | I | USA | 229 | 9 months | 52 | 48 | Black ‐ 90% Other – 7% Hispanic ‐ 3% |
— | — | — | — |
| Szilagyi 2006 | P | I | USA | 3006 | — | 51 | 49 | Other – 41% Black ‐ 35% White ‐ 17% Hispanic ‐ 7% |
— | — | — | — |
| Szilagyi 2013 | P | I | USA | 4115 | 14 | 50 | 50 | — | — | — | — | — |
| David 2012 | P | Physical activity | USA | 71 | 57 | 0 | 100 | White ‐ 93% Other ‐ 7% |
— | — | — | — |
| Dubbert 2002 | P | Physical activity | USA | 181 | 69 | 99 | 1 | — | — | Mean (SD) number of comorbidities IG: 3.8 (1.5) CG: 3.9 (1.4) |
Yes | USD 15 for completing each visit to help defray expenses |
| Jarvis 1997 | P | Physical activity | USA | 85 | 67 | 24 | 76 | Other ‐ 70% Black ‐ 30% |
— | Mean co‐morbidities: 3 | — | — |
| King 2007 | P | Physical activity | USA | 218 | 61 | 31 | 69 | White ‐ 90% Other ‐ 10% |
— | — | — | — |
| Morey 2009 | P | Physical activity | USA | 398 | 78 | 100 | 0 | White ‐ 77% Black ‐ 23% |
— | Mean (SD) number of diseases IG: 5.2 (2.5) CG: 5.5 (2.7) |
— | — |
| Morey 2012 | P | Physical activity | USA | 302 | 67 | 97 | 3 | White ‐ 70% | — | Mean (SD) number of comorbidities IG: 4.2 (2.4) CG: 3.9 (2.4) |
— | — |
| Pinto 2002 | P | Physical activity | USA | 298 | 46 | 28 | 72 | White ‐ 45% Black ‐ 45% Other ‐ 10% |
— | — | — | — |
| Sparrow 2011 | P | Physical activity | USA | 103 | 71 | 69 | 31 | — | — | Depression (unclear %) | — | — |
| Baker 2014 | P | Screening | USA | 450 | 60 | 28 | 72 | Hispanic 87% Other‐ 13% |
— | ≥ 1 long‐term conditions ‐ 68% | No | — |
| Cohen‐Cline 2014 | P | Screening | USA | 11,010 | 61 | 54 | 46 | White ‐ 86% Other ‐ 14% |
— | — | — | — |
| Corkrey 2005 | P | Screening | Australia | 75,532 | — | 0 | 100 | — | — | — | — | — |
| DeFrank 2009 | P | Screening | USA | 3547 | — | 0 | 100 | White ‐ 88% Black ‐ 11% Asian or Other ‐ 1% |
— | — | — | — |
| Durant 2014 | P | Screening | USA | 47,097 | 58 | 47 | 53 | — | — | — | — | — |
| Fiscella 2011 | P | Screening | USA | 469 | — | 56 (for colorectal cancer) |
44 (for colorectal cancer) |
White ‐ 61% Black ‐ 28% Latinos ‐ 5% Asian ‐ 5% |
— | — | — | — |
| Fortuna 2014 | P | Screening | USA | 1008 | — | 45 | 55 | White ‐ 48% Black ‐ 37% Other ‐ 15% |
— | — | No | — |
| Hendren 2014 | P | Screening | USA | 366 | — | — | — | White ‐ 50% Black ‐ 41% Other (including Hispanic) ‐ 9% |
— | — | — | — |
| Heyworth 2014 | P | Screening | USA | 4685 | 57 | 0 | 100 | — | — | Anticonvulsants ‐ 6% Corticosteroids ‐ 4% COPD (unclear %) Oophorectomy ‐ 3% |
— | — |
| Mosen 2010 | P | Screening | USA | 6000 | 60 | 50 | 50 | White ‐ 93% Other ‐ 7% |
— | Obesity ‐ 40% | — | — |
| Phillips 2015 | P | Screening | USA | 685 | 58 | 38 | 62 | Non‐Hispanic white ‐ 78% Black ‐ 13% Other ‐ 9% |
— | — | — | — |
| Simon 2010a | P | Screening | USA | 20,936 | 57 | 47 | 53 | White ‐ 86% Other ‐ 9% Black ‐ 5% |
— | — | — | — |
| Solomon 2007 | P | Screening | USA | 1973 | 69 | 8 | 92 | — | — | Use of oral glucocorticoids ‐ 22% Fractures ‐ 12% |
— | — |
| Mahoney 2003 | P | Stress management | USA | 100 (caregiver) | 63 (caregiver) | 22 (caregiver) | 78 (caregiver) | Black ‐ 64% Hispanic ‐ 21% White ‐ 15% Other ‐ 1% |
— | — | — | — |
| Aharonovich 2012 | P | Substance use | USA | 33 | 46 | 76 | 24 | White ‐ 64% White ‐ 15% Hispanic ‐ 21% |
— | HIV medication ‐ 64% Hepatitis A, B, or C ‐ 49% |
Yes | USD 20 gift certificates for each assessment |
| Bennett 2012 | P | Weight management | USA | 365 | 55 | 31 | 69 | Black ‐ 71% Hispanic ‐ 13% White ‐ 4% Other ‐ 2% |
— | Cholesterol medication ‐ 36% Diabetes medication ‐ 30% Mean BMI ‐ 37 kg/m2 |
Yes | USD 50 reimbursement at the first 3 follow‐up visits and USD 75 at 24 months |
| Bennett 2013 | P | Weight management | USA | 194 | 35 | 0 | 100 | Black ‐ 100% | — | Hypertension ‐ 36% Metabolic syndrome ‐ 31% Depression ‐ 22% Diabetes mellitus ‐ 7% |
Yes | Reimbursements of USD 50 each at baseline and at all follow‐up study visits |
| Estabrooks 2008 | P | Weight management | USA | 77 | 59 | 29 | 71 | White ‐ 68% Hispanic ‐ 18% Other ‐ 7% Black ‐ 4% Asian ‐ 3% |
— | — | — | — |
| Estabrooks 2009 | P | Weight management | USA | 220 | 11 | 54 | 46 | White‐ 63% Hispanic ‐ 26% Other ‐ 11% |
— | — | — | — |
| Goulis 2004 | P | Weight management | Greece | 122 | 44 | 12 | 88 | — | — | Hypertension ‐ 13% Diabetes mellitus ‐ 2% |
— | — |
| Vance 2011 | P | Weight management | USA | 140 | — | — | — | — | — | — | — | — |
| Wright 2013 | P | Weight management | USA | 50 (child) | 10 (child) 40 (parent) |
58 (child) 4 (parent) | 42 (child) 96 (parent) | Black ‐ 72% Other ‐ 22% White ‐ 6% (parent) |
— | BMI (child) ‐ 25.7 kg/m2 BMI (parent) ‐ 34 kg/m2 |
Yes | For completing assessments (USD 40 parents; USD 10 child) |
| Dini 1995 | E | Appointment reminder | USA | 517 | — | — | — | — | — | — | — | — |
| Griffin 2011 | E | Appointment reminder | USA | 3610 | 63 | 95 | 5 | White ‐ 83% Other ‐ 16% Hispanic ‐ 1% |
— | — | — | — |
| Maxwell 2001 | E | Appointment reminder | USA | 2304 | 29 | — | 100 | Hispanic ‐ 66% Black ‐ 19% White ‐ 13% Other ‐ 2% |
— | — | — | — |
| Parikh 2010 | E | Appointment reminder | USA | 12,092 | 56 | 43 | 57 | — | — | — | — | — |
| Reekie 1998 | E | Appointment reminder | UK | 1000 | — | 33 | 67 | — | — | — | — | — |
| Tanke 1994 | E | Appointment reminder | USA | 2008 | 19d | 54 | 46 | Spanish‐speaking ‐ 39% Vietnamese‐speaking ‐ 28% English‐speaking ‐14% Other – 13% Tagalog‐speaking Filipino – 6% |
— | — | — | — |
| Tanke 1997 | E | Appointment reminder | USA | 701 | < 12e | 45 | 55 | English‐speaking ‐ 59% Spanish‐speaking ‐ 29% Vietnamese‐speaking ‐ 3% Other – 9% |
— | — | — | — |
| Moore 2013 | M | Illicit drugs addiction | USA | 36 | 41 | 58 | 42 | White ‐ 58% Black ‐ 28% Other – 14% |
On methadone treatment mean = 21.7 | — | Yes | USD 20 per week for completing weekly assessments and providing a urine sample |
| Andersson 2012 | M | Alcohol consumption | Sweden | 1423 | — | — | — | — | — | — | — | — |
| Hasin 2013 | M | Alcohol consumption | USA | 254 | 46 | 78 | 22 | Black ‐ 49% Hispanic ‐ 45% Other – 6% |
12.8y | HIV/AIDS (unclear %) | Yes | USD 20; USD 40 at last 2 post‐treatment follow‐ups |
| Helzer 2008 | M | Alcohol consumption | USA | 338 | 46 | 64 | 36 | White ‐ 97% | Currently dependent ‐ 67% | — | Yes | USD 30 for the index, USD 25 for the 3‐month, and USD 60 for the 6‐month assessment |
| Litt 2009 | M | Alcohol consumption | USA | 110 | 49 | 58 | 42 | White ‐ 86% Black ‐9%, Hispanic‐3% Other‐2% |
Mean of 1.2 (SD 2.4) treatments for alcohol dependence | — | Yes | The possible total incentive was USD 50.00 per week |
| Mundt 2006 | M | Alcohol consumption | USA | 60 | 42 | 55 | 45 | White ‐ 95% Black ‐5% |
52.3 heavy drinking days within past 3 months | — | Yes | Patients were paid USD 75 for the 30‐day follow‐up, USD 125 for the 90‐day follow‐up, and USD 200 for the 180‐day follow‐up |
| Rose 2015 | M | Alcohol consumption | USA | 158 | 49 | 53 | 47 | — | Regular alcohol use mean = 17.94 years | — | Yes | USD 25 for each interview |
| Rubin 2012 | M | Alcohol consumption | USA | 47 | 57 | 60 | 40 | Caucasian ‐ 83% African‐American ‐ 13% | — | — | — | — |
| Simpson 2005 | M | Alcohol consumption | USA | 98 | 46 | 91 | 9 | White ‐ 45% Black ‐ 40% Native American ‐ 7% Other ‐ 6% Hispanic ‐ 2% |
— | — | Yes | USD 25.00 each for the baseline and for the follow‐up assessments |
| Vollmer 2006 | M | Asthma | USA | 6948 | 52 | 35 | 65 | White ‐ 92% Other ‐ 8% |
— | Beta agonist ‐ 55% Oral steroids ‐ 46% COPD ‐ 33% |
— | — |
| Xu 2010 | M | Asthma | Australia | 121 | 7 | 53 | 47 | — | — | — | — | — |
| Cleeland 2011 | M | Cancer | USA | 79 | 60 | 53 | 47 | White ‐ 85% Black ‐ 15% |
— | — | — | — |
| Kroenke 2010 | M | Cancer | USA | 405 | 59 | 32 | 68 | White ‐ 80% Black‐ 18% Other ‐ 2% |
— | Depression ‐ 76% Pain ‐ 68% |
— | — |
| Mooney 2014 | M | Cancer | USA | 250 | 55 | 24 | 76 | White/Caucasian ‐ 91% Other ‐ 9% |
— | — | — | — |
| Siegel 1992 | M | Cancer | USA | 239 | 58 | 50 | 50 | White ‐ 89% Black‐ 6% Hispanic ‐ 4% Other 1% |
Mean (SD) time since cancer diagnosis‐ IG: 36 months (35) CG: 26 months (32) |
Mean (SD) symptoms (out of 13) IG: 3.4 (2.2) CG: 4.0 (2.4) |
— | — |
| Sikorskii 2007 | M | Cancer | USA | 437 | 57 | 25 | 75 | — | — | Mean comorbidities: 2 | — | — |
| Spoelstra 2013 | M | Cancer | USA | 119 | 60 | 31 | 69 | White ‐ 76% Asian ‐ 17 % Black ‐ 7% |
— | Capecitabine ‐ 35% Erlotinib ‐ 24% Lapatinib ‐ 9% Imatinibf ‐ 8% Temozolomide ‐ 6% Sunitinib ‐ 5% Sorafenib ‐ 2.5% Methotrexate ‐ 1.7% Cyclophosphamide ‐ 0.8% |
— | — |
| Yount 2014 | M | Cancer | USA | 253 | 61 | 49 | 51 | White ‐ 58% Black ‐ 36% Other ‐ 6% | — | Planned single chemotherapy ‐ 9% Planned combination chemotherapy ‐ 90% |
— | — |
| Kroenke 2014 | M | Chronic pain | USA | 250 | 55 | 83 | 17 | White ‐ 77 % | ≤ 5 years = 29% 6‐10 years = 19% > 10 years = 52% |
Major depression‐ 24% Post‐traumatic stress disorder‐ 17% |
— | — |
| Naylor 2008 | M | Chronic pain | USA | 55 | 46 | 14 | 86 | White ‐ 96% Other ‐ 4% |
— | — | — | — |
| Halpin 2009 | M | COPD | UK | 79 | 69 | 74 | 26 | — | — | SABA ‐ 75% LAMA ‐ 43% LABA/ICS ‐ 43% ICS ‐ 33% SAMA ‐ 32% Oral steroids ‐ 25% LABA ‐ 18% |
— | — |
| Adams 2014 | M | Adherence | USA | 475 | 5 (child) 35 (parent) | 52 (child) 7 (parent) | 48 (child) 93 (parent) | Black ‐ 67% (child) 47% (parent); Other – 33% (child) 53% (parent) |
— | — | Yes | Gift cards |
| Bender 2010 | M | Adherence | USA | 50 | 42 | 36 | 64 | White ‐ 58% Black ‐ 20% Hispanic ‐ 18% Asian ‐ 4% |
— | — | Yes | USD 25 for each completed visit |
| Bender 2014 | M | Adherence | USA | 1187 | — | — | — | — | — | — | — | — |
| Boland 2014 | M | Adherence | USA | 70 | 66 | 49 | 51 | African American ‐ 58% European ‐ 32% Asian ‐ 6% Hispanic ‐ 3% Middle Eastern ‐ 1% |
Median 5 years in IG; 4.5 years in CG | Bimatoprost ‐ 11.5% Travoprost ‐ 17.5% Latanoprost ‐ 71.5% Bilateral medication ‐ 70% |
— | — |
| Cvietusa 2012 | M | Adherence | USA | 1393 | — | — | — | — | — | — | — | — |
| Derose 2009 | M | Adherence | USA | 13,057 | 51 | 54 | 46 | Other ‐ 48 % White ‐ 23% Hispanic ‐ 14% Black ‐ 10% Asian ‐ 5% |
— | — | — | — |
| Derose 2013 | M | Adherence | USA | 5216 | 56 | 49 | 51 | Hispanic ‐ 30% White ‐ 28% Unknown ‐ 23% Black ‐ 10% Asian and Pacific Islander ‐ 7.1% Other ‐ 1.7% Native American‐ 0.2% |
— | Mean low‐density lipoproteins = 146 mg/dL | — | — |
| Feldstein 2006 | M | Adherence | USA | 961 | 59 | 47 | 53 | — | — | Statins ‐ 32% Depression ‐ 11% |
— | — |
| Friedman 1996 | M | Adherence | USA | 267 | 77 | 23 | 77 | Other ‐ 89 % Black: 11% |
— | Other – 81% Heart disease ‐ 32% Diabetes mellitus ‐ 18% Stroke ‐ 7% |
— | — |
| Glanz 2012 | M | Adherence | USA | 312 | 63 | 62 | 38 | Black ‐ 91% White ‐ 9% |
— | — | Yes | USD 25 gift card |
| Green 2011 | M | Adherence | USA | 8306 | — | — | — | — | — | — | — | — |
| Ho 2014 | M | Adherence | USA | 241 | 64 | 98 | 2 | White ‐ 78% | — | Hypertension ‐ 91% Hyperlipidaemia ‐ 85% Diabetes mellitus ‐ 45% Chronic kidney disease ‐ 23% Chronic lung disease ‐ 20% Prior heart failure ‐ 12% Peripheral arterial disease ‐ 10% Cerebrovascular disease ‐ 7% |
— | — |
| Leirer 1991 | M | Adherence | USA | 16 | 71 | 31 | 69 | — | — | — | Yes | USD 25 for participating |
| Lim 2013 | M | Adherence | USA | 80 | 66 | 51 | 49 | White ‐ 62% African‐American ‐ 10% Hispanic/Latino ‐ 9% Asian ‐ 9% East Indian ‐ 6% |
Mean IG: 25.79 months; CG: 22.1 months |
Number of medical problems: IG: 3.43 CG: 3.32 |
— | — |
| Migneault 2012 | M | Adherence | USA | 337 | 57 | 30 | 70 | Black ‐ 100% | — | BMI ‐ 34.4 kg/m2 Diabetes ‐ 38% Stroke ‐ 7.5% |
— | — |
| Mu 2013 | M | Adherence | USA | 4,237,821 | 56 | 38.5 | 61.5 | — | — | Correspondence with the author: "All participants were on maintenance medications" | — | — |
| Ownby 2012 | M | Adherence | USA | 27 | 80 | — | — | — | — | Participants had cognitive (memory) impairment and were on donepezil, rivastigmine, or galantamine | — | — |
| Patel 2007 | M | Adherence | USA | 15,051 | 57 | 53 | 47 | — | — | — | — | — |
| Reynolds 2011 | M | Adherence | USA | 30,610 | — | — | — | — | — | — | — | — |
| Sherrard 2009 | M | Adherence | Canada | 331 | 63 | — | — | — | — | — | — | — |
| Simon 2010b | M | Adherence | USA | 1200 | 51 | 62 | 38 | Other ‐ 95% Black ‐ 5% |
— | Insulin ‐ 19.4% (participants) | — | — |
| Stacy 2009 | M | Adherence | USA | 497 | 54 | 38 | 62 | — | — | Lipitor – 54% Zocor – 16% Other statin – 16% |
— | — |
| Stuart 2003 | M | Adherence | USA | 647 | — | — | — | — | — | — | — | — |
| Vollmer 2011 | M | Adherence | USA | 8517 | 54 | 34 | 66 | White ‐ 50% Other – 26% Asian ‐ 11% Mixed – 7% Native Hawaiian/Pacific Islander ‐ 4% Black ‐ 2% American Indian/Alaskan Native – 1% |
— | COPD ‐ 33% | — | — |
| Vollmer 2014 | M | Adherence | USA | 21,752 | 64 | 53 | 47 | White ‐ 47% Asian ‐ 17% Black ‐15% Native Hawaiian/Pacific Islander ‐ 11% Black ‐ 2% American Indian/Alaskan Native – 1% |
— | Diabetes mellitus ‐ 78% CVD ‐ 36% Statin only ‐ 40% ACEI/ARB only ‐ 25% Statin and ACEI/ARB ‐ 35% low‐density lipoproteins among statin users (mean) = 93.4 mg/dL |
— | — |
| Graziano 2009 | M | Diabetes mellitus | USA | 119 | 62 | 55 | 45 | White ‐ 77% Other – 23% |
— | — | Yes | USD 25 |
| Homko 2012 | M | Diabetes mellitus | USA | 80 | 30 | 0 | 100 | White ‐ 41% Black ‐ 34% Hispanic ‐ 18% Asians or others ‐ 7% |
— | BMI ‐ 34.1 kg/m2 | — | — |
| Katalenich 2015 | M | Diabetes mellitus | USA | 98 | 59 | 40 | 60 | Black ‐ 65% White ‐ 30% Other ‐ 3% Hispanic ‐ 1% Asian ‐ 1% |
— | Other antidiabetic medications + insulin ‐ 80% Basal‐bolus regimen ‐ 40% Long‐acting insulin only ‐ 33% Mixed insulin only ‐ 17% Short‐acting insulin only ‐ 10% |
— | — |
| Khanna 2014 | M | Diabetes mellitus | USA | 75 | 52 | 59 | 41 | Hispanic ‐ 100% | — | — | Yes | USD 10 for initial visit and USD 20 incentive card at the follow‐up |
| Kim 2014 | M | Diabetes mellitus | USA | 100 | — | — | — | — | — | Psychiatric illness ‐ 46% Had been hospitalised over the past year ‐ 28% |
— | — |
| Lorig 2008 | M | Diabetes mellitus | USA | 417 | 53 | 38 | 62 | Hispanic ‐ 100% | — | — | — | — |
| Piette 2000 | M | Diabetes mellitus | USA | 248 | 55 | 41 | 59 | Hispanic ‐ 50% White ‐ 29% Other – 21% |
— | BMI ‐ 33.7 kg/m2 Mean comorbidities: 1 |
— | — |
| Piette 2001 | M | Diabetes mellitus | USA | 272 | 61 | 97 | 3 | White ‐ 60% Black ‐ 18% Hispanic ‐ 12% Other ‐ 10% |
— | BMI ‐ 31 kg/m2 Mean comorbidities: 2 |
— | — |
| Schillinger 2009 | M | Diabetes mellitus | USA | 339 | 56 | 43 | 57 | Hispanic ‐ 47% Asian ‐ 22% Black ‐ 20% White ‐ 8% Other ‐ 2% |
— | BMI: 31 kg/m2 | Yes | USD 15 and USD 25 for the baseline and 1‐year follow‐up visits, respectively |
| Williams 2012 | M | Diabetes mellitus | Australia | 120 | 57 | 63 | 37 | — | — | Low depression – 73% Intermediate depression – 23% High depression – 4% Low anxiety – 89% Intermediate anxiety – 8% High anxiety – 3% BMI ‐ 33 kg/m2 Insulin – 43% |
— | — |
| Capomolla 2004 | M | Heart failure | Italy | 133 | 57 | 88 | 12 | — | — | Diuretics ‐ 89% ACE inhibitors ‐ 84% Carvedilol ‐ 50% Nitrates ‐ 40% Digitalis ‐ 33% K + saver ‐ 21% |
— | — |
| Chaudhry 2010 | M | Heart failure | USA | 1653 | 61d | 58 | 42 | White ‐ 49% Black ‐ 39% Other – 12% (inclusive of Hispanic or Latino – 3%) |
— | Beta‐blocker – 79% Loop diuretic – 78% Hypertension ‐ 77% ACE inhibitor or ARB – 70% Coronary artery disease ‐ 50% Diabetes mellitus ‐ 47% Chronic kidney disease ‐ 46% Aldosterone‐receptor antagonist – 33% Digoxin – 25% COPD ‐ 21% |
No | — |
| Krum 2013 | M | Heart failure | Australia | 405 | 73 | 63 | 37 | — | — | Diuretics ‐ 80% Heart failure specific beta‐blockers ‐ 61% Systolic heart failure ‐ 60% Hypertension ‐ 60% ACE inhibitors ‐ 57.5% Atrial fibrillation ‐ 37.5% Diabetes mellitus ‐ 30.5% Aldosterone antagonist ‐ 26% ARB ‐ 25% Diastolic heart failure ‐ 18.5% Pacemaker ‐ 12% Internal cardio defibrillator ‐ 4.5% |
— | — |
| Kurtz 2011 | M | Heart failure | France | 138 | 68 | 79 | 21 | — | — | Loop diuretic – 92% ACE/AT2– 79% Beta‐blocker – 79% Spironolactone – 29% Digoxin – 9% (mean values) |
— | — |
| Shet 2014 | M | HIV | India | 631 | — | 57 | 43 | Asian ‐100% | — | Zidovudine‐based antiretroviral treatment – 44% Tenofovir‐based antiretroviral treatment – 44% Stavudine‐based antiretroviral treatment – 12% |
Yes | Mobile phone plus wage compensation |
| Hyman 1996 | M | Hypercholestorolaemia | USA | 115 | 48 | 25 | 75 | White ‐ 87% Other – 13% |
— | — | — | — |
| Hyman 1998 | M | Hypercholesterolaemia | USA | 123 | 57 | 25 | 75 | Black ‐ 77% Other – 23% |
— | Mean BMI ‐ 31 kg/m2 | — | — |
| Bove 2013 | M | Hypertension | USA | 241 | 60 | 21 | 79 | Black ‐ 81% White‐ 15% Hispanic ‐ 3% Other ‐ 1% |
— | Hyperlipidaemia ‐ 46% Diabetes ‐ 32% |
— | — |
| Dedier 2014 | M | Hypertension | USA | 253 | 58 | 27 | 73 | Black ‐ 100% | — | — | — | — |
| Harrison 2013 | M | Hypertension | USA | 64,773 | 61 | 46 | 54 | White ‐ 41%, Hispanic ‐ 25% Black ‐ 17% Other – 9% Asian ‐ 8% |
— | Cardiovascular disease ‐ 38% Diabetes mellitus ‐ 27% Chronic kidney disease ‐ 10% |
— | — |
| Magid 2011 | M | Hypertension | USA | 283 | 66 | 65 | 35 | White ‐ 65% Other – 18% Hispanic ‐ 17% |
— | Diabetes mellitus or chronic kidney disease – 55% | Yes | Clinically validated electronic blood pressure cuffs were provided at no cost to those who did not own one |
| Piette 2012 | M | Hypertension | Honduras; Mexico | 200 | 58 | 33 | 67 | — | — | Blood pressure medication – 83% Diabetes mellitus ‐ 23% BMI ‐ 30.7 kg/m2 |
— | — |
| Farzanfar 2011 | M | Mental health | USA | 164 | 39 | 24 | 76 | White ‐ 56% Black ‐ 32% Other – 12% |
— | — | — | — |
| Greist 2002 | M | Mental health | USA | 218 | 39 | 58 | 42 | White ‐ 93% Other – 7% |
— | Social phobia ‐ 9%, Generalised anxiety disorder ‐8% Simple phobia – 6% Major depression – 2% Dysthymia – 2% |
— | — |
| Zautra 2012 | M | Mental health | USA | 73 | 54 | 18 | 82 | Other – 74% Hispanic – 26% |
— | — | — | — |
| DeMolles 2004 | M | OSAS | USA | 30 | 46 | — | — | — | — | BMI ‐ 38 kg/m2 | — | — |
| Sparrow 2010 | M | OSAS | USA | 250 | 55d | 82 | 18 | — | — | BMI ‐ 35.1 kg/m2 | — | — |
| Brendryen 2008 | M | Smoking | Norway | 396 | 36 | 47 | 53 | — | — | — | Yes | All participants in both groups received a sample packet of nicotine replacement therapy products. |
| Carlini 2012 | M | Smoking | USA | 521 | 36 | 36 | 64 | White ‐ 81% Black ‐ 6% Other – 5% Hispanic/Latino ‐ 4% Native American – 3% Asian ‐ 1% |
— | ≥ 1 long‐term conditions ‐ 47% | No | — |
| Ershoff 1999 | M | Smoking | USA | 332 | 30 | 0 | 100 | White ‐ 61% Black ‐ 16% Hispanic ‐ 15% Other – 8% |
— | — | — | — |
| McNaughton 2013 | M | Smoking | Canada | 44 | 53 | 67 | 33 | — | Mean cigarettes/d: intervention ‐ 18.5 control ‐ 17.3 |
— | — | — |
| Peng 2013 | M | Smoking | Taiwan | 116 | 20 | 92 | 8 | Asian ‐ 100% | — | — | Yes | Equivalent of USD 6 |
| Regan 2011 | M | Smoking | USA | 731 | 52 | 56 | 44 | — | — | — | — | — |
| Reid 2007 | M | Smoking | Canada | 100 | 54 | 68 | 32 | — | — | Acute coronary syndrome ‐ 83% | — | — |
| Reid 2011 | M | Smoking | Canada | 440 | — | — | — | — | — | — | — | — |
| Rigotti 2014 | M | Smoking | USA | 397 | 53 | 48 | 52 | White ‐ 81% Hispanic ‐ 6% Black ‐ 4% Other/unknown ‐ 4% Native American ‐ 3% Asian/Pacific Islander ‐2.5% |
Mean cigarettes/d: IG = 17.1 CG = 16.3 |
Depressive symptoms (mean) IG = 9.3 CG = 10.3 |
Yes | USD 50 for a saliva sample |
| Velicer 2006 | M | Smoking | USA | 2054 | 51 | 77 | 23 | White ‐ 89%, Black ‐ 5%, Other ‐ 4% Native American ‐ 2% |
Mean cigarettes/d IG = 23.85 CG = 25.18 |
— | — | — |
| Houlihan 2013 | M | Spinal cord dysfunction | USA | 142 | 48 | 61 | 39 | White ‐ 80% (inclusive of Hispanic or Latino – 7%) Black ‐ 11% Other ‐ 9% |
11.7 y | Depression – 39% Pressure ulcers ‐ 7% |
— | — |
aStudy type: P: prevention; M: management; E: either. bStudy subtype: COPD: chronic obstructive pulmonary disease; HIV: human immunodeficiency virus; I: immunisation; LAMA: long‐acting muscarinic antagonist; OSAS: obstructive sleep apnoea syndrome; SABA: short‐acting β 2‐agonist; SAMA: short‐acting muscarinic antagonist
cPlease note that for reporting of participants' ethnicity, the terms used by authors of the included studies have been used in each case and are cited directly from each of the included studies. dMedian. eMajority of the participants. Other abbreviations: CG: control group; IG: intervention group.
3. Intervention.
| Study ID | ATCSa | Contentb | Theoryc | BCTsd | Received instructions? | Callere | Telephone keypadf | Toll free | Study duration | Call durationg | Frequencyh | Intensity i | Speaker features | Security arrangementj |
| Adams 2014 | IVR | AF | — | 1 | — | P | Other | — | 25 months | 29.3 min | — | — | Synthetic speech | — |
| Aharonovich 2012 | ATCS Plus | AF,SF | MI | 9, 25, 40 | Yes | E | Yes | Yes | 2 months | 1‐3 min | Daily | — | — | — |
| Andersson 2012 | IVR | AF | — | 25 | — | — | — | — | 1.5 months | — | — | < 500 words | — | — |
| Baker 2014 | Unidirectional¹ | AF | TCD | 1, 42 | No | H | — | — | 6 months | — | 2 | 92 words | — | — |
| Bender 2010 | IVR | AF | HBM | 20, 21, 42 | — | H | Yes | Yes | 2.5 months | < 5 min | 2 | — | — | — |
| Bender 2014 | IVR | AF | — | 20,21 | — | — | — | — | 24 months | — | — | — | — | — |
| Bennett 2012 | ATCS Plus | AF, CF | SCT, TRA, TTM | 3, 9, 12, 13, 17, 20, 21, 25, 33, 39, 40, 42 | — | — | — | — | 24 months | — | — | — | — | — |
| Bennett 2013 | ATCS Plus¹ | AF, CF | SCT, TRA, TTM, MI | 3, 9, 12, 13, 17, 20, 21, 25, 33, 39, 40, 42 | — | H | — | — | 12 months | 2–4 min | Weekly | — | — | — |
| Boland 2014 | IVR | AF | — | 29,42 | — | H | Yes | — | 3 months | — | Daily | 51 words | — | Reminder information was sent securely to Memotext¹ |
| Bove 2013 | ATCS Plus¹ | AF, CF, SF | — | 9,10,42 | Yes | P | Yes¹ | Yes | 6 months | — | Biweekly | — | — | Password and log‐in |
| Brendryen 2008 | ATCS Plus¹ | AF, SF | CBT, SCT, MI, SRT, SCL, RP | 3,12, 20,27, 34, 39 | Yes | P | Yes | — | 24 months | — | Twice daily then biweekly¹ for 6 weeks | — | Personal pronouns and active voice | — |
| Capomolla 2004 | ATCS Plus | AF, CF | — | 20, 42 | Yes | P | Yes | Yes | 12 months | — | Daily | — | — | PIN² |
| Carlini 2012 | ATCS Plus | AF, CF | — | 3 | — | H | Yes | Yes | 4 months | — | — | — | — | — |
| Chaudhry 2010 | ATCS Plus | AF, CF | — | 20, 42 | Yes | P | Yes | Yes | 6 months | — | Daily | — | — | — |
| Cleeland 2011 | ATCS Plus | AF, SF | — | 21 | Yes | H | Yes | — | 1 month | 4 weeks | Biweekly | — | — | — |
| Cohen‐Cline 2014 | IVR | AF | — | 1,42 | — | H | — | — | 12 months | 5 min¹ | 1 | — | — | — |
| Corkrey 2005 | ATCS Plus | AF, CF | — | 3, 27, 39 | Yes | H | Yes | — | 6 months | — | — | — | — | — |
| Cvietusa 2012 | ATCS Plus | AF, CF | — | 29,42 | — | H | Other | — | 12 months | — | ≤ 3 | — | — | — |
| David 2012 | ATCS Plus | AF, CF | TTM, SCT, PST | 3,10 | Yes | E | — | — | 3 months | 15‐30 s² | Twice daily | — | — | — |
| Dedier 2014 | IVR | AF | TTM, SCT | 1,9 | — | H | — | — | 3 months | 10 min | Weekly | — | Pre‐recorded human speech | — |
| DeFrank 2009 | IVR | AF | HBM¹ | 27, 42 | — | H | Yes | — | 24 months | 69 s | Average ‐ 3 | 224 words | Female voice | Verification³ |
| DeMolles 2004 | IVR | AF | — | 3, 18, 20, 40, 42 | Yes | P | Yes | — | 2 months | — | 3‐day call², weekly | — | — | Password protected⁴ |
| Derose 2009 | ATCS Plus | AF, SF | — | 40, 42 | — | H | Yes | Yes | 6 months | 40 s | 1 | 100 words | — | PIN⁵ |
| Derose 2013 | ATCS Plus | AF, SF | — | 40, 42 | — | H | — | Yes | 3 months | 40 s | 1 | — | — | — |
| Dini 1995 | Unidirectional | AF | — | 40 | No | H | — | — | 1 months | — | 1 | — | — | — |
| Dini 2000 | Unidirectional | AF | — | 42 | No | H | — | — | 36 months | — | 1³ | — | — | — |
| Dubbert 2002 | Unidirectional¹ | AF | TTM | 9,10,40 | — | H | — | — | 10 months | — | — | Approx 30 words | Nurse | — |
| Durant 2014 | IVR | AF | — | 42 | — | H | — | — | 2 weeks | — | 1‐2 attempts | — | — | — |
| Ershoff 1999 | IVR | AF | TTM | 20, 39 | Yes | P | Yes | Yes | 34 weeks | 5 min | — | — | Professional | Password protected⁴, PIN² |
| Estabrooks 2008 | IVR | AF | — | 3, 9 | Yes | — | — | — | 3 months | 1‐10 min³ | Weekly | — | — | — |
| Estabrooks 2009 | ATCS Plus | AF, CF | GM | 2, 3, 9, 15, 20 | — | E | — | — | 12 months | — | 10 | — | — | — |
| Farzanfar 2011 | IVR | AF | — | 3, 6, 20, 30, 39, 42 | Yes | E | Yes | Yes | 6 months | 30‐90 min² | Monthly | — | Female voice actor | Password protected⁴ |
| Feldstein 2006 | IVR | AF | — | 39, 42 | — | — | — | — | 25 days | — | — | — | — | PIN⁶ |
| Fiscella 2011 | ATCS Plus¹ | AF, CF | — | 20,42 | — | H | — | — | 26 weeks | — | Up to 4 | — | — | — |
| Fortuna 2014 | Unidirectional | AF | — | 29,30 | — | H | — | — | 12 months | — | 2 | — | — | — |
| Franzini 2000 | Unidirectional | AF | — | 40,42 | No | H | — | — | — | — | — | — | — | — |
| Friedman 1996 | IVR | AF | SCT | 21, 32, 35, 39 | — | E | Yes | Yes | 6 months | 4 min | Weekly | — | — | Password protected⁴ |
| Glanz 2012 | IVR | AF | — | 3,16 | — | E | Other | — | 9 months | — | 12 | — | — | — |
| Goulis 2004 | IVR | AF | — | 1, 10, 20, 21, | Yes | — | — | — | 6 months | 15 min | Weekly | — | — | — |
| Graziano 2009 | IVR | AF | HBM | 3, 7, 20, 21, 42 | — | H | — | — | 12 months | > 1 min | Daily | — | Trained actor | PIN⁷ |
| Green 2011 | IVR | AF | — | 16 | — | H | Yes | — | — | — | — | — | — | — |
| Greist 2002 | ATCS Plus | AF, SF | BT | 34 | — | E | Yes | — | 3 months | 8.6 min¹ | 12 | — | — | — |
| Griffin 2011 | ATCS Plus | AF, CF | HBM, SMP | 3, 7, 27, 30, 40 | — | H | — | — | 6W | — | 1 | — | — | — |
| Halpin 2009 | ATCS Plus | AF, CF, SF | — | 21, 40, 42 | Yes | H | — | — | 4 months | — | Daily, 4⁴ | — | — | — |
| Harrison 2013 | Unidirectional | AF | — | 20,42 | — | H | — | — | 1 month | — | — | 80 words | — | — |
| Hasin 2013 | ATCS Plus | AF, CF, SF | MI | 9,12 | Yes | P | — | Yes | 12 months | 60 days | Daily | 1‐3 min | — | — |
| Helzer 2008 | ATCS Plus | AF,CF | — | 20,34 | Yes | P | Yes | Yes | 6 months | 2 min | Daily | — | — | — |
| Hendren 2014 | ATCS Plus¹ | AF, CF | — | 20,42 | — | H | — | — | 25 weeks | 25 s | Up to 4 | — | — | — |
| Hess 2013 | Unidirectional | AF | — | 16 | — | H | — | — | 3 months | 1 min | Monthly | 2 30‐s scripts | — | — |
| Heyworth 2014 | ATCS Plus | AF, CF | — | 16 | — | H | — | — | 3 months | 4‐5 min | 1 | — | — | — |
| Ho 2014 | ATCS Plus¹ | AF, CF | — | 20,42 | — | H | — | — | 12 months | — | Monthly⁵ | — | — | — |
| Homko 2012 | IVR | AF | — | 21 | Yes | P | Yes | Yes | 26 months | — | Weekly | 45 s of speaking | — | PIN² |
| Houlihan 2013 | IVR | AF | TTM, SCT | 4,20,21 | Yes | H | — | — | 6 months | 4.12 min | Weekly | 12.4 calls¹ | Digitised speech | — |
| Hyman 1996 | IVR | AF | — | 20, 39, 42 | — | E | Yes | — | 6 months | — | Daily | — | — | — |
| Hyman 1998 | ATCS Plus | AF, CF | SCT | 20, 39, 42 | — | E | Yes | — | 6 months | 2‐3 min | Biweekly | — | — | — |
| Jarvis 1997 | IVR | AF | TTM | 7, 9, 20, 39 | Yes | P | Yes | — | 3 months | — | Weekly | — | — | Password protected⁴ |
| Katalenich 2015 | ATCS Plus | AF,CF, SF | — | 16,21,30 | — | E | — | — | 6 months | — | Daily | — | — | — |
| Khanna 2014 | ATCS Plus | AF, SF | — | 20 | Yes | H | Yes | — | 3 months | — | 2.2/week | 26 calls¹ | Female voice | — |
| Kim 2014 | ATCS Plus | AF, CF | — | 20,29,30 | — | H | — | — | 12 months | ≤ 10 min | Weekly | — | — | — |
| King 2007 | IVR | AF | SCT, TTM | 3, 9, 20, 39 | Yes | H | Yes | — | 12 months | 10‐15 min | Weekly⁶ | — | — | — |
| Kroenke 2010 | ATCS Plus¹ | AF, CF | TCM | 39 | — | E | — | — | 12 months | — | Biweekly, weekly, bimonthly, monthly⁷ | — | — | — |
| Kroenke 2014 | ATCS Plus¹ | AF, CF | — | 21,39 | — | H | — | — | 12 months | — | Weekly⁸ | — | — | — |
| Krum 2013 | ATCS Plus | AF, CF, SF | — | 20,21,42 | — | E | Yes | — | 12 months | — | Monthly | 18 questions | — | — |
| Kurtz 2011 | IVR | AF | — | 39 | No | P | Yes | — | 24 months | 48 s¹ | Weekly | — | — | — |
| LeBaron 2004 | ATCS Plus | AF, SF | — | 40, 42 | — | H | — | — | 24 months | — | — | — | — | — |
| Leirer 1991 | IVR | AF | — | 20,42 | Yes | H | Yes | — | 2 weeks | — | — | 3 segments | Personalised voice messages | — |
| Lieu 1998 | IVR | AF | — | 42 | — | H | — | — | 4 months | 96.8 s | — | — | — | — |
| Lim 2013 | Unidirectional | AF | — | 42 | — | H | — | — | 5 months | — | Monthly | — | — | — |
| Linkins 1994 | Unidirectional | AF | — | 42 | — | H | — | — | 5 months | — | 2/d⁹ | — | — | — |
| Litt 2009 | ATCS Plus | AF,SF | CBT | 3,20,34,38 | — | H | Yes | — | 12 weeks | 2.5 min | 8/d¹⁰ | — | — | — |
| Lorig 2008 | ATCS Plus | AF, CF | — | 21 | — | — | — | — | 15 months | 90 s | Monthly | — | — | — |
| Magid 2011 | ATCS Plus¹ | AF, CF | — | 20, 21, 25, 42 | Yes | P | Yes | — | 6 months | 5‐10 min | Weekly | — | — | — |
| Mahoney 2003 | ATCS Plus | AF, SF | PT, PM | 3, 13, 25, 39, 42 | Yes | P | Yes | Yes | 18 months | 18 min | — | 22 h/d² | Professional radio announcer | Password protected⁴ |
| Maxwell 2001 | Unidirectional | AF | — | 40 | No | H | — | — | 2 months | — | — | — | — | — |
| McNaughton 2013 | IVR | AF | — | 20, 21, 25, 34, 42 | — | H | Other | — | 24 months | 3‐5 min | Biweekly | — | — | — |
| Migneault 2012 | IVR | AF | SCT, TTM, MI | 25, 39 | Yes | — | Yes | Yes | 8 months | — | Weekly | — | African – American voice professionals | — |
| Mooney 2014 | ATCS Plus | AF, SF, CF | — | 21 | — | P | Yes | Yes | 1.5 months | 5.18 min¹ | Daily | — | — | Personalised password |
| Moore 2013 | ATCS Plus | AF, SF | CBT | 17,34,38 | Yes | H | Yes | — | 1 month | 9.3 min¹ | Daily | — | — | — |
| Morey 2009 | Unidirectional¹ | AF | SCT, TTM | 9, 10, 20, 25, 39 | — | H | — | — | 12 months | — | Monthly | Approx 60 words | Primary care provider | — |
| Morey 2012 | Unidirectional¹ | AF | SCT, TTM | 9, 10, 20, 25, 39 | — | H | — | — | 12 months | — | Monthly | Approx 60 words | Primary care provider | — |
| Mosen 2010 | IVR | AF | — | 27, 42 | — | H | Yes | Yes | 6 months | 1 min | 3 | — | — | — |
| Mu 2013 | IVR | AF | — | 25, 39 | — | H | — | — | 1 month | — | — | — | — | Correspondence with the author: "Upon answering a call, patients are required to authenticate with their date of birth." |
| Mundt 2006 | ATCS Plus | AF, CF, SF | CBT | 4,20,34,38 | Yes | E | — | Yes | 6 months | 9.2 min | Daily | — | — | Valid ID number and a personally selected 4‐digit pass code |
| Nassar 2014 | Unidirectional | AF | — | 29 | Yes | H | — | — | 2 months | — | At least every 3 days | Every hour for 2 consecutive hours | Community health worker | — |
| Naylor 2008 | IVR | AF | CBT | 3, 16, 20, 22, 25, 39, 42 | Yes | P | — | Yes | 4 months | 3‐16 min | Daily | — | Experienced therapist | — |
| Ownby 2012 | Unidirectional | AF | — | 42 | — | H | — | — | 24 months | — | Daily | — | First author | — |
| Parikh 2010 | IVR | AF | — | 40 | — | H | — | — | 4 months | — | — | — | — | — |
| Patel 2007 | IVR | AF | — | 39, 42 | — | — | — | — | 6 months | — | 3 | — | — | — |
| Peng 2013 | ATCS Plus | AF, SF | CBT, TTM, MI |
9, 0, 12, 20, 21 | — | H | Yes | — | 2 months | 18.9 min^^ | Biweekly weeks 1‐3, weekly weeks 4‐6, no call week 7, weekly week 8‐9 | 8.61²,³ | — | — |
| Phillips 2015 | IVR | AF | — | 29, 30 | — | H | — | — | 3.5 months | — | up to 5 times | — | — | — |
| Piette 2000 | ATCS Plus | AF, CF | SCT | 3, 18, 21, 25, 39 | No | E | Yes | Yes | 24 months | 1‐8 min² | Biweekly¹¹ | — | Human voice | PIN² |
| Piette 2001 | ATCS Plus | AF, CF | SCT | 3, 18, 21, 25, 39 | — | H | Yes | — | 12 months | 1‐8 min² | Biweekly¹¹ | — | — | — |
| Piette 2012 | ATCS Plus | AF, CF | — | 13, 20, 21, 39 | Yes | — | Yes | Yes | 1.5 months | ≤ 9 min | Weekly | — | Native speaker | — |
| Pinto 2002 | ATCS Plus | AF, SF | DMT, SCT, TTM | 3, 19, 20, 32 | Yes | P | Yes | — | 6 months | 10 min | Weekly (first 3 months), and at least biweekly thereafter | — | Digitised human speech | — |
| Reekie 1998 | Unidirectional | AF | — | 39, 40 | No | H | — | — | — | — | — | — | Receptionist | — |
| Regan 2011 | ATCS Plus | AF, CF | — | 20, 42 | — | H | — | — | 3 months | — | — | — | — | — |
| Reid 2007 | ATCS Plus | AF, CF | — | 3, 9, 13, 39, 40, 42 | — | H | — | — | 12 months | 1‐20 min⁵ | 3 | — | — | — |
| Reid 2011 | ATCS Plus | AF, CF | — | 20, 42 | — | — | — | — | 12 months | — | 8 | — | — | — |
| Reynolds 2011 | IVR | AF | — | 42 | — | P | — | — | — | — | — | — | — | — |
| Rigotti 2014 | ATCS Plus | AF, CF, SF | — | 13, 34 | — | H | — | Yes | 6 months | — | 5 times¹² | — | — | — |
| Rose 2015 | ATCS Plus | AF, CF, SF | CBT | 4, 20, 34, 38 | Yes | P | — | — | 4 months | — | Daily | — | — | — |
| Rubin 2012 | IVR | AF | MI | 9, 12 | — | H | Other | — | 6 months | — | ≤ 26 calls over 13 weeks | — | — | — |
| Schillinger 2009 | ATCS Plus | AF, CF | CCM, SCT | 1, 3, 9, 10, 13, 20, 21, 35, 39 | — | E | Yes | Yes | 12 months | 6‐12 min | Weekly | — | — | — |
| Sherrard 2009 | ATCS Plus | AF, CF | — | 27, 39, 42 | — | H | — | — | 6 months | — | 11 | — | — | Password protected⁴ |
| Shet 2014 | IVR¹ | AF | TPB | 16,20 | — | H | — | — | 24 months | — | Weekly | — | — | — |
| Siegel 1992 | IVR | AF | — | 17, 20, 42 | — | H | Other | — | 6 weeks | — | 3 calls 6 weeks apart | 12 questions; 397 words | Digitally stored voice | — |
| Sikorskii 2007 | IVR | AF | — | 17, 20, 30, 39, 40 | — | H | Yes | — | 2 months | — | Weekly¹³ | — | Female voice | — |
| Simon 2010a | IVR | AF | GMDBC, Others² | 3, 27, 39 | Yes | E | — | — | 3 months | 2‐6 min | — | — | — | Verification |
| Simon 2010b | ATCS Plus | AF, CF | — | 30, 42 | No | H | No | — | 12 months | — | 3¹⁴ | — | Human voice | — |
| Simpson 2005 | IVR | AF | — | 20 | Yes | P_H | Yes | Yes | 1 months | — | Daily | — | — | — |
| Solomon 2007 | ATCS Plus¹ | AF, CF | — | 16 | — | H | — | Yes | — | — | — | — | Female voice | — |
| Sparrow 2010 | IVR | AF | SCT, MI | 3, 12, 17, 20, 25, 39, 40, 42 | — | E | Yes | — | 12 months | — | Weekly then monthly¹⁵ | — | — | Password protected⁴ |
| Sparrow 2011 | IVR | AF | SCT | 3, 12, 17, 20, 25, 39, 40, 42 | Yes | E | Yes | — | 12 months | — | Weekly then monthly¹⁵ | — | — | Password protected⁴ |
| Spoelstra 2013 | ATCS Plus | AF, CF | CBT | 2, 20 | Yes | H | Yes | — | 2 months | — | Weekly | — | — | — |
| Stacy 2009 | ATCS Plus | AF, SF | HBM, CCM, SCT, TTM, MI, SRT, RL | 2, 3, 20, 32, 39 | — | H | — | Yes | 6 months | — | 3 | — | — | — |
| Stehr‐Green 1993 | Unidirectional | AF | — | 42 | — | H | — | — | 1 month | — | 1³ | — | Human voice | — |
| Stuart 2003 | IVR¹ | AF | — | 9, 10, 42 | Yes | P | Yes | — | 3 months | — | Daily/2 weeks; weekly/10 weeks | 25 calls | Female voice | — |
| Szilagyi 2006 | Unidirectional | AF | — | 42 | — | H | — | — | 18 months | — | Weekly | — | — | — |
| Szilagyi 2013 | Unidirectional | AF | — | 42 | — | H | — | — | 12 months | — | — | — | — | — |
| Tanke 1994 | Unidirectional | AF | HBM | 7*, 39, 40, 42 | No | H | — | — | — | — | 1¹⁶ | — | Female using native languages | — |
| Tanke 1997 | Unidirectional | AF | HBM | 39, 40, 42 | No | H | — | — | — | — | 1¹⁶ | — | Female using native languages | — |
| Tucker 2012 | IVR | AF | BET | 9, 20, 25, 34 | Yes | — | — | — | 6 months | ≤ 5 min | Daily | — | — | PIN⁶ |
| Vance 2011 | ATCS Plus | AF,SF | — | 10 | — | — | — | — | 3 months | — | 3/week | — | — | — |
| Velicer 2006 | IVR¹ | AF | TTM | 4, 13, 20, 34, 38 | — | E | Yes | — | 6 months | 15‐20 min | Weekly¹⁷ | — | — | — |
| Vollmer 2006 | ATCS Plus | AF, CF | — | 39 | — | H | Other | — | 10 months | < 10 min | 3¹⁸ | — | — | — |
| Vollmer 2011 | ATCS Plus | AF, CF | — | 20, 42 | — | H | Other | Yes | 18 months | 2‐3 min | — | — | — | — |
| Vollmer 2014 | ATCS Plus | AF, CF, SF | — | 20, 42 | Yes | H | Other | Yes | 12 months | 2‐3 min | Monthly | — | — | — |
| Williams 2012 | IVR | AF | — | 3, 21, 39 | Yes | P | Yes | Yes | 6 months | 5‐20 min | Weekly | — | — | PIN⁶ |
| Wright 2013 | IVR | AF | SCT | 2, 9, 10 | No | P | Other | — | 3 months | — | Biweekly | — | Synthetic speech | — |
| Xu 2010 | IVR | AF | — | 21, 40 | — | H | Yes | — | 6 months | — | Biweekly | — | — | — |
| Yount 2014 | ATCS Plus | AF, SF | — | 21, 40 | — | P | Yes | — | 3 months | — | Weekly | — | — | PIN |
| Zautra 2012 | Unidirectional | AF | SCT | 4,13 | — | — | — | — | — | — | — | — | — | — |
aATCS ¹For more detailed evaluation of multimodal/complex interventions, please refer to Table 16.
bContent delivery: AF: automated functions; CF: communicative functions; SF: supplementary functions. cTheory: BET: behavioural economic theory; BT: behavioural therapy; CBT: cognitive behavioural therapy; CCT: self‐management support strategies using chronic care model; DMT: Golan's model based on social–ecologic theory decision making theory; GMDBC: general model of the determinants of behavioural change; HBM: health belief model process theory; MI: motivational interviewing; PM: Pearlin's model of AD caregiver's stress; RL: reflective listening; RP: relapse prevention; SCT: social cognitive theory; SMP: social marketing principles; SRT: self‐regulation theory; TCD: theory of cognitive dissonance; TCM: 3‐component model; TPB: theory of planned behaviour; TRA: theory of reasoned action; TTM: transtheoretical model. ¹For enhanced letter reminders group. ²Synthesis of behavioural theories.
dBehaviour change techniques: 1 ‐ action planning; 2 ‐ agree behavioural contract; 3 ‐ barrier identification/problem solving; 4 ‐ emotional control training; 5 ‐ environmental restructuring; 6 ‐ facilitate social comparison; 7 ‐ fear arousal; 8 ‐ general communication skills training; 9 ‐ goal setting (behaviour); 10 ‐ goal setting (outcome); 11 ‐ model/demonstrate the behaviour; 12 ‐ motivational interviewing; 13 ‐ plan social support/social change; 14 ‐ prompt anticipated regret; 15 ‐ prompt identification as a role model/position advocate; 16 ‐ prompt practice; 17 ‐ prompt review of behavioural goals; 18 ‐ prompt review of outcome goals; 19 ‐ prompt self talk; 20 ‐ prompt self‐monitoring of behaviour; 21 ‐ prompt self‐monitoring of behavioural outcome; 22 ‐ prompt use of imagery; 23 ‐ prompting focus on past success; 24 ‐ prompting generalisation of a target behaviour; 25 ‐ provide feedback on performance; 26 ‐ provide information about other's approval; 27 ‐ provide information on consequences of behaviour in general; 28 ‐ provide information on consequences of behaviour to the individual; 29 ‐ provide information on where and when to perform the behaviour; 30 ‐ provide instruction on how to the perform the behaviour; 31 ‐ provide normative information about others' behaviour; 32 ‐ provide rewards contingent on effort or progress towards behaviour; 33 ‐ provide rewards contingent on successful behaviour; 34 ‐ relapse prevention/coping planning; 35 ‐ set graded tasks; 36 ‐ shaping; 37 ‐ stimulate anticipation of future rewards; 38 ‐ stress management; 39 ‐ tailoring; 40 ‐ teach to use prompts/cues; 41 ‐ time management; 42 ‐ use of follow up prompts. ¹Only those in the IG received importance statement.
eCaller: E ‐ either participant or healthcare provider/researcher; H ‐ healthcare provider/researcher; P ‐ participant; P_H ‐ If P fails to call then H calls.
fTelephone keypad for response: the calls were made using speech recognition (or speech‐enabled) technology; ¹‐ both data entry via Web screen or voice or telephone keypad.
gDuration of calls ¹Mean value. ²Assessments: 5‐8 min, health tips: 30‐60 s, healthcare education module: 3‐5 min. ³7 calls provided about 5–10 min of counselling, while the remaining 5 calls provided a tip of the week that lasted < 1 min. ⁴Screening session. ⁵20 min ‐ telecounselling, 30‐60 s ‐ health tips, 3‐5 min (optional) ‐ interactive self‐care education module.
hFrequency ¹Twice daily, follow‐up phase ‐ daily for another 4 weeks, twice a week for another 2 weeks, and then once a week. ²1st call 3 days after starting CPAP. ³Up to 9 attempts. ⁴Alert calls. ⁵The medication reminder calls occurred monthly; the medication refill calls were synchronised to when a medication refill was due. During months 2‐6 of the intervention, participants received both medication reminder (monthly) and medication refill calls (timed to refill due dates) for the 4 medications of interest. During months 7‐12 of the intervention, participants only received medication refill calls; ⁶2 weekly calls, 3 biweekly, and 10 monthly calls. ⁷Weeks 1‐3, biweekly; weeks 4‐11, weekly; months 3‐6, bimonthly; months 7‐12, monthly. ⁸For the first month, every other week for months 2 and 3, and monthly for months 4 through 12. ⁹Twice daily for 7 days until successful telephone contact was established. ¹⁰For assessment only (a total of 12 sessions were administered). ¹¹Up to 6 call attempts. ¹²At 2, 14, 30, 60, and 90 days postdischarge. ¹³ Except week 5. ¹⁴Up to six attempts, leaving up to two messages requesting a call back. ¹⁵1st month ‐ weekly followed by monthly calls. ¹⁶Up to 5 follow‐up calls at half hour intervals if busy phone lines or non‐response. ¹⁷Weekly for the first month, biweekly the second month, and monthly for months 3–6 and applied to smokers who received nicotine replacement therapy. ¹⁸5 months apart.
iIntensity ¹Mean value. ²Except for 2 h during the night for network file backup. ³Estimate for IG only.
jSecurity arrangement ¹Memotext ‐ the place where the reminders were actually generated. ²Personal identification number. ³Automated messages instructed the listener to 'press 1' if the call had reached the intended recipient, and they were not left on answering machines. ⁴Confidential password was used to access the system. ⁵Personal identification number (PIN) ‐ medical record number. ⁶PIN ‐ health record number and year of birth; ⁷PIN ‐ study number and telephone number.
4. Intervention Complexity Assessment Tool for Systematic Reviews.
| Assessment levels and criteria for each dimension | Study | Assessment of the intervention (a‐d)/description of the intervention/justification | Control (or usual care) |
| Core dimension 1: active components included in the intervention compared with the control | |||
| a. More than 1 component and delivered as a bundle b. More than 1 component c. 1 component |
Baker 2014 | (a.) A mailed reminder letter, a free faecal immunochemical test, an automated telephone and text message reminding them that they were due for screening and that a faecal immunochemical test was being mailed to them, an automated telephone and text reminder 2 weeks later for those who did not return the faecal immunochemical test, and personal telephone outreach by a colorectal cancer screening navigator after 3 months | (b.) Usual care included computerised reminders, standing orders for medical assistants to give patients home faecal immunochemical test, and clinician feedback on colorectal cancer screening rates |
| Bennett 2013 | (a.) Behaviour change goals, self‐monitoring via IVR phone calls, tailored skills training materials, monthly interpersonal counselling calls, and a 12‐month gym membership. | (b.) Control group received + newsletters that covered general wellness topics but did not discuss weight, nutrition, or physical activity | |
| Bove 2013 | (a.) Internet‐ and telephone‐based telemedicine system + automatically generated emails or telephone calls as reminders + sphygmomanometer, a weighting scale (if needed), a pedometer and instructions on their use | (c.) Control group received usual care | |
| Brendryen 2008 | (a.) Email, webpages, IVR and short message service (SMS) + craving helpline | (c.) Control group received self‐help (booklet) | |
| Dubbert 2002 | (a.) 10 personal phone calls from the nurse interspersed randomly with 10 automated phone calls + clinic‐based activity counselling | (b.) Clinic‐based activity counselling + no calls | |
| Fiscella 2011 | (b.) Clinician prompt, patient prompts, patient outreach consisting of 2 personalised letters which also include testing kits for colorectal cancer and up to 4 ATCS calls over 26 weeks | (c.) The clinician was responsible for discussing cancer screening with the patients and for initiating any referral or for handing out faecal occult blood testing cards over 12 months | |
| Hendren 2014 | (b.) Letters, ATCS calls, a point‐of‐care prompt and mailing of a home colorectal cancer testing kit; and medical record reviews at week 12 | (c.) Usual care received blinded chart review | |
| Ho 2014 | (b.) Medication reconciliation and tailoring, patient education (provided through automated voice messages and pharmacist telephone calls when requested by the patient), collaborative care between pharmacists and providers (primary care providers or cardiologists), and voice messaging reminders (educational and medication refill reminder calls). | (c.) Usual care received standard hospital discharge instructions e.g., numbers to call, follow‐up appointments, diet and exercise advice, a discharge medication list, and educational information about cardiac medications | |
| Kroenke 2010 | (a.) Symptom monitoring by a nurse + automated monitoring either via IVR or by Internet + medications (analgesics, antidepressants) | (c.) Usual care from oncologist | |
| Kroenke 2014 | (a.) Symptom monitoring, either via IVR or by Internet + nurse care + stepped care with analgesics | (c.) Usual care from primary care physician | |
| Magid 2011 | (b.) Patient education, home blood pressure monitoring, home blood pressure measurement reporting to an ATCS, and clinical pharmacist management of hypertension with physician oversight + usual care | (c.) The control group received usual care | |
| Morey 2009 | (b.) Baseline in‐person and biweekly then monthly telephone counselling by a lifestyle counsellor, one‐time clinical endorsement of physical activity and monthly automated telephone messaging by primary care provider, and quarterly tailored mailings of progress in physical activity. | (c.) Patients in the control group received usual care | |
| Morey 2012 | (b.) 1 in‐person baseline counselling session, regular telephone counselling, physician endorsement in clinic with monthly ATCS calls encouragement, and tailored mailed materials, plus a consult to a Veterans Affairs (VA) weight management program. | (b.) Patients in the control group received usual care + MOVE | |
| Shet 2014 | (b.) An IVR call once a week + a weekly non‐interactive neutral pictorial message sent out as a reminder 4 days after the IVR call + usual care | (b.) Usual care included up to 3 counselling sessions + antiretroviral treatment | |
| Solomon 2007 | (b.) Education and reminders delivered to primary care physicians + mailings and ATCS | (c.) The control group received no education | |
| Stuart 2003 | (b.) Treatment team education and patient self‐care education, nurse telephone call and IVR program | (c.) Treatment team education and patient self‐care education | |
| Velicer 2006 | (a.) Automated counselling plus nicotine replacement therapy, manuals, and expert system (TEL + EXP + NRT + MAN) | (c.) The control group received stage (of change) matched manuals | |
| Core dimension 2: behaviours or actions of intervention recipients or participants to which the intervention is directed | |||
| a. Single target b. Dual target c. Multitarget d. Variesa |
Baker 2014 | (a.) Single target: colorectal cancer screening | (a.) Single target: colorectal cancer screening |
| Bennett 2013 | (a.) Single target: weight management | (a.) Single target: weight management | |
| Bove 2013 | (c.) Single target: diet, exercise, smoking and blood pressure control | (a.) Single target: blood pressure control | |
| Brendryen 2008 | (a.) Single target: smoking abstinence | (a.) Single target: smoking abstinence | |
| Dubbert 2002 | (c.) Multiple target: physical activity; BMI; mobility; quality of life | (c.) Multiple target: physical activity; BMI; mobility; quality of life | |
| Fiscella 2011 | (b.) Dual target: breast cancer and colorectal cancer screening | (b.) Dual target: breast cancer and colorectal cancer screening | |
| Hendren 2014 | (b.) Dual target: breast cancer and colorectal cancer screening | (b.) Dual target: breast cancer and colorectal cancer screening | |
| Ho 2014 | (c.) Medication adherence, blood pressure, blood lipid levels | (c.) Medication adherence, blood pressure, blood lipid levels | |
| Kroenke 2010 | (b.) Dual target: pain and depression management | (b.) Dual target: pain and depression management | |
| Kroenke 2014 | (a.) Single target: musculoskeletal pain management | (a.) Single target: musculoskeletal pain management | |
| Magid 2011 | (b.) Dual target: blood pressure monitoring and blood pressure measuring | (b.) Dual target: blood pressure monitoring and blood pressure measuring | |
| Morey 2009 | (c.) Multitarget: improving gait speed, self‐reported physical activity, function and disability | (c.) Multitarget: improving gait speed, self‐reported physical activity, function and disability | |
| Morey 2012 | (c.) Multitarget: improving blood sugar indices, anthropometric measures, and self‐reported physical activity, health‐related quality of life, and physical function | (c.) Multitarget: improving blood sugar indices, anthropometric measures, and self‐reported physical activity, health‐related quality of life, and physical function | |
| Shet 2014 | (a.) Single target: antiretroviral treatment medication adherence | (a.) Single target: antiretroviral treatment medication adherence | |
| Solomon 2007 | (a.) Single target: osteoporosis screening | (d.) Varies | |
| Stuart 2003 | (a.) Single target: antidepressant medication adherence | (a.) Single target: antidepressant medication adherence | |
| Velicer 2006 | (a.) Single target: smoking abstinence | (a.) Single target: smoking abstinence | |
| Core dimension 3: organisational levels and categories targeted by the intervention | |||
| a. Multilevel b. Multicategory c. Single category |
Baker 2014 | (c.) Intervention directed only at single category of individuals within the individual level: patients past due for colorectal cancer screening | (c.) Intervention directed only at single category of individuals within the individual level: patients past due colorectal cancer screening |
| Bennett 2013 | (c.) Intervention directed only at single category of individuals within the individual level: obese females of Black ethnic origin | (c.) Obese females of black ethnic origin | |
| Bove 2013 | (c.) Intervention directed only at single category of individuals within the individual level: subjects with elevated blood pressure | (c.) Intervention directed only at single category of individuals within the individual level: subjects with elevated blood pressure | |
| Brendryen 2008 | (c.) Intervention directed only at single category of individuals within the individual level: tobacco smokers | (c.) Tobacco smokers | |
| Dubbert 2002 | (c.) Sedentary primary care patients | (c.) Sedentary primary care patients | |
| Fiscella 2011 | (c.) Intervention directed only at single category of individuals within the individual level: patients past due recommended screening | (c.) Patients past due recommended screening | |
| Hendren 2014 | (c.) Intervention directed only at single category of individuals within the individual level: patients past due recommended screening | (c.) Patients past due recommended screening | |
| Ho 2014 | (c.) Intervention directed only at single category of individuals within the individual level: patients after hospitalisation for acute coronary syndrome | (c.) Intervention directed only at single category of individuals within the individual level: patients after hospitalisation for acute coronary syndrome | |
| Kroenke 2010 | (c.) Intervention directed only at single category of individuals within the individual level: cancer patients with depression and pain | (c.) Cancer patients with depression and pain | |
| Kroenke 2014 | (c.) Intervention directed only at single category of individuals within the individual level: patients with musculoskeletal pain | (c.) Patients with musculoskeletal pain | |
| Magid 2011 | (c.) Intervention directed only at single category of individuals within the individual level: patients with hypertension | (c.) Patients with hypertension | |
| Morey 2009 | (c.) Intervention directed only at single category of individuals within the individual level: sedentary (otherwise healthy) older adults | (c.) Intervention directed only at single category of individuals within the individual level: sedentary (otherwise healthy) older adults | |
| Morey 2012 | (c.) Intervention directed only at single category of individuals within the individual level: older adults at risk of diabetes mellitus | (c.) Intervention directed only at single category of individuals within the individual level: older adults at risk of diabetes mellitus | |
| Shet 2014 | (c.) Intervention directed only at single category of individuals within the individual level: patients with HIV | (c.) Intervention directed only at single category of individuals within the individual level: patients with HIV | |
| Solomon 2007 | (b.) Intervention directed at 2 or more categories of individuals within the individual level: primary care physicians and their patients at‐risk of osteoporosis | (b.) Control intervention directed at 2 or more categories of individuals within the individual level: primary care physicians and their patients at‐risk of osteoporosis | |
| Stuart 2003 | (c.) Intervention directed only at single category of individuals within the individual level: patients with depression | (c.) Intervention directed only at single category of individuals within the individual level: patients with depression | |
| Velicer 2006 | (c.) Intervention directed only at single category of individuals within the individual level: tobacco smokers | (c.) Tobacco smokers | |
| Core dimension 4: the degree of tailoring intended or flexibility permitted across sites or individuals in intervention implementation/application | |||
| a. Fully tailored/flexible b. Moderately tailored/flexible c. Inflexible d. Variesa |
Baker 2014 | (b.) Moderately tailored/flexible: a mailed reminder letter, a free faecal immunochemical test, an automated telephone and text message reminder, an automated telephone and text reminder 2 weeks later (inflexible); personal telephone outreach (flexible) | (b.) Moderately tailored/flexible: computerised reminders, standing orders to give patients home faecal immunochemical test (inflexible); clinician feedback on colorectal cancer screening rates (flexible) |
| Bennett 2013 | (b.) Moderately tailored/flexible: self‐monitoring via IVR phone calls (inflexible); behaviour change goals, tailored skills training materials, monthly interpersonal counselling calls, and a 12‐month gym membership (flexible) | (c.) Newsletters sent were inflexible | |
| Bove 2013 | (c.) Telemedicine system, reminders, sphygmomanometer, weighting scale and pedometer have all been standardised | (d.) Varies across interventions included in the review | |
| Brendryen 2008 | (c.) E‐mail, web‐pages, IVR and SMS inflexible; quote: "Early in the morning, the user receives an e‐mail with instructions to open the day's web page. Each day for 6 weeks, the client opens a web page that is unique to that particular programme day." | (c.) Quote: "The booklet contains general cessation information, a 48‐day quit calendar, a 10‐day quit log, the telephone number of the national quit‐line and links to relevant and open on‐line tobacco cessation resources" | |
| Dubbert 2002 | (b.) Moderately tailored/flexible: nurse used a semi‐standardised protocol. | (d.) Varies across interventions included in the review | |
| Fiscella 2011 | (c.) Clinician prompt, patient prompts, patient outreach all have been highly standardised | (b.) Discussions with patients were moderately tailored/flexible | |
| Hendren 2014 | (c.) Letters, ATCS calls, point‐of‐care prompts and blinded chart reviews all have been highly standardised | (c.) Blinded chart reviews have been highly standardised | |
| Ho 2014 | (b.) Moderately tailored/flexible: medication reconciliation and tailoring, patient education, collaborative care between pharmacists and providers (flexible); and voice messaging reminders (inflexible) | (b.) Usual care was moderately tailored/flexible | |
| Kroenke 2010 | (c.) Nurse care (using evidence‐based guidelines) and IVR monitoring and medications (all not flexible) | (d.) Varies across interventions included in the review | |
| Kroenke 2014 | (c.) Symptom monitoring, either via IVR or by Internet, nurse care and stepped care with analgesics (not flexible) | (d.) Varies across interventions included in the review | |
| Magid 2011 | (b.) Patient education, home blood pressure monitoring, home blood pressure measurement reporting to an ATCS (not flexible); and clinical pharmacist management of hypertension with physician oversight (flexible) | (d.) Varies across interventions included in the review | |
| Morey 2009 | (b.) Moderately tailored/flexible: quote: "Providers were encouraged to modify the script to suit their personal style." | (d.) Varies across interventions included in the review | |
| Morey 2012 | (b.) Moderately tailored/flexible: baseline counselling, regular telephone counselling, physician endorsement in clinic with monthly ATCS calls encouragement, and tailored mailed materials, plus a consult to a Veterans Affairs (VA) weight management programme | (d.) Varies across interventions included in the review | |
| Shet 2014 | (c.) An IVR call once a week + a weekly non‐interactive neutral pictorial message sent out as a reminder 4 days after the IVR call + usual care (inflexible) | (c.) Usual care counselling sessions + antiretroviral treatment (inflexible) | |
| Solomon 2007 | (b.) An advance letter, an ATCS call, and the opportunity to schedule a bone mineral density test (not flexible); specially trained pharmacists educated physicians (flexible). | (d.) Varies across interventions included in the review | |
| Stuart 2003 | (b.) Moderately tailored/flexible: treatment team education and patient self‐care education, nurse telephone call and IVR programme | (b.) Moderately tailored/flexible: treatment team education and patient self‐care education, nurse telephone call | |
| Velicer 2006 | (b.) Automated counselling plus nicotine replacement therapy, manuals, and expert system were all moderately tailored/flexible | (c.) Stage‐based self‐help manuals were inflexible | |
| Core dimension 5: the level of skill required by those delivering the intervention | |||
| a. High level skills b. Intermediate level skills c. Basic skills d. Variesa |
Baker 2014 | (b.) Intermediate level skills required in setting up the IVR phone calls and text reminders, providing outreach calls | (b.) Intermediate level skills required in providing feedback on colorectal cancer screening rates |
| Bennett 2013 | (b.) Intermediate level skills required in delivering behaviour change goals, setting up the IVR phone calls, producing tailored skills materials and monthly interpersonal counselling calls | (c.) No specialised skills required in writing the newsletter | |
| Bove 2013 | (b.) Intermediate level skills required in reviewing patients' reports (physicians), motivating patients (nurses), setting up the reminder calls, emails | (c.) No specialised skills required in providing usual care | |
| Brendryen 2008 | (a.) Creating/writing emails, web‐pages, IVR and SMS requires high level skills | (c.) No specialised skills required in writing the booklet | |
| Dubbert 2002 | (b.) Intermediate level skills required in prerecording automated telephone messages | (d.) Varies across interventions included in the review | |
| Fiscella 2011 | (b.) Intermediate level skills required in e.g. prerecording automated telephone reminders | (c.) No specialised skills required in discussing breast cancer/colorectal cancer screening | |
| Hendren 2014 | (b.) Intermediate level skills required in e.g. prerecording automated telephone reminders | (c.) No specialised skills required in reviewing charts | |
| Ho 2014 | (b.) Intermediate level skills required in e.g. educating patients and/or prerecording telephone reminders | (c.) No specialised skills required in providing usual care | |
| Kroenke 2010 | (b.) Intermediate level skills required from nurses to manage pain and depression | (b.) Intermediate level skills required from nurses to manage pain and depression | |
| Kroenke 2014 | (b.) Intermediate level skills required from nurses to manage musculoskeletal pain | (c.) Basic skills required from primary care physicians | |
| Magid 2011 | (b.) Intermediate level skills required from pharmacists and physicians to manage hypertension | (d.) Varies | |
| Morey 2009 | (b.) Intermediate level skills required from primary care providers in e.g., recording automated messages, counselling and consulting patients | (c.) Basc level skills required from primary care providers | |
| Morey 2012 | (b.) Intermediate level skills required from primary care providers in recording automated messages, counselling and consulting patients | (b.) Intermediate level skills required from primary care providers in providing MOVE | |
| Shet 2014 | (b.) Intermediate level skills required in setting up the IVR phone calls + pictorial messages | (c.) Basic skills required | |
| Solomon 2007 | (a.) Extensive specialised skills required: "The visits were conducted by specially trained pharmacists . . . These pharmacists also underwent a 1‐ day training program focused on osteoporosis and conducted by 2 of the study authors. This program included lectures on the epidemiology, diagnosis, and treatment of osteoporosis. Also, it reviewed principles of academic detailing and the specific goals of this intervention." | (d.) Varies | |
| Stuart 2003 | (b.) Intermediate level skills required in e.g., prerecording IVR calls | (c.) Basic skills required in delivering education and nurse calls | |
| Velicer 2006 | (b.) Intermediate level skills required in recording automated messages, providing feedback reports | (c.) Basic skills required | |
| Core dimension 6: the level of skill required for the targeted behaviour when entering the study by those receiving the intervention in order to meet the intervention's objectives | |||
| a. High level skills b. Intermediate level skills c. Basic skills d. Variesa |
Baker 2014 | (c.) No specialised skills required | (c.) No specialised skills required |
| Bennett 2013 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Bove 2013 | (b.) Intermediate level skills required. Quote: "subjects were trained on use of a computer and the Internet and were introduced to the Web site at the research centre. Telemedicine subjects received instructions on use of an optional telephone communication system". They also received instructions on the use of sphygmomanometer, weighting scale and pedometer | (c.) No specialised skills required | |
| Brendryen 2008 | (b.) Access to the Internet, email and a cell phone on a daily basis was required | (c.) No specialised skills required | |
| Dubbert 2002 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Fiscella 2011 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Hendren 2014 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Ho 2014 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Kroenke 2010 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Kroenke 2014 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Magid 2011 | (b.) Patients were instructed about use of the ATCS, and trained on using an electronic blood pressure cuff | (d.) Varies across interventions included in the review | |
| Morey 2009 | (d.) Varies across interventions included in the review | (c.) No specialised skills required | |
| Morey 2012 | (d.) Varies across interventions included in the review | (c.) No specialised skills required | |
| Shet 2014 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Solomon 2007 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Stuart 2003 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Velicer 2006 | (c.) No specialised skills required | (c.) No specialised skills required | |
| Core dimension 7: the degree of interaction between intervention components/the independence/interdependence of intervention components | |||
| a. High level interaction
b. Moderate
c. Independent d. Variesa e. Unclear or unable to assess |
Baker 2014 | (a.) High level interaction; quote: "The majority of faecal occult blood testing completions were accomplished with mailing FITs and sending automated voice and text reminders" | (d.) Varies across interventions included in the review |
| Bennett 2013 | (b.) Moderate level of interaction; quote: "comprised 5 mutually reinforcing components" | (e.) Unclear or unable to assess in individuals receiving usual care | |
| Bove 2013 | (b.) Moderate level of interaction of the intervention components: the automated calls and emails and the use of sphygmomanometer to measure blood pressure, weighting scale and pedometer to promote physical activity | (e.) Unclear or unable to assess in patients receiving usual care | |
| Brendryen 2008 | (a.) High level interaction; quote: "further research is necessary to detect the active intervention ingredients and their relative contributions" | (c.) Independent | |
| Dubbert 2002 | (a.) High level interaction; a synergistic effect has been observed | (e.) Unclear or unable to assess in patients receiving no calls | |
| Fiscella 2011 | (a.) High level interaction; quote: "combined interventions are superior to simpler interventions such as reminders" | (c.) Independent | |
| Hendren 2014 | (a.) There is substantial interaction or inter‐dependency between ATCS calls, a point‐of‐care prompt and mailing of a home colorectal cancer testing kits | (c.) Independent | |
| Ho 2014 | (b.) Moderate level of interaction: the intervention components are considered to be mutually reinforcing | (e.) Unclear or unable to assess in patients receiving usual care | |
| Kroenke 2010 | (a.) High level interaction; triggered telephone calls occurred when ATCS monitoring indicated inadequate symptom improvement, non‐adherence to medication, adverse effects, suicidal ideation | (e.) Unclear or unable to assess in patients receiving usual care | |
| Kroenke 2014 | (a.) High level interaction; IVR and nurse calls prompted adjustments in type or dose of analgesics delivered | (e.) Unclear or unable to assess in patients receiving usual care | |
| Magid 2011 | (a.) There was a high level interaction between the intervention components: Quote: "This difference was likely due to greater therapy intensification (number and intensity of hypertension medications) in the intervention group" | (e.) Unclear or unable to assess in patients receiving usual care | |
| Morey 2009 | (b.) Moderate level of interaction: personal and automatic calls are considered to be mutually reinforcing | (e.) Unclear or unable to assess in patients receiving usual care | |
| Morey 2012 | (b.) Moderate level of interaction: personal and automatic calls are considered to be mutually reinforcing | (e.) Unclear or unable to assess in patients receiving usual care | |
| Shet 2014 | (c.) The IVR calls and pictorial messages were independent of each other | (e.) Unclear or unable to assess in patients receiving usual care | |
| Solomon 2007 | (e.) Unable to assess the degree of interaction between physician education and ATCS calls | (e.) Unclear or unable to assess in patients receiving no intervention | |
| Stuart 2003 | (e.) Unable to assess the degree of interaction between education, nurse calls and IVR calls | (d.) Varies across interventions included in the review | |
| Velicer 2006 | (c.) Automated calls, nicotine replacement therapy, manuals, and expert system were independent of each other | (e.) Unclear or unable to assess in patients receiving stage‐matched manuals only | |
| Core dimension 8: the interaction between the intervention and the context or setting | |||
| a. Highly context dependent
b. Moderately context dependent
c. Independent of context d. Variesa e. Unclear or unable to assess |
Baker 2014 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review |
| Bennett 2013 | (e.) Unable to assess the level of interaction between the intervention and the context | (e.) Unable to assess the level of interaction between the intervention and the context | |
| Bove 2013 | (e.) Unable to assess the level of interaction between the intervention and the context | (d.) Varies across interventions included in the review | |
| Brendryen 2008 | (e.) Unable to assess the level of interaction between the intervention and the context | (e.) Unable to assess the level of interaction between the intervention and the context | |
| Dubbert 2002 | (e.) Unable to assess the level of interaction between the intervention and the context | (e.) Unable to assess the level of interaction between the intervention and the context | |
| Fiscella 2011 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Hendren 2014 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Ho 2014 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Kroenke 2010 | (e.) Unable to assess the level of interaction between the intervention and the context | (d.) Varies across interventions included in the review | |
| Kroenke 2014 | (e.) Unable to assess the level of interaction between the intervention and the context | (d.) Varies across interventions included in the review | |
| Magid 2011 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Morey 2009 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Morey 2012 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Shet 2014 | (e.) Unable to assess the level of interaction between the intervention and the context | (e.) Unable to assess the level of interaction between the intervention and the context | |
| Solomon 2007 | (e.) Unable to assess the level of interaction between the intervention and the context | (d.) Varies across interventions included in the review | |
| Stuart 2003 | (e.) Unable to assess the level of interaction between the intervention and the context | (d.) Varies across interventions included in the review | |
| Velicer 2006 | (e.) Unable to assess the level of interaction between the intervention and the context | (e.) Unable to assess the level of interaction between the intervention and the context | |
| Core dimension 9: the degree to which the effects of an intervention are modified by factors relating to recipient, provider, or implementation factors | |||
| a. Highly dependent on individual‐level factors
b. Moderately dependent on individual‐level factors
c. Largely independent of individual‐level factors d. Variesa e. Unclear or unable to assess |
Baker 2014 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess |
| Bennett 2013 | (b.) Moderately dependent on individual‐level factor, i.e. registered dietitians or personalized progress reports | (e.) Unclear or unable to assess | |
| Bove 2013 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Brendryen 2008 | (c.) Largely independent of individual‐level factors | (c.) Largely independent of individual‐level factors | |
| Dubbert 2002 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Fiscella 2011 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Hendren 2014 | (d.) Varies across interventions included in the review | (c.) The effects of the blinded chart reviews are not modified substantially by recipient or provider factors | |
| Ho 2014 | (d.) Varies across interventions included in the review | (d.) Varies across interventions included in the review | |
| Kroenke 2010 | (b.) Moderately dependent on individual‐level factor, i.e. nurse and pain‐psychiatrist specialist interaction | (e.) Unclear or unable to assess | |
| Kroenke 2014 | (b.) Moderately dependent on individual‐level factor, i.e. nurse management | (e.) Unclear or unable to assess | |
| Magid 2011 | (b.) Moderately dependent on individual‐level factor, i.e. clinical pharmacist management with physician oversight | (e.) Unclear or unable to assess | |
| Morey 2009 | (e.) Unclear or unable to assess | (e.) Unclear or unable to assess | |
| Morey 2012 | (e.) Unclear or unable to assess | (e.) Unclear or unable to assess | |
| Shet 2014 | (e.) Unclear or unable to assess | (e.) Unclear or unable to assess | |
| Solomon 2007 | (b.) The effects of the intervention are modified by one of recipient or factors, e.g. pharmacists' knowledge | (e.) Unclear or unable to assess | |
| Stuart 2003 | (e.) Unclear or unable to assess | (e.) Unclear or unable to assess | |
| Velicer 2006 | (e.) Unclear or unable to assess | (e.) Unclear or unable to assess | |
| Core dimension 10: the length of the causal pathway between the intervention and the outcome it is intended to affect | |||
| a. Pathway variable, long
b. Pathway linear, long
c. Pathway linear, short d. Variesa e. Unclear or unable to assess |
Baker 2014 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess |
| Bennett 2013 | (c.) Pathway linear, short. Quote: "The high rates of IVR call engagement and their correlation with greater weight losses" | (e.) Unclear or unable to assess | |
| Bove 2013 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Brendryen 2008 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Dubbert 2002 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Fiscella 2011 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Hendren 2014 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Kroenke 2010 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Kroenke 2014 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Magid 2011 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Morey 2009 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Morey 2012 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Shet 2014 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Solomon 2007 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Stuart 2003 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
| Velicer 2006 | (d.) Varies across interventions included in the review | (e.) Unclear or unable to assess | |
aVaries across interventions to be considered for/included in the review. Dimension 1: lists each component of the intervention and indicate whether they are delivered independently, together in bundles, or as integrated packages. If the intervention comprises 'usual care' plus an additional component, list 'usual care' as one component. Include dose, frequency, and duration of intervention if applicable. Dimension 2: lists each behaviour or action; consider whether target behaviours are single, repeated, or linked. Dimension 3: indicates which level(s) are targeted. Dimension 4: indicates the degree of flexibility including variation in implementation from site to site permitted and/or intervention designed to tailor to individuals or specific implementation settings (there could be a rigid protocol where no variation is permitted or a loose protocol, i.e. most components of the intervention are tailored/flexible). Dimension 5: indicates the level of skill required Indicate whether the required skills are multidisciplinary, interdisciplinary or single disciplinary. Note: there may be no new skills required. Dimension 6: describes or lists the skills required Dimension 7: describes the interaction between intervention components. Note: interaction may not be reported or may be implicit. Dimension 8: describes the degree to which the effects of the intervention are dependent on the context or setting in which it is implemented. Dimension 9: indicates the degree of modification. Dimension 10: describes the causal pathway. It may or may not be linear, and there may be more than one causal pathway. It may be helpful to use diagrams.
Results of the search
The database searches yielded 14,347 records (CENTRAL: N = 1150; MEDLINE: N = 3768; Embase: N = 4714; PsycINFO: N = 2070; CINAHL: N = 435; Web of Science: N = 585; GlobalHealth: N = 679; WHOLIS: N = 291; LILACS: N = 108; ASSIA: N = 547). We identified a further 10 studies through Google searching. All records were imported into Endnote, and after de‐duplication (N = 3600), a total of 10,757 records remained for the first phase of the screening process. Based on title and abstract, we judged 384 records to be potentially eligible and retrieved the full text copies for detailed assessment. Screening the full text of 384 records resulted in inclusion of 132 trials that met our review inclusion criteria (Figure 6).
Included studies
Full details of each trial are presented in Characteristics of included studies; a summary is given below. We included a total of 132 studies in the review. Full data were not available for 64 others, which we present in Ongoing studies.
The included trials were published between 1991 and 2015: 5 had cluster designs (Feldstein 2006; Hess 2013; Franzini 2000; Krum 2013; Stuart 2003), 6 were quasi‐randomised (Dini 1995; Heyworth 2014; Kurtz 2011; Linkins 1994; Siegel 1992; Tanke 1994), and 121 had a parallel‐group design. No CBA or ITS studies met our inclusion criteria. Trial duration ranged from 25 days to 46 months, and study sample sizes varied from 16 to 4,237,821. Most studies took place in the USA (n = 114).
Eighty‐four studies focused on management of long‐term conditions, 41 were preventive healthcare studies, and 7 were specific to neither (appointment reminders/non‐attendance rates) (Figure 7). Table 14 presents further information about participant characteristics. Twenty‐two trials used unidirectional ATCS (102,240 participants), 50 used IVR (4,402,631 participants), 60 used ATCS Plus (154,932 participants). Seventeen studies used ATCS as part of complex/multimodal interventions (9886 participants). The two most common theories underpinning ATCS interventions among the included studies were the transtheoretical model (n = 16) and Bandura's social cognitive theory (n = 21) (Bandura 2001). The most common behaviour change technique was the use of follow‐up prompts (n = 57), followed by self‐monitoring of behaviour (n = 53). Table 15 presents details of other theories or behaviour change techniques used or intervention characteristics, and Table 17 presents information about primary measures and effectiveness of ATCS. Table 13 summarises continuous and dichotomous data related to primary outcomes (from at least two studies in the same category). A description of all 17 studies using complex/multimodal interventions, which by definition had two or more active components and in five studies were delivered as a bundle, appear with ratings of intervention complexity in Table 16.
7.
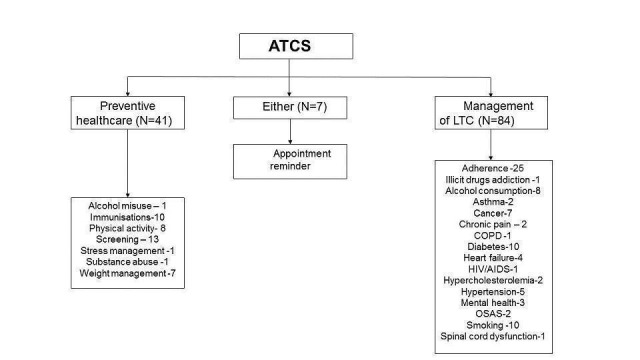
Subgroups for preventive health and/or management of long term conditions in this review
5. Effectiveness of ATCS.
| Study ID | Typea | Subtype | Participant age (years) | Sex | Ethnicityb | Primary outcome measures | Effectc |
| Tucker 2012 | P | Alcohol misuse | 41‐70 | > 50% M | W | Drinking practices Spending on alcohol |
2 2 (median effect = 2) |
| Franzini 2000 | P | Immunisation | — | — | — | Immunisation status Cost‐effectiveness |
1 1 (median effect = 1) |
| Hess 2013 | P | Immunisation | ≥ 71 | — | — | Herpes zoster immunisations | 1 |
| Dini 2000 | P | Immunisation | 0‐21 | — | — | Immunisation status | 2 |
| LeBaron 2004 | P | Immunisation | 0‐21 | M = F (± 3%) | W,B,H | Completion by the age of 24 months of the 4‐3‐1‐3 immunisations series | 2 |
| Lieu 1998 | P | Immunisation | 0‐21 | — | — | Immunisation status | 2 |
| Linkins 1994 | P | Immunisation | — | M = F (± 3%) | W,B | Immunisation status | 1 |
| Nassar 2014 | P | Immunisation | 22‐40 | > 50% F | W,B | Immunisation rate | 2 |
| Stehr‐Green 1993 | P | Immunisation | 0‐21 | M = F (± 3%) | B,H | Immunisation status | 2 |
| Szilagyi 2006 | P | Immunisation | 0‐21 | M = F (± 3%) | W,B,H | Immunisation status | 2 |
| Szilagyi 2013 | P | Immunisation | 0‐21 | M = F (± 3%) | — | Immunisation status Preventive visit rate |
1 1 |
| David 2012 | P | Physical activity | 41‐70 | > 50% F | W | 1‐mile walk after the intervention | 5 |
| Dubbert 2002 | P | Physical activity | 41‐70 | > 50% M | — | Self‐reported (diary) walking adherence | 1 |
| Jarvis 1997 | P | Physical activity | 41‐70 | > 50% F | B | Minutes walked per week | 1 |
| King 2007 | P | Physical activity | 41‐70 | > 50% F | W | Minutes of moderate to vigorous physical activity | 1 |
| Morey 2009 | P | Physical activity | ≥ 71 | > 50% M | W,B | Gait speed (usual and rapid) Self‐reported physical activity Function and disability |
2, 1 1 2 (median effect = 2) |
| Morey 2012 | P | Physical activity | 41‐70 | > 50% M | W | Homeostasis model assessment of insulin resistance | 2 |
| Pinto 2002 | P | Physical activity | 41‐70 | > 50% F | W,B | Energy expenditure in moderate‐intensity‐physical activity % meeting recommendations for moderate‐intensity‐physical activity Motivational readiness for physical activity |
2 2 2 (median effect = 2) |
| Sparrow 2011 | P | Physical activity | ≥ 71 | > 50% M | — | Muscle strength Balance Walk distance Mood |
1 1 2 1 (median effect = 1) |
| Baker 2014 | P | Screening | 41‐70 | > 50% F | H | Colorectal cancer screening adherence (faecal occult blood testing) | 1 |
| Cohen‐Cline 2014 | P | Screening | 41‐70 | > 50% M | W | Receipt of any recommended colorectal cancer screening | 1 |
| Corkrey 2005 | P | Screening | — | > 50% F | — | Screening rate | 2 |
| DeFrank 2009 | P | Screening | — | > 50% F | W,B,A | Mammography adherence | 1 |
| Durant 2014 | P | Screening | 41‐70 | M = F (± 3%) | — | Receipt of colorectal cancer screening after 3 months | — |
| Fiscella 2011 | P | Screening | — | > 50% F | W,B,H,A | Chart documentation of breast cancer screening, colorectal cancer screening, or both | 1 |
| Fortuna 2014 | P | Screening | — | > 50% F | W,B | Breast cancer and colorectal cancer screening | 2 |
| Hendren 2014 | P | Screening | — | > 50% F | W,B,H | Documentation of breast cancer screening, colorectal cancer screening, or both | 1 |
| Heyworth 2014 | P | Screening | 41‐70 | > 50% F | — | Bone mineral density screening after 12 months | 1 |
| Mosen 2010 | P | Screening | 41‐70 | M = F (± 3%) | W | Completion of faecal occult blood testing at 6 months | 1 |
| Phillips 2015 | P | Screening | 41‐70 | > 50% F | W,B | Completed mammogram or colorectal cancer screening within 36 weeks of randomisation | 2 |
| Simon 2010a | P | Screening | 41‐70 | M = F (± 3%) | W | Colorectal cancer screening | 2 |
| Solomon 2007 | P | Screening | 41‐70 | > 50% F | — | Bone mineral density testing and/or filling a prescription for a bone active medication | 1 |
| Mahoney 2003 | P | Stress management among caregivers |
41‐70 | > 50% F | W,B | Caregiver's appraisal of the bothersome nature of caregiving Anxiety Depression |
2 2 2 (median effect = 2) |
| Aharonovich 2012 | P | Substance use | 41‐70 | > 50% M | W,H | Days using primary drug | 2 |
| Bennett 2012 | P | Weight management | 41‐70 | > 50% F | B,H | Change in body weight and BMI | 1 |
| Bennett 2013 | P | Weight management | 22‐40 | > 50% F | B | Change in body weight and BMI | 1 |
| Estabrooks 2008 | P | Weight management | 41‐70 | > 50% F | W,B,H,A | Physical activity Dietary habits Weight loss |
2 2 2 (median effect = 2) |
| Estabrooks 2009 | P | Weight management | 0‐21 | > 50% M | W,H | BMI z‐score Physical activity and sedentary behaviour Dietary habits Eating disorder symptoms |
2 2 2 2 (median effect = 2) |
| Goulis 2004 | P | Weight management | 41‐70 | > 50% F | — | Body weight BMI Systolic blood pressure Diastolic blood pressure Plasma glucose Serum triglycerides Serum serum high‐density lipoprotein‐cholesterol Total serum cholesterol SF‐36 EQ‐5D Obesity Assessment Survey |
1 2 2 2 2 1 1 2 2 2 2 (median effect = 2) |
| Vance 2011 | P | Weight management | — | — | — | Weight change | 2 |
| Wright 2013 | P | Weight management | 0‐21 | > 50% M | W,B | BMI Calorie intake Fat intake Fruit intake Vegetable intake Television‐viewing time |
2 2 2 2 2 2 (median effect = 2) |
| Dini 1995 | E | Appointment reminder | — | — | — | Appointment adherence | 1 |
| Griffin 2011 | E | Appointment reminder | 41‐70 | > 50% M | W | Appointment non‐attendance Preparation non‐adherence |
2 2 (median effect = 2) |
| Maxwell 2001 | E | Appointment reminder | 22‐40 | > 50% F | W,B,H | Attendance rate | 2 |
| Parikh 2010 | E | Appointment reminder | — | M = F (± 3%) | — | Appointment adherence | 1 |
| Reekie 1998 | E | Appointment reminder | — | — | — | Appointment adherence | 2 |
| Tanke 1994 | E | Appointment reminder | 0‐21 | > 50% M | H | Appointment adherence | 1 |
| Tanke 1997 | E | Appointment reminder | 0‐21 | > 50% F | W,H | Appointment adherence (3‐day interval) | 1 |
| Moore 2013 | M | Illicit drugs addiction | 41‐70 | > 50% M | W,B | Patient interest Perceived efficacy Ease of use Treatment satisfaction Retention rate Drug consumption Methadone counselling Coping |
5 5 5 4 4 2 2 2 (median effect = 4) |
| Andersson 2012 | M | Alcohol consumption | — | — | — | AUDIT score | 1 |
| Hasin 2013 | M | Alcohol consumption | 41‐70 | > 50% M | B,H | Number of drinks per drinking day | 1 |
| Helzer 2008 | M | Alcohol consumption | 41‐70 | > 50% M | W | Weekly alcohol consumption | 3 |
| Litt 2009 | M | Alcohol consumption | 41‐70 | > 50% M | W,B,H | Proportion of days abstinent Proportion of heavy drinking days Continuous abstinence Drinking problems Coping problems |
1 2 2 2 2 (median effect = 2) |
| Mundt 2006 | M | Alcohol consumption | 41‐70 | > 50% M | W,B | Self‐reported drinking patterns Blood alcohol content Work and social adjustment scale Obsessive–compulsive drinking scale SF‐36 health survey Drinker inventory of consequences |
2 2 2 2 2 2 (median effect = 2) |
| Rose 2015 | M | Alcohol consumption | 41‐70 | M = F (± 3%) | — | Alcohol consumption | 2 |
| Rubin 2012 | M | Alcohol consumption | 41‐70 | > 50% M | W,B | Number of heavy drinking days per month % days abstinent per month Drinks per drinking day |
2 2 2 (median effect = 2) |
| Simpson 2005 | M | Alcohol consumption | 41‐70 | > 50% M | W,B | Drinking habits Alcohol craving Post‐traumatic stress disorder symptoms |
2 2 2 (median effect = 2) |
| Vollmer 2006 | M | Asthma | 41‐70 | > 50% F | W | Healthcare utilisation Medication use QoL |
2 2 2 (median effect = 2) |
| Xu 2010 | M | Asthma | 0‐21 | M = F (± 3%) | — | Healthcare utilisation | 4 |
| Cleeland 2011 | M | Cancer | 41‐70 | > 50% M | W | Number of symptom threshold events Cumulative distribution of symptom threshold events Differences in mean symptom severity between discharge and follow‐up |
1 2 2 (median effect = 2) |
| Kroenke 2010 | M | Cancer | 41‐70 | > 50% F | W,B | Depression severity Pain severity |
1 1 (median effect = 1) |
| Mooney 2014 | M | Cancer | 41‐70 | > 50% F | W | Symptom presence, severity, and distress data | 2 |
| Siegel 1992 | M | Cancer | 41‐70 | M = F (± 3%) | W,B,H | Prevalence of unmet needs | 2 |
| Sikorskii 2007 | M | Cancer | 41‐70 | > 50% F | — | Symptom severity | 2 |
| Spoelstra 2013 | M | Cancer | 41‐70 | > 50% F | W,B,A | Adherence to medications Symptom severity |
2 1 (median effect = 2) |
| Yount 2014 | M | Cancer | 41‐70 | M = F (± 3%) | W,B,H | Symptom burden | 2 |
| Naylor 2008 | M | Chronic Pain | 41‐70 | > 50% F | W | Pain Function/disability Coping |
1 1 1 (median effect = 1) |
| Kroenke 2014 | M | Chronic Pain | 41‐70 | > 50% M | W | Pain intensity | 1 |
| Halpin 2009 | M | Chronic obstructive pulmonary disease | 41‐70 | > 50% M | — | Frequency of exacerbations Proportion of patients experiencing 1 or more exacerbations |
2 2 (median effect = 2) |
| Adams 2014 | M | Adherence | 0‐21 | > 50% M | B | Comprehensiveness of screening and counselling | 1 |
| Bender 2010 | M | Adherence | 41‐70 | > 50% F | W,B,H,A | Medication adherence | 1 |
| Bender 2014 | M | Adherence | 0‐21 | — | — | Medication adherence | 1 |
| Boland 2014 | M | Adherence | 41‐70 | M = F (± 3%) | W,B,H,A | Medication adherence | 1 |
| Cvietusa 2012 | M | Adherence | 0‐21 | — | — | Medication adherence | 1 |
| Derose 2009 | M | Adherence | 41‐70 | > 50% M | W,B,H,A | Adherence (completion of all 3 recommended laboratory tests) | 2 |
| Derose 2013 | M | Adherence | 41‐70 | M = F (± 3%) | W,B,H,A | Medication adherence | 1 |
| Feldstein 2006 | M | Adherence | 41‐70 | M = F (± 3%) | — | Completion of all recommended laboratory tests | 1 |
| Friedman 1996 | M | Adherence | ≥ 71 | > 50% F | B | Medication adherence Systolic blood pressure Diastolic blood pressure |
1 2 1 (median effect = 1) |
| Glanz 2012 | M | Adherence | 41‐70 | > 50% M | W,B | Medication adherence Refill adherence Appointment adherence |
2 2 2 (median effect = 2) |
| Green 2011 | M | Adherence | — | — | — | Medication refill rate | 1 |
| Ho 2014 | M | Adherence | 41‐70 | > 50% M | W | Medication adherence | 1 |
| Leirer 1991 | M | Adherence | ≥ 71 | > 50% F | — | Medication non‐adherence Cognitive assessment |
1 2 (median effect = 2) |
| Lim 2013 | M | Adherence | 41‐70 | M = F (± 3%) | W,B,H,A | Adherence rate Therapeutic coverage |
2 2 (median effect = 2) |
| Migneault 2012 | M | Adherence | 41‐70 | > 50% F | B | Medication adherence Diet Moderate or greater intensity physical activity |
2 1 4 (median effect = 2) |
| Mu 2013 | M | Adherence | — | — | — | Medication adherence | 1 |
| Ownby 2012 | M | Adherence | ≥ 71 | — | — | Medication adherence | 1 |
| Patel 2007 | M | Adherence | 41‐70 | M = F (± 3%) | — | HRQLAdherence to statins | 1 |
| Reynolds 2011 | M | Adherence | — | — | — | Medication adherence (refill rate) | 1 |
| Sherrard 2009 | M | Adherence | 41‐70 | — | — | Adherence and adverse events | 1 |
| Simon 2010b | M | Adherence | 41‐70 | > 50% M | B | Retinopathy examination | 4 |
| Stacy 2009 | M | Adherence | 41‐70 | > 50% F | — | 6‐month point prevalence | 1 |
| Stuart 2003 | M | Adherence | — | — | — | Adherence to medications | 2 |
| Vollmer 2011 | M | Adherence | 41‐70 | > 50% F | W,B,A | Medication adherence | 1 |
| Vollmer 2014 | M | Adherence | 41‐70 | M = F (± 3%) | W,B,A | Medication adherence | 1 |
| Graziano 2009 | M | Diabetes mellitus | 41‐70 | > 50% M | W | Glycated haemoglobin | 2 |
| Homko 2012 | M | Diabetes mellitus | 41‐70 | > 50% F | W,B,H | Maternal blood glucose level Infant birth weight |
2 2 (median effect = 2) |
| Katalenich 2015 | M | Diabetes mellitus | 41‐70 | > 50% F | W,B,H,A | Glycated haemoglobin Medication adherence Quality of life Cost‐effectiveness |
2 2 2 1 (median effect = 2) |
| Khanna 2014 | M | Diabetes mellitus | 41‐70 | > 50% M | H | Glycated haemoglobin | 4 |
| Kim 2014 | M | Diabetes mellitus | — | — | — | Glycated haemoglobin | 1 |
| Lorig 2008 | M | Diabetes mellitus | 41‐70 | > 50% F | H | Glycated haemoglobin Health distress Global health Hypoglycaemia Hyperglycaemia Activity limitation Fatigue Physical activity levels Communication with physician Glucose monitoring Self‐efficacy Healthcare utilisation |
4 4 4 2 4 4 4 2 4 1 4 2 (median effect = 4) |
| Piette 2000 | M | Diabetes mellitus | 41‐70 | > 50% F | W,H | Depression
Anxiety
Self‐efficacy
Days in bed because of illness Days cut down on activities because of illness Diabetes‐specific health‐related quality of life Satisfaction with care (English speakers only) General health‐related quality of life (English speakers only) |
1 2 1 1 2 6 1 1 (median effect = 1) |
| Piette 2001 | M | Diabetes mellitus | 41‐70 | > 50% M | W,B,H | Glucose monitoring Foot inspection Weight monitoring Medication adherence Glycated haemoglobin Serum glucose levels Diabetic symptoms (all) Hyperglycaemic symptoms Hypoglycaemic symptoms Vascular symptoms Other symptoms Satisfaction with care (summary score) |
1 1 2 4 2 2 1 2 2 2 1 1 (median effect = 2) |
| Schillinger 2009 | M | Diabetes mellitus | 41‐70 | > 50% F | W,B,H,A | Change in self management behaviour (self‐monitoring of blood glucose and self‐monitoring of diabetic foot) | 1 |
| Williams 2012 | M | Diabetes mellitus | 41‐70 | > 50% M | — | Glycated haemoglobin Health‐related quality of life (mental) Health‐related quality of life (physical) |
1 1 2 (median effect = 1) |
| Capomolla 2004 | M | Heart failure | 41‐70 | > 50% M | — | All‐cause mortality Re‐hospitalisation Emergency room use (composite outcome) |
1 |
| Chaudhry 2010 | M | Heart failure | 41‐70 | > 50% M | W,B | Readmission for any reason or death from any cause | 4 |
| Krum 2013 | M | Heart failure | ≥ 71 | > 50% M | — | Packer clinical composite score: death, hospital admission for heart failure, withdrawal from study due to worsening heart failure, 7‐point global health assessment questionnaire | 2 |
| Kurtz 2011 | M | Heart failure | 41‐70 | > 50% M | — | Cardiovascular deaths and hospitalisations (outcomes in isolation included cardiovascular deaths, hospitalisations for heart failure, and time to primary endpoint) | 1 |
| Shet 2014 | M | HIV | — | > 50% M | A | Time to virological failure (viral load > 400 copies/mL on 2 consecutive measurements) | 2 |
| Hyman 1996 | M | Hypercholestorolemia | 41‐70 | > 50% F | W | Total cholesterol reduction | 2 |
| Hyman 1998 | M | Hypercholesterolemia | 41‐70 | > 50% F | B | Total cholesterol reduction | 2 |
| Bove 2013 | M | Hypertension | 41‐70 | > 50% F | W,B,H | Blood pressure control at 6 months | 2 |
| Dedier 2014 | M | Hypertension | 41‐70 | > 50% F | H | Change in minutes of moderate or greater physical activity Change in systolic blood pressure |
1 2 (median effect = 2) |
| Harrison 2013 | M | Hypertension | — | — | — | Blood pressure | 1 |
| Magid 2011 | M | Hypertension | 41‐70 | > 50% M | W,H | Proportion to achieve guideline‐recommended blood pressure goals Systolic blood pressure Diastolic blood pressure |
2 1 2 (median effect = 2) |
| Piette 2012 | M | Hypertension | 41‐70 | > 50% F | — | Systolic blood pressure | 2 |
| Farzanfar 2011 | M | Mental health | 22‐40 | > 50% F | W,B | Quality of life (physical scale score and mental scale score) Depression Stress levels Total well‐being |
2, 2 2 2 2 (median effect = 2) |
| Greist 2002 | M | Mental health | 22‐40 | > 50% M | W | Yale‐Brown obsessive compulsive scale (YBOCS) score | 1 |
| Zautra 2012 | M | Mental health | — | — | — | Emotional health Physical health Stress |
1 1 1 (median effect = 1) |
| DeMolles 2004 | M | Obstructive sleep apnoea syndrome | 41‐70 | — | — | Continuous positive airway pressure use | 2 |
| Sparrow 2010 | M | Obstructive sleep apnoea syndrome | 41‐70 | > 50% M | — | Continuous positive airway pressure use | 1 |
| Brendryen 2008 | M | Smoking | 22‐40 | M = F (± 3%) | — | Repeated point abstinence | 1 |
| Carlini 2012 | M | Smoking | 22‐40 | > 50% F | W,B,H,A | Re‐enrollment into quit line support | 1 |
| Ershoff 1999 | M | Smoking | 22‐40 | > 50% F | W,B | Smoking abstinence | 2 |
| McNaughton 2013 | M | Smoking | 41‐70 | > 50% M | — | Self‐reported abstinence Biochemically confirmed smoking abstinence |
2 4 (median effect = 3) |
| Peng 2013 | M | Smoking | 0‐21 | > 50% M | A | Stage of change Self‐efficacy Decisional balance |
5 5 5 (median effect = 5) |
| Regan 2011 | M | Smoking | 41‐70 | > 50% M | — | Smoking abstinence | 4 |
| Reid 2007 | M | Smoking | 41‐70 | > 50% M | — | Smoking abstinence | 2 |
| Reid 2011 | M | Smoking | — | — | — | Smoking abstinence | 2 |
| Rigotti 2014 | M | Smoking | 41‐70 | M = F (± 3%) | W,B,H,A | Biochemically confirmed tobacco abstinence at 6 months | 1 |
| Velicer 2006 | M | Smoking | 41‐70 | > 50% M | W,B,A | 24‐h point prevalence 7‐d point prevalence 6‐month prolonged abstinence |
2 2 2 (median effect = 2) |
| Houlihan 2013 | M | Spinal cord dysfunction | 41‐70 | > 50% M | W,B,H | Prevalence of pressure ulcers Depression severity Healthcare utilisation |
2 1 2 (median effect = 2) |
aStudy type: E: either prevention or management; M: management of long‐term condition; P: prevention. bEthnicity: A: American Indian/Alaskan native; B: black/African American; H: Hispanic; W: white. cEffect: 1: Significant positive; 2: non‐sig positive; 3: significant negative; 4: non‐significant negative; 5: no difference (significant); 6: no difference (non‐significant)
In this section, we generally report the relevant outcomes from individual studies according to the priority (primary, secondary) assigned by the trial authors. However, we reorganise this information in Effects of interventions according to the primary and secondary outcomes identified for this review.
ATCS for preventive healthcare
Forty‐one studies evaluated the effectiveness of ATCS in preventive healthcare; study subtypes included alcohol misuse, immunisations, physical activity, screening, stress management among caregivers, substance abuse, and weight management.
Alcohol misuse
Tucker 2012 evaluated the effectiveness of IVR versus assessment‐only control for supporting natural resolutions in community‐dwelling problem drinkers in the USA (N = 187 participants). The participants' mean age was 45 years, and 63% were male. Participants in the intervention group received verbal feedback about their previous week's goals and set new goals for the following week. They listened to daily educational modules (up to five minutes for 24 weeks) on goal setting, relapse prevention, and support for stable resolution such as social networking, and they received monthly feedback letters summarising calling and drinking patterns. Outcomes were drinking practices and spending on alcohol.
Immunisation
Ten studies, all in the USA, evaluated ATCS for promoting immunisation uptake (Dini 2000; Franzini 2000; Hess 2013; LeBaron 2004; Lieu 1998; Linkins 1994; Nassar 2014; Stehr‐Green 1993; Szilagyi 2006; Szilagyi 2013). Sample sizes ranged from 50 participants in Nassar 2014 to 11,982 participants in Hess 2013. Six studies included more than 1000 participants (Dini 2000; Franzini 2000; LeBaron 2004; Linkins 1994; Szilagyi 2006; Szilagyi 2013).
Interventions generally focused on vaccinations for children (participants were parents), with some studies also focusing on adult immunisation (Hess 2013; Nassar 2014).
Eight studies used unidirectional ATCS (Dini 2000; Franzini 2000; Hess 2013; Linkins 1994; Nassar 2014; Stehr‐Green 1993; Szilagyi 2006; Szilagyi 2013), while LeBaron 2004 used ATCS Plus and Lieu 1998, IVR. Only LeBaron 2004 used communicative functions in addition to automated functions. Healthcare professionals initiated short calls (under two minutes) at a frequency ranging from twice per day in Linkins 1994 to once per month in Hess 2013. Typically, interventions aimed at providing follow‐up prompts.
Several studies had additional intervention arms including elements such as letter reminders or other forms of outreach (Dini 2000; Franzini 2000; LeBaron 2004; Lieu 1998; Szilagyi 2013). Controls included no calls (Dini 2000; Franzini 2000; Hess 2013; Linkins 1994; Stehr‐Green 1993), usual care (LeBaron 2004; Szilagyi 2006; Szilagyi 2013), letter only (Lieu 1998), or health information (Nassar 2014).
The primary outcome for all studies was immunisation status. Other primary outcomes included cost‐effectiveness (Franzini 2000) and preventive visit rate (Szilagyi 2013), while secondary outcomes were satisfaction (Nassar 2014), acceptability and costs (Dini 2000; Lieu 1998), and costs and process evaluation (Szilagyi 2013).
Physical activity
Eight studies, all in the USA, evaluated the effectiveness of ATCS for improving physical activity levels (David 2012; Dubbert 2002; Jarvis 1997; King 2007; Morey 2009; Morey 2012; Pinto 2002; Sparrow 2011). Sample sizes ranged from 71 in David 2012 to 398 in Morey 2009, and mean participant age ranged from 57 years in David 2012 to 71 years in Sparrow 2011.
David 2012 and Pinto 2002 used ATCS Plus; Jarvis 1997, King 2007, and Sparrow 2011, IVR; and Dubbert 2002, Morey 2009, and Morey 2012, unidirectional ATCS. In addition to the customary automated functions, David 2012 used communicative functions and Pinto 2002, supplementary functions. In David 2012, Dubbert 2002, Jarvis 1997, King 2007, Morey 2009, Morey 2012, and Pinto 2002, interventions were underpinned by the transtheoretical model, and in David 2012, King 2007, Morey 2009, Morey 2012, Pinto 2002, and Sparrow 2011, also by social cognitive theory. Participants in four studies could use touch‐tone telephone keypads to communicate with the system (Jarvis 1997; King 2007; Pinto 2002; Sparrow 2011). Call duration ranged from 10 to 30 seconds twice per day in David 2012 to 10 to 15 minutes (weekly) in King 2007.
Two studies had more than one intervention arm: King 2007 included automated advice (IVR) versus human advice arms, whereas Dubbert 2002 assessed 20 nurse‐delivered phone calls versus 10 nurse‐delivered plus 10 automated phone calls. Three studies used multimodal/complex interventions (see Table 16), including elements such as nurse‐delivered phone calls plus clinic‐based counselling (Dubbert 2002); biweekly and then monthly telephone counselling, clinical endorsement of physical activity, and quarterly tailored mailings of progress (Morey 2009); and in‐person baseline counselling, regular telephone counselling, physician endorsement in clinic, tailored mailings, and a consult to a Veterans Affairs (VA) weight management programme (Morey 2012).
In studies with one intervention arm, comparators included no‐coach IVR (David 2012), usual care (Jarvis 1997; Morey 2009), usual care + MOVE programme (Morey 2012), ATCS Plus call promoting healthy eating (Pinto 2002), and attention‐control via IVR (Sparrow 2011). Controls in other trials included attention‐control in King 2007 and no calls in Dubbert 2002.
Six studies measured adherence to physical activity (e.g. minutes or distance walking), usually as a primary outcome (Dubbert 2002; Jarvis 1997; King 2007; Morey 2009; Morey 2012; Pinto 2002; Sparrow 2011). Studies also assessed other outcomes: physical functioning and well‐being (King 2007);quality of life (Dubbert 2002); satisfaction (Jarvis 1997); energy expenditure and motivational readiness for physical activity (Pinto 2002); muscle strength, balance, and mood (Sparrow 2011); ability to complete a one‐mile walk after the intervention, body weight, BMI, waist and hip circumference, and self‐efficacy (David 2012); gait speed (usual and rapid), function and disability, and change in minutes of moderate/vigorous physical activity per week (Morey 2009); and fasting insulin and glucose levels using homeostasis model assessment of insulin resistance (HOMA‐IR), HbA1C, anthropometric measures, health‐related quality of life, and physical function (Morey 2012).
Screening
Thirteen studies evaluated ATCS for improving screening rates in Australia (Corkrey 2005) and the USA (Baker 2014; Cohen‐Cline 2014; DeFrank 2009; Durant 2014; Fiscella 2011; Fortuna 2014; Hendren 2014; Heyworth 2014; Mosen 2010; Phillips 2015; Simon 2010a; Solomon 2007). Sample sizes ranged from 366 in Hendren 2014 to 75,532 in Corkrey 2005, and mean participant age ranged from 40 years in DeFrank 2009 to 69 years in Solomon 2007. In Solomon 2007, 22% of patients were on oral glucocorticoids, while in Baker 2014, 68% had one or more long‐term conditions (LTC).
Five studies used ATCS Plus (Corkrey 2005; Fiscella 2011; Hendren 2014; Heyworth 2014; Solomon 2007); six, IVR (Cohen‐Cline 2014; DeFrank 2009; Durant 2014; Mosen 2010; Phillips 2015; Simon 2010a); and two, unidirectional ATCS (Baker 2014; Fortuna 2014). Corkrey 2005, Fiscella 2011, Hendren 2014, Heyworth 2014, and Solomon 2007 used communicative functions in addition to automated functions. A few studies specified the theoretical model underpinning the intervention: the health belief model (DeFrank 2009), the general model of the determinants of behavioural change (Simon 2010a), or theory of cognitive dissonance (Baker 2014). Typically, short calls (25 seconds to five minutes) provided information on consequences of behaviour in general, planning action, identifying barriers and solving problems as well as providing follow‐up prompts. Several studies had more than one intervention arm: DeFrank 2009 compared telephone calls (IVR) versus enhanced letter reminders; Fortuna 2014 assessed a letter plus unidirectional ATCS versus letter plus unidirectional ATCS Plus prompt versus letter plus personal call; Heyworth 2014 compared usual care plus IVR versus mailing plus usual care; and Phillips 2015 assessed IVR calls versus personalised letter versus IVR plus personalised letter. Several of the studies used multimodal/complex interventions with elements such as mailings, test kits, and personal counselling (see Table 16 for more information). In studies with more than one intervention arm, comparators (the least active arms) included enhanced usual care reminders (DeFrank 2009); reminder letter only (Fortuna 2014; Phillips 2015); or usual care alone (Heyworth 2014). Other controls consisted of usual care or no intervention (calls).
The primary outcome of most trials was documentation of one or more types of screening attendance at 3 to 12 months of the intervention (Baker 2014; Cohen‐Cline 2014; Corkrey 2005; Durant 2014; Fortuna 2014; Fiscella 2011; Hendren 2014; Heyworth 2014; Mosen 2010; Phillips 2015; Simon 2010a). DeFrank 2009 measured repeat adherence to screening, while Solomon 2007 assessed performance of bone mineral density testing or filling a prescription for a bone active medication. Four trials evaluated cost (Baker 2014; Corkrey 2005; Durant 2014; Phillips 2015).
Stress management among caregivers
One study in the USA (N = 100 dyads) evaluated the effectiveness of IVR for stress management in caregivers of people with disruptive behaviours associated with Alzheimer's disease (AD) (Mahoney 2003). The mean age of the caregivers was 63 years. and over 78% of them were women.
The trial compared usual care versus an ATCS Plus intervention with both automated and communicative functions, underpinned by process theory and Pearlin's model of caregiver stress. The intervention aimed to identify barriers/solve problems, plan social support/social change, provide feedback on performance, and tailor and provide follow‐up prompts. The IVR calls (lasting 18 min on average) provided advice on managing stress and their charges' behavioural problems, opportunities to communicate confidentially with nurse specialists or peers (through an online forum), and social conversation based on participants' interests.
The primary outcomes reported were the caregivers' experience of caregiving, anxiety, and depression.
Substance abuse
Aharonovich 2012 (N = 33) compared an ATCS Plus intervention versus motivational interviewing alone for reducing non‐injection drug use in participants (mean age 46, 76% men) with HIV in the USA. Participants were substance users attending HIV clinics.
The intervention consisted of brief counselling based on motivational interviewing aimed at goal setting, providing feedback on performance and teaching to use prompts/cues. Short (one to three min) daily calls used automated and supplementary functions and included personalised questions about the previous day's use of primary drug, amount in dollars spent on that drug, use of other drugs, HIV medication adherence, and feelings of wellness, stress, and overall quality of that day. Participants received immediate feedback and personal calls from a counsellor when they failed to call for 48 hours.
The main outcome was the number of days using the primary drug in the past 30 days.
Weight management
Seven studies based in Greece and the USA evaluated the effectiveness of ATCS in facilitating weight management in adults and/or children (Bennett 2012; Bennett 2013; Estabrooks 2008; Estabrooks 2009;Goulis 2004; Vance 2011; Wright 2013). Sample sizes ranged from 50 (dyads) in Wright 2013 to 365 participants in Bennett 2012, while mean age ranged from 10 years in Wright 2013 to 59 years in Estabrooks 2008. Many participants had co‐morbidities such as diabetes mellitus, metabolic syndrome, hypertension, and depression.
Three studies used ATCS Plus (Bennett 2012; Estabrooks 2009;Vance 2011); and four, an IVR system (Bennett 2013, Estabrooks 2008, Goulis 2004, and Wright 2013). The automated systems in Bennett 2012, Bennett 2013, and Estabrooks 2009 also had communicative functions, and in Vance 2011, they had supplementary functions. In three studies, interventions were underpinned by social cognitive theory (Bennett 2012; Bennett 2013; Wright 2013), and in one the intervention was embedded in Golan's model based on social ecologic theory (Estabrooks 2009). Typically, interventions aimed at planning action, identifying barriers, solving problems, setting goals, planning social support or social change, self‐monitoring of behaviour or behavioural outcome, providing feedback on performance, or providing rewards contingent on successful behaviour. Calls lasted from 1 to 10 min weekly in Estabrooks 2008 to 15 minutes weekly in Goulis 2004.
One study (Bennett 2013) used multimodal/complex interventions. For instance, in addition to IVR calls, the participants also received behaviour change goals, tailored skills training materials, monthly interpersonal counselling calls, and a 12‐month gym membership. Two studies had more than one intervention arm: Estabrooks 2009 included the Family Connections (FC) IVR versus FC ‐ workbook; and Vance 2011 used interactive telephone counselling (ITC) plus control intervention versus online behaviour‐based incentives (BI) plus control intervention versus control intervention plus ITC and BI. In these studies, comparators included FC group in Estabrooks 2009; and written materials and group meetings monthly in Vance 2011. Controls in other trials included usual care in Bennett 2012; Bennett 2013; Goulis 2004; or no intervention in Estabrooks 2008; Wright 2013.
In terms of outcomes, all studies assessed BMI or BMI z‐scores, usually as primary outcomes. Other outcomes were related to weight loss and other anthropometric measures (Bennett 2012; Bennett 2013; Estabrooks 2008; Estabrooks 2009; Goulis 2004; Vance 2011), dietary intake (Estabrooks 2008; Estabrooks 2009; Wright 2013), physical activity (Estabrooks 2008; Estabrooks 2009), television‐viewing time (Wright 2013), blood pressure (Bennett 2012; Goulis 2004; Vance 2011), lipid and glucose biomarkers (Goulis 2004; Vance 2011), health‐related quality of life (Goulis 2004), user satisfaction (Estabrooks 2008), adherence to medication or behavioural change (Bennett 2012; Bennett 2013), and adverse events (Bennett 2012; Bennett 2013).
ATCS for reducing non‐attendance rate (preventive healthcare or management of long‐term conditions)
All seven studies in this category evaluated the effectiveness of ATCS in providing appointment reminders or reducing non‐attendance rates (Dini 1995; Griffin 2011; Maxwell 2001; Parikh 2010; Reekie 1998; Tanke 1994; Tanke 1997). Reekie 1998 took place in the UK, while the rest were in the USA. Sample size ranged from 701 in Tanke 1997 to 12,092 in Parikh 2010, and the mean reported age of participants ranged from 19 years in Tanke 1994 to 63 years in Griffin 2011.
Parikh 2010 compared IVR versus staff reminder or no reminder. Griffin 2011 compared ATCS Plus three or seven days prior to appointment versus nurse‐delivered reminder, and the remaining studies assessed unidirectional ATCS versus no reminder (Dini 1995; Maxwell 2001; Tanke 1997), postal reminder (Maxwell 2001; Reekie 1998), staff reminder (Reekie 1998), automated reminders plus staff and postal reminder (Reekie 1998), and automated reminders plus importance statement, authority statement, and both (Tanke 1994). Only Griffin 2011 used communicative functions in addition to automated functions. Typically, participants received a single, completed (i.e. answered) reminder call before an appointment; these included instructions, opportunities to cancel or confirm appointment, information on consequences of non‐adherence, and prompts for follow‐up. Tanke 1994 and Tanke 1997 drew solely from the health belief model, while Griffin 2011 also consulted the model of social marketing principles.
The primary outcome in all studies was appointment adherence. Griffin 2011 also reported outcomes on appointment non‐attendance and preparation non‐adherence. Secondary outcomes included perceptions about the calls (Griffin 2011), satisfaction (Parikh 2010), attitudes (Tanke 1994), and perceptions of reminders (Tanke 1997).
ATCS for managing long‐term conditions
Eighty‐four studies evaluated the effectiveness of ATCS for managing long‐term conditions, focusing on adherence to medications/laboratory tests (the comparison that provides the most generally applicable evidence across conditions), addiction, alcohol consumption, asthma, cancer, chronic pain, chronic obstructive pulmonary disease, diabetes mellitus, heart failure, HIV, hypercholesterolaemia, hypertension, mental health, obstructive sleep apnoea syndrome, smoking, and spinal cord injury.
Adherence to medications/laboratory tests
Twenty‐five studies, all in North America, evaluated the effectiveness of ATCS in facilitating adherence to medications or laboratory tests (Adams 2014; Bender 2010; Bender 2014; Boland 2014; Cvietusa 2012; Derose 2009; Derose 2013; Feldstein 2006; Friedman 1996; Glanz 2012; Green 2011; Ho 2014; Leirer 1991; Lim 2013; Migneault 2012; Mu 2013; Ownby 2012; Patel 2007; Reynolds 2011; Sherrard 2009; Simon 2010b; Stacy 2009; Stuart 2003; Vollmer 2011; Vollmer 2014). Sample size ranged from 16 in Leirer 1991 to 4,237,821 in Mu 2013, with 10 studies' samples exceeding 1000 (Bender 2014; Cvietusa 2012; Derose 2009; Derose 2013; Green 2011; Patel 2007; Reynolds 2011; Simon 2010b; Vollmer 2011; Vollmer 2014). Mean age ranged from 5 years in Adams 2014 to 80 years in Ownby 2012. Participants were recruited from primary care (Feldstein 2006), or they had a variety of chronic conditions: diabetes mellitus (Derose 2009; Friedman 1996; Ho 2014; Simon 2010b; Vollmer 2014); coronary heart disease and/or cerebrovascular disease (Friedman 1996; Ho 2014; Vollmer 2014); hypertension, hyperlipidaemia, chronic kidney disease, chronic lung disease, peripheral arterial disease (Ho 2014; Vollmer 2014); or cognitive (memory) impairment (Ownby 2012).
Nine studies assessed an ATCS Plus system: in Cvietusa 2012, versus an unspecified control; in Derose 2009, versus no intervention, letter, letter plus call, letter plus call plus letter, or call plus letter; in Derose 2013, Sherrard 2009, Simon 2010b, and Vollmer 2011, versus usual care; in Stacy 2009, versus a generic enhanced care package (single IVR call plus self‐help booklet); and in Vollmer 2014, versus a less intensive IVR intervention. Participants in Ho 2014 received usual care or a complex/multimodal intervention including medication reconciliation and tailoring, patient education (through pharmacist telephone calls when requested by the patient), and collaborative care between pharmacists and providers (primary care providers or cardiologists).
Fifteen studies compared an IVR system: in Adams 2014, versus a less intensive IVR intervention (single automated call); in Bender 2010, Leirer 1991, and Mu 2013, versus no intervention; in Bender 2014, Boland 2014, Friedman 1996, Glanz 2012, Green 2011, Migneault 2012, Patel 2007, and Reynolds 2011, versus usual care; and in Feldstein 2006, versus electronic medical records or pharmacy team outreach. Stuart 2003 compared a multimodal/complex intervention versus education or education plus nurse calls, and Vollmer 2014 compared IVR to IVR Plus.
Two studies assessed unidirectional ATCS: Lim 2013 compared it to no intervention and Ownby 2012 compared automated reminding versus tailored information or no intervention.
Only four studies used supplementary functions in addition to automated functions (Derose 2009; Derose 2013; Stacy 2009; Vollmer 2014), while six studies also used communicative functions (Cvietusa 2012; Ho 2014; Sherrard 2009; Simon 2010b, Vollmer 2011; Vollmer 2014). Interventions were based on the health belief model (Bender 2010; Stacy 2009), the chronic care model (Stacy 2009), social cognitive theory (Friedman 1996; Migneault 2012), transtheoretical model (Migneault 2012); motivational interviewing (Migneault 2012); self‐regulation theory, and reflective listening (Stacy 2009).
Typically, interventions were aimed at providing information on consequences of behaviour in general, planning action, identifying barriers and solving problems as well as providing follow‐up prompts, tailoring, prompting self‐monitoring of behaviour, providing rewards contingent on effort or progress towards behaviour or providing information on consequences of behaviour. Call duration ranged from single, 40‐second calls in Derose 2009 and Derose 2013 to 29.3 minutes in Adams 2014.
Studies measured medication adherence in a variety of ways: medication possession ratio (MPR) (Bender 2014; Patel 2007), refill rates (Bender 2010; Boland 2014; Cvietusa 2012; Derose 2013; Friedman 1996; Glanz 2012; Green 2011; Ho 2014; Lim 2013; Migneault 2012; Mu 2013; Ownby 2012; Reynolds 2011; Stuart 2003; Vollmer 2011; Vollmer 2014), or other methods (Adams 2014; Sherrard 2009). In contrast, Leirer 1991 measured non‐adherence by calculating the time difference between the participant's self‐specified time for taking the medication and the actual time they took to scan the appropriate bar code label; investigators also measured cognitive assessment using the Schaie‐Thurstone adult mental abilities test. Eight studies measured other indicators related to healthcare usage (e.g. completion of recommended tests, visits to the emergency room) or coverage (Adams 2014; Bender 2014; Derose 2009; Feldstein 2006; Lim 2013; Simon 2010b; Sherrard 2009; Vollmer 2011). Five studies assessed participant and/or physician satisfaction (Adams 2014; Cvietusa 2012; Friedman 1996; Sherrard 2009; Stuart 2003). Four studies measured achievement of behavioural or clinical targets such as blood pressure, as both primary and secondary outcomes (Friedman 1996; Ho 2014; Migneault 2012; Vollmer 2014). Finally, Bender 2010 used the asthma control test, asthma quality of life questionnaire, and beliefs about medications questionnaire; Sherrard 2009 measured a composite outcome of adherence and adverse events, and Stacy 2009 reported outcome on point prevalence persistency.
Illicit drugs addiction
Moore 2013 (N = 36) evaluated ATCS Plus versus usual care for opioid dependency in participants (mean age 41, 58% men) receiving methadone maintenance and continuing to use illicit drugs. The study took place in the USA and aimed to prompt review of behavioural goals, prevent relapses, plan coping, or manage stress. Underpinned by social cognitive theory, the intervention used automated and communicative functions to provide patients with immediate assistance, training, and support and self‐monitoring in their own environment. Calls lasted an average of nine minutes daily for 28 days. Outcomes included patient interest, perceived efficacy, treatment satisfaction, retention rate, self‐reported drug use, methadone counselling, ease of use and coping skills.
Alcohol consumption
Eight studies evaluated the effectiveness of ATCS for managing alcohol intake: seven in the USA (Hasin 2013; Helzer 2008; Litt 2009; Mundt 2006; Rose 2015; Rubin 2012; Simpson 2005) and one in Sweden (Andersson 2012). Sample sizes ranged from 47 participants in Rubin 2012 to 1423 participants in Andersson 2012, and mean participant age ranged from 46 years in Hasin 2013 and Simpson 2005 to 57 years in Rubin 2012. The mean duration of alcoholism was over 10 years in all studies, and participants in Hasin 2013 were HIV positive.
Three studies were primarily interested in IVR: Andersson 2012 was a four‐arm trial comparing a single IVR call, a single online intervention, repeated IVR calls, and repeated online interventions; Rubin 2012 compared IVR versus an information pamphlet; and Simpson 2005 compared daily or weekly calls with a no‐intervention control. The remaining five compared ATCS Plus: to advice/education (Hasin 2013), usual care (Rose 2015), or other interventions or control (Helzer 2008; Litt 2009; Mundt 2006). Litt 2009 compared ATCS Plus versus a packaged cognitive behavioural therapy (CBT) intervention via IVR. Mundt 2006 had three arms: daily IVR with personal follow‐up on noncompliant callers (i.e. ATCS Plus), daily IVR without follow‐up, and usual care. Helzer 2008 had four arms: ATCS Plus with feedback, ATCS Plus with feedback and financial compensation; automated daily phone calls (ATCS only); and no calls, with a brief intervention and standard care. Systems in Litt 2009 and Helzer 2008 had supplementary functions, and those in Hasin 2013, Mundt 2006, and Rose 2015 had both communicative and supplementary functions in addition to the automated ones. The intervention was underpinned by CBT in three studies (Litt 2009; Mundt 2006; Rose 2015) and by motivational interviewing (MI) in two (Hasin 2013; Rubin 2012). The interventions were aimed at goal setting and motivational interviewing (Hasin 2013; Rubin 2012); providing feedback on performance (Andersson 2012); training of emotional control, prompting self‐monitoring of behaviour, preventing relapses/coping planning, and/or managing stress (Litt 2009; Mundt 2006; Rose 2015); prompting self‐monitoring of behaviour (Helzer 2008; Simpson 2005). The duration of intervention ranged from one month in Simpson 2005 to six months in Helzer 2008, Mundt 2006, and Rubin 2012, and it was delivered daily in Hasin 2013, Helzer 2008, Mundt 2006, Rose 2015, and Simpson 2005.
Primary outcomes included the alcohol use disorders identification test (AUDIT) score (Andersson 2012); proportion of days abstinent, proportion of heavy drinking days, continuous abstinence, drinking problems, and coping problems (Litt 2009); drinking days, heavy drinking days, and total drinks consumed (Mundt 2006); drinking habits, alcohol craving, and post‐traumatic stress disorder symptoms (Simpson 2005); number of drinks per drinking day in the last 30 days (Hasin 2013); weekly alcohol consumption (Helzer 2008); alcohol consumption (Rose 2015); and number of heavy drinking days per month, percent days abstinent per month, drinks per drinking day (Rubin 2012). Secondary outcomes included participant perceptions of the system (Rose 2015).
Asthma
Two studies evaluated ATCS for managing asthma (Vollmer 2006; Xu 2010).
Vollmer 2006 (N = 6948) compared ATCS Plus with automated and communicative functions versus staff calls or usual care in adults (mean age 52 years) in the USA, Healthcare professionals initiated three IVR calls lasting under 10 minutes, five months apart. The system asked questions related to healthcare utilisation, and participants received tailored feedback. Participants at high risk of exacerbations were flagged up and their primary care provider was alerted, triggering a follow‐up contact. In addition, the IVR system assigned a primary care provider to participants who did not regularly visit a consistent provider for asthma care. Outcomes included healthcare utilisation, asthma control, medication use, quality of life, and acceptability.
Xu 2010 (N = 121) studied children (mean age 7 years) in Australia, comparing a nurse support group versus an IVR system where participants received calls twice a week that asked questions about asthma symptoms and medication use. Based on touch‐tone responses, they received educational messages, appropriate messages from the asthma management plan, and medication reminders. Primary care physician had access to the reports generated by the IVR system. Outcomes included healthcare utilisation, medication use, health‐related quality of life, and cost.
Cancer
Seven studies, all in the USA, evaluated ATCS for helping cancer patients (Cleeland 2011; Kroenke 2010; Mooney 2014; Sikorskii 2007; Siegel 1992; Spoelstra 2013; Yount 2014). Sample sizes ranged from 79 participants in Cleeland 2011 to 437 participants in Sikorskii 2007, and mean age from 57 years in Sikorskii 2007 to 61 years in Yount 2014. Participants in Kroenke 2010 and Mooney 2014 had a variety of other co‐morbidities, and participants in Spoelstra 2013 were taking antineoplastic medications.
Five studies assessed an ATCS Plus system, comparing it to to a less intensive (IVR monitoring) intervention (Cleeland 2011), usual care (Kroenke 2010; Yount 2014), attention only via IVR (Mooney 2014), and a less intensive (adherence only) IVR intervention (Spoelstra 2013), By contrast, Siegel 1992 compared IVR versus a research interview by an experienced clinician, and Sikorskii 2007 compared it to telephone calls by specially trained nurses. In addition to automated functions, Kroenke 2010 and Spoelstra 2013 used communicative functions; Cleeland 2011 and Yount 2014, supplementary functions; and Mooney 2014, both. Kroenke 2010 used a multimodal/complex intervention (symptom monitoring by a nurse and medications) and was underpinned by the three‐component model, whereas Spoelstra 2013 had a CBT basis.
Typically, interventions were aimed at prompting self‐monitoring of behaviour and behavioural outcome, prompting review of behavioural goals, providing instructions on how to perform the behaviour, tailoring and teaching to use prompts/cues. The frequency of calls ranged from daily in Mooney 2014 to twice a week and then twice a month in Kroenke 2010.
Primary outcomes were symptom threshold events, cumulative distribution of symptom threshold events, differences in mean symptom severity between discharge and follow‐up (Cleeland 2011); depression and pain severity (Kroenke 2010); symptom severity, distress, and burden (if a symptom was present) (Mooney 2014; Sikorskii 2007; Spoelstra 2013; Yount 2014); the prevalence of unmet needs (Siegel 1992); and adherence to medications (Spoelstra 2013). Secondary outcomes included health‐related quality of life, disability, healthcare use (outpatient physician visits), and co‐interventions (depression treatments) in Kroenke 2010; system usability and acceptability in Mooney 2014; and health‐related quality of life, treatment satisfaction, symptom management barriers, and self‐efficacy in Yount 2014.
Chronic pain
Kroenke 2014 (N = 250) and Naylor 2008 (N = 55) evaluated ATCS versus usual care for managing chronic pain in adults (mean age 55 years and 46 years, respectively) in the USA.
Naylor 2008 used an IVR intervention underpinned by CBT, aiming to identify barriers; solve problems; prompt practice, self‐monitoring of behaviour, or imagery; and provide feedback on performance and follow‐up prompts. The calls lasted 3 to 16 minutes and consisted of daily self‐monitoring questionnaire that assessed coping, perceived pain control, mood, medication use, and stress. Participants were able to access a verbal review of eight different pain management skills they learned during the 11 weeks of CBT (relaxation response, diaphragmatic breathing, positive self‐talk, cognitive restructuring, activity‐rest pacing, distraction techniques, reappraisal of pain, and defusing catastrophising). Once a month the group therapist analysed computer‐collated patient‐specific data and called the IVR to record a personalised message with advice and encouragement for each participant. Outcomes were pain (total pain experience, pain intensity), function/disability, and coping.
Kroenke 2014 used an ATCS Plus system and multimodal/complex intervention (with nursing care and analgesics) with automated and communicative functions, aiming at tailoring and self‐monitoring of behavioural outcome. The calls were scheduled weekly for the first month, every other week for months 2 and 3, and monthly for months 4 through 12. Investigators assessed pain, anxiety, depression, the degree of improvement; analgesic adverse effects, adherence, and whether a medication change was desired. Primary outcomes included pain intensity, while secondary outcomes included difference in response rates, and mean brief pain inventory interference and pain severity scale scores, at 12 months.
Chronic obstructive pulmonary disease (COPD)
Halpin 2009 (N = 79) compared ATCS versus no intervention for managing COPD. The trial took place in the UK. Participants had a mean age of 69, were mostly men (74%), and were taking long and short‐acting muscarinic antagonists as well as short‐acting β 2‐agonists. Investigators tested an ATCS Plus system with automated, communicative, and supplementary functions, aiming at prompting self‐monitoring of behavioural outcomes, teaching to use prompts/cues; and using follow‐up prompts. Participants received weekly automated alert calls with tailored advice, an information pack with important information about their condition, thermometers to monitor the temperature in the bedroom and living room, and advice on recognising early symptoms of an exacerbation. Participants also completed a daily diary comprising the EXACT questionnaire plus additional questions such as the colour of their phlegm, presence of symptoms of a cold or flu, visit to a doctor or nurse on that day for breathing problems or a cold, and need for the study team to contact them. The responses to these questions were used as a trigger to contact the participant to determine if an exacerbation was starting.
The primary outcomes were frequency of exacerbations and proportion of patients experiencing one or more exacerbations. Secondary outcomes included changes in health status.
Diabetes mellitus
Ten studies evaluatedATCS for managing diabetes mellitus (Graziano 2009; Homko 2012; Katalenich 2015; Khanna 2014; Kim 2014; Lorig 2008; Piette 2000; Piette 2001; Schillinger 2009; Williams 2012). With the exception of Williams 2012, which took place in Australia, all the studies were in the USA. Sample sizes ranged from 75 participants in Khanna 2014 to 417 participants in Lorig 2008, and mean age ranged from 30 years in Homko 2012 to 62 years in Graziano 2009.
Participants in five studies had a BMI above 30 kg/m2 (Homko 2012; Piette 2000; Piette 2001; Schillinger 2009; Williams 2012); they were pregnant in Homko 2012 (33 weeks or less) and had elevated blood pressure and cholesterol levels in Khanna 2014. In Kim 2014, 46% of participants were diagnosed with psychiatric illnesses; and 28% had been hospitalised in the past year.
Seven studies compared an ATCS Plus system versus usual care (Katalenich 2015; Khanna 2014; Kim 2014; Lorig 2008; Piette 2000; Piette 2001; Schillinger 2009), and in the case of Schillinger 2009, also versus support, education, and patient activation. The remaining studies compared an IVR system with usual care (Homko 2012; Graziano 2009; Williams 2012). In addition to automated functions, five studies used communicative functions (Kim 2014; Lorig 2008; Piette 2000; Piette 2001; Schillinger 2009), one study used supplementary functions (Khanna 2014), and one study used both communicative and supplementary functions (Katalenich 2015). Three studies were underpinned by social cognitive theory (Piette 2000; Piette 2001; Schillinger 2009) and one was based on the chronic care model (Schillinger 2009). Typically, interventions were aimed at planning action, setting goals, identifying barriers and solving problems, prompting self‐monitoring of behaviour and/or behavioural outcomes, providing feedback on performance, tailoring and providing follow‐up prompts. Call duration and frequency ranged from 90 seconds monthly in Lorig 2008 to 5 to 20 minutes weekly in Williams 2012.
Primary outcomes included glycated haemoglobin (Graziano 2009; Katalenich 2015; Khanna 2014; Kim 2014; Lorig 2008; Piette 2001; Williams 2012); blood glucose level and infant birth weight (Homko 2012); health‐ or diabetes‐related quality of life (Katalenich 2015; Piette 2000; Williams 2012); self‐efficacy (Lorig 2008; Piette 2000); medication adherence and cost‐effectiveness (Katalenich 2015); health distress, global health, hypoglycaemia, hyperglycaemia, activity limitation, fatigue, glucose monitoring, and healthcare utilisation (Lorig 2008); depression, anxiety, days in bed because of illness, days cut down on activities because of illness (Piette 2000); glucose monitoring, foot inspection, weight monitoring, medication use, diabetic symptoms (all), and satisfaction with care (Piette 2001); and change in self‐management behaviours (consisting of the four domains/sub‐scales: self‐monitoring of blood glucose and self‐monitoring of diabetic foot, diet and exercise) (Schillinger 2009).
Secondary outcomes included self‐monitoring of blood glucose frequency (Graziano 2009); systolic blood pressure, diastolic blood pressure, BMI, waist circumference, total cholesterol, triglycerides, high‐density lipoproteins, and low‐density lipoproteins (Khanna 2014); outpatient speciality services utilisation (Piette 2001); and behavioral, functional, and metabolic outcomes (Schillinger 2009).
Heart failure
Four studies evaluated ATCS versus usual care for reducing healthcare utilisation in people with heart failure (Capomolla 2004; Chaudhry 2010; Krum 2013; Kurtz 2011); Kurtz 2011 had a third arm implementing a multidisciplinary team approach during visits to the heart failure clinic. Trials took place in the USA (Chaudhry 2010), Australia (Krum 2013), France (Kurtz 2011), and Italy (Capomolla 2004). Sample sizes ranged from 138 participants in Kurtz 2011 to 1653 participants in Chaudhry 2010, while mean age ranged from 57 years in Capomolla 2004 to 73 years in Krum 2013. Participants in Chaudhry 2010 and Krum 2013 had several co‐morbidities such as coronary artery disease, chronic kidney disease, chronic obstructive pulmonary disease, diabetes mellitus, and hypertension.
Three studies used an ATCS Plus system (Chaudhry 2010; Capomolla 2004; Krum 2013), while Kurtz 2011 used an IVR system. Chaudhry 2010 and Capomolla 2004 used communicative functions in addition to automated ones, and Krum 2013 used supplementary functions as well. Typically, interventions were aimed at prompting self‐monitoring of behaviour and/or behavioural outcome as well as tailoring and providing follow‐up prompts. The mean call duration, reported in one study (Kurtz 2011) was 48 seconds (weekly). In Chaudhry 2010 and Capomolla 2004, participants placed calls once a day; and in Krum 2013, participants or staff called once a month. The duration of intervention ranged from six months in Chaudhry 2010 to 24 months in Kurtz 2011.
Capomolla 2004 reported a composite primary outcome considering rehospitalisation, cardiac mortality and emergency room use; outcomes in isolation included hospitalisation for heart failure, cardiac mortality, all‐cause mortality, all‐cause hospitalisation (chronic heart failure, cardiac cause and other cause) and emergency room use. Chaudhry 2010 measured readmission for any reason or death from any cause, and Kurtz 2011 reported cardiovascular deaths and hospitalisation for heart failure, both in isolation and as a composite or adverse events. Finally, Krum 2013 reported the Packer clinical composite score (death, hospital admission for heart failure, withdrawal from study due to worsening heart failure, seven‐point global health assessment questionnaire) as its primary outcome. For the purposes of this review, we separated these component outcomes and reported data for each of the following individually: all‐cause mortality, hospitalisation for heart failure, all‐cause hospitalisation and global health (hospitalisation for heart failure or for any cause were identified as secondary outcomes by this study). Secondary outcomes also included intervention adherence in Capomolla 2004; and hospitalisation for heart failure, number of days in the hospital, number of hospitalisations, and adverse events in Chaudhry 2010.
HIV/AIDS
Shet 2014 (N = 631) evaluated ATCS versus usual care for managing HIV in India. The trial used an IVR intervention underpinned by the theory of planned behaviour, which aimed at goal setting, prompting self‐monitoring of behaviour, providing feedback on performance and relapse prevention/coping planning. Intensity and duration of calls was weekly for 24 months. In addition to IVR calls, the multimodal/complex intervention included a weekly non‐interactive neutral pictorial message sent out as a reminder four days after the IVR call plus usual care that consisted of to three counselling sessions and antiretroviral treatment. Primary outcomes were time to virological failure (viral load > 400 copies/mL on two consecutive measurements), and secondary outcomes were medication adherence (pill count), death rate, and attrition rate.
Hypercholesterolaemia
Two studies(total N = 238) evaluated ATCS versus usual care for managing hypercholesterolaemia in the USA (Hyman 1996; Hyman 1998). Mean participant age was 48 years in Hyman 1996 and 57 years in Hyman 1998. Participants in Hyman 1998 had a mean BMI greater than 30 kg/m2; and 58% of them had had history of smoking.
Hyman 1996 used an IVR system with daily interaction, and Hyman 1998 used an ATCS Plus intervention, underpinned by social cognitive theory, with two to three minute calls twice weekly. Interventions aimed at prompting self‐monitoring of behaviour, tailoring, and providing follow‐up prompts. The primary outcome reported in both studies was total cholesterol reduction. Secondary outcomes included acceptability of the IVR system (Hyman 1996), self‐efficacy, dietary knowledge, and fat intake scale (Hyman 1998).
Hypertension
Five studies evaluated ATCS for managing hypertension; one took place in Honduras/Mexico (Piette 2012), and four were in the USA (Bove 2013; Dedier 2014; Harrison 2013; Magid 2011). Sample size ranged from 166 participants in Bove 2013 to 64,773 participants in Harrison 2013, while mean age ranged from 58 years in Dedier 2014 and Piette 2012 to 66 years in Magid 2011. Participants in Bove 2013,Magid 2011, and Harrison 2013 were diagnosed with diabetes mellitus.
Bove 2013 and Magid 2011 compared multimodal/complex interventions including an ATCS Plus system with additional communicative (and in the case of Bove 2013, also supplementary) functions versus usual care. In addition to ATCS, participants in Bove 2013 received a sphygmomanometer, a weighting scale if needed, and a pedometer, whereas in Magid 2011 they also received patient education, home blood pressure monitoring, and clinical pharmacist management of hypertension with physician oversight in addition to usual (standard) care. Piette 2012 compared an ATCS system with communicative functions to primary care and education. Dedier 2014 assessed an IVR system underpinned by social cognitive theory versus primary care and education, while Harrison 2013 evaluated a unidirectional ATCS versus usual care. Interventions were typically aimed at planning action and setting goals, prompting self‐monitoring of behavioural outcome, providing rewards contingent on effort or progress towards behaviour, setting graded tasks and tailoring, prompting self‐monitoring of behaviour and providing follow‐up prompts or providing feedback on performance. Call duration was typically up to 10 min (weekly) in Magid 2011 and Dedier 2014. Call frequency was biweekly in Bove 2013.
All studies monitored blood pressure as a primary outcome, while Dedier 2014 also assessed change in minutes of moderate or intensive physical activity. Secondary outcomes included health status, depression, satisfaction, and medication‐related problems in Piette 2012 and medication adherence in Magid 2011.
Mental health
Three studies in the USA evaluated ATCS for managing mental health problems (Farzanfar 2011; Greist 2002; Zautra 2012). Sample sizes ranged from 73 in Zautra 2012 to 218 in Greist 2002, while mean participant age was 39 years in Farzanfar 2011 and Greist 2002 and 54 years in Zautra 2012. Mental problems included mild to moderate depression (Zautra 2012), social phobia and generalised anxiety disorder (9% each in Greist 2002).
Farzanfar 2011 compared an IVR counselling intervention versus advice only for facilitating social comparison, prompting self‐monitoring of behaviour, providing instruction on how to perform the behaviour, tailoring, and providing follow‐up prompts. The included TLC‐Detect system aimed at identifying undiagnosed and untreated mental health problems, with an initial 30 to 90 minute screening call and monthly follow‐up calls. Greist 2002 assessed a computer‐driven ATCS Plus system (via IVR) with supplementary functions, underpinned by the theory of behavioural change, versus clinician‐guided behaviour therapy or relaxation‐only therapy. The trial's focus was relapse prevention/coping planning; participants called 12 or more times to record a message for a behavioural therapist, who responded within 72 hours. Final steps also included barrier identification, problem solving, and relapse prevention techniques. In addition, participants also received a programmed workbook. The last study, Zautra 2012, compared two unidirectional ATCS interventions (one for personal control/mastery and the other for mindful awareness/acceptance), underpinned by social cognitive theory, versus a healthy lifestyle control. The focus of the study was emotional control training and planning of social support/social change.
The primary outcomes included quality of life (physical health scale and mental health scale), total depression, perceived stress levels/score, and total well‐being (WHO‐5) in Farzanfar 2011; Yale‐Brown obsessive compulsive scale in Greist 2002; and depression and stress in Zautra 2012. Secondary outcomes included clinical and patient global impressions and depression (Hamilton rating scale for depression) in Greist 2002 and satisfaction in Greist 2002 and Farzanfar 2011.
Obstructive sleep apnoea syndrome (OSAS)
Two studies in the USA evaluated ATCS for managing OSAS (DeMolles 2004; Sparrow 2010). Sample sizes were 30 and 250 participants, respectively, with mean ages of 46 years and 55 years. Both studies included participants who were obese (BMI greater than 35 kg/m2), and 82% of participants in Sparrow 2010 were men.
Both studies assessed an IVR system with automated functions. DeMolles 2004 compared once weekly calls (for two months) to usual care for barrier identification/problem solving, prompting review of outcome goals or self‐monitoring of behaviour, teaching to use prompts/cues and using of follow‐up prompts. Sparrow 2010 compared an IVR intervention underpinned by social cognitive theory and motivational interviewing consisting of once weekly (for the first month) then once monthly (up to one year) calls versus attention placebo control. The intervention aimed at barrier identification/problem solving, motivational interviewing, prompting review of behavioural goals, self‐monitoring of behaviour, providing feedback on performance, tailoring, teaching to use prompts/cues and using follow‐up prompts.
The primary outcome in both studies was continuous positive airway pressure (CPAP) use. Secondary outcomes included the sleep symptoms checklist, functional outcomes of sleep questionnaire (DeMolles 2004; Sparrow 2010), and depression (Sparrow 2010).
Smoking
Ten studies evaluated ATCS for managing tobacco dependence: five studies were conducted in the USA (Carlini 2012; Ershoff 1999; Regan 2011; Rigotti 2014; Velicer 2006), three in Canada (McNaughton 2013; Reid 2007; Reid 2011), one in Norway (Brendryen 2008), and one in Taiwan (Peng 2013). Sample sizes ranged from 44 in McNaughton 2013 to 2054 in Velicer 2006, and mean participant age ranged from 20 years in Peng 2013 to 54 years in Reid 2007. In Carlini 2012, 43% of participants had one or more chronic conditions. Participants in Reid 2007 were diagnosed with acute coronary syndrome and were hospitalised prior to the smoking cessation intervention.
Seven studies used an ATCS Plus system (Brendryen 2008; Carlini 2012; Peng 2013; Reid 2007; Reid 2011; Regan 2011; Rigotti 2014), one of which was a multimodal/complex intervention where participants received emails, web pages, SMS and an access to craving helpline (Brendryen 2008). Three studies used an IVR system (Ershoff 1999; McNaughton 2013; Velicer 2006), two of which had three arms: Ershoff 1999 compared the IVR intervention versus motivational interviewing or booklet only control, whereas Velicer 2006 compared three multimodal/complex interventions: nicotine replacement therapy (NRT) plus manual, NRT plus manual plus expert system, and NRT plus manual plus expert system plus IVR. Comparators in other studies included self‐help intervention (booklet) (Brendryen 2008), inactive IVR call (Carlini 2012; Peng 2013; Regan 2011), usual care (Reid 2007; Reid 2011; Rigotti 2014), and no calls (McNaughton 2013).
In addition to automated functions, four studies used communicative functions (Carlini 2012; Reid 2007; Reid 2011; Regan 2011), two used supplementary functions (Brendryen 2008; Peng 2013), and one used both (Rigotti 2014). Theoretical underpinnings included cognitive behavioural theory (Brendryen 2008; Peng 2013), motivational interviewing (Brendryen 2008; Peng 2013), relapse prevention and self‐regulation theory (Brendryen 2008), social cognitive theory (Brendryen 2008), and transtheoretical model of change (Peng 2013; Ershoff 1999; Velicer 2006). Interventions were typically aimed at planning action and setting goals, prompting self‐monitoring of behavioural outcome, providing rewards contingent on effort or progress towards behaviour, providing information on consequences of behaviour in general, setting graded tasks, tailoring, prompting self‐monitoring of behaviour and providing follow‐up prompts, providing feedback on performance, identifying barrier/solving problems, motivating individuals, planning social support/social change or preventing relapses/planning coping. The duration of intervention ranged from three calls only in Reid 2007 to biweekly IVR calls for two years in McNaughton 2013. The call duration ranged from 3 to 5 minutes in McNaughton 2013 to 18.9 minutes in Peng 2013.
Primary outcome measures included smoking abstinence rates (McNaughton 2013; Regan 2011; Reid 2007; Reid 2011; Velicer 2006), repeated point abstinence (Brendryen 2008); re‐enrolment into quit line support (Carlini 2012); biochemically confirmed smoking abstinence (Ershoff 1999; McNaughton 2013; Rigotti 2014); stage of change, self‐efficacy, and decisional balance (Peng 2013). Secondary outcome measures included nicotine replacement therapy adherence, self‐efficacy and nicotine dependence (averaged score) in Brendryen 2008; satisfaction with the intervention in Ershoff 1999; medication use in Regan 2011; and self‐reported tobacco abstinence and costs in Rigotti 2014.
Spinal cord dysfunction
One study (N = 142) compared an IVR system versus usual care for managing spinal cord injury or multiple sclerosis in the USA (Houlihan 2013). Participants' mean age was 48 years; they were predominantly men (61%) who had had their condition for an average of 11.7 years. At baseline, they were also diagnosed with pressure ulcers or depression. The intervention consisted of weekly calls lasting an average of 4.12 minutes, and it was underpinned by the transtheoretical model of change and social cognitive theory. The intervention was aimed at emotional control training, prompting self‐monitoring of behaviour and self‐monitoring of behavioural outcome. Authors reported prevalence of pressure ulcers, depression severity, and healthcare utilisation.
Excluded studies
We excluded 252 studies at the full‐text screening stage. Studies with reasons for exclusion are presented in Characteristics of excluded studies. These reasons pertained to a wrong type of intervention in 165 (65%) studies; inappropriate design in 65 studies (26%); no preventive healthcare/management of long‐term conditions in 21 (8%); or others (1%).
Risk of bias in included studies
We present our judgements about each risk of bias item across all included studies as (summary) percentages in Figure 8. Figure 9 shows judgements about each risk of bias item for each included study separately.
8.
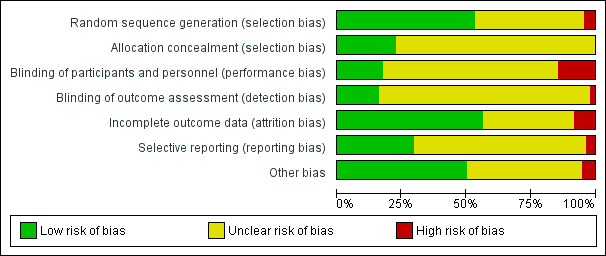
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
9.
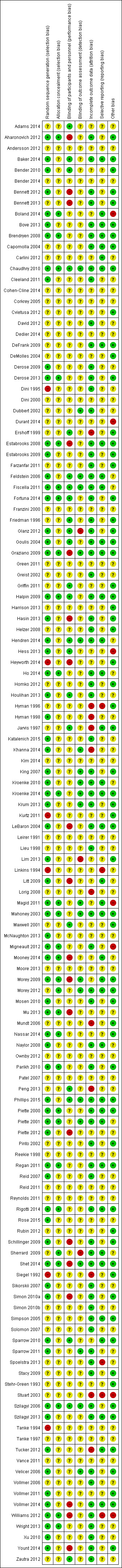
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Among 132 included trials, 70 (53%) precisely explained an adequate randomisation process, so we rated them as being at low risk of bias. Fifty‐six studies (42%) had an unclear method of sequence generation, meaning there was insufficient information to assign a high or low risk rating. We considered six studies (5%) to be at high risk of bias for random sequence generation (Dini 1995; Heyworth 2014; Kurtz 2011; Linkins 1994; Siegel 1992; Tanke 1994). Heyworth 2014 used pseudo‐random number generator, and Dini 1995 assigned clients with last names beginning with the letters A through L to receive the intervention. Kurtz 2011 allocated participants without medical practitioner or telephone to the intervention group, and Linkins 1994 allocated children to an intervention group if their telephone numbers ended in an odd number. Siegel 1992 assigned participants to the experimental or control group based on the block of time during which investigators identified them, and Tanke 1994 used a quasi‐experimental design because of economic limitations/lack of resources.
Among the included trials, 30 (23%) explained how they performed allocation concealment, meriting their rating as being at low risk of bias. We assessed the other 102 (77%) studies as being at unclear risk of bias for allocation concealment (selection bias), meaning there was insufficient information to allow judgement of high or low risk. We did not consider any of the included studies to be at high risk of bias in this domain.
Blinding
Among the included trials, 23 (17.4%) precisely described an adequate procedure for blinding of participants and personnel, and we rated them as being at low risk of bias. Ninety studies (68.1%) had an unclear method of blinding, meaning there was insufficient information to allow judgement of high or low risk. We considered 19 studies (14.3%) to be at high risk of performance bias (Aharonovich 2012; Bennett 2012; Bennett 2013; Estabrooks 2008; Graziano 2009; Hasin 2013; Heyworth 2014; LeBaron 2004; Mu 2013; Litt 2009; Mooney 2014; Morey 2009; Piette 2012; Schillinger 2009; Shet 2014; Simon 2010a; Vollmer 2014; Williams 2012; Yount 2014). In these studies, the authors of primary studies clearly mentioned the reasons for lack of blinding.
Among the included trials, 21 (15.9%) described an adequate procedure for blinding of outcome assessors. We rated these studies as being at low risk of bias for this item. One hundred and eight studies (81.8%) had an unclear method of blinding of outcome assessors, meaning there was insufficient information to allow judgement of high or low risk. We considered three studies (2.2%) to be at high risk of detection bias (Glanz 2012; Sherrard 2009; Lim 2013); similarly, the reasons for non‐blinding of outcome assessors were clearly mentioned.
Incomplete outcome data
In 74 trials (56%), there was no substantial loss of data, or we considered that authors imputed them using appropriate methods. We rated these studies as being at low risk of bias for this domain. Forty‐eight studies (36%) had an unclear method of addressing of incomplete data, meaning there was insufficient information about reporting of attrition/exclusions to permit judgement of low or high risk of bias. We considered 11 studies (8%) to be at high risk of attrition bias (Ershoff 1999; Hyman 1996; Hyman 1998; Jarvis 1997; Khanna 2014; Lorig 2008; Mundt 2006; Peng 2013; Siegel 1992; Stuart 2003; Tucker 2012). Four trials included only the completers in the final analyses (Ershoff 1999; Hyman 1996; Jarvis 1997; Lorig 2008). Peng 2013 and Tucker 2012 potentially applied simple imputations inappropriately, and there was an imbalance in numbers and no reasons for missing data. Four studies all had a high attrition rate, potentially introducing bias (Hyman 1998; Khanna 2014; Siegel 1992 and Stuart 2003).
Selective reporting
Among the included trials, we considered 39 (29.5%) to be at low risk of reporting bias, meaning that authors reported all relevant outcomes of interest or that study protocols were available. We assigned an unclear rating to 88 studies (66.6%), meaning there was insufficient information to permit judgement of whether any risk of this bias was present. We considered five studies (4%) to be at high risk of reporting bias (Hyman 1996; Linkins 1994; Spoelstra 2013; Stuart 2003; Williams 2012). Hyman 1996 used a complete case analysis. Linkins 1994 did not report data on the differences between the groups by county, type of residence, ethnicity, sex, or age, and Spoelstra 2013 did not report outcomes on depression scores at the study's completion. Although the authors of Stuart 2003 mentioned that there were no significant differences in medication adherence among the three groups, the analyses were restricted to one subgroup of patients who completed the IVR calls. Williams 2012 did not report six‐month secondary outcomes.
Other potential sources of bias
In 66 trials (50%), there were no baseline imbalances, indicating low risk of other bias. Fifty‐nine studies (44.6%) had an unclear risk for this item, meaning there was insufficient information about baseline imbalances to permit judgement of low or high risk. We considered seven studies (5%) to have a potentially high risk of other bias because of significant baseline imbalances (Boland 2014; Durant 2014; Hess 2013; Magid 2011; Migneault 2012; Williams 2012), or in the case of Stuart 2003, because authors failed to report baseline characteristics.
We included five cluster RCTs in the review (Feldstein 2006; Franzini 2000; Hess 2013; Krum 2013; Stuart 2003). Only Krum 2013 appropriately adjusted for clustering in the analysis. For the remaining four studies, it was not possible to determine whether selective recruitment of cluster participants was likely to introduce bias, as they did not report sufficient details. Several indicated baseline differences between groups (Franzini 2000; Hess 2013), and one did not report any information about this (Stuart 2003). We calculated an approximate sample size for Hess 2013, while the other three studies have unit of analysis errors that may lead to overly precise effect estimates being reported for these studies (Feldstein 2006; Franzini 2000; Stuart 2003).
Overall quality of the evidence
We also assessed and reported on the quality of the evidence, using the GRADE criteria. Appendix 13 presents results of this assessment for each study, and we report them alongside the main results for the review in each 'Summary of findings' table.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12
Summary of findings for the main comparison. Preventive healthcare: effects of ATCS on health services uptake (immunisations).
| ATCS versus control on immunisation rates | ||||||
|
Patient or population: participants at risk of under‐immunisation (children, adolescents and adults)
Settings: primary care
Intervention: ATCS (ATCS+, IVR, unidirectional) Comparison: no intervention, usual care or health information (letter) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ATCS | |||||
|
Behavioural outcome: immunisation rate ATCS Plus, IVR, unidirectional versus no calls, letters, usual care at median follow‐up of 4 months |
Study populationa: children Comparator: no intervention |
RR 1.25 (1.18 to 1.32) |
10,454 (5 studies) | ⊕⊕⊕⊝ Moderatec | Franzini 2000 (N = 1138) reported that compared with controls (no calls), unidirectional ATCS (autodialer) may increase immunisation rates in children (86% versus 64%, low certainty).d | |
| 308 per 1000 | 385 per 1000 (363 to 406) | |||||
| Moderateb | ||||||
| 373 per 1000 | 466 per 1000 (440 to 492) | |||||
|
Behavioural outcome: immunisation rate Unidirectional ATCS versus usual care at median follow‐up of 15 months |
Study populationa: adolescents Comparator: usual care |
RR 1.06 (1.02 to 1.11) | 5725 (2 studies) | ⊕⊕⊕⊝ Moderatee | Szilagyi 2013 (N = 4115) also reported that unidirectional ATCS probably slightly improves the uptake of preventive care visits, compared with usual care (63% ATCS versus 59% usual care; moderate certainty evidencef). | |
| 543 per 1000 | 576 per 1000 (554 to 603) | |||||
| Moderateb | ||||||
| 540 per 1000 | 572 per 1000 (551 to 599) | |||||
|
Behavioural outcome: immunisation rate Unidirectional ATCS versus no calls or health information at median follow‐up of 2.5 months |
Study populationa: adults Comparator: no calls or health information |
RR 2.18 (0.53 to 9.02) |
1743 (2 studies) | ⊕⊝⊝⊝ Very lowg,h | — | |
| 10 per 1000 | 21 per 1000 (5 to 88) | |||||
| Moderateb | ||||||
| 66 per 1000 | 144 per 1000 (35 to 595) | |||||
|
Adverse outcome: unintended adverse events attributable to the intervention ATCS+, IVR, unidirectional versus various controls |
No studies reported adverse events. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ATCS Plus: automated telephone communication systems with additional functions; ATCS: automated telephone communication systems; CI: confidence interval; IVR: interactive voice response; RR: risk ratio; unidirectional ATCS enable non‐interactive voice communication and use one‐way transmission of information or reminders. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aThe assumed risk represents the mean control group risk across studies (calculated by GRADEPro). bThe assumed risk represents the median control group risk across studies (calculated by GRADEPro). cDowngraded as all six studies were rated as at unclear risk of bias on most domains, including all unclear on allocation concealment; and one study at high risk for randomisation, one study at high risk of performance bias (−1). dDowngraded as results are from only one cluster RCT that failed to adequately adjust for clustering in analysis (−1); all risk of bias domains were rated as at unclear risk (−1). eDowngraded as one of two studies was rated as at unclear risk on allocation concealment and attrition bias domains (−1). fDowngraded as study was rated as at unclear risk on allocation concealment and attrition bias domains (−1). gDowngraded as both studies were rated as at unclear on attrition bias, and one study (Hess 2013) was rated as at unclear risk on allocation concealment and at high risk of bias on the 'other' domain (reflecting baseline imbalances between groups and a lack of information to judge whether selective recruitment of participants was adjusted for (−1). hDowngraded as there were wide confidence intervals around the effect estimate (imprecision) (−1); downgraded as substantial level of heterogeneity was detected (inconsistency) (−1).
Summary of findings 2. Preventive healthcare: effects of ATCS on physical activity levels.
| ATCS versus control on physical activity levels | |||
|
Patient or population: participants at risk of developing long‐term conditions Settings: various settings Intervention: ATCS (multimodal/complex intervention, ATCS+, IVR) Comparison: no intervention, usual care, or IVR | |||
| Outcomes | Effect of intervention a | No of participants (studies) | Quality of the evidence (GRADE) |
|
Behavioural outcome: physical activity Multimodal/complex interventionb versus no calls |
The intervention may slightly improve the frequency of walks. | 181 (1 study) |
⊕⊕⊝⊝ Lowc |
|
Behavioural outcome: physical activity, 12 months Multimodal/complex interventiond versus usual care |
The intervention probably has mixed effects on gait speeds, little effect on functional outcomes (moderate certaintye) and may slightly increase physical activity levels (low certaintyf). | 700 (2 studies) |
— |
|
Behavioural outcome: physical activity ATCS Plus versus IVR control |
2 studies reported that ATCS Plus intervention may have little or no effect on different indices of physical activity. | 369 (2 studies) |
⊕⊕⊝⊝ Lowc |
|
Behavioural outcome: physical activity IVR versus usual care, control or health education |
3 studies reported that IVR interventions may slightly improve several indices of physical activity (muscle strength, balance, moderate to vigorous physical activity) but may have little or no effect on others (physical activity levels, walking distance). | 216 (3 studies) |
⊕⊕⊝⊝ Lowg |
|
Clinical outcome: metabolic markers, 12 months Multimodal/complex interventiond versus usual care |
The intervention may have little or no effect on glycated haemoglobin, fasting insulin and glucose levels. | 302 (1 study) |
⊕⊕⊝⊝ Lowf |
|
Clinical outcome: body weight measures Multimodal/complex interventiond ATCS Plus versus usual care or control |
ATCS Plus intervention may have little or no effect on BMI, weight, waist or waist‐hip ratio, compared with control (71 participants; low certainty evidencec). Multimodal/complex intervention may have little or no effect on BMI, waist circumference or physical function, compared with usual care (302 participants; low certainty evidencef). |
373 (2 studies) |
⊕⊕⊝⊝ Low |
|
Adverse outcome: unintended adverse events attributable to the intervention Multimodal/complex intervention, ATCS Plus, IVR versus various controls |
No studies reported adverse events. | — | — |
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | |||
| ATCS: automated telephone communication systems; ATCS Plus: automated telephone communication systems with additional functions; IVR: interactive voice response. | |||
aThe findings presented are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bMultimodal intervention included 10 nurse‐delivered and 10 automated phone calls. cDowngraded as randomisation and allocation concealment were rated as at unclear risk of bias (−1); and results (for each outcome) were obtained from a single study at some potential risk of bias (−1). dMultimodal intervention included counselling by lifestyle counsellor, automated telephone messaging, endorsement and tailored mailings. eDowngraded as results were obtained from a single study (−1). fDowngraded as randomisation was rated as at unclear risk of bias (−1), and results for each outcome were obtained from a single study at some potential risk of bias (−1). gDowngraded as one study was at unclear risk for randomisation and at high risk for attrition, while two studies were at unclear risk for allocation concealment (−1); results were obtained from a single study (for each outcome) at some potential risk of bias (−1).
Summary of findings 3. Preventive healthcare: effects of ATCS on health services uptake (screening).
| ATCS versus control on screening rates | ||||||
|
Patient or population: participants at risk for breast, colorectal or cervical cancer; or osteoporosis Settings: primary, secondary and tertiary care Intervention: ATCS (multimodal/complex intervention, ATCS Plus, IVR, unidirectional) Comparison: usual care, enhanced usual care or no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Usual care or enhanced usual care or no intervention | ATCS | |||||
|
Behavioural outcome: breast cancer screening Multimodal/complex intervention versus usual care at 12 months follow‐up |
Study populationa | RR 2.17 (1.55 to 3.04) | 462 (2 studies) | ⊕⊕⊕⊕ High | — | |
| 167 per 1000 | 363 per 1000 (259 to 508) | |||||
| Moderateb | ||||||
| 167 per 1000 | 363 per 1000 (259 to 508) | |||||
|
Behavioural outcome: breast cancer screening IVR versus enhanced usual care at median follow‐up of 12 months |
Study populationa | RR 1.05 (0.99 to 1.11) | 2599 (2 studies) | ⊕⊕⊕⊝ Moderatec | Unidirectional ATCS versus letter 1 further study (Fortuna 2014) (N = 1008) found that unidirectional ATCS (plus letter) probably has little or no effect on breast cancer screening rates at 12 months, adjusted OR 1.3 (95% CI 0.7 to 2.4; moderate certaintyd). |
|
| 585 per 1000 | 614 per 1000 (579 to 649) | |||||
| Moderateb | ||||||
| 432 per 1000 | 454 per 1000 (428 to 480) | |||||
|
Behavioural outcome: colorectal cancer screening Multimodal/complex intervention versus usual care at median follow‐up of 12 months |
Study populationa | RR 2.19 (1.88 to 2.55) | 1013 (3 studies) | ⊕⊕⊕⊕ High | — | |
| 249 per 1000 | 545 per 1000 (468 to 635) | |||||
| Moderateb | ||||||
| 167 per 1000 | 366 per 1000 (314 to 426) | |||||
|
Behavioural outcome: colorectal cancer screening IVR versus usual care at 6‐month follow‐up |
Study populationa | RR 1.36 (1.25 to 1.48) | 16915 (2 studies) | ⊕⊕⊕⊝ Moderatee | IVR versus control 1 other study (Durant 2014) (N = 47,097) reported that IVR probably increases screening, with 1773 participants from the IVR group and 100 from the no‐call control group completing colorectal cancer screening within 3 months (moderate certaintyf). IVR versus usual care 1 study (Mosen 2010) (N = 6000) also reported that IVR probably increases completion of any colorectal cancer screening (moderate certaintyg). |
|
| 119 per 1000 | 161 per 1000 (148 to 176) | |||||
| Moderateb | ||||||
| 119 per 1000 | 162 per 1000 (149 to 176) | |||||
|
Behavioural outcome: colorectal cancer screening IVR, unidirectional ATCS versus usual care or letter at longer (9‐12 months) follow‐up |
Study populationa | RR 1.01 (0.97 to 1.05) | 21,335 (2 studies) | ⊕⊕⊕⊝ Moderateh | IVR versus usual care 1 study (Simon 2010a) (N = 20,000) also reported that IVR probably increases slightly colorectal cancer screening via colonoscopy (moderate certaintyi). Unidirectional ATCS versus letter 1 further study (Fortuna 2014) (N = 1008) at 12 months found that unidirectional ATCS (plus letter) has probably little or no effect on colorectal cancer screening rates at 12 months (15.3% versus 12.2%; adjusted OR 1.2; 95% CI 0.6 to 2.4; moderate certaintyd). |
|
| 302 per 1000 | 305 per 1000 (293 to 317) | |||||
| Moderateb | ||||||
| 245 per 1000 | 247 per 1000 (238 to 257) | |||||
|
Behavioural outcome: cervical cancer screening ATCS Plus versus control (no calls) at 3 month follow‐up |
See comment | See comment | Not estimable | 75,532 (1 study) |
⊕⊕⊕⊝ Moderatej | Corkrey 2005 found that ATCS Plus intervention probably slightly improves cervical cancer screening rates at 3 months. |
|
Adverse outcome: unintended adverse events attributable to the intervention Multimodal/complex intervention, ATCS Plus, IVR, unidirectional versus various controls |
No studies reported adverse events. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ATCS: automated telephone communication systems; ATCS Plus: automated telephone communication systems with additional functions; BMD: bone mineral density; CI: confidence interval; HR: hazard ratio; IVR: interactive voice response; OR: odds ratio; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aThe assumed risk represents the mean control group risk across studies (calculated by GRADEPro). bThe assumed risk represents the median control group risk across studies (calculated by GRADEPro). cDowngraded as risk of bias was unclear for allocation concealment in both studies, and randomisation and blinding rated unclear in one study (−1). dDowngraded as confidence intervals were wide (imprecision) and included both a potential harm and a potential benefit (−1). eDowngraded as risk of bias was unclear for all items in one study, and in the other allocation concealment and blinding were rated as unclear (−1). fDowngraded as risk of bias was unclear for all items except 'other' bias, which was rated as high risk (−1). gDowngraded as risk of bias was rated unclear for allocation concealment and blinding (−1). hDowngraded as risk of bias was rated as unclear for allocation concealment in both studies and blinding was rated high risk in one study (−1). iDowngraded as risk of bias was rated unclear for allocation concealment and high risk for blinding (−1). jDowngraded as all items were rated as at unclear risk of bias (−1).
Summary of findings 4. Preventive healthcare: effects of ATCS on weight management.
| ATCS versus control for body weight | ||||||
|
Patient or population: overweight or obese individuals (both children and adults)
Settings: various settings
Intervention: ATCS (multimodal/complex intervention, ATCS Plus, IVR) Comparison: usual care, no intervention or control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Commentsa | |
| Assumed risk | Corresponding risk | |||||
| Controls | ATCS | |||||
|
Clinical and behavioural outcome: BMI score in adults Multimodal/complex intervention, ATCS Plus or IVR versus usual care at median follow‐up of 18 months |
The mean BMI in the control groups was 34.7 kg/m2 | The mean BMI of adults in the intervention groups was 0.64 kg/m2lower (1.38 lower to 0.11 higher) | Not estimable | 672 (3 studies) | ⊕⊕⊝⊝ Lowb | ATCS Plus versus control Vance 2011 (N = 140) found that ATCS Plus may reduce slightly BMI (low certainty evidencec). |
| Clinical and behavioural outcome: body weight in adults, 12 weeks | See comment | See comment | Not estimable | See comment | See comment | ATCS Plus versus control Vance 2011 (N = 140) found that ATCS Plus may reduce slightly body weight and waist circumference (low certainty evidencec). IVR versus control Estabrooks 2008 (N = 77) reported that IVR may have little or no effect on body weight (percent lost or change in) (low certainty evidenced). |
| Clinical and behavioural outcome: body weight in adults, at median follow‐up of 18 months | See comment | See comment | Not estimable | See comment | See comment | ATCS (multimodal/complex intervention, ATCS Plus, IVR) versus usual care Bennett 2012 (N = 365) found that ATCS Plus probably slightly reduces body weight at 18 months (moderate certainty evidence).eBennett 2013 (N = 194) found that multimodal/complex intervention may reduce body weight at 18 months (low certainty evidence).f IVR versus usual care Goulis 2004 (N = 122) found that IVR probably reduces slightly body weight but probably has little or no effect on obesity assessment scores at 6 months (moderate certainty evidence).f |
| Clinical and behavioural outcome: blood pressure, blood glucose, cholesterol levels | See comment | See comment | Not estimable | See comment | See comment | ATCS (ATCS Plus, IVR) versus usual care/control Bennett 2012 (N = 365) found that ATCS Plus probably has little or no effect on systolic or diastolic blood pressure at 18 months (moderate certainty evidencee). ATCS Plus versus control Vance 2011 found that ATCS Plus may slightly improve slightly systolic blood pressure and blood glucose levels at 12 weeks (low certainty evidencec). IVR versus usual care Goulis 2004 (N = 122) found that IVR probably has little or no effect on systolic or diastolic blood pressure, plasma glucose levels, or high‐density lipoprotein cholesterol, but it probably slightly reduces total cholesterol and triglyceride levels at 6 months (moderate certainty evidence).e |
| Clinical outcome: BMI z‐score in children at median follow‐up of 7.5 months | See comment | See comment | Not estimable | See comment | ⊕⊕⊕⊝ Moderatee | ATCS Plus versus control Estabrooks 2009 (N = 220) found that ATCS Plus has probably little or no effect on BMI z‐scores in children at 12 months. IVR versus control Wright 2013 (N = 100) found that IVR has probably little or no effect on BMI z‐scores in children at 3 months. |
| Behavioural outcome: physical activity, dietary habits in children at median follow‐up of 7.5 months | See comment | See comment | Not estimable | See comment | ⊕⊕⊕⊝ Moderate4 | ATCS Plus versus control Estabrooks 2009 (N = 220) found that ATCS Plus has probably little or no effect on self‐reported physical activity, sedentary behaviours or dietary habits at 12 months. IVR versus control (no calls) Wright 2013 (N = 100) found that IVR has probably little or no effect on total caloric intake, fruit intake, or sedentary behaviours at 3 months. |
|
Adverse outcome: unintended adverse events attributable to the intervention IVR versus usual care |
See comment | See comment | See comment | 559 (2 studies) |
See comment |
Bennett 2012 (N = 365) reported 1 serious musculoskeletal injury in the intervention group and 3 events (1 cardiovascular and 2 cases of gallbladder disease) in the usual care group (moderate certainty evidence).e,g Bennett 2013 (N = 194) reported 6 serious adverse events in the intervention arm, including gynaecological surgery in 2 participants and knee replacement, breast abscess, musculoskeletal injury, and cancer diagnosis in 1 participant each; all participants except the one with the cancer diagnosis required hospitalisation (low certainty evidence).f,g |
| *The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ATCS: automated telephone communication systems; ATCS Plus: automated telephone communication systems with additional functions; BMI: body Mass Index; CI: confidence interval; IVR: interactive voice response; SMD: Standardised mean difference. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aAdditional findings presented are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bDowngraded as allocation concealment was rated as at unclear risk of bias in all three studies, and randomisation unclear in one study, with high risk of performance bias in two studies (−1); downgraded as substantial level of heterogeneity was detected (inconsistency) (−1). cDowngraded as all items were rated as at unclear risk of bias (−1); and results were obtained from a single small study at potential risk of bias (−1). dDowngraded as performance bias was rated as high risk (−1); and results were obtained from a single very small study at potential risk of bias (−1). eDowngraded as results were each obtained from a single small study (−1). fDowngraded as randomisation and allocation concealment was rated as at unclear risk and performance bias was rated as high risk (−1); and results were obtained from a single small study at potential risk of bias (−1). gThe authors of the study could not conclusively determine whether reported events resulted from study participation.
Summary of findings 5. Preventive healthcare or management of long‐term conditions: effects of ATCS as appointment reminders/reducing non‐attendance rates.
| ATCS versus control as appointment reminders (reducing non‐attendance rates) | |||
|
Patient or population: patients/healthcare consumers
Settings: various settings
Intervention: ATCS (ATCS Plus, IVR, unidirectional) Comparison: no intervention (calls) or nurse‐delivered calls | |||
| Outcomes | Effect of interventiona | No of participants (studies) | Quality of the evidence (GRADE) |
|
Health behaviour: attendance rates, 6 weeks ATCS Plus versus nurse‐delivered calls |
ATCS Plus calls delivered 3 or 7 days prior to flexible sigmoidoscopy or/and colonoscopy examinations probably have little or no effect on appointment non‐attendance or preparation non‐adherence. | 3610 (1 study) |
⊕⊕⊕⊝ Moderateb |
|
Health behaviour: attendance rates, 4 months IVR versus no calls |
IVR improves attendance rates: OR 1.52 (95% CI 1.34 to 1.71). | 12,092 (1 study) |
⊕⊕⊕⊕ High |
|
Health behaviour: return tuberculin test rate, 3 days Unidirectional ATCS versus no calls |
Unidirectional ATCS may improve test return rates. | 701 (1 study) |
⊕⊕⊝⊝ Lowc |
|
Health behaviour: attendance rates, 1 month Unidirectional ATCS versus no calls |
Undirectional ATCS may improve attendance rates RR 1.60 (95% CI 1.29 to 1.98). | 517 (1 study) |
⊕⊕⊝⊝ Lowc |
|
Health behaviour: attendance rates, 6‐8 weeks Unidirectional ATCS versus no calls |
2 studies reported conflicting results: Reekie 1998 (N = 1000) reported that unidirectional ATCS probably decrease non‐attendance rates at 6 weeks; while Maxwell 2001 (N = 2304) reported the interventions probably have little or no effect at 2 months. | 3304 (2 studies) |
⊕⊕⊕⊝ Moderated |
|
Health behaviour: attendance rates, 6 months Unidirectional ATCS versus no calls |
Unidirectional ATCS may improve attendance: OR 1.50 (P < 0.01). | 2008 (1 study) |
⊕⊕⊝⊝ Lowe |
|
Adverse outcome: unintended adverse events attributable to the intervention ATCS Plus, IVR, unidirectional ATCS versus various controls |
No studies reported adverse events. | ||
| ATCS: automated telephone communication systems; ATCS Plus: automated telephone communication systems with additional functions; CI: confidence interval; IVR: interactive voice response; OR: odds ratio; RR: risk ratio. | |||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | |||
aThe findings presented are based on a narrative summary and synthesis of results, many of which were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bDowngraded as most items (including randomisation and allocation concealment) were rated as being at unclear risk of bias (−1). cDowngraded as both studies considered were rated as being at high risk of bias on randomisation and at unclear risk on allocation concealment and other items (‐2) (Dini 1995; Tanke 1994). dDowngraded as all items were rated as being at unclear risk of bias (−1). eDowngraded as randomisation was rated as at high risk of bias; and study was rated as at unclear risk of bias on other items (‐2).
Summary of findings 6. Long‐term management: effects of ATCS on adherence to medication or laboratory tests.
| ATCS versus control for adherence to medication or laboratory tests | ||||
|
Patient or population: patients with various conditions or at risk of low adherence to medication or laboratory tests Settings: various settings Intervention: ATCS (multimodal/complex intervention, ATCS Plus, IVR, unidirectional ATCS) Comparison: usual care, no calls, controls (other ATCS) | ||||
| Outcomes | Effect of interventionsa | No of participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Behavioural outcome: adherence to medication Multimodal/complex interventionsb versus usual care or control |
The effects of multimodal/complex interventions are inconclusive. | 888 (2 studies) |
See comment | Ho 2014 (N = 241) reported that the multimodal/complex intervention probably improves adherence to cardioprotective medications at 12 months (moderate certaintyc). Stuart 2003 (N = 647) found uncertain effects of the intervention on adherence to antidepressant medications (very low certaintyc,d). |
|
Behavioural outcome: adherence to medication ATCS Plus versus control or single IVR call |
Results suggest that ATCS Plus probably slightly improve measures of adherence. | 2340 (2 studies) |
See comment | Cvietusa 2012 (N = 1393) reported that ATCS Plus, compared with control, probably improves time to first inhaled corticosteroid refill and probably slightly improves the proportion of days with medication on hand in children (moderate certaintye). Stacy 2009 (N = 947) reported that ATCS Plus probably slightly improves statin adherence at 6 months, compared with a single IVR call (moderate certaintyf). |
|
Behavioural outcome: adherence to laboratory tests ATCS Plus or IVR versus no intervention or usual care |
Results suggest that ATCS Plus probably has little or no effect on adherence to testing, while IVR probably improves test completion. | 15,218 (3 studies) |
See comment | ATCS Plus versus no intervention Derose 2009 (N = 13,057) found that ATCS Plus probably has little or no effect on adherence to testing (completion of all 3 recommended laboratory tests for diabetes patients) at 12 weeks (moderate certaintyg). Simon 2010b (N = 1200) found that these interventions probably have little or no effect on retinopathy examination rates or tests for glycaemia, hyperlipidaemia or nephropathy in diabetic patients at 12 months (moderate certaintyh). IVR versus usual care Feldstein 2006 (N = 961) found that IVR probably improves patients' completion of all recommended laboratory tests at 25 days follow‐up (moderate certaintyi). |
|
Behavioural outcome: adherence to medication or composite outcome (medication adherence and rate of adverse events) ATCS Plus versus usual care |
Results indicate that ATCS Plus probably improves medication adherence and may slightly improve a composite measure. | 35,816 (4 studies) |
See comment | 2 studies (Derose 2013 (N = 5216) and Vollmer 2014 (N = 21,752)) reported that ATCS Plus probably improves adherence to statins to some extent. Vollmer 2011 (N = 8517) found that ATCS Plus probably slightly improves adherence to inhaled corticosteroids (moderate certaintyj). Sherrard 2009 (N = 331) found that ATCS Plus may slightly improve a composite measure of medication adherence and adverse events at 6 months follow‐up (low certaintyc,k). |
|
Behavioural outcome: adherence to medication or laboratory tests IVR versus control |
Results suggest that IVR probably improves slightly medication adherence. | 4,238,362 (4 studies) |
See comment | Adams 2014 (N = 475) found that IVR may slightly improve comprehensiveness of screening and counselling (low certaintyc,l). Bender 2010 (N = 50) reported that IVR may improve adherence to anti‐asthmatic medications at 2.5 months follow‐up (low certaintyc,e). Leirer 1991 (N = 16) reported that IVR may slightly reduce medication non‐adherence (low certaintym). Mu 2013 (N = 4,237,821) found that IVR probably slightly improves medication refill rates at 1 month (moderate certaintyn). |
|
Behavioural outcome: adherence to medication IVR versus usual care |
Results indicate that IVR probably slightly improves some measures of medication adherence. | 56,140 (8 studies) |
See comment | 2 studies (Boland 2014 (N = 70); Friedman 1996 (N = 267)) reported that IVR probably slightly improves adherence to glaucoma and anti‐hypertensive medications at 3 and 6 months respectively (moderate certainty).o 2 further studies (Glanz 2012 (N = 312); Migneault 2012 (N = 337)) reported that IVR has probably little or no effect on medication adherence at 8 and 12 months, respectively (moderate certainty).p 2 studies (Green 2011 (N = 8306); Reynolds 2011 (N = 30,610)) assessed adherence via refill rates, reporting that IVR probably slightly improves medication refill rates at 2 weeks (moderate certainty).q 2 further studies reported medication adherence assessed by medication possession ratio (MPR) at different time points. Patel 2007 (N = 15,051) found that IVR probably slightly improves MPR at 3 to 6 months, while Bender 2014 (N = 1187) reported that IVR probably improves MPR at 24 months (both studies of moderate certaintyr). |
|
Behavioural outcome: adherence to medication Unidirectional ATCS versus control |
Results suggest that unidirectional ATCS may have little effect, or improve medication adherence to a small degree. | 107 (2 studies) |
See comment | 2 studies (Lim 2013 (N = 80); Ownby 2012 (N = 27)) reported that the intervention may have little effect or slightly improve medication adherence (low certaintys). |
|
Clinical outcome: blood pressure Multimodal/complex, ATCS Plus, IVR versus usual care |
Results suggest that ATCS Plus probably slightly reduces blood pressure, while multimodal/complex or IVR interventions probably have little or no effect on blood pressure. | 22,597 (3 studies) |
See comment | Multimodal/complex intervention versus usual care Ho 2014 (N = 241) reported that multimodal intervention probably has little or no effect on achieving reduced blood pressure targets (moderate certaintyc). ATCS Plus versus usual care Vollmer 2014 (N = 21,752) reported that ATCS Plus probably slightly reduces systolic blood pressure (moderate certaintyt). IVR versus usual care Migneault 2012 (N = 337) reported that IVR probably has little or no effect on systolic or diastolic blood pressure (moderate certaintyc), while Friedman 1996 (N = 267) found that IVR may have little or no effect on systolic blood pressure but may slightly decrease diastolic blood pressure (low certaintyc,f). |
|
Adverse outcome: unintended adverse events attributable to the intervention Multimodal/complex intervention, ATCS Plus, IVR, unidirectional versus various controls |
No studies reported adverse events. | |||
| ATCS Plus: automated telephone communication systems with additional functions; CI: confidence interval; HR: hazard ratio; IVR: interactive voice response; MPR: medication possession ratio; OR: odds ratio; RR: risk ratio; SD: standard deviation | ||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||
aMultimodal intervention included ATCS Plus, medication reconciliation and tailoring, patient education and collaborative care in Ho 2014; and education, nurse‐delivered call and IVR in Stuart 2003. bThe findings presented are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. cDowngraded as results were obtained from a single study at potential risk of bias (−1). dDowngraded as rated as at high risk for attrition, reporting and other bias and at unclear risk on randomisation and allocation concealment (‐2). eDowngraded as almost all items were rated as being at unclear risk of bias (−1). fDowngraded as rated as at unclear risk of bias on randomisation, allocation concealment and other items (−1). gDowngraded as rated at unclear risk of bias on allocation concealment and other items (−1). hDowngraded as rated as at unclear risk for all items (except attrition bias, rated as low risk) (−1). iFeldstein 2006 did not appear to account for clustering, which may have resulted in an overestimation of the precision of the effect estimate (−1). jThree studies assessed together (Derose 2013; Vollmer 2011; Vollmer 2014): downgraded for risk of bias (allocation concealment rated as unclear in two studies and performance bias rated as high risk in one study) (−1). kDowngraded as rated at unclear risk of bias on randomisation and at high risk of detection bias (−1). lDowngraded as rated at unclear risk of bias on most items (except performance bias, rated as low risk) (−1). mDowngraded as all items were rated as being at unclear risk of bias (−1) and results were obtained from a single study with a very small sample size (N = 16) (−1). nDowngraded as most items were rated as being at unclear risk of bias (except randomisation and allocation concealment); performance bias rated as high (−1). oTwo studies assessed together (Boland 2014; Friedman 1996): downgraded for risk of bias as allocation concealment was rated as unclear in both studies, randomisation and attrition bias rated unclear in one study each, and there was a high risk of other bias (baseline imbalances) in one study (−1). pTwo studies assessed together (Glanz 2012; Migneault 2012): downgraded for risk of bias as allocation concealment was rated as unclear in one study, and detection bias and other bias (baseline imbalances) were both rated as being at high risk in one study (−1). qTwo studies assessed together (Green 2011; Reynolds 2011): downgraded for risk of bias as all items were rated as unclear in both studies (−1). rDowngraded as all items were rated as being at unclear risk of bias (−1). sTwo studies assessed together (Lim 2013; Ownby 2012): downgraded for risk of bias as allocation concealment and attrition bias were rated as being at unclear risk in both studies, and detection bias was rated as being at high risk in one study (−1); downgraded on imprecision as combined sample size was small (N = 107) (−1). tDowngraded as allocation concealment was at unclear risk of bias, and there was a high risk of performance bias (−1).
Summary of findings 7. Long‐term management: effects of ATCS on alcohol consumption.
| ATCS versus control on alcohol consumption | |||
|
Patient or population: participants addicted to alcohol Settings: various settings Intervention: ATCS (ATCS Plus, IVR) Comparison: no intervention, usual care, advice/education or packaged CBT | |||
| Outcomes | Effect of interventiona | No of participants (studies) | Quality of the evidence (GRADE) |
|
Behavioural outcomes: number of drinks per drinking day ATCS Plus, IVR versus usual care, (various) controls at median follow‐up of 2 months |
ATCS Plus versus usual care Rose 2015 (N = 158) reported that ATCS Plus may have little or no effect on the number of drinks per drinking day at 2 months (low certaintyb,c). ATCS Plus versus control (advice/education) Hasin 2013 (N = 254) found that ATCS Plus may reduce the number of drinks per drinking day in the last 30 days at 2 months (low certaintyb,c), but it may have little effect at 12 months. IVR versus control (information) Rubin 2012 (N = 47) reported that IVR may slightly reduce the number of drinks per drinking day at 6 months (low certaintyc,e). |
459 (3 studies) |
⊕⊕⊝⊝ Low |
|
Behavioural outcomes: drinking days, heavy drinking days, or total number of drinks consumed ATCS Plus, IVR versus (various) controls |
ATCS Plus versus no intervention Mundt 2006 (N = 60) found that ATCS Plus may have little or no effect on drinking days, heavy drinking days, or total number of drinks consumed (low certaintyc,f). ATCS Plus versus control (packaged CBT) Litt 2009 (N = 110) found that ATCS Plus may have little or no effect on the number of heavy drinking days at 12 weeks posttreatment (low certaintyc,g). IVR versus control (information) Rubin 2012 (N = 47) reported that IVR may slightly reduce the number of heavy drinking days per month at 6 months (low certaintyc,e). |
217 (3 studies) |
⊕⊕⊝⊝ Low |
|
Behavioural outcomes: proportion of days abstinent, other alcohol consumption indices, 12 weeks ATCS Plus versus control (packaged CBT) |
ATCS Plus may slightly reduce the proportion of days abstinent but have little or no effect on coping or drinking problems or continuity of abstinence (Litt 2009). | 110 (1 study) |
⊕⊕⊝⊝ Lowc,g |
|
Behavioural outcomes: weekly alcohol consumption, 6 months ATCS Plus versus usual care |
ATCS Plus may have little or no effect on weekly alcohol consumption (Helzer 2008). | 338 (1 study) |
⊕⊕⊝⊝ Lowc,h |
|
Behavioural outcomes: AUDIT score, 6 weeks IVR versus control (no intervention) |
IVR probably improve slightly AUDIT scores (Andersson 2012). | 1423 (1 study) |
⊕⊕⊕⊝ Moderatei |
|
Behavioural outcomes: other alcohol consumption indices, 4 weeks IVR versus control (no intervention) |
IVR may have little or no effect on drinking habits, alcohol craving, or PTSD symptoms (Simpson 2005). | 98 (1 study) |
⊕⊕⊝⊝ Lowc,h |
|
Adverse outcome: unintended adverse events attributable to the intervention ATCS Plus, IVR versus various controls |
No studies reported adverse events. | ||
| ATCS Plus: automated telephone communication systems with additional functions; AUDIT: Alcohol Use Disorders Identification Test; CBT: cognitive behavioural therapy; IVR: interactive voice response; PTSD: post‐traumatic stress disorder. | |||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | |||
aThe findings presented in this table are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bDowngraded as all items except randomisation were rated as being at unclear risk of bias (−1). cResults were obtained from a single small study at potential risk of bias (−1). dDowngraded as allocation concealment was rated as being at unclear risk of bias, and there was a high risk of performance bias (−1). eDowngraded as all items except 'other' bias were rated as being at unclear risk of bias (−1). fDowngraded as rated as being at unclear risk of bias on randomisation, allocation concealment and others, and at high risk of attrition bias (−1). gDowngraded as rated as being at unclear risk of bias on allocation concealment and attrition bias, and at high risk of performance bias (−1). hDowngraded as rated as being at unclear risk of bias on randomisation, allocation concealment and other items (−1). iDowngraded as all items were rated as being at unclear risk of bias (−1).
Summary of findings 8. Long‐term management: effects of ATCS on severity of cancer symptoms.
| ATCS versus control on severity of cancer symptoms | ||||
|
Patient or population: cancer patients Settings: various settings Intervention: ATCS (multimodal/complex intervention, ATCS Plus, IVR) Comparison: usual care, control (other ATCS, nurse‐delivered calls) | ||||
| Outcomes | Effects of interventiona | No of participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Clinical outcomes: symptoms (severity or burden) ATCS Plus versus usual care (via ATCS) or control, 4‐12 weeks |
Results suggest that ATCS Plus may have little or no effect on symptom severity, distress or burden. | 701 (4 studies) |
See comment | Cleeland 2011 (N = 79) found that ATCS Plus may slightly reduce symptom threshold events and cumulative distribution of symptom threshold events; and it may have little or no effect on mean symptom severity between discharge and 4 week follow‐up (low certaintyb,c). Mooney 2014 (N = 250) found that ATCS Plus probably has little or no effect on symptom severity scores at 6 week follow‐up (moderate certaintyc). Spoelstra 2013 (N = 119) found that ATCS Plus may have little or no effect on symptom severity at 10 week follow‐up (low certaintyc,d). Yount 2014 (N = 253) reported that ATCS Plus may have little or no effect on symptom burden at 12 weeks (low certaintyc,e). |
|
Clinical outcomes: symptom severity, 10 weeks IVR versus nurse delivered calls |
Results suggest that IVR may have little or no effect on symptom severity. | 437 (1 study) |
⊕⊕⊝⊝ Lowc,f | — |
|
Clinical outcomes: pain Multimodal/complex interventiong versus usual care |
Results indicate that multimodal intervention probably reduces pain at 3 months and probably slightly reduces pain at 12 months. | 405 (1 study) |
⊕⊕⊕⊝ Moderatec | — |
|
Clinical outcomes: depression Multimodal/complex interventiong versus usual care |
Results indicate that multimodal intervention probably slightly reduces depression at 3 and 12 months. | 405 (1 study) |
⊕⊕⊕⊝ Moderatec | — |
|
Clinical outcomes:distress, 6 weeks ATCS Plus versus usual care (via IVR) |
Results indicate that ATCS Plus probably has little or no effect on distress. | 250 (1 study) |
⊕⊕⊕⊝ Moderatec | — |
|
Behavioural outcome: medication adherence ATCS Plus versus usual care |
Results indicate that ATCS Plus may have little or no effect on medication non‐adherence. | 119 (1 study) |
⊕⊕⊝⊝ Lowc,d | — |
|
Adverse outcome: unintended adverse events attributable to the intervention Multimodal/complex intervention, ATCS Plus, IVR versus various controls |
No studies reported adverse events. | |||
| ATCS: automated telephone communication systems; ATCS Plus: automated telephone communication systems with additional functions; IVR: interactive voice response. | ||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||
aThe findings presented in this table are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bDowngraded as allocation concealment was rated as being at unclear risk of bias (−1). cDowngraded as results were obtained from a single study at potential risk of bias (−1). dDowngraded as randomisation and allocation concealment were rated as being at unclear risk of bias, and selective reporting rated as high risk (−1). eDowngraded as randomisation and allocation concealment were rated as being at unclear risk of bias, and performance bias was rated as being at high risk (−1). fDowngraded as allocation concealment was rated as being at unclear risk of bias, along with several other items (−1). gMultimodal/complex intervention included ATCS plus symptom monitoring by a nurse and medications.
Summary of findings 9. Long‐term management: effects of ATCS in the management of diabetes mellitus.
| ATCS versus usual care for managing diabetes mellitus | ||||||
|
Patient or population: patients with diabetes mellitus
Settings: various settings
Intervention: ATCS (ATCS Plus, IVR) Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Commentsa | |
| Assumed risk | Corresponding risk | |||||
| Usual care | ATCS | |||||
|
Clinical outcome: glycated haemoglobin or blood glucose ATCS Plus, IVR versus usual care at median follow‐up of 6 months |
The mean glycated haemoglobin in the control groups was 8.41% | The mean glycated haemoglobin in the intervention groups was 0.26% lower (0.50 to 0.01 lower) | Not estimable | 1216 (7 studies) | ⊕⊕⊝⊝ Lowb | ATCS Plus versus usual care 1 further study, Katalenich 2015 (N = 98), found that ATCS Plus may have little or no effect on median glycated haemoglobin levels compared with usual care at 6 months follow‐up (low certaintyc). IVR versus usual care 1 additional study, Homko 2012 (N = 80), found that IVR may have little or no effect on fasting blood glucose levels in pregnancy or infant birth weight at 26 months (low certaintyc). |
|
Behavioural outcome: self‐monitoring of diabetic foot (various scales) ATCS Plus versus usual care at 12 months follow‐up |
The mean self‐monitoring of diabetic foot in the control groups was 4.5 (range from 0 to 7, with higher scores indicating better foot care) | The mean self‐monitoring of diabetic foot in the intervention groups was 0.40 points higherd (0.10 to 0.71 points higher) | Not estimable | 498 (2 studies) | ⊕⊕⊕⊝ Moderatee | — |
|
Behavioural outcome: self‐monitoring of blood glucose ATCS Plus, IVR versus usual care, 6‐12 months |
See comment | See comment | Not estimable | See comment | See comment | ATCS Plus versus usual care Lorig 2008 (N = 417) found that ATCS Plus may have little no effect on self‐monitoring of blood glucose at 6 months (low certainty evidencef). At 12 months, 2 studies (Piette 2001 (N = 272); Schillinger 2009 (N = 339)) reported that ATCS Plus probably slightly improves self‐monitoring of blood glucose (moderate certaintye). IVR versus usual care Graziano 2009 (N = 112) found that IVR probably slightly increases the mean change in frequency of self‐monitoring of blood glucose (moderate certainty evidenceg). |
|
Behavioural outcome: medication adherence or use ATCS Plus versus usual care, 6‐12 months |
See comment | See comment | Not estimable | 370 (2 studies) |
See comment | Katalenich 2015 (N = 98) reported that ATCS Plus may have little or no effect on adherence rates at 6 months (low certaintyc), and Piette 2001 (N = 272) found that ATCS Plus has probably little or no effect on medication use at 12 months (moderate certaintyg. |
|
Behavioural outcome: physical activity, diet, weight monitoring ATCS Plus versus usual care, 6‐12 months |
See comment | See comment | Not estimable | 1028 (3 studies) |
See comment |
Lorig 2008 (N = 417) found that ATCS Plus may have little or no effect on aerobic exercise at 6 months (low certaintyf). Schillinger 2009 (N = 339) found that ATCS Plus may slightly improve diet and exercise and moderate intensity physical activity levels, but it may have little or no effect on vigorous intensity physical activity levels at 12 months (low certaintyc). Piette 2001 (N = 272) reported that ATCS Plus probably has little or no effect on weight monitoring (moderate certaintyg). |
|
Adverse outcome: unintended adverse events attributable to the intervention ATCS Plus, IVR versus usual care |
No studies were found that reported adverse events. | |||||
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ATCS Plus: automated telephone communication systems with additional functions; CI: confidence interval; HRQoL: health‐related quality of life; IVR: interactive voice response; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aAdditional results are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bDowngraded as allocation concealment was rated as being at unclear risk in four studies and attrition bias was rated as being at high risk in two studies (−1), and there was a moderate level of heterogeneity in the results (−1). cDowngraded as allocation concealment was rated as being at unclear risk (−1), and results were based on a single small study at some potential risk of bias (−1). dAn SD of 1.7 (on a 7‐point Likert scale, where higher score means better behavioural outcome) was chosen from a representative study by Schillinger 2009, and this was used to convert the SMD to a familiar scale. 0.24 (SMD) x 1.7 (SD) = 0.40 points higher (on a 7 point scale). eTwo studies assessed together (Piette 2001; Schillinger 2009): downgraded as allocation concealment was rated as being at unclear risk in one study and performance bias was rated as being high risk in one study (−1). fDowngraded as all items were rated as being at unclear risk, except attrition bias which was rated as being at high risk of bias (−1), and results were based on a single study at some risk of bias (−1). gDowngraded as results were based on a single study (−1).
Summary of findings 10. Long‐term management: effects of ATCS in patients with heart failure.
| ATCS versus usual care for patients with heart failure | ||||||
|
Patient or population: patients with heart failure
Settings: various settings
Intervention: ATCS (multimodal/complex intervention, ATCS Plus, IVR) Comparison: usual care or usual community care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Commentsa | |
| Assumed risk | Corresponding risk | |||||
| Usual care or usual community care | ATCS | |||||
|
Clinical outcome: cardiac mortality ATCS Plus, IVR versus usual care or usual community care at median follow‐up of 11.5 months |
Study populationb | RR 0.60 (0.21 to 1.67) | 215 (2 studies) | ⊕⊝⊝⊝ Very lowd,e | — | |
| 95 per 1000 | 57 per 1000 (20 to 158) | |||||
| Moderatec | ||||||
| 96 per 1000 | 58 per 1000 (20 to 160) | |||||
|
Clinical outcome: all‐cause mortality ATCS Plus versus usual care or usual community care at median follow‐up of 11 months |
Study populationb |
RR 1 (0.79 to 1.28) |
2165 (3 studies) | ⊕⊕⊕⊝ Moderatef | — | |
| 106 per 1000 | 106 per 1000 (84 to 136) | |||||
| Moderatec | ||||||
| 106 per 1000 | 106 per 1000 (84 to 136) | |||||
|
Clinical outcome: heart failure hospitalisation ATCS Plus, IVR versus usual care or usual community care at median follow‐up of 11.5 months |
See comment | See comment | Not estimable | 2329 (4 studies) |
See comment | ATCS Plus versus usual care or usual community care Chaudhry 2010 (N = 1653) found that the intervention had little or no effect on hospitalisation for heart failure (high certainty). Krum 2013 (N = 405) also reported that there was probably little or no effect of the intervention for this same outcome (moderate certaintyg), while Capomolla 2004 (N = 133) reported that ATCS Plus may decrease hospitalisation rates for heart failure (low certaintyh). IVR versus usual care Kurtz 2011 (N = 138) reported that IVR intervention has uncertain effects on hospitalisation for heart failure (very low certaintyi). |
|
Clinical outcome: all‐cause hospitalisation ATCS Plus versus usual care or usual community care |
See comment | See comment | Not estimable | 2191 participants (3 studies) |
See comment | ATCS Plus versus usual care Capomolla 2004 (N = 133) found that ATCS Plus may reduce all‐cause hospitalisation (for chronic heart failure, cardiac cause and other cause; low certaintyh), and Krum 2013 (N = 405) similarly reported that the intervention probably slightly decreased all‐cause hospitalisation (moderate certaintyg).fChaudhry 2010 (N = 1653) found that ATCS Plus has little or no effect on readmission for any reason (high certainty). |
|
Clinical outcome: global health (well‐being) rating (7‐item questionnaire) ATCS Plus versus usual care 12 months |
See comment | See comment | Not estimable | 405 participants (1 study) |
⊕⊕⊕⊝ Moderateg | Krum 2013 (N = 405) reported that ATCS Plus probably increases slightly the proportion of patients with improved global health questionnaire ratings at 12 months. |
|
Clinical outcome: emergency room and other health service use outcomes ATCS Plus versus usual care or usual community care |
See comment | See comment | Not estimable | 1786 participants (2 studies) |
See comment | Emergency room use Capomolla 2004 (N = 133) found that ATCS Plus may reduce emergency room use at (median) 11 months (low certaintyh). Other service use Chaudhry 2010 (N = 1653) found that ATCS Plus had little or no effect on number of days in hospital or number of hospitalisations (readmissions)(high certainty). |
|
Adverse outcome: unintended adverse events attributable to the intervention ATCS Plus, IVR versus usual care |
See comment | See comment | See comment | 1791 (2 studies) |
See comment | ATCS Plus versus usual care Chaudhry 2010 (N = 1653) reported that no adverse events had occurred during the study (high certainty). IVR versus usual care Kurtz 2011 (N = 138) classified adverse events as cardiac mortality plus rehospitalisation for heart failure, reporting uncertain effects upon this composite outcome (very low certaintyi). |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ATCS Plus: automated telephone communication systems with additional functions; CI: confidence interval; CI: confidence interval; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aAdditional results are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bThe assumed risk represents the mean control group risk across studies (calculated by GRADEPro). cThe assumed risk represents the median control group risk across studies (calculated by GRADEPro). dDowngraded as selection bias was rated as being at high risk in one study and allocation concealment was rated as being at unclear risk in both (−1). eDowngraded as the total number of events is less than 300 (−1), and wide CIs around the effect estimate included both a substantial potential benefit and a substantial potential harm (−1). fDowngraded as risk of bias was unclear on randomisation in one study and allocation concealment in two studies (Capomolla 2004; Krum 2013) (−1). gDowngraded as result is based on a single study (−1). hDowngraded as randomisation and allocation concealment judged as being at unclear risk of bias (−1); downgraded as results are based on a single study (−1). iDowngraded as randomisation judged as being at high risk and unclear on allocation concealment and other items (‐2); downgraded as result is based on a single study (−1).
Summary of findings 11. Long‐term management: effects of ATCS in the management of hypertension.
| ATCS versus usual care for management of hypertension | |||||
|
Patient or population: patients with hypertension
Settings: various settings
Intervention: ATCS (multimodal/complex intervention, ATCS Plus, IVR, unidirectional) Comparison: usual care, with and without education | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (comparisons) | Quality of the evidence (GRADE) | Commentsa | |
| Assumed risk | Corresponding risk | ||||
| Usual care | ATCS | ||||
|
Clinical outcome: systolic blood pressure (automated sphygmomanometer or electronic pressure monitor) ATCS Plus or IVR versus usual care at median follow‐up of 6 weeks |
The mean systolic blood pressure in the control group was 141.1 mmHg | The mean systolic blood pressure in the intervention groups was
1.89 mmHg lower (2.12 to 1.66 lower) |
65,256 (3 studies) | ⊕⊕⊕⊝ Moderateb | 1 additional study (Dedier 2014) (N = 253) reported that compared with usual care plus education, IVR may have little or no effect on systolic blood pressure at 3 months (low certaintyc). |
|
Clinical outcome: diastolic blood pressure (automated sphygmomanometer and electronic cuff) ATCS Plus, unidirectional versus usual care at median follow‐up of 14 weeks |
The mean diastolic blood pressure in the control group was 81.2 mmHg | The mean diastolic blood pressure in the intervention groups was 0.02 mmHg higher (2.62 lower to 2.66 higher) |
65,056 (2 studies) | ⊕⊕⊝⊝ Lowd,e | — |
|
Clinical outcome: blood pressure control, 26 weeks Multimodal/complex interventionf versus usual care |
See comment | See comment | 166 (1 study) |
⊕⊕⊕⊝ Moderateg | Bove 2013 (N = 241) found that a multimodal/complex intervention probably has little or no effect on blood pressure control. |
|
Clinical outcome: Health statush, depressioni, 6 weeks ATCS Plus versus enhanced usual care (plus information) |
See comment | See comment | 200 (1 study) |
⊕⊕⊝⊝ Lowj | Piette 2012 (N = 200) found that ATCS Plus may slightly improve health status and may decrease depressive symptoms. |
|
Behavioural outcome: medication use Multimodal/complexk, ATCS Plus versus usual care or enhanced usual care (plus information) |
See comment | See comment | 483 (2 studies) |
⊕⊕⊝⊝ Low | Multimodal/complex versus usual care Magid 2011 (N = 283) found that multimodal/complex intervention may have little or no effect on medication adherence assessed by Medication Possession Ratio or proportion adherent (low certaintyl). ATCS Plus versus enhanced usual care Piette 2012 (N = 200) found that ATCS Plus may reduce the number of medication‐related problemsm (low certaintyj). |
|
Behavioural outcome: physical activity levels, 12 weeks IVR versus enhanced usual care |
See comment | See comment | 253 (1 study) |
⊕⊕⊝⊝ Lowc | IVR versus enhanced usual care Dedier 2014 (N = 253) reported that IVR may slightly increase physical activity levels. |
|
Adverse outcome: unintended adverse events attributable to the intervention Multimodal/complex intervention, ATCS Plus, IVR, unidirectional ATCS versus various controls |
No studies reported adverse events. | ||||
| ATCS Plus: automated telephone communication systems with additional functions; CI: confidence interval; IVR: interactive voice response; MD: mean difference; SD: standard deviation. | |||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | |||||
aAdditional results are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bDowngraded as risk of bias for randomisation was rated unclear in one study, allocation concealment was rated as at unclear risk in two studies, and in one study each, performance bias and other bias (baseline imbalances in blood pressure) were rated as being at high risk (−1). cDowngraded as all domains were judged to be at unclear risk of bias (−1), and results were based on a single small study at some potential risk of bias (−1). dDowngraded due to unclear risk of bias for allocation concealment in one study, and high risk for other bias (baseline imbalances in blood pressure) in one study (−1). eDowngraded as a substantial amount of heterogeneity was detected and effects were in opposite directions (−1). fMultimodal/complex intervention included ATCS Plus plus sphygmanometer, a weighting scale, pedometer and instructions on their use. gDowngraded as results were based on a single small study at some potential risk of bias (−1). hHealth status was self‐reported perceived general health status, assessed on a 5‐point scale (where 1 = poor, 2 = fair, 3 = good, 4 = very good, and 5 = excellent). iDepression assessed using the 10‐item Center for Epidemiological Studies‐Depression Scale. jDowngraded as risk of bias was rated as unclear for allocation concealment and most other domains, with a high risk of performance bias (−1); and results were based on a single small study at some potential risk of bias (−1). kMultimodal/complex intervention included ATCS Plus plus patient education, home blood pressure monitoring, and clinical pharmacist management of hypertension with physician oversight. lDowngraded due to high risk of bias for other bias (baseline imbalances in blood pressure) (−1); results were based on a single small study at some potential risk of bias (−1). mMedication‐related problems assessed using a 7‐item scale (yes/no responses) on barriers to medication taking, including cost, side effects, complexity of regimen, worries over taking medicines and/or over long‐term effects of medication.
Summary of findings 12. Long‐term management: effects of ATCS on smoking cessation.
| ATCS versus control for smoking cessation | ||||||
|
Patient or population: patients with tobacco dependence
Settings: various settings
Intervention: ATCS (multimodal/complex intervention, ATCS Plus, IVR) Comparison: usual care, control (no calls, 'placebo' (inactive) ATCS, self‐help intervention, stage‐matched manuals) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Commentsa | |
| Assumed risk | Corresponding risk | |||||
| Control | ATCS | |||||
|
Behavioural outcome: smoking abstinence Multimodal/complex intervention, ATCS Plus, IVR versus (various) controls or usual care at median follow‐up of 12 months |
Study populationb | RR 1.2 (0.98 to 1.46) | 2915 (7 studies) | ⊕⊕⊝⊝ Lowd,e | ATCS Plus versus usual care 1 further study, Reid 2011 (N = 440), reported that ATCS Plus may improve smoking abstinence rates at 26 weeks, and this may be maintained at 52 weeks (low certainty evidencef). |
|
| 201 per 1000 | 241 per 1000 (197 to 293) | |||||
| Moderatec | ||||||
| 241 per 1000 | 289 per 1000 (236 to 352) | |||||
|
Behavioural outcome: medication use Multimodal/complex, ATCS Plus versus control (inactive IVR or self‐help booklet) |
See comment | See comment | See comment | 1127 (2 studies) |
⊕⊕⊕⊝ Moderateg |
Multimodal/complex intervention versus control (self‐help booklet) Brendryen 2008 (N = 396) found that a multimodal/complex intervention probably has little or no effect on adherence to NRT (moderate certainty evidence). ATCS Plus versus control (inactive IVR) Regan 2011 (N = 731) found that ATCS Plus probably has little or no effect on medication use (moderate certainty evidence). |
|
Behavioural outcome: support programme enrolment ATCS Plus versus control (inactive IVR) |
See comment | See comment | See comment | 521 (1 study) |
⊕⊕⊝⊝ Lowh | Carlini 2012 found that ATCS Plus may improve re‐enrolment into a quit line support programme. |
|
Adverse outcome: unintended adverse events attributable to the intervention Multimodal/complex intervention, ATCS Plus, IVR versus various controls |
No studies were found that reported adverse events. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ATCS Plus: automated telephone communication systems with additional functions; CI: confidence interval; IVR: interactive voice response; NRT: nicotine replacement therapy; OR: odds ratio; RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aAdditional results are based on a narrative summary and synthesis of results that were not amenable to statistical analysis; please see Effects of interventions for detailed findings. bThe assumed risk represents the mean control group risk across studies (calculated by GRADEPro). cThe assumed risk represents the median control group risk across studies (calculated by GRADEPro). d Downgraded due to unclear risk of bias for allocation concealment in four studies and high risk of attrition bias in one study (−1). eDowngraded for inconsistency, as two studies by Ershoff 1999 and McNaughton 2013 showed contradictory results favouring the control group and heterogeneity was moderate overall (−1). fDowngraded as all items were judged to be at an unclear risk of bias (−1), and results were based on a single study at some risk of bias (−1). gDowngraded as results (for each outcome) were based on a single study (−1). hDowngraded as most items were judged to be at unclear risk of bias (−1), and results were based on a single study at some risk of bias (−1).
Table 13 presents additional information about the effects of ATCS interventions for both continuous and dichotomous outcomes for each study. Table 17 summarises the effectiveness of ATCS by specific categories and subcategories used to organise the review along with the effect estimates and selected median effect estimates.
ATCS for preventive healthcare
Alcohol misuse
Tucker 2012 evaluated an ATCS intervention versus control for preventing alcohol misuse.
Primary outcomes: behavioural outcomes
The IVR intervention may have little or no effect on drinking practices or spending on alcohol compared with control (assessment‐only) group (P > 0.20; low certainty evidence).
Immunisations
Ten studies evaluated ATCS compared with no calls, letters, usual care or health information for promoting immunisations (Dini 2000; Franzini 2000; Hess 2013; LeBaron 2004; Lieu 1998; Linkins 1994; Nassar 2014; Stehr‐Green 1993; Szilagyi 2006; Szilagyi 2013). For a summary of the effects of these comparisons on immunisation uptake, see Table 1. We considered studies by separate population groups (children, adolescents, adults) as there was otherwise a high degree of heterogeneity in a pooled effect estimate.
Primary outcomes: behavioural outcomes
Immunisation rate
Children: ATCS versus control
Meta‐analysis of five studies considered to be sufficiently homogeneous found that ATCS (ATCS Plus, IVR, unidirectional) probably increased the uptake of immunisations in children compared with controls (no calls, letter, or usual care) (RR 1.25, 95% CI 1.18 to 1.32; moderate certainty evidence; Analysis 1.1; Dini 2000; LeBaron 2004; Lieu 1998; Linkins 1994; Stehr‐Green 1993). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 1.99, df = 4 (P = 0.74); I2 = 0%).
1.1. Analysis.
Comparison 1 ATCS vs control for improving health services uptake (immunisations), Outcome 1 Immunisation in children.
We could not include Franzini 2000 in the meta‐analysis, as it used a cluster RCT design and did not report sufficient information to allow for statistical pooling (i.e. regarding cluster size and within‐cluster or between‐cluster variance). Franzini 2000 reported that compared with controls (no calls), unidirectional ATCS (Autodialer) may increase immunisation rates in children (270/314 (86%) intervention group versus 273/429 (64%) control group, low certainty evidence).
Adolescents: unidirectional ATCS versus usual care
Meta‐analysis of two studies considered to be sufficiently homogeneous found that unidirectional ATCS, compared with usual care, probably slightly increased immunisation status of adolescents (RR 1.06, 95% CI 1.02 to 1.11; moderate certainty evidence; Analysis 1.2; Szilagyi 2006; Szilagyi 2013). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 0.28, df = 1 (P = 0.60); I2 = 0%). Szilagyi 2013 also reported that compared with usual care, unidirectional ATCS probably improved slightly the uptake of preventive care visits (63% ATCS versus 59% usual care; HR = 1.1, 95% CI 1.0 to 1.2; P < 0.05; moderate certainty evidence).
1.2. Analysis.
Comparison 1 ATCS vs control for improving health services uptake (immunisations), Outcome 2 Immunisation in adolescents.
Adults: unidirectional ATCS versus no calls or health information
Two studies contributed data to this comparison and were considered sufficiently homogeneous to warrant meta‐analysis (Hess 2013; Nassar 2014). Hess 2013 used a cluster design but did not adjust for clustering; to calculate effective sample size, we used the Fleiss‐Cuzick estimator (see Appendix 14 for calculations). Meta‐analysis of the two studies found that the effects of unidirectional ATCS, compared with no calls in Hess 2013 or health information in Nassar 2014 were uncertain for immunisations in adults (RR 2.18, 95% CI 0.53 to 9.02; very low certainty evidence; Analysis 1.3). There was a substantial level of heterogeneity in the pooled studies (Tau2 = 0.68; Chi2 = 2.71, df = 1 (P = 0.10); I2 = 63%).
1.3. Analysis.
Comparison 1 ATCS vs control for improving health services uptake (immunisations), Outcome 3 Immunisation in adults.
Secondary outcomes
Process outcomes: satisfaction/acceptability of ATCS
Children
Over 85% of the participants in Dini 2000 responded positively about the acceptability of unidirectional ATCS. Lieu 1998 found ATCS (IVR) to be an acceptable medium to deliver immunisation‐related reminders, with over 91% of the participants who received the intervention finding it very easy or somewhat easy to understand. Neither study reported comparison group data.
Adolescents
For 388 (27%) households in the unidirectional ATCS group, the reminder call was unanswered or was picked up by voice mail, but authors reported no comparison group data (Szilagyi 2013).
Adults
Nassar 2014 reported that the unidirectional ATCS intervention may lead to a slight increase in participants reporting that they learnt about the H1N1 virus (66.6% of participants), compared with 63.6% in the health information group (P = 0.41; low certainty).
Process outcomes: cost‐effectiveness
Children
In Dini 2000, unidirectional ATCS was more cost‐effective than phone plus letters (USD 4300 vs USD 4738) but less cost‐effective than letters only (USD 2254) (no data available for the no‐calls comparison group). Franzini 2000 reported that the average cost per child in the Autodialer was USD 15.46 compared with USD 11.46 in the controls (no calls); the incremental physician's office cost per child immunised relative to control was USD 4.06 (low certainty). In Lieu 1998, the estimated cost per child immunised was USD 9.80 using automated telephone messages alone, compared with USD 10.50 for letters alone.
Adolescents
Szilagyi 2013 reported that the total cost of the unidirectional ATCS intervention (excluding research costs) was USD 23,738.00, but authors did not report cost data for the usual care comparison group. Of all adolescents receiving a telephone reminder, the average cost was USD 16.68 per adolescent per year.
Physical activity
Eight studies evaluated various types of ATCS for improving physical activity levels, comparing them to no‐coach IVR call, no calls, usual care, usual care plus MOVE programme, attention only, or an IVR call promoting healthy eating (David 2012; Dubbert 2002; Jarvis 1997; King 2007; Morey 2009; Morey 2012; Pinto 2002; Sparrow 2011). For this outcome, the studies were too heterogeneous for statistical pooling. For a summary of the effects of these comparisons on physical activity and related outcomes, see Table 2.
Primary outcomes: behavioural outcomes
Various indices of physical activity
Multimodal/complex intervention versus no intervention
Dubbert 2002 found that the intervention (10 nurse delivered calls plus 10 automated phone calls) may have improved slightly the frequency of walks compared with no calls during initiation (P = 0.003) and maintenance (P = 0.004) phases (low certainty evidence).
Multimodal/complex intervention versus usual care
Morey 2009 reported that the intervention (a combination of counselling by a lifestyle counsellor, automated telephone messaging, endorsement and tailored mailings) had probably little or no effect on usual gait speed or functional/disability outcomes, but probably improved slightly rapid gait speed (P = 0.04) and minutes of moderate/vigorous physical activity per week, compared with usual care at 12 months (mean (SD) = 126.6 min/week (142.9) versus 69.6 min/week (116.1); P < 0.001; moderate certainty evidence). Similarly, Morey 2012 reported that the multimodal intervention may slightly increase endurance physical activity at 12 months (mean (SD) = 133.60 min/week (136.47) versus 112.62 min/week (135.45); P < 0.001; low certainty evidence).
Together, these results suggest that multimodal/complex interventions may have little effect on several indices of physical activity, compared with usual care or no intervention.
ATCS Plus versus control (IVR)
David 2012 found that the ATCS Plus intervention may have little or no effect on time to complete the one‐mile walk compared with (no‐coach IVR call) controls. Similarly, Pinto 2002 found that compared with IVR control group, the intervention may have improved slightly the proportion of participants meeting recommendations for moderate‐intensity or vigorous‐intensity physical activity (P = 0.04), energy expenditure (P = 0.02), and motivational readiness (P = 0.04) at three months, but may have little or no effect on these outcomes at six months. In both studies the level of certainty for the evidence was low.
Together, these results suggest that ATCS Plus interventions may have little effect on several indices of physical activity, compared with IVR controls.
IVR versus usual care or attention or general health education (via IVR)
Jarvis 1997 found that the intervention may have little or no effect on physical activity levels (minutes walked per week) compared with usual care at three months (low certainty evidence). King 2007 reported that compared with attention control, the intervention may increase slightly minutes of moderate to vigorous physical activity at 6 and 12 months (P = 0.01, P = 0.045), but it may have little or no effect on this outcome at 18 months (P = 0.10; low certainty evidence). Sparrow 2011 found that compared with weekly general health education (via IVR) controls, the intervention may have improved slightly muscle strength (P = 0.035), balance (P = 0.029), and reduce depressive symptoms (P = 0.030), but may have little or no effect on walking distance (P = 0.91; low certainty evidence).
Taken together, these results suggest that IVR interventions may slightly improve several indices of physical activity, but the quality of evidence is low, and results are mixed across different measures of physical activity.
Overall, the results suggest that less complex ATCS interventions (i.e. IVR interventions) may be slightly more likely to improve outcomes related to exercise than more complex interventions (ATCS Plus or multimodal interventions) when compared with usual care or various controls. However, these interventions were not directly tested against one another.
Primary outcomes: clinical outcomes
Body mass index (BMI), anthropometric measures, metabolic markers
Multimodal/complex intervention versus usual care
Morey 2012 reported that there may be little or no differences between the multimodal intervention (similar to Morey 2009, a combination of counselling by a lifestyle counsellor, automated telephone messaging, endorsement and tailored mailings) and usual care in terms of fasting insulin and glucose levels, glycated haemoglobin (mean (SD) = 5.90% (0.44) versus 5.93% (0.36); P = 0.08); BMI (mean (SD) = 30.74 kg/m2 (3.88) versus 30.64 kg/m2 (3.62); P = 0.31); waist circumference (mean (SD) = 103.92 cm (10.02) versus 104.43 cm (11.73); P = 0.68); or physical function (mean (SD) = 62.52 (21.79) versus 66.24 (20.91); P = 0.09; low certainty evidence).
ATCS Plus versus control
David 2012 found that the ATCS Plus intervention may have little or no effect on BMI, weight (kg), waist (cm) or waist‐hip ratio, compared with (no‐coach IVR call) controls (low certainty evidence).
Together, these results suggest that ATCS Plus and multimodal/complex interventions may have little effect on measures of body weight or metabolic markers, compared with usual care or control.
Secondary outcomes
Cognitive outcomes: self‐efficacy
David 2012 found that the ATCS Plus intervention may have little or no effect on self‐efficacy for walking compared with no‐coach IVR call controls (low certainty evidence).
Process outcomes: satisfaction with ATCS
In Jarvis 1997, users were very satisfied with the IVR system. Analysis of users' satisfaction data shows a high user satisfaction score for Telephone‐Linked Communication for Activity Counseling and Tracking (IVR), with the mean of 8.6 points (where 1 = very dissatisfied and 10 = very satisfied); 74% of the women rated their satisfaction with the intervention as 10 of 10. Intervention users' perceived benefit score was 7.5 of 10; 63% of the women rated the benefit of TLC as 10 of 10. However, for satisfaction and perceived benefit outcomes, authors reported no data for the usual care comparison group.
Patient‐centred outcomes: quality of life
In Dubbert 2002 the multimodal intervention may have had little or no effect on physical or mental health quality of life as measured by the Short Form‐36 Health Survey (SF‐36) summary scores, compared with no intervention (low certainty evidence). King 2007 reported that the intervention may have little or no effect on physical functioning and well‐being at 12‐months, compared with attention control (IVR group: vitality plus scale (range from 10 (negative) to 50 (positive) adjusted mean square = 35.9 points (SD 6.3) versus attention control: 34.8 points (SD 5.8); IVR group: satisfaction with fitness scale (20 items) adjusted mean square = 32.8 points (SD 12.1) versus control: 30.0 points (SD 11.9); low certainty evidence). Morey 2012 reported there may be little or no differences between the multimodal intervention and usual care in terms of health‐related quality of life at 12 months (mean (SD) = 58.12 points (42.29) versus 61.68 points (41.82); P = 0.92; scale from 0 to 100, with higher scores indicating better outcome; low certainty evidence).
Screening
Thirteen trials compared ATCS intervention to no intervention, usual care or usual community care for changing screening rates (Baker 2014; Cohen‐Cline 2014; Corkrey 2005; DeFrank 2009; Durant 2014; Fiscella 2011; Fortuna 2014; Hendren 2014; Heyworth 2014; Mosen 2010; Phillips 2015; Simon 2010a; Solomon 2007). For a summary of the effects of these comparisons on screening rates for different conditions, see Table 3.
Primary outcomes: clinical outcomes
Breast cancer screening
Multimodal/complex intervention versus usual care
Fiscella 2011 and Hendren 2014 compared the effects of usual care with those of multimodal/complex interventions, which included combinations of multiple ATCS calls, patient outreach (letters), and prompts for patients and clinicians, on screening rates for breast cancer at 12 months.
Meta‐analysis of these two studies, considered to be sufficiently homogeneous, found that the multimodal/complex intervention increased breast cancer screening rates compared with usual care (RR 2.17, 95% CI 1.55 to 3.04; high certainty evidence; Analysis 2.1). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 0.79, df = 1 (P = 0.37); I2 = 0%).
2.1. Analysis.
Comparison 2 ATCS vs control for improving health services uptake (screening rates), Outcome 1 Breast cancer screening.
IVR versus enhanced usual care (letter or reminder)
Meta‐analysis of two studies considered to be sufficiently homogeneous found that compared with enhanced usual care (letter or reminder, IVR has probably little or no effect on breast cancer screening (RR 1.05, 95% CI 0.99 to 1.11; moderate certainty evidence; Analysis 2.1; DeFrank 2009; Phillips 2015). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 0.26, df = 1 (P = 0.61); I2 = 0%).
Unidirectional ATCS (plus letter) versus letter alone
Fortuna 2014 found that compared with letter alone, unidirectional ATCS (plus letter) probably has little or no effect on breast cancer screening rates at 12 months (22.8% versus 17.8%; adjusted OR 1.3, 95% CI 0.7 to 2.4; moderate certainty evidence).
Overall, these results suggest that more complex ATCS interventions (i.e. multimodal interventions) may be more likely to improve outcomes related to breast cancer screening than less complex interventions (IVR or unidirectional ATCS), when compared with usual care or control. However, these interventions were not directly tested against one another.
Colorectal cancer screening
Multimodal/complex intervention versus usual care
Baker 2014, Fiscella 2011, and Hendren 2014 compared usual care versus multimodal/complex interventions, which included combinations of ATCS calls, letters, prompts for patients and clinicians, and provision of testing (colorectal cancer kits), on colorectal cancer screening rates.
Meta‐analysis of these three studies, considered to be sufficiently homogeneous, found that multimodal/complex interventions increased colorectal cancer screening rates (RR 2.19, 95% CI 1.88 to 2.55; high certainty evidence; Analysis 2.2). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 1.29, df = 2 (P = 0.52); I2 = 0%).
2.2. Analysis.
Comparison 2 ATCS vs control for improving health services uptake (screening rates), Outcome 2 Colorectal cancer screening.
IVR versus control (no call)
Durant 2014 compared IVR with control, reporting that IVR probably increased colorectal cancer screening, with 1773 participants from the IVR group and 100 from the no calls control group completing colorectal cancer screening within three months (without segmentation) (moderate certainty evidence).
IVR versus usual care or enhanced usual care (letter)
Meta‐analysis of two studies considered to be sufficiently homogeneous found that compared with usual care, IVR probably increased colorectal cancer screening at six months (RR 1.36, 95% CI 1.25 to 1.48; moderate certainty evidence; Analysis 2.2; Cohen‐Cline 2014; Mosen 2010). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 1.01, df = 1 (P = 0.31); I2 = 1%). Mosen 2010 also reported that compared with usual care, IVR probably increased completion of any colorectal cancer screening (23.9% versus 17.6%; moderate certainty evidence).
Two other studies evaluating this comparison reported results at later time points (Phillips 2015; Simon 2010a).
Meta‐analysis of these two studies, considered to be sufficiently homogeneous, found that IVR had probably little or no effect on colorectal cancer screening rates, compared with usual care or letters only at longer follow‐up (9 to 12 months) (RR 1.01, 95% CI 0.97 to 1.05; moderate certainty evidence; Analysis 2.2). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 0.47, df = 1 (P = 0.49); I2 = 0%). Simon 2010a also reported that IVR probably improved slightly colorectal cancer screening: a total of 21.4% of participants in the IVR group and 20.3% in the usual care group underwent colonoscopy following the intervention (adjusted OR 1.08, 95% CI 1.00 to 1.16; P = 0.04; moderate certainty evidence). The trialists reported including screening via colonoscopy as a secondary outcome as they anticipated that the intervention may also increase rates of uptake due to increased public awareness that colonoscopy is the most sensitive and frequently recommended screening test (Simon 2010a).
Overall these results suggest that compared with usual care or letter, IVR interventions probably increase colorectal cancer screening rates at some time points (6 months), but probably have little or no effect on colorectal cancer screening rates at later time points (9 to 12 months).
Unidirectional ATCS versus letter
Fortuna 2014 found that compared with letter alone, unidirectional ATCS (plus letter) had probably little or no effect on colorectal cancer screening rates at 12 months (15.3% versus 12.2%; adjusted OR 1.2, 95% CI 0.6 to 2.4; moderate certainty evidence).
Overall, these results suggest that more complex ATCS interventions (i.e. multimodal interventions) may be slightly more likely to improve colorectal cancer screening rates than less complex interventions (IVR and unidirectional ATCS) when compared with usual care or letters alone. However, these interventions were not directly tested against one another.
Cervical cancer screening
ATCS Plus versus control (no call)
Corkrey 2005 compared an ATCS Plus intervention with control, reporting that the intervention probably improved slightly the cervical cancer screening rate at two months (increase by 0.43%; moderate certainty evidence).
Osteoporosis screening
Multimodal/complex intervention versus no intervention
Solomon 2007 found that a multimodal intervention (education and reminders delivered to primary care physicians, mailings and ATCS) may increase the uptake of bone mineral density test or filling a prescription for osteoporosis medication at 10 months, compared with no intervention (adjusted model: 14% versus 10%; RR 1.52, 95% CI 1.13 to 2.05; P = 0.006; low certainty evidence).
ATCS Plus versus usual care
Heyworth 2014 reported that the effects of the ATCS Plus intervention versus usual care for bone mineral density screening were uncertain (adjusted analyses 18.6% versus 24.6 %, P < 0.001; very low certainty evidence).
Overall, these results suggest that multimodal interventions increase breast cancer and colorectal cancer screening rates when compared with usual care, and when compared with control they may increase osteoporosis screening rates. An ATCS Plus intervention probably slightly improves the rate of cervical cancer screening compared with control; however, results are based on a single comparison. The effects of ATCS Plus interventions on osteoporosis screening rates are uncertain. Compared with control, usual care or enhanced usual care, IVR interventions probably improve colorectal cancer screening rates at earlier (six months) but not later time points, but they probably have little or no effect on breast cancer screening rates. Unidirectional ATCS interventions, compared with letter or control, probably have little or no effect on breast cancer or colorectal cancer screening rates.
Secondary outcomes
Process outcomes: cost‐effectiveness
ATCS versus controls
In Baker 2014, the estimated cost of the multimodal outreach intervention was USD 34.59 per patient, and the estimated cost per completed colorectal cancer screening test was USD 43.13; however, no cost‐effectiveness data were available for the usual care arm. In Corkrey 2005 the cost per additional screen for cervical cancer in the IVR group was AUD 388.23 (in a random sample of women who were aged 20 to 69 years, without a hysterectomy, and unscreened); authors provided no cost‐effectiveness data for the control group. Durant 2014 reported a communication cost per screening of USD 14.84; this was further calculated to 18,738 colorectal cancer prevention years, with a resultant communication cost of USD 1.56 per colorectal cancer prevention year. In Phillips 2015, the cost of mammography mailings was USD 2.36, and colorectal cancer letters (including faecal immunochemical test kits) cost USD 7.17 per patient per mailing, compared with USD 0.92 per patient receiving IVR alone.
Stress management
Primary outcomes: clinical outcomes
Carers' psychological outcomes
ATCS Plus versus usual care
Mahoney 2003 found that compared with usual care, ATCS Plus has probably little or no effect on caregivers' appraisal of the bothersome nature of care, depression, or state anxiety at 6, 12, and 18 months (moderate certainty evidence).
Substance use
Primary outcomes: clinical outcomes
Days of drug use
ATCS Plusversus versus motivational interviewing
Aharonovich 2012 found that compared with usual delivery of motivational interviewing, delivery via ATCS Plus delivered motivational interviewing probably had little or no effect on days of using primary drug over the previous 30 days at 30 and 60 days post‐treatment (Cohen's d = 0.62; moderate certainty evidence).
Weight management
Seven studies evaluated ATCS for facilitating weight management: five in adults and two in children (Bennett 2012; Bennett 2013; Estabrooks 2008; Estabrooks 2009;Goulis 2004; Vance 2011; Wright 2013). For a summary of the effects of these comparisons on weight management and related outcomes in adults and children, see Table 4.
Primary outcomes: clinical and behavioural outcomes in adults
BMI scores
ATCS (multimodal/complex intervention, ATCS Plus, IVR) versus usual care/no intervention
Five trials evaluated ATCS versus usual care or no intervention for weight management in adults (Bennett 2012; Bennett 2013; Estabrooks 2008; Goulis 2004; Vance 2011). Meta‐analysis of three trials considered to be sufficiently homogeneous showed that compared with usual care, ATCS interventions may have reduced slightly BMI in adults (MD −0.64 kg/m2, 95% CI −1.38 to 0.11; low certainty evidence; Analysis 3.1; Bennett 2012; Bennett 2013; Goulis 2004). There was a substantial level of heterogeneity among the studies (Tau2 = 0.25; Chi2 = 6.41, df = 2 (P = 0.04); I2 = 69%). Vance 2011 did not provide sufficient data to contribute to the meta‐analysis but reported that BMI in the intervention group (ATCS Plus plus written materials and group meetings) may have slightly been improved (mean reduction = 0.46 kg/m2; P < 0.001), compared with control (written materials and group meetings) (low certainty evidence). We did not include the remaining two trials in the meta‐analysis, as they reported weight loss rather than BMI (Estabrooks 2008, Vance 2011). The three studies pooled in meta‐analysis for BMI (Bennett 2012; Bennett 2013; Goulis 2004) also measured weight loss and other primary outcomes, reported below.
3.1. Analysis.
Comparison 3 ATCS vs control for reducing body weight, Outcome 1 BMI adults.
Weight loss
ATCS (multimodal/complex intervention, ATCS Plus, IVR) versus usual care/controls
Bennett 2012 found that compared with usual care (self‐help booklet), the ATCS Plus intervention probably reduced slightly body weight in adults at 18 months (MD −0.95 kg, 95% CI −2.03 to 0.14; moderate certainty evidence). Bennett 2013 found that compared with usual care, the multimodal/complex intervention may have reduced body weight in adults at 18 months (MD −1.7 kg, 95% CI −3.3 to −0.2; low certainty evidence).
Vance 2011 found that compared with written materials and monthly group meetings alone, the addition of ATCS Plus to these interventions may have reduced slightly body weight (for within‐group differences P < 0.001; mean reduction = 6.11 kg) and waist circumference (P < 0.001; mean reduction = 1.94 cm; low certainty evidence).
IVR versus usual care/control
Estabrooks 2008 found that compared with no calls, IVR may have had little or no effect on the percentage of lost body weight (mean (SD) 2.63% (3.08) versus 1.64% (1.78); P = 0.13) and on the change in body weight (mean (SD) 85.9 kg (18.6) versus 85.8 kg (18.2), P = 0.13) at three months (low certainty evidence). Goulis 2004 found that, compared with usual care, IVR probably reduced slightly body weight at six months (mean (SD) 89.2 kg (14.7) versus 99.6 kg (23.8); P = 0.05), but it probably had little or no effect on obesity assessment scores (mean (SD) 45.9 (19.6) versus 50.8 (16.5); moderate certainty evidence).
Blood pressure, glucose and cholesterol levels
ATCS (ATCS Plus, IVR) versus usual care
Bennett 2012 found that there was probably little or no difference between the ATCS Plus intervention and usual care (self‐help booklet) arms at 18 months in terms of systolic (MD −5.83 mmHg, 95% CI −10.38 to −1.28) or diastolic (MD −2.24 mmHg, 95% CI −5.16 to 0.69) blood pressure (moderate certainty evidence).
ATCS Plus versus control
Vance 2011 found that compared with a control group (written materials and group meetings), the intervention group (ATCS Plus plus written materials and group meetings) may have improved slightly their systolic blood pressure (P = 0.01; mean reduction = 2.97 mmHg) and blood glucose levels (P = 0.02; mean reduction = 3.02 mg/dL) at 12 weeks (low certainty evidence).
IVR versus usual care
Goulis 2004 found that, compared with usual care, IVR probably had little or no effect on systolic blood pressure (mean intervention group (SD) 123.8 mmHg (14.2) versus 128.6 mmHg (19.4) usual care); diastolic blood pressure (mean intervention group (SD) 74.6 mmHg (8.5) versus 79.5 mmHg (14.0) usual care); plasma glucose levels (mean intervention group (SD) 104.7 mg/dL (25.0) versus 108.3 mg/dL (31.3) usual care); or high‐density lipoprotein cholesterol (mean intervention group (SD) 47.5 mg/dL (12.0) versus 45.3 mg/dL (12.1) usual care), but it probably reduced slightly total cholesterol (mean intervention group (SD) 220.7 mg/dL (42.6) versus 239.6 mg/dL (41.5) usual care; P = 0.05); and triglyceride levels at six months (mean intervention group (SD) 122.3 mg/dL (31.4) versus 140.7 mg/dL (37.2) usual care; P = 0.01; moderate certainty evidence).
Medication adherence
ATCS Plus versus usual care
Bennett 2012 found that there was probably little or no difference between the ATCS Plus intervention and usual care (self‐help booklet) arms at 18 months in terms of medication adherence measured with the Hill‐Bone compliance to hypertension therapy scale (MD −0.31, 95% CI −0.86 to 0.25, P = 0.28; moderate certainty evidence).
Physical activity
IVR versus control
Estabrooks 2008 found that compared with no calls, IVR may have had little or no effect on daily minutes of moderate to vigorous physical activity (mean (SD) 25.15 min/d (29.82) versus 21.38 min/d (12.18), P = 0.47) or dietary habits (starting the conversation questionnaire scale (range from 7 (best) to 31 (worst)) at three months (mean 19.34 points (2.61) versus 20.13 points (2.84), P = 0.60; low certainty evidence).
Adverse outcomes
In Bennett 2012, there was one serious musculoskeletal injury reported in the intervention group and three events (one cardiovascular and two cases of gallbladder disease) in the usual care group. In Bennett 2013, there were six serious adverse events reported in participants in the multimodal ATCS intervention arm. These included gynaecological surgery in two participants and knee replacement, breast abscess, musculoskeletal injury, and cancer diagnosis in one participant each. All of these events required hospitalisation except for the cancer diagnosis. Authors of both studies reported that they could not determine whether the adverse events resulted from participation in the study.
Overall, these results suggest that ATCS (multimodal, ATCS Plus) interventions may slightly reduce BMI scores and body weight in adults, compared with usual care or control, while IVR interventions appear less effective. The effects of interventions on other clinical or behavioural measures appear mixed. It is not clear whether adverse events are associated with ATCS interventions or not.
Primary outcomes:clinical and behavioural outcomes in children
Weight management (BMI z‐scores)
Two trials that were too heterogeneous for pooling evaluated different ATCS interventions for facilitating weight management in children (Estabrooks 2009;NCT01953653).
ATCS Plus versus control
Estabrooks 2009 found that compared with Family Connections (education by a dietician in small groups) control group, ATCS Plus had probably little or no effect on BMI z‐scores (mean intervention (SD) 1.98 kg/m2 (0.03) versus control 1.95 kg/m2 (0.04)); moderate self‐reported physical activity (mean intervention (SD) 2.79 days/week (1.95) versus control 2.71 days/week (2.21)); sedentary behaviours (screen time) (mean intervention (SD) 5.47 h/d (1.96) versus control 5.60 h/d (2.04)); or dietary habits (sugary drinks) (mean intervention (SD) 1.80 L/week (1.64) versus control 1.76 L/week (1.85)) at 12 months (moderate certainty evidence).
IVR versus control
Wright 2013 found that compared with a wait‐list control, IVR probably had little or no effect on BMI z‐scores (mean intervention (SD) 1.9 kg/m2 (0.28) versus control 1.9 kg/m2 (0.3), P = 0.48)); total caloric intake (mean intervention (SD) 744.0 kcal (385.0) versus control 958 kcal (475.0); P = 0.06); fruit intake (mean intervention (SD) 1.1 cups/day (0.7) versus control 1.5 cups/day (1.1); P = 0.12)), and sedentary behaviours (television viewing time) (mean intervention (SD) 1.0 h/d (1.5) versus control 1.8 h/d (2.4); P = 0.22)) at three months (moderate certainty evidence).
Overall, these results suggest that ATCS interventions, compared with control, probably have little effect on weight management assessed by BMI z‐scores or other proxy measures of weight management in children.
Secondary outcomes
Process outcomes: adherence to the service
ATCS versus usual care
At 24 months in Bennett 2012, intervention group participants had completed 70.6% of the total 18 telephone counselling calls; 80.4% had completed calls 1 to 6; 65.0%, calls 7 to 12; and 66.7%, calls 13 to 18. Over 40.0% of intervention participants tracked their behaviour change goals weekly for at least 50% of trial weeks, and 25.0% tracked weekly for at least 75% of trial weeks. However, authors reported no data for these measures of adherence for the usual care (self‐help booklet) group.
Process outcomes: satisfaction
IVR versus control
Estabrooks 2008 reported that more than 50% of the participants in the IVR group were satisfied with the intervention, but authors reported no comparative data for satisfaction in the control group.
Patient‐centred outcomes: quality of life
IVR versus usual care
Goulis 2004 found that, compared with usual care, IVR probably had little or no effect on quality of life (as measured both by EQ‐5D and SF‐36 instruments) (moderate certainty evidence).
ATCS for reducing non‐attendance rate (preventive healthcare or management of long‐term conditions)
Seven studies evaluated ATCS (as appointment reminders) versus no intervention or nurse‐delivered reminder calls for reducing non‐attendance rates (Dini 1995; Griffin 2011; Maxwell 2001; Parikh 2010; Reekie 1998; Tanke 1994; Tanke 1997). For this outcome, the studies were too heterogeneous for statistical pooling. For a summary of the effects of these comparisons on appointment attendance, see Table 5.
Primary outcomes: behavioural outcomes
Non‐attendance rates
ATCS Plus versus nurse‐delivered calls
Griffin 2011 found that compared with a nurse‐delivered call, an ATCS Plus call delivered either three or seven (IVR3 or IVR7) days prior to flexible sigmoidoscopy or/and colonoscopy examinations probably had little or no effect on either appointment non‐attendance or preparation non‐adherence at six weeks (moderate certainty evidence).
IVR versus no reminder
Parikh 2010 found that compared with no reminder, IVR improved attendance at four months (OR 1.52, 95% CI 1.34 to 1.71, P < 0.0001; high certainty evidence).
Unidirectional ATCS versus control (no calls)
Two studies compared the effects of unidirectional ATCS and control on attendance rates at time points up to one month (Dini 1995; Tanke 1997), and three studies assessed the effects of this comparison at time points ranging from six weeks to six months (Maxwell 2001; Reekie 1998; Tanke 1994).
Dini 1995 found that unidirectional ATCS may have improved attendance at one month (rate ratio 1.60, 95% CI 1.29 to 1.98, P < 0.05). Tanke 1997 reported that compared with no calls, unidirectional ATCS may have improved return rates of tuberculin test at three days (OR 1.71, P < 0.05). Taken together, these studies provided low certainty evidence for this outcome.
In three further studies of low certainty, which assessed non‐attendance rates at later time points, there were mixed results when unidirectional ATCS interventions were compared with no‐call control groups. Reekie 1998 reported that unidirectional ATCS probably reduced non‐attendance rates at six weeks (OR 3.41, 95% CI 1.87 to 6.2, P < 0.001; moderate certainty evidence). In contrast, Maxwell 2001 found that unidirectional ATCS probably had little or no effect on non‐attendance rates at two months (moderate certainty evidence), while Tanke 1994 found that attendance rates may have been increased at six months (OR 1.50, P < 0.01; low certainty evidence).
Overall, these results suggest that certain ATCS interventions (IVR, unidirectional ATCS) may improve attendance rates when compared with control, although the certainty of the evidence varied from high to low.
Secondary outcomes
Process outcomes: satisfaction
ATCS Plus, IVR, unidirectional versus controls (nurse‐delivered calls, no calls)
Griffin 2011 reported that the intervention may have had little or no effect on participants' perceptions of experiences compared with the nurse‐call control group for flexible sigmoidoscopy. However, for the colonoscopy group, those who had received the nurse‐delivered calls versus the IVR3 or the IVR7 intervention calls (ATCS Plus) had slightly more positive perceptions about the call (35% versus 21% versus 26%; low certainty evidence). In Parikh 2010, 72% of the participants in the IVR group stated that the reminder was helpful, compared with 31% in no reminder (control) group who answered the same question (high certainty evidence). In Tanke 1994, 85% of the participants in the unidirectional ATCS group stated that the reminders were helpful (attitude questionnaire, question 3: mean response 6.73; scale range from 1 (negative) to 7 (positive)). In Tanke 1997, 65% of the participants in the unidirectional ATCS group endorsed the most positive response about the automated reminders.
ATCS for managing long‐term conditions
Adherence to medication or laboratory tests
We included 25 studies that compared ATCS with various control strategies (no intervention, usual care, or other ATCS interventions) for facilitating adherence to either medications or laboratory tests (Adams 2014; Bender 2010; Bender 2014; Boland 2014; Cvietusa 2012; Derose 2009; Derose 2013; Feldstein 2006; Friedman 1996; Glanz 2012; Green 2011; Ho 2014; Leirer 1991; Lim 2013; Migneault 2012; Mu 2013; Ownby 2012; Patel 2007; Reynolds 2011; Sherrard 2009; Simon 2010b; Stacy 2009; Stuart 2003; Vollmer 2011; Vollmer 2014). In several of these studies, we could group results and consider them together, as interventions and outcomes were similar. For other studies, we could not combine results with data from other trials within the same comparison due to differences in outcome measures, timing of outcome assessment, or both. For a summary of the effects of ATCS interventions, compared with various controls, on adherence to either medications or laboratory tests in various groups of participants, see Table 6.
Primary outcomes: behavioural outcomes
Adherence
Multimodal/complex interventions versus usual care or control (education and call)
Ho 2014 reported that compared with the usual care group, multimodal intervention (ATCS Plus, medication reconciliation and tailoring, patient education and collaborative care) probably improved adherence to cardioprotective medications at 12 months (89% versus 74%, P = 0.003; moderate certainty evidence). Stuart 2003 reported uncertain effects of a complex intervention (education, nurse‐delivered call and IVR intervention) versus control on adherence to antidepressant medications at four months (very low certainty evidence).
ATCS Plus versus control or other ATCS
Cvietusa 2012 reported that compared with control group (unspecified), ATCS Plus probably improved time to first inhaled corticosteroid refill (HR 1.26, 95% CI 1.12 to 1.42), and probably improved slightly the proportion of days with medication on hand in children (38% versus 28%, P < 0.001; moderate certainty evidence). Stacy 2009 reported that compared with an enhanced care control group (via IVR), ATCS Plus probably improved statin adherence (measured with six‐month point prevalence persistency; adjusted OR 1.64, 95% CI 1.19 to 2.26; moderate certainty evidence).
ATCS Plus versus usual care or no calls
Three studies reported the effects of ATCS Plus versus usual care on medication adherence, and we considered findings together.
Derose 2013 reported that ATCS Plus probably improved adherence to statins (RR 1.63, 95% CI 1.50 to 1.76, P < 0.001), as did Vollmer 2014, reporting a small increase in statin adherence at 12 months (mean change 0.02, 95% CI 0.01 to 0.03). Similarly, Vollmer 2011 reported an increase in adherence to inhaled corticosteroids (mean change 0.02, 95% CI 0.01 to 0.03, P = 0.002). Taken together these results suggest that ATCS Plus interventions, compared with usual care, probably improve medication adherence (moderate certainty evidence).
Three further studies assessed the effects of ATCS Plus on other measures of adherence that could not be combined.
Sherrard 2009 found that compared with usual care, ATCS Plus may have improved medication adherence compared with usual care (74.5% versus 49.7% compliant with the intervention; RR 0.34, 95% CI 0.20 to 0.56; P < 0.001) and may have improved slightly a composite measure that assessed increased medication adherence and reduced adverse events (51% versus 39%, RR 0.60, 95% CI 0.37 to 0.96, P = 0.041; low certainty evidence).
Derose 2009 found that compared with no calls, ATCS Plus probably had little or no effect on adherence to testing (completion of all three recommended laboratory tests for diabetes patients) at 12 weeks (OR 1.09, 95% CI 0.92 to 1.28; moderate certainty evidence).
Simon 2010b found that compared with usual care (no intervention), ATCS Plus probably had little or no effect on retinopathy examination rates (adjusted HR 0.93, 95% CI 0.71 to 1.22) tests for glycaemia (HR 0.72, 95% CI 0.38 to 1.37), hyperlipidaemia (HR 1.31, 95% CI 0.56 to 3.05), or nephropathy (HR 1.14, 95% CI 0.69 to 1.89) in diabetic patients at 12 months (moderate certainty evidence).
Overall, these results suggest that ATCS Plus interventions probably improve adherence to medications but may have little effect on adherence to tests, compared with usual care or no calls.
IVR versus control (other ATCS) or no calls
Four studies evaluated IVR interventions compared with other ATCS or no calls for effects on adherence but reported different outcome measures that could not be combined.
Adams 2014 found that compared with a single IVR call, the more comprehensive (repeated) IVR intervention may have slightly improved the comprehensiveness of screening and counselling in primary care parent‐child consultations (85.7% intervention group versus 72.6% control; P = 0.04; low certainty evidence). Bender 2010 reported that compared with no calls, IVR may have improved adherence to anti‐asthmatic medications at 10 weeks (intervention group mean 64.5% (SD 17.2) versus control mean 49.1% (SD 16.8) adherent at 10 weeks, P = 0.003; low certainty evidence). Leirer 1991 reported that compared with no calls, the IVR intervention may have reduced slightly medication non‐adherence (assessed as mean hours not adhering to medication, mean intervention group (SD) 3.68 h (2.62) versus 14.76 h (SD 13.98) control group; P < 0.03); low certainty evidence). Mu 2013 found that compared with no calls, IVR probably improved slightly medication refill rates at one month (26.41% intervention versus 21.85% control, P < 0.001; moderate certainty evidence).
Overall these results suggest that IVR interventions probably slightly improve measures of medication and other adherence compared with control (other ATCS) or no calls, but evidence was of uniformly low certainty.
IVR versus usual care
Nine studies assessed the effects of IVR interventions compared with usual care. Several studies reported comparable outcomes and time points and could be grouped for consideration.
Four studies reported medication adherence: two at 3 to 6 months (Boland 2014; Friedman 1996), and two at 8 to 12 months (Glanz 2012; Migneault 2012).
Boland 2014 reported that IVR improved adherence to glaucoma medications at three months (IVR median (range) 73% (32 to 96) versus usual care 67% (7 to 98), as did Friedman 1996 for anti‐hypertensive medication adherence at 6 months (6% higher in IVR group, P = 0.03). In comparison, at later time points, Migneault 2012 and Glanz 2012 reported little effect on adherence when IVR was compared with education‐only usual care at 8 months or usual care at 12 months, respectively.
Taken together, these studies suggest that IVR interventions probably slightly increase medication adherence at shorter time points (up to six months) but probably have little or no effect at longer time points when compared with usual care (moderate certainty evidence).
Two studies assessed IVR versus usual care for medication adherence, using refill rates, and we considered their findings together. Green 2011 and Reynolds 2011 reported that the IVR intervention increased medication refill rates by 5.7% (P < 0.001) and 6.3% (P < 0.001), respectively, at two weeks. Taken together, these results suggest that IVR probably slightly increased medication adherence, assessed by refill rates at two weeks (moderate certainty evidence).
Bender 2014 and Patel 2007 assessed the effects of IVR on medication adherence, as measured by the medication possession ratio (MPR), but we did not consider them together because they measured outcomes at very different time points. Patel 2007 reported that the IVR intervention led to a very slight increase in the MPR at three to six months, compared with usual care (0.759 intervention group versus 0.738 usual care (moderate certainty evidence). In comparison, Bender 2014 reported that the MPR probably increases by 25.4% with IVR over usual care over the 24‐month interval (moderate certainty evidence).
Feldstein 2006 assessed the effects of IVR interventions on adherence to testing (completion of all recommended laboratory tests), reporting that compared with usual care, the IVR intervention probably improved participants' adherence (HR 4.1, 95% CI 3.0 to 5.6, P < 0.001; moderate certainty evidence). However, this study did not adjust for clustering (unit of analysis error) and so may have reported an overly precise effect estimate.
Overall, the results suggest that IVR interventions probably improve adherence to medications/laboratory tests when compared with usual care; however, most results were based on studies of moderate certainty evidence, and the size of effects were variable and sometimes very small.
Unidirectional ATCS versus control (no intervention)
Two studies assessed the effects of unidirectional ATCS interventions in comparison with no intervention on medication adherence: Lim 2013 reported little effect on adherence at five months, while Ownby 2012 reported a small increase in medication adherence (mean (ATCS group) 75.7, 95% CI 65.0 to 86.5 versus mean (control group) 60.3, 95% CI 47.2 to 73.2; P = 0.02). Taken together, results from these two studies suggest that unidirectional ATCS may improve adherence to medications to a small degree compared with control, although this is based on low certainty evidence.
Primary outcomes: clinical outcomes
Blood pressure/lipids, disease control
Multimodal/complex intervention versus usual care
Ho 2014 reported that compared with usual care, a multimodal intervention (ATCS Plus, medication reconciliation and tailoring, patient education and collaborative care) probably had little or no effect on achieving reduced blood pressure targets (49% usual care versus 59% intervention group; P = 0.23) or low‐density lipoprotein cholesterol level targets (83% usual care versus 72% intervention; P = 0.14; moderate certainty evidence).
ATCS Plus versus usual care
Vollmer 2014 reported that compared with usual care, ATCS Plus probably reduced slightly overall systolic blood pressure (mean change= −0.5 mmHg, 95% CI −1.0 to 0.0; P = 0.041) but probably had little or no effect on overall low‐density lipoprotein levels (mean Δ change −0.6 ml/dL, 95% CI −1.8 to 0.7; P = 0.379; moderate certainty evidence).
IVR versus usual care
In Migneault 2012 the IVR intervention probably had little or no effect on diet, physical activity, systolic blood pressure, or diastolic blood pressure at 12 months (moderate certainty evidence). Similarly, Friedman 1996 reported that IVR may have had little or no effect on systolic blood pressure at six months (mean change from baseline −11.5 mmHg intervention group versus −6.8 mmHg usual care; P = 0.20) but that it may have slightly decreased diastolic blood pressure (mean change from baseline −5.2 mmHg intervention group versus −0.8 mmHg usual care; P = 0.02; low certainty evidence).
IVR versus no calls
Bender 2010 reported that compared with no calls, IVR probably had little or no effect on asthma control test (5‐item questionnaire where higher scores indicate better outcome) (intervention group mean (SD) −1.12 (3.90) versus −1.84 (4.14) control; P = 0.530; moderate certainty evidence).
Unidirectional ATCS versus control
Lim 2013 reported that there may have been little effect or no difference between unidirectional ATCS and control in terms of therapeutic coverage (low certainty evidence).
Secondary outcomes
Process outcomes: healthcare use
ATCS Plus versus usual care
Sherrard 2009 reported that the ATCS Plus intervention may have had little or no effect on emergency room visits (RR 1.04, 95% CI 0.63 to 1.73) or hospitalisations (RR 0.77, 95% CI 0.41 to 1.45; low certainty evidence), while Vollmer 2011 reported that among the participants who were successfully contacted, the rate of acute asthma healthcare utilisation may have increased slightly in the intervention group compared with usual care control (RR 1.06, P = 0.038; low certainty evidence).
Process outcomes: satisfaction with ATCS
Multimodal/complex intervention versus control (education and call)
In Stuart 2003, 50% of the participants rated the system as very helpful, 40% as somewhat helpful, and 10% as not helpful; authors did not provide data for the comparison group (very low certainty evidence).
ATCS Plus versus usual care
In Sherrard 2009, 90% of the participants were satisfied with the medication information provided by ATCS Plus, and 93% responded that they preferred an IVR follow‐up as opposed to no calls (low certainty evidence). Authors did not report comparative data for this study.
IVR versus control
Adams 2014 reported that parents in the IVR personal health partner (PHP) intervention group were slightly more likely than those in control group (single IVR call) to report feeling "more prepared"for the visit (81% versus 67%, P = 0.001) and to report that use of PHP reduced their visit time (63% versus 45%, P < 0.001). However, authors also reported that the IVR intervention may have had little or no effect on medication management (19.1% versus 9.7%; P = 0.19; low certainty evidence). In Friedman 1996, 85% of the physicians stated they read reports from the IVR system regularly.
Process outcomes: acceptability of service
ATCS Plus versus control
In Cvietusa 2012, two‐thirds of intervention group parents reported that the ATCS Plus calls were helpful and that the programme improved the care of their child's asthma.
IVR versus usual care
In Friedman 1996, 94% of patients reported that the IVR system "was easy to use". There were no data presented for comparison groups for the acceptability outcomes in either of these two studies, and the evidence was of low certainty.
Process outcomes: cost‐effectiveness
IVR versus usual care
In Friedman 1996, the computed cost per patient user for six months of IVR use was USD 32.50 (low certainty evidence). There were no comparison data presented for costs.
Cognitive outcomes: beliefs, cognition
IVR versus no calls
Bender 2010 reported that compared with no calls, IVR probably improved beliefs about medications (range scores above 0 (more positive beliefs) and scores below 0 (more negative beliefs)) (intervention group mean (SD) 0.25 (1.07) versus −0.51 (0.913) control; P = 0.007; moderate certainty evidence), while Leirer 1991 reported that compared with no calls, the IVR intervention may have had little or no effect on cognitive abilities (low certainty evidence).
Patient‐centred outcomes: quality of life
IVR versus no calls
Bender 2010 reported that compared with no calls, IVR probably had little or no effect on asthma‐related quality of life (32 questions where higher scores indicate better outcome) (intervention group mean (SD) −0.15 (0.92) versus −0.38 (1.06) control; P = 0.42; moderate certainty evidence).
Illicit drug addiction
We only identified one study that focused on addiction to illicit drugs (Moore 2013).
Primary outcomes: clinical outcomes
Substance use
ATCS Plus versus usual care
Moore 2013 reported that compared with usual care, ATCS Plus may have had little or no effect on self‐reported opioid, cannabis, or cocaine use (low certainty evidence).
Primary outcomes: behavioural outcomes
ATCS Plus may have had little or no effect on the number of counselling sessions attended when compared with usual care at four weeks (mean (SD) intervention group 3.3 sessions (9.5) versus 1.0 session (1.0) usual care; adjusted P = 0.72; low certainty evidence).
Secondary outcomes
Cognitive outcomes: coping skills
The intervention may have had little or no effect on coping skills when compared with usual care at four weeks (mean 0.82 intervention group versus mean 0.54 usual care group; low certainty evidence).
Process outcomes: acceptability of ATCS
Ratings of acceptability and perceived efficacy (each rated from 1 to 5 points on an ascending scale) showed negligible change over the four weeks of study. In the intervention group, mean interest at the end of the study was 3.6 (SD 0.9), mean perceived efficacy was 3.7 (SD 1.0), and mean perceived ease of use was 4.8 (SD 0.4). For these acceptability outcomes, authors reported no data from the comparison group.
Process outcomes: satisfaction
ATCS Plus may have had little or no effect on satisfaction with methadone treatment scores (five‐item Likert‐like scale) when compared with usual care at four weeks (mean (SD) 4.1 (1.2) intervention group versus 4.4 (0.8) usual care group; adjusted P = 0.62; low certainty evidence).
Alcohol consumption
Eight trials compared ATCS to no intervention, usual care, another intervention (advice/education; packaged cognitive behavioural therapy (via IVR)) or an informational pamphlet in managing alcohol consumption (Andersson 2012; Hasin 2013; Helzer 2008; Litt 2009; Mundt 2006; Rose 2015; Rubin 2012; Simpson 2005). For this outcome, the studies were too heterogeneous for statistical pooling. For a summary of the effects of these comparisons on alcohol intake, see Table 7.
Primary outcomes: behavioural outcomes
Alcohol consumption
ATCS Plus versus no intervention or usual care
Three studies compared ATCS Plus versus control or usual care, reporting several different measures of alcohol use (Helzer 2008; Mundt 2006; Rose 2015).
Helzer 2008 found that compared with control (no calls), ATCS Plus may have had little or no effect on weekly alcohol consumption (number of drinks/week) at six months (mean 22.4 intervention group versus 18.3 control group; P > 0.05; low certainty evidence). Likewise, Mundt 2006 found that compared with no intervention, ATCS Plus may have had little or no effect on drinking days, heavy drinking days, or total drinks consumed (P > 0.05; low certainty evidence). Rose 2015 reported that compared with usual care, ATCS Plus may have had little or no effect on the number of drinks per drinking day (P = 0.45; low certainty evidence).
Overall, these results suggest that ATCS Plus interventions may have little or no effect, when compared with no intervention or usual care, on measures of alcohol consumption, although the certainty of the evidence was low in all cases.
ATCS Plus versus another intervention
Two studies compared ATCS Plus interventions with another form of intervention, reporting different alcohol use measures that could not be combined.
Compared with advice/education, Hasin 2013 found that ATCS Plus may have reduced the number of drinks per drinking day in the last 30 days at two months (effect size Cohen's d = 0.44, 95% CI 0.07 to 0.81, P = 0.01; low certainty evidence), but it probably had little or no effect at 12 months. Litt 2009 compared ATCS Plus with packaged cognitive behavioural therapy, finding a slight reduction in the proportion of days abstinent at 12 weeks post‐treatment (P < 0.05) but negligible effect on the number of heavy drinking days, coping or drinking problems, or continuity of abstinence (low certainty evidence).
Overall, these results suggest that ATCS Plus interventions may have little or no effect on alcohol consumption when compared with selected other interventions.
IVR versus control (no intervention)
Two studies compared the effects of IVR and control on different measures of alcohol consumption.
Andersson 2012 found that compared with no intervention, IVR probably improved slightly results of the AUDIT score at six weeks (moderate certainty evidence). Simpson 2005 found that compared with no calls, IVR may have had little or no effect on drinking habits, alcohol craving, or post‐traumatic stress disorder symptoms at four weeks (low certainty evidence).
IVR versus control (information)
Rubin 2012 reported that compared with an informational pamphlet, IVR may have reduced slightly the number of heavy drinking days per month (effect size −0.74, P = 0.02) and drinks per drinking day (effect size −0.49), and it may have increased slightly the percent days abstinent per month (effect size 0.45) at six‐month follow‐up (low certainty evidence).
Overall, these results suggest that IVR interventions may slightly improve some measures of alcohol consumption, compared with no intervention or information provision, but the size of the effect is small and the evidence of low certainty.
Secondary outcomes
Process outcomes:acceptability of ATCS
ATCS Plus versus usual care
In Rose 2015, 88% of the patients found the ATCS system easy to use overall (88% responded 'somewhat' or 'very easy'), and users rated each feature as somewhat or very useful (low certainty evidence). There were no comparison data presented for acceptability.
Asthma
Vollmer 2006 and Xu 2010 evaluated two different ATCS interventions versus usual care for managing asthma.
Primary outcomes: clinical outcomes
Asthma control
ATCS Plus versus usual care
Vollmer 2006 found that compared with usual care, ATCS Plus may have had little or no effect on asthma control in the 12 months post‐randomisation (low certainty evidence).
Primary outcomes: behavioural outcomes
Medication use
ATCS Plus versus usual care
Vollmer 2006 found that compared with usual care, ATCS Plus may have had little or no effect on medication use (past four weeks) in the 12 months post‐randomisation (low certainty evidence).
IVR versus usual care
Xu 2010 found that compared with usual care, IVR may have had little or no effect on medication (oral steroid rescue medication) use (OR 0.55, 95% CI 0.22 to 1.38; P = 0.20) (low certainty evidence).
Overall, these results suggest that ATCS interventions may have little or no effect on improving selected outcomes in asthma, compared with usual care, but the evidence was of low certainty and was based on only two trials.
Secondary outcomes
Patient‐centred outcomes: quality of life
ATCS Plus versus usual care
Vollmer 2006 found that compared with usual care, ATCS Plus may have had little or no effect on quality of life (low certainty evidence).
IVR versus usual care
Xu 2010 found that compared with usual care, IVR may have had little or no effect on health‐related quality of life (low certainty evidence).
Process outcomes: satisfaction
ATCS Plus versus usual care
Vollmer 2006 suggested that ATCS Plus probably had little or no effect on satisfaction, compared with usual care. The mean satisfaction with asthma care (on a 7 point scale) was 6 and 5.9 in the intervention and usual care groups, respectively (P = 0.17; low certainty evidence).
Process outcomes: cost‐effectiveness/resource use
ATCS Plus versus usual care
Vollmer 2006 found that compared with usual care, ATCS Plus may have had little or no effect on healthcare use in the 12 months post‐randomisation (low certainty evidence).
IVR versus usual care
Xu 2010 found that compared with usual care, IVR may have reduced slightly the total healthcare costs (mean AUD −451, 95% CI −1075 to 172), but it may have had little or no effect on healthcare utilisation (OR 1.17, 95% CI 0.46 to 2.98, P = 0.75; low certainty evidence).
Cancer
Seven studies evaluated the effectiveness of ATCS compared with control, usual care, usual care delivered by another ATCS (IVR), interviews with clinicians, or telephone calls by nurses in managing cancer patients (Cleeland 2011; Kroenke 2010; Mooney 2014; Siegel 1992; Sikorskii 2007; Spoelstra 2013; Yount 2014). For this outcome, the studies were too heterogeneous for statistical pooling. For a summary of the effects of these comparisons on symptom severity in cancer patients, see Table 8.
Primary outcomes: clinical outcomes
Symptom severity, distress, or burden
Multimodal/complex intervention versus usual care
Kroenke 2010 reported that compared with usual care, a multimodal/complex intervention (ATCS plus symptom monitoring by a nurse and medications) probably reduced pain at three months (standardised effect size* 0.67, 95% CI 0.33 to 1.02) and probably reduced slightly pain at 12 months (standardised effect size 0.39, 95% CI, 0.01 to 0.77) (moderate certainty evidence).
*Standardised effect sizes were calculated as the mean group difference divided by the pooled baseline SD, where an effect size of 0.2 is modest and 0.5 is moderate (according to authors' definition).
ATCS Plus versus control or usual care delivered via ATCS
Cleeland 2011 found that compared with automated monitoring (via IVR) and usual symptom care, ATCS Plus may have reduced slightly symptom threshold events (rate ratio (for difference between groups) 0.88, 95% CI 0.78 to 0.98) and the cumulative distribution of symptom threshold events; however, it may have had little or no effect on mean symptom severity between discharge and follow‐up (low certainty evidence). Mooney 2014 found that compared with an attention control group (via IVR), ATCS Plus probably had little or no effect on symptom severity or distress scores (MD 0.06, P = 0.58; moderate certainty evidence). Spoelstra 2013 found that compared with usual care (symptom management toolkit (SMT) and an automated voice response (AVR) phone system alone), the ATCS Plus intervention (AVR system and SMT complemented by nurse strategies to manage unresolved symptoms and improve adherence) may have had little or no effect on symptom severity (range 0 (the symptom did not occur) to 10 (worst imaginable) (mean (SD) intervention group 11.0 (10.4) versus 11.6 (12.1) usual care group); low certainty evidence). Yount 2014 reported that compared with monitoring alone (via IVR), ATCS Plus (monitoring and reporting functions) may have had little or no effect on symptom burden at 12 weeks (low certainty evidence).
Overall, these results suggest that ATCS Plus interventions may have little or no effect on symptoms (severity, distress or burden) in cancer patients, when compared with control or usual care delivered via another ATCS, although the evidence was of mostly low certainty, and in some studies the involvement of ATCS systems as part of usual care may have prevented any effects of the intervention from being detected.
IVR versus nurse calls
Sikorskii 2007 found that compared with telephone calls by nurses, the automated telephone symptom management intervention may have had little or no effect on symptom severity (low certainty evidence).
Depression
Multimodal/complex intervention versus usual care
Kroenke 2010 reported that compared with usual care, a multimodal/complex intervention probably reduced slightly depression at 3 months (standardised effect size 0.42, 95% CI 0.16 to 0.69) and at 12 months (standardised effect size 0.41, 95% CI 0.08 to 0.72), but it probably had little or no effect on disability (range from 0 to 10) (mean (SD) intervention 3.95 points (2.95) versus usual care 4.57 points (3.24); P = 0.011) or co‐interventions (depression treatment by mental health professional) (mean (SD) intervention 34 (26.6) versus usual care 39 (29.8); P = 0.56) at 12 months follow‐up (moderate certainty evidence).
Primary outcomes: behavioural outcomes
Medication adherence
ATCS Plus versus usual care (via IVR)
Spoelstra 2013 found that compared with usual care (symptom management toolkit (SMT) and an automated voice response (AVR) phone system alone), the ATCS Plus intervention (AVR system and SMT complemented by nurse strategies to manage unresolved symptoms and improve adherence) may have had little or no effect on medication non‐adherence (intervention group 40% versus usual care group 18%; low certainty evidence).
Overall, compared with usual care or control, these results suggest that multimodal/complex interventions probably improve both pain and depression measured at different time points, whereas ATCS Plus interventions may have little or no effect on symptoms or adherence to medications. Similarly, IVR may have little or no effect on symptoms, compared with either control or when used as a comparison with ATCS Plus, although evidence was of generally low certainty and based on few studies.
Secondary outcomes
Patient‐centred outcomes: quality of life
Multimodal/complex interventions versus usual care
Kroenke 2010 reported that the multimodal intervention probably had little or no effect on overall quality of life (range from 0 (worse) to 10 (better)) compared with usual care (mean (SD) intervention group 6.20 points (2.27) versus 6.07 points (2.18) usual care group; P = 0.46) at 12 months follow‐up (moderate certainty evidence).
ATCS Plus versus control (via IVR)
Yount 2014 reported that compared with monitoring alone (via IVR), ATCS Plus (monitoring and reporting functions) may have had little or no effect on health‐related quality of life (27‐item, with higher scores indicating better outcome) (intervention mean (SD) 77.9 points (19.8) versus control 77.1 points (18.0); P = 0.78) at 12 weeks (low certainty evidence).
Process outcomes: healthcare use, costs
Multimodal/complex intervention versus usual care
Kroenke 2010 reported that the multimodal intervention probably had little or no effect on healthcare use compared with usual care (mean (SD) intervention 15.6 outpatient physician visits (9.9) versus usual care 16.4 outpatient physician visits(13.4); P = 0.55) at 12 months follow‐up (moderate certainty evidence).
Process outcomes: satisfaction, acceptability of the service
ATCS Plus versus control (via IVR)
In Mooney 2014, participants reported high satisfaction and ease of use for the automated ATCS Plus system. Overall, 94% found the automated system quite or very easy to use, 91% found the call length acceptable, and 77% said they were quite or very satisfied with using the system. Authors reported no comparison group data for this acceptability outcome. Yount 2014 reported that compared with monitoring alone (via IVR), ATCS Plus (monitoring and reporting functions) may have had little or no effect on satisfaction with explanations provided to them (mean (SD) 2.60 (0.57) versus 2.70 (0.53); P = 0.23) at 12 weeks (low certainty evidence).
Cognitive outcomes: barriers, unmet needs
ATCS Plus versus control (via IVR)
Yount 2014 reported that compared with monitoring alone (via IVR), ATCS Plus (monitoring and reporting functions) may have had little or no effect on symptom management barriers (mean (SD) 56.7 (14.4) versus 52.7 (16.9); P = 0.094) or self‐efficacy (mean (SD) 88.2 (18.9) versus 90.5 (19.9); P = 0.45) at 12 weeks (low certainty evidence).
IVR versus control
Siegel 1992, comparing a comprehensive clinician‐delivered needs assessment with IVR‐delivered needs assessment, reported uncertain effects on the prevalence of unmet needs (very low certainty evidence).
Chronic pain
Kroenke 2014 and Naylor 2008 evaluated two different ATCS interventions versus usual care.
Primary outcomes: clinical outcomes
Pain
Multimodal/complex intervention versus usual care
Kroenke 2014 found that compared with usual care, the intervention (ATCS Plus, nurse care, and stepped care with analgesics) probably reduced pain intensity at 12 months (mean (SD) intervention group 3.57 (2.22) versus 4.59 (2.13) usual care group; MD = −1.02, 95% CI −1.58 to −0.47; P < 0.001, where a 1 point change is clinically relevant), pain severity (scores range from 0 to 10,with higher scores representing worse pain) (MD −1.00, 95% CI −1.53 to −0.46; P < 0.001), pain interference (brief pain inventory) (MD −1.05, 95% CI −1.71 to −0.39; P < 0.001), and differences in response rates at 12 months (total pain score responders) (MD 1.91, 95% CI 1.36 to 2.69; P < 0.001; moderate certainty evidence).
IVR versus usual care
Naylor 2008 reported that compared with usual care, IVR may have reduced slightly typical pain intensity (range from 0 (no pain) to 10 (worst pain)) (mean usual care −1.0 (SD 1.8) versus IVR group mean −2.3 (SD 2.3) at eight‐month follow‐up (low certainty evidence).
Overall, these results suggest that a multimodal/complex intervention probably improves, and an IVR intervention may slightly improve, measures of chronic pain management in adults.
Secondary outcomes
Patient‐centred outcomes: quality of life
Naylor 2008 reported that compared with usual care, IVR may have slightly improved function/disability and coping as measured with SF‐36 mental health composite (mean (SD) 10.4 (14.2) versus 1.1 (12.0); P < 0.05), SF‐36 physical health composite (mean (SD) 8.9 (10.1) versus 2.6 (7.3); P < 0.001), and total pain experience (mean (SD) −18.1 (13.5) versus −3.5 (11.4); P < 0.0001); at eight‐month follow‐up (low certainty evidence).
Chronic obstructive pulmonary disease (COPD)
Primary outcomes: clinical outcomes
Exacerbations, health status
ATCS Plus versus control (no calls)
Halpin 2009 reported that compared with no calls, the ATCS Plus intervention probably had little or no effect on the frequency of exacerbations or the proportion of participants experiencing one or more COPD exacerbation, and that there were probably little or no differences in the frequency, severity, or duration of events measured with the EXAcerbations of Chronic pulmonary disease Tool (EXACT) and patient‐reported outcome scale, nor were there changes in health status (mean (standard error (SE)) intervention 49.7 points (2.4) versus control 51.5 points (2.4) between the ATCS Plus and no calls control group at four months (moderate certainty evidence).
Diabetes mellitus
Ten studies evaluated ATCS versus usual care for managing diabetes mellitus (Graziano 2009; Homko 2012; Katalenich 2015; Khanna 2014; Kim 2014; Lorig 2008; Piette 2000; Piette 2001; Schillinger 2009; Williams 2012). In several of these studies, we could combine results because outcome measures and timing were comparable. In other cases, we could not combine results with data from other studies within the same comparison due to differences in outcome measures, timing of outcome assessment, or both. For a summary of the effects of ATCS interventions, compared with usual care for managing diabetes mellitus, see Table 9.
Primary outcomes: clinical outcomes
Glycated haemoglobin
ATCS (ATCS Plus or IVR) versus usual care
We performed meta‐analysis on seven trials considered to be sufficiently homogeneous (Graziano 2009; Khanna 2014; Kim 2014; Lorig 2008; Piette 2001; Schillinger 2009; Williams 2012). It showed that compared with usual care, ATCS (ATCS Plus, IVR) may have reduced slightly glycated haemoglobin levels (MD −0.26%, 95% CI −0.50 to −0.01; low certainty evidence; Analysis 4.1). There was a moderate level of heterogeneity of the pooled studies (Tau2 = 0.06; Chi2 = 11.41, df = 5 (P = 0.04); I2 = 48%).
4.1. Analysis.
Comparison 4 ATCS vs usual care for managing diabetes mellitus, Outcome 1 Glycated haemoglobin.
Homko 2012 and Katalenich 2015 did not report data amenable to meta‐analysis for this outcome, reporting different outcomes or the same outcome differently. Reporting median glycated haemoglobin levels, Katalenich 2015 found that compared with usual care, ATCS Plus may have had little or no effect at six months (P > 0.05; low certainty evidence). Homko 2012 found that compared with usual care, IVR may have had little or no effect on fasting blood glucose levels in pregnancy (P = 0.26) or infant birth weight at 26 months (P = 0.30; low certainty evidence).
Blood glucose levels, diabetes‐related symptoms
ATCS Plus versus usual care
Lorig 2008 found that compared with usual care, ATCS Plus may have improved symptoms of hypoglycaemia (range from 0 to 12, with higher scores indicating worse outcome) (mean intervention change (SD) −0.453 (1.80) versus 0.029 (1.46); P = 0.042) and symptoms of hyperglycaemia (range from 0 to 12, with higher scores indicating worse outcome) (mean intervention change (SD) −0.827 (2.11) versus 0.029 (2.09); P < 0.001) at six months (low certainty evidence).
Piette 2001 found that compared with usual care, ATCS Plus probably slightly improved diabetes‐related symptoms (all symptoms) at 12 months (adjusted values: intervention group mean (SE) 3.7 (0.2) versus 4.4 (0.2); P = 0.04; moderate certainty evidence).
Blood pressure, blood lipids
ATCS Plus versus usual care
Khanna 2014 found that compared with usual care, ATCS Plus may have had little or no effect on systolic blood pressure (P = 0.43), diastolic blood pressure (P = 0.93), total cholesterol (P = 0.70), triglycerides (P = 0.55), high‐density lipoprotein (P = 0.75), or low‐density lipoprotein levels (P = 0.08) at three months (low certainty evidence).
Schillinger 2009 found that compared with usual care, ATCS Plus may have had little or no effect on systolic blood pressure (mean intervention (SD) 136.9 mmHg (20.4) versus 141.5 mmHg (23.9), standardised effect size 0.19, P = 0.20) or diastolic blood pressure (mean intervention (SD) 75.4 mmHg (12.3) versus 78.5 mmHg (18.5), standardised effect size 0.14, P = 0.40; low certainty evidence).
BMI, anthropometrics
ATCS Plus versus usual care
Khanna 2014 found that compared with usual care, ATCS Plus may have had little or no effect on BMI (P = 0.21) or waist circumference (P = 0.31) at three months (low certainty evidence). Schillinger 2009 found that compared with usual care, ATCS Plus may have had little or no effect on BMI (mean intervention (SD) 30.7 kg/m2 (6.9) versus 31.4 kg/m2 (8.5), standardised effect size −0.06, P = 0.8); low certainty evidence).
Psychological outcomes, mental health
ATCS Plus versus usual care
Piette 2000 found that compared with usual care, ATCS Plus probably had little or no effect on anxiety (P = 0.496) but probably improved slightly symptoms of depression (P = 0.023) (moderate certainty evidence). Lorig 2008 found that compared with usual care, ATCS Plus may have improved health distress (five‐items scale) (mean intervention change (SD) 0.595 (1.30) versus control −0.089 (1.29); P = 0.009) at six months (low certainty evidence). Schillinger 2009 found that compared with usual care, ATCS Plus may have had little or no effect on mental health (SF‐12, scale range 0–100 with higher scores indicating better outcome) (mean intervention (SD) 67.0 (25.8) versus 64.2 (27.2), standardised effect size 0.18, P = 0.20) (low certainty evidence).
Functional status
ATCS Plus versus usual care
Piette 2000 found that compared with usual care, ATCS Plus probably had little or no effect on decreased activity due to illness (P = 0.248) but probably reduced slightly days in bed because of illness (P = 0.026; moderate certainty evidence). Lorig 2008 found that compared with usual care, ATCS Plus may have had little or no effect on self‐reported global health (range from 0 to 5, with higher scores indicating better outcome) (mean intervention change (SD) −0.128 (1.30) versus control −0.023 (0.807); P = 0.713), activity limitation (range from 0 to 4) (mean intervention change (SD) −0.149 (1.05) versus control −0.119 (1.12); P = 0.273), or fatigue (range from 0 to 10, with higher scores indicating worse fatigue) (mean intervention change (SD) −0.254 (3.08) versus −0.145 (3.48); P = 0.694) at six months (low certainty evidence). Schillinger 2009 found that compared with usual care, ATCS Plus may have had little or no effect on physical health functional status (SF‐12, scale range 0–100 with higher scores indicating better outcome) (mean intervention (SD) 60.2 (29.1) versus 56.7 (31.3), standardised effect size 0.11, P = 0.4 ) but may have improved slightly functional status (mean intervention (SD) 1.4 bed days/month (2.7) versus 3.1 bed days/month (7.2), rate ratio 0.5, 95% CI 0.3 to 1.0, P = 0.05; low certainty evidence).
Primary outcomes:behavioural outcomes
Self‐monitoring of diabetic foot
ATCS Plus versus usual care
Meta‐analysis of two trials, considered to be sufficiently homogeneous, suggested that compared with usual care, ATCS Plus probably improved slightly self‐monitoring of diabetic foot (SMD 0.24, 95% CI 0.06 to 0.42; moderate certainty evidence; Analysis 4.2; Piette 2001; Schillinger 2009). There was no evidence of heterogeneity among the studies (Tau2 = 0.00; Chi2 = 0.67, df = 1 (P = 0.41); I2 = 0%). We expressed the effect size as standardised mean difference (SMD) because the studies used different measurement instruments, i.e. seven‐ item Likert‐like scale and telephone interview.
4.2. Analysis.
Comparison 4 ATCS vs usual care for managing diabetes mellitus, Outcome 2 Self‐monitoring of diabetic foot.
Self‐monitoring of blood glucose
ATCS Plus versus usual care
Lorig 2008 found that compared with usual care, ATCS Plus may have had little or no effect on self‐monitoring of blood glucose (mean intervention change (SD) 0.05 times/week (0.39) versus control 0.08 times/week (0.37); P = 0.457) at six months (low certainty evidence). At 12 months, however, pooled data from two studies showed that ATCS Plus probably improved slightly self‐monitoring of blood glucose compared with usual care (moderate certainty evidence)(Piette 2001; Schillinger 2009).
IVR versus usual care
Graziano 2009 found that compared with usual care, IVR probably increased slightly the mean change in frequency of self‐monitoring of blood glucose (P < 0.001; moderate certainty evidence).
Weight monitoring
ATCS Plus versus usual care
Piette 2001 found that compared with usual care, ATCS Plus probably had little or no effect on weight monitoring at 12 months (range from 0 = never to 5 = daily) (adjusted values: intervention group mean (SE) 2.6 (0.1) versus 2.5 (0.1); P = 0.60; moderate certainty evidence).
Physical activity, diet
ATCS Plus versus usual care
Lorig 2008 found that compared with usual care, ATCS Plus may have had little or no effect on aerobic exercise (mean intervention change (SD) 3.60 min/week (107) versus control −3.47 min/week (115); P = 0.891) at six months (low certainty evidence). Schillinger 2009 found that compared with usual care, ATCS Plus may have slightly improved diet (mean (SD) 4.4 (1.1) versus 3.9 (1.5), standardised effect size 0.42; P = 0.003), and exercise (mean (SD) 2.6 (2.0) versus 1.9 (1.8), standardised effect size 0.47, P = 0.0008) and may have improved moderate intensity physical activity levels (two more hours/week with intervention) (standardised effect size 0.31, P = 0.03) but may have had little or no effect on vigorous intensity physical activity levels (standardised effect size 0.21, P = 0.10) at 12 months (low certainty evidence).
Medication adherence
ATCS Plus versus usual care
Katalenich 2015 found that compared with usual care, ATCS Plus may have had little or no effect on adherence rates at six months (P = 0.04; low certainty evidence). Piette 2001 found that compared with usual care, ATCS Plus probably had little or no effect on medication use at 12 months (adjusted values: intervention group any medication problem 45 versus 39; P = 0.40; moderate certainty evidence).
Overall, the results suggest that compared with usual care, ATCS interventions (ATCS Plus, IVR) probably slightly reduce glycated haemoglobin levels and probably slightly improve self‐monitoring of diabetic foot and blood glucose levels. ATCS Plus interventions may also slightly improve symptoms associated with diabetes, depression, and distress, but they may have little or no effect on medication adherence or use, anxiety, blood pressure, BMI, or weight monitoring, and they appear to have mixed effects on functional measures, diet, and physical activity levels.
Secondary outcomes
Process outcomes: satisfaction with care
ATCS Plus versus usual care
Piette 2001 found that compared with usual care, ATCS Plus probably improved slightly satisfaction with care measured with the Employee Health Care Value Survey (range from 1 = poor to 5 = excellent) at 12 months (adjusted values: intervention group mean (SE) 3.8 (0.05) versus usual care 3.7 (0.04); P = 0.05; moderate certainty evidence). Schillinger 2009 found that compared with usual care, ATCS Plus may have improved participant assessment of chronic illness care (100‐point scale, with higher scores representing greater chronic care model alignment) (mean intervention (SD) 58.9 (23.1) versus 48.2 (26.5), standardised effect size 0.51; P = 0.0003); low certainty evidence).
Process outcomes: cost‐effectiveness
ATCS Plus versus usual care
Katalenich 2015 found that compared with usual care, ATCS Plus may have reduced healthcare expenditure (estimated cost for intervention USD 681.82 per participant versus estimated cost of USD 1131.07 usual care per participant, P < 0.001; low certainty evidence).
Process outcomes: healthcare use
ATCS Plus versus usual care
Lorig 2008 found that compared with usual care, ATCS Plus may have had little or no effect on healthcare utilisation as measured with physician visits (mean intervention change (SD) −0.028 visits/past six months (3.14) versus −0.064 visits/past six months (2.64); P = 0.852), accident and emergency visits (mean intervention change (SD) −0.107 visits/past six months (0.820) versus control −0.081 visits/past six months (0.943); P = 0.665), or length of hospital stay (mean intervention change (SD) 0.35 days (7.18) versus control −0.09 days (1.49); P = 0.26) (low certainty evidence). Piette 2001 found that compared with usual care, ATCS Plus probably increased the use of specialty services including podiatry clinics (adjusted values: intervention group 62 visits versus 42 visits; P = 0.003), foot examinations (92 examinations versus 72 examinations; P = 0.0002), and diabetes clinics (61 visits versus 25 visits; P = 0.03), and probably increased slightly cholesterol testing (87 versus 78; P = 0.05). However, it probably had little or no effect on opthalmopathy visits (40 visits versus 38 visits; P = 0.8; moderate certainty evidence).
Cognitive outcomes: self‐efficacy
ATCS Plus versus usual care
Lorig 2008 reported that ATCS Plus may have improved self‐efficacy scores (assessed on a 0 to 10 scale) (mean change intervention (SD) 0.695 points (2.36) versus usual care 0.004 points (2.37); P < 0.001; low certainty evidence). Piette 2000 found that compared with usual care, ATCS Plus probably improved slightly self‐efficacy (P = 0.006; moderate certainty evidence).
Patient‐centred outcomes: quality of life
ATCS Plus versus usual care
Katalenich 2015 found that compared with usual care, ATCS Plus may have had little or no effect on on quality of life at six months (P = 0.04; low certainty evidence). Piette 2000 found that compared with usual care, ATCS Plus probably had little or no effect on diabetes‐specific health‐related quality of life (P = 0.770; moderate certainty evidence). Williams 2012 found that compared with usual care, IVR may have improved the mental health‐related quality of life component of the SF‐36 (MD 3.0, 95% CI 0.8 to 5.2 P = 0.007) but may have had little or no effect on the physical component (MD 0.4, 95% CI −1.7 to 2.4, P = 0.7; low certainty evidence).
Heart failure
Four studies evaluated ATCS versus usual care for improving health outcomes and reducing healthcare utilisation in participants with heart failure (Capomolla 2004; Chaudhry 2010; Krum 2013; Kurtz 2011). For a summary of the effects of ATCS interventions versus usual care on heart failure outcomes, see Table 10.
Below, we report results for individual outcomes except for the study by Kurtz 2011, which defined adverse events as a composite outcome of cardiac mortality plus rehospitalisation for heart failure.
Primary outcomes: clinical outcomes
Hospitalisation for heart failure
Four studies reported the effects of ATCS interventions on this outcome, but we could not statistically pool results because of high heterogeneity (over 90%). We therefore present the results narratively.
ATCS Plus versus usual care or usual community care
Chaudhry 2010 found that compared with usual care, the intervention had little or no effect on hospitalisation for heart failure (27.5% intervention group versus 27% usual care; P = 0.81; high certainty evidence), with Krum 2013 also reporting that there was probably little or no effect for the intervention on this same outcome (14.3% intervention group versus 16.7% usual care; adjusted HR 0.78, 95% CI 0.45 to 1.33, P = 0.36; moderate certainty evidence). Capomolla 2004 reported that ATCS Plus may decrease hospitalisation rates for heart failure (25.4% intervention group versus 87.9% usual community care; P < 0.05; low certainty evidence).
IVR versus usual care
Kurtz 2011 reported that the IVR intervention had uncertain effects on hospitalisation for heart failure (13% intervention group versus 34% usual care; P < 0.05; very low certainty evidence).
Cardiac mortality
ATCS Plus, IVR versus usual care
Meta‐analysis of two trials, considered to be sufficiently homogeneous, found that ATCS had uncertain effects on cardiac mortality compared with usual care (RR 0.60, 95% CI 0.21 to 1.67; very low certainty evidence; Analysis 5.1; Capomolla 2004; Kurtz 2011). There was no evidence of heterogeneity (Chi2 = 0.99, df = 1 (P = 0.32); I2 = 0%).
5.1. Analysis.
Comparison 5 ATCS vs usual care for reducing healthcare utilisation in patients with heart failure, Outcome 1 Cardiac mortality.
All‐cause mortality
ATCS Plus versus usual care or usual community care
Meta‐analysis of three trials, considered to be sufficiently homogeneous, found that ATCS probably had little or no effect on all‐cause mortality compared with usual care or usual community care (RR 1.00, 95% CI 0.79 to 1.28; moderate certainty evidence; Analysis 5.2; Capomolla 2004; Chaudhry 2010; Krum 2013). There was no evidence of heterogeneity (Chi2 = 1.06, df = 2 (P = 0.59); I2 = 0%).
5.2. Analysis.
Comparison 5 ATCS vs usual care for reducing healthcare utilisation in patients with heart failure, Outcome 2 All‐cause mortality.
All‐cause hospitalisation
ATCS Plus versus usual care or usual community care
Capomolla 2004 found that compared with usual community care, ATCS Plus may have reduced all‐cause hospitalisation (for chronic heart failure, cardiac cause and other cause; 22 in intervention group versus 77 in control group; P < 0.009; low certainty evidence), and Krum 2013 similarly reported that the intervention probably slightly decreased all‐cause hospitalisation (45.9% intervention group versus 55.9% usual care; P = 0.021; moderate quality evidence). However, Chaudhry 2010 (the largest, highest quality study) found that the ATCS Plus intervention had little or no effect on readmission for any reason (49.3% intervention group versus 47.4% usual care; P = 0.45; high certainty evidence).
Global health rating
ATCS Plus versus usual care
Krum 2013 reported that the intervention probably improved slightly the proportion of participants with improved global health questionnaire ratings at 12 months (35.6% intervention group versus 28.4% receiving usual care; no further data; moderate certainty evidence).
Adverse events
ATCS Plus versus usual care
Chaudhry 2010 did not report any adverse events during the study period.
IVR versus usual care
Kurtz 2011 classified adverse events as cardiac mortality plus rehospitalisation for heart failure (reported as individual outcomes above), with uncertain effects upon this composite outcome reported (22% in intervention group versus 44% usual care group; P < 0.04; very low quality evidence).
Overall, these results suggest that, compared with usual care, ATCS interventions probably have little or no effect on hospitalisation for heart failure, all‐cause mortality, or all‐cause hospitalisation. Effects on cardiac mortality are uncertain, as are adverse events associated with the intervention in this population.
Secondary outcomes
Process outcomes: usability of ATCS
ATCS Plus versus usual care
Capomolla 2004 found that adherence to the ATCS system was 81%. There were no comparison group data for the usability outcome in this study (low certainty evidence).
Process outcomes: cost‐effectiveness/resource use
ATCS Plus versus usual care
Capomolla 2004 found that compared with usual community care, ATCS Plus may have reduced emergency room use at (median) 11 months (1 visit in intervention group versus 12 visits in usual care group, P < 0.05; low certainty evidence).
Chaudhry 2010 found that compared with usual care, the intervention had little or no effect on length of hospital stay (mean (SD) intervention group 7.2 days (15.6) versus 7.0 days (14.9) usual care, P = 0.27) or number of hospitalisations (none: 50.7% intervention versus 52.6% usual care group; one admission: 24% intervention versus 25.6% usual care; five or more admissions: 3% intervention versus 2.4% usual care group; high certainty evidence).
HIV/AIDS
Only Shet 2014 assessed the effects of ATCS interventions in HIV/AIDS, comparing a complex multimodal intervention (a combination of IVR calls, a weekly non‐interactive neutral pictorial message, plus three counselling sessions and antiretroviral treatment) with usual care.
Primary outcomes: clinical outcomes
Time to virological failure
Shet 2014 reported that the intervention did not change the time to virological failure (unadjusted HR 0.98, 95% CI 0.67 to 1.47, P = 0.95; high certainty evidence).
Mortality
There were 21/315 (6.7%) deaths in the intervention compared with 23/316 (7.3%) in usual care arm. Mortality assessment showed that 4.51 deaths per 100 person‐years (95% CI 2.94 to 6.91) occurred in the intervention arm, compared with 5.04 deaths per 100 person‐years (3.35 to 7.58) in the standard care arm (high certainty evidence).
Primary outcomes: behavioural outcomes
Medication adherence
Shet 2014 found that the complex intervention had little or no effect on medication adherence (unadjusted incidence rate ratio 1.24, 95% CI 0.93 to 1.65, P = 0.14; high certainty evidence).
Attrition from the study
Attrition occurred at the rate of 3.43 dropouts per 100 person‐years (95% CI 2.10 to 5.61) and 4.82 dropouts per 100 person‐years (3.17 to 7.31) in the intervention and usual care arms, respectively (high certainty evidence).
Hypercholesterolaemia
Hyman 1996 and Hyman 1998 evaluated ATCS (IVR and ATCS Plus, respectively) versus usual care for managing hypercholesterolaemia.
Primary outcomes: clinical outcomes
Total cholesterol
ATCS Plus versus usual care
Hyman 1998 found that compared with usual care, ATCS Plus may have had little or no effect on total cholesterol levels (P = 0.58; low certainty evidence).
IVR versus usual care
Hyman 1996 found that compared with usual care, IVR may have had little or no effect on total cholesterol levels (P = 0.94; low certainty evidence).
Primary outcomes:behavioural outcomes
Dietary fat intake
ATCS Plus versus usual care
Hyman 1998 found that ATCS Plus may have had little or no effect on dietary fat intake (−2.1 versus −2.0; low certainty evidence).
Overall, these results suggest that, compared with usual care, ATCS interventions may have very little or no effect on total cholesterol levels or dietary intake of fats in people with hypercholesterolemia, although evidence was of low certainty and from a small number of studies.
Secondary outcomes
Cognitive outcomes: knowledge, self‐efficacy
ATCS Plus versus usual care
Hyman 1998 found that ATCS Plus may have had little or no effect on self‐efficacy or on knowledge about saturated and polyunsaturated fats: at baseline both groups scored 37% of items correct on a 9‐point knowledge scale; postintervention, the ATCS Plus group improved by 0.14 and the usual care group by 0.06 items on the scale (low certainty evidence).
Process outcomes: acceptability
IVR versus usual care
Hyman 1996 reported that 83.3% of a subset evaluating the IVR intervention indicated the phone messages were helpful. There was no comparison group for this acceptability outcome.
Hypertension
Five trials evaluated the effectiveness of ATCS compared with usual care with and without education for managing hypertension (Bove 2013; Dedier 2014; Harrison 2013; Magid 2011; Piette 2012). For a summary of the effects of these comparisons on hypertension, see Table 11.
Primary outcomes: clinical outcomes
ATCS (multimodal/complex intervention, ATCS Plus, unidirectional ATCS) versus usual care or enhanced usual care (plus information)
Systolic blood pressure
Meta‐analysis of three trials, considered to be sufficiently homogeneous, found that ATCS probably reduced slightly systolic blood pressure compared with usual care with or without information (MD −1.89 mmHg, 95% −2.12 to −1.66; moderate certainty evidence; Analysis 6.1; Harrison 2013; Magid 2011; Piette 2012). There was no evidence of heterogeneity among the pooled studies (Tau2 = 0.00; Chi2 = 1.48, df = 2 (P = 0.48); I2 = 0%).
6.1. Analysis.
Comparison 6 ATCS vs usual primary care and education or usual care for managing hypertension, Outcome 1 Systolic blood pressure.
Diastolic blood pressure
Meta‐analysis of two trials reported no effect for ATCS on diastolic blood pressure compared with usual care (MD 0.02 mmHg, 95% CI −2.62 to 2.66; low certainty evidence; Analysis 6.2; Harrison 2013; Magid 2011). There was a substantial degree of heterogeneity in the meta‐analysed studies (Tau2 = 2.84; Chi2 = 3.63, df = 1 (P = 0.06); I2 = 72%).
6.2. Analysis.
Comparison 6 ATCS vs usual primary care and education or usual care for managing hypertension, Outcome 2 Diastolic blood pressure.
We did not include two studies in the meta‐analysis, as they reported different outcomes or insufficient information to allow inclusion (Bove 2013; Dedier 2014).
Bove 2013 found that compared with usual care, a multimodal/complex intervention (ATCS Plus plus sphygmomanometer, a weighting scale, pedometer, and instructions on their use) probably had little or no effect on blood pressure control at six months (54.5% controlled in intervention group versus 52.3% in usual care group, P = 0.43; moderate certainty evidence).
Dedier 2014 reported that compared with usual care plus education, IVR may have had little or no effect on systolic blood pressure at three months (P > 0.05; low certainty evidence).
Health status
ATCS Plus versus enhanced usual care (plus information)
Piette 2012 found that compared with enhanced usual care, ATCS Plus may have slightly improved overall health status (mean (SE) 2.5 (0.09) versus 2.1 (0.08), P = 0.0009, where 1 = poor and 5 = excellent) at six weeks (low certainty evidence).
Depression
ATCS Plus versus enhanced usual care (usual care plus information)
Piette 2012 found that compared with enhanced usual care, ATCS Plus may have reduced depressive symptoms on the 10‐item Center for Epidemiologic Studies Depression Scale (CESD) at six weeks (MD −2.5, 95% CI −4.1 to −0.8; P = 0.004; low certainty evidence).
Primary outcomes: behavioural outcomes
Medication adherence/use
Multimodal/complex versus usual care
Magid 2011 found that compared with usual care, a multimodal/complex intervention (ATCS Plus plus patient education, home blood pressure monitoring, and clinical pharmacist management of hypertension with physician oversight) may have had little or no effect on medication adherence assessed as either medication possession ratio (mean intervention group 0.85 (SD 0.19) versus usual care group mean 0.84 (SD 0.19), P = 0.88) or the proportion of people adherent (69.9% intervention versus 69.4% usual care classified as adherent; low certainty evidence).
ATCS Plus versus enhanced usual care (plus information)
Piette 2012 found that compared with enhanced usual care, ATCS Plus may have reduced the number of medication‐related problems measured using a seven‐item index (intervention group mean (SE) 2.8 (0.2) versus control group 3.6 (0.2)) at six weeks (low certainty evidence).
Physical activity
IVR versus enhanced usual care
Dedier 2014 reported that compared with usual care plus education, IVR may have increased slightly physical activity levels (143.2 min/week intervention group versus 110.2 min/week control group, P = 0.007; low certainty evidence).
Overall, these results suggest that, compared with usual care, ATCS interventions may have little or no effect on blood pressure or medication adherence in people with hypertension but may improve some outcomes such as medication problems, depressive symptoms, physical activity, and perceived health status to a small degree. However, almost all results were based on low certainty evidence.
Secondary outcomes
Process outcomes: satisfaction
ATCS Plus versus enhanced usual care
Piette 2012 found that compared with usual care and information, ATCS Plus may have improved slightly participants' satisfaction with hypertension care scores at six weeks (mean (SE) intervention group 1.8 (0.06) versus 1.4 (0.09) usual care group; P = 0.06; where 0 = not receiving care for hypertension; 1 = receiving care but dissatisfied; 2 = satisfied; low certainty evidence).
Mental health
Three studies evaluated different ATCS interventions versus advice only (Farzanfar 2011), relaxation therapy (Greist 2002), or healthy lifestyle (Zautra 2012) for managing mental health problems.
Primary outcomes: clinical outcomes
Obsessive compulsive disorder symptoms
ATCS Plus versus control (relaxation therapy)
Greist 2002 found that compared with control, ATCS Plus may have improved symptoms of obsessive compulsive disorder (Yale‐Brown obsessive compulsive scale score, range 0‐40) at three months (mean (SD) intervention group 19.0 points (7.2) versus control 24.1 points (6.7); P < 0.001; low certainty evidence).
Depression, stress symptoms, other outcomes
ATCS Plus versus control (relaxation therapy)
Greist 2002 found that compared with control, ATCS Plus may have had little or no effect on depressive symptoms measured with the Hamilton rating scale for depression (range 0‐50) at three months (mean intervention group (SD) 9.6 points (7.9) versus 10.0 points (8.2); P = 0.16) but may have improved results on the clinical global impressions scale (38% versus 14% 'much' or 'very much' improved; P = 0.002) and the patient's global impressions scale (38% versus 15% 'much' or 'very much' improved; P = 0.004) (low certainty evidence).
IVR versus control (advice)
Farzanfar 2011 reported that compared with control, IVR may have had little or no effect on depressive symptoms measured with total depression score (scale from 0 to 27 with higher values indicating more depression) at six months (mean change from baseline for intervention group (SD) −2.2 points (4.7) versus −1.8 points (4.5) or symptoms of stress measured with stress questionnaire score (score from 1 to 16 with higher values indicating greater stress) (mean change from baseline for intervention group (SD) −2.1 points (3.4) versus −1.8 points (3.1); low certainty evidence).
Unidirectional ATCS versus control (healthy lifestyle)
Zautra 2012 found that compared with control, the intervention may have had little or no effect on stress but may have reduced slightly depressive symptoms at one month (P < 0.05; low certainty evidence).
Well‐being
IVR versus control (advice)
Farzanfar 2011 reported that compared with control, IVR may have had little or no effect on well‐being index total scores (score from 0 to 25 with higher values indicating better functioning) (mean change from baseline for intervention group (SD) 3.7 points (6.8) versus 3.5 points (7.1); low certainty evidence).
Overall, these results suggest that, compared with various controls, ATCS interventions may have little or no effect on several indices of mental health, but the results are based on a small number of studies, with evidence of low certainty.
Secondary outcomes
Process outcomes: acceptability of service
IVR versus control (advice)
In Farzanfar 2011, more than 60% of the participants found the ATCS intervention useful, user‐friendly, informative and appropriately paced (low certainty evidence). Authors reported no comparison group data for this outcome.
Process outcomes: satisfaction
ATCS Plus versus control (relaxation therapy)
Greist 2002 found that compared with control, ATCS Plus may have improved satisfaction scores (low certainty evidence).
Patient‐centred outcomes: quality of life
IVR versus control (advice)
Farzanfar 2011 reported that compared with control, IVR may have had little or no effect on quality of life at six months (physical health scale) but may have improved slightly quality of life mental health scale scores (scale from 0 to 100) at six months (mean increase from baseline for intervention group (SD) 10.9 (10.1) versus 6.0 (12.7); P < 0.10 with higher scores indicating better outcome; low certainty evidence).
Obstructive sleep apnoea syndrome (OSAS)
DeMolles 2004 and Sparrow 2010 assessed ATCS interventions (IVR) versus usual care or attention placebo, respectively, for managing the symptoms of OSAS.
Primary outcomes: clinical outcomes
Sleep symptoms
IVR versus usual care or control (attention placebo via IVR)
DeMolles 2004 found that compared with usual care, IVR may have had little or no effect on improving functional outcomes of sleep (P = 0.171) but may have slightly improved scores on the sleep symptoms checklist (maximum score 45, lower score indicates improvement) (intervention group mean (SD) 9.4 (6.0) versus usual care group mean 13.4 (6.6), P = 0.047; low certainty evidence).
Sparrow 2010 found that compared with control, the slightly increased continuous positive airway pressure (CPAP) adherence in the IVR group was associated with a greater reduction in depressive symptoms (regression coefficient −0.028, SE 0.014, 95% CI 0.056 to 0.000, P = 0.048) and improvements in function (regression coefficient 0.021, SE 0.007, 95% CI 0.008 to 0.035, P = 0.003; low certainty evidence).
Primary outcomes: behavioural outcomes
CPAP use
IVR versus usual care or control (attention placebo via IVR)
DeMolles 2004 found that compared with usual care, IVR may have increased slightly CPAP use at two months (intervention group mean (SD) 4.4 h nightly use (3.0) versus 2.9 h nightly use (2.4) in usual care group, P = 0.07; low certainty evidence). Sparrow 2010 found that compared with control, IVR may have increased slightly CPAP use at both 6 months (median 2.4 h nightly use intervention group versus 1.48 h nightly use control) and 12 months (median 2.98 h nightly use intervention group versus 0.99 h nightly use control group; low certainty evidence).
Overall, these results suggest that, compared with usual care or attention placebo, IVR interventions may slightly increase CPAP use in both the short and long term, with mixed effects on functional sleep outcomes and symptoms, although these results are based on low certainty evidence from only two small studies.
Smoking
We included 10 studies that evaluated ATCS versus various controls (no calls, usual care, control ('placebo' ATCS (IVR), self‐help intervention, stage‐matched manuals) on smoking abstinence and related outcomes (Brendryen 2008; Carlini 2012; Ershoff 1999; McNaughton 2013; Peng 2013; Reid 2007; Reid 2011; Regan 2011; Rigotti 2014; Velicer 2006). For a summary of the effects of ATCS interventions compared with various controls, see Table 12.
Primary outcomes: clinical outcomes
Smoking abstinence
ATCS (multimodal/complex intervention, ATCS Plus, IVR) versus control (no calls, usual care, inactive IVR)
Meta‐analysis of seven trials considered to be sufficiently homogeneous suggested that, compared with control, ATCS may have had little or no effect on maintaining smoking abstinence (RR 1.20, 95% CI 0.98 to 1.46; low certainty evidence; Analysis 7.1; Brendryen 2008; Ershoff 1999; McNaughton 2013; Regan 2011; Reid 2007; Rigotti 2014; Velicer 2006). There was a moderate level of heterogeneity of the meta‐analysed studies (Tau2 = 0.04; Chi2 = 12.35, df = 6 (P = 0.05); I2 = 51%).
7.1. Analysis.
Comparison 7 ATCS for smoking cessation, Outcome 1 Smoking abstinence.
Smoking abstinence (other measures)
ATCS Plus, IVR versus usual care or no calls
Rigotti 2014 also reported that compared with usual care, ATCS Plus improved self‐reported continuous abstinence rates at six months (28% versus 16%; RR 1.70, 95% CI 1.15 to 2.51; P = 0.007; high certainty evidence); while McNaughton 2013 reported that compared with no calls, IVR may have had little or no effect on biochemically confirmed smoking abstinence at two years (21.7% of intervention group versus 42.9% of control group; P = 0.13; low certainty evidence).
We did not include three studies in meta‐analysis: Reid 2011 did not report sufficient information to allow us to include their data on abstinence, while Carlini 2012 and Peng 2013 reported outcomes other than abstinence rates.
ATCS Plus versus usual care
Reid 2011 reported that compared with usual care, ATCS Plus may have improved the continuous smoking abstinence rate at 26 weeks (38.7% versus 29.5%; adjusted OR 1.58, 95% CI 1.04 to 2.42; P = 0.034), and this was maintained at 52 weeks (35.6% versus 28.6%; adjusted OR 1.45; 95% CI 0.94 to 2.22; P = 0.093; low certainty evidence).
Primary outcomes: behavioural outcomes
Medication use
Complex/multimodal intervention versus control (self‐help booklet)
Brendryen 2008 found that compared with control, a multimodal/complex intervention probably had little or no effect on adherence to nicotine replacement therapy (93% in intervention group versus 87% control group; P = 0.07; moderate certainty evidence).
ATCS Plus versus control (inactive IVR)
Regan 2011 found that compared with control, ATCS Plus probably had little or no effect on medication use (moderate certainty evidence).
Support programme enrolment
ATCS Plus versus control (inactive IVR)
Carlini 2012 found that compared with control, ATCS Plus may have improved re‐enrolment into a quitline support programme (OR 11.2, 95% CI 5.4 to 23.3, P < 0.001; low certainty evidence).
Overall, these results suggest that compared with various controls, ATCS interventions may have little or no effect on maintenance of smoking abstinence. ATCS Plus interventions increase abstinence at six months, but effects of IVR and ATCS Plus at longer time points appear inconsistent. ATCS Plus may improve cessation programme support enrolment, with probably little or no effect on adherence to medication, but the certainty of the evidence was variable (moderate to low).
Secondary outcomes
Process outcomes: cost‐effectiveness
ATCS Plus versus usual care
Rigotti 2014 found that the incremental per‐participant costs in the intervention group were USD 540 (year 1) and USD 294 (subsequent years) (high certainty evidence). There was no comparative data presented for cost‐effectiveness outcomes.
Process outcomes: acceptability
IVR versus control (booklet)
Ershoff 1999 reported that 25% of intervention non‐users felt that they did not know enough about the automated system; 33% did not think it could help them to quit smoking, and 20% did not like the idea of entering information into a computer. There was no comparison group for satisfaction outcomes.
Cognitive outcomes: self‐efficacy
Complex/multimodal intervention versus control (self‐help booklet)
Brendryen 2008 found that compared with a self‐help booklet, ATCS Plus (complex intervention) probably increased smoking cessation self‐efficacy (seven‐point scale) at 12 months (mean intervention group (SD) 5.10 points (1.41) versus control 4.38 points (1.31); P < 0.001); moderate certainty evidence).
ATCS Plus versus control (inactive IVR)
Peng 2013 found that compared with control, ATCS Plus may have had little or no effect on self‐efficacy, stage of change or decisional balance toward smoking cessation at four weeks (P > 0.05; low certainty evidence).
Spinal cord dysfunction
One study evaluated IVR versus usual care for managing spinal cord dysfunction (Houlihan 2013).
Primary outcomes: clinical outcomes
Pressure ulcers, depression
Houlihan 2013 reported that compared with usual care, the IVR (CareCall) may have had little or no effect on the number of pressure ulcers (in adjusted models), but may have reduced slightly the severity of depression at six months in those with depression at baseline (effect size −0.56; P = 0.038; low certainty evidence).
Sensitivity analyses
There were not enough data (at least 10 studies) included in any of the pooled analyses to perform sensitivity analyses.
Assessment of publication bias
Formal assessment of potential publication bias was not feasible given the small number of trials contributing data to outcomes within different comparisons in this review.
Discussion
ATCS is a technology platform through which health professionals can collect relevant information or deliver decision support, goal setting, coaching, reminders or health‐related knowledge to consumers via smartphones, tablets, landlines, or mobile phones, using either telephones' touch‐tone keypad or voice recognition software. ATCS have the potential to transform modern healthcare systems by empowering consumers, changing their behaviours, improving clinical outcomes, and preventing disease. This systematic review evaluated the evidence on the effectiveness of ATCS interventions for improving a wide variety of health‐related outcomes related to preventive healthcare and the management of long‐term conditions.
Summary of main results
ATCS for preventive healthcare
Effectiveness of ATCS for improving immunisation uptake
The evidence suggests that ATCS (ATCS Plus, IVR, unidirectional) probably increase the uptake of immunisations in children compared with no calls, letters, or usual care (moderate certainty evidence). Compared with usual care, it probably slightly increases immunisation uptake in adolescents (moderate certainty evidence) and has uncertain effects on uptake in adults (very low certainty evidence) (Table 1). We considered results separately by population, as there was otherwise too high a degree of heterogeneity in pooled effect estimates. Subgroup analyses by type of ATCS were not possible due to the unequal number of studies in respective categories (ATCS Plus versus IVR versus unidirectional ATCS) and the small number of studies both within each comparison and overall. Although the evidence is promising for improving immunisation uptake, further studies may reduce the level of uncertainty associated with some of the results, particularly those in adults.
Effectiveness of ATCS for improving physical activity levels
Evidence for the effectiveness of ATCS in improving physical activity levels is of generally low certainty. Results suggest that multimodal/complex and ATCS Plus interventions may have little effect on several indices of body weight, metabolic markers or physical activity, whereas IVR interventions may improve several, but not all, measures of physical activity, when compared with usual care or other controls (Table 2). Although the evidence may indicate some promising effects for selected ATCS interventions, studies of higher methodological quality are needed to inform both practice and policy.
Effectiveness of ATCS for improving uptake of screening
The evidence suggests that for breast cancer screening, multimodal/complex interventions increase screening rates (high certainty evidence), whereas IVR or unidirectional ATCS interventions probably each have little or no effect (moderate certainty evidence) compared with control, usual care or enhanced usual care. For colorectal cancer screening, multimodal/complex interventions increase screening rates (high certainty evidence) compared with usual care, and IVR interventions probably improve screening rates at six months but not at later time points (moderate certainty evidence) when compared with control, usual care, or enhanced usual care. Unidirectional ATCS interventions probably have little or no effect on colorectal cancer screening rates (moderate certainty evidence) when compared with control. For cervical cancer, an ATCS Plus intervention probably slightly improves the rate of screening when compared with control (moderate certainty evidence), while for osteoporosis screening, a multimodal intervention may increase the uptake of screening compared with no intervention (low certainty evidence), but the effects of an ATCS Plus intervention are uncertain when compared with usual care (Table 3). These results suggest that more complex ATCS interventions (i.e. multimodal/complex interventions), may be more likely to improve outcomes related to breast cancer and colorectal cancer screening than less complex interventions (IVR and unidirectional ATCS). However, no trials directly tested these interventions against one another. Overall, the evidence is encouraging for the effectiveness of some (complex/multimodal) ATCS interventions for increasing screening uptake, and it seems unlikely that future trials will change the existing level of certainty.
Effectiveness of ATCS for reducing body weight
In adults, the evidence suggests that compared with various control, ATCS (multimodal/complex, ATCS Plus) may support slight weight loss (reduction in BMI or body weight), but effects of IVR were mixed (low certainty evidence) (Table 4). The effects of interventions on other clinical or behavioural measures in adults are mixed, and it is not clear whether adverse events may be associated with ATCS interventions, or not. In children, the evidence suggests that compared with control, ATCS interventions (ATCS Plus or IVR) probably have little effect on weight management assessed by BMI z‐scores or other proxy measures of weight management (moderate certainty evidence). For studies assessing the effects of ATCS on weight management, meta‐analysis was not possible due to the small number of studies and high degree of heterogeneity across studies. Overall, trials are needed to reduce the existing level of uncertainty related to the effects of ATCS interventions on weight management in both adults and children, and to investigate further any possible adverse events associated with ATCS interventions in this area.
Effectiveness of ATCS for reducing non‐attendance rates (appointment reminders)
The evidence suggests that compared with no calls, ATCS Plus interventions probably have little or no effect on attendance rates. IVR or unidirectional interventions may each improve attendance rates (either preventive healthcare or management of long‐term conditions), although the effects were somewhat inconsistent across time points (Table 5), and the evidence varied from high to low certainty. Further trials, which include economic modelling or cost‐effectiveness analyses, may reduce the level of uncertainty about the effects of the range of ATCS interventions for improving appointment attendance.
ATCS for managing long‐term conditions
Effectiveness of ATCS for improving adherence to medications or laboratory tests
The effects of ATCS on adherence to medications or laboratory tests provides the most general evidence across management of long‐term conditions; see Table 6. The evidence suggests that the effects of multimodal/complex interventions versus usual care or control are inconsistent, and the evidence was of variable certainty, so more research is necessary to draw firm conclusions. However, ATCS Plus interventions probably improve medication adherence slightly to moderately compared with usual care or control but probably have little effect on adherence to tests. IVR interventions probably slightly improve measures of medication adherence compared with control and probably improve adherence to tests. The evidence also suggests that IVR interventions probably slightly improve adherence to medications at six months but have little or no effect at longer time points when compared with usual care. However, it is worth noting that most results were based on studies of moderate certainty evidence, and the size of effects were variable. For unidirectional ATCS, the evidence suggests that compared with control, these interventions may have little effect or may improve adherence to medications to a small degree. The effects of ATCS interventions on clinical outcomes (blood pressure control, blood lipids, asthma control, therapeutic coverage) were inconsistent, and we generally found little or no effect for the interventions. However, only a small number of studies contributed clinical outcome data, and the evidence was of moderate to low certainty, meaning that further research assessing these outcomes is needed to more clearly determine health effects as well as behavioural (adherence) effects. None of the ATCS interventions were directly tested against one another. Overall, the evidence suggests that some ATCS interventions might have promising effects on medication or test adherence, but further high quality research is needed to better define the size of effects and to reduce uncertainty before such interventions might be considered for use as part of routine practice. Having said this, the company that conducted the largest RCT in this area finds value in and continues to place automated telephone refill reminders for medication.
Effectiveness of ATCS for reducing alcohol consumption
The evidence suggests that ATCS Plus interventions may have little or no effect on measures of alcohol consumption when compared with no intervention, usual care, or other interventions (cognitive–behavioural therapy or education/advice), although the certainty of the evidence was low in all cases. Similarly, IVR interventions may slightly improve some measures of alcohol consumption compared with no intervention or information provision, but the size of the effect is small, and the evidence of generally low certainty (Table 7). In this area, studies were too heterogeneous for statistical pooling, and further research seems likely to change the certainty of the evidence relating to the effects of ATCS interventions.
Effectiveness of ATCS for reducing severity of cancer symptoms
The evidence suggests that compared with usual care or control, multimodal/complex interventions probably reduce pain and depression at three months and beyond, although possibly to a smaller degree at later time points. ATCS Plus interventions may have little or no effect on symptoms (severity, distress or burden) or medication adherence, although the evidence was of mostly low certainty and in some studies the involvement of ATCS systems as part of usual care delivery may have prevented any effects of the intervention from being detected. Similarly, IVR may have little or no effect on severity of symptoms, compared with either control or ATCS Plus, although the evidence was of generally low certainty and based on few studies (Table 8). Further research in this area seems likely to change our certainty in the effects of using ATCS to try to alleviate cancer symptoms.
Effectiveness of ATCS for managing diabetes mellitus
The evidence suggests that, compared with usual care, ATCS interventions (ATCS Plus, IVR) may slightly reduce glycated haemoglobin levels and probably slightly improve diabetes‐related self‐management behaviours such as self‐monitoring of feet and blood glucose levels, but they may have little or no effect on weight monitoring or medication adherence or use, and they appear to have mixed effects on diet and physical activity levels (Table 9). ATCS Plus interventions may sometimes be more cost‐effective than usual care, but they may also influence healthcare use in ways whose impact is not yet fully understood. Overall, the evidence, although promising for some outcomes, was of low to moderate certainty. Future research, including studies that directly compare ATCS Plus and IVR interventions against one another, might reduce the existing uncertainties.
Effectiveness of ATCS for heart failure
Compared with usual care or usual community care, ATCS interventions (ATCS Plus, IVR) probably have little or no effect on hospitalisation for heart failure, all‐cause mortality or all‐cause hospitalisation. Effects on cardiac mortality are uncertain due to the very low certainty of the evidence for this outcome. Effects of ATCS on adverse events in this population are also uncertain due to the inconsistent findings of the two studies that specifically looked for adverse events (Table 10).
Effectiveness of ATCS for hypertension
Compared with usual care or enhanced usual care, ATCS interventions (multimodal/complex, ATCS Plus, IVR, unidirectional ATCS) may have little or no effect on blood pressure in people with hypertension. The evidence was of variable certainty (from low to moderate). Although for systolic blood pressure there was probably a small decrease with the use of ATCS, this was not confirmed by changes to diastolic blood pressure, which were negligible. ATCS interventions may have small positive effects on related outcomes including medication problems, depression symptoms, physical activity, and perceived health status, but little or no effect on medication adherence. The evidence is thus currently inconclusive for the main outcomes, and most results were based on low certainty evidence. Future trials might be considered to reduce the existing level of uncertainty in this area (Table 11).
Effectiveness of ATCS for smoking cessation
The evidence suggests that compared with various controls or usual care, ATCS interventions (multimodal/complex, ATCS Plus, IVR) may have little or no effect on maintenance of smoking abstinence; the evidence was of generally low certainty, and there was a moderate level of heterogeneity of the meta‐analysed studies. ATCS Plus interventions may increase abstinence at six months, but the effects of IVR and ATCS Plus at longer time points appear inconsistent. ATCS Plus may improve cessation programme support enrolment, with probably little or no effect on adherence to medications, but the certainty of the evidence was variable (moderate to low). See Table 12.
Overall completeness and applicability of evidence
We identified two studies from low‐income (Honduras/Mexico and India) and one from middle‐income (Taiwan) countries, and the remaining 129 studies were conducted in high‐income countries (the UK, the USA, Australia, Norway, France, Greece, Italy, Sweden, and Canada). Only 14 studies took place in the 1990s, while the remaining 118 date from 2000 onwards. In most studies, information about the theoretical model underpinning the ATCS intervention was missing. In a similar vein, a description of the call's content was often insufficient, making it difficult to analyse, interpret, or replicate the findings in any depth, or to replicate the component studies.
In terms of practical application of the ATCS interventions, a large proportion of studies did not report whether or not participants received instructions on how to use the system. In several trials, it was unclear whether patients or healthcare professionals initiated the calls or whether (or not) the participants used a telephone keypad to interact with the systems. Information about the intervention's duration, frequency and intensity; safety (adverse effects) and cost‐effectiveness; security arrangements; or speakers' features was frequently missing, too.
There are several possible advantages of ATCS systems. These include convenience, low cost, 24‐hour access, and participant anonymity, meaning that responses may be less prone to the influences of stigma and perceived social desirability (Phillips 2015; Schroder 2009; Szilagyi 2013). Previous studies have also reported that both patients and professionals report a high degree of satisfaction with ATCS systems (Abu‐Hasaballah 2007), which is consistent with our findings. The small number of studies assessing satisfaction or acceptability of ATCS systems reported that participants generally rated these aspects highly, which may add to the appeal of these systems in practice. ATCS systems may also provide a means to engage difficult‐to‐reach populations (Schroder 2009). However, some people with disabilities, such as severe hearing loss or difficulties with speech, may be unable to use such interventions or to engage with them fully, so researchers and practitioners should carefully consider the populations to which ATCS interventions might be best directed prior to implementation.
Included studies rarely reported adverse events associated with the delivery of ATCS interventions, such as information overload, preference for interactions with humans, or potentially worsened clinical or health‐related outcomes. These remain a major uncertainty in the evidence around the possible benefits and harms of this group of interventions as a whole and require assessment through future studies.
We realise that we have been unable to meet some of the review's objectives, including determining which intervention design components may contribute to positive behavioural change, or which type(s) of ATCS are most effective for preventive healthcare or the management of long‐term conditions. However, we considered subgroup analyses to be unfeasible because of the unequal distribution and insufficient number of studies in respective subgroups/categories and comparisons and because of the considerable heterogeneity of populations, interventions, comparator groups, and outcome measures used. Nevertheless, we managed to establish that in some instances complex/multimodal interventions appeared to be more effective than less complex ones, but this was observational in nature and varied across different conditions included in the review. This possible relationship between complexity of the ATCS intervention and effectiveness needs further investigation, possibly by unpacking and delineating the most active components and essential features of ATCS interventions. For instance, exploring whether the degree of interactivity of ATCS influences effectiveness in different contexts is one such avenue. Identifying features of ATCS interventions that are key to their effectiveness for different purposes will also be important. Such questions might include considering whether and how preventive interventions (e.g. screening and immunisation reminders) are different from interventions used for managing long‐term conditions. The role and purposes of ATCS interventions in these latter contexts may encompass a wider range of individual purposes, over variable time periods (e.g. episodic, continuous) and may require a greater degree of individual tailoring to meet the needs of users.
Direct comparisons between different ATCS types would also be helpful in better understanding the effects of such interventions and to more clearly identify essential versus non‐essential components and features. This review included studies that used complex/multimodal interventions as well as a wide variety of comparisons, including similar ATCS interventions against one another (e.g. Cleeland 2011; Peng 2013; Pinto 2002; Spoelstra 2013). While this increases the generalisability of the findings, much remains to be determined despite the large body of recent literature assembled here.
We acknowledge that this review's scope is very broad (both preventive healthcare and management of long‐term conditions), and one of its strengths is that it is the first systematic and rigorous attempt to organise and evaluate the evidence of effectiveness on this topic area. We also acknowledge that there are many other potential ways of structuring or organising this review, such as according to the type of intervention (rather than condition), by the types of outcomes, or with an exclusive focus on preventive healthcare (rather than in combination with management of long‐term conditions). We will consider factors such as these when planning the update of this review, and we will also assess the usefulness of different theoretical frameworks and/or logic models as a basis for structuring or informing the review at a general level.
Quality of the evidence
We assessed the quality of evidence using the GRADE system and presented findings in Table 6 for the comparison that provides the most general evidence across long‐term conditions, and 'Summary of findings tables' 1 to 5 and 7 to 12 for additional comparisons. We found the certainty of evidence for most outcomes to be low, but this was variable (ranging from very low to high). It was predominantly low in certain subcategories of conditions, including adherence to medications or laboratory tests, alcohol consumption, appointment reminders, diabetes mellitus, physical activity and smoking, and it was predominantly of moderate quality for screening and cancer symptoms. In other cases such as immunisation, heart failure, hypertension, and weight management, the quality of the evidence varied considerably by outcome.
Reasons for downgrading the evidence most commonly pertained to the risk of bias (i.e. methodological limitations of included studies): we downgraded once where there was mostly an unclear risk of bias across all seven domains of the tool or when there was a high risk of selection bias and attrition bias, and we downgraded twice if there was a high risk of bias for multiple domains of randomisation; allocation concealment; or attrition, performance, or detection bias. We also downgraded once if the results were from a single study for a particular comparison/outcome (unless that study was large, precise, and generally without major limitations assessed by risk of bias). Other reasons for downgrading the evidence included inconsistency (we downgraded once where there was high heterogeneity/differences in direction of effect); indirectness (we downgraded once for one outcome only ‐ physical activity levels where there were differences in population and comparisons used); and imprecision (we downgraded once if the sample size was small or the effect estimate had wide confidence intervals that gave different messages about the effects of the intervention at the upper and lower limits of the confidence interval). On the whole, we considered the randomisation procedure to be adequate in 53% of the studies and allocation concealment in 23%. We considered outcome data to be complete in 56% of the studies and selective reporting to carry a low risk in 29.5%. There were no baseline imbalances (indicating a low risk of 'other' bias) in 50% of the studies. However, as with many behavioural interventions, almost 83% of the studies either did not blind both participants and personnel, or they abandoned or inadequately described blinding, undermining our confidence that measures taken by the study were adequate to prevent knowledge of who received the intervention. Similarly, 83% of the studies were at unclear or high risk for blinding of outcome assessors, and while this may in many cases be more possible to achieve, even with behavioural interventions, only a minority of studies clearly performed this step.
Overall, the high potential for bias in many of the included studies (and so within subcategories of the review) reduces our certainty in the results (reflected by the GRADE ratings) and by extension our inferences from the findings. While this review provides the first rigorous, systematic assessment of the evidence of effectiveness across this broad area, the findings are constrained by the quality of the evidence in many of the identified subcategories. Future updates of this review may elect to focus on areas in which high(er) quality evidence exists, and they may include enough accumulated studies within particular topic subcategories to enable exploration of the robustness of effects through sensitivity analyses or other analytic approaches.
Potential biases in the review process
We minimised potential biases in the review process by strictly adhering to the guidelines outlined by Higgins 2011. Specifically, we believe that we have utilised a comprehensive search strategy; and in all cases, two reviewers independently assessed eligibility criteria, extracted data, assessed risk of bias, and used the GRADE criteria to critically evaluate the quality of the evidence. However, it is possible that we have missed some relevant studies through our search processes. We also acknowledge that some of the review objectives have not been met, including the exploration of interventional design components that may contribute to positive behavioural change of consumers. This was due primarily to the unequal number and distribution of studies in respective categories (unidirectional, IVR, ATCS Plus, multimodal/complex interventions), rather than to deliberate decisions not to conduct such planned analyses. We also made the decision to present in 'Summary of findings' tables only those condition areas for which we had identified four or more studies for inclusion. We made this decision purely due to the size and scope of the review, not based on the findings of the studies. We do not believe that this approach has introduced bias to the review but report our methods in the interests of transparently documenting our decisions as researchers.
Agreements and disagreements with other studies or reviews
A review by Lieberman 2012 recommended that IVR‐based treatment approaches be employed by multidisciplinary clinics and practitioners who treat patients with chronic pain, as these technologies are clinically beneficial, versatile, and cost‐effective. Although that review was not systematic and therefore more susceptible to bias, it is generally in line with the findings of the present review. Similarly, Corkrey 2002b concluded that IVR shows promise in a number of health areas. They stressed the importance of further research into certain unexplored areas such as systematic evaluation of voice, multilingual interfaces, touch‐phone prevalence, survey response rates, sample bias, use by the elderly, and acceptability. Piette 2012c suggested that automated telephone monitoring and self‐care support calls can improve some outcomes of chronic disease management, such as glycaemic control and blood pressure control, in low‐ and middle‐income countries. Similar Cochrane reviews investigated the effectiveness of mobile phone messaging (SMS, MMS) for preventive healthcare (Vodopivec‐Jamsek 2012; Gurol‐Urganci 2013), telephone‐ or mobile‐delivered interventions for preventing HIV infection in HIV‐negative persons (Van Velthoven 2013), and reminder systems to improve patient adherence to tuberculosis clinic appointments (Liu 2014). All reviews found limited evidence to support the effectiveness of those interventions.
Authors' conclusions
Implications for practice.
Automated telephone communication systems have the potential to play an important role in the modern healthcare. The available evidence suggests that these systems have potentially important benefits. Furthermore, these systems typically have a high degree of customisation and adaptability to providers' and patients' needs and requirements, and technology (e.g. voice recognition) is improving rapidly. Several types of ATCS have been identified; however, there is insufficient evidence to determine which is most effective across all health areas. Several practical matters need to be considered including data protection and confidentiality of telephone numbers, participants' age (preference of smartphones versus landlines), language and dialect/ethnical‐cultural differences, staffing (including health personnel or computer programmers), overall programme costs including service providers, seamless integration with electronic medical records, storage (and back‐ups), and server use. When interpreting the findings of this systematic review, practitioners need to consider other factors such as participants' health state or geographical location, or features of the intervention such as the frequency, duration, and intensity of delivery, which may be related to the aims of the communication. Automated telephone communication systems that promote health and disease prevention may have a useful application when uptake of those services or interventions is low. Due to several gaps in the evidence base, we currently recommend the use of ATCS for managing long‐term conditions only in an evaluative context, as these conditions typically have multidimensional aetiology and pathogenesis and require more complex therapeutic solutions. In such contexts, the use of ATCS may need to be embedded within systems of care and consider both benefits and potential harms associated with automating communication between healthcare professionals and patients. The certainty of evidence ranged from very low to high, and it was low for the comparison that provided the most general evidence across management of long‐term conditions, meaning that future research is likely to impact on the findings presented here.
Implications for research.
This is a promising and growing area of research, as reflected by our inclusion of over 100 randomised trials in a decade involving over 4 million participants. Our growing understanding of behaviour change psychology and human‐technology interactions offers new avenues to further explore the (cost‐)effectiveness, acceptability and also safety/adverse‐effects of ATCS interventions. There are many potential applications of this innovative technology, and the role of ATCS will grow with the trend to replace or supplement human interventions with technology. Future research could focus on the potential incorporation of visual/video communication (e.g. from an avatar) into automated voice messages, thereby making the intervention even more interactive. Delineating the most active components of, or performing direct comparisons between, complex/multimodal interventions and unidirectional ATCS in various health conditions might prove beneficial. Future research in the area may also look at different certainties of evidence, or different organisational structures, and these could be informed by theoretical models to better understand the mechanism of action of this range of interventions on a wide variety of health outcomes.
Acknowledgements
We would like to thank Igor Wei, John Kis‐Rigo, and Caroline Pang Soo Ling for their invaluable support with devising the search strategy for this review. We also acknowledge the referees and the editors for their valuable comments and suggestions. We are grateful to Dr Monika Semwal for initially validating the data extraction form and to Dr Ram Bajpai for his statistical and methodological inputs. We also thank Dr Simon Lewin for his generous role in validating the iCAT_SR tool, Professors Azeem Majeed from Diabetes Research Network and Rifat Atun for their contributions, Dr Nami Minorikawa for writing the initial protocol and designing the initial data extraction form, and Dr Lucinda Cash‐Gibson for revising the protocol and refining the data extraction form.
Appendices
Appendix 1. CENTRAL search strategy
#1 (automat* or interactive*) near/5 (telephon* or phone* or voice* or hotline* or "hot line*")
#2 voice next (response or recognition or messag* or system* or technolog*)
#3 speech‐recognition
#4 computer* near/2 (telephon* or phone*)
#5 touch‐tone
#6 (prerecorded or pre‐recorded) and (telephon* or phone* or voice* or hotline* or "hot line*" or call or calls or message*)
#7 automat* next (call* or answer*)
#8 answering next (service* or machine*)
#9 {or #1‐#8}
#10 (automat* or computer*) and (intervention* or counsel* or advice* or advis* or educat* or remind* or messag* or service* or support or appointment*)
#11 (telephon* or phone*) near/5 (system or technology)
#12 (telephone* or phone or phones or teleconsultation* or hotline* or answering‐service*):kw,ti
#13 (#10 or #11) and #12
#14 #9 or #13 in Trials
Appendix 2. MEDLINE (Ovid) search strategy
1. ((automat* or interactive*) adj5 (telephon* or phone? or voice* or hotline* or hot line*)).ti,ab,kw.
2. (voice adj (response or recognition or messag* or mail* or service* or system* or technolog*)).ti,ab,kw.
3. speech recognition software/
4. (computer* adj3 (telephon* or phone?)).ti,ab,kw.
5. touch tone.ti,ab,kw.
6. answering services/
7. ((prerecorded or pre‐recorded) and (telephon* or phone? or voice* or hotline* or hot line* or call* or messag*)).ti,ab,kw.
8. (automat* adj (call* or answer*)).ti,ab,kw.
9. (answering adj (service* or machine*)).ti,ab,kw.
10. or/1‐9
11. ((automat* or computer*) and (intervention* or counsel* or advice* or advis* or educat* or remind* or messag* or service* or support or appointment*)).ti,ab,kw.
12. ((telephon* or phone?) adj5 (system or technology)).ti,ab,kw.
13. 11 or 12
14. exp telephone/ or hotlines/
15. 13 and 14
16. 10 or 15
17. randomized controlled trial.pt.
18. controlled clinical trial.pt.
19. random*.tw.
20. placebo*.tw.
21. drug therapy.fs.
22. trial.tw.
23. groups.ab.
24. clinical trial.pt.
25. evaluation studies.pt.
26. research design/
27. follow up studies/
28. prospective studies/
29. cross over studies/
30. comparative study.pt.
31. (experiment* or intervention*).tw.
32. (pre test or pretest or post test or posttest).tw.
33. (preintervention or postintervention).tw.
34. time series.tw.
35. (cross over or crossover or factorial* or latin square).tw.
36. (assign* or allocat* or volunteer*).tw.
37. (control* or compar* or prospectiv*).tw.
38. (impact* or effect? or chang* or evaluat*).tw.
39. or/17‐38
40. 16 and 39
Appendix 3. Embase (Ovid) search strategy
1. ((automat* or interactive*) adj5 (telephon* or phone? or voice* or hotline* or hot line*)).ti,ab,kw.
2. (voice adj (response or recognition or messag* or mail* or service* or system* or technolog*)).ti,ab,kw.
3. automatic speech recognition/
4. IVR system/
5. (computer* adj3 (telephon* or phone?)).ti,ab,kw.
6. touch tone.ti,ab,kw.
7. ((prerecorded or pre‐recorded) and (telephon* or phone? or voice* or hotline* or hot line* or call* or messag*)).ti,ab,kw.
8. (automat* adj (call* or answer*)).ti,ab,kw.
9. (answering adj (service* or machine*)).ti,ab,kw.
10. or/1‐9
11. ((automat* or computer*) and (intervention* or counsel* or advice* or advis* or educat* or remind* or messag* or service* or support or appointment*)).ti,ab,kw.
12. ((telephon* or phone?) adj5 (system or technology)).ti,ab,kw.
13. 11 or 12
14. telephone/ or teleconsultation/
15. 13 and 14
16. 10 or 15
17. randomized controlled trial/
18. controlled clinical trial/
19. single blind procedure/ or double blind procedure/
20. crossover procedure/
21. random*.tw.
22. trial.tw.
23. placebo*.tw.
24. ((singl* or doubl*) adj (blind* or mask*)).tw.
25. (experiment* or intervention*).tw.
26. (pre test or pretest or post test or posttest).tw.
27. (preintervention or postintervention).tw.
28. (cross over or crossover or factorial* or latin square).tw.
29. (assign* or allocat* or volunteer*).tw.
30. (control* or compar* or prospectiv*).tw.
31. (impact* or effect? or chang* or evaluat*).tw.
32. time series.tw.
33. or/17‐32
34. 16 and 33
Appendix 4. PsycINFO (Ovid) search strategy
1. ((automat* or interactive*) adj5 (telephon* or phone? or voice* or hotline* or hot line*)).ti,ab,id.
2. (voice adj (response or recognition or messag* or system* or technolog*)).ti,ab,id.
3. automated speech recognition/
4. (computer* adj2 (telephon* or phone?)).ti,ab,id.
5. touch tone.ti,ab,id.
6. ((prerecorded or pre‐recorded) and (telephon* or phone? or voice* or hotline* or hot line* or call* or message*)).ti,ab,hw,id.
7. (automat* adj (call* or answer*)).ti,ab,id.
8. (answering adj (service* or machine*)).ti,ab,id.
9. ((automat* or computer*) and (intervention* or counsel* or advice* or advis* or educat* or remind* or messag* or service* or support or appointment*) and (phone? or telephon*)).ti,ab,hw,id.
10. ((telephon* or phone?) adj3 (system* or technology)).ti,id.
11. or/1‐10
12. ("29" or "32" or "33" or "34" or "35").cc.
13. (health* or medic* or patient* or clinic* or hospital* or illness* or disease* or disorder* or therap* or physician* or doctor* or psychotherap* or psychiatr* or telemedic* or treatment* or counsel*).ti,ab,hw,id,jw.
14. 12 or 13
15. 11 and 14
16. random*.ti,ab,hw,id.
17. (experiment* or intervention*).ti,ab,hw,id.
18. trial*.ti,ab,hw,id.
19. placebo*.ti,ab,hw,id.
20. ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)).ti,ab,hw,id.
21. treatment effectiveness evaluation/
22. mental health program evaluation/
23. (pre test or pretest or post test or posttest).ti,ab,hw,id.
24. (preintervention or postintervention).ti,ab,hw,id.
25. (cross over or crossover or factorial* or latin square).ti,ab,hw,id.
26. (assign* or allocat* or volunteer*).ti,ab,hw,id.
27. (control* or compar* or prospectiv*).ti,ab,hw,id.
28. (impact* or effect? or chang* or evaluat*).ti,ab,hw,id.
29. time series.ti,ab,hw,id.
30. exp experimental design/
31. ("0430" or "0450" or "0451" or "1800" or "2000").md.
32. or/16‐31
33. 15 and 32
Appendix 5. CINAHL (Ebsco) search strategy
| S27 | s26 |
| S26 | s10 and s25 |
| S25 | S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 |
| S24 | AB "time series" or TI "time series" |
| S23 | AB ("pre test" or pretest or "post test" or posttest or preintervention or postintervention) or TI ("pre test" or pretest or "post test" or posttest or preintervention or postintervention) |
| S22 | TI (singl* or doubl* or tripl* or trebl*) and TI (blind* or mask*) |
| S21 | AB (singl* or doubl* or tripl* or trebl*) and AB (blind* or mask*) |
| S20 | AB (random* or trial or placebo* or assign* or allocat* or volunteer* or factorial* or experiment* or control* or compar* or intervention* or chang* or evaluat* or impact* or effect?) or TI (random* or trial or placebo* or assign* or allocat* or volunteer* or factorial* or experiment* or control* or compar* or intervention* or chang* or evaluat* or impact* or effect?) |
| S19 | PT Clinical Trial |
| S18 | MH Quasi‐Experimental Studies+ |
| S17 | MH Quantitative Studies |
| S16 | MH Placebos |
| S15 | MH Crossover Design |
| S14 | MH Comparative Studies |
| S13 | MH Random Assignment |
| S12 | MH Experimental Studies+ |
| S11 | "randomi?ed controlled trial" or PT randomized controlled trial |
| S10 | s1 or s2 or s3 or s4 or s5 or s6 or s7 or s8 or s9 |
| S9 | (telephon* or phone*) N3 (system or technology) |
| S8 | ((automat* or computer*) and (intervention* or counsel* or advice* or advis* or educat* or remind* or messag* or service* or support or appointment*)) and MW (phone* or telephon* or teleconsultation* or hotline* or answering‐service*) |
| S7 | answering N1 (service* or machine*) |
| S6 | automat* N1 (call* or answer*) |
| S5 | (prerecorded or pre‐recorded) and (telephon* or phone* or voice* or hotline* or "hot line*" or call or calls or message*) |
| S4 | computer* N2 (telephon* or phone*) |
| S3 | "speech recognition" |
| S2 | voice N1 (response or recognition or messag* or system* or technolog*) |
| S1 | (automat* or interactive*) N5 (telephon* or phone* or voice* or hotline* or "hot line*") |
Appendix 6. Web of Science search strategy
| # 11 | #9 and #10 Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 10 | TS=(health* or *medic* or patient* or clinic* or hospital* or illness* or disease* or disorder* or *therap* or physician* or doctor* or psychiatr* or treatment* or counsel*) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 9 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 8 | TS=(touch‐tone) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 7 | TS=(answering near/1 (service* or machine*)) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 6 | TS=(automat* near/1 (call* or answer*)) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 5 | TS=((prerecorded or pre‐recorded) and (telephon* or phone* or voice* or hotline* or "hot line*" or call or calls or message*)) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 4 | TS=("speech recognition" and (software or automat* or interactive*)) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 3 | TS=(computer* near/2 (telephon* or phone*)) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 2 | TS=(voice near/1 (response or recognition or messag* or system* or technolog*)) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
| # 1 | TS=((automat* or interactive*) near/5 (telephon* or phone* or voice* or hotline* or "hot line*")) Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH |
Appendix 7. GLOBAL HEALTH (Ebsco) search strategy
S1 ((automat* or interactive*) N5 (telephon* or phone? or voice* or hotline* or hot line*))
S2 (voice N3 (response or recognition or messag* or mail* or service* or system* or technolog*))
S3 DE computer software AND (speech or voice) N3 recognition*
S4 (computer* N3 (telephon* or phone?))
S5 TX "touch tone"
S6 TX "answering service*
S7 ((prerecorded or pre‐recorded) and (telephon* or phone? or voice* or hotline* or hot line* or call* or messag*))
S8 (automat* N3 (call* or answer*))
S9 (answering N3 (service* or machine*))
S10 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9
S11 ((automat* or computer*) and (intervention* or counsel* or advice* or advis* or educat* or remind* or messag* or service* or support or appointment*))
S12 ((telephon* or phone?) N5 (system or technology)).
S13 S11 OR S12
S14 DE "telephones"
S15 TX "hotlines" or "hot?lines" or "hot lines"
S16 S13 AND (S14 OR S15)
S17 S10 AND S16
S18 DE randomized controlled trials
S19 SU controlled clinical trial* or TX control* clinic* N1 trial*
S20 TX random*
S21 TX placebo*
S22 DU drug therapy
S23 TX trial
S24 AB groups
S25 SU clinical trial* or TX clinic* N1 trial*
S26 TX "evaluation stud*"
S27 TX "research design*"
S28 DE follow up or TX "follow up stud*"
S29 TX "prospective stud*"
S30 TX "cross over stud*"
S31 TX "comparative stud*"
S32 TX (experiment* or intervention*)
S33 TX (pre test or pretest or post test or posttest)
S34 TX (preintervention or postintervention)
S35 TX "time series"
S36 TX (cross over or crossover or factorial* or latin square)
S37 TX (assign* or allocat* or volunteer*)
S38 TX (control* or compar* or prospectiv*)
S39 TX (impact* or effect? or chang* or evaluat*)
S40 S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39
S41 S17 AND S40
Appendix 8. WHOLIS search strategy
words or phrase "(automat* or interactive*) N4 (telephon* or phone* or voice* or hotline* or "hot line*")" OR words or phrase "voice N1 (response or recognition or messag* or system* or technolog*)" OR words or phrase "speech recognition" OR words or phrase "computer* N1 (telephon* or phone*)" OR words or phrase "touch tone" or automat* N1 (call* or answer*)" OR words or phrase "prerecorded or pre‐recorded and telephon* or phone* or voice* or hotline* or "hot line*" or call or calls or message*" OR words or phrase "answering N1 (service* or machine*)"
Appendix 9. Trial registers (keywords used)
Automated OR Interactive OR Telephone OR Communication OR speech recognition OR voice recognition OR prerecorded OR pre‐recorded OR answering OR service OR machine AND randomised OR randomized
Appendix 10. Grey literature (keywords used)
Automated telephone calls OR interactive telephone calls OR computer generated calls OR pre‐recorded calls OR speech recognition OR voice recognition
Appendix 11. Abbreviations and glossary terms
| ATCS | automated telephone communication system |
| AUDIT | Alcohol Use Disorders Identification Test |
| BMI | body mass index |
| CBA | control before and after |
| HR | hazard ratio |
| HR‐QoL | health related‐quality of life |
| ITS | interrupted time series |
| IVR | interactive voice response |
| MD | mean difference |
| NS | not specified |
| OR | odds ratio |
| PE | percent effect |
| PIN | personal identification number |
| QoL | quality of life |
| r | Pearson's correlations coefficient |
| RCT | randomised controlled trial |
| RD | risk difference |
| RR | relative risk |
| SAMA | short‐acting muscarinic antagonist |
| SD | standard deviation |
| SEM | standard error of the mean |
| SF‐12/36 | 12/36 Item Short Form Survey |
| SMBG | self monitoring of blood glucose |
| SMD | standardised mean difference |
| TLC | telephone‐linked computer |
Appendix 12. Standardised wording to describe results
| Level (quality) of evidence |
Important benefit or harm |
Less important benefit or harm |
No important benefit/harm or null effect |
| High | improves* | improves slightly | little or no difference in [outcome] |
| Moderate | probably improves | probably improves slightly | probably little or no difference in [outcome] |
| Low | may improve | may improve slightly | may have little or no difference in [outcome]** |
| Very low | We are uncertain whether [intervention] improves [outcome] | ||
| No events or rare events | Use comments in SoF table in a plainer language or summarise the results | ||
| No studies | No studies were found that looked at [outcome] | ||
Appendix 13. Quality of the evidence (GRADE)
| Condition | Study | Notes | Overall quality rating |
| PREVENTIVE HEALTHCARE | |||
| Alcohol misuse | Tucker 2012 | Downgrade −1 risk of bias as unclear on allocation concealment, high risk of attrition bias. Also −1 as single study, relatively small (N < 200) |
Low |
|
Immunisation Children ATCS Plus, IVR, unidirectional vs no calls, letters, or usual care |
Dini 2000 | Risk of bias rated unclear, including allocation concealment; −1 for all domains Large sample (N > 1200) |
Overall GRADE Risk of bias largest study at higher risk; downgrade −1 overall Imprecision okay, CIs fairly confined, large total sample Inconsistency okay; all CIs overlap, some variability at CI ends (2 smallest studies) Indirectness okay Publication bias okay Moderate |
| LeBaron 2004 | Risk of bias −1 as unclear rating on allocation concealment, and high on performance bias | ||
| Lieu 1998 | Risk of bias −1 as unclear on randomisation and allocation concealment. Fairly large sample (N > 700), although CIs cross the line of no effect this is a fairly small effect size |
||
| Linkins 1994 | Risk of bias ‐ randomisation and others high risk; allocation concealment unclear, −2 Sample size N > 8000 |
||
| Stehr‐Green 1993 | Risk of bias all rated unclear, including allocation concealment; −1 Sample N ˜ 230 |
||
|
Immunisation Children Unidirectional vs no calls |
Franzini 2000 | Risk of bias all rated unclear, including allocation concealment; −1 Sample size > 1100 Note unit of analysis error (cluster RCT): data unadjusted for clustering, effects estimates may be overly precise (−1) |
Low |
| Adolescents Unidirectional ATCS vs usual care |
Szilagyi 2006 | Risk of bias all okay, low risk; do not downgrade Sample size good, N ˜ 3000 |
Overall GRADE Risk of bias −1 some risk of bias due to unclear allocation concealment, attrition bias in 1/2 studies Imprecision: okay, good overall sample size and effect estimate fairly precise Inconsistency: heterogeneity fine Indirectness Publication bias Moderate |
| Szilagyi 2013 | Risk of bias −1 as unclear on allocation concealment and attrition bias Sample size good, N ˜ 4100 |
||
| Adults Unidirectional ATCS vs no calls or health information |
Hess 2013 | Risk of bias−1 as unclear on allocation concealment and attrition bias; high risk on other bias (baseline imbalances) Very large sample (N ˜ 11,000), but unadjusted for clustering. Once adjusted (approximate sample size), CIs wide and give different messages about direction of effects |
Overall GRADE Risk of bias −1 as unclear on allocation concealment in 1/2 studies, unclear an attrition bias both studies, high risk other bias one study; so some possibility of bias Imprecision: possibly problematic, although large N overall CIs are wide −1 Inconsistency: heterogeneity −1 Indirectness Publication bias Very low |
| Nassar 2014 | Risk of bias not downgraded as randomisation and allocation concealment were adequate Very small sample size (N = 50) |
||
| Physical activity | Dubbert 2002 | Risk of bias −1 as unclear risk on randomisation and allocation concealment Results from a single small (N < 200) study −1 |
Low |
| Morey 2009 | Risk of bias no downgrading −1 for results from a single study |
Moderate | |
| Morey 2012 | Risk of bias −1 as rated unclear on randomisation Results based on single study −1 |
Low | |
| David 2012 | Risk of bias−1 as both randomisation and allocation concealment unclear Small sample size (N = 71); results from a single small study −1 |
Low | |
| Pinto 2002 | Risk of bias −1 as randomisation and allocation concealment both unclear −1 for results from a single study |
Low | |
| Jarvis 1997 | Risk of bias −1 as unclear for randomisation, high risk for attrition bias Small sample (N < 100) −1 single small study |
Low | |
| King 2007 | Risk of bias −1 as allocation concealment unclear −1 for single small study contributing to the results |
Low | |
| Sparrow 2011 | Risk of bias −1 as allocation concealment unclear −1 for single small study |
Low | |
|
Screening breast cancer Multimodal versus usual care |
Fiscella 2011 | Risk of bias no downgrading as all key items rated low risk Imprecision okay |
Overall GRADE Risk of bias okay, no downgrading Imprecision may be an issue: total number of events is ˜ 130. CIs bit wide but both give messages of appreciable benefit, consistent. Do not downgrade. Inconsistency: both have effects in the same direction; CIs overlap; I2 fine Indirectness ‐ okay Publication bias High Important effect size |
| Hendren 2014 | Risk of bias no downgrading as all key items rated low risk Imprecision okay |
||
| IVR vs enhanced usual care | DeFrank 2009 | Risk of bias −1 as randomisation, allocation concealment and blinding all unclear Large sample size (N ˜ 3500) imprecision seems okay |
Overall GRADE Risk of bias −1 as both studies allocation concealment rated unclear, other items in 1/2 studies unclear. Some risk of bias. Imprecision may be an issue: total number of events is N < 100; sample size is N ˜ 2500, CIs are small. Do not downgrade. Inconsistency: both have effects in the same direction; CIs overlap; I2 fine Indirectness ‐ okay Publication bias Moderate |
| Phillips 2015 | Risk of bias did not deduct any points as although allocation concealment was rated unclear all other items were rated as low risk Reasonable sample size (N > 650), some imprecision |
||
| Unidirectional ATCS plus letter vs letter | Fortuna 2014 | Risk of bias no rating down as all key items are low risk Single study but large and with no real potential risk of bias; however confidence intervals are wide and include both potential harm and benefit; −1 for imprecision |
Moderate |
|
Colorectal cancer screening Multimodal/ complex vs usual care |
Baker 2014 | Risk of bias −1 for unclear allocation concealment Not −1 for single study since all 3 are combined for an overall statement of effects ‐ GRADED together |
Overall GRADE Risk of bias no major risk Imprecision okay (approx N > 1250 combined studies). Effects are consistently positive; CIs tight and give same overall message. Inconsistency: no problems, individual study estimates are consistent, I2 low. Indirectness okay Publication bias High Important effect size |
| Fiscella 2011 | Risk of bias no downgrading as all key items rated low risk Imprecision okay |
||
| Hendren 2014 | Risk of bias no downgrading as all key items rated low risk Imprecision okay |
||
| IVR vs control | Durant 2014 | Risk of bias −1, unclear on key domains except other bias (high risk) Very large sample > 45,000; do not downgrade for results coming from single study |
Moderate |
| IVR vs usual care Combined these: comparable comparison, outcome and timing (other two studies in this group not combined as longer time points approx 9 and 12 months) |
Cohen‐Cline 2014 Colorectal cancer screening rate at 6 months |
Risk of bias −1 all items rated unclear | Overall GRADE Risk of bias −1 overall as allocation concealment unclear (and blinding may be problematic) Imprecision: combined samples are large (N > 15,000); estimates fairly precise Inconsistency ‐ estimates are very close; I2 fine Indirectness Publication Moderate Important effect size |
|
Mosen 2010 Faecal occult blood testing at 6 months |
Risk of bias −1 as allocation concealment unclear, also all blinding unclear | ||
| Combined these two as comparable comparison, comparable outcome and timing (approx 9 and 12 months) |
Phillips 2015 Colorectal cancer screening within 36 weeks of randomisation (approx 9 months) |
Risk of bias ‐ did not deduct any points although allocation concealment was rated unclear all other items were rated low risk Reasonable sample size (N > 650), some imprecision |
Overall GRADE Risk of bias −1 overall as allocation concealment unclear in both studies (and blinding may be problematic) Imprecision: large sample size; CIs are close Inconsistency ‐ estimates are very close; I2 fine Publication Indirectness Moderate |
|
Simon 2010a Faecal occult blood testing within 12 months of intervention |
Risk of bias −1 as allocation concealment unclear, high risk for blinding (performance bias) imprecision seems okay, estimate is pretty tight and large (N > 20,000) |
||
| Unidirectional ATCS plus letter vs letter | Fortuna 2014 | Risk of bias no rating down as all key items are low risk Single study but large and with no real potential risk of bias; however CIs are wide and include both potential harm and benefit; −1 for imprecision |
Moderate |
|
Osteoporosis screening Multimodal/complex vs usual care |
Solomon 2007 | Risk of bias −1 as almost all items (including randomisation, allocation concealment and all blinding) were rated unclear Imprecision okay and sample size is okay as are CIs −1 for single study contributing to results |
Low |
| ATCS Plus vs usual care | Heyworth 2014 | Risk of bias −2 as high risk on randomisation and most of the rest unclear. think this is a less important effect (fairly small) Results based on a single study so −1 |
Very low |
| Cervical cancer screening | Corkrey 2005 | Risk of bias −1 as all items rated unclear Very large sample (N > 75,000); therefore do not downgrade for single study contributing to results |
Moderate |
| Stress management | Mahoney 2003 | Risk of bias no downgrading all low risk Imprecision (small N, large CIs relative to means); Results based on a single small study (N = 100) −1 |
Moderate |
| Substance abuse | Aharonovich 2012 | Risk of bias no downgrading most criteria low risk. Blinding unclear/ high risk might be a slight problem Tiny sample, downgrade −1 as results based on single small study |
Moderate |
|
Weight management ATCS vs usual care Adults – BMI (pooled 3 studies) |
Bennett 2012 | — | Overall GRADE Risk of bias allocation concealment unclear in all 3 studies; randomisation unclear in 1; probably some risk with blinding problems (both Bennett studies rated as high risk of performance bias) Rate down −1 Imprecision: reasonable sample size (N ˜) 650; CIs not too wide Dowgraded −1 on inconsistency; I2 = 69% Publication Indirectness Low Less important effect (small) |
| Bennett 2013 | For adverse effects, single study outcomes, downgraded as results were obtained from a single small study at potential risk of bias (−2). | ||
| Goulis 2004 | — | ||
| Weight loss adult ATCS+ vs control |
Vance 2011 | Risk of bias downgrade for −1 unclear on all items Downgrade −1 as results based on single small study |
Low |
| Weight loss adult IVR vs control |
Estabrooks 2008 | Risk of bias −1. Most items are low risk, but high risk of performance bias Downgrade −1 as results based on single very small study (N = 77) |
Low |
| Goulis 2004 | Downgrade −1 as results based on single small study; risk of bias no downgrading | Moderate | |
| Weight loss children ATCS Plus vs control |
Estabrooks 2009 | Risk of bias no downgrading Downgrade −1 as results based on single small study (N = 220) |
Moderate |
| Weight loss children IVR vs control |
Wright 2013 | Risk of bias no downgrading; key items are rated as low risk However results based on small (N = 50 pairs) single study, downgrade −1 |
Moderate |
| Blood pressure ATCS vs usual care |
Bennett 2012 | Risk of bias okay not to downgrade (allocation concealment is unclear but other key items are low risk) Results based on single study, (N = 220) so −1 |
Moderate |
| ATCS Plus vs control | Vance 2011 | Risk of bias downgrade for −1 unclear on all items Rate down −1 further for results based on single small study |
Low |
| EITHER PREVENTIVE HEALTHCARE OR MANAGEMENT OF LONG‐TERM CONDITIONS | |||
|
Reducing non‐attendance rates Unidirectional ATCS vs usual care Considered together although not meta‐analysed: same outcome at same time point 1 month |
Dini 1995 Non‐attendance rate |
Risk of bias −2 as high risk on randomisation, unclear on allocation concealment and others | Overall GRADE Risk of bias −2 high risk on randomisation, unclear on allocation concealment and others Imprecision okay Inconsistency ‐ heterogeneity good Indirectness Publication bias? Low |
|
Tanke 1994 Non‐attendance rate |
Risk of bias −2 high risk on randomisation, unclear on allocation concealment and others | ||
| 3 days Unidirectional ATCS vs usual care |
Tanke 1997 Return of tuberculosis test |
Risk of bias −1 all items rated unclear Single study contributing to results −1 |
Low |
| Later time point Unidirectional ATCS vs control |
Maxwell 2001 Non‐attendance rate 6 weeks |
Risk of bias −1 almost all unclear Do not downgrade for single study contributing to results as large sample (N > 2000) |
Moderate |
| Later time point Unidirectional ATCS vs control |
Reekie 1998 Non‐attendance rate 2 months |
Risk of bias −1 all unclear Do not downgrade for single study contributing to results as large sample (N = 1000) |
Moderate |
| ATCS Plus vs nurse |
Griffin 2011 Appointment non‐attendance and preparation non‐adherence |
Risk of bias −1 almost all rated unclear Results from a single study, but large sample (N > 3600); do not downgrade |
Moderate |
| IVR vs none |
Parikh 2010 Non‐attendance rate |
Risk of bias do not downgrade, mostly low risk Results from a single study – but large sample. Do not downgrade |
High |
| MANAGEMENT OF LONG‐TERM CONDITIONS | |||
|
Illicit drugs addiction ATCS Plus vs usual care |
Moore 2013 | Risk of bias downgrade −1 (all unclear) Single very small (N = 36) study contributing to results −1 |
Low |
|
Alcohol consumption ATCS vs control Different outcomes for these 3 studies, can't combine |
Helzer 2008 Weekly alcohol |
Risk of bias −1 as mostly unclear, including randomisation and allocation concealment Single study contributing to results −1 |
Low |
|
Mundt 2006 Drinking days |
Risk of bias −1 unclear on randomisation and allocation concealment, and others; high risk of attrition bias Single study contributing to results −1 |
Low | |
|
Rose 2015 No.drinks/drink days |
Risk of bias −1 as mostly unclear Single study contributing to results −1 |
Low | |
| ATCS vs another intervention |
Hasin 2013 No. drinks/drink day, 2 and 12 months |
Risk of bias−1 as allocation concealment rated unclear And high risk performance bias Single study contributing to results (N = 254), −1 |
Low |
|
Litt 2009 Proportion of days abstinent at 12 weeks, number of heavy drinking days, coping or drinking problems, continuity of abstinence |
Risk of bias −1 as allocation concealment and attrition bias unclear, and high risk of performance bias Single study contributing to results −1 |
Low | |
| IVR vs control (none) 2 studies but different outcome measures so not combined |
Andersson 2012 AUDIT scores |
Risk of bias −1 as all rated unclear Do not further downgrade for single study contributing to results as large sample (N > 1400) |
Moderate |
|
Simpson 2005 Drinking habits, craving, post‐traumatic stress disorder |
Risk of bias −1 as randomisation and allocation concealment rated unclear. Single study contributing to results −1 |
Low | |
| IVR vs control (information) | Rubin 2012 | Risk of bias −1 as almost all rated unclear Single study contributing to results −1 |
Low |
|
Asthma Different interventions, different outcomes, cannot combine |
Vollmer 2006 ATCS Plus vs usual care |
Risk of bias −1 as unclear on randomisation and allocation concealment Single study contributing to results −1 |
Low |
|
Xu 2010 IVR vs usual care |
Risk of bias −1 as unclear on allocation concealment, while low risk for some many others are unclear Single study contributing to results −1 |
Low | |
| Cancer |
Kroenke 2010 Complex vs usual care |
Risk of bias okay as while usual care on allocation concealment other key items are low risk Single study contributing to results −1 |
Moderate |
| ATCS Plus versus usual care via ATCS Similar intervention and comparison groups, different outcomes/ measures/ time points so can't assess together |
Cleeland 2011 ATCS Plus vs IVR monitoring |
Risk of bias −1 as usual care on allocation concealment and while low risk for some many others are unclear Single study contributing to results −1 (small N < 100) |
Low |
|
Mooney 2014 ATCS Plus vs IVR attention control |
Risk of bias okay, randomisation and allocation concealment low risk; attrition was unclear but relatively balanced numbers Single study contributing to results −1 |
Moderate | |
|
Yount 2014 ATCS Plus vs IVR |
Risk of bias −1 as unclear on allocation concealment and while low risk for some many others unclear, also high risk of performance bias. Single study contributing to results −1 |
Low | |
|
Spoelstra 2013 Symptom Management Toolkit (SMT) and an Automated Voice Response (AVR) phone system alone, the ATCS Plus intervention (AVR system and SMT complemented by nurse strategies) |
Risk of bias −1 as unclear risk on randomisation and allocation concealment, also high risk of selective reporting. Single study contributing to results −1 |
Low | |
| IVR vs nurse calls | Sikorskii 2007 | Risk of bias −1 as unclear on allocation concealment and while low risk for some items most others are unclear Single study contributing to results −1 |
Low |
| IVR vs usual care | Siegel 1992 | Risk of bias −2 as high risk rating on randomisation and attrition bias, unclear on allocation concealment and on most others Single study contributing to results −1 |
Very low |
|
Chronic pain Complex vs usual care |
Kroenke 2014 | No downgrading for risk of bias as all items low risk Single study contributing to results −1, sample size not large |
Moderate |
| IVR vs usual care | Naylor 2008 | Risk of bias −1 as unclear on allocation concealment and while low risk for some most others are unclear Single study contributing to results, −1 for single very small (N = 55) study |
Low |
| Chronic obstructive pulmonary disease | Halpin 2009 | Risk of bias okay as low risk, not downgraded Single study contributing to results −1, sample size small |
Moderate |
|
Adherence to medication or laboratory tests Multimodal vs usual care Different outcome measures, cannot combine |
Ho 2014 | Risk of bias okay as low risk, not downgraded Single study contributing to results −1, sample size small |
Moderate |
| Stuart 2003 | Risk of bias −2 as high risk for attrition bias, reporting and other bias; unclear on all other items including randomisation and allocation concealment Note cluster RCT apparently without adjustment for clustering (unit of analysis error). Single study with methodological limitations contributing to results −1 |
Very low | |
| ATCS Plus vs control/IVR Different outcome measures, cannot combine |
Cvietusa 2012 | Risk of bias −1 as all items rated unclear except other bias (low) Do not downgrade further for single study contributing to results (large sample, N > 1000) |
Moderate |
| Stacy 2009 | Risk of bias −1 as randomisation and allocation concealment both unclear, many other items unclear Do not downgrade further for single study contributing to results (large sample, N approx 1000) |
Moderate | |
| ATCS Plus vs usual care Do not rate down on quality for a single study as considered together in synthesis ‐ medication adherence |
Derose 2013 | Do not rate down on risk of bias, most items low risk Also do not downgrade for single study as well‐designed and large (N > 5000) |
Overall GRADE Risk of bias −1 (allocation concealment unclear in 2/3 studies) Imprecision okay Inconsistency okay (all the same direction) Indirectness Publication bias Moderate |
| Vollmer 2011 | Risk of bias −1 as allocation concealment unclear and while low risk for some most others are unclear (but −1 as single study for secondary outcomes ) | ||
| Vollmer 2014 | Risk of bias −1 as allocation concealment unclear and while low risk for many, high risk of performance bias Do not downgrade further for single study contributing to results (large sample N > 20,000) |
||
| ATCS Plus versus usual care or no calls Composite measure, cannot combine |
Sherrard 2009 | Risk of bias −1 as randomisation unclear and while low risk for many high risk of detection bias Single study contributing to results −1 |
Low |
| ATCS Plus versus usual care or no calls Test adherence 12 weeks |
Derose 2009 | Risk of bias −1 as allocation concealment unclear and while low risk for some most others are unclear Do not downgrade further for single study contributing to results (large sample N > 13,000) |
Moderate |
| ATCS Plus versus usual care or no calls Test adherence 12 months |
Simon 2010b | Risk of bias −1 as most unclear risk (only attrition bias low risk) Do not downgrade further for single study contributing to results (large sample N = 1200) |
Moderate |
| IVR vs control/other IVR Didn't combine the results as different outcome measures reported |
Adams 2014 Multiple IVR vs single IVR control Comprehensiveness of screening/counselling |
Risk of bias −1 as mostly unclear risk ratings (except performance bias) Single study contributing to results −1 |
Low |
|
Bender 2010 IVR vs none Adherence to medication |
Risk of bias −1 as mostly unclear risk ratings (allocation concealment and other items) Single study contributing to results −1 |
Low | |
|
Leirer 1991 IVR vs none |
Risk of bias −1 as all unclear risk of bias ratings Single study contributing to results −1; very small study (N = 16) |
Low | |
|
Mu 2013 IVR versus none |
Risk of bias −1 as some items rated as unclear but low on sequence generation and allocation concealment; rated as high on performance bias Do not downgrade further for single study contributing to results (very large sample N > 4,000,000) |
Moderate | |
| IVR vs usual care Did not combine these as same comparison but measured at very different time points |
Bender 2014 Medication Possession Ratio 24 months |
Risk of bias −1 as all unclear risk ratings Do not downgrade further for single study contributing to results (large sample N > 1000) |
Moderate |
|
Patel 2007 Medication Possession Ratio 3‐6 months |
Risk of bias −1 as all unclear risk ratings Do not downgrade further for single study contributing to results (large sample N > 15,000) |
Moderate | |
| IVR vs usual care |
Feldstein 2006 Test completion |
Risk of bias okay as while usual care on allocation concealment other key items are low risk Note unit of analysis error (cluster RCT): data unadjusted for clustering (−1) Do not downgrade further for single study contributing to results (large sample N = 961) |
Moderate |
| Combine these as similar outcomes, adherence 3‐6 months |
Boland 2014 Adherence to medications, 3 months |
Risk of bias −1 as unclear on several items (attrition bias, blinding) and high risk for other bias (baseline imbalances) | Overall GRADE Risk of bias −1 as unclear on allocation concealment both studies, unclear on randomisation and attrition bias 1 study; high other risk for baseline imbalance 1 study. Imprecision okay Inconsistency okay Indirectness Publication bias Moderate |
|
Friedman 1996 Medication adherence, 6 months |
Risk of bias −1 as unclear on randomisation and allocation concealment Single study contributing to results −1 for secondary outcomes |
||
| Combine these as similar outcomes, adherence 8‐ 12 months |
Glanz 2012 Medication adherence, 12 months |
Risk of bias −1 as allocation concealment unclear, high risk of detection bias | Overall GRADE Risk of bias −1 as unclear on allocation concealment 1 study; high risk of detection bias 1 study; high risk of other bias (baseline imbalances) 1 study Imprecision okay Inconsistency okay Indirectness Publication bias Moderate |
|
Migneault 2012 Medication adherence, 8 months |
Risk of bias okay not to downgrade as low risk on key items, otherwise unclear except high risk for other bias (baseline imbalance) (−1 for secondary outcomes where it is the only study reporting the outcome) |
||
| Combined, similar intervention and outcome and time point |
Green 2011 Medication refill rate, 2 weeks |
Risk of bias −1 as all items rated unclear | Overall GRADE −1 Risk of bias due to all items rated unclear Imprecision ‐ very large samples, okay Inconsistency good, effect estimates are very close Indirectness Publication Moderate |
|
Reynolds 2011 Medication refill rate, 2 weeks |
Risk of bias −1 as all items rated unclear | ||
| Unidirectional IVR vs control | Lim 2013 | Risk of bias −1 as allocation concealment and attrition bias unclear, high risk detection bias Single study −1 for secondary outcomes |
Overall GRADE Risk of bias −1 all items unclear rating Imprecision −1 as very small combined sample size Inconsistency okay Indirectness Publication bias Low |
| Ownby 2012 | Risk of bias −1 as allocation concealment and all other items are unclear Single very small study −1 |
||
|
Diabetes ATCS Plus/IVR vs usual care (pooled) |
Graziano 2009 | Risk of bias do not downgrade Small sample (N = 112) (for secondary outcomes where single study −1) |
Overall GRADE Risk of bias −1 as allocation concealment unclear (+ other items) in 4/7 studies Imprecision okay, effect estimate is quite precise even though combined sample is only N ˜ 1,200 Inconsistency −1; moderate; effects in different directions Indirectness Publication bias Low |
| Khanna 2014 | Risk of bias allocation concealment unclear, attrition high risk, others unclear except randomisation, −1 Small (N < 100) |
||
| Lorig 2008 | Risk of bias all unclear except attrition high risk, −1 | ||
| Piette 2001 | Risk of bias all okay, do not downgrade Sample size okay (N > 250) |
||
| Williams 2012 | Risk of bias low on key items but high on selective reporting & others, −1 Small sample (N = 120) |
||
| Kim 2014 | Risk of bias all unclear Small sample (N = 100) |
||
| Schillinger 2009 | Risk of bias −1 as allocation concealment unclear Sample size okay (for secondary outcomes where it is the only study contributing data −1) |
||
| ATCS Plus vs usual care Median glycated haemoglobin |
Katalenich 2015 | Risk of bias −1 as allocation concealment unclear Very small sample (N < 100), single study contributing to results −1 |
Low |
| IVR vs usual care | Homko 2012 | Risk of bias −1 as allocation concealment and most other items unclear Very small sample (N < 100), single study contributing to results −1 |
Low |
| ATCS Plus vs usual care pooled Diabetic foot care |
Piette 2001 | Risk of bias all okay, do not downgrade Sample size okay (N > 250) For secondary outcomes, result from single study and while good for risk of bias still relatively small, so −1 |
Overall GRADE Risk of bias −1 as possible risk due to allocation concealment unclear Imprecision not bad although CIs are reasonably large Inconsistency okay Indirectness Publication bias Moderate |
| Schillinger 2009 | Risk of bias −1 as allocation concealment unclear Sample size okay For secondary outcomes where it is the only study contributing data −1 |
||
| Self‐monitoring blood glucose ATCS Plus vs usual care 6 month data |
Lorig 2008 | Risk of bias all unclear except attrition high risk, −1 Single study contributing to results (for 6 month data) −1 |
Low |
| 12 month data | Piette 2001 | Risk of bias all okay, do not downgrade Sample size okay (N > 250) For secondary outcomes, single study contributing to results−1 |
Overall GRADE Risk of bias −1 as allocation concealment unclear in 1/2 studies Imprecision okay, reasonable sample size Inconsistency okay Indirectness Publication bias Moderate |
| Schillinger 2009 | Risk of bias −1 as allocation concealment unclear For secondary outcomes −1 for single study contributing to data |
||
| Depression, anxiety, self‐efficacy, days in bed because of illness, days cut down on activities because of illness, diabetes‐specific health‐related quality of life and satisfaction with care, general health‐related quality of life (both in English speakers only) ATCS Plus versus usual care |
Piette 2000 | Risk of bias all okay as low risk predominates Single small (N < 250) contributing data, −1 |
Moderate |
| Heart failure |
Capomolla 2004 ATCS Plus |
Risk of bias −1, unclear on randomisation and allocation concealment, other items mostly low risk Small sample (N < 150) For outcomes where only a single study −1 (low) |
Pooled in meta‐analysis Risk of bias −1 due to high risk randomisation in 1/2; unclear on allocation concealment in both studies Imprecision: CIs are not too wide although sample size combined is small −1 Inconsistency okay Indirectness Publication bias Low For the outcome of cardiac mortality assessed as very low certainty as CIs include both a potential substantial benefit and a potential substantial harm. |
|
Kurtz 2011 IVR |
Risk of bias −2, high risk on randomisation, unclear on allocation concealment and other items Small sample (N < 150) For outcomes where only a single study −1 (very low) |
||
|
Krum 2013 ATCS Plus |
Risk of bias not downgraded as low risk on several key items (although allocation concealment unclear) For outcomes where only a single study (N < 500), −1 |
Moderate | |
|
Chaudhry 2010 ATCS Plus |
Risk of bias all rated low risk, do not downgrade Good sample size (N > 1500) |
High | |
| HIV/AIDS | Shet 2014 | Risk of bias all good except one element of blinding. Given that research staff etc were blinded this is unlikely to be a big issue; do not downgrade Reasonable sample size (N > 600) |
High |
| Hypercholesterolemia |
Hyman 1996 IVR |
Risk of bias −1 as most items rated unclear (including randomisation and allocation concealment), attrition bias high risk Smallish sample (N ˜ 120), single study contributing to data−1 |
Low |
|
Hyman 1998 ATCS Plus |
Risk of bias −1 as most items unclear risk (including allocation concealment); attrition bias high risk Smallish sample (N ˜ 120), single study contributing to data−1 |
Low | |
|
Hypertension IVR vs usual care+ |
Dedier 2014 IVR |
Risk of bias −1, all items rated unclear Sample size N ˜ 250, single study contributing to data −1 |
Low |
| Multimodal vs usual care |
Bove 2013 ATCS Plus complex |
Risk of bias not downgraded as most items low risk but allocation concealment unclear Sample size 166, single study contributing to data−1 |
Moderate |
| Pooled in meta‐analysis for systolic blood pressure |
Magid 2011 ATCS Plus complex |
Risk of bias okay, most key items rated low risk, attrition bias possibly a bit problematic but ITT analysis was used. Other bias high risk (baseline imbalances in blood pressure) Downgrade −1 Sample > 250; for secondary outcomes −1 for single study contributing to results (low) |
Overall GRADE Risk of bias −1 as unclear ratings for key items: allocation concealment unclear in 2/3 studies, randomisation in 1/3, high risk performance bias 1/3 and high other risk of bias(baseline imbalance) 1/3 studies. Imprecision may be a problem (wide CIs, effects would be different at either end, i.e. benefit and harm possible within the 95% CI range ‐ although this would not be a substantial harm i.e. only just into favouring control values). Did not deduct a point Heterogeneity low Indirectness Publication bias Moderate |
|
Piette 2012 ATCS Plus |
Risk of bias −1 as most items rated unclear, including allocation concealment; and high risk of performance bias Sample N ˜ 200; for secondary outcomes −1 for single study contributing to results |
||
|
Harrison 2013 Uni‐direct |
Risk of bias −1 as almost all items rated unclear (including randomisation and allocation concealment) Very large sample (> 50,000) |
||
| Pooled in meta‐analysis for diastolic blood pressure |
Magid 2011 ATCS Plus complex |
Risk of bias okay, most key items rated low risk, attrition bias possibly a bit problematic but ITT analysis was used. Other bias high risk (baseline imbalances in blood pressure) Downgrade −1 Sample N > 250; for secondary outcomes −1 for single study contributing to results |
Overall GRADE Risk of bias ‐ 1 as 1/2 studies unclear on allocation concealment and other items, high risk of other bias in 1/2 studies Imprecision CIs cover both benefit and harm – but these are small effect sizes in both directions so do not downgrade. Inconsistency −1 as effects are in different directions and I2 >70% Indirectness Publication bias Low |
|
Harrison 2013 Uni‐direct |
Risk of bias −1 as almost all items rated unclear (including randomisation and allocation concealment) Very large sample (N > 50,000) |
||
|
Mental health IVR vs control |
Farzanfar 2011 IVR |
Risk of bias −1 as randomisation and allocation concealment unclear, as were other items Sample N ˜ 160 Single study contributing to results, −1 |
Low |
| ATCS Plus vs control |
Greist 2002 ATCS Plus |
Risk of bias −1 as randomisation and allocation concealment unclear, as were other items Sample N ˜ 200 Single study contributing to results, −1 |
Low |
| Unidirectional vs control |
Zautra 2012 Uni‐directional |
Risk of bias −1 as randomisation and allocation concealment unclear, as were other items Sample very small N ˜ 70 Single study contributing to results, −1 |
Low |
|
OSAS Not pooled, different time points (2 months, 12 months) |
DeMolles 2004 | Risk of bias −1, almost all items rated unclear Very small sample size N ˜ 30 Single study contributing to results, −1 |
Low |
| Sparrow 2010 | Risk of bias −1 as rated unclear for allocation concealment and attrition bias Sample N ˜ 250 Single study contributing to results, −1 |
Low | |
|
Smoking Pooled for abstinence |
Ershoff 1999 IVR + booklet vs booklet |
Risk of bias −1, unclear on randomisation and allocation concealment; high risk attrition bias Sample N ˜ 300 |
Overall GRADE Risk of bias −1 as 4/7 unclear on allocation concealment and other items Imprecision okay Inconsistency problem, effect estimates fall on both sides of the line, I2 substantial −1 Indirectness Publication bias Low |
|
McNaughton 2013 IVR vs no calls |
Risk of bias −1, all except randomisation rated unclear Very small sample N = 44 (where only study contributing to results −1) |
||
|
Reid 2007 ATCS Plus vs usual care |
Risk of bias −1 allocation concealment unclear plus other items unclear Small sample N = 100 |
||
|
Rigotti 2014 ATCS Plus vs usual care |
Risk of bias okay, low risk on all key items, do not downgrade Sample size N ˜ 400 |
||
|
Regan 2011 ATCS Plus vs inactive ATCS (IVR + callback vs IVR) |
Risk of bias okay, low risk on all key items, otherwise unclear Sample size N ˜ 700 Downgrade −1 for where a single study contributing to outcome (moderate) |
||
|
Velicer 2006 Multimodal IVR vs usual care/ none? |
Risk of bias −1 as unclear on allocation concealment, others are low/unclear Good sample size >2000 |
||
|
Brendryen 2008 ATCS Plus complex intervention vs self‐help booklet |
Risk of bias okay, nearly all low risk; do not downgrade Sample size N = 396 Downgrade −1 for where a single study contributing to outcome (moderate) |
||
|
Reid 2011 ATCS Plus vs usual care |
Risk of bias −1, all unclear, including allocation concealment and randomisation Sample N ˜ 440 Single study contributing to results, −1 |
Low | |
|
Peng 2013 ATCS Plus vs inactive IVR |
Risk of bias −1, all unclear, including allocation concealment and randomisation Sample N ˜ 120 Single study contributing to results, −1 |
Low | |
|
Carlini 2012 ATCS Plus vs inactive IVR |
Risk of bias −1, almost all unclear rating including allocation concealment Sample size okay, N = 500 Single study contributing to results, −1 |
Low | |
| Spinal cord dysfunction |
Houlihan 2013 IVR vs usual care |
Risk of bias −1 as allocation concealment unclear, several other items unclear Smallish sample; single study contributing to results, −1 |
Low |
Appendix 14. Approximate analyses of cluster‐randomised trial for the meta‐analysis
| Study | Hess 2013 | ||
| intervention | no. patients (n_i) | no. vaccin (Z_i) | Z_i*(n_i‐Z_i)/n_i |
| A | 454 | 4 | 3.964758 |
| B | 1191 | 25 | 24.47523 |
| C | 1156 | 30 | 29.22145 |
| D | 351 | 10 | 9.7151 |
| E | 729 | 17 | 16.60357 |
| F | 392 | 17 | 16.26276 |
| G | 642 | 16 | 15.60125 |
| H | 684 | 27 | 25.93421 |
| Total.I | 5599 | 146 | 141.7783 |
| Control | |||
| I | 816 | 0 | 0 |
| J | 657 | 11 | 10.81583 |
| K | 1231 | 5 | 4.979691 |
| L | 435 | 3 | 2.97931 |
| M | 579 | 0 | 0 |
| N | 1152 | 3 | 2.992188 |
| O | 1157 | 21 | 20.61884 |
| P | 356 | 3 | 2.974719 |
| Total.C | 6383 | 46 | 45.36058 |
| Overall Total (N) | 11982 | 192 | 187.1389 |
| no. clusters (k) | 16 | ||
| pi | 0.016024036 | ||
| ICC.Fleiss‐Cuzick | 0.00812106 | ||
| average cluster size (M) | 748.875 | ||
| design effect | 7.073537484 | ||
| original data | ATCS events: 146; total: 5599 and control events: 46; total: 6383 | ||
| intervention | 5599 | 146 | |
| control | 6383 | 46 | |
| updated data | divided by the design effect | ||
| intervention | 791.5417163 | 20.64030909 | |
| control | 902.3773486 | 6.503111082 | |
Data and analyses
Comparison 1. ATCS vs control for improving health services uptake (immunisations).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Immunisation in children | 5 | 10454 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [1.18, 1.32] |
| 2 Immunisation in adolescents | 2 | 5725 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [1.02, 1.11] |
| 3 Immunisation in adults | 2 | 1743 | Risk Ratio (M‐H, Random, 95% CI) | 2.18 [0.53, 9.02] |
Comparison 2. ATCS vs control for improving health services uptake (screening rates).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Breast cancer screening | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Multimodal/complex interventions | 2 | 462 | Risk Ratio (M‐H, Random, 95% CI) | 2.17 [1.55, 3.04] |
| 1.2 IVR | 2 | 2599 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.99, 1.11] |
| 2 Colorectal cancer screening | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Multimodal/complex intervention | 3 | 1013 | Risk Ratio (M‐H, Random, 95% CI) | 2.19 [1.88, 2.55] |
| 2.2 IVR (shorter follow‐up) | 2 | 16915 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [1.25, 1.48] |
| 2.3 IVR (longer follow‐up) | 2 | 21335 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.97, 1.05] |
Comparison 3. ATCS vs control for reducing body weight.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 BMI adults | 3 | 672 | Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.38, 0.11] |
Comparison 4. ATCS vs usual care for managing diabetes mellitus.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Glycated haemoglobin | 7 | 1216 | Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.50, ‐0.01] |
| 2 Self‐monitoring of diabetic foot | 2 | 498 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [0.06, 0.42] |
Comparison 5. ATCS vs usual care for reducing healthcare utilisation in patients with heart failure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cardiac mortality | 2 | 215 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.21, 1.67] |
| 2 All‐cause mortality | 3 | 2165 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.79, 1.28] |
Comparison 6. ATCS vs usual primary care and education or usual care for managing hypertension.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Systolic blood pressure | 3 | 65256 | Mean Difference (IV, Random, 95% CI) | ‐1.89 [‐2.12, ‐1.66] |
| 2 Diastolic blood pressure | 2 | 65056 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐2.62, 2.66] |
Comparison 7. ATCS for smoking cessation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Smoking abstinence | 7 | 2915 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.98, 1.46] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adams 2014.
| Methods |
Aim: to determine whether use of Personal Health Partner (PHP) was associated with significant differences in parental report of primary care visit content. Additional goals included evaluating the intervention effect on medication management, asthma care, and parent and clinician satisfaction Study design: RCT; recruitment: primary care (mail) Study duration: 25 months; study type: prevention; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: children aged 4 months to 11 years (and their parents) who had a routine healthcare maintenance or well‐child visit. Parents and children had to speak English and could not be planning to move away from the Boston area within 3 months Sample size: 475; mean age: 5 years (child) 35 years (parent);sex: women ‐ 48% (child), 93% (parent); men ‐ 52% (child) 7% (parent); ethnicity: African‐Americana 67% (child); 47% (parent); other 33% (child); 53% (parent) Country: USA |
|
| Interventions |
Personal Health Partner (PHP) tailors call content based on the participant's age and prescription of asthma medication. Call content was based on American Academy of Pediatrics Bright Futures topics reflected in the electronic health record (EHR) templates at the study site as well as Medicaid‐recommended health risk questions for routine healthcare maintenance (RHCM), asthma symptoms, and medication safety. When available, PHP scripts were based on validated tools. RHCM areas include general health supervision, developmental screening, diet and physical activity, tuberculosis risk assessment, smoking risk assessment, and maternal depression screening. Each call also addressed medication safety, examining what medications on the EHR medication list the child was actually taking, age‐appropriate medication use, and proper use of asthma controller and reliever medication if applicable. The day before each scheduled visit, PHP data were transferred to the EHR. PHP questions yielding actionable data generate an "Alert" displayed within the "Alerts" section of the "Patient Entered Data Review" form. Control group completed a single automated call, but the content was limited to the 18‐question Framingham Safety Survey. At the completion of the call, parents in the control group received tailored advice related to unsafe behaviours reported during the call. Because the Framingham Safety Survey was not part of routine primary care at Boston Medical Center, data from these calls were not shared with the EHR. |
|
| Outcomes | Comprehensiveness of screening and counselling (primary), assessment of medications and their management, and parent and clinician satisfaction (secondary) | |
| Funding | Agency for Healthcare Research and Quality, grant R18HS017248 | |
| Declaration of conflict of interest | No potential conflicts of interest disclosed | |
| Power calculations for sample size | No | |
| Notes | The authors have been contacted for results from the Medication Adherence Scale with no response | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Children were randomly assigned to groups at the start of each call". Comment: insufficient information to judge whether random sequence generation was ensured |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Study staff members were not aware of allocation group at the time of interviews" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | No results from the Medication Adherence Scale have been reported. Comment: insufficient information to judge whether this introduced bias |
| Other bias | Unclear risk | Insufficient information |
Aharonovich 2012.
| Methods |
Aims: to compare motivational interviewing (MI) HealthCall to MI‐only to reduce non‐injection drug use (NIDU) in urban HIV primary care patients Study design: RCT; recruitment: primary care (health professional referral) Study duration: 2 months; study type: prevention; subtype: substance abuse |
|
| Participants |
Inclusion criteria: HIV‐positive, English‐ or Spanish‐speaking, aged 18 years, enrolled in a New York City hospital‐affiliated HIV primary care clinic, using drugs ≥ 4 days during the prior 30 days (including illicit non‐injection drugs or prescription drugs taken without prescription or more than prescribed) Sample size: 33; mean age: 46 years; sex: men ‐ 76%; women ‐ 24%; ethnicity: African American 64%, Hispanic 21%, Caucasian (understood to be white) 15% Country: USA |
|
| Interventions |
MI + HealthCall: participants call HealthCall daily via a toll‐free number to report on the targeted health behaviour and potentially related moods, behaviours, and situations that occurred in the prior 24 h. HealthCall menu for NIDU included a short set of prerecorded questions in English or Spanish about the previous day covering use of primary drug, dollar amount spent on the drug used, use of other drugs, HIV medication adherence, and feelings of wellness, stress, and overall quality of the day. Participants responded by pressing numbers on the telephone keypad. After the practice call, counsellors helped participants identify an accessible telephone and convenient time for daily calls and set the watch alarm to this time as a reminder to call. Counselors were bilingual (English/Spanish) and from the same race/ethnic groups as most of the participants. HealthCall data were automatically uploaded to a database and used to provide personalised feedback to participants about their drug use in a single‐page form that included a computer‐generated graph of participants' drug use as called into the IVR and a set of summary statistics during the 30‐ and 60‐day visits. The personalised graph contained the participant's goal set in the baseline MI interview with the counsellor (NIDU Goal), with diamond‐shaped dots representing the dollar amount of drugs used on the days that the participant called HealthCall Participants in MI‐only arm (control) received a 20–25 min MI at baseline, using standard MI techniques, e.g. dialogue about health consequences of NIDU, exploring ambivalence, barriers to change, developing a change plan, including (for those who chose) a specific NIDU‐reduction goal (reflected in USD amounts) for the next 30 days. Participants then received a digital alarm watch which they were told they could use as a medication reminder. At 30 and 60 days, counsellor and participant met for 10–15 min to review overall drug use and set or re‐set a drug reduction goal for the next 30 days. |
|
| Outcomes | Days used primary drug in last 30 days (primary); patient satisfaction (secondary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation was done via 10‐block standard ABAB design" |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were blinded to their random assignment until after the MI session" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Counsellors were not blinded to their random assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Treatment groups did not differ on attrition (p = 0.10) and thus attrition is not likely to be a source of bias in our results." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | No significant baseline differences |
Andersson 2012.
| Methods |
Aims: to study if there is a difference in effect between automated interventions delivered by IVR and over the Internet Study design: RCT; recruitment: other ‐ university (web‐based survey) Study duration: 6 weeks; study type: management; subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: Swedish university students having an AUDIT score above cutoff (8 and 6) Sample size: 1423; mean age: *; sex: *; ethnicity: * Country: Sweden |
|
| Interventions |
Single IVR call of less than 500 words, one week after the baseline assessment, consisting of feedback on the baseline assessment and instructions on how to obtain a recommended Blood Alcohol Concentration (BAC) below 0.6‰ (0.06 percentages) Single Internet‐delivered intervention given one week after baseline Repeated IVR call Repeated Internet‐delivered intervention given 1 and 2 weeks after intervention No intervention (controls) |
|
| Outcomes | Alcohol Use Disorders Identification Test (primary) | |
| Funding | Swedish National Institute of Public Health and Edwin Berger Foundation | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | In the present review we report a comparison between single IVR call and no intervention. Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Baker 2014.
| Methods |
Aims: to determine whether a multifaceted intervention increases adherence to annual faecal occult blood testing compared with usual care Study design: RCT; recruitment: community centre (organisation referral) Study duration: 12 months; study type: prevention; subtype: screening |
|
| Participants |
Inclusion criteria: age 51 to 75 years; preferred language listed as English or Spanish; and a negative faecal occult blood testing result obtained between 1 March 2011, and 28 February 2012 Sample size: 450; mean age: 60 years; sex: men ‐ 28%; women ‐ 72%; ethnicity: Latino ‐ 87%, other ‐ 13% Country: USA |
|
| Interventions |
The multimodal intervention group received (1) a mailed reminder letter, a free faecal immunochemical test with low‐literacy instructions, and a postage‐paid return envelope; (2) an automated telephone and text message reminding them that they were due for screening and that a faecal immunochemical test was being mailed to them; (3) an automated telephone and text reminder 2 weeks later for those who did not return the faecal immunochemical test; and (4) personal telephone outreach by a colorectal cancer screening navigator after 3 months in addition to UC which included computerised reminders, standing orders for medical assistants to give participants home faecal immunochemical tests, and clinician feedback on colorectal cancer screening rates. Usual care (control group) at participating health centres included computerised reminders, standing orders for medical assistants to give participants home faecal immunochemical tests, and clinician feedback on colorectal cancer screening rates. |
|
| Outcomes | Completion of faecal occult blood testing within 6 months of the date the participant was due for annual screening (primary) Costs (secondary) | |
| Funding | Grant P01 HS021141‐ the Agency for Healthcare Research and Quality | |
| Declaration of conflict of interest | None reported | |
| Power calculations for sample size | To detect a 10% difference (45% vs 35%) with 80% power (2‐tailed alpha = 0.05), we would need 752 participants (376 in each arm).This is less than the 800 participants that we estimated will be eligible for the study | |
| Notes | The estimated cost of the outreach intervention was USD 34.59 per participant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Investigators were blinded to the outcomes in the control group |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "Using only EHR data for outcome assessment is conceptually similar to blinded outcome assessment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 450 participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Outcomes of interest reported |
| Other bias | Low risk | Groups were comparable at baseline |
Bender 2010.
| Methods |
Aim: to test the effectiveness of a theory‐based IVR intervention to improve adherence to controller medications among adults with asthma Study design: RCT; recruitment: community (advert in newspaper) Study duration: 10 weeks; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: no significant disease or disorder (chronic health disorders, current substance abuse or dependence, mental retardation, or psychiatric disorder); and lack of participation in any other asthma‐related research or clinical trial Sample size: 50; mean age:42 years;sex: women ‐ 59%; men ‐ 41% Ethnicity: white ‐ 58%, African American ‐ 20%, Hispanic ‐ 18%, Asian ‐ 4% Country: USA |
|
| Interventions |
In the IVR group, each participant received ≥ 2 calls separated by 1 month. Calls were programmed to reach out at several time points throughout the day and evening until the participant answered. If an answering machine was reached, a toll‐free number was provided, which the participant could use to call back. When a call connection was completed, the IVR call identified itself as coming from the Denver Interactive Asthma Learning System program and verified that the correct person had been called. Content of the call then included an explanation of how the call works followed by 3 questions inquiring whether during the previous week the participant had been awakened at night, had limited their activities, or had used their rescue inhaler more than twice because of asthma symptoms (symptom module). Participants who responded affirmatively to any of the 3 questions were told that daily use of their controller medication should help prevent such symptoms and were advised to discuss the symptoms with their physician. All participants also listened to a short module about the benefits of their asthma medication and were asked about whether they were filling and using their medication, with IVR responses tailored to specific participant responses (refill module). Finally, participants were informed about the Lung Line, a free telephone service staffed by nurses capable of answering most questions about asthma, and about the Colorado Quit Line, offering free telephone based tobacco cessation intervention (resources module) Participants in the control group received no calls. |
|
| Outcomes | Medication adherence (primary); Asthma Control Test, Asthma Quality of Life Questionnaire, Beliefs about Medications Questionnaire (secondary) | |
| Funding | Astra Zeneca | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | Power and sample size calculations indicated that 25 participants in each group would provide 75% power to detect a group difference of 36% | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A randomisation table generated before study initiation determined group assignment by order of entry into the study" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The investigators remained blind to treatment until the final data set was completed" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Participants were comparable at baseline |
Bender 2014.
| Methods |
Aim: to improve adherence in paediatric asthma Study design: RCT; recruitment: secondary care (*) Study duration: 24 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: children, ages 3‐12 years, treated for persistent asthma at Kaiser Permanente of Colorado Sample size: 1187; mean age: *sex: * ethnicity: * Country: USA |
|
| Interventions |
Parents in the IVR group received a call reminding them that inhaled corticosteroid fill was overdue, and assisted with automated mail order refills or transfer to a Kaiser Permanente of Colorado pharmacy or asthma nurse specialist. Telephone calls in this group pulled information from the electronic health record (EHR) enabling the automated call to provide personalised participant and medication information. Parents in the control group received usual care |
|
| Outcomes | Medication adherence (primary); utilisation of care (secondary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Bennett 2012.
| Methods |
Aims: to evaluate the effectiveness of a behavioural intervention that emphasised weight loss and hypertension medication adherence among primary care patients in the community health centre setting Study design: RCT; recruitment: community centre (telephone) Study duration: 24 months; study type: prevention; subtype: weight management |
|
| Participants |
Inclusion criteria: BMI 30‐50 kg/m2 (and weighing < 181.4 kg (400 pounds)), undergoing treatment for hypertension, aged ≥ 21 years, and enrolled participant at one of the participating community health centres (CHC). Additionally, participants had to read and speak English or Spanish, provide informed consent, and be willing to change diet, physical activity, and weight Sample size: 365; mean age: 55 years; sex: men ‐ 31%; women ‐ 69%; ethnicity: non‐Hispanic black ‐ 71%, Hispanic ‐ 13%, non‐Hispanic white ‐ 4%, other – 12% Country: USA |
|
| Interventions |
Be Fit, Be Well: participants can choose to use either the Internet or print + IVR as a mode of delivery of the intervention. In print + IVR condition, participants track their behavioural goals daily on a paper log and then enter this information weekly using the telephone keypad during their IVR telephone call. The goals are divided into 3 categories: dietary, physical activity, and lifestyle goals. For the first 13 weeks, participants work on 3 goals; for the rest of the intervention period, they work on 4 goals simultaneously. Participants pick new behaviour change goals every 13 weeks. 2 goals ("Walk 10,000 steps per day" and "Take your blood pressure medicine the right way every day") remain constant throughout the intervention period. Skill training materials, in print, provide instruction in behavioural strategies to facilitate achieving their behavioural goals. The also provide additional dietary, physical activity, and lifestyle goals that may need additional contextualisation. Participants monitor their behavioural goals over the telephone using IVR. After entering data on their behaviour, participants receive immediate feedback on their progress compared to the previous entry. Participants receive social support via telephone coaches administered by community health educators (CHE) and group support sessions. CHE call the participants once a month in the 1st year and then bimonthly in the following year, during which they discuss progress, barriers, strategies to overcome barriers,self‐monitoring, and social support. Each call lasts for 15‐20 min. Group sessions include an interactive skill training and a physical activity component. The intervention materials include information on community resources such as public parks, local walking groups, and farmers' markets that can aid participants in their behaviour change efforts. All participants receive a walking kit that includes a pedometer and maps of the local community with associated step counts.Participants receive a personalised, tailored behaviour change "prescription" (generated from the baseline data) with the doctor's signature included electronically. This "prescription" presents recommendations for making changes in the targeted risk behaviours, and lets patients know that their doctor considers these recommendations to be important to their health Participants in the control group received usual care (self‐help booklet) |
|
| Outcomes | Change in body weight and BMI (primary); change in blood pressure; medication adherence; adverse‐events (secondary) | |
| Funding | National Heart, Lung, and Blood Institute; National Cancer Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | The trial was designed to provide 80% power to detect a mean weight change in 24 months of 2.75 kg in the intervention arm, assuming no weight change in usual care | |
| Notes | All participants are diagnosed with hypertension. In addition, 36% are diagnosed with hypercholesterolaemia, and 20% with type 2 diabetes mellitus | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated allocations were performed, blocked by clinic and sex |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The trial design precluded blinding either patients or interventionists to treatment assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All 365 participants are included in the primary outcomes analysis, including 15 participants (4.1%) who had only a baseline assessment." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Both the groups were balanced in all other characteristics at baseline |
Bennett 2013.
| Methods |
Aims: to compare changes in weight and cardiometabolic risk during a 12‐month period among black women randomised to a primary care–based behavioural weight gain prevention intervention or to usual care Study design: RCT; recruitment: community centre (mail) Study duration: 18 months; study type: prevention; subtype: weight management |
|
| Participants |
Inclusion criteria: aged 25‐44 years, BMI of 25‐34.9 kg/m2, ≥ 1 visit to a Piedmont Health Center in the previous 24 months, North Carolina residency, and self‐reported English fluency Sample size: 194; mean age: 35 years; sex: women ‐ 100%; ethnicity: black ‐ 100% Country: USA |
|
| Interventions |
The multimodal intervention (the Shape Program) contained 5 components: obesogenic behaviour change goals; self‐monitoring via IVR phone calls; tailored skills training materials; 12 interpersonal counselling calls; and a 12‐month YMCA membership Participants in the control group received usual care: study staff made no attempts to influence the medical treatment provided to those in the usual care arm. Every 6 months, we sent usual‐care participants newsletters that covered general wellness topics but did not discuss weight, nutrition, or physical activity |
|
| Outcomes | Change in body weight and BMI (primary); maintenance of change at 18 months; adverse‐events (secondary) | |
| Funding | R01DK078798 from the National Institute for Diabetes and Digestive and Kidney Diseases; and K05CA124415 from the National Cancer Institute | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | This trial was designed to have 80% power to detect significant BMI differences of 1.03 kg/m2 between treatment groups 12 months after baseline | |
| Notes | 6 serious adverse events were reported among participants in the intervention arm, including gynaecological surgery in 2 participants and knee replacement, breast abscess, musculoskeletal injury, and cancer diagnosis in 1 participant each; all participants except the one with the cancer diagnosis required hospitalisation. The authors of the study could not conclusively determine whether reported events resulted from study participation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After completing baseline assessments, research staff initiated a computer‐generated randomisation algorithm to allocate participants equally (1:1) across the two treatment arms (intervention and usual care); those in the intervention arm were further randomised to one of two interventionists." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The study design precluded blinding patients and interventionists to treatment assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data balanced in numbers across groups (low attrition). ITT analysis was used to include all participants who received the intervention or usual care in the analysis. ITT analyses were based on the mean difference in weight and BMI between treatment arms at 12 months after adjustment for health centre. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | The groups were well‐balanced at baseline. |
Boland 2014.
| Methods |
Aims: to assess the ability of automated reminders to improve adherence with once‐daily glaucoma medications Study design: RCT; recruitment: primary care (*) Study duration: 6 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: patients non‐adherent with their medications after 3 months of electronic monitoring (prospective cohort study phase) Sample size: 70; mean age: 66 years; sex: men ‐ 49%, women ‐ 51%; ethnicity: African American ‐ 58%, European ‐ 32%, Asian ‐ 6%, Hispanic ‐ 3%, Middle Eastern ‐ 1% Country: USA |
|
| Interventions |
Automated reminders (by telephone or text message) informed each participant in the intervention group that it was time to take his or her medication. The IVR system also allowed participants to reset the reminder and receive it again in 1 hour: "Hello, this is your automated reminder to take your eye drop. Press 1 if you have or are about to take your drop. If you are not able to take your eye drop right now and would like a second reminder in 1 hour, please press 2 now." Participants in the control group received usual care |
|
| Outcomes | Medication adherence | |
| Funding | Microsoft BeWell Fund | |
| Declaration of conflict of interest | None reported | |
| Power calculations for sample size | No | |
| Notes | Communication with the author: "there was only one person (1.42% of the sample) who specified SMS (text) reminders in the study, however" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Study participants were then assigned to a control or intervention group using assignments randomised equally in blocks of 10 and placed in envelopes." |
| Allocation concealment (selection bias) | Low risk | Quote: "Study participants were then assigned to a control or intervention group using assignments randomised equally in blocks of 10 and placed in envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Large percentage of participants lost to and unavailable for follow‐up, however ITT analysis was used in addition to real efficacy approach" |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | High risk | Quote: "At baseline, there were statistically significant differences between the two groups with regard to age, educational level, and Mini‐Mental State Examination (MMSE) score" |
Bove 2013.
| Methods |
Aims: to compare the effectiveness of an Internet and telephone‐based telemedicine communication system to usual care from a primary care provider in managing patients with hypertension Study design: RCT; recruitment: primary care (advert in clinic) Study duration: 6 months; study type: management; study subtype: hypertension |
|
| Participants |
Inclusion criteria: systolic blood pressure > 140 mmHg Sample size: 241; mean age: 60 years;sex: women ‐ 79%; men ‐ 21%; ethnicity: African American ‐ 81%, white‐ 15%, Hispanic ‐ 3%, other ‐ 1% Country: USA |
|
| Interventions |
Participants in the multimodal intervention group reported their weight, blood pressure, steps/day, cigarettes/day, at least twice weekly via an Internet or IVR phone system to the clinical centre. If the systolic blood pressure was < 140 mmHg, thetelemedicine system automatically sent a short message to the participant stating that the measures were acceptable, a short message on health care, and instructions to continue with the scheduled transmission of data. Monthly blood pressure summaries were sent to all subjects and to their primary care providers Participants in the control group received usual care by their physicians |
|
| Outcomes | Blood pressure control at 6 months (primary) | |
| Funding | The Agency for Healthcare Quality and Research | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | To achieve a power of 0.8 with α value of 0.05, the authors aimed to recruit 252 subjects to accommodate a dropout rate of 20% and an expected 30% incidence of diabetes | |
| Notes | The telemedicine (intervention group) subjects used telephone communication 65% of the time | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Consecutive patients were assigned a random number from a random number list. Patients assigned odd numbers were placed in the control group, and patients assigned even numbers were placed in the telemedicine group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data balanced in numbers across groups (low attrition) |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐defined outcomes have been reported |
| Other bias | Low risk | Participants were comparable at baseline |
Brendryen 2008.
| Methods |
Aims:To assess the long‐term efficacy of a fully automated digital multimedia smoking cessation intervention Study design: RCT; recruitment: community (banner advertisements in Internet newspapers) Study duration: 12 months; study type: management; study subtype: smoking |
|
| Participants |
Inclusion criteria: people who were willing to make an attempt to quit smoking, were aged ≥ 18 years, smoked ≥ 10 cigarettes daily and had access to the Internet, email and a cellphone on a daily basis Sample size: 396; mean age: 36 years; sex: men ‐ 50%, women ‐ 50%; ethnicity: * Country: Norway |
|
| Interventions |
Multimodal intervention (Happy Ending (HE)). The IVR programme lasted for 6 weeks, with participants receiving 2 messages per day, delivered through mobile phones. In the morning when the participants logged on to the HE, they received IVR message. They received automated reminders if failed to log in. In the evening, participants received an automated call that asked about their smoking behaviour during the day. If they had smoked, they were directed to the tailored relapse prevention therapy. Craving helpline was available 24 h from day 15 onwards and participants were able to choose to hear therapeutic problem solving message related to emotion regulation, motivation boost, or stress regulation. Participants were encouraged to call the helpline each time they felt tempted to have a cigarette. Until week 11, the intervention had multiple daily contact points and was highly intensive. HE recommended the use of nicotine replacement therapy and they could choose between gum (2 mg or 4 mg) and patches (15 mg/16 h). HE also offered an 11‐month follow‐up phase. During this phase, the log‐off procedure continued daily for another 4 weeks, twice a week for another 2 weeks, and then once a week for the remaining follow‐up period. All the features provided in the active phase remained functional including craving helpline and supportive IVR messages. Participants in the control group received self‐help intervention (booklet) |
|
| Outcomes | Repeated point abstinence at 1, 3, 6 and 12 months post‐cessation (primary); nicotine replacement therapy adherence, self‐efficacy and nicotine dependence (secondary) | |
| Funding | University of Oslo, Happy Ending AS and the Norwegian Research Council. Pfizer Norway provided a free supply of nicotine replacement therapy | |
| Declaration of conflict of interest | The second author has a financial interest in the intervention, as a shareholder of Happy Ending AS | |
| Power calculations for sample size | The report confirms that power analysis was performed. 396 were required | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Quote: "The names and identities of the subjects, however, were concealed to the experimenter during randomization." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods; ITT analysis was used to include all participants who received the intervention or usual care in the analysis |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are of interest in the review have been reported. |
| Other bias | Low risk | Quote: "At baseline, there were no variables on which treatment and control subjects differed significantly" |
Capomolla 2004.
| Methods |
Aims: to evaluate the effectiveness of comprehensive home telemonitoring service (TMS) in participants discharged from a Heart Failure Unit Study design: RCT; recruitment: primary care (organisation referral) Study duration:12 months; study type: management; subtype: heart failure |
|
| Participants |
Inclusion criteria: patients with chronic heart failure Sample size: 133; mean age: 57 years; sex: men ‐ 88%, women ‐ 12%; ethnicity: * Country: Italy |
|
| Interventions |
TMS: participants called a toll‐free number. After entering the unique identification code, the IVR system asked a series of question about vital signs and symptoms such as weight, systolic blood pressure, heart rate, dyspnoea, asthenia, oedema, therapy changes, blood urea nitrogen, creatinine, sodium, potassium, and bilirubin. Participants answered by using the touchpad of their home or mobile phone. If advice or help was needed, participants could leave a message to contact the medical staff. Those who failed to call the system for > 2 days were personally contacted by phone. Similarly, those with abnormal readings were flagged up and received a phone call from the medical team. Participants in the control group received usual community care. At discharge, participants were referred to their community primary care physician and cardiologist or cardiology department. During follow‐up the process of care was governed by different providers which managed the participant's needs with a heterogeneous range of strategies: emergency room management, hospital admission and outpatient access |
|
| Outcomes | All‐cause mortality; re‐hospitalisations; emergency room use (composite primary); and adherence to the treatment (secondary) | |
| Funding | Ministero della Salute funds | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | All participants received educational materials, including cardiac failure book, telemonitoring service booklet, daily computerised medications plan, pillboxes with scheduling time, summary sheets of domestic and physical activities. Participants received an individualised personal care plan designed by the physician | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All assigned participants were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are of interest in the review have been reported. |
| Other bias | Low risk | Quote: "No significant clinical or instrumental differences were observed between two groups" |
Carlini 2012.
| Methods |
Aims: to test the efficacy of IVR in recycling low‐income smokers who had previously used Quitline (QL) support back to QL support for a new quit attempt Study design: RCT; recruitment: primary care (mail) Study duration: 4 months; study type: management; study subtype: smoking |
|
| Participants |
Inclusion criteria: previous Quitline callers and current smokers. Sample size: 521; mean age: 40 years;sex: women ‐ 62.50%; men ‐ 37.50%; ethnicity: white, non‐Hispanic ‐ 81%, African American ‐ 6%, other – 5%, Hispanic or Latino ‐ 4%, Native American or Pacific Islander – 3%, Asian ‐ 1% Country: USA |
|
| Interventions |
The ATCS Plus intervention utilised in this trial was developed in 2 steps. The first step focused on creating the content of the IVR messages: 4 prototype IVR messages about possible barriers to re‐engagement in QL support for quitting smoking were developed, based on previous work with low income ethnic/racial minority smokers. These prototype messages were tested and changed according to feedback received through individual telephone interviews with fifteen Medicaid insured and uninsured smokers who had previously used a QL and agreed to be contacted further. The messages aimed to redefine relapse as a learning opportunity and not as a failure; motivate new quit attempts by reminding smokers about benefits in quitting (e.g. personal health and well being, financial savings, concern for family members); educate smokers about the different offerings of QL support services; reiterate how QL support can increase the chances of quitting; and inform smokers of their eligibility to re‐enrol in QL services The control group received only the first 2 components of the ATCS intervention (greeting and screening of smoking status), followed by a message thanking them for the information |
|
| Outcomes | Re‐enrollment into Quitline support line (primary) | |
| Funding | National Cancer Institute grants: R21CA141568 and 1R25‐CA117865 | |
| Declaration of conflict of interest | No competing interests | |
| Power calculations for sample size | No | |
| Notes | ClinicalTrials.gov Identifier: NCT01260597 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "Eligible participants were randomised to the intervention or usual care prior to entry into the IVR calling database." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐defined outcomes have been reported |
| Other bias | Unclear risk | Insufficient information |
Chaudhry 2010.
| Methods |
Aims: to determine the effect of automated symptom and self‐reported weight monitoring compared with usual care on the combined endpoint of all cause hospitalisation and mortality in patients recently hospitalised for heart failure Study design: RCT; recruitment: secondary care (organisational referral) Study duration: 6 months; study type: management; study subtype: heart failure |
|
| Participants |
Inclusion criteria: patients recently discharged from a heart failure hospitalisation Sample size: 1653; median age: 61 years;sex: women ‐ 42%; men ‐ 58%; ethnicity: white ‐ 49%, black ‐ 39%, other – 12% (inclusive of Hispanic or Latino – 3%) Country: USA |
|
| Interventions |
Tele‐HF: an automated, daily symptom and self‐reported weight monitoring intervention. During each call, participants heard a series of questions about general health and heart‐failure symptoms, and they enter responses using the telephone keypad. Information from the telemonitoring system was downloaded daily to a secure Internet site and was reviewed every weekday (except on holidays) by site coordinators. Any variance in any of the information are flagged up for clinician's attention who would then offer advice to the participant (e.g. modify diet, increase diuretic dose or adhere to medications); consult with the physicians in their practice site; advise an urgent clinic or emergency department visit; or refer the participant to another specialist, as appropriate. Participants in the control group received usual care (educational materials) |
|
| Outcomes | Readmission for any reason or death from any cause (primary); hospitalisation for heart failure, number of days in the hospital, number of hospitalisations, and adverse events (secondary) | |
| Funding | National Heart, Lung, and Blood Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | With an alpha error of 0.05 and a power of 90%, for a 25% relative risk reduction, 1640 participants were needed (820 in each group), with a follow‐up period of 6 months | |
| Notes | Adherence in the telemonitoring group was defined as placement of ≥ 3 calls a week to the telemonitoring system (a cutoff point representing approximately half the expected usage). A total of 85.6% of participants in the telemonitoring group made ≥ 1 call; among these participants, adherence to the intervention was highest, at 90.2%, during the first week of the study period and decreased to 55.1% by week 26. A total of 29,163 variances were generated during the study period, with a median of 21 (interquartile range, 5 to 54) per participant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: sequence of computer‐generated random numbers, with stratification on the basis of the study site |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was centralized and performed by telephone. Randomization is stratified by study site, and force randomised within each study site in blocks of 20 (10 intervention, 10 control), to ensure a balance across study arms within each site. The randomisation sequence is developed by the coordinating centre using a computer random‐number generator. The sequence is unknown to the attending cardiologists and nurses" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study investigators and personnel (except for members of the data and safety monitoring board) were unaware of the treatment‐group results until endpoint data had been finalised for all the participants |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "An independent Events Review Committee will assess and classify the primary and secondary end point events in a centralized and blinded manner . . . A committee of physicians, all of whom were unaware of the treatment‐group assignments, adjudicated each potential readmission to ensure that the event qualified as a readmission." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐specified outcomes have been reported in the pre‐specified way |
| Other bias | Low risk | Quote: "Baseline characteristics of the patients were similar between the two groups" |
Cleeland 2011.
| Methods |
Aims: to examine whether at‐home symptom monitoring plus feedback to clinicians about severe symptoms contributes to more effective postoperative symptom control Study design: RCT; recruitment: primary care (advert in clinic) Study duration: 1 month; study type: management; study subtype: cancer |
|
| Participants |
Inclusion criteria: men and women scheduled for thoracic surgery for primary lung cancer or lung metastases; ≥ 18 years old, able to understand English and the study requirements, and willing and able to respond to a repeated IVR‐administered symptom rating scale Sample size: 79; mean age:60 years;sex: women ‐ 47%; men ‐ 53%; ethnicity: white, non‐Hispanic ‐ 85%, other ‐ 15% Country: USA |
|
| Interventions |
In the intervention group, the IVR screened the 5 targeted symptoms. On the occurrence of ≥ 1 symptom threshold events for a participant, the IVR system immediately generated an email alert to the surgical team's advanced practice nurse (APN). The email provided the participant's name, phone number(s), and case history number, along with the severity of each symptom that had generated a symptom. If a participant missed a scheduled call, the IVR system initiated up to 2 more calls, spaced 45 min apart. If a participant in the intervention group had ≥ 1 symptom threshold events, the staff member initiated an alert email to the participant's surgical team. Participants in the control group received only automated monitoring and usual symptom care. |
|
| Outcomes | Symptom threshold events, cumulative distribution of symptom threshold events, differences in mean symptom severity (primary) | |
| Funding | RSGPB‐03‐244‐01‐BBP from the American Cancer Society, and Grant No. R01 CA026582 from the National Cancer Institute | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | 59 participants per arm would be needed to detect a medium effect size difference in postoperative symptom severity between groups, using a 2 tailed alpha = 0.05 and 80% power | |
| Notes | 2 different types of ATCS were compared against each other | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment was completed electronically by MD Anderson's protocol management system." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All 79 patients completed the 4‐week study" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Cohen‐Cline 2014.
| Methods |
Aims: to understand whether IVR could be effective to engage individuals overdue for colorectal cancer screening in community practice settings and to determine if the effect would persist over time Study design: RCT; recruitment: primary care (telephone) Study duration: 12 months; study type: prevention; study subtype: screening |
|
| Participants |
Inclusion criteria: men and women aged 50–81 years who were not adherent to colorectal cancer screening Sample size: 11,010; mean age: 61 years;sex: women ‐ 46%; men ‐ 54%; ethnicity: white ‐ 86%, other – 14% Country: USA |
|
| Interventions |
The intervention was a single IVR telephone call (average length = 5 min) to the primary telephone number listed in the participant's records. The call included the following features: assessment of prior colorectal cancer screening; information about the benefits of screening and elicitation of the barriers to screening; and offer of a faecal occult blood testing kit mailed to the participant's home. The IVR call mentioned both faecal occult blood testing and colonoscopy as recommended screening tests. If the IVR system left a message, only 1 additional message was sent. When there was no answer or a busy signal at the telephone number, up to 6 total attempts were made to reach the participant Participants in the control group received usual care, defined as a personalised outreach letter, mailed annually to all Group Health members before their birthday, informing them of upcoming preventive service needs, including cancer screening |
|
| Outcomes | The receipt of any recommended colorectal cancer screening (primary) | |
| Funding | NA | |
| Declaration of conflict of interest | One author (DCG) is a shareholder in Group Health Physicians, which contracts exclusively with Group Health Cooperative to provide medical services. The remaining authors declared no conflicts of interest | |
| Power calculations for sample size | No | |
| Notes | Participants in both the intervention and usual care could have received the outreach letter at any point during the 12‐month follow‐up period near their birthday | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We randomised 10,000 individuals to the intervention and 3279 individuals to usual care. Because the intervention was originally implemented as a pilot quality improvement initiative, the decision was made to maximize the number of individuals who could receive the IVR intervention with the available resources." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | There were significantly more men in the control group (P < 0.001), but there is insufficient evidence that this imbalance has introduced bias. |
Corkrey 2005.
| Methods |
Aims: to assess the efficacy of an IVR brief intervention in increasing cervical screening rates in 1 Australian region; to determine the cost per additional cervical screen; to compare the cost per additional cervical screen to other cervical screening interventions Study design: RCT; recruitment: primary care (mail) Study duration: 6 months; study type: prevention; subtype: screening |
|
| Participants |
Inclusion criteria: women, aged 18–69 years who had not had a hysterectomy Sample size: 75,532;Mean age: * ; sex: women ‐ 100% Country: Australia |
|
| Interventions |
Brief advice IVR cervical screening intervention was provided by Generalized Electronic Interviewing System (GEIS) software. The GEIS software explained the nature of the call; identified if women aged 18–69 years were present; selected 1 eligible woman; determined her screening status; delivered a message that either congratulated her on being correctly screened, a message of encouragement if she was under‐screened, or another message appropriate to her status; offered additional messages to counter common barriers to screening; offered additional information on cervical screening and cancer; offered to readout contact sources where she could obtain more information; offered to have someone ring her back if she still had questions; and offered to record any question she may wished answered. GEIS could reschedule the call and participants could request call backs. GEIS generated an email to advise a local staff member responsible for cervical screening promotion in the Hunter region along with any question the woman had recorded. The script contain domains concerned with Pap status determination, cervical screening barrier messages, demographic items, information items, and contact numbers Participants in the control group received no calls |
|
| Outcomes | Cervical cancer screening status at 6 months (primary); costs (secondary) | |
| Funding | Hunter Medical Research Institute and the University of Newcastle | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "To obtain a screening rate increase equal to 1.0% of the adult female population, an additional 75,532 (0.01/2) = 378 women would be needed to be screened in the intervention postcodes." | |
| Notes | The cost per additional screening obtained in this study is favourable compared to the other studies, which suggests that the IVR method could be used to target identified individuals | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "A brief advice IVR cervical screening intervention was delivered to 17,008 randomly selected households in the Hunter region in New South Wales (NSW) between April and July 2001 in 15 randomly selected postcodes. The change in screening rates before and after the intervention was compared to another 15 randomly selected control postcodes" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Cvietusa 2012.
| Methods |
Aim: to test whether a speech recognition (SR) reminder system would improve adherence to an ICS in a large unselected population of paediatric asthma patients Study design: RCT; recruitment: * Study duration: 12 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: children, aged 3‐12 years with persistent asthma Sample size: 1393; mean age:*sex: * ethnicity: * Country: USA |
|
| Interventions |
The intervention group received up to 3 tailored SR reminder calls when they were due to refill their inhaled corticosteroids. The calls provided information about asthma, facilitated a rapid inhaled corticosteroids refill, and offered an opportunity to receive a call back from an asthma nurse specialist Control group (no further information) |
|
| Outcomes | Medication adherence (refill rate) (primary); acceptability/satisfaction (secondary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "There were no statistically significant differences between the intervention and control groups in age, sex, co‐morbidities, and length of HMO enrolment." |
David 2012.
| Methods |
Aims: to conduct a feasibility study of self‐monitoring with a pedometer administered through an IVR system and mobile phones; to examine the added benefit of a human coach Study design: RCT; recruitment: community (advert elsewhere ‐ radio, television, newsletter) Study duration: 3 months; study type: prevention; study subtype: physical activity |
|
| Participants |
Inclusion criteria: BMI of 25–40 kg/m2, postmenopausal status, access to a mobile phone during the intervention and willingness to walk ≥ 30 min per day Sample size: 71; mean age: 57 years;sex: women ‐ 100%; ethnicity: white ‐ 93%, other ‐ 7% Country: USA |
|
| Interventions |
Coach group: participants assigned to the coach condition were introduced to the coach by the study facilitator. The coach was trained by the study team to offer a lifestyle intervention. She explained the intervention and offered the steps goal for the first week after reviewing the participant's baseline physical activity and time taken to complete the 1‐mile walk. Then the coach trained the participant to use the pedometer and the IVR system and identified herself as the person who would offer support during the intervention. To receive help from the coach, participants were asked to call the IVR system and leave a message for her. After the baseline visit, the participants interacted only via the telephone and IVR system. 2 daily telephone interactions with the IVR system were scheduled. The IVR system called the participant's mobile phone between 07:00 and 17:00, during a 2‐hour period identified by the participant. To minimise disruption during working hours, this call was limited to 3 questions: an assessment of whether the participant had walked or planned to walk that day, the participant's self‐efficacy to achieve the steps goal for the day and a general enquiry about whether the participant was having a good or bad day. In addition, participants called the IVR system every evening to enter their daily step count from the pedometer and receive an intervention message. During the call, they provided an assessment of self‐efficacy for walking the following day, an assessment of the present day and satisfaction with their walking plan for that day. Participants could use their mobile phone or a land‐line for the evening call The no‐coach (control) group received similar Instructions and training to the coach condition and were offered by the same individual, but with 2 exceptions: the individual did not identify herself as the coach, and participants were not informed that they had access to a coach. Participants had also access to the same technical support for problems with the IVR system or the pedometer. Thus the subjects in the no‐coach condition interacted only with the IVR system. |
|
| Outcomes | 1‐mile walk after the intervention (primary); body weight; BMI; waist and hip circumference; self‐efficacy (secondary) | |
| Funding | National Center for Research Resources: UL1RR025755 | |
| Declaration of conflict of interest | Not mentioned | |
| Power calculations for sample size | No | |
| Notes | Delivery of the intervention was both via mobile and landline; first call was initiated by the system (IVR); and the second one by participants themselves | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "At the end of this visit, participants were stratified by BMI and randomized to the coach or no‐coach condition." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Withdrawal, attrition and retention rates were not significantly different between treatment arms." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Participants in the no‐coach group had higher BMI at baseline (P = 0.29), but unclear whether this has introduced bias. |
Dedier 2014.
| Methods |
Aims: to test the ability of an automated, interactive, culturally adapted telephone exercise coach to increase physical activity and lower blood pressure in urban African Americans with poorly controlled hypertension Study design: RCT; Recruitment: primary care (mail) Study duration: 3 months; Study type: management; Study subtype: hypertension |
|
| Participants |
Inclusion criteria: sedentary, hypertensive, adults in primary care Sample size: 253; Mean age: 58 years;sex: women ‐ 73%; men ‐ 27% Ethnicity: African American ‐ 100% Country: USA |
|
| Interventions |
Participants in the intervention group received Telephone‐Linked Care for Physical Activity (TLC‐PA); computerised system that 'converses' with participants by telephone using pre‐recorded human speech Participants in the control group received usual primary care and an educational brochure on hypertension |
|
| Outcomes | Change in minutes of moderate or greater physical activity from baseline to 3 months; and change in systolic blood pressure from baseline to 3 months (primary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Participants in the control group had higher blood pressure at baseline; but unclear whether this has introduced bias. |
DeFrank 2009.
| Methods |
Aims: to compare the efficacy of 3 types of reminders in promoting annual repeat mammography screening Study design: RCT; recruitment: other ‐ health plan (mail and telephone) Study duration: 42 months; study type: prevention; study subtype: screening |
|
| Participants |
Inclusion criteria: women residents of North Carolina aged 40–75 years; were enrolled with the State Health Plan for 2 years; had their last screening mammograms (enrolment mammograms) between September 2003 and September 2004, and had only 1 mammogram in the designated timeframe (to exclude those who had diagnostic mammograms) Sample size: 3547; mean age: > 40 years; sex: women ‐ 100%; ethnicity: white ‐ 88%, black ‐ 11%, Asian, Native Hawaiian/Pacific Islander, American Indian/Alaskan Native or other ‐ 1% Country: USA |
|
| Interventions |
Participants in the intervention group received automated telephone calls by TeleVox Software, Inc, consisting of reminders 3 months prior to mammography due dates. The message was 69 seconds long and consisted of 224 words. Those who listened to ≥ 20 seconds were considered as successful contact as key message content (due for a mammogram) was delivered during this time. In total, they received 3 reminders. Call attempts were terminated after a 2‐week call window or 10 unsuccessful call attempts to reach intended recipients. Message contents included: dates of women's last mammograms; information about benefits of mammography; recommended guidelines; contact information for the National Cancer Institute's Cancer Information Service; and State Health Plan coverage The second arm received enhanced letter reminders (the same information as the other 2 reminders with several additions; additional text, informed by the Health Belief Model, about the severity of breast cancer and breast cancer susceptibility, names and telephone numbers for the facility where recipients had their last mammograms, and stickers to remind women to make and keep their mammogram appointments) The enhanced usual care group received reminders (mailed letters, included dates of women's last mammograms; information about benefits of mammography; recommended guidelines; contact information for the National Cancer Institute's Cancer Information Service; and State Health Plan coverage) |
|
| Outcomes | Mammography adherence (primary) | |
| Funding | National Cancer Institute | |
| Declaration of conflict of interest | None | |
| Power calculations for sample size | To provide 80% power to detect a 6% difference in effect among intervention arms, with alpha 0.05, the sample size required was 3545 participants | |
| Notes | This is a comparison between automated telephone reminder and enhanced usual care reminders | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Prior to study recruitment, women were assigned randomly to one of three reminder groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were intent‐to‐treat and included all study participants (n= 3547)" |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | Low risk | Comment: groups were comparable across all baseline characteristics |
DeMolles 2004.
| Methods |
Aims: to investigate the effectiveness of totally automated telephone technology in improving adherence to prescribed continuous positive airway pressure (CPAP) therapy Study design: RCT; recruitment: other ‐ home care company (telephone) Study duration: 2 months; study type: management; study subtype: obstructive sleep apnoea syndrome (OSAS) |
|
| Participants |
Inclusion criteria: English‐speaking adults, having a physician diagnosis of OSAS, and polysomnography demonstrating 15 episodes of apnoea or hypopnoea per hour of sleep Sample size: 30; mean age: 46 years; sex: * ; ethnicity: * Country: USA |
|
| Interventions |
Telephone‐linked communications technology (TLC) CPAP is based on patterns of CPAP adherence and side‐effect profiles. After receiving salutation, participants enter personal password for maintaining security and confidentiality. TLC assessed participants' frequency and duration of CPAP use during the previous week (except for the first call, in which 3 days' use were collected). In case of non‐use of the CPAP, or use for fewer than 4 h per night (on nights they used it) or fewer than 5 nights per week (or fewer than 2 nights in the case of the 3‐day call), the system proceeded to ask a series of questions aimed at identifying the cause of CPAP non‐adherence (side effects, difficulty using CPAP, lack of perceived benefit, machine malfunction). The severity of each side effect was also ascertained. For those with good adherence, TLC reinforces this behaviour. The call is initiated by participants 3 days after starting CPAP therapy (3‐day call) and thereafter weekly (1‐week call) for a total of 2 months. Calls could be made at any time of day that was convenient for the user. If participant failed to call TLC on a scheduled day, TLC called that person the next day, repeating calls periodically during a time period set with the user. If 2 days elapsed from the day of the scheduled call, the system administrator was notified automatically and informed the research assistants working on the project, who then would follow up with the participant to determine why the call was not made. TLC ascertains the severity of OSAS‐related symptoms, including snoring, breathing pauses, and daytime sleepiness. Those with OSAS symptoms, TLC recommends follow‐up with their physician as well as provide a brief counselling dialogue, focusing on appropriate CPAP use, expected benefits, correct CPAP operating technique, and potential side effects and their treatment. Reinforcement of the need for regular CPAP use was provided , stressing that regular use would reduce daytime sleepiness and could also have the additional benefit of reducing the risk of cardiovascular disease. Continuous reports including frequency and duration of CPAP use, side effects, and OSAS symptoms was sent to the physicians, biweekly or on a need basis. Participants in the control group received usual care alone. |
|
| Outcomes | CPAP use (primary); sleep symptoms checklist; functional outcomes of sleep questionnaire (secondary) | |
| Funding | VA Health Services Research and Development Service | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "At the conclusion of a baseline examination . . . eligible participants were randomised to either TLC and usual medical care or usual medical care alone." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "At baseline, intervention and usual‐care participants had similar characteristics; there were no differences at P < 0.05 level" |
Derose 2009.
| Methods |
Aims: to evaluate the effectiveness of automated systems to prompt patients with diabetes mellitus to obtain overdue laboratory tests Study design: RCT; recruitment: other ‐ health plan (mail and telephone) Study duration: 6 months; study type: management; study subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: health plan members with diabetes were passively enrolled if they met the following criteria: (1) age older than 18 years; (2) no HbA1C, low‐density lipoproteins, and urinary microalbumin tests in more than 365 days; and (3) a birthday within the next 3 months Sample size: 13,057; mean age: 51 years; sex: men ‐ 54%; women ‐ 46%; ethnicity: other or unknown – 48%, white ‐ 23%, Hispanic ‐ 14%, black ‐ 10%, Asian ‐ 5% Country: USA |
|
| Interventions | Thetelephone call group received a single call beginning with a standard greeting saying that the message to follow was from Kaiser Permanente. The message was in English and informed the recipient to call a toll‐free number to receive a message from his or her health plan. Members who called in used an interactive menu to select English or Spanish and retrieved the message by inputting their medical record number. Message content: "Telephone calls began with a standard greeting saying that the message to follow was from Kaiser Permanente. The message was in English and informed the recipient to call a toll‐free number to receive a message from his or her health plan. Members who called in used an interactive menu to select English or Spanish and retrieved the message by inputting their medical record number." The member was informed that he or she may have diabetes and was due for laboratory tests that had already been ordered. The tests were named, and the member was directed to go to his or her local health plan laboratory for the tests.The message duration was 40 s long and consisted of 100 words. Letter group received a single letter. Letter + call group received a letter followed by a telephone call at 4 weeks for non‐response. Call + letter group received a telephone call followed by a letter at 4 weeks for non‐response. Letter + call + letter group received a letter that is followed by a telephone call at 4 weeks for non‐response, followed by a second letter at 8 weeks for continued non‐response. Control group received no intervention. |
|
| Outcomes | Adherence to all 3 laboratory tests (glycated haemoglobin, low‐density lipoproteins, and urinary microalbumin) by 12 weeks (primary) | |
| Funding | Merck Health Management Services | |
| Declaration of conflict of interest | None | |
| Power calculations for sample size | Aimed for 90% power to detect a difference between 35% (call group) and 40% (call + letter group), which required 2008 participants per group | |
| Notes | This is a comparison between telephone call group and control | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computerised random number generator was used |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All subjects' data were analysed according to initial randomisation whether the subject was successfully contacted or was lost to follow‐up" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "Randomization resulted in small but statistically significant (P = .002) differences in the distribution of race/ethnicity across study arms. There were no significant (P < .05) differences in the distribution of other subject characteristics across study arms." |
Derose 2013.
| Methods |
Aim: to evaluate an automated system to decrease primary non‐adherence to statins for lowering cholesterol Study design: RCT; recruitment: other ‐ health plan (organisational referral) Study duration: 10 weeks; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: ≥ 1 years of membership from the prescription date and no gap in enrolment more than 30 days during the past year; 24 years and older at the time of the prescription; no record of the statin prescription being filled at a health plan pharmacy after 1 to 2 weeks. Sample size: 5216; mean age: 56 years;sex: women ‐ 51%; men ‐ 49% ethnicity: white ‐ 28%, black ‐ 10%, Hispanic ‐ 30%, Asian and Pacific Islander ‐ 7%, other ‐ 2%, unknown ‐ 23% Country: USA |
|
| Interventions |
ATCS Plus: participants were contacted 1 to 2 weeks after the prescription date by an automated telephone call to retrieve a personalised message from the health plan. If no one answered, messages were left on answering machines directing participants to call a toll‐free number to retrieve their message. Busy signals resulted in up to 2 more attempts to make telephone contact on subsequent days. Calls were made between 10 am and 8 pm. 1 week after the initiation of calls, participants who still did not fill their prescription were sent a letter. The letters were expected to arrive 9 to 11 days after the first outreach contact by telephone. More than 95% of all health plan members have a telephone number on record, and more than 99% have an address. Telephone calls began with a standard greeting saying that the message was from Kaiser Permanente. The message could be retrieved through interactive messaging during the call or by dialling a toll‐free number. The personalised message conveyed that a statin drug was prescribed by their clinician and there was no record of the drug being dispensed by health plan pharmacies. The potential importance of the medication was described, and participants were encouraged to either have the prescription filled or contact the prescribing physician. The contact number of the local health plan pharmacy was provided. The telephone message was accessed in either English or Spanish and was approximately 40 seconds in duration. The letter was printed on one side in English and the other side in Spanish, and the text occupied approximately half a page. Letters were signed using the prescribing physician's name, a standard outreach practice in the health plan Control group received usual care (no calls) |
|
| Outcomes | Medication (statins) adherence (primary) | |
| Funding | Merck Sharp & Dohme Corp, a subsidiary of Merck & Co Inc, Whitehouse Station, New Jersey | |
| Declaration of conflict of interest | Ms Marrett is an employee of Merck. Dr Tunceli is an employee of Merck and owns stock in the company | |
| Power calculations for sample size | We aimed for sufficient power to detect a 5% difference in adherence between the study arms based on a response rate of 20% in the control arm. Use of a significance level of 0.05, 90% power, a 2‐sided test of proportions, and equal‐sized groups required 1504 participants per group | |
| Notes | Quote: "Although a detailed cost analysis was not attempted, the marginal costs of the telephone calls and mailings were approximately USD 1.70 per person" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A study programmer used computer‐generated random numbers to sort participants into the intervention and control groups in equal proportion (day 0)." |
| Allocation concealment (selection bias) | Low risk | Quote:"Assignment was concealed from study investigators and analysts. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All participants' data were analysed according to initial randomisation (intent‐to‐treat) whether or not the participant was successfully contacted." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | No statistically significant differences were noted between groups at baseline |
Dini 1995.
| Methods |
Aims: to evaluate the effectiveness of computer generated telephone reminder calls in increasing kept appointment rates in a public health setting Study design: quasi‐RCT; recruitment: primary care (organisational referral) Study duration: 1 month; study type: either; subtype: appointment reminder |
|
| Participants |
Inclusion criteria: all clients with scheduled appointments for any of 4 public health programmes (immunisation, well child, or family planning) at the health clinic were eligible for participation Sample size: 517; mean age: * sex: * ethnicity: * Country: USA |
|
| Interventions |
Computer‐generated telephone reminder: households of clients received 1 of 4 automated telephone messages specific to the programme for which the clients had an appointment. The messages were delivered between 6 pm and 9 pm on the evening preceding the scheduled appointments. Up to 9 attempts was made in order to get a successful contact Participants in the control group did not receive reminders (no intervention) |
|
| Outcomes | Appointment adherence (primary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | The cost per additional appointment kept was USD 5.20 during the first full year of operation and USD 1.04 for subsequent years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Clients with last names beginning with the letters A through L were as signed to receive a computer‐generated telephone reminder message during the evening prior to their scheduled appointment. Clients with last names beginning with the letters M through were designated as controls and did not receive a reminder message." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Dini 2000.
| Methods |
Aims: to assess the sustained impact of computer generated messages on immunisation coverage during the first 2 years of life Study design: RCT; recruitment: primary care (organisational referral) Study duration: 36 months; study type: prevention; study subtype: immunisation |
|
| Participants |
Inclusion criteria: all children who were 60 to 90 days of age, who had received the first dose of diphtheria‐tetanus‐pertussis or poliovirus (PV) vaccines, and who had telephone numbers listed in the pre‐existing computerised health department database Sample size: 1227 mean age: * sex: * ethnicity: * Country: USA |
|
| Interventions |
Telephone messages alone received 1 telephone reminder message prior to the scheduled immunisation date and up to 4 telephone recall messages (1/week) over the 4‐week period following the due date. Contacts were made during weekday evening hours between 6:00 pm and 9:00 pm and on Saturdays from noon to 8:00 pm (up to 5 messages) Telephone messages + letters (up to 5 messages and/or letters) Letters only (up to 5 letters) No notification control |
|
| Outcomes | Immunisation series completion at 24 months of age (primary); acceptability and costs (secondary) | |
| Funding | National Immunisation Programme, CDC | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | Target sample size was 1200 | |
| Notes | Costs per month (and per year) were as follows: telephone messages alone, USD 139 (USD 1672); telephone messages + letter, USD 126 (USD 1518); and letters only, USD 66 (USD 796). There were no cost‐effectiveness data available for no notification control group. This is a comparison between the telephone messages alone and control groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Children enrolled in the evaluation were randomised to receive telephone messages followed by letters (Group A); telephone messages alone (Group B); letters only (Group C); or no notification (Group D)." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "No significant differences were noted between groups with regard to sex (p = 0.12), number of children in the household (p = 0.69), or whether children were insured by Medicaid (p = 0.72). However, significant ethnic and language differences were noted between groups." Insufficient evidence that this imbalance has introduced bias. |
Dubbert 2002.
| Methods |
Aims: to test a hypothesis that participants who received telephone follow‐up nurse counselling would report greater adherence to the walking goals than participants who received no follow‐up calls, and those who received personal calls would report greater adherence than participants receiving a mixture of personal and automated calls Study design: RCT; recruitment: primary care (mail) Study duration: 12 months; study type: prevention; subtype: physical activity |
|
| Participants |
Inclusion criteria: 60–80 years of age, enrolled in primary care clinic, non‐institutionalised and independent in activities of daily living, stable health, willing to increase walking for exercise and attend research clinic visits, and satisfactory performance on a 6‐minute walking test Sample size: 181; mean age: 69 years; sex: men ‐ 99%; women ‐ 1%; ethnicity: * Country: USA |
|
| Interventions |
20 personal phone calls delivered by a nurse Multimodal intervention received 10 personal phone calls from the nurse interspersed randomly with 10 automated phone calls (P&AC) that delivered a message recorded by the nurse. Automated calls were phased in beginning with month 2. The schedule of calls was not predictable. Automated calls, designed to maintain contact and cue walking in an inexpensive and efficient manner, delivered a brief message recorded by the nurse such as, "This is your STEPS nurse reminding you to keep up your walking . . . the weather is hot now so be sure to drink plenty of water." These were delivered by a Phone Tree (Personal Communication Systems, Winston‐Salem, NC). Control received no phone calls. |
|
| Outcomes | Self‐reported (diary) walking adherence (primary); quality of life (secondary) | |
| Funding | Department of Veterans Affairs Health Services Research and Development Service | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between the multimodal intervention and control. There was no evidence of a pattern of increased risk associated with increased walking (the intervention effect). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After the intervention components common to all participants were completed, they were randomised to one of the three groups for different telephone follow‐up interventions" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The data collector was blinded to intervention group assignment and at the end of the trial was unable to guess individual patient group assignment better than what would be predicted by chance. The nurse was blinded to walking diary adherence data and other self‐report follow‐up data" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate; missing outcome data balanced in numbers, with similar reasons for missing data across groups. Quote: "Only 31 (15%) of the 212 randomised participants failed to complete the 12‐month trial." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "BL participant characteristics were not different between any of the three treatment groups"; however participants in complex intervention arm had lower educational status; were living in rural area; and smoked more cigarettes than participants in the other 2 groups. There is insufficient evidence that this imbalance has introduced bias. |
Durant 2014.
| Methods |
Aims: to develop a methodology that stratifies members by likelihood of completing a colorectal cancer screening Study design: RCT; recruitment: other ‐ insurance company (organisational referral) Study duration: 3 months; study type: prevention; study subtype: screening |
|
| Participants |
Inclusion criteria: members of an insurance plan from Horizon Blue Cross Blue Shield of New Jersey eligible for colorectal cancer screening Sample size: 47,097; mean age: 58 years;sex: women ‐ 53%; men ‐ 47%; ethnicity:* Country: USA |
|
| Interventions |
Participants in the IVR group received 1 call with varying messaging. Depending on the number of non‐adherent members and the segments' health descriptions, an outreach segment may contain ≥ 1 model segments Participants in the control group received no calls |
|
| Outcomes | Receipt of colorectal cancer screening at 3 months (primary); costs (secondary) | |
| Funding | Silverlink Communications | |
| Declaration of conflict of interest | Drs Durant and Newsom are employees of Silverlink Communications, have attended meetings and conferences for the company, and own stock options. Dr Berger is an employee of Silverlink Communications. Dr Pomerantz is an employee of Horizon Blue Cross Blue Shield of New Jersey. Ms Rubin has no financial interests to disclose. | |
| Power calculations for sample size | A power analysis was performed before the launch of the intervention to determine the minimal size needed for each segment, given an estimated effect size of 2% increase for each graded segment and an α level = .05 | |
| Notes | Authors of this study were contacted for unpublished analyses on 14 June 2015. The authors were seeking approval to share data. Communication cost per screening was USD 14.84. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Another 400 members per outreach segment were randomly assigned to a control group and received no communication." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | High risk | Quote: "Given that the sizes of the segmented groups were determined by the insurer's nonadherent population and not via a recruitment method, it was determined at the launch of the communication that the comparison of the completion rate of segment 4 and segment 5 was underpowered given the segment sizes and the estimated effect size" |
Ershoff 1999.
| Methods |
Aims: to develop and evaluate cost‐effective intervention strategies for pregnant smokers with diverse demographic and smoking related characteristics Study design: RCT; recruitment: other ‐ health plan (telephone) Study duration: 34 weeks; study type: management; study subtype: smoking |
|
| Participants |
Inclusion criteria: English‐speaking women 18 years of age or older who self‐reported to be active smokers at their initial prenatal appointment Sample size: 332; mean age: 30 years; sex: women ‐ 100%; ethnicity: white ‐ 61%, black ‐ 16%, Hispanic ‐ 15%, other – 8% Country: USA |
|
| Interventions |
IVR. Women assigned to this group were sent Living Smoke‐Free and had access to a computerised interactive telephone support system developed with InfoMedics. Subjects were mailed an informational brochure and provided a unique identification number and password to gain access to the system. A subsequent 10‐minute telephone call from a health educator answered questions and provided further details on use of the system. Using a touch‐tone telephone, subjects could access the IVR programme with a toll‐free number 7 days a week, 24 h a day. Upon calling the system, subjects were asked a series of questions about their smoking behaviour, beliefs, and readiness to change. Users provided answers through their touch‐tone telephone keypad. In response, the programme provided stage‐appropriate customised messages recorded by a professional voice model. With stored data from previous calls, the programme automatically reinforced any positive changes made by a smoker over time (e.g. a reduction of > 25% in number of cigarettes smoked per day, a decision to set a quit date). Each call was designed to be approximately 5 min in length and included stage relevant interactive exercises, a summary and reinforcement of key messages and goal commitments, and advice to review Living Smoke‐Free Motivational interviewing (MI). Women assigned to the MI group were sent Living Smoke‐Free and were provided telephone counselling by nurse educators trained in the techniques of MI. MI has been defined as a "directive, client‐centred counselling style for helping clients explore and resolve ambivalence about behaviour change." It emerged as an alternative to direct persuasion in counselling people with addictive problems. MI conceptualises motivation as a state that fluctuates from time to time or situation to situation, rather than as an inherent character trait. Thus, motivation is perceived as open to therapeutic intervention. The dangers of prenatal smoking have been widely disseminated and pregnant women report strong belief in that harm. MI attempts to highlight and help resolve ambivalence resulting from the discrepancy between beliefs and behaviour through reflection, advice, and support. Investigators trained 17 preterm nurse educators experienced in telephone‐based patient counselling in the principles and strategies of MI. The training consisted of a 6‐hour session led by nationally‐known experts, a 2‐hour small‐group meeting, and an 85‐page reference manual with salary support for up to 8 h of self‐study. Booklet only. Women assigned to this group only received Living Smoke‐Free. The multicolour, 32‐page booklet was developed by the investigators in collaboration with Krames Communications, a Division of the StayWell Co. Targeted to the lifestyle of pregnant smokers, it is printed in clear type and written at an eighth‐grade reading level. Multiracial/ethnic illustrations of smokers were designed to appeal to a wide audience of pregnant women. Visual and written messages tailored to stage of readiness to change are presented through 4 different characters, each representing a different stage. The booklet includes advice about preparing to quit, setting a quit date, methods for quitting, obtaining social support, and relapse prevention strategies. Advice about exercise, diet, and stress management are also included. |
|
| Outcomes | Smoking abstinence (biochemically confirmed); satisfaction with the intervention (secondary) | |
| Funding | Robert Wood Johnson Foundation | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | At alpha set at 0.05 and power at 0.80 (1‐tailed test), 125 participants per group were needed to detect the 13% difference in quit rates projected for the booklet‐only versus IVR comparison | |
| Notes | This is a comparison between IVR arm and booklet arm only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After random assignment to one of the three intervention groups . . . subjects were mailed a copy of the self‐help smoking cessation booklet, Living Smoke‐Free—A Healthier Start for You and Your Baby." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Providers were blind to study participation and group assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only participants who remained in the intervention were included in the final analysis. Although the reasons for attrition such as abortion/miscarriage (n = 31), disenrollment from the health plan prior to delivery (n = 22), and delivery prior to the 32nd week of pregnancy (n = 5) were reported. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "No statistically significant differences were observed for any baseline measures" |
Estabrooks 2008.
| Methods |
Aims: to determine the feasibility and effectiveness of automated telephone support calls targeting physical activity and healthful eating as strategies for weight loss for patients with pre‐diabetes. Study design: RCT; recruitment: other ‐ community (in‐person during diabetes prevention classes) Study duration: 12 weeks; study type: prevention; subtype: weight management |
|
| Participants |
Inclusion criteria: adults participating in diabetes prevention class, English‐speaking, not pregnant during the study period, had access to a telephone, and were not concurrently enrolled in another research study involving diabetes management or weight management. Sample size: 77; mean age: 59 years; sex: men ‐ 39%, women ‐ 71%; ethnicity: white ‐ 68%, Hispanic ‐ 18%, other or unknown ‐ 7%, black ‐ 4%, Asian ‐ 3% Country: USA |
|
| Interventions |
Participants in the intervention group received IVR calls that were designed to address and reinforce the messages delivered in the pre‐diabetes class and the content of the participant action plans. Participants had the option to choose to listen to messages related to either nutrition or physical activity, followed by behaviour change techniques between goal‐setting and self‐monitoring. Received 7 counselling calls lasting 5‐10 min while 5 calls provided either physical activity or nutrition tip, that lasted for a minute. Participants in the control group did not receive calls (no intervention). |
|
| Outcomes | Physical activity; dietary habits; weight (percent lost) (primary); satisfaction (secondary) | |
| Funding | Department of Prevention at Kaiser Permanente Colorado | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | ClinicalTrials.gov Identifier: NCT00384488 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization occurred at the class‐level and was completed by a research assistant who chose a slip of paper with study group assignment from a hat" |
| Allocation concealment (selection bias) | Low risk | Study participants were not informed of the study arm until they completed the informed consent as to not influence the decision to participate |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "While research staff was unblinded to study arm designation, study participants were not informed of the study arm until they completed the informed consent as to not influence the decision to participate". |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no differences in dropout rate between study conditions. |
| Selective reporting (reporting bias) | Low risk | The protocol was available, and all outcomes of interest were reported. |
| Other bias | Low risk | Groups were balanced at baseline. |
Estabrooks 2009.
| Methods |
Aims: to determine the effectiveness of automated telephone counselling to support parents of overweight or at‐risk children to change the home environment to foster more healthful child eating and activity behaviours, thereby reducing child BMI and BMI z‐scores Study design: RCT; recruitment: * (telephone) Study duration: 12 months; study type: prevention; subtype: weight management |
|
| Participants |
Inclusion criteria: children aged 8–12 years with a BMI of 85th percentile for their age who received care from Kaiser Permanente Colorado Sample size: 220; mean age: 11 years; sex: boys ‐ 54%; girls ‐ 46%; ethnicity: white ‐ 63%, Hispanic ‐ 26%, other – 11% Country: USA |
|
| Interventions |
The Family Connections (FC) IVR group received 10 calls, 1st call a week after the group session, the call contents were tailored to participants responses using logic branching method. Calls can be initiated by either the system or the participant. At each call, the goals set in the previous week are assessed, and participants hear related tips and then select specific messages. Calls concluded with a goal setting procedure. The 6th IVR‐counselling call provided parents with instruction on a family goal‐setting procedure related to physical activity and eating based on the 5A's model. Calls 7–10 reinforced the information delivered in the initial 6 calls. FC workbook. A 61‐page workbook was developed to promote increased physical activity and the consumption of fruits and vegetables in concert with decreased sugared‐drink consumption and television viewing/recreational computer time. The workbook included 2 distinct sections. Part 1 targeted 3 days of intervention, and part 2 targeted 2 days, each with specific homework assignments. The workbook encouraged parents to complete 5 days of intervention across a single week. Homework assignments were intended to encourage lasting changes in the families. All parents randomly assigned to this intervention received the workbook from study research assistants FC group. This intervention consisted of 2 small‐group sessions (2 h each, spaced 1 week apart) held at a local clinic and delivered by a dietitian. Each session included 10–15 parents representing distinct children and utilised the Family Connections workbook. The first session focused on parents' behavioural health skills and knowledge of weight, nutrition, and physical activity. It also identified key parenting skills: limit setting, effective communication, and role modelling. This session concluded with role playing, problem‐solving, and the development of an action plan. Session 2 integrated the knowledge acquired in Session 1, the experiences associated with the action plan, and strategies for restructuring the home environment. The session again concluded with parents' completing an action plan for parental behaviours, role modelling, and changes to the home environment that would facilitate healthy eating and physical activity |
|
| Outcomes | BMI z‐score, physical activity; sedentary behaviour; dietary habits (primary) | |
| Funding | Garfield Memorial Fund, Kaiser Permanente Colorado Weight Management Program | |
| Declaration of conflict of interest | None | |
| Power calculations for sample size | Sample size calculations were completed, varying the detectable effect sizes from small to medium with a power of 0.8. The result was a need for 42 participants per intervention to detect a medium effect and 64 participants to detect a small effect | |
| Notes | This is a comparison between FC IVR group and FC group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Through a random‐numbers table, participants were assigned randomly . . . to the FC‐workbook, the FC‐group, or the FC‐IVR intervention." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers across groups. ITT analysis was used to include all participants who received the intervention or FC workbook in the analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were balanced at baseline. Quote: "The intervention conditions did not differ on any demographic variables." |
Farzanfar 2011.
| Methods |
Aims: to test the feasibility and impact of an automated workplace mental health assessment and intervention Study design: RCT; Recruitment: primary care (advert in clinic) Study duration: 6 months; study type: management; subtype: mental health |
|
| Participants |
Inclusion criteria: ability to speak and understand conversational English, 18 years of age or older, access to a touch‐tone telephone, not undergoing mental health treatment or currently taking a medication prescribed for mental health treatment, and experiencing some type of emotional distress as indicated by scoring positive on the WHO‐5 Well‐being Index and the Functional Impairment question Sample size: 164; mean age: 39 years; sex: men ‐ 24%, women ‐ 76%; ethnicity: white ‐ 56%, black/African American ‐ 32%, other – 12% Country: USA |
|
| Interventions |
Telephone‐Linked Communications (TLC) detect system is an automated mental health screening and counselling programme that employees could access from any phone. The assessment is made in a hierarchical manner. Those testing positive proceed to 2nd level of more disorder‐specific and in‐depth screening by additional screening instruments. This provides extensive information about user's mental health problem, including its symptoms, natural history, and available treatments. It also directs the user to the referral sub‐module providing disorder‐specific information on both self‐management and professional help appropriate to the level of its severity as determined by the system's assessment. Follow‐up calls were used to check user's adherence to the system's advice and to check if they had sought professional assistance or engaged in self‐help. For those who did not adhere, an intervention follow‐up module provided tailored educational materials, including description of the disorder and providing treatment options. Both intervention and follow‐up calls provided an option to spread out the information into multiple sessions to reduce the time burden. This also included a validation function that checked whether the health care providers agreed with the system's assessment. Each call lasted between 30‐90 min. The calls used digitised voice of a female voice actor who received coaching to deliver the message appropriately Participants in the control group received advice only (via IVR) |
|
| Outcomes | Quality of life (physical health scale and mental health scale), total depression, perceived stress levels/score, total well‐being (WHO‐5) (primary); acceptability of service/satisfaction (secondary) | |
| Funding | CDC | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After eligibility screening, baseline data were collected from study participants, who were subsequently randomised and connected to the automated program to receive assessment for mental health disorders (all subjects) and intervention (only experimental subjects)." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis was used to include all participants who received the intervention or control group in the analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "There were no significant demographic differences between the two study groups at baseline" |
Feldstein 2006.
| Methods |
Aims: to evaluate interventions to improve laboratory monitoring at initiation of medication therapy Study design: cluster RCT with 15 clusters; recruitment: other ‐ health plan (organisational referral) Study duration: 25 days study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: adults aged 18 years & above; spoke English; had continuous HMO membership for ≥ 12 months, a pharmacy benefit,and a telephone number; had received a new prescription of a study medication from their PCP; and had not had recommended baseline laboratory monitoring within 5 days after the medication dispensing Sample size: 961; mean age: 59 years; sex: men ‐ 47%; women ‐ 53 %; ethnicity:* Country: USA |
|
| Interventions |
Automated telephone voice message (AVM): AVM prompted participants to seek preordered laboratory tests. A personalised message retrieved after entering a health record number and year of birth stated that the medication the participant had been dispensed required laboratory monitoring; messages referenced the actual drug dispensed and the monitoring tests required. The participant was advised that the testing had been ordered and could be completed at any health maintenance organisations laboratory The EMR intervention consisted of a participant‐specific electronic message to the PCP from the chair of the participant safety committee. The message stated that computer records indicated that the participant had been dispensed a new medication, laboratory monitoring was recommended, and the participant had not received the test(s) between 6 months before and 5 days after the dispensing. The message referenced internal and external guideline resources, recommended specific tests, and provided a sample letter the PCP could send to the participant to request that he or she go to the laboratory. Pharmacy Team Outreach Intervention began with a telephone call from a nurse in the pharmacy department to the participant to encourage laboratory testing. If the nurse successfully contacted the participant, a follow‐up letter reminded the participant to obtain the laboratory test(s). If telephone contact was not successful, the nurse sent a letter suggesting that the participant go in for testing. If participants had questions or concerns about their medication during the contacts, a pharmacist was available for consultation. Usual care (controls) |
|
| Outcomes | Completion of all recommended baseline laboratory tests (primary) | |
| Funding | This project was supported by Kaiser Permanente's Garfield Memorial Fund and cooperative agreement U18 HS010391 from the Agency for Healthcare Research and Quality | |
| Declaration of conflict of interest | None reported | |
| Power calculations for sample size | "Using retrospective data, we estimated that 25% of the UC group would receive laboratory testing by 30 days after a new medication was dispensed. With 200 participants per group, we determined that we could detect a difference of approximately 13% between the groups with a probability of 0.80." | |
| Notes | This is a comparison between the AVM arm versus usual care. 3 clusters (267 participants) were allocated to AVM and 4 clusters (237 participants) to usual care; remaining clusters (n = 8) were arms not considered in this review. Note that analysis did not appear to adjust for clustering; therefore a unit of analysis error exists that may result in overly precise effect estimates for this study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The random sequence was generated by a computerized random‐number generator" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "All 15 clinics were randomised at one time; therefore, allocation concealment was not an issue." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Patient participants were masked from the nature of the study. Because of the nature of the intervention, the study nurse conducting the interventions was not blinded to group assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Primary outcomes were obtained entirely from electronic records, and the study analyst was blinded to study group assignment before ascertainment of outcomes." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "No patients were lost to follow‐up." |
| Selective reporting (reporting bias) | Low risk | Outcomes of interest reported |
| Other bias | Unclear risk | There was a small baseline imbalance, but it is unlikely that this influenced the results. Quote: "The other characteristics of the study groups were also similar except that the AVM group had a smaller proportion of female PCPs". There was insufficient information to judge whether selective recruitment of cluster participants may have occurred. |
Fiscella 2011.
| Methods |
Aim: to examine the impact of a multimodal intervention on mammography and colorectal cancer screening rates in a safety‐net practice caring for underserved patients Study design: RCT; recruitment: primary care (health professional referral) Study duration: 12 months; study type: prevention; subtype: screening |
|
| Participants |
Inclusion criteria: registered patient at the practice; (≥ 1 visit to the practice in the past 2 years (to ensure participants were actively receiving care at the practice); aged 40‐75 years for mammography screening, and 50‐75 years for colorectal cancer screening; past due for annual mammography or colorectal cancer screening (recommended intervals are 10 years for those screened through colonoscopy, 5 years for those screened with sigmoidoscopy and/or barium enema, and annually for those screened through faecal occult blood tests). Sample size: 469; mean age: *; sex: women ‐ 56%; men ‐ 44% (for colorectal cancer); ethnicity: white ‐ 61%; black/African Amercian ‐ 28%; Hispanic ‐ 5%; Asian ‐ 5% Country: USA |
|
| Interventions |
Multimodal intervention: outreach to unscreened participants consisted of 2 personalised letters and up to 4 automated telephone reminder (ATR) calls. The automated telephone reminders were scripted, pre‐recorded messages that include the participant's first name. The message identified the callers and the practices; it then informed the participants they were past due and the phone number to call to schedule a screening (mammography) or an appointment (to discuss colorectal cancer). The first letter was sent within the first week of enrolment. This was followed by 2 completed ATRs at week 2 and 6. For participants who remain unscreened, a second letter was mailed out at week 12 followed by a third ATR at week 14. For participants past due for colorectal cancer screening, the letter included a testing kit for faecal immunochemical testing for home use. A final ATR was made at week 26. Both the letters and ATRs provided the phone number of the outreach worker if help is needed. Using a 3‐way call option, the outreach worker could link participants with mammography schedulers or with the National Breast and Cervical Cancer Early Detection Program (NBCCEP), which provides free screening for the uninsured. The intervention also included participant and physicians prompts. Participants in the control group received usual care (chart review). |
|
| Outcomes | Chart documentation of breast cancer screening, colorectal cancer screening, or both (primary) | |
| Funding | RSGT‐08‐077‐01‐CPHPS American Cancer Society | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | 80% power to detect a difference of 18% in the mammography group and 13% in the colorectal screening group using 95% confidence intervals has been calculated | |
| Notes | Clinicaltrials.gov Identifier: NCT00818857 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was stratified by screening type (mammography or colorectal cancer) to ensure that comparable groups of patients are randomised to each arm." |
| Allocation concealment (selection bias) | Low risk | Quote: "Unique ID numbers were assigned to patients that identify their intervention group." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The statistician maintained the key; all other study personnel were blinded to the intervention group assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Baseline and follow‐up measures were taken by a research assistant who is blinded to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quuote: "We adopted an intention‐to‐treat analysis. That is, all patients originally assigned to a group were analysed." |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all outcomes of interest have been reported in the pre‐specified way. |
| Other bias | Unclear risk | Quote: "There was no statistically significant baseline difference between the intervention and control groups for the mammography intervention. Race was the only characteristic that differed between participants at baseline between those in the intervention and control groups in the colorectal cancer group" |
Fortuna 2014.
| Methods |
Aims: to assess the relative impact of various components of the reminder, recall, and outreach (RRO) model on breast cancer and colorectal cancer screening rates within a safety net practice Study design: RCT; recruitment: primary care (mail) Study duration: 12 months; study type: prevention; study subtype: screening |
|
| Participants |
Inclusion criteria: being a registered patient at the study clinic; being an active patient at the practice (having ≥ 1 visit to the practice in the last 2 years); women aged 40–74 for breast cancer screening; aged 50 to 74 for colorectal cancer screening; past due for breast cancer or colorectal cancer screening Sample size: 1008; mean age: inestimable;sex: women ‐ 55%; men ‐ 45% ethnicity: non‐Hispanic white ‐ 48%, non‐Hispanic black ‐ 37%, other (including Hispanic) – 15% Country: USA |
|
| Interventions |
Letter and automated telephone message (letter + autodial) group received the letter plus a series of up to 5 automated telephone calls. Investigators used the participants' most current available telephone numbers from the medical record. Telephone calls were attempted for up to 2 weeks at varying times throughout the day/evening until a person or an answering machine responded. The automated message contained similar information to the letter, with instructions to call the outreach worker or the practice to arrange for screening or with questions. These calls were delivered to participants on weeks 2 and 8 following randomisation. Until there was documented screening, chart reviews were performed on weeks 12 and 26. Automated telephone messages were repeated on weeks 14, 28, and 38 for participants remaining unscreened at these time periods. Letter + autodial + prompt group received the same intervention as above plus paper prompts delivered at the time of a participant‐initiated visit. We used paper prompts because this enabled us to deliver similar prompts to participants and clinicians simultaneously, and because of doubts regarding effects of electronic prompts on clinician screening. Research staff reviewed scheduling modules weekly to check for planned acute and preventive visits by participants in this group. Prompts were delivered to the treating clinician at the point of care to remind the participant and provider about overdue screening. Prompts were provided at both acute and preventive visits. The back of each colorectal cancer prompt sheet summarised advantages and limitations for colorectal cancer screening modalities as a way of facilitating clinician–participant discussion. The prompt addressed both colonoscopy and faecal immunochemical tests. Letter + personal call group received the letter plus a personal telephone call from a trained outreach worker. These telephone calls were attempted up to 3 times, at varying times of the day and varying days of the week, with a 1‐week period between attempts. When/if the participant was reached, the outreach worker explained that she was calling on behalf of the practice to remind the participant that s/he was overdue for cancer screening. She used motivational interviewing principles to encourage screening and offered assistance with scheduling an appointment, as well as relevant telephone numbers and logistical assistance, including referral(s) for free mammography and faecal immunochemical test for the uninsured. Participants that did not want to undergo a colonoscopy were offered a mailed faecal immunochemical test as an alternative method of colorectal cancer screening. If a participant refused to have any screening tests done for breast cancer or colorectal cancer, it was indicated in the patient registry and interventions were stopped Reminder letter. A single letter from the practice using the participant's most current available home address from the medical record. The letter, with a personalised salutation, indicated to the participant that s/he was overdue for screening and included information regarding the importance of screening and how to schedule screening. The letter provided the name and telephone number of the outreach worker available to provide assistance with scheduling mammography or arranging colonoscopy referrals. The letter also indicated that free screening for uninsured/underinsured participants was available through a state sponsored programme. Letters were available in English and Spanish. |
|
| Outcomes | Electronic medical records documentation of mammography screening at 52 weeks (primary) | |
| Funding | American Cancer Society ‐ RSGT‐08‐077‐01‐CPHPS | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | No | |
| Notes | This is a comparison between letter + autodial group versus letter only (control) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computerised random number generator (random number algorithm, stratified by the type of screening(s) was used |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was concealed … An offsite study statistician, who was blinded to the identity of the patient, assigned participants equally into one of the four intervention groups" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of study personnel was ensured. Quote: "Healthcare personnel and study staff were unaware of group assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "All subjects were analysed in the originally assigned study group, based on intention‐to‐treat" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were balanced at baseline. Quote: "There were no significant differences in participants at baseline between the four intervention groups" |
Franzini 2000.
| Methods |
Aims: to measure the efficacy of reminder/recall systems (manual postcard or a computer generated phone message) in private provider offices through collection of return visits and vaccine delivery rates Study design: cluster RCT with 6 clusters; recruitment: primary care (organisational referral) Study duration: *; study type: prevention; subtype: immunisation |
|
| Participants |
Inclusion criteria: children < 12 months of age and eligible for first, second, or third diphtheria‐tetanus‐pertussis vaccine Sample size: 1138; mean age: *; sex: *; ethnicity: * Country: USA |
|
| Interventions |
Autodialer: participants received an automated reminder message about their upcoming visits for immunisation 7 days prior to the appointment The mailing arm received a postcard reminder 7 days prior to the appointment. No calls (control) |
|
| Outcomes | Immunisation status; cost‐effectiveness (both primary) | |
| Funding | Association of Teachers of Preventive Medicine, National Centers for Disease Control, National Immunisation Program | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between Autodialer and control; 295 participants in mailing arm were not included in the review. Note that analysis did not appear to adjust for clustering; therefore a unit of analysis error exists that may result in overly precise effect estimates for this study. The average cost per child in the Autodialer (intervention) group was USD 15.46 and in the control the average cost per child was USD 11.46. These do not include start‐up costs. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Sites were randomly assigned to one of three arms of the study: mail, Autodialer, or control" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | There was insufficient information reported to allow an assessment of whether cluster participants were selectively recruited. Baseline imbalances may have existed, quote, "With the exception of age, demographic characteristics of the sites were not uniform." |
Friedman 1996.
| Methods |
Aims: to assess the impact of telecommunication system on antihypertensive medication adherence and blood pressure control Study design: RCT; recruitment: community centres (mail and telephone) Study duration: 6 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: aged 60 years and above, be under the care of a physician for hypertension, and be prescribed antihypertensive medication Sample size: 267; mean age: 76 years; sex: men ‐ 23%, women ‐ 77%; ethnicity: other – 89%, black ‐ 11% |
|
| Interventions |
The Telephone‐Linked Computer (TLC) system is an interactive computer‐based telecommunications system that is totally automated and carries out telephone conversations with hypertension patients in their homes for the purpose of monitoring their blood pressure and treatment, and counselling them to be adherent to their medication regimens. TLC speaks to participants over the telephone using computer‐controlled speech while the participants communicate using the touch‐tone keypad on their telephones. TLC applications promoted self‐efficacy by setting small incremental goals and by providing positive feedback and reinforcement regarding the users' actions. During the conversation, participants reported their blood pressure, their understanding of their prescribed antihypertensive medication regimen (medication names, dosages, and frequency of administration), their adherence to the medication regimen, and whether they had symptoms known to be side effects of their antihypertensive medications. TLC provided education and motivational counselling to improve medication adherence. At the end of the conversation, the information provided by the participant was stored in a database and was transmitted to the participant's physician on a printed report in which data was displayed over time and clinically significant information was highlighted. Calls can be initiated by either TLC or the user, and are made once weekly, each lasting for 4 min. Participants also received training to use TLC and an automated sphygmomanometer. Participants in this group continued to receive usual care Participants in the control group received usual care alone |
|
| Outcomes | Change in antihypertensive medication adherence (primary); systolic blood pressure and diastolic blood pressure during 6 months (primary); satisfaction (participants and physicians); cost‐effectiveness (both secondary) | |
| Funding | National Heart, Lung and Blood Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | The system was cost‐effective, especially for non‐adherent participant users ‐ USD 3.69 per 1 mmHg improvement in diastolic blood pressure at 80% baseline adherence to USD 0.87 per 1 mmHg improvement at 50% adherence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "During the home visit a trained field technician confirmed final eligibility and completed baseline measurements, after which participants were randomly assigned to either the TLC or usual care groups using a paired randomisation protocol." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blindig of personnel ensured. Quote: "All participants received a final home visit 6 months after entry into the study when all study measurements were re‐administered by technicians blinded to the study assignments." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers, with similar reasons for missing data across groups. Quote: "There were no significant differences in the characteristics of TLC users and nonusers who dropped out of the study" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | There was no statistically significant difference in any characteristic between individuals randomised to TLC or to usual care. |
Glanz 2012.
| Methods |
Aims: to determine the efficacy of an automated, interactive, telephone‐based health communication intervention for improving glaucoma treatment adherence among patients in 2 hospital‐based eye clinics Study design: RCT; recruitment: secondary care (mail and telephone) Study duration:12 months; study type: management; study subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: treatment for their eye condition at 1 of the 2 participating eye clinics; aged 18‐80 years; white or black/African American; have a home or cellular telephone; speak and understand English; be diagnosed with glaucoma or ocular hypertension for ≥ 1 year; be prescribed daily doses of topical glaucoma treatments for at least the past year; no eye surgery within the past 3 months; have better than 20/200 vision in at least 1 eye; and be able to read or have someone who can help them with reading printed materials. Participants also had to acknowledge non‐adherence, in the past year, with medication taking, obtaining refills or clinic appointments in a screening interview Sample size: 312; mean age: 63 years;sex: women ‐ 37.5%; men ‐ 62.5% ethnicity: white ‐ 9%; black/African American ‐ 91%. Country: USA |
|
| Interventions |
Automated, interactive, telephone‐based health communication intervention and accompanying printed materials. The telephone intervention consisted of 12 educational telephone calls over a 9‐month period: a call every 2 weeks during months 1 and 2; a call every 3 weeks during months 3, 4, and 5; and a call every 4 weeks during months 6, 7, 8, and 9. The objectives of the calls were to provide individually tailored messages to encourage adherence with medication taking, appointment keeping, and refills; provide information about glaucoma; and intervene on barriers to adherence. The telephone‐based health communication intervention utilised interactive voice recognition technology to facilitate interest, participation, and interaction with call recipients and to standardise the content and delivery of the calls. Participants had the option to respond orally or use a telephone keypad. Telephone calls were primarily outbound, but participants had the option to call into the system if they missed a call. After 5 days of unsuccessful attempts to deliver a call, a reminder card was sent requesting that the participant call in to receive his or her message. Each call was structured to include a salutation; a medication regimen review; the core conversation, with tips to address barriers to adherence; general glaucoma information; and a closing. Participants in the control group received usual care. |
|
| Outcomes | Self‐reported medication adherence; self‐reported refill adherence (primary) | |
| Funding | National Institutes of Health grant R01 EY016997 and National Eye Institute Core Grant for Vision Research P30 EY 006360 | |
| Declaration of conflict of interest | None reported | |
| Power calculations for sample size | Using a 2‐group design and a planned sample size of 300 participants, there was adequate power (80%) to detect a 15‐20% percentage point difference in adherence with glaucoma treatment at 12‐month follow‐up. Investigators used software programme Power and Precision by Borenstein et al. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random number generator was used in Excel (Microsoft), and participants were randomised in blocks of 10." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Medical providers were masked to assignment because they were not directly involved in the trial" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Research interviewers were not masked to assignment because it was necessary to determine treatment group participants' preferences for intervention delivery" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate (intervention = 7, control = 5). Missing outcome data balanced in numbers across groups. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were balanced at baseline |
Goulis 2004.
| Methods |
Aims: to determine if home‐centred monitoring through telemedicine has an impact on clinical characteristics, metabolic profile and quality of life in overweight and obese participants Study design: RCT; recruitment: secondary care (organisational referral) Study duration: 6 months; study type: prevention; subtype: weight management |
|
| Participants |
Inclusion criteria: adults aged ≥ 18 years; BMI > 25 kg/m2, and could operate regular phones and electronic microdevices. Participants were also not on any obesity pharmaceutical treatment in the past year. Sample size: 122 ; mean age: 44 years; sex: men ‐ 12%; women ‐ 88 %; ethnicity:* Country: Greece |
|
| Interventions |
All participants of intervention group (in addition to care as usual) were supplied with an electronic blood pressure monitor (Card Guard CG800BP) and an electronic weight scale (Rowenta). They were given a treatment plan, where they had to measure and transmit 3 times a week, for 6 months, their blood pressure and weight and answer 2 life style questions: 'Did you follow your diet plan during the last 2 days?' and 'Did you follow your exercise plan during the last 2 days?'. The participants chose the type of data transmission they preferred among 3 options: Automated Call Centre through a regular phone, Wireless Application Protocol (WAP) server through a cellular phone and World Wide Web (Internet) server through a personal computer. All of them chose the Automated Call Centre Participants in the control group received usual care, which included a regular, hospital‐based, obesity treatment programme on an outpatient basis consisted of diet and physical activity guidelines |
|
| Outcomes | Clinical parameters (body weight, BMI, systolic blood pressure, diastolic blood pressure); laboratory parameters (plasma glucose, serum triglycerides, serum high‐density lipoprotein‐cholesterol and total serum cholesterol), obesity assessment (primary); Health Related Quality of Life, European Quality of Life (5 Dimensions) (secondary) | |
| Funding | European Commission: distance Information Technologies for Home Care for Citizens' Health System (CHS), IST‐1999‐13352 | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "Power calculation indicated that a minimum sample size of N = 100 was required, assuming 0.10 level of significance and 80 percent statistical power" | |
| Notes | During the study, intervention group and control group participants engaged in a hospital‐based, obesity treatment programme based on diet and physical activity guidelines. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised into intervention and control groups with a proportion of 1:2. Upon meeting the eligibility criteria and signing the consent form, all patients were allocated using central computerized randomizations. The random numbers were generated in blocks of six. Patients who received an odd number formed the intervention group, whereas patients who received an even number served as the control group" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "all patients were allocated using central computerized randomisation" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of key study personnel was ensured. Quote: "Both physicians and dieticians were blinded to the treatment arm of the patient" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Data were analysed in an intention‐to‐treat way using the LOFC procedure (last observation carried forward)." |
| Selective reporting (reporting bias) | Low risk | All of the study's pre‐specified outcomes that are of interest in the review have been reported |
| Other bias | Low risk | There were no baseline differences between the groups |
Graziano 2009.
| Methods |
Aims: to determine the impact of a daily, automated telephone intervention on glycated haemoglobin levels; self‐monitoring blood glucose (SMBG) frequency; self‐reported beliefs regarding severity of diabetes, susceptibility to complications of diabetes, and the benefits of and barriers to self‐management of diabetes compared with standard care in adults with type 2 diabetes mellitus Study design: RCT; recruitment: primary care (health professional referral) Study duration:12 months; study type: management; subtype: diabetes |
|
| Participants |
Inclusion criteria: aged ≥ 50 years with a diagnosis of type 2 diabetes mellitus documented in the medical record for ≥ 12 months, glycated haemoglobin levels equal to or greater than 7.0% within the past month, speak and understand English, access to either a landline or cellular phone, ability to hear and orally respond to automated telephone voice commands, responsible for own self‐care, access to reliable glucose meter that has 3‐month storage capacity, and self‐care regimen that includes SMBG at least daily Sample size: 119; mean age: 62 years; sex: men ‐ 55%, women ‐ 45%; ethnicity: white ‐ 77%; non‐white – 23% Country: USA |
|
| Interventions | In addition to care as usual, the intervention group received daily, automated, prerecorded voice message lasting less than a minute related to type 2 diabetes mellitus. A trained actor playing "Alice," a 60‐year‐old woman with type 2 diabetes mellitus recorded the scripted messages in a professional recording studio. The messages changed every day during the 90‐day intervention period. Messages focused on the American Association of Diabetes Educators' AADE7 Self‐care Behaviours including healthy eating, being active, monitoring (i.e. SMBG), taking medication, problem‐solving, reducing risks, and healthy coping. The messages also focused on changing attitudes and beliefs regarding the susceptibility and severity of type 2 diabetes mellitus and reduction of barriers related to performing self‐care behaviours. Participants chose the time of day they wanted to receive the automated calls and the telephone number they wanted the system to call. The system delivered up to 3 calls each day. If there was no answer or if an answering machine picked up the first call, the system called back an additional 2 times at 15‐minute intervals. If the call was not received by the participant after the third attempt, the system called back the next day at the previously agreed time. No messages were left. Participants were asked to answer and respond to as many calls as possible throughout the study. After listening to the prerecorded message, participants responded to Alice's questions regarding SMBG. The responses are relayed to a website that the investigators have access to. The system was programmed to send an email alert to the investigator when a participant reported a blood glucose level equal to or greater than 400 mg/dL, equal to less than 60 mg/dL, or an answer of 'yes' to either of the final questions. The investigator followed up with a telephone call to the participant and to the participant's clinic if necessary. Participants in the control group received usual care. |
|
| Outcomes | Glycated haemoglobin (primary); self‐monitoring of blood glucose frequency (secondary) | |
| Funding | Novo Nordisk | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | An effect size of −0.6 glycated haemoglobin percentage points ± 1.2 percentage points was used for the power calculation. These calculations assumed a sample size of 60 per group, 80% power, and a 2‐sided t‐test with type 1 error set at 0.05 | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A predetermined randomisation schedule from a series of permuted blocks was employed for each stratum" |
| Allocation concealment (selection bias) | Low risk | Quote: "Opaque randomisation envelopes that contained the randomisation assignment were labelled with participants' study numbers by a third party prior to initiation of the study." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Blinding of participants and the investigator was not possible because of the nature of the intervention. An attempt was made to avoid drawing attention to the randomisation assignment when providers were present" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Laboratory personnel who ran the HbA1c assays were unaware of the patients' study status." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (intervention n = 2, control n = 4). Missing outcome data balanced in numbers, with similar reasons for missing data across groups. Quote: "One participant in the study died shortly after being allocated to the treatment group and another participant in that group did not comply with study follow‐up procedures. 2 participants in the comparison group were lost to follow‐up, and 2 participants did not comply with study follow‐up procedures" |
| Selective reporting (reporting bias) | Low risk | Outcomes of interest reported |
| Other bias | Low risk | Groups were balanced at baseline; no significant differences were found (P < 0.05) |
Green 2011.
| Methods |
Aims: to evaluate the effectiveness of an automated telephone system reminding participants with hypertension to obtain overdue antihypertensive medication refills Study design: RCT; recruitment: other ‐ health plan (*) Study duration: *; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: participants aged ≥ 18 years with hypertension identified from a case‐identification database Sample size: 8306; mean age: *; sex: *; ethnicity: * Country: USA |
|
| Interventions |
Intervention group: the outreach consisted of an automated telephone call that instructed the member to order a refill for their overdue prescription by calling the number on their medication bottle or by using the Kaiser Permanente online refill system. Participants in the control group received usual care. |
|
| Outcomes | Refill rate at 2 weeks (primary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Greist 2002.
| Methods |
Aims: to compare the value of computer‐guided behaviour therapy value with that of a clinician‐guided behaviour therapy and systematic relaxation as a control treatment Study design: RCT; recruitment: primary care (adverts in radio, newspapers and articles, health professional referrals) Study duration: 3 months; study type: management; subtype: mental health |
|
| Participants |
Inclusion criteria: participants aged ≥ 14 years with a primary diagnosis of obsessive compulsive disorder for ≥ 2 years on the Structured Clinical Interview for DSM‐IV Sample size: 218; mean age: 39 years; sex: men ‐ 58%; women ‐ 42%; ethnicity: white ‐ 93%, other – 7% Country: USA |
|
| Interventions |
Computer‐based behaviour therapy. BT STEPS is a 9‐step, computer‐driven IVR system that allows participants with obsessive compulsive disorder to telephone from home and progress through a self‐paced workbook. Clinician‐guided behaviour therapy consisted of 11 weekly 1‐hour (or longer) sessions to negotiate self‐exposure homework to be done for ≥ 1 hour daily between sessions and recorded in daily diaries. Sessions were audiotaped and rated blindly by an expert behaviour therapist for quality of instructions Relaxation therapy. Participants receiving relaxation therapy were asked to perform progressive relaxation exercises for ≥ 1 hour daily and to keep daily relaxation diaries for 10 weeks |
|
| Outcomes | Yale‐Brown obsessive compulsive scale (primary); Clinical and Patient's Global Impressions; depression (Hamilton Rating for Depression Scale); satisfaction (secondary) | |
| Funding | Pfizer, Inc | |
| Declaration of conflict of interest | Drs Greist and Kobak, Mr Wenzel, and Ms Hirsch are employees of Healthcare Technology Systems (HTS), Madison, Wisconson. Ms Mantle was employed at HTS during this study and is currently self‐employed in Boise, Idaho. Mr Wenzel and Ms Hirsch own stock in HTS. Drs Marks and Baer receive royalties from BT STEPS. BT STEPS is a trademark of HTS. Dr Clary is an employee of Pfizer, Inc. | |
| Power calculations for sample size | "Sample size aimed for a power of 0.90, using estimates of means and standard deviations from a meta‐analysis of multicenter obsessive compulsive disorder trials." | |
| Notes | This is a comparison between computer‐based behaviour therapy and relaxation therapy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After screening by a clinician, patients were randomly assigned to 10 weeks of behavior therapy treatment guided by (1) a computer accessed by telephone and a user workbook or (2) a behavior therapist or (3) systematic relaxation guided by an audiotape and manual." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "Sessions [clinician‐guided therapy] were audiotaped and rated blindly by an expert behaviour therapist for quality of instructions." Comment: insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "In an intent‐to‐treat analysis, the last available post randomisation rating was input to endpoint for subjects who stopped prematurely." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Griffin 2011.
| Methods |
Aims: to assess the equivalence of theory‐based phone messages and education provided by an IVR system and by nurse‐delivered calls (NDCs) in promoting appointment attendance and adherence to preparation instructions for flexible sigmoidoscopy (FS) and colonoscopy, to compare the effect of the timing of IVR messages delivered 3 days versus 7 days before the scheduled appointment, and to evaluate any differences in patient satisfaction between IVR messages and NDCs Study design: RCT; recruitment: primary care (organisational referral) Study duration: 6 weeks; study type: either; subtype: appointment reminders |
|
| Participants |
Inclusion criteria: patients with upcoming FS or colonoscopy appointments scheduled in 2 gastrointestinal (GI) endoscopic procedure clinics at the Minneapolis Veterans Affairs Medical Center. Participants included those being screened and those having follow‐up appointments after receipt of abnormal test results Sample size: 3610; mean age: 63 years; sex: men ‐ 95% , women ‐ 5%; ethnicity: white ‐ 83%, non‐white ‐ 3%, other or > 1 race or unknown ‐ 14% Country: USA |
|
| Interventions |
Arm a: IVR‐3 Arm b: IVR‐7 Participants in the IVR study arms (IVR7 and IVR3) were mailed appointment information and preparation instructions and materials identical to those mailed in the NDC arm. Phone calls were programmed to start in the morning. If an answering machine picked up on the initial call, the IVR system left a general message about the purpose of the call. The system was programmed to call again in the afternoon and then again in the evening until the participant answered. Messages were left only on the first attempt. If the IVR call was not completed that day, the process was repeated the following day. Participants who answered the call had the option to have the system call back at a later time. An IVR call was considered complete if the participant answered and confirmed his or her appointment. The IVR system allowed participants to verify and confirm their appointment, respond to instructions about logistics, request additional preparation materials, answer queries about their current health, listen to preparation instructions, have any information repeated, ask for a summary of instructions, or leave a message for a nurse who would call back within 24 h. Embedded in these messages was the educational information about susceptibility and severity of colorectal cancer, as well as motivational messages that addressed risks, benefits, barriers, and self‐efficacy associated with preparation and procedures. At any time during the call, the participant could request to be transferred to the clinic to leave a message for a nurse Nurse delivered calls (arm c). A recovery room nurse attempted to call to remind participants of the appointment and review preparation instructions 7 days before the appointment |
|
| Outcomes | Appointment non‐attendance and preparation non‐adherence for FS (primary); perceptions about the call (secondary) | |
| Funding | Department of Veterans Affairs, Veterans Health Administration | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | "Using an equivalence boundary of 0.10, a sample size of 743 subjects per group provided 90% power for the study with a level of .05 divided by 3 and an underlying 65% baseline completion rate." | |
| Notes | ClinicalTrials.gov Identifier: NCT00310362. Non‐attendance was defined as cancelling the appointment or not attending the appointment. Appointments cancelled by the clinic were not considered as non‐attendance. Preparation non‐adherence assessed whether participants had adequately prepared to complete the procedure. Procedure notes was used to determine if the participant was adequately prepared or if the physician was unable to evaluate the quality of the preparation, attitudes and beliefs. This is a comparison between IVR‐3 and NDC 7 days before the procedure. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote:" Clinic procedure nurses and physicians were blinded to the randomised conditions." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Comment: groups were balanced with no significant baseline differences |
Halpin 2009.
| Methods |
Aims: to assess whether the health forecasting system can predict periods of higher risk and to assess the effect of the service on the frequency and severity of COPD exacerbations Study design: RCT; recruitment: primary care (*) Study duration: 4 months; study type: management; subtype: chronic obstructive pulmonary disease |
|
| Participants |
Inclusion criteria: all people aged > 40 with a diagnosis of chronic obstructive pulmonary disease confirmed with spirometry (forced expiratory volume in 1 second < 80% predicted, forced expiratory volume in 1 second/forced vital capacity ratio < 0.7) at 3 general practices in Devon, UK Sample size: 79; mean age: 69 years; sex: men ‐ 74%, women ‐ 26%; ethnicity:* Country: UK |
|
| Interventions |
Alert calls were made to the participant's normal telephone as occurs in the Healthy Outlook Service. The BlackBerry Smart Phones had their phone capabilities disabled and were only used for data collection and not to contact participants. The script for the alert call was successfully used in 2 pilot studies and as part of the routine health forecasting service since 2007. Automated calls were made on Tuesday evenings, with up to 2 repeat calls if the first was not answered Participants in the control group received no calls. |
|
| Outcomes | Frequency of exacerbations and proportion of participants experiencing ≥ 1 exacerbations (primary); changes in health status (secondary) | |
| Funding | AstraZeneca | |
| Declaration of conflict of interest | "The authors (JMG, EMH, SWV, DN, EMH, SN, ABS, AB, MVR) report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article" | |
| Power calculations for sample size | "The study was powered to identify a 30% reduction in the proportion of patients experiencing an exacerbation, assuming (on the basis of previous studies) that 90% of patients in the control group would exacerbate over the winter." | |
| Notes | 75% of participants were on short‐acting β 2‐agonists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Quote: "An independent researcher who was not part of the study team used a list of binomial random numbers generated in block sizes of four to randomly allocate the participants" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The investigators were unaware of which patients were allocated to receive the forecast and patients were not informed of their allocation" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (intervention n = 1, control n = 1). Missing outcome data balanced in numbers across groups. Quote: "Two patients did not complete the trial" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes of interest to the review have been reported |
| Other bias | Low risk | Groups were balanced at baseline. Quote: "The two groups were generally well matched; however, more patients in the group receiving alert calls had attended a chronic obstructive pulmonary disease education or exercise/rehabilitation programme and more controls were receiving inhaled corticosteroids/LABA therapy." |
Harrison 2013.
| Methods |
Aims: to evaluate the effectiveness of a telephonic outreach programme to improve blood pressure control among participants with hypertension Study design: RCT; recruitment: other ‐ health plan (organisational referral) Study duration: 4 weeks; study type: management; subtype: hypertension |
|
| Participants |
Inclusion criteria: Kaiser Permanente Southern California members > 18 years identified in a hypertension registry Sample size: 64,773; mean age: 61 years sex: men ‐ 46%, women ‐ 54%; ethnicity: white ‐ 41%, black ‐ 17%, Hispanic ‐ 25%, other/unknown – 9%, Asian ‐ 8% Country: USA |
|
| Interventions |
Outreach occurred 9‐16 August 2010, using an automated telephone messaging system. If the telephone call was answered by a live person or by a voicemail system, the automated message was delivered. Failed call attempts (i.e. busy signal or no answer) resulted in a maximum of 2 additional call attempts on the same day. Telephone calls were made between 10 am and 8 pm. The content of the automated message was developed by the KPSC outreach team. The message included a greeting stating the call was from Kaiser Permanente, an invitation to have a blood pressure measurement at a KPSC medical centre, and the hours of operation of the medical centre. The automated message was played by default in English with an option to listen to the message in Spanish Participants in the control group received usual care. |
|
| Outcomes | Blood pressure (primary) | |
| Funding | Southern California Permanente Medical Group | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We randomised the eligible members on August 2, 2010, to a usual care arm (n=33,154) and an intervention arm (n=33,150) and subsequently excluded 1531 individuals (4.8%): 1528 did not have a valid telephone number and 3 were on a "do not call" list." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were balanced at baseline. Quote: "There were no statistically significant differences between patients in the intervention arm compared with those in the usual care arm" |
Hasin 2013.
| Methods |
Aims: to test the efficacy of motivational interviewing (MI) only and MI + HealthCall for drinking reduction among HIV primary care patients Study design: RCT; recruitment: primary care (health professional referral) Study duration:12 months; study type: management; study subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: ≥ 4 US drinks of alcohol at least once, in the prior 30 days; HIV‐positive; English‐ or Spanish‐speaking; aged 18 years; and treated at the clinic Sample size: 254; mean age:46 years;sex: women ‐ 22%; men ‐ 78% ethnicity: African American ‐ 49%, Hispanic ‐ 45%, other ‐ 6% Country: USA |
|
| Interventions |
In MI + Health Call group, participants accessed the system via a toll‐free number for daily 1–3 min calls, answering pre‐recorded questions about 'yesterday' (morning, afternoon, evening) to ensure consistent reporting periods regardless of the hour called. Brief self‐monitoring questions covered alcohol consumption (e.g. 'How many beers did you drink yesterday?') and reasons for drinking or not drinking. Additional questions covered mood, medication adherence and well‐being. MI only. At baseline, counsellors administered a 20–25 min individual MI using standard techniques to motivate reduced drinking, encouraging participants to set a drinking‐reduction goal. Counsellors then provided the pamphlet and watch. At 30 and 60 days, counsellor and participant met for 10–15 min, discussed the participant's drinking during the past month, evaluated the drinking goal and set a new goal if participants wished. Participants in the control group received advice/education |
|
| Outcomes | Number of drinks per drinking day in the last 30 days (primary) | |
| Funding | CDC: R01AA014323, K05AA014223 and the New York State Psychiatric Institute | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | N = 90 per group would provide 80% power at alpha = 0.05 to detect a moderate treatment effect on number of drinks per drinking day (d = 0.4) | |
| Notes | This is a comparison between MI + HealthCall versus advice/education | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In a parallel three‐arm individually randomised design (1:1:1 allocation ratio), 258 participants were assigned to advice/education control, MI‐only or MI+HealthCall between August 2007 and May 2010, with groups balanced on depression, drug abuse, unstable housing and hepatitis using urn randomisation" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Counselors and patients were not blinded to treatments after assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition ‐ 94.5% of participants provided end‐of‐treatment data. Quote: "We conducted three sensitivity analyses to understand the robustness of our NumDD findings. Two involved multiple imputation" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "Treatment groups did not differ on these or other (e.g. demographic) variables." |
Helzer 2008.
| Methods |
Aims: to facilitate participant self‐monitoring and provide personalised feedback after a brief alcohol intervention by a primary care provider Study design: RCT; recruitment: primary care (health professional referral) Study duration: 6 months; study type: management; Study subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: adults aged ≥ 21 who reported a pre‐BI average alcohol consumption exceeding NIAAA recommended guidelines of 7 and 14 standard drinks per week for women and men, respectively; who met the heavy drinking criterion of 4/5 drinks in a single day (NIAAA, 2005); or who endorsed ≥ 1 CAGE items Sample size: 338; mean age: 46 years;sex: men ‐ 64%, women ‐ 36% ethnicity: white ‐ 97% Country: USA |
|
| Interventions |
IVR + feedback: 6 months of daily calls plus monthly feedback in the form of a mailed, printed graph showing daily consumption reported to the IVR in comparison to participant's stated drinking goal, with each mailing including a personalised note from Dr Helzer to heighten the saliency of the graphs IVR + feedback + compensation: daily calls and monthly feedback (graph and personal note) as described above plus a financial incentive based on frequency of the participant's daily calls. The incentive amounted to about USD 13 per week for a perfect calling record IVR: daily phone calls for 6 months to the automated IVR system to report alcohol consumption and other items for the past 24 h No IVR: BI and standard follow‐up treatment only, no calls to the IVR system |
|
| Outcomes | Weekly alcohol consumption (primary) | |
| Funding | National Institute on Alcohol Abuse and Alcoholism grants AA 11954 and AA 14270 | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between IVR + feedback and no IVR. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "Patients who satisfied all inclusion/exclusion criteria and signed the informed consent were randomised to one of four study conditions" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Follow‐up data were obtained for 284 subjects at 3 months (84%) and 273 at 6 months (81%). Of the 54 (16%) participants who did not complete a follow‐up assessment, 32 were lost to follow‐up and 22 declined to participate after randomisation." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "There were no significant differences between participants in the four randomised groups on any of the measured subject characteristics" |
Hendren 2014.
| Methods |
Aim: to assess an intervention to increase cancer screening among participants in a safety‐net primary care practice Study design: RCT; recruitment: primary care (health professional referral) Study duration: 12 months; study type: prevention; subtype: screening |
|
| Participants |
Inclusion criteria: overdue for the targeted cancer screening and average‐risk for the cancer by EHR review. Age criteria were age 40–74 years for mammography (women) or 50–74 years for colorectal cancer (men and women) on the date of randomisation Sample size: 366; mean age: *; sex: *; ethnicity: non‐Hispanic white ‐ 50%, non‐Hispanic black ‐ 41%, other race including Hispanic ‐ 9% Country: USA |
|
| Interventions |
Multimodal intervention consisted of letters, automated telephone calls, a point‐of‐care prompt and mailing of a home testing kit to colorectal cancer screening participants. An automated telephone reminder system (Televox system) was utilised to deliver automated calls to the telephone number in the practice database for each intervention participant. The automated phone calls contained similar information to the letters, but in a brief form (approximately 25 s), with a phone number to call to arrange for screening. The automated calls were made on weeks 2 and 6 of the intervention period and repeated on weeks 14 and 25 for participants remaining unscreened on EHR review performed on week 11. Participants in the control group received usual care (blinded chart review). |
|
| Outcomes | Breast cancer or colorectal cancer screening uptake at 12 months (primary) | |
| Funding | American Cancer Society (RSGT‐08‐077‐01‐CPHPS) | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | The total cost for the automated calls was about USD 0.92, including the preparation of each list of call recipients from the database and the monitoring of post‐call status | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An offsite study statistician randomised participants to intervention or control groups using a random number algorithm stratified by the type of screening required (breast cancer, colorectal cancer or both)." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Healthcare and data abstraction personnel were blinded to group assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "a research assistant blinded to treatment assignment abstracted data from the EHR" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "An intention‐to‐treat analysis was performed; that is, all patient originally assigned to a group were analysed." |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐defined outcomes have been reported |
| Other bias | Unclear risk | Quote: "There were no significant differences in participants at baseline between those in the intervention and control groups in the colorectal cancer group". However, there were borderline significant differences in household income and age. |
Hess 2013.
| Methods |
Aims: to measure the impact of an automated outbound telephone messaging system on herpes zoster (HZ) vaccinations among older adults in the community pharmacy setting Study design: cluster RCT; recruitment: primary care (organisational referral) Study duration: 3 months; study type: prevention; study subtype: immunisation |
|
| Participants |
Inclusion criteria: > 60 years of age, who had filled ≥ 1 prescription at a study pharmacy location during December 2006 Sample size: 16 pharmacies with a total of 11,982 participants; mean age: 72 years;sex: * ethnicity: * Country: USA |
|
| Interventions |
Automated outbound telephone messaging system in which the scripts were recorded and sent as an incoming automated telephone call to households using cNotify (Cintech, Mason, OH), which is an outbound messaging tool. Two 30‐second scripts were created to educate participants about their risk for developing HZ and invite them to speak to their pharmacist about vaccination opportunities Participants in the control group received no calls. |
|
| Outcomes | The number of HZ vaccines administered (primary) | |
| Funding | APhA Foundation Incentive Grant | |
| Declaration of conflict of interest | Potential declared | |
| Power calculations for sample size | No | |
| Notes | The intervention was delivered to 9650 "households" due to duplicated phone numbers being deleted to rule out back to back messages being delivered to the same number for different people. Cluster RCT with 16 clusters randomised. Of these, 8 (5599 participants) were allocated to intervention and 8 (6383 participants) were allocated to control. Note clustering was unadjusted for in the paper: to calculate effective sample size in Hess 2013 study, we used the Fleiss‐Cuzick estimator (see Appendix 14 for calculations). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "16 pharmacies were randomised by a simple randomisation process into two cluster groups of 8 pharmacies each" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of key study personnel was ensured. Quote: "The results of the randomisation were not disclosed to pharmacists" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "Because of the nature of the intervention, complete blinding was not possible" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | High risk | Participants in the intervention group were significantly older than control group participants (P < 0.001); not possible to judge selective recruitment of cluster participants based on the information reported. |
Heyworth 2014.
| Methods |
Aims: to examine whether telephonic IVR or participant mailing could increase rates of bone mineral density testing in high risk, menopausal women Study design: quasi‐RCT; recruitment: other ‐ health plan (*) Study duration:12 months; study type: prevention; study subtype: osteoporosis |
|
| Participants |
Inclusion criteria: women between the ages of 50 and 64 years who, in addition to age, had ≥ 1 risk factor for osteoporosis as follows: recent discontinuation of hormone replacement therapy; exposure to oral corticosteroids, anti‐seizure medication, or tobacco use; history of fracture; or bilateral oophorectomy without evidence of hormone replacement therapy or oral contraceptive use. Sample limited to women who had no evidence of bone mineral density screening in the 2 years prior to the randomisation and who did not have a diagnosis of osteoporosis and were not known to be taking any FDA‐approved treatment for osteoporosis Sample size: 4685; mean age:57 years;sex: women ‐ 100%; ethnicity: * Country: USA |
|
| Interventions | In addition to usual care, the IVR intervention was a single call lasting approximately 4–5 min. Each IVR call began with identification of the participant and proceeded if identification was correctly confirmed. A script was designed for the call that included a branching algorithm to calculate a fracture‐risk score, as well as the opportunity for women to indicate whether or not they had undergone bone mineral density testing, and whether or not they planned to follow up with their physician to discuss osteoporosis The participant mailing was a packet that included 5 illustrated pamphlets on osteoporosis, calcium and vitamin D, bone mineral density testing, osteoporosis risk assessment, and information about bone health and osteoporosis prevention + usual care Usual care group |
|
| Outcomes | Bone mineral density screening within 12 months (primary) | |
| Funding | Merck, West Point, PA | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | No information | |
| Notes | This is a comparison of IVR (intervention) versus UC (control) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Within each triplet, a pseudo‐random number generator assigned the patient panels of each primary care physician to a single treatment arm" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Because this study was non‐blinded, it is possible that patients in the usual care group became aware of the interventions to increase osteoporosis screening through communication with patients in the intervention groups, thus reducing the effect of the interventions" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were balanced at baseline. Quote: "Clinical and demographic characteristics of the study participants were similar across the three study groups at baseline" |
Ho 2014.
| Methods |
Aims: to test a multifaceted intervention to improve adherence to cardiac medications Study design: RCT; recruitment: primary care (*) Study duration: 12 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: all patients who were admitted with acute coronary syndrome (ACS) as the primary reason for hospital admission and who used the VA for their usual source of care were screened for eligibility to participate Sample size: 241; mean age: 64 years; sex: men ‐ 98%, women ‐ 2%; ethnicity: white ‐ 78% Country: USA |
|
| Interventions |
Participants in the multimodal intervention group received: medication reconciliation and tailoring; patient education; collaborative care between pharmacists and providers (PCPs or cardiologists); and voice messaging reminders (educational and medication refill reminder calls). The voice messaging system contacts participants at regularly scheduled intervals. There are 2 types of calls: medication reminder and medication refill calls. The medication reminder calls occurred monthly. The medication refill calls were synchronised to when a medication refill was due. The calls occurred 14 days prior to the refill due date, 7 days prior to the refill due date, and on the due date. During months 2 through 6 of the intervention, participants received both medication reminder (monthly) and medication refill calls (timed to refill due dates) for the 4 medications of interest. During months 7 through 12 of the intervention, participants only received medication refill calls Participants in the control group received usual care (standard hospital discharge instructions e.g. numbers to call, follow‐up appointments, diet and exercise advice, a discharge medication list, and educational information about cardiac medications) |
|
| Outcomes | The proportion of participants who are adherent with cardioprotective medications (β‐blockers, statins, clopidogrel, and ACE inhibitors) (primary); achievement of blood pressure and LDL cholesterol level targets (secondary) | |
| Funding | Veterans Health Administration Health Service Research & Development (HSR&D) Investigator Initiated Award (grant IIR 08‐302); Research Career Scientist Award VA HSR&D 08‐027 | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | We planned to recruit 280 participants over an 18‐month period and to follow participants for 12 months to have 80% power to detect a difference of 15% in the proportion of participants who were adherent to their cardioprotective medications | |
| Notes | ClinicalTrials.gov Identifier:NCT00520988. The annual incremental programme cost of the multifaceted intervention was USD 360 per participant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible patients with ACS were randomised using blocked randomisation stratified by study site in a 1:1 ratio to INT or UC" |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation sequence was concealed until a patient consented to participate and was generated centrally using the graphical user interface implemented for the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "At this visit, three blood pressure measurements were taken in standard fashion by someone blinded to study group assignment (eg, after 5 minutes of rest and 2 minutes apart between measurements)". Comment: insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "We used an intent‐to‐treat approach for all analyses" |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐specified outcomes have been reported in the pre‐specified way |
| Other bias | Unclear risk | Quote: "Baseline characteristics of the patients were comparable . . . Usual care patients were more likely to undergo coronary artery bypass graft surgery (17.1% vs 6.7%; P = .02)." Insufficient evidence to judge that this imbalance has introduced bias |
Homko 2012.
| Methods |
Aims: to examine the impact of an enhanced telemedicine system on glucose control and pregnancy outcomes in women with gestational diabetes mellitus Study design: RCT; recruitment: secondary care (organisational referral) Study duration: 26 months; study type: management; subtype: gestational diabetes |
|
| Participants |
Inclusion criteria: women aged 18‐45 years with a documented diagnosis of gestational diabetes mellitus on a 3‐h oral glucose tolerance test, using the criteria of Carpenter and Coustan. Women were required to be at ≤ 33 weeks of gestation at study entry Sample size: 80; mean age: 30 years; sex: men ‐ 0%; women ‐ 100%; ethnicity: white ‐ 41%, African American ‐ 34%, Latino/Hispanic ‐ 18 %, Asian and other – 7% Country: USA |
|
| Interventions |
ITSMyHealthrecord: the IVR system can be accessed from any phone over a dedicated toll‐free number and includes asynchronous phone messaging between clinicians and participants as well as automated reminders for participants to transmit data. Participants were prompted to input clinical data (i.e. blood glucose readings, changes in medication, and episodes of hypoglycaemia) and identify the day and time using the phone's keypad. They were provided feedback, emotional support, and reinforcement regarding diabetes self‐management with each transmission. In addition, women received a brief educational message/tip each time they accessed the system either by phone or Internet. Both systems allow women to append a message or ask a question (the IVR is set to accept 45 s of speaking, while the Internet‐based method allows virtually unlimited text input) after transmitting their health data. The data and messages are then queued for the clinician to respond to when he or she accesses the clinician portal of the system in which the participant data reside Participants in the control group received usual care. |
|
| Outcomes | Maternal glucose control and infant birth weight (primary) | |
| Funding | National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health | |
| Declaration of conflict of interest | "CJH, LD, KR, WM, DM, and JG have nothing to disclose. WPS has stock ownership in Insight Telehealth Systems. A.A.B. is a consultant for Insight Telehealth Systems." | |
| Power calculations for sample size | NA | |
| Notes | Mean BMI: 34.1 kg/m2; participants in both groups monitor their blood glucose levels daily (before breakfast and 2 h after each meal), perform foetal movement counting 3 times a day, and also record insulin doses and episodes of hypoglycaemia | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Women were randomised into one of two groups: telemedicine or control (usual care)." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (intervention n = 4, control n = 2). Missing outcome data balanced in numbers, with similar reasons for missing data across groups. Quote: "Data were available for 38 women in the control group and 36 in the intervention group" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "There were no significant differences at baseline between the two groups" |
Houlihan 2013.
| Methods |
Aims: to evaluate the efficacy of a novel telehealth intervention, CareCall, on reducing pressure ulcers and depression and enhancing the use of appropriate health care in persons with spinal cord dysfunction Study design: RCT; recruitment: other ‐ community disability organisations, rehabilitation medicine outpatient clinics and inpatient services (*) Study duration: 6 months; study type: management; subtype: spinal cord dysfunction |
|
| Participants |
Inclusion criteria: wheelchair users ≥ 6 h/day during normal waking hours, more or equal to 18 years of age, report of physician confirmed diagnosis of multiple sclerosis or spinal cord injury, absence of cognitive impairment on the Telephone Interview of Cognitive Status‐Modified (TICS‐M), score more or equal to 20, able to give written, informed consent, able to speak and understand conversational English, health insurance or pending health insurance (any kind), available for the full 6 months of the study, able to complete CareCall Training Call, living in a private residence of any kind Sample size: 142; mean age: 48 years; sex: men ‐ 61%, women ‐ 39%; ethnicity: white ‐ 80% (inclusive of Hispanic or Latino – 7%), African American ‐ 11%, other ‐ 9% |
|
| Interventions |
Participants in the intervention group received weekly automated calls from the CareCall for 6 months and could call into CareCall any time. The CareCall scripts were organised into modules, integrating content relevant to: skin care, depression and wellness, and healthcare utilisation. The system also included relevant prerecorded vignettes from people with spinal cord dysfunction, and relevant recorded comments from healthcare professionals. These modules used branching logic based on personalised information and participants' responses during calls to tailor content throughout. Participants in the control group received usual care (current standard of care). They also received a CareCall resource book developed by clinical experts, containing information and local resources. |
|
| Outcomes | Prevalence of pressure ulcers; depression severity; healthcare utilisation (all primary) | |
| Funding | CDC, Grant no. 5R01DD000155, the Department of Health and Human Services; and the National Institute of Disability and Rehabilitation Research, Grant nos. H133N060024, H133N110019, and H133N120002, the Department of Education | |
| Declaration of conflict of interest | Dr Friedman had stock ownership and a consulting agreement with Infomedics, the company that owns commercial rights to the TLC technology used in the computerised intervention. He is also a member of its board of directors. The remaining authors declared no conflict of interest. | |
| Power calculations for sample size | No | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We allocated participants to study groups using a stratified block randomization method to ensure balance by recruitment site" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All study staff collecting data were masked as to study group assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (intervention n = 4, control n = 3). Missing outcome data balanced in numbers. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "At baseline, there were no statistically significant study group differences in the prevalence of pressure ulcers, mean severity of depression or the percentage reporting issues with health‐care availability. However, the intervention group reported more emergency room visits and hospitalizations compared with control group subjects." |
Hyman 1996.
| Methods |
Aims: to evaluate the effectiveness of an automated telephone system as a relapse intervention in participants who completed a 4 week class based cholesterol lowering diet protocol Study design: RCT; recruitment: primary care (*) Study duration: 6 months; study type: management; subtype: hypercholesterolemia |
|
| Participants |
Inclusion criteria: participants who completed a 4‐week class based on cholesterol lowering diet protocol Sample size: 115; mean age: 48 years; sex: men ‐ 25%; women ‐ 75%; ethnicity: non‐Hispanic Caucasian ‐ 87%, other – 13% Country: USA |
|
| Interventions |
Computer‐phone system: asks participants 2‐4 prerecorded questions about recent eating behaviour, low‐fat nutrition knowledge, behavioural or maintenance skills, or expectations that may influence maintenance of cholesterol lowering behaviours. Participants responded by pressing the appropriate number on their touch‐tone phone. Based on this information, they received tailored feedback. Those failing to call the system in the first week received a reminder during the second week. Participants could leave a message for research staff who would then provide their response Participants in the control group received usual care. |
|
| Outcomes | Total cholesterol reduction (primary); acceptability of the system (secondary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Complete case analysis. Quote: "A total of 16 participants dropped out and their measures were not used in the final analysis. Comparison of drop‐outs with completers showed no significant difference for age, BMI, baseline cholesterol, ethnicity, sex, smoking habits or education." |
| Selective reporting (reporting bias) | High risk | Weight outcomes at follow‐up were not provided |
| Other bias | Low risk | There were no significant differences at baseline between the 2 groups |
Hyman 1998.
| Methods |
Aims: to test the feasibility and effectiveness of a diet intervention (consisting of interactive mailings, computer‐generated phone calls, and classes) in hypercholesteraemic low‐income public clinic patients Study design: RCT; recruitment: primary care (telephone) Study duration: 6 months; study type: management; subtype: hypercholesterolemia |
|
| Participants |
Inclusion criteria: aged 18–65 years, have a past TC measurement, have a total cholesterol > 200 mg/dL, be English‐speaking, not require insulin, not be over 200% ideal body weight, not have cancer other than skin cancer, not have triglycerides over 400 mg/dL, plan to remain in the area ≥ 6 months, and not be on lipid‐lowering drugs Sample size: 123; mean age: 57 years; sex: men ‐25 %; women ‐ 75%; ethnicity: African American ‐ 77%, other – 23% Country: USA |
|
| Interventions |
IVR arm: participants continued to receive usual care but were offered and encouraged to use all 3 components of the system: mailed diet questionnaires with individualised mailed feedback, computer‐interactive phone calls, and a programme of 4 hour‐long classes. Intervention development was guided by social cognitive theory so that calls could provide opportunities for modelling, feedback and reinforcement, increasing self‐efficacy for change. The intervention also sought to increase practical skills such as reading labels, eating out, modifying recipes, and self‐monitoring. The intervention components were developed to reduce participant burden while utilising behavioural approaches to lifestyle change and to maintain sufficient contact, monitoring, and feedback, yet be practical for primary care Participants in the control group received usual care. Physicians in general provide very brief dietary counselling and prescribe lipid‐lowering drugs as deemed appropriate. Hypercholesterolaemic patients may be referred to clinic registered dietitians. After the trial the UC subjects were offered the series of classes |
|
| Outcomes | Total cholesterol reduction (primary); self‐efficacy; dietary knowledge; fat intake scale (secondary) | |
| Funding | American Heart Association Texas Affiliate 91R‐172 | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Blocked randomisation. Quote: "Allocated to treatment in a 1:1 ratio using a fixed randomisation scheme with blocks of size four." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate. Quote: "Of the 123 subjects, 80.5% (99) completed follow‐up cholesterol measurements." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "The 123 subjects randomised into the two study groups were generally comparable although the special intervention group had more African Americans (P = 0.04) and were younger at 54.6 versus 58.7 years of age (P = 0.03)". Comment: intervention group had significantly more African‐Americans and young participants compared to the control group. There is insufficient evidence that this imbalance has introduced bias |
Jarvis 1997.
| Methods |
Aims: to evaluate the effectiveness of telecommunications technology to underpin an intervention that would be effective, easy to use, convenient, inexpensive, require little time commitment, and amenable to widespread distribution Study design: RCT; recruitment: primary care (mail and telephone) Study duration: 3 months; study type: prevention; subtype: physical activity |
|
| Participants |
Inclusion criteria: aged ≥ 60 years, English‐speaking, had to be sedentary (defined as participating in < 60 min of physical activity per week, with a minimum of 20 min of exercise per time and a minimum of 3 times per week), and also needed to have touch‐tone telephone service Sample size: 85; mean age: 67 years; sex: men ‐ 24%; women ‐ 76%; ethnicity: other ‐ 70%, African American ‐ 30% Country: USA |
|
| Interventions |
The Telephone‐Linked Communication (TLC) System is an interactive computer‐based telecommunication system that converses with participants in their homes over their telephone to motivate and improve health‐related behaviours. TLC 'speaks' to users over the telephone using computer‐controlled speech generation. Users communicate with TLC by using their telephone touch‐tone keypad. TLC functions as a monitor or 'counsellor' that provides positive feedback to reinforce or change the individual's health behaviour. TLC stores the user's response in a database. The information provided by the person controls the direction of the conservation. This information is also forwarded to the person's physician on a report, similar to a laboratory report, in which medical problems are highlighted. Participants in the control group received usual care. |
|
| Outcomes | Minutes walked per week (primary); satisfaction (secondary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Then subjects were randomised to use TLC‐ACT, or to a usual medical care control group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "'Research staff and subjects were blinded to the study assignment until the baseline questionnaire was completed." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Complete case analysis. Quote: " The analysis was performed on the 68 subjects who completed the study" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes of interest to the review were reported |
| Other bias | Low risk | Quote: "There were no significant differences between the groups based on age, number of co‐morbidities, Stage of Adoption of Physical Activity, and minutes walked over the 4 recall days at baseline." |
Katalenich 2015.
| Methods |
Aims: to assess the utility and cost‐effectiveness of an automated Diabetes Remote Monitoring and Management System (DRMS) in glycaemic control versus usual care Study design: RCT; recruitment: primary care (*) Study duration: 6 months; study type: management; subtype: diabetes |
|
| Participants |
Inclusion criteria: patients with an glycated haemoglobin between 7.0% and 9.0%, aged ≥ 18 years, and currently taking or starting insulin Sample size: 98; mean age: 59 years; sex: men ‐ 40%; women ‐ 60%; ethnicity: black ‐ 65%; white ‐ 30%; Hispanic ‐ 1%; Asian ‐ 1%; other ‐ 3% Country: USA |
|
| Interventions | Participants in Diabetes Remote Monitoring and Management System (DRMS) were contacted daily, either through text messaging or automated voice. From these messages, participants could either respond by submitting their blood glucose levels or respond at a later time. If a participant did not submit his or her blood glucose level at the initial contact, the DRMS would text or call again that same day to remind the participant to check his or her blood glucose. However, if a participant submitted a reading before the reminder, the system would not contact the participant on that day. Providers could monitor the progress of their patients through a web‐based, secure portal, and information could also be downloaded directly into electronic medical records. Participants in the control group received usual care. |
|
| Outcomes | Glycated haemoglobin; medication adherence; quality of life; cost‐effectiveness (all primary) | |
| Funding | Eli Lilly, National Institute of General Medical Sciences, National Institutes of Health | |
| Declaration of conflict of interest | Potential declared | |
| Power calculations for sample size | NA | |
| Notes | 60% of participants used phone calls to report into the system, and 40% used text messages exclusively. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomised, after informed consent was obtained, to either the intervention (DRMS) group or the control group by using a random‐number table" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All statistical analysis used intent‐to‐treat methodology" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | There were some baseline differences between the groups in demographics; unclear whether those introduced bias. |
Khanna 2014.
| Methods |
Aims: to determine if automated telephone nutrition support counselling could help patients improve glycaemic control by duplicating a successful pilot in Mexico in a Spanish‐speaking population Study design: RCT; recruitment: primary care (telephone) Study duration: 3 months; study type: management; subtype: diabetes |
|
| Participants |
Inclusion criteria: ≥ 2 visits to the clinic in the last 1 year and a glycated haemoglobin level of > 8.0% on most recent visit, and any insulin status Sample size: 75; mean age: 52 years; sex: men ‐ 59%, women ‐ 41%; ethnicity: Hispanic (Spanish‐speaking) ‐ 100% |
|
| Interventions |
The system was designed and implemented using a Dialogic telephone card installed in a desktop computer and connected to a landline, programmed using Telesage software (Boston, MA). The system was designed to create a 'summary' estimate of high‐glycaemic index food consumption on survey conclusion that was then provided to participants at the conclusion of the call. If the sum of all high glycaemic index foods in the previous 24‐hour period was 2 or fewer servings, the message was one of congratulations and positive feedback; if 3‐4 servings, the message was more cautious and provided some education about appropriate low‐glycaemic index foods; and if ≥ 5 servings, then it provided a more educational message regarding high and low‐glycaemic index foods Participants in the control group received usual care. |
|
| Outcomes | Glycated haemoglobin (primary); systolic blood pressure; diastolic blood pressure; BMI; waist circumference; total cholesterol; triglycerides; serum high‐density lipoproteins; serum Low density lipoproteins (secondary) | |
| Funding | National Institute of Diabetes and Digestive and Kidney Diseases for Diabetes Translational Research (CDTR) at Kaiser Permanente and University of California, San Francisco (P30DK092924) | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | An 80% power to detect a difference in glycated haemoglobin of approximately 1.2% ± 1.5% between groups, and assuming 15% loss to follow‐up, investigators aimed to enrol 80 total participants into the study | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator. Quote: "Patients were selected into one arm or the other of the study using a random number generator" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "We conducted a prospective, randomised, open‐label trial (ClinicalTrials.gov #NCT01040676) with blinded endpoint assessment" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition. Quote: "There was significant loss to follow‐up despite several attempts to reach patients" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "Patients in the intervention arm were broadly similar to those in the control arm but trended toward being more likely to be men (P = 0.12), having a larger waist circumference (P = 0.053), and being on a different number of diabetes medications (P = .07)" |
Kim 2014.
| Methods |
Aims: to enhance engagement in low‐income adults with poorly controlled diabetes (glycated haemoglobin > 9%) Study design: RCT; recruitment: primary care (*) Study duration: 12 months; study type: management; subtype: diabetes |
|
| Participants |
Inclusion criteria: English‐ and Spanish‐speaking patients with telephone access who receive primary care at San Francisco General Hospital; glycated haemoglobin > 9% Sample size: 100; mean age: *; sex: *; ethnicity: * |
|
| Interventions |
Participants in the intervention group received weekly, 10‐min, automated phone calls, which delivered educational vignettes and detected triggers such as diabetes‐related adverse events or requests for medical appointments, medication assistance or a callback from a healthcare provider. Triggers were addressed with a follow‐up call from a diabetes specialist (NP, MD or CDE) within 48 h. Participants in the control group received usual care |
|
| Outcomes | Glycated haemoglobin (primary) | |
| Funding | McKesson Foundation | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "patients with telephone access who receive primary care at San Francisco General Hospital were randomly selected to receive calls." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
King 2007.
| Methods |
Aims: to evaluate the effectiveness of telephone‐based physical activity guidance and support delivered via a trained health educator or an automated system across an extended period of 12 months Study design: RCT; recruitment: primary care and community (advert elsewhere ‐ promotion in local media outlets, flyers and brochures in health clinics, pharmacies, senior centres, and other community settings) study duration: 12 months; study type: prevention; subtype: physical activity |
|
| Participants |
Inclusion criteria: aged ≥ 55 years, English‐speaking, not currently engaging in more than 60 min/week of moderate or vigorous intensity physical activity, free of any medical condition, BMI ≤ 40 kg/m2, alcohol intake ≤ 3 drinks/day, able to speak and understand English, and access to a touch‐tone phone Sample size: 218; mean age: 61 years; sex: men ‐ 31%; women ‐ 69%; ethnicity: white ‐ 90 %, other – 10% Country: USA |
|
| Interventions |
Automated advice (IVR) arm: the system spoke to participants using computer‐controlled speech generation; participats communicated using the touch‐tone keypad of their telephones. The contents included physical activity assessment (type, frequency, duration, steps accumulated on the pedometer), progress evaluation, individualised problem‐solving, goal‐setting, feedback, and delivery of positive support and tailored advice. Each call lasted 10‐15 min and occurred bi‐weekly then weekly. Quality control was implemented through semi‐weekly evaluation of the technical performance of the automated system via TLC's automatic contact summarisation database, as well as daily monitoring of the automated system's telephone helpline that was used by participants to report any problems while using the TLC system Human advice arm: this arm consisted primarily of telephone‐assisted physical activity counselling by a trained health educator. Individuals received an initial in‐person 30‐40 min health educator‐led instructional session, including development of an individualised plan emphasising a gradual progression of activity frequency, duration, and intensity towards a goal of ≥ 30 min of moderate‐intensity endurance exercise (primarily brisk walking) on most days of the week. The remaining intervention contacts occurred via brief (i.e. 10‐15 min) structured counsellor‐initiated telephone calls that occurred on a bi‐weekly, then monthly basis. Each participant was scheduled to receive approximately 15 contacts during the study year during which they received individualised information, support, and problem‐solving around physical activity barriers. Attention‐control arm: individuals randomised to this arm were offered weekly health education classes that focused on a variety of non‐physical activity topics of interest to middle‐ and older aged adults such as nutrition and home safety, and they were asked not to change their usual physical activity patterns during the 12‐month study period. At the end of 12 months, people in this arm were offered a 6‐month health educator‐delivered telephone based exercise programme. |
|
| Outcomes | Minutes of moderate to vigorous physical activity (primary); physical functioning and well‐being (secondary) | |
| Funding | National Institute on Aging | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "A sample size of approximately 61 participants completing per group was judged to be adequate for detecting a 30 minute per week across 7 days as measured by the physical activity recall in moderate or vigorous physical activity at 90% power with 2‐sided alpha set at 0.05." | |
| Notes | This is a comparison between the IVR arm and the health education (attention‐control) classes. This study had a follow‐up of 18 months reported in King 2014 but no comparisons were made between these arms at that point. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomly assigned using a computerized version of the Efron procedure." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All study assessment staff were blinded to participant study arm assignments." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers, with similar reasons for missing data across groups. Quote: "Of the 218 individuals enrolled in CHAT, 189 (86.7%) had 6‐and 12‐month 7‐Day physical activity recall data.The retention rates were not significantly different across the three study arms." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "Participants were similar across the three study arms on the major baseline variables of interest." |
Kroenke 2010.
| Methods |
Aims: to determine whether centralised telephone‐based care management coupled with automated symptom monitoring can improve depression and pain in cancer patients Study design: RCT; recruitment: primary care (healthcare professional referral) Study duration: 12 months; study type: management; subtype: cancer |
|
| Participants |
Inclusion criteria: patients presenting for oncology clinic visits; depression with PHQ‐8 score of 10 or greater, with depressed mood and/or anhedonia; pain ‐ at least moderate in severity, defined as a Brief Pain Inventory worst score in the past week of 6 or greater, persistent despite a patient's having tried ≥ 1 different analgesic medication and cancer related Sample size: 405; mean age: 59 years; sex: men ‐ 32%, women ‐ 68%; ethnicity: white ‐ 80%, black ‐ 18%, other ‐ 2% Country: USA |
|
| Interventions |
Multimodal intervention (automated symptom monitoring (ASM)) was performed using either interactive voice–recorded telephone calls or Web‐based surveys based on participant preference. The 21‐item survey included the PHQ‐9 depression scale, 8 pain items from the Brief Pain Inventory (3 severity and 5 interference), and a single question for each of the following: medication adherence, adverse effects, global improvement, and whether the participant wanted a nurse care manager call. The monitoring survey was administered twice a week for the first 3 weeks, then weekly during weeks 4 through 11, twice a month during months 3 through 6, and once a month during months 7 through 12. However, more frequent administration could be reinstituted for participants who underwent treatment changes. Those not completing their scheduled assessment were contacted by telephone by the nurse care manager. In addition to ASM, participants also received telephone care management (delivered by nurse) and medication management (delivered by oncologist) Participants in the control group received usual care. |
|
| Outcomes | Depression severity; pain severity (primary); health‐related quality of life; disability; healthcare use (outpatient physician visits); and co‐interventions (depression treatments) (secondary) | |
| Funding | National Cancer Institute, National Institutes of Health | |
| Declaration of conflict of interest | Dr Kroenke reported receiving research funding from Eli Lilly and Pfizer, and honoraria as a speaker, consultant, or advisory board member from Eli Lilly, Pfizer, and Forest Laboratories. No other authors reported disclosures | |
| Power calculations for sample size | The study was powered to detect clinically significant improvement in depression (HSCL‐20) and pain (Brief Pain Inventory). It was determined that 97 participants per symptom group would provide 80% power to detect a 20% absolute difference in response rates with 2‐tailed alpha < 0.05 | |
| Notes | "Symptom‐specific disability was high, with participants reporting an average of 16.8 of the past 28 days (i.e. 60% of their days in the past 4 weeks) during which they either were confined to bed (5.6 days) or had to reduce their usual activities by 50% (11.2 days) due to pain or depression. Moreover, 176 (43%) reported being unable to work due to health‐related reasons." Correspondence with the author: "The majority of patients did the symptom monitoring by IVR (89.3% by IVR; only 10.7% by web)" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was computer‐generated in randomly varying block sizes of 4, 8 and 12 and stratified by symptom type (pain only, depression only, or both pain and depression)" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All five assessments (baseline, 1, 3, 6, and 12 months) were administered by telephone interview and conducted by research assistants blinded to treatment arm." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers, with similar reasons for missing data across groups. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "Analyses were based on intention‐to‐treat in all randomised participants" |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all of the study's pre‐specified outcomes of interest have been reported |
| Other bias | Unclear risk | There were no significant differences between the intervention and usual‐care groups except for marginally significant differences for sex (P = 0.0512) and marital status (P = 0.0527). There is insufficient evidence that this imbalance has introduced bias. |
Kroenke 2014.
| Methods |
Aims: to determine the effectiveness of a telecare intervention for chronic pain Study design: RCT; recruitment: primary care (mail and telephone) Study duration: 36 months; study type: management; subtype: chronic pain |
|
| Participants |
Inclusion criteria: participants aged 18‐65 years were eligible if they had pain that was musculoskeletal, defined as regional (joints, limbs, back, neck) or more generalised (fibromyalgia or chronic widespread pain); moderately severe, defined as a pain intensity item score of 5 or higher for either 'average' or 'worst' pain in the past week; and persistent (i.e. 3 months) despite trying ≥ 1 analgesic medication Sample size: 250; mean age: 55 years; sex: men ‐ 83%, women ‐ 17%; ethnicity: white race ‐ 77 % Country: USA |
|
| Interventions |
Multimodal intervention (automated symptom monitoring (ASM)), either by interactive voice recorded telephone calls or by Internet, depending on their preferences. Reports from ASM were scheduled weekly for the first month, every other week for months 2 and 3, and monthly for months 4 through 12. The 15‐item ASM measure included 7 symptom items: 3 pain items from the PEG instrument, 2 anxiety items from the 2‐Item Generalized Anxiety Disorder Questionnaire, and 2 depression items from the Patient Health Questionnaire 2. The other 8 items asked about how difficult pain made it to carry out usual activities; degree of relief from pain medications; global change in pain (worse, same, better) and, if better, the degree of improvement; analgesic adverse effects, adherence, and whether a medication change was desired; and a request for the nurse to call. Participants in this group also received optimised analgesic management by a team consisting of a nurse care manager and physician pain specialist Participants randomised to usual care continued to receive care for their chronic musculoskeletal pain from their primary care physician |
|
| Outcomes | Pain intensity (primary); difference in response rates: mean Brief Pain Inventory interference; and pain severity scale scores (secondary) | |
| Funding | Department of Veterans Affairs (VA) Health Services Research and Development (VA HSR&D) Merit Review award to Dr Kroenke (IIR 07‐119) and a VA Career Development Award to Dr Krebs (CDA 07‐215) | |
| Declaration of conflict of interest | Dr Kroenke reported receiving honoraria from Eli Lilly outside the submitted work. No other authors reported disclosures | |
| Power calculations for sample size | Investigators determined that 100 participants were needed per group to detect a between‐group treatment difference of 0.4 SD in the Brief Pain Inventory total score (representing a small to moderate treatment effect), presuming a 2‐sided alpha < 0.05 and 80% power. Allowing for up to 20% attrition, the enrolment target was set at 250 participants. | |
| Notes | Correspondence with the author: "In a second more recent trial of ours (SCOPE) that also used IVR vs. web, we found 51% used IVR and 49% used web. Although we did not report results differently, we did a multivariable model on the primary pain outcome, and found that mode of symptom monitoring (IVR vs. web) did NOT make a difference in the treatment effect." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was stratified by patient opioid medication use at baseline (yes or no). To maintain allocation concealment, assignment to treatment group was determined by a computer‐generated randomisation list with randomly varying block sizes of 4 and 8." |
| Allocation concealment (selection bias) | Low risk | Quote: "To maintain allocation concealment, assignment to treatment group was determined by a computer‐generated randomisation list with randomly varying block sizes of 4 and 8." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessment was ensured. Quote: "Research assistants responsible for outcome assessments were blinded to treatment group assignment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low drop‐out rate. Missing data have been imputed using appropriate methods. Quote: "As a sensitivity analysis, multiple imputation analysis was also performed." |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐specified outcomes have been reported in the pre‐defined way. |
| Other bias | Low risk | Groups were balanced in terms of baseline characteristics |
Krum 2013.
| Methods |
Aims: to determine whether an automated telephone support system would improve quality of life and reduce death and hospital admissions for rural and remote heart failure patients Study design: cluster RCT; recruitment: primary care (*) Study duration: 12 months; study type: management; study subtype: heart failure |
|
| Participants |
Inclusion criteria: New York Heart Association (NYHA) class II–IV heart failure, left ventricular ejection fraction < 40% on echocardiogram, or echocardiographic features of diastolic dysfunction with impaired ventricular relaxation reported with no other diagnostic explanation for chronic heart failure‐type symptoms such as chronic obstructive airways disease and bronchial asthma; a recent primary hospital discharge diagnosis of heart failure within the previous 5 years; touch‐tone telephone access and the ability to operate this system Sample size: 405; median age: 73 years;sex: women ‐ 37%; men ‐ 63%; ethnicity: * Country: Australia |
|
| Interventions | The TeleWatchTM system is a telephone‐based automated telemedicine system developed by Johns Hopkins Biomedical Engineering in conjunction with their clinical heart failure group. This telemedicine system was required to be dialled into by the participant on an at least a monthly basis at which time questions were asked with regard to heart failure clinical status, medical management of their condition, and social questions relevant to their heart failure status. Participants in the control group received usual care (standard general practice management of heart failure) |
|
| Outcomes | Packer clinical composite score (death, hospital admission for heart failure, withdrawal from study due to worsening heart failure, 7‐point global health assessment questionnaire) (primary); hospitalisation for any cause; death or hospitalisation; and heart failure hospitalisation (secondary) | |
| Funding | National Health and Medical Research Council, National Heart Foundation of Australia, and Medical Benefits Fund | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | Calculations indicated that a shift of approximately 11% (to 37%, 47%, 16% in the intervention arm) corresponding to an odds ratio of 1.78 was able to be detected with 80% power using this sample size | |
| Notes | Cluster RCT; analyses appropriately adjusted for clustering at practice level by using a robust variance estimator Cluster RCT with 143 GPs (127 GP clusters) GPs recruiting 434 patients, of whom 405 were enrolled into the study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The study involved cluster randomisation at the level of the general practitioner (1:1, usual care, usual care plus intervention, stratified by rural, remote and outer metropolitan area [RRMA] classification). This was to minimize contamination across the two interventions to which patients were randomised." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All patients regardless of treatment allocation were followed up by an independent reviewer, blinded to treatment allocation, and asked to complete a telephone survey at baseline and at 6 and 12 months." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Intention‐to‐treat analyses were performed for all endpoints." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "Patients were well matched at baseline for disease severity, co‐morbidities, haemodynamic parameters, and concomitant medications". Insufficient information reported to judge whether or not selective recruitment of clusters may have introduced bias. |
Kurtz 2011.
| Methods |
Aims: to assess the effect on cardiovascular death or re‐hospitalisation for heart failure of 3 different clinical management strategies: standard heart failure care, management in a cardiology clinic and home telephone self‐monitoring Study design: quasi‐RCT; recruitment: * (*) Study duration: 12 months; study type: management; subtype: heart failure |
|
| Participants |
Inclusion criteria: patients with left ventricular systolic dysfunction (LVEF 45%), recently discharged from hospital or diagnosed with acute or worsening heart failure up to 3 months before the study, between January 2007 and January 2008 Sample size: 138; mean age: 68 years; sex: men ‐ 79%, women ‐ 21%; ethnicity: * Country: France |
|
| Interventions |
Automated home telephone self‐monitoring (Telecard): participants were asked to call an automated system once a week, to listen to the voice questions and to answer using the telephone keypad. Guide Vocal‐Web (Guide Vocal‐Web, France Telecom, Orange Business Service, France) is software for specifying interactive voice dialogues between human and telephone. Briefly, using a computer linked to an Orange business website service, 3 heart failure‐related questions displayed in a tree manner with nodes were edited. Questions were about weight change, dyspnoea and general health. The text was then converted into a synthetic voice message. Participants were able to listen to audio advice, inviting them to repeat their call after a week (stable), after 3 days (minor worsening heart failure), to proceed to a medical visit (suspected worsening heart failure), or they were directly connected to cardiology clinic care giver (high risk of hospitalisation according to the algorithm) Cardiology clinic. A multidisciplinary team approach during visits to the heart failure clinic. Usual care |
|
| Outcomes | Cardiovascular deaths, hospitalisation for heart failure (classified together as adverse events) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Most of the participants received beta‐blockers, ACE/AT2 inhibitors and diuretics. Cardiac re‐synchronisation therapy was delivered in 27% of participants. This is a comparison between the Telecard arm and the UC arm |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were allocated to three different groups for heart failure monitoring in a non‐randomised fashion" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "All groups were similar in their clinical characteristics at inclusion" |
LeBaron 2004.
| Methods |
Aims: to evaluate the impact of large‐scale, registry‐based reminder‐recall interventions on low immunisation rates in an inner‐city population Study design: RCT; recruitment: other – public health clinics, community health centres, hospitals, outpatient departments, private practices (organisational referral) Study duration: 24 months; study type: prevention; subtype: immunisation |
|
| Participants |
Inclusion criteria: residing in Fulton County, receiving care through its health department clinics or the public hospital health system, and were born between 1 July 1995, and 6 August 1996 Sample size: 3050; median age: 9 months; sex: boys ‐ 49%, girls ‐ 51%; ethnicity: black, non‐Hispanic ‐ 76%, Hispanic ‐ 14%, white, non‐Hispanic ‐ 7%, other, non‐Hispanic – 3% Country: USA |
|
| Interventions |
Autodialer (automated telephone or mail reminder recall). 7 days before a dose was due, a computer connected to a telephone delivered a recorded message to the family. Content: child should be taken to his or her health care provider for the needed dose. If there was no answer or a busy signal, the call was repeated every 30‐60 min. If these efforts failed to reach a person or an answering machine or if the telephone number was non‐working or not present in the database, an automated postcard with the same message was mailed to the family no later than 5 days before the due date. If 6 days after the due date the needed dose was not present in the registry, a computerised telephone message (or postcard in the absence of a working telephone) was sent to the family indicating that the child was behind in his or her immunisations. Unless the registry recorded the immunisation, the telephone message was repeated on days 11, 17, and 23. If these efforts failed, a computerised postcard was sent on day 28. All telephone calls were made between 5:30 and 9:00 pm. At the start of each message, an option for a Spanish‐language version was presented, and postcards contained the message in both Spanish and English. Outreach (in‐person telephone, mail, or home visit recall). Within 7 days of a child failing to receive a dose by the due date, the outreach worker attempted to contact the family by telephone or postcard in the absence of a working telephone. If 7 days later the dose was still not in the registry, a postcard was sent. If 30 days later the dose was still missing, a home visit was attempted, with continued monthly efforts until contact was made. At the home visit, the outreach worker attempted to determine what was needed to assist the family in obtaining immunisation for the child. The principal outreach worker was a college‐educated, African American woman who had been raised in inner‐city Atlanta. For Hispanic families, outreach was provided by a bilingual, college‐educated, Hispanic worker. The outreach workers and other study functions were supervised by a person with a doctorate in community psychology and extensive experience in conducting inner‐city studies Combination (Autodialer with outreach backup) Usual care (no interventions beyond normal clinic procedure, which in certain cases involved non‐automated postcard recall systems) |
|
| Outcomes | Completion by the age of 24 months of the 4‐3‐1‐3 vaccination series | |
| Funding | National Immunisation Program, CDC, and the Georgia Department of Human Resources, Atlanta | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | The study population of 3050 provided 80% power for detection of 5% differences in immunisation rates among groups | |
| Notes | This is a comparison between Autodialer arm and usual care arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator. Quote: "At study initiation, participants were assigned by computer generated random numbers to 1 of 4 groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and study staff were not blinded. Quote: "We did not attempt blinding" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "All analyses were based on intention to treat" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Low risk | No significant difference between the intervention and control groups for any demographic or vaccination characteristic |
Leirer 1991.
| Methods |
Aims: to investigate whether inexpensive telephone voice mail technology be used to improve medication adherence Study design: RCT; recruitment: community centre (advert in clinic) Study duration: 2 weeks; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: elders with no debilitating illness, depression, significant cognitive impairment, or medication schedules involving ≥ 2 drugs Sample size: 16; mean age: 71 years; sex: men ‐ 31%; women ‐ 69%; ethnicity: * Country: USA |
|
| Interventions |
Intervention group received TeleMinder, a computer hardware and software system that makes it possible for health care providers to enter elders' names, addresses, phone numbers, medication schedules, and other relevant information into a database. The health care provider also speaks the elders' names and a set of voice message segments that can later be merged in different combinations to make personalised voice messages for all or any subset of elders in the data base. TeleMinder message included the following: it asked them to verify that it had reached the correct person, it reminded them which medications they were supposed to scan, and it gave them 6 choices. These choices were hearing: the medication reminder again, a joke of the day, a health care tip of the day, the famous birthdays of the day, the big band 'name‐that‐tune' quiz, or they could hang up the phone. If they listened to 1 of the 4 messages, it was followed by a repeat of the medication reminder message, a brief goodbye message, and finally the phone line would disconnect. Participants in the control group received no calls. |
|
| Outcomes | Medication non‐adherence; cognitive assessment (primary) | |
| Funding | SBIR grants #1 R44 AC06957‐02 and #R44AC06753‐02 from the National Institute on Aging | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This study has a very small sample size. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After selecting 16 subjects for phase one of the experiment, eight subjects were randomly assigned to the voice mail condition and eight to the control condition." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | No baseline data provided. Insufficient evidence to judge whether this has introduced bias. |
Lieu 1998.
| Methods |
Aims: to evaluate the effectiveness and cost‐effectiveness of sending letters, automated telephone messages, or both to families of under‐immunised 20‐month‐olds in an HMO Study design: RCT; recruitment: other ‐ health plan (organisational referral) Study duration: 4 months; study type: prevention; subtype: immunisations |
|
| Participants |
Inclusion criteria: under‐immunised 20‐month‐olds living in the residence areas of 10 northern California medical centres of the Kaiser Permanente Medical Care Program of Northern California, a non‐profit, group‐model health maintenance organisation Sample size: 752; mean age: 20 m; sex: * ; ethnicity:* Country: USA |
|
| Interventions |
An automated telephone message (IVR) alone. A prerecorded message approximately 1‐min long was sent to each family, stating that the child was overdue for immunisations and providing the telephone numbers of the advice/appointment lines at the nearest Kaiser Permanente clinics. The message was personalised to the extent that the child's first name was spoken by software that generated the name from text. The system prompted the listener to choose the language in which the message was to be delivered (English, Spanish, or Cantonese), asked him or her to confirm that the correct family had been reached, and also enabled him to replay the message if desired. The system kept records of the results of each call. Messages were sent on Tuesdays between 5 pm and 9 pm by the Customer‐Activated Appointment Processing Services (CAAPS), an automated telephone message system. Telephone numbers that could not be reached because there was no answer either by a person or an answering machine were called again the following evening, up to 6 attempts. An automated telephone message followed by a letter 1 week later A letter followed by an automated telephone message 1 week later Letter alone. The letters were personalised; printed in English, Spanish, and Cantonese; and included a list of which immunisations were needed by 24 months of age *Quote: "The current study did not randomise patients to no intervention because a previous randomised controlled trial in our setting had found that letters increased immunisation relative to no intervention. However, to estimate the proportion of under‐immunised 20‐month‐olds who would receive immunisations with no intervention, we evaluated a comparison group of similar patients who turned 20 months old during January 1996." |
|
| Outcomes | Immunisation status by 24 months of age (primary); costs; acceptability (secondary) | |
| Funding | Northern California Kaiser Permanente and CDC | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | The sample size of 160 children to each intervention group was expected to have 80% power to detect a 16% difference in the percentage of children receiving any immunisation during the 4 months after their families were sent the message | |
| Notes | This is a comparison between the IVR alone arm and the letter alone arm. Costs of using automated telephone messages alone were USD 9.80, and USD 10.50 using letters alone | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Families of under immunized children were equally randomised to receive one of four interventions" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "The primary analysis classified patients on the basis of intention‐to‐treat, i.e., a family assigned to receive an automated telephone message or letter was analysed as part of the assigned group regardless of whether our record indicated they received a completed message or letter" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Lim 2013.
| Methods |
Aim: to determine whether multiple interventions influence adherence to glaucoma medication and to study the relationship between personality type and adherence Study design: RCT; recruitment: tertiary care (*) Study duration: 5 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: controlled disease (intraocular pressure at target level) on monotherapy with a topical prostaglandin agent; 18 years or older Sample size: 80; mean age: 66;sex: men ‐ 49%, women ‐ 51%; ethnicity: white ‐ 62%, African American ‐ 10%, Hispanic/Latino ‐ 9%, Asian ‐ 9%, East Indian ‐ 6% Country: USA |
|
| Interventions |
Participants in the intervention group received a programmed automated telephone call (SmartTalk, Televox Inc., Mobile, AL) once per month reminding them to take their eye drop medication. At the 3‐month visit, they participated in a scripted, interactive educational session with the research coordinator. The educational session, which lasted approximately 20‐30 min, reviewed the definition of glaucoma and its ability to cause blindness; the importance of using eye medications to control glaucoma; tips on using eye drop medication; and demonstration of how to instil eye drops into the eye. The control group was seen at the baseline visit and received a standard 5‐month follow‐up visit at the time of study completion. Although this group was also instructed in and monitored using the medication event monitoring system (MEMS) system, they did not receive any additional patient education materials or telephone reminders regarding glaucoma. The control group did not receive an attention placebo |
|
| Outcomes | Adherence rate; therapeutic coverage (both primary) | |
| Funding | Allergan Incorporated and Research to Prevent Blindness, New York, NY | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | A sample size of 127 per group to achieve a power of 80% was calculated. However, medication dosing is different in our study (once daily dosing) than in Kass' prior studies and this may greatly alter the true sample size. In addition, investigators were also looking for a difference in adherence rates based on physician intervention and automated monthly telephone reminders, which is different than in the Kass studies. Therefore, 1/3 of the calculated sample size was chosen as a pilot study. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were prospectively randomised to either an intervention or a nonintervention group using a random number table." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Informed consent, interviews collecting demographic data and medical history, and testing sessions were administered by trained research assistants who were not masked to diagnosis" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data were balanced in numbers, with similar reasons for missing data across groups. However, insufficient information to judge if missing data have been imputed using appropriate methods. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "No statistically significant difference existed between patients in the intervention and nonintervention groups in terms of age, sex, self‐reported ethnicity, glaucoma diagnosis, average length of diagnosis, number of systemic medications, number of medical problems, vision, intraocular pressure, highest level of education reported, and highest level of income reported" (Table 14) |
Linkins 1994.
| Methods |
Aims: to assess the effectiveness of computer‐generated telephone reminder and recall messages in increasing preschool immunisation visits Study design: quasi‐RCT;recruitment: other ‐ county health departments (organisational referral) Study duration: 5 months; study type: prevention; subtype: immunisation |
|
| Participants |
Inclusion criteria: any child younger than 2 years if his or her computerised immunisation record contained a telephone number and if the child was due or late for immunisation(s) at any time during the 4‐month enrolment period Sample size: 8002; mean age: < 2 years; sex: boys ‐ 51%, girls ‐ 49%; ethnicity: black ‐ 50%, white ‐ 45%, other – 5% (including Hispanic, Asian, and unknown) Country: USA |
|
| Interventions |
Intervention: before each calling session, children whose households were scheduled to receive a message were identified by the computer; telephone numbers and immunisation categories of these children were then downloaded to the automated dialing machine (System 606, Telecorp Systems Ine, Roswell, GA). For each calling session, the automated dialing machine recorded household‐specific information on the number of attempted contacts made and whether a successful contact had occurred. Following each calling session, this information was uploaded and merged with the study file.The households of children in the intervention group were called by the automated dialling machine twice daily for 7 days until successful telephone contact was established. To maximize the probability of reaching a parent, all weekday telephone attempts were made during evening hours. For children who were due for an immunisation, attempts at telephone contact began the day before the child was due. For children who were late for an immunisation, attempts at telephone contact began immediately after randomisation. Immunisation visits were immediately recorded in each health department's immunisation database when any child arrived for an immunisation. All children randomised to receive a telephone message received a second message if no immunisation visit was made in the week following the first successful telephone contact Control group received no calls. |
|
| Outcomes | Immunisation status at 1 month | |
| Funding | CDC | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequence generated in a non‐random way (odd or even numbers). Quote: "Children were allocated to an intervention group if their telephone numbers were assigned to an odd number; all other children were assigned to the non‐intervention group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | High risk | Data on the differences between the groups by county, type of residence, ethnicity, sex, or age were not reported |
| Other bias | Unclear risk | Insufficient information |
Litt 2009.
| Methods |
Aims: to explore whether an individualised assessment and treatment programme (via IVR) could be devised that would train adaptive coping skills to alcoholic patients more effectively than current manual‐based coping skills treatments Study design: RCT; recruitment: primary care (advert elsewhere ‐ newspaper and radio, other research programmes) Study duration: 16 weeks; study type: management; subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: to be eligible individuals had to be ≥ 18 years old, meet DSM‐IV criteria for alcohol abuse or dependence, and be willing to accept random assignment to either of the 2 treatment conditions Sample size: 110; mean age: 49 years; sex: men ‐ 58%, women ‐ 42%; ethnicity: white ‐ 86%, black ‐ 9%, Hispanic ‐ 3%, other ‐ 2% Country: USA |
|
| Interventions |
The Individualized Assessment and Treatment Program (IATP) employed a functional analysis of participants' behaviour as assessed by the IVR system during the 2‐week pretreatment experience‐sampling period. The situations that each participant encountered during experience sampling monitoring were reconstructed from the monitoring data, along with accompanying mood states, cognitive appraisals and coping actions taken. A functional analysis chart with this information was prepared by a research assistant and delivered to the therapist prior to the first IATP treatment session. IATP sessions focused on training 4 basic coping skills sets in each situation: avoidance, escape, environmental modification, and personal coping. Sessions 1 to 3 were devoted to analysing the high‐risk situations shown in the personalised functional analysis chart. Coping skills training initially addressed identification and avoidance of the participant's specific high‐risk situations. For situations that could not be avoided, training included skills such as environmental modification, drink refusal and assertiveness specifically tailored for dealing with the identified high‐risk situations, escape from high‐risk situations, and 'personal coping'. Homework was individualised, and built on information revealed in the functional analysis chart, as well as other situations recalled by the participant. Packaged Cognitive‐Behavioural Therapy was based on cognitive‐behavioural principles and designed to remediate deficits in skills for coping with interpersonal and intrapersonal antecedents to drinking. The treatment, based on manuals developed for previous clinical research and for Project MATCH, provided a structured experience using didactic presentations, behavioural rehearsal, and homework practice exercises. Homework was prescribed after every session, and was relevant to the material covered in that session. |
|
| Outcomes | Proportion of days abstinent; proportion of heavy drinking days; continuous abstinence; drinking problems; coping problems (all primary) | |
| Funding | R21‐AA014202 from the National Institute on Alcohol Abuse and Alcoholism, and General Clinical Research Center grant M01‐RR06192 from the National Institutes of Health | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | A sample size of 50 per cell was determined to be sufficient to test most hypotheses with a power of 0.80 and alpha set at 0.05 based on effect sizes derived from previous studies of coping skills measures and outcomes | |
| Notes | ClinicalTrials.gov Identifier:NCT00298792. This is a comparison of 2 different interventions delivered via IVR | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were assigned to treatment using an urn randomisation procedure that balanced the two groups for sex, age, baseline readiness to change, self‐efficacy and Coping Strategies Scale Total score" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "the failure to blind research assistants to treatment assignment must be considered a weakness" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review have been reported |
| Other bias | Unclear risk | Insufficient information |
Lorig 2008.
| Methods |
Aims: to determine whether Spanish Diabetes Self‐Management Program (SDSMP) participants receiving monthly automated telephone reinforcement would maintain improvements in health status, health behaviours, and self‐efficacy at 18 months better than those not receiving reinforcement Study design: RCT;recruitment: other – community (word of mouth, announcements in churches, clinics, and Spanish language mass media) Study duration:18 months; study type: management; subtype: diabetes |
|
| Participants |
Inclusion criteria: participants were ≥ 18 years, not pregnant or in care for cancer, and had type 2 diabetes. They were enrolled in the SDSMP trial. Also included the control participants who had subsequently taken the SDSMP Sample size: 417; mean age: 53 years; sex: men ‐ 38%, women ‐ 62%; ethnicity: Hispanic (Spanish‐speaking) ‐ 100% (73% born in Mexico) Country: USA |
|
| Interventions |
Participants received automated telephone reinforcement once a month. They were greeted and asked to rate their diabetes self‐efficacy in the next month; had option to listen to two, 90‐s vignettes about various aspects of diabetes, and each of 15 vignettes was offered twice over 15 months—participants might hear about how Alexandra solved problems eating with her family or how Jose talked to his doctor about impotence; participants could leave a message. If necessary, a staff member responded to these messages. Participants in the control group received usual care. |
|
| Outcomes | Glycated haemoglobin; health distress; global health; hypoglycaemia; hyperglycaemia; activity limitation; fatigue; glucose monitoring; self‐efficacy; healthcare utilisation (all primary) | |
| Funding | National Institutes of Health/National Institutes of Nursing Research Grant, Michigan Diabetes Research and Training Center | |
| Declaration of conflict of interest | KL receives royalties from Bull Publications for Tomando Control de su Salud, the book used by course participants | |
| Power calculations for sample size | NA | |
| Notes | The SDSMP is a 6‐week programme offered 2.5 h weekly by 2 peer leaders. Programmes were held in community settings in 6 San Francisco Bay Area counties. Class sizes ranged from 10 to 15 including participants' family and friends. Spanish‐speaking peer leaders (N = 43) came from the same communities as the participants. Most had type 2 diabetes and were not health professionals. They received 4 days of training. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Following baseline data collection, most study participants were randomised to three groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Complete case analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Comment: groups were comparable across all baseline characteristics but sex (control group had significantly more women participants compared with intervention, i.e. 67.2% vs 57.1%); however it is unclear if this imbalance has introduced bias. |
Magid 2011.
| Methods |
Aims: to determine if a multimodal intervention composed of patient education, home blood pressure monitoring, blood pressure measurement reporting to an IVR phone system, and clinical pharmacist follow‐up improves blood pressure control compared with usual care. Study design: RCT;recruitment: primary care (telephone) Study duration: 6 months; study type: management; subtype: hypertension |
|
| Participants |
Inclusion criteria: patients with hypertension who were taking ≤ 4 antihypertensive medications and who had elevations in 2 of the 3 most recent electronic blood pressure measurements Sample size: 283; mean age: 65 years; sex: men ‐ 65%, women ‐ 35%; ethnicity: white ‐ 65%, other – 18%, Hispanic ‐ 17% Country: USA |
|
| Interventions |
Multimodal intervention included the following components: patient education, home blood pressure monitoring, home blood pressure measurement reporting to an IVR phone system, and clinical pharmacist management of hypertension with physician oversight. Participants input their systolic and diastolic blood pressure reading using the touch‐tone keypad of their phone during the weekly IVR calls. IVR, after calculating the average, provided feedback on whether their blood pressure measurements were at goal. They also had an opportunity to listen to educational messages or to request a call from the clinical pharmacist to answer questions. The blood pressure measurements were also reviewed by clinical pharmacists and participants received appropriate counselling. Those who did not enter any blood pressure measurements into the IVR system after 10 days received an automated reminder call, followed by a call from the pharmacist 4 days later Participants in the control group received usual care. |
|
| Outcomes | Change in systolic and diastolic blood pressure (primary); medication adherence (secondary) | |
| Funding | American Heart Association and Colorado Department of Public Health and Environment | |
| Declaration of conflict of interest | "Dr Ho reports serving as a consultant for Wellpoint, Inc. The other authors (DJM, KLO, DWB, LKW, KES, ACLK, MEP, EPH) report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article." | |
| Power calculations for sample size | NA | |
| Notes | ClinicalTrials.gov Identifier: NCT01162759 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A block randomisation design was used to ensure balance within healthcare systems. A random allocation sequence was computer generated using stratified randomisation with an allocation ratio of 1:1" |
| Allocation concealment (selection bias) | Low risk | Quote: "The sequence was concealed until the intervention and usual care groups were assigned at the baseline visit." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The research assistant who obtained the blood pressure measurements was blinded to patient study group assignment." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Of 338 patients enrolled in the study, 283 (84%) completed the 6‐month visit . . . Our primary analyses applied intent‐to‐treat principles to patients who completed the end‐of‐study visit . . .Patients who did not complete the study had higher baseline systolic and diastolic blood pressure" |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol is available; and all of the study's pre‐specified outcomes that are relevant to the review have been reported |
| Other bias | High risk | Baseline imbalance. The intervention had significantly higher systolic blood pressure compared with the control group. Quote: "At baseline, the mean (SD) blood pressures were significantly higher for 138 intervention patients vs 145 usual care patients" |
Mahoney 2003.
| Methods |
Aims: to assess the effects of computer‐mediated automated IVR intervention designed to assist family caregivers managing persons with disruptive behaviours related to Alzheimer's disease (AD) Study design: RCT; recruitment: primary care and community (organisational referral and media adverts) Study duration: 18 months; study type: management; subtype: stress management |
|
| Participants |
Inclusion criteria: over the age of 21, provided ≥ 4 h per day of assistance or supervision for a minimum of 6 months to a family member with AD who had ≥ 2 impairments of instrumental activities of daily living (e.g. driving, shopping, or managing money) or 1 activity of daily living (e.g. toileting, bathing, eating), and exhibited ≥ 1 AD‐related disturbing behaviour Sample size: 1100 dyads; mean age: 63 years; sex: men ‐ 22%, women ‐ 78%; ethnicity: white ‐ 79%, black or African American ‐ 16%, Hispanic ‐ 2%, other – 2% Country: USA |
|
| Interventions |
Telephone‐Linked Care (REACH for TLC): participants chose the type of component, frequency, duration, and timing of the usage. The automated IVR conversation monitored the caregiver's stress levels and provided information on how to manage the care recipient's behavioural problems. Personal mailbox allowed caregivers to anonymously send and receive confidential communications through voice mail among themselves or to communicate with a clinical nurse specialist who directly answered or triaged questions to a multidisciplinary professional panel of AD experts. Bulletin board users anonymously posted messages and received responses back from other users. Activity–respite conversation provided personalised pleasant conversation to engage the listener in a safe, comforting, and non‐demanding activity. Participants in the control group received usual care. |
|
| Outcomes | Caregiver's appraisal of the bothersome nature of care‐giving; anxiety; depression (primary) | |
| Funding | National Institutes of Health (NIH) National Institute on Aging | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Two separate computer‐generated random assignment lists, one for men and one for women, were generated for each recruitment site, ensuring that each intervention and control group was balanced by sex and site." |
| Allocation concealment (selection bias) | Low risk | Quote: "After the completion of the baseline data, the interviewer opened an envelope that contained the group assignment." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All participants were subsequently interviewed at time points of 6, 12, and 18 months by different telephone interviewers who were blind to the study assignments except for the user satisfaction survey at the completion of the intervention period" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers, with similar reasons for missing data across groups. "There was no significant difference in the frequency of missing data between intervention and control groups for the outcome measures (p > 0.05)" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Low risk | Quote: "The intervention and control groups did not differ significantly for any of the outcome dimensions at baseline." |
Maxwell 2001.
| Methods |
Aims: to determine the impact of reminder systems on appointment non‐adherence rates in an low‐income inner city clinic population Study design: RCT; recruitment: primary care (organisational referral) Study duration: 2 months; study type: either; subtype: appointment reminders |
|
| Participants |
Inclusion criteria: patients due for an initial/annual gynaecology visit or initial prenatal intake visit in the women's health department over a period of 2 months Sample size: 2304; mean age: 29 years; sex: women ‐ 100%; ethinicty: Hispanic ‐ 66%, black ‐ 19%, white ‐ 13%, other ‐ 2% Country: USA |
|
| Interventions |
Automated telephone reminder of their appointment the day prior to the actual appointment Postcard reminder No reminder (control group) |
|
| Outcomes | Attendance rate | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | The criterion for significance (alpha) was set at 0.05 (2‐tailed). To determine whether the sample size was sufficient to test our hypothesis, power was calculated using historical Hartford Hospital data and data reported previously in the literature. With the given effect size, a sample size of 1140 would have a power of 90 percent to yield a statistically significant result using a 3 x 2 Chi2 contingency test. | |
| Notes | This is a comparison between automated telephone and no reminder. The other intervention included postcard reminder | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients who verbally consented to participate in the study were randomly assigned to receive a phone reminder, mailed reminder, or no reminder (control group)" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of study personnel was ensured. Quote: "Group assignment was unknown to those administering health care" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "There were no significant differences in characteristics between the control and intervention groups for either the caregivers or the care recipients enrolled in the study" |
McNaughton 2013.
| Methods |
Aims: to test whether IVR telephony may decrease the relapse rate after smoking cessation Study design: RCT; recruitment: other ‐ community (newspaper advert) Study duration: 24 months; study type: management; subtype: smoking |
|
| Participants |
Inclusion criteria: smoking ≥ 35 cigarettes per week or ≥ 5 cigarettes per day for ≥ 2 years with no period of abstinence longer than 3 months Sample size: 44; mean age: 53 years; sex: men ‐ 67%; women ‐ 33%; ethnicity: * Country: Canada |
|
| Interventions | After 12 weeks, the intervention group continued to receive IVR calls every 2 weeks from weeks 13–52. The IVR intervention consisted of 2 parts: establishing it is speaking to the study participant and the main data collection section. As instructed at the beginning of the call, the participant answers 'yes' or 'no' to all questions except when asked about their level of confidence and their side effects. The IVR asks if they have had a cigarette since their quit date, if they have smoked a cigarette, even a puff, if they have used varenicline in the last 14 days, have they experienced any side effects, how confident they are that they will remain a non‐smoker, and would they like to have a study nurse call them to help prevent relapse or provide advice about varenicline. Finally, there is a positive reinforcing message thanking and congratulating them followed by "remaining smoke‐free is the single most important thing you can do for your health". The calls are 3–5 min long, depending on their answers and which part of the algorithm they are directed to. The IVR made a call on their quit day, then on day 3, 8, and 11, and every 2 weeks thereafter The control group received no further IVR calls (no intervention) |
|
| Outcomes | Self‐reported abstinence; biochemically confirmed smoking abstinence (both primary) | |
| Funding | Pfizer (Canada) | |
| Declaration of conflict of interest | Jiri Frohlich was a member of Pfizer (Canada) Medical Advisory Board and received speaking honoraria. He also participated in several clinical trials and received grants for investigator initiated studies. | |
| Power calculations for sample size | NA | |
| Notes | In phase 1 of the study, participants also received a 12‐week supply of varenicline: 0.5 mg to be taken on days 1–3, 0.5 mg twice a day on days 4–7, and 1 mg twice a day until the end of week 12. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants who had quit smoking at 12 weeks were randomised into 2 groups matched by their level of motivation and level of addiction as per psychometric questionnaire at baseline. This was a stratified randomisation whereby participants were categorized by motivation and addiction." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Participants in the intervention smoked mean (SD) no. of cigarettes per day at baseline: 18.5 (6.6) versus 17.3 (8.6) in control. Insufficient evidence to judge whether this has introduced bias. |
Migneault 2012.
| Methods |
Aims: to evaluate a culturally adapted, automated telephone system to help hypertensive, urban African American adults improve their adherence to their antihypertensive medication regimen and to evidence‐based guidelines for dietary behaviour and physical activity Study design: RCT; recruitment: primary care (mail and telephone) Study duration: 12 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: self‐identification as African American; a diagnosis of hypertension on the active problem list of the patient's medical chart; a current prescription for ≥ 1 antihypertensive medications; ≥ 1 primary care office visits in the previous 2 months; 2 elevated clinic blood pressure readings in the previous 6 months (systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg among non‐diabetic patients, and ≥ 130/80 among diabetic patients); and age ≥ 35 years Sample size: 337; Mean age:57 years; sex: men ‐ 30 %; women ‐ 70 %; ethnicity: African American ‐ 100 % Country: USA |
|
| Interventions |
Telephone‐Linked Care for Hypertension: at the onset, participants received a 75‐page resource manual that described hypertension, listed dietary recommendations, heart healthy food recipes, and local resources for exercise, and provided information to support antihypertensive medication adherence. Based on the manual, they received a 20‐min education session, and were given a pedometer and a digital weight scale. Participants in the intervention group also received a digital home blood pressure monitor. The automated telephone intervention delivered 1 call per week for 32 weeks. The first 3 calls introduced the 3 targeted behaviours and their role in blood pressure control. Subsequent calls were arranged as modules on medication adherence, physical activity, and diet, and were delivered in the order chosen by the participant. Each call consisted of an introduction, a section for reporting health information collected on study‐issued home measurement devices (pedometers, sphygmomanometers, weight scales), and theory‐based interactive education and counselling on the targeted behaviour. Physical activity module consisted of 12 calls to increase levels of moderate‐or‐greater intensity physical activity. The diet module consisted of 9 calls ‐ 1 overview call and 2 calls for each of 4 topics: fruits and vegetables, fibre, sodium, and fat. The content of these calls was designed to promote the DASH diet. The medication adherence module consisted of 8 calls. Study staff monitored participant use of the system and contacted those who did not call to assist or re‐engage them with the system Participants in the control group received usual care (education‐only). |
|
| Outcomes | Medication adherence (primary); diet; physical activity; blood pressure (secondary) | |
| Funding | National Heart, Lung, and Blood Institute | |
| Declaration of conflict of interest | "Dr. Friedman has stock ownership and a consulting agreement with InfoMedics, the company that owns commercial rights to the TLC technology used in the computerized intervention. He is also a member of its Board of Directors. None of the other authors has any potential conflicts of interest to disclose." | |
| Power calculations for sample size | "Based on power analyses and projected attrition, we sought to randomise 360 patients expecting 300 to complete the 8‐month study assessment thus providing sufficient power to analyse the three primary behavioral outcomes." | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was accomplished using a random number generator to assign subjects to one of the two groups" |
| Allocation concealment (selection bias) | Low risk | Quote: "Neither participants nor research assistants knew the group assignment until after baseline assessments were complete." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Missing data were imputed using the last value carried forward. For cases where data were available at time points before and after the missing value, the mean of these two values was used." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | High risk | Quote: "Intervention group participants reported more moderate‐or‐greater physical activity per week than controls (162.4 min. vs. 126.3 min., p=0.04), and a greater percentage of the intervention group met national moderate‐or‐greater physical activity recommendations (38.5% vs. 26.2%, p<0.02). In addition, more intervention group participants than controls reported a history of stroke (11.2% vs. 4.2%, p<0.02)." Comment: groups were not comparable with significant baseline differences in physical activity (one of the study's primary outcomes) and stroke history |
Mooney 2014.
| Methods |
Aims: to enable oncology providers to receive and act on alert reports from patients about unrelieved symptoms during chemotherapy treatment Study design: RCT; recruitment: community centres and clinics (in‐person at the clinic) Study duration: 45 days; study type: management; subtype: cancer |
|
| Participants |
Inclusion criteria: eligible patients were to receive ≥ 3 chemotherapy cycles, were ≥ 18 years, had daily access to a touch‐tone telephone, understood English or Spanish, were physically and mentally able to participate, and reported ≥ 1 symptom of moderate or greater intensity during their first chemotherapy cycle Sample size: 250; mean age: 55.5 years; sex: men ‐ 24%; women ‐ 76%; ethnicity: Caucasian ‐ 91%, other ‐ 9% Country: USA |
|
| Interventions |
Automated monitoring system to report daily on 10 symptoms—pain, fatigue, nausea/vomiting, fever, trouble sleeping, anxiety, depressed mood, sore mouth, diarrhoea, and constipation. The symptoms were selected from the literature and confirmed in our pilot study as most frequently reported by patients receiving chemotherapy. Participants were queried if symptoms were present in the past 24 h and, if present, they rated severity and distress on a 1–10 scale. The 1–10 numeric scale is commonly used clinically and is an accepted standard in the measurement of symptoms; questions could be stated easily on the phone and answered numerically with the touch‐tone keypad. If fever was reported, the highest temperature was entered numerically; in addition, distress but not severity was measured for fever. For the treatment group, at completion of the phone call, the system immediately faxed or emailed (based on provider preference) symptom alert reports to the participant's oncologist and oncology nurse. Alert thresholds varied by symptom; they were initially established by an expert panel and then revised based on pilot work. 2 thresholds were set: a simple alert when severity or distress was > 5 or 7 (depending on the symptom) on the 10‐point scale and trend alerts based on a pattern of moderate severity over several days. For example, pain generated an alert when pain was rated at 5 or greater, whereas fatigue generated an alert at 7 or a trend alert based on a pattern of 3 out of the past 7 days reported at moderate levels (4–6). The report included not only severity and distress but a symptom profile including answers to drill‐down questions such as the number of vomiting episodes, oral intake, dizziness, and use of antiemetics for nausea. Reports also included graphs of symptom patterns since the first day of chemotherapy. On every call, all participants, regardless of group, were advised to call their oncology providers if they had concerns about their symptoms. In all of the participating provider teams, normal usual care procedure for unrelieved symptoms was to instruct participants to call the clinic office for symptom concerns Attention control group received equivalent contact time with the automated system including identical voice and assessment questions. They understood that the data they submitted were for research purposes only and were not available for clinical action. On every call, all participants, regardless of group, were advised to call their oncology providers if they had concerns about their symptoms. In all of the participating provider teams, normal usual care procedure for unrelieved symptoms was to instruct participants to call the clinic office for symptom concerns |
|
| Outcomes | Symptom severity, and distress (primary); system usability and acceptability (secondary) | |
| Funding | National Institutes of Health, National Cancer Institute (R01 CA89474) | |
| Declaration of conflict of interest | None reported | |
| Power calculations for sample size | A post hoc sensitivity analysis was conducted with G*Power to access available statistical power. With a sample size of 223 participants, investigators had sufficient power (1 −Β)=0.91 to detect a small effect size Cohen's d = 0.10 and alpha = 0.05 | |
| Notes | Similar ATCS interventions were compared with each other. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were stratified by provider team to ensure equivalency of the treatment and control groups within teams and then randomly assigned to treatment or attentional control. Random assignments in blocks of ten were generated for each provider stratification group." |
| Allocation concealment (selection bias) | Low risk | Quote: "Research staff and patients did not know assignment until after informed consent." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Providers were not informed of random assignment but could not be blinded as they would only receive alert reports about treatment group patients." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Twenty‐seven participants dropped from the treatment group (21%) and 31 from the control group (26%), a non‐significant difference (p>0.05)." Comment: insufficient information whether this drop‐out rate introduced bias. |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Unclear risk | The intervention had significantly more women and breast cancer diagnosed participants compared with the control, but there is insufficient evidence that this imbalance has introduced bias. Quote: "Comparisons of group equivalence at baseline indicated that the treatment group was over‐represented by women (chi‐square 4.89; p=0.027) and breast cancer diagnosis (chi‐square=9.56; p=0.023)." |
Moore 2013.
| Methods |
Aims: to evaluate feasibility, acceptability, and initial efficacy of a therapeutic IVR system for opioid dependent patients receiving methadone maintenance who were continuing to use illicit drugs while enrolled in treatment Study design: RCT; recruitment: primary care (clinic posters and flyers, brochures provided to counsellors, and word‐of‐mouth) Study duration: 1 month; study type: management; subtype: illicit drugs addiction |
|
| Participants |
Inclusion criteria: no current suicide or homicide risk; lack of a DSM‐IV current psychotic or bipolar disorder; not involved in another treatment study; ability to read or understand English; and lack of a life‐threatening or unstable medical problem Sample size: 36; mean age: 41 years; sex: men ‐ 58%; women ‐ 42%; ethnicity: white ‐ 58%, black ‐ 28%, other – 14% Country: USA |
|
| Interventions |
The Recovery Line plus treatment‐as‐usual involved a therapeutic IVR orientation session, 4 weeks of 24‐h access to the system, a participant notebook with summary Recovery Line information, and a weekly reminder from staff to use the system. The Recovery Line system was developed for participants to use in their own environment and obtain immediate assistance, training, and support for improved coping. Modules were designed to be brief (< 15 min) and easy to understand. System components included self‐monitoring, coping with urges and cravings, identifying/avoiding risky situations, and managing moods and stress. For self‐monitoring, a daily questionnaire of 3 items was included immediately upon system log in ("How are you doing?" "Have you taken your methadone today?" "Have you used illicit drugs since your last call?") Participants in the control group received usual care. The proposed system was meant to serve as an enhancement of current services being delivered, which included the requirement to attend 1 individual session per month and encouragement to attend open access groups (with ≥ 10 typically available Monday–Friday) covering a range of topics, including introduction to methadone, weekend planning, overdose planning, and spirituality. These are the services provided in the standard care comparison condition. |
|
| Outcomes | Patient interest; perceived efficacy; treatment satisfaction; drug consumption (self‐reported use); methadone counselling; ease of use; coping skills (all primary) | |
| Funding | National Institute on Drug Abuse Grants and through the State of Connecticut, Department of Mental Health and Addiction Services support of the Connecticut Mental Health Center | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | None | |
| Notes | ClinicalTrials.gov Identifier: NCT01315184 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised (N=36) to 4 weeks of treatment‐as‐usual (TAU) or Recovery Line plus TAU." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "There were no statistically significant differences between the two treatment conditions, but several trends were controlled through covariance adjustments." There is insufficient evidence that these covariates have introduced bias. |
Morey 2009.
| Methods |
Aims: to determine the effects of multicomponent physical activity counselling (PAC) promoting physical activity guidelines on gait speed and related measures of physical activity and function in older veterans Study design: RCT; recruitment: primary care (mail and telephone) Study duration: 12 months; study type: prevention; subtype: physical activity |
|
| Participants |
Inclusion criteria: patients were eligible for the study if they could walk 30 feet without human assistance and did not engage in regular physical activity Sample size: 398; mean age: 78 years; sex: men ‐ 100%; ethnicity: white ‐ 77% Country: USA |
|
| Interventions |
Multimodal intervention group received: baseline in‐person and biweekly then monthly telephone counselling by a lifestyle counsellor, onetime clinical endorsement of physical activity and monthly automated telephone messaging by primary care provider, and quarterly tailored mailings of progress in physical activity Participants in the control group received usual care. |
|
| Outcomes | Gait speed (usual and rapid); self‐reported physical activity; function and disability (all primary); change in min of moderate/vigorous physical activity per week (secondary) | |
| Funding | Veterans Affairs Rehabilitation Research and Development # E3386R and NIH grant AG028716 | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | Quote: "We powered the sample size for this study to be able to detect a between group difference of 0.10 m/sec in both usual and rapid gait speeds." | |
| Notes | 1 participant died in the intervention group; 6 died in the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was computer generated by a statistician" |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was . . . sealed envelopes stored in the Veterans LIFE Study office until randomisation." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The study was unblinded and patients were aware of the study objectives." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All assessments were made at baseline, three, six, and 12 months by individuals blinded to randomisation status" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Return for follow‐up was similar for both groups with slightly more withdrawals in the PAC group [16 (8%)] than in the UC group [11 (5.5%)]. There were no differences between dropouts and individuals completing the trial except for usual gait speed which was significantly lower in the drop outs (−0.9 m/sec, p = 0.016)." Insufficient evidence to judge whether this introduced bias. |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐specified outcomes have been reported accordingly. |
| Other bias | Low risk | Baseline characteristics were similar between the 2 groups. |
Morey 2012.
| Methods |
Aims: to determine whether a home‐based multi‐component physical activity counselling (PAC) intervention is effective in reducing glycaemic measures in older prediabetic outpatients Study design: RCT; recruitment: primary care (mail and telephone) Study duration: 12 months; study type: prevention; subtype: physical activity |
|
| Participants |
Inclusion criteria: impaired glucose tolerance defined as a fasting glucose between 100–125 mg/dL, free from a diagnosis of diabetes, have a glycated haemoglobin below 7%, and not be on diabetes medications. A BMI between 25 and 45 kg/m2 was required Sample size: 302; mean age: 67 years; sex: men ‐ 97%, women ‐ 3%; ethnicity: white race ‐ 70% Country: USA |
|
| Interventions |
Multimodal intervention group received: 1 in‐person baseline counselling session, regular telephone counselling, physician endorsement in clinic with monthly automated (telephone calls) encouragement, and tailored mailed materials, plus a consult to a Veterans Affairs (VA) weight management programme Participants in the control group received usual care plus MOVE programme |
|
| Outcomes | Fasting insulin and glucose levels measured with homeostasis model assessment of insulin resistance (HOMA‐IR); glycated haemoglobin; anthropometric measures; self‐reported physical activity; health‐related QOL; physical function | |
| Funding | VA Health Services Research and Development grant IIR‐06‐252‐3; National Institute on Aging grant AG028716; VA Rehabilitation Research Service grants (RRD‐E2756R, RRD‐E3386R) and National Cancer Institute grant CA106919; Department of Veterans Affairs Health Services Research and Development Career Scientist Award (RCS 08‐027) | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | Power estimates were calculated using data from the STRRIDE study in which a group receiving a low dose of moderate exercise, equivalent to the dose of moderate exercise advocated for the Enhanced Fitness Study, reduced fasting insulin by 1.3 units while the control group experienced an increase in fasting insulin of 0.92 units with a pooled standard deviation of 3.9. With correction for multiple comparisons between adaptive strategies and a projected 12.5% attrition rate based on our previous experience, our sample size was 80% powered to detect a standardised difference of 0.39 in fasting insulin for a 2‐tailed test | |
| Notes | 2 participants died in the intervention group; 1 died in the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Adaptive randomisation will allow us to mimic primary care by altering treatment based upon patient compliance". Insufficient information to judge whether this introduced bias. |
| Allocation concealment (selection bias) | Low risk | Quote: "A statistician with no participant contact delivered sealed randomisation assignments to the project coordinator. These were kept in a locked cabinet until randomisation occurred." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All of the outcomes were assessed at baseline, three months and 12 months by individuals blinded to intervention status" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were performed under the intent‐to‐treat criteria" |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all pre‐specified outcomes have been reported accordingly |
| Other bias | Low risk | Quote: "Sensitivity analyses revealed no baseline differences between groups for age, race, number of symptoms, general health and physical function" |
Mosen 2010.
| Methods |
Aims: to determine the effect of an automated telephone intervention on completion of faecal occult blood testing Study design: RCT; recruitment: other ‐ health plan (organisational referral) Study duration: 6 months; study type: prevention; subtype: screening |
|
| Participants |
Inlcusion criteria: eligible participants were due for routine colorectal cancer screening (and in whom stool occult blood testing was a clinically appropriate option) and who met other criteria such as: those due for colorectal cancer screening who have not had any of the following: colonoscopy within 10 years, flexible sigmoidoscopy or double‐contrast barium enema within 5 years, faecal occult blood testing screening within past 12 months, or order for faecal occult blood testing/double‐contrast barium enema in past 3 months Sample size: 6000; mean age: 60 years; sex: men ‐ 50%, women ‐ 50%; ethnicity: white ‐ 92%, non‐white – 7%, unknown ‐ 1% Country: USA |
|
| Interventions |
Automated Telephone Contact Intervention group received up to three 1‐min automated telephone calls providing a brief overview, including information about the benefits of colorectal cancer screening, and encouraged faecal occult blood testing as a relatively simple and low‐risk method of cancer screening. Recipients could request faecal occult blood testing cards by pressing a number via touch‐tone telephone. If a live person did not answer, callers heard a detailed message with a telephone number they could call to request cards. Participants who did not complete faecal occult blood testing screening received up to 2 reminder calls, 6 weeks apart. Call content was identical to the first automated telephone call. 1 additional reminder call was targeted to intervention participants who had requested an faecal occult blood testing kit but did not return the completed faecal occult blood testing cards within 4 to 5 weeks from the date of request. The call to non‐returners (call type 2) emphasised the benefits of colorectal cancer screening and reminded participants to return completed faecal occult blood testing cards. Participants were given the opportunity to request additional faecal occult blood testing cards if needed. Participants in the control group received usual care. Participants randomised to UC did not receive the telephone contact intervention but may have been referred for colorectal cancer screening by their clinicians during normal care processes. |
|
| Outcomes | Completion of faecal occult blood testing during the 6 months after call initiation; screening through any the US Preventive Services Task Force recommended colorectal cancer screening modality during the RCT and included receipt of faecal occult blood test, colonoscopy, flexible sigmoidoscopy, or double‐contrast barium enema. | |
| Funding | National Cancer Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | We had 80% power to detect an absolute difference of 2.8% (relative difference of 28.6%), assuming the faecal occult blood test return rate was 9.7% in UC versus 12.5% in the intervention group. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 6000 patients were randomly assigned either to receive usual care (UC; n=3000) or automated telephone contacts (n=3000), using a stratified randomisation approach, balancing on age, sex, and prior colorectal cancer screening." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attritions were small (< 2% in both groups) and unlikely to introduce bias |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were similar at baseline. Quote: "No statistically significant differences were found between the 2 populations for any of the baseline characteristics." |
Mu 2013.
| Methods |
Aims: to evaluate the impact of an automated telephone reminder system on patients' on‐time maintenance medications refills Study design: RCT; recruitment: population level Study duration: 1 month; study type: prevention; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inlcusion criteria: participants due for medication refills Sample size: 4,237,821; mean age: 56 years; sex: men ‐ 38.5%; women ‐ 61.5%; ethnicity: * Country: USA |
|
| Interventions |
Participants on maintenance prescription received automated IVR calls, 3 days before their refill was due, as a reminder. If participants had multiple medications due on a single day, only 1 call for all medications was made. A maximum of 2 attempts was made for unanswered calls. If both attempts fail and a participant's voicemail was available, a message was left with phone number to call back. Messages did not identify the medication by name or any other form of protected health information. Upon answering a call, participants were required to authenticate with their date of birth. After the participants agreed to refill, their maintenance medications were automatically processed for pick‐up. Participants received calls every time they have medication to refill. Participants in the control group received no calls. |
|
| Outcomes | Daily and cumulative refill rates (the percentage of prescriptions refilled on or by a specific date around the expected refill date) | |
| Funding | Correspondence with the authors: "Yes, the study was funded internally by Walgreens Co." | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Correspondence with the authors: "Yes, this was a simple randomised study. On the first day that a patient qualified for the study, the campaign management system would assign the patient to a test or control group based on the random number. The random numbers were generated by the system based on random seed that was changed every month." |
| Allocation concealment (selection bias) | Low risk | Correspondence with the authors: "Yes, the randomisation was automated without researcher involvement" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Correspondence with the authors: "No." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Mundt 2006.
| Methods |
Aims: to evaluate the feasibility of a computer automated IVR system to reduce relapse following discharge from residential treatment Study design: RCT; recruitment: primary care (health professional referral) Study duration: 6 months; study type: management; subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: men and women, aged 20–61 years, treated for alcohol dependence at the Herrington Recovery Center, a residential treatment facility of the Rogers Memorial Hospital Sample size: 60; mean age: 42 years; sex: men ‐ 55%, women ‐ 45%; ethnicity: Caucasian ‐ 95%, African American ‐ 5% Country: USA |
|
| Interventions |
Daily IVR reporting with personal follow‐up on non‐compliant callers. The study coordinator/counsellor was instructed to make a personal telephone call to participants any time they failed to make a daily call to the IVR system for 2 consecutive days. If participants did not begin using the system thereafter, the coordinator/counsellor continued calling them daily for ≥ 10 days. After 10 consecutive days of prompting non‐compliant participants to use the system without success, the coordinator/counsellor continued to call the participants at least twice each week until system use began or they withdrew consent for study participation Daily IVR reporting without follow‐up; participants had access to the same daily IVR reporting system but were not contacted or prompted to use it if they did not make daily calls to the system No IVR reporting (control group) |
|
| Outcomes | Self‐reported drinking days, heavy drinking days and total drinks | |
| Funding | 1R43AA12366 from the NIAAA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "The relatively small sample sizes would provide inadequate statistical power to support clinical efficacy of any treatment effect that was not extremely large and that even modest study dropout rates would diminish the limited statistical power even further." | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Volunteers to participate in the study were randomly assigned to one of three treatment groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition reduced the already small sample size by 20%. Missing data have not been imputed using appropriate methods. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were similar at baseline. Quote: "No significant difference was evident between the randomised groups regarding sex, age, and length of stay in residential treatment" |
Nassar 2014.
| Methods |
Aims: to test the efficacy of a new automated call‐monitoring system for second and third trimester predominantly Medicaid‐eligible pregnant women in an urban free standing birth centre to promptly detect symptoms of influenza and assure rapid treatment to prevent adverse outcomes from influenza Study design: RCT; recruitment: primary care (*) Study duration: 2 months; study type: prevention; subtype: immunisation |
|
| Participants |
Inclusion criteria: pregnant for ≥ 12 weeks but not yet 38 weeks pregnant, attending Family Health and Birth Center for prenatal care (FHBC is the urban free‐standing birth centre, within Developing Families Center), able to speak English, operate a cell phone and agree to attend prenatal care visits Sample size: 50; mean age: 24 years; sex: men ‐ 0%; women ‐ 100%; ethnicity: African American ‐ 86%, white ‐ 14 % Country: USA |
|
| Interventions |
Automated telephone system called the automated call group participants every day at the time selected by the participant and asked questions about whether she had developed ≥ 1 of the specific influenza symptoms mentioned in the call in the past 24 h. If the participant answered 'yes', then the recording stated that she should speak immediately to the nurse midwife on call Participants in the control group received health information |
|
| Outcomes | Immunisation rate; satisfaction | |
| Funding | National Institute of Child Health and Human Development | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The random number generator in Excel was used to generate random numbers" |
| Allocation concealment (selection bias) | Low risk | Quote: "Random numbers were put into sealed envelopes and were opened at time of enrolment" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "None of the differences between experimental and control group were statistically significant at alpha of 0.05" |
Naylor 2008.
| Methods |
Aims: to assess the effectiveness of therapeutic IVR intervention in increasing treatment compliance and adherence in chronic pain patients and improving outcome at follow‐up Study design: RCT; recruitment: primary care (organisational referral) Study duration: 4 months; study type: management; subtype: chronic pain |
|
| Participants |
Inclusion criteria: at least 6 months of musculoskeletal pain (such as back pain, osteoarthritis, or fibromyalgia); met study threshold for severity of pain "over the past four weeks'' of ≥ 4 on a 10‐point scale measured at baseline on the McGill Pain Questionnaire short form; able to perform usual self‐care; had ongoing health care from a physician; aged ≥ 18, owned a touch‐tone phone Sample size: 55; mean age: 46 years; sex: men ‐ 14%, women ‐ 86%; ethnicity: white/Caucasian ‐ 96%, other 4% Country: USA |
|
| Interventions |
The intervention group received IVR calls. The system included the following:
Participants in the control group received usual care |
|
| Outcomes | Pain (total pain experience, pain intensity); Function/disability; Coping | |
| Funding | National Institute of Drug Addiction (NIDA), National Institute of Arthritis, Musculoskeletal and Skin Diseases (NIAMS), National Institute on Alcohol Abuse and Alcoholism (NIAAA) | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "The study was powered to detect an effect size of 0.5 using ANCOVA for the endpoint comparisons between the two groups." | |
| Notes | Only those participants who successfully completed 11 weeks of group CBT were recruited in the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Consenting subjects were stratified by level of pain and by sex, and then randomised to one of the two study groups" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization was done after group therapy was completed in order to avoid the risk of differential CBT exposure based on group assignment." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All participants who successfully completed CBT and who agreed to be randomised were retained for the primary analyses. For 3 cases with missing data at the second or third follow‐ups the average of the scores from the prior and following time points was used. Two participants from the TIVR group who were missing the final set of questionnaires were assumed to have regressed to the baseline." |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Unclear risk | Insufficient information |
Ownby 2012.
| Methods |
Aim: to evaluate the effect of 2 distinct interventions on medication adherence in elders treated for memory problems while taking factors such as depression and cognitive status into account Study design: RCT; recruitment: primary care (health professional referral) Study duration: 24 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: clinically judged to have a memory problem and were being treated with 1 of the approved cholinesterase inhibitor medications (donepezil, rivastigmine, or galantamine) or memantine and judged to be able to give informed consent for their participation Sample size: 27; mean age: 80;sex: * ethnicity: * Country: USA |
|
| Interventions |
Automated reminding: participants in this condition participated in regular study visits and assessments, but also received automated daily phone calls consisting of a recorded message from the investigator reminding the participant to take their medication. The message consisted of a recording of the first author stating that he was calling the participant to remind them to take their medication, either in Spanish or English Tailored information: participants in this condition at the second study visit received a 20‐min tailored information intervention that consisted of completing a questionnaire about information they wanted to receive about memory disorders and their treatment Participants in the control group received no intervention |
|
| Outcomes | Medication adherence | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | Quote: "Given the small sample size employed in this study, it is possible that we simply did not have adequate statistical power to detect a relation that may have been present." | |
| Notes | This is a comparison between automated reminding and control arms. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were recruited during routine clinical visits at the memory disorders clinic or from contact information available because they had participated in other research studies at the clinic and randomised to one of the three conditions after written informed consent was obtained." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Parikh 2010.
| Methods |
Aims: to compare the no‐show rates of an automated appointment reminder system, clinic staff reminder, or no system at all Study deign: RCT; recruitment: tertiary care (health professional referral) Study duration: 4 months; study type: either; subtype: appointment reminder |
|
| Participants |
Inclusion criteria: patients in ≥ 1 of 10 specialty outpatient practices of the University of Medicine and Dentistry of New Jersey–Robert Wood Johnson Medical School: heart transplantation, rheumatology, pulmonary, nephrology, haematology, general internal medicine, gastroenterology, endocrinology, cardiology, and allergy/infectious disease Sample size: 12,092; mean age: 56 years; sex: men ‐ 43%, women ‐ 57%; ethnicity:* |
|
| Interventions |
Automated appointment reminder system attempted to reach the participant each night for 3 nights before the appointment. As determined by each specialty, a practice‐customised computerised or live voice recording was played after a phone call was answered. The recipient of the call had the option of confirming the appointment or cancelling the appointment. After 3 attempts if an appointment was not confirmed, the participant remained registered for the appointment Staff reminder No reminder |
|
| Outcomes | Non‐attendance rate; satisfaction | |
| Funding | None | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | A sample size (per group) of 1059 was calculated to be sufficient to detect a change from 8% to 5% (638 for 9% to 5%) with a power of 80% (beta) | |
| Notes | This is a comparison between automated system and no reminder. Additional group consists of clinical staff reminder group (STAFF) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were then randomised by a computer‐generated allocation sequence into 1 of the 3 groups" |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation sequence was concealed from the investigators and clinic staff." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Clinic staff were not blinded to the patients they were instructed to call; however, they were unaware to which group (ie, AUTO or NONE) the remaining scheduled patients were assigned." Comment: insufficient information whether blinding was achieved |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers, with similar reasons for missing data across groups. Quote: "Analysis of the no‐shows was performed by intention to treat"" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "Baseline characteristics of the 4 groups were similar" |
Patel 2007.
| Methods |
Aims: to evaluate the ability of interactive voice recognition (IVR) technology to improve statin adherence in a cohort of new start patients Study design: RCT; recruitment: * (organisational referral) Study duration: 6 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: adults continuously enrolled in the health plan for 2 years, and new users of statin therapy (no statin prescription for past 12 months) Sample size: 15,051; mean age: *; sex: * ethnicity:* Country: USA |
|
| Interventions |
Participants in the intervention group received 3 automated phone calls; call 1 provided disease state education, call 2 was a refill reminder, and call 3 addressed the importance of physician follow‐up. The programme provided customised interaction based on participant response, primary vs secondary cardiovascular disease prevention, and refill behaviour Participants in the control group received usual care (control) |
|
| Outcomes | Medication adherence | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "a total of 6833 members were randomised to the intervention group" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Peng 2013.
| Methods |
Aims: to evaluate the effectiveness of a web‐phone intervention in changing smoking behaviour Study design: RCT; recruitment: other ‐ university (military officer referral) Study duration: 9 weeks; study type: management; subtype: smoking |
|
| Participants |
Inclusion criteria: smoking university students Sample size: 116; mean age: 20 years; sex: men ‐ 92%; women ‐ 8%; ethnicity: Asian ‐ 100% Country: Taiwan |
|
| Interventions |
The automated web‐phone intervention (WPI) delivered phone calls that assessed participants' smoking status and based on their responses, delivered motivational and educational recorded messages. The messages covered themes that were most frequently covered in the Taiwan Smokers Helpline counselling sessions based on the participant's stage of change. The question "Have you quit smoking cigarettes?" with the time frame modified for the current week of the 9‐week WPI was asked via a WPI automated phone call. The answers and scoring were 'No, and I do not intend to quit in the next 3 months', 'No, but I intend to quit in the next 3 months', 'No, but I intend to quit in the next 30 days', 'Yes, I quit less than 3 months ago'; and 'Yes, I quit more than 3 months ago'. The control group received the observation call in weeks 1 and 9 along with 2 assessments per week for 3 weeks, 1 assessment for 3 weeks, and 1 assessment for the last 3 weeks |
|
| Outcomes | Stage of change; self‐efficacy; decisional balance | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Similar ATCS components were evaluated Correspondence with the author: "The intervention was based on automated IVR system which was consisted of reminders and questions and options." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After the recruiting procedure, the 116 participants were assigned a unique number and randomly assigned using a systematic numbering system into one of the three groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The double‐blind principle was applied so neither the researcher nor the participants knew which group participants were in" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No description of drop‐outs; imbalance in numbers and reasons for missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Phillips 2015.
| Methods |
Aims: to compare the effectiveness of personalised letters, automated telephone calls, and both on breast cancer and colorectal cancer screening Study design: RCT; recruitment: primary care (organisational referral) Study duration: 36 weeks; study type: prevention; subtype: screening |
|
| Participants |
Inclusion criteria: registered patient at the study clinic; having ≥ 1 visit to the practice in the past 2 years; 50‐74 years old; and past due for mammography or colorectal cancer screening based on medical record documentation Sample size: 685; mean age: 58 years; sex: men ‐ 38%, women ‐ 62%; ethnicity: non‐Hispanic white ‐ 78%, non‐Hispanic black ‐ 13%, other (e.g. Hispanic) ‐ 9% Country: USA |
|
| Interventions |
Automated telephone calls (IVR) in up to 3 waves through a commercial vendor. IVR calls were attempted at varying times (up to 5 times) until a person or an answering machine responded during the first wave (week 1). These calls were repeated during the second wave (week 5). Participants who remained unscreened following a reassessment of screening (week 10) received a third wave (weeks 12 to 14). The automated messages contained content similar to that in the letter, including a number to call if they wanted a faecal immunochemical test to be mailed Personalised letter, signed by the participant's physician, explaining that the participant was past due for cancer screening; the importance of cancer screening; how to schedule the screening; the name and telephone number of the outreach worker available to assist participants with arranging screening; and the availability of free mammography and colorectal cancer screening IVR + personalised letter. Women eligible for both interventions received 1 letter indicating they were past due for both screenings and/or 2 separate automated calls indicating they were past due for mammography and colorectal cancer screening |
|
| Outcomes | Completed mammogram or colorectal cancer screening within 36 weeks of randomisation (documented)(primary) | |
| Funding | American Cancer Society (RSGT‐08‐077‐01‐CPHPS) and the Agency for Healthcare Research and Quality (1 K18 HS022440‐01) | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between the IVR alone arm and arm personalised letter alone arm. Costs: IVR: USD 0.92 per participant; Letter: USD 7.17 per participant/mailing; IVR + letter: USD 3.28/participant for breast cancer screening; and USD 8.09/participant for colorectal cancer screening | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A statistician, who was offsite and blinded to the patients' identities, assigned participants equally to 1 of the 3 intervention groups using a computer‐generated random number algorithm. Randomization was stratified by the type of screening(s) for which the participants were past due (breast cancer, colorectal cancer, or both)" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After confirming eligibility through medical record abstraction, each participant was assigned a unique study identification number" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of study personnel was ensured. Quote: "The office clinicians and study staff were blinded to group assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessment was ensured. Quote: "Research assistants, who were blinded to the intervention, abstracted data (screening date and results available by week 36)." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All participants were analysed in the originally assigned study group based on intention to treat." |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review have been reported |
| Other bias | Low risk | Groups were balanced at baseline with no statistically significant differences |
Piette 2000.
| Methods |
Aims: to assess the impact of automated telephone disease management (ATDM) calls with telephone nurse follow‐up as a strategy for improving outcomes such as mental health, self‐efficacy, satisfaction with care, and health‐related quality of life (HRQL) among low‐income patients with diabetes mellitus Study design: RCT; recruitment: primary care (organisational referral) Study duration: 12 months; study type: management; subtype: diabetes mellitus |
|
| Participants |
Inclusion criteria: adults with a diagnosis of diabetes or an active prescription for a hypoglycaemic agent Sample size: 248; mean age: 55 years; sex: men ‐ 41%, women ‐ 59%; ethnicity: Hispanic ‐ 50%, white ‐ 29%, other – 21% Country: USA |
|
| Interventions |
Automated telephone disease management calls consisted of hierarchically structured messages composed of statements and queries recorded in a human voice. Each message began with an introductory script in which the nature of the call was explained to whoever was the initial call recipient. Biweekly ATDM assessment calls ‐ to check for blood glucose testing in the prior week. Those who had, were asked to indicate the time of their last self‐ monitored blood glucose (SMBG) reading and report the SMBG test result in milligrams per decilitre. Each assessment also included questions about intervention participants' perceptions of their glycaemic control; symptoms of poor control, foot problems, chest pain, and breathing problems; and self‐care issues related to SMBG and foot care. At a later stage, they were offered additional automated self‐care education calls that focused on glucose self‐monitoring, foot care, and medication adherence. Here, participants reported specific barriers to self‐care and received tailored education and advice. Within the medication adherence segment of the calls, participants were asked about their adherence to insulin, oral hypoglycaemic medications, antihypertensive medications, and antilipaemic medications. Compliant received positive feedback and reinforcement while those reporting sub‐optimal adherence were asked about specific barriers and were given advice about overcoming each barrier. The calls also asked whether the participant had a retinal examination in the prior year. At the end of each call, participants were instructed to call the study nurse if they had health problems or questions not covered in the assessment. Participants also had periodic telephone contact with a registered nurse who addressed their ATDM‐reported problems. The nurse was located outside the medical centre and had neither face‐to‐face contact with participants or ready access to their records. Her information base was limited to medical record data abstracted during the enrolment process, ATDM problem reports, and her notes from prior telephone contacts. Each interaction takes between 5‐8 min. All calls were outbound and were placed at times that the participant indicated were convenient. A small number of contacts were initiated by the participants themselves using the study's toll‐free telephone number, which was provided at baseline and during each ATDM call Participants in the control group received usual care. They had no contact with the system for clinical assessments, participant education, appointment reminders, or follow‐up data collection. |
|
| Outcomes | Depression; anxiety; days in bed because of illness; days cut down on activities because of illness (all primary); diabetes‐specific HRQL; self‐efficacy (secondary) | |
| Funding | American Diabetes Association, Department of Veterans Affairs | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | Target sample size for this study was defined to have sufficient statistical power to detect a 1% between‐group difference in glycated haemoglobin (i.e. 9% versus 8%) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was based on a table of randomly permuted numbers" |
| Allocation concealment (selection bias) | Low risk | Quote: "Neither providers, research staff, nor prospective participants had knowledge of group assignment until the patient had consented to participate." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "Outcome analyses were conducted on an intent‐to‐treat basis" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Low risk | Quote: "Baseline characteristics of intervention and usual care patients were similar, although patients in the intervention group were slightly older (P=0.072) and more likely to use insulin (P=0.035). There were no significant differences between the 2 groups in any baseline measures of patient‐centred outcomes." |
Piette 2001.
| Methods |
Aims: to evaluate automated telephone disease management (ATDM) with telephone nurse follow‐up as a strategy for improving diabetes treatment processes and outcomes in Department of Veterans Affairs (VA) clinics Study design: RCT; recruitment: primary care (organisational referral) Study duration: 12 months; study type: management; subtype: diabetes mellitus |
|
| Participants |
Inclusion criteria: adults with a diagnosis of diabetes or an active prescription for a hypoglycaemic agent Sample size: 272; mean age: 61 years; sex: men ‐ 97%, women ‐ 3%; ethnicity: white ‐ 60%, black ‐18%, Hispanic ‐ 12%, other – 10% Country: USA |
|
| Interventions |
Automated telephone calls. The automated calls consisted of hierarchically structured messages composed of statements and queries recorded in a human voice. All calls were outbound (i.e. participants received the calls), and each assessment lasted 5–8 min. During each ATDM assessment, participants used their touch‐tone keypad to report information about their self‐monitored blood glucose (SMBG) readings, other self‐care activities, perceived glycaemic control, symptoms, and use of guideline‐recommended medical care. At the end of each assessment, participants were given the option of listening to health promotion messages Participants in the control group received usual care. |
|
| Outcomes | Glycated haemoglobin; self‐monitoring of blood glucose; self‐monitoring of feet; self‐monitoring of diet; medication use; diabetic symptoms (all); satisfaction with care (all primary); speciality outpatient services use (secondary) | |
| Funding | Health Services Research and Development Service, Mental Health Strategic Health Care Group, Quality Enhancement Research Initiative, American Diabetes Association, Department of Veterans Affairs | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised using sealed envelopes containing group assignments and a sequence generated using a table of random numbers" |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomised using sealed envelopes containing group assignments and a sequence generated using a table of random numbers" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "HbA1c and serum glucose levels were measured at baseline and 12 months in one laboratory by staff who were blinded to patients' experimental condition." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "All analyses of intervention effects were conducted on an intent‐to‐treat basis" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Unclear risk | Quote: "Intervention and control groups had similar characteristics at baseline. However, intervention patients were more likely than control patients to be white and have somewhat more complications." Unclear whether this has introduced bias. |
Piette 2012.
| Methods |
Aims: to evaluate the feasibility of utilising an IVR system to supplement hypertension self‐management for patients in underdeveloped regions in Mexico and Honduras Study design: RCT; recruitment: primary care (organisational referral) Study duration: 6 weeks; study type: management; subtype: hypertension |
|
| Participants |
Inclusion criteria: participants having access and were able to use a telephone, and had a systolic blood pressure suggesting hypertension (i.e. systolic blood pressure ≥ 130 mmHg if diabetic or ≥ 140 mmHg if non‐diabetic) Sample size: 200; mean age: 58 years; sex: men ‐ 33%, women ‐ 67%; ethnicity:* Country: Honduras; Mexico |
|
| Interventions |
Participants in intervention group received a series of weekly automated monitoring and behaviour change calls, as a reminder to check their blood pressure regularly and were asked about: recent systolic values above and below the normal range, medication adherence, and intake of salty foods. Based on this information, participants received additional self‐care information during the call and prompts to seek medical attention or medication refills to address unacceptably high or low blood pressure. Structured email alerts for health workers were generated automatically when participants reported that at least half the time in the prior week they had a systolic blood pressure > 140 mm Hg (non‐diabetic participants), > 130 mm Hg (diabetic participants), or systolic blood pressure < 100 mmHg (all participants). Alerts also were generated if the participant reported rarely or never taking their blood pressure medication or less than a 2‐week supply. Participants also had the option of enrolling with a family member or friend, who received a brief automated telephone update regarding the participant's self‐reported health status each week, including information about the participant's hypertension self‐care and how that caregiver could help the participant self‐manage more effectively. The intervention focused mainly on providing information and self‐management education to participants. At the onset, participants were given an electronic home blood pressure monitor and were instructed how to measure their blood pressure and keep a written record of the results. Whenever possible, an automated phone call was placed during enrolment to familiarise the participant with the call content and how to respond using their touch‐tone phone.The telecommunications infrastructure for the automated calls was maintained on a US server and interfaced with local telephone systems via session initiation protocol (SIP) lines and VoIP technology Participants in the control group received usual care and information |
|
| Outcomes | Blood pressure (primary); health status; depression, satisfaction, medication‐related problems (secondary) | |
| Funding | University of Michigan (UM), OMRON TM | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | ClinicalTrials.gov Identifier: NCT01484782 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After completing informed consent, participants were randomised to the intervention or usual care group based on a computer‐generated series of numbers that ensured balance between experimental groups within each country" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Given the nature of the intervention, it was not possible to blind patients or their clinicians to their experimental assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "Baseline characteristics were similar for intervention and control patients in the analytic sample. However, intervention and control patients differed at baseline in the percentage reporting use of antihypertensive medication. This variable was included as an additional control for confounding in multivariate models." Unclear whether this has introduced bias. |
Pinto 2002.
| Methods |
Aims: to examine the effects of a totally automated physical activity counselling system on self‐reported physical activity among sedentary adults Study design: RCT; recruitment: primary care (mail and telephone) Study duration: 6 months; study type: prevention; subtype: physical activity |
|
| Participants |
Inclusion criteria: > 25 years; sedentary (otherwise healthy individuals) with a sub‐optimal diet; not engaged in regular moderate to vigorous intensity physical activity Sample size: 298; mean age: 46 years; sex: men ‐ 28%, women ‐ 72%; ethnicity: white ‐ 45%; black ‐ 45%; other ‐ 10% Country: USA |
|
| Interventions |
The telephone‐linked communication‐physical activity promoted moderate‐intensity physical activity based on the transtheoretical model of behaviour change and social cognitive theory. At the beginning of each conversation, the system inquired about the user's current level of moderate‐intensity‐physical activity, defined as the number of days during the previous week the person engaged in such activities and the average number of minutes per day. The system also asks users to enter the value of a daily pedometer reading taken the day before the call. For users not yet engaging in any moderate‐intensity physical activity, the system assesses their intention to do so, to determine their motivational readiness. For users who engage in moderate‐intensity‐physical activity, the system determines whether they are at the goal level, as defined by CDC and the American College of Sports Medicine guidelines Participants in the control group (TLC‐Eat) received an automated intervention promoting healthy eating, which was also delivered via telephone |
|
| Outcomes | Energy expenditure; proportion of participants who met recommendations for moderate‐vigorous intensity physical activity; motivational readiness for physical activity (all primary) | |
| Funding | National Heart, Lung and Blood Institute (HL55664) and the Harvard Pilgrim Health Care Foundation | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison of 2 similar ATCS interventions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "At the home visit, we obtained informed consent, randomised participants to one of the study arms, and trained them to use the TLC system." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods. Quote: "Secondary analyses were performed using multiple imputation to account for the potential impact of subject dropout" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were similar across all baseline characteristics |
Reekie 1998.
| Methods |
Aims: to test the effectiveness of different systems of reminding patients about their appointments in order to reduce the rate of failed attendance Study design: RCT; recruitment: primary care (organisational referral) Study duration: 6 weeks; study type: either; subtype: appointment reminder |
|
| Participants |
Inclusion criteria: participants with dental appointments Sample size: 1000; mean age:* ; sex: men ‐ 33%, women ‐ 67%; ethnicity:* Country: UK |
|
| Interventions |
Automated telephone call Automated telephone + postal reminders + manual telephone Manual telephone call Postal reminder No reminder (controls) |
|
| Outcomes | Appointment non‐attendance (primary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | For a 5% difference in response rate between intervention and control, with a significant level of 0.05, 500 participants per group were required | |
| Notes | This is a comparison between the automated telephone call arm and control. All reminder methods provided a net cost saving to the practice during the operation of the study (4‐5 weeks). The savings were: postal, GBP 201; manual telephone, GBP 280; automated telephone, GBP 198; and automated telephone + postal reminders + manual telephone, GBP 296. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Regan 2011.
| Methods |
Aims: to assess the feasibility of replacing a live telephone follow‐up call to recently hospitalised smokers with an automated IVR system and test whether the system could be used to connect patients to postdischarge counselling Study design: RCT; recruitment: secondary care (in‐person at the end of inpatient counselling sessions) Study duration: 12 weeks; study type: management; subtype: smoking |
|
| Participants |
Inclusion criteria: patients were eligible for enrolment if they were identified on admission as having smoked cigarettes in the past year, received bedside counselling from the Massachusetts General Hospital (MGH) Tobacco Treatment Service (TTS) during their hospital stay, were discharged to home, and had not been enrolled at a previous admission during the study period Sample size: 731; mean age: 52 years; sex: men ‐ 56%, women ‐ 44%; ethnicity:* Country: USA |
|
| Interventions |
IVR + call back (CB). Participants received a series of 4 calls from the IVR system, at 3, 7, 14, and 30 days after discharge. The day 7 and day 30 calls were cancelled if the participant had indicated in a previous call that he or she did not want to stop smoking but the day 14 call was always made to assess smoking status outcomes. In addition to the assessment made for the other groups, participants in this group were offered a CB from a counsellor ("Would you like to have your smoking cessation counsellor contact you to help create a quit plan or provide advice about medications?"). To focus counselling efforts on those most likely to benefit from them, CB offers were made only to those who either had not smoked in the past 7 days or wanted to quit within the next 2 weeks. CB was offered within 48 h, with counsellors making 3 attempts to call, and spent about 10 min addressing participant's concerns. Participants who did not respond to the IVR at Day 14 were called by staff. Participants in the control group received a call from the IVR system 14 days after discharge, at which smoking status ("Have you smoked a cigarette, even a puff, in the past 7 days?") and cessation medication use since discharge (nicotine replacement therapy, bupropion, and varenicline) were assessed. The IVR system made up to 8 attempts to reach a participant over 48 h. Participants who were not reached by the IVR system were called by a research assistant who attempted to complete the outcome assessment. |
|
| Outcomes | Self‐reported abstinence rates; self‐reported cessation medication use (primary) | |
| Funding | National Heart Lung and Blood Institute | |
| Declaration of conflict of interest | "Dr. Rigotti has received research grant funding from Pfizer, Sanofi‐Aventis, and Nabi Biopharmaceuticals for the study of investigational and/or marketed smoking cessation products. She is an unpaid consultant for Pfizer and Free & Clear, Inc." | |
| Power calculations for sample size | NA | |
| Notes | This study compares IVR + call back, i.e. ATCS Plus with IVR only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomised by the counsellor immediately after giving consent. Group assignment was stratified by tobacco counsellor in balanced blocks of 4 randomly ordered assignments." |
| Allocation concealment (selection bias) | Low risk | Quote: "Each counsellor carried a set of sealed, sequentially numbered manila envelopes, each containing an individual assignment, along with an information sheet for the patient describing the corresponding IVR call protocol." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "After obtaining consent, the counsellor randomised the patient by opening the next envelope and reviewing the information sheet with the patient. In this way, the counsellors remained blind to the group assignment until after the patient had been counselled and enrolled." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment was conducted by the IVR system. Those who did not respond were contacted by the research assistant. However, it is unclear whether the research assistant was blinded. Quote: "Participants who were not reached by the IVR system were called by a research assistant who attempted to complete the outcome assessment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was small (n=3 in each group). Missing outcome data balanced in numbers across groups. |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review have been reported |
| Other bias | Low risk | Quote: "There were no significant differences between the arms for age, sex, cigarettes/day before admission, intention to remain quit after discharge, or the percent admitted to a cardiac service." |
Reid 2007.
| Methods |
Aims: to determine the feasibility and potential efficacy of an IVR monitoring and follow‐up system to support smoking cessation in smokers hospitalised with coronary heart disease Study design: RCT; recruitment: tertiary care (organisational referral) Study duration: 12 months; study type: management; subtype: smoking |
|
| Participants |
Inclusion criteria: participants were current smokers (≥ 5 cigarettes per day) over the age of 18 years, hospitalised at UOHI (University of Ottawa Heart Institute) for acute coronary syndrome (ACS), elective PCI or diagnostic catheterisation related to coronary heart disease Sample size: 100; mean age: 54 years; sex: men ‐ 68%, women ‐ 32%; ethnicity:* Country: Canada |
|
| Interventions |
The IVR group received automated telephone follow‐up calls 3, 14, and 30 days after discharge inquiring about their smoking status and confidence in remaining smoke‐free. When deemed necessary, they were offered additional counselling. The IVR system posed a series of questions concerning current smoking status, confidence in staying smoke‐free over the time period until the next planned call, and the use of pharmacotherapy, self‐help materials and other forms of cessation support. If participants admitted that they had resumed smoking but wanted to make another quit attempt soon or indicated that their confidence in remaining smoke‐free was low (less than 7 on a 10‐point scale), the IVR system flagged the participant in the software interface in order to ensure that they would be contacted by the nurse‐specialist, who then provided additional assistance consisting of counsellor‐led telephone sessions. Telephone counselling consisted of up to three 20‐min telephone counselling sessions over an 8‐week period. For participants who had returned to smoking but wished to make another quit attempt, the nurse‐specialist provided encouragement, reviewed problems encountered during the initial quit attempt, and helped identify possible solutions. They also assisted participants to set a new quit date, make preparations for quitting, access pharmacotherapy (if necessary), and recruit social support. For participants who were not smoking but whose confidence in remaining smoke‐free was low, the nurse‐specialist provided encouragement and assisted them in identifying tempting situations that were undermining confidence. The nurse‐specialist and the participant then worked to develop strategies to deal with these situations using cue control, healthful alternatives, pharmacotherapy and/or social support. Participants in the control group received usual care. Usual care participants received no further treatment after discharge, but were free to avail themselves of the outpatient smoking cessation programme and any other community resources they chose to access. |
|
| Outcomes | Self‐reported abstinence rate at 52 weeks (primary) | |
| Funding | Canadian Tobacco Control Research Initiative | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | Feasibility study; power calculation was not performed | |
| Notes | All participants received the same UOHI standard in‐hospital treatment, which consisted of: personalised advice to quit smoking; access to nicotine replacement therapy during hospitalisation (if necessary); brief bedside counselling with a nurse‐specialist; a self‐help guide; and the provision of information about the UOHI outpatient smoking cessation programme and other community programmes. This treatment is consistent with current clinical practice guidelines for hospitalised smokers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned to either a usual care (UC) control group or an IVR experimental group. Group assignment was mediated through the Clinical Epidemiology Unit's data centre, using a computer generated randomisation list. The randomisation was made in blocks of six" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information. Quote: "Research staff were unaware of the treatment allocation prior to randomizations" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Loss to follow up was relatively low; it did not differ significantly between groups. There was no significant difference between the UC and IVR groups as to the proportion of participants completing follow‐up measures at 12 weeks (100% versus 96.0%) or 52 weeks (83.7% versus 86.0%). One patient in the UC group died during the follow‐up period and was not included in analysis". Comment: low attrition (n = 1), unlikely to introduce bias |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Comment: groups were similar across all baseline characteristics but education level (participants in the UC group were more likely to have completed some postsecondary education); however, it is unclear whether this has introduced bias |
Reid 2011.
| Methods |
Aims: to determine if continuous abstinence from smoking would be higher 26 and 52 weeks after discharge in smokers who received interactive voice‐response (IVR) mediated telephone follow‐up and triage to nurse counselling compared to those receiving standard care Study design: RCT; recruitment: secondary care (*) Study duration: 12 months; study type: management; subtype: smoking |
|
| Participants |
Inclusion criteria: smokers (≥ 5 cigarettes/day) aged ≥ 18, diagnosed with coronary heart disease, and recently hospitalised at the University of Ottawa Heart Institute (UOHI) Sample size: 440; mean age: * sex: * ethnicity: * Country: Canada |
|
| Interventions |
ATCS Plus: participants received automated telephone calls 3, 14, 30, 60, 90, 120, 150, and 180 days after discharge. The calls posed a series of questions concerning smoking status, confidence in staying smoke‐free, and use of cessation medications. If the participant identified that they had resumed smoking or indicated that their confidence in remaining smoke‐free was low, they were contacted by a nurse‐counsellor who provided additional assistance. Participants in the control group received usual care that included: in‐hospital nurse counselling; nicotine replacement therapy (NRT) during hospitalisation; and a recommendation for ongoing NRT following discharge. |
|
| Outcomes | Self‐reported continuous abstinence, 26 and 52 weeks after hospital discharge (primary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "A total of 440 smokers (5 cigarettes/d) hospitalised with coronary heart disease at the University of Ottawa Heart Institute were randomised to either standard care (SC) or IVR" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Reynolds 2011.
| Methods |
Aims: to test the effectiveness of an automated telephone reminder intervention to improve adherence to medications to lower cholesterol among adults with cardiovascular disease in a large, diverse integrated healthcare system Study design: RCT; recruitment: other ‐ health system (organisational referral) Study duration: 3 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: participants aged 18 years and older identified from a cardiovascular disease case‐identification database. Participants had a prescription for a cholesterol‐lowering agent overdue for refill between 2 weeks and 6 weeks Sample size: 30,610; mean age: * sex: * ethnicity: * Country: USA |
|
| Interventions |
Automated telephone outreach: an automated telephone call instructs participants to order a refill for their overdue prescription by calling the number on their medication bottle or by using an online refill system Participants in the control group received usual care. |
|
| Outcomes | Refill rate at 2 weeks | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Data extraction based on abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "participants were randomly assigned to either an automated telephone outreach or a control group (usual care)." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Rigotti 2014.
| Methods |
Aims: to determine whether an intervention to sustain tobacco treatment after hospital discharge increases smoking cessation rates compared with standard care Study design: RCT; recruitment: secondary care (health professional referral) Study duration: 6 months; study type: management; subtype: smoking |
|
| Participants |
Inclusion criteria: current smokers (smoked ≥1 cigarette/day during the month before admission), received smoking cessation counselling in the hospital, stated that they planned to try to quit smoking after discharge Sample size: 397; mean age: 53 years; sex: men ‐ 48%, women ‐ 52%; ethnicity: white, non‐Hispanic ‐ 81%, Hispanic ‐ 6%, black, non‐Hispanic ‐ 4%, other or unknown ‐ 4%, Native American ‐ 3%, Asian/Pacific Islander ‐ 2.5% Country: USA |
|
| Interventions |
Intervention group received extended care: provision of 3 months of free medication of the participant's choice at discharge (nicotine replacement, bupropion, or varenicline); 5 automated outbound IVR phone calls at 2, 14, 30, 60, and 90 days after discharge; advice and support messages that prompted smokers to stay quit, encouraged proper use and adherence to cessation medication, offered medication refills, and triaged smokers to a return telephone call from a live counsellor for additional support. The automated telephone script encouraged participants to request a callback from a counsellor if they had low confidence in their ability to stay quit, had resumed smoking but still wanted to quit, needed a medication refill, had problems with a medication, or had stopped using any medication. A trained counsellor made the return telephone calls using a standardised protocol. A fax sent to the primary care clinician of each participant informed him/her of the treatment programme Participants in the control group received usual care, which included advice to contact a free telephone quit line and use smoking cessation medication after discharge |
|
| Outcomes | Biochemically confirmed tobacco abstinence at 6 months (primary); self‐reported tobacco abstinence; costs (secondary) | |
| Funding | RC1 HL099668 and K24 HL004440 from the National Institutes of Health/National Heart, Lung, and Blood Institute; the National Cancer Institute, the National Institute on Drug Abuse, and the National Institutes of Health Office of Behavioral and Social Science Research; 1IK2CX000918‐ 01A1 (Dr Japuntich) from the US Department of Veterans Affairs Clinical Sciences Research and Development Service | |
| Declaration of conflict of interest | Dr Rigotti reported being an unpaid consultant for Pfizer Inc and AlereWellbeing Inc regarding smoking cessation; receiving royalties from UpToDate for reviews on smoking cessation; and receiving reimbursement for travel expenses from Pfizer to attend a consultant meeting. Dr Levy reported being a paid consultant to CVS Inc to provide expertise on tobacco policy. Dr Park reported receiving a grant from Pfizer to provide free varenicline for use in a trial funded by the National Cancer Institute. Dr Singer reported being a paid consultant for Pfizer Inc on matters separate from smoking cessation. No other disclosures were reported | |
| Power calculations for sample size | A sample of 330 was planned to provide 83% power to detect a 15% difference (20% vs 35%) in the primary outcome. The sample was increased to 400 without interim analysis to add statistical power | |
| Notes | The incremental per‐participant costs in the intervention group were USD 540 (year 1) and USD 294 (subsequent years) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned (1:1) to sustained care or standard care in permuted blocks of 8, stratified by daily cigarette consumption (<10 vs .10) and admitting service (cardiac vs other)." |
| Allocation concealment (selection bias) | Low risk | Quote: "Treatment assignment was concealed in sequentially numbered sealed envelopes within each stratum. Research staff opened the next envelope corresponding to the participant's randomisation stratum." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The analyses were performed using an intent‐to‐treat approach" |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is available and all of the study's pre‐specified outcomes that are relevant to the review were reported in the pre‐specified way. |
| Other bias | Low risk | Comment: groups were similar across all baseline characteristics. |
Rose 2015.
| Methods |
Aims: to test the efficacy of a novel, fully automated continuing care programme, Alcohol Therapeutic IVR Study design: RCT; recruitment: primary care and community (clinic referrals, public service announcements, and local advertising online and in print) Study duration: 12 months; study type: management; subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: age 18 or older, diagnosis of current or lifetime DSM‐IV Alcohol Dependence, past 90 days' report of ≥ 1 drink and ≥ 1 symptom of Alcohol Abuse or Alcohol Dependence, and attendance at ≥ 8 outpatient CBT sessions Sample size: 158; mean age: 49 years; sex: men ‐ 53%, women ‐ 47%; ethnicity: * Country: USA |
|
| Interventions |
Alcohol Therapeutic IVR for 4 months. Participants were encouraged to call daily, but were not paid for calling. In the first month, participants who missed 2 consecutive Alcohol Therapeutic IVR calls received a single reminder phone call from an RA, who offered assistance with any technical difficulties and/or provided suggestions for remembering to call, as appropriate. In months 2–4, a reminder call was made if a participant missed 3 consecutive Alcohol Therapeutic IVR calls. There were 6 primary components to the Alcohol Therapeutic IVR: daily journal, targeted daily feedback, CBT skills encouragement, coping skills review, coping skills practice, and monthly personalised therapist message. Daily journal (compulsory) consisted of: 16 items that assessed mood states, craving, confidence in abstaining, number of risk situations, time with non‐users, sobriety support, substance free recreation, coping management, and use of coping skills. Participants were instructed to respond to items based on the previous calendar day. If a participant indicated alcohol or drug use, a follow‐up question for the current day's use was asked. If a participant reported current use and missed a previous day's call, they were asked to report on alcohol and drug use for that missed day and any previous missed days up to 1 week prior. If a participant's daily journal indicated alcohol or drug use, high craving, low confidence, and/or low coping levels, that report was 'red flagged' as indicating high risk. These participants received a feedback message Participants in the control group received usual care. |
|
| Outcomes | Alcohol consumption (number of drinks per drinking day) (primary); participant perceptions of the system (secondary) | |
| Funding | National Institute on Alcohol Abuse and Alcoholism | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | The study was estimated to have power (1‐beta) = 0.80 using alpha = 0.05 to detect a moderate effect size (Cohen's d = 0.45) for primary analyses of all randomised participants. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "At the conclusion of CBT, participants returned to the research office for an assessment, and were randomised in a 1:1 allocation to either ATIVR or usual care. Randomization was stratified based on whether subjects had legal issues pending relating to their alcohol use. Within each stratum, a blocked randomisation was used to insure that an equal number of subjects were randomised to each of the two treatment conditions within each sequential block of 10 participants." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcomes were balanced in numbers across groups, but reasons for missing data were not provided. Quote: "There was no differential follow‐up rate across groups". |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Comment: groups were similar across all baseline characteristics but drinking days (the IVR group had nearly significantly more drinking days per week than control group at baseline (P = 0.08)); however, it is unclear whether this imbalance has introduced bias. |
Rubin 2012.
| Methods |
Aims: to provide an initial test of a totally automated, multi‐session treatment for problem drinkers in the community using a sophisticated IVR system with speech recognition Study design: RCT; recruitment: other (adverts in newspapers and on the Internet) Study duration: 6months; study type: management; subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: problem drinkers Sample size: 47; mean age: 57 years; sex: men ‐ 60%, women ‐ 40%; ethnicity: Caucasian ‐ 83%, African‐American ‐ 13% Country: USA |
|
| Interventions |
The intervention group: Miller and Munoz's self‐help book, Controlling Your Drinking: Tools to Make Moderation Work for You (2005) was adapted into a computer‐controlled IVR system that incorporated Miller and Munoz's strategies while enhancing the motivational aspects of the programme; participants could receive up to 26 calls over 13 weeks Participants in the control group received an informational pamphlet in the mail. |
|
| Outcomes | Number of heavy drinking days per month; percent days abstinent per month; drinks per drinking day | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Information from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "There were no significant differences between groups at baseline on demographics or drinking variables." |
Schillinger 2009.
| Methods |
Aims: to examine the effectiveness of 2 self management strategies (SMS) across outcomes corresponding to the chronic care model Study design: RCT; recruitment: primary care (organisational referral) Study duration: 12 months; study type: management; subtype: diabetes |
|
| Participants |
Inclusion criteria: adult with type 2 diabetes having suboptimal glycaemic control; a glycated haemoglobin value of 8% in the previous 12 months; ≥ 1 primary care visit in the previous 12 months; English‐, Spanish‐, or Cantonese‐speaking; did not have limited vision or were hearing‐impaired; and no diagnoses of psychotic illness or end‐stage renal disease Sample size: 339; mean age: 55 years; sex: men ‐ 41%, women ‐ 59%; ethnicity: white/Latino ‐ 47%, Asian ‐ 23%, African American ‐ 21%, white/non‐Latino ‐ 8%, other/unknown – 1% Country: USA |
|
| Interventions |
The IDEALL Automated Telephone Disease Management (ATDM): the ATDM system provides weekly calls with rotating queries in participants' native language for 9 months regarding: self‐care (e.g. symptoms, medication adherence, diet, physical activity, self‐monitoring of blood glucose, smoking), psychosocial issues (e.g. coping, depressive symptoms), referrals for preventive services (e.g. ophthalmologist). Each call took 6‐12 min to complete. Participants selected call times at enrolment and could alter preferred times or call the system toll free. Participants respond via touch‐tone commands. Depending on the response to an individual item, participants also receive automated health education messages in the form of narratives. Participants answering "out of range" on ≥ 1 item, based on predetermined clinical thresholds, receive a call back from a language concordant nurse care manager within 24 to 72 h. The care manager helps participants problem‐solve around the issue identified in the report or any other concerns, with a focus on collaborative goal setting with action plans. Support, education, and patient activation through monthly group medical visits with physician and health educator Usual care |
|
| Outcomes | Self‐management behaviours (primary consisting of the 4 domains/sub‐scales: self‐monitoring of blood glucose and self‐monitoring of diabetic foot, diet and exercise); and behavioural, functional, and metabolic outcomes (secondary) | |
| Funding | The Commonwealth Fund, Agency for Healthcare Research and Quality, the California Endowment, the San Francisco Department of Public Health, the California Healthcare Foundation, National Institutes of Health | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | "We determined that 339 subjects would result in 100 subjects in each arm at the end of the study (n= 300), providing 80% power to detect a difference in diabetes self‐care of 0.49 days/week, using 2 tailed tests, of 0.05, and Bonferroni correction for three group comparisons. However, the study was not adequately powered to provide definitive answers regarding relative impacts across subgroups, such as those with limited English proficiency and limited literacy." | |
| Notes | This is a comparison between ATDM arm and UC. The annual cost of the ATSM intervention per QALY gained, relative to usual care, was USD 65,167 for start‐up and ongoing implementation costs combined, and USD 32,333 for ongoing implementation costs alone. In sensitivity analyses, costs per QALY ranged from USD 29,402 to USD 72,407. The per‐participant cost to achieve a 10% increase in the proportion of intervention participants meeting American Diabetes Association exercise guidelines was estimated to be USD 558 when all costs were considered and USD 277 when only ongoing costs were considered. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were allocated using stratified (on languages) blocked randomisation." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Because the study was not blinded and because the usual care group did not receive any additional SMS intervention, systematic inaccuracies in patient‐reported outcomes may have occurred due to recall bias or social desirability." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were conducted on an intent‐to‐treat basis." Comment: missing data have been imputed using appropriate methods. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "There were no statistically significant differences in baseline characteristics across arms" |
Sherrard 2009.
| Methods |
Aims: to determine if IVR can improve medication adherence and reduce adverse events as patients transition from hospital to home among postoperative cardiac surgical patients Study design: RCT; recruitment: secondary care (organisational referral) Study duration: 6 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: adults who were discharged from the UOHI were considered for inclusion if they underwent coronary artery bypass grafts and/or valvular surgery, had telephone service to their home, and spoke either English or French Sample size: 331; mean age: 63 years; sex: * ethnicity: * Country: Canada |
|
| Interventions |
Automated telephone calls at a predetermined time for 6 months, with calls made at 1, 2, 3, 4, 6, 8, 10, 12, 16, 20 and 24 weeks after discharge. The IVR system recorded participants' voiced responses (yes or no) into a central database. Used an algorithm of 11 questions addressing medication adherence, reporting of adverse events, providing information on common medications, and offering general medication safety tips. The intent of the IVR algorithm was to provide early identification of issues permitting timely intervention, provide a mechanism for tracking medication adherence, and provide medication information at the time deemed most valuable by the participant at his or her request and to provide longer term follow‐up as the participant transitioned from hospital to home. If the participant responded "yes" to medicine adherence, the system provided a short description of the medication, including trade and generic names, desired effects and possible adverse effects. Participants could use the callback option from a nurse if they wish to discuss any concerns. Participants in the control group received usual care. |
|
| Outcomes | Medication adherence and adverse events (composite primary outcome); emergency room visits and hospitalisations; medication adherence; patient satisfaction | |
| Funding | Canadian Patient Safety Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "A sample size of 166 patients per group was sufficient to detect the important difference of 16% in the primary outcome with an alpha‐value of 0.05 and power of 80% using the Fisher exact tests. A dropout rate of 10% was anticipated over the six‐month follow‐up period and, therefore, a sample size of 368 patients (184 per group) was needed to assess the important difference of 16% in the primary outcome." | |
| Notes | ClinicalTrials.gov Identifier: NCT01151800. All data were stored in the IVR system using a study identifier. The data were password protected and the drive was backed up daily for protection against data loss | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "Randomization occurred once consent to participate was obtained." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation to the treatment group was blinded by using a sealed envelope identified by study number and containing the random allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessment was not blinded. Quote: "The six month surveys were conducted by telephone interview by the research nurse coordinator who had intervened with the patients during the study" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Statistical analysis was conducted on an intention‐to‐treat basis." Comment: missing data have been imputed using appropriate methods. ITT analysis was used to include all participants who received the intervention or usual care in the analysis |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol was available; and all of the study's pre‐specified outcomes that are relevant to the review have been reported |
| Other bias | Unclear risk | Quote: "There were no statistical differences in baseline characteristics between the 2 groups other than the variable of employment status, which showed a clinically insignificant yet statistically significant difference." Comment: unclear whether this has introduced bias. |
Shet 2014.
| Methods |
Aims: to assess whether customised mobile phone reminders would improve adherence to therapy and thus decrease virological failure among HIV infected patients starting antiretroviral treatment Study design: RCT; recruitment: primary care (advert in clinic) Study duration: 24 months; study type: management; subtype: HIV |
|
| Participants |
Inclusion criteria: HIV infected individuals with adequate documentation of their HIV positive status, aged 18‐60 years, ART naive, and meeting the criteria for start of first‐line ART as per the 2007 Indian national guidelines Sample size: 631; mean age: inestimable; sex: men ‐ 57%, women ‐ 43%; ethnicity: Asian ‐100% Country: India |
|
| Interventions |
Multimodal intervention was a customised motivational voice call that went out once a week at a time selected by each participant. The participant also chose the sex and language of the pre‐recorded voice call. This automated call began with a greeting and the hope that the participant was feeling well, followed by an inquiry whether medications were taken as prescribed. The message was considered interactive or bidirectional, since it required the participant to respond to a question about the previous day's pill doses, by pressing '1' for yes or '2' for no. If the participant failed to respond to the call, a maximum of 3 more calls were made over the ensuing 24 h until a response was obtained. The second aspect of the intervention included a weekly non‐interactive neutral pictorial message sent out as a reminder 4 days after the automated call. Participants in this group also received usual care. Participants in the control group received usual care, which included up to 3 counselling sessions prior to initiation of ART, routine clinical and laboratory tests at baseline, and follow‐up assessments every 6 months. First line ART regimens included those based on zidovudine, stavudine, or tenofovir, along with lamivudine and either nevirapine or efavirenz, and were dispensed free of cost as generic fixed‐dose combination pills every 1‐3 months. |
|
| Outcomes | Time to virological failure (primary); ART adherence measured by pill count; death rate; attrition rate (secondary) | |
| Funding | European Union, Framework Program 7 (No 222946) | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | A total sample of 532 participants (266 in each arm) would provide 90% power to detect such a risk difference in a 2‐sided log‐rank test with significance level of 0.05. Expecting an attrition rate of 10%, the trial was planned to have a minimum of 600 participants | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was performed stratified for sex, in permuted blocks of four or six." |
| Allocation concealment (selection bias) | Low risk | Quote: "Sequentially numbered opaque sealed envelopes were used as a method of allocation concealment." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Patients and the randomisation team were aware of the intervention assignment; while research staff assessing patients, laboratory staff, statisticians, and authors were blind to the allocation." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Patients and the randomisation team were aware of the intervention assignment; while research staff assessing patients, laboratory staff, statisticians, and authors were blind to the allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods. Quote: "Trial analysis was performed using an intention‐to‐treat principle that included all originally randomised patients" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review have been reported |
| Other bias | Low risk | Comment: groups were similar across all baseline characteristics |
Siegel 1992.
| Methods |
Aims: to evaluate the efficacy of automated telephone needs assessment coupled with social worker follow‐up in outpatients with advanced cancer who were receiving chemotherapy Study design: quasi‐RCT; recruitment: secondary care (in‐person at chemotherapy clinics or by letter with a follow‐up phone call) Study duration: 24 months; study type: management; subtype: cancer |
|
| Participants |
Inclusion criteria: had primary tumours of the breast, colon/rectum, or lung; had recurrent or metastatic disease or non‐resectable tumours; were receiving non‐adjuvant outpatient chemotherapy; were 21 years of age or older; and spoke English with sufficient fluency to validly respond to the automated surveys and the research interview Sample size: 239; mean age: 58 years; sex: men ‐ 50%, women ‐ 50%; ethnicity: white ‐ 89%, black‐ 6%, Hispanic ‐ 4%, other 1% Country: USA |
|
| Interventions |
Intervention group received 3 automated telephone surveys (surveys 1, 2, and 3), scheduled approximately 6 weeks apart. The system was configured to: call participants at times they designated as convenient; conduct needs assessment surveys with them in a high‐quality, natural sounding, digitally stored voice; reliably interpret, confirm, and register their verbal answers to 12 questions; and identify participants who reported unmet need(s) so that they could receive prompt follow‐up by a social worker. Outcome was to be assessed in a final comprehensive needs assessment through an interview held with a social worker 6 weeks after the participant's completion of the automated surveys + the approximately hour‐long research interview by an experienced clinician. Participants in the control group completed the research interview for the comprehensive needs assessment within 2 weeks + the approximately hour‐long research interview by the experienced clinician. |
|
| Outcomes | The prevalence of unmet needs | |
| Funding | National Cancer Institute (CA 41012) | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "To simplify field operations, blocks of time were randomly assigned as periods of accrual for either the experimental or control group; each eligible patient was assigned to the experimental or control group based on the block of time during which the patient was identified." Comment: non‐random assignment |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "In the experimental group, the interviewer was never the same social worker who worked with the patient during the intervention. This was done to avoid any bias that might be associated with interviewer's knowledge of the patient's intervention history" Comment: insufficient information to judge whether assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate. Quote: "Of the 266 patients accrued into the experimental group, 109 (41%) completed both the series of automated surveys and the final assessment interview within the study period, and 157 (59%) did not". |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "The control and experimental groups did not differ significantly with respect to almost all sociodemographic characteristics. However, patients in the experimental group were somewhat older than patients in the control group (mean age 60 versus 57 years)." Comment: groups were similar across all baseline characteristics. It is unlikely that the small age difference has introduced bias. |
Sikorskii 2007.
| Methods |
Aims: to test 2 multimodal interventions for multiple symptoms experienced by patients with multiple cancer sites Study design: RCT; recruitment: primary care (organisational referral) Study duration: 10 weeks; study type: management; subtype: cancer |
|
| Participants |
Inclusion criteria: aged 21 years and above, having a diagnosis of a solid tumour cancer or non‐Hodgkin's lymphoma, undergoing a course of chemotherapy, speak and read English, and having a touch‐tone telephone Sample size: 437; mean age: 57 years; sex: men ‐ 26%, women ‐ 74%; ethnicity:* Country: USA |
|
| Interventions |
Automated telephone symptom management (ATSM): prerecorded pleasant female voice queried participants about severity of 17 symptoms: fatigue, pain, dyspnoea, insomnia, distress, nausea, fever, difficulty remembering, lack of appetite, dry mouth, vomiting, numbness and tingling, diarrhoea, cough, constipation, weakness, and alopecia. If they report severity in ≥ 4 symptoms, then the call directed them to the relevant part in the symptom management guide (SMG) for strategies to manage those symptoms. Participants advised to call the oncology office if they report severity of ≥ 7 symptoms or if there was no improvement. On subsequent calls, in participants with severity of ≥ 4 symptoms in the previous calls, ATSM enquired if the participants tried the strategies suggested in the SMG and whether it helped in lowering the severity. Numerical prompts were used so participants could respond using their telephone keypad. When all symptoms above threshold at the previous contact were evaluated, the system then reviewed the current severity of all symptoms. Calls by specially trained nurses |
|
| Outcomes | Symptom severity | |
| Funding | National Cancer Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "The trial was powered to detect an effect size of 0.37 for group differences on symptom severity at 10 weeks." | |
| Notes | Both total fixed and variable costs were greater for the nurse arm; total costs per participant were USD 69 and USD 167 for the ATSM and nurse arm respectively. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "[Participants] were randomized into either the NASM or the ATSM using a computer minimisation program that balanced the arms with respect to recruitment location and site of cancer". |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers across groups. ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "A total of 13 patients (10 in the ATSM and 3 in the NASM) did not complete any of the intervention contacts, but had 10‐week interviews. These patients were included in the intention‐to‐treat analysis of interview data" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "Most measures including symptom severity were equivalent at baseline." Comment: groups were similar across all baseline characteristics |
Simon 2010a.
| Methods |
Aims: to test the effectiveness of automated telephone outreach with speech recognition to improve rates of screening for colorectal cancer. The hypothesis is that the intervention improves rates of screening overall and specifically rates of colonoscopy. Study design: RCT; recruitment: primary care (organisational referral) Study duration: 12 months; study type: prevention; subtype: screening |
|
| Participants |
Inclusion criteria: aged 50‐64 at baseline and continuous enrolment in health plan Sample size: 20,936; mean age: 57 years; sex: men ‐ 47%, women ‐ 53%; ethnicity: white ‐ 86%, other – 9%, black ‐ 5% Country: USA |
|
| Interventions |
Automated telephone outreach (ATO) calls followed a script and branching algorithm that was informed by a theoretical framework, with the aim to educate the participants about the risk of colorectal cancer and about the importance and methods of screening, and to encourage them to contact their primary care providers to arrange for colorectal cancer screening. The calls used speech recognition technology and delivered the message with prerecorded human conversation either to the participant directly, or to another member who would then convey it to the intended participant. When unreachable, the system leaves a message and asks participants to call back. Participants in the control group received usual care |
|
| Outcomes | Colorectal cancer screening including faecal occult blood testing, double‐contrast barium enema, flexible sigmoidoscopy, or colonoscopy within 12 months following the intervention (primary); screening by colonoscopy during the 12‐month period following the intervention (secondary) | |
| Funding | Harvard Pilgrim Health Care Foundation | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | The ATO calls verified participants identify and only after securing their permission did it proceed with the interaction regarding colorectal cancer screening. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We randomly allocated to intervention and usual care arms, using a computerized random‐number generator" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The study was not blinded" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers, with similar reasons for missing data across groups. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Groups were similar at baseline. Quote: "There were no baseline differences between the two study groups on any of the measured variables." |
Simon 2010b.
| Methods |
Aims: to assess the effects of automated telephone outreach with speech recognition (ATO‐SR) on rates of testing for retinopathy, glycaemia, hyperlipidaemia, and nephropathy in a diverse population of privately insured patients with diabetes. Study design: RCT; recruitment: primary care (organisational referral) Study duration:12 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: individuals with no insurance claim for a dilated eye examination in the prior year and no claim for ≥ 1 of the following tests: glycated haemoglobin, low‐density lipoproteins, or microalbumin. Sample size: 1200; mean age: 51 years; sex: men ‐ 62%, women ‐ 38%; ethnicity: other – 95%, black ‐ 5% Country: USA |
|
| Interventions |
ATO‐SR: the computerised system placed 3 calls to the participants' home telephone numbers, encouraging the participants to fulfil recommended testing if it had not been performed in the preceding year. The system offered a live telephone call back to assist in scheduling tests and also offered to send participants the following items: a voucher that would allow the provider to waive the co‐payment for a dilated eye examination; an educational nutrition video; a cookbook; or a pill box. For each of the 3 intervention calls, the automated telephone system made up to 6 attempts to reach the participant, leaving up to 2 messages requesting a call back. The system used speech recognition to respond to participants with segments of recorded text spoken with a human voice Participants in the control group received usual care (no intervention). |
|
| Outcomes | Retinopathy examination (primary); tests for glycaemia, hyperlipidaemia, and nephropathy (secondary) | |
| Funding | American Diabetes Association, Agency for Healthcare Research and Quality, National Institute of Diabetes and Digestive and Kidney Diseases | |
| Declaration of conflict of interest | "No potential conflicts of interest relevant to this article were reported" | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis was used to include all participants who received the intervention or usual care in the analysis. Quote: "The main analyses included all subjects in the groups to which they were randomised" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "Compared with the usual care group, the intervention group was younger (50 vs. 52 years, P 0.02) and had a greater proportion of men (64 vs.41%, P 0.04); the groups were comparable on other socio‐demographic measures and clinical indicators" Comment: groups were similar across all baseline characteristics but age and sex; however, it is unclear whether this imbalance has introduced bias. |
Simpson 2005.
| Methods |
Aims: to evaluate compliance with 2 IVR monitoring protocols, subjective experiences with monitoring, and change in symptoms associated with monitoring (i.e. measurement reactivity). Study design: RCT; recruitment: primary care (advert in clinic) Study duration: 4 weeks; study type: management; subtype: alcohol consumption |
|
| Participants |
Inclusion criteria: all participants who had consumed alcohol in the prior 28 days, met diagnostic criteria for an alcohol use disorder (APA, 1994), and indicated an intention to abstain from alcohol and other drug use over the coming month Sample size: 98; mean age: 46 years; sex: men ‐ 91%, women ‐ 9%; ethnicity: non‐Hispanic white ‐ 45%, African American ‐ 40%, Native American ‐ 7%, other ‐ 6%, Hispanic ‐ 2% Country: USA |
|
| Interventions |
Daily IVR. Participants called a pre‐recorded IVR system daily using a toll‐free telephone number. A monitoring protocol to assess participant's alcohol substance use behaviour was used and they responded using an 8‐point response option (0–7 on the telephone key pad) in order to use 9 as a skip option and to reduce confusion for participants (i.e. omitting 8 as an option and not requiring an extra key stroke after each entry to signal the end of an entry). IVR system automatically tracked compliance with the monitoring protocol. When participants failed to call the system as scheduled the study coordinator attempted to contact participants within 2 working days in order to reconstruct the data from missed calls verbally and to resolve any difficulties. If participants indicated clinical deterioration during follow‐up calls, they were encouraged by the study coordinator to contact their clinical provider and were given the appropriate phone numbers to facilitate this. Participants in the IVR monitoring conditions received instruction on how to call into the IVR system and completed a practice call to familiarise themselves with the procedures. Participants received a "cheat sheet" that included the toll free number, the study coordinator's telephone number, their study ID number, and a list of the monitoring questions and response options. They also received incentives for each call that they made. At the end of each call, the IVR system informed the participants of the amount of money accumulated in their accounts. They could use the # key to repeat a question and the * key to back up to the previous question Weekly IVR calls No calls (controls) |
|
| Outcomes | Drinking habits; alcohol craving; PTSD symptoms (all primary) | |
| Funding | University of Washington Alcohol and Drug Abuse Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between daily IVR versus no call | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "At the end of the baseline assessment participants were randomly assigned to one of three conditions" Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed using appropriate methods. Quote: "Missing data on multi‐item scales were handled in the following ways: mean scores for the PACS were imputed for the two cases where one item was missing, and scores for the PCL‐C were generated with no mean imputation when ≥ 16 of the 17 items were completed; scores were not produced for three participants who were missing more than 1 item. No other missing data imputation techniques were used." |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Low risk | Comment: groups were similar across all baseline characteristics |
Solomon 2007.
| Methods |
Aims: to test the effectiveness of an intervention to improve care in patients at‐risk of osteoporosis Study design: RCT; recruitment: primary care (organisational referral) Study duration: 10 months; study type: prevention; subtype: screening |
|
| Participants |
Inclusion criteria: women 65 years of age and over; women and men 45 and older with a prior fracture of the hip, spine, forearm, or humerus; and women and men 45 and older who had used oral glucocorticoids for ≥ 90 days Sample size: 1973 participants; mean age: 69 years; sex: men ‐ 8%, women ‐ 92%; ethnicity: * Country: USA |
|
| Interventions |
Participants in the multimodal intervention group received education + an introductory letter from Horizon Blue Cross Blue Shield of New Jersey and then an automated telephone call from the insurer inviting them to undergo bone mineral density testing. This call employed IVR technology that has been used for other screening tests. Such automated calling provides tailored education through a branching logic algorithm. For example, people who had never had a bone mineral density test but expressed an interest were offered specific encouragement, "It's great that you plan on having a bone density test; the best way to tell if a person is at risk for osteoporosis is to have a bone density test. The test only takes about 5 minutes, you don't have to take off your clothes, and it's painless." At the conclusion of the educational call, participants were able to transfer directly to a centralised radiology service to schedule a bone mineral density test. Participants in the control group received no intervention. |
|
| Outcomes | Either undergoing a bone mineral density testing or filling a prescription for a bone active medication | |
| Funding | Merck and Co., Inc.; NIH (AR48616, AG027066), the Arthritis Foundation, and the Engalitcheff Arthritis Outcomes Initiative | |
| Declaration of conflict of interest | Drs Weiss and Chen are both employees of Merck and Co., Inc | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "We conducted a randomised controlled trial among primary care physicians and their at‐risk patients" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: missing data have been imputed using appropriate methods. An ITT analysis was used to include all participants who received the intervention or no intervention in the analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Between‐group differences at baseline were adjusted for as covariates. There is insufficient evidence that these differences have introduced bias. |
Sparrow 2010.
| Methods |
Aims: to investigate the effectiveness of an automated telemedicine intervention to improve adherence to continuous positive airway pressure (CPAP) Study design: RCT; recruitment: primary care (home visit) Study duration:12 months; study type: management; subtype: obstructive sleep apnoea syndrome (OSAS) |
|
| Participants |
Inclusion criteria: aged 18 to 80 years with a physician diagnosis of OSAS and with polysomnography demonstrating an apnoea‐hypopnoea index (AHI) >10 Sample size: 250; mean age: 55 years; sex: men ‐ 82%, women ‐ 18%; ethnicity: * Country: USA |
|
| Interventions |
Telephone‐linked communications for CPAP (TLC‐CPAP): content includes assessment of the participant's perceptions about and experiences with OSAS and CPAP therapy and the participant's reported CPAP use (h per night and nights per week) during the week preceding each call; assessment of the participant's goals with regard to OSAS therapy; and feedback and counselling to enhance motivation to use CPAP and address barriers and poor self‐efficacy. A side effect management module addressing mucocutaneous side effects, air leaks and mask discomfort was developed and incorporated in the dialogues as appropriate. Participants in the control group received attention placebo: general health education via a TLC system. This system provides general information about a variety of health topics via telephone calls delivered on the same schedule as the TLC‐CPAP calls made by the intervention group. At each call, participants selected a topic from a list of 61 content areas that included common symptoms, medical conditions and preventive medicine topics |
|
| Outcomes | CPAP use (primary); sleep symptoms checklist; functional outcomes of sleep questionnaire; depression (secondary) | |
| Funding | Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service | |
| Declaration of conflict of interest | MA is a paid employee of Philips/Respironics Inc and is a stockholder of Philips stock | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was stratified by sex, age and AHI using a randomised block design to ensure balance of these factors in the treatment arms." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study personnel was blinded. Quote: "All data were collected by research assistants blind to group assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data balanced in numbers across groups; however, reasons for missing data are not provided. Quote: "CPAP adherence data were available from either the 6‐ or 12‐month follow‐up visit in 93.6% of subjects (figure 1), who were therefore included in the primary analysis" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Low risk | Quote: "The baseline characteristics of the intervention and control groups were similar." |
Sparrow 2011.
| Methods |
Aims: to investigate the effectiveness of an automated telemedicine intervention that provides real‐time guidance and monitoring of resistance training in the home Study design: RCT; recruitment: primary care (*) Study duration: 12 months; study type: prevention; subtype: physical activity |
|
| Participants |
Inclusion criteria: no angina pectoris (unless symptomatically resolved post‐revascularisation), no history of myocardial infarction within 6 months or remote (> 6 months) myocardial infarction with current myocardial ischaemia on exercise stress test, no history of ventricular dysrhythmia requiring therapy, baseline systolic blood pressure smaller than 165 mmHg and/or diastolic blood pressure smaller than 100 mmHg, and not currently participating in a regular exercise programme less than once a week for 20 min per session Sample size: 103; mean age: 71 years; sex: men ‐ 69 %; women ‐ 31 %; ethnicity: * Country: USA |
|
| Interventions |
Telephone‐Linked Computer‐based Long‐term Interactive Fitness Trainer (TLC‐LIFT) system called participants, with a target exercise schedule of 3 days per week. At the initiation visit, users indicated what their preferred time to exercise was, and this was the time that TLC‐LIFT was scheduled to call. The TLC‐LIFT system is security enabled, so at the beginning of a call, each participant was asked to enter a personal password (PIN) to ensure security and confidentiality. Following the identification confirmation, TLC‐LIFT asked the participant if he/she was ready to perform his/her exercises. If the participant was not ready, he/she was asked to call a toll‐free number when ready, which informed TLC‐LIFT to call the person shortly thereafter to begin the exercise session. If the person failed to call back within 4 h of TLC's call, calls were repeated periodically during a time period previously set by the user. After a 24‐hour period had elapsed without the user completing a scheduled exercise session, the TLC system administrator was notified automatically and informed a staff member so that he or she could contact the user. Participants in the control group received attention: general health education via a TLC system at weekly intervals. This system provides general information about a variety of health topics via telephone calls. At each call, participants selected a topic from a list of content areas that included common symptoms, medical conditions, and preventive medicine topics. The health information dialogues were adapted from Harvard Health Letter articles (http://www.health.harvard.edu). The dialogs were developed to allow users to identify subtopics about which they wanted more information, and to skip others, and avoided long stretches of uninterrupted talking by the system |
|
| Outcomes | Muscle strength; balance; walk distance; mood (all primary) | |
| Funding | Rehabilitation Research and Development Service of the Department of Veterans Affairs, the Boston Claude D. Pepper Older Americans Independence Centre, and the US Department of Agriculture | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | Study sample of 100 evaluable participants, approximately equally divided between intervention and control groups, provided 99.9% power to detect the smaller of these effects at a (2) = 0.05, and 80% power to detect a more conservative effect of 0.57 SD | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After eligible participants gave written informed consent, we collected baseline study data and then randomised them to one of two groups using a computer‐based algorithm (randomize function in Visual Basic) to perform random assignment without blocking or stratification." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Data for analyses were collected during four clinic‐based examinations (baseline, 3, 6, and 12 months), conducted by research assistants blind to group assignment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were performed by intention to treat, using all outcome data collected regardless of adherence to assigned treatment" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "The intervention and control groups were similar on baseline characteristics except for 6‐minute walk (p=.02; Table 14)." Comment: groups were similar across all baseline characteristics but 6‐minute walk; however, it is unclear whether this imbalance has introduced bias |
Spoelstra 2013.
| Methods |
Aims: to examine Automated Voice Response (AVR) to manage symptoms and adherence to oral agents Study design: RCT; recruitment: tertiary care (*) Study duration: 10 weeks; study type: management; subtype: cancer |
|
| Participants |
Inclusion criteria: 21 years or older, having a solid tumour cancer; diagnosis, and being on non‐hormonal oral agents; understood English; having a touch‐tone phone and no hearing deficits that interfered with using a telephone; having no cognitive deficits; willing to complete phone contacts; and not being diagnosed with an emotional or psychological disorder Sample size: 119; mean age: 60 years; sex: men ‐ 31 %; women ‐ 69 %; ethnicity: white ‐ 76%, black ‐ 7%, other ‐ 17 % Country: USA |
|
| Interventions |
AVR system + symptom management toolkit (SMT) + nurse strategies to manage unresolved symptoms and improve adherence. In addition to the AVR calls, participants with ≥ 1 symptoms rated at a 4 or greater or non‐adherence defined as less than 80% during the immediate past 7‐day period received a brief telephone call from the nurse to deliver strategies to assist participants to manage symptoms and/or improve their adherence. Participants were called weekly until symptom severity fell below 4 or until adherent SMT + AVR phone system alone. Participants in this arm received calls from the AVR system; symptoms were assessed, and those reporting severity at a 4 or higher on a 0‐10 scale for any symptom were referred to the SMT for self‐management of symptoms. Adherence to oral agents was identified via participant report (no nurse was involved) AVR + SMT + nurse strategies to improve adherence alone. In group 3, in addition to the AVR calls, participants received brief calls from a nurse when the adherence rate was less than 100% to improve their adherence. Participants were called weekly until adherent. |
|
| Outcomes | Adherence to medications; symptom severity (both primary) | |
| Funding | GlaxoSmithKline; Mary Margaret Walther Behavioural Oncology Group and the State of Michigan Nurse Corp | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | Study was powered to detect a medium effect size of 0.50 for pairwise differences between groups on symptom severity and adherence | |
| Notes | This is a comparison between AVR + SMT + nurse strategies to manage unresolved symptoms and improve adherence and SMT + AVR alone. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "After completion of the baseline interview, patients were randomised into the groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates with reasons were provided; attrition was balanced across the groups. |
| Selective reporting (reporting bias) | High risk | No outcomes reported on depression scores at the study's completion |
| Other bias | Unclear risk | Insufficient information |
Stacy 2009.
| Methods |
Aims: to assess the impact of a behaviour change programme to increase statin adherence using IVR technology Study design: RCT; recruitment: other ‐ health benefit company (organisational referral) Study duration: 6 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: continuously enrolled in the plan with a pharmacy benefit for a minimum of 12 months prior to the date of the index statin; no pharmacy claims evidence of any lipid‐lowering agent in the 6‐month period prior to the index statin; 21 years of age or older; and a statin prescription with a 30‐day supply. Sample size: 497; mean age: 54 years; sex: men ‐ 38%, women ‐ 62%; ethnicity:* Country: USA |
|
| Interventions |
Intervention group: automated calls were generated by a computerised voice activated technology (VAT) that provided highly tailored messages that specifically reinforced adherence, persistence with statin medication by using a combination of behavioural science theories and techniques in a personalised or tailored manner dependent on the participant's previous response characteristics. 6 calls were attempted over a period of 10 days. If an answering machine or another member of the household was reached, the participant was asked to call back at a toll‐free number. If the targeted participant was reached, and the calls went ahead, then a verbal informed consent was read. The subsequent calls referred respondents to the health plan website for additional information regarding dyslipidaemia, risk reduction, and lipid‐lowering medication. These calls were coupled with a print guide (mailed at the conclusion of the first call) that provided tailored messages designed to enhance commitment, improve communication with the health care team, and address specific barriers to adherence. Participants in the control group received enhanced care, which included non‐tailored behavioural advice from a single IVR call, coupled with a non‐tailored, generic, self‐help cholesterol management guide received through the mail. This guide provided educational material on cholesterol and lipid values, a brief knowledge quiz, and a non‐tailored action plan. |
|
| Outcomes | Medication (statins) adherence (measured with 6‐month point prevalence persistency) | |
| Funding | NA | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | "it was anticipated that control group would have a 6‐month point prevalence rate of 65%, and that exposure to the experimental intervention would increase this rate to 75%.With power set at 0.80 and alpha at <0.05 (1‐sided test), it was necessary to impanel 260 participants per group. To account for 10% disenrollment over the 6‐month follow‐up period, approximately 290 participants per group were enrolled." | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "the IVR system randomly assigned subjects to either the experimental or the enhanced care control group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "With the exception of the item assessing the number of chronic medications in the 3‐month period prior to the index statin (participants assigned to the experimental group had a lower number of concomitant medications), no statistically significant group differences were detected between the groups." Comment: groups were similar across all baseline characteristics but the number of chronic medications; however, it is unclear whether this has introduced bias. |
Stehr‐Green 1993.
| Methods |
Aims: to evaluate the effectiveness of computer‐generated telephoned reminders used to raise the rates of on‐time immunisation among preschool‐age children in 2 public clinics in Atlanta, GA Study design: RCT; recruitment: primary care (health professional referral) Study duration: 1 month; study type: prevention; subtype: immunisation |
|
| Participants |
Inclusion criteria: children due to receive diphtheria‐tetanus‐pertussis, poliovirus, or measles, mumps and rubella vaccines during the study's 6‐week enrolment period in February and March 1990 Sample size: 229; mean age: 9 months; sex: boys ‐ 52%, girls ‐ 48%;ethnicity: black ‐ 91%, other – 6%, Hispanic ‐ 3% Country: USA |
|
| Interventions |
Automated telephone reminder from the Fulton County Health Department. The text of the standard message, which was delivered in a normal human voice, was: "This is the Fulton County Health Department calling to remind you that your child is due for an immunisation or 'shot' this month. Please call the health centre for an appointment or bring your child in to the health centre any day this week, Monday through Friday, between 8:30 am and 4 pm. Immunisations are important to protect your child from certain diseases, such as whooping cough, measles, and polio. They are also required for day care or school attendance." Calls were made during 5 days, beginning the day before the child became due for his or her immunisation. A maximum of 9 attempts (not counting wrong numbers, non‐working numbers, or mis‐dials) were made to each child's home, until an answer was obtained; ≥ 5 of the calls were made between 6 and 9 pm. Calls not answered, responses by an answering machine (for which no reminder message was left), hang‐ups within 10 seconds, and busy signals were classified as missed attempts. Participants in the control group received no calls. |
|
| Outcomes | Immunisation status | |
| Funding | CDC, Atlanta, Ga, and Cooperative Agreement TS‐622 from the Association for Teachers of Preventive Medicine, Washington, DC | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Of the 229 children who met the eligibility criteria for entry into the study, 6 were lost to follow‐up (that is, clinic records could not be located after their follow‐up period), and 1 was deferred from receiving further vaccinations, pending medical evaluation." Comment: attrition was small (n = 7) and reasons for attrition were provided; however, it is unclear whether the attrition was similar across groups |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Comment: groups were similar across all baseline characteristics |
Stuart 2003.
| Methods |
Aims: to explore the use of an innovative IVR system to increase participant adherence with antidepressant medication prescribed in primary care settings Study design: cluster RCT; recruitment: primary care practices (*) Study duration: 12 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: ≥ 18 years old, able to read English, not currently taking an antidepressant medication; newly prescribed an antidepressant medication by their primary care provider; access to a touch‐tone telephone; and willingness to participate in the study. Sample size: 647; mean age: *; sex: *; ethnicity:* Country: USA |
|
| Interventions |
Education: treatment team education and participant self‐care education Education + call: as above + 1 office nurse telephone call within 2 days of the visit when the antidepressant medication was prescribed. Education + call + IVR: as above + an IVR programme lasting for 3 months. A script was written for each of the IVR calls. In addition, the answer to each question generated a set of choices for the participant to respond to using a touch‐tone phone. |
|
| Outcomes | Adherence to (antidepressant) medication (primary); satisfaction (secondary) | |
| Funding | Eli Lilly & Company | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between education + call versus education + call +IVR. Cluster RCT with 30 primary care study sites as the unit of randomisation. Note that analysis did not appear to adjust for clustering, therefore a unit of analysis error exists that may result in overly precise effect estimates for this study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study was randomised controlled clinical trial of 647 patients" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "all patients a given site received 1 of 3 randomly assigned treatment strategies" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition in the intervention group. No description of drop‐outs in the control group. Quote: "Of the 232 assigned to the IVR, 116 (50%) either never used the system or stopped using it before the 12‐week IVR program was completed" |
| Selective reporting (reporting bias) | High risk | The authors mentioned that there were no significant differences in medication adherence among the 3 groups. However, the analysis was restricted to 1 sub‐group of participants who completed the IVR calls. |
| Other bias | High risk | No baseline characteristics were provided. It was not possible to assess the possibility of selective recruitment of cluster participants based on the information reported. |
Szilagyi 2006.
| Methods |
Aims: to measure the effect of telephone‐based reminder/recall on immunisation and well‐child care (WCC) visit rates among adolescents in urban practices Study design: RCT; recruitment: primary care (organisational referral) Study duration: 18 months; study type: prevention; subtype: immunisation |
|
| Participants |
Inclusion criteria: subjects with a birth date between 1 June 1983, and 31 May 1987 (aged 11‐14 years at the start of the intervention) Sample size: 3006; mean age:* sex: boys ‐ 50%, girls ‐ 50%; ethnicity: other or unknown – 41%, black non‐Hispanic ‐ 35%, white non‐Hispanic ‐ 17%, Hispanic ‐ 7% Country: USA |
|
| Interventions |
Automated telephone message reminder system (Autodialer). The intervention mimicked an appointment‐scheduling module that is linked to a telephone‐reminder system. Adolescents were called if they were due for an annual WCC visit, a tetanus booster (5 years since diphtheria and tetanus toxoids and pertussis vaccination), or a hepatitis B vaccination according to Advisory Committee on Immunisation Practices guidelines. A variable number of calls was placed depending on the need for immunisations or WCC visits and prior response to reminder calls. The calls were voice recordings in English to request a vaccination appointment or WCC visit or to remind families of upcoming scheduled appointments. Calls were made 6 days per week during the day or early evening. During the initial 11 months of the 18‐month clinical trial, telephone calls were stopped if recipients indicated from a telephone menu option that the telephone number was incorrect, the adolescent had left the practice, the parent requested calls to be stopped, or no appointment was scheduled despite 5 calls placed within 30 days ('unresponsive numbers'). After 11 months, the Autodialer telephone reminder calls were restarted for those participants with 'unresponsive numbers' to give families a second opportunity to respond to subsequent reminders. Participants in the control group received usual care. |
|
| Outcomes | Immunisation status | |
| Funding | CDC and Association for Teachers of Preventive Medicine, Washington, DC | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "To detect a 10% improvement in baseline immunisation rates of 50% (power of 0.80; =.05) within each practice required more than 750 adolescents per practice." | |
| Notes | The study design stratified for age group (11‐12 years and 13‐14 years) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "[Participants were] randomly allocated into a study group (n=1496) or control group (n=1510) using a random‐number generator with the child as the unit of randomisation" |
| Allocation concealment (selection bias) | Low risk | Quote: "Health care professionals were unaware of group allocation for specific subjects because the intervention used research personnel and reminders from a central office." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Health care professionals were unaware of group allocation for specific participants because the intervention used research personnel and reminders from a central office" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Blinded medical record reviews at the end of the study using a standardized medical record review form." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Intention‐to‐treat analyses were performed for the 1496 study and 1510 control subjects" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "Study and control groups were similar with respect to age group, sex, practice, insurance, and race/ethnicity" |
Szilagyi 2013.
| Methods |
Aims: to assess the impact of a managed care‐based patient reminder/recall system on immunisation rates and preventive care visits among low‐income adolescents Study design: RCT; recruitment: primary care (organisational referral) Study duration: 12 months; study type: prevention; subtype: immunisation |
|
| Participants |
Inclusion criteria: adolescents aged 10.5 through 17 years enrolled in Monroe Plan on 31 December 2009, with a primary care provider in a participating practice Sample size: 4115; mean age:* sex: boys ‐ 50%, girls ‐ 50%; ethnicity:* Country: USA |
|
| Interventions |
Telephone reminders were sent at the same frequency as letters by an Autodialer service in which a recorded human voice in English or Spanish was used, with a message that mirrored the information in the letter reminders Mail reminders. The letters provided the practice's telephone number. Letters were sent at 10‐week intervals for Tdap, MCV4, and preventive care visits (maximum of 5 reminders over 12 months) Participants in the control group received usual care |
|
| Outcomes | Immunisation status; preventive visit rate (both primary); process evaluation; costs (both secondary) | |
| Funding | CDC | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | The study had > 90% power for a 5% improvement in immunisation rates at study end assuming 50% for controls (2‐sided alpha = 0.05), using survival analysis and an intention to‐treat analysis | |
| Notes | Among all adolescents who received a reminder, the cost averaged USD 18.78 or USD 16.68 per adolescent per year for mail reminder group and telephone reminder group, respectively. There were no cost‐effectiveness data available for usual care group. This is a comparison between Autodialer and no intervention. The other intervention included mailed reminders. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation by AB (using Stata 9.2) stratifying on practice, age in years, and sex" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information. Quote: "Health care providers were unaware of group assignment." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | An intention to‐treat data analysis was used. |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Low risk | Quote: "The control and intervention groups had similar demographics (Table 14) and baseline immunisation and preventive visit rates." |
Tanke 1994.
| Methods |
Aims: to evaluate the effectiveness of automated telephone reminder on appointment reminder in patients undergoing tuberculosis care Study design: quasi‐RCT; recruitment: other ‐ county health department (organisational referral) Study duration: 6 months; study type: either; subtype: appointment reminder |
|
| Participants |
Inclusion criteria: participants with a scheduled appointments in the Tuberculosis Control Programme of Santa Clara County Health Department over a period of 6 months Sample size: 2008; median age: 19 years; sex: male ‐ 54 %; female ‐ 46 %; ethnicity: Spanish‐speaking ‐ 39%, Vietnamese‐speaking ‐ 28%, English‐speaking ‐14%, other – 13%, Tagalog‐speaking Filipino – 6% Country: USA |
|
| Interventions |
Teleminder: an automated telephone reminder call of their upcoming appointment in either English, Spanish, Tagalog, or Vietnamese was made 1 day prior to the appointment. Additional information about the clinic address and the time of appointment was also provided. Participants had the option to hear to the message again if they remained online. Participants receiving authoritative endorsement identified the source of message as coming from the Public Health Nurse at the Health Department while in the importance statement, the following statement was added ‐ "coming to this appointment is important so that you and your family will not become seriously ill." Message was sent between 6 pm and 9 pm, the evening before the scheduled appointment. Message was left on answering machine and if the line was busy, up to 5 attempts were made at half hour intervals Basic reminder + authority endorsement Basic reminder + importance statement Basic reminder + authority endorsement + importance statement No reminder (controls) |
|
| Outcomes | Attendance rate (primary); satisfaction (attitude questionnaire) (secondary) | |
| Funding | National Institute of Allergy & Infectious Diseases; National Institute on Ageing | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between Teleminder arm and control | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐random sequence generation. Quote: "random assignment of patients to conditions and the delivery of multiple messages on the same day would have required substantially more experimenter time" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Tanke 1997.
| Methods |
Aims: to assess the impact of automated telephone reminder on tuberculin skin test return Study design: RCT; recruitment: * (organisational referral) Study duration: 2 months; study type: either; subtype: appointment reminder |
|
| Participants |
Inclusion criteria: participants of Santa Clara County immunisation programme who received tuberculin skin test Sample size: 701; age: 55% < 12 years; sex: boys ‐ 45 %; girls ‐ 55 %; ethnicity: English‐speaking ‐ 59%, Spanish‐speaking ‐ 29%, Vietnamese‐speaking ‐ 3%, other – 9% Country: USA |
|
| Interventions |
Participants in the Teleminder group received an automated reminder in either English, Spanish, or Vietnamese between 6 pm and 9 pm of the evening before the scheduled day to have the tuberculin skin test read. The message was pre‐recorded by a female speaker that also provided the time and place of appointment. The message was repeated twice and if it reached an answering machine, the message was saved. If the line was busy, then up to 5 attempts were made, at half‐hour intervals Participants in the control group received no calls |
|
| Outcomes | Return of tuberculin test (primary); satisfaction (perceptions about reminders) (secondary) | |
| Funding | National Institute of Allergy & Infectious Diseases; National Institute on Ageing | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A research assistant randomly assigned the participants to either a control or an experimental group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Tucker 2012.
| Methods |
Aims: to evaluate the effectiveness of IVR self‐monitoring to support natural resolutions among community‐dwelling problem drinkers who had recently stopped high‐risk drinking without treatment and who were abstaining or engaging in low‐risk drinking. Study design: RCT; recruitment: community (media adverts) Study duration: 6 months; study type: prevention; subtype: alcohol |
|
| Participants |
Inclusion criteria: participants aged ≥ 21 years, problem drinking history more than 2 years, currently not taking any drugs except nicotine, and cessation of high‐risk drinking in the past 3–16 weeks without alcohol‐focused interventions Sample size: 187; age: 45 years; sex: men ‐ 63 %; women ‐ 37 %; ethnicity: white ‐ 54%, other race/ethnicity ‐ 46% Country: USA |
|
| Interventions |
Participants in the intervention group received IVR: the system was programmed using commercial software (SmartQ Version 5 [5.0.141], Telesage, Inc., Chapel Hill, NC). A daily survey assessed ounces of beer, wine, and distilled spirits consumed; use of other drugs to 'get high'; and dollars spent on alcohol and other drugs during the preceding day (defined as the 24‐hour period midnight‐to‐midnight yesterday). When no substance use was reported, participants answered questions about other prior‐day activities to balance call duration. 4 once‐a‐week surveys on Mondays through Thursdays assessed other relevant domains (e.g. strategies used to avoid/limit drinking, activities paired with drinking) Participants in the control group received an assessment‐only. |
|
| Outcomes | Drinking practices; spending on alcohol (both primary) | |
| Funding | National Institutes of Health/National Institute on Alcohol Abuse and Alcoholism (NIH/NIAAA) | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | No significant IVR main effects were found in any analysis either before or after adjusting for covariates (all ps > .20). Significant effects by compiler average causal effect (CACE) models examined IVR self‐monitoring effects. The other report from this trial had different aims: "to assess IVR in community‐dwelling HIV/AIDS patients in rural Alabama self‐monitored for enhancing daily HIV risk behaviours reporting.". Inclusion criteria: age ≥ 19 years (the age of majority in Alabama); reported use of alcohol or illicit drugs and sex with a partner within the past 3 months (in order to obtain sexually active substance users, the high risk target population for HIV risk reduction programmes); no health problems that precluded participation (e.g. dementia, psychosis); were not living in the HSC Hospice or other residential facility (e.g. inpatient substance abuse treatment programme) and were not taking any medication (e.g. disulfiram, methadone) that would substantially constrain opportunities for engaging in the risk behaviours of interest; and had daily phone access; Sample size: 54; mean age: 38 years; percentage of men ‐ 65 % and women ‐ 35 %; ethnicity: black ‐ 43%; and outcomes: changes in risk behaviours. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Urn randomisation used sex and race as balancing factors" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate. Data were not imputed using appropriate methods. Quote: "The follow‐up rate was about 70%. This suboptimal rate was partially addressed by including a 'missing' category as an outcome code along with the 3 resolution outcomes so that the analyses included all enrolled participants" |
| Selective reporting (reporting bias) | Low risk | Comment: all of the study's pre‐specified outcomes that are relevant to the review were reported |
| Other bias | Low risk | Comment: groups were similar across all baseline characteristics |
Vance 2011.
| Methods |
Aims: to determine the effectiveness of delivering 4 different interactive telephone technology programmes to reduce weight and improve blood glucose, insulin, high‐density lipoproteins, and triglycerides values Study design: RCT; recruitment: * (*) Study duration: 12 weeks; study type: prevention; subtype: weight management |
|
| Participants |
Inclusion criteria: * Sample size: 140; mean age: * sex: * ethnicity: * Country: USA |
|
| Interventions |
Interactive telephone counselling (ITC) + control Online behaviour‐based incentives + control ITC + behaviour‐based incentives + control Control ‐ written materials and once monthly group meetings |
|
| Outcomes | Weight change (primary); BMI; waist circumference; systolic blood pressure; blood glucose (secondary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between ITC + control versus and control. Information derived from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Velicer 2006.
| Methods |
Aims: to perform an effectiveness trial of nicotine replacement therapy (NRT) in combination with 3 low‐cost behavioural therapies (manuals, tailored expert system interventions, and an automated counselling intervention) Study design: RCT; recruitment: primary care (mail) Study duration: 30 months; study type: management; subtype: smoking |
|
| Participants |
Inclusion criteria: self‐identification as a smoker who regularly smoked ≥ 10 cigarettes per day and, therefore, met the requirements for using NRT Sample size: 2054; mean age: 51 years; sex: women ‐ 23%, men ‐ 77%; ethnicity: white ‐ 89%, black ‐ 5%, other ‐ 4%, Native American ‐ 2% Country: USA |
|
| Interventions |
Multimodal intervention automated counselling + NRT, manuals, and expert system (TEL + EXP + NRT + MAN). The interactive telecommunications system was developed for this study and employed a series of prerecorded voice files assembled in the form of a conversation that was tailored to the responses of the smoker. The telecommunications contacts served to both complete the assessment of progress on the 14 TTM variables and provide instant automated feedback. Material similar to that in the written paragraphs of the expert system progress reports was presented during the call and reproduced verbally Expert system + NRT and manuals (EXP + NRT + MAN) NRT + manuals (NRT + MAN) Stage‐matched manuals (MAN) |
|
| Outcomes | Smoking abstinence | |
| Funding | National Cancer Institute Grant CA71356 | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | This is a comparison between the multimodal intervention and the stage‐matched manuals | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After completing the survey, all eligible smokers were randomised by computer‐based random number generator to one of four intervention conditions" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Subjects were blinded to their treatment condition until they received the first intervention material; thus, awareness of the treatment condition could not influence the readiness for study participation. However, subjects were aware that several of the possible treatment conditions included NRT and that up to four follow‐up assessments by telephone were scheduled over the following 30 months." Insufficient information to judge whether this has introduced bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessment ensured. Quote: "The survey centre staff was blind to treatment condition." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The intention‐to‐treat analysis was conducted on the entire sample of 2,054 subjects identified as at risk for smoking" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "As a randomisation check, tests of significance ( p < .01) were performed to determine whether there were any differences between the four groups. All tests were non significant." |
Vollmer 2006.
| Methods |
Aims: to test the ability of an automated telephone outreach intervention to reduce acute healthcare utilisation and improve quality of life among adult asthma patients in a large managed care organisation Study design: RCT; recruitment: other ‐ health plan (organisational referral) Study duration: 10 months; study type: management; subtype: asthma |
|
| Participants |
Inclusion criteria: aged ≥ 18 years and either on the Kaiser Permanente Northwest (KPNW) high‐risk asthma registry or had ≥ 180 days of antiasthma medication dispensing during the 2‐year period 2000‐2001 and ≥ 1 medical contact for asthma during the same 2 years Sample size: 6,948; mean age: 52 years; sex: men ‐ 35%, women ‐ 65%; ethnicity: white, non‐Hispanic ‐ 92%, other – 8% Country: USA |
|
| Interventions |
Automated telephone outreach system (ATOS): the calls consisted of a series of questions designed to assess recent emergency department or hospital care for which the member had not had a follow‐up visit, current level of asthma control, current patterns of asthma medication use, and whether the member could identify a primary care provider whom he or she usually saw for asthma care. Based on the responses to these initial questions, members were offered (optional) tailored feedback regarding their overall level of asthma control and their use of asthma medications. Feedback was designed to convey a positive message without being prescriptive. The calls lasted less than 10 min and were made using speech‐recognition technology. The telephone message were translated into text message that was continuously updated in the electronic medical record. Participants at high risk of a future exacerbation are flagged and an electronic alert via electronic surveillance system placed in the medical record prompting their provider to review the encounter and clear the alert from the record Live calls (the same script as above) Usual care (controls) |
|
| Outcomes | Healthcare utilisation; asthma control; medication use; quality of life (all primary); satisfaction/acceptability to participants (secondary) | |
| Funding | CDC and the Kaiser Permanente Care Management Institute | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | Per protocol, the 2 intervention arms (automated and live‐person calling) were combined for the primary and post hoc analyses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Eligible individuals were randomly assigned to either usual care (n = 3367) or telephone outreach (n = 3581)." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The primary outcome analysis used an intention‐to‐treat design that included in the intervention group all randomised individuals, as well as persons who declined to participate in the intervention" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
Vollmer 2011.
| Methods |
Aims: to evaluate the effectiveness of an intervention based on health information technology (HIT) that used speech recognition software to promote adherence to inhaled corticosteroids among individuals with asthma who were members of a large health maintenance organisation Study design: RCT; recruitment: other ‐ health plan (mail) Study duration: 18 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: treatment for asthma during the 12‐month period prior to randomisation; ≥ 1 dispensing of a respiratory medication at a Kaiser Permanente Northwest or Kaiser Permanente Hawaii outpatient pharmacy during the 12‐month period prior to randomisation; aged ≥ 18 years, continuous Kaiser Permanente membership from the start of the baseline year until the time of randomisation Sample size: 8517; mean age: 54 years; sex: men ‐ 34%; women ‐ 66%; ethnicity: white ‐ 50%, unknown – 26%, Asian ‐ 11%, mixed – 7%, Native Hawaiian/Pacific Islander ‐ 4%, African American ‐ 2%, American Indian/Alaskan Native – 1% Country: USA |
|
| Interventions |
Participants in the intervention group received IVR: 3 basic IVR call types, each of which typically lasted 2‐3 min: a refill reminder call, a tardy refill call, and an initiator/restart call. Each month, participants' electronic medical records were scanned to determine who was eligible for which type of call. The tardy refill call went to individuals who were more than 1 month past their projected refill date. It not only reminded participants that they were due for an inhaled corticosteroids refill, but also assessed asthma control, explored inhaled corticosteroids adherence barriers, and provided tailored educational messages. Poorly controlled participants who declined to be transferred to the automated pharmacy refill line were offered the option to speak to a live pharmacist. The initiator/restart call was designed to provide support to participants who were either starting inhaled corticosteroids for the first time (new users) or were lapsed users. These calls went to individuals with an inhaled corticosteroids order or dispensing in the previous month and no other inhaled corticosteroids dispensing in the previous 6 months, and were similar to the tardy refill calls in that they included probes for asthma control and adherence barriers and offered tailored educational messages Participants in the control group received usual care. |
|
| Outcomes | Medication adherence (primary); asthma‐related healthcare utilisation (secondary) | |
| Funding | NA | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | "A priori power calculations showed near‐100% power to detect differences of 0.04 in adherence and 85% power to detect differences of 0.5 on the 7‐point mini‐AQLQ score." | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "[Participants] were randomised to either the intervention or usual care arms, with randomisation stratified by region and the clinic facility to which each patient was paneled." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: missing data have been imputed using appropriate methods. An ITT analysis was used to include all participants who received the intervention or usual care in the analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "Baseline characteristics of the intervention and usual care groups were very similar." |
Vollmer 2014.
| Methods |
Aims: to evaluate the utility of 2 electronic medical record‐linked, automated phone reminder interventions for improving adherence to cardiovascular disease medications Study design: RCT; recruitment: other ‐ health plan (organisational referral) Study duration: 12 months; study type: management; subtype: adherence to medication/laboratory tests |
|
| Participants |
Inclusion criteria: ≥ 40 years with diabetes mellitus and/or cardiovascular disease, suboptimally (< 90%) adherent to a statin or ACE inhibitor/angiotensin receptor blocker (ARB) during the previous 12 months, and due or overdue for a refill Sample size: 21,752; mean age: 64 years; sex: men ‐ 53%; women ‐ 47%; ethnicity: white ‐ 47%, Asian ‐ 17%, African American ‐15%, native Hawaiian/Pacific Islander ‐ 11%, unknown ‐ 9%, American Indian/Alaskan Native – 1% Country: USA |
|
| Interventions |
IVR calls. IVR participants received automated phone calls when they were due or overdue for a refill. The calls used speech‐recognition technology to educate participants about their medications and help them refill prescriptions (we created separate 'refill' and 'tardy' calls). The flow of each call was determined by participants' responses; each call lasted 2‐3 min. At randomisation, IVR participants received a pamphlet explaining these calls. Both call types offered a transfer to Kaiser Permanente's automated pharmacy refill line. The tardy call also offered a transfer to a live pharmacist. With permission, obtained at the first successful call contact, the programme left detailed messages on answering machines or with another household member Enhanced IVR (IVR Plus). In addition to IVR calls, participants in the IVR Plus arm received a personalised reminder letter if they were 60‐89 days overdue and a live outreach call if they were ≥ 90 days overdue, as well as electronic medical records‐based feedback to their primary care provider. IVR Plus participants received additional materials, including a personalised health report with their latest blood pressure and cholesterol levels, a pill organiser, and bimonthly mailings Usual care participants had access to the full range of usual services, including each region's normal education and care management outreach efforts to encourage statin and ACEI/ARB use |
|
| Outcomes | Medication adherence (primary); blood pressure and lipid levels (secondary) | |
| Funding | R01HS019341 from the Agency for Healthcare Research and Quality | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | The study had roughly 90% power to detect effects of 0.032 (3.2 percentage points) in adherence for statins and 0.045 (4.5 percentage points) for ACEI/ARBs in sex‐specific subgroup analyses, and effects of 0.039 (statins) and 0.045 (ACEI/ARBs) in subgroups defined by terciles of some baseline factor | |
| Notes | The estimated costs were USD 9 to USD 17 per participant per year for IVR and USD 36 to USD 47 for IVR Plus. No costs for UC were provided. This is a comparison between IVR and control. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated randomisation assignments were stratified by region and blocked to assure balance across treatment arms." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Neither participants nor providers were blinded to treatment assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "We used an intention‐to‐treat analysis to compare primary and secondary outcomes between intervention and UC participants." |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is available and all of the study's pre‐specified outcomes that are relevant to the review have been reported. |
| Other bias | Low risk | Quote: "Baseline characteristics of the intervention and UC groups for the pooled statin and ACEI/ARB analysis samples were very similar" |
Williams 2012.
| Methods |
Aims: to investigate the effects of the TLC Diabetes programme on health outcomes postintervention (time point 2) and at 12‐month follow‐up (time point 3) Study design: RCT; recruitment: primary care and the community (adverts in newspapers, flyers, newsletters and through diabetic clinics) Study duration: 12 months; study type: management; subtype: diabetes |
|
| Participants |
Inclusion criteria: participants with type 2 diabetes diagnosis of ≥ 3 months; aged 18‐70 years; residing in the greater Brisbane area (Australia); a glycated haemoglobin level of ≥ 7.5%; stable diabetes pharmacotherapy type for ≥ 3 months; stable pharmacotherapy dosage for ≥ 4 weeks; ability to clearly speak and understand English via the telephone, and weekly access to a telephone Sample size: 120 ; mean age: 57 years; sex: men ‐ 62.5%; women ‐ 37.5%; ethnicity: * Country: Australia |
|
| Interventions |
Telephone‐Linked Care (TLC) Diabetes system: participants receive TLC Diabetes kit containing the TLC Handbook, an ACCU‐CHEK Advantage glucose meter, test strips, and a Bluetooth device with which to upload their blood glucose results to the TLC Diabetes system. They call the system weekly using a landline or mobile phone. TLC's responses, including feedback and encouragement, were tailored according to information entered in the TLC database at the start and the answers that it received from participants during all calls. TLC stressed on the following self‐management behaviours: blood glucose testing (covered in all calls), nutrition (calls 9‐12; 21‐24), physical activity (calls 5‐8; 17‐20) and medication‐taking (calls 1‐4; 13‐16). Participants in the control group received usual care. |
|
| Outcomes | Glycated haemoglobin; health‐related quality of life (physical and mental components of the Short‐Form‐26 (SF‐26) scale) (all primary) | |
| Funding | National Health Medical Research Council project grant, HCF Health and Medical Research Foundation, and Queensland Health | |
| Declaration of conflict of interest | Dr Friedman has stock ownership and a consulting agreement with Infomedics, the company that owns commercial rights to the TLC technology used in the computerised intervention. He is also a member of its Board of Directors. The other authors declare that they have no competing interests | |
| Power calculations for sample size | With 80% power and a type 1 error of 5% (2‐tailed), it was possible to detect a difference in the primary outcome, glycated haemoglobin, of 0.61% between the intervention and control arms (based on a standard deviation change of 1.0% between the randomised arms). | |
| Notes | 43% of total participants were on insulin (injected). Mean BMI: 33 kg/m2. The TLC coordinator phones intervention participants after their first 2 calls to the TLC system and at weeks 6, 12 and 20, to identify and resolve any issues faced during their use of the TLC Diabetes system or to identify reasons for not calling regularly. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The arm allocation was conducted using a 4 x 4 block randomised block design with the participant as the unit of randomisation." |
| Allocation concealment (selection bias) | Low risk | Correspondence with the author: "We used opaque envelopes, so all envelopes were prepared at the start of the trial, contained allocation to intervention or control according to randomisation schedule.' |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The treating physicians were not blinded to the allocation." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data have been imputed using appropriate methods. Quote: "To account for subjects lost to follow‐up in intention‐to‐treat analyses, multiple imputation was performed using ten imputed datasets" |
| Selective reporting (reporting bias) | High risk | The protocol lists about 16 secondary outcome measures that were not reported in the 6‐month report. Correspondence with the author: "these data have been collected but I'm afraid no analyses have been performed yet. We could not fit the 6‐month secondary outcomes into this paper unfortunately." |
| Other bias | High risk | Quote: "Comparison of the baseline characteristics across usual care and intervention arms revealed important differences in e‐GFR which showed a significantly greater impairment in renal function in the intervention compared with usual care arm, and creatinine. Other differences observed were in age, education, and self‐care behaviours (adherence to blood glucose testing recommendations and daily insulin/diabetes medications, and foot inspections)." |
Wright 2013.
| Methods |
Aims: to evaluate the acceptability and feasibility of a scalable obesity treatment programme integrated with paediatric primary care and delivered using IVR to families from underserved populations Study design: RCT; recruitment: primary care (advert in clinic) Study duration: 3 months; study type: prevention; subtype: weight management |
|
| Participants |
Inclusion criteria: 9‐12 years old, a BMI 0‐5 BMI points above the 95th percentile for age and sex, attended a paediatric visit within the last year, and due for an annual well‐child exam in 4 months Sample size: 50 dyads; mean age: 10 years; sex: boys ‐ 58%, girls ‐ 42%; ethnicity: white ‐ 6%, African American ‐ 72%, other ‐ 22% Country: USA |
|
| Interventions |
Intervention: both parents and children received a 12‐week telephone counselling delivered by an automated IVR system. The intervention also included an EHR behavioural counselling tool used by the PC clinician during well‐child follow‐up visits. Similar but separate interventions were developed for parents and children. The IVR was designed to monitor, educate, and counsel parents and children on healthy weight management and television time through weekly IVR telephone conversations. During these conversations, the system spoke to participants using computerised voice by means of text‐to‐speech technology. Participants communicated by speaking into the telephone receiver or by pressing keys on the telephone keypad. The conversation is tailored to the individual user of the IVR such that the IVR asked questions and provides tailored feedback based on the user's response. Questions are asked to monitor the user's behaviour and provided education and theory‐based behaviour change strategies for the targeted behaviours as well as generate a conversation that is more human‐like. The HEAT system stores responses that are used to tailor the questions asked during the same conversation or inform subsequent calls Participants in the control group received no calls (wait‐list). |
|
| Outcomes | BMI z‐score; calorie intake; fat intake; fruit intake; vegetable intake; television‐viewing time (all primary) | |
| Funding | National Institute of Child and Human Development (NICHD R21 HD050939‐02) | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Fifty parent‐child dyads were randomised in blocks of six to either the intervention condition (HEAT) or WLC condition. The blocks were generated by an investigator who did not have contact with the participants." |
| Allocation concealment (selection bias) | Low risk | Quote: "Assignments to condition were placed in sealed envelopes and opened after all baseline measures were completed." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Intention‐to‐treat analyses with baseline values carried forward for those missing at follow‐up were also conducted" |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Comment: groups were similar across all baseline characteristics but weight and height; however, it is unclear whether this has introduced bias |
Xu 2010.
| Methods |
Aims: to evaluate the effects of an automated IVR system and specialist nurse support to reduce health care utilisation and improve health‐related quality of life in children with asthma Study design: RCT; recruitment: secondary care (*) Study duration: 6 months; study type: management; subtype: asthma |
|
| Participants |
Inclusion criteria: children and adolescents aged 3‐16 years with doctor‐diagnosed asthma who had either had an admission to hospital in the previous 12 months or had presented at least once to an emergency department or to their general practitioner or specialist with acute asthma requiring oral steroid rescue in the previous 12 months Sample size: 121; mean age: 7 years; sex: men ‐ 53%, women ‐ 47%; ethnicity:* Country: Australia |
|
| Interventions |
IVR: participants received an automated telephone call twice a week on their home phone or mobile phone. Children over 12 years old were encouraged to answer calls themselves. Parents answered calls for children younger than 12 years old. The IVR system asked questions about asthma symptoms and medication use and participants entered clinical data using the keypad on the phone. Educational messages, appropriate information from the asthma management plan, and medication reminders were given. Reports generated from the electronic system were sent to the primary physician electronically or by fax Nurse support group Usual care (control group) |
|
| Outcomes | Healthcare utilisation (primary); use of oral steroid rescue; health‐related quality of life; costs (secondary) | |
| Funding | Asthma Foundations of Australia and Royal Children's Hospital Foundation Brisbane Australia | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | NA | |
| Notes | IVR was more cost‐effective than usual care in reducing the total health care costs (mean AUD −451 (95% CI −1075, 172); but less cost‐effective than nurse support group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Block randomisation was used with random block sizes of three or six to create an allocation to one of the three groups for all study subjects" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "One child in the control group was lost to follow‐up during the study." Comment: low attrition rate and unlikely to have introduced bias |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Quote: "The groups were reasonably well matched at baseline, although the control group had fewer hospital admissions and ED presentations over the previous 12 months compared with Nurse Support and IVR groups at baseline." Comment: groups were similar across all baseline characteristics but hospital admissions and ED presentation; however, it is unclear whether this has introduced bias. |
Yount 2014.
| Methods |
Aims: to evaluate the efficacy of technology‐based symptom monitoring and reporting in reducing symptom burden in patients with advanced lung cancer Study design: RCT; recruitment: primary care (*) Study duration: 12 weeks; study type: management; subtype: cancer |
|
| Participants |
Inclusion criteria: ≥ 18 years old, English‐speaking, having advanced non‐small cell lung cancer or small cell lung cancer, receiving active treatment with traditional chemotherapy no later than day 1 of cycle 2 or receiving oral therapy, having access to a telephone, and life expectancy of ≥ 6 months Sample size: 253; mean age: 61 years; sex: men ‐ 49%, women ‐ 51%; ethnicity: white ‐ 58%, black or African American ‐ 36%, other ‐ 6% Country: USA |
|
| Interventions |
Participants in the intervention group received monitoring and reporting (MR group) via IVR. The participants delivered reports of clinically significant symptoms to their clinical team for further assessment and/or management; and had paper copies of longitudinal, graphical displays of symptom scores available Participants in the control group received monitoring alone (MA) via IVR |
|
| Outcomes | Symptom burden (primary); quality of life; treatment satisfaction; symptom management barriers; self‐efficacy (secondary) | |
| Funding | National Cancer Institute (R01‐CA115361) | |
| Declaration of conflict of interest | None declared | |
| Power calculations for sample size | "The study was powered to detect a difference between the two study groups in SDS total score. For this endpoint, a standardized effect size (mean group difference/common standard deviation) of 0.33 has been suggested to be meaningful in the measurement of PROs in several different cancer populations" | |
| Notes | Both groups received ATCS interventions | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After providing informed consent, participants completed baseline measures and were randomly assigned by computer in a 1:1 ratio to the MR or the MA group. Randomization was blocked, stratified by institution, with a goal of enrolling 100 participants from each of the three sites (total N = 300), 150 in each group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "This was a non‐blinded, randomised, controlled trial of technology‐based symptom monitoring with reporting (MR group) to the clinical team compared with symptom monitoring alone (MA group)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "A blinded interim analysis of symptom severity and study burden data was planned after half of the randomised patients (N = 150) had reached the week 12 assessment, and this analysis was reviewed by the institutional cancer centre data and safety monitoring board." Insufficient information to judge whether blinded assessments were performed. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were based on intention‐to‐treat in all randomised participants and were not adjusted for multiple comparisons." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Low risk | Quote: "The study groups were equivalent in baseline characteristics" |
Zautra 2012.
| Methods |
Aims: to examine the effects of a brief, daily intervention targeting either personal control/mastery (MC) or mindful awareness/acceptance (MA) compared with a placebo treatment that consisted of tips to a healthy life‐style (HT) Study design: RCT; recruitment: community (phone and home visits) Study duration: 1 month; study type: management; subtype: depression |
|
| Participants |
Inclusion criteria: individuals with mild to moderate symptoms of depression Sample size: 73; mean age: * sex: * ethnicity: other – 74%, Hispanic – 26% Country: USA |
|
| Interventions |
Personal control/mastery. Intervention was delivered in pre‐recorded messages via phone each morning. Each evening, participants completed an on‐line daily diary that included the outcome measures Mindful awareness/acceptance (delivered as above) Healthy lifestyle (controls) |
|
| Outcomes | Stress; depression | |
| Funding | NIA Grant RO1–AG‐6026006 | |
| Declaration of conflict of interest | NA | |
| Power calculations for sample size | NA | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "Seventy‐three adults recruited to participate in the trial, and randomly assigned to MC, MA, or HT conditions" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of study personnel was ensured. Quote: "The research assistants were blinded to the hypotheses of the study and did not have access to the daily diary data of the participants at any time during the study." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate. Missing outcome data balanced in numbers, with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
ACE: angiotensin‐converting‐enzyme; ART: antiretroviral therapy; AT2: angiotensin 2; ATCS: automated telephone communication system; BI: brief intervention; BMI; body mass index; CBT: cognitive behavioural therapy; CDC: Centers for Disease Control and Prevention; COPD: chronic obstructive pulmonary disease; CPAP: continuous positive airway pressure; DSM: Diagnostic and Statistical Manual of Mental Disorders; EHR: electronic health record; EMR: electronic medical record; FDA: Food and Drug Administration; HMO: health maintenance organisation; ITT: intention‐to‐treat; IVR: interactive voice recognition; MI: motivational interviewing; NA: not available; NIAAA: National Institute on Alcohol Abuse and Alcoholism; OSAS: obstructive sleep apnoea syndrome; QALY: quality‐adjusted life year; PCI: percutaneous coronary intervention; PCP: primary care provider; PHQ‐8/9: personal health questionnaire, version 8/9; PTSD: post‐traumatic stress disorder; RCT: randomised controlled trial; UC: usual care; UOHI: University of Ottawa Heart Institute. aPlease note that for reporting of participants' ethnicity, the terms used by authors of the included studies have been used in each case and are cited directly from each of the included studies.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aarons 2012 | Intervention does not use an ATCS |
| Abbott 2013 | Intervention does not use an ATCS |
| Adie 2010 | Intervention does not use an ATCS |
| Agel 2001 | No preventive healthcare or management of long‐term condition |
| Aharonovich 2006 | Inappropriate study design |
| Aikens 2015a | Inappropriate study design |
| Aikens 2015b | Inappropriate study design |
| Albert 2014 | Inappropriate study design |
| Albert 2015 | Inappropriate study design |
| Albisser 2001 | Inappropriate study design |
| Albisser 2005 | Inappropriate study design |
| Alemagno 1996 | Inappropriate study design |
| Alemi 1994 | Inappropriate study design |
| Alemi 1995 | Inappropriate study design |
| Alemi 1996 | Intervention does not use an ATCS |
| Alemi 1996a | Intervention does not use an ATCS |
| Alkema 2007 | Intervention does not use an ATCS |
| Allen 2013 | Intervention does not use an ATCS |
| Alsabbagh 2013 | Intervention does not use an ATCS |
| Altfeld 2013 | Intervention does not use an ATCS |
| Anderson 2004 | Intervention does not use an ATCS |
| Andersson 2013 | No preventive healthcare or management of long‐term condition |
| Andersson 2014 | No preventive healthcare or management of long‐term condition |
| Arezina 2011 | Intervention does not use an ATCS |
| Armstrong 2009 | Intervention does not use an ATCS |
| Aseltine 2010 | Intervention does not use an ATCS |
| Avery 2004 | Intervention does not use an ATCS |
| Avery 2004a | Intervention does not use an ATCS |
| Bambauer 2005 | Intervention does not use an ATCS |
| Barohn 2013 | Inappropriate study design |
| Bartholomew 2011 | Intervention does not use an ATCS |
| Basch 2006 | Intervention does not use an ATCS |
| Bastian 2002 | Intervention does not use an ATCS |
| Bellazzi 2003 | Intervention does not use an ATCS |
| Bellazzi 2004 | Intervention does not use an ATCS |
| Berkman 2014 | Intervention does not use an ATCS |
| Berman 2012 | No preventive healthcare or management of long‐term condition |
| Bexelius 2010 | Inappropriate study design |
| Bigby 1983 | Intervention does not use an ATCS |
| Bischof 2008 | Intervention does not use an ATCS |
| Bischof 2010 | Intervention does not use an ATCS |
| Bjorner 2014a | No preventive healthcare or management of long‐term condition |
| Bjorner 2014b | No preventive healthcare or management of long‐term condition |
| Blackstone 2009 | No preventive healthcare or management of long‐term condition |
| Bloom 2004 | Intervention does not use an ATCS |
| Blumenthal 2014 | Intervention does not use an ATCS |
| Boekeloo 1998 | Inappropriate study design |
| Boisseau 2010 | Inappropriate study design |
| Bombardier 2013 | Intervention does not use an ATCS |
| Boren 2006 | Inappropriate study design |
| Borland 2003 | Intervention does not use an ATCS |
| Borland 2013 | Intervention does not use an ATCS |
| Borsari 2014 | Intervention does not use an ATCS |
| Bosworth 2008 | Intervention does not use an ATCS |
| Bowen 2010 | Intervention does not use an ATCS |
| Brown 2004 | Intervention does not use an ATCS |
| Brown 2007 | Intervention does not use an ATCS |
| Bruce 2005 | Intervention does not use an ATCS |
| Brustad 2003 | Inappropriate study design |
| Budin 2008 | Intervention does not use an ATCS |
| Burda 2012 | Inappropriate study design |
| Buscemi 2011 | Intervention does not use an ATCS |
| Bustamante 2013 | Intervention does not use an ATCS |
| Candy 2004 | Intervention does not use an ATCS |
| Carcaise‐Edinboro 2008 | Intervention does not use an ATCS |
| Carlbring 2006 | Intervention does not use an ATCS |
| Carmody 2013 | Intervention does not use an ATCS |
| Cecinati 2010 | Intervention does not use an ATCS |
| Chae 2000 | Intervention does not use an ATCS |
| Champion 2007 | Intervention does not use an ATCS |
| Chang 2010 | Inappropriate study design |
| Chiu 2010 | Intervention does not use an ATCS |
| Choudhry 2013 | Inappropriate study design |
| Collins 2003 | No preventive healthcare or management of long‐term condition |
| Collins 2010 | No preventive healthcare or management of long‐term condition |
| Cooney 2015 | Inappropriate study design |
| Corkrey 2002a | Inappropriate study design |
| Costanza 2007 | Intervention does not use an ATCS |
| Coughey 2010 | Intervention does not use an ATCS |
| Crawford 2005 | Inappropriate study design |
| Crawford 2014 | Inappropriate study design |
| Cudkowicz 2013 | Intervention does not use an ATCS |
| Curry 1995 | Intervention does not use an ATCS |
| Curry 2003 | Intervention does not use an ATCS |
| Dalal 2011a | No preventive healthcare or management of long‐term condition |
| Dalal 2011b | No preventive healthcare or management of long‐term condition |
| Damschroder 2010 | Intervention does not use an ATCS |
| Datta 2010 | Intervention does not use an ATCS |
| Datto 2003 | Intervention does not use an ATCS |
| Davidoff 1985 | Inappropriate study design |
| Day 2002 | Intervention does not use an ATCS |
| De San Miguel 2013 | Intervention does not use an ATCS |
| Decker 2009 | Inappropriate study design |
| Denis 2012 | Intervention does not use an ATCS |
| Depp 2015 | Intervention does not use an ATCS |
| Digenio 2009 | Intervention does not use an ATCS |
| Duncan 2014 | Intervention does not use an ATCS |
| Durso 2003 | Inappropriate study design |
| Dyches 1999 | Inappropriate study design |
| Eakin 2009 | Intervention does not use an ATCS |
| Eakin 2010 | Intervention does not use an ATCS |
| Eakin 2012 | Intervention does not use an ATCS |
| Eisdorfer 2003 | Intervention does not use an ATCS |
| Elliott 2013 | No preventive healthcare or management of long‐term condition |
| Elston 2010 | Intervention does not use an ATCS |
| Eng 2013 | No preventive healthcare or management of long‐term condition |
| Fadol 2011 | Inappropriate study design |
| Fairhurst 2008 | Intervention does not use an ATCS |
| Farabee 2013 | Intervention does not use an ATCS |
| Faridi 2008 | Intervention does not use an ATCS |
| Farmer 2005 | Intervention does not use an ATCS |
| Feldstein 2009 | Inappropriate study design |
| Fischer 2001 | No preventive healthcare or management of long‐term condition |
| Fischer 2014 | Inappropriate study design |
| Fisher 2013 | Intervention does not use an ATCS |
| Flax 2014 | No preventive healthcare or management of long‐term condition |
| Franc 2014 | Intervention does not use an ATCS |
| Furber 2010 | Intervention does not use an ATCS |
| Fursse 2008 | Intervention does not use an ATCS |
| Gazmararian 2010 | Inappropriate study design |
| Gilbert 2006 | Intervention does not use an ATCS |
| Gilman 2014 | Inappropriate study design |
| Glasgow 1996 | Intervention does not use an ATCS |
| Glasgow 2008 | Intervention does not use an ATCS |
| Goel 2008 | Intervention does not use an ATCS |
| Gonzalez 1997 | Inappropriate study design |
| Greaney 2012 | Intervention does not use an ATCS |
| Green 2010 | Intervention does not use an ATCS |
| Green 2013 | Intervention does not use an ATCS |
| Greene 1998 | Inappropriate study design |
| Greenley 2012 | Intervention does not use an ATCS |
| Groeneveld 2010 | Intervention does not use an ATCS |
| Haas 2015 | Intervention does not use an ATCS |
| Hall 2000 | Intervention does not use an ATCS |
| Hanauer 2009 | Intervention does not use an ATCS |
| Hardy 2011 | Intervention does not use an ATCS |
| Hasin 2014 | Inappropriate study design |
| Haynes 2006 | Inappropriate study design |
| Hedeker 2003 | Intervention does not use an ATCS |
| Henry 2012 | Inappropriate study design |
| Hersey 2012 | Intervention does not use an ATCS |
| Hettema 2012 | Inappropriate study design |
| Hollis 2005 | Intervention does not use an ATCS |
| Horng 2004 | Intervention does not use an ATCS |
| Horton 2008 | No preventive healthcare or management of long‐term condition |
| Hubbard 2007 | Intervention does not use an ATCS |
| Hurling 2007 | Intervention does not use an ATCS |
| Hurling 2013 | Intervention does not use an ATCS |
| Hwang 2014 | Intervention does not use an ATCS |
| Jacobs 2004 | Intervention does not use an ATCS |
| Jacobs 2011 | Intervention does not use an ATCS |
| Jiménez‐Muro 2013 | Intervention does not use an ATCS |
| Johnson 2014 | Inappropriate study design |
| Joyce 2008 | Intervention does not use an ATCS |
| Katz 2008 | Intervention does not use an ATCS |
| Kauer 2012 | Intervention does not use an ATCS |
| Kearney 2009 | Intervention does not use an ATCS |
| Kempe 2012 | Inappropriate study design |
| Kim 2007 | Intervention does not use an ATCS |
| Kim 2008 | Intervention does not use an ATCS |
| Kim 2012 | Inappropriate study design |
| Kim 2013 | Intervention does not use an ATCS |
| Klausen 2012 | Intervention does not use an ATCS |
| Kobak 1997 | Inappropriate study design |
| Kobak 2015 | Intervention does not use an ATCS |
| Kolt 2007 | Intervention does not use an ATCS |
| Konstam 2011 | Intervention does not use an ATCS |
| Kristal 2000 | Intervention does not use an ATCS |
| Kwon 2010 | Intervention does not use an ATCS |
| Kwon 2012 | Intervention does not use an ATCS |
| Ladyzynski 2007 | Intervention does not use an ATCS |
| Larocque 2014 | Inappropriate study design |
| Leichter 2013 | Intervention does not use an ATCS |
| Leigh 2014 | Inappropriate study design |
| Leimig 2008 | Intervention does not use an ATCS |
| Leon 1999 | No preventive healthcare or management of long‐term condition |
| Levin 2011 | Intervention does not use an ATCS |
| Levinson 2008 | Intervention does not use an ATCS |
| Lewis 2010 | Intervention does not use an ATCS |
| Lichtenstein 2008 | Intervention does not use an ATCS |
| Lim 2011 | Intervention does not use an ATCS |
| Linder 2014 | Intervention does not use an ATCS |
| Lindner 2013 | Intervention does not use an ATCS |
| Lindsay 2014 | Inappropriate study design |
| Liu 2008 | Intervention does not use an ATCS |
| Liu 2011 | Intervention does not use an ATCS |
| Lovejoy 2014 | Intervention does not use an ATCS |
| Ludman 2007 | Intervention does not use an ATCS |
| Mahoney 1999 | Inappropriate study design |
| Markert 2013 | Intervention does not use an ATCS |
| Marshall 1993 | Inappropriate study design |
| McCann 2009 | Intervention does not use an ATCS |
| McDaniel 2005 | Inappropriate study design |
| Miskelly 2005 | Intervention does not use an ATCS |
| Mollon 2008 | Inappropriate study design |
| Mooney 2002 | Inappropriate study design |
| Mooney 2013 | Inappropriate study design |
| Naylor 2002 | Inappropriate study design |
| O'Brien 1998 | Intervention does not use an ATCS |
| Oake 2009 | Inappropriate study design |
| Odegard 2012 | Intervention does not use an ATCS |
| Orsama 2013 | Intervention does not use an ATCS |
| Osgood‐Hynes 1998 | Inappropriate study design |
| Pakhale 2015 | Intervention does not use an ATCS |
| Patrick 2000 | Inappropriate study design |
| Patten 2003 | Data for ATCS group unavailable. Contact with author: "I apologize for not being helpful and regret that the value of the data cannot be extended by inclusion in the systematic review. Apparently, the back‐up files for this project were scored on 3.5 inch floppy disks (!!) that were discarded during an office move". |
| Pellegrini 2012 | Intervention does not use an ATCS |
| Pinto 2011 | Intervention does not use an ATCS |
| Pinto 2013a | Intervention does not use an ATCS |
| Pinto 2013b | Intervention does not use an ATCS |
| Pizzi 2014 | Intervention does not use an ATCS |
| Prochaska 2001 | Intervention does not use an ATCS |
| Ramelson 1999 | Inappropriate study design |
| Riegel 2006 | Intervention does not use an ATCS |
| Rizvi 2011 | Intervention does not use an ATCS |
| Roberts 2007 | Intervention does not use an ATCS |
| Rolnick 1997 | Intervention does not use an ATCS |
| Rose 2010 | Inappropriate study design |
| Rosser 1992 | Intervention does not use an ATCS |
| Rothemich 2010 | Intervention does not use an ATCS |
| Rubin 2006 | Inappropriate study design |
| Salisbury 2013 | Intervention does not use an ATCS |
| Sano 2013 | No preventive healthcare or management of long‐term condition |
| Sano 2014 | No preventive healthcare or management of long‐term condition |
| Schuurman 1980 | Inappropriate study design |
| Scott 2011 | Inappropriate study design |
| Seto 2012 | Intervention does not use an ATCS |
| Shah 2014 | Intervention does not use an ATCS |
| Siddiqui 2011 | Intervention does not use an ATCS |
| Silveira 2011 | Intervention does not use an ATCS |
| Simon 2000 | Intervention does not use an ATCS |
| Simon 2004 | Intervention does not use an ATCS |
| Simon 2006 | Intervention does not use an ATCS |
| Simpson 2011a | Inappropriate study design |
| Simpson 2011b | Intervention does not use an ATCS |
| Skolarus 2012 | No preventive healthcare or management of long‐term condition |
| Soran 2008 | Intervention does not use an ATCS |
| Statland 2011 | Inappropriate study design |
| Stevens 2008 | Intervention does not use an ATCS |
| Stiles‐Shields 2014 | Intervention does not use an ATCS |
| Stockwell 2012 | Intervention does not use an ATCS |
| Tourangeau 2002 | Inappropriate study design |
| Tucker 2013 | Inappropriate study design |
| VanWormer 2009 | Intervention does not use an ATCS |
| Veroff 2013 | No preventive healthcare or management of long‐term condition |
| Vivier 2000a | Intervention does not use an ATCS |
| Vivier 2000b | Intervention does not use an ATCS |
| Wade 2010 | Inappropriate study design |
| Wu 2014a | Intervention does not use an ATCS |
| Wu 2014b | Intervention does not use an ATCS |
| Yoon 2008 | Intervention does not use an ATCS |
| Zhu 2012 | Intervention does not use an ATCS |
ATCS: automated telephone communication system.
Characteristics of ongoing studies [ordered by study ID]
Almeida 2014.
| Trial name or title | diaBEAT‐it! |
| Methods |
Aims: to determine the reach of each active intervention, the effectiveness of the strategies in supporting patients to lose and maintain a 5% weight loss, and the cost‐effectiveness of the interventions in achieving standard weight loss Study design: RCT; recruitment: primary care (mail and telephone) Study duration: ongoing; study type: management; subtype: diabetes |
| Participants |
Inclusion criteria: age > 18; BMI > 25; and indicates high risk for developing diabetes, based on the diabetes risk test calculator Sample size: 360; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: small group intervention + 12 months of interactive voice response telephone follow‐up (SG‐IVR) Arm b: DVD version of the small group intervention with the same IVR follow‐up (DVD‐IVR) Arm c: standard care |
| Outcomes | Weight loss; reach; cost; physical activity; dietary intake |
| Starting date | 2014 |
| Contact information | falmeida@vt.edu |
| Notes | Clinicaltrials.gov identifier: NCT02162901 |
Ashmore 2013.
| Trial name or title | COPD‐SMART |
| Methods |
Aims: to determine if a self‐management lifestyle physical activity intervention would improve physical functioning and dyspnoea Study design: RCT; recruitment: primary care (mail and telephone) Study duration: ongoing study type: management; subtype: chronic obstructive pulmonary disease |
| Participants |
Inclusion criteria: age ≥ 45 years; physician diagnosis of chronic obstructive pulmonary disease; forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio < 70% and FEV1 < 70%; modified Medical Research Council dyspnoea score ≥ 2 Sample size: 305; mean age: 69; sex: women ‐ 50%, men ‐ 50%; ethnicity: white ‐ 92%, black ‐ 6%, Hispanic ‐ 1%, other ‐ 1% Country: USA |
| Interventions |
Intervention group received self‐management needs assessment; chronic obstructive pulmonary disease self‐management education (Weeks 1‐6); physical activity self‐management (weeks 7‐36) ‐ the program is delivered using a structured workbook supported by one‐on‐one telephone counselling every other week by the health coach with computer assisted telephone calls on alternating weeks Usual care continued regular follow‐up with their physician and to call the health coach using a toll‐free number if they have any questions. Study‐related contact occurs through monthly automated telephone calls, which collect health care utilisation data, and follow‐up visits for data collection at 6, 12, and 18 months |
| Outcomes | Chronic Respiratory Questionnaire (CRQ) dyspnoea domain and 6‐minute walk distance; other CRQ domains (fatigue, emotion, and mastery); Quality of Life (SF‐12); Health care utilisation; Process outcomes |
| Starting date | 2010 |
| Contact information | david.coultas@va.gov |
| Notes | Clinicaltrials.gov identifier: NCT1108991 |
Baker 2013.
| Trial name or title | Boston Osteoarthritis Strengthening telephone linked‐communication (BOOST TLC) |
| Methods |
Aims: to empower and motivate people with knee OA to adhere to strengthening exercise after participating in a class Study design: RCT; Recruitment: community (*) Study duration: ongoing Study type: management; Sub ‐ type: osteoarthritis |
| Participants |
Inclusion criteria: subjects with painful knee osteoarthritis (OA) Sample size: 100; Mean age: * sex: * Ethnicity: * Country: USA |
| Interventions |
Arm a: TLC is an automated, interactive conversation system that speaks with a recorded human voice. During the conversation the system asks questions, comments on the users' responses and educates and counsels them. TLC stores the users' answers in a database used to direct current and future TLC conversations. The system is run by a scheduling protocol with the ability to receive and make calls Arm b: the control group receives an automated message once per month, reminding them to strength train and record their progress in their log. |
| Outcomes | Pain and physical function; timed physical function tasks; isokinetic muscle strength |
| Starting date | 2013 |
| Contact information | bsenkbeil@rheumatology.org |
| Notes | — |
Droste 2013.
| Trial name or title | ICT‐supported cardiovascular disease prevention through phone‐based automated lifestyle coaching |
| Methods |
Aims: to support cardiovascular disease patients in performing appropriate behaviour changes in order to minimise their individual risk factors Study design: RCT; recruitment: * Study duration: ongoing study type: prevention; subtype: cardiovascular disease |
| Participants |
Inclusion criteria: already suffered a stroke or transient ischaemic attack (TIA) or ≥ 2 risk factors for stroke: high blood pressure, overweight; low physical activity; smoking; unhealthy diet Sample size: 94; mean age: * sex: * ethnicity: * Country: Luxemburg |
| Interventions |
Arm a: computer‐based lifestyle coaching system via IVR Arm b: no details of control group |
| Outcomes | Change in systolic blood pressure; serum high‐density lipoproteins, low‐density lipoproteins and triglycerides levels; glycated haemoglobin; glycaemia; BMI; acceptance; efficacy |
| Starting date | January 2013 |
| Contact information | Department of Neurology, Centre Hospitalier de Luxembourg, Luxembourg |
| Notes | ClinicalTrials.gov identifier: NCT02444715 |
Emmons 2008.
| Trial name or title | A sustainable approach to increasing cancer screening (CATCH) |
| Methods |
Aims: to compare the efficacy of two intervention arms intended to increase breast, cervical, and colon cancer screening rates among patients served by community health centres. Study design: RCT; recruitment: * Study duration: ongoing; study type: prevention; subtype: screening |
| Participants |
Inclusion criteria: all eligible patients, using centre guidelines, in need of: breast, cervical or colorectal cancer screenings. Sample size: 13,675; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: consistent, but spaced‐out calls generated by an IVR system reminding them of breast, cervical and colon cancer screenings needed, as applicable. Arm b: IVR calls followed up by prevention care coordinator calls for those who do not respond to IVR |
| Outcomes | Change in population level cancer screening level at the health clinics involved |
| Starting date | September 2008 |
| Contact information | Karen Emmons, Harvard School of Public Health |
| Notes | ClinicalTrials.gov identifier: NCT01395459 |
Estabrooks 2011.
| Trial name or title | CardiACTION! |
| Methods |
Aims: to assess whether physical activity behaviour change is more likely when the participants' social‐cognitive beliefs are intervened upon (individual intervention), when access is provided to environmental resources for physical activity (environmental intervention), or when both social‐cognitive beliefs and access to environmental physical activity resources are manipulated (combination intervention including individual and environmental intervention components) Study design: randomised 2 × 2 factorial trial; recruitment: primary care (health professional referral) Study duration: ongoing; study type: prevention; subtype: physical activity |
| Participants |
Inclusion criteria: patients who did not report meeting the recommended guidelines for physical activity (i.e. < 150 min of moderate physical activity per week), spoke English, did not currently have a fitness facility membership, and had a telephone Sample size: *; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: interactive computer session Arm b: automated telephone counselling. Over 6 months participants received frequent contacts delivered via IVR automated telephone calls and mailings, each providing intervention‐specific information to encourage and facilitate physical activity or healthful eating behaviour change Arm c: tailored mailings Arm d: combination intervention |
| Outcomes | Changes in physical activity levels |
| Starting date | — |
| Contact information | estabrkp@vt.edu |
| Notes | — |
Fellows 2012.
| Trial name or title | Health and economic effects from linking bedside and outpatient tobacco cessation services for hospitalised smokers in two large hospitals: study protocol for a RCT |
| Methods |
Aims: the study assesses the effectiveness and cost‐effectiveness of linking a practical inpatient assisted referral to outpatient cessation services plus interactive voice recognition (AR + IVR) follow‐up calls, compared to usual care inpatient counselling (UC) Study design: RCT; recruitment: secondary care (*) Study duration: ongoing; study type: management; subtype: smoking |
| Participants |
Inclusion criteria: aged ≥ 18 years who smoked ≥ 1 cigarettes in the past 30 days, willing to remain abstinent postdischarge, have a working phone, live within 50 miles of the hospital, speak English, and have no health‐related barriers to participation Sample size: 900; mean age: *; sex: men (KPNW ‐ 51.7%, OHSU ‐ 51.7%); women (KPNW ‐ 48.3%, OHSU ‐ 48.3%); Ethnicity: KPNW: white ‐ 79.4%, Hispanics ‐ 2.2%, black ‐ 4.1%; OHSU: white ‐ 89.0%, Hispanics ‐ 3.5%, Black ‐ 5.3% Country: USA |
| Interventions |
Participants in the AR + IVR arm will receive a brief inpatient cessation consult plus a referral to available outpatient cessation programs and medications, and 4 IVR follow‐up calls over 7 weeks postdischarge. Control group will receive usual care. |
| Outcomes | Self‐reported 3‐day smoking abstinence at 6 months postrandomisation for outpatient cessation services plus interactive voice recognition (AR + IVR) participants compared to usual care |
| Starting date | — |
| Contact information | — |
| Notes | ClinicalTrials.gov identifier: NCT01236079 |
Forster 2015.
| Trial name or title | Information systems‐enabled outreach for preventing adverse drug events (ISTOP‐ADE) |
| Methods |
Aims: to determine whether the ISTOP‐ADE system, compared to routine care, will reduce: the probability of discontinuing the use of prognosis‐altering medications; the probability of a patient experiencing a severe ADE; the proportion of patients experiencing ADEs, preventable ADEs and ameliorable ADEs; and health services utilisation Study design: RCT; recruitment: primary care (health professional referral) Study duration: ongoing; study type: management; subtype: adherence to medication/laboratory tests |
| Participants |
Inclusion criteria: French‐ and English‐speaking adult patients (age >18) who receive a high‐risk incident prescription, use Régie de l’assurance maladie du Québec insurance to pay for medications and are followed by a physician who has consented to be in the Medical Office of the 21st Century research network Sample size: 2200; mean age: * sex: * ethnicity: * Country: Canada |
| Interventions |
Arm a: IVR system paired with pharmacist support Arm b: routine care |
| Outcomes | Medication persistence; healthcare utilisation |
| Starting date | Date registered: 10 January 2014 |
| Contact information | aforster@ohri.ca |
| Notes | ClinicalTrials.gov identifier: NCT02059044 |
Glasgow 2007.
| Trial name or title | Linking self‐management and primary care for diabetes 2 (LB2) |
| Methods |
Aims: to evaluate the impact of 2 different interactive, multimedia self‐management programs, relative to 'enhanced' usual care Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: diabetes |
| Participants |
Inclusion criteria: being 25‐75 years of age, live independently, have a telephone, are able to read in either English or Spanish, able to access the Internet at least twice per week are capable of providing informed consent, have been diagnosed with type 2 diabetes for at least 1 year are overweight (BMI ≥ 25), and have at least one additional UKPDS equation risk factor (i.e. high lipids, hypertension, glycated haemoglobin, or smoking) Sample size: 463; mean age: 60 years; sex: men ‐ 52%; women ‐ 48%;ethnicity: Latino ‐ 23% Country: USA |
| Interventions |
Arm a: computer‐assisted self‐management plus social support. An interactive, automated self‐management (ASM) programme that uses web and interactive voice recognition (IVR) media combined with enhanced support in the form of group Diabetes Care Management visits and live follow‐up phone calls from Diabetes Care Managers Arm b: computer‐assisted self‐management (CASM). An interactive ASM programme that uses web and interactive voice recognition (IVR) media Arm c: usual care |
| Outcomes | Improvement in health behaviours (e.g. dietary patterns, physical activity, medication taking); and biologic outcomes (glycated haemoglobin, lipid ratio, blood pressure, and smoking status) |
| Starting date | January 2007 |
| Contact information | Russell E Glasgow, PhD, Kaiser Permanente |
| Notes | ClinicalTrials.gov identifier: NCT00987285 |
Heapy 2011.
| Trial name or title | Interactive voice response (IVR)‐based treatment for chronic low back pain |
| Methods |
Aims: the proposed study will test how well an innovative IVR method can be used for delivering treatment for chronic low back pain Study design: RCT; recruitment: secondary care Study duration: ongoing; study type: management; subtype: pain |
| Participants |
Inclusion criteria: presence of at least a moderate level of pain (i.e. pain scores of ≥ 4) and presence of pain for a period of ≥ 3 months; ability to participate safely in the walking portion of the intervention as evidenced by ability to walk at least one block; availability of a touch‐tone telephone and computer with Internet access in the participant's residence; veteran receiving care at VA Connecticut Healthcare System Sample size: 230; mean age: 58.6 years sex: men ‐ 83%; women ‐ 17%; ethnicity: white ‐ 56.5% Country: USA |
| Interventions |
Arm a: interactive CBT. IVR treatment consisted of a patient workbook supplemented by 10 weeks of daily IVR calls that provided pre‐recorded didactic information and weekly, pre‐recorded personalised therapist feedback. It also included daily IVR calls to collect pain‐related symptoms, adherence to pain coping skill practice and pedometer‐measured step counts Arm b: CBT |
| Outcomes | Numeric Rating Scale of Pain Intensity |
| Starting date | May 2011 |
| Contact information | — |
| Notes | ClinicalTrials.gov identifier: NCT01025752 |
Kulnawan 2011.
| Trial name or title | Diabetes telephone‐linked care system for self‐management support in Thailand |
| Methods |
Aims: to develop the diabetes telephone‐linked care system for self‐management support and test acceptability in terms of system uses, satisfaction and perception of easiness, helpfulness, and emotion with the system Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: diabetes |
| Participants |
Inclusion criteria: * Sample size: 112; mean age: * sex: * ethnicity: * Country: Thailand |
| Interventions |
The intervention group received the automated telephone system with diabetes knowledge IVR subsystem as the telephone‐linked care (TLC) No details of the control group reported |
| Outcomes | Glycemic control; patient satisfaction; system usability |
| Starting date | 2011 |
| Contact information | nittayawan@yahoo.com |
| Notes | — |
McDaniel 2010.
| Trial name or title | Technology‐enhanced quitline services to prevent smoking relapse (TEQ) |
| Methods |
Aims: to see if automated telephone monitoring will enhance existing quit line services, such as Alere Wellbeing's Quit For Life programme, and help people quit smoking. Study design: RCT; recruitment: * Study duration: ongoing study type: management; subtype: smoking |
| Participants |
Inclusion criteria: ≥ 18 years of age; enrolled in Free & Clear, Inc. services; self‐reported abstinence for at least 24 h at the quit date call; able to read and speak English; personal access to a touch‐tone telephone or cellular telephone Sample size: 1785; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: quit line service + 20 automated monitoring calls Arm b: quit line Service + 10 automated monitoring calls Arm c: usual care |
| Outcomes | Participant smoking status |
| Starting date | April 2010 |
| Contact information | Anna M McDaniel, PhD RN FAAN, Indiana University |
| Notes | ClinicalTrials.gov identifier: NCT00888992 |
Mooney 2010.
| Trial name or title | Hospice and end‐of‐life symptom monitoring & support using an automated system designed for family caregivers (SCP) |
| Methods |
Aims: to test an automated monitoring and coaching system for family caregivers during home hospice Study design: RCT; recruitment: secondary care (*) Study duration: ongoing study type: management; subtype: cancer |
| Participants |
Inclusion criteria for patient/caregiver dyad: both patient and caregiver are adults aged ≥ 18 years; patient has a limited life expectancy and has histological diagnosis of cancer; caregiver is caring for a family member with a limited life expectancy and admitted to one of the participating home care hospice or palliative care programmes; caregiver is English‐speaking and writing; caregiver has access to a telephone on a daily basis; caregiver is cognitively and physically able to use the phone unassisted and complete questionnaire; patient is assigned to a nurse case manager who has consented to participate in the research project; caregiver and patient intend to reside in the local area until the time of the patient's death Sample size: 450; mean age: 73 years; sex: men ‐ 52 %; women ‐ 48 %; ethnicity: white/Caucasian ‐ 95% Country: USA |
| Interventions |
Arm a: intervention group will receive a computer‐based telecommunication system to monitor symptoms as perceived and reported by the family caregiver; tailored care management messages that SCP provides directly to the caregivers to promote care management based on the individualised patient symptom profile and caregiver distress; and an automated alerting function that notifies the hospice nurse of unrelieved symptoms that have exceeded a pre‐set threshold Arm b: control group will receive usual care. |
| Outcomes | Family caregiver's assessment of dying patient's symptom severity level at end‐of‐life; caregiver's report their assessment of the severity of patient's symptoms daily |
| Starting date | May 2010 |
| Contact information | Kathi.Mooney@nurs.utah.edu |
| Notes | ClinicalTrials.gov identifier: NCT02112461 |
Mori 2009.
| Trial name or title | Telerehabilitation intervention to promote exercise for diabetes |
| Methods |
Aims: to develop an innovative strategy to address the problems of obesity and diabetes by promoting exercise adoption Study design: RCT; recruitment: * Study duration: ongoing; study type: prevention; subtype: physical activity |
| Participants |
Inclusion criteria: clinical diagnosis of type 2 diabetes mellitus; receive a medical clearance from physician; be sedentary; be interested in exercising; have a BMI > 25 kg/m2; have glycated haemoglobin of 7%‐10%; be on medication for diabetes Sample size: 89; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: Telephone‐Linked Care ‐ Promoting Exercise for Diabetes (TLC‐PED), a method that uses IVR and speech recognition technologies, will be developed to provide individualised and personalised motivational messages using automated telephone calls for veterans with type 2 diabetes who participate in a home‐based walking programme. Arm b: usual care |
| Outcomes | 7‐day physical activity recall; a self‐report measure of minutes of physical activity over the previous 7 days |
| Starting date | January 2009 |
| Contact information | Deanna L Mori, PhD, VA Medical Center, Jamaica Plain Campus |
| Notes | ClinicalTrials.gov identifier: NCT00334113 |
NCT00505024.
| Trial name or title | Interactive voice response system (IVRS) for managing symptoms of patients following thoracic surgery |
| Methods |
Aims: to study the effectiveness of the IVR system (IVRS), which is designed to send a report to a patient's doctor about severe symptoms they are experiencing Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: cancer |
| Participants |
Inclusion criteria: patients scheduled for thoracic surgery for non‐small cell lung cancer, esophageal cancer and lung metastasis; aged ≥ 18, of any sex, who were English‐speaking and residing in the United States. Sample size: 100; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: IVR system + symptoms report (twice weekly) Arm b: IVR system only |
| Outcomes | NA |
| Starting date | 2006 |
| Contact information | Xin Shelley Wang, MD; Anderson Cancer Center |
| Notes | Clinicaltrials.gov: NCT00505024 |
NCT00625638.
| Trial name or title | Interactive voice response system in advanced cancer patients |
| Methods |
Aims: to determine whether the IVR system, supplemented by nursing telephone intervention (NTI), results in better symptom management and quality of life than standard care for individuals with advanced cancer as evidenced by reduced scores on symptom measures. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: cancer |
| Participants |
Inclusion criteria: individuals with advanced cancer (incurable disease) who are seen in the supportive care centre at MD Anderson Cancer Center, who have a pain score of ≥ 4 or higher on the average pain scale item of the brief pain inventory for ≥ 2 weeks and at least 1 other symptom on the ESAS (fatigue, nausea, depression, anxiety, drowsiness, shortness of breath, appetite, sleep), who are able to identify a primary caregiver who also agrees to participate in the study, who have no clinical evidence of cognitive failure in the opinion of the referring MD. Caregivers must be able to understand the instructions for the study, be ≥ 18 years of age, have access and utilise a touch‐tone telephone, be willing to engage in a telephone follow‐up with the IVR system and nurses every Monday, Wednesday and Friday, be willing to follow up by phone or in person on day 8 (+/‐ 3 days) and return for a follow‐up visit on day 15 (+/‐5 days), be willing and able to provide written informed consent; be a partner, parent, sibling, or child of the individual with advanced cancer; reside with the individual with advanced cancer and be responsible for most of the individual with advanced cancer's care Sample size: 136; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: IVR system phone calls made once daily, each taking about 3‐5 min to complete Arm b: standard care |
| Outcomes | Better symptom management and improved quality of life for participants |
| Starting date | January 2008 |
| Contact information | Sriram Yennurajalingam, MD, MD Anderson Cancer Center |
| Notes | ClinicalTrials.gov identifier: NCT00625638 |
NCT00876330.
| Trial name or title | Improving antihypertensive and lipid‐lowering therapy (CERT2) |
| Methods |
Aims: to evaluate the impact of electronic health record clinical decision support and automated telephone outreach on antihypertensive and lipid‐lowering therapy in ambulatory care Study design: RCT; recruitment:* Study duration: ongoing; study type: management; subtype: cardiovascular disease |
| Participants |
Inclusion criteria: Medical doctors, nurse practitioners, physician assistants, or doctors of osteopathic medicine practicing in primary care or medical subspecialties and using eClinical Works EHR .Patients of eligible physicians who have hypertension or hyperlipidaemia Sample size: 6000; mean age: * sex: * ethnicity: * Country:USA |
| Interventions |
Arm a: hypertension and hyperlipidemia intervention with automated telephone outreach Arm b: hypertension and hyperlipidemia intervention using clinical decision support |
| Outcomes | The main outcome measure will be the proportion of participants at treatment goal |
| Starting date | May 2009 |
| Contact information | Steven Simon, VA Boston Healthcare System |
| Notes | ClinicalTrials.gov identifier: NCT00876330 |
NCT01079533.
| Trial name or title | Initiation of colon cancer screening in veterans or 'Start Screening Now' (SSN) |
| Methods |
Aims: to increase first time colorectal cancer screening colorectal cancer among veterans aged ≥ 50 Study design: factorial RCT; recruitment: * Study duration: ongoing; study type: prevention; subtype: screening |
| Participants |
Inclusion criteria: veterans aged 50‐64. Sample size: 1504; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: in step 1, investigators will evaluate a theory‐based minimal cue delivered by a letter, telephone call, or automated telephone call. People who do not complete colorectal cancer screening in step 1 will be randomised to step 2 using principles of motivational interviewing. Step 2 also will determine whether an automated approach, telephone‐linked communication (TLC), is as effective as a telephone counsellor in promoting initiation of colorectal cancer screening. Steps 1 and 2 together will address the important issue of the 'dose' needed to encourage completion of colorectal cancer screening. Arm b: a survey‐only control arm will be compared to the experimental arm to determine whether the 3 different delivery channels are equally efficacious and cost‐effective |
| Outcomes | Colorectal cancer screening |
| Starting date | July 2008 |
| Contact information | Sally Vernon, the University of Texas Health Science Center, Houston |
| Notes | ClinicalTrials.gov identifier: NCT01079533 |
NCT01120704.
| Trial name or title | Evaluation of treatments to improve smoking cessation medication adherence |
| Methods |
Aims: to identify treatments that improve the use of cessation medications and to determine whether an increase in medication use results in increased cessation success. Study design: factorial RCT; recruitment: * Study duration: ongoing; study type: management; subtype: smoking |
| Participants |
Inclusion criteria: ≥ 18 years of age or older; report smoking ≥ 5 cigarettes/day for the previous 6 months; able to read and write English; agree to attend visits, to respond to coaching calls, and to respond to IVR phone prompts; plans to remain in the intervention catchment area for at least 12 months; currently interested in quitting smoking (defined as would like to try to quit in the next 30 days). Sample size: 544; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: automated adherence prompting phone calls. Participants in this condition will receive fully automated prompts with messages designed to encourage participants to take their medication. Adherence prompting calls will occur twice in the first week of the quit attempt, and then once a week in weeks 2, 3, 4, 5, and 7. Those in the 26‐Week medication condition who are assigned to the active adherence prompting calls intervention, will receive one prompting call a week during Weeks 11, 15, 19 and 23. Arm b: electronic medication monitoring device (the helping hand) + feedback Arm c: cognitive medication adherence counselling (CAM) Arm d: intensive maintenance counselling Arm e: long‐term combination nicotine replacement therapy (patch + gum) Arm f: short‐term combination nicotine replacement therapy (patch + gum) |
| Outcomes | Latency to relapse |
| Starting date | June 2010 |
| Contact information | Michael C Fiore, MD, MPH, MBA, University of Wisconsin School of Medicine and Public Health, Center for Tobacco Research and Intervention |
| Notes | ClinicalTrials.gov identifier: NCT01120704 |
NCT01125371.
| Trial name or title | Computerized brief alcohol intervention (BI) for binge drinking HIV at‐risk and infected women |
| Methods |
Aims: to examine two novel brief alcohol intervention delivery strategies specifically tailored to be culturally/socially relevant to this minority population Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: alcohol use |
| Participants |
Inclusion criteria: 18 years of age or older; HIV infected or HIV negative and attending the Baltimore City Health Department sexually transmitted infection clinic for STI‐related services; consumes an average of 8 or more drinks per week OR has had two binge drinking episodes (4 drinks/occasion) in the last 3 months; sexually active; cognitively able to understand proposed research design (10 min screening, followed by random assignment to one of three study groups (if individual fulfills criteria for RCT enrollment); able to speak and understand English; able and willing to receive text messages Sample size: 450; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: computerised brief alcohol intervention + IVR booster calls: clinic‐based computerised brief alcohol intervention (delivered once) followed by 3 booster phone calls using interactive voice response technology + text messages Arm b: computerised brief alcohol intervention: clinic‐based computer‐delivered brief alcohol intervention delivered one time Arm c: attention control |
| Outcomes | Reduction in alcohol use |
| Starting date | Geetanjali Chander, MD |
| Contact information | Geetanjali Chander, MD, Johns Hopkins University |
| Notes | ClinicalTrials.gov identifier: NCT01125371 |
NCT01131143.
| Trial name or title | Trial of provider‐to‐patient interactive voice response (IVR) calls to improve weight management in community health centers (CHCs) |
| Methods |
Aims: to test the effect of provider to patient interactive voice response (IVR) calls in local Community Health Centers within a weight management program. Study design: RCT; recruitment: * Study duration: ongoing; study type: prevention; subtype: weight management |
| Participants |
Inclusion criteria: adult patients who have screened positive for overweight or obesity Sample size: 1228; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: a phone call with the pre‐recorded doctor's voice will be made to their patients who have been pre‐screened for obesity before the participant's appointments, prompting the participants to ask about physical activity, nutrition, and weight loss. Arm b: a phone call with a pre‐recorded neutral voice will be made to the doctor's patients who have been prescreened for obesity before their patient's appointments. The call will prompt them to ask their doctor about physical activity, nutrition, and weight loss. |
| Outcomes | Weight loss |
| Starting date | June 2009 |
| Contact information | Daniel O Clark, PhD, Indiana School of Medicine |
| Notes | ClinicalTrials.gov identifier: NCT01131143 |
NCT01188135.
| Trial name or title | Antidepressant adherence via telephonic interactive voice recognition (IVR) |
| Methods |
Aims: to carry out a trial of a low‐cost, IT‐enabled antidepressants adherence program, specifically a direct‐to‐patient, automated telephone interactive voice recognition (IVR) intervention to boost patient antidepressants persistence Study design: RCT; recruitment: secondary care (*) Study duration: ongoing; study type: management; subtype: mental health |
| Participants |
Inclusion criteria: Kaiser Permanente NW Region health plan members aged 21‐75 and be members for at least 6 months prior to the initial antidepressive medications dispense; with an EMR chart diagnosis or presenting complaint of a unipolar mood diagnosis, anxiety disorder, or any subclinical or 'not otherwise categorised' (NOC) variant of these. Sample size: 6000; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: no contact control arm Arm b: usual care (UC) control condition Arm c: UC plus the IVR automated telephone programme Arm d: UC plus the IVR automated telephone programme plus receipt of psycho‐education materials about antidepression medication use |
| Outcomes | Medication adherence (based on prescription refill data); cost‐effectiveness |
| Starting date | August 23, 2010 |
| Contact information | Clarke, Gregory; Kaiser Foundation Research Institute, Oakland, CA, United States |
| Notes | ClinicalTrials.gov identifier: NCT01188135 |
NCT01199666.
| Trial name or title | Text message reminder‐recalls for early childhood vaccination |
| Methods |
Aims: to demonstrate the effectiveness of tailored text message appointment and immunisation reminders linked to a well‐established and functional immunisation registry to increase coverage rates and timeliness of the sentinel vaccines of measles, mumps and rubella and hepatitis A. Study design: RCT; recruitment:* Study duration: ongoing; study type: prevention; subtype: immunisations |
| Participants |
Inclusion criteria: parents of child aged 9‐25 months; child with ≥ 1 visit to one of the participating clinical sites in the previous 12 months; parental cell phone number recorded in the registration system Sample size: 2586; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: automated phone call appointment reminder hep A: recall letter, automated phone call appointment reminder Arm b: text message reminders |
| Outcomes | Immunisation uptake (receipt of measles, mumps and rubella) |
| Starting date | June 2011 |
| Contact information | Melissa Stockwell, MD, MPH, Columbia University |
| Notes | ClinicalTrials.gov identifier: NCT01199666 |
NCT01229722.
| Trial name or title | ARemind: a personalized system to remind for adherence |
| Methods |
Aims: to continue and complete development of a cellular phone‐based system that assists patients with their medication adherence Study design: RCT; recruitment: * Study duration: ongoing study type: management; subtype: adherence to medications/laboratory tests |
| Participants |
Inclusion criteria: stable ART (no change of ART for 3 months), ≥ 18 years of age self‐report adherence < 85% Sample size: 70; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: aRemind will personalise reminder messages based on adherence levels and facilitate patient phone calls with social workers/adherence counsellors when appropriate. It will also consist of a text‐messaging, IVR, or phone‐based pill count remote adherence assessment module Arm b: beepers are handheld portable devices which can be attached to a belt. At regular intervals corresponding to the participant's preferred reminder time, they buzz for a few minutes or until the participant presses a button to stop the buzzing. |
| Outcomes | Adherence to anti‐retroviral therapy |
| Starting date | October 2011 |
| Contact information | Vikram Sheel Kumar, Dimagi Inc. |
| Notes | ClinicalTrials.gov identifier: NCT01229722 |
NCT01260207.
| Trial name or title | Using IVR to maintain ACS patients on best practice guidelines (IVR‐ACS BPG) |
| Methods |
Aims: to determine whether IVR technology can be used to bring postdischarge care for acute coronary syndrome (ACS) closer to best practice guidelines (BPGs) Study design: RCT; recruitment:* Study duration: ongoing; study type: management; subtype: adherence to medications/laboratory tests |
| Participants |
Inclusion criteria: patients discharged from London Health Science Centre with ACS (acute myocardial infarction, STEMI, NSTEMI or unstable angina); patients who have a land line telephone service at home; patients who speak English Sample size: *; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: participants in this arm will receive IVR follow‐up telephone calls at 1, 3, 6, 9, and 12 months postdischarge consisting of predetermined questions related to medication management, smoking cessation, diet, exercise and education as recommended by the ACC/AHA BPG for ACS. Upon completion of the IVR follow‐up, all participants will be called by a member of the clinical research staff and asked to complete a follow‐up survey. Arm b: usual care |
| Outcomes | Adherence with best practice guidelines |
| Starting date | January 2010 |
| Contact information | Neville Suskin, Lawson Health Research Institute |
| Notes | ClinicalTrials.gov identifier: NCT01260207 |
NCT01484717.
| Trial name or title | Interactive voice response technology to mobilize contingency management for smoking cessation |
| Methods |
Aims: to examine the effectiveness of using interactive voice response technology (IVR) to implement contingency management in smokers who want to quit Study design: randomised controlled trial; recruitment: * Study duration: ongoing study type: management; subtype: smoking |
| Participants |
Inclusion criteria: regular cigarette smoker, age ≥ 18, mailing address and valid photo I.D, wants transdermal nicotine Sample size: 90; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: contingency management for abstinence from cigarettes. Telephone counselling and nicotine patch plus contingency management (contingency management for smoking abstinence + transdermal nicotine + telephone counselling) Arm b: transdermal nicotine+ telephone counselling |
| Outcomes | Longest duration of abstinence |
| Starting date | January 2012 |
| Contact information | Sheila Alessi, PhD, University of Connecticut Health Center |
| Notes | ClinicalTrials.gov Identifier: NCT01484717 |
NCT01530958.
| Trial name or title | Kidney awareness registry and education (KARE) |
| Methods |
Aims: to evaluate the feasibility and acceptability of two different interventions aimed at improving health outcomes among patients with chronic kidney disease, who are at high risk of chronic kidney disease progression Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: hypertension |
| Participants |
Inclusion criteria: patients with chronic kidney disease (defined as estimated Glomerular Filtration Rate < 60 mL/min/1.73m2 or proteinuria consistently over 3 months) who speak English, Spanish or Cantonese and have a primary care provider Sample size: 100; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: automated telephone self‐management (ATSM) + health coach. Participants with chronic kidney disease will participate in an ATSM programme, which blends automated phone calls with live targeted call‐backs from a health coach. Participants will receive bi‐weekly automated calls for 52 weeks in their native language, consisting of pre‐recorded queries pertaining to the disease management, preventive services, and lifestyle changes. Participants will interact with the system using a touch‐tone keypad; out‐of‐range values or invalid responses will prompt a live call‐back within 24‐48 h by a health coach. Arm b: usual care |
| Outcomes | Change in blood pressure |
| Starting date | April 2013 |
| Contact information | Neil Powe, MD, University of California, San Francisco |
| Notes | ClinicalTrials.gov identifier: NCT01530958 |
NCT01609842.
| Trial name or title | Hybrid effectiveness‐implementation study to improve clopidogrel adherence |
| Methods |
Aims: to test the effectiveness of a successfully piloted, evidence‐based, multifaceted intervention to improve patient adherence to clopidogrel following percutaneous coronary intervention (PCI) Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: adherence to medications/laboratory tests |
| Participants |
Inclusion criteria: all patients undergoing PCI with either a bare‐metal (BMS) or drug‐eluting stent (DES) and are prescribed clopidogrel regardless of the intended treatment duration; other potential antiplatelet medications (thienopyridines) used following PCI to accommodate changes in practice (e.g. prasugrel, ticagrelor, or ticlopidine); all patients undergoing PCI and receiving clopidogrel at the randomised sites, regardless of gender, ethnicity or race. Based on data from the national Clinical Assessment, Reporting and Tracking (CART) system, we anticipate ˜23% minorities (African American 16.8%, Hispanic 4.4%, Asian/American Indian 1.4%) and 3.1% women will be included in the study. Sample size: 2500; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: phone reminders and pharmacist. An alerted inpatient pharmacist or a designated study team member will bring the clopidogrel medication to the participant who has received a coronary stent. The participant will return home and receive IVR refill reminder calls. Arm b: usual care |
| Outcomes | Medication adherence |
| Starting date | January 2014 |
| Contact information | Michael Ho, MD PhD, VA Eastern Colorado Health Care System, Denver, CO |
| Notes | ClinicalTrials.gov identifier: NCT01609842 |
NCT01672385.
| Trial name or title | Improving transition outcomes through accessible health IT and caregiver support |
| Methods |
Aims: to determine the extent to which the CarePartner model for supporting effective transitions from hospital to home improves outcomes of care, including lower readmission rates, emergency department visits, and improved patient functional status. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: cardiovascular disease |
| Participants |
Inclusion criteria: being discharged from study site with any diagnoses that indicate a chronic condition with a high risk of short‐term readmission, for example: stroke, heart failure, coronary artery disease, cardiac arrhythmias, COPD, peripheral vascular disease, deep venous thrombosis, pulmonary embolism, pneumonia, diabetes, urinary tract infection, cellulitis, gastroenteritis, fevers, and other infections; at least 50 years of age Sample size: 1692; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: telemonitoring plus self‐management support; automated telephone calls that ask about their health and self‐care along with tailored health‐related feedback. The participant's CarePartner receives health update reports about the participant and how they can help via e‐mail. Urgent health problems are reported to the participant's health care team via fax or e‐mail. Arm b: usual care |
| Outcomes | Short‐term readmission rates, emergency department visits, and participants' functional status |
| Starting date | August 2012 |
| Contact information | John Piette, University of Michigan |
| Notes | ClinicalTrials.gov identifier: NCT01672385 |
NCT01672398.
| Trial name or title | Trial of the CarePartner program for improving the quality of transition support |
| Methods |
Aims: to determine the extent to which the CarePartner model for supporting effective transitions from hospital to home improves outcomes of care, including short‐term readmission rates, emergency department visits, and patients' functional status. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: cardiovascular disease |
| Participants |
Inclusion criteria: being discharged from study site with any diagnoses that indicate a chronic condition with a high risk of short‐term readmission, for example: stroke, heart failure, coronary artery disease, cardiac arrhythmias, COPD, peripheral vascular disease, deep venous thrombosis, pulmonary embolism, pneumonia, diabetes, urinary tract infection, cellulitis, gastroenteritis, fevers, and other infections; at least 21 years of age Sample size: 844; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: telemonitoring plus self‐management support; automated telephone calls that ask about their health and self‐care along with tailored health‐related feedback. The participant's CarePartner receives health update reports about the participant and how they can help via e‐mail. Urgent health problems are reported to the participant's health care team via fax or e‐mail. Arm b: usual care |
| Outcomes | Short‐term readmission rates, emergency department visits, and patients' functional status |
| Starting date | August 2012 |
| Contact information | John Piette, University of Michigan |
| Notes | ClinicalTrials.gov identifier: NCT01672398 |
NCT01700894.
| Trial name or title | Women's Walking Program (WWP3) |
| Methods |
Aims: to compare the effects at 24 weeks and 48 weeks of the WWP plus three telephone conditions on increasing adherence to lifestyle physical activity over baseline physical activity. Study design: RCT; recruitment: * Study duration: ongoing; study type: prevention; subtype: physical activity |
| Participants |
Inclusion criteria: Afican American women; sedentary, defined as no participation in regular planned (3 or more times a week) moderate (e.g. walking) or vigorous (e.g. jogging, speed walking) in the past 6 months; aged 40‐65 years; able to commit to attending the study group visits and have a telephone; without disabilities that would prevent regular participation in physical activity such as walking as determined by the physical activity readiness questionnaire (PAR‐Q) and baseline screening. Sample size: 288; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: walking programme + motivational interviewing calls Arm b: walking programme + automated calls Arm c: walking programme |
| Outcomes | Adherence to physical activity prescription |
| Starting date | March 2010 |
| Contact information | JoEllen Wilbur, PhD, APN, FAAN, Rush University Medical Center |
| Notes | ClinicalTrials.gov identifier: NCT01700894 |
NCT01701791.
| Trial name or title | Telemedicine for depression in primary care |
| Methods |
Aims: to evaluate the feasibility and effectiveness of a care support programme developed in conjunction with the PC‐based assessment for patients suffering from depression, as based on two main objectives: to support GP decisions with treatment algorithms and improve the quality of GP and mental health service collaboration; and to improve patient adherence and treatment adherence by using appropriate telecommunication tools and technologically advanced tools to conduct systematic routine assessment. Study design: cluster randomised trial; recruitment: * Study duration: ongoing; study type: management; subtype: adherence to medication/laboratory tests |
| Participants |
Inclusion criteria: patients aged 18‐65 years; PHQ‐9 score of ≥ 14 at baseline; IDS‐SR score of ≥ 26 at baseline; no filling of antidepressant medication; prescription for 270 prior days; illiteracy or the lack of working telephone to receive reminders. Sample size: 400; mean age: * sex: * ethnicity: * Country: Italy |
| Interventions |
Arm a: GPs will use a CDSS with treatment algorithms, supervision from a consultant psychiatrist, and dispatch to participants of reminders via mobile texting or automatic mobile (or landline) phone calls to improve adherence to the treatment prescribed Arm b: treatment as usual |
| Outcomes | Proportion of participants reaching remission |
| Starting date | January 2013 |
| Contact information | Matteo Balestrieri, MD, IRCCS Centro San Giovanni di Dio Fatebenefratelli (gdegirolamo@fatebenefratelli.it) |
| Notes | ClinicalTrials.gov Identifier: NCT01701791 |
NCT01706380.
| Trial name or title | 3M Study ‐ Maria Malmö mobile telephone study |
| Methods |
Aims: to examine the effect on treatment retention of a mobile telephone follow‐up technique (interactive voice response), with or without personal feedback. Study design: RCT; recruitment: outpatient clinics Study duration: ongoing; study type: management; subtype: substance use |
| Participants |
Inclusion criteria: patient applying for substance use disorder treatment at outpatient facility Maria Malmö, Malmö, Sweden, who are < 25 years old and who provide written informed consent to participate in the study Sample size: 120; mean age: * sex: * ethnicity: * Country: Sweden |
| Interventions |
Arm a: IVR with personal feedback; twice weekly for 3 months with respect to symptoms and substance use, in both arms. This group also receives a personalised and automated feedback describing whether the symptom status of the participant is better, worse or equal, compared to the preceding follow‐up. Arm b: IVR without personal feedback |
| Outcomes | Retention in substance use disorder treatment at 3 months |
| Starting date | October 8, 2012 |
| Contact information | Anders C Håkansson, Region Skane |
| Notes | ClinicalTrials.gov identifier: NCT01706380 |
NCT01737073; NCT02508285.
| Trial name or title | Comprehensive opioid management in patient aligned care teams (COMPACT) |
| Methods |
Aims: to test the effectiveness of COMPACT for improving pain‐relevant outcomes including physical functioning and pain intensity; to determine whether opioid monitoring promotes guideline concordant care; and to examine key components of the intervention process to inform future implementation. Study design: factorial RCT; recruitment: * Study duration: ongoing; study type: management; subtype: pain |
| Participants |
Inclusion criteria: presence of at least moderate non‐cancer, non‐headache pain (i.e. pain scores of ≥ 4 as measured by the Numeric Rating Scale) for a period of ≥ 3 months; receipt of chronic opioid therapy as defined by ≥ 90 continuous days out of any 104 day period in the prior 12 months; ability to participate safely in the walking portion of the intervention as evidenced by ability to walk at least one block; availability of a landline or cellular telephone Sample size: 308; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: the IVR system will be used to deliver a 12‐week course of opioid education and self‐management support followed by 24 weeks of skill maintenance training. Self‐management skills will include walking, stretching, pleasant activities, pacing, relaxation, cognitive restructuring, opioid education and sleep. Arm b: monitoring will include: proactive, IVR‐collected monthly information regarding opioid risk; and based on participants' IVR reports, automated output of electronic medical record documentation regarding participants' status for use by the primary care team |
| Outcomes | Pain‐related physical functioning; 7‐item interference sub‐scale of the brief pain inventory; providers' concordance with chronic opioid treatment practice guidelines |
| Starting date | October 2015 |
| Contact information | Alicia A Heapy, PhD, VA Connecticut Healthcare System |
| Notes | ClinicalTrials.gov identifier: NCT02508285; and NCT01737073 |
NCT01756001.
| Trial name or title | GlowCaps adherence randomized control trial |
| Methods |
Aims: to study simple "behavioral economics" interventions that rely on consumer engagement to overcome cognitive and motivational barriers to medication adherence. Study design: RCT; recruitment: * Study duration: ongoing study type: management; subtype: adherence to medications/laboratory tests |
| Participants |
Inclusion criteria: patients diagnosed with chronic disease aged 16‐64 Sample size: 600; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: incentives and reminders (email reminders, text message reminders, or daily phone call reminders) Arm b: reminders only Arm c: no intervention |
| Outcomes | Medication adherence (number of doses taken) |
| Starting date | February 2015 |
| Contact information | Judd Kessler, University of Pennsylvania |
| Notes | ClinicalTrials.gov identifier: NCT01756001 |
NCT01778751.
| Trial name or title | Advanced comprehensive diabetes care for veterans with poorly‐controlled diabetes (ACDC) |
| Methods |
Aims: to determine whether home telehealth‐based implementation of an evidence‐based intervention targeting veterans with persistent poorly controlled diabetes (PPDM) can improve glycated haemoglobin, patient self‐management, and comorbid depressive symptoms in this high‐risk, high‐cost population. Study design: RCT; recruitment: * Study duration: ongoing study type: management; subtype: diabetes |
| Participants |
Inclusion criteria: veterans with type 2 diabetes managed for > 1 year at an eligible site (Durham, Raleigh, Greenville, or Morehead City) will be eligible for enrolment. Veterans with PPDM (defined as the presence of at least 2 glycated haemoglobin values of > 9.0% during the past year with no readings of < 9.0% despite ongoing medical care) by reviewing electronic medical records and soliciting referrals from primary physicians. Sample size: 50; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: health technology (HT) programme, provided with standard tele‐monitoring equipment by HT nursing staff (current HT practice at DVAMC is use of the Health Buddy 3 device for participants with landline phones and the Cardiocom IVR system for participants with cell phones), and will receive the study intervention for 6 months. Veterans without depressive symptoms on baseline PHQ‐9 assessment (PHQ‐9 < 10) will not initially be entered into the depression symptom management component of the intervention, but will be monitored for new symptoms throughout the intervention. Arm b: diabetes educational materials and management per their primary provider |
| Outcomes | Diabetes control; change in glycated haemoglobin from baseline to 6 months |
| Starting date | December 2013 |
| Contact information | Matthew Crowley, MD, VA Office of Research and Development |
| Notes | ClinicalTrials.gov identifier: NCT01778751 |
NCT01794988.
| Trial name or title | Can therapy alter CNS processing of chronic pain? A longitudinal study |
| Methods |
Aims: to investigate whether a psycho‐therapeutic approach, group CBT + relapse prevention programme, Therapeutic Interactive Voice Response (TIVR), modifies the dysfunctional sensory, emotional, and cognitive neural circuitry associated with chronic pain Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: pain |
| Participants |
Inclusion criteria: at least 12 months of muscular‐skeletal, non‐neuropathic pain Sample size: 120; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: 4 months of TIVR Arm b: group CBT Arm c: pain education Arm d: no intervention |
| Outcomes | Pain |
| Starting date | July 2010 |
| Contact information | Magdalena Naylor, MD, PhD, University of Vermont |
| Notes | ClinicalTrials.gov identifier: NCT01794988 |
NCT01852656.
| Trial name or title | Effectiveness of influenza vaccine reminder systems |
| Methods |
Aims: to test the effectiveness and cost of different methods of reminders for annual influenza immunisation among adults with asthma and chronic obstructive pulmonary disease Study design: RCT; recruitment: * Study duration: ongoing; study type: prevention; subtype: immunisations |
| Participants |
Inclusion criteria: aged 19‐64 years; enrolled in Kaiser Permanente Colorado health plan; diagnosis of asthma and/or COPD Sample size: 12,255; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: IVR only reminder group Arm b: postcard and IVR reminder group Arm c: postcard only reminder group |
| Outcomes | Receipt of influenza vaccine |
| Starting date | September 2012 |
| Contact information | Matthew F. Daley, MD, Kaiser Permanente |
| Notes | ClinicalTrials.gov identifier: NCT01852656 |
NCT01900561.
| Trial name or title | Optimizing veteran‐centered prostate cancer survivorship care |
| Methods |
Aims: to conduct an RCT to compare a personally tailored automated telephone symptom management intervention for improving symptoms and symptom self‐management versus usual care Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: cancer |
| Participants |
Inclusion criteria: veteran patient at one of the three study sites, history of treatment for prostate cancer treated by surgery, radiation or androgen deprivation therapy between 1‐5 years prior to identification Sample size: 650; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: the intervention will consist of two components: automated telephone monitoring of prostate cancer survivor symptoms and goals for symptom reduction, based on a patient empowerment approach, and personally tailored newsletters that incorporate elements of CBT to improve survivors' identification with the material, confidence/self‐efficacy in symptom management, and to reduce common cognitive distortions related to successful implementation of behaviour change. Intervention‐group participants will receive 4 automated assessment and self‐management support calls over a 3‐month period (at baseline, 1 month, 2 months, 3 months) Arm b: enhanced usual care |
| Outcomes | The Expanded Prostate Cancer Index |
| Starting date | April 2015 |
| Contact information | Sarah T Hawley, PhD MPH BA, VA Office of Research and Development |
| Notes | ClinicalTrials.gov identifier: NCT01900561 |
NCT01940016.
| Trial name or title | Communication & peer support effects on physical activity in overweight postmenopausal women (BePHIT) |
| Methods |
Aims: to design, develop and test the feasibility of implementing a physical activity intervention using tailored communication and IVR technology Study design: RCT; recruitment: * Study duration: ongoing; study type: prevention; subtype: weight management |
| Participants |
Inclusion criteria: present a letter/documentation from a primary physician stating that they can participate in a physical activity programme that will require walking up to 10,000 steps per day, have a BMI of 25‐40 kg/m2 (inclusive), be postmenopausal, defined as no period for 12 months if over age 55, or no period for 12 months; also, women who have had their ovaries removed will be considered as postmenopausal, willing to participate in a wellness programme that lasts 12 weeks and involves walking for at least 30 min a day on most days, access to a cell phone during the 12‐week intervention, functional knowledge of English Sample size: 71; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: 12‐week physical activity intervention (walking programme) and receive health mail messages via IVR system and from a health coach. Participants in this arm of the study interacted with the IVR system and had the option of interacting with the health coach. Arm b: 12‐week physical activity intervention (walking programme) and receive health mail messages via IVR system. Participants in this arm of the study only interacted with the IVR system. |
| Outcomes | Change in time taken to complete a one mile walk |
| Starting date | April 2007 |
| Contact information | Electra Paskett, Ohio State University Comprehensive Cancer Center |
| Notes | ClinicalTrials.gov identifier: NCT01940016 |
NCT01953653.
| Trial name or title | Feasibility of using a structured daily diary |
| Methods |
Aims: to implement a 66‐day structured daily diary with 90 HIV‐positive young men who have sex with men (MSM) to explore relationships among daily mood, stressful events, social support, substance use, sexual behavior, and adherence to ART among youth who are currently prescribed to take medication Study design: randomised cross‐over trial; recruitment: * Study duration: ongoing; study type: prevention; subtype: HIV |
| Participants |
Inclusion criteria: receives services at one of the selected Adolescent Medicine Trial Unit (AMTU) sites; HIV‐1 infection as documented in the participant's medical record by at least one of the following criteria: reactive HIV screening test result with an antibody‐based, FDA‐licensed assay followed by a positive supplemental assay (e.g. HIV‐1 Western Blot, HIV‐1 indirect immunofluorescence); positive HIV‐1 DNA polymerase chain reaction (PCR) assay; plasma HIV‐1 quantitative RNA assay > 1000 copies/mL; or positive plasma HIV‐1 RNA qualitative assay; aged 16‐24 years, inclusive, at the time of screening; born biologically men and self‐identifies as man at the time of screening; HIV‐infected through sexual behavior; at least one self‐reported sexual encounter with another man involving oral or anal sex in the past 12 months prior to screening; at least one self‐reported episode of unprotected vaginal or anal intercourse within the past 90 days prior to screening and/or substance use, defined as at least 1 occasion in which ≥ 4 alcoholic beverages were consumed and/or ≥ 2 occasions of illicit drug use, in the past 90 days, as assessed by the assessment of substance use and sexual behavior questionnaire; has active cell phone service; is able to access his cell phone 7 days a week between 6:00 pm and 6:00 am the next morning; and is willing and able to use approximately 10 min of talk time and receive 2 text messages per day; consistent Internet access 7 days a week between 6:00 pm and 6:00 am the next morning; ability to understand, read, and speak English; ability to read at a fifth grade level, as assessed by the rapid estimate of adolescent literacy in medicine (REALM)‐TEEN; and willingness to provide signed informed consent for study participation. Sample size: 67; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: IVR system Arm b: interactive web response (IWR) system |
| Outcomes | Number of participants who complete the 66‐day structured daily diary; participant responses to how diary can provide personalised feedback on triggers to risk behaviors |
| Starting date | February 2013 |
| Contact information | Patrick Wilson, PhD, Columbia University |
| Notes | ClinicalTrials.gov identifier: NCT01953653 |
NCT01958359.
| Trial name or title | Screening and brief intervention via IVR for problematic use of alcohol: a randomized controlled trial |
| Methods |
Aims: the study evaluates the efficacy of two interactive voice recognition (IVR) interventions, short IVR and therapeutic IVR Study design: RCT; recruitment: * Study duration: ongoing Study type: management; Sub ‐ type: alcohol |
| Participants |
Inclusion criteria: alcohol Use Disorders Identification Test (AUDIT) >7 for men or AUDIT >5 for women. Sample size: 260; mean age: * sex: * ethnicity: * Country: Sweden |
| Interventions |
Arm a: therapeutic IVR‐based conversation offering a menu of exercises and vignettes Arm b: IVR‐based alcohol diary with feedback Arm c: untreated control group |
| Outcomes | Change in total AUDIT score, as a summarised measure of alcohol use (including alcohol consumption and alcohol‐related problems |
| Starting date | February 2011 |
| Contact information | Anne H Berman, Karolinska Institutet |
| Notes | ClinicalTrials.gov Identifier: NCT01958359 |
NCT01973946.
| Trial name or title | Cancer symptom monitoring telephone system with nurse practitioner (NP) follow up |
| Methods |
Aims: to test a daily telephone‐based automated symptom monitoring and response system to track and further treat unrelieved symptoms for patients living at home during chemotherapy treatment as compared with usual care which consists of participants calling their oncology provider for symptom concerns. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: cancer |
| Participants |
Inclusion criteria: adult (age ≥ 18); histological diagnosis of cancer; life expectancy of at least 3 months and cognitively able to participate; beginning a new course of chemotherapy that is planned for a minimum of 3 cycles; care is under the direction of one of the 8 designated provider teams; English‐speaking; has access to a telephone on a daily basis and is able to use the phone unassisted as verified by the study staff during participant orientation Sample size: 358; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: participants call the automated monitoring system daily to report presence, severity, and distress on 11 symptoms. The system provided automated self‐care coaching based on the symptoms reported and automatically generated alerts to the study NP if symptoms exceeded preset thresholds. 2 thresholds were set: a simple alert when severity or distress was ≥ 4 on a 10‐point scale and trend alerts based on a pattern of moderate severity over several days. The alerts went into a case management site. The study NP logged into the system daily and responded to the alerts within 24 h by calling participants to further assess the symptoms and to intensify symptom treatment using evidence based guidelines. Arm b: control group will receive usual care (via IVR). |
| Outcomes | Medical encounters telephone interview; symptom‐related interference with daily activities; SF‐36 functional status; work interference; work limitations questionnaire |
| Starting date | September 2007 |
| Contact information | Kathi.Mooney@nurs.utah.edu |
| Notes | ClinicalTrials.gov identifier: NCT01973946 |
NCT02001129.
| Trial name or title | Improving follow‐up adherence in a primary eye care setting |
| Methods |
Aims: to examine the effectiveness of three different ways of helping patients attend their recommended eye care appointments. Study design: RCT; recruitment: * Study duration: ongoing; study type: either; subtype: appointment reminders |
| Participants |
Inclusion criteria: aged ≥ 18 years; primary eye care patients who were recommended for a 6‐, 12‐, or 24‐month follow‐up appointment in September 2013 to November 2013; access to a telephone Sample size: 1000; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: automated telephone call Arm b: personalised telephone call Arm c: usual care |
| Outcomes | Appointment adherence |
| Starting date | August 2013 |
| Contact information | Julia Haller, Wills Eye |
| Notes | ClinicalTrials.gov identifier: NCT02001129 |
NCT02043184.
| Trial name or title | Improving adherence to oral cancer agents and self care of symptoms using an IVR |
| Methods |
Aims: to test and compare 2 strategies for improving adherence to their oral cancer medication prescriptions to standard care. Study design: factorial RCT; recruitment: * Study duration: ongoing; study type: management; subtype: adherence to medications/laboratory tests |
| Participants |
Inclusion criteria: ≥ 21 years, newly prescribed one of the designated oral cancer medications for treatment of cancer, ECOG score of 0,1, or 2, or Karnofsky score of 50 or higher, patient of one of the participating National Cancer Institute comprehensive cancer centres, able to speak, read, and understand English, able and willing to receive phone calls Sample size: 274; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: standard care for 12 weeks Arm b: standard care for 8 weeks + daily IVR for 4 weeks Arm c: daily IVR 8 weeks Arm d: daily IVR 4 weeks, every other day IVR 4 weeks |
| Outcomes | Medication adherence using pill count and self report |
| Starting date | March 2013 |
| Contact information | Barbara Given, Michigan State University (Barb.Given@hc.msu.edu) |
| Notes | ClinicalTrials.gov identifier: NCT02043184 |
NCT02056002.
| Trial name or title | Peer‐driven intervention for sleep apnea (PCORI) |
| Methods |
Aims: to test whether participants in the peer‐driven intervention with IVR (PDI‐IVR) group will experience a greater participant satisfaction (measured by Likert scale and PACIC) and perception of care coordination (measured by CPCQ) than participants in the usual care (control) group. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: OSAS |
| Participants |
Inclusion criteria: obstructive sleep apnea; 18‐85 years of age; availabilityaof cell or other reliable phone line (for subjects) Sample size: 257; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: IVR. Once a week for the first month followed by 4 phone conversations over the subsequent 2‐month period (8 scheduled telephone interactions) and as needed in the subsequent 3 months. There will be no more than 10 such 'as‐needed' phone calls in the latter 3 months between participant and peer‐buddy. Therefore, over the 6 months, there will not be in excess of 18 phone calls per subject assigned to peer‐buddy. Each phone conversation will last a maximum of 30 min. The PDI‐IVR system will be programmed to recognise the peer‐buddy's phones (cell or home) and be programmed to link this with the participant's phones (cell or home) and thereby protect the privacy of both participants Arm b: usual care |
| Outcomes | Patient rating of sleep‐specific services |
| Starting date | January 2014 |
| Contact information | Sairam Parthasarathy, MD, University of Arizona |
| Notes | ClinicalTrials.gov identifier: NCT02056002 |
NCT02118454.
| Trial name or title | Antiretroviral adherence and quality‐of‐life support for HIV+ patients in India with twice‐daily IVR calls with health and mental health messaging compared to weekly IVR survey only control condition: the mobile‐messaging adherence and support for health study, India. (MASHIndia) |
| Methods |
Aims: to test whether twice‐daily IVR calls made at the estimated times of patients' antiretroviral (ART) medication dosing and 3 reminder calls for monthly clinic appointments, will result in improvements in ART adherence, appointment attendance, health indicators (CD4 cell counts), coping skills, social support, depressive symptoms, and other quality of life indicators, compared to a control group receiving one IVR assessment call each week, over 6 months. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: adherence to medications/laboratory tests |
| Participants |
Inclusion criteria: age ≥ 18; HIV +; taking first‐line ART 6 months or longer; missed taking any ART dose in the previous 6 months Able to speak and understand Bengali, Hindi, or English; willing to receive health‐related IVR messages on mobile phones; able to provide informed consent. Phase 2A ‐ client at Mamata Care and Treatment Center (MCTC) or member of Mamata Network of Positive Women (MNPW), or peer referral of MCTC client or MNPW member; received a CD4 count result in the prior 2 months. Phase 2B ‐ patient at Calcutta School of Tropical Medicine ART Centre, or peer referral of a patient Sample size: 400; mean age: * sex: * ethnicity: * Country: India |
| Interventions |
Arm a: daily IVR calls intervention: consisting of 2 automated voice calls ('intervention messages') each day for 6 months, + 1 IVR assessment call (consisting of 4 questions) every week for 6 months Arm b: weekly IVR survey only control condition: consisting of standard care, + 1 IVR assessment call (consisting of 4 questions) every week for 6 months |
| Outcomes | Change in antiretroviral medication adherence measured by AIDS Clinical Trials Group (ACTG) self‐report measure |
| Starting date | April 2014 |
| Contact information | NA |
| Notes | ClinicalTrials.gov identifier: NCT02118454 |
NCT02124980.
| Trial name or title | Automated recovery line for medication assisted treatment |
| Methods |
Aims: to test the effectiveness of Recovery Line in substance abuse Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: addiction |
| Participants |
Inclusion criteria: ≥ 18 years old; currently receiving methadone maintenance treatment; illicit drug use in the past 14 days or a positive urine screen for any tested illicit drug Sample size: 60; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: Recovery Line plus usual care (RL + UC). Recovery Line is an automated computer‐based IVR system that provides CBT‐based modules. The RL + UC condition will include the customised therapeutic recommendations developed in Phase 1, and the contact reminders messages and time frame that maximised system use in Phase 2. Participants will receive an orientation, 24‐hour access, encouragement to use the system from clinic staff reminder, and technical assistance line for system problems. Participants will receive 12 weeks of system access. Arm b: usual care |
| Outcomes | Bi‐weekly urine screens negative for illicit drugs; self‐reported drug use; monthly days of self reported illicit drug abstinence |
| Starting date | October 2015 |
| Contact information | Brent A. Moore, Yale University |
| Notes | ClinicalTrials.gov identifier: NCT02124980 |
NCT02204956.
| Trial name or title | Smoking cessation following psychiatric hospitalisation |
| Methods |
Aims: to adapt an Extended Care (ExC) model to smokers with severe mental illness (SMI) engaged in a psychiatric hospitalisation and to conduct a randomised, pragmatic effectiveness trial designed to assess the benefit of this adapted ExC in real‐world practice Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: smoking |
| Participants |
Inclusion criteria: ≥ 18 years of age, current smoker (i.e.≥ 5 cigarettes/day when not hospitalised) Sample size: 422; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: extended care. A 40‐min, in‐hospital motivational counselling session about smoking cessation, 8 IVR phone calls over 90 days, including the possibility of a warm transfer to a telephone tobacco quit line and prescriptions for combination (2 types of) nicotine replacement medications. Arm b: brief education. A brief 5‐10 min education session with a hospital staff member, during which they will be provided with: a brochure describing the services of their local tobacco quit line and the services provided, and a brochure describing FDA‐approved smoking cessation medications, their usage and side effects. |
| Outcomes | Biochemically verified smoking abstinence via saliva cotinine |
| Starting date | April 2015 |
| Contact information | Nancy A Rigotti, MD Massachusetts General Hospital |
| Notes | ClinicalTrials.gov identifier: NCT02204956 |
NCT02240420.
| Trial name or title | Diabetes prevention among post‐partum women with history of gestational diabetes (Star‐Mama) |
| Methods |
Aims: to develop a patient‐tailored telephone‐base counselling intervention for young Latino women who are at high risk of diabetes. Study design: RCT; recruitment: * Study duration: ongoing study type: management; subtype: weight management |
| Participants |
Inclusion criteria: postpartum Latino women (English or Spanish speakers) with history of gestational diabetes; aged ≥ 18 Sample size: 180; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: 6 months weekly automated phone calls with queries and narratives about health habits. The participant's answers will be sent to a health coach who will follow up with the participant, and develop a plan with the participant to address her needs. Arm b: educational resource support |
| Outcomes | Weight loss |
| Starting date | December 2014 |
| Contact information | Margaret A Handley, MPH, PhD, University of California, San Francisco |
| Notes | ClinicalTrials.gov identifier: NCT02240420 |
NCT02266277.
| Trial name or title | System Alignment for VaccinE Delivery (SAVED): improving rates of influenza and pneumococcal vaccination through patient outreach, improved medical record accuracy and targeted physician alerts |
| Methods |
Aims: to improve the capture of vaccinations administered to Reliant Medical Group (RMG) patients in the community, hospitals and nursing facilities via system‐level health information exchange (HIE) Study design: factorial RCT; recruitment: by invitation Study duration: ongoing; study type: prevention; subtype: immunisations |
| Participants |
Inclusion criteria: RMG patients ≥ 18 years of age. Overdue for vaccination against influenza and/or not up‐to‐date on vaccination for pneumococcal vaccine per RMG EHR data. No documented allergy to the vaccination in question. Sample size: 30,000; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: e‐portal message with IVR call Arm b: e‐portal message with no IVR call Arm c: no e‐portal message with IVR call Arm d: no e‐portal message with no IVR call (control, e‐portal users) Arm e: IVR call Arm f: no IVR call (control, non e‐portal users) |
| Outcomes | Percent of intervention participants with self‐reported influenza vaccinations documented in electronic health record (EHR) |
| Starting date | October 10, 2014 |
| Contact information | Sarah Cutrona, University of Massachusetts, Worcester |
| Notes | ClinicalTrials.gov identifier: NCT02266277 |
NCT02328326.
| Trial name or title | Caring Others Increasing EngageMent in PACT (CO‐IMPACT) |
| Methods |
Aims: to compare 2 methods of increasing engagement in care and success in diabetes management, among patients with diabetes with high‐risk features, who also have family members involved in their care. Study design: RCT; recruitment:* Study duration: ongoing; study type: management; subtype: diabetes |
| Participants |
Inclusion criteria: provide signed and dated informed consent form; willing to comply with all study procedures and plan to be be available for the duration of the study; men or women, aged 30‐70 years old; plan to get most diabetes care at Ann Arbor VA over the subsequent 12 months; able to use telephone to respond to bi‐weekly automated IVR calls; be able to identify an adult family member or friend who is regularly involved in their health management or health care (involved with medications, managing sugars, coming to appointments, etc); have a diagnosis of diabetes and be at high‐risk for diabetes complications, defined as: a diagnosis of diabetes based on encounter diagnoses from 1 inpatient or 2 outpatient encounters (ICD9 code of 250.xx, 357.2x, 362.xx, 366.41, 962.3 or E932.3) OR a diabetes medication (at least one > 3 month prescription from VA drug classes HS501 (insulin) or HS502, other than metformin), have an assigned VAAAHS primary care provider and at least 2 visits to VAAHS primary care in the previous 12 months, poor glycaemic control (last glycated haemoglobin > 9% or glycated haemoglobin > 8% among participants < 55 years old) OR poor blood pressure control (last blood pressure 160/100 or mean 6 month blood pressure > 150/90); active AAVA primary care patients ‐ at least 2 visits in last 12 months (for patients) Sample size: 480; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: patient and supporter (dyad) receive one coaching session on action planning, communicating with providers, navigation skills and support skills; preparation by phone before patients primary care visits; after‐visit summaries by mail; and biweekly automated phone calls to prompt action on new patient health concerns Arm b: patient and their health supporter (dyad) will receive PACT care for high‐risk diabetes, which includes (at primary care team discretion): nurse care manager visits, diabetes education classes, chronic disease self‐management groups, telehealth, clinical pharmacist visits |
| Outcomes | Patient activation; cardiac event 5‐year risk score |
| Starting date | January 2016 |
| Contact information | VA Ann Arbor Healthcare System, Ann Arbor, MI, Ann‐Marie.Rosland@va.gov |
| Notes | ClinicalTrials.gov identifier: NCT02328326 |
NCT02360605.
| Trial name or title | Health literacy interventions to overcome disparities in colorectal cancer screening |
| Methods |
Aims: to compare the effectiveness of 2 distinct follow‐up strategies to promote colorectal cancer screening: a prevention coordinator (PC) approach vs an automated telephone reminder (ATR) system Study design: randomised controlled trial; recruitment: * Study duration: ongoing; study type: prevention; subtype: screening |
| Participants |
Inclusion criteria: a patient of the identified clinics, age 50‐75 (based on ACS guidelines) and can speak and understand English Sample size: 800; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: automated telephone reminder Arm b: prevention coordinator Arm c: health literacy appropriate education and demonstration |
| Outcomes | Colorectal cancer screening rate |
| Starting date | February 2015 |
| Contact information | Connie L Arnold, PhD (carnol@lsuhsc.edu) |
| Notes | ClinicalTrials.gov Identifier: NCT02360605 |
NCT02382731.
| Trial name or title | Interventions to support long‐term adherence and decrease cardiovascular events post‐myocardial infarction (ISLAND) |
| Methods |
Aims: to evaluate whether and in what format to sustain and/or scale‐up post‐MI educational reminder interventions. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: adherence to medications/laboratory tests |
| Participants |
Inclusion criteria: patients aged 18 years and older having a coronary angiography following a myocardial infarction (ST‐elevation myocardial infarction or non‐ST‐elevation myocardial infarction), with evidence of coronary artery disease (> 50% blockage of left main or > 70% blockage of either other main cardiac arteries); discharged from the catheterisation centre alive, either home or to a local (non‐cardiac) hospital; and Ontario residents Sample size: 2571; mean age: * sex: * ethnicity: * Country: Canada |
| Interventions |
Arm a: usual care + letters + automated calls (IVR phone calls to the participant delivered approximately 2 weeks after the letters, as well as personalised telephone follow‐up by trained peer health workers for participants identified by the IVR system as non‐adherent. The automated algorithm is designed to identify patients who are non‐adherent and who may benefit from personalised educational phone call and/or system navigation support by the peer health worker. Peer health workers will not provide clinical advice. Arm b: usual care + letters |
| Outcomes | Medication adherence |
| Starting date | September 2015 |
| Contact information | Noah Ivers, Women's College Hospital |
| Notes | ClinicalTrials.gov identifier: NCT02382731 |
NCT02429297.
| Trial name or title | Developing accessible telehealth programs for diabetes and hypertension management in bolivia |
| Methods |
Aims: to evaluate the feasibility and impact of an automated phone system in monitoring and improving self‐care and health outcomes among patients with diabetes and/or hypertension in Bolivia, in addition to assessing the additional benefit of support from a family member or friend. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: diabetes/hypertension |
| Participants |
Inclusion criteria: 21‐80 years of age; diagnosis of hypertension, a systolic blood pressure > 140 mmHg, and/or diagnosis of diabetes; access to a functional cell phone; able to respond to automated telephone calls Sample size: 100; mean age: * sex: * ethnicity: * Country: Bolivia |
| Interventions |
Arm a: experimental: participant only ‐ health information technology/care manager (HITCM)‐only participants enrolling without a CarePartner receive weekly HITCM automated assessment and self‐care support calls with feedback to the clinical team. Arm b: experimental: participant and CarePartner ‐ HITCM‐only participants enrolling with a CarePartner receive weekly HITCM automated assessment and self‐care support calls with feedback to the clinical team. Arm c: experimental: participant and CarePartner ‐ HITCM + CP participants enrolling with a CarePartner receive weekly HITCM automated assessment and self‐care support calls with feedback to the clinical team plus updates to their CarePartner via phone or email. |
| Outcomes | Change from baseline on self‐care behaviours and health at 16 weeks |
| Starting date | June 2014 |
| Contact information | John Piette, University of Michigan |
| Notes | ClinicalTrials.gov identifier: NCT02429297 |
NCT02442089.
| Trial name or title | Impact of automated calls on pediatric patient attendance in Chile (Health Call) |
| Methods |
Aims: evaluate whether a patient reminder system, Health Call, can decrease the overall failure to attend appointment rate as a percentage of overall appointments. Study design: RCT; recruitment: * Study duration: ongoing; study type: either; subtype: appointment reminder |
| Participants |
Inclusion criteria: guardian with a phone number (landline or mobile) who is able to receive and answer voice calls, is willing to take part in the study and complete the consent form, is sufficiently proficient in Spanish so as to complete the questionnaire, has a referral appointment at Hospital Luis Calvo Mackenna who is ≤ 18 years of age Sample size: 564; mean age: * sex: * ethnicity: * Country: Chile |
| Interventions |
Arm a: Health Call is an automated interactive voice reminder system that can contact guardians of patients ahead of their child's appointment, asks then confirms a security question about the participant, then, if the call recipient passes the security screen, provides a reminder about upcoming appointment. Arm b: no calls |
| Outcomes | 'Do not attend' (DNA) |
| Starting date | December 2013 |
| Contact information | William Weiss, DrPH, MA (bweiss@jhsph.edu), Johns Hopkins Bloomberg School of Public Health |
| Notes | Clinicaltrials.gov: NCT02442089 |
NCT02478359.
| Trial name or title | Walk On! Physical activity coaching |
| Methods |
Aims: to determine the effectiveness of a 12‐month physical activity coaching intervention (Walk On!) compared to standard care for 1650 COPD patients from a large integrated health care system Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: COPD |
| Participants |
Inclusion criteria: patients with any COPD‐related hospitalisation, emergency department visit or observational stay in the previous 12 months; COPD‐related encounters are defined according to the Centers for Medicare and Medicaid Services (CMS) and National Quality Forum (NQF) criteria for the Hospital Readmission Reduction Program. The following principal discharge diagnoses of COPD (ICD‐9 codes: 491.21, 491.22, 491.8, 491.9, 492.8, 493.20, 493.21, 493.22, and 496) or respiratory failure (ICD‐9 codes: 518.81, 518.82, 518.84, 799.1) with a secondary diagnosis of COPD exacerbation (ICD‐9 codes: 491.21, 491.22, 493.21, 493.22) will be used; age > 40 years; on at least a bronchodilator or steroid inhaler prior to the encounter or if not on an inhaler, had a previous disease diagnosis; continuous health plan membership in the 12 months prior to the encounter Sample size: 1650; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: the 12‐month Walk On! intervention includes a baseline in‐person assessment, collaborative monitoring of steps using 2 types of activity sensors, semi‐automated step goal recommendations using an IVR system or web application, ongoing individualised reinforcement from a physical activity coach, and peer/family support. Arm b: usual care |
| Outcomes | Composite: all‐cause hospitalisations, emergency department (ED) visits, observational stays, and mortality |
| Starting date | June 2015 |
| Contact information | Huong Q Nguyen, PhD, RN, Kaiser Permanente |
| Notes | ClinicalTrials.gov identifier: NCT02478359 |
Ratanawongsa 2012.
| Trial name or title | SelfManagement Automated and Real‐Time telephonic support (SMARTSteps) |
| Methods |
Aims: to investigate differences in 6‐month changes in patient‐centred outcomes including quality of life and functional status (SF‐12 and number of days spent in bed due to illness), comparing participants exposed to ATSM with wait‐list controls and comparing participants exposed to ATSM (SMARTSteps‐ONLY) with ATSM augmented by medication adherence and intensification (SMARTSteps‐PLUS) Study design: stepped wedge; recruitment: primary care (mail and telephone) Study duration: ongoing; study type: management; subtype: diabetes |
| Participants |
Inclusion criteria: San Francisco Health Plan (SFHP) membership; ≥ 1 primary care clinic visit in the preceding 24 months at one of our designated clinics; age ≥ 18 years; a diagnosis of diabetes (type 1 or 2); English‐, Cantonese‐, or Spanish‐speaking; access to a touch‐tone phone; and plans to remain in the region during the evaluation period (12 months) Sample size: 362; mean age: 55 years; sex: women ‐ 71%, men ‐ 29%; ethnicity: Asian ‐ 58.6%, black ‐ 6.9%, white ‐ 9.4%, Hispanic ‐ 22.4% Native American/Eskimo ‐ 0.3%, Hawaiian/Pacific Islander ‐ 0.8%, other ‐1.4%, Unknown ‐ 0.3% Country: USA |
| Interventions |
Arm a: SMARTSteps‐ONLY received the ATSM intervention within 2 weeks. Developed with extensive input from participants to be sensitive to literacy, language, and culture in the target populations, this ATSM system provided 27 weeks of 8‐12 min weekly calls in English, Cantonese, or Spanish. Participants specified the weekday and time convenient for their schedules or called toll‐free into the system if they missed their scheduled call. The content consisted of rotating sets of queries about self‐care (such as diet, exercise, and medication adherence), psychosocial issues (such as depressive symptoms), and access to preventive services (such as eye care). Participants responded via touch‐tone commands, and based on their answers, participants heard automated health education messages in the form of narratives Arm b: SMARTSteps‐PLUS intervention to detect and intervene for participants whose medication treatment was sub‐optimal Arm c: wait‐list (controls) continued to receive usual care through their clinics, as well as all existing SFHP benefits (reminders and incentives for receipt of recommended health services, including laboratory testing, eye and foot examination, and influenza vaccination). At the end of the 6‐month wait‐list period, each participant "crossed‐over" to begin SMARTSteps‐ONLY or SMARTSteps‐PLUS, depending on initial randomisation arm. |
| Outcomes | Quality of life and functional status; diabetes self‐efficacy and self‐management behaviour; medication adherence in the preceding 7 days; participant perspectives on the structure of their care; glycated haemoglobin; blood pressure; low‐density lipoproteins |
| Starting date | April 2009 |
| Contact information | ratanawongsan@medsfgh.ucsf.edu |
| Notes | ClinicalTrials.gov identifier: NCT00683020 |
Reid 2015.
| Trial name or title | The Helping HAND 2 |
| Methods |
Aims: to test the hypothesis that a multi‐component sustained care intervention is more effective than standard care in helping hospitalised cigarette smokers stop smoking after hospital discharge Study design: RCT; recruitment: secondary care (health professional referral) Study duration: ongoing; study type: management; subtype: smoking |
| Participants |
Inclusion criteria: admission to a participating hospital; received tobacco cessation counselling for > 5 min in hospital; age ≥18 years; current daily smoker (defined as having smoked ≥ 1 cigarette/day in the past month when smoking as usual); plan to sustain or initiate a quit attempt immediately after hospital discharge Sample size: 1350; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: multi‐component sustained care: the IVR calls at 2, 12, 28, 58, and 88 days after discharge. For each call, the IVR system makes up to 8 attempts to reach participants for each scheduled call, beginning on the scheduled call day and proceeding with 2 attempts per day for 4 days or until the call is completed; access to smoking cessation telephone counselling support; pharmacotherapy Arm b: standard care (control) group receive the same bedside counselling session in the hospital as the intervention group. The counsellor informs smokers about postdischarge counselling resources, provides specific advice to call the state telephone quit line, makes a specific recommendation to the hospital physician for postdischarge medication, and completes a consultation note in the participant's hospital record. No additional resources are provided to the participant after discharge from the hospital |
| Outcomes | Tobacco abstinence (biochemically validated); self‐reported tobacco abstinence; duration of tobacco abstinence after discharge; proportion of participants who make a 24‐h quit attempt after discharge |
| Starting date | December 2012 |
| Contact information | zreid@partners.org |
| Notes | ClinicalTrials.gov identifier: NCT01714323 |
Ritchie 2012.
| Trial name or title | The E‐Coach |
| Methods |
Aims: to test the E‐Coach intervention in congestive heart failure and COPD patients admitted to a large tertiary hospital Study design: RCT; recruitment: tertiary care (health professional referral) Study duration: ongoing; study type: management; subtype: heart failure |
| Participants |
Inclusion criteria: patients are considered for inclusion if they were admitted from home with chronic heart failure or COPD, have an estimated prognosis of greater than 6 months, are English‐speaking, have a telephone, and are expected to be discharged to home Sample size: 478; mean age: 63 years; sex: women ‐ 47%; men ‐53%; ethnicity: * Country: USA |
| Interventions |
Arm a: E‐Coach intervention is delivered through an IVR monitoring system that is based on Coleman's 4 pillars of care transition support and a web‐based 'dashboard' for care transition nurses, with alerts of patient/caregiver concerns after discharge. After discharge, Ida is programmed to call participants daily for 7 days and for an additional 21 sessions thereafter (either daily or every 3 days, depending on participant preference). In a stepped‐care approach, the IVR is then supported by the care transition nurse, who monitors participant issues through the E‐Coach IVR secure web‐based dashboard. Support for participant self‐management is provided through personal telephone‐based interactions when needed, up to 2 months (60 days) after discharge. Clients are advised to use condoms as dual protection from HIV and sexually transmitted infections as appropriate. Follow‐up calls to clients are made during preferred times indicated by the client on her registration form. Clients in the intervention arm are also able to call the MOTIF service at any time to request to speak with a counsellor. Clients who opt to receive the OC or injectable can opt in to receive additional reminder messages appropriate to their method (that is, to start a new packet of pills or when to receive a new injection). The sixth and final voice message provides similar information to the first five, but also reminds the client that this will be the last message they will receive. Arm b: control group received usual care (no intervention). |
| Outcomes | Rehospitalisations; rehospitalisations at 90 days; community tenure |
| Starting date | 1 June 2010 |
| Contact information | critchie@uab.edu, christine.ritchie@ucsf.edu |
| Notes | ClinicalTrials.gov identifier: NCT01135381 |
Silveira 2010.
| Trial name or title | Care partners: web‐based support for caregivers of veterans undergoing chemotherapy |
| Methods |
Aims: to determine if VA patients undergoing chemotherapy who receive automated telephonic assessment and symptom management advice plus web‐based feedback to inform and engage a CarePartner report significant improvement in the number and severity of symptoms compared to patients receiving monitoring only. Study design: RCT; recruitment: * Study duration: ongoing; study type: management; subtype: cancer |
| Participants |
Inclusion criteria: all participants must be ≥ 18 years, cognitively intact, English‐speaking, able to hear, and own a telephone. Patients can have any solid tumour; must be initiating IV cytotoxic chemotherapy and, if recurrent, have experienced a 1 month treatment free interval. Caregivers must have a computer with high speed Internet access. Sample size: 214; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: participants receive automated telephone symptom assessment and symptom management advice; caregivers receive access to a website that updates them on participant's symptoms and provides tailored problem solving advice. Arm b: participants receive automated telephone symptom assessment and symptom management advice; caregivers receive nothing. |
| Outcomes | Symptom severity |
| Starting date | October 2010 |
| Contact information | Maria J Silveira, MD MA MPH, VA Ann Arbor Healthcare System, Ann Arbor, MI |
| Notes | ClinicalTrials.gov identifier: NCT00983892 |
Smith 2013.
| Trial name or title | MObile Technology for Improved Family Planning (MOTIF) |
| Methods |
Aims: to evaluate a mobile phone‐based intervention using voice messages to support postabortion family planning (PAFP) in Cambodia by testing whether additional regular, structured, interactive mobile phone‐based support improves use of PAFP Study design: RCT; recruitment: primary care (health professional referral) Study duration: ongoing; study type: prevention; subtype: sexual health |
| Participants |
Inclusion criteria: participants are eligible for the trial if they are attending for induced abortion, aged ≥ 18 years, own a mobile phone, do not want to have a child at the present time and are willing to receive simple voice messages from Marie Stopes International Cambodia related to contraception Sample size: 500; mean age: * sex: * ethnicity: Cambodian Country: the Netherlands |
| Interventions |
Arm a: six automated voice messages to remind clients about available family planning methods and provide a conduit for additional support. Clients can respond to message prompts to request a phone call from a counsellor, or alternatively state they have no problems. Clients requesting to talk to a counsellor, or who do not respond to the message prompts, receive a call from a Marie Stopes International Cambodia counsellor who provides individualised advice and support regarding family planning. Arm b: standard of care without the additional mobile phone‐based support |
| Outcomes | Use of an effective modern method of contraception at 4 months; repeat abortion; contraceptive discontinuation |
| Starting date | 30 March 2013 |
| Contact information | christopher.smith@lshtm.ac.uk |
| Notes | ClinicalTrials.gov identifier: NCT01823861 |
Te Boveldt 2011.
| Trial name or title | Rationale, design, and implementation protocol of the Dutch clinical practice guideline pain in patients with cancer: a cluster RCT with Short Message Service (SMS) and IVR |
| Methods |
Aims: to evaluate the implementation of the Dutch guideline Pain in Patients with Cancer to improve pain reporting, pain measurement, and hence pain control in patients with cancer and pain Study design: cluster RCT; recruitment: secondary care (health professional referral) Study duration: ongoing; study type: management; subtype: cancer pain |
| Participants |
Inclusion criteria: diagnosed with cancer; aged ≥ 18 years; pain intensity of 3 or more on a numeric rating scale for the worst pain experienced in the last 24 h; and having and being familiar with the use of a mobile phone Sample size: 210; mean age: * sex: * ethnicity: * Country: the Netherlands |
| Interventions |
Arm a: SMS‐IVR + personal advice by phone on how to reduce pain if rating is ≥ 5 or higher on a numeric rating scale (NRS) of 0‐10. The research nurse of the hospital, specialised in pain treatment and trained for this project, will provide the personal advice Arm b: control group will receive a leaflet on cancer pain |
| Outcomes | The first primary outcome is the percentage of all participants that visit the medical oncology outpatient clinic with adequate pain therapy/medication. Pain treatment adequacy will be calculated with both the Cleeland's Pain Management Index (PMI) and Ward's variation of the PMI |
| Starting date | November 2009 |
| Contact information | n.teboveldt@anes.umcn.nl |
| Notes | Netherlands Trial Register (NTR): NTR2739 |
Wright 2014.
| Trial name or title | The study of automated telephone programs for the maintenance of dietary change |
| Methods |
Aims: to compare two theory‐based interventions (social cognitive theory (SCT) vs goal systems theory (GST)) designed to maintain previously achieved improvements in fruit and vegetableconsumption Study design: RCT; recruitment: other ‐ voter registration list (mail and telephone) Study duration: ongoing; study type: prevention; subtype: cancer |
| Participants |
Inclusion criteria: participants were adults ≥ 18 years old who consumed less than the recommended level of fruits and vegetables (i.e. ≤ 5 servings/day), lived in the Boston area, had access to a touch‐tone telephone, and were generally healthy Sample size: 1049; mean age: * sex: * ethnicity: * Country: USA |
| Interventions |
Arm a: TLC maintenance intervention based on SCT used a skills‐based approach to build self‐efficacy. It assessed confidence in and barriers to eating fruit and vegetables, provided feedback on how to overcome barriers, plan ahead, and set goals Arm b: control group received assessment only |
| Outcomes | Fruit and vegetable intake; self‐efficacy; costs |
| Starting date | July 2006 |
| Contact information | julie.wright@umb.edu |
| Notes | Clinicaltrials.gov: NCT00148525 |
ACS: acute coronary syndrome; ART: antiretroviral therapy; ATCS: automated telephone communication system; ATSM: automated telephone self‐management; BMI; body mass index; CBT: cognitive behavioural therapy; CDSS: clinical decision support system; CPCQ: client perceptions of coordination questionnaire; COPD: chronic obstructive pulmonary disease; ECOG: Eastern Cooperative Oncology Group; EHR: electronic health record; EMR: electronic medical record; ESAS: Edmonton symptom assessment system; FDA: Food and Drug Administration; GP: general practitioner; IDS‐SR: inventory of depressive symptomatology (self‐report); IVR: interactive voice response; MI: motivational interviewing; NA: not available; NSTEMI: non‐ST‐elevation myocardial infarction; OSAS: obstructive sleep apnoea syndrome; PACIC: patient assessment of chronic illness care; PCI: percutaneous coronary intervention; PHQ‐9: personal health questionnaire, version 9; RCT: randomised controlled trial; SF‐36: Short Form‐36‐Health Survey; STEMI: ST‐elevation myocardial infarction; UC: usual care; UKPDS: UK Prospective Diabetes Study; VA: Veteran's Administration.
Differences between protocol and review
Objectives: we added a third secondary objective since publishing the protocol: to explore "the behaviour change techniques and theoretical models underpinning the ATCS interventions" to better understand any plausible mechanisms of action that underpin the interventions.
Methods: at protocol stage, the exclusions listed in Types of interventions included studies that "were exclusively for the purpose of electronic history‐taking or risk assessment with no health promotion or interactive elements". We have been modified this to "were exclusively for the purpose of electronic history‐taking or data collection or risk assessment with no health promotion or interactive elements"
We removed the following exclusion stated at protocol stage: "Studies that evaluate the groups that receive similar ATCS components but the interventions differ only by the advanced communicative functions (such as access to an advisor) or supplementary functions (such as email and short messaging service)", because it contradicted the extended inclusion criteria (please see point immediately below).
In Types of interventions, the protocol stated: "We will also include comparisons of one type of ATCS against another". We have altered this to: "We also included studies that compared ATCS interventions (e.g. unidirectional ATCS versus ATCS versus ATCS Plus) to compare the effects of different intervention designs on preventive healthcare or management of long‐term conditions."
In Types of outcome measures, the protocol stated: "To select only one of multiple outcomes, we used the following approach . . . Select the primary outcome which was identified by the publication authors (we took into consideration the possibility of selective outcome reporting bias; we attempted to compare the primary outcomes stated in the protocol with the ones listed in the review, to assist our judgement of this; when no primary outcome was identified, we selected the one specified in the sample size calculation; where there was no sample size calculation, we ranked the effect estimates and selected the median effect estimate." We have altered this to, "For each study we selected all relevant primary outcomes related to human physiology or health behaviour, as these are likely to be most meaningful to clinicians, consumers, the general public, administrators and policymakers." We followed a similar approach for selection of secondary outcomes, with the following text inserted: "For each study, we selected all relevant secondary outcomes as these were also meaningful for the various stakeholders."
The Information Specialist modified the search strategy for MEDLINE.
Unit of analysis issues: the protocol stated: "the comparator arm will be split equally between each treatment arm"; we changed this to: "we compared the relevant ATCS arm with the least active control arm", i.e. from studies with multiple intervention arms only one arm was included without splitting the comparison group.
Unit of analysis issues: we had planned to impute estimates of the ICC using external sources; however, we managed to calculate the ICC using the Fleiss‐Cuzick estimator for binary data in Hess 2013 study.
We incorporated an additional outcome. quality of life, under Secondary outcomes, Patient‐centred outcomes to add outcomes from medical care that are important to patients.
We also incorporated another secondary process outcome, cost‐effectiveness, to add a further layer of information relating to the description and evaluation of resource use associated with ATCS interventions, which might be used in a decision‐making process.
Dealing with missing data: we planned to contact the authors or impute the standard deviations from other similar studies; however, we managed to calculate the standard deviations from other statistics, such as 95% confidence intervals, standard errors, or P values.
Contributions of authors
Pawel Posadzki: revised the protocol, re‐ran the searches, screened, extracted and analysed and synthesised data, wrote and revised the drafts.
Nikolaos Mastellos: screened studies, extracted data, and revised the drafts.
Rebecca Ryan: managed the project, assessed methodological quality, revised the drafts.
Laura H Gunn: revised the drafts, and contributed to the statistical methods sections.
Lambert M Felix: revised the protocol, contributed to the design of the conceptual framework, and refined the data extraction form.
Yannis Pappas: revised the drafts.
Marie‐Pierre Gagnon: revised the drafts.
Steven A Julious: provided statistical expertise.
Brian Oldenburg: provided content expertise, revised the drafts.
Josip Car: conceived the idea for the review, managed the project, and revised the drafts.
All authors contributed to the writing or editing of the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
The NW London NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC), the Imperial NIHR Biomedical Research Centre, and the Imperial Centre for Patient Safety and Service Quality (CPSSQ), UK.
The Department of Primary Care & Public Health at Imperial College London is grateful for support from the NW London NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC), the Imperial NIHR Biomedical Research Centre, and the Imperial Centre for Patient Safety and Service Quality (CPSSQ). The views expressed in this publication are those of the authors and not necessarily those of the NIHR, BRC or CPSSQ.
Declarations of interest
Pawel Posadzki: none known.
Nikolaos Mastellos: none known.
Rebecca Ryan: This work was completed by RR as part of her role as editor with CCCG, funded by a Cochrane Infrastructure Grant provided by the National Health and Medical Research Council (NHMRC).
Laura H Gunn: none known.
Lambert M Felix: none known.
Yannis Pappas: none known.
Marie‐Pierre Gagnon: none known.
Steven A Julious:none known.
Liming Xiang: none known.
Brian Oldenburg: none known.
Josip Car: none known.
New
References
References to studies included in this review
Adams 2014 {published data only}
- Adams WG, Phillips BD, Bacic JD, Walsh KE, Shanahan CW, Paasche‐Orlow MK. Automated conversation system before paediatric primary care visits: a randomised trial. Pediatrics 2014;134(3):e691‐9. [DOI] [PubMed] [Google Scholar]
Aharonovich 2012 {published data only}
- Aharonovich E, Greenstein E, O'Leary A, Johnston B, Seol SG, Hasin DS. HealthCall: technology‐based extension of motivational interviewing to reduce non‐injection drug use in HIV primary care patients ‐ a pilot study. AIDS Care 2012;24(12):1461‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersson 2012 {published data only}
- Research Society on Alcoholism. 35th Annual Scientific Meeting of the Research Society on Alcoholism, 23‐27 June 2012, San Francisco (CA). Alcoholism: Clinical and Experimental Research 2012;36:11A‐303A. [DOI: 10.1111/j.1530-0277.2012.01803.x] [DOI] [PubMed] [Google Scholar]
Baker 2014 {published data only}
- Baker DW, Brown T, Buchanan DR, Weil J, Balsley K, Ranalli L, et al. Comparative effectiveness of a multifaceted intervention to improve adherence to annual colorectal cancer screening in community health centres: a randomised clinical trial. JAMA Internal Medicine 2014;174(8):1235‐41. [DOI] [PubMed] [Google Scholar]
- Baker DW, Brown T, Buchanan DR, Weil J, Cameron KA, Ranalli L, et al. Design of a randomised controlled trial to assess the comparative effectiveness of a multifaceted intervention to improve adherence to colorectal cancer screening among patients cared for in a community health centre. BMC Health Services Research 2013;13:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Brown T, Buchanan DR, Weil J, Cameron KA, Ranalli L, et al. Improving rates of annual colorectal cancer screening among Latino patients. Journal of General Internal Medicine 2013;28 Suppl 1:S106. [Google Scholar]
- Baker DW, Brown T, Goldman SN, Liss DT, Kollar S, Balsley K, et al. Two year follow‐up of the effectiveness of a multi faceted intervention to improve adherence to annual colorectal cancer screening in community health centres. Cancer Causes & Control 2015;26(11):1685‐90. [DOI] [PubMed] [Google Scholar]
Bender 2010 {published data only}
- Bender BG, Apter A, Bogen DK, Dickinson P, Fisher L, Wamboldt FS, et al. Test of an interactive voice response intervention to improve adherence to controller medications in adults with asthma. Journal of the American Board of Family Medicine 2010;23(2):159‐65. [DOI] [PubMed] [Google Scholar]
Bender 2014 {published data only}
- Bender B, Cvietusa P, Goodrich GC, Lowe R, Nuanes H, Shetterly S, et. al. A 24‐month randomised, controlled trial of an automated speech recognition program to improve adherence in paediatric asthma. Journal of Allergy and Clinical Immunology 2014;133(2):AB166. [Google Scholar]
Bennett 2012 {published data only}
- Bennett GG, Warner ET, Glasgow RE, Askew S, Goldman J, Ritzwoller DP, et al. Obesity treatment for socio‐economically disadvantaged patients in primary care practice. Archives of Internal Medicine 2012;172(7):565‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritzwoller DP, Glasgow RE, Sukhanova AY, Bennett GG, Warner ET, Greaney ML, et al. Economic analyses of the Be Fit Be Well program: a weight loss program for community health centers. Journal of General Internal Medicine 2013;28(12):1581‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner ET, Glasgow RE, Emmons KM, Bennett GG, Askew S, Rosner B, et al. Recruitment and retention of participants in a pragmatic randomized intervention trial at three community health clinics: results and lessons learned. BMC Public Health 2013;13:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh HC, Clark JM, Emmons KE, Moore RH, Bennett GG, Warner ET, et al. Independent but coordinated trials: insights from the practice‐based Opportunities for Weight Reduction Trials Collaborative Research Group. Clinical Trials 2010;7(4):322‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bennett 2013 {published data only}
- Bennett GG, Foley P, Levine E, Whiteley J, Askew S, Steinberg DM, et al. Behavioural treatment for weight gain prevention among black women in primary care practice: a randomised clinical trial. JAMA Internal Medicine 2013;173(19):1770‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley P, Levine E, Askew S, Puleo E, Whiteley J, Batch B, et al. Weight gain prevention among black women in the rural community health centre setting: the Shape Program. BMC Public Health 2012;12(305):1‐11. [DOI: 10.1186/1471-2458-12-305] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg DM, Levine EL, Lane I, Askew S, Foley PB, Puleo E, et al. Adherence to self‐monitoring via interactive voice response technology in an eHealth intervention targeting weight gain prevention among Black women: randomised controlled trial. Journal of Medical Internet Research 2014;16(4):e114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boland 2014 {published data only}
- Boland MV, Chang DS, Frazier T, Plyler R, Jefferys JL, Friedman DS. Automated telecommunication‐based reminders and adherence with once‐daily glaucoma medication dosing: the automated dosing reminder study. JAMA Ophthalmology 2014;132(7):845‐50. [DOI] [PubMed] [Google Scholar]
Bove 2013 {published data only}
- Bove AA, Homko CJ, Santamore WP, Kashem M, Kerper M, Elliott DJ. Managing hypertension in urban underserved subjects using telemedicine‐‐a clinical trial. American Heart Journal 2013;165(4):615‐21. [DOI] [PubMed] [Google Scholar]
- Kashem A, Keper M, Homko CJ, Santamore WP, Hewitt V, Eubanks A, et al. Hypertension management in urban underserved patients using an Internet communication system. Journal of the American College of Cardiology 2011;57(14s1):E1280. [Google Scholar]
Brendryen 2008 {published data only}
- Brendryen H, Drozd F, Kraft P. A digital smoking cessation program delivered through Internet and cell phone without nicotine replacement (happy ending): randomised controlled trial. Journal of Medical Internet Research 2008;10(5):e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brendryen H, Kraft P. Happy Ending: a randomised controlled trial of a digital multi‐media smoking cessation intervention. Addiction 2008;103(3):478–84. [DOI] [PubMed] [Google Scholar]
- Brendryen H, Kraft P, Schaalma H. Looking inside the black box: using intervention mapping to describe the development of the automated smoking cessation intervention 'Happy Ending'. Journal of Smoking Cessation 2010;5(1):29‐56. [Google Scholar]
Capomolla 2004 {published data only}
- Capomolla S, Pinna G, Rovere MT, Maestri R, Ceresa M, Ferrari M, et al. Heart failure case disease management program: a pilot study of home telemonitoring versus usual care. European Heart Journal Supplements 2004;6(Suppl F):F91‐8. [Google Scholar]
Carlini 2012 {published data only}
- Carlini BH, McDaniel AM, Weaver MT, Kauffman RM, Cerutti B, Stratton RM, et al. Reaching out, inviting back: using Interactive voice response (IVR) technology to recycle relapsed smokers back to Quitline treatment‐‐a randomised controlled trial. BMC Public Health 2012;6(12):507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaudhry 2010 {published data only}
- Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, et al. Telemonitoring in patients with heart failure. New England Journal of Medicine 2010;363(24):2301‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cleeland 2011 {published data only}
- Cleeland CS, Wang XS, Shi Q, Mendoza TR, Wright SL, Berry MD, et al. Automated symptom alerts reduce postoperative symptom severity after cancer surgery: a randomised controlled clinical trial. Journal of Clinical Oncology 2011;29(8):994‐1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen‐Cline 2014 {published data only}
- Cohen‐Cline H, Wernli KJ, Boles‐Hall M, Bradford SC, Bounds L, Grossman D. Use of interactive voice response systems to improve colorectal cancer screening. American Journal of Epidemiology 2012;175(Suppl 11):S102. [Google Scholar]
- Cohen‐Cline H, Wernli KJ, Bradford SC, Boles‐Hall M, Grossman DC. Use of interactive voice response to improve colorectal cancer screening. Medical Care 2014;52(6):496‐9. [DOI] [PubMed] [Google Scholar]
Corkrey 2005 {published data only}
- Corkrey R, Parkinson L, Bates L. Pressing the key pad: trial of a novel approach to health promotion advice. Preventive Medicine 2005;41(2):657‐66. [DOI] [PubMed] [Google Scholar]
Cvietusa 2012 {published data only}
- Cvietusa PJ, Magid DJ, Goodrich G, Wagner N, Lowe R, Nuanes H, et al. A speech recognition (SR) reminder system improves adherence to ICS among pediatric asthma patients. Journal of Allergy and Clinical Immunology 2012;129(2):AB142. [Google Scholar]
David 2012 {published data only}
- David P, Buckworth J, Pennell ML, Katz ML, DeGraffinreid CR, Paskett ED. A walking intervention for postmenopausal women using mobile phones and Interactive Voice Response. Journal of Telemedicine and Telecare 2012;18(1):20‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llanos AA, Krok JL, Peng J, Pennell ML, Vitolins MZ, Degraffinreid CR, et al. Effects of a walking intervention using mobile technology and interactive voice response on serum adipokines among postmenopausal women at increased breast cancer risk. Hormones and Cancer 2014;5(2):98‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dedier 2014 {published data only}
- Dedier J, Wright JA, Friedman RH. Heeren T. Randomized controlled trial of a culturally adapted, automated telephone exercise coach to improve physical activity among hypertensive African‐Americans. Journal of General Internal Medicine 2014;29(Suppl 1):S192‐3. [Google Scholar]
DeFrank 2009 {published data only}
- DeFrank JT, Rimer BK, Gierisch JM, Bowling MJ, Farrell D, Skinner CS. Impact of mailed and automated telephone reminders on receipt of repeat mammograms: a randomized controlled trial. American Journal of Preventive Medicine 2009;36(6):459–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierisch JM, Bowling JM, DeFrank JT, Rimer BK, Matuszewski JM, Farrell D, et al. Finding the minimal intervention needed for sustained mammography adherence. American Journal of Preventive Medicine 2010;39(4):334‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierisch JM, Earp JA, Brewer NT, Rimer BK. Longitudinal predictors of nonadherence to maintenance of mammography. Cancer Epidemiology Biomarkers and Prevention 2010;19(4):1103‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierisch JM, O'Neill SC, Rimer BK, DeFrank JT, Bowling JM, Skinner CS. Factors associated with annual‐interval mammography for women in their 40s. Cancer Epidemiology 2009;33(1):72‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
DeMolles 2004 {published data only}
- DeMolles DA, Sparrow D, Gottlieb DJ, Friedman R. A pilot trial of a telecommunications system in sleep apnoea management. Medical Care 2004;42(8):764‐9. [DOI] [PubMed] [Google Scholar]
Derose 2009 {published data only}
- Derose SF, Nakahiro RK, Ziel FH. Automated messaging to improve compliance with diabetes test monitoring. American Journal of Managed Care 2009a;15(7):425‐31. [PubMed] [Google Scholar]
Derose 2013 {published data only}
- Derose SF, Green K, Marrett E, Tunceli K, Cheetham TC, Chiu VY, et al. Automated outreach to increase primary adherence to cholesterol‐lowering medications. JAMA Internal Medicine 2013;173(1):38‐43. [DOI] [PubMed] [Google Scholar]
Dini 1995 {published data only}
- Dini EF, Linkins RW, Chaney M. Effectiveness of computer‐generated telephone messages in increasing clinic visits. Archives of Pediatrics & Adolescent Medicine 1995;149(8):902‐5. [DOI] [PubMed] [Google Scholar]
Dini 2000 {published data only}
- Dini EF, Linkins RW, Sigafoos J. The impact of computer‐generated messages on childhood immunization coverage. American Journal of Preventive Medicine 2000;18(2):132‐9. [DOI] [PubMed] [Google Scholar]
Dubbert 2002 {published data only}
- Dubbert PM, Cooper KM, Kirchner KA, Meydrech EF, Bilbrew D. Effects of nurse counseling on walking for exercise in elderly primary care patients. Journals of Gerontology Series A ‐ Biological Sciences & Medical Sciences 2002;57(11):M733‐40. [DOI] [PubMed] [Google Scholar]
Durant 2014 {published data only}
- Durant KT, Newsom J, Rubin E, Berger J, Pomerantz G. Increasing preventive health services via tailored health communications. American Journal of Managed Care 2014;20(10):828‐35. [PubMed] [Google Scholar]
Ershoff 1999 {published data only}
- Ershoff DH, Quinn VP, Boyd NR, Stern J, Gregory M, Wirtschafter D. The Kaiser Permanente prenatal smoking cessation trial: when more isn't better, what is enough?. American Journal of Preventive Medicine 1999;17(3):161‐8. [DOI] [PubMed] [Google Scholar]
Estabrooks 2008 {published data only}
- Estabrooks PA, Smith‐Ray RL. Piloting a behavioural intervention delivered through interactive voice response telephone messages to promote weight loss in a pre‐diabetic population. Patient Education & Counseling 2008;72(1):34‐41. [DOI] [PubMed] [Google Scholar]
Estabrooks 2009 {published data only}
- Estabrooks PA, Shoup JA, Gattshall M, Dandamudi P, Shetterly S, Xu S. Automated telephone counselling for parents of overweight children: a randomised controlled trial. American Journal of Preventive Medicine 2009;36(1):35‐42.e2. [DOI] [PubMed] [Google Scholar]
Farzanfar 2011 {published data only}
- Farzanfar R, Locke SE, Heeren TC, Stevens A, Vachon L, Thi Nguyen MK, et al. Workplace telecommunications technology to identify mental health disorders and facilitate self‐help or professional referrals. American Journal of Health Promotion 2011;25(3):207‐16. [DOI] [PubMed] [Google Scholar]
- Farzanfar, R, Finkelstein, D. Evaluation of a workplace technology for mental health assessment: a meaning‐making process. Computers in Human Behavior 2012;28(1):160‐5. [Google Scholar]
Feldstein 2006 {published data only}
- Feldstein AC, Smith DH, Perrin N, Yang X, Rix M, Raebel MA, et al. Improved therapeutic monitoring with several interventions: a randomised trial. Archives of Internal Medicine 2006;166(17):1848‐54. [DOI] [PubMed] [Google Scholar]
Fiscella 2011 {published data only}
- Fiscella K, Humiston S, Hendren S, Winters P, Idris A, Li SXL, et al. A multimodal intervention to promote mammography and colorectal cancer screening in a safety‐net practice. Journal of the National Medical Association 2011;103(8):762‐8. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Yosha A, Hendren SK, Humiston S, Winters P, Ford P, et al. Get screened: a pragmatic randomised controlled trial to increase mammography and colorectal cancer screening in a large, safety net practice. BMC Health Services Research 2010;10:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fortuna 2014 {published data only}
- Fortuna RJ, Idris A, Winters P, Humiston SG, Scofield S, Hendren S, et al. Get screened: a randomised trial of the incremental benefits of reminders, recall, and outreach on cancer screening. Journal of General Internal Medicine 2014;29(1):90‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Franzini 2000 {published data only}
- Franzini L, Rosenthal J, Spears W, Martin HS, Balderas L, Brown M, et al. Cost‐effectiveness of childhood immunization reminder/recall systems in urban private practices. Pediatrics 2000;106(1 II):177‐83. [PubMed] [Google Scholar]
- The American Pediatric Society and The Society for Pediatric Research. Improving return visits in private provider offices through immunization reminder/recall. Pediatric Research 1998;43(Suppl 4):113. [Google Scholar]
Friedman 1996 {published data only}
- Friedman RH, Kazis LE, Jette A, Smith MB, Stollerman J, Torgerson J, et al. A telecommunications system for monitoring and counselling patients with hypertension. Impact on medication adherence and blood pressure control. American Journal of Hypertension 1996;9(4 Pt 1):285‐92. [DOI] [PubMed] [Google Scholar]
- Friedman RH, Stollerman J, Rozenblyum L, Belfer D, Selim A, Mahoney D, et al. A telecommunications system to manage patients with chronic disease. Studies in Health Technology & Informatics 1998;52 Pt 2:1330‐4. [PubMed] [Google Scholar]
Glanz 2012 {published data only}
- Glanz K, Beck AD, Bundy L, Primo S, Lynn MJ, Cleveland J, et al. Impact of a health communication intervention to improve glaucoma treatment adherence. Results of the interactive study to increase glaucoma adherence to treatment trial. Archives of Ophthalmology 2012;130(10):1252‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goulis 2004 {published data only}
- Goulis DG, Giaglis GD, Boren SA, Lekka I, Bontis E, Balas EA, et al. Effectiveness of home‐centred care through telemedicine applications for overweight and obese patients: a randomised controlled trial. International Journal of Obesity 2004;28:1391‐8. [DOI] [PubMed] [Google Scholar]
Graziano 2009 {published data only}
- Graziano JA, Gross CR. A randomised controlled trial of an automated telephone intervention to improve glycaemic control in type 2 diabetes. Advances in Nursing Science 2009;32(3):E42‐57. [DOI] [PubMed] [Google Scholar]
Green 2011 {published data only}
- 26th Annual Scientific Meeting and Exposition of the American Society of Hypertension, Inc, 2011 May 24, New York (NY). Automated outreach for antihypertensive medication refill reminders. Journal of Clinical Hypertension 2011;13(Suppl 1):A155. [Google Scholar]
Greist 2002 {published data only}
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ, et al. Behaviour therapy for obsessive‐compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. The Journal of Clinical Psychiatry 2002;63(2):138‐45. [DOI] [PubMed] [Google Scholar]
Griffin 2011 {published data only}
- Griffin JM, Hulbert EM, Vernon SW, Nelson D, Hagel EM, Nugent S, et al. Improving Endoscopy Completion: Effectiveness of an Interactive Voice Response System. American Journal of Managed Care 2011;17(3):199‐208. [PubMed] [Google Scholar]
Halpin 2009 {published data only}
- Halpin D, Laing‐Morton T, Levy M, Marno P. Effect of an innovative automated interactive health forecast alert system on rate of exacerbations of COPD. Thorax 2009;64(Suppl 4):A115. [Google Scholar]
- Halpin DM, Laing‐Morton T, Spedding S, Levy ML, Coyle P, Lewis J, et al. A randomised controlled trial of the effect of automated interactive calling combined with a health risk forecast on frequency and severity of exacerbations of COPD assessed clinically and using EXACT PRO. Primary Care Respiratory Journal 2011;20(3):324‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harrison 2013 {published data only}
- Harrison TN, Ho TS, Handler J, Kanter MH, Goldberg RA, Reynolds K. A randomised controlled trial of an automated telephone intervention to improve blood pressure control. Journal of Clinical Hypertension (Greenwich) 2013;15(9):650‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hasin 2013 {published data only}
- Amrhein P, Aharonovich E, Greenstein E, Hasin D. Patient commitment strength during MI, healthcall participation, and drinking outcomes: results from a randomised trial of HIV primary care patients. Alcoholism: Clinical and Experimental Research. 2012; Vol. 36:68A.
- Hasin D, Aharonovich E, Greenstein E, Pavlicova M, Wainberg M, Helzer J, et al. Drinking reduction in HIV primary care: a randomised trial of healthcall, a technology‐based enhancement to brief motivational interviewing. Alcoholism: Clinical and Experimental Research 2012;36:161A. [Google Scholar]
- Hasin DS, Aharonovich E, O'Leary A, Greenstein E, Pavlicova M, Arunajadai S, et al. Reducing heavy drinking in HIV primary care: a randomised trial of brief intervention, with and without technological enhancement. Addiction 2013;108(7):1230‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Helzer 2008 {published data only}
- Fazzino TL, Harder VS, Rose GL, Helzer JE. A daily process examination of the bidirectional relationship between craving and alcohol consumption as measured via interactive voice response. Alcoholism: Clinical and Experimental Research 2013;37(12):2161‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guth S, Lindberg SA, Badger GJ, Thomas CS, Rose GL, Helzer JE. Brief intervention in alcohol‐dependent versus nondependent individuals. Journal of Studies on Alcohol and Drugs 2008;69(2):243‐50. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Rose GL, Badger GJ, Searles JS, Thomas CS, Lindberg SA, et al. Using interactive voice response to enhance brief alcohol intervention in primary care settings. Journal of Studies on Alcohol and Drugs 2008;69(2):251‐8. [DOI] [PubMed] [Google Scholar]
Hendren 2014 {published data only}
- Hendren S, Winters P, Humiston S, Idris A, Li SX, Ford P, et al. Randomized, controlled trial of a multimodal intervention to improve cancer screening rates in a safety‐net primary care practice. Journal of General Internal Medicine 2014;29(1):41‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hess 2013 {published data only}
- Hess R. Impact of automated telephone messaging on zoster vaccination rates in community pharmacies. Journal of American Pharmacists Association (2003) 2013;53(2):182‐7. [DOI] [PubMed] [Google Scholar]
Heyworth 2014 {published data only}
- Heyworth L, Kleinman K, Oddleifson S, Bernstein L, Frampton J, Lehrer M, et al. Comparison of interactive voice response, patient mailing, and mailed registry to encourage screening for osteoporosis: a randomised controlled trial. Osteoporosis International 2014;25(5):1519‐26. [DOI] [PubMed] [Google Scholar]
- Heyworth L, Kleinman K, Oddleifson S, Bernstein L, Frampton J, Salvato K, et al. Screening for osteoporosis in high risk, menopausal women: a randomised trial of interactive voice response. Journal of General Internal Medicine 2011;26:S207. [Google Scholar]
Ho 2014 {published data only}
- Ho PM, Lambert‐Kerzner A, Carey EP, Fahdi IE, Bryson CL, Melnyk SD, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomised clinical trial. JAMA Internal Medicine 2014;174(2):186‐93. [DOI] [PubMed] [Google Scholar]
- Lambert‐Kerzner A, Giacco EJ, Fahdi IE, Bryson CL, Melnyk SD, Bosworth HB, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures (Medication study) after acute coronary syndrome hospital discharge. Circulation Cardiovascular Quality and Outcomes 2012;5(4):571‐6. [DOI] [PubMed] [Google Scholar]
- Lambert‐Kerzner A, Havranek EP, Plomondon ME, Albright K, Moore A, Gryniewicz K, et al. Patients' perspectives of a multifaceted intervention with a focus on technology: a qualitative analysis. Circulation: Cardiovascular Quality and Outcomes 2010;3(6):668‐74. [DOI] [PubMed] [Google Scholar]
- Welch LK, Olson KL, Snow KE, Pointer L, Lambert‐Kerzner A, Havranek EP, et al. Systolic blood pressure control after participation in a hypertension intervention study. The American Journal of Managed Care 2011;17(7):473‐8. [PubMed] [Google Scholar]
Homko 2012 {published data only}
- Homko CJ, Deeb LC, Rohrbacher K, Mulla W, Mastrogiannis D, Gaughan J, et al. Impact of a telemedicine system with automated reminders on outcomes in women with gestational diabetes mellitus. Diabetes Technology and Therapeutics 2012;14(7):624‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Houlihan 2013 {published data only}
- Houlihan BV, Jette A, Friedman RH, Paasche‐Orlow M, Ni P, Wierbicky J, et al. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord 2013;51(9):715‐20. [DOI] [PubMed] [Google Scholar]
- Houlihan BV, Jette A, Ni P, Paasche‐Orlow M, Friedman RH, Ducharme S, et al. Efficacy of "care call" telerehabilitation intervention for persons with spinal cord dysfunction: Randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2011;92(10):1690. [Google Scholar]
- Mercier HW, Jette A, Houlihan B. Differential impact and use of a telehealth intervention by persons with multiple sclerosis or spinal cord injury. Archives of Physical Medicine and Rehabilitation 2014;95(10):e34‐e5. [Google Scholar]
Hyman 1996 {published data only}
- Hyman DJ, Herd JA, Ho KS, Dunn JK, Gregory KA. Maintenance of cholesterol reduction using automated telephone calls. American Journal of Preventive Medicine 1996;12(2):129‐33. [PubMed] [Google Scholar]
Hyman 1998 {published data only}
- Hyman DJ, Ho KS, Dunn JK, Simons‐Morton D. Dietary intervention for cholesterol reduction in public clinic patients. American Journal of Preventive Medicine 1998;15(2):139‐45. [DOI] [PubMed] [Google Scholar]
Jarvis 1997 {published data only}
- Jarvis KL, Friedman RH, Heeren T, Cullinane PM. Older women and physical activity: using the telephone to walk. Womens Health Issues 1997;7(1):24‐9. [DOI] [PubMed] [Google Scholar]
Katalenich 2015 {published data only}
- Katalenich B, Shi L, Liu S, Shao H, McDuffie R, Carpio G, et al. Evaluation of a remote monitoring system for diabetes control. Clinical Therapeutics 2015;37(6):1216‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khanna 2014 {published data only}
- Khanna R, Stoddard PJ, Gonzales EN, Villagran‐Flores M, Thomson J, Bayard P, et al. An automated telephone nutrition support system for Spanish‐speaking patients with diabetes. Journal of Diabetes Science and Technology 2014‐20;8(6):1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna RR, Stoddard PJ, Villagran‐Flores M, Bayard P, Thompson J, Gonzales R. An automated telephone nutrition support system for Spanish‐speaking patients with diabetes. Journal of General Internal Medicine 2012;27(Suppl 2):S116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2014 {published data only}
- Kim S, Ruiz‐Barros V, Tang A, Kuo C, Quan J, Horton C, et al. Provider‐augmented automated telephone self‐management (ATSM) lowers A1C in a high‐risk, safety net population. Diabetes 2014;63:A84. [Google Scholar]
King 2007 {published data only}
- Hekler EB, Buman MP, Otten J, Castro CM, Grieco L, Marcus B, et al. Determining who responds better to a computer‐ vs. human‐delivered physical activity intervention: results from the community health advice by telephone (CHAT) trial. International Journal of Behavioral Nutrition and Physical Activity 2013;10(109):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Friedman R, Marcus B, Castro C, Napolitano M, Ahn D, et al. Ongoing physical activity advice by human versus computers: the community health advice by telephone (CHAT) trial. Health Psychology 2007;26(6):718‐27. [DOI] [PubMed] [Google Scholar]
- King AC, Hekler EB, Castro CM, Buman MP, Marcus BH, Friedman RH, et al. Exercise advice by humans versus computers: maintenance effects at 18 months. Health Psychology 2014;33(2):192‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kroenke 2010 {published data only}
- Kroenke K, Theobald D, Norton K, Sanders R, Schlundt S, McCalley S, et al. The Indiana Cancer Pain and Depression (INCPAD) trial. Design of a telecare management intervention for cancer‐related symptoms and baseline characteristics of study participants. General Hospital Psychiatry 2009;31(3):240‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Theobald D, Wu J, Norton K, Morrison G, Carpenter J, et al. Effect of telecare management on pain and depression in patients with cancer: a randomised trial. JAMA ‐ Journal of the American Medical Association 2010;304(2):163‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kroenke 2014 {published data only}
- Kroenke K, Krebs E, Wu J, Bair MJ, Damush T, Chumbler N, et al. Stepped Care to Optimize Pain care Effectiveness (SCOPE) trial study design and sample characteristics. Contemporary Clinical Trials 2013;34(2):270‐81. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Krebs EE, Wu J, Yu Z, Chumbler NR, Bair MJ. Telecare collaborative management of chronic pain in primary care: a randomised clinical trial. JAMA 2014;312(3):240‐8. [DOI] [PubMed] [Google Scholar]
- Scott E, Kroenke K, Wu J, Yu Z. Reductions in depression, anxiety and pain catastrophising predict fewer pain disability days and lower pain intensity among primary care patients. Journal of Pain 2014;15(4):S12. [Google Scholar]
Krum 2013 {published data only}
- Krum H, Forbes A, Yallop J, Driscoll A, Croucher J, Chan B, et al. Telephone support to rural and remote patients with heart failure: the Chronic Heart Failure Assessment by Telephone (CHAT) study. Cardiovascular Therapeutics 2013;31(4):230‐7. [DOI] [PubMed] [Google Scholar]
Kurtz 2011 {published data only}
- Kurtz B, Lemercier M, Pouchin SC, Benmokhtar E, Vallet C, Cribier A, et al. Automated home telephone self‐monitoring reduces hospitalisation in patients with advanced heart failure. Journal of Telemedicine & Telecare 2011;17(6):298‐302. [DOI] [PubMed] [Google Scholar]
LeBaron 2004 {published data only}
- LeBaron CW, Starnes DM, Rask KJ. The impact of reminder‐recall interventions on low vaccination coverage in an inner‐city population. Archives of Pediatrics & Adolescent Medicine 2004;158(3):255‐61. [DOI] [PubMed] [Google Scholar]
Leirer 1991 {published data only}
- Leirer VO, Morrow DG, Tanke ED, Pariante GM. Elders' nonadherence: its assessment and medication reminding by voice mail. Gerontologist 1991;31(4):514‐20. [DOI] [PubMed] [Google Scholar]
Lieu 1998 {published data only}
- Lieu TA, Capra AM, Makol J, Black SB, Shinefield HR. Effectiveness and cost‐effectiveness of letters, automated telephone messages, or both for underimmunised children in a health maintenance organization. Pediatrics 1998a;101(4):E3. [DOI] [PubMed] [Google Scholar]
Lim 2013 {published data only}
- Lim MC, Watnik MR, Imson KR, Porter SM, Granier AM. Adherence to glaucoma medication: The effect of interventions and association with personality type. Journal of Glaucoma 2013;22(6):439‐46. [DOI] [PubMed] [Google Scholar]
Linkins 1994 {published data only}
- Linkins RW, Dini EF, Watson G, Patriarca PA. A randomised trial of the effectiveness of computer‐generated telephone messages in increasing immunization visits among preschool children. Archives of Pediatrics & Adolescent Medicine 1994;148(9):908‐14. [DOI] [PubMed] [Google Scholar]
Litt 2009 {published data only}
- Litt MD, Kadden RM, Kabela‐Cormier E. Individualized assessment and treatment program for alcohol dependence: results of an initial study to train coping skills. Addiction 2009;104(11):1837‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorig 2008 {published data only}
- Lorig K, Ritter PL, Villa F, Piette JD. Spanish diabetes self‐management with and without automated telephone reinforcement: two randomised trials. Diabetes Care 2008;31(3):408‐414. [DOI] [PubMed] [Google Scholar]
Magid 2011 {published data only}
- Magid DJ, Ho PM, Olson KL, Brand DW, Welch LK, Snow KE, et al. A multimodal blood pressure control intervention in 3 healthcare systems. American Journal of Managed Care 2011;17(4):e96‐103. [PubMed] [Google Scholar]
- Magid DJ, Olson KL, Billups SJ, Wagner NM, Lyons EE, Kroner BA. A pharmacist‐led, American Heart Association Heart360 Web‐enabled home blood pressure monitoring program. Circulation. Cardiovascular quality and outcomes 2013;6(2):157‐63. [DOI] [PubMed] [Google Scholar]
Mahoney 2003 {published data only}
- Mahoney DF, Tarlow BJ, Jones RN. Effects of an automated telephone support system on caregiver burden and anxiety: findings from the REACH for TLC intervention study. Gerontologist 2003;43(4):556‐67. [DOI] [PubMed] [Google Scholar]
- Mahoney DM, Tarlow B, Jones RN, Tennstedt S, Kasten L. Factors affecting the use of a telephone‐based intervention for caregivers of people with Alzheimer's disease. Journal of Telemedicine and Telecare 2001;7(3):139‐48. [DOI] [PubMed] [Google Scholar]
Maxwell 2001 {published data only}
- Maxwell S, Maljanian R, Horowitz S, Pianka MA, Cabrera Y, Greene J. Effectiveness of reminder systems on appointment adherence rates. Journal of Health Care for the Poor & Underserved 2001;12(4):504‐14. [DOI] [PubMed] [Google Scholar]
McNaughton 2013 {published data only}
- McNaughton B, Frohlich J, Graham A, Young QR. Extended interactive voice response telephony (IVR) for relapse prevention after smoking cessation using varenicline and IVR: a pilot study. BMC Public Health 2013;13:824. [DOI] [PMC free article] [PubMed] [Google Scholar]
Migneault 2012 {published data only}
- Migneault JP, Dedier JJ, Wright JA, Heeren T, Campbell MK, Morisky DE, et al. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African‐Americans: a randomised controlled trial. Annals of Behavioral Medicine 2012;43(1):62‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mooney 2014 {published data only}
- American Society of Clinical Oncology. 48th Annual Meeting of the American‐Society‐of‐Clinical‐Oncology (ASCO), JUN 01‐06, 2012, Chicago (IL). Journal of Clinical Oncology 2012;30(15):9137. [AB 9137] [Google Scholar]
- Dunson WA, Mooney K, Bec SL, Wong B, Wujci D. NCCN symptom guidelines coupled with nurse practitioner follow‐up reduce moderate to severe symptom days by half or greater in cancer patients receiving outpatient chemotherapy. Journal of the National Comprehensive Cancer Network 2013;11(3):244. [Google Scholar]
- Mooney K, Beck SL, Wong B, Dunson WA Jr, Wujcik D. An automated telephone remote monitoring system with nurse practitioner follow‐up improves relief of individual symptoms after chemotherapy. Supportive Care in Cancer 2012;20:S253. [Google Scholar]
- Mooney KH, Beck SL, Friedman RH, Farzanfar R, Wong B. Automated monitoring of symptoms during ambulatory chemotherapy and oncology providers' use of the information: a randomised controlled clinical trial. Supportive Care in Cancer 2014;22(9):2343‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 2013 {published data only}
- Moore BA, Cutter CJ, Mahoney AP, Grandpre N. Call behaviour and reported drug use within an automated telephone‐based treatment system for methadone patients. Drug and Alcohol Dependence 2015;146:e45. [Google Scholar]
- Moore BA, Fazzino T, Barry DT, Fiellin DA, Cutter CJ, Schottenfeld RS, et al. The Recovery Line: a pilot trial of automated, telephone‐based treatment for continued drug use in methadone maintenance. Journal of Substance Abuse Treatment 2013;45(1):63‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morey 2009 {published data only}
- Hall KS, Crowley GM, Bosworth HB, Howard TA, Morey MC. Individual progress toward self‐selected goals among older adults enrolled in a physical activity counselling intervention. Journal of Aging and Physical Activity 2010;18(4):439‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Crowley GM, McConnell ES, Bosworth HB, Sloane R, Ekelund CC, et al. Change in goal ratings as a mediating variable between self‐efficacy and physical activity in older men. Annals of Behavioral Medicine 2010;39(3):267‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman KM, Hall KS, Sloane R, Peterson MJ, Bosworth HB, Ekelund C, et al. Is diabetes associated with poorer self‐efficacy and motivation for physical activity in older adults with arthritis?. Scandinavian Journal of Rheumatology 2010;39(5):380‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman KM, Sloane R, Peterson MJ, Bosworth HB, Ekelund C, Pearson M, et al. The impact of self‐reported arthritis and diabetes on response to a home‐based physical activity counselling intervention. Scandinavian Journal of Rheumatology 2010;39(3):233‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lum H, Sloane R, Huffman KM, Kraus VB, Thompson DK, Kraus WE, et al. Plasma acylcarnitines are associated with physical performance in elderly men. The Journals of Gerontology. Series A, Biological sciences and medical sciences 2011;66(5):548‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey MC, Peterson MJ, Pieper CF, Sloane R, Crowley GM, Cowper P, et al. Project LIFE‐ Learning to Improve Fitness and function in Elders: methods, design, and baseline characteristics of randomised trial. Journal of Rehabilitation Research & Development 2008;45(1):31‐42. [DOI] [PubMed] [Google Scholar]
- Morey MC, Peterson MJ, Pieper CF, Sloane R, Crowley GM, Cowper PA, et al. The Veterans Learning to Improve Fitness and Function in Elders Study: a randomized trial of primary care‐based physical activity counseling for older men. Journal of the American Geriatrics Society 2009;57(7):1166‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morey 2012 {published data only}
- Hall KS, Beckham JC, Bosworth HB, Sloane R, Pieper CF, Morey MC. PTSD is negatively associated with physical performance and physical function in older overweight military Veterans. Journal of Rehabilitation Research and Development 2014;51(2):285‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Pieper CF, Edelman DE, Yancy WS Jr, Green JB, Lum H, et al. Lessons learned when innovations go awry: a baseline description of a behavioural trial‐the Enhancing Fitness in Older Overweight Veterans with Impaired Fasting Glucose study. Translational Behavioral Medicine 2011;1(4):573‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey MC, Pieper CF, Edelman DE, Yancy Jr WS, Green JB, Lum H, et al. Enhanced fitness: A randomised controlled trial of the effects of home‐based physical activity counselling on glycaemic control in older adults with prediabetes mellitus. Journal of the American Geriatrics Society 2012;60(9):1655‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Povsic TJ, Sloane R, Green JB, Zhou J, Pieper CF, Pearson MP, et al. Depletion of circulating progenitor cells precedes overt diabetes: a substudy from the VA enhanced fitness trial. Journal of Diabetes and its Complications. 2013;27(6):633‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Povsic TJ, Sloane R, Zhou J, Pieper CF, Pearson MP, Peterson ED, et al. Lower levels of circulating progenitor cells are associated with low physical function and performance in elderly men with impaired glucose tolerance: a pilot substudy from the VA Enhanced Fitness trial. The Journals of Gerontology. Series A, Biological sciences and medical sciences 2013;68(12):1559‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turer CB, Bernstein IH, Edelman DE, Yancy WS, Jr. Low HDL predicts differential blood pressure effects from two weight‐loss approaches: a secondary analysis of blood pressure from a randomised, clinical weight‐loss trial. Diabetes, Obesity and Metabolism 2012;14(4):375‐8. [DOI] [PubMed] [Google Scholar]
Mosen 2010 {published data only}
- Mosen DM, Feldstein AC, Perrin N, Rosales AG, Smith DH, Liles EG, et al. Automated telephone calls improved completion of fecal occult blood testing. Medical Care 2010;48(7):604‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DH, Feldstein AC, Perrin N, Rosales AG, Mosen DM, Liles EG, et al. Automated telephone calls to enhance colorectal cancer screening: economic analysis. American Journal of Managed Care 2012;18(11):691‐9. [PMC free article] [PubMed] [Google Scholar]
Mu 2013 {published data only}
- Mu Y, Rudkin K, Lou Y, Ewing S, Taitel M. Impact of automated telephonic reminders on patient ontime medication refills: initial findings of a randomised study. Value in Health 2013;16(3):A33. [Google Scholar]
Mundt 2006 {published data only}
- Mundt JC, Moore HK, Bean P. An interactive voice response program to reduce drinking relapse: a feasibility study. Journal of Substance Abuse Treatment 2006;30(1):21‐9. [DOI] [PubMed] [Google Scholar]
Nassar 2014 {published data only}
- Nassar AF, Alemi F, Hetmyer A, Alemi Y, Randolph LA, Ramey SL. Automated monitoring to detect H1N1 symptoms among urban, Medicaid‐eligible, pregnant women: a community‐partnered randomised controlled trial. Journal of Community Health 2014;39(1):159‐66. [DOI] [PubMed] [Google Scholar]
Naylor 2008 {published data only}
- Naylor M, Krauthamer M, Cloud G. Interactive voice response as a therapeutic tool for chronic pain and opioid use reduction. European Journal of Pain 2009;13:S269‐S70. [Google Scholar]
- Naylor MR, Keefe FJ, Brigidi B, Naud S, Helzer JE. Therapeutic Interactive Voice Response for chronic pain reduction and relapse prevention. Pain 2008;134(3):335‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor MR, Naud S, Keefe FJ, Helzer JE. Therapeutic interactive voice response (TIVR) to reduce analgesic medication use for chronic pain management. Journal of Pain 2010;11(12):1410‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ownby 2012 {published data only}
- Ownby RL, Hertzog C, Czaja SJ. Tailored information and automated reminding to improve medication adherence in Spanish‐ and English‐speaking elders treated for memory impairment. Clinical Gerontologist 2012;35(3):1‐17. [DOI: 10.1080/07317115.2012.657294] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parikh 2010 {published data only}
- Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The effectiveness of outpatient appointment reminder systems in reducing no‐show rates. American Journal of Medicine 2010;123(6):542‐8. [DOI] [PubMed] [Google Scholar]
Patel 2007 {published data only}
- Patel MH, Schaaf DT, Flores DN, Fleszar GJ, Jan SA. The impact of interactive voice recognition technology on adherence to statin therapy. Value in Health 2007;10(3):A57‐A8. [Google Scholar]
Peng 2013 {published data only}
- Peng WB. Evaluation of a web‐phone intervention system on preventing smoking relapse. Dissertation Abstracts International Section A: Humanities and Social Sciences 2011;72(3‐A):1083. [Google Scholar]
- Peng WB. Schoech D. Evaluation of a web‐phone intervention system in changing smoking behaviour—a randomized controlled trial. Journal of Technology in Human Services 2013;31(3):248–68. [Google Scholar]
- Schoech D, Bolton KW. Automating and supporting care management using web‐phone technology: results of the 5‐year Teleherence project. Journal of Technology in Human Services 2015;33(1):16‐37. [Google Scholar]
Phillips 2015 {published data only}
- Phillips L, Hendren S, Humiston S, Winters P, Fiscella K. Improving breast and colon cancer screening rates: a comparison of letters, automated phone calls, or both. Journal of the American Board of Family Medicine 2015;28(1):46‐54. [DOI] [PubMed] [Google Scholar]
Piette 2000 {published data only}
- Piette JD. Perceived access problems among patients with diabetes in two public systems of care. Journal of General Internal Medicine 2000;15(11):797‐804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, McPhee SJ, Weinberger M, Mah CA, Kraemer FB. Use of automated telephone disease management calls in an ethnically diverse sample of low‐income patients with diabetes. Diabetes Care 1999;22(8):1302‐9. [DOI] [PubMed] [Google Scholar]
- Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow‐up on patient‐centred outcomes of diabetes care: a randomised, controlled trial. Medical Care 2000;38(2):218‐30. [DOI] [PubMed] [Google Scholar]
- Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Can automated calls with nurse follow‐up improve self‐care and glycaemic control among vulnerable patients with diabetes? A randomised controlled trial. American Journal of Medicine 2000;108:20‐7. [DOI] [PubMed] [Google Scholar]
- Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow‐up improve self‐care and glycaemic control among vulnerable patients with diabetes?. American Journal of Medicine 2000;108(1):20‐7. [DOI] [PubMed] [Google Scholar]
Piette 2001 {published data only}
- Piette JD. Perceived access problems among patients with diabetes in two public systems of care. Journal of General Internal Medicine 2000;15(11):797‐804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, Kraemer FB, Weinberger M, McPhee SJ. Impact of automated calls with nurse follow‐up on diabetes treatment outcomes in a department of veterans affairs health care system. Diabetes Care 2001;24:202‐208. [DOI] [PubMed] [Google Scholar]
Piette 2012 {published data only}
- Piette JD, Datwani H, Gaudioso S, Foster SM, Westphal J, Perry W, et al. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle income countries. Telemedicine and e‐Health 2012;18(8):613‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, Marinec N, Gallegos‐Cabriales EC, Gutierrez‐Valverde JM, Rodriguez‐Saldana J, Mendoz‐Alevares M, et al. Spanish‐speaking patients' engagement in interactive voice response (IVR) support calls for chronic disease self‐management: Data from three countries. Journal of Telemedicine and Telecare 2013;19(2):89‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinto 2002 {published data only}
- Delichatsios HK, Friedman RH, Glanz K, Tennstedt S, Smigelski C, Pinto BM, et al. Randomized trial of a "talking computer" to improve adults' eating habits. American Journal of Health Promotion 2001;15(4):215‐24. [DOI] [PubMed] [Google Scholar]
- Glanz K, Shigaki D, Farzanfar R, Pinto B, Kaplan B, Friedman RH. Participant reactions to a computerized telephone system for nutrition and exercise counseling. Patient Education and Counseling 2003;49(2):157‐63. [DOI] [PubMed] [Google Scholar]
- Pinto BM, Friedman R, Marcus BH, Kelley H, Tennstedt S, Gillman MW. Effects of a computer‐based, telephone‐counselling system on physical activity. American Journal of Preventive Medicine 2002;23(2):113‐20. [DOI] [PubMed] [Google Scholar]
Reekie 1998 {published data only}
- Reekie D, Devlin H. Preventing failed appointments in general dental practice: a comparison of reminder methods. British Dental Journal 1998;185(9):472‐4. [DOI] [PubMed] [Google Scholar]
Regan 2011 {published data only}
- Regan S, Reyen M, Lockhart AC, Richards AE, Rigotti NA. An interactive voice response system to continue a hospital‐based smoking cessation intervention after discharge. Nicotine & Tobacco Research 2011;13(4):255‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reid 2007 {published data only}
- Reid RD, Pipe AL, Quinlan B, Oda J. Interactive voice response telephony to promote smoking cessation in patients with heart disease: a pilot study. Patient Education & Counseling 2007;66(3):319‐26. [DOI] [PubMed] [Google Scholar]
Reid 2011 {published data only}
- Canadian Cardiovascular Society. 64th Annual Meeting of the Canadian Cardiovascular Society; Vancouver, BC. Canadian Journal of Cardiology 2011;27(5 Suppl 1):S67. [Google Scholar]
Reynolds 2011 {published data only}
- Reynolds K, Green KR, Vansomphone SS, Scott RD, Cheetham TC. Automated outreach for cholesterol‐lowering medication refill reminders. European Heart Journal 2011;32(Suppl 1):230‐1. [Google Scholar]
Rigotti 2014 {published data only}
- Japuntich SJ, Regan S, Viana J, Tymoszczuk J, Reyen M, Levy DE, et al. Comparative effectiveness of post‐discharge interventions for hospitalised smokers: study protocol for a randomised controlled trial. Trials 2012;13(124):1‐13. [DOI: 10.1186/1745-6215-13-124] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti NA, Regan S, Levy DE, Japuntich S, Chang Y, Park ER, et al. Sustained care intervention and postdischarge smoking cessation among hospitalised adults a randomised clinical trial. JAMA ‐ Journal of the American Medical Association 2014;312(7):719‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Society of General Internal Medicine. 36 th Annual Meeting of the Society‐of‐General‐Internal‐Medicine, APR 24‐27, 2013, Denver (CO). Journal of General Internal Medicine 2013;28(Suppl 1):S160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rose 2015 {published data only}
- Rose GL, Skelly JM, Badger GJ, Ferraro TA, Helzer JE. Efficacy of automated telephone continuing care following outpatient therapy for alcohol dependence. Addictive Behaviors 2015;41:223‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose GL, Skelly JS, Badger GJ, Helzer JE. Continuing care after outpatient CBT: a randomised trial of alcohol therapeutic interactive voice response for relapse prevention. Alcoholism: Clinical and Experimental Research 2013;37 Special Issue(Suppl 2):200A. [Google Scholar]
Rubin 2012 {published data only}
- Rubin A, Cunniff E, Saitz R, Heeren T, Gulliver SB, Friedman RH. An IVR multi‐session treatment program for risky drinkers: initial efficacy. Alcoholism: Clinical and Experimental Research 2012;36:0421. [Google Scholar]
Schillinger 2009 {published data only}
- Handley MA, Shumway M, Schillinger D. Cost‐effectiveness of automated telephone self‐management support with nurse care management among patients with diabetes. Annals of Family Medicine 2008;6(6):512‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyles CR, Schillinger D, Lopez A, Handley M, Ratanawongsa N, Sarkar U. Safety events during an automated telephone self‐management support intervention. Journal of Diabetes Science and Technology 2013;7(3):596‐601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratanawongsa N, Bhandari VK, Handley M, Rundall T, Hammer H, Schillinger D. Primary care provider perceptions of the effectiveness of two self‐management support programs for vulnerable patients with diabetes. Journal of Diabetes Science and Technology 2012;6(1):116‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar U, Handley MA, Gupta R, Tang A, Murphy E, Seligman HK, et al. Use of an interactive, telephone‐based self‐management support program to identify adverse events among ambulatory diabetes patients. Journal of General Internal Medicine 2008;23(4):459‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger D, Hammer H, Wang F, Palacios J, McLean I, Tang A, et al. Seeing in 3‐D: examining the reach of diabetes self‐management support strategies in a public health care system. Health Education & Behavior 2008;35(5):664‐82. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Wang F, Handley M, Hammer H. Effects of self‐management support on structure, process, and outcomes among vulnerable patients with diabetes. Diabetes Care 2009;32(4):559‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace A, Perkhounkova Y, Tseng H, Schillinger D. Influence of patient characteristics on assessment of diabetes self‐management support. Nursing Research and Practice 2013;62(2):106‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sherrard 2009 {published data only}
- Sherrard H, Struthers C, Kearns SA, Wells G, Chen L, Mesana T. Using technology to create a medication safety net for cardiac surgery patients: a nurse‐led randomised control trial. Canadian Journal of Cardiovascular Nursing 2009;19(3):9‐15. [PubMed] [Google Scholar]
Shet 2014 {published data only}
- Costa A, Shet A, Kumarasamy N, Ashorn P, Eriksson B, Bogg L, et al. Design of a randomised trial to evaluate the influence of mobile phone reminders on adherence to first line antiretroviral treatment in South India‐‐the HIVIND study protocol. BMC Medical Research Methodology 2010;10:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues R, Bogg L, Shet A, Kumar DS, Costa A. Mobile phones to support adherence to antiretroviral therapy: what would it cost the Indian National AIDS Control Programme?. Journal of the International AIDS Society 2014;17:19036. [DOI: 10.7448/IAS.17.1.19036] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues R, Shet A, Swaroop N, Shastri S, Bogg L, Costa A. Mobile phone adherence support for antiretroviral therapy: what would it cost the National AIDS Control Program in India?. Journal of the International AIDS Society 2012;15:278‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shet A, Costa A, Kumarasamy N, Rodrigues R, Bewari BB, Ashorn P, et al. Effect of mobile telephone reminders on treatment outcome in HIV: evidence from a randomised controlled trial in India. British Medical Journal 2014;349:g5978. [DOI: 10.1136/bmj.g5978] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siegel 1992 {published data only}
- Christ G, Siegel K. Monitoring quality‐of‐life needs of cancer patients. Cancer 1990;65(3 Suppl):760‐5. [DOI] [PubMed] [Google Scholar]
- Siegel K, Mesagno FP, Chen JY, Klein L, Bowles ME, McKenna M, et al. Computerized telephone assessment of the 'concrete' needs of chemotherapy outpatients: a feasibility study. Journal of Clinical Oncology 1988;6(11):1760‐7. [DOI] [PubMed] [Google Scholar]
- Siegel K, Mesagno FP, Karus DG, Christ G. Reducing the prevalence of unmet needs for concrete services of patients with cancer: evaluation of a computerized telephone outreach system. Cancer 1992;69(7):1873‐83. [DOI] [PubMed] [Google Scholar]
Sikorskii 2007 {published data only}
- Given C, Given B, Jeon S, Sikorskii A, Champion V, McCorkle R. A randomised trial comparing a nurse delivered intervention with an automated voice intervention for managing symptoms among cancer patients. Psycho‐oncology 2006;15(1):6‐7. [Google Scholar]
- Given C, Sikorskii A, Siddiqi A, Given, B. Comparing cognitive behavioural and educational strategies; does age moderate the impact of interventions on symptom severity among cancer patients. Psycho‐oncology 2009;18(Suppl):S71‐S72. [Google Scholar]
- Given CW, Bradley C, You M, Sikorskii A, Given B. Costs of novel symptom management interventions and their impact on hospitalizations. Journal of Pain and Symptom Management 2010;39(4):663‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given CW, Sikorskii A, Tamkus D, Given B, You M, McCorkle R, et al. Managing symptoms among patients with breast cancer during chemotherapy: results of a two‐arm behavioral trial. Journal of Clinical Oncology 2008;26(36):5855‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikorskii A, Given CW, Given B, Jeon S, Decker V, Decker D, et al. Symptom management for cancer patients: a trial comparing two multimodal interventions. Journal of Pain & Symptom Management 2007;34(3):253‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikorskii A, Given CW, Given B, Jeon S, You M. Differential symptom reporting by mode of administration of the assessment: automated voice response system versus a live telephone interview. Medical Care 2009;47(8):866‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikorskii A, Given CW, Siddiqi AEA, Champion V, McCorkle R, Spoelstra SL, et al. Testing the differential effects of symptom management interventions in cancer. Psycho‐Oncology 2015;24(1):25‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikorskii A, Given CW, You M, Jeon S, Given BA. Response analysis for multiple symptoms revealed differences between arms of a symptom management trial. Journal of Clinical Epidemiology 2009;62(7):716‐724. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2010a {published data only}
- Simon SR, Zhang F, Soumerai SB, Ensroth A, Bernstein L, Fletcher RH, et al. Failure of automated telephone outreach with speech recognition to improve colorectal cancer screening: a randomised controlled trial. Archives of Internal Medicine 2010;170(3):264‐270. [DOI] [PubMed] [Google Scholar]
Simon 2010b {published data only}
- Simon SR, Trinacty CM, Soumerai SB, Piette JD, Meigs JB, Shi P, et al. Improving diabetes care among patients overdue for recommended testing: a randomised controlled trial of automated telephone outreach. Diabetes Care 2010;33(7):1452‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simpson 2005 {published data only}
- Simpson TL, Kivlahan DR, Bush KR, McFall ME. Telephone self‐monitoring among alcohol use disorder patients in early recovery: a randomised study of feasibility and measurement reactivity. Drug and Alcohol Dependence 2005a;79:241–50. [DOI] [PubMed] [Google Scholar]
Solomon 2007 {published data only}
- Polinski JM, Patrick A, Truppo C, Breiner L, Chen YT, Egan C, et al. Interactive voice response telephone calls to enhance bone mineral density testing. American Journal of Managed Care 2006;12(6):321‐5. [PubMed] [Google Scholar]
- Shu AD, Stedman MR, Polinski JM, Jan SA, Patel M, Truppo C, et al. Adherence to osteoporosis medications after patient and physician brief education: post hoc analysis of a randomised controlled trial. American Journal of Managed Care 2009;15(7):417‐24. [PMC free article] [PubMed] [Google Scholar]
- Solomon DH, Polinski JM, Stedman M, Truppo C, Breiner L, Egan C, et al. Improving care of patients at‐risk for osteoporosis: a randomised controlled trial. Journal of General Internal Medicine 2007;22(3):362‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sparrow 2010 {published data only}
- Sparrow D, Aloia M, Demolles DA, Gottlieb DJ. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax 2010;65(12):1061‐6. [DOI] [PubMed] [Google Scholar]
Sparrow 2011 {published data only}
- Sparrow D, Gottlieb DJ, Demolles D, Fielding RA. Increases in muscle strength and balance using a resistance training program administered via a telecommunications system in older adults. The Journals of Gerontology. Series A, Biological sciences and medical sciences 2011;66(11):1251‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spoelstra 2013 {published data only}
- Spoelstra SL, Given BA, Given CW, Grant M, Sikorskii A, You M, et al. An intervention to improve adherence and management of symptoms for patients prescribed oral chemotherapy agents: an exploratory study. Cancer Nursing 2013;36(1):18‐28. [DOI] [PubMed] [Google Scholar]
Stacy 2009 {published data only}
- Stacy JN, Schwartz SM, Ershoff D, Shreve MS. Incorporating tailored interactive patient solutions using interactive voice response technology to improve statin adherence: results of a randomised clinical trial in a managed care setting. Population Health Management 2009;12(5):241‐54. [DOI] [PubMed] [Google Scholar]
Stehr‐Green 1993 {published data only}
- Stehr‐Green PA, Dini EF, Lindegren ML, Patriarca PA. Evaluation of telephoned computer‐generated reminders to improve immunization coverage at inner‐city clinics. Public Health Reports 1993;108(4):426‐30. [PMC free article] [PubMed] [Google Scholar]
Stuart 2003 {published data only}
- Stuart GW, Laraia MT, Ornstein SM, Nietert PJ. An interactive voice response system to enhance antidepressant medication compliance. Topic in Health Information Management 2003;24(1):15‐20. [PubMed] [Google Scholar]
Szilagyi 2006 {published data only}
- Szilagyi PG, Schaffer S, Barth R, Shone LP, Humiston SG, Ambrose S, et al. Effect of telephone reminder/recall on adolescent immunization and preventive visits: results from a randomised clinical trial. Archives of Pediatrics & Adolescent Medicine 2006;160(2):157‐63. [DOI] [PubMed] [Google Scholar]
Szilagyi 2013 {published data only}
- Szilagyi PG, Albertin C, Humiston SG, Rand CM, Schaffer S, Brill H, et al. A randomised trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Academic Pediatrics 2013;13(3):204‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tanke 1994 {published data only}
- Tanke ED, Leirer VO. Automated telephone reminders in tuberculosis care. Medical Care 1994;32(4):380‐389. [DOI] [PubMed] [Google Scholar]
Tanke 1997 {published data only}
- Tanke ED, Martinez CM, Leirer VO. Use of automated reminders for tuberculin skin test return. American Journal of Preventive Medicine 1997;13(3):189‐192. [PubMed] [Google Scholar]
Tucker 2012 {published data only}
- Schroder KE, Tucker JA, Simpson CA. Telephone‐based self‐change modules help stabilize early natural recovery in problem drinkers. Journal of Studies on Alcohol and Drugs 2013;74(6):902‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson CA, Huang J, Roth DL, Chandler SD, Tucker JA. Predictors of utilization of an IVR self‐monitoring program by problem drinkers with recent natural resolutions. Drug and Alcohol Dependence 2012;126(1‐2):111‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Blum ER, Xie L, Roth DL, Simpson CA. Interactive voice response self‐monitoring to assess risk behaviours in rural substance users living with HIV/AIDS. AIDS Behaviors 2012;16(2):432‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Roth DL, Huang J, Crawford MS, Simpson CA. Effects of interactive voice response self‐monitoring on natural resolution of drinking problems: utilization and behavioral economic factors. Journal of Studies on Alcohol and Drugs 2012;73(4):686‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vance 2011 {published data only}
- Vance DE, Wright MA, McKie PR, Burton L, Ard J, Klapow J, et al. Evaluating the impact of an interactive telephone technology and incentives when combined with a behavioral intervention for weight loss. Obesity 2011;19:S115. [Google Scholar]
Velicer 2006 {published data only}
- Velicer WF, Friedman RH, Fava JL, Gulliver SB, Keller S, Sun XW, et al. Evaluating nicotine replacement therapy and stage‐based therapies in a population‐based effectiveness trial. Journal of Consulting and Clinical Psychology 2006;74(6):1162‐72. [DOI] [PubMed] [Google Scholar]
Vollmer 2006 {published data only}
- American Thoracic Society. American Thoracic Society International Conference; May 15‐20 2009; San Diego (CA). AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE 2009;179:A1089. [DOI: ] [Google Scholar]
- Feldstein A, Vollmer W, Rand C. Automated phone calls improved adherence to inhaled corticosteroids. Value in Health 2009;12(7):A490. [Google Scholar]
- Vollmer WM, Kirshner M, Peters D, Drane A, Stibolt T, Hickey T, et al. Use and impact of an automated telephone outreach system for asthma in a managed care setting. American Journal of Managed Care 2006;12(12):725‐33. [PubMed] [Google Scholar]
Vollmer 2011 {published data only}
- Owen‐Smith A, Vupputuri S, Rand C, Tom J, Williams A, Smith D, et al. The patient study: lessons learned during the development of a multi‐site, pragmatic randomised control trial in a large health maintenance organization. Circulation 2012;125(Suppl 10):AP146. [Abstract P146] [Google Scholar]
- Schneider J, Waterbury A, Feldstein A, Donovan J, Vollmer WM, Dubanoski J, et al. Maximizing acceptability and usefulness of an automated telephone intervention: lessons from a developmental mixed‐methods approach. Health Informatics Journal 2011;17(1):72‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer WM, Feldstein A, Smith DH, Dubanoski JP, Waterbury A, Schneider JL, et al. Use of health information technology to improve medication adherence. American Journal of Managed Care 2011;17(Special issue):SP79‐SP87. [PMC free article] [PubMed] [Google Scholar]
- Vollmer WM, Xu M, Feldstein A, Smith D, Waterbury A, Rand C. Comparison of pharmacy‐based measures of medication adherence. BMC Health Services Research 2012;12:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vollmer 2014 {published data only}
- Vollmer WM, Owen‐Smith AA, Tom JO, Laws R, Ditmer DG, Smith DH, et al. Improving adherence to cardiovascular disease medications with information technology. American Journal of Managed Care 2014;20(11 Spec No. 17):SP502‐10. [PMC free article] [PubMed] [Google Scholar]
Williams 2012 {published data only}
- Bird D, Oldenburg B, Cassimatis M, Russell A, Ash S, Courtney MD, et al. Randomised controlled trial of an automated, interactive telephone intervention to improve type 2 diabetes self‐management (Telephone‐Linked Care Diabetes Project): study protocol. BMC Public Health 2010;10:599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams ED, Bird D, Forbes AW, Russell A, Ash S, Friedman R, et al. Randomised controlled trial of an automated, interactive telephone intervention (TLC Diabetes) to improve type 2 diabetes management: baseline findings and six‐month outcomes. BMC Public Health 2012;3(12):602. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wright 2013 {published data only}
- Wright JA, Phillips BD, Watson BL, Newby PK, Norman GJ, Adams WG. Randomized trial of a family‐based, automated, conversational obesity treatment program for underserved populations. Obesity (Silver Spring) 2013;21(9):E369‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2010 {published data only}
- Xu C, Jackson M, Scuffham PA, Wootton R, Simpson P, Whitty J, et al. A randomised controlled trial of an interactive voice response telephone system and specialist nurse support for childhood asthma management. Journal of Asthma 2010;47(7):768‐73. [DOI] [PubMed] [Google Scholar]
Yount 2014 {published data only}
- Yount SE, Rothrock N, Bass M, Beaumont JL, Pach D, Lad T, et al. A randomized trial of weekly symptom telemonitoring in advanced lung cancer. Journal of Pain and Symptom Management 2014;47(6):973‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zautra 2012 {published data only}
- Zautra AJ, Davis MC, Reich JW, Sturgeon JA, Arewasikporn A. An examination of automated telephone interventions in mindfulness and mastery for depressed community residents. Psychosomatic Medicine 2012;74(3):A91‐A92. [Google Scholar]
References to studies excluded from this review
Aarons 2012 {published data only}
- Aarons GA, Green AE, Palinkas LA, Self‐Brown S, Whitaker DJ, Lutzker JR, et al. Dynamic adaptation process to implement an evidence‐based child maltreatment intervention. Implementation Science: IS 2012;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Abbott 2013 {published data only}
- Abbott SA, Friedland BA, Sarna A, Katzen LL, Rawiel U, Srikrishnan AK, et al. An evaluation of methods to improve the reporting of adherence in a placebo gel trial in Andhra Pradesh, India. AIDS & Behavior 2013;17(6):2222‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Adie 2010 {published data only}
- Adie K, James MA. Does telephone follow‐up improve blood pressure after minor stroke or TIA. Age and Ageing 2010;39(5):598‐603. [DOI] [PubMed] [Google Scholar]
Agel 2001 {published data only}
- Agel J, Rockwood T, Mundt JC, Greist JH, Swiontkowski M. Comparison of Interactive voice response and written self‐administered patient surveys for clinical research. Orthopedics 2001;24(12):1155‐7. [DOI] [PubMed] [Google Scholar]
Aharonovich 2006 {published data only}
- Aharonovich E, Hatzenbuehler M L, Johnston B, O'Leary A, Morgenstern J, Wainberg M L, et al. A low‐cost, sustainable intervention for drinking reduction in the HIV primary care setting. AIDS Care 2006;18(6):561‐8. [DOI] [PubMed] [Google Scholar]
Aikens 2015a {published data only}
- Aikens JE, Rosland AM, Piette JD. Improvements in illness self‐management and psychological distress associated with telemonitoring support for adults with diabetes. Primary Care Diabetes 2015;9(2):127‐134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aikens 2015b {published data only}
- Aikens JE, Trivedi R, Aron DC, Piette JD. Integrating support persons into diabetes telemonitoring to improve self‐management and medication adherence. Journal of General Internal Medicine 2015;30(3):319‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Albert 2014 {published data only}
- Albert SM, King J, Boudreau R, Prasad T, Lin CJ, Newman AB. Primary prevention of falls: effectiveness of a statewide program. American Journal of Public Health 2014;104(5):e77‐e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Albert 2015 {published data only}
- Albert SM, King J, Keene RM. Assessment of an interactive voice response system for identifying falls in a statewide sample of older adults. Preventive Medicine 2015;71:31‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Albisser 2001 {published data only}
- Albisser A M. Clinical studies with home glucose clamping. Annales d'Endocrinologie 2001;62(1 Pt 1):11‐8. [PubMed] [Google Scholar]
Albisser 2005 {published data only}
- Albisser A M, Sakkal S, Wright C. Home blood glucose prediction: validation, safety, and efficacy testing in clinical diabetes. Diabetes Technology & Therapeutics 2005;7(3):487‐96. [DOI] [PubMed] [Google Scholar]
Alemagno 1996 {published data only}
- Alemagno SA, Cochran D, Feucht TE, Stephens RC, Butts JM, Wolfe SA. Assessing substance abuse treatment needs among the homeless: a telephone‐based interactive voice response system. American Journal of Public Health 1996;86(11):1626‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alemi 1994 {published data only}
- Alemi F, Stephens R, Parran T, Llorens S, Bhatt P, Ghadiri A, et al. Automated monitoring of outcomes: application to treatment of drug abuse. Medical Decision Making 1994;14(2):180‐7. [DOI] [PubMed] [Google Scholar]
Alemi 1995 {published data only}
- Alemi F, Higley P. Reaction to "talking" computers assessing health risks. Medical Care 1995;33(3):227‐33. [DOI] [PubMed] [Google Scholar]
Alemi 1996 {published data only}
- Alemi F, Alemagno S A, Goldhagen J, Ash L, Finkelstein B, Lavin A, et al. Computer reminders improve on‐time immunization rates. Medical Care 1996;34(10 Suppl):OS45‐51. [DOI] [PubMed] [Google Scholar]
Alemi 1996a {published data only}
- Alemi F, Stephens RC, Javalghi RG, Dyches H, Butts J, Ghadiri A. A randomized trial of a telecommunications network for pregnant women who use cocaine. Medical Care 1996;34(10 Suppl):OS10‐20. [DOI] [PubMed] [Google Scholar]
Alkema 2007 {published data only}
- Alkema Gretchen E, Wilber Kathleen H, Shannon George R, Allen D. Reduced mortality: the unexpected impact of a telephone‐based care management intervention for older adults in managed care. Health Services Research 2007;42(4):1632‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Allen 2013 {published data only}
- Allen JK, Stephens J, Dennison Himmelfarb CR, Stewart KJ, Hauck S. Randomized controlled pilot study testing use of smartphone technology for obesity treatment. Journal of Obesity 2013;2013(151597):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alsabbagh 2013 {published data only}
- Alsabbagh MW, Lemstra M, Eurich D, Wilson TW, Robertson P, Blackburn DF. Pharmacist intervention in cardiac rehabilitation: a randomised controlled trial. Journal of Cardiopulmonary Rehabilitation and Prevention 2012;32(6):394‐9. [DOI] [PubMed] [Google Scholar]
Altfeld 2013 {published data only}
- Altfeld SJ, Shier GE, Rooney M, Johnson TJ, Golden RL, Karavolos K, et al. Effects of an enhanced discharge planning intervention for hospitalized older adults: a randomized trial. The Gerontologist 2013;53(3):430‐40. [DOI] [PubMed] [Google Scholar]
Anderson 2004 {published data only}
- Anderson ES, Anderson T, Heckman TG, Kalichman SC, Kochman A, Sikkema KJ. Emotional distress in nonmetropolitan persons living with HIV disease enrolled in a telephone‐delivered, coping improvement group intervention. Health Psychology 2004;23(1):94‐100. [DOI] [PubMed] [Google Scholar]
Andersson 2013 {published data only}
- Research Society on Alcoholism. 36th Annual Scientific Meeting of the Research Society on Alcoholism, June 22‐26 – Orlando (FL). Alcoholism: Clinical and Experimental Research 2013;37(Special Issue Suppl 2):260A. [DOI] [PubMed] [Google Scholar]
Andersson 2014 {published data only}
- Andersson C, Danielsson S, Silfverberg‐Dymling G, Löndahl G, Johansson BA. Evaluation of Interactive Voice Response (IVR) and postal survey in follow‐up of children and adolescents discharged from psychiatric outpatient treatment: a randomised controlled trial. Springerplus 2014;3(77):1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arezina 2011 {published data only}
- Arezina CH. The Effect of Interactive Music Therapy on Joint Attention Skills in Preschool Children with Autism Spectrum Disorder [Masters Thesis]. Lawrence: University of Kansas, 2011. [1510876:73] [Google Scholar]
Armstrong 2009 {published data only}
- Armstrong April W, Watson Alice J, Makredes M, Frangos Jason E, Kimball Alexandra B, Kvedar Joseph C. Text‐message reminders to improve sunscreen use: a randomised, controlled trial using electronic monitoring. Archives of Dermatology 2009;145(11):1230‐6. [DOI] [PubMed] [Google Scholar]
Aseltine 2010 {published data only}
- Academic ED SBIRT Research Collaborative. The impact of screening, brief intervention and referral for treatment in emergency department patients' alcohol use: A 3‐, 6‐and 12‐month follow‐up. Alcohol and Alcoholism 2010;45(6):514‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Avery 2004 {published data only}
- Avery L, Clark M, Hampson SE, Simpson R. Effects of a tailored lifestyle self‐management intervention in patients with type 2 diabetes. British Journal of Health Psychology 2004;9(3):365‐79. [DOI] [PubMed] [Google Scholar]
Avery 2004a {published data only}
- Avery L, Clark M, Hampson SE, Simpson R. Effects of a brief tailored intervention on the process and predictors of lifestyle behaviour change in patients with type 2 diabetes. Psychology, Health & Medicine 2004;9(4):440‐9. [DOI] [PubMed] [Google Scholar]
Bambauer 2005 {published data only}
- Bambauer KZ, Aupont O, Stone PH, Locke SE, Mullan MG, Colagiovanni J, et al. The effect of a telephone counselling intervention on self‐rated health of cardiac patients. Psychosomatic Medicine 2005;67(4):539‐45. [DOI] [PubMed] [Google Scholar]
Barohn 2013 {published data only}
- Barohn R, Statland J, Bundy B, Wang Y, Raja Rayan D, Trivedi J, et al. An interactive voice response diary for stiffness in non‐dystrophic myotonia. Clinical and Translational Science 2013;6(2):121. [Google Scholar]
Bartholomew 2011 {published data only}
- Bartholomew ML, Church K, Graham G, Burlingame J, Zalud I, Sauvage L, et al. Managing diabetes in pregnancy using cell phone/internet technology. American Journal of Obstetrics and Gynecology 2011;204(1 Suppl):S113‐S4. [Google Scholar]
Basch 2006 {published data only}
- Basch C E, Wolf R L, Brouse C H, Shmukler C, Neugut A, DeCarlo L T, et al. Telephone outreach to increase colorectal cancer screening in an urban minority population. American Journal of Public Health 2006;96(12):2246‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bastian 2002 {published data only}
- Bastian L A, McBride C M, Fish L, Lyna P, Farrell D, Lipkus I M, et al. Evaluating participants' use of a hormone replacement therapy decision‐making intervention. Patient Education and Counseling 2002;48(3):283‐91. [DOI] [PubMed] [Google Scholar]
Bellazzi 2003 {published data only}
- Bellazzi R, Arcelloni M, Bensa G, Blankenfeld H, Brugues E, Carson E, et al. Design, methods, and evaluation directions of a multi‐access service for the management of diabetes mellitus patients. Diabetes Technology and Therapeutics 2003;5(4):621‐9. [DOI] [PubMed] [Google Scholar]
Bellazzi 2004 {published data only}
- Bellazzi R, Arcelloni M, Ferrari P, Decata P, Hernando ME, Garcia A, et al. Management of patients with diabetes through information technology: Tools for monitoring and control of the patients' metabolic behavior. Diabetes Technology and Therapeutics 2004;6(5):567‐78. [DOI] [PubMed] [Google Scholar]
Berkman 2014 {published data only}
- Berkman ET, Giuliani NR, Pruitt AK. Comparison of text messaging and paper‐and‐pencil for ecological momentary assessment of food craving and intake. Appetite 2014;81:131‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berman 2012 {published data only}
- Berman A, Farzanfar R, Kristiansson M, Carlbring P, Friedman R. Design and development of a telephone‐linked care (TLC) system to reduce impulsivity among violent forensic outpatients and probationers. Journal of Medical Systems 2012;36(3):1031‐42. [DOI] [PubMed] [Google Scholar]
Bexelius 2010 {published data only}
- Bexelius C, Merk H, Sandin S, Nyrén O, Kühlmann‐Berenzon S, Linde A, et al. Interactive voice response and web‐based questionnaires for population‐based infectious disease reporting. European Journal of Epidemiology 2010;25(10):693‐702. [DOI] [PubMed] [Google Scholar]
Bigby 1983 {published data only}
- Bigby J, Giblin J, Pappius E M, Goldman L. Appointment reminders to reduce no‐show rates. A stratified analysis of their cost‐effectiveness. Journal of the American Medical Association 1983;250(13):1742‐5. [PubMed] [Google Scholar]
Bischof 2008 {published data only}
- Bischof G, Grothues JM, Reinhardt S, Meyer C, John U, Rumpf HJ. Evaluation of a telephone‐based stepped care intervention for alcohol‐related disorders: a randomised controlled trial. Drug & Alcohol Dependence 2008;93(3):244‐51. [DOI] [PubMed] [Google Scholar]
Bischof 2010 {published data only}
- Bischof G, Grothues JM, Reinhardt S, Meyer C, John U, Rumpf HJ. Stepped‐care intervention for alcohol problems: A cost‐effective approach for brief interventions in primary care?. Alcoholism: Clinical and Experimental Research 2010;34:29A. [Google Scholar]
Bjorner 2014a {published data only}
- Bjorner JB, Rose M, Gandek B, Stone AA, Junghaenel DU, Ware JE, Jr. Difference in method of administration did not significantly impact item response: an IRT‐based analysis from the Patient‐Reported Outcomes Measurement Information System (PROMIS) initiative. Quality of Life Research 2014;23(1):217‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjorner 2014b {published data only}
- Bjorner JB, Rose M, Gandek B, Stone AA, Junghaenel DU, Ware JE, Jr. Method of administration of PROMIS scales did not significantly impact score level, reliability, or validity. Journal of Clinical Epidemiology 2014;67(1):108‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blackstone 2009 {published data only}
- Blackstone Mercedes M, Wiebe Douglas J, Mollen Cynthia J, Kalra A, Fein Joel A. Feasibility of an interactive voice response tool for adolescent assault victims. Academic Emergency Medicine 2009;16(10):956‐62. [DOI] [PubMed] [Google Scholar]
Bloom 2004 {published data only}
- Bloom PN, Lipkus IM, McBride CM, Pollak KI, Schwartz‐Bloom RD, Tilson E. A randomized trial comparing the effects of self‐help materials and proactive telephone counseling on teen smoking cessation. Health Psychology 2004;23(4):397‐406. [DOI] [PubMed] [Google Scholar]
Blumenthal 2014 {published data only}
- Blumenthal JA, Emery CF, Smith PJ, Keefe FJ, Welty‐Wolf K, Mabe S, et al. The effects of a telehealth coping skills intervention on outcomes in chronic obstructive pulmonary disease: primary results from the INSPIRE‐II study. Psychosomatic Medicine 2014;76(8):581. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boekeloo 1998 {published data only}
- Boekeloo BO, Schamus LA, Simmens SJ, Cheng TL. Ability to measure sensitive adolescent behaviours via telephone. American Journal of Preventive Medicine 1998;14(3):209‐16. [DOI] [PubMed] [Google Scholar]
Boisseau 2010 {published data only}
- Boisseau N, Burde A, Bachmann P, Senesse P, Hebuterne X. A telephone‐linked computer system for home enteral nutrition. Journal of Telemedicine and Telecare 2010;16(7):363‐7. [DOI] [PubMed] [Google Scholar]
Bombardier 2013 {published data only}
- Bombardier CH, Ehde DM, Gibbons LE, Wadhwani R, Sullivan MD, Rosenberg DE, et al. Telephone‐based physical activity counseling for major depression in people with multiple sclerosis. Journal of Consulting and Clinical Psychology 2013;81(1):89‐99. [DOI] [PubMed] [Google Scholar]
Boren 2006 {published data only}
- Boren SA, De LG, Chanetsa F, Donaldson J, Krishna S, Balas E. Evaluation of a Diabetes Education Call Center Intervention. Telemedicine Journal and E‐health 2006;12(4):457‐65. [DOI] [PubMed] [Google Scholar]
Borland 2003 {published data only}
- Borland R, Balmford J, Segan C, Livingston P, Owen N. The effectiveness of personalized smoking cessation strategies for callers to a Quitline service. Addiction 2003;98(6):837‐46. [DOI] [PubMed] [Google Scholar]
Borland 2013 {published data only}
- Borland R, Balmford J, Benda P. Population‐level effects of automated smoking cessation help programs: a randomized controlled trial. Addiction 2013;108(3):618‐28. [DOI] [PubMed] [Google Scholar]
Borsari 2014 {published data only}
- Borsari B, Short EE, Mastroleo NR, Hustad JTP, Tevyaw TOL, Barnett NP, et al. Phone‐delivered brief motivational interventions for mandated college students delivered during the summer months. Journal of Substance Abuse Treatment 2014;46(5):592‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bosworth 2008 {published data only}
- Bosworth HB, Olsen MK, Neary A, Orr M, Grubber J, Svetkey L, et al. Take Control of Your Blood pressure (TCYB) study: a multifactorial tailored behavioral and educational intervention for achieving blood pressure control. Patient Education and Counseling 2008;70(3):338‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bowen 2010 {published data only}
- Bowen DJ, Powers D. Effects of a mail and telephone intervention on breast health behaviors. Health Education & Behavior 2010;37(4):479‐89. [DOI] [PubMed] [Google Scholar]
Brown 2004 {published data only}
- Brown KS, Cameron R, Kawash B, McDonald PW, Madill C, Smith PM. Telephone counseling for population‐based smoking cessation. American Journal of Health Behavior 2004;28(3):231‐41. [DOI] [PubMed] [Google Scholar]
Brown 2007 {published data only}
- Brown RL, Saunders LA, Bobula JA, Mundt MP, Koch PE. Randomized‐controlled trial of a telephone and mail intervention for alcohol use disorders: three‐month drinking outcomes. Alcoholism, Clinical and Experimental Research 2007;31(8):1372‐9.. [DOI] [PubMed] [Google Scholar]
Bruce 2005 {published data only}
- Bruce Jr A, Bazargan‐Hejazi S. Evaluating a tailored intervention to increase screening mammography in an urban area. Journal of the National Medical Association 2005;97(10):1350‐60. [PMC free article] [PubMed] [Google Scholar]
Brustad 2003 {published data only}
- Brustad M, Skeie G, Braaten T, Slimani N, Lund E. Comparison of telephone vs face‐to‐face interviews in the assessment of dietary intake by the 24 h recall EPIC SOFT program ‐ The Norwegian calibration study. European Journal of Clinical Nutrition 2003;57(1):107‐13. [DOI] [PubMed] [Google Scholar]
Budin 2008 {published data only}
- Budin WC, Hoskins CN, Haber J, Sherman DW, Maislin G, Cater JR, et al. Breast cancer: education, counseling, and adjustment among patients and partners: a randomized clinical trial. Nursing Research 2008;57(3):199‐213. [DOI] [PubMed] [Google Scholar]
Burda 2012 {published data only}
- Burda C, Haack M, Duarte AC, Alemi F. Medication adherence among homeless patients: a pilot study of cell phone effectiveness. Journal of the American Academy of Nurse Practitioners 2012;24(11):675‐81. [DOI] [PubMed] [Google Scholar]
Buscemi 2011 {published data only}
- Buscemi J. A Randomised Clinical Trial of a Brief Motivational Intervention (BMI) for obesity in college students [PhD thesis]. Memphis: The University of Memphis, 2011. [Google Scholar]
Bustamante 2013 {published data only}
- Bustamante EE. Physical Activity Intervention for ADHD and DBD [PhD Thesis]. Chicago: University of Illinois, 2013. [Google Scholar]
Candy 2004 {published data only}
- Candy B, Chalder T, Cleare AJ, Hotopf M, Wessely S. A randomised controlled trial of a psycho‐educational intervention to aid recovery in infectious mononucleosis. Journal of Psychosomatic Research 2004;57(1):89‐94. [DOI] [PubMed] [Google Scholar]
Carcaise‐Edinboro 2008 {published data only}
- Carcaise‐Edinboro P, McClish D, Kracen AC, Bowen D, Fries E. Fruit and vegetable dietary behavior in response to a low‐intensity dietary intervention: the rural physician cancer prevention project. The Journal of Rural Health 2008;24(3):299‐305. [DOI] [PubMed] [Google Scholar]
Carlbring 2006 {published data only}
- Carlbring P, Bohman S, Brunt S, Buhrman M, Westling B E, Ekselius L, et al. Remote treatment of panic disorder: a randomised trial of Internet‐based cognitive behavior therapy supplemented with telephone calls. American Journal of Psychiatry 2006;163(12):2119‐25. [DOI] [PubMed] [Google Scholar]
Carmody 2013 {published data only}
- Carmody TP, Duncan CL, Huggins J, Solkowitz SN, Lee SK, Reyes N, et al. Telephone‐delivered cognitive‐behavioral therapy for pain management among older military veterans: a randomized trial. Psychological Services 2013;10(3):265‐75. [DOI] [PubMed] [Google Scholar]
Cecinati 2010 {published data only}
- Cecinati V, Esposito S, Scicchitano B, Delvecchio GC, Amato D, Pelucchi C, et al. Effectiveness of recall systems for improving influenza vaccination coverage in children with oncohematological malignancies. Human Vaccines 2010;6(2):194‐7. [DOI] [PubMed] [Google Scholar]
Chae 2000 {published data only}
- Chae YM, Park HJ, Cho JG, Hong GD, Cheon KA. The reliability and acceptability of telemedicine for patients with schizophrenia in Korea. Journal of Telemedicine and Telecare 2000;6(2):83‐90. [DOI] [PubMed] [Google Scholar]
Champion 2007 {published data only}
- Champion V, Skinner CS, Hui S, Monahan P, Juliar B, Daggy J, et al. The effect of telephone versus print tailoring for mammography adherence. Patient Education and Counseling 2007;65(3):416‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chang 2010 {published data only}
- Chang A, Liberman JN, Moyna A, Matlin OS, Raval K, Krull I, et al. Improving persistency for maintenance medication therapy through an interactive voice response program. Journal of Managed Care Pharmacy 2010;16(2):156. [Google Scholar]
Chiu 2010 {published data only}
- Chiu CW, Wong FKY. Effects of 8 weeks sustained follow‐up after a nurse consultation on hypertension: a randomised trial. International Journal of Nursing Studies 2010;47(11):1374‐82. [DOI] [PubMed] [Google Scholar]
Choudhry 2013 {published data only}
- Society‐of‐General‐Internal‐Medicine. 36th Annual Meeting of the Society‐of‐General‐Internal‐Medicine, APR 24‐27, 2013, Denver (CO). Journal of General Internal Medicine 2013;28(Suppl 1):S145‐S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Collins 2003 {published data only}
- Collins RL, Kashdan TB, Gollnisch G. The feasibility of using cellular phones to collect ecological momentary assessment data: application to alcohol consumption. Experimental and Clinical Psychopharmacology 2003;11(1):73‐8. [DOI] [PubMed] [Google Scholar]
Collins 2010 {published data only}
- Collins RL, Vincent P, Dermen K, Vetter C, Wilson S, Smith J. A daily process approach to evaluating 3 brief motivation‐based interventions to reduce young adults' alcohol use. Alcoholism: Clinical and Experimental Research 2010;34(6):293A. [Google Scholar]
Cooney 2015 {published data only}
- Cooney NL, Litt MD, Sevarino KA, Levy L, Kranitz LS, Sackler H, et al. Concurrent alcohol and tobacco treatment: Effect on daily process measures of alcohol relapse risk. Journal of Consulting and Clinical Psychology 2015;83(2):346‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Corkrey 2002a {published data only}
- Corkrey R, Parkinson L. A comparison of four computer‐based telephone interviewing methods: getting answers to sensitive questions. Behavior Research Methods, Instruments, & Computers 2002;34(3):354‐63. [DOI] [PubMed] [Google Scholar]
Costanza 2007 {published data only}
- Costanza ME, Luckmann R, Stoddard AM, White MJ, Stark JR, Avrunin JS, et al. Using tailored telephone counselling to accelerate the adoption of colorectal cancer screening. Cancer Detection and Prevention 2007;31(3):191‐8. [DOI] [PubMed] [Google Scholar]
Coughey 2010 {published data only}
- Coughey K, Klein G, West C, Diamond James J, Santana A, McCarville E, et al. The Child Asthma Link Line: a coalition‐initiated, telephone‐based, care coordination intervention for childhood asthma. Journal of Asthma 2010;47(3):303‐9. [DOI] [PubMed] [Google Scholar]
Crawford 2005 {published data only}
- Crawford AG, Sikirica V, Goldfarb N, Popiel RG, Patel M, Wang C, et al. Interactive voice response reminder effects on preventive service utilization. American Journal of Medical Quality 2005;20(6):329‐36. [DOI] [PubMed] [Google Scholar]
Crawford 2014 {published data only}
- Crawford J, Larsen‐Cooper E, Jezman Z, Cunningham SC, Bancroft E. SMS versus voice messaging to deliver MNCH communication in rural Malawi: assessment of delivery success and user experience. Global Health Science & Practice 2014;2(1):35‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cudkowicz 2013 {published data only}
- Cudkowicz ME, Berg LH, Shefner JM, Mitsumoto H, Mora JS, Ludolph A, et al. Dexpramipexole versus placebo for patients with amyotrophic lateral sclerosis (EMPOWER): a randomised,double‐blind, phase 3 trial. Lancet Neurology 2013;12(11):1059‐67. [DOI] [PubMed] [Google Scholar]
Curry 1995 {published data only}
- Curry SJ, McBride C, Grothaus LC, Louie D, Wagner EH. A randomized trial of self‐help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. Journal of Consulting and Clinical Psychology 1995;63(6):1005‐14. [DOI] [PubMed] [Google Scholar]
Curry 2003 {published data only}
- Curry SJ, Ludman EJ, Grothaus LC, Donovan D, Kim E. A randomized trial of a brief primary‐care‐based intervention for reducing at‐risk drinking practices. Health Psychology 2003;22(2):156‐65. [PubMed] [Google Scholar]
Dalal 2011a {published data only}
- Dalal AA, Nelson L, Gilligan T, McLeod L, Lewis S, Demuro‐Mercon C. Evaluating patient‐reported outcome measurement comparability between paper and alternate versions, using the lung function questionnaire as an example. Value in Health 2011;14(5):712‐20. [DOI] [PubMed] [Google Scholar]
Dalal 2011b {published data only}
- Dalal AA, Nelson LM, Gilligan T, McLeod LD, Lewis S, DeMuro C. Measurement comparability between paper and alternate versions: recommended assessment steps using the lung function questionnaire as an example. Value in Health 2011;14(3):A145. [DOI] [PubMed] [Google Scholar]
Damschroder 2010 {published data only}
- Damschroder L J, Lutes L D, Goodrich D E, Gillon L, Lowery J C. A small‐change approach delivered via telephone promotes weight loss in veterans: results from the ASPIRE‐VA pilot study. Patient Education and Counseling 2010;79(2):262‐6. [DOI] [PubMed] [Google Scholar]
Datta 2010 {published data only}
- Datta Santanu K, Oddone Eugene Z, Olsen Maren K, Orr M, McCant F, Gentry P, et al. Economic analysis of a tailored behavioral intervention to improve blood pressure control for primary care patients. American Heart Journal 2010;160(2):257‐63. [DOI] [PubMed] [Google Scholar]
Datto 2003 {published data only}
- Datto Catherine J, Thompson R, Horowitz D, Disbot M, Oslin David W. The pilot study of a telephone disease management program for depression. General Hospital Psychiatry 2003;25(3):169‐77. [DOI] [PubMed] [Google Scholar]
Davidoff 1985 {published data only}
- Davidoff M, Katz R. Automated telephone therapy for improving auditory comprehension in aphasic adults. Cognitive Rehabilitation 1985;3(2):26‐8. [Google Scholar]
Day 2002 {published data only}
- Day SX, Schneider PL. Psychotherapy using distance technology: a comparison of face‐to‐face, video, and audio treatment. Journal of Counseling Psychology 2002;49(4):499‐503. [Google Scholar]
Decker 2009 {published data only}
- Decker V, Spoelstra S, Miezo E, Bremer R, You M, Given C, et al. A pilot study of an automated voice response system and nursing intervention to monitor adherence to oral chemotherapy agents. Cancer Nursing 2009;32(6):E20‐9. [DOI] [PubMed] [Google Scholar]
Denis 2012 {published data only}
- Denis B. Tailored telephone counselling to increase adherence of underusers in an organized colorectal cancer screening program with FOBT: a randomised controlled trial. Gastroenterology 2012;142(5):S767‐8. [Google Scholar]
Depp 2015 {published data only}
- Depp CA, Ceglowski J, Wang VC, Yaghouti F, Mausbach BT, Thompson WK, et al. Augmenting psychoeducation with a mobile intervention for bipolar disorder: a randomized controlled trial. Journal of Affective Disorders 2015;174:23‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
De San Miguel 2013 {published data only}
- San Miguel K, Smith J, Lewin G. Telehealth remote monitoring for community‐dwelling older adults with chronic obstructive pulmonary disease. Telemedicine Journal and E‐health: The Official Journal of the American Telemedicine Association 2013;19(9):652‐7. [DOI] [PubMed] [Google Scholar]
Digenio 2009 {published data only}
- Digenio AG, Mancuso JP, Gerber RA, Dvorak RV. Comparison of methods for delivering a lifestyle modification program for obese patients. Annals of Internal Medicine 2009;150(4):255‐62. [DOI] [PubMed] [Google Scholar]
Duncan 2014 {published data only}
- Duncan M, Vandelanotte C, Kolt GS, Rosenkranz RR, Caperchione CM, George ES, et al. Effectiveness of a web‐ and mobile phone‐based intervention to promote physical activity and healthy eating in middle‐aged males: randomized controlled trial of the ManUp study. Journal of Medical Internet Research 2014;16(6):e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Durso 2003 {published data only}
- Durso S C, Wendel I, Letzt A M, Lefkowitz J, Kaseman D F, Seifert R F. Older adults using cellular telephones for diabetes management: a pilot study. Medsurg Nursing 2003;12(5):313‐7. [PubMed] [Google Scholar]
Dyches 1999 {published data only}
- Dyches H, Alemagno S, Llorens SA, Butts JM. Automated telephone‐administered substance abuse screening for adults in primary care. Health Care Management Science 1999;2(4):199‐204. [DOI] [PubMed] [Google Scholar]
Eakin 2009 {published data only}
- Eakin E, Reeves M, Lawler S, Graves N, Oldenburg B, Mar CD, et al. Telephone counseling for physical activity and diet in primary care patients. American Journal of Preventive Medicine 2009;36(2):142‐9. [DOI] [PubMed] [Google Scholar]
Eakin 2010 {published data only}
- Eakin E, Reeves M, Winkler E, Lawler S, Owen N. Maintenance of physical activity and dietary change following a telephone‐delivered intervention. Health Psychology 2010;29(6):566‐73. [DOI] [PubMed] [Google Scholar]
Eakin 2012 {published data only}
- Eakin E, Reeves M, Dunstan D, Healy G, Winkler E, Marshall A, et al. Living well with diabetes: six‐month randomised trial outcomes of a telephone‐delivered weight loss intervention. Journal of Science and Medicine in Sport 2012;15(S1):S202. [Google Scholar]
Eisdorfer 2003 {published data only}
- Eisdorfer C, Czaja SJ, Loewenstein DA, Rubert MP, Arguelles S, Mitrani VB, et al. The effect of a family therapy and technology‐based intervention on caregiver depression. Gerontologist 2003;43(4):521‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elliott 2013 {published data only}
- Elliott MN, Brown JA, Lehrman WG, Beckett MK, Hambarsoomian K, Giordano LA, et al. A randomized experiment investigating the suitability of speech‐enabled IVR and web modes for publicly reported surveys of patients' experience of hospital care. Medical Care Research and Review 2013;70(2):165‐84. [DOI] [PubMed] [Google Scholar]
Elston 2010 {published data only}
- Elston J, Honan W, Powell R, Gormley J, Stein K. Do metronomes improve the quality of life in people with Parkinson's disease? A pragmatic, single‐blind, randomised cross‐over trial. Clinical Rehabilitation 2010;24(6):523‐32. [DOI] [PubMed] [Google Scholar]
Eng 2013 {published data only}
- Eng JA, Richman JS, Houston T, Ritchie C. Health literacy did not influence effectiveness of computer telephony‐based post‐discharge support. Journal of General Internal Medicine 2013;28:S84‐85. [Google Scholar]
Fadol 2011 {published data only}
- Fadol AP, Mendoza T, Shah P, Cleeland C. Heart failure in cancer: is interactive voice response system (IVRS) feasible for symptom management?. Journal of Cardiac Failure 2011;17:8S. [Google Scholar]
Fairhurst 2008 {published data only}
Farabee 2013 {published data only}
- Farabee D, Cousins SJ, Brecht ML, Antonini VP, Lee AB, Brummer J, et al. A comparison of four telephone‐based counselling styles for recovering stimulant users. Psychology of Addictive Behaviors 2013;27(1):223‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faridi 2008 {published data only}
- Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz David L. Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self‐management: the NICHE pilot study. Journal of Evaluation in Clinical Practice 2008;14(3):465‐9. [DOI] [PubMed] [Google Scholar]
Farmer 2005 {published data only}
- Farmer AJ, Gibson OJ, Dudley C, Bryden K, Hayton PM, Tarassenko L, et al. A randomised controlled trial of the effect of real‐time telemedicine support on glycaemic control in young adults with type 1 diabetes. Diabetes Care 2005;28(11):2697‐702. [DOI] [PubMed] [Google Scholar]
Feldstein 2009 {published data only}
- Feldstein Adrianne C, Perrin N, Rosales A, Schneider J, Rix Mary M, Keels K, et al. Effect of a multimodal reminder program on repeat mammogram screening. American Journal of Preventive Medicine 2009;37(2):94‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fischer 2001 {published data only}
- Fischer R, Meyer N, Weitkunat R, Crispin A, Schotten K, Uberla K. Population‐based health monitoring via computer‐assisted telephone interviews in Bavaria [Bevölkerungsbezogenes Gesundheitsmonitoring in Bayern mit computerassistierten Telefoninterviews]. Gesundheitswesen 2001;63(Suppl 2):S123‐9. [DOI] [PubMed] [Google Scholar]
Fischer 2014 {published data only}
- Fischer MA, Choudhry NK, Bykov K, Brill G, Bopp G, Wurst AM, et al. Pharmacy‐based interventions to reduce primary medication nonadherence to cardiovascular medications. Medical Care 2014;52(12):1050‐4. [DOI] [PubMed] [Google Scholar]
Fisher 2013 {published data only}
- Fisher WA, Orsama AL, Lahteenmaki J, Harno K, Kulju M, Wintergerst E, et al. Remote patient reporting and automated mobile telephone feedback reduce HbA1c and weight in individuals with type 2 diabetes: results of pilot research. Diabetes Technology and Therapeutics 2013;15(Suppl 1):A8. [DOI] [PubMed] [Google Scholar]
Flax 2014 {published data only}
- Flax VL, Negerie M, Ibrahim AU, Leatherman S, Daza EJ, Bentley ME. Integrating group counseling, cell phone messaging, and participant‐generated songs and dramas into a microcredit program increases Nigerian women's adherence to international breastfeeding recommendations. Journal of Nutrition 2014;144(7):1120‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Franc 2014 {published data only}
- Franc S, Daoudi A, Joubert M, Fagour C, Boucherie B, Benamo E, et al. Telediab2 study: short‐term and long‐term results. Diabetes 2014;63(Suppl 1):A244‐5. [Google Scholar]
Furber 2010 {published data only}
- Furber S, Butler L, Phongsavan P, Mark A, Bauman A. Randomised controlled trial of a pedometer‐based telephone intervention to increase physical activity among cardiac patients not attending cardiac rehabilitation. Patient Education and Counseling 2010;80(2):212‐8. [DOI] [PubMed] [Google Scholar]
Fursse 2008 {published data only}
- European‐Federation‐for‐Medical‐Informatic. 21st International Congress of the European‐Federation‐for‐Medical‐Informatic (MIE2008), MAY 25‐28, 2008, Gothenburg, SWEDEN. Studies in Health Technology and Informatics 2008;136:181‐6. [Google Scholar]
Gazmararian 2010 {published data only}
- Gazmararian J, Jacobson KL, Pan Y, Schmotzer B, Kripalani S. Effect of a pharmacy‐based health literacy intervention and patient characteristics on medication refill adherence in an urban health system. Annals of Pharmacotherapy 2010;44(1):80‐7. [DOI] [PubMed] [Google Scholar]
Gilbert 2006 {published data only}
- Gilbert H, Sutton S. Evaluating the effectiveness of proactive telephone counselling for smoking cessation in a randomized controlled trial. Addiction 2006;101(4):590‐8. [DOI] [PubMed] [Google Scholar]
Gilman 2014 {published data only}
- The Society for Academic Emergency Medicine (SAEM). SAEM Annual Meeting, May 13‐17, 2014, Dallas (TX). Academic Emergency Medicine 2014;21(Suppl 1):S145‐S6.. [DOI] [PubMed] [Google Scholar]
Glasgow 1996 {published data only}
- Glasgow RE, Toobert DJ, Hampson SE. Effects of a brief office‐based intervention to facilitate diabetes dietary self‐management. Diabetes Care 1996;19(8):835‐42. [DOI] [PubMed] [Google Scholar]
Glasgow 2008 {published data only}
- Glasgow RE, Estabrooks PA, Marcus AC, Smith TL, Gaglio B, Levinson AH, et al. Evaluating initial reach and robustness of a practical randomized trial of smoking reduction. Health Psychology 2008;27(6):780‐8. [DOI] [PubMed] [Google Scholar]
Goel 2008 {published data only}
- Goel A, George J, Burack RC. Telephone reminders increase re‐screening in a county breast screening program. Journal of Health Care for the Poor and Underserved 2008;19(2):512‐21. [DOI] [PubMed] [Google Scholar]
Gonzalez 1997 {published data only}
- Gonzalez GM, Costello CR, Tourette TR, Joyce LK, Valenzuela M. Bilingual telephone‐assisted computerized speech‐recognition assessment: is a voice‐activated computer program a culturally and linguistically appropriate tool for screening depression in English and Spanish?. Cultural Diversity and Mental Health 1997;3(2):93‐111. [DOI] [PubMed] [Google Scholar]
Greaney 2012 {published data only}
- Greaney ML, Sprunck‐Harrild K, Bennett GG, Puleo E, Haines J, Viswanath KV, et al. Use of email and telephone prompts to increase self‐monitoring in a web‐based intervention: randomized controlled trial. Journal of Medical Internet Research 2012;14(4):e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Green 2010 {published data only}
- Green BB, Wang CY, Horner K, Catz S, Meenan RT, Vernon SW, et al. Systems of support to increase colorectal cancer screening and follow‐up rates (SOS): design, challenges, and baseline characteristics of trial participants. Contemporary Clinical Trials 2010;31(6):589‐603. [DOI] [PMC free article] [PubMed] [Google Scholar]
Green 2013 {published data only}
- Green BB, Wang CY, Anderson ML, Chubak J, Meenan RT, Vernon SW, et al. An automated intervention with stepped increases in support to increase uptake of colorectal cancer screening: a randomised trial. Annals of Internal Medicine 2013;158(5 Pt 1):301‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greene 1998 {published data only}
- Greene L. A Comparison of Nursing Interventions Used to Increase Immunization Rates in Children [MSc Thesis]. Newport: Northern Kentucky University, 1998. [Google Scholar]
Greenley 2012 {published data only}
- Crohn's & Colitis Foundation of America. Crohn's‐and‐Colitis‐Foundation's‐National‐Clinical‐and‐Research Conference on Advances in Inflammatory Bowel Diseases, DEC 13‐15, 2012, Hollywood (FL). Inflammatory Bowel Diseases 2012;18(Suppl 1):S6. [DOI] [PubMed] [Google Scholar]
Groeneveld 2010 {published data only}
- Groeneveld IF, Proper KI, Beek AJ, Mechelen W. Sustained body weight reduction by an individual‐based lifestyle intervention for workers in the construction industry at risk for cardiovascular disease: Results of a randomised controlled trial. Preventive Medicine 2010;51(3‐4):240‐6. [DOI] [PubMed] [Google Scholar]
Haas 2015 {published data only}
- Haas JS, Linder JA, Park ER, Gonzalez I, Rigotti NA, Klinger EV, et al. Proactive tobacco cessation outreach to smokers of low socioeconomic status: a randomised clinical trial. JAMA Internal Medicine 2015;175(2):218‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hall 2000 {published data only}
- Hall JA, Huber DL. Telephone management in substance abuse treatment. Telemedicine Journal and E‐Health 2000;6(4):401‐7. [DOI] [PubMed] [Google Scholar]
Hanauer 2009 {published data only}
- Hanauer David A, Wentzell K, Laffel N, Laffel Lori M. Computerized Automated Reminder Diabetes System (CARDS): e‐mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technology & Therapeutics 2009;11(2):99‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardy 2011 {published data only}
- Hardy H, Kumar V, Doros G, Farmer E, Drainoni M L, Rybin D, et al. Randomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapy. AIDS Patient Care and STDs 2011;25(3):153‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hasin 2014 {published data only}
- Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Addiction Science & Clinical Practice 2014;9(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haynes 2006 {published data only}
- Haynes JM, Sweeney EL. The effect of telephone appointment‐reminder calls on outpatient absenteeism in a pulmonary function laboratory. Respiratory Care 2006;51(1):36‐9. [PubMed] [Google Scholar]
Hedeker 2003 {published data only}
- Hedeker D, Mermelstein R, Wong SC. Extended telephone counseling for smoking cessation: does content matter?. Journal of Consulting and Clinical Psychology 2003;71(3):565‐74. [DOI] [PubMed] [Google Scholar]
Henry 2012 {published data only}
- Henry SR, Goetz MB, Asch SM. The effect of automated telephone appointment reminders on HIV primary care no‐shows by veterans. Journal of the Association of Nurses in AIDS Care 2012;23(5):409‐18. [DOI] [PubMed] [Google Scholar]
Hersey 2012 {published data only}
- Hersey JC, Khavjou O, Strange LB, Atkinson RL, Blair SN, Campbell S, et al. The efficacy and cost‐effectiveness of a community weight management intervention: a randomised controlled trial of the health weight management demonstration. Preventive Medicine 2012;54(1):42‐9. [DOI] [PubMed] [Google Scholar]
Hettema 2012 {published data only}
- Hettema JE, Hosseinbor S, Ingersoll KS. Feasibility and reliability of interactive voice response assessment of HIV medication adherence: research and clinical implications. HIV Clinical Trials Journal 2012;13(5):271‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollis 2005 {published data only}
- Hollis JF, Polen MR, Whitlock EP, Lichtenstein E, Mullooly JP, Velicer WF, et al. Teen reach: outcomes from a randomized, controlled trial of a tobacco reduction program for teens seen in primary medical care. Pediatrics 2005;115(4):981‐9. [DOI] [PubMed] [Google Scholar]
Horng 2004 {published data only}
- Horng F, Chueh K. Effectiveness of telephone follow‐up and counselling in aftercare for alcoholism. Journal of Nursing Research (Taiwan Nurses Association) 2004;12(1):11‐20. [DOI] [PubMed] [Google Scholar]
Horton 2008 {published data only}
- Horton RJ, Minniti A, Mireylees S, McEntegart D. A randomised trial to determine the impact on compliance of a psychophysical peripheral cue based on the Elaboration Likelihood Model. Contemporary Clinical Trials 2008;29(6):823‐8. [DOI] [PubMed] [Google Scholar]
Hubbard 2007 {published data only}
- Hubbard RL, Leimberger JD, Haynes L, Patkar AA, Holter J, Liepman MR, et al. Telephone enhancement of long‐term engagement (TELE) in continuing care for substance abuse treatment: a NIDA clinical trials network (CTN) study. The American Journal on Addictions 2007;16(6):495‐502. [DOI] [PubMed] [Google Scholar]
Hurling 2007 {published data only}
- Hurling R, Catt M, Boni MD, Fairley BW, Hurst T, Murray P, et al. Using Internet and mobile phone technology to deliver an automated physical activity program: randomised controlled trial. Journal of Medical Internet Research 2007;9(2):e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hurling 2013 {published data only}
- Hurling R, Claessen JP, Nicholson J, Schäfer F, Tomlin CC, Lowe CF. Automated coaching to help parents increase their children's brushing frequency: an exploratory trial. Community Dental Health 2013;30(2):88‐93. [PubMed] [Google Scholar]
Hwang 2014 {published data only}
- Fox N, Hirsch‐Allen AJ, Goodfellow E, Wenner J, Fleetham J, Ryan CF, et al. The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. Sleep 2012;35(4):477‐81. [ClinicalTrials.gov Identifier:NCT02279901] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jacobs 2004 {published data only}
- Jacobs AD, Ammerman AS, Ennett ST, Campbell MK, Tawney KW, Aytur SA, et al. Effects of a tailored follow‐up intervention on health behaviors, beliefs, and attitudes. Journal of Women's Health 2004;13(5):557‐68. [DOI] [PubMed] [Google Scholar]
Jacobs 2011 {published data only}
- Jacobs N, Bourdeaudhuij I, Thijs H, Dendale P, Claes N. Effect of a cardiovascular prevention program on health behavior and BMI in highly educated adults: a randomized controlled trial. Patient Education and Counseling 2011;85(1):122‐6. [DOI] [PubMed] [Google Scholar]
Jiménez‐Muro 2013 {published data only}
- Jiménez‐Muro A, Nerín I, Samper P, Marqueta A, Beamonte A, Gargallo P, et al. A proactive smoking cessation intervention in postpartum women. Midwifery 2013;29(3):240‐5. [DOI] [PubMed] [Google Scholar]
Johnson 2014 {published data only}
- Johnson TJ, Wilbur J, Fogg L, Schoeny M. The cost of increasing physical activity and decreasing body mass index for mid‐life African women. Value in Health 2014;17(7):A487. [A487] [DOI] [PubMed] [Google Scholar]
Joyce 2008 {published data only}
- Joyce GF, Niaura R, Maglione M, Mongoven J, Larson‐Rotter C, Coan J, et al. The effectiveness of covering smoking cessation services for medicare beneficiaries. Health Services Research 2008;43(6):2106‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Katz 2008 {published data only}
- Katz DL, Nordwall B. Novel interactive cell‐phone technology for health enhancement. Journal of Diabetes Science & Technology 2008;2(1):147‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kauer 2012 {published data only}
- Kauer SD, Reid SC, Crooke AH, Khor A, Hearps SJ, Jorm AF, et al. Self‐monitoring using mobile phones in the early stages of adolescent depression: randomised controlled trial. Journal of Medical Internet Research 2012;14(3):e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kearney 2009 {published data only}
- Kearney N, McCann L, Norrie J, Taylor L, Gray P, McGee‐Lennon M, et al. Evaluation of a mobile phone‐based, advanced symptom management system (ASyMS©) in the management of chemotherapy‐related toxicity. Supportive Care in Cancer 2009;17(4):437‐44. [DOI] [PubMed] [Google Scholar]
Kempe 2012 {published data only}
- Kempe KL, Shetterly SM, France EK, Levin TR. Automated phone and mail population outreach to promote colorectal cancer screening. American Journal of Managed Care 2012;18(7):370‐8. [PubMed] [Google Scholar]
Kim 2007 {published data only}
Kim 2008 {published data only}
- Kim H S, Song M S. Technological intervention for obese patients with type 2 diabetes. Applied Nursing Research 2008;21(2):84‐9. [DOI] [PubMed] [Google Scholar]
Kim 2012 {published data only}
- Kim HG, Geppert J, Quan T, Bracha Y, Lupo V, Cutts DB. Screening for postpartum depression among low‐income mothers using an interactive voice response system. Maternal and Child Health Journal 2012;16(4):921‐8. [DOI] [PubMed] [Google Scholar]
Kim 2013 {published data only}
- Kim SE, Michalopoulos C, Kwong RM, Warren A, Manno MS. Telephone care management's effectiveness in coordinating care for Medicaid beneficiaries in managed care: a randomized controlled study. Health Services Research 2013;48(5):1730‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klausen 2012 {published data only}
- Klausen SH, Mikkelsen UR, Hirth A, Wetterslev J, Kjærgaard H, Søndergaard L, et al. Design and rationale for the PREVAIL study: effect of e‐Health individually tailored encouragements to physical exercise on aerobic fitness among adolescents with congenital heart disease‐‐a randomised clinical trial. American Heart Journal 2012;163(4):549‐56. [DOI] [PubMed] [Google Scholar]
Kobak 1997 {published data only}
- Kobak KA, Taylor LH, Dottl SL, Greist JH, Jefferson JW, Burroughs D, et al. Computerized screening for psychiatric disorders in an outpatient community mental health clinic. Psychiatric Services 1997;48(8):1048‐57. [DOI] [PubMed] [Google Scholar]
Kobak 2015 {published data only}
- Kobak KA, Greist R, Jacobi DM, Levy‐Mack H, Greist JH. Computer‐assisted cognitive behavior therapy for obsessive‐compulsive disorder: a randomised trial on the impact of lay vs. professional coaching. Annals of General Psychiatry 2015;14(10):doi: 10.1186/s12991‐015‐0048‐0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kolt 2007 {published data only}
- Kolt GS, Schofield GM, Kerse N, Garrett N, Oliver M. Effect of telephone counselling on physical activity for low‐active older people in primary care: a randomised, controlled trial. Journal of the American Geriatrics Society 2007;55(7):986‐92. [DOI] [PubMed] [Google Scholar]
Konstam 2011 {published data only}
- Konstam V, Gregory D, Chen J, Weintraub A, Patel A, Levine D, et al. Health‐related quality of life in a multicenter randomised controlled comparison of telephonic disease management and automated home monitoring in patients recently hospitalised with heart failure: SPAN‐CHF II trial. Journal of Cardiac Failure 2011;17(2):151‐7. [DOI] [PubMed] [Google Scholar]
Kristal 2000 {published data only}
- Kristal AR, Curry SJ, Shattuck AL, Feng Z, Li S. A randomised trial of a tailored, self‐help dietary intervention: The Puget sound eating patterns study. Preventive Medicine 2000;31(4):380‐9. [DOI] [PubMed] [Google Scholar]
Kwon 2010 {published data only}
- Kwon SB, Hong SS, Kang SY, Jung S, Hwang SH. Telephone call reminders and attendance in an electromyography laboratory. Journal of Neurology 2010;257(Suppl 1):S185. [Google Scholar]
Kwon 2012 {published data only}
- Kwon SB, Jung S, Kang SY, Hong SS, Hwang SH. The effect of telephone call reminders on electrodiagnostic laboratory attendance in Korea. Healthmed 2012;6(8):2850‐55. [Google Scholar]
Ladyzynski 2007 {published data only}
- Ladyzynski P, Wojcicki JM. Home telecare during intensive insulin treatment‐‐metabolic control does not improve as much as expected. Journal of telemedicine and telecare 2007;13(1):44‐7. [DOI] [PubMed] [Google Scholar]
Larocque 2014 {published data only}
- Larocque N, Calder LA, Calder‐Sprackman S, Cagaanan R, Zlepnig J, Cwinn AA, et al. Efficacy of phone follow‐up in reducing adverse events in the emergency department: a pilot project. Canadian Journal of Emergency Medicine 2014;16(1):S42. [Google Scholar]
Leichter 2013 {published data only}
- Leichter SB, Bowman K, Adkins RA, Jelsovsky Z. Impact of remote management of diabetes via computer: The 360 study ‐ a proof‐of‐concept randomised trial. Diabetes Technology and Therapeutics 2013;15(5):434‐8. [DOI] [PubMed] [Google Scholar]
Leigh 2014 {published data only}
- Leigh BC, Brewer DD, Seddig EL. Collecting daily self‐reports of injection drug use via automated telephone interviewing. Drug & Alcohol Review 2014;33(4):446‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leimig 2008 {published data only}
- Leimig R, Gower G, Thompson DA, Winsett RP. Infection, rejection, and hospitalizations in transplant recipients using telehealth. Progress in Transplantation 2008;18(2):97‐102. [DOI] [PubMed] [Google Scholar]
Leon 1999 {published data only}
- Leon AC, Kelsey JE, Pleil A, Burgos TL, Portera L, Lowell KN. An evaluation of a computer assisted telephone interview for screening for mental disorders among primary care patients. Journal of Nervous and Mental Disease 1999;187(5):308‐11. [DOI] [PubMed] [Google Scholar]
Levin 2011 {published data only}
- Levin W, Campbell DR, McGovern KB, Gau JM, Kosty DB, Seeley JR, et al. A computer‐assisted depression intervention in primary care. Psychological Medicine 2011;41(7):1373‐83. [DOI] [PubMed] [Google Scholar]
Levinson 2008 {published data only}
- Levinson AH, Glasgow RE, Gaglio B, Smith TL, Cahoon J, Marcus AC. Tailored behavioral support for smoking reduction: development and pilot results of an innovative intervention. Health Education Research 2008;23(2):335‐46. [DOI] [PubMed] [Google Scholar]
Lewis 2010 {published data only}
- Lewis KE, Annandale JA, Warm DL, Hurlin C, Lewis MJ, Lewis L. Home telemonitoring and quality of life in stable, optimised chronic obstructive pulmonary disease. Journal of Telemedicine & Telecare 2010;16(5):253‐9. [DOI] [PubMed] [Google Scholar]
Lichtenstein 2008 {published data only}
- Lichtenstein E, Boles SM, Lee ME, Hampson SE, Glasgow RE, Fellows J. Using radon risk to motivate smoking reduction II: randomized evaluation of brief telephone counseling and a targeted video. Health Education Research 2008;23(2):191‐201. [DOI] [PubMed] [Google Scholar]
Lim 2011 {published data only}
- Lim S, Kang SM, Shin H, Lee HJ, Yoon JW, Yu SH, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care 2011;34(2):308‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linder 2014 {published data only}
- Linder JA, Haas J, Rigotti NA, Park ER, Kontos E, Gonzalez I, et al. Proactive outreach of tobacco cessation treatment to disadvantaged smokers after a primary care visit: a randomized controlled trial. Journal of General Internal Medicine 2014;29(Suppl 1):S184. [Google Scholar]
Lindner 2013 {published data only}
- Lindner P, Ivanova E, Ly KH, Andersson G, Carlbring P. Guided and unguided CBT for social anxiety disorder and/or panic disorder via the Internet and a smartphone application: study protocol for a randomised controlled trial. Trials 2013;14(437):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lindsay 2014 {published data only}
- Lindsay JA, Minard CG, Hudson S, Green CE, Schmitz JM. Using prize‐based incentives to enhance daily interactive voice response (IVR) compliance: a feasibility study. Journal of Substance Abuse Treatment 2014;46(1):74‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2008 {published data only}
- Liu WT, Wang CH, Lin HC, Lin SM, Lee KY, Lo YL, et al. Efficacy of a cell phone‐based exercise programme for COPD. European Respiratory Journal 2008;32(3):651‐9. [DOI] [PubMed] [Google Scholar]
Liu 2011 {published data only}
- Liu WT, Huang CD, Wang CH, Lee KY, Lin SM, Kuo HP. A mobile telephone‐based interactive self‐care system improves asthma control. The European Respiratory Journal 2011;37(2):310‐7. [DOI] [PubMed] [Google Scholar]
Lovejoy 2014 {published data only}
- Lovejoy TI, Heckman TG. Depression moderates treatment efficacy of an HIV secondary‐prevention intervention for HIV‐positive late middle‐age and older adults. Behavioral Medicine 2014;40(3):124‐33. [DOI] [PubMed] [Google Scholar]
Ludman 2007 {published data only}
- Ludman EJ, Simon GE, Tutty S, Korff M. A randomized trial of telephone psychotherapy and pharmacotherapy for depression: continuation and durability of effects. Journal of Consulting and Clinical Psychology 2007;75(2):257‐66. [DOI] [PubMed] [Google Scholar]
Mahoney 1999 {published data only}
- Mahoney D, Tennstedt S, Friedman R, Heeren T. An automated telephone system for monitoring the functional status of community‐residing elders. Gerontologist. 1999;39(2):229‐34. [DOI] [PubMed] [Google Scholar]
Markert 2013 {published data only}
- Markert J, Alff F, Zschaler S, Gausche R, Kiess W, Bluher S. Prevention of childhood obesity: Recruiting strategies via local paediatricians and study protocol for a telephone‐based counselling programme. Obesity Research and Clinical Practice 2013;7(6):e476‐e86. [DOI] [PubMed] [Google Scholar]
Marshall 1993 {published data only}
- Marshall B J, Hoffman S R, Babadzhov V, Babadzhov M, McCallum R. The Automatic Patient Symptom Monitor (APSM): a voice mail system for clinical research. Proceedings of the Annual Symposium on Computer Application [sic] in Medical Care.. 1993:32‐6. [PMC free article] [PubMed]
McCann 2009 {published data only}
- McCann L, Maguire R, Miller M, Kearney N. Patients' perceptions and experiences of using a mobile phone‐based advanced symptom management system (ASyMS) to monitor and manage chemotherapy related toxicity. European Journal of Cancer Care 2009;18(2):156‐64. [DOI] [PubMed] [Google Scholar]
McDaniel 2005 {published data only}
- McDaniel AM, Benson PL, Roesener GH, Martindale J. An integrated computer‐based system to support nicotine dependence treatment in primary care. Nicotine & Tobacco Research 2005;7(1):S57‐66. [DOI] [PubMed] [Google Scholar]
Miskelly 2005 {published data only}
- Miskelly F. Electronic tracking of patients with dementia and wandering using mobile phone technology. Age & Ageing 2005;34(5):497‐9. [DOI] [PubMed] [Google Scholar]
Mollon 2008 {published data only}
- Mollon B, Holbrook Anne M, Keshavjee K, Troyan S, Gaebel K, Thabane L, et al. Automated telephone reminder messages can assist electronic diabetes care. Journal of Telemedicine and Telecare 2008;14(1):32‐6. [DOI] [PubMed] [Google Scholar]
Mooney 2002 {published data only}
- Mooney KH, Beck SL, Friedman RH, Farzanfar R. Telephone‐linked care for cancer symptom monitoring. Cancer Practice 2002;10(3):147‐54. [DOI] [PubMed] [Google Scholar]
Mooney 2013 {published data only}
- Mooney K, Beck SL, Wong B, Dunson Jr WA, Wujcik D. The prevalence of hospitalizations, emergency department/urgent care visits for unrelieved symptoms during chemotherapy. Supportive Care in Cancer 2013;21(Suppl 1):S267‐S8. [Google Scholar]
Naylor 2002 {published data only}
- Naylor MR, Helzer JE, Naud S, Keefe FJ. Automated telephone as an adjunct for the treatment of chronic pain: A pilot study. Journal of Pain 2002;3(6):429‐38. [DOI] [PubMed] [Google Scholar]
O'Brien 1998 {published data only}
- O'Brien G, Lazebnik R. Telephone call reminders and attendance in an adolescent clinic. Pediatrics. 1998;101(6):E6. [DOI] [PubMed] [Google Scholar]
Oake 2009 {published data only}
- Oake N, Van WC, Rodger MA, Forster AJ. Effect of an interactive voice response system on oral anticoagulant management. Canadian Medical Association Journal 2009;180(9):927‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Odegard 2012 {published data only}
- Odegard PS, Christensen DB. MAP study: RCT of a medication adherence program for patients with type 2 diabetes. Journal of the American Pharmacists Association 2012;52(6):753‐62. [DOI] [PubMed] [Google Scholar]
Orsama 2013 {published data only}
- Orsama AL, Lahteenmaki J, Harno K, Kulju M, Wintergerst E, Schachner H, et al. Active assistance technology reduces glycosylated hemoglobin and weight in individuals with type 2 diabetes: results of a theory‐based randomized trial. Diabetes Technology and Therapeutics 2013;15(8):662‐9. [DOI] [PubMed] [Google Scholar]
Osgood‐Hynes 1998 {published data only}
- Osgood‐Hynes DJ, Greist JH, Marks IM, Baer L, Heneman SW, Wenzel KW, et al. Self‐administered psychotherapy for depression using a telephone‐accessed computer system plus booklets: An open U.S.‐U.K. study. Journal of Clinical Psychiatry 1998;59(7):358‐65. [DOI] [PubMed] [Google Scholar]
Pakhale 2015 {published data only}
- Pakhale S, Baron J, Armstrong MA, Garde A, Reid RD, Alvarez G, et al. A pilot randomized controlled trial of smoking cessation in an outpatient respirology clinic. Canadian Respiratory Journal 2015;22(2):91‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patrick 2000 {published data only}
- Patrick L. Automated telephone assessment and education with nurse follow up improved self care and glycaemic control in patients with diabetes... commentary on Piette JD, Weinberger M, McPhee SJ et al. Do automated calls with nurse follow‐up improve self‐care and glycaemic control among vulnerable patients with diabetes?. The American Journal of Medicine 2000;108(1):20‐7. [DOI] [PubMed] [Google Scholar]
Patten 2003 {published data only}
- Patten SB. Prevention of depressive symptoms through the use of distance technologies. Psychiatric Services 2003;54(3):396‐8. [DOI] [PubMed] [Google Scholar]
Pellegrini 2012 {published data only}
- Pellegrini CA, Duncan JM, Moller AC, Buscemi J, Sularz A, DeMott A, et al. A smartphone‐supported weight loss program: design of the ENGAGED randomised controlled trial. BMC Public Health 2012;12(1041):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinto 2011 {published data only}
- Pinto BM, Goldstein MG, Papandonatos GD, Farrell N, Tilkemeier P, Marcus BH, et al. Maintenance of exercise after phase II cardiac rehabilitation: a randomized controlled trial. American Journal of Preventive Medicine 2011;41(3):274‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinto 2013a {published data only}
- Pinto BM, Papandonatos GD, Goldstein MG. A randomised trial to promote physical activity among breast cancer patients. Health Psychology 2013;32(6):616‐26. [DOI] [PubMed] [Google Scholar]
Pinto 2013b {published data only}
- Pinto BM, Papandonatos GD, Goldstein MG, Marcus BH, Farrell N. Home‐based physical activity intervention for colorectal cancer survivors. Psycho‐oncology 2013;22(1):54‐64. [DOI] [PubMed] [Google Scholar]
Pizzi 2014 {published data only}
- Pizzi LT, Zangalli C, Murchison AP, Hale N, Hark L, Dai Y, et al. Comparative effectiveness and costs of strategies to improve follow‐up for diabetic eye care visits. Value in Health 2014;17(3):A129. [Google Scholar]
Prochaska 2001 {published data only}
- Prochaska JO, Velicer WF, Fava JL, Ruggiero L, Laforge RG, Rossi JS, et al. Counselor and stimulus control enhancements of a stage‐matched expert system intervention for smokers in a managed care setting. Preventive Medicine 2001;32(1):23‐32. [DOI] [PubMed] [Google Scholar]
Ramelson 1999 {published data only}
- Ramelson HZ, Friedman RH, Ockene JK. An automated telephone‐based smoking cessation education and counselling system. Patient Education and Counseling 1999;36(2):131‐44. [DOI] [PubMed] [Google Scholar]
Riegel 2006 {published data only}
- Riegel B, Carlson B, Glaser D, Romero T. Randomized controlled trial of telephone case management in Hispanics of Mexican origin with heart failure. Journal of Cardiac Failure 2006;12(3):211‐9. [DOI] [PubMed] [Google Scholar]
Rizvi 2011 {published data only}
- Rizvi SL, Dimeff LA, Skutch J, Carroll D, Linehan MM. A pilot study of the DBT coach: an interactive mobile phone application for individuals with borderline personality disorder and substance use disorder. Behaviour Therapy 2011;42(4):589‐600. [DOI] [PubMed] [Google Scholar]
Roberts 2007 {published data only}
- Roberts N, Meade K, Partridge M. The effect of telephone reminders on attendance in respiratory outpatient clinics. Journal of Health Services Research & Policy 2007;12(2):69‐72. [DOI] [PubMed] [Google Scholar]
Rolnick 1997 {published data only}
- Rolnick SJ, Klevan D, Cherney L, Lando HA. Nicotine replacement therapy in a group model HMO. HMO practice/HMO Group 1997;11(1):34‐7. [PubMed] [Google Scholar]
Rose 2010 {published data only}
- Rose G L, MacLean C D, Skelly J, Badger G J, Ferraro T A, Helzer J E. Interactive voice response technology can deliver alcohol screening and brief intervention in primary care. Journal of General Internal Medicine 2010;25(4):340‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosser 1992 {published data only}
- Rosser WW, Hutchison BG, McDowell I, Newell C. Use of reminders to increase compliance with tetanus booster vaccination. CMAJ 1992;146(6):911‐7. [PMC free article] [PubMed] [Google Scholar]
Rothemich 2010 {published data only}
- Rothemich SF, Woolf SH, Johnson RE, Devers KJ, Flores SK, Villars P, et al. Promoting primary care smoking‐cessation support with quitlines: the QuitLink randomized controlled trial. American Journal of Preventive Medicine 2010;38(4):367‐74. [DOI] [PubMed] [Google Scholar]
Rubin 2006 {published data only}
- Rubin A, Migneault JP, Marks L, Goldstein E, Ludena K, Friedman RH. Automated telephone screening for problem drinking. Journal of Studies on Alcohol 2006;67(3):454‐7. [DOI] [PubMed] [Google Scholar]
Salisbury 2013 {published data only}
- Salisbury C, Foster NE, Hopper C, Bishop A, Hollinghurst S, Coast J, et al. A pragmatic randomised controlled trial of the effectiveness and cost‐effectiveness of 'PhysioDirect' telephone assessment and advice services for physiotherapy. Health Technology Assessment 2013;17(2):1‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sano 2013 {published data only}
- Sano M, Egelko S, Donohue M, Ferris S, Kaye J, Hayes TL, et al. Developing dementia prevention trials: baseline report of the Home‐Based Assessment study. Alzheimer Disease and Associated Disorders 2013;27(4):356‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sano 2014 {published data only}
- Sano M, Egelko S, Donohue MC, Kaye J, Mundt J, Sun CK, et al. Assessing clinical progression for dementia prevention trial: results from the HBA trial. Alzheimer's and Dementia 2014;10(4):P138. [Google Scholar]
Schuurman 1980 {published data only}
- Schuurman JH, Haes WF, Huisman J. Effects of the automatic telephone answering service on venereal disease in Rotterdam. Health Education Journal 1980;39(2):47‐51. [DOI] [PubMed] [Google Scholar]
Scott 2011 {published data only}
- Scott GA. Treat to target using interactive voice messaging to enhance primary care physician management of hypertension. The Journal of Clinical Hypertension 2011;13(Suppl 1):A158. [Google Scholar]
Seto 2012 {published data only}
- Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Mobile phone‐based tele‐monitoring for heart failure management: a randomised controlled trial. Journal of Medical Internet Research 2012;14(1):e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2014 {published data only}
- Shah SJ, Hong CS, Cronin PR, Bearnot BI, Richardson CA, Fosburgh BW, et al. Effectiveness of targeted phone calls to reduce noshows in a hospital‐based primary care clinic: A randomised controlled trial. Journal of General Internal Medicine 2014;29:S80‐S1. [Google Scholar]
Siddiqui 2011 {published data only}
- Siddiqui AA, Sifri R, Hyslop T, Andrel J, Rosenthal M, Vernon SW, et al. Race and response to colon cancer screening interventions. Preventive Medicine 2011;52(3‐4):262‐4. [DOI] [PubMed] [Google Scholar]
Silveira 2011 {published data only}
- Silveira MJ, Given CW, Cease KB, Sikorskii A, Given B, Northouse LL, et al. Cancer Carepartners: improving patients' symptom management by engaging informal caregivers. BMC Palliative Care 2011;10(21):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2000 {published data only}
- Simon G E, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ 2000;320(7234):550‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2004 {published data only}
- Simon GE, Ludman EJ, Tutty S, Operskalski B, Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomised controlled trial. Journal of the American Medical Association 2004;292(8):935‐42. [DOI] [PubMed] [Google Scholar]
Simon 2006 {published data only}
- Simon GE, Ludman EJ, Operskalski BH. Randomized trial of a telephone care management program for outpatients starting antidepressant treatment. Psychiatric Services 2006;57(10):1441‐5. [DOI] [PubMed] [Google Scholar]
Simpson 2011a {published data only}
- Simpson CA, Xie L, Blum ER, Tucker JA. Agreement between prospective interactive voice response telephone reporting and structured recall reports of risk behaviors in rural substance users living with HIV/AIDS. Psychology of Addictive Behaviors 2011;25(1):185‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simpson 2011b {published data only}
- Simpson T, Rosenthal C, Gurrad B, Luterek J, Kaysen D. A pilot study evaluating mechanisms of change among patients with comorbid PTSD and alcohol dependence: methods and feasibility. Alcoholism: Clinical and Experimental Research 2011;35(6):142A. [Google Scholar]
Skolarus 2012 {published data only}
- Skolarus TA, Holmes‐Rovner M, Hawley ST, Dunn RL, Barr KLC, Willard NR, et al. Monitoring quality of life among prostate cancer survivors: the feasibility of automated telephone assessment. Urology 2012;80(5):1021‐6. [DOI] [PubMed] [Google Scholar]
Soran 2008 {published data only}
- Soran OZ, Pina IL, Lamas GA, Kelsey SF, Selzer F, Pilotte J, et al. A randomised clinical trial of the clinical effects of enhanced heart failure monitoring using a computer‐based telephonic monitoring system in older minorities and women. Journal of Cardiac Failure 2008;14(9):711‐7. [DOI] [PubMed] [Google Scholar]
Statland 2011 {published data only}
- Statland JM, Wang Y, Richesson R, Bundy B, Herbelin L, Gomes J, et al. An interactive voice response diary for patients with non‐dystrophic myotonia. Muscle and Nerve 2011;44(1):30‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stevens 2008 {published data only}
- Stevens VJ, Funk KL, Brantley PJ, Erlinger TP, Myers VH, Champagne CM, et al. Design and implementation of an interactive website to support long‐term maintenance of weight loss. Journal of Medical Internet Research 2008;10(1):e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stiles‐Shields 2014 {published data only}
- Stiles‐Shields C, Kwasny MJ, Cai X, Mohr DC. Therapeutic alliance in face‐to‐face and telephone‐administered cognitive behavioral therapy. Journal of Consulting and Clinical Psychology 2014;82(2):349‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stockwell 2012 {published data only}
- Stockwell MS, Kharbanda EO, Martinez RA, Vargas CY, Vawdrey DK, Camargo S. Effect of a text messaging intervention on influenza vaccination in an urban, low‐income paediatric and adolescent population: a randomised controlled trial. JAMA 2012;307(16):1702‐8. [DOI] [PubMed] [Google Scholar]
Tourangeau 2002 {published data only}
- Tourangeau R, Steiger DM, Wilson D. Self‐administered questions by telephone ‐ evaluating interactive voice response. Public Opinion Quarterly 2002;66(2):265‐78. [Google Scholar]
Tucker 2013 {published data only}
- Tucker JA, Simpson CA, Huang J, Roth DL, Stewart KE. Utility of an interactive voice response system to assess antiretroviral pharmacotherapy adherence among substance users living with HIV/AIDS in the rural South. AIDS Patient Care STDS 2013;27(5):280‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
VanWormer 2009 {published data only}
- VanWormer J J, Martinez A M, Benson G A, Crain A L, Martinson B C, Cosentino D L, et al. Telephone counselling and home telemonitoring: the Weigh by Day Trial. Am J Health Behav 2009;33(4):445‐54. [DOI] [PubMed] [Google Scholar]
Veroff 2013 {published data only}
- Veroff DR, Ochoa‐Arvelo T, Venator B. A randomized study of telephonic care support in populations at risk for musculoskeletal preference‐sensitive surgeries. BMC Medical Informatics and Decision Making 2013;13(21):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vivier 2000a {published data only}
- Vivier PM, Alario AJ, O'Haire C, Dansereau LM, Jakum EB, Peter G. The impact of outreach efforts in reaching underimmunized children in a Medicaid managed care practice. Archives of Pediatric Adolescent Medicine 2000;154(12):1243‐7. [DOI] [PubMed] [Google Scholar]
Vivier 2000b {published data only}
- Vivier PM, Alario AJ, O'Haire C, Dansereau LM, Jakum EB, Peter G. The impact of outreach efforts in reaching underimmunized children in a Medicaid managed care practice. Archives of Pediatrics and Adolescent Medicine 2000;154(12):1243‐7. [DOI] [PubMed] [Google Scholar]
Wade 2010 {published data only}
- Wade M, Ruddy MC, Lonny R, Kummer P, Snyder A, Krakauer R. Impact of interactive home blood pressure monitoring on a hypertensive medicare population. Journal of Investigative Medicine 2010;58(4):651‐2. [Google Scholar]
Wu 2014a {published data only}
- Wu S, Ell K, Gross‐Schulman SG, Sklaroff LM, Katon WJ, Nezu AM, et al. Technology‐facilitated depression care management among predominantly Latino diabetes patients within a public safety net care system: comparative effectiveness trial design. Contemporary Clinical Trials 2014;37(2):342‐54. [DOI] [PubMed] [Google Scholar]
Wu 2014b {published data only}
- Wu S, Vidyanti I, Liu P, Hawkins C, Ramirez M, Guterman J, et al. Patient‐centered technological assessment and monitoring of depression for low‐income patients. Journal of Ambulatory Care Management 2014;37(2):138‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yoon 2008 {published data only}
Zhu 2012 {published data only}
- Zhu SH, Cummins SE, Wong S, Gamst AC, Tedeschi GJ, Reyes‐Nocon J. The effects of a multilingual telephone quitline for Asian smokers: a randomised controlled trial. Journal of the National Cancer Institute 2012;104(4):299‐310. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Almeida 2014 {published data only}
- Almeida FA, Pardo KA, Seidel RW, Davy BM, You W, Wall SS, et al. Design and methods of "diaBEAT‐it!": a hybrid preference/randomised control trial design using the RE‐AIM framework. Contemporary Clinical Trials 2014;38(2):383‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ashmore 2013 {published data only}
- Ashmore J, Russo R, Peoples J, Sloan J, Jackson BE, Bae S, et al. Chronic obstructive pulmonary disease self‐management activation research trial (COPD‐SMART): Design and methods. Contemporary Clinical Trials 2013;35(2):77‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo R, Coultas D, Ashmore J, Peoples J, Sloan J, Jackson BE, et al. Chronic obstructive pulmonary disease self‐management activation research trial (COPD‐SMART): results of recruitment and baseline patient characteristics. Contemporary Clinical Trials 2015;41:192‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2013 {published data only}
- Baker K, Ledingham A, Lavalley MP, Keysor JJ, Felson DT. Automated telephone‐linked communication: a novel approach to enhance long‐term adherence to resistance training exercise among people with knee osteoarthritis. Arthritis and Rheumatism 2013;65(Suppl 10):S776. [Google Scholar]
Droste 2013 {published data only}
- Droste DW, Vittore D, Spassova L, Rösch N. ICT‐supported CVD prevention through phone‐based automated lifestyle coaching. Journal of the Neurological Sciences 2013;333(Suppl 1):e257. [Google Scholar]
- Spassova L, Vittore D, Droste D, Rosch N. Automated lifestyle coaching for cerebro‐cardiovascular disease prevention. Studies in Health Technology and Informatics 2013;190:234‐6. [PubMed] [Google Scholar]
Emmons 2008 {published data only}
- Greaney ML, Jesus M, Sprunck‐Harrild KM, Tellez T, Bastani R, Battaglia TA, et al. Designing audience‐centred interactive voice response messages to promote cancer screenings among low‐income Latinas. Preventing Chronic Disease 2014;11:E40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Estabrooks 2011 {published data only}
- Estabrooks PA, Glasgow RE, Xu S, Dzewaltowski DA, Lee RE, Thomas D, et al. Building a multiple modality, theory‐based physical activity intervention: the development of CardiACTION. Psychology of Sport and Exercise 2011;12(1):46‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fellows 2012 {published data only}
- Fellows JL, Mularski R, Waiwaiole L, Funkhouser K, Mitchell J, Arnold K, et al. Health and economic effects from linking bedside and outpatient tobacco cessation services for hospitalised smokers in two large hospitals: study protocol for a randomised controlled trial. Trials 2012;13(129):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Forster 2015 {published data only}
- Forster AJ, Erlanger TE, Jennings A, Auger C, Buckeridge D, Walraven C, et al. Effectiveness of a computerized drug‐monitoring program to detect and prevent adverse drug events and medication non‐adherence in outpatient ambulatory care: Study protocol of a randomised controlled trial. Trials 2015;16(2):1‐7. [DOI: 10.1186/1745-6215-16-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glasgow 2007 {published data only}
- Glasgow RE, Christiansen SM, Kurz D, King DK, Woolley T, Faber AJ, et al. Engagement in a diabetes self‐management website: usage patterns and generalizability of program use. Journal of Medical Internet Research 2011;13(1):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heapy 2011 {published data only}
- Egan C, Higgins D, LaChappelle K, Czlapinski R, Kirlin J, Spreyer K, et al. Initial feasibility reports of a novel cognitive behavioral therapy (CBT) pain self‐management treatment modality. The Journal of Pain 2014;15(4):S109. [ClinicalTrials.gov Identifier:NCT01025752] [Google Scholar]
- Heapy AA, Higgins DM, LaChappelle KM, Kirlin J, Goulet JL, Czlapinski RA, et al. Cooperative pain education and self‐management (COPES): study design and protocol of a randomized non‐inferiority trial of an interactive voice response‐based self‐management intervention for chronic low back pain. BMC Musculoskeletal Disordders 2016;17(85):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kulnawan 2011 {published data only}
- Kulnawan N, Jiamjarasrangsi W, Suwanwalaikorn S, Kittisopee T, Meksawan K, Thadpitakkul N, et al. Diabetes telephone‐linked care system for self‐management support in Thailand. Journal of the Medical Association of Thailand 2011;94(10):1189‐97. [PubMed] [Google Scholar]
McDaniel 2010 {published data only}
- McDaniel AM, Vickerman KA, Stump TE, Monahan PO, Fellows JL, Weaver MT, et al. A randomised controlled trial to prevent smoking relapse among recently quit smokers enrolled in employer and health plan sponsored quitlines. BMJ Open 2015;5(6):e007260. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mooney 2010 {published data only}
- Mooney K, Berry P, Wong B, Donaldson G. Helping cancer‐family caregivers with end‐of‐life home symptom management: Initial evaluation of an automated symptom monitoring and coaching system.. Journal of Clinical Oncology 2014;32(Suppl 31):A85. [Google Scholar]
Mori 2009 {published data only}
- Seligowski AV, Pless Kaiser AP, Niles BL, Mori DL, King LA, King DW. Sleep quality as a potential mediator between psychological distress and diabetes quality of life in veterans with type 2 diabetes. Journal of Clinical Psychology 2013;69(10):1121‐31. [DOI] [PubMed] [Google Scholar]
NCT00505024 {published data only}
- NCT00505024. Interactive Voice Response System (IVRS) for Managing Symptoms of Patients Following Thoracic Surgery. clinicaltrials.gov/ct2/show/NCT00505024?term=NCT00505024&rank=1 (accessed 10 November 2016). [Google Scholar]
NCT00625638 {published data only}
- NCT00625638. Interactive Voice Response System in Advanced Cancer Patients [Symptom Assessment in Advanced Cancer Patients Using an Interactive Voice Response (IVR) System]. clinicaltrials.gov/ct2/show/NCT00625638?term=NCT00625638&rank=1 (accessed 10 November 2016).
NCT00876330 {published data only}
- NCT00876330. Improving Antihypertensive and Lipid‐Lowering Therapy (CERT2) [CERT‐HIT: A Multimodal Intervention to Improve Antihypertensive and Lipid‐lowering Therapy]. clinicaltrials.gov/ct2/show/NCT00876330?term=NCT00876330&rank=1 (accessed 10 November 2016).
NCT01079533 {published data only}
- NCT01079533. Initiation of Colon Cancer Screening in Veterans or "Start Screening Now" (SSN) [Initiation of Colon Cancer Screening in Veterans]. clinicaltrials.gov/ct2/show/NCT01079533?term=NCT01079533&rank=1 (accessed 10 November 2016).
NCT01120704 {published data only}
- NCT01120704. Evaluation of Treatments to Improve Smoking Cessation Medication Adherence. clinicaltrials.gov/ct2/show/NCT01120704?term=NCT01120704&rank=1 (accessed10 November 2016).
NCT01125371 {published data only}
- NCT01125371. Computerized Brief Alcohol Intervention (BI) for Binge Drinking HIV At‐Risk and Infected Women. clinicaltrials.gov/ct2/show/NCT01125371?term=NCT01125371&rank=1 (accessed10 November 2016).
NCT01131143 {published data only}
- NCT01131143. Trial of Provider‐to‐Patient Interactive Voice Response (IVR) Calls to Improve Weight Management in Community Health Centers (CHCs). clinicaltrials.gov/ct2/show/NCT01131143?term=NCT01131143&rank=1 (accessed10 November 2016).
NCT01188135 {published data only}
- NCT01188135. Antidepressant Adherence via Telephonic Interactive Voice Recognition (IVR). clinicaltrials.gov/ct2/show/NCT01188135?term=NCT01188135&rank=1 (accessed10 November 2016).
NCT01199666 {published data only}
- NCT01199666. Text Message Reminder‐Recalls For Early Childhood Vaccination [Text 4 Health‐Kids: Text Message Reminder‐Recalls For Early Childhood Vaccination]. clinicaltrials.gov/ct2/show/NCT01199666?term=NCT01199666&rank=1 (accessed 10 November 2016).
NCT01229722 {published data only}
- NCT01229722. ARemind: A Personalized System to Remind for Adherence (ARemind). clinicaltrials.gov/ct2/show/NCT01229722?term=NCT01229722&rank=1 (accessed10 November 2016).
NCT01260207 {published data only}
- NCT01260207. Using IVR to Maintain ACS Patients on Best Practice Guidelines (IVR‐ACS BPG) [Using Interactive Voice Response to Improve Disease Management and Compliance With Acute Coronary Syndrome Best Practice Guidelines]. clinicaltrials.gov/ct2/show/NCT01260207?term=NCT01260207&rank=1 (accessed 10 November 2016).
NCT01484717 {published data only}
- NCT01484717. Interactive Voice Response Technology to Mobilize Contingency Management for Smoking Cessation. clinicaltrials.gov/ct2/show/NCT01484717 (accessed10 November 2016).
NCT01530958 {published data only}
- NCT01530958. Kidney Awareness Registry and Education (KARE) [The Kidney Awareness Registry and Education Study]. clinicaltrials.gov/ct2/show/NCT01530958?term=NCT01530958&rank=1 (accessed10 November 2015).
NCT01609842 {published data only}
- NCT01609842. Hybrid Effectiveness‐Implementation Study to Improve Clopidogrel Adherence. clinicaltrials.gov/ct2/show/NCT01609842?term=NCT01609842&rank=1 (accessed10 November 2016).
NCT01672385 {unpublished data only}
- NCT01672385. Improving Transition Outcomes Through Accessible Health IT and Caregiver Support. clinicaltrials.gov/ct2/show/NCT01672385?term=NCT01672385&rank=1 (accessed10 November 2016).
NCT01672398 {published data only}
- NCT01672398. Trial of the CarePartner Program for Improving the Quality of Transition Support. clinicaltrials.gov/ct2/show/NCT01672398?term=NCT01672398&rank=1 (accessed10 November 2015).
NCT01700894 {published data only}
- NCT01700894. Women's Walking Program (WWP3) [Reducing Health Disparities in African American Women: Lifestyle Physical Activity Adherence]. clinicaltrials.gov/ct2/show/NCT01700894?term=NCT01700894&rank=1 (accessed 10 November 2016).
NCT01701791 {published data only}
- NCT01701791. Telemedicine for Depression in Primary Care [The Efficacy of Telemedicine for Improving Depression Outcomes in Primary Care]. clinicaltrials.gov/ct2/show/NCT01701791?term=NCT01701791&rank=1 (accessed 10 November 2016). [Google Scholar]
NCT01706380 {published data only}
- NCT01706380. 3M Study ‐ Maria Malmö Mobile Telephone Study [A Randomized Controlled Trial of Interactive Voice Response With and Without Personal Feedback in the Treatment of Adolescents With Substance Use Disorders]. clinicaltrials.gov/ct2/show/NCT01706380?term=NCT01706380&rank=1 (accessed10 November 2016).
NCT01737073; NCT02508285 {published data only}
- NCT02508285. Comprehensive Opioid Management in Patient Aligned Care Teams (COMPACT). clinicaltrials.gov/ct2/show/NCT01737073?term=NCT02508285&rank=1 (accessed10 November 2016).
NCT01756001 {published data only}
- NCT01756001. GlowCaps Adherence Randomized Control Trial [Using Behavioral Economics to Promote Medication Adherence and Habit Formation]. clinicaltrials.gov/ct2/show/NCT01756001?term=NCT01756001&rank=1 (accessed10 November 2016). [Google Scholar]
NCT01778751 {published data only}
- NCT01778751. Advanced Comprehensive Diabetes Care for Veterans With Poorly‐Controlled Diabetes. clinicaltrials.gov/ct2/show/NCT01778751?term=NCT01778751&rank=1 (accessed10 November 2016).
NCT01794988 {published data only}
- NCT01794988. Can Therapy Alter CNS Processing of Chronic Pain: A Longitudinal Study. clinicaltrials.gov/ct2/show/NCT01794988?term=NCT01794988&rank=1 (accessed10 November 2016).
NCT01852656 {published data only}
- NCT01852656. Effectiveness of Influenza Vaccine Reminder Systems. clinicaltrials.gov/ct2/show/NCT01852656?term=NCT01852656&rank=1 (accessed10 November 2016).
NCT01900561 {published data only}
- NCT01900561. Optimizing Veteran‐Centered Prostate Cancer Survivorship Care. clinicaltrials.gov/ct2/show/NCT01900561?term=NCT01900561&rank=1 (accessed10 November 2016).
NCT01940016 {published data only}
- NCT01940016. Communication & Peer Support Effects on Physical Activity in Overweight Postmenopausal Women (BePHIT) [A Feasibility Study on the Effects of Tailored Communication and Health Coach Support on Physical Activity in Overweight Postmenopausal Women: BePHIT]. clinicaltrials.gov/ct2/show/NCT01940016?term=NCT01940016&rank=1 (accessed 10 November 2016).
NCT01953653 {published data only}
- NCT01953653. Feasibility of Using a Structured Daily Diary [Feasibility of Using a Structured Daily Diary to Assess Mood, Stressful Events, Support, Substance Use, and Sexual Behavior in HIV‐Positive Young Men Who Have Sex With Men]. clinicaltrials.gov/ct2/show/NCT01953653?term=NCT01953653&rank=1 (accessed 10 November 2016).
NCT01958359 {published data only}
- NCT01958359. Screening and Brief Intervention Via IVR for Problematic Use of Alcohol: A Randomized Controlled Trial. clinicaltrials.gov/ct2/show/NCT01958359?term=NCT01958359&rank=1 (accessed10 November 2016).
NCT01973946 {published data only}
- NCT01973946. Cancer Symptom Monitoring Telephone System With Nurse Practitioner (NP) Follow up [Telephone Linked Care: An IT Enabled Integrated System for Cancer Symptom Relief]. clinicaltrials.gov/ct2/show/NCT01973946?term=NCT01973946&rank=1 (accessed10 November 2016).
NCT02001129 {published data only}
- NCT02001129. Improving Follow‐Up Adherence in a Primary Eye Care Setting [Improving Follow‐Up Adherence in a Primary Eye Care Setting: A Prospective, Randomized Controlled Trial]. clinicaltrials.gov/ct2/show/NCT02001129?term=NCT02001129&rank=1 (accessed10 November 2016).
NCT02043184 {published data only}
- NCT02043184. Improving Adherence to Oral Cancer Agents and Self Care of Symptoms Using an IVR. clinicaltrials.gov/ct2/show/NCT02043184?term=NCT02043184&rank=1 (accessed10 November 2016).
NCT02056002 {published data only}
- NCT02056002. Peer‐Driven Intervention for Sleep Apnea (PCORI) [Peer‐Driven Intervention as an Alternate Model of Care Delivery and Coordination for Sleep Apnea]. clinicaltrials.gov/ct2/show/NCT02056002?term=NCT02056002&rank=1 (accessed10 November 2016). [Google Scholar]
NCT02118454 {published data only}
- NCT02118454. Antiretroviral Adherence and Quality‐of‐life Support for HIV+ Patients in India With Twice‐daily Interactive Voice Response (IVR) Calls With Health and Mental Health Messaging Compared to Weekly IVR Survey Only Control Condition: The Mobile‐messaging Adherence and Support for Health Study, India. (MASHIndia) [ART Adherence Behaviour and Practices Among HIV Positives in Kolkata, India‐a Pilot Project]. clinicaltrials.gov/ct2/show/NCT02118454?term=NCT02118454&rank=1 (accessed 10 November 2016).
NCT02124980 {published data only}
- NCT02124980. Automated Recovery Line for Medication Assisted Treatment. clinicaltrials.gov/ct2/show/NCT02124980?term=NCT02124980&rank=1 (accessed10 November 2016).
NCT02204956 {published data only}
- NCT02204956. Smoking Cessation Following Psychiatric Hospitalization [Extended Care for Smoking Cessation Following Psychiatric Hospitalization]. clinicaltrials.gov/ct2/show/NCT02204956?term=NCT02204956&rank=1 (accessed10 November 2016).
NCT02240420 {published data only}
- NCT02240420. Diabetes Prevention Among Post‐partum Women With History of Gestational Diabetes (Star‐Mama) [Reaching High Risk Post‐partum Women for Nutritional Assessment and Counseling Via a Telephone‐based Coaching Program]. clinicaltrials.gov/ct2/show/NCT02240420?term=NCT02240420&rank=1 (accessed10 November 2016).
NCT02266277 {published data only}
- NCT02266277. System Alignment for VaccinE Delivery (SAVED): Improving Rates of Influenza and Pneumococcal Vaccination Through Patient Outreach, Improved Medical Record Accuracy and Targeted Physician Alerts. clinicaltrials.gov/ct2/show/NCT02266277?term=NCT02266277&rank=1 (accessed10 November 2016).
NCT02328326 {published data only}
- NCT02328326. Caring Others Increasing EngageMent in PACT (CO‐IMPACT) [Engaging Veterans and Family Supporters in PACT to Improve Diabetes Management]. clinicaltrials.gov/ct2/show/NCT02328326?term=NCT02328326&rank=1 (accessed10 November 2016).
NCT02360605 {published data only}
- NCT02360605. Health Literacy Interventions to Overcome Disparities in CRC Screening. clinicaltrials.gov/ct2/show/NCT02360605 (accessed10 November 2016).
NCT02382731 {published data only}
- NCT02382731. Previous Study | Return to List | Next StudyInterventions to Support Long‐Term Adherence aNd Decrease Cardiovascular Events Post‐Myocardial Infarction (ISLAND). clinicaltrials.gov/ct2/show/NCT02382731?term=NCT02382731&rank=1 (accessed10 November 2016).
NCT02429297 {published data only}
- NCT02429297. Developing Accessible Telehealth Programs for Diabetes and Hypertension Management in Bolivia. clinicaltrials.gov/ct2/show/NCT02429297?term=NCT02429297&rank=1 (accessed10 November 2016).
NCT02442089 {published data only}
- NCT02442089. Impact of Automated Calls on Pediatric Patient Attendance in Chile (Health Call) [Health Call: A Randomized Control Trial of Interactive Automated Reminder Calls to Reduce Failure to Attend Rates at an Urban Referral Hospital in Chile]. clinicaltrials.gov/ct2/show/NCT02442089?term=NCT02442089&rank=1 (accessed 10 November 2016).
NCT02478359 {published data only}
- NCT02478359. Walk On! Physical Activity Coaching [Patient‐Centered Physical Activity Coaching in COPD: A Pragmatic Trial]. clinicaltrials.gov/ct2/show/NCT02478359?term=NCT02478359&rank=1 (accessed10 November 2016).
Ratanawongsa 2012 {published data only}
- Ratanawongsa N, Handley MA, Quan J, Sarkar U, Pfeifer K, Soria C, et al. Quasi‐experimental trial of diabetes Self‐Management Automated and Real‐Time Telephonic Support (SMARTSteps) in a Medicaid managed care plan: study protocol. BMC Health Services Research 2012;12(22):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reid 2015 {published data only}
- Reid ZZ, Regan S, Kelley JH, Streck JM, Ylioja T, Tindle HA, et al. Comparative effectiveness of post‐discharge strategies for hospitalised smokers: study protocol for the Helping HAND 2 randomised controlled trial. BMC Public Health 2015;15(109):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ritchie 2012 {published data only}
- Ritchie C, Richman J, Sobko H, Bodner E, Phillips B, Houston T. The E‐Coach transition support computer telephony implementation study: protocol of a randomised trial. Contemporary Clinical Trials 2012;33(6):1172‐9. [DOI] [PubMed] [Google Scholar]
Silveira 2010 {published data only}
- Silveira MJ, Given CW, Cease KB, Sikorskii A, Given B, Northouse LL, et al. Cancer Carepartners: Improving patients' symptom management by engaging informal caregivers. BMC Palliative Care 2011;10(21):1‐11. [NCT00983892] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2013 {published data only}
- Smith C, Ngo TD, Edwards P, Free C. MObile Technology for Improved Family planning: update to randomised controlled trial protocol. Trials 2014;15(440):1‐3. [NCT01823861] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C, Vannak U, Sokhey L, Ngo TD, Gold J, Khut K, et al. MObile Technology for Improved Family planning services (MOTIF): study protocol for a randomised controlled trial. Trials 2013;14(427):1‐9. [NCT01823861] [DOI] [PMC free article] [PubMed] [Google Scholar]
Te Boveldt 2011 {published data only}
- Boveldt N, Engels Y, Besse K, Vissers K, Vernooij‐Dassen M. Rationale, design, and implementation protocol of the Dutch clinical practice guideline pain in patients with cancer: a cluster randomised controlled trial with Short Message Service (SMS) and Interactive Voice Response (IVR). Implementation Science: IS 2011;6:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boveldt ND, Engels Y, Besse TC, Vissers KCP, Vernooij‐Dassen MJ. Implementation of the dutch clinical practice guideline pain in patients with cancer: A clustered randomised controlled trial with short message service (SMS) and interactive voice response (IVR). Palliative Medicine 2012;26(4):455‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wright 2014 {published data only}
- Wright JA, Quintiliani LM, Turner‐McGrievy GM, Migneault JP, Heeren T, Friedman RH. Comparison of two theory‐based, fully automated telephone interventions designed to maintain dietary change in healthy adults: study protocol of a three‐arm randomised controlled trial. JMIR Research Protocols 2014;3(4):e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abraham 2008
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychology 2008;27(3):379‐87. [DOI] [PubMed] [Google Scholar]
Abu‐Hasaballah 2007
- Abu‐Hasaballah A, James A, Aseltine HR Jr. Lessons and pitfalls of interactive voice response in medical research. Contemporary Clinical Trials 2007;28(5):593‐602. [DOI] [PubMed] [Google Scholar]
Ajzen 1985
- Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J editor(s). Action Control: From Cognition to Behavior. New York: Springer‐Verlag, 1985:11‐39. [Google Scholar]
Bandura 2001
- Bandura A. Social cognitive theory: an agentic perspective. Annual Review of Psychology 2001;52:1‐26. [DOI] [PubMed] [Google Scholar]
Baranowski 2012
- Baranowski T, Frankel L. Gaming and technology for weight control and health promotion in children. Childhood Obesity 2012;8(1):34‐7. [DOI] [PubMed] [Google Scholar]
Barlow 2002
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self‐management approaches for people with chronic conditions: a review. Patient Education and Counseling 2002;48(2):177‐87. [DOI] [PubMed] [Google Scholar]
Car 2004
- Car J, Sheikh A. Email consultations in health care: 1‐scope and effectiveness. BMJ 2004;329(7643):435‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carolan 2014
- Carolan I, Smith T, Hall A, Swallow VM. Emerging communities of child‐healthcare practice in the management of long‐term conditions such as chronic kidney disease: qualitative study of parents' accounts. BMC Health Services Research 2014;14(292):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cash‐Gibson 2012
- Cash‐Gibson L, Felix LM, Minorikawa N, Pappas Y, Gunn LH, Majeed A, Atun R, Car J. Automated telephone communication systems for preventive healthcare and management of long‐term conditions (Protocol). Cochrane Database of Systematic Reviews 2012;Art. No.: CD009921. DOI: 10.1002/14651858.CD009921(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
Centre for Reviews and Dissemination 2008
- University of York, Centre for Reviews and Dissemination. Systematic reviews: CRDs guidance for undertaking reviews in health care. www.york.ac.uk/inst/crd/pdf/Systematic_Reviews.pdf (accessed prior to 30 October 2016).
Chandler 2013
- Chandler J, Churchill R, Higgins J, Lasserson T, Tovey D. Methodological Standards for the Conduct of New Cochrane Intervention Reviews Booklet Version 1. The Cochrane Collaboration, 2013. Available from editorial‐unit.cochrane.org/sites/editorial‐unit.cochrane.org/files/uploads/PLSBooklet2.pdf.
Corkrey 2002b
- Corkrey R, Parkinson L. Interactive voice response: review of studies 1989‐2000. Behavior Research Methods, Instruments, and Computers 2002;34(3):342‐53. [DOI] [PubMed] [Google Scholar]
Delichatsios 2001
- Delichatsios HK, Friedman RH, Glanz K, Tennstedt S, Smigelski C, Pinto BM, et al. Randomized trial of a "talking computer" to improve adults' eating habits. American Journal of Health Promotion 2001;15(4):215‐24. [DOI] [PubMed] [Google Scholar]
Demain 2015
- Demain S, Goncalves AC, Areia C, Oliveira R, Marcos AJ, Marques A, et al. Living with, managing and minimising treatment burden in long term conditions: a systematic review of qualitative research. PLOS ONE 2015;10(5):e0125457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edelman 2000
- Edelman JR. Psychosocial Aspects of the Health Care Process. Essex: Pearson Education Limited, 2000. [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
EndNote 2015 [Computer program]
- Thomson Reuters [Computer program]. Version X7.3 for Windows. Philadelphia: Clarivate Analytics, 2015.
Family Health Teams 2006
- Family Health Teams. Advancing primary health care: guide to health promotion and disease prevention. Family Health Teams 2006:1‐12.
Fisher 2007
- Fisher L, Glasgow RE. A call for more effectively integrating behavioral and social science principles into comprehensive diabetes care. Diabetes Care 2007;30(10):2746‐9. [DOI] [PubMed] [Google Scholar]
Galdas 2015
- Galdas P, Darwin Z, Fell J, Kidd L, Bower P, Blickem C, et al. A systematic review and meta ethnography to identify how effective, cost‐effective, accessible and acceptable self‐management support interventions are for men with long‐term conditions (SELF‐MAN). Health Services and Delivery Research 2015;3(34):1‐336. [DOI: 10.3310/hsdr03340] [DOI] [Google Scholar]
Gammon 2015
- Gammon D, Berntsen GK, Koricho AT, Sygna K, Ruland C. The chronic care model and technological research and innovation: a scoping review at the crossroads. Journal of Medical Internet Research 2015;17(2):e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gee 2015
- Gee PM, Greenwood DA, Paterniti DA, Ward D, Miller LM. The eHealth Enhanced Chronic Care Model: a theory derivation approach. Journal of Medical Internet Research 2015;17(4):e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glasgow 2004
- Glasgow ER, Bull SS, Piette JD, Steiner JF. Interactive behaviour change technology: a partial solution to the competing demands of primary care. American Journal of Preventive Medicine 2004;27(2):80‐7. [DOI] [PubMed] [Google Scholar]
Glenton 2010
- Glenton C, Santesso N, Rosenbaum S, Stromme Nilsen E, Radar T, Ciapponi A, et al. Presenting the results of Cochrane systematic reviews to a consumer audience: a qualitative study. Medical Decision Making 2010;30(5):566‐77. [DOI] [PubMed] [Google Scholar]
Gourlan 2015
- Gourlan M, Bernard P, Bortolon C, Romain AJ, Lareyre O, Carayol M, et al. Efficacy of theory‐based interventions to promote physical activity. a meta‐analysis of randomised controlled trials. Health Psychology Review 2016;10(1):50‐66. [DOI] [PubMed] [Google Scholar]
GRADEpro 2016 [Computer program]
- GRADEprofiler [Computer program on www.gradepro.org]. McMaster University, 2014, Version [2016].
Gullotta 2014
- Gullotta TP, Bloom M. The Encyclopaedia of Primary Prevention and Health Promotion. 2nd Edition. Springer US, 2014. [Google Scholar]
Gurol‐Urganci 2013
- Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Atun R, Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD007458.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haluza 2015
- Haluza D, Jungwirth D. ICT and the future of health care: aspects of health promotion. International Journal of Medical Informatics. 2015;84(1):48‐57. [DOI] [PubMed] [Google Scholar]
Hardeman 2005
- Hardeman W, Sutton S, Griffin S, Johnston M, White A, Wareham NJ, et al. A causal modelling approach to the development of theory‐based behaviour change programmes for trial evaluation. Health Education Research 2005;20(6):676‐87. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JP, White IR, Wood AM. Imputation methods for missing outcome data in meta‐analysis of clinical trials. Clinical Trials 2008;5(3):225‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Jackson 2005
- Jackson N, Waters E. Criteria for the systematic review of health promotion and public health interventions: for the Guidelines for Systematic Reviews in Health Promotion and Public Health Taskforce. Health Promotion International 2005;20(4):367‐74. [DOI] [PubMed] [Google Scholar]
Jekauc 2015
- Jekauc D, Volkle M, Wagner MO, Mess F, Reiner M, Renner B. Prediction of attendance at fitness center: a comparison between the theory of planned behavior, the social cognitive theory, and the physical activity maintenance theory. Frontiers in Psychology 2015;6(121):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kelly 2009
- Kelly MP, Stewart E, Morgan A, Killoran A, Fischer A, Threlfall A, et al. A conceptual framework for public health: NICE's emerging approach. Public Health 2009;123(1):e14‐e20. [DOI] [PubMed] [Google Scholar]
Krauss 2001
- Krauss, RM. The psychology of verbal communication. International Encyclopedia of the Social & Behavioral Sciences. Elsevier, 2001:16161‐5. [Google Scholar]
Krishna 2002
- Krishna S, Balas EA, Boren SA, Maglaveras N. Patient acceptance of educational voice messages: a review of controlled clinical studies. Methods of Information in Medicine 2002;41(5):360‐9. [PubMed] [Google Scholar]
Krupinski 2006
- Krupinski E, Dimmick S, Grigsby J, Mogel G, Puskin D, Speedie S, et al. Research recommendations for the American Telemedicine Association. Telemedicine Journal and E‐health 2006;12(5):579‐89. [DOI] [PubMed] [Google Scholar]
Lee 2003
- Lee H, Friedman ME, Cukor P, Ahern D. Interactive voice response system (IVRS) in health care services. Nursing Outlook 2003;51(6):277‐83. [DOI] [PubMed] [Google Scholar]
Lee 2011
- Lee A, Siu CF, Leung KT, Lau LCH, Chan CCM, Wong KK. General practice and social service partnership for better clinical outcomes, patient self efficacy and lifestyle behaviours of diabetic care: randomised control trial of a chronic care model. Postgraduate Medical Journal 2011;87(1032):688‐93. [DOI] [PubMed] [Google Scholar]
Leventhal 1984
- Leventhal H, Nerenz DR, Steele DJ. Illness representations and coping with health threats. In: Baum A, Taylor SE, Singer JE editor(s). Handbook of Psychology and Health. Vol. 4, Hilsdale, NJ: Lawrence Erlbaum Associates, 1984. [Google Scholar]
Lewin 2015
- Lewin S, Noyes J, Chandler J, Hendry M on behalf of the iCAT_SR group. Improving understanding of intervention complexity: the Intervention Complexity Assessment Tool for Systematic Reviews (iCAT_SR). 2013.colloquium.cochrane.org/abstracts/improving‐understanding‐intervention‐complexity‐intervention‐complexity‐assessment‐tool‐sy.html (accessed 10 November 2016). [Google Scholar]
Lieberman 2012
- Lieberman G, Naylor MR. Interactive voice response technology for symptom monitoring and as an adjunct to the treatment of chronic pain. Translational Behavioural Medicine 2012;2(1):93‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2014
- Liu Q, Abba K, Alejandria MM, Sinclair D, Balanag VM, Lansang MA. Reminder systems to improve patient adherence to tuberculosis clinic appointments for diagnosis and treatment. Cochrane Database of Systematic Reviews 2014, Issue 11. [DOI: 10.1002/14651858.CD006594.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maheu 2001
- Maheu MM, Whitten P, Allen A. E‐Health, Telehealth, and Telemedicine. San Francisco, CA: Jossey Bass, 2001. [Google Scholar]
McCorkle 2011
- McCorkle R, Ercolano E, Lazenby M, Schulman‐Green D, Schilling LS, Lorig K, et al. Self‐management: enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer Journal for Clinicians 2011;61(1):50‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Michie 2009
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta‐regression. Health Psychology 2009;28(6):690‐701. [DOI] [PubMed] [Google Scholar]
Michie 2010
- Michie S, Prestwich A. Are interventions theory‐based? Development of a theory coding scheme. Health Psychology 2010;29(1):1‐8. [DOI] [PubMed] [Google Scholar]
Michie 2011
- Michie S, Hyder N, Walia A, West R. Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation. Addictive Behaviors 2011;36(4):315‐9. [DOI] [PubMed] [Google Scholar]
Mundt 2001
- Mundt JC, Ferber KL, Rizzo M, Greist JH. Computer‐automated dementia screening using a touch tone telephone. Archives of Internal Medicine 2001;161(20):2481‐7. [DOI] [PubMed] [Google Scholar]
O'Dowd 2014
- O'Dowd A. NHS plans new workforce for long term conditions. BMJ 2014;349:g5667. [DOI] [PubMed] [Google Scholar]
Oake 2009b
- Oake N, Jennings A, Walraven C, Forster AJ. Interactive voice response systems for improving delivery of ambulatory care. American Journal of Managed Care 2009;15(6):383‐91. [PubMed] [Google Scholar]
Pappas 2011
- Pappas Y, Car J. Emerging technologies for health communication. In: Hill S editor(s). The Knowledgeable Patient: Communication and Participation in Health. Oxford: Wiley‐Blackwell, 2011:208‐17. [Google Scholar]
Piatt 2006
- Piatt GA, Orchard TJ, Emerson S, Simmons D, Songer T, Brooks MM, et al. Translating the chronic care model into the community: results from a randomised controlled trial of a multifaceted diabetes care intervention. Diabetes Care 2006;29(4):811‐7. [DOI: 10.2337/diacare.29.04.06.dc05-1785] [DOI] [PubMed] [Google Scholar]
Piette 2007
- Piette JD. Interactive behavior change technology to support diabetes self‐management: where do we stand?. Diabetes Care 2007;30(10):2425‐32. [DOI: 10.2337/dc07-1046] [DOI] [PubMed] [Google Scholar]
Piette 2012c
- Piette JD, Lun KC, Moura LA, Fraser HS, Mechael PN, Powell J, et al. Impacts of e‐health on the outcomes of care in low‐ and middle‐income countries: where do we go from here?. Bulletin of the World Health Organization 2012;90(5):365‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prochaska 1984
- Prochaska J, DiClemente C. The Transtheoretical Approach: Crossing Traditional Boundaries of Therapy. Homewood, IL: Dow Jones‐Irwin, 1984. [Google Scholar]
Puskin 2010
- Puskin DS, Cohen Z, Ferguson AS, Krupinski E, Spaulding R. Implementation and evaluation of telehealth tools and technologies. Telemedicine Journal and E‐Health 2010;16(1):96‐102. [DOI] [PubMed] [Google Scholar]
Reidel 2008
- Reidel K, Tamblyn R, Patel V, Huang A. Pilot study of an interactive voice response system to improve medication refill compliance. BMC Medical Informatics and Decision Making 2008;9(8):46. [DOI: 10.1186/1472-6947-8-46] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rodgers 2009
- Rodgers M, Sowden A, Petticrew M, Arai L, Roberts H, Britten N, et al. Testing methodological guidance on the conduct of narrative synthesis in systematic reviews: effectiveness of interventions to promote smoke alarm ownership and function. Evaluation 2009;15(1):49‐73. [Google Scholar]
Rosen 2015
- Rosen RC, Stephens‐Shields AJ, Cunningham GR, Cifelli D, Cella D, Farrar JT, et al. Comparison of interactive voice response (IVR) with paper administration of instruments to assess functional status, sexual function, and quality of life in elderly men. Quality of Life Research 2016;25(4):811‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosenstock 1974
- Rosenstock I. Historical origins of the Health Belief Model. Health Education Monographs 1974;2(4):336‐53. [DOI] [PubMed] [Google Scholar]
Ryan 2011
- Ryan R, Hill S, Prictor M, McKenzie J, Cochrane Consumers and Communication Review Group. Study Quality Guide. www.latrobe.edu.au/chcp/assets/downloads/StudyQualityGuide_May2011.pdf (accessed 24 April 2015).
Ryan 2009
- Ryan R, Hill S, Broclain D, Horey D, Oliver S, Prictor M, Cochrane Consumers and Communication Review Group. Study Design Guide. www.latrobe.edu.au/chcp/cochrane/resources.html (accessed 24 May 2011).
Sawmynaden 2012
- Sawmynaden P, Atherton H, Majeed A, Car J. Email for the provision of information on disease prevention and health promotion. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD007982.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schroder 2009
- Schroder EEK, Johnson JC. Interactive voice response technology to measure HIV‐related behaviour. Current HIV/AIDS Reports 2009;6(4):210‐6. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Presenting results and 'Summary of findings' tables. In: In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available at www.cochrane‐handbook.org. [ Available at www.cochrane‐handbook.org; accessed 26.03.2015]
Ukoumunne 1999
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JA, Burney PG. Methods for evaluating area‐wide and organisation‐based interventions in health and health care: a systematic review. Health Technology Assessment 1999;3(5):iii‐92. [PubMed] [Google Scholar]
Van Velthoven 2013
- Van‐Velthoven MH, Tudor Car L, Gentry S, Car J. Telephone delivered interventions for preventing HIV infection in HIV‐negative persons. Cochrane Database of Systematic Reviews 2013, Issue 5. [DOI: 10.1002/14651858.CD009190.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vo 2015
- Vo PT, Bogg T. Testing Theory of Planned Behavior and Neo‐Socioanalytic Theory models of trait activity, industriousness, exercise social cognitions, exercise intentions, and physical activity in a representative U.S. sample. Frontiers in Psychology 2015;6:1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vodopivec‐Jamsek 2012
- Vodopivec‐Jamsek V, Jongh T, Gurol‐Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD007457.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagner 2002
- Wagner EH, Davis C, Schaefer J, Korff M, Austin B. A survey of leading chronic disease management programs: are they consistent with the literature?. Journal of Nursing Care Quality 2002;16(2):67‐80. [PubMed] [Google Scholar]
Webb 2006
- Webb M, Howson H. International overview of the evidence on effective service models in chronic disease management. wales.gov.uk/topics/health/publications/health/reports/internatoverviewchronicdisease?lang=en (accessed 26 May 2011).
Webb 2010
- Webb TL, Joseph J, Yardley L, Michie S. Using the Internet to promote health behavior change: a systematic review and meta‐analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research 2010;12(1):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2001
- Williams C, Whitfield G. Written and computer‐based self‐help treatments for depression. British Medical Bulletin 2001;57(1):133‐44. [DOI] [PubMed] [Google Scholar]
World Bank 2012
- The World Bank. World development report 2012. World development report 2012. Vol. ISBN: 978‐0‐8213‐8825‐9, Washington, DC, 2012. [Google Scholar]
References to other published versions of this review
Cash‐Gibson
- Cash‐Gibson L, Felix LM, Minorikawa N, Pappas Y, Gunn LH, Majeed A, et al. Automated telephone communication systems for preventive healthcare and management of long‐term conditions. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD009921] [DOI] [PMC free article] [PubMed] [Google Scholar]


