Abstract
Objective
Psychological pain lies at the heart of human experience. However, it may also be abnormally intense and/or prolonged in pathological states, with negative outcomes. A simple and reliable measure of psychological pain for clinical use would be useful. In this study, we present a preliminary validation of a simple visual analog scale jointly measuring psychological and physical pain.
Methods
Two samples of adult (non elderly) depressed patients and healthy controls were independently recruited in two locations in Canada and the USA (N=48/46 and 20/200, respectively). Six dimensions were successively scored on a paper visual analog scale measuring current, mean and worst pain over the last 15 days, for physical then psychological pain.
Results
All physical and psychological pain dimensions discriminated depressed from non-depressed subjects. Among depressed patients, psychological pain scores were higher than physical pain scores for a given period of assessment. Moreover, correlations between dimensions from the same pain category (physical or psychological) were higher than between different pain categories. Psychological pain was mainly correlated with depression and hopelessness scales while physical pain was mainly correlated with anxiety scales. Secondary analyses showed that psychological (and some physical) pain measures were correlated with suicidal ideas in one location, but no difference in pain scores was found between patients with vs. without a history of suicidal acts in both samples. Childhood trauma positively correlated with several pain dimensions.
Conclusion
The PPP-VAS appears to be a valid tool in terms of discriminative capacities and convergent-divergent validities. Validation in different samples, including adolescents and elderly, and in various psychiatric and medical conditions will have to be conducted, in addition to the assessment of concurrent and predictive validities, and the confirmation of sensitivity to change. The role of psychological pain in the suicidal process needs to be further elucidated.
Keywords: psychological pain, depression, visual analog scale, suicidal ideas
1. Introduction
Psychological pain (also named mental pain or psychache) lies at the heart of the human social experience. It is a natural state occurring in response to particular events, notably those related to loss, grief, failure, shame or guilt. The end of a relationship, the thought of having committed something wrong or hurt somebody, the loss of a beloved one are all classical situations triggering painful feelings. While everybody has experienced psychological pain, an explicit definition is complicated. Shneidman proposed “an introspective experience of negative emotions such as anger, despair, fear, grief shame, guilt, hopelessness, loneliness and loss” (Shneidman, 1993). In an attempt to give a more unified definition, Meerwijk and Weiss (Meerwijk and Weiss, 2011) proposed to define psychological pain as “a lasting, unsustainable, and unpleasant feeling resulting from negative appraisal of an inability or deficiency of the self “ Recent research has started to study the biological mechanisms of psychological pain, notably those occurring in situations such as social exclusion (Eisenberger and Lieberman, 2004; Danziger et al., 2006; Hsu et al., 2013; DeWall et al., 2015; Jollant et al., 2017). It has been suggested that processing of social pain, an evolutionary mechanism aiming at avoiding social disconnection, may partly share neural and biochemical mechanisms with physical pain processing (Eisenberger, 2012).
While often a normal phenomenon, psychological pain is found in more pervasive forms in psychiatric conditions such as depression or borderline personality disorder (Tossani, 2013; Ducasse et al., 2014). Furthermore, research has suggested a significant risk of suicidal ideas and acts in those experiencing psychological pain (Shneidman, 1993; Verrocchio et al., 2016). When compared to other risk factors such as hopelessness and depression, psychological pain was found to be a stronger predictor of suicidality (Troister et al., 2015). Furthermore, in a sample of high-risk suicidal students, change in psychache was the only significant predictor of change in suicidal ideation (Troister and Holden, 2012). Caceda et al. (Cáceda et al., 2014, 2017) also observed a parallel reduction in psychological pain and suicidal ideation during care. Recent works suggest that motivation for pain avoidance, associated with deficient information processing, underlie suicidal ideation (Xie et al., 2014, 2017). Finally, the use of analgesics such as buprenorphine to treat suicidal ideas (Yovell et al., 2016) suggests that psychological pain could be a relevant target of therapeutic interventions in suicidal crisis.
In a context of growing clinical and scientific interest in psychological pain, a reliable and simple measurement tool becomes necessary. To date, several questionnaires/scales are available (Tossani, 2013): The illustrated Psychological Pain Assessment Scale (Shneidman, 1999), the Psychache Scale (Holden et al., 2001), the Orbach and Mikulincer Mental Pain scale (Orbach et al., 2003), the Mee-McBunney Psychological Pain Assessment Scale (Mee et al., 2011), or the Three-Dimensional Psychological Pain Scale (Li et al., 2014). As psychological pain is a subjective experience that everybody identifies but also an experience difficult to define and describe with words, the use of a visual analog scale (VAS) unrelated to specific definitions and concepts was recently proposed (Olie et al., 2010). VAS are simple and quick to run tools routinely used to assess physical pain in medicine and surgery (Bijur et al., 2001). Interestingly, research has highlighted that physical and psychological pain may be inter-correlated during the suicidal crisis, with an increase in pain tolerance threshold during the suicidal climax (Cáceda et al., 2017). Therefore, using a similar tool to simultaneously assess both psychological and physical pains could be particularly relevant.
The Psychological and Physical Pain VAS (PPP-VAS) was first used in a sample of French depressed inpatients including 87 with a recent history of suicidal acts, 61 with a past history of suicidal acts, and 62 without any history of suicidal act (Olie et al., 2010). Scores were dichotomized into “high” and “low” according to their median for analyses. High current psychological pain levels were more often found in both suicide attempter groups than in patient controls. Moreover, high current psychological pain was associated with high current suicidal ideas (also measured with a VAS). Cáceda et al. (Cáceda et al., 2017) reported higher scores for current, mean and worst psychological pain in 52 American (recent) suicide attempters than in 64 current suicide ideators and 24 depressed non suicidal patients, themselves showing higher scores than 40 healthy controls. As previously explained, score reductions were observed over the following 3-5 days in a care context.
This useful and easy-to-use scale needs to be validated. In the present paper, we run a series of initial validation in two independent samples of depressed patients and healthy controls. We notably tested i) discrimination capacities between depressed and non-depressed individuals, and between physical and psychological dimensions, and ii) convergent and divergent validities, i.e. the fact that psychological pain measured with this scale correlates more with measures reflecting psychological pain such as depression and hopelessness than with measures of anxiety. In secondary analyses, we examined the previously reported association between psychological pain and suicidality. Finally, we explored a potential association between psychological pain and childhood trauma as developmental insults have previously been reported as risk factors of physical pain (Tesarz et al., 2016).
We hypothesized that PPP-VAS scores of psychological pain would 1) be higher in depressed patients than healthy controls; 2) partly but not totally overlap with PPP-VAS physical pain scores, and be higher in depressed subjects; 3) correlate with scales measuring depression and hopelessness but not anxiety. Moreover, we expected psychological pain measures to 4) correlate with measures of current suicidal ideas; 5) be higher in suicide attempters than non-attempter patients; and 6) correlate with histories of childhood trauma.
2. Methods
2.1. Population
Montreal (Canada).
Male and female participants aged 18 to 55 years old were recruited as part of a clinical and neuroimaging study on suicidal behavior. The population included 46 un-medicated and currently depressed outpatients (DP), and 48 healthy controls (HC) with no personal or first- or second-degree family history of suicidal behavior or depression. All patients were depressed at the time of scanning with a diagnosis of major depressive episode according to SCID-I following DSM-IV criteria (First et al., 2012) and a Hamilton Depression Rating Scale-24 items (HAMD-24) score higher than 18 (Hamilton, 1960). Only patients with a major depressive disorder were recruited. None of the participants were medicated at the time of the scanning, and most participants had withdrawn from any pharmacological treatment more than 7 days before. Exclusion criteria included a lifetime history of schizophrenia or bipolar disorder, a history of alcohol/substance abuse or dependence spanning the previous six months, a major general medical condition requiring ongoing pharmacological treatment, a lifetime history of severe head trauma or central nervous system disorder. This study was conducted at the Douglas Mental Health University Institute in Montréal, Canada, and approved by the local ethics committee. Participants received 100 CAD for their time.
Little Rock (USA).
Male and female participants from 18 to 65 years old were recruited as part of two different studies on suicidal behavior. The population included 194 currently depressed patients (69 unmedicated and 125 receiving antidepressant medication), and 20 healthy controls with no personal or first- or second-degree family history of suicidal behavior or depression. All patients were at least moderately depressed (Beck Depression Inventory (BDI-II) (Beck et al., 1996) > 13) and had a diagnosis of major depressive episode according to MINI (Sheehan et al., 1998) or SCID-I following DSM-IV criteria (First et al., 2012). Only patients with a major depressive disorder were included in this report. Exclusion criteria included: inability to read, write, and speak English; inability to provide informed consent; involuntary hospitalization; history of dementia, neurovascular, or neurodegenerative conditions; history of schizophrenia, schizoaffective disorder, or unspecified psychosis; opioid use within the last month; undergoing alcohol, benzodiazepine, opioid or barbiturate withdrawal and physical disabilities that prohibit task performance, such as blindness or deafness. A subset of these subjects underwent fMRI scanning and had additional exclusion criteria: taking medication that will interfere with blood oxygen level dependent (BOLD) signal, non-removable ferromagnetic objects; history of claustrophobia; positive pregnancy test. Subjects were recruited from the psychiatric inpatient units, University of Arkansas for Medical Sciences (UAMS) psychiatric outpatient clinics of the UAMS Psychiatric Research Institute, and the local Little Rock community. Subjects received 20-100 USD for their participation. UAMS Institutional Review Board approved all procedures.
2.2. The Physical and Psychological Pain - Visual Analog Scale (PPP-VAS)
Six dimensions are successively measured with the PPP-VAS: current, mean and worst physical pain over the last 15 days, followed by the same measures for psychological pain. Each dimension is visually presented as a horizontal rectangle labeled at extremities with “no pain” (on the left) and “maximal pain” (on the right). Current suicidal ideas were also measured in the original version in a similar fashion, in addition to frequency of suicidal ideas scored from 0 (never) to 4 (always). The version used in the current Montreal sample omitted the measurement of suicidal ideas. Instructions are purposely limited to simple sentences, e.g. “Please score the level of your psychological pain” and no explicit definition is given. Scores from 0 to 10 were noted inside the rectangles in the original version and the one used in Little Rock, and participants had to circle the level of their pain. In the Montreal version, we used a more classical VAS format, i.e. open rectangles with participants being instructed to draw a vertical line; Scores were then standardized corresponding to the measurement in centimeters from the left of the box to the line, divided by the length of the box multiplied by 10. The total duration of PPP-VAS completion is less than 1 min.
2.3. Clinical assessment
Montreal.
The following scales were used: the HAMD-24, the BDI-I (Beck et al., 1961); the Scale for Suicidal Ideation (SSI) (Beck et al., 1979), clinician based version for the current period; the Suicide Intent Scale (SIS) (Beck et al., 1974b), the Hamilton Rating Scale for Anxiety (HAM-A) (Hamilton, 1959); the Childhood Trauma Questionnaire (CTQ) (Bernstein et al., 2003); and the National Adult Reading Test (NART) to measure verbal IQ (Beardsall and Brayne, 1990). The Columbia-Suicide Severity Rating Scale (C-SSRS) (Posner et al., 2011) was used to assess current suicidal ideas, a history of suicide attempt and non-suicidal self-injury.
Little Rock.
The BDI-II, the Beck Anxiety Inventory (BAI) (Beck et al., 1988), the Beck Hopelessness Scale (BHS) (Beck et al., 1974a), the C-SSRS and the CTQ were used.
2.4. Statistical analysis
As non-normal distributions were found for most dependent variables, non-parametric tests were used. Mann-Whitney tests were used to compare quantitative variables between DP and HC. Chi-square tests were used to compare qualitative variables. Wilcoxon’s tests were used to compare quantitative values within the same group. Spearman’s tests were used for correlation analyses. P-values below 0.05 were considered as statistically significant, with a Bonferroni’s correction in case of multiple analyses (see level of correction in text). Analyses were performed using SPSS 23 (SPSS, Inc., Chicago, IL).
3. Results and statistical analyses
3.1. Populations characteristics
Montreal.
The Montreal sample (Table 1) consisted in 48 DP and 46 HC. Compared to HC, DP were older but gender distribution and NART scores were similar between groups. DP had higher HAMD-24, BDI-II, HAM-A, and CTQ scores than HC, as expected. Among the 48 DP, 16 (34.8%) had a history of suicide attempt. There was no significant correlation between any of the PPP-VAS dimensions and age or NART scores in the whole sample (co-variating for depression status), and no gender difference in scores among HC or DP.
Table 1.
Characteristics of the Montreal sample, and comparison between Healthy controls and Depressed patients.
| HC | DP | Chi2 or U | p | |
|---|---|---|---|---|
| N | 48 | 46 | ||
| Age, mean (SD) | 32.3 (6.5) | 41.0 (10.4) | 562.5 | <10−3 |
| Females, N (%) | 28 (58.3) | 29 (63.0) | .2 | .4 |
| Total standardized NART score, mean (SD) | 75.0 (12.8) | 71.2 (13.7) | 880.5 | .3 |
| Total HAMD score, mean (SD) | 1.7 (2.5) | 29.9 (6.1) | 1.0 | <10−3 |
| Total HAMA score, mean (SD) | 1.6 (2.6) | 18.0 (5.9) | 2.5 | <10−3 |
| Total BDI score, mean (SD) | 1.5 (2.4) | 31.2 (10.3) | 0.0 | <10−3 |
| Number of previous MDE, mean (SD) | – | 2.0 (1.1) | ||
| Age at first MDE, mean (SD) | – | 35.4 (11.7) | ||
| Total SSI score (current), mean (SD) | 0 (0) | 8.6 (7.9) | 322.0 | <10−3 |
| Total SSI score (most severe), mean (SD) | 0 (0) | 15.1 (9.9) | 184.0 | <10−3 |
| CTQ emotional abuse, mean (SD) | 4.1 (3.2) | 12.3 (5.4) | 158.0 | <10−3 |
| CTQ physical abuse, mean (SD) | 3.0 (2.5) | 8.2 (5.4) | 328.5 | <10−3 |
| CTQ sexual abuse, mean (SD) | 3.0 (2.6) | 9.0 (5.6) | 269.0 | <10−3 |
| CTQ emotional neglect, mean (SD) | 10.6 (4.7) | 16.5 (5.7) | 380.5 | <10−3 |
| CTQ physical neglect, mean (SD) | 5.6 (1.6) | 9.4 (4.1) | 379.0 | <10−3 |
Footnotes: HC: Healthy Controls; DP: Depressed Patients; SD: Standard Deviation; HAMD: Hamilton Depression Rating Scale – 24 items; HAMA: Hamilton Anxiety Rating Scale; BDI: Beck depression Inventory – first version; MDE: Major Depressive Episode; SSI: Scale for Suicidal ideation; NART: National Adult Reading Test; CTQ: Childhood Trauma Questionnaire.
Little Rock.
The sample (Table 2) consisted in 200 DP and 20 HC. Age and gender distribution were similar between groups but DP had lower education level than HC. BDI-II, BAI, BHS, and CTQ scores were higher in DP than HC, as expected. Among the 200 DP, 138 (69%) had a history of suicide attempt. After co-variating for depression status, several PPP-VAS scores were correlated with age (rs between .20 and .33, p<10−3) but not education level. There was no difference according to gender in HC, but higher current psychological pain in females than males among DP (mean=7.7 (Standard Deviation (SD)=2.5) vs. 6.7 (2.8), p=.009).
Table 2.
Characteristics of the Little Rock sample, and comparisons between Healthy controls and Depressed patients.
| HC | DP | Chi2 or U | p | |
|---|---|---|---|---|
| N | 20 | 200 | ||
| Age, mean (SD) | 33.4 (10.8) | 36.3 (12.2) | 1719.0 | .3 |
| Females, N (%) | 12 (60.0) | 131 (65.5) | .2 | .4 |
| Education level (years), mean (SD) | 15.8 (2.5) | 13.4 (2.2) | 908.5 | <10−3 |
| Total BDI-II score, mean (SD) | 1.6 (1.6) | 36.9 (11.6) | 9.5 | <10−3 |
| Total BAI score, mean (SD) | 2.7 (3.6) | 29.7 (13.9) | 97.5 | <10−3 |
| Total BHS score, mean (SD) | 0.9 (1.1) | 12.9 (6.0) | 116.5 | <10−3 |
| CTQ emotional abuse, mean (SD) | 7.0 (3.4) | 12.5 (6.5) | 158.0 | .001 |
| CTQ physical abuse, mean (SD) | 6.2 (1.7) | 10.8 (5.8) | 328.5 | .001 |
| CTQ sexual abuse, mean (SD) | 6.8 (4.8) | 9.2 (7.3) | 269.0 | .1 |
| CTQ emotional neglect, mean (SD) | 1.9 (2.7) | 8.9 (5.2) | 380.5 | <10−3 |
| CTQ physical neglect, mean (SD) | 4.0 (2.0) | 6.8 (4.5) | 379.0 | .001 |
Footnotes: HC: Healthy Controls; DP: Depressed Patients; SD: Standard Deviation; BDI-II: Beck Depression Inventory, second version; BAI: Beck Anxiety Inventory; BHS: Beck Hopelessness Scale; CTQ: Childhood Trauma Questionnaire.
3.2. Discriminative capacities between depressed and non-depressed individuals
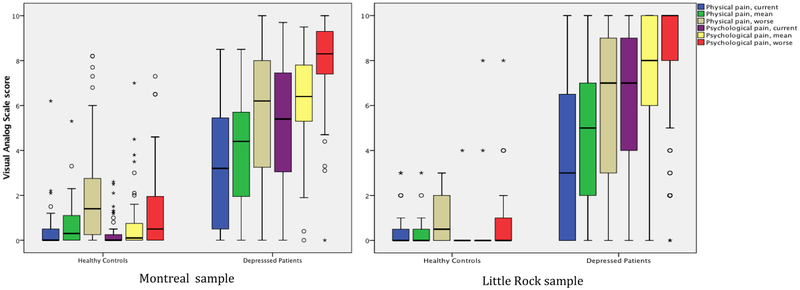
As expected, all 6 PPP-VAS dimensions were scored higher in DP than HC in both samples (all p-values < 10−3). As can be seen in Graph 1, there was very limited overlap in score distributions between DP and HC for a given dimension.
Graph 1.
Distribution of PPP-VAS scores for each dimension according to depression status in Montreal (left) and in Little Rock (right).
Footnotes: Black line inside box = median of distribution; Upper and lower limits of a box = 75th and 25th percentiles of the distribution (the box therefore represents 50% of the sample); Vertical lines = range between minimal and maximal values within 1.5 times the length of a box; Stars and circles = extreme minimal and maximal values beyond 1.5 (circles) and 3 (stars) times the length of the box.
3.3. Discrimination capacities between physical and psychological pain dimensions
Analyses were conducted in DP only (Table 3).
Table 3.
Correlations between physical and psychological pain dimensions in the two samples
| 1. Current | 2. Worst | 3. Mean | 4. Current | 5. Worst | 6. Mean | |
|---|---|---|---|---|---|---|
| Physical pain | psychological pain | |||||
| Montreal | ||||||
| 1. | ||||||
| 2. | .68* | |||||
| 3. | .74* | .71* | ||||
| 4. | .31 | .05 | .19 | |||
| 5. | −.06 | .14 | −.13 | .41* | ||
| 6. | .12 | .04 | .26 | .61* | .40* | |
| Little Rock | ||||||
| 1. | ||||||
| 2. | .72* | |||||
| 3. | .72* | .85* | ||||
| 4. | .31* | .19 | .20 | |||
| 5. | .12 | .23* | .18 | .50* | ||
| 6. | .15 | .22* | .31* | .40* | .67* | |
p<.003 (significant at Bonferroni’s correction level)
Montreal.
After Bonferroni’s correction (p=.003, 15 analyses), all physical pain dimensions significantly correlated with each other. Psychological pain dimensions also correlated with each other. Inter-category (physical vs. psychological) correlational tests showed non-significant results. When dimensions measuring the same period (current, worst or mean) were compared, psychological pain was always scored higher than physical pain dimensions (all p<10−3).
Little Rock.
Similarly, all physical pain dimensions correlated with each other and all psychological pain dimensions correlated with each other. Regarding inter-category correlations, four correlations (out of six) between psychological and physical pain dimensions were significant at Bonferroni’s level and usually smaller than intra-category correlations. Again, psychological pain scores were all higher than physical pain scores for the same period (all p<10−3).
Overall, as shown in Graph 1 and Table 3, psychological pain scores were higher than physical pain scores in DP, and there were some significant but small and limited correlations between physical and psychological pain categories while intra-category correlations were all highly significant.
3.4. Convergent/divergent validities
Here again, analyses were conducted in DP only (Table 4).
Table 4.
Correlations between physical and psychological pain dimensions and symptomatic questionaires in the two samples
| 1. Current | 2. Worst | 3. Mean | 4. Current | 5. Worst | 6. Mean | |
|---|---|---|---|---|---|---|
| physical pain | psychological pain | |||||
| Montreal | ||||||
| BDI-I | .14 | .12 | −.03 | .40 | .58* | .20 |
| HAM-D | .19 | .22 | .38 | .17 | .17 | .19 |
| HAM-A | .44* | .37 | .56* | .27 | .03 | .09 |
| Little Rock | ||||||
| BDI - II | .24* | .21* | .23* | .55* | .46* | .35* |
| BAI | .28* | .31* | .37* | .31* | .25* | .24* |
| BHS | .07 | −.07 | .00 | .39* | .23* | .15 |
p<.003 (significant at Bonferroni’s correction level)
BDI: Beck Depression Inventory; HAM-D: Hamilton Depression Rating Scale (24 items); HAM-A: Hamilton Anxiety Rating Scale; BAI: Beck Anxiety Inventory; BHS: Beck Hopelessness Scale.
Montreal.
After Bonferroni’s correction (p=.003, 18 analyses), BDI total scores were correlated with worst psychological pain (rs=.58, p<10−3) with a trend for current psychological pain (.40, p=.008) but not physical pain dimensions. No PPP-VAS dimension correlated with HAM-D total scores although a trend was found with mean physical pain (rs=.38, p=.009). HAM-A total scores were correlated with current (rs=.44, p=.002) and mean physical pain (rs=.56, p<10−3) (and a trend for worst pain (rs=.37, p=0.005)), but not with any psychological pain dimensions.
Little Rock.
After Bonferroni’s correction (p=.003, 18 analyses), BDI total scores were correlated with all PPP-VAS scores, although more strongly with the psychological than the physical pain dimensions. The opposite was true for the BAI total scores with slightly stronger correlations with the physical than the psychological pain dimensions. Finally, the BHS was correlated with current (.39, p<10−3) and mean psychological pain (.23, p=0.001) but not with any physical pain dimensions.
In summary, psychological pain dimensions tended to correlate more with depression and hopelessness scales than anxiety scales, while the opposite was true for physical pain dimensions.
3.5. Correlation with suicidal ideas
Montreal.
Assessment of suicidal ideation was made according to three tools: the SSI, the C-SSSR (5 scores: “Wish to be dead”, “Non-Specific Active Suicidal Thoughts”, “Active Suicidal Ideation with Any Methods (Not Plan) without Intent to Act”, “Active Suicidal Ideation with Some Intent to Act, without Specific Plan”, “Active Suicidal Ideation with Specific Plan and Intent”), and BDI-item 9. After Bonferroni’s correction (p=.001, 42 analyses), we found no significant correlation between PPP-VAS pain dimensions and suicidal ideas, and no association with C-SSSR items. There was only a small trend for worst psychological pain, which was moderately correlated with BDI-item 9 (rs=.34, p=.03).
Little Rock.
In this sample, suicidal ideas were assessed using BDI-item 9, the seventh dimension (current suicidal ideas) of the PPP-VAS original version, and the C-SSRS. After Bonferroni’s correction (p=.001, 42 analyses), psychological but not physical pain dimensions were correlated with BDI-item 9 (current: .44; mean: .28, worst: .23; all p<10−3). Moreover, significant correlations were found between PPP-VAS item 7 and the three PPP-VAS psychological pain dimensions (current: rs=.62, mean: .24, worst: .26; all p<10−3) but not physical dimensions at the exception of current physical pain (.29, p<10−3). Regarding the C-SSRS, higher scores were found in the presence vs. absence of all 5 types of suicidal ideas for current psychological pain, and of 3 types of suicidal ideas (“Wish to be dead”, “Non-Specific Active Suicidal Thoughts”, and “Active Suicidal Ideation with Specific Plan and Intent”) for current physical pain (all <10−3).
In summary, measures of current suicidal ideas were correlated with psychological pain in the Little Rock but not in the Montreal sample. Interestingly, current physical pain also correlated with two out three suicidal ideas measures.
3.6. Association with a history of suicidal behaviors
Montreal.
Both suicide attempters and non-attempter DP scored higher than HC on all scores (all p<10−3). Although scores tended to be higher in suicide attempters than in patient controls, none of the comparisons was significant between these two groups. Moreover, there was no significant correlation between any PPP-VAS dimension and measures of suicidal intent using the SIS for the last and the most severe suicidal acts.
Little Rock.
Similarly, PPP-VAS scores did not statistically differ between patients with vs. without a lifetime history of suicide attempt, while both groups scored higher than HC. Similar results were found for a lifetime history of non-suicidal self-injury.
3.7. Correlation with CTQ scores
Analyses were conducted in both groups combined.
Montreal.
After Bonferroni’s correction (p=.002, 30 analyses) and co-variating for depression status, no CTQ score correlated with any of the 6 PPP-VAS dimensions. However, a trend was observed between current physical pain and both sexual abuse (rs=.30, p=.006) and physical neglect (rs=.32, p=.004), and between worst psychological pain and emotional neglect (rs=.30, p=.006).
Little Rock.
After co-variating for depression status, significant correlations were found between CTQ emotional abuse and mean (.42, p=.001) and worst (.40, p=.002) psychological pain.
4. Discussion
In this preliminary validation study of the PPP-VAS conducted in two independent samples of depressed subjects and controls, most expected results were supported: 1) All PPP-VAS dimension scores were significantly higher in patients than in healthy subjects suggesting that the PPP-VAS is able to discriminate these two groups. 2) Among patients, physical and psychological pain categories partly overlap, but correlations were higher between dimensions of the same category than between dimensions of different categories and scores of psychological dimensions were higher than those of physical dimensions for a given period of assessment. These results suggest that participants seem to be able to distinguish physical from psychological pain in spite of the fact that explicit definitions were not given. 3) Correlations were higher between psychological pain and depression / hopelessness than anxiety, while the opposite was true for physical pain, in line with the expected divergent and convergent validities.
Regarding psychological pain in DP, score variations were larger for current than for worst psychological pain over the last 15 days with an intermediate position for mean pain, with few subjects scoring below 5 for worst psychological pain. Worst and mean psychological pain measures may therefore be interesting global markers of psychological pain during a depressive episode, while current psychological pain may show more fluctuations and be more relevant to measure changes over short period of time. This will need to be further assessed with repeated measures within a day and across several days, and the investigation of the effect of particular care interventions.
Surprisingly, the association between psychological pain and suicidal ideas and acts was more limited than expected (Olie et al., 2010; Troister and Holden, 2012; Ducasse et al., 2017). Association between suicidal ideas and psychological (and to a lower extent physical) pain was mostly found in the Little Rock sample. The lack of correlation in the Montreal sample may notably stem from limited statistical power due to the smaller sample size. Regarding a history of suicidal act, there was no difference between those with vs. without a history of suicidal act in both samples. One explanation may be the time limitation (currently or last 15 days) of the PPP-VAS that cannot capture the psychic state during remote suicide attempts. Another explanation may be that psychological pain is mainly involved in the early phases of the suicidal process, with psychache leading to suicidal ideas while acting out when suicidal necessitates additional mechanisms such as poor inhibition or impaired decision-making (Jollant et al., 2011). A recent meta-analysis tends to support this hypothesis, with a higher effect size between psychological pain and suicidal ideas than between psychological pain and suicide attempts (Ducasse et al., 2017). Also, a cohort study of individuals with histories of medically serious suicide attempts could not confirm a link between psychological pain measured with the Orbach and Mikulincer Mental Pain scale and suicidal acts (Trakhtenbrot et al., 2016). The respective role of the various steps involved in the suicidal process and the diverse suicidal pathways will have to be further clarified.
Finally, significant correlations between some physical and psychological pain dimensions and some CTQ scores suggest that developmental factors are associated with impaired perception of pain as previously shown for physical pain (Tesarz et al., 2016). Previous studies have shown deleterious effects of early life adversity on the development of a wide range of physiological processes including epigenetic, cognitive, emotional and brain alterations (Turecki et al., 2012). Impaired regulation of psychological pain perception may therefore be another consequence of childhood trauma. This will need to be more specifically studied.
Several limitations have to be underlined. First, we did not measure the concurrent validity of the PPP-VAS with other scales designed to measure psychological pain. This will be the objective of future studies. It should however be noted here that, in the absence of specific markers of psychological pain, there is no gold standard scale. Moreover, most previous scales were developed without concurrent validation - at one exception (Li et al., 2014) - usually focusing on discriminative capacities (between suicide attempters or depressed patients and healthy controls) and convergent validities (with depression, anxiety or hopelessness scales). Second, the size of the samples prevented us from running path analyses. This could have been interesting to investigate a mediating role of pain in the association between childhood trauma and suicidal ideas and acts. Third, changes in the design of the PPP-VAS used in Montreal and Little Rock may have modified its properties and explain some of the differences between the two sites.
5. Conclusion
The PPP-VAS appears to be a valid tool to jointly measure psychological and physical pain in depressed subjects with interesting discriminative capacities (depressed vs. euthymic; psychological vs. physical pain), and convergent/divergent validities (depression vs. anxiety). The main advantage of this scale remains its ease of use: PPP-VAS takes very little time to complete, takes almost no extra-time from clinicians, and could therefore be easily added to patients’ evaluation in a similar fashion as what is done with physical pain-VAS in medicine and surgery. Validity in other age groups (adolescents, elderly) and other psychiatric and medical conditions will need to be tested. Concurrent validity against scales measuring psychological pain will also have be conducted, keeping in mind the various definitions of psychological pain intrinsic to these scales. The sensitivity to change following care and treatment will need to be confirmed, and the predictive validity notably in terms of suicidal ideas and acts but also quality of life and general health outcomes will also have to be assessed.
Highlights.
The PPP-VAS is a simple analog scale for physical and psychological pain
An initial validation was conducted in depressed patients and healthy controls
The PPP-VAS showed good discriminative and convergent/divergent validities
The association with suicidality was not as strong as expected
Acknowledgements
This research was allowed thanks to a Canadian Institutes for Health Research (CIHR) grant to Dr. F. Jollant. Dr. F. Jollant held a “chercheur-boursier clinicien” salary grant from the Fond de Recherche du Québec – Santé (FRQS) at the time of the study.
This work was partially funded by the Clinician Scientist Program of the University Arkansas for Medical Sciences, NCATS UL1TR000039, NIGMS P30 GM110702, and NIH/NIA AG12411 awards to Dr. R Cáceda.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethical statement
All participants gave informed written consent. This study was approved by the Douglas Mental Health University Institute research ethics board, and the University of Arkansas for Medical Sciences (UAMS) research ethic board.
All authors declare no conflict of interest.
References
- Beardsall L, Brayne C, 1990. Estimation of verbal intelligence in an elderly community: a prediction analysis using a shortened NART. Br J Clin Psychol. 29, 83–90. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A, 1979. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 47, 343–352. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L, 1974a. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 42, 861–865. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA, 1988. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 56, 893–897. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK 1996. Manual for the Beck depression inventory-II. San Antonio: TX, psychological corporation, p. 38p. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, 1961. An inventory for measuring depression. Arch Gen Psychiatry. 4, 561–571. [DOI] [PubMed] [Google Scholar]
- Beck RW, Morris JB, Beck AT, 1974b. Cross-validation of the Suicidal Intent Scale. Psychol Rep. 34, 445–446. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W, 2003. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 27, 169–190. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Silver W, Gallagher EJ, 2001. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 8, 1153–1157. [DOI] [PubMed] [Google Scholar]
- Cáceda R, Durand D, Cortes E, Prendes-Alvarez S, Moskovciak T, Harvey PD, Nemeroff CB, 2014. Impulsive choice and psychological pain in acutely suicidal depressed patients. Psychosom Med. 76, 445–451. 10.1097/PSY.0000000000000075 [DOI] [PubMed] [Google Scholar]
- Cáceda R, Kordsmeier NC, Golden E, Gibbs HM, Delgado PL, 2017. Differential Processing of Physical and Psychological Pain during Acute Suicidality. Psychother Psychosom. 86, 116–118. 10.1159/000450713 [DOI] [PubMed] [Google Scholar]
- Danziger N, Prkachin KM, Willer JC, 2006. Is pain the price of empathy? The perception of others’ pain in patients with congenital insensitivity to pain. Brain. 129, 2494–2507. 10.1093/brain/awl155 [DOI] [PubMed] [Google Scholar]
- DeWall CN, Chester DS, White DS, 2015. Can acetaminophen reduce the pain of decision-making. Journal of Experimental Social Psychology. 56, 117–120. [Google Scholar]
- Ducasse D, Courtet P, Olié E, 2014. Physical and social pains in borderline disorder and neuroanatomical correlates: a systematic review. Curr Psychiatry Rep. 16, 443 10.1007/s11920-014-0443-2 [DOI] [PubMed] [Google Scholar]
- Ducasse D, Holden RR, Boyer L, Artéro S, Guillaume S, Courtet P, Olié E, 2017. Psychological Pain in Suicidality: A Meta-Analysis. J Clin Psychiatry. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, 2012. The pain of social disconnection: examining the shared neural underpinnings of physical and social pain. Nat Rev Neurosci. 13, 421–434. 10.1038/nrn3231 [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD, 2004. Why rejection hurts: a common neural alarm system for physical and social pain. Trends Cogn Sci. 8, 294–300. 10.1016/j.tics.2004.05.010 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW 2012. Structured Clinical Interview for DSM-IV® Axis I Disorders (SCID-I), Clinician Version, Administration Booklet. New York: American Psychiatric Publishing. [Google Scholar]
- Hamilton M, 1959. The assessment of anxiety states by rating. Br J Med Psychol. 32, 50–55. [DOI] [PubMed] [Google Scholar]
- Hamilton M, 1960. A rating scale for depression. J Neurol Neurosurg Psychiatry. 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RR, Mehta K, Cunningham EJ, McLeod LD, 2001. Development and preliminary validation of a scale of psychache. Canadian Journal of Behavioral Science. 33, 224–232. [Google Scholar]
- Hsu DT, Sanford BJ, Meyers KK, Love TM, Hazlett KE, Wang H, Ni L, Walker SJ, Mickey BJ, Korycinski ST, Koeppe RA, Crocker JK, Langenecker SA, Zubieta JK, 2013. Response of the μ-opioid system to social rejection and acceptance. Mol Psychiatry. 18, 1211–1217. 10.1038/mp.2013.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jollant F, Lawrence NL, Olie E, Guillaume S, Courtet P, 2011. The suicidal mind and brain: A review of neuropsychological and neuroimaging studies. World J Biol Psychiatry. 12, 319–339. 10.3109/15622975.2011.556200 [DOI] [PubMed] [Google Scholar]
- Jollant F, Near J, Turecki G, Richard-Devantoy S, 2017. Spectroscopy markers of suicidal risk and mental pain in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry. 73, 64–71. 10.1016/j.pnpbp.2016.10.005 [DOI] [PubMed] [Google Scholar]
- Li H, Xie W, Luo X, Fu R, Shi C, Ying X, Wang N, Yin Q, Wang X, 2014. Clarifying the role of psychological pain in the risks of suicidal ideation and suicidal acts among patients with major depressive episodes. Suicide Life Threat Behav. 44, 78–88. 10.1111/sltb.12056 [DOI] [PubMed] [Google Scholar]
- Mee S, Bunney BG, Bunney WE, Hetrick W, Potkin SG, Reist C, 2011. Assessment of psychological pain in major depressive episodes. J Psychiatr Res. 45, 1504–1510. 10.1016/j.jpsychires.2011.06.011 [DOI] [PubMed] [Google Scholar]
- Meerwijk EL, Weiss SJ, 2011. Toward a unifying definition of psychological pain. Journal Loss & Trauma. 16, 402–412. [Google Scholar]
- Olie E, Guillaume S, Jaussent I, Courtet P, Jollant F, 2010. Higher psychological pain during a major depressive episode may be a factor of vulnerability to suicidal ideation and act. J Affect Disord. 120, 226–230. 10.1016/j.jad.2009.03.013 [DOI] [PubMed] [Google Scholar]
- Orbach I, Mikulincer M, Sirota P, Gilboa-Schechtman E, 2003. Mental pain: a multidimensional operationalization and definition. Suicide Life Threat Behav. 33, 219–230. [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ, 2011. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 168, 1266–1277. 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC, 1998. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 59 Suppl 20, 22–33;quiz 34. [PubMed] [Google Scholar]
- Shneidman ES, 1993. Suicide as psychache. J Nerv Ment Dis. 181, 145–147. [DOI] [PubMed] [Google Scholar]
- Shneidman ES, 1999. The psychological pain assessment scale. Suicide Life Threat Behav. 29, 287–294. [PubMed] [Google Scholar]
- Tesarz J, Eich W, Treede RD, Gerhardt A, 2016. Altered pressure pain thresholds and increased wind-up in adult patients with chronic back pain with a history of childhood maltreatment: a quantitative sensory testing study. Pain. 157, 1799–1809. 10.1097/j.pain.0000000000000586 [DOI] [PubMed] [Google Scholar]
- Tossani E, 2013. The concept of mental pain. Psychother Psychosom. 82, 67–73. 10.1159/000343003 [DOI] [PubMed] [Google Scholar]
- Trakhtenbrot R, Gvion Y, Levi-Belz Y, Horesh N, Fischel T, Weiser M, Treves I, Apter A, 2016. Predictive value of psychological characteristics and suicide history on medical lethality of suicide attempts: A follow-up study of hospitalized patients. J Affect Disord. 199, 73–80. 10.1016/j.jad.2016.03.054 [DOI] [PubMed] [Google Scholar]
- Troister T, D’Agata MT, Holden RR, 2015. Suicide risk screening: Comparing the Beck Depression Inventory-II, Beck Hopelessness Scale, and Psychache Scale in undergraduates. Psychol Assess. 27, 1500–1506. 10.1037/pas0000126 [DOI] [PubMed] [Google Scholar]
- Troister T, Holden RR, 2012. A two-year prospective study of psychache and its relationship to suicidality among high-risk undergraduates. J Clin Psychol. 68, 1019–1027. 10.1002/jclp.21869 [DOI] [PubMed] [Google Scholar]
- Turecki G, Ernst C, Jollant F, Labonte B, Mechawar N, 2012. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 35, 14–23. 10.1016/j.tins.2011.11.008 [DOI] [PubMed] [Google Scholar]
- Verrocchio MC, Carrozzino D, Marchetti D, Andreasson K, Fulcheri M, Bech P, 2016. Mental Pain and Suicide: A Systematic Review of the Literature. Front Psychiatry. 7, 108 10.3389/fpsyt.2016.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie W, Li H, Luo X, Fu R, Ying X, Wang N, Yin Q, Zou Y, Cui Y, Wang X, Shi C, 2014. Anhedonia and pain avoidance in the suicidal mind: behavioral evidence for motivational manifestations of suicidal ideation in patients with major depressive disorder. J Clin Psychol. 70, 681–692. 10.1002/jclp.22055 [DOI] [PubMed] [Google Scholar]
- Xie W, Li H, Zou Y, Sun X, Shi C, 2017. A suicidal mind tends to maintain less negative information in visual working memory. Psychiatry Res. 10.1016/j.psychres.2017.09.043 [DOI] [PubMed] [Google Scholar]
- Yovell Y, Bar G, Mashiah M, Baruch Y, Briskman I, Asherov J, Lotan A, Rigbi A, Panksepp J, 2016. Ultra-Low-Dose Buprenorphine as a Time-Limited Treatment for Severe Suicidal Ideation: A Randomized Controlled Trial. Am J Psychiatry. 173, 491–498. 10.1176/appi.ajp.2015.15040535 [DOI] [PubMed] [Google Scholar]