Abstract
Background: Many resources are available for adults, but there are few community-based programs for overweight and obese children. Community engagement may be instrumental in overcoming barriers physicians experience in managing childhood obesity. Our objective was to design and test the feasibility of a community-based (YMCA), family-centered, low-cost intervention for overweight and obese children.
Methods: Children 6–11 years over the 85th BMI percentile for age and sex were recruited to YMCA sites in four North Carolina communities. The children had physical activity sessions three times weekly for 3 months (one activity session weekly was family night). The parents received a once-weekly nutrition education class conducted by a registered dietitian using the NC Eat Smart Move More curriculum (10 sessions). Changes in BMI were measured at 3, 6, and 12 months and diet and activity behaviors at 3 and 12 months after baseline.
Results: Significant reductions were observed in BMI percentile for age and BMI z-scores at 3, 6, and 12 months. Improvements occurred in dietary and physical activity behaviors, including drinking fewer sugar-sweetened beverages, spending more time in physically active behaviors, and spending less time in sedentary behaviors. The program was low-cost, and qualitative comments suggest the parents and children benefited from the experience.
Conclusions: This low-cost YMCA-based intervention was associated with BMI reductions and positive nutritional and activity behavior changes, providing an additional strategy for addressing childhood obesity in community settings.
Introduction
One-third of children and adolescents in the United States are overweight or obese, and the dramatic rise in the prevalence of pediatric obesity has been predicted to lead to a decline in overall life expectancy.1,2 Given the large number of children affected, there is an overwhelming need for effective treatments for this population.
The challenges of treating obesity in the office include lack of reimbursement, lack of time, lack of nutrition services, and lack of community resources.3 These barriers have limited the role of primary care providers in addressing the obesity epidemic. Community-based obesity prevention/treatment programs are a potential referral resource for physicians challenged with the increasing number of overweight/obese children and adolescents in their practices. However, the availability, content, and quality of these resources vary significantly by geographic location, patient age, and appropriateness of the intervention for children.4,5
The purpose of this study was to assess the feasibility of a community-based (YMCA), family-centered, low-cost intervention for overweight and obese children.
Methods
Research Design
A survey of local YMCAs was conducted by the North Carolina YMCA to assess interest in participating in the study. On the basis of this survey, children were recruited from pediatric and family practice offices, medical center clinics, schools, and churches to four YMCAs in Chapel Hill, Goldsboro, Raleigh, and Winston-Salem, North Carolina. The children's primary care providers were not involved in the program. However, primary care pediatricians supervised the program at two sites, two general academic pediatricians at another site, and a pediatric endocrinologist at the fourth site. We included youth 6–11 years of age with a BMI for age and sex greater than the 85th percentile, without serious or chronic medical conditions, no dietary or activity restrictions, and with English-speaking parents. The study was approved by the institutional review boards at Duke University Medical Center, the University of North Carolina School of Medicine, and Wake Forest School of Medicine. A flyer describing the program noted a $25.00 registration fee for which the participants received a 3-month family membership at the YMCA. No families were turned away for inability to pay the fee, and they received a full refund if they remained in the program.
Recruitment took place from July to October of 2009, and follow-up was completed in October, 2010. Measurements were recorded at baseline and at 3, 6, and 12 months (Fig. 1). Celebration parties with healthy snacks and sandwiches were held at 3, 6, and 12 months as an incentive for parents to bring the children back for height and weight measurements and to complete a diet and activity questionnaire.
Figure 1.
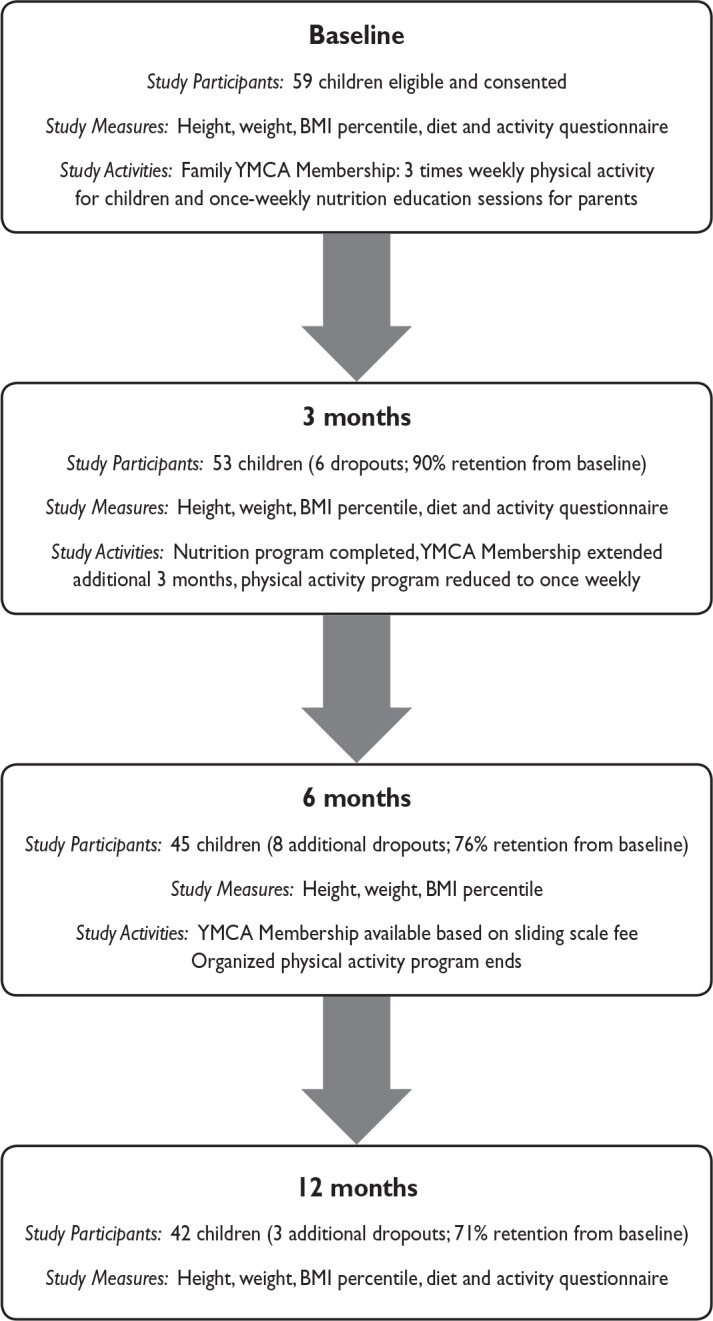
Healthy, Fit, and Strong Program pilot study design.
Measures
Participants were measured and weighed using a portable stadiometer (SECA 214) and electronic scale (SECA 803). Height (to eighths of an inch) and weight (to tenths of a pound) were recorded on a standard form with the date of measurement, date of birth, ethnicity, and sex. BMI was calculated, and BMI percentiles for age and sex determined using the CDC website (www.cdc.gov/growthcharts). Child eating and activity behaviors were assessed with a brief (5- to 10-minute) diet and activity questionnaire (developed by the Principal Investigator) focusing on six behaviors associated with obesity (sugar-sweetened drinks, dining out, fruit and vegetable intake, snacks, physical activity, and TV/screen time). The diet and activity questionnaire was completed by the parents at baseline and at 3 and 12 months. The questionnaire in an expanded format is being used as a screening tool in a large national study with plans to validate this measure at the conclusion of the study.
Intervention
After the parents signed the consent form, families of children enrolled in the program paid the $25.00 commitment fee and received a 3-month family membership at the YMCA. If they remained in the program for 3 months, the family YMCA membership was extended for 3 more months at no additional cost. Those families remaining in the program at 6 months had the $25.00 fee returned. At 12 months, the parents received a $25.00 gift certificate for bringing their child back for height and weight measurements and completing the diet and activity questionnaire.
Physical Activity Program—Children and Parents
The physical activity program for the children took place three times per week at the four YMCA sites, usually from 6 pm to 7 pm. Each site had 2–3 staff members engaged in the program and trained by the YMCA. The YMCA program directors met at study meetings where they could exchange information on their respective programs. The physical activity program was based on having fun, not losing weight. “Family nights” were scheduled once weekly to encourage parents to participate with their children. Activities included soccer, basketball, kickball, dodge ball, races and active games, Zumba and hip-hop dancing, roller skating, and swimming. We intentionally did not use exercise machines or “active” video games so that children could continue similar low-cost family activities at home. After 3 months, the activity program was decreased to once weekly. At 6 months, the organized activity program ended, but parents were encouraged to continue family activities at home and could join the YMCA based on a sliding scale fee.
Nutrition Program—Parents
The nutrition program for the parents consisted of 10 interactive weekly sessions for 1 hour conducted by a registered dietitian. The children did not attend the nutrition curriculum sessions. The curriculum was developed by a North Carolina Eat Smart Move More Panel of Experts and provided by the Nutrition Services Branch of the North Carolina Division of Public Health (www.EatSmartMoveMoreNC.com). It is culturally appropriate for Caucasian, African-American, and Latino families and has been used statewide in Women, Infants, and Children (WIC) clinics. The dietitians were selected by the physician directors or YMCA and were locally based. The curriculum included an instructor manual for the dietitian with sample scripts, key points for discussion, parent handouts, and recipes for each session. Topics included:
Plan, shop, fix and eat (prepare and eat meals at home),
Shop for value (read labels),
Make smart breakfast and lunch choices,
Make smart drink choices,
Smart-size portions,
Make smart choices when eating fast food,
Choose more fruits and vegetables,
Move more every day (increase physical activity),
Limit screen time,
Choose “MyPlate.”
Statistical Considerations
Descriptive statistics (means, standard deviations, frequencies, etc.) are presented for pretreatment participant characteristics and the outcome measures mentioned above. Exact binomial confidence intervals were calculated for the estimated proportions and approximate intervals were calculated for estimated means. BMI was measured at baseline and at 3, 6, and 12 months after the intervention began, and BMI z-scores and percentiles were determined based on age and sex using the CDC website (www.cdc.gov/growthcharts). Repeated measures analysis of variance was used to assess changes in BMI (log transformed) over time, and linear contrasts were used to assess pairwise differences. An unstructured covariance matrix was used to account for the correlation in measures over time. A rank transformation was used for BMI percentile, and a repeated measures model was used to assess changes over time as described for BMI. Parents were asked to record dietary and beverage intakes for their child and the amount of time spent in various active and sedentary activities at baseline, 3 months, and 1 year. Paired t-tests were used to assess changes in these measures over time.
Results
Study Population
Between July and October, 2009, 59 children were recruited who met eligibility criteria. Twenty-five (42%) were 6–8 years and 34 (58%) were 9–11 years old. Thirty-seven (63%) were female; 32 (54%) were African American, 5 (8%) were Hispanic, and 22 (38%) were white. Baseline BMI percentile for age and sex was between the 85th and 94th percentiles for 8 children (14%), between the 95th and 98th percentiles for 25 children (42%), and equal or greater than the 99th percentile for 26 children (44%). The median (range) BMI z-score was 2.19 (1.06–3.51).
Key Results
Feasibility
Recruitment was initially slow because our screening criteria limited eligibility to children between the 85th and 97th BMI percentiles. Recruitment improved when we expanded the criteria to include all children above the 85th percentile. Retention at the four sites at 12 months varied from 45% to 100%. Overall retention at the combined sites was 71%. There were no statistically significant differences between those who did and did not drop out for any characteristics. Average attendance across the four sites was 60% for physical activity sessions and 51% for nutrition sessions
BMI changed significantly over time; and the difference from baseline was significant at 3 and 6 months (p = 0.001 and 0.017, respectively), but not at 1 year (Table 1). The changes in BMI percentile and BMI z-scores from baseline to 3, 6, and 12 months were statistically significant.
Table 1.
Changes in BMI Over Time among Study Participants
| BMI Measure | Baseline (n = 59) Mean (SD) | 3 Months (n = 53) Mean (SD) | 6 Months (n = 45) Mean (SD) | 1 Year (n = 42) Mean (SD) |
|---|---|---|---|---|
| BMI | 28.2 (6.6) | 27.2 (5.7)* | 26.7 (5.4)* | 27.1 (4.8) |
| BMI percentile | 97.5 (2.8) | 97.0 (3.4)** | 96.2 (4.7)** | 95.9 (4.9)** |
| BMI z-score | 2.19 (0.49) | 2.10 (0.50)** | 2.02 (0.52)** | 1.97 (0.52)** |
| Change from baseline | Least squares means (95% CI) | |||
| BMI | −0.45 (−0.70, −0.19) | −0.51 (−0.89, −0.13) | 0.01 (−0.53, 0.55) | |
| BMI percentile | −0.47 (−0.73, −0.21) | −1.04 (−1.60, −0.48) | −1.38 (−2.36, −0.40) | |
| BMI z-score | −0.065 (−0.093, −0.036) | −0.112 (−0.156, −0.068) | −0.152 (−0.216, −0.088) |
p < 0.05. **p < 0.001.
SD, Standard deviation; CI, confidence interval.
Eating and activity behaviors
The number of “fruit” drinks and regular sodas consumed per day decreased significantly from baseline to 3 months [d = −0.39; 95% confidence interval (CI) = −0.80, 0.01, p = 0.05] and (d = −0.22; 95% CI = −0.42, −0.02, p = 0.03), respectively, and 1 year (d = −0.53; 95% CI = −0.99, −0.08, p = 0.02) and (d = −0.52; 95% CI = −0.88, −0.15, p = 0.01), respectively (Table 2). The number of hours per week spent in physical activity at 3 months and 12 months (d = 3.55; 95% CI = 1.00, 6.10, p = 0.01) and (d = 3.6; 95% CI = 1.2, 6.1, p < 0.01) and servings of fruit per day at 12 months (d = 0.41; 95% CI = 0.10, 0.72, p = 0.01) increased significantly. Television viewing (hours/week) decreased significantly at 3 months (d = −3.1; 95% CI = −4.8, −1.4, p < 0.01), but not at 1 year (d = −1.7; 95% CI = −3.8, 0.4, p = 0.11), whereas video games decreased significantly at 1 year (d = −1.7; 95% CI = 3.4, −0.03, p = 0.05). Fast food intake (times/week) decreased significantly at 3 months (d = −1.30; 95% CI = −2.23, −0.37, p = 0.01), but not at 1 year (d = −0.41; 95% CI = −1.79, 0.96, p = 0.55).
Table 2.
Children's Eating and Activity Behaviors Over Time
| Baseline | 3 Months | 1 Year | |||
|---|---|---|---|---|---|
| Behavior | n Mean (SD) | n Mean (SD) | pa | n Mean (SD) | pa |
| Eating habits | |||||
| Fast food out (times/week) | 57 2.75 (2.39) | 42 1.71 (1.40) | 0.01 | 34 2.53 (3.25) | 0.55 |
| Snacks (servings/day) | 46 2.09 (0.86) | 39 2.09 (0.79) | 0.87 | 33 2.33 (0.96) | 0.40 |
| Fruit (servings/day) | 52 1.85 (0.92) | 39 2.13 (0.98) | 0.41 | 34 2.41 (0.89) | 0.01 |
| Vegetables (servings/day) | 52 1.77 (0.88) | 41 2.12 (1.12) | 0.17 | 34 2.18 (0.94) | 0.13 |
| Drinking habits (glasses/day) | |||||
| Juice | 56 1.09 (0.92) | 43 0.95 (0.95) | 0.20 | 34 1.21 (1.27) | 0.61 |
| Fruit drinks | 55 1.16 (1.23) | 42 0.62 (0.96) | 0.05 | 33 0.45 (0.71) | 0.02 |
| Sports drinks | 53 0.34 (0.71) | 41 0.12 (0.33) | 0.21 | 33 0.27 (0.72) | 0.49 |
| Regular soda | 55 0.53 (0.90) | 40 0.28 (0.55) | 0.03 | 34 0.18 (0.46) | 0.01 |
| Sweet tea | 51 0.39 (0.75) | 42 0.29 (0.74) | 0.44 | 34 0.21 (0.59) | 0.84 |
| Any sugar drink | 58 3.31 (2.86) | 43 2.21 (2.35) | 0.02 | 34 2.29 (2.18) | <0.01 |
| Activities (hours/week) | |||||
| Physical activity | 56 11.4 (6.33) | 43 15.0 (7.28) | 0.01 | 34 14.9 (7.27) | <0.01 |
| Watching TV | 57 14.3 (7.09) | 42 11.4 (5.63) | <0.01 | 34 12.2 (6.10) | 0.11 |
| Playing video games | 59 4.95 (5.13) | 42 4.58 (4.19) | 0.85 | 34 3.56 (3.62) | 0.05 |
Assessing change from baseline.
SD, Standard deviation.
Parent Evaluation of Program
The parents completed an evaluation of the program at 3 and 12 months. Thirty-three of 35 parents (94%) said they would recommend the program to other families. Parents were asked to provide ideas for improving the program. Suggestions included increasing the duration of the activity program beyond 3 months, scheduling family activity nights more frequently, providing cooking demonstrations, and including the children in the nutrition education component of the program. A brief evaluation form was also completed by the children, and results were overwhelmingly positive. In many instances, it was the children who were encouraging the parents to bring them to the activity sessions.
Discussion
The purpose of the Healthy, Fit, and Strong Program was to assess the feasibility of delivering a low-cost, family-centered obesity prevention/treatment program through the YMCA, offering nutrition education for the parents and fun activities for the children. We found a significant decrease in BMI z-score (−0.15 units) in the children over the 12-month follow-up period. A change of this magnitude has been related to improvement in total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-C), and insulin levels.6 Significant increases were seen in physical activity, and TV time was reduced. Fruit, but not vegetable, intake was increased. Fruit juice and soda intake decreased.
Forty-four percent of the participants were over the 99th BMI percentile (extreme obesity). Such children are at higher risk of cardiovascular and metabolic complications of obesity.7 Importantly, the children in our study who were >99th BMI percentile at baseline continued to show a significant decrease in BMI z-score at the 12-month follow-up.
Limitations of our study include the small number of participants and a 29% dropout rate over the 12-month follow-up. Because this was a feasibility study, we did not include a control group. Nutritional changes were self-reported and may have been subject to recall bias. Finally, the program was not meant as a substitute for clinical multidisciplinary, intensive treatment programs for extreme obesity at tertiary care centers.
Nutrition education in our study was directed to the parents; children were not included in these sessions. This decision was based on literature documenting parents as the primary source of family behavior change. Golan and Crow8 reported that a family-centered approach targeting solely the parents was more effective in reducing weight in obese 6- to 11-year-old Israeli children at 7-year follow-up than a child-centered approach.
Attendance at education sessions can also influence study outcomes. Wolcott et al.9 noted that the main barrier affecting continued participation in a program was lack of transportation. Other barriers included competing activities such as school sports, parent work schedules, and inconvenient times for the sessions. In our study, the average attendance was 60% for the activity sessions and 51% for nutrition sessions, and the parents reported similar barriers, especially competing schedules.
Program Location and Sustainability
There are over 2600 YMCAs across the United States serving over 20 million people, including 9 million youth under age 18. The YMCAs are the nation's largest provider of child care, afterschool programs, and youth sports.10 The wide reach of the YMCA, their commitment to fitness and health, and the need for more standardized, effective community programs suggest that these sites are natural partners for health improvement interventions.
Our program took place at four YMCAs in North Carolina. However, this program could be conducted in other settings such as community centers, schools, or churches. The low cost, availability of the curriculum on a CD, and simple study design make this a program that easily could be replicated in other communities (see Table 3). Our next step is testing the feasibility of this program in other settings, such as school systems.
Table 3.
Budget per Site for the Healthy, Fit, and Strong Program Pilot Study (Cost Based on 20 Families)
| Items needed | Cost |
|---|---|
| Start-up expenses (estimated) | |
| Curriculum instructor notebook in black and white with CD of all materials or CD only for $1.00 | $40.00 |
| Equipment and games | $400.00 |
| Portable stadiometer (SECA 214) | $200.00 |
| Electronic scale (SECA 803) | $60.00 |
| Total start-up expenses | $700.00 |
| Ongoing expenses | |
| Session handouts for parents and children (black and white printing) | $100.00 ($5.00 per family) |
| Registered dietitian (10 sessions @ $100/session) | $1,000.00 |
| YMCA program staff (weekly activity sessions, 3x/week for 12 weeks) | $450.00 |
| Snacks and celebration parties | $500.00 |
| Total ongoing expenses | $2,050.00 |
| Overall total expenses | $2,750.00 |
Conclusion
Our pilot study results suggest that this basic, low-cost program could be developed to provide a referral source for office-based practitioners seeking a community-based program for prevention and treatment of overweight and moderately obese children.
Acknowledgments
We are grateful to the following individuals for their participation/support in the study: Cameron Graham, M.P.H., Steve Shore, M.S.W., John Rusher, M.D., Christopher Griffin, M.D., Sheila Britt-Smith, R.D., Stephanie Howard, R.D., Emily Ford Yoon M.P.H., R.D., Patricia Andrews, M.P.H., R.D., Phill Morgan, John Richards, Laura Blackwell, Luke Harris, Lisa Weston, Lisa Mischley, and Greg Lee. We thank Karen Klein, M.A., E.L.S. (Research Support Core, Wake Forest University Health Sciences) for editorial contributions. We would also like to thank Rhonda Blaine for her assistance in preparation and submission of the manuscript. We would especially like to thank the NC YMCA and the participating YMCAs for their strong support of this study.
This study was supported by the North Carolina Health and Wellness Trust Fund and the North Carolina Pediatric Society Foundation. Dr. Perrin was supported by an National Institutes of Health Career Development Award (K23-HD051817) during this project.
Data from this manuscript were presented in poster format at the Pediatric Academic Societies Annual Meeting, April 28 to May 1, 2012, Boston, MA.
Author Disclosure Statement
No competing financial interests exist for any of the authors.
References
- 1. Wang Y, Beydoun MA. The obesity epidemic in the United States-gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 2. Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med 2005;352:1138–1145 [DOI] [PubMed] [Google Scholar]
- 3. Perrin EM, Flower KB, Garrett J, et al. Preventing and treating obesity: Pediatricians’ self-efficacy, barriers, resources, and advocacy. Ambul Pediatr 2005;5:150–156 [DOI] [PubMed] [Google Scholar]
- 4. Collins CE, Warren J, Neve M, et al. Measuring effectiveness of dietetic interventions in child obesity: A systematic review of randomized trials. Arch Pediatr Adolesc Med 2006;160:906–922 [DOI] [PubMed] [Google Scholar]
- 5. Atlantis E, Barnes EH, Singh MA. Efficacy of exercise for treating overweight in children and adolescents: A systematic review. Int J Obes (Lond) 2006;30:1027–1040 [DOI] [PubMed] [Google Scholar]
- 6. Kirk S, Zeller M, Claytor R, et al. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res 2005;13:876–882 [DOI] [PubMed] [Google Scholar]
- 7. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 2004;350: 2362–2374 [DOI] [PubMed] [Google Scholar]
- 8. Golan M, Crow S. Targeting parents exclusively in the treatment of childhood obesity: Long term results. Obes Res 2004;12:357–361 [DOI] [PubMed] [Google Scholar]
- 9. Wolcott D, Huberty J, Mcllvain H, et al. Changing health behaviors: Exploring families’ participation in a family-based community intervention for overweight/obese children. Child Obes 2011;7:206–214 [Google Scholar]
- 10. YMCA of USA. Statistical summary, 2009. Available at www.ymca.net/ Last accessed February23, 2012.


