Abstract
Background
This is an updated version of the original Cochrane Review, first published in Issue 1, 2003 and updated in 2015. This review is one in a series of Cochrane Reviews investigating pair‐wise monotherapy comparisons.
Epilepsy is a common neurological condition in which abnormal electrical discharges from the brain cause recurrent unprovoked seizures. It is believed that with effective drug treatment, up to 70% of individuals with active epilepsy have the potential to become seizure‐free and go into long‐term remission shortly after starting drug therapy with a single antiepileptic drug in monotherapy.
Worldwide, carbamazepine and phenobarbitone are commonly used broad‐spectrum antiepileptic drugs, suitable for most epileptic seizure types. Carbamazepine is a current first‐line treatment for partial onset seizures, and is used in the USA and Europe. Phenobarbitone is no longer considered a first‐line treatment because of concerns over associated adverse events, particularly documented behavioural adverse events in children treated with the drug. However, phenobarbitone is still commonly used in low‐ and middle‐income countries because of its low cost. No consistent differences in efficacy have been found between carbamazepine and phenobarbitone in individual trials; however, the confidence intervals generated by these studies are wide, and therefore, synthesising the data of the individual trials may show differences in efficacy.
Objectives
To review the time to withdrawal, remission, and first seizure of carbamazepine compared with phenobarbitone when used as monotherapy in people with partial onset seizures (simple or complex partial and secondarily generalised) or generalised onset tonic‐clonic seizures (with or without other generalised seizure types).
Search methods
For the latest update, we searched the following databases on 18 August 2016: the Cochrane Epilepsy Group Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies Online (CRSO), MEDLINE (Ovid, from 1946), the US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov), and the World Health Organization International Clinical Trials Registry Platform (ICTRP). Previously we also searched SCOPUS (from 1823) as an alternative to Embase, but this is no longer necessary, because randomised controlled trials (RCTs) and quasi‐RCTs in Embase are now included in CENTRAL. We handsearched relevant journals and contacted pharmaceutical companies, original trial investigators, and experts in the field.
Selection criteria
RCTs in children or adults with partial onset seizures or generalised onset tonic‐clonic seizures with a comparison of carbamazepine monotherapy versus phenobarbitone monotherapy.
Data collection and analysis
This was an individual participant data (IPD) review. Our primary outcome was 'time to withdrawal of allocated treatment', and our secondary outcomes were 'time to achieve 12‐month remission', 'time to achieve six‐month remission', 'time to first seizure post‐randomisation', and 'adverse events'. We used Cox proportional hazards regression models to obtain study‐specific estimates of hazard ratios (HRs) with 95% confidence intervals (CIs), with the generic inverse variance method used to obtain the overall pooled HR and 95% CI.
Main results
IPD were available for 836 participants out of 1455 eligible individuals from six out of 13 trials; 57% of the potential data. For remission outcomes, HR > 1 indicated an advantage for phenobarbitone, and for first seizure and withdrawal outcomes, HR > 1 indicated an advantage for carbamazepine.
The main overall results (pooled HR adjusted for seizure type, 95% CI) were HR 1.50 for time to withdrawal of allocated treatment (95% CI 1.15 to 1.95; P = 0.003); HR 0.93 for time to achieve 12‐month remission (95% CI 0.72 to 1.20; P = 0.57); HR 0.99 for time to achieve six‐month remission (95% CI 0.80 to 1.23; P = 0.95); and HR 0.87 for time to first seizure (95% CI 0.72 to 1.06; P = 0.18). Results suggest an advantage for carbamazepine over phenobarbitone in terms of time to treatment withdrawal and no statistically significant evidence between the drugs for the other outcomes. We found evidence of a statistically significant interaction between treatment effect and seizure type for time to first seizure recurrence (Chi² test for subgroup differences P = 0.03), where phenobarbitone was favoured for partial onset seizures (HR 0.76, 95% CI 0.60 to 0.96; P = 0.02) and carbamazepine was favoured for generalised onset seizures (HR 1.23, 95% CI 0.88 to 1.77; P = 0.27). We found no evidence of an interaction between treatment effect and seizure type for the other outcomes. However, methodological quality of the included studies was variable, with 10 out of the 13 included studies (4 out of 6 studies contributing IPD) judged at high risk of bias for at least one methodological aspect, leading to variable individual study results, and therefore, heterogeneity in the analyses of this review. We conducted sensitivity analyses to examine the impact of poor methodological aspects, where possible.
Authors' conclusions
Overall, we found evidence suggestive of an advantage for carbamazepine in terms of drug effectiveness compared with phenobarbitone (retention of the drug in terms of seizure control and adverse events) and evidence suggestive of an association between treatment effect and seizure type for time to first seizure recurrence (phenobarbitone favoured for partial seizures and carbamazepine favoured for generalised seizures). However, this evidence was judged to be of low quality due to poor methodological quality and the potential impact on individual study results (and therefore variability (heterogeneity) present in the analysis within this review), we encourage caution when interpreting the results of this review and do not advocate that the results of this review alone should be used in choosing between carbamazepine and phenobarbitone. We recommend that future trials should be designed to the highest quality possible with considerations for allocation concealment and masking, choice of population, choice of outcomes and analysis, and presentation of results.
Keywords: Adult; Child; Humans; Anticonvulsants; Anticonvulsants/therapeutic use; Carbamazepine; Carbamazepine/therapeutic use; Epilepsies, Partial; Epilepsies, Partial/drug therapy; Epilepsy, Generalized; Epilepsy, Generalized/drug therapy; Epilepsy, Tonic‐Clonic; Epilepsy, Tonic‐Clonic/drug therapy; Phenobarbital; Phenobarbital/therapeutic use; Randomized Controlled Trials as Topic; Remission Induction; Seizures; Seizures/prevention & control
Title: Carbamazepine versus phenobarbitone monotherapy (single drug treatment) for epilepsy
Background
Epilepsy is a common neurological disorder in which abnormal electrical discharges from the brain cause recurrent seizures. We studied two types of epileptic seizures in this review: generalised onset seizures in which electrical discharges begin in one part of the brain and move throughout the brain, and partial onset seizures in which the seizure is generated in and affects one part of the brain (the whole hemisphere of the brain or part of a lobe of the brain).
For around 70% of people with epilepsy, a single antiepileptic drug can control generalised onset or partial onset seizures. Worldwide, phenobarbitone and carbamazepine are commonly used antiepileptic drugs; however, carbamazepine is used more commonly in the USA and Europe because of concerns over side‐effects associated with phenobarbitone, particularly concerns over behavioural changes in children treated with phenobarbitone. Phenobarbitone is still commonly used in developing countries in Africa, Asia, and South America because of the low cost of the drug.
Review methods
In this review, we evaluated the evidence from 13 randomised controlled clinical trials comparing phenobarbitone with carbamazepine based on how effective the drugs were at controlling seizures (i.e. whether people had recurrence of seizures or had long periods of freedom from seizures (remission)) and how tolerable any related side‐effects of the drugs were. We were able to combine data for 836 people from six of the 13 trials; for the remaining 619 people from seven trials, data were not available to use in this review.
Key results
Results of the review suggest that people are more likely to withdraw from phenobarbitone treatment earlier than from carbamazepine treatment, because of seizure recurrence, side‐effects of the drug, or both. Results also suggest that recurrence of seizures after starting treatment with phenobarbitone may happen earlier than treatment with carbamazepine for people with generalised seizures, but vice‐versa for people with partial onset seizures. We found no difference between carbamazepine and phenobarbitone for people achieving long periods of seizure freedom (six‐ or 12‐month remission of seizures).
Conclusions
We recommend that the results of this review are interpreted with caution as we were unable to combine the data for all people treated in trials comparing carbamazepine or phenobarbitone. Also, for four of the six trials used in our results, we found at least one problem in the design of the trial, which may have impacted upon the quality of the results of the individual trials, and therefore our results from combining trial data. We judge that the quality of the evidence in this review is low and we do not recommend using the results of this review alone for making a choice between carbamazepine or phenobarbitone for the treatment of epilepsy. We recommend that all future trials comparing these drugs or any other antiepileptic drugs should be designed using high quality methods to ensure results are also of high quality.
How up‐to‐date is this review?
The review authors searched for studies that had been published up to August 2016.
Summary of findings
Summary of findings for the main comparison.
Summary of findings ‐ Carbamazepine compared with phenobarbitone for epilepsy (primary outcome)
| Carbamazepine compared with phenobarbitone for epilepsy | ||||||
|
Patient or population: adults and children with newly onset partial or generalised epilepsy Settings: outpatients Intervention: carbamazepine Comparison: phenobarbitone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI)¹ | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Phenobarbitone | Carbamazepine | |||||
|
Time to withdrawal of allocated treatment ‐ all participants, stratified by epilepsy type Range of follow‐up (all participants): 0 to 4653 days |
390 per 1000 | 281 per 1000 (224 to 350) | HR 1.50 (1.15 to 1.95) | 676 (4 studies) |
⊕⊕⊝⊝ low2,3 | HR > 1 indicates a clinical advantage for carbamazepine |
|
Time to withdrawal of allocated treatment Subgroup: generalised onset seizures Range of follow‐up (all participants): 0 to 4653 days |
286 per 1000 | 197 per 1000 (110 to 340) | HR 1.53 (0.81 to 2.88) | 156 (3 studies) |
⊕⊕⊝⊝ low2,3 | HR > 1 indicates a clinical advantage for carbamazepine |
|
Time to withdrawal of allocated treatment Subgroup: partial onset seizures Range of follow‐up (all participants): 0 to 4272 days |
420 per 1000 | 307 per 1000 (239 to 385) | HR 1.49 (1.12 to 2.00) | 520 (4 studies) |
⊕⊕⊝⊝ low2,3 | HR > 1 indicates a clinical advantage for carbamazepine |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The assumed risk is calculated as the event rate in the phenobarbitone treatment group. The corresponding risk in the carbamazepine treatment group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). The corresponding risk is calculated as the assumed risk x the relative risk of the intervention where relative risk = (1 ‐ exp(HR x ln(1 ‐ assumed risk)) )/assumed risk. CI: confidence interval; RR: risk ratio; HR: hazard ratio; exp: exponential. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Pooled HR for all participants adjusted for seizure type. 2There was high risk of bias for at least one element of three studies included in the analysis; de Silva 1996 and Heller 1995 were open‐label, and the lack of masking may have influenced the withdrawal rates in the study. Placencia 1993 did not adequately conceal allocation for all participants, which may have influenced the withdrawal rates in the study. There were inconsistencies in Placencia 1993 between published data and IPD, which the authors could not resolve. 3Substantial heterogeneity was present between studies; sensitivity analyses showed that Placencia 1993 contributed the largest amount of variability to analysis.
Summary of findings 2.
Summary of findings ‐ Carbamazepine compared with phenobarbitone for epilepsy (secondary outcome)
| Carbamazepine compared with phenobarbitone for epilepsy | ||||||
|
Patient or population: adults and children with newly onset partial or generalised epilepsy Settings: outpatients Intervention: carbamazepine Comparison: phenobarbitone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI)¹ | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Phenobarbitone | Carbamazepine | |||||
|
Time to achieve 12‐month remission ‐ all participants, stratified by epilepsy type Range of follow‐up (all participants): 0 to 4222 days |
367 per 1000 | 346 per 1000 (280 to 422) |
HR 0.93 (0.72 to 1.20) |
683 (4 studies) | ⊕⊕⊝⊝ low2,3 | HR > 1 indicates a clinical advantage for phenobarbitone |
|
Time to achieve 12‐month remission Subgroup: generalised onset seizures Range of follow‐up (all participants): 0 to 4163 days |
500 per 1000 | 358 per 1000 (247 to 503) |
HR 0.64 (0.41 to 1.01) |
158 (3 studies) | ⊕⊕⊝⊝ low2,3 | HR > 1 indicates a clinical advantage for phenobarbitone |
|
Time to achieve 12‐month remission Subgroup: partial onset seizures Range of follow‐up (all participants): 0 to 4222 days |
329 per 1000 | 358 per 1000 (276 to 453) |
HR 1.11 (0.81 to 1.51) |
525 (4 studies) | ⊕⊕⊝⊝ low2,3 | HR > 1 indicates a clinical advantage for phenobarbitone |
|
Time to first seizure ‐ all participants, stratified by epilepsy type Range of follow‐up (all participants): 0 to 4108 days |
487 per 1000 | 536 per 1000 (467 to 604) |
HR 0.87 (0.72 to 1.06) |
822 (6 studies) |
⊕⊕⊝⊝ low4,5,6 | HR > 1 indicates a clinical advantage for carbamazepine |
|
Time to first seizure ‐ Subgroup: generalised onset seizures Range of follow‐up (all participants): 0 to 4108 days |
548 per 1000 | 475 per 1000 (361 to 602) |
HR 1.23 (0.86 to 1.77) |
238 (5 studies) |
⊕⊕⊝⊝ low4,5,6 | HR > 1 indicates a clinical advantage for carbamazepine |
|
Time to first seizure ‐ Subgroup: partial onset seizures Range of follow‐up (all participants): 0 to 4108 days |
462 per 1000 | 557 per 1000 (475 to 644) |
HR 0.76 (0.60 to 0.96) |
584 (6 studies) |
⊕⊕⊝⊝ low4,5,6 | HR > 1 indicates a clinical advantage for carbamazepine |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The assumed risk is calculated as the event rate in the phenobarbitone treatment group. The corresponding risk in the carbamazepine treatment group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). The corresponding risk is calculated as the assumed risk x the relative risk of the intervention where relative risk = (1 ‐ exp(HR x ln(1 ‐ assumed risk)) )/assumed risk. CI: confidence interval; RR: risk ratio; HR: hazard ratio; exp: exponential. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Pooled HR for all participants adjusted for seizure type. 2There was high risk of bias for at least one element of three studies included in the analysis; de Silva 1996 and Heller 1995 were open‐label, and the lack of masking may have influenced the withdrawal rates in the study. Placencia 1993 did not adequately conceal allocation for all participants, which may have influenced the withdrawal rates in the study and therefore the remission rates in the study. 3Substantial heterogeneity was present between studies; sensitivity analyses showed that Placencia 1993 contributed the largest amount of variability to the analysis. 4There was high risk of bias for at least one element of four studies included in the analysis; de Silva 1996 and Heller 1995 were open‐label, and the lack of masking may have influenced the withdrawal rates in the study. Placencia 1993 was not adequately concealed for all participants, which may have influenced the withdrawal rates in the study and therefore the seizure recurrence rates in the trial. There were inconsistencies between published data and IPD, which the authors could not resolve in Banu 2007. 5Substantial heterogeneity was present between studies; sensitivity analyses showed that Placencia 1993 and Ogunrin 2005 contributed the largest amount of variability to the analysis. 6Misclassification of seizure type in Ogunrin 2005 for 19 individuals may have impacted on the trial result. Sensitivity analysis to adjust for misclassification reduced the amount of heterogeneity in the analysis.
Background
This is an updated version of the original Cochrane Review, first published in Issue 1, 2003 (Tudur Smith 2003), and updated in 2015.
Description of the condition
Epilepsy is a common neurological condition in which abnormal electrical discharges from the brain cause recurrent unprovoked seizures. Epilepsy is a disorder of many heterogenous seizure types, with an estimated incidence of 33 to 57 per 100,000 person‐years worldwide (Annegers 1999; Hirtz 2007; MacDonald 2000; Olafsson 2005; Sander 1996), accounting for approximately 1% of the global burden of disease (Murray 1994).
The lifetime risk of epilepsy onset is estimated to be 1300 to 4000 per 100,000 person‐years (Hauser 1993; Juul‐Jenson 1983), and the lifetime prevalence could be as large as 70 million people worldwide (Ngugi 2010). It is believed that with effective drug treatment, up to 70% of individuals with active epilepsy have the potential to go into long‐term remission shortly after starting drug therapy (Cockerell 1995; Hauser 1993; Sander 2004), and around 70% of individuals can achieve seizure freedom using a single antiepileptic drug in monotherapy (Cockerell 1995). Current National Institute for Health and Care Excellence (NICE) guidelines recommend that both adults and children with epilepsy should be treated with monotherapy, wherever possible (NICE 2012). The remaining 30% of individuals experience refractory or drug‐resistant seizures, which often require treatment with combinations of antiepileptic drugs or alternative treatments, such as epilepsy surgery (Kwan 2000).
We studied two seizure types in this review: generalised onset seizures in which electrical discharges begin in one part of the brain and move throughout the brain, and partial onset seizures in which the seizure is generated in and affects one part of the brain (the whole hemisphere of the brain or part of a lobe of the brain).
Description of the intervention
Carbamazepine and phenobarbitone are among the most commonly used and earliest drugs licensed for the treatment of epileptic seizures; phenobarbitone has been used as monotherapy for partial seizures and generalised tonic‐clonic seizures for over 50 years (Gruber 1962), and carbamazepine, for over 30 years (Shakir 1980). Current NICE guidelines for adults and children recommend carbamazepine as a first‐line treatment for partial onset seizures and as a second‐line treatment for generalised tonic‐clonic seizures if first‐line treatments, sodium valproate and lamotrigine, are deemed unsuitable (NICE 2012). However, there is evidence that carbamazepine may exacerbate some other generalised seizure types, such as myoclonic and absence seizures (Liporace 1994; Shields 1983; Snead 1985).
Phenobarbitone is no longer considered a first‐line treatment in the USA and most of Europe because of concerns over short‐ and long‐term tolerability (Wallace 1997); particularly in children, there is concern about behavioural disturbance caused by phenobarbitone (Trimble 1988). One open‐label paediatric study in the UK, de Silva 1996, withdrew the phenobarbitone arm of the trial because of concerns about behavioural problems and difficulties getting paediatricians to randomise individuals. However, the largest reported randomised controlled trial (RCT) investigating phenobarbitone as monotherapy in adults with partial seizures, Mattson 1985, did not find phenobarbitone to be more associated with adverse events than other study drugs (carbamazepine, phenytoin, and primidone). In fact, phenobarbitone was significantly associated with the lowest incidence of motor disturbances (ataxia (lack of voluntary co‐ordination of muscle movements), incoordination, nystagmus, and tremor) and gastrointestinal problems.
Phenobarbitone is still used as a first‐line drug in low‐ and middle‐income countries (Banu 2007; Ogunrin 2005; Pal 1998). Two paediatric trials conducted in Bangladesh (Banu 2007), and rural India (Pal 1998), comparing phenobarbitone with carbamazepine and phenytoin, respectively, found no excess in behavioural side‐effects from phenobarbitone, but a trial in Nigerian adults (Ogunrin 2005), showed evidence of an association between phenobarbitone and worsening of cognitive impairments, particularly memory deficits.
Both carbamazepine and phenobarbitone have been shown to have teratogenic (disturbances to foetal development) effects, where the risk is estimated to be two to three times that of the general population (Meador 2008; Morrow 2006); carbamazepine is associated particularly with neural tube defects (Matlow 2012), and phenobarbitone is associated with low folic acid levels and megaloblastic anaemia (anaemia characterised by many large immature and dysfunctional red blood cells; Meador 2008). In addition to concerns over behavioural and cognitive adverse events, phenobarbitone is commonly associated with somnolence (sedation) and connective tissue abnormalities, such as Dupuytren's contracture and frozen shoulder (Baulac 2002).
How the intervention might work
Antiepileptic drugs suppress seizures by reducing neuronal excitability (MacDonald 1995). Phenobarbitone and carbamazepine are broad‐spectrum treatments suitable for many seizure types, and both have an anticonvulsant mechanism through blocking ion channels, binding with neurotransmitter receptors, or through inhibiting the metabolism or reuptake of neurotransmitters (Ragsdale 1991), and the modulation of gamma‐aminobutyric acid‐A (GABA‐A) receptors (Rho 1996).
Why it is important to do this review
The aim of this review was to summarise efficacy and tolerability data from existing trials comparing carbamazepine and phenobarbitone when used as monotherapy treatments. The adverse event profiles of the two drugs are well documented (see example references from Description of the intervention), and the largest reported RCT investigating carbamazepine and phenobarbitone as monotherapy in adults with partial seizures, Mattson 1985, found carbamazepine to be significantly better at controlling seizures than phenobarbitone, but other trials, including trials recruiting individuals with generalised onset seizures, have found no differences in efficacy between the two drugs (Banu 2007; Bidabadi 2009; Cereghino 1974; Chen 1996; Cossu 1984; Czapinski 1997; de Silva 1996; Feksi 1991; Heller 1995; Mitchell 1987; Ogunrin 2005; Placencia 1993). Although individual studies have found no consistent differences in efficacy, the confidence intervals generated by these studies are wide, and they have not excluded important differences in efficacy, which synthesising the data of the individual trials may show.
There are difficulties in undertaking a review of epilepsy monotherapy trials, as the important efficacy outcomes require analysis of time‐to‐event data (for example, time to first seizure after randomisation). Although methods have been developed to synthesise time‐to‐event data using summary information (Parmar 1998; Williamson 2002), the appropriate statistics are not commonly reported in published epilepsy trials (Nolan 2013a). Furthermore, although most epilepsy monotherapy trials collect seizure data, there has been no uniformity in the definition and reporting of outcomes. For example, trials may report time to 12‐month remission but not time to first seizure or vice versa, or some trials may define time to first seizure from the date of randomisation while others use the date of achieving maintenance dose. Trial investigators have also adopted differing approaches to the analysis, particularly with respect to the censoring of time‐to‐event data. For these reasons, we performed this review using individual participant data (IPD), which helps to overcome these problems. This review is one in a series of Cochrane IPD Reviews investigating pair‐wise monotherapy comparisons. These data have also been included in a network meta‐analysis (Tudur Smith 2007), undertaken following a previous version of this review.
Objectives
To review the time to withdrawal, remission, and first seizure of carbamazepine compared with phenobarbitone when used as monotherapy in people with partial onset seizures (simple or complex partial and secondarily generalised) or generalised onset tonic‐clonic seizures (with or without other generalised seizure types).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) using either an adequate method of allocation concealment (e.g. sealed opaque envelopes) or a 'quasi' method of randomisation (e.g. allocation by date of birth).
Studies may have been double‐blind, single‐blind, or unblinded.
Studies must have included a comparison of carbamazepine monotherapy with phenobarbitone monotherapy in individuals with epilepsy.
Types of participants
Children or adults with partial onset seizures (simple partial, complex partial, or secondarily generalised tonic‐clonic seizures) or generalised onset tonic‐clonic seizures (with or without other generalised seizure types).
Individuals with a new diagnosis of epilepsy or who had a relapse following antiepileptic monotherapy withdrawal.
Types of interventions
Carbamazepine or phenobarbitone as monotherapy.
Types of outcome measures
Below is a list of outcomes investigated in this review. Reporting of these outcomes in the original trial report was not an eligibility requirement for this review.
Primary outcomes
Time to withdrawal of allocated treatment (retention time). This was a combined outcome reflecting both efficacy and tolerability, as the following may have caused withdrawal of treatment: continued seizures, side‐effects, non‐compliance, or the initiation of additional add‐on treatment (i.e. allocated treatment had failed). This is an outcome to which the participant makes a contribution and is the primary outcome measure recommended by the Commission on Antiepileptic Drugs of the International League Against Epilepsy (ILAE 1998; ILAE 2006).
Secondary outcomes
Time to achieve 12‐month remission (seizure‐free period).
Time to achieve six‐month remission (seizure‐free period).
Time to first seizure post‐randomisation.
Adverse events (all reported whether related or unrelated to treatment).
Search methods for identification of studies
Electronic searches
Searches were run for the original review in 2003 and subsequent searches were run in October 2013 and September 2014. For the latest update we searched the following databases on 18 August 2016, with no language restrictions.
The Cochrane Epilepsy Group Specialised Register using the search strategy outlined in Appendix 1.
The Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies Online (CRSO) using the search strategy outlined in Appendix 2.
MEDLINE Ovid (1946 to 18 August 2016) using the search strategy outlined in Appendix 3.
The US National Institutes of Health Ongoing Trials Register using the search terms 'carbamazepine and phenobarbital and epilepsy' (ClinicalTrials.gov).
The World Health Organization International Clinical Trials Registry Platform using the search terms 'carbamazepine and phenobarbital and epilepsy' (ICTRP).
Previously we also searched SCOPUS (1823 to 18 September 2014) as an alternative to Embase, using the search strategy outlined in Appendix 4, but this is no longer necessary, because randomised and quasi‐RCTs in Embase are now included in CENTRAL.
Searching other resources
In addition, we handsearched relevant journals, reviewed the reference lists of retrieved studies to search for additional reports of relevant studies, and contacted Novartis (manufacturers of carbamazepine), and experts in the field for information of any ongoing studies, as well as original investigators of relevant trials found.
Data collection and analysis
Selection of studies
Two review authors (SJN and AGM) independently assessed trials for inclusion, resolving any disagreements by mutual discussion.
Data extraction and management
We requested the following IPD for all trials meeting our inclusion criteria.
Trial methods
method of generation of random list
method of concealment of randomisation
stratification factors
blinding methods
Participant covariates
gender
age
seizure types
time between first seizure and randomisation
number of seizures prior to randomisation (with dates)
presence of neurological signs
electroencephalographic (EEG) results
computerised tomography/magnetic resonance imaging (CT/MRI) results
Follow‐up data
treatment allocation
date of randomisation
dates of follow‐up
dates of seizures post‐randomisation or seizure frequency data between follow‐up visits
dates of treatment withdrawal and reasons for treatment withdrawal
dose
dates of dose changes
For each trial for which we did not obtain IPD, we carried out an assessment to see whether any relevant aggregate level data had been reported or could be indirectly estimated using the methods of Parmar 1998 and Williamson 2002.
Three studies involving 804 participants, provided seizure data in terms of the number of seizures recorded between each follow‐up visit rather than specific dates of seizures (Feksi 1991; Mattson 1985; Placencia 1993). To enable the calculation of time‐to‐event outcomes, we applied linear interpolation to approximate dates of seizures between follow‐up visits. For example, if the study recorded four seizures between two visits that occurred on 1 March 1990 and 1 May 1990 (interval of 61 days), then the date of first seizure would be approximately 13 March 1990. This allowed the computation of an estimate of the time to six‐month remission, 12‐month remission, and first seizure.
We calculated time to six‐month and 12‐month remission from the date of randomisation to the date (or estimated date) that the individual had first been free of seizures for six or 12 months, respectively. If the person had one or more seizures in the titration period, a six‐month or 12‐month seizure‐free period could also occur between the estimated date of the last seizure in the titration period and the estimated date of the first seizure in the maintenance period.
We calculated time to first seizure from the date of randomisation to the date that we estimated their first seizure to have occurred. If seizure data were missing for a particular visit, we censored these outcomes at the previous visit. We also censored these outcomes if the individual died or if follow‐up ceased prior to the occurrence of the event of interest. We used these methods in the remaining four trials involving 326 participants (Banu 2007; de Silva 1996; Heller 1995; Ogunrin 2005), for which we directly received outcome data (dates of seizures after randomisation).
In the Ogunrin 2005 trial, all 37 participants completed the 12‐week trial duration without withdrawing from the study. For four trials (685 participants), we extracted dates and reason for treatment withdrawal from trial case report forms for the original review (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993).
Two review authors independently extracted data from all case report forms, resolving disagreements by reconsidering the case report forms at conference. For the analysis of time‐to‐event, we defined an 'event' as either the withdrawal of the allocated treatment because of poor seizure control, adverse events, or both. We also classed non‐compliance with the treatment regimen or the addition of another antiepileptic drug as 'events'. We censored the outcome if treatment was withdrawn because the individual achieved a period of remission or if the individual was still on allocated treatment at the end of follow‐up. The Banu 2007 trial (108 participants), provided the reason for withdrawal of allocated treatment and date of last follow‐up visit. Withdrawal of allocated treatment did not always coincide with date of last follow‐up visit (i.e. several participants had the allocated treatment substituted for the other trial drug and continued to be followed up). Dates of withdrawal of allocated treatment could not be provided; therefore, we could not include participants from this trial in the outcome 'time to withdrawal of allocated treatment'.
Assessment of risk of bias in included studies
Two review authors (SJN and JW) independently assessed all included studies for risk of bias according to the Cochrane Risk of Bias tool (Higgins 2011), resolving any disagreements by discussion.
Measures of treatment effect
We measured all outcomes in this review as time‐to‐event outcomes with the hazard ratio (HR) used as the measure of treatment effect. We calculated outcomes from IPD provided, where possible, or extracted from published studies.
Unit of analysis issues
We did not have any unit of analysis issues. The unit of allocation and analysis was individual for all included studies, and no studies included in meta‐analysis were of a repeated measures (longitudinal) nature or of a cross‐over design.
Dealing with missing data
For each trial that supplied IPD, we reproduced results from trial results where possible and performed consistency checks.
We cross‐checked trial details against any published report of the trial and contacted original trial authors if we found missing data, errors, or inconsistencies.
If study authors could not resolve inconsistencies between IPD and published data, depending on the extent of the inconsistencies, we performed sensitivity analysis (see Sensitivity analysis) or excluded the data from the meta‐analysis.
We reviewed the chronological randomisation sequence and checked the balance of prognostic factors, taking account of factors stratified for in the randomisation procedure.
Assessment of heterogeneity
We assessed heterogeneity statistically using the Q test (P < 0.10 for significance) and the I² statistic (greater than 50% indicating considerable heterogeneity; Higgins 2003), output produced using the generic inverse variance approach in Data and analyses, and visually by inspecting forest plots.
Assessment of reporting biases
Two review authors (SJN and JW) undertook all full quality and 'Risk of bias' assessments. In theory, a review using IPD should overcome issues of reporting biases, as unpublished data can be provided and unpublished outcomes calculated. Any selective reporting bias detected could be assessed with the Outcome Reporting Bias In Trials (ORBIT) classification system (Kirkham 2010).
Data synthesis
We carried out our analysis on an intention‐to‐treat basis (that is, we analysed participants in the group to which they were randomised, irrespective of which treatment they actually received). Therefore, for the time‐to‐event outcomes 'time to six‐month remission', 'time to 12‐month remission', and 'time to first seizure post‐randomisation', we did not censor participants if treatment was withdrawn.
For all outcomes, we investigated the relationship between the time‐to‐event and treatment effect of the antiepileptic drugs. We used Cox proportional hazards regression models to obtain study‐specific estimates of log (HR) or treatment effect and associated standard errors in statistical SAS software, version 9.2.The model assumes that the ratio of hazards (risks) between the two treatment groups is constant over time (i.e. hazards are proportional). We tested this proportional hazards assumption of the Cox regression model for each outcome of each study by testing the statistical significance of a time‐varying covariate in the model. We evaluated overall estimates of HRs (with 95% confidence intervals (CIs)) using the generic inverse variance method in MetaView. We expressed results as a HR and a 95% CI.
By convention, a HR greater than 1 indicates that an event is more likely to occur earlier on carbamazepine than on phenobarbitone. Hence, for time to withdrawal of allocated treatment or time to first seizure, a HR greater than 1 indicates a clinical advantage for phenobarbitone (e.g. a HR of 1.2 would suggest a 20% increase in risk of withdrawal from carbamazepine compared with phenobarbitone), and for time to six‐month and 12‐month remission, a HR greater than 1 indicates a clinical advantage for carbamazepine.
Subgroup analysis and investigation of heterogeneity
Because of the strong clinical belief that some antiepileptic drugs are more effective in some seizure types than others (see Description of the intervention and How the intervention might work), we stratified all analyses by seizure type (partial onset versus generalised onset), according to the classification of main seizure type at baseline. We classified partial seizures (simple or complex) and partial secondarily generalised seizures as partial epilepsy.
We classified primarily generalised seizures as generalised epilepsy. We conducted a Chi² test of interaction between treatment and epilepsy type. If we found significant statistical heterogeneity to be present, we performed meta‐analysis with a random‐effects model in addition to a fixed‐effect model, presenting the results of both models and performing sensitivity analyses to investigate differences in study characteristics.
Sensitivity analysis
We performed several sensitivity analyses to test the robustness of our results to characteristics of the included studies.
Placencia 1993 concealed allocation via opaque sealed envelopes; however, the trial did not use this method for all trial participants. As inadequate allocation concealment could lead to biased selection of participants, we performed sensitivity analysis excluding data from Placencia 1993 for each outcome and observed any change to results and conclusions.
Following consistency checks of IPD for Placencia 1993 and Banu 2007, we found some inconsistencies between the data provided and the results in the publications in terms of withdrawal and seizure recurrences, respectively. Therefore, we performed sensitivity analyses for outcomes 'time to withdrawal of allocated treatment' and 'time to first seizure', respectively, to investigate any impact of these inconsistencies on our results. For Placencia 1993, we compared reason for withdrawal in the data provided with reasons reported in the publication and performed a sensitivity analysis of those withdrawals that we classed as 'events' or 'censored observations' (see Effects of interventions for further details). Regarding Banu 2007, we did not have sufficient information to examine the classification of participants as 'events' and 'censored observations' in the analysis of 'time to first seizure'; therefore, we performed a simple sensitivity analysis excluding data from Banu 2007 from the outcome of 'time to first seizure' and observed any change to results and conclusions.
de Silva 1996 withdrew the phenobarbitone arm of the trial after 10 children were randomised to phenobarbitone due to concerns over unacceptable side‐effects. The trial did not randomise any further children to phenobarbitone and continued with the three other treatment arms: carbamazepine, phenytoin, and sodium valproate. For the primary and secondary outcomes of this review, we included all children randomised to carbamazepine (n = 54) and phenobarbitone (n = 10) from de Silva 1996, and to account for the imbalance between children randomised to the two drugs on this trial, we performed sensitivity analysis including only those children who were randomised before the withdrawal of the phenobarbitone arm from the trial. For sensitivity analysis, we analysed 20 children (10 males and 10 females), 10 randomised to each drug, nine with generalised seizures and 11 with partial seizures. We performed this sensitivity analysis for each outcome and observed any change to results and conclusions.
Misclassification of seizure type is a recognised problem in epilepsy; whereby, some people with generalised seizures have been mistakenly classed as having partial onset seizures and vice versa. There is clinical evidence that individuals with generalised onset seizures are unlikely to have an 'age of onset' greater than 25 to 30 years (Malafosse 1994). Such misclassification impacted upon the results of a review in our series of pair‐wise reviews for monotherapy in epilepsy comparing phenytoin with sodium valproate, in which nearly 50% of participants analysed may have had their seizure type misclassified (Nolan 2013b). Given the overlap of studies contributing to this review and the phenytoin versus sodium valproate review, we suspected that misclassification of seizure type could also be likely in this review, so we examined the distribution of age at onset for individuals with generalised seizures.
Banu 2007 and de Silva 1996 were paediatric studies, and Mattson 1985 recruited participants with partial seizures only, so there were no participants with new onset generalised seizures over the age of 30 in these studies.
Twenty‐two out of 70 individuals (31%) with generalised onset seizures were over the age of 30 in Heller 1995, 19 out of 30 individuals (63%) with generalised onset seizures were over the age of 30 in Ogunrin 2005, and 24 out of 59 individuals (41%) with generalised onset seizures were over the age of 30 in Placencia 1993. Therefore, out of 245 participants from the six studies providing IPD, 65 (27%) may have been wrongly classified as having new onset generalised seizures.
To investigate misclassification for each outcome, we reclassified the 65 individuals with generalised seizure types and age at onset greater than 30 into an 'uncertain seizure type' group and re‐analysed three subgroups (partial onset, generalised onset, uncertain seizure type).
'Summary of findings' tables and quality of the evidence (GRADE)
For the 2016 update, we have added two 'Summary of findings' tables to the review (outcomes in the tables decided before the update started based on clinical relevance).
Table 1 reports the primary outcome of 'time to treatment withdrawal' in the subgroups of participants with partial onset seizures, generalised onset seizures, and overall, adjusted by epilepsy type.
Table 2 reports the secondary outcomes of 'time to 12‐month remission' and 'time to first seizure' in the subgroups of participants with partial onset seizures, generalised onset seizures, and overall, adjusted by epilepsy type.
We determined the quality of the evidence using the GRADE approach (Atkins 2004), where we downgraded evidence in the presence of high risk of bias in at least one trial, indirectness of the evidence, unexplained heterogeneity or inconsistency, imprecision of results, and high probability of publication bias. We downgraded evidence by one level if the limitation was considered serious and two levels if considered very serious, as judged by the review authors. Under the GRADE approach, evidence may also be upgraded if a large treatment effect is demonstrated with no obvious biases or if a dose‐response effect exists.
Results
Description of studies
Results of the search
We identified 267 records from the databases and search strategies outlined in Electronic searches. We found one further record by searching other resources (handsearching). We removed 98 duplicate records and screened 170 records (title and abstract) for inclusion in the review.
We excluded 148 records based on the title and abstract and assessed 22 full‐text articles for inclusion in the review. We excluded nine studies (see Excluded studies below) and included 13 studies in the review (see Included studies).
Following an updated search in August 2016, we identified 123 records from Electronic searches. We removed 35 duplicate records and screened 88 records (title and abstract) for inclusion in the review. All 88 records were clearly irrelevant and excluded.
See Figure 1 for a PRISMA study flow diagram (Moher 2009).
Figure 1.
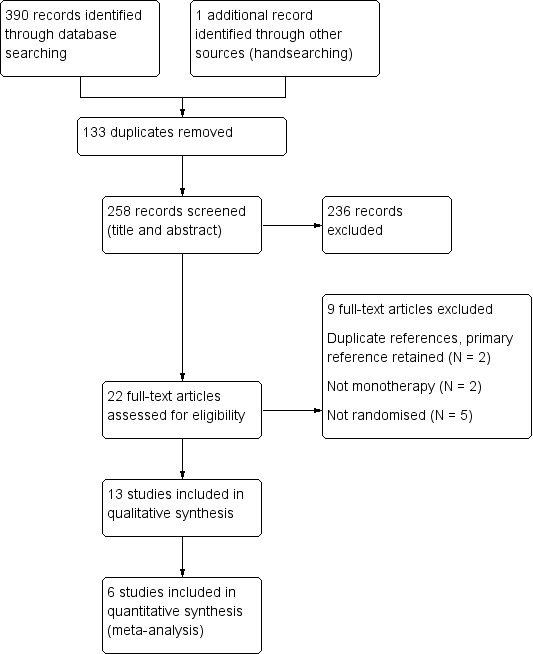
Study flow diagram.
Included studies
We included 13 trials in this review (Banu 2007; Bidabadi 2009; Cereghino 1974; Chen 1996; Cossu 1984; Czapinski 1997; de Silva 1996; Feksi 1991; Heller 1995; Mattson 1985; Mitchell 1987; Ogunrin 2005; Placencia 1993). Two included studies were available in abstract form only (Bidabadi 2009; Czapinski 1997), and one included study was published in Italian, which we translated into English (Cossu 1984).
Two trials recruited individuals of all ages (Feksi 1991; Placencia 1993); five trials recruited children only (de Silva 1996 defined children as under the age of 16, Banu 2007 and Chen 1996 defined children as under the age of 15, and Bidabadi 2009 and Mitchell 1987 defined children as under the age of 12), and the remaining six trials recruited adults only. Of the adults‐only trials, three defined adults to be individuals above the age of 18 (Cereghino 1974; Czapinski 1997; Mattson 1985), one trial classed adults as older than 13 years (Heller 1995), one trial classed adults as older than 14 years (Ogunrin 2005), and one trial classed adults as older than 15 years (Cossu 1984). Seven trials recruited individuals with partial onset seizures and generalised onset seizures (Banu 2007; Chen 1996; de Silva 1996; Feksi 1991; Heller 1995; Ogunrin 2005; Placencia 1993), three trials recruited individuals with partial onset seizures only (Cereghino 1974; Mattson 1985; Mitchell 1987), one trial recruited individuals with partial seizures and secondarily generalised seizures (Bidabadi 2009), one trial recruited individuals with complex partial seizures only (Czapinski 1997), and one trial recruited individuals with temporal lobe epilepsy only (Cossu 1984).
Ten trials recruited individuals with new onset seizures, or previously untreated seizures, or both (Banu 2007; Chen 1996; Cossu 1984; Czapinski 1997; de Silva 1996; Feksi 1991; Heller 1995; Mitchell 1987; Ogunrin 2005; Placencia 1993); one trial recruited institutionalised participants with uncontrolled seizures (Cereghino 1974); one trial recruited "previously untreated or under‐treated" individuals (Mattson 1985); and one trial (reported only in abstract form) provided no information regarding new onset of seizures in participants (Bidabadi 2009).
Five trials were conducted in Europe (Bidabadi 2009; Cossu 1984; Czapinski 1997; de Silva 1996; Heller 1995); three trials were conducted in the USA (Cereghino 1974; Mattson 1985; Mitchell 1987); one trial was conducted in Taiwan (Chen 1996); and four trials were conducted in rural areas or developing countries, or both: one trial in Nigeria (Ogunrin 2005), one trial in Bangladesh (Banu 2007), one trial in Kenya (Feksi 1991), and one trial in Ecuador (Placencia 1993).
We did not obtain individual participant data (IPD) for six trials, with a total of 317 participants, as suitable seizure data for the outcomes examined in this review were not recorded (Chen 1996; Mitchell 1987), the trial authors no longer had a copy of the data (Cereghino 1974), or trial authors did not respond to our data requests (Bidabadi 2009; Cossu 1984; Czapinski 1997). A further trial, which randomised 302 participants (Feksi 1991), provided access to an IPD dataset, but this was not the final dataset used for the analysis published by the original authors. The pharmaceutical company that sponsored the trial, Ciba‐Geigy, who at that time held the product license for carbamazepine, held the final dataset. Since the trial was undertaken, there have been a number of mergers and restructures within the industry, and the current owners of the data are Novartis. Unfortunately, Novartis were unable to locate the data for this trial. The dataset that we had for this trial contained a number of problems and inconsistencies, and we therefore decided not to include this trial in the meta‐analysis. None of these seven trials reported the specific time‐to‐event outcomes chosen for this review, and we could not extract sufficient aggregate data from the trial publications in any other trial. Therefore, we could not include them in data synthesis. Table 4 contains full details of outcomes considered and summaries of results in each eligible trial for which IPD were not available.
Table 1.
Outcomes considered and summary of results for trials with no IPD
| Trial | Outcomes reported | Summary of results |
| Bidabadi 2009 |
|
|
| Cereghino 1974 |
|
|
| Chen 1996 |
|
|
| Cossu 1984 | Changes in memory function from baseline after 3 weeks of treatment (verbal, visual, (visual‐verbal and visual‐non‐verbal), acoustic, tactile, and spatial) |
|
| Czapinski 1997 |
|
|
| Feksi 1991 |
|
PB (n = 123), CBZ (n = 126)
|
| Mitchell 1987 |
|
|
CBZ: carbamazepine IQ: intelligence quotient PB: phenobarbitone WISC‐R scale: the Wechsler Intelligence Scale for Children
IPD were available for the remaining six trials, which recruited a total of 836 participants, representing 57% of 1455 individuals from all 13 identified eligible trials. Four trials provided computerised data directly (Banu 2007; Mattson 1985; Ogunrin 2005; Placencia 1993), and the authors of two trials (de Silva 1996; Heller 1995), supplied a combination of both computerised and hard copy data (although mostly computerised).
Data were available for the following participant characteristics (percentage of 836 participants with data available): sex (99%, data missing for 6 participants in de Silva 1996 and 4 participants in Mattson 1985); seizure type (100%); drug randomised (99%, data missing for 6 participants in de Silva 1996); age at randomisation (99%, data missing for 1 participant in Heller 1995, 6 participants in de Silva 1996, and 5 participants in Mattson 1985); number of seizures in six months prior to randomisation (98%, data missing for 5 participants from Banu 2007, 1 participant in Heller 1995, 6 participants in de Silva 1996, and 7 participants in Mattson 1985); and time since first seizure to randomisation (94%, data missing for 2 participants in Heller 1995, 6 participants in de Silva 1996, 5 participants in Mattson 1985, and all 37 participants in Ogunrin 2005).
Three trials provided the results of neurological examinations for 220 participants (27%) (de Silva 1996; Heller 1995; Ogunrin 2005). Three trials provided electroencephalographic (EEG) results for 600 participants (72%) (103 participants from Banu 2007, 305 participants from Mattson 1985, and all participants from Placencia 1993). Two trials provided computerised tomography/magnetic resonance imaging (CT/MRI) results for 304 participants (36%) (26 from Banu 2007 and 278 from Mattson 1985).
See the 'Characteristics of included studies' tables for a detailed description of each study included in this review.
Excluded studies
We excluded two duplicate trials (Cereghino 1973; Smith 1987), and we retained the most relevant primary reference for each trial in the review (Cereghino 1974 and Mattson 1985, respectively). We excluded five studies that were not randomised controlled trials (RCTs) (Bird 1966; Castro‐Gago 1998; Hansen 1980; Kuzuya 1993; Sabers 1995), and we excluded two trials that did not use carbamazepine and phenobarbitone monotherapy (Marjerrison 1968; Meador 1990). See the 'Characteristics of excluded studies' tables for further details.
Risk of bias in included studies
For further details, see the 'Characteristics of included studies' tables, Figure 2, and Figure 3.
Figure 2.
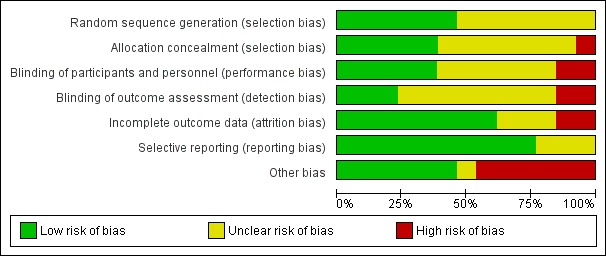
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies
Figure 3.
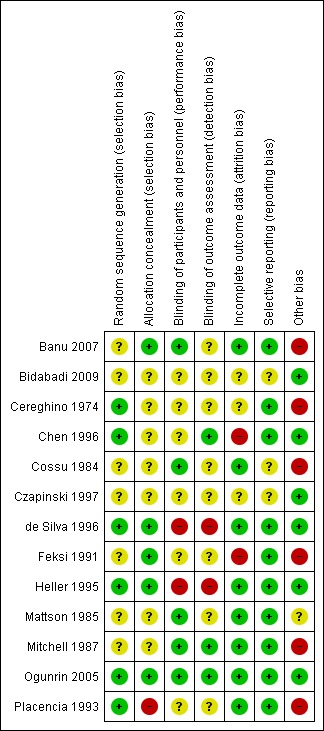
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study
Allocation
(1) Trials for which we received individual participant data (IPD)
Three trials reported adequate methods of randomisation and allocation concealment and we judged all three to be at low risk of bias: two trials used permuted blocks to generate a random list and concealed allocation by using sealed opaque envelopes (de Silva 1996; Heller 1995); and one trial used number tables to generate a random list and concealed allocation by allocating the randomised drug on a different site to where participants were randomised (Ogunrin 2005). One trial reported only that participants were randomised with stratification for seizure type (Mattson 1985); no further information was provided in the study publication or from the authors regarding the methods of generation of the random list and concealment of allocation and we judged this study at unclear risk of bias. For two trials, neither the study publication nor the authors provided the method of generation of the random list; one trial reported that allocation was concealed using sealed envelopes prepared on a different site to recruitment of participants (Banu 2007), and the other trial reported that allocation was concealed by sealed opaque envelopes, but this method was not used for all participants in the trial; we judged this trial to be at high risk of bias for allocation concealment (Placencia 1993). This inadequate allocation concealment may have resulted in selection bias in this trial, so we performed sensitivity analyses for all outcomes excluding participants from this trial (see Sensitivity analysis and Effects of interventions).
(2) Trials for which no IPD were available
Two trials reported adequate methods of randomisation: random number tables (Cereghino 1974); and simple randomisation of block size three (Chen 1996), but they provided no details on concealment of allocation.
Three trials reported that the participants were 'randomised' or 'randomly allocated', etc. but did not provide information about the method of generation of the random list or allocation concealment (Bidabadi 2009; Cossu 1984; Czapinski 1997).
One trial reported that it concealed allocation by the use of sealed opaque envelopes but did not report the method of generation of the random list (Feksi 1991), and one trial reported that it "randomised [children] using a scheme that balanced drug distribution by age and sex" but did not provide further details about the method of generation of the random list (Mitchell 1987). This trial also did not report any details on allocation concealment, and the trial used some non‐randomised children in some analyses (see Other potential sources of bias).
Blinding
(1) Trials for which we received IPD
One trial double‐blinded participants and personnel using an additional blank tablet (Mattson 1985); however, it was unclear if this trial blinded the outcome assessor. One trial blinded participants and the outcome assessors who performed cognitive testing but did not blind a research assistant recruiting participants and providing counselling on medication adherence (Ogunrin 2005). Similarly, another trial blinded participants and a psychologist and therapist throughout the trial, while not blinding the treating physician for practical and ethical reasons (Banu 2007). We judged that the open‐label elements of these two studies were unlikely to have influenced the results of these trials. However, the latter trial blinded a researcher throughout the trial duration, but unblinded the researcher for analysis, which may have impacted upon results. One trial, Placencia 1993, did not report any information on blinding in the study publication, and no information was available from the study authors. Two trials were unblinded for "practical and ethical reasons" (de Silva 1996; Heller 1995); however, it is likely that the unblinded design of de Silva 1996 contributed to the early withdrawal of the phenobarbitone arm, which is likely to have had an effect on the overall results of the trial. Further, as the two trials were conducted under the same protocol, the open design may have also contributed to the withdrawal rates in Heller 1995 and influenced the overall results; we judged both trials at high risk of performance and detection bias.
(2) Trials for which no IPD were available
One trial was described as double‐blind (Cossu 1984), but it was unclear exactly who was blinded (participants, personnel, outcome assessors). One paediatric trial blinded participants (and parents) and psychometric testers but unblinded clinicians for follow‐up (Mitchell 1987). One trial described that cognitive testers were single‐blinded, Chen 1996, but gave no further details on blinding of participants and personnel.
The remaining four trials did not provide any information on masking of participants, personnel, or outcome assessors; we judged them to be at unclear risk of performance and detection bias (Bidabadi 2009; Cereghino 1974; Czapinski 1997; Feksi 1991).
Incomplete outcome data
(1) Trials for which we received IPD
In theory, a review using IPD should overcome issues of attrition bias as unpublished data can be provided, unpublished outcomes calculated, and all randomised participants can be analysed by an intention‐to‐treat approach. All six trials provided IPD for all randomised individuals and reported the extent of follow‐up for each individual; we judged all six trials to be at low risk of attrition bias (Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993). We queried any missing data with the original study authors. From the information provided by the study authors, we deemed the small amount of missing data present (included studies) to be missing at random and not affecting our analysis.
(2) Trials for which no IPD were available
Two trials reported attrition rates and analysed all randomised participants using an intention‐to‐treat approach (Cossu 1984; Mitchell 1987). Two trials reported attrition rates, but it was unclear if they analysed all participants (Cereghino 1974; Czapinski 1997), and one trial did not report attrition rates, and it was unclear if it analysed all participants (Bidabadi 2009). Two studies included only those who completed the study in the final analysis (Chen 1996; Feksi 1991), excluding 6% and 17.5% of participants, respectively, from the final results. This approach is not intention‐to‐treat, so we deemed these two studies to be at a high risk of attrition bias.
Selective reporting
We requested study protocols in all IPD requests; however, protocols were not available for any of the 13 included trials, so we made a judgement of the risk of bias based on the information included in the publications or from the IPD we received (see the 'Characteristics of included studies' tables for more information).
(1) Trials for which we received IPD
In theory, a review using IPD should overcome issues of reporting biases as unpublished data can be provided and unpublished outcomes calculated. We received sufficient IPD to calculate the four outcomes ('time to withdrawal of allocated treatment', 'time to six‐month remission, 'time to 12‐month remission', and 'time to first seizure') for four of the six trials (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993). The study duration of Ogunrin 2005 was 12 weeks, and all randomised participants completed the study without withdrawing; therefore, we could only calculate 'time to first seizure' for this trial. Banu 2007 did not record the dates of all seizures after randomisation and dates of withdrawal for allocated treatment for all participants; therefore, we could only calculate 'time to first seizure' for this trial.
(2) Trials for which no IPD were available
Four trials reported either cognitive outcomes, seizure outcomes, adverse events, or a combination of these (Chen 1996; Cereghino 1974; Feksi 1991; Mitchell 1987). One trial reported cognitive outcomes only, but no adverse events or seizure outcomes (Cossu 1984); however, as no protocols were available for the aforementioned three trials, we do not know whether either seizure outcomes, recording of adverse events, or both, were planned a priori. Two trials were in abstract form only and did not provide sufficient information to assess selective reporting bias (Bidabadi 2009; Czapinski 1997).
Other potential sources of bias
We detected another source of bias in six of the 13 included trials.
Following consistency checks of IPD for Placencia 1993 and Banu 2007, we found some inconsistencies between the data provided and the results in the publications in terms of withdrawal and seizure recurrences, respectively, which the authors could not resolve and we judged these trials to be at high risk of other bias. We performed sensitivity analysis to investigate the impact of the inconsistent data on our outcomes (see Sensitivity analysis and Effects of interventions). Furthermore, we received IPD for a seventh trial (Feksi 1991), but too many inconsistencies were present for this data to be usable (see Included studies for further details).
One trial had a cross‐over design (Cereghino 1974); such a design is unlikely to be appropriate for monotherapy treatment because of carryover effects from one treatment period into another (participants were also treated during washout periods with their 'regular medication'), and such a design does not allow long‐term outcomes, such as the time‐to‐event outcomes of interest in this review. For future updates of this review, we will exclude studies of a cross‐over design.
We included one trial with very small participant numbers (six participants randomised to each drug) and very short‐term follow‐up (three weeks), and it was unclear if this trial was adequately powered and of sufficient duration to detect differences (Cossu 1984). For future updates of this review, we will review our inclusion criteria in terms of participant numbers and trial duration.
Another trial had several potential sources of other bias (Mitchell 1987); there was evidence that the trial may have been underpowered to detect differences between the treatments, one of the tools for outcome assessment was not fully validated, and non‐randomised children from a related pilot study were included in analysis for some of the outcomes.
Effects of interventions
Table 4 provides a summary of the outcomes reported in trials for which no IPD were available. Table 5 gives details regarding the number of individuals (with IPD) contributing to each analysis.Table 1 summarises results for primary outcome 'time to withdrawal of allocated treatment' and Table 2, for secondary outcomes 'time to six‐ and 12‐month remission', and 'time to first seizure'. Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, and Figure 11 show survival curve plots (cumulative incidence). We produced all cumulative incidence plots in Stata software version 11.2 using data from all trials providing IPD combined (Stata 2009). We would have liked to stratify by trial in survival curve plots, but we do not know of any software that allows for this; we hope that such software may have been developed for future updates of this review.
Table 2.
Number of participants contributing to each analysis
| Trial | Number randomised |
Time to withdrawal of allocated treatment |
Time to 12‐month remission |
Time to six‐month remission |
Time to first seizure | ||||||||||
| CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | |
| Banu 2007¹ | 54 | 54 | 108 | Information not available | Information not available | Information not available | 54 | 54 | 108 | ||||||
| de Silva 1996² | 54 | 10 | 64 | 53 | 10 | 63 | 54 | 10 | 64 | 54 | 10 | 64 | 54 | 10 | 64 |
| Heller 1995³ | 61 | 58 | 119 | 60 | 55 | 115 | 61 | 58 | 119 | 61 | 58 | 119 | 61 | 58 | 119 |
| Mattson 1985⁴ | 155 | 155 | 310 | 154 | 155 | 309 | 154 | 155 | 309 | 154 | 155 | 309 | 151 | 151 | 302 |
| Ogunrin 2005⁵ | 19 | 18 | 37 | Information not available | Information not available | Information not available | 19 | 18 | 37 | ||||||
| Placencia 1993⁶ | 95 | 97 | 192 | 94 | 95 | 189 | 95 | 96 | 191 | 95 | 96 | 191 | 95 | 97 | 192 |
| Total | 438 | 392 | 830 | 361 | 315 | 676 | 364 | 319 | 683 | 364 | 319 | 683 | 434 | 388 | 822 |
CBZ: carbamazepine PB: phenobarbitone ¹The date of withdrawal of allocated treatment was not recorded in all cases for Banu 2007, so we could not calculate 'time to withdrawal of allocated treatment'. The date of first seizure after randomisation was recorded, but all dates of subsequent seizures were not recorded; therefore, we could calculate 'time to first seizure', but we could not calculate 'time to six‐month remission' and 'time to 12‐month remission'. ²We received IPD for 70 participants recruited in de Silva 1996; the randomised drug was not recorded in six participants. Reasons for treatment withdrawal were not available for one participant randomised to CBZ; we did not include this participant in the analysis of time to treatment withdrawal. ³Reasons for treatment withdrawal were not available for four participants (one randomised to CBZ and three to PB) in Heller 1995; we did not include these participants in the analysis of time to treatment withdrawal. ⁴No follow‐up data after randomisation were available for one participant randomised to CBZ in Mattson 1985. Dates of seizure recurrence were not available for seven participants (three randomised to CBZ and four to PB); we did not include these participants in the analysis of time to first seizure. ⁵The study duration of Ogunrin 2005 was 12 weeks; therefore, six‐ and 12‐month remission of seizures could not be achieved, so we could not calculate these outcomes. All randomised participants completed the study without withdrawing from treatment, so we could not analyse the time to treatment withdrawal. ⁶Reasons for treatment withdrawal were not available for three participants (one randomised to CBZ and two randomised to PB) in Placencia 1993. We did not include these participants in the analysis of time to treatment withdrawal. Seizure data after occurrence of first seizure were not available for one participant randomised to PB, so we did not include this participant in the analyses of time to six‐month and time to 12‐month remission.
Figure 4.
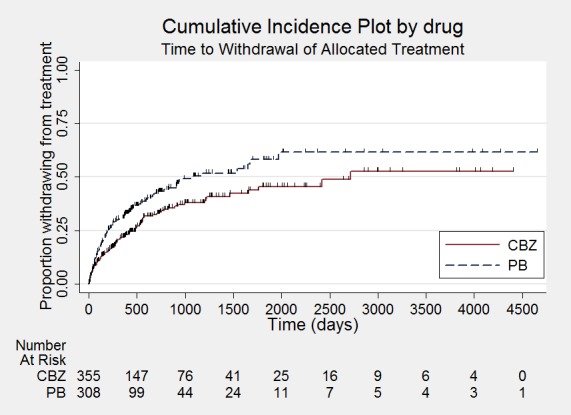
Time to withdrawal of allocated treatment
Figure 5.
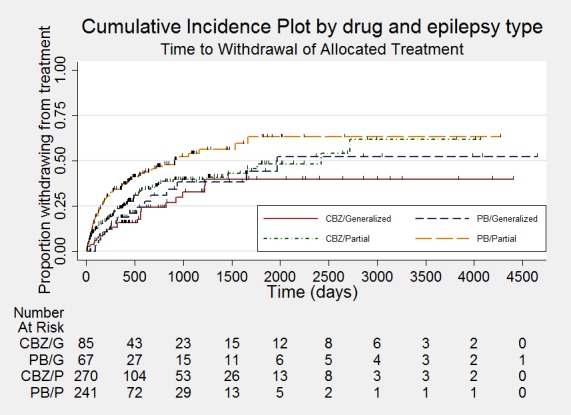
Time to withdrawal of allocated treatment ‐ stratified by epilepsy type
Figure 6.
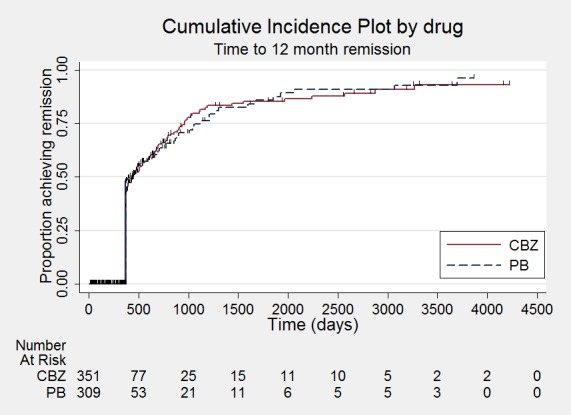
Time to 12‐month remission
Figure 7.
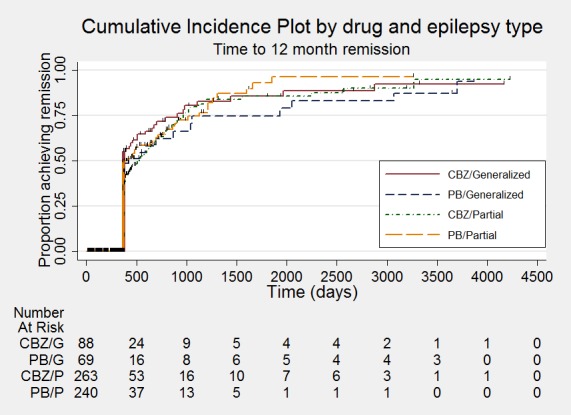
Time to 12‐month remission ‐ stratified by epilepsy type
Figure 8.
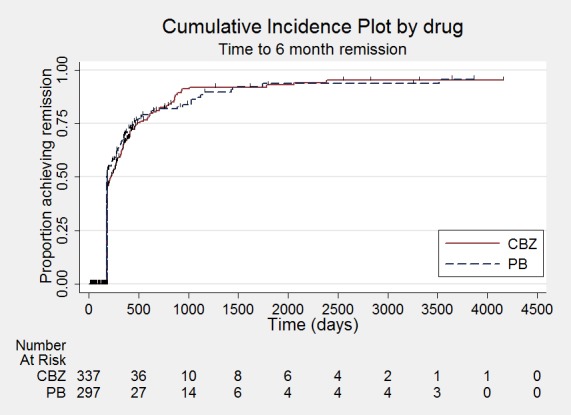
Time to six‐month remission
Figure 9.
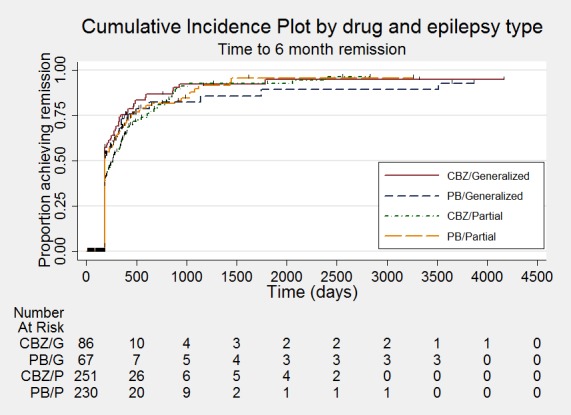
Time to six‐month remission ‐ stratified by epilepsy type
Figure 10.
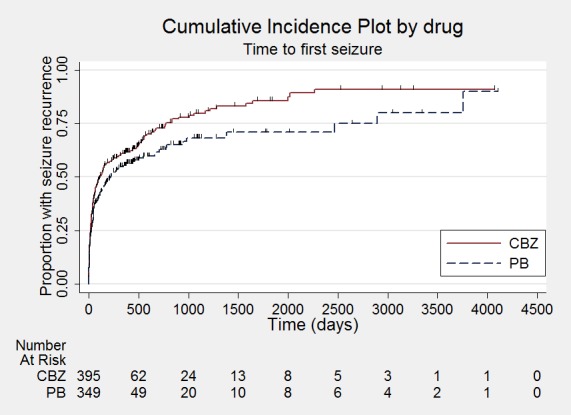
Time to first seizure
Figure 11.
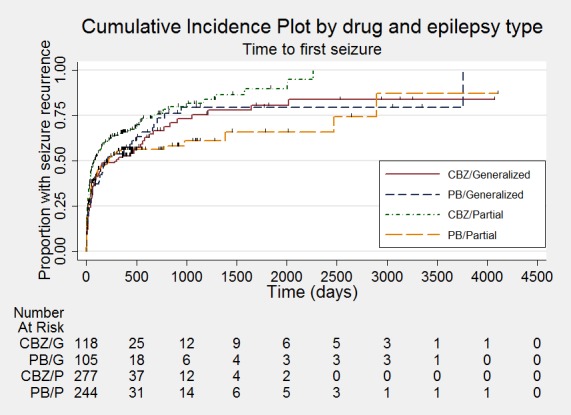
Time to first seizure ‐ stratified by epilepsy type
All hazard ratios (HRs) presented below were calculated by generic inverse variance fixed‐effect meta‐analysis, unless otherwise stated.
(1) Time to withdrawal of allocated treatment
For this outcome, a HR greater than one indicates a clinical advantage for carbamazepine.
Times to withdrawal of allocated treatment and reasons for withdrawal were available for 676 participants from four of the six trials providing IPD (97.8% of 691 participants from de Silva 1996, Heller 1995, Mattson 1985, and Placencia 1993 (see Included studies and Table 5) and 46.4% of the total 1455 participants from the 13 included studies). Mattson 1985 did not record follow‐up data for one participant randomised to carbamazepine. de Silva 1996 did not record the randomised drug for six participants, and the reason for withdrawal was not available for one participant randomised to carbamazepine and could not be determined from the case notes. Similarly, in Heller 1995, for one participant randomised to carbamazepine and three participants randomised to phenobarbitone and in Placencia 1993, for one participant randomised to carbamazepine and two participants randomised to phenobarbitone, the reason for withdrawal was not available and could not be determined from the case notes. We did not include these 15 participants with missing outcome data in the analysis of 'time to withdrawal of allocated treatment'. All participants completed the 12‐week study in Ogunrin 2005 and so could not contribute to the analysis of 'time to withdrawal of allocated treatment'. From the IPD provided by Banu 2007, we were able to establish reasons for treatment withdrawal for all participants, but the date of withdrawal of allocated treatment was not available for all participants (see Data extraction and management for further details); therefore, we could not calculate the 'time to withdrawal of allocated treatment' for this study.
Among the 784 participants for which we had reasons for treatment withdrawal (Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993), 393 participants prematurely withdrew from treatment (50%): 216 out of 415 participants randomised to carbamazepine (52%) and 178 out of 369 participants randomised to phenobarbitone (48%). (See Table 6 for reasons for premature termination of the study by treatment and how we classified these withdrawals in analysis). We deemed 235 participants (30%) to have withdrawn for reasons related to the study drug, 125 (30%) on carbamazepine and 110 (30%) on phenobarbitone, and we classed these withdrawals as 'events' in analysis. We classed the other 158 withdrawals to be not related to the study drug and censored these participants in analysis, in addition to those who completed the study without withdrawing.
Table 3.
Reasons for premature discontinuation (withdrawal of allocated treatment)
| Reason for early termination | Classification | de Silva 1996¹ | Heller 1995¹ | Mattson 1985 | Placencia 1993² | Banu 2007³ | Total⁴ | ||||||
| CBZ n = 53 | PB = 10 | CBZ n = 60 | PB = 55 | CBZ n = 154 | PB = 155 | CBZ = 94 | PB = 95 | CBZ = 54 | PB = 54 | CBZ = 415 | PB = 369 | ||
| Adverse events | Event | 3 | 2 | 8 | 12 | 11 | 5 | 5 | 5 | 0 | 0 | 27 | 24 |
| Seizure recurrence | Event | 12 | 2 | 5 | 7 | 3 | 7 | 0 | 0 | 1 | 2 | 21 | 18 |
| Both seizure recurrence and adverse events | Event | 6 | 4 | 4 | 3 | 30 | 26 | 0 | 0 | 0 | 0 | 40 | 33 |
| Non‐compliance/participant choice | Event | 0 | 0 | 0 | 0 | 11 | 19 | 13 | 9 | 6 | 0 | 30 | 28 |
| Another AED added/AED changed | Event | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 7 | 4 | 7 | 7 |
| Participant went into remission | Censored | 18 | 1 | 6 | 3 | 0 | 0 | 0 | 0 | 0 | 2 | 24 | 6 |
| Lost to follow‐up | Censored | 0 | 0 | 0 | 0 | 26 | 26 | 11 | 5 | 7 | 15 | 44 | 46 |
| Death⁵ | Censored | 0 | 0 | 0 | 0 | 4 | 2 | 2 | 1 | 0 | 0 | 6 | 3 |
| Other⁶ | Censored | 0 | 0 | 0 | 0 | 16 | 13 | 0 | 0 | 0 | 0 | 16 | 13 |
| Completed the study (did not withdraw) | Censored | 14 | 1 | 37 | 30 | 53 | 54 | 63 | 75 | 33 | 31 | 200 | 191 |
AED: antiepileptic drug CBZ: carbamazepine n: number of individuals contributing to the outcome 'time to treatment withdrawal' PB: phenobarbitone ¹Four participants for Heller 1995 (one on CBZ and three on PB) and one for de Silva 1996 (CBZ) had missing reasons for treatment withdrawal. ²There were inconsistencies between IPD and the publication of Placencia 1993; we performed sensitivity analysis (see Effects of interventions). There were missing reasons for treatment withdrawal for three participants (one on CBZ and two on PB); we did not include these participants in the analysis. ³Banu 2007 provided reasons for treatment withdrawal, but dates of treatment withdrawal could not be provided for all participants, so we could not calculate 'time to withdrawal of allocated treatment'. ⁴All participants in Ogunrin 2005 completed the study without withdrawing; therefore, this study did not contribute to 'time to withdrawal of allocated treatment'. ⁵Death was due to reasons not related to the study drug. ⁶Other reasons from Mattson 1985: participants developed other medical disorders including neurological and psychiatric disorders.
The overall pooled HR (for 676 participants) was 1.49 (95% confidence interval (CI) 1.15 to 1.94, P = 0.003, from fixed‐effect analysis), indicating a statistically significant advantage for carbamazepine; in other words, participants withdrew significantly earlier from phenobarbitone than carbamazepine in the four included trials. There was moderate statistical heterogeneity between trials (Chi² test = 7.07, df = 3, P = 0.07, I² statistic = 58%, see Analysis 1.1). When we repeated the analysis using random‐effects, the pooled HR was 1.50 (95% CI 0.95 to 2.38, P = 0.07), still indicating an advantage for carbamazepine, but this advantage was no longer statistically significant.
Analysis 1.1.
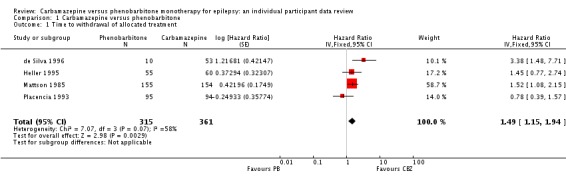
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 1 Time to withdrawal of allocated treatment.
We performed sensitivity analysis excluding participants from Placencia 1993 from analysis because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 7). This sensitivity analysis resulted in a larger advantage for carbamazepine with a pooled HR of 1.66 (95% CI 1.25 to 2.20, P = 0.0005, calculated with fixed‐effect) and reduced heterogeneity (Chi² test = 3.24, df = 2, P = 0.20, I² statistic = 35%) but no change to conclusions. Further, in Placencia 1993, we also found inconsistencies (between IPD dataset and published results) in the number of participants who withdrew from allocated treatment for certain reasons, which the trial authors could not resolve. These inconsistencies were as follows.
Table 4.
Sensitivity analyses
| Analysis |
Time to withdrawal of allocated treatment |
Time to 12‐month remission |
Time to six‐month remission |
Time to first seizure¹ | |
| Original analysis | Participants | 676 (Analysis 1.2) | 683 (Analysis 1.4) | 683 (Analysis 1.6) | 822 (Analysis 1.8) |
|
Pooled HR (95% CI) P value |
1.50 (1.15 to 1.95) P = 0.003 |
0.93 (0.72 to 1.20) P = 0.57 |
0.99 (0.80 to 1.23) P = 0.95 |
0.87 (0.72 to 1.06) P = 0.18 |
|
| Heterogeneity | I² statistic = 35% | I² statistic = 55% | I² statistic = 58% | I² statistic = 44% | |
| Sensitivity analysis for Placencia 1993² |
Participants | 487 | 492 | 492 | 630 |
|
Pooled HR (95% CI) P value |
1.66 (1.25 to 2.20) P = 0.0005 |
0.82 (0.61 to 1.09) P = 0.15 |
0.88 (0.68 to 1.14) P = 0.34 |
0.87 (0.71 to 1.08) P = 0.22 |
|
| Heterogeneity | I² statistic = 35% | I² statistic = 0% | I² statistic = 0% | I² statistic = 34% | |
| Sensitivity analysis for de Silva 1996³ |
Participants | 633 | 640 | 640 | 779 |
|
Pooled HR (95% CI) P value |
1.42 (1.08 to 1.86) P = 0.01 |
0.90 (0.69 to 1.17) P = 0.42 |
0.97 (0.78 to 1.21) P = 0.79 |
0.87 (0.71 to 1.06) P = 0.17 |
|
| Heterogeneity | I² statistic = 0% | I² statistic = 57% | I² statistic = 60% | I² statistic = 39% | |
CI: confidence interval HR: hazard ratio ¹We performed sensitivity analyses for potential misclassification of seizure type (see Analysis 1.9) and because of inconsistencies between published data and IPD for Banu 2007 (see Sensitivity analysis and Effects of interventions for full details). ²We performed sensitivity analysis excluding all randomised participants in Placencia 1993 because of inadequate allocation concealment in the study. We performed further sensitivity analysis for the outcome 'time to withdrawal of allocation concealment' because of inconsistencies between published data and IPD for Placencia 1993 (see Sensitivity analysis and Effects of interventions for full details). ³We performed sensitivity analysis including only the participants in de Silva 1996, which were randomised before the phenobarbitone arm was withdrawn (see Sensitivity analysis and Effects of interventions for full details).
Analysis 1.2.
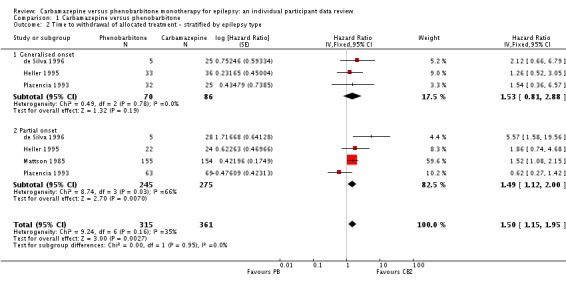
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 2 Time to withdrawal of allocated treatment ‐ stratified by epilepsy type.
Analysis 1.4.
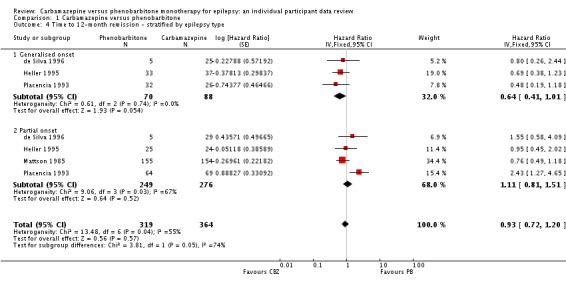
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 4 Time to 12‐month remission ‐ stratified by epilepsy type.
Analysis 1.6.
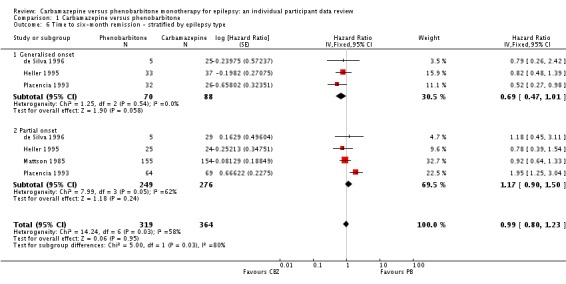
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 6 Time to six‐month remission ‐ stratified by epilepsy type.
Analysis 1.8.
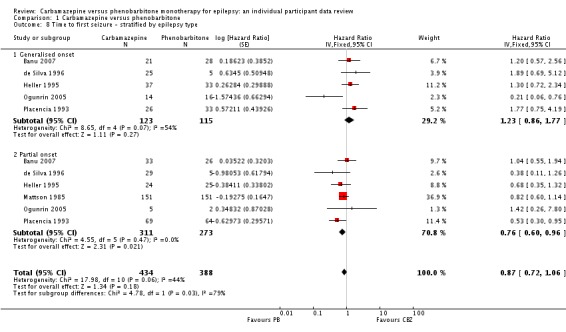
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 8 Time to first seizure ‐ stratified by epilepsy type.
Results from the IPD dataset: 51 participants withdrew, 31 from carbamazepine and 20 from phenobarbitone: 16 participants left the area (lost to follow‐up), 10 withdrew due to adverse effects, 22 withdrew for personal reasons or no stated reason (classed as an event), and three died (see Table 6).
Results in the trial report: 53 participants withdrew, 31 from carbamazepine and 22 from phenobarbitone: 18 participants left the area (lost to follow‐up), five withdrew because of adverse effects, three died, and 27 withdrew for personal reasons or no stated reason.
As the overall number of events and censored observations was similar (results from the IPD dataset: 51 withdrew, 32 events, 19 censored; and results in the trial report: 53 withdrew, 32 events, 21 censored) and as our sensitivity analysis excluding results of Placencia 1993 gave similar results and an unchanged conclusion, we feel that these inconsistencies are minor and are unlikely to have had a large impact on the overall results. In the primary analysis of Placencia 1993, we classed those who withdrew for 'no clearly articulated reason' as events in the analysis; in other words, the withdrawal was due to the study drug. However, it is also possible that these participants may have withdrawn for reasons not related to the study drug, and we therefore should have censored them in the analysis. We performed a further sensitivity analysis censoring the 19 participants who withdrew for 'no clearly articulated reason'. Again, the results of the sensitivity analysis were similar to the primary analysis, showing a slightly larger statistically significant advantage for carbamazepine (pooled HR 1.65, 95% CI 1.26 to 2.17, P = 0.0003), and again, heterogeneity was substantially reduced after censoring these participants (Chi² test = 3.25, df = 3, P = 0.35, I² statistic = 8%).
In Placencia 1993 (primary analysis with events and censored observations as summarised in Table 6), there was some evidence that the proportional hazards assumption of the Cox model may have been violated; the P value of the time‐varying covariate was 0.084. In sensitivity analysis under our alternative assumption regarding censoring (we censored participants who withdrew for 'no clearly articulated reason' rather than analyse them as events), there was no evidence that the proportional hazards assumption of the Cox model was violated; the P value of the time‐varying covariate was 0.824. We therefore assume that the non‐proportionality of Placencia 1993 in our primary analysis was likely to be due to our assumptions regarding censoring of participants. The proportional hazards assumption of the Cox model was satisfied for all other trials included in analysis.
For participants with generalised onset seizures (136), the pooled HR was 1.53 (95% CI 0.81 to 2.88, P = 0.19; Table 1), suggesting an advantage for carbamazepine that was not statistically significant. There was no evidence of statistical heterogeneity between trials (Chi² test = 0.49, df = 2, P = 0.78, I² statistic = 0%, see Analysis 1.2).
For participants with partial onset seizures (520), the pooled HR was 1.49 (95% CI 1.12 to 2.00, P = 0.007; Table 1), indicating a statistically significant advantage for carbamazepine, but a large amount of statistical heterogeneity was present between trials (Chi² test = 8.74, df = 3, P = 0.03, I² statistic = 66%). When we repeated the analysis using random‐effects, the pooled HR for participants with partial onset seizures was 1.58 (95% CI 0.82 to 3.06, P = 0.17), still indicating an advantage for carbamazepine, but this advantage was no longer statistically significant.
Overall, the pooled HR (adjusted for seizure type) was 1.50 (95% CI 1.15 to 1.95, P = 0.003, from fixed‐effect analysis; Analysis 1.2; Table 1), providing evidence of a statistically significant advantage for carbamazepine. When we repeated the analysis using random‐effects (Chi² test = 9.24, df = 6, P = 0.16, I² statistic = 35%), the pooled HR was 1.53 (95% CI 1.02 to 2.28, P = 0.04). In this case, the advantage of carbamazepine was still statistically significant. We found no interaction between treatment and seizure type (generalised versus partial onset) (Chi² test = 0.00, df = 1, P = 0.95, I² statistic = 0%).
The sensitivity analysis including only the 20 participants randomised in de Silva 1996 before the withdrawal of the phenobarbitone arm gave similar results with a pooled HR (adjusted for seizure type for 633 participants) of 1.42 (95% CI 1.08 to 1.86, P = 0.01) and heterogeneity between trials was reduced to 0 in this analysis (Chi² test = 5.66, df = 3, P = 0.14, I² statistic = 0%). Results within each seizure group were also similar in this sensitivity analysis, with a pooled HR (for 115 participants with generalised seizures) of 1.37 (95% CI 0.69 to 2.73, P = 0.37, I² statistic = 0%) and a pooled HR of 1.43 (95% CI 1.06 to 1.92, P = 0.02, I² statistic = 46%) for 498 participants with partial seizures (see Table 7 for further details).
Following reclassification of the 65 participants aged 30 or older with new onset generalised seizures in Heller 1995, Ogunrin 2005, and Placencia 1993 (see Sensitivity analysis), results were very similar and conclusions were unchanged (results available from review authors).
Inadequate allocation concealment in Placencia 1993 may have influenced withdrawal rates if participants, or personnel, or both, were aware of which drug the participants had been assigned; from the data we received, 19% of participants withdrew from the carbamazepine arm, and 15% of participants withdrew from the phenobarbitone arm while the other three studies included in the analysis showed more participants withdrawing from the phenobarbitone arm than the carbamazepine arm. Furthermore, inconsistencies between published data and data provided to us and unclear definitions for reason of withdrawal (participants withdrew for 'no clearly articulated reason') was likely to have influenced the results of our analysis. These factors in the Placencia 1993 trial in addition to the continuation of the carbamazepine arm in de Silva 1996 after the withdrawal of the phenobarbitone arm are all factors that are likely to have contributed to the heterogeneity in Analysis 1.1 and Analysis 1.2. These factors may have confounded the results of our primary analyses in this review.
(2) Time to achieve 12‐month remission
For this outcome, a HR greater than one indicates a clinical advantage for phenobarbitone.
Data for 683 participants from four trials were available for analyses of time to 12‐month remission and time to six‐month remission (98.8% of 691 participants from de Silva 1996, Heller 1995, Mattson 1985, and Placencia 1993 (see Included studies and Table 5) and 46.9% of the total 1455 participants from the 13 included studies). Mattson 1985 recorded no follow‐up data for one participant randomised to carbamazepine. de Silva 1996 did not record the randomised drug for six participants, and in Placencia 1993, seizure data after occurrence of first seizure were not available for one participant randomised to phenobarbitone, so we did not include this participant in the analyses. The study duration of Ogunrin 2005 was 12 weeks, so 12‐month remission was not possible among participants in this trial. Banu 2007 recorded the date of first seizure after randomisation, but all dates of subsequent seizures were not available; therefore, we could calculate 'time to first seizure' but not 'time to six‐month remission' and 'time to 12‐month remission'.
Two hundred and eighty out of 683 participants (41%) achieved 12‐month remission; 163 out of 384 (45%) on carbamazepine and 117 out of 319 (37%) on phenobarbitone. The overall pooled HR (for 683 participants) was 0.93 (95% CI 0.72 to 1.19, P = 0.57; Table 2), suggesting no advantage for either drug. There was no evidence of statistical heterogeneity between trials (Chi² test = 3.54, df = 3, P = 0.32, I² statistic = 15%, see Analysis 1.3).
Analysis 1.3.
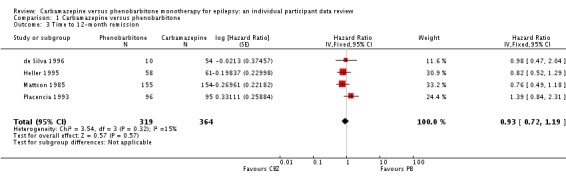
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 3 Time to 12‐month remission.
We performed sensitivity analysis excluding participants from Placencia 1993 from the analysis because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 7). This sensitivity analysis resulted in a pooled HR of 0.82 (95% CI 0.61 to 1.09, P = 0.17), suggesting an advantage for carbamazepine that was not statistically significant. Again, there was no evidence of statistical heterogeneity between trials (Chi² test = 0.33, df = 2, P = 0.85, I² statistic = 0%). Our conclusion did not change following the sensitivity analysis.
In Placencia 1993, there was evidence that the proportional hazards assumption of the Cox model may have been violated; the P value of the time‐varying covariate was < 0.001. On closer inspection of the participants in Placencia 1993, all 60 participants who achieved 12‐month remission achieved immediate remission (i.e. did not have any seizures at all in the first 12 months of follow‐up). The trial followed up a further 42 participants for more than 365 days (up to 548 days); however, none of these participants achieved a 12‐month period of seizure freedom during the trial, so we censored them all at their last follow‐up date (after 365 days). This observation would explain the apparent change in treatment effect over time in Placencia 1993, and therefore the violation of the proportional hazards assumption. When we analysed separately those who achieved immediate 12‐month remission, the proportional hazards assumption was satisfied (P value of time‐varying covariate was 0.872). The proportional hazards assumption of the Cox model was satisfied for all other trials included in the analysis.
For participants with generalised onset seizures (158), the pooled HR was 0.64 (95% CI 0.41 to 1.01, P = 0.05; Table 2), suggesting a borderline statistically significant advantage for carbamazepine. There was no evidence of statistical heterogeneity between studies for participants with generalised seizures (Chi² test = 0.61, df = 2, P = 0.74, I² statistic = 0%). For participants with partial onset seizures (525), the pooled HR was 1.11 (95% CI 0.81 to 1.51, P = 0.52; Table 2 ), suggesting an advantage for phenobarbitone that was not statistically significant. A considerable amount of statistical heterogeneity was present between studies for participants with partial onset seizures (Chi² test = 9.06, df = 3, P = 0.03, I² statistic = 67%). When we repeated the analysis with random‐effects, the result for participants with generalised seizures was unchanged, and for participants with partial onset seizures, the pooled HR was 1.24 (95% CI 0.69 to 2.22, P = 0.47), showing a larger advantage for phenobarbitone that was not statistically significant. Overall, the pooled HR (adjusted for seizure type for 683 participants, fixed‐effect) was 0.93 (95% CI 0.72 to 1.20, P = 0.57), suggesting no clear overall advantage for either drug, but a considerable amount of heterogeneity was present between studies (Chi² test = 13.48, df = 6, P = 0.04, I² statistic = 55%). When we repeated the analysis with random‐effects, results were similar and conclusions unchanged. We found a statistically significant interaction between treatment and seizure type (generalised versus partial onset) (Chi² test = 3.81, df = 1, P = 0.05, I² statistic = 73.8%, see Analysis 1.4, calculated with fixed‐effect).
Upon visual inspection of forest plots in Analysis 1.4, it was clear that Placencia 1993 was the main source of the heterogeneity between studies in the subgroup of participants with partial onset seizures. The other three studies showed moderate, non‐significant effect sizes while Placencia 1993 showed a large, significant effect size in favour of phenobarbitone (HR 2.43, 95% CI 1.27 to 4.65). This effect was not shown in the subgroup of participants with generalised onset seizures in participants in Placencia 1993 (HR 0.48, 95% CI 0.19 to 1.18). Repeating our sensitivity analysis from above, excluding Placencia 1993 from analysis due to inadequate allocation concealment, heterogeneity reduced to 0 (I² statistic = 0%) in all analyses, and there was no longer evidence of an interaction between treatment and seizure type. Results were also changed for participants with generalised onset seizures (101) (pooled HR 0.71, 95% CI 0.42 to 1.19, P = 0.19), showing an advantage for carbamazepine that was no longer statistically significant; for participants with partial onset seizures (394), a pooled HR of 0.88 (95% CI 0.62 to 1.25, P = 0.47) showed a change in direction of effect, now indicating an advantage for carbamazepine that was not statistically significant. And overall, the pooled HR (adjusted for seizure type for 495 participants) was 0.82 (95% CI 0.61 to 1.10, P = 0.18), suggesting an advantage for carbamazepine that was not statistically significant.
The sensitivity analysis excluding participants randomised to carbamazepine following withdrawal of the phenobarbitone arm in the de Silva 1996 trial gave similar results, with an estimated pooled HR of 0.90 (95% CI 0.69 to 1.17, P = 0.42). Results within each seizure group were also similar, with a pooled HR of 0.59 (95% CI 0.37 to 0.95, P = 0.03) for participants with generalised seizures (137) and a pooled HR of 1.09 (95% CI 0.79 to 1.49, P = 0.61) for participants with partial seizures (503), resulting in no changes in conclusions (see Table 7 for further details).
Following reclassification of the 65 participants aged 30 or older with new onset generalised seizures in Heller 1995, Ogunrin 2005, and Placencia 1993 (see Sensitivity analysis), results were very similar and conclusions were unchanged (results available from review authors).
As in the analysis of our primary outcome, Placencia 1993 seemed to be contributing the majority of the variability between trial results. This could have been a knock‐on effect of the inadequate allocation concealment in this trial, which was likely to have influenced the withdrawal rates in this study, and in turn the number of participants remaining in the trial who could achieve 12‐month remission. Again, we conclude that the inclusion of this study may have confounded the results of this outcome.
(3) Time to achieve six‐month remission
For this outcome, a HR greater than 1 indicates a clinical advantage for phenobarbitone. See 'time to 12‐month remission' for details of participants included in the analyses of time to six‐month remission.
Three hundred and eighty‐seven out of 683 participants (57%) achieved six‐month remission, 213 out of 384 (59%) on carbamazepine and 117 out of 319 (55%) on phenobarbitone. The overall pooled HR (for 683 participants) was 1.02 (95% CI 0.83 to 1.26, P = 0.86), suggesting no advantage for either drug. There was no evidence of statistical heterogeneity between trials (Chi² test = 3.63, df = 3, P = 0.30, I² statistic = 17%, see Analysis 1.5).
Analysis 1.5.
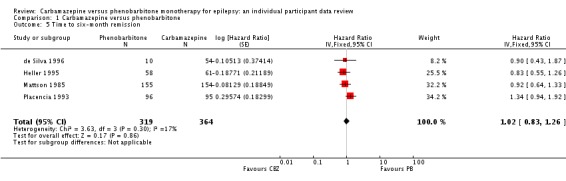
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 5 Time to six‐month remission.
We performed sensitivity analysis excluding participants from Placencia 1993 from the analysis because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 7). This sensitivity analysis resulted in a pooled HR of 0.88 (95% CI 0.68 to 1.14, P = 0.34), suggesting an advantage for carbamazepine that was not statistically significant. Again, there was no evidence of statistical heterogeneity between trials (Chi² test = 0.14, df = 2, P = 0.93, I² statistic = 0%). Our conclusion did not change following the sensitivity analysis.
In Mattson 1985, there was an indication that the proportional hazards assumption may have been violated (see Data synthesis); the P value of the time‐varying covariate was 0.054, and visual inspection of the cumulative incidence plot (Figure 12) showed crossing of the curves at around 300 days. In other words, up to 300 days, participants on phenobarbitone seemed to be achieving six‐month remission earlier than those on carbamazepine, but this changed after 300 days. However, participant numbers were reduced by 300 days (83 participants at risk out of 308 randomised), so small changes may have been magnified at this time.
Figure 12.
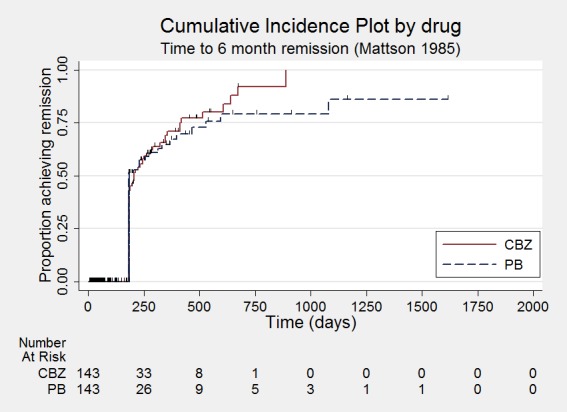
Time to six‐month remission ‐ Mattson 1985
As a sensitivity analysis, we fitted a piecewise Cox regression model to investigate any change in treatment effect over time, assuming proportional hazards within each interval. From the visual inspection of Figure 12, we split the follow‐up period of Mattson 1985 into three intervals: 0 to 182.5 days (immediate six‐month remission), 182.5 to 300 days, and over 300 days (maximum follow‐up: 1616 days). We estimated separate HRs for each interval.
For 'interval 0 to 182.5 days' (74 events from 308 at participants at risk), the HR was 1.06 (95% CI 0.63 to 1.77, P = 0.83), indicating no clear advantage of either drug. For 'interval 182.5 to 300 days' (22 events from 83 participants at risk), the HR was 0.65 (95% CI 0.37 to 1.15, P = 0.14), suggesting an advantage for carbamazepine that was not statistically significant. For 'interval over 300 days' (20 events from 41 participants at risk), the HR was 0.92 (95% CI 0.64 to 1.33, P = 0.65), suggesting no clear advantage of either drug.
These results suggest some indication of a change in treatment effect over time, with no clear advantage between the two drugs in the early stages of the trial for immediate remission; an advantage for carbamazepine emerged after the initial six months, which was no longer present by the end of the study. However, the CIs of estimates were wide, particularly for later times in the trial due to small numbers of events and participants and risk, so we do not have statistically significant evidence to support the hypothesis of a change in treatment effect over time for Mattson 1985. Thus, we conclude that the observed difference in treatment effect around 180 to 300 days compared with the rest of the study follow‐up was likely to be due to chance that more participants on carbamazepine achieved six‐month remission than those on phenobarbitone at this time (16 participants on carbamazepine compared with 6 on phenobarbitone in this time interval) while the numbers of participants achieving six‐month remission were more comparable at other time points. The proportional hazards assumption of the Cox model was satisfied for all other trials included in the analysis.
For participants with generalised onset seizures (158), the pooled HR was 0.69 (95% CI 0.47 to 1.01, P = 0.06), suggesting a borderline statistically significant advantage for carbamazepine. There was no evidence of statistical heterogeneity between studies for participants with generalised seizures (Chi² test = 1.25, df = 2, P = 0.54, I² statistic = 0%). For participants with partial onset seizures (525), the pooled HR of 1.17 (95% CI 0.90 to 1.50, P = 0.24) suggested an advantage for phenobarbitone that was not statistically significant. A considerable amount of statistical heterogeneity was present between studies for participants with partial onset seizures (Chi² test = 7.99, df = 3, P = 0.05, I² statistic = 62%). When we repeated the analysis with random‐effects, the result for participants with generalised seizures was unchanged, and for participants with partial onset seizures, the pooled HR of 1.15 (95% CI 0.73 to 1.82, P = 0.54) still showed an advantage for phenobarbitone that was not statistically significant. Overall, the pooled HR (adjusted for seizure type for 683 participants, fixed‐effect) was 0.99 (95% CI 0.80 to 1.23, P = 0.95), suggesting no clear overall advantage for either drug, but a considerable amount of heterogeneity was present between studies (Chi² test = 14.24, df = 6, P = 0.03, I² statistic = 58%). When we repeated the analysis with random‐effects, results were similar and conclusions unchanged. We found a statistically significant interaction between treatment and seizure type (generalised versus partial onset) (Chi² test = 5.00, df = 1, P = 0.03, I² statistic = 80.0%, see Analysis 1.6, calculated with fixed‐effect).
As in Analysis 1.4, from visual inspection of forest plots in Analysis 1.6, it was clear that Placencia 1993 was the main source of the heterogeneity between studies in the subgroup of participants with partial onset seizures. The other three studies showed moderate, non‐significant effect sizes, while Placencia 1993 showed a large, significant effect size in favour of phenobarbitone (HR 1.95, 95% CI 1.25 to 3.04). Again, this effect was not shown in the subgroup of participants with generalised onset seizures in participants in Placencia 1993 (HR 0.52, 95% CI 0.27 to 0.98). Repeating our sensitivity analysis from above as in the analysis of 'time to 12‐month remission', excluding Placencia 1993 from analysis because of inadequate allocation concealment, reduced heterogeneity to 0 (I² statistic = 0%) in all analyses, and there was no longer evidence of an interaction between treatment and seizure type. Results were also changed for participants with generalised onset seizures (101), with a pooled HR of 0.81 (95% CI 0.50 to 1.32, P = 0.40) showing an advantage for carbamazepine that was not statistically significant; for participants with partial onset seizures (394), a pooled HR of 0.91 (95% CI 0.67 to 1.24, P = 0.56) showed a change in direction of effect, again indicating an advantage for carbamazepine that was not statistically significant. And overall, the pooled HR (adjusted for seizure type for 495 participants) was 0.88 (95% CI 0.68 to 1.14, P = 0.34), suggesting an advantage for carbamazepine that was not statistically significant.
The sensitivity analysis excluding participants randomised to carbamazepine following the withdrawal of the phenobarbitone arm in the de Silva 1996 trial gave similar results, with an estimated pooled HR of 0.97 (95% CI 0.78 to 1.21, P = 0.79). Results within each seizure group were also similar, with a pooled HR of 0.66 (95% CI 0.45 to 0.98, P = 0.04) for participants with generalised seizures (137) and a pooled HR of 1.14 (95% CI 0.88 to 1.48, P = 0.31) for participants with partial seizures (503), resulting in no changes in conclusions (see Table 7 for further details).
Following reclassification of the 65 participants aged 30 or older with new onset generalised seizures in Heller 1995, Ogunrin 2005, and Placencia 1993 (see Sensitivity analysis), results were very similar and conclusions were unchanged (results available from review authors).
As in the analysis of our outcomes 'time to withdrawal of allocated treatment' and 'time to 12‐month remission', Placencia 1993 seemed to be contributing the majority of the variability between trial results (see the above outcomes for discussion). Again, we conclude that the inclusion of this study may have confounded the results of this outcome.
4) Time to first seizure post‐randomisation
For this outcome, a HR greater than one indicates a clinical advantage for carbamazepine.
We had data for 822 participants from six trials (98.3% of 836 participants from Banu 2007, de Silva 1996, Heller 1995, Mattson 1985, Ogunrin 2005, and Placencia 1993 (see Included studies and Table 5)). de Silva 1996 did not record the randomised drug for six participants, and dates of seizure recurrence were not available for eight participants (4 randomised to carbamazepine and 4 to phenobarbitone) in Mattson 1985; therefore, we did not include these 14 participants in the analysis.
Four hundred and fifty‐three out of 822 participants (55%) experienced seizure recurrence, 264 out of 434 (61%) on carbamazepine and 189 out of 388 (49%) on phenobarbitone. The overall pooled HR (for 822 participants) was 0.87 (95% CI 0.72 to 1.06, P = 0.18; Table 2), suggesting an advantage for phenobarbitone that was not statistically significant. There was no evidence of statistical heterogeneity between trials (Chi² test = 6.26, df = 5, P = 0.28, I² statistic = 20%, see Analysis 1.7).
Analysis 1.7.
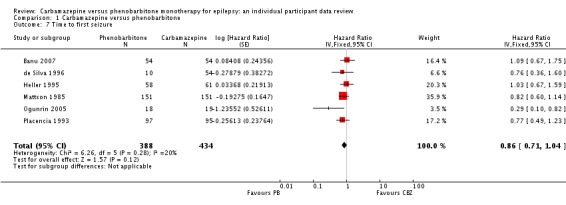
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 7 Time to first seizure.
We performed sensitivity analysis excluding participants from Placencia 1993 from analysis because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 7). This sensitivity analysis resulted in a pooled HR of 0.87 (95% CI 0.71 to 1.08, P = 0.22), still suggesting an advantage for phenobarbitone that was not statistically significant. Again, there was no significant evidence of statistical heterogeneity between trials (Chi² test = 6.04, df = 4, P = 0.20, I² statistic = 34%). Our conclusion did not change following the sensitivity analysis.
In Banu 2007, we found inconsistencies (between the IPD dataset and published results), which the study authors could not resolve; the publication reported that only seven participants had experienced no seizures from the start of treatment (3 randomised to phenobarbitone and 4 randomised to carbamazepine); however, from IPD provided, 21 participants did not experience seizures from the start of treatment (12 randomised to phenobarbitone and 9 randomised to carbamazepine). Given these inconsistencies and the limited data available on seizure recurrence, we performed sensitivity analysis excluding the participants from Banu 2007 from Analysis 1.7. This sensitivity analysis resulted in a pooled HR of 0.82 (95% CI 0.66 to 1.01, P = 0.06), suggesting a slightly larger advantage to phenobarbitone, which is now borderline statistically significant. Again, there was no evidence of statistical heterogeneity between trials (Chi² test = 5.11, df = 4, P = 0.28, I² statistic = 22%). This sensitivity analysis showed that Banu 2007, a trial which showed a small, non‐significant advantage for carbamazepine, may have confounded the results of our analysis; without the inclusion of this trial, our results indicated a larger, borderline statistically significant advantage for phenobarbitone for the outcome of time to first seizure.
For participants with generalised onset seizures (238), the pooled HR was 1.23 (95% CI 0.86 to 1.77, P = 0.27; Table 2), suggesting an advantage for carbamazepine that was not statistically significant. A considerable amount of statistical heterogeneity was present between studies for participants with generalised onset seizures (Chi² test = 8.65, df = 4, P = 0.07, I² statistic = 54%). For participants with partial onset seizures (584), the pooled HR of 0.76 (95% CI 0.60 to 0.96, P = 0.02; Table 2) suggested a statistically significant advantage for phenobarbitone. There was no evidence of statistical heterogeneity between studies for participants with partial onset seizures (Chi² test = 4.55, df = 5, P = 0.47, I² statistic = 0%). When we repeated the analysis with random‐effects, the result for participants with partial onset seizures was unchanged, and for participants with generalised onset seizures, the pooled HR of 1.15 (95% CI 0.66 to 2.02, P = 0.62) still showed an advantage for carbamazepine that was not statistically significant. Overall, the pooled HR (adjusted for seizure type for 822 participants, fixed‐effect) was 0.87 (95% CI 0.72 to 1.06, P = 0.18), suggesting an advantage for phenobarbitone that was not statistically significant. A considerable amount of heterogeneity was present between studies (Chi² test = 17.98, df = 10, P = 0.06, I² statistic = 44%). When we repeated the analysis with random‐effects, the results were similar and conclusions unchanged. We found a statistically significant interaction between treatment and seizure type (generalised versus partial onset) (Chi² test = 4.78, df = 1, P = 0.03, I² statistic = 79.1%, see Analysis 1.8, calculated with fixed‐effect).
From visual inspection of forest plots in Analysis 1.8, it was clear that Ogunrin 2005 was the main source of the heterogeneity between studies in the subgroup of participants with generalised onset seizures. The other four studies showed non‐significant advantages of carbamazepine, while Ogunrin 2005 showed a large, significant effect size in favour of phenobarbitone (HR 0.21, 95% CI 0.06 to 0.76). The subgroup of participants with partial onset seizures in participants in Ogunrin 2005 did not show this effect (HR 1.42, 95% CI 0.26 to 7.80). Reclassification of the 65 participants aged 30 or older with new onset generalised seizures in Heller 1995, Ogunrin 2005, and Placencia 1993 (see Sensitivity analysis) into an uncertain seizure type group (see Analysis 1.9) reduced heterogeneity between studies for the remaining 757 participants to 0 (I² statistic = 0%); the results among participants with partial onset seizures were unchanged. For participants with generalised onset seizures (173), a pooled HR of 1.39 (95% CI 0.86 to 1.77, P = 0.13) indicated a larger advantage of carbamazepine that still does not reach statistical significance. (We note that we could not calculate the HR for Ogunrin 2005 as following reclassification, only a single participant remained in the phenobarbitone group and did not experience seizure recurrence). Among the group of participants with 'uncertain' seizure type (65), the pooled HR of 1.22 (95% CI 0.59 to 2.51, P = 0.59) suggested an advantage of carbamazepine that was not statistically significant. A considerable amount of heterogeneity was present in the analysis of reclassified participants (Chi² test = 4.78, df = 2, P = 0.09, I² statistic = 58%), which was perhaps unsurprising as this relatively small group was made up of participants with 'uncertain' and likely different seizure types. Following reclassification, a statistically significant interaction between treatment and seizure type (generalised versus partial onset) still existed (Chi² test = 6.64, df = 2, P = 0.04, I² statistic = 69.9%, see Analysis 1.9), indicating an advantage for phenobarbitone for participants with partial onset seizures and an advantage for carbamazepine for participants with generalised onset seizures.
Analysis 1.9.
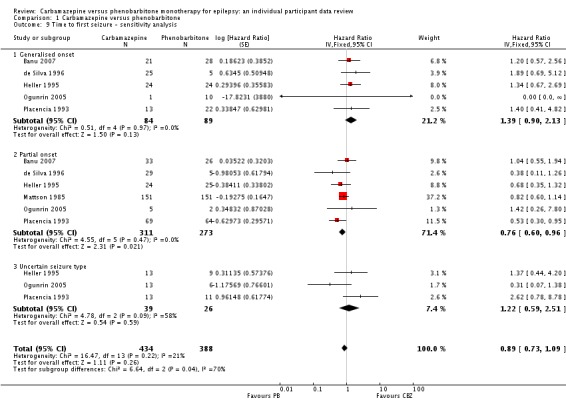
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 9 Time to first seizure ‐ sensitivity analysis.
The sensitivity analysis excluding participants randomised to carbamazepine following withdrawal of the phenobarbitone arm in the de Silva 1996 trial gave similar results, with an estimated pooled HR of 0.87 (95% CI 0.71 to 1.06, P = 0.10). Results within each seizure group were also similar, with a pooled HR of 1.20 (95% CI 0.82 to 1.75) for participants with generalised seizures (217) and a pooled HR of 0.77 (95% CI 0.61 to 0.97, P = 0.007) for participants with partial seizures (562) (see Table 7 for further details).
In de Silva 1996, there was an indication that the proportional hazards assumption may have been violated (see Data synthesis); the P value of the time‐varying covariate was 0.08, and visual inspection of the cumulative incidence plot (Figure 13) showed crossing of the curves at around 100 days. In other words, up to 100 days, more participants on carbamazepine seemed to be experiencing first seizure recurrence earlier than those on phenobarbitone, but this changed after 100 days. However, participant numbers were reduced by 100 days (26 participants at risk out of 64 randomised), so small changes may have been magnified at this time. Furthermore, curves also seemed to cross at around 800 days, when even fewer participants remained at risk of first seizure in the trial (11 participants at risk out of 64 randomised).
Figure 13.
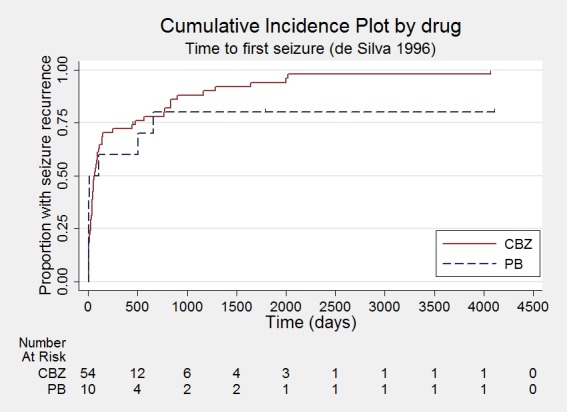
Time to first seizure ‐ de Silva 1996
As a sensitivity analysis, we fitted a piecewise Cox regression model to investigate any change in treatment effect over time assuming proportional hazards within each interval. From the visual inspection of Figure 13, we split the follow‐up period of de Silva 1996 into three intervals: 0 to 100 days, 100 to 800 days, and over 800 days (maximum follow‐up 4163 days). We estimated separate HRs for each interval.
For 'interval 0 to 100 days' (38 events from 64 participants at risk), the HR was 0.92 (95% CI 0.36 to 2.34, P = 0.83), indicating no clear advantage of either drug. For 'interval 100 to 800 days' (14 events from 26 participants at risk), the HR was 1.06 (95% CI 0.55 to 2.01, P = 0.86), again, suggesting no clear advantage of either drug. Over 800 days, 11 participants remained at risk; however, neither of the two remaining participants randomised to phenobarbitone experienced an event (shown by the flattening of the curve at around 700 to 800 days in Figure 13); therefore, the HR of first seizure recurrence was undefined over this time period. Furthermore, in sensitivity analysis excluding participants randomised to carbamazepine following withdrawal of the phenobarbitone arm in the de Silva 1996 trial, there was no longer evidence that the proportional hazards assumption had been violated; the P value of the time‐varying covariate was 0.316 among these 20 participants.
We did not find any statistically significant evidence to support a change in treatment effect over time in de Silva 1996 for the outcome of 'time to first seizure'. We conclude that the imbalance in participant numbers in the two randomised groups (54 randomised to carbamazepine and 10 randomised to phenobarbitone) magnified the apparent crossing of the survival plots over time and the majority of participants experiencing an event (60 participants experienced a seizure while only four were censored in this analysis) was also likely to be an influence. The proportional hazards assumption of the Cox model was satisfied for all other trials included in the analysis.
We conclude from this analysis that there was likely to be a difference in efficacy of the drugs (in terms of time to first seizure recurrence after randomisation) by seizure type, that participants with generalised seizures experience seizure recurrence later on carbamazepine than phenobarbitone, and that participants with partial onset seizures experience seizure recurrence later on phenobarbitone than carbamazepine. The overall trend towards an advantage for phenobarbitone for all included participants reflects that the majority of participants included in this analysis had partial onset seizures (71% of 822 included participants). It was possible that inconsistencies in data provided to us (Banu 2007), and misclassification of seizure type in participants over the age of 30 (Heller 1995;Ogunrin 2005; Placencia 1993), may have confounded the results of this analysis. However, in a sensitivity analysis to take account of these confounding factors, the association between treatment and seizure type still existed and therefore could be a true association.
5) Adverse events
We extracted all reported information related to adverse events from the study publications. Cossu 1984 did not report any findings related to adverse events, and without access to protocols, we are uncertain if these data were collected (see Selective reporting (reporting bias)). (See Table 8 for details of all adverse event data provided in the other 12 studies included in this review). Two studies reported only numbers of withdrawals due to adverse events (Chen 1996; Czapinski 1997), and two reported the rate of adverse events/number of participants reporting adverse events (Bidabadi 2009; Placencia 1993); these four studies did not report specific adverse events. For the eight studies that did report specific adverse events, the most commonly reported events (reported by two or more studies) were:
Table 5.
Adverse event data (narrative report)
| Trial | Adverse event data¹ | Summary of reported results | |
| Carbamazepine (CBZ) | Phenobarbitone (PB) | ||
| Banu 2007² | Reported list of 'problems' at the last visit (provided as IPD) | CBZ (n = 54): speech/learning delay (n = 6), headaches (n = 3), restlessness/hyperactivity/poor attention/irritability (n = 6), psychomotor deterioration/delay (n = 2), sleep disturbances (n = 2), fatigue (n = 1), hydrocephalus (build up of fluid on the brain) (n = 1), CBZ hypersensitivity (n = 1), aggression (n = 1), temper tantrums (n = 1), other behavioural problems (n = 5), poor cognition (n = 1), mild stroke (n = 1), mild right‐sided weakness (n = 1), intolerable behavioural problems (n = 6) | PB (n = 54): speech/learning delay (n = 7), restlessness/hyperactivity/poor attention/irritability (n = 8), sleep disturbances (n = 1), fatigue (n = 1), poor cognition (n = 2), aggression (n = 1), temper tantrums (n = 3), breath‐holding attacks (n = 1), other behavioural problems (n = 3), facial twitching (n = 1), left‐sided weakness (n = 1), leg pain (n = 1), vomiting (n = 1), intolerable behavioural problems (n = 4) |
| Bidabadi 2009³ | Rate of drug side‐effects | No statistical significant difference was seen after treatment between 2 groups in the rate of drug side‐effects | No statistical significant difference was seen after treatment between 2 groups in the rate of drug side‐effects |
| Cereghino 1974²,⁴ | Most frequently observed side‐effects | Gastrointestinal side‐effects and "impaired function" (general malaise). Frequency not clearly stated | Gastrointestinal side‐effects and "impaired function" (general malaise). Frequency not clearly stated |
| Chen 1996 | Withdrawal from the study due to 'allergic reactions' | CBZ (n = 24): 1 participant withdrew due to an allergic reaction | PB (n = 23): 2 participants withdrew due to allergic reactions |
| Cossu 1984 | No adverse events reported | Not reported | Not reported |
| Czapinski 1997³ | "Exclusions due to adverse events or no efficacy" | Proportion "excluded": 30% (out of 30 randomised to CBZ) | Proportion "excluded": 33.3% (out of 30 randomised to PB) |
| de Silva 1996⁵,⁶ | "Unacceptable" adverse events leading to drug withdrawal | CBZ (n = 54): drowsiness (n = 1), blood dyscrasia (n = 1) | PB (n = 10): drowsiness (n = 1), behavioural (n = 5) |
| Feksi 1991 | Reports of minor adverse events and side‐effects leading to drug withdrawal | CBZ (n = 150): withdrawals due to side‐effects: skin rash (n = 4), psychosis (n = 1), aggressive behaviour (n = 1). Minor adverse events: CBZ: 46 participants reported 68 adverse events |
PB (n = 152): withdrawals due to side‐effects: skin rash (n = 1), psychosis (n = 1), hyperactivity (n = 3). Minor adverse events: 58 participants reported 86 adverse events |
| Heller 1995⁵ | "Unacceptable" adverse events leading to drug withdrawal |
CBZ (n = 61): drowsiness (n = 3), rash (n = 2), headache (n = 1), depression (n = 1) | PB (n = 58): drowsiness (n = 4), lethargy (n = 4), rash (n = 1), dizziness (n = 2), headaches (n = 1), nausea and vomiting (n = 1) |
| Mattson 1985² | Narrative report of 'adverse effects' and 'serious side‐effects' | CBZ (n = 155): motor disturbance (ataxia, incoordination, nystagmus, tremor ‐ 33%), dysmorphic and idiosyncratic side‐effects (gum hypertrophy, hirsutism, acne, and rash ‐ 14%), gastrointestinal problems (27%), decreased libido or impotence (13%). No serious side‐effects | PB (n = 155): motor disturbance (ataxia, incoordination, nystagmus, tremor ‐ 24%), dysmorphic and idiosyncratic side‐effects (gum hypertrophy, hirsutism, acne, and rash ‐11 %), gastrointestinal problems (13%), decreased libido or impotence (16%). No serious side‐effects |
| Mitchell 1987 | Systemic side‐effects and side‐effects leading to drug change | CBZ (n = 15): 4 participants switched from CBZ to PB; 3 due to systemic side‐effects (1 with persistent rashes and 1 with marked granulocytopenia (decrease of granulocytes (white blood cells)) and 1 due to behavioural changes | PB (n = 18): 1 participant switched from PB to CBZ due to substantial behavioural side‐effects |
| Ogunrin 2005² | Participant‐reported symptomatic complaints (provided as IPD) | CBZ (n = 19), memory impairment (n = 9), psychomotor retardation (n = 1), inattention (n = 1), transient rash (n = 1), CBZ‐induced cough (n = 1) | PB (n = 18), memory impairment (n = 13), psychomotor retardation (n = 8), inattention (n = 9) |
| Placencia 1993 | Number of participants reporting side‐effects | CBZ (n = 95): 53 participants reported at least 1 side‐effect | PB (n = 97): 50 participants reported at least 1 side‐effect |
CBZ: carbamazepine; PB: phenobarbitone ¹We recorded adverse event data as reported narratively in the publications; therefore, exact definition of a symptom may vary. Adverse event data were supplied as IPD for Banu 2007 and Ogunrin 2005. Adverse event data were not requested in original IPD requests (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993), but will be for all future IPD requests. For numbers of withdrawals due to adverse events in studies for which we received IPD (Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993), see Table 6. ²Bidabadi 2009 and Czapinski 1997 are abstracts only so very little information was reported. ³Participants may report more than one adverse event. ⁴Note that the recruited participants in this study were institutionalised; therefore, the "precise nature of side‐effects was not always determinable". The two most frequently occurring side‐effects were reported as the frequency of participants reporting the side‐effect on each day of the treatment period; however, overall totals of participants reporting each side‐effect were not reported. ⁵Participants may have withdrawn due to adverse event alone or a combination of adverse events and poor efficacy (seizures). ⁶The phenobarbitone arm of de Silva 1996 was stopped prematurely after 10 children were randomised to this arm because of concerns over behavioural adverse events (see the 'Characteristics of included studies' tables).
For carbamazepine
Gastrointestinal side‐effects including abdominal pain, nausea, and vomiting (Cereghino 1974; Mattson 1985).
Drowsiness/tiredness/fatigue/sedation (Banu 2007; de Silva 1996; Heller 1995).
Headaches (Banu 2007; Heller 1995).
Motor disturbance (including ataxia, incoordination, nystagmus, tremor, slowing of mental function, inattention, psychomotor retardation) (Banu 2007; Mattson 1985; Ogunrin 2005).
Dysmorphic and idiosyncratic side‐effects (rash, gum hypertrophy, hirsutism, acne, other skin problems) (Feksi 1991; Heller 1995; Mattson 1985; Mitchell 1987; Ogunrin 2005).
Cognitive side‐effects and impairments including depression and memory problems (Banu 2007; Feksi 1991; Heller 1995; Ogunrin 2005).
Behavioural‐related side‐effects (aggression, behavioural changes, etc.) (Banu 2007; Feksi 1991; Mitchell 1987).
For phenobarbitone
Gastrointestinal side‐effects including abdominal pain, nausea, and vomiting (Banu 2007; Cereghino 1974; Heller 1995; Mattson 1985).
Drowsiness/tiredness/fatigue/sedation (Banu 2007; de Silva 1996; Heller 1995).
Motor disturbance (including ataxia, incoordination, nystagmus, tremor, slowing of mental function, inattention, psychomotor retardation) (Banu 2007; Mattson 1985; Ogunrin 2005).
Dysmorphic and idiosyncratic side‐effects (rash, gum hypertrophy, hirsutism, acne, other skin problems) (de Silva 1996; Feksi 1991; Heller 1995; Mattson 1985).
Cognitive side‐effects and impairments including depression and memory problems (Banu 2007; Feksi 1991; Ogunrin 2005).
Behavioural‐related side‐effects (aggression, behavioural changes, etc.) (Banu 2007; de Silva 1996; Mitchell 1987).
It was difficult to summarise the 'most common' adverse events overall across the 12 studies or deduce whether carbamazepine or phenobarbitone were most associated with specific adverse events because of the differences in methods of reporting adverse event data across the studies (see Table 8). We did not include requests for adverse event data for individuals in the original IPD requests for earlier versions of this review, but we will pledge to do this in all future IPD requests.
Discussion
Summary of main results
The results of this review provide statistically significant evidence of an advantage for carbamazepine over phenobarbitone (phenobarbitone) for our primary global effectiveness outcome 'time to withdrawal of allocated treatment', when accounting for partial onset and generalised onset seizure types of 676 participants (pooled hazard ratio (HR) 1.50, 95% confidence interval (CI) 1.15 to 1.95, P = 0.003). However, a substantial amount of heterogeneity was present between individual results of the four included studies (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993), and when we accounted for this heterogeneity in random‐effects analysis, the advantage for carbamazepine was less convincing (pooled HR was 1.53, 95% CI 1.02 to 2.28, P = 0.04). We found no evidence of a difference between the two seizure types included in this review with respect to our primary outcome.
Sensitivity analyses for the primary outcome showed that poor methodological aspects of a single trial, Placencia 1993, recruiting 192 participants (13% of total eligible participants from 13 trials), contributed much variability to this analysis. This study did not adequately conceal allocation to participants, or personnel, or both, which may have influenced withdrawal rates in the study. Furthermore, there were inconsistencies between reasons for withdrawal of allocated treatment in the participant data provided to us and those reported in the published paper, in addition to unclear reasons for withdrawal, which are likely to have introduced variability into the analysis. Also, the withdrawal of the phenobarbitone arm within an included paediatric study, de Silva 1996, because of concerns of serious behavioural adverse events, was likely to have introduced variability and bias into the results of our primary outcome (see Quality of the evidence); therefore, we encourage caution when interpreting the results of our primary outcome.
For our two remission outcomes ('time to 12‐month and six‐month remission'), we did not find any statistically significant differences between carbamazepine and phenobarbitone overall or by seizure type. Again, a substantial amount of variability was present between studies, mostly contributed by Placencia 1993. We believe that it was likely that the inadequate allocation concealment in this trial also influenced the remission outcomes (i.e. the withdrawal rates in this study influenced by inadequate allocation concealment in turn influence the number of participants remaining in the trial who could achieve six‐ or 12‐month remission).
In the analysis of our other secondary efficacy outcome 'time to first seizure', among 822 participants in six included studies (Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993), we found evidence of an advantage of phenobarbitone that did not reach statistical significance (pooled HR 0.87, 95% CI 0.72 to 1.06, P = 0.18). For this outcome, we did find a statistically significant difference in outcome by seizure type (P value for Chi² test of subgroup differences); for 238 participants with generalised onset seizures, the pooled HR of 1.23 (95% CI 0.86 to 1.77, P = 0.27) suggested an advantage for carbamazepine that was not statistically significant, and for 584 participants with partial onset seizures, the pooled HR of 0.76 (95% CI 0.60 to 0.96, P = 0.02) suggested a statistically significant advantage for phenobarbitone. Again, there was variability between individual study results likely to be due to the methodological aspects of Placencia 1993 discussed above, inconsistencies between data provided and published data in Banu 2007, and potential misclassification of seizure type, particularly evident in Ogunrin 2005. However, following sensitivity analyses to account for these potential sources of variability, the association between outcome and seizure type remained statistically significant; therefore, we conclude that participants with generalised seizures experience seizure recurrence later on carbamazepine than phenobarbitone and that participants with partial onset seizures experience seizure recurrence later on phenobarbitone than carbamazepine. We also conclude that the overall trend in favour of phenobarbitone for this outcome was likely to reflect the distribution of seizure types of participants included in this analysis (71% of included participants were classified as having partial onset seizures).
The direction of the association between seizure type and outcome (advantage for carbamazepine for generalised seizures and advantage for phenobarbitone for partial seizures) was unexpected given documented evidence that carbamazepine may exacerbate some generalised seizure types, such as myoclonic and absence seizures (Liporace 1994; Shields 1983; Snead 1985), and that current guidelines recommend carbamazepine as a first‐line drug for the treatment of partial seizures (NICE 2012).
For all outcomes in this review, we would encourage caution over the interpretation of the results because of concerns regarding Overall completeness and applicability of evidence (see below), and we would not advocate basing a choice between these two drugs on the results of this review alone.
Overall completeness and applicability of evidence
We believe our systematic electronic searches identified all relevant evidence for this review. We have gratefully received IPDfor 1138 individuals (78% of individuals from all eligible trials) from the authors of seven trials (Banu 2007; de Silva 1996; Feksi 1991; Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993), which included a comparison of phenobarbitone with carbamazepine for the treatment of epilepsy. However, we were not able to include the data from one trial (Feksi 1991), recruiting 302 participants (representing 21% of the total number in the 13 eligible trials and 27% of the total number of participants from the trials for which we received IPD), because of many inconsistencies in the dataset that could not be resolved and we felt were too extensive to account for in sensitivity analysis (see Included studies).
We could not include in any analysis 317 individuals (22%) from the other six relevant trials (Bidabadi 2009; Cereghino 1974; Chen 1996; Cossu 1984; Czapinski 1997; Mitchell 1987), as IPD were not available and the published reports did not report outcomes of interest. Therefore, in total, we were able to include data for 836 participants from six trials (57% of individuals from all eligible trials).
However, while we received data for 836 participants for our primary effectiveness analysis, we were not able to include all data in all of our analyses; because of the short three‐month duration of the trial, we were unable to include 37 participants from Ogunrin 2005 in our remission analysis, and in this short follow‐up time, no participants withdrew from treatment; therefore, this study could not contribute to our primary outcome of 'time to withdrawal of allocated treatment' either. We were also unable to include 108 participants from Banu 2007 in analyses of treatment withdrawal and remission as we did not receive dates of treatment withdrawals and subsequent seizures after first seizure recurrence. Therefore, our primary outcome was, in fact, based on 676 participants (47% of individuals from all eligible trials).
Having to exclude data from nearly half of the eligible participants due to lack of IPD and insufficient reporting in study publications was likely to have impacted on the applicability of the evidence; therefore, we encourage caution in the interpretation of all results in this review. However, it was difficult to quantify exactly how large this impact was on the results of this review (see Potential biases in the review process).
Four trials contributing around 80% of the participant data to this review recruited adults only (Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993); the other two studies contributing around 20% of data were paediatric trials (Banu 2007; de Silva 1996). Also, the largest single trial contributing over a third of the participant data to this review, Mattson 1985, recruited individuals with partial onset seizures only. Therefore, only around 30% of participants included in this review were experiencing generalised onset seizures. Furthermore, there is evidence within this review to suggest that up to 27% of individuals with newly onset generalised seizures may have had their seizure type misclassified. For these reasons, the results of this review may not be fully generalisable to children or to individuals with generalised onset seizures, and more evidence recruiting these types of participants is required.
Quality of the evidence
The six trials for which IPD were made available were generally of quite good methodological quality; however, four out of the six trials for which we received IPD were at high risk of bias for at least one aspect (see Figure 3), which may have introduced bias into analyses.
Three of the trials contributing 27% of the participant data to this review described adequate methods of randomisation and allocation concealment (de Silva 1996; Heller 1995; Ogunrin 2005); however, the other two largest single trials contributing 50% of participant data to this review did not describe the method of randomisation or allocation concealment used, or both, and this information was not available from study authors (Banu 2007; Mattson 1985). We are uncertain whether this lack of information has impacted on the results of this review. One study contributing 23% of participant data to this review reported that an adequate method of allocation concealment was not used for all randomised participants, and we believe this inadequate allocation concealment may have influenced rates of withdrawal if participants, or clinicians, or both, were aware of the allocated treatment, which may have had a further knock‐on effect on our remission outcomes (see Effects of interventions).
Three of the trials providing IPD blinded participants and outcome assessors (Banu 2007; Mattson 1985; Ogunrin 2005); and the other two trials, de Silva 1996 and Heller 1995, were designed as pragmatic open‐label trials, as masking of treatment would not be "practicable or ethical", would "undermine compliance", and would "introduce bias due to a very large dropout rate" as blinding does not conform to standard clinical practice of increasing drug doses to therapeutic ranges (Heller 1995).
However, despite this reasoning, withdrawal rates across the double‐blind, Mattson 1985, and open‐label, de Silva 1996; Heller 1995, studies included in 'time to withdrawal of allocated treatment' were very similar (see Table 6 for further details); 37% of participants withdrew from Mattson 1985 (40% randomised to phenobarbitone and 36% randomised to carbamazepine), 36% of participants withdrew from Heller 1995 (40% randomised to phenobarbitone and 28% randomised to carbamazepine), and 46% of participants withdrew from de Silva 1996 (80% from phenobarbitone and 40% from carbamazepine). There was no statistically significant evidence of a difference in withdrawal rates between the double‐blind study and the two studies of an open‐label design (Chi² test, P = 0.82). It is however, debatable whether double‐blind design is the most appropriate for trials of monotherapy in epilepsy of long duration, and whether such a design does have an impact upon the dropout rate, and therefore, the results of the trial. The overall withdrawal rate in de Silva 1996 was greatly influenced by the high withdrawal rate of children randomised to phenobarbitone (80%), which led to the withdrawal of that treatment arm from the four‐treatment study because of concerns of serious adverse events. It is difficult to know if preconceptions of phenobarbitone and documented associations of the drug with adverse behavioural effects in children directly led to the withdrawal of the drug and if the same outcome would have occurred if the study had been double‐blinded. It is also interesting to note that within the other paediatric study within this review conducted in a rural area of Bangladesh (Banu 2007), there were no documented withdrawals of the allocated treatment (carbamazepine or phenobarbitone) due to adverse events, and in fact, in this study, significantly more children withdrew from carbamazepine than phenobarbitone for reasons related to the study drug (11% withdrew from phenobarbitone, 26% withdrew from carbamazepine, Chi² test, P = 0.05, see Table 6). Unfortunately, we could not include this study in the analysis of 'time to withdrawal of allocated treatment' as dates of treatment withdrawal were not available for all participants. Furthermore, a trial comparing phenobarbitone with phenytoin conducted in India, Pal 1998, in which phenobarbitone was concluded to be an "effective and acceptable antiepileptic drug for rural Indian children" did not report concerns regarding adverse events of phenobarbitone in children.
We note the influence of country of recruitment over the methodological design and perhaps the results of the trial; within the USA and Europe where many treatment options are available, phenobarbitone is no longer considered to be a first‐line agent in favour of more tolerable first‐line agents, such as carbamazepine and lamotrigine (NICE 2012), whereas in developing or rural regions where income is limited and newer generation antiepileptic drugs are not readily available or affordable, older and cheaper drugs, such as phenobarbitone, are more likely to be used as comparators.
While an IPD approach to analysis allows us to use unpublished data, therefore, reducing attrition and reporting bias, for two of the studies contributing 36% of participant data, we found inconsistencies between published data and participant data provided to us in terms of withdrawal information and seizure recurrence, respectively (Banu 2007; Placencia 1993), which the study authors could not resolve. In both cases, it was likely that the inconsistencies within these studies contributed to the considerable heterogeneity present within the analyses in this review.
Further differences between the studies were in the population recruited (age of participants and seizure types). We discuss these differences in Potential biases in the review process.
Trials for which no IPD were available were generally of poorer quality than those for which we received IPD. A lot of methodological information in these studies was not reported or unclear: two trials presented incomplete outcome data following exclusion of participants (Chen 1996; Feksi 1991); one study used an inadequate cross‐over design for investigating monotherapy treatments (Cereghino 1974); two trials were likely to have been underpowered to detect a difference between the drugs (Cossu 1984; Mitchell 1987); one trial may have been underpowered, too; and two trials available only in abstract or summary form, provided only very limited information on trial methodology (Bidabadi 2009; Czapinski 1997).
Overall, because of the documented methodological issues that may have introduced bias into our meta‐analyses, we rated the evidence provided in this review as 'low' quality according to GRADE criteria (See Table 1 and Table 2) and would not advocate use of the evidence in this review for clinical decision‐making between the two drugs.
Potential biases in the review process
We were able to include IPD for 836 out of 1455 eligible participants (57%) from six out of 13 studies in this review and conducted all analyses as IPD analyses. Such an approach has many advantages, such as allowing the standardisation of definitions of outcomes across trials, and attrition and reporting biases are reduced as we can perform additional analyses and calculate additional outcomes from unpublished data. For the outcomes we used in this review that are of a time‐to‐event nature, an IPD approach is considered to be the 'gold standard' approach to analysis (Parmar 1998).
However, despite the advantages of this approach, for reasons out of our control, we were not able to obtain IPD for 619 participants from seven eligible studies, and no aggregate data were available for our outcomes of interest in study publications; therefore, we had to exclude 43% of eligible participants from our analyses, which may have introduced bias into the review.
Given that no statistically significant differences were found between the drugs in terms of proportions of participants seizure‐free and proportions of participants withdrawing from allocated treatment in the seven studies for which IPD were not available (where recorded, see Table 4), we do not believe that our conclusions would have changed for the outcomes of this review had the IPD for the seven studies been available. We do however, recommend caution when interpreting results of analyses of this review because of potential retrieval bias from the exclusion of 43% of eligible participants from seven studies in this review.
Furthermore, five out of the seven studies that we were not able to include in meta‐analysis were at high risk of bias for at least one methodological aspect (see Figure 3 and Risk of bias in included studies); therefore, inclusion of this data may have introduced bias into our results. We also judged four out of the six studies with IPD provided for analysis to be at high risk of bias for at least one methodological element; we addressed these issues in sensitivity analysis and discussed at length for each analysis (see Sensitivity analysis and Effects of interventions).
We have good evidence from previous reviews conducted by the Cochrane Epilepsy Group that misclassification of seizure type is an important issue in epilepsy trials (Marson 2000; Nolan 2013b). We believe that the results of the original trials, and hence the results of the outcome 'time to first seizure', are likely to have been confounded by classification bias, particularly the 19 individuals from Ogunrin 2005 classified with new onset generalised seizures over the age of 30, and Malafosse 1994, contributing a large amount of variability to the analysis of 'time to first seizure'.
Ogunrin 2005 classified generalised and partial onset seizures according to the International League Against Epilepsy (ILAE) classification of 1981 (Commission 1981), rather than the revised ILAE classification in 1989 (Commission 1989), which may have led to misclassification. Furthermore, Ogunrin 2005 was conducted in Nigeria, a developing country without access to the same facilities as trials conducted in the USA and Europe; therefore, seizure types were classified clinically, and electroencephalographics (EEGs)/magnetic resonance images (MRIs) were not required for diagnosis of epilepsy. Clinical classification may also have contributed to potential misclassification in this study.
Finally, we made some assumptions in the statistical methodology used in this review. Firstly, when we received only follow‐up dates and seizure frequencies, we used linear interpolation to estimate seizure times. We are aware that an individual's seizure patterns may be non‐linear; therefore, we recommend caution when interpreting the numerical results of the seizure‐related outcomes. We also made an assumption that treatment effect for each outcome did not change over time (proportional hazards assumption, see Data synthesis). For all four of the outcomes, there was evidence that one of the trials may have violated this assumption. Sensitivity analysis showed that changes in treatment effect tended to occur in the later stages of the studies when small participant numbers were being followed up; therefore, small changes in treatment effect would be magnified. However, we are aware that in studies of long duration (de Silva 1996, Heller 1995, and Mattson 1985 followed up participants for between 3 and 10 years), the assumption of treatment effect remaining constant over time is unlikely to be appropriate, for example, there is likely to be a difference between participants who achieve immediate remission compared with participants who achieve later remission. Therefore, if more data can be made available to us for updates of this review, we would like to perform statistical analyses that allow for treatment effects to vary over time.
Agreements and disagreements with other studies or reviews
We have found no consistent differences in individual trials between phenobarbitone and carbamazepine with respect to seizure control or seizure type (Banu 2007; Bidabadi 2009; Cereghino 1974; Chen 1996; Cossu 1984; Czapinski 1997; de Silva 1996; Feksi 1991; Heller 1995; Mattson 1985; Mitchell 1987; Ogunrin 2005; Placencia 1993). However, within these trials, confidence intervals around estimates have been wide and equivalence cannot be inferred.
The adverse event profiles of the two drugs, particularly phenobarbitone with relation to behavioural changes in children, are well documented (see Description of the intervention). Results of this review suggest that phenobarbitone may be more likely to be withdrawn earlier than carbamazepine; however, results across studies were variable and should be interpreted with caution. There was no evidence in this review that participants are more likely to withdraw from phenobarbitone due to adverse events compared with carbamazepine. We found no differences between the two drugs in terms of time to remission of seizures; however, we found evidence of an advantage for phenobarbitone in terms of time to first seizure recurrence for partial onset seizures and an advantage for carbamazepine in terms of time to first seizure recurrence for generalised onset seizures. This result goes against documented evidence that carbamazepine may exacerbate some generalised seizure types (Liporace 1994; Shields 1983; Snead 1985), and that carbamazepine should be one of the drugs of first choice for new onset partial seizures (NICE 2012).
To our knowledge, together with previous versions of this review, this is the only systematic review and meta‐analysis that compares phenobarbitone and carbamazepine monotherapy for partial onset seizures and generalised onset tonic‐clonic seizures. A network meta‐analysis has been published (Tudur Smith 2007), comparing all direct and indirect evidence from phenobarbitone, carbamazepine, and other standard and new antiepileptic drugs licensed for monotherapy. Results of this network meta‐analysis showed a statistically significant advantage for carbamazepine compared with phenobarbitone for 'time to withdrawal of allocated treatment' for participants with partial onset seizures and a statistically significant advantage for phenobarbitone compared with carbamazepine for 'time to first seizure' for participants with partial onset seizures. No statistically significant differences were found between the drugs for participants with generalised onset seizures. The results of this review generally agree with the results of the network meta‐analysis. The network meta‐analysis is currently being updated to include more recently published studies, such as Banu 2007 and Ogunrin 2005; therefore, we will compare the results of this review with the updated network meta‐analysis.
Authors' conclusions
Current UK guidelines recommend carbamazepine or lamotrigine as first‐line treatment for adults and children with new onset partial seizures and sodium valproate for adults and children with new onset generalised seizures (NICE 2012).
The results of this review suggest that carbamazepine is likely to be a more effective drug than phenobarbitone in terms of treatment retention (withdrawals due to lack of efficacy or adverse events or both). The results of this review also suggest an association between treatment and seizure type for time to first seizure recurrence, with an advantage for phenobarbitone for partial onset seizures and an advantage for carbamazepine for generalised onset seizures. However, studies contributing to the analyses were of varying quality with variable results; therefore, we do not advise that results of this review alone should form the basis of a treatment choice for a patient with newly onset seizures. Because of documented evidence of carbamazepine worsening certain generalised seizure types and behavioural‐related adverse events associated with phenobarbitone, particularly in children, we emphasise caution and careful clinical follow‐up if these drugs are chosen for these specific subgroups of participants. We also recommend caution in the use of these drugs in women of child‐bearing potential because of documented teratogenic effects where the risk is estimated to be two to three times that of the general population (Meador 2008; Morrow 2006).
Few consistent differences in efficacy have been found between these two commonly used antiepileptic drugs in individual trials. The methodological quality of studies comparing these two drugs has been variable, producing variable individual study results introducing heterogeneity into the pooled results of this review and therefore making the pooled results difficult to interpret. If there are differences in efficacy and tolerability across heterogeneous populations of individuals such as those studied here, it is likely that these differences are small. It has been argued that future comparative antiepileptic drug trials should be powered to establish equivalence (Jones 1996), and therefore be capable of detecting what is considered to be the smallest important clinical difference.
This review highlights the need for the design of future antiepileptic drug monotherapy trials that recruit individuals of all ages with specific epilepsy syndromes powered to detect a difference between particular antiepileptic drugs. An approach likely to reflect and inform clinical practice, as well as being statistically powerful, would be to recruit heterogeneous populations for whom epilepsy syndromes have been adequately defined, with testing for interaction between treatment and epilepsy syndrome. In view of potential problems of misclassification, syndromes will have to be well defined, with adequate checking mechanisms to ensure that classifications are accurate and a system to recognise uncertainty surrounding epilepsy syndromes in individuals within trials.
Consideration is also required in the design of a trial regarding whether to blind participants and outcome assessors to treatment allocation. While an open‐label design is a more pragmatic and practical approach for large long‐term studies, when trials involve drugs with documented adverse event profiles, such as phenobarbitone, masking of treatment may be important to avoid preconceptions of the drug being more likely to be associated with serious adverse events, which the results of this review did not show.
The choice of outcomes at the design stage of a trial and the presentation of the results of outcomes, particularly of a time‐to‐event nature, require very careful consideration. While the majority of studies of a monotherapy design record an outcome measuring efficacy (seizure control) and an outcome measuring tolerability (adverse events), there is little uniformity between the definition of the outcomes and the reporting of the summary statistics related to the outcomes (Nolan 2013a), making an aggregate data approach to meta‐analysis in reviews of monotherapy studies impossible. Where trial authors cannot or will not make IPD available for analysis, we are left with no choice but to exclude a proportion of relevant evidence from the review, which will impact upon the interpretation of results of the review and applicability of the evidence and conclusions. The International League Against Epilepsy recommends that studies of a monotherapy design should adopt a primary effectiveness outcome of 'time to withdrawal of allocated treatment (retention time)' and should be of a duration of at least 48 weeks to allow for assessment of longer‐term outcomes, such as remission (ILAE 1998; ILAE 2006). If studies followed these recommendations, an aggregate data approach to meta‐analysis may be feasible, reducing the resources and time required from an IPD approach.
A network meta‐analysis has also been published (Tudur Smith 2007), comparing all direct and indirect evidence from phenobarbitone, carbamazepine, and other standard and new antiepileptic drugs licensed for monotherapy. This review and the network meta‐analysis will be updated as more information becomes available; however, we acknowledge that as phenobarbitone is no longer considered to be a first‐line agent for newly diagnosed individuals, in favour of newer agents, such as lamotrigine and levetiracetam, it is unlikely that a substantial amount of new evidence will become available for this review.
Acknowledgements
This review was supported by the National Institute for Health Research (NIHR), via Cochrane Programme Grant funding to the Epilepsy Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service (NHS) or the Department of Health.
We are greatly indebted to all of the original trialists that provided IPD and input into this review. We are grateful to the Cochrane Epilepsy Group Trials Search Co‐ordinator, Graham Chan, for performing all electronic searches, and Giacomo Frosi for translation of the Italian study.
We acknowledge Paula Williamson for contributions to the original review.
Appendices
Appendix 1. Cochrane Epilepsy Group Specialized Register search strategy
#1 MeSH DESCRIPTOR Carbamazepine Explode All
#2 Carbamazepine OR Carbamezepine OR CBZ OR SPD417 OR Apo‐Carbamazepine OR Atretol OR Biston OR Calepsin OR Carbagen OR Carbamazepen OR Carbatrol OR Carbazepine OR Carbelan OR Epitol OR Equetro OR Finlepsin OR Karbamazepin OR Lexin OR Neurotol OR Novo‐Carbamaz OR Nu‐Carbamazepine OR Sirtal OR Stazepin OR Stazepine OR Taro‐Carbamazepine OR Tegretal OR Tegretol OR Telesmin OR Teril OR Timonil
#3 #1 OR #2
#4 MeSH DESCRIPTOR Phenobarbital Explode All
#5 Phenobarbital OR Fenobarbital OR Phenobarbitol OR Phenobarbitone OR "Phenobarbituric Acid" OR Phenylethylbarbiturate OR "Phenylethylbarbituric Acid" OR Phenylethylmalonylurea OR Adonal OR Aephenal OR Agrypnal OR Amylofene OR Aphenylbarbit OR Aphenyletten OR Barbenyl OR Barbinal OR Barbiphen OR Barbiphenyl OR Barbipil OR Barbita OR Barbivis OR Barbonal OR Barbophen OR Bardorm OR Bartol OR Bialminal OR Blu‐Phen OR Cabronal OR Calmetten OR Calminal OR Cardenal OR Chinoin OR Codibarbita OR Coronaletta OR Cratecil OR Damoral OR Dezibarbitur OR Dormina OR Dormiral OR Dormital OR Doscalun OR Duneryl OR Ensobarb OR Ensodorm OR Epanal OR Epidorm OR Epilol OR Episedal OR Epsylone OR Eskabarb OR Etilfen OR Euneryl OR Fenbital OR Fenemal OR Fenosed OR Fenylettae OR Gardenal OR Gardepanyl OR Glysoletten OR Haplopan OR Haplos OR Helional OR Hennoletten OR Henotal OR Hypnaletten OR Hypnette OR Hypno‐Tablinetten OR Hypnogen OR Hypnolone OR Hypnoltol OR Hysteps OR Lefebar OR Leonal OR Lephebar OR Lepinal OR Lepinaletten OR Linasen OR Liquital OR Lixophen OR Lubergal OR Lubrokal OR Lumen OR Lumesettes OR Lumesyn OR Luminal OR Lumofridetten OR Luphenil OR Luramin OR Molinal OR Neurobarb OR Nirvonal OR Noptil OR Nova‐Pheno OR Nunol OR Parkotal OR Pharmetten OR Phen‐Bar OR Phenaemal OR Phenemal OR Phenemalum OR Phenobal OR Phenobarbyl OR Phenoluric OR Phenolurio OR Phenomet OR Phenonyl OR Phenoturic OR Phenyletten OR Phenyral OR Phob OR Polcominal OR Prominal OR Promptonal OR Seda‐Tablinen OR Sedabar OR Sedicat OR Sedizorin OR Sedlyn OR Sedofen OR Sedonal OR Sedonettes OR Sevenal OR Sinoratox OR Solfoton OR Solu‐Barb OR Sombutol OR Somnolens OR Somnoletten OR Somnosan OR Somonal OR Spasepilin OR Starifen OR Starilettae OR Stental OR Talpheno OR Teolaxin OR Teoloxin OR Thenobarbital OR Theoloxin OR Triabarb OR Tridezibarbitur OR Triphenatol OR Versomnal OR Zadoletten OR Zadonal OR PB
#6 #4 OR #5
#7 ((adjunct* or "add‐on" or "add on" or adjuvant* or combination* or polytherap*) not (monotherap* or alone or singl*)):TI
#8 (#3 AND #6 AND INREGISTER) NOT #7
Appendix 2. CENTRAL via CRSO search strategy
#1 MESH DESCRIPTOR Carbamazepine EXPLODE ALL TREES
#2 biston OR carbamazepin OR carbamazepina OR carbamazepine OR carbamazepinee OR carbamazepines OR carbamazepinesr OR carbamazepinetreated OR carbatrol OR cbz OR epitol OR equetro OR neurotop OR tegretol OR teril OR timonil
#3 #1 OR #2
#4 MESH DESCRIPTOR Phenobarbital EXPLODE ALL TREES
#5 luminal OR phenobarbital OR phenobarbitalprophylaxe OR phenobarbitals OR phenobarbitol OR phenobarbitone
#6 #4 OR #5
#7 (epilep* OR seizure* OR convuls*):TI,AB,KY
#8 MESH DESCRIPTOR Epilepsy EXPLODE ALL TREES
#9 MESH DESCRIPTOR Seizures EXPLODE ALL TREES
#10 #7 OR #8 OR #9
#11 #3 AND #6 AND #10
#12 ((adjunct* OR "add‐on" OR "add on" OR adjuvant* OR combination* OR polytherap*) NOT (monotherap* or alone or singl*)):TI
#13 #11 NOT #12
#14 ("Conference Abstract"):PT AND INEMBASE
#15 #13 NOT #14
Appendix 3. MEDLINE search strategy
The following search strategy is based on the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE (Lefebvre 2011).
1. exp Carbamazepine/
2. (Carbam?zepine or CBZ or SPD417 or Apo‐Carbamazepine or Atretol or Biston or Calepsin or Carbagen or Carbamazepen or Carbatrol or Carbazepine or Carbelan or Epitol or Equetro or Finlepsin or Karbamazepin or Lexin or Neurotol or Novo‐Carbamaz or Nu‐Carbamazepine or Sirtal or Stazepin or Stazepine or Taro‐Carbamazepine or Tegretal or Tegretol or Telesmin or Teril or Timonil).tw.
3. 1 or 2
4. exp Phenobarbital/
5. (Fenobarbital or Phenobarbit?l or Phenobarbitone or "Phenobarbituric Acid" or Phenylethylbarbiturate or "Phenylethylbarbituric Acid" or Phenylethylmalonylurea or Adonal or Aephenal or Agrypnal or Amylofene or Aphenylbarbit or Aphenyletten or Barbenyl or Barbinal or Barbiphen or Barbiphenyl or Barbipil or Barbita or Barbivis or Barbonal or Barbophen or Bardorm or Bartol or Bialminal or Blu‐Phen or Cabronal or Calmetten or Calminal or Cardenal or Chinoin or Codibarbita or Coronaletta or Cratecil or Damoral or Dezibarbitur or Dormina or Dormiral or Dormital or Doscalun or Duneryl or Ensobarb or Ensodorm or Epanal or Epidorm or Epilol or Episedal or Epsylone or Eskabarb or Etilfen or Euneryl or Fenbital or Fenemal or Fenosed or Fenylettae or Gardenal or Gardepanyl or Glysoletten or Haplopan or Haplos or Helional or Hennoletten or Henotal or Hypnaletten or Hypnette or Hypno‐Tablinetten or Hypnogen or Hypnolone or Hypnoltol or Hysteps or Lefebar or Leonal or Lephebar or Lepinal or Lepinaletten or Linasen or Liquital or Lixophen or Lubergal or Lubrokal or Lumen or Lumesettes or Lumesyn or Luminal or Lumofridetten or Luphenil or Luramin or Molinal or Neurobarb or Nirvonal or Noptil or Nova‐Pheno or Nunol or Parkotal or Pharmetten or Phen‐Bar or Phenaemal or Phenemal or Phenemalum or Phenobal or Phenobarbyl or Phenoluric or Phenolurio or Phenomet or Phenonyl or Phenoturic or Phenyletten or Phenyral or Phob or Polcominal or Prominal or Promptonal or Seda‐Tablinen or Sedabar or Sedicat or Sedizorin or Sedlyn or Sedofen or Sedonal or Sedonettes or Sevenal or Sinoratox or Solfoton or Solu‐Barb or Sombutol or Somnolens or Somnoletten or Somnosan or Somonal or Spasepilin or Starifen or Starilettae or Stental or Talpheno or Teolaxin or Teoloxin or Thenobarbital or Theoloxin or Triabarb or Tridezibarbitur or Triphenatol or Versomnal or Zadoletten or Zadonal or PB).tw.
6. 4 or 5
7. exp Epilepsy/
8. exp Seizures/
9. (epilep$ or seizure$ or convuls$).tw.
10. 7 or 8 or 9
11. exp Pre‐Eclampsia/ or exp Eclampsia/
12. 10 not 11
13. (randomized controlled trial or controlled clinical trial or pragmatic clinical trial).pt. or (randomi?ed or placebo or randomly).ab.
14. clinical trials as topic.sh.
15. trial.ti.
16. 13 or 14 or 15
17. exp animals/ not humans.sh.
18. 16 not 17
19. 3 and 6 and 12 and 18
20. ((adjunct$ or "add‐on" or "add on" or adjuvant$ or combination$ or polytherap$) not (monotherap$ or alone or singl$)).ti.
21. 19 not 20
22. remove duplicates from 21
Earlier versions of this review used the following search strategy.
1. randomized controlled trial.pt.
2. controlled clinical trial.pt.
3. exp Randomized Controlled Trials/
4. exp Random Allocation/
5. exp Double‐Blind Method/
6. exp Single‐Blind Method/
7. clinical trial.pt.
8. exp Clinical Trials/
9. (clin$ adj trial$).ab,ti.
10. ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).ab,ti.
11. exp PLACEBOS/
12. placebo$.ab,ti.
13. random$.ab,ti.
14. exp Research Design/
15. or/1‐14
16. (animals not humans).sh.
17. 15 not 16
18. phenobarbit$.tw. or exp Phenobarbital/
19. carbamazepin$.tw.
20. exp Carbamazepine/
21. 18 and (19 or 20)
22. (epilep$ or seizure$ or convulsion$).tw.
23. exp Epilepsy/
24. exp Seizures/
25. 22 or 23 or 24
26. 21 and 25
27. 26 and 17
Appendix 4. Scopus search strategy
(((TITLE(carbamazepine OR carbamezepine OR cbz OR spd417 OR apo‐carbamazepine OR atretol OR biston OR calepsin OR carbagen OR carbamazepen OR carbatrol OR carbazepine OR carbelan OR epitol OR equetro OR finlepsin OR karbamazepin OR lexin OR neurotol OR novo‐carbamaz OR nu‐carbamazepine OR sirtal OR stazepin OR stazepine OR taro‐carbamazepine OR tegretal OR tegretol OR telesmin OR teril OR timonil)) OR (ABS(carbamazepine OR carbamezepine OR cbz OR spd417 OR apo‐carbamazepine OR atretol OR biston OR calepsin OR carbagen OR carbamazepen OR carbatrol OR carbazepine OR carbelan OR epitol OR equetro OR finlepsin OR karbamazepin OR lexin OR neurotol OR novo‐carbamaz OR nu‐carbamazepine OR sirtal OR stazepin OR stazepine OR taro‐carbamazepine OR tegretal OR tegretol OR telesmin OR teril OR timonil))) AND ((TITLE(phenobarbital OR fenobarbital OR phenobarbitol OR phenobarbitone OR "Phenobarbituric Acid" OR phenylethylbarbiturate OR "Phenylethylbarbituric Acid" OR phenylethylmalonylurea OR adonal OR aephenal OR agrypnal OR amylofene OR aphenylbarbit OR aphenyletten OR barbenyl OR barbinal OR barbiphen OR barbiphenyl OR barbipil OR barbita OR barbivis OR barbonal OR barbophen OR bardorm OR bartol OR bialminal OR blu‐phen OR cabronal OR calmetten OR calminal OR cardenal OR chinoin OR codibarbita OR coronaletta OR cratecil OR damoral OR dezibarbitur OR dormina OR dormiral OR dormital OR doscalun OR duneryl OR ensobarb OR ensodorm OR epanal OR epidorm OR epilol OR episedal OR epsylone OR eskabarb OR etilfen OR euneryl OR fenbital OR fenemal OR fenosed OR fenylettae OR gardenal OR gardepanyl OR glysoletten OR haplopan OR haplos OR helional OR hennoletten OR henotal OR hypnaletten OR hypnette OR hypno‐tablinetten OR hypnogen OR hypnolone OR hypnoltol OR hysteps OR lefebar OR leonal OR lephebar OR lepinal OR lepinaletten OR linasen OR liquital OR lixophen OR lubergal OR lubrokal OR lumen OR lumesettes OR lumesyn OR luminal OR lumofridetten OR luphenil OR luramin OR molinal OR neurobarb OR nirvonal OR noptil OR nova‐pheno OR nunol OR parkotal OR pharmetten OR phen‐bar OR phenaemal OR phenemal OR phenemalum OR phenobal OR phenobarbyl OR phenoluric OR phenolurio OR phenomet OR phenonyl OR phenoturic OR phenyletten OR phenyral OR phob OR polcominal OR prominal OR promptonal OR seda‐tablinen OR sedabar OR sedicat OR sedizorin OR sedlyn OR sedofen OR sedonal OR sedonettes OR sevenal OR sinoratox OR solfoton OR solu‐barb OR sombutol OR somnolens OR somnoletten OR somnosan OR somonal OR spasepilin OR starifen OR starilettae OR stental OR talpheno OR teolaxin OR teoloxin OR thenobarbital OR theoloxin OR triabarb OR tridezibarbitur OR triphenatol OR versomnal OR zadoletten OR zadonal OR pb)) OR (ABS(phenobarbital OR fenobarbital OR phenobarbitol OR phenobarbitone OR "Phenobarbituric Acid" OR phenylethylbarbiturate OR "Phenylethylbarbituric Acid" OR phenylethylmalonylurea OR adonal OR aephenal OR agrypnal OR amylofene OR aphenylbarbit OR aphenyletten OR barbenyl OR barbinal OR barbiphen OR barbiphenyl OR barbipil OR barbita OR barbivis OR barbonal OR barbophen OR bardorm OR bartol OR bialminal OR blu‐phen OR cabronal OR calmetten OR calminal OR cardenal OR chinoin OR codibarbita OR coronaletta OR cratecil OR damoral OR dezibarbitur OR dormina OR dormiral OR dormital OR doscalun OR duneryl OR ensobarb OR ensodorm OR epanal OR epidorm OR epilol OR episedal OR epsylone OR eskabarb OR etilfen OR euneryl OR fenbital OR fenemal OR fenosed OR fenylettae OR gardenal OR gardepanyl OR glysoletten OR haplopan OR haplos OR helional OR hennoletten OR henotal OR hypnaletten OR hypnette OR hypno‐tablinetten OR hypnogen OR hypnolone OR hypnoltol OR hysteps OR lefebar OR leonal OR lephebar OR lepinal OR lepinaletten OR linasen OR liquital OR lixophen OR lubergal OR lubrokal OR lumen OR lumesettes OR lumesyn OR luminal OR lumofridetten OR luphenil OR luramin OR molinal OR neurobarb OR nirvonal OR noptil OR nova‐pheno OR nunol OR parkotal OR pharmetten OR phen‐bar OR phenaemal OR phenemal OR phenemalum OR phenobal OR phenobarbyl OR phenoluric OR phenolurio OR phenomet OR phenonyl OR phenoturic OR phenyletten OR phenyral OR phob OR polcominal OR prominal OR promptonal OR seda‐tablinen OR sedabar OR sedicat OR sedizorin OR sedlyn OR sedofen OR sedonal OR sedonettes OR sevenal OR sinoratox OR solfoton OR solu‐barb OR sombutol OR somnolens OR somnoletten OR somnosan OR somonal OR spasepilin OR starifen OR starilettae OR stental OR talpheno OR teolaxin OR teoloxin OR thenobarbital OR theoloxin OR triabarb OR tridezibarbitur OR triphenatol OR versomnal OR zadoletten OR zadonal OR pb))) AND ((TITLE‐ABS‐KEY(epilep* OR "infantile spasm" OR seizure OR convuls* OR (syndrome W/2 (aicardi OR angelman OR doose OR dravet OR janz OR jeavons OR "landau kleffner" OR "lennox gastaut" OR ohtahara OR panayiotopoulos OR rasmussen OR rett OR "sturge weber" OR tassinari OR "unverricht lundborg" OR west)) OR "ring chromosome 20" OR "R20" OR "myoclonic encephalopathy" OR "pyridoxine dependency") AND NOT (TITLE(*eclampsia) OR INDEXTERMS(*eclampsia))) OR (TITLE‐ABS‐KEY(lafora* W/4 (disease OR epilep*)) AND NOT (TITLE(dog OR canine) OR INDEXTERMS(dog OR canine)))) AND (TITLE((randomiz* OR randomis* OR controlled OR placebo OR blind* OR unblind* OR "parallel group" OR crossover OR "cross over" OR cluster OR "head to head") PRE/2 (trial OR method OR procedure OR study)) OR ABS((randomiz* OR randomis* OR controlled OR placebo OR blind* OR unblind* OR "parallel group" OR crossover OR "cross over" OR cluster OR "head to head") PRE/2 (trial OR method OR procedure OR study)))) AND NOT (TITLE((adjunct* OR "add‐on" OR "add on" OR adjuvant* OR combination* OR polytherap*) AND NOT (monotherap* OR alone OR singl*)))
Data and analyses
Comparison 1.
Carbamazepine versus phenobarbitone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to withdrawal of allocated treatment | 4 | 676 | Hazard Ratio (Fixed, 95% CI) | 1.49 [1.15, 1.94] |
| 2 Time to withdrawal of allocated treatment ‐ stratified by epilepsy type | 4 | 676 | Hazard Ratio (Fixed, 95% CI) | 1.50 [1.15, 1.95] |
| 2.1 Generalised onset | 3 | 156 | Hazard Ratio (Fixed, 95% CI) | 1.53 [0.81, 2.88] |
| 2.2 Partial onset | 4 | 520 | Hazard Ratio (Fixed, 95% CI) | 1.49 [1.12, 2.00] |
| 3 Time to 12‐month remission | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 0.93 [0.72, 1.19] |
| 4 Time to 12‐month remission ‐ stratified by epilepsy type | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 0.93 [0.72, 1.20] |
| 4.1 Generalised onset | 3 | 158 | Hazard Ratio (Fixed, 95% CI) | 0.64 [0.41, 1.01] |
| 4.2 Partial onset | 4 | 525 | Hazard Ratio (Fixed, 95% CI) | 1.11 [0.81, 1.51] |
| 5 Time to six‐month remission | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 1.02 [0.83, 1.26] |
| 6 Time to six‐month remission ‐ stratified by epilepsy type | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 0.99 [0.80, 1.23] |
| 6.1 Generalised onset | 3 | 158 | Hazard Ratio (Fixed, 95% CI) | 0.69 [0.47, 1.01] |
| 6.2 Partial onset | 4 | 525 | Hazard Ratio (Fixed, 95% CI) | 1.17 [0.90, 1.50] |
| 7 Time to first seizure | 6 | 822 | Hazard Ratio (Fixed, 95% CI) | 0.86 [0.71, 1.04] |
| 8 Time to first seizure ‐ stratified by epilepsy type | 6 | 822 | Hazard Ratio (Fixed, 95% CI) | 0.87 [0.72, 1.06] |
| 8.1 Generalised onset | 5 | 238 | Hazard Ratio (Fixed, 95% CI) | 1.23 [0.86, 1.77] |
| 8.2 Partial onset | 6 | 584 | Hazard Ratio (Fixed, 95% CI) | 0.76 [0.60, 0.96] |
| 9 Time to first seizure ‐ sensitivity analysis | 6 | 822 | Hazard Ratio (Fixed, 95% CI) | 0.89 [0.73, 1.09] |
| 9.1 Generalised onset | 5 | 173 | Hazard Ratio (Fixed, 95% CI) | 1.39 [0.90, 2.13] |
| 9.2 Partial onset | 6 | 584 | Hazard Ratio (Fixed, 95% CI) | 0.76 [0.60, 0.96] |
| 9.3 Uncertain seizure type | 3 | 65 | Hazard Ratio (Fixed, 95% CI) | 1.22 [0.59, 2.51] |
What's new
Last assessed as up‐to‐date: 18 August 2016.
| Date | Event | Description |
|---|---|---|
| 26 April 2017 | Amended | Declarations of interest section updated. |
History
Protocol first published: Issue 1, 2000 Review first published: Issue 1, 2003
| Date | Event | Description |
|---|---|---|
| 18 August 2016 | New search has been performed | Searches updated 18 August 2016; no new studies identified. |
| 18 August 2016 | New citation required but conclusions have not changed | Conclusions are unchanged. |
| 22 September 2014 | New search has been performed | Searches updated 22 September 2014. |
| 22 September 2014 | New citation required but conclusions have not changed | Four new included studies. Conclusions remain unchanged. |
| 12 August 2009 | Amended | Copyedits made at editorial base. |
| 24 September 2008 | Amended | Converted to new review format. |
| 1 October 2006 | New search has been performed | We re‐ran our searches on 1st October 2006; no new studies were identified. |
Differences between protocol and review
December 2014: The title was changed to specify that the review uses individual participant data (IPD).
Update 2015: We added sensitivity analyses following the discovery of inconsistencies between IPD provided and published papers. The existence of such inconsistencies could not have been known at the time of writing the original protocol.
Update 2015: We added the outcomes 'time to six‐month remission' and 'adverse events' for consistency with the other reviews in the series of Cochrane IPD reviews investigating pair‐wise monotherapy comparisons.
Update 2016: We added 'Summary of findings' tables to the update in 2015 and added text in the Methods section for 'Summary of findings' tables in August 2016.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Single‐centre, double‐blind randomised controlled trial of participants recruited from clinical referral to a multidisciplinary child development centre at a children's hospital in Dhaka, Bangladesh 2 treatment arms: CBZ and PB |
|
| Participants | 108 children between the ages of 2 to 15 with 2 or more generalised tonic‐clonic, partial, or secondarily generalised seizures in the previous year Number randomised: CBZ = 54, PB = 54 61 male children (56%) 59 with partial seizures (55%) 26 had previous AED treatment (24%) Mean age (range): 6 (2 to 15 years) Study duration: 12 months Range of follow‐up: 0 to 20.5 months |
|
| Interventions | Monotherapy with CBZ (immediate release) or PB Starting daily dose: CBZ = 1.5 mg/kg/day, PB = 5 mg/kg/day Maximum daily dose: CBZ = 4 mg/kg/day, PB = 16 mg/kg/day |
|
| Outcomes |
|
|
| Notes | We received IPD for all randomised participants. We received reasons for withdrawal of allocated treatment as well as the date of the last follow‐up visit, but withdrawal of allocated treatment did not always coincide with the date of the last follow‐up visit (i.e. several participants had the allocated treatment substituted for the other trial drug and continued to be followed up). Dates of withdrawal of allocated treatment could not be provided; therefore, we could not calculate 'time to withdrawal of allocated treatment'. We received the date of first seizure after randomisation, but dates of other seizures in the follow‐up time could not be provided; therefore, we calculated 'time to first seizure' for all participants, but we could not calculate the time to six‐ and 12‐month remission. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were 'randomly assigned to treatment'; the method of randomisation was not stated and not provided by the authors. |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed by sealed envelopes prepared on a different site to the site of recruitment of participants. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, a psychologist, and a therapist were blinded throughout the trial. The treating physician was unblinded for practical and ethical reasons. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | A researcher performing outcome assessment was blinded throughout the trial but unblinded for analysis. It was unclear if this could have influenced the results. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates were reported. We analysed all randomised participants from the IPD provided². |
| Selective reporting (reporting bias) | Low risk | We calculated 1 outcome for this review from the IPD provided². We could not calculate other outcomes for this review as the appropriate data were not recorded/not available. All cognitive outcomes from the study were well reported. |
| Other bias | High risk | There were inconsistencies between rates of seizure recurrence between the data provided and the published paper, which the authors could not resolve (see Sensitivity analysis). |
| Methods | Six‐month, systematic, simple randomised trial of children referred to a child neurology clinic (the author was from Guilan University of Medical Sciences, Iran, so it was likely that the study was also conducted there) 2‐arm trial: CBZ and PB |
|
| Participants | Children aged 2 to 12 years with partial seizures with secondary generalisation Number randomised: CBZ = 36, PB = 35 36 male children (53%) 100% partial seizures, the per cent newly diagnosed was not stated Age range: 2 to 12 years Study duration: 6 months Mean follow‐up: not stated |
|
| Interventions | Monotherapy with PB or CBZ. Doses started or achieved not stated | |
| Outcomes |
|
|
| Notes | The trial was reported in abstract form only with very limited information. Outcomes chosen for this review were not reported; IPD were not available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial was described as a 'systematic simple randomised study'; no further information was provided. |
| Allocation concealment (selection bias) | Unclear risk | No information was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information was provided on blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information was provided on blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No attrition rates were reported; it was unclear if all participants were analysed. |
| Selective reporting (reporting bias) | Unclear risk | There was no protocol available; the study was available in abstract format only. Outcomes for this review were not available. |
| Other bias | Low risk | We detected no other bias. |
| Methods | Randomised, double‐blind cross‐over trial with 3, 21‐day treatment periods and a 2‐week washout period (regular medications used) 3 treatment arms: CBZ, phenytoin, and PB |
|
| Participants | Institutionalised adult participants with uncontrolled seizures on current medication Number randomised: PB = 45, CBZ = 45 41 participants (91%) with partial epilepsy 28 (62%) male participants Age range: 18 to 51 years Study duration: 13 weeks (3 x 21‐day treatment periods plus 2 x 2‐week washout periods) |
|
| Interventions | Monotherapy with PB or CBZ Daily dose: PB = 300 mg/day or CBZ = 1200 mg/day | |
| Outcomes |
|
|
| Notes | The outcomes chosen for this review were not reported due to the cross‐over design of the trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation of groups from random number tables (confirmed by author). |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided on blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided on blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawal rates reported, no further information provided. |
| Selective reporting (reporting bias) | Low risk | All efficacy and tolerability outcomes specified in the methods sections reported well in the results section. No protocol available, outcomes for this review not available due to trial cross‐over design. |
| Other bias | High risk | Cross‐over design may not be appropriate for monotherapy designs, likely carryover effects from one period to another so the comparison may not be entirely monotherapy. |
| Methods | Randomised, parallel group study conducted in Taiwan 3 treatment arms: CBZ, PB, sodium valproate |
|
| Participants | Children with 2 or more previously untreated unprovoked epileptic seizures Number randomised: PB = 25, CBZ = 26; number analysed: PB = 23, CBZ = 25 (see notes) Mean age (range): PB = 9.9 (7 to 15 years), CBZ = 10.8 (7 to 15 years) CBZ versus PB: 26 (54%) participants with partial epilepsy 25 (52%) male participants Study duration: 12 months Range of follow‐up: not stated |
|
| Interventions | Monotherapy with PB or CBZ. Dose started or achieved not stated | |
| Outcomes |
|
|
| Notes | 2 children from the PB group and 1 child from the CBZ group withdrew from the study because of allergic reactions. Published results were presented for children who completed the study only. Outcomes chosen for this review were not reported; IPD were not available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were allocated with "simple randomisation of block size 3." |
| Allocation concealment (selection bias) | Unclear risk | No information was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The cognitive assessor was 'single‐blinded', implying that participants and personnel were unblinded, but no further information was provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The cognitive assessor was single‐blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawal rates were reported; results were presented only for those who completed the study (CBZ versus PB: 3/51 (6%) excluded from analysis). An ITT approach was not taken. |
| Selective reporting (reporting bias) | Low risk | All cognitive, efficacy, and tolerability outcomes specified in the methods sections were reported well in the results section. No protocol was available. Outcomes chosen for this review were not reported. |
| Other bias | Low risk | We detected no other bias |
| Methods | Randomised, double‐blind study to assess short‐term therapy of CBZ and PB on cognitive and memory function conducted in Italy 3 treatment arms: CBZ, PB, and placebo | |
| Participants | Participants with newly diagnosed and untreated temporal lobe epilepsy with no seizures in the previous month Number randomised: CBZ = 6, PB = 6 100% partial (temporal lobe epilepsy), 100% newly diagnosed Mean age (SD): CBZ = 26.33 (9.73) years, PB = 18.5 (2.56) years Age range: 15 to 45 years 1 male and 5 females in each group Study duration: 3 weeks; all participants completed in 3 weeks |
|
| Interventions | Monotherapy with CBZ or PB, Dose started and achieved not stated | |
| Outcomes |
|
|
| Notes | The trial was published in Italian; the characteristics and outcomes were translated. Outcomes chosen for this review were not reported; IPD were not available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial was described as randomised ('randomizzazione' in Italian); no further information was available. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial is described as double‐blind ('condizioni di doppia cecità' in Italian), we assume this refers to participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided on blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed this short study and contribute to analysis. |
| Selective reporting (reporting bias) | Unclear risk | Cognitive and memory outcomes described in methods section well reported in results section. No seizure outcomes or adverse events reported and outcomes chosen for this review not reported. No protocol available so unclear if seizure outcomes were planned a priori. |
| Other bias | High risk | Very small participant numbers and very short‐term follow‐up. Unclear if this study was adequately powered and of sufficient duration to detect differences. |
| Methods | 36‐month randomised comparative study 4 treatment arms: CBZ, sodium valproate, phenytoin, PB |
|
| Participants | Adults with newly diagnosed epilepsy with partial complex seizures Number randomised: PB = 30, CBZ = 30 100% partial epilepsy (partial complex seizures) Age range: 18 to 40 years Percentage male and range of follow‐up: not mentioned |
|
| Interventions | Monotherapy with PB or CBZ Starting doses CBZ = 400 mg/day, PB = 100 mg/day. Dose achieved not stated |
|
| Outcomes |
|
|
| Notes | This was an abstract only. Outcomes chosen for this review were not reported. IPD were pledged but not received. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study was randomised, but no further information was provided. |
| Allocation concealment (selection bias) | Unclear risk | No information was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information was provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information was provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Exclusion rates" were reported for all treatment groups; no further information was provided. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available; the study was available in abstract format only. Outcomes for this review were not available. |
| Other bias | Low risk | We detected no other bias. |
| Methods | Randomised, parallel group, open‐label paediatric study conducted in 2 centres in the UK 4 treatment arms: CBZ, sodium valproate, phenytoin, PB |
|
| Participants | Children with newly diagnosed epilepsy (2 or more untreated partial or generalised tonic‐clonic seizures in the 12 months preceding the study) Number randomised: PB = 10, CBZ = 54 (see notes) 35 children (55%) with partial epilepsy 34 (53%) male children Mean age (range): 9 (3 to 16) years Range of follow‐up: 3 to 88 (months) |
|
| Interventions | Monotherapy with PB or CBZ Median daily dose achieved: PB = not stated; CBZ = 400 mg/day |
|
| Outcomes |
|
|
| Notes | 6 of the first 10 children assigned to PB had unacceptable adverse effects, so no further children were assigned to PB. The 10 children randomised to PB were retained in analysis. We received IPD for all outcomes of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A randomisation list was generated using permuted blocks of size 8 or 16 with stratification for centre, seizure type, and presence of neurological signs. |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed via 4 batches of concealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded ‐ the authors stated that masking of treatment would not have been "practicable or ethical" and would have "undermine[d] compliance". Lack of masking could have led to early withdrawal of the PB arm from the trial. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded ‐ the authors stated masking of treatment would not have been "practicable or ethical" and would have "undermine[d] compliance". Lack of masking could have led to early withdrawal of the PB arm from the trial, which was likely to have influenced the overall results. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates were reported; we analysed all randomised participants from the IPD provided² |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported or calculated with the IPD provided² |
| Other bias | Low risk | We detected no other bias |
| Methods | Randomised parallel group trial conducted among residents of the Nakuru district, a semi‐urban population of rural Kenya 2 treatment arms: CBZ and PB |
|
| Participants | Participants had a history of generalised tonic‐clonic seizures and at least 2 generalised tonic‐clonic seizures within the preceding year (with or without other seizure types) and untreated in the 3 months prior to the study. 79 (26%) participants had been treated in the past with AEDs Number randomised: PB = 150, CBZ = 152 115 (38%) of participants had experienced partial seizures 173 (57%) male participants Mean age (range): 21 (6 to 65 years) Range of follow‐up: participants followed up for up to 1 year |
|
| Interventions | Monotherapy with CBZ or PB Starting doses: PB: 6 to 10 years of age: 30 mg/day, 11 to 15 years of age: 45 mg/day, 16+ years of age: 60 mg/day CBZ: 6 to 10 years of age: 400 mg/day, 11 to 15 years of age: 500 mg/day, 16+ years of age: 600 mg/day Dose achieved not stated |
|
| Outcomes |
|
|
| Notes | IPD were made available but not used because of inconsistencies and problems with the data provided (see Included studies for further details). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants randomised with random number list, no information provided on method of generating random list. |
| Allocation concealment (selection bias) | Low risk | Allocation concealed via sealed opaque envelopes (information provided by study author). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rates reported, results presented only for participants completing 12 months follow‐up (results not presented for 53 (17.5%) participants out of 302 who withdrew from treatment), approach is not ITT. |
| Selective reporting (reporting bias) | Low risk | No protocol available, outcomes chosen for this review not reported. Seizure outcomes and adverse events well reported. |
| Other bias | High risk | Inconsistencies with IPD and published results so IPD could not be used (see Included studies for further details). |
| Methods | Randomised, parallel group, open‐label study conducted in 2 centres in the UK 4 treatment arms: CBZ, sodium valproate, phenytoin, PB |
|
| Participants | Adults with newly diagnosed epilepsy (2 or more untreated partial or generalised tonic‐clonic seizures in the 12 months preceding the study) Number randomised: PB = 58, CBZ = 61 49 participants (41%) with partial epilepsy 55 (46%) male participants Mean age (range): 32 (13 to 77) years Range of follow‐up: 1 to 91 months |
|
| Interventions | Monotherapy with PB or CBZ. Median daily dose achieved: PB = 105 mg/day; CBZ = 600 mg/day | |
| Outcomes |
|
|
| Notes | We received IPD for all outcomes of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation list generated using permuted blocks of size 8 or 16 with stratification for centre, seizure type and presence of neurological signs. |
| Allocation concealment (selection bias) | Low risk | Allocation concealed via 4 batches of concealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded, authors state masking of treatment would not be “practical” and would have “introduced bias due to a very large dropout rate.” Lack of blinding may have lead to more withdrawals of PB. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded, authors state masking of treatment would not be “practical” and would have “introduced bias due to a very large dropout rate.” Lack of blinding may have lead to more withdrawals of PB which is likely to have influenced the overall results. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates reported, all randomised participants analyses from IPD provided² |
| Selective reporting (reporting bias) | Low risk | All outcomes reported or calculated with IPD provided² |
| Other bias | Low risk | No other bias detected |
| Methods | Multicentre, randomised, parallel group, double‐blinded study over 10 centres in the USA with separate randomisation schemes used for each seizure type 4 treatments: CBZ, phenytoin, PB, primidone |
|
| Participants | Adults with previously untreated or under‐treated simple or complex partial or secondary generalised tonic‐clonic seizures Number randomised: CBZ = 155, PB = 155 100% partial epilepsy 268 (88%) male participants Mean age (range): 41 (18 to 82) years Range of follow‐up: 1 to 177 months |
|
| Interventions | Monotherapy with PB or CBZ Median daily dose achieved: PB = 160 mg/day; CBZ = 800 mg/day |
|
| Outcomes |
|
|
| Notes | We received IPD for all outcomes of this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised with stratification for seizure type. The method of randomisation was not stated and not provided by the authors. |
| Allocation concealment (selection bias) | Unclear risk | No information was provided in the publication or by the study authors. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The trial was double‐blind (participants and personnel), which was achieved using an additional blank tablet. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear if outcome assessment was blinded; no information was provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates were reported; we analysed all randomised participants from the IPD provided². |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported or calculated with the IPD provided². |
| Other bias | Unclear risk | We detected no other bias. |
| Methods | Randomised, double‐blind, single‐centre, parallel paediatric study conducted in Los Angeles, USA 2 treatment arms: CBZ and PB |
|
| Participants | Children with newly diagnosed epilepsy Number randomised: PB = 18, CBZ = 15 100% partial epilepsy, 100% newly diagnosed 20 (61%) male children Mean age (range): PB = 7.89 (2 to 12 years), CBZ = 6.07 (2 to 12 years) Study duration: 12 months Range of follow‐up: not reported |
|
| Interventions | Monotherapy with PB or CBZ. Doses started and achieved not stated | |
| Outcomes |
|
|
| Notes | 33 participants were randomised to PB (18) and CBZ (15) in this study; 6 children were enrolled into a six‐month pilot study (PB (4) CBZ (2)) prior to the randomised study. The 6 children were included in six‐month follow‐up psychometric data. Outcomes for this review were not reported; IPD were not available. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 33 children were "randomised using a scheme that balanced drug distribution by age and sex"; no further details were provided on the randomisation scheme. 6 non‐randomised children were also used in some analyses. |
| Allocation concealment (selection bias) | Unclear risk | No information was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The trial blinded participants (and parents); clinicians were unblinded for clinical follow‐up. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The trial blinded psychometric (cognitive) testers blinded for clinical follow‐up. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates were reported; results were reported for all children who completed each stage of follow‐up. |
| Selective reporting (reporting bias) | Low risk | Cognitive/behavioural outcomes, seizure control outcomes, and adverse events were all well reported. No protocol was available; outcomes for this review were not reported. |
| Other bias | High risk | There was evidence that the study may have been underpowered to detect differences (e.g. 55% power to find a 5‐point difference in IQ score). The behavioural questionnaire was not fully validated. Non‐randomised children from a pilot study were included in the results for psychometric outcomes and medical outcomes. |
| Methods | Double‐blinded, parallel group, randomised study conducted in a single‐centre in Nigeria. 3 treatment arms: carbamazepine, phenytoin, phenobarbitone | |
| Participants | Consectuive newly diagnosed participants aged 14 or over presenting at the outpatient neurology clinic of the University Teaching Hopsital, Benin City, Nigeria, with recurrent, untreated afebrile seizures Number randomised: PB = 18, CBZ = 19 7 participants with partial seizures (19%) 22 male participants (59%) Mean age (range): 23.62 years (14 to 38 years) Range of follow‐up: all participants followed up for 12 weeks |
|
| Interventions | Monotherapy with PB or CBZ. Median daily dose (range): PB = 120 mg (60 to 180 mg), CBZ = 600 mg (400 mg to 1200 mg) | |
| Outcomes |
|
|
| Notes | We received IPD for all randomised participants. The study duration was 12 weeks; all participants completed the study without withdrawing; therefore, we could not calculate the outcomes 'time to withdrawal of allocated drug', 'time to six‐month remission', and 'time to 12‐month remission'. We calculated 'time to first seizure' from the IPD provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study randomised participants using simple randomisation: Each participant was asked to pick 1 from a table of numbers (1 to 60); the numbers corresponded to allocation of 1 of 3 drugs (the author provided information). |
| Allocation concealment (selection bias) | Low risk | Recruitment/randomisation of participants and allocations of treatments took place on different sites (the author provided information). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were single‐blinded. The study did not blind the research assistant recruiting participants and counselling on medication adherence. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Investigators performing cognitive assessments were single‐blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants completed the study. We analysed all randomised participants from the IPD provided². |
| Selective reporting (reporting bias) | Low risk | We calculated 1 outcome for this review from the IPD provided². Other outcomes for this review were not available because of short study length. All cognitive outcomes from the study were well reported. |
| Other bias | Low risk | We detected no other bias. |
| Methods | Randomised parallel group study conducted in the context of existing community health care in a rural highland area of a developing country (Ecuador) | |
| Participants | Participants with a history of at least 2 afebrile seizures and no previous AED treatment in the 4 weeks preceding the study were eligible Number randomised: PB = 97, CBZ = 95 133 participants (69%) with partial epilepsy 67 (35%) male participants Mean age (range): PB = 28.6 (2 to 68 years), CBZ = 29.2 (2 to 68 years) Study duration: 12 months Range of follow‐up: 0 to 53.4 months |
|
| Interventions | Monotherapy with PB or CBZ. Minimum maintenance doses by age groups: 2 to 5 years: PB: 15 mg/day, CBZ: 150 mg/day; 6 to 10 years: PB: 30 mg/day, CBZ: 300 mg/day; 11 to 15 years: PB: 45 mg/day, CBZ: 500 mg/day; > 16 PB: 60 mg/day, CBZ: 600 mg/day. Doses gradually increased Doses achieved not stated |
|
| Outcomes |
|
|
| Notes | We received IPD for all outcomes used in this review. Results in the published paper were given for 139 participants who completed 6 months' follow‐up, but we received IPD for all 192 participants randomised. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomised with random number list, no information provided on method of generating random list. |
| Allocation concealment (selection bias) | High risk | Allocation concealed used sealed opaque envelopes but method not used for all participants (information provided by study author). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates reported, all randomised participants analysed from IPD provided². |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported or calculated with the IPD provided². |
| Other bias | High risk | Inconsistencies between number and reasons of withdrawals between the data and the published paper which could not be resolved by the authors (see Sensitivity analysis). |
AED: antiepileptic drug CBZ: carbamazepine IPD: individual participant data IQ: intelligence quotient ITT: intention‐to‐treat PB: phenobarbitone WISC‐R scale: the Wechsler Intelligence Scale for Children
²For studies for which we received IPD (Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993), attrition and reporting bias were reduced as we requested attrition rates and unpublished outcome data.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bird 1966 | It was unclear whether this trial was randomised and whether participants received either CBZ or PB as monotherapy. |
| Castro‐Gago 1998 | The trial was not randomised, and the treatment choice was made based on types of seizures. |
| Cereghino 1973 | This was a preliminary analysis of Cereghino 1974. |
| Hansen 1980 | The trial was not randomised; participants were already on CBZ or PB monotherapy upon entry into the study. |
| Kuzuya 1993 | The trial was not randomised; participants were already on CBZ or PB monotherapy upon entry into the study. |
| Marjerrison 1968 | CBZ or PB therapy were added to current treatment. We could not make a comparison between CBZ monotherapy and PB monotherapy. |
| Meador 1990 | We could not make a comparison between CBZ monotherapy and PB monotherapy. This was a cross‐over trial, but some participants were receiving treatment at the start of the first period, which had to be withdrawn slowly. |
| Sabers 1995 | The trial was not fully randomised: "The treatment was chosen at random unless the individual diagnoses required a specific drug." |
| Smith 1987 | This reported the same trial as Mattson 1985, and Mattson 1985 gave more relevant information. |
CBZ: carbamazepine PB: phenobarbitone
Contributions of authors
SJ Nolan assessed studies for inclusion in the review update, assessed risk of bias in all included studies, performed analyses in SAS version 9.2, Stata version 11.2, and MetaView, added survival plots and a 'Summary of findings' table, and updated the text of the review under the supervision of C Tudur Smith and AG Marson.
C Tudur Smith was the lead investigator on the original review, assessed eligibility and methodological quality of original individual studies, organised and cleaned the IPD sets, performed data validation checks and statistical analyses, and co‐wrote the original review.
AG Marson obtained IPD from trial investigators, provided guidance with the clinical interpretation of results, assessed eligibility and methodological quality of individual studies, and co‐wrote the original review.
J Weston independently assessed risk of bias in all included studies.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute for Health Research, UK.
This review was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Epilepsy Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Sarah J Nolan: nothing to declare.
Anthony G Marson: A consortium of pharmaceutical companies (GSK, EISAI, UCB Pharma) funded the National Audit of Seizure Management in Hospitals (NASH) through grants paid to The University of Liverpool. Professor Tony Marson is Theme Leader for Managing Complex Needs at NIHR CLAHRC NWC.
Jennifer Weston: nothing to declare.
Catrin Tudur Smith: nothing to declare.
Edited (no change to conclusions)
References
References to studies included in this review
- Banu SH, Jahan M, Koli UK, Ferdousi S, Khan NZ, Neville B. Side effects of phenobarbital and carbamazepine in childhood epilepsy: randomised controlled trial. BMJ 2007;334(7605):1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidabadi E. Comparison of the effects of phenobarbital versus carbamazepine as single drug therapy in partial seizure with secondary generalization in children. Epilepsia 2009;50 Suppl 10:167. [Google Scholar]
- Cereghino JJ, Brock JT, Meter JC, Penry JK, Smith LD, White BG. Carbamazepine for epilepsy. A controlled prospective evaluation. Neurology 1974;24(5):401‐10. [DOI] [PubMed] [Google Scholar]
- Chen YJ, Kang WM, So WCM. Comparison of antiepileptic drugs on cognitive function in newly diagnosed epileptic children: a psychometric and neurophysiological study. Epilepsia 1996;37(1):81‐6. [DOI] [PubMed] [Google Scholar]
- Cossu G, Monaco F, Piras MR, Grossi E. Short‐term therapy with carbamazepine and phenobarbital: effects on cognitive functioning in temporal lobe epilepsy [Trattamento a breve termine con carbamazepina e fenobarbital: efftto sulle funzioni mnesiche nell'epilessia temporale]. Bollettino Lega Italiana contro l'Epilessia 1984;45/46:377‐9. [Google Scholar]
- Czapinski P, Terczynski A, Czapinska E. Randomised 36‐month comparative study of valproic acid, phenytoin, phenobarbital and carbamazepine efficacy in patients with newly diagnosed epilepsy with partial complex seizures. Epilepsia 1997;38 Suppl(3):42. [Google Scholar]
- Silva M, MacArdle B, McGowan M, Hughes E, Stewart J, Neville BG, et al. Randomised comparative monotherapy trial of phenobarbitone, phenytoin, carbamazepine, or sodium valproate for newly diagnosed childhood epilepsy. Lancet 1996;347(9003):709‐13. [DOI] [PubMed] [Google Scholar]
- Feksi AT, Kaamugisha J, Sander JW, Gatiti S, Shorvon SD. Comprehensive primary health care antiepileptic drug treatment programme in rural and semi‐urban Kenya. ICBERG (International Community‐based Epilepsy Research Group). Lancet 1991;337(16):406‐9. [DOI] [PubMed] [Google Scholar]
- Heller AJ, Chesterman P, Elwes RD, Crawford P, Chadwick D, Johnson AL, et al. Phenobarbitone, phenytoin, or sodium valproate for newly diagnosed epilepsy: a randomized comparative monotherapy trial. Journal of Neurology, Neurosurgery, and Psychiatry 1995;58(1):44‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson RH, Cramer JA, Collins JF, Smith DB, Delgado‐Escueta AV, Browne TR, et al. Comparison of carbamazepine, phenobarbital, phenytoin, and primidone in partial and secondarily generalized tonic‐clonic seizures. New England Journal of Medicine 1985;313(3):145‐51. [DOI] [PubMed] [Google Scholar]
- Mitchell WG, Chavez JM. Carbamazepine versus phenobarbital for partial onset seizures in children. Epilepsia 1987;28(1):56‐60. [DOI] [PubMed] [Google Scholar]
- Ogunrin O, Adamolekun B, Ogunniyi A. Cognitive effects of anti‐epileptic drugs in Nigerians with epilepsy. African Journal of Neurological Sciences 2005;24(1):18‐24. [Google Scholar]
- Placencia M, Sander JW, Shorvon SD, Roman M, Alarcon F, Bimos C, et al. Antiepileptic drug treatment in a community health care setting in northern Ecuador: a prospective 12‐month assessment. Epilepsy Research 1993;14(3):237‐44. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Bird CAK, Griffin BP, Miklaszewska JM, Galbraith AW. Tegretol (carbamazepine): a controlled trial of a new anti‐convulsant. British Journal of Psychiatry 1966;112:737‐42. [Google Scholar]
- Castro‐Gago M, Eiris‐Punal J, Novo‐Rodriguez MI, Couceiro J, Camina F, Rodriguez‐Segade S. Serum carnitine levels in epileptic children before and during treatment with valproic acid, carbamazepine, and phenobarbital. Journal of Child Neurology 1998;13(11):546‐9. [DOI] [PubMed] [Google Scholar]
- Cereghino JJ, Brock JT, White BG, Penry JK. Evaluation of carbamazepine in epileptic patients. Neurology 1973;23:433. [DOI] [PubMed] [Google Scholar]
- Hansen BS, Dam M, Brandt J, Hvidberg EF, Angelo H, Christensen JM, et al. Influence of dextropropoxyphene on steady state serum levels and protein binding of three anti‐epileptic drugs in man. Acta Neurologica Scandinavica 1980;61(6):357‐67. [DOI] [PubMed] [Google Scholar]
- Kuzuya T, Hasegawa T, Shimizu K, Nabeshima T. Effect of anti‐epileptic drugs on serum zinc and copper concentrations in epileptic patients. International Journal of Clinical Pharmacology, Therapy, & Toxicology 1993;31(2):61‐5. [PubMed] [Google Scholar]
- Marjerrison G, Jedlicki SM, Keogh RP, Hrychuk W, Poulakakis GM. Carbamazepine: behavioral, anticonvulsant and EEG effects in chronically‐hospitalized epileptics. Diseases of the Nervous System 1968;29(2):133‐6. [PubMed] [Google Scholar]
- Meador KJ, Loring DW, Huh K, Gallagher BB, King DW. Comparative cognitive effects of anticonvulsants. Neurology 1990;40:391‐4. [DOI] [PubMed] [Google Scholar]
- Sabers A, Moller A, Dam M, Smed A, Arlien‐Soborg P, Buchman J, et al. Cognitive function and anticonvulsant therapy: effect of monotherapy in epilepsy. Acta Neurologica Scandinavica 1995;92(1):19‐27. [DOI] [PubMed] [Google Scholar]
- Smith DB, Mattson RH, Cramer JA, Collins JF, Novelly RA, Craft B. Results of a nationwide Veterans Administration Cooperative Study comparing the efficacy and toxicity of carbamazepine, phenobarbital, phenytoin, and primidone. Epilepsia 1987;28(Suppl 3):S50‐8. [DOI] [PubMed] [Google Scholar]
Additional references
- Annegers JF, Dubinsky S, Coan SP, Newmark ME, Roht L. The incidence of epilepsy and unprovoked seizures in multiethnic, urban health maintenance organizations. Epilepsia 1999;40(4):502‐6. [DOI] [PubMed] [Google Scholar]
- Atkins D, Best D, Briss PA, Eccles M, Falck‐Ytter Y, Flottorp S, et al. GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baulac M, Cramer JA, Mattson RH. Phenobarbital and other barbiturates: adverse effects. In: Levy RH, Mattson RH, Meldrum BS, et al. editor(s). Antiepileptic Drugs. 5th Edition. Philadelphia: Lippincott Williams & Wilkins, 2002:528‐40. [Google Scholar]
- Cockerell OC, Johnson AL, Sander JW, Hart YM, Shorvon SD. Remission of epilepsy: results from the National General Practice Study of Epilepsy. Lancet 1995;346(8968):140‐4. [DOI] [PubMed] [Google Scholar]
- Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Epilepsia 1981;22(4):489‐501. [DOI] [PubMed] [Google Scholar]
- Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia 1989;30(4):389‐99. [DOI] [PubMed] [Google Scholar]
- Gruber CM, Brock JT, Dyken MD. Comparison of the effectiveness of phenobarbital, mephobarbital, primidone, dipheylhydantoin, ethotoin, metharbital, and methylphenylhydantion in motor seizures. Clinical Pharmacology and Therapeutics 1962;3:23‐8. [DOI] [PubMed] [Google Scholar]
- Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota 1935 ‐ 1984. Epilepsia 1993;34:453‐68. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbookfor Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org..
- Hirtz D, Thurman DJ, Gwinn‐Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R. How common are the "common" neurologic disorders?. Neurology 2007;68:326‐37. [DOI] [PubMed] [Google Scholar]
- ILAE Commission on Antiepileptic Drugs. Considerations on designing clinical trials to evaluate the place of new antiepileptic drugs in the treatment of newly diagnosed and chronic patients with epilepsy. Epilepsia 1998;39(7):799‐803. [DOI] [PubMed] [Google Scholar]
- Glauser T, Ben‐Menachem E, Bourgeois B, Cnaan A, Chadwick D, Guerreiro C, et al. ILAE treatment guidelines: evidence based analysis of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia 2006;47(7):1094‐120. [DOI] [PubMed] [Google Scholar]
- Jones B, Jarvis P, Lewis JA, Ebbutt AF. Trials to assess equivalence: the importance of rigorous methods. BMJ 1996;313(7048):36‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juul‐Jenson P, Foldspang A. Natural history of epileptic seizures. Epilepsia 1983;24:297‐312. [DOI] [PubMed] [Google Scholar]
- Kirkham JJ, Dwan KM, Altman DG, Gamble C, Dodd S, Smyth R, et al. The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ 2010;340:c365. [DOI] [PubMed] [Google Scholar]
- Kwan P, Brodie MJ. Early identification of refractory epilepsy. New England Journal of Medicine 2000;342:314‐9. [DOI] [PubMed] [Google Scholar]
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Liporace JD, Sperling MR, Dichter MA. Absence seizures and carbamazepine in adults. Epilepsia 1994;35(5):1026‐8. [DOI] [PubMed] [Google Scholar]
- MacDonald RL, Kelly KM. Antiepileptic drug mechanisms of action. Epilepsia 1995;36(Suppl 2):S2‐12. [DOI] [PubMed] [Google Scholar]
- MacDonald BK, Johnson AL, Goodridge DM, Cockerell OC, Sander JWA, Shorvon SD. Factors predicting prognosis of epilepsy after presentation with seizures. Annals of Neurology 2000;48:833‐41. [PubMed] [Google Scholar]
- Malfosse A, Genton P, Hirsch E, Marescaux C, Broglin D, Bernasconi R. Idiopathic Generalised Epilepsies: Clinical, Experimental and Genetic. Eastleigh: John Libbey and Company, 1994. [Google Scholar]
- Marson AG, Williamson PR, Hutton JL, Clough HE, Chadwick DW. Carbamazepine versus valproate monotherapy for epilepsy. Cochrane Database of Systematic Reviews 2000, Issue 3. [DOI: 10.1002/14651858.CD001030] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matlow J, Koren G. Is carbamazepine safe to take during pregnancy?. Canadian Family Physician 2012;58:163‐4. [PMC free article] [PubMed] [Google Scholar]
- Meador K, Reynolds M, Crean S, Fahrbach K, Probst C. Pregnancy outcomes in women with epilepsy: a systematic reviews and meta‐analysis of published pregnancy registries and cohorts. Epilepsy Research 2008;81:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: The PRISMA Statement. BMJ 2009;339:2535. [PMC free article] [PubMed] [Google Scholar]
- Morrow J, Russel A, Guthrie E, Parsons L, Robertson I, Waddell R, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. Journal of Neurology, Neurosurgery, and Neuropsychiatry 2006;77(2):193‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, Lopez AD. Global comparative assessments in the health sector. World Health Organization. Geneva, 1994.
- Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life‐time epilepsy: a meta‐analytic approach. Epilepsia 2010;51:883‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. The epilepsies: the diagnosis and management of the epilepsies in adults and children in primary and secondary care; Clinical Guidance 137. London: National Institute for Health and Care Excellence, 2012. [Google Scholar]
- Nolan SJ, Sutton L, Marson A, Tudur Smith C. Consistency of outcome and statistical reporting of time‐to‐event data: the impact on Cochrane Reviews and meta‐analyses in epilepsy. 21st Cochrane Colloquium: Better Knowledge for Better Health. Quebec City, 2013:114‐5. [Google Scholar]
- Nolan SJ, Marson AG, Pulman J, Tudur Smith C. Phenytoin versus valproate monotherapy for partial onset seizures and generalised onset tonic‐clonic seizures. Cochrane Database of Systematic Reviews 2013, Issue 8. [DOI: 10.1002/14651858.CD001769.pub2] [DOI] [PubMed] [Google Scholar]
- Olafsson E, Ludvigsson P, Gudmundsson G, Hesdorfer D, Kjartansson O, Hauser WA. Incidence of unprovoked seizures and epilepsy in Iceland and assessment of the epilepsy syndrome classification: a prospective study. Lancet Neurology 2005;4:627‐34. [DOI] [PubMed] [Google Scholar]
- Pal DK, Das T, Chaudhury G, Johnson AL, Neville BG. Randomised controlled trial to assess acceptability of phenobarbital for childhood epilepsy in rural India. Lancet 1998;351(9095):19‐23. [DOI] [PubMed] [Google Scholar]
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta‐analyses of the published literature for survival endpoints. Statistics in Medicine 1998;17(24):2815‐34. [DOI] [PubMed] [Google Scholar]
- Ragsdale DS, Scheuer T, Catterall WA. Frequency and voltage dependent inhibition of type hA Naı channels, expressed in a mammalian cell line, by local anesthetic, antiarrhythmic, and anticonvulsant drugs. Molecular Pharmacology 1991;40:756‐65. [PubMed] [Google Scholar]
- Rho JM, Donevan SD, Rogawski MA. Direct activation of GABAA receptors by barbiturates in cultured rat hippocampal neurons. The Journal of Physiology 1996;497(2):509‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander JW, Shorvon SD. Epidemiology of the epilepsies. Journal of Neurology, Neurosurgery, and Psychiatry 1996;61(5):433‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander JW. The use of anti‐epileptic drugs ‐ principles and practice. Epilepsia 2004;45(6):28‐34. [DOI] [PubMed] [Google Scholar]
- Shakir RA. Sodium valproate, phenytoin and carbamazepine as sole anticonvulsants. The place of sodium valproate in the treatment of epilepsy. London: Academic Press Inc (London) Ltd and the Royal Society of Medicine, 1980:7‐16. [Google Scholar]
- Shields WD, Saslow E. Myoclonic, atonic, and absence seizures following institution of carbamazepine therapy in children. Neurology 1983;33:1487‐9. [DOI] [PubMed] [Google Scholar]
- Snead OC, Hosey LC. Exacerbation of seizures in children by carbamazepine. New England Journal of Medicine 1985;313:916‐21. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11. CollegeStation, TX: StataCorp LP, 2009.
- Trimble MR, Cull C. Children of school age: the influence of antiepileptic drugs on behavior and intellect. Epilepsia 1988;29(Suppl 3):S15‐19. [DOI] [PubMed] [Google Scholar]
- Tudur Smith C, Marson AG, Chadwick DW, Williamson PR. Multiple treatment comparisons in epilepsy monotherapy trials. Trials 2007;5(8):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace H, Shorvon SD, Hopkins A, O'Donoghue M. Guidelines for the Clinical Management of Adults with Poorly Controlled Epilepsy. London: Royal College of Physicians, 1997. [Google Scholar]
- Williamson PR, Tudur Smith C, Hutton JL, Marson AG. Aggregate data meta‐analysis with time‐to‐event outcomes. Statistics in Medicine 2002;21(11):3337‐51. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Nolan SJ, Marson AG, Weston J, Tudur Smith C. Carbamazepine versus phenobarbitone monotherapy for epilepsy: an individual participant data review. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD001904.pub2] [DOI] [PubMed] [Google Scholar]
- Tudur C, Marson AG, Williamson PR, Hutton JL, Chadwick DW. Carbamazepine vs phenobarbitone monotherapy for epilepsy. Cochrane Database of Systematic Reviews 2000, Issue 1. [DOI: 10.1002/14651858.CD001904] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudur Smith C, Marson AG, Williamson PR. Carbamazepine versus phenobarbitone monotherapy for epilepsy. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD001904] [DOI] [PubMed] [Google Scholar]


