Abstract
Purpose
Individuals with osteoarthritis can experience difficulty walking and poor strength, possibly leading to falls and fractures. Exercise has been found to increase strength and bone mineral density. The purpose of this study was to determine the effects of 6 months of t'ai chi on knee muscle strength, bone mineral density, and fear of falling in older women with osteoarthritis.
Methods
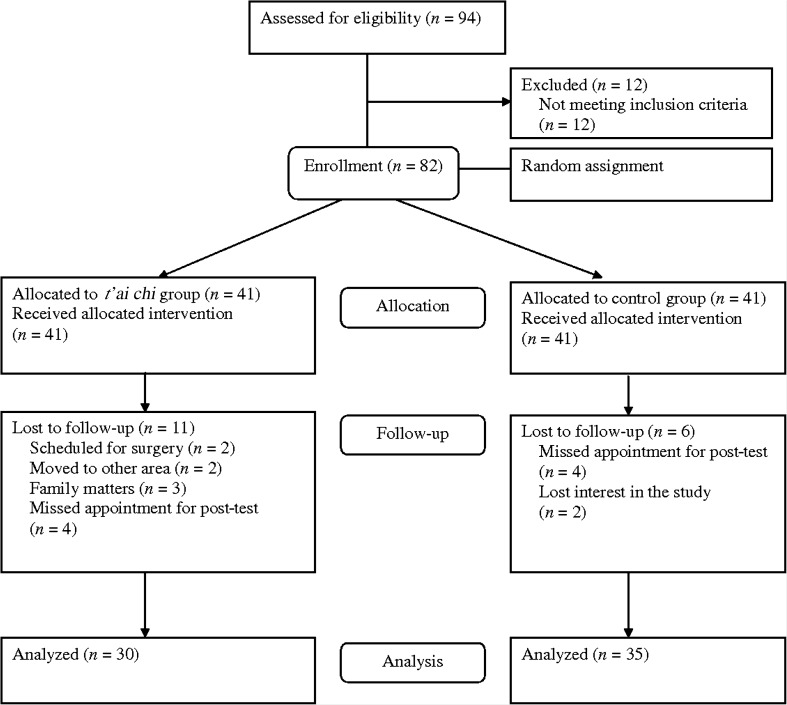
Eighty-two (82) women with osteoarthritis, recruited from outpatient clinics and community health centers, were randomly assigned to either a t'ai chi group and took part in a t'ai chi program, or a control group. Of these, 30 subjects (mean age = 63 years) in the t'ai chi group and 35 (mean age = 61 years) in the control group completed post-test measures at 6 months.
Results
After the 6-month study period, subjects in the t'ai chi program had significantly greater knee extensor endurance (pre- to post-test mean increase = 36.4 W/kg, versus 1.1 W/kg for the controls), and significantly greater bone mineral density in the neck of the proximal femur (mean change = 0.09, versus −0.10 for the controls), Ward's triangle (mean change = 0.04, versus −0.04 for the controls), and trochanter (mean change = 0.07, versus −0.05 for the controls) than the controls. However, knee extensor and flexor strength did not differ significantly between the groups. The fear of falling during daily activities reduced significantly more in the t'ai chi group (mean change = −2.40, versus 0.66 for the controls).
Conclusions
T'ai chi increased knee extensor muscle endurance and bone mineral density in older women with osteoarthritis, and decreased their fear of falling during daily activities. Further study with long-term follow-up is needed to substantiate the role of t'ai chi exercise in the prevention of fall and its related fracture.
Introduction
Osteoarthritis (OA) is one of the most pervasive diseases and is the leading cause of disability worldwide.1 The incidence of OA increases with age, women being more susceptible than men, especially in those older than 50 years.1 Individuals with OA can experience difficulty walking and have a higher relative risk of falling and fall-related fractures.2 OA has been associated with an increase in bone mineral density (BMD); however, this association remains controversial.3 Despite a higher bone density, older women with OA are not protected against osteoporotic fracture, possibly due to knee pain, increased bone resorption with menopause and aging, worsened postural stability, and an increased risk of falls.3–5 Having OA and the associated difficulty walking, together with balance deficit and muscle weakness might increase the risk of falling by threefold.6
One of the most effective prevention strategies for reducing the risk of falling is exercise that focuses on improving muscle strength, balance, and coordination.7 Women, and especially older women with OA, are less likely to participate in any type of physical exercise due to their fear of falling and poor confidence, which leads to deconditioning and loss of function.8 An exercise intervention for those with OA should be pursued judiciously because physical exercise, depending upon its nature, can exert either injurious or beneficial effects on the joints.9
Various forms of exercise have been prescribed for this population, and Sun-style t'ai chi, designed specifically for arthritis, has been considered safe and effective for promoting balance control, flexibility, and bone health in persons with OA.10 Older adults or those with arthritis can safely perform and enjoy t'ai chi exercise because of its slow circular movements with adjustable low-to-moderate intensity that can be performed at any time and place without special equipment.11 Sun-style t'ai chi exercise is characterized by slow, continuous, and gentle motions with a smaller and higher stance (due to agile steps) than other t'ai chi styles, and hence may be more suited to older adults with OA.12
According to a systematic review of clinical trials, 8–16 weeks of t'ai chi training significantly improves balance, flexibility, and knee extensor strength, and reduces the incidence of falls in community-dwelling elderly patients.13 Although there are only a few randomized clinical trials of t'ai chi in those with OA, there is some evidence that this form of exercise is effective for reducing pain and difficulties in performing daily activities,10,14 which represent major risks for falling in this population. In randomized studies, t'ai chi exercise was found to be beneficial for retarding bone loss in postmenopausal women15 and in community-living elderly women.16 T'ai chi might thus reduce the risk of falls, and hence fall-related fractures, in older women with OA. However, there are no published controlled studies of t'ai chi that have examined muscle strength and BMD in this population. The purpose of the present study was therefore to determine the effects of t'ai chi on knee muscle strength and endurance, BMD, and fear of falling in persons with OA.
Methods
Study population
In an experimental design with random assignment, women with OA were recruited from the Hospital of Rheumatic Disease and community health centers while applying the following inclusion criteria: (1) age 55 years or older; (2) clinical and radiographic evidence of OA; (3) no chronic disease or disability that would prevent completion of the t'ai chi program, such as ischemic heart disease or cerebrovascular attack; and (4) no participation in a regular exercise program during the previous year. A rheumatologist (S.C.B.) reviewed medical records to identify patients with OA, using the classification of OA of the knee from the American College of Rheumatology, with osteophytes exhibiting a Kellgren-Lawrence grade of ≥2.17 For those recruited from the community health centers, the diagnosis of OA was validated by the primary physician of the subjects according to the same classification. Figure 1 depicts the screening procedures of the subjects in this study.
FIG. 1.
Screening process and criteria for inclusion in the study.
A required sample size of 35 subjects for each group was estimated using GPower 3.018 for an F-test between two independent samples, with an α of 0.05, an effect size of 0.34, and a power of 0.80. The effect size used was based on a randomized prospective study of t'ai chi for BMD in postmenopausal women.15
After obtaining approval by an internal review board at the university hospital where the research was conducted, potential subjects were recruited by physician's referrals from the hospital outpatient clinic for rheumatic disease and from community health centers. The potential participants were told that they could be assigned either to the exercise group or the self-help management group, and those who were assigned to the self-help management group would have a chance to participate in an exercise program after the study period. After providing written informed consent to participate, the subjects were randomly assigned to either an experimental or a control group using a computer-generated random number. After pretest measures, those in the t'ai chi group exercised twice a week for 3 weeks to learn the t'ai chi form, and then once a week for the remainder of the 6-month study period. The control group received a self-help education program designed for arthritic patients for 2 hours once a month for 6 months. The compliance was high with the mean attendance rate at 93.2% (standard deviation [SD] = 4.6%) for the t'ai chi group, and at 95.7% (SD = 7.3%) for the control group, which was not significant different between the groups. After 6 months of t'ai chi, 30 patients in the experimental (t'ai chi) group and 35 in the control group completed post-test measures, indicating that 20% of the subjects had dropped out of the study.
Intervention
The t'ai chi program was developed specifically for those with arthritis, using 31 forms of Sun-style t'ai chi with qigong breathing exercise.12 To ensure the safety of the participants with OA, t'ai chi movements used the following principles: (1) bending knees with a higher stance, (2) keeping both arms lower than the shoulder, (3) moving forward and backward with following steps, and (4) turning the body with smaller steps.19 Certified t'ai chi instructors led the program, which comprised 10 minutes of warming-up exercise from the joint of the neck to the ankles, 40–45 minutes of t'ai chi, and 5–10 minutes of cooling-down exercise involving stretching the arm and leg muscles and a breathing exercise. Those in the t'ai chi group were also encouraged to practice t'ai chi every day for at least 20 minutes at home. The exercise log was distributed to the participants each week to record the amount of time or frequency they performed t'ai chi every day, and returned at the following session. The research personnel closely monitored the exercise log every week and called each subject during the week to ensure that the participants practiced t'ai chi regularly at home.
Subjects in the control group participated in a self-help education program 2 hours once a month for 6 months, which has been developed for patients with arthritis based on the Arthritis Self-Management Program.20 This program has been used in Korea since 1997 to enhance the individual's self-management skills and knowledge through increasing self-efficacy.21 The program comprised (1) principles of the self-help program and goal setting, (2) relaxation and flexibility exercise, (3) endurance and strengthening exercise, (4) prevention of osteoporosis and energy conservation, (5) pain management and folk medicine, and (6) medication and self-control methods. The participants in the control group were encouraged to apply the self-management skills to their daily activities at home, and the research personnel contacted each individual in the control group prior to the monthly session by phone to assess their health status and the performance of self-management skills based on the self-management protocol, and to ensure their participation in the following session. Most of those in the control group (95.7%) completed all six sessions of the self-management program.
Outcome assessment
Outcome variables for knee muscle strength and endurance, BMD, and fear of falling were measured at before commencement of the study (pretest) and after the 6-month study period (post-test). An exercise specialist at a university hospital sports center conducted the outcome measurements while being blind to the group assignment. Demographic information and the fear-of-falling scale were obtained during interviews by trained research assistants.
Knee muscle strength and endurance
Knee muscle strength and endurance were measured bilaterally at speeds of 60°/sec and 180°/sec, respectively, using an isokinetic dynamometer (Cybex 770, Lumex, Ronkonkoma, NY). Subjects were positioned with 90° hip flexion, with their hands resting on the arms of the dynamometer. The length of the dynamometer arm, which was fastened to the distal portion of the tibia by a Velcro strap, was adjusted to the length of the subject's leg. The subjects practiced isokinetic movements in submaximal repetitions to familiarize themselves with the equipment before the actual measurements were made. Verbal encouragement was given during the test performance. Knee extensor and flexor muscle strength are presented as peak torque normalized to body weight (Nm/kg). Knee extensor and flexor muscle endurance are presented as average power normalized to body weight (W/kg) at 180°/sec. The scores from the right and left knees were added as a measure of lower body strength in terms of the strength and endurance of knee flexion and extension.
Bone mineral density
The BMD of the left proximal femur was measured by dual-energy x-ray absorptiometry (DEXA) (GE Luna PIXImus, Lunar Corporation, Madison, WI) for the neck, Ward's triangle, and trochanter. DEXA was considered a precise measure for BMD for the conventional clinical regions of interest such as the femoral neck.22 The standard T score for BMD (i.e., a comparison of a patient's BMD to that of a healthy 30-year-old of the same sex and ethnicity) was used for the analysis. To ensure the accuracy of the DEXA system, the quality control measurement was run to pass a calibration procedure at the beginning of each-day measurement according to the PIXImus series operators manual. After the calibration, all required information of each individual (birth date, weight and height, sex and ethnicity, ID number) was added at the main screen of the program prior to the measurement. The BMD was measured according to the standard protocol by the specialist at the hospital lab, who was blind to the group assignment.
Fear of falling
The 11-item Korean version of the Survey of Activities and Fear of Falling in the Elderly was used.23 Subjects rated their fear of falling as a result of performing daily activities from 0 (“not at all worried”) to 3 (“very worried”). Cronbach's α was 0.91 for the original study22 and 0.91 for the Korean version of the scale.24
Statistical analysis
Data were analyzed using SPSSWIN V.15 (SPSS Inc., Chicago, IL). Descriptive statistics were used for demographics and outcome variables. Independent t tests were used to assess significant group differences in baseline measures. Analysis of covariance was used to compare the group differences at the post-test after adjusting for the baseline measures.
Results
Demographic characteristics of subjects
The mean age of the subjects and their duration of suffering from OA were 62 years and 3 years (range: 6 months–13 years), respectively, and they had a mean of 12 years of education. Most were married (n = 51, 78.5%), and only 9% (n = 6) of the subjects were still employed. More than half (n = 39) reported other chronic diseases beside OA, and about 70% (n = 49) of the subjects performed their daily activities with assistance. About 42% (n = 27) of the subjects perceived their health as either poor or very poor. There were no significant group differences in the demographic data (Table 1).
Table 1.
Demographic Characteristics of the Subjects by Group
| T'ai chi (n = 30) | Control (n = 35) | ||||
|---|---|---|---|---|---|
| Variable | Mean (SD) | Mean (SD) | t test | p | |
| Age (years) | 63.03 (7.27) | 61.20 (7.96) | 0.97 | 0.33 | |
| Time since the diagnosis (months) | 45.23 (46.33) | 26.42 (31.64) | 1.87 | 0.06 | |
| Education (years) | 12.73 (2.96) | 11.54 (3.21) | 1.54 | 0.12 | |
| Admission frequency | 1.46 (2.62) | 0.91 (1.19) | 1.11 | 0.26 | |
| Frequency (%) | Frequency (%) | χ2 | P | ||
|---|---|---|---|---|---|
| Marital status | Married | 25 (83.3) | 26 (74.3) | 0.78 | 0.54 |
| Other | 5 (16.7) | 9 (25.7) | |||
| Economic status | High | 1 (3.3) | 1 (2.9) | 1.24 | 0.58 |
| Middle | 26 (86.7) | 27 (77.1) | |||
| Low | 3 (10.0) | 7 (20.0) | |||
| Employed | No | 27 (90.0) | 32 (91.4) | 0.03 | 0.84 |
| Yes | 3 (10.0) | 3 (8.6) | |||
| Chronic disease | No | 15 (50.0) | 11 (31.4) | 2.32 | 0.13 |
| Yes | 15 (50.0) | 24 (68.6) | |||
| Current activities of daily living | Independent | 9 (30.0) | 7 (20.0) | 2.41 | 0.29 |
| Need assistance | 21 (70.0) | 26 (74.3) | |||
| Dependent | 0 (0) | 2 (5.7) | |||
| Perceived health | Very poor | 3 (10.0) | 3 (8.6) | 2.06 | 0.35 |
| Poor | 7 (23.3) | 14 (40.0) | |||
| Good | 20 (66.7) | 18 (51.4) |
SD, standard deviation.
Group comparisons for baseline measures
Group comparisons at the pretest revealed that the outcome variables were not significantly different, supporting similar distributions between the groups. Knee strength and endurance were similar between the groups. The subjects were mostly in an osteopenic state, with T scores between −0.78 and −2.31. There were no significant differences between the groups with regard to BMD T scores of the femoral neck, Ward's triangle, and trochanter. Fear of falling also did not differ significantly between the groups (Table 2).
Table 2.
Mean Group Comparisons of Knee Muscle Strength, Bone Mineral Density, and Fear of Falling
| Pretest | Posttest | |||||
|---|---|---|---|---|---|---|
| Variable | T'ai chi (n = 30) Mean (SD) |
Control (n = 35) Mean (SD) |
T'ai chi (n = 30) Mean (SD) |
Control (n = 35) Mean (SD) |
Fa | P |
| Knee strength (Nm/kg) | ||||||
| Flexor | 120.1 (35.8) | 116.9 (26.1) | 129.5 (40.1) | 123.9 (29.2) | 0.26 | 0.60 |
| Extensor | 222.5 (64.2) | 230.0 (54.3) | 232.5 (67.0) | 229.3 (57.2) | 1.69 | 0.19 |
| Knee endurance (W/kg) | ||||||
| Flexor | 106.2 (44.3) | 103.3 (36.5) | 117.3 (44.2) | 117.4 (52.5) | 0.06 | 0.80 |
| Extensor | 223.0 (83.2) | 247.7 (73.3) | 259.4 (87.4) | 248.8 (74.9) | 6.67 | 0.01 |
| Bone mineral density (T score) | ||||||
| Neck | −1.49 (1.05) | −1.32 (0.78) | −1.40 (1.01) | −1.42 (0.74) | 17.32 | <0.01 |
| Ward's triangle | −2.27 (1.14) | −2.31 (0.76) | −2.22 (1.19) | −2.37 (0.72) | 5.68 | 0.02 |
| Trochanter | −0.80 (1.03) | −0.78 (0.78) | −0.73 (1.06) | −0.83 (0.72) | 7.36 | <0.01 |
| Fear of falling | 23.06 (6.13) | 23.45 (5.27) | 20.66 (6.16) | 24.11 (5.60) | 6.40 | 0.01 |
Analysis of covariance with pretest scores as covariates.
SD, standard deviation.
Group comparisons of outcomes at post-test
After controlling for pretest measures (Table 2), the strength (Nm/kg) of the knee flexors and knee extensors did not differ significantly between the t'ai chi and control groups. In contrast, muscle endurance in the knee extensors but not in the knee flexors was significantly higher in the t'ai chi group (mean change from 223.0 to 259.4, versus 247.7 to 248.8 for the controls, F = 6.67, p = 0.01).
The change in the BMD over the 6-month study period was significantly higher in the t'ai chi group than in the group in the femoral neck (mean change = 0.09, versus −0.10 for the controls, F = 17.32, p < 0.01), Ward's triangle (mean change = 0.04, versus −0.04 for the controls, F = 5.68, p = 0.02), and trochanter (mean change = 0.07, versus −0.05 for the controls, F = 7.36, p < 0.01). Over the 6-month study period, T scores improved by 2% (Ward's triangle), 6% (neck), and 8% (trochanter) in the t'ai chi group, while the control group showed slightly decreased T scores in all areas.
The fear of falling during daily activities decreased significantly in the t'ai chi group (mean change = −2.40, SD = 5.54) but remained unchanged or even slightly increased in the control group (mean change = 0.65, SD = 6.08).
Discussion
The major obstacle to fall prevention for individuals with OA has been recognized as instability affecting their ability to function that results from quadriceps muscle weakness, pain, and altered neuromuscular control.25 In older women with OA, our 6-month Sun-style t'ai chi exercise program produced significantly greater knee extensor muscle endurance and BMD of the proximal femur, and less fear of falling during daily activities than the controls (educational group). Muscle strengthening is a key component of exercise for OA, but traditional muscle-strengthening exercise might not be appropriate for this population. A meta-analysis of exercise interventions for arthritis revealed that balance exercise, including t'ai chi, had the most significant impact on lowering fall risk.7
Numerous investigators have focused on the mechanisms underlying t'ai chi to explain how it could reduce fall-related risks in this population. The slow and controlled body movements of t'ai chi require continuous knee flexion and extension during the weight-bearing phase of the movement, and thus increase isokinetic strength in the knee extensors.26 However, in the present study isokinetic strength was not greater in the t'ai chi group, but muscle endurance of the knee extensors was significantly higher. This is consistent with the findings of a study by Tseng and colleagues,27 who compared muscle activation profiles of the lower extremities between t'ai chi stepping and normal gait. Using electromyography, they found that muscle activity in the knee extensors was higher during t'ai chi stepping than during normal gait.27 More importantly, greater isokinetic knee extensor strength has been associated with higher postural stability26 and improved movement accuracy after practicing t'ai chi.28
The t'ai chi participants in this study showed significantly greater T scores of the proximal femur at 6 months than the participants in the control (education) group. Previous randomized trials of t'ai chi found a significantly smaller loss of BMD in the hip in elderly women after 12 months of t'ai chi,16 and in the weight-bearing bones of postmenopausal women.29 Older women with OA are a high-risk group for fracture because those with knee OA have an even lower hip BMD on the affected leg,30 and increased bone resorption after menopause.5 The increase in BMD observed in the early stages of OA patients was not considered a protective factor for overall facture risk for this population.31 In previous studies, the duration of t'ai chi has been varied from 6 months to 12 months to induce beneficial effects on BMD, while the effects were not consistent across the population due to potential variation of the intensity of t'ai chi.15,16 In Woo's study, the t'ai chi was beneficial in retarding bone loss in elderly women who are likely to be physically more frail, while it showed no benefit to men with regard to BMD.16
Although empirical evidence of the impact of t'ai chi on BMD is limited by the quantity and quality of research to date,32 previous randomized studies have shown the positive effects of relatively shorter duration of exercise on BMD (assessed by DEXA) in various populations. After participating in a high-intensity resistance exercise for 6 months, 35 postmenopausal women improved the lumbar BMD (1.03%) compared to the randomized control group.33 The healthy elderly men with normal BMD also showed improved BMD (p < 0.05) of the proximal femur (Ward's triangle) after 16 weeks of resistance exercise training.34 A systematic review revealed that the duration of weight-bearing exercise required at least 4–8 months for a result of less bone loss, and over 9 months or longer for an increase in BMD in postmenopausal women as compared to the control group.35 Therefore, the frail elderly, such as older women with OA, could also benefit from strength exercise or weight-bearing exercise to help preserve bone density by engaging in moderate intensity exercise 2–5 times a week lasting from 45 to 70 minutes a session for at least 4 months or longer.35
The underlying mechanism of t'ai chi to induce beneficial effects on bone health could be understood by considering characteristics of t'ai chi as a weight-bearing exercise. T'ai chi increases weight bearing, which might contribute to a greater BMD. The foot–floor impact force is about 2–4 times lower for t'ai chi than during normal walking36 due to the coordinated activation of the lower extremities.37 While maintaining a low dynamic impact to the foot, t'ai chi movements involve multiple loading and unloading patterns with full weight-bearing movement.37 T'ai chi movement involves maintaining knee flexion while moving in various directions, and is associated with larger peak shear forces and larger peak moments in the lower-extremity joints when compared to normal gait.36 The biomechanics of t'ai chi might explain the improved BMD of the t'ai chi participants in the present study, but further studies are needed to confirm these effects in older women with OA.
Fear of falling is a fundamental health problem in elderly people with or without a history of falling for maintaining their physical independence,38 and it ultimately limits the performance of daily activities.39 Improvement in confidence regarding avoiding falls has been associated with balance and mobility as independent risk factors for falls in older women, and has become a target of intervention programs for fall prevention.40 In the present study, the fear of falling after 6 months was lower in the t'ai chi group than in the control group. In a randomized fall-prevention study involving 49 community-dwelling elderly, an 8-week t'ai chi program also improved balance and reduced fear of falling.41 Further study is warranted to assess the effects of t'ai chi on fall prevention, while also accounting for fall risk factors such as balance, muscle strength, and BMD.
The Sun-style t'ai chi program designed for patients with arthritis in the present study was simple and easy to learn for older adults with OA. Participants were able to learn the basic 12 movements in 3 weeks (six sessions), and therefore a 6-month study period could be long enough for them to feel comfortable practicing t'ai chi at home in addition to the supervised session. The positive changes in knee muscle endurance and BMD of the hip found in the present study could reduce the risk of falls and fractures, while reducing the fear of falling during daily activities could increase the independence of older adults with OA.
The results of the present study should be interpreted with caution. The small sample size along with the presence of within-group variability might explain insignificant findings in some outcome measures. Moreover, dropout rates of 24% and 15% for the t'ai chi and control (education) group, respectively, could have produced biased findings. Although compliance (attendance rates) during the study period was high for both groups, the different levels of face time resulting in more psychosocial interactions with the t'ai chi group may have impacted outcomes, and may contribute to observed group differences. The findings of the study show the performance of t'ai chi exercise is beneficial for retarding bone loss in weight-bearing bones in women with OA, yet further study with long-term follow-up is needed to substantiate the role of t'ai chi exercise in the prevention of fall and its related fracture.
Disclosure Statement
No competing financial interests exist.
References
- 1.CDC. Arthritis. National Centers for Chronic Disease Prevention and Health Promotion. 2008. www.cdc.gov/arthritis/arthritis/osteoarthritis.htm. [May 14;2008 ]. www.cdc.gov/arthritis/arthritis/osteoarthritis.htm
- 2.Tinetti ME. Gordon C. Sogolow E, et al. Fall-risk evaluation and management: Challenges in adopting geriatric care practices. Gerontologist. 2006;46:717–725. doi: 10.1093/geront/46.6.717. [DOI] [PubMed] [Google Scholar]
- 3.Arden NK. Griffiths GO. Hart DJ, et al. The association between osteoarthritis and osteoporotic fracture: The Chingford Study. Br J Rheumatol. 1996;35:1299–1304. doi: 10.1093/rheumatology/35.12.1299. [DOI] [PubMed] [Google Scholar]
- 4.Jones G. Nguyen T. Sambrook PN, et al. Osteoarthritis, bone density, postural stability, and osteoporotic fractures: A population based study. J Rheumatol. 1995;22:921–925. [PubMed] [Google Scholar]
- 5.Bettica P. Cline G. Hart DJ, et al. Evidence for increased bone resorption in patients with progressive knee osteoarthritis: Longitudinal results from the Chingford study. Arthritis Rheum. 2002;46:3178–3184. doi: 10.1002/art.10630. [DOI] [PubMed] [Google Scholar]
- 6.Guideline for the prevention of falls in older persons: American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001;49:664–672. [PubMed] [Google Scholar]
- 7.Simkin B. Even Frail Elderly Patients Can Benefit from Exercise. www.cmellc.com/geriatrictimes/g020831.html. [Sep 20;2008 ];Geriatric Times. 2002 3:1–5. [Google Scholar]
- 8.Messinger-Rapport BJ. Thacker HL. Prevention for the older woman. Mobility: A practical guide to managing osteoarthritis and falls. Part 6. Geriatrics. 2003;8:22–29. [PubMed] [Google Scholar]
- 9.Manninen P. Riihimaki H. Heliovaara M. Suomalainen O. Physical exercise and risk of severe knee osteoarthritis requiring arthroplasty. Rheumatology (Oxford) 2001;40:432–437. doi: 10.1093/rheumatology/40.4.432. [DOI] [PubMed] [Google Scholar]
- 10.Song R. Lee EO. Lam P. Bae SC. Effects of t'ai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: A randomized clinical trial. J Rheumatol. 2003;30:2039–2044. [PubMed] [Google Scholar]
- 11.Choi JH. Moon JS. Song R. Effects of Sun-style t'ai chi exercise on physical fitness and fall prevention in fall-prone older adults. J Adv Nurs. 2005;51:150–157. doi: 10.1111/j.1365-2648.2005.03480.x. [DOI] [PubMed] [Google Scholar]
- 12.Lam P. Horstman J. Overcoming Arthritis: How to Relieve Pain and Restore Mobility Through a Unique T'ai Chi Program. London, UK: Dorling Kindersley; 2002. [Google Scholar]
- 13.Wang C. Collet JP. Lau J. The effect of t'ai chi on health outcomes in patients with chronic conditions: A systematic review. Arch Intern Med. 2004;64:493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 14.Lee MS. Pittler MH. Ernst E. T'ai chi for osteoarthritis: A systematic review. Clin Rheumatol. 2008;27:211–218. doi: 10.1007/s10067-007-0700-4. [DOI] [PubMed] [Google Scholar]
- 15.Chan K. Qin L. Lau M, et al. A randomized, prospective study of the effects of t'ai chi chun exercise on bone mineral density in postmenopausal women. Arch Phys Med Rehabil. 2004;85:717–722. doi: 10.1016/j.apmr.2003.08.091. [DOI] [PubMed] [Google Scholar]
- 16.Woo J. Hong A. Lau E. Lynn H. A randomised controlled trial of t'ai chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing. 2007;36:262–268. doi: 10.1093/ageing/afm005. [DOI] [PubMed] [Google Scholar]
- 17.Altman R. Asch E. Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 18.Erdfelder E. Faul F. Buchner A. GPOWER: A general power analysis program. Behav Res Methods Instrum Comput. 1996;28:1–11. [Google Scholar]
- 19.Song R. Lee EO. Lam P. Bae SC. Effects of a Sun-style t'ai chi exercise on arthritic symptoms, motivation and the performance of health behaviors in women with osteoarthritis. J Korean Acad Nurs. 2007;37:249–256. doi: 10.4040/jkan.2007.37.2.249. [DOI] [PubMed] [Google Scholar]
- 20.Lorig KR. Arthritis self-management: A patient education program. Rehabil Nurs. 1982;7:16–20. doi: 10.1002/j.2048-7940.1982.tb02272.x. [DOI] [PubMed] [Google Scholar]
- 21.Lee EO. Park SY. Kim JI, et al. The effects of self-help education increasing self efficacy on the health promotion for the arthritis patients. J Muscle Joint Health. 1997;4:1–14. [Google Scholar]
- 22.Sievanen H. Oja P. Vuori I. Precision of dual-energy x-ray absortiometry in determining bone mineral density and content of various skeletal sites. J Nucl Med. 1991;33:1137–1142. [PubMed] [Google Scholar]
- 23.Lachman ME. Howland J. Tennstedt S, et al. Fear of falling and activity restriction: The survey of activities and fear of falling in the elderly (SAFE) J Gerontol B Psychol Sci Soc Sci. 1998;53:43–50. doi: 10.1093/geronb/53b.1.p43. [DOI] [PubMed] [Google Scholar]
- 24.Sohng KY. Moon JS. A survey on activities and fear of falling in the home-dwelling elderly in Seoul and Gyonggi-do. J Korean Community Nurs. 2008;14:157–166. [Google Scholar]
- 25.Bennell K. Hinman R. Exercise as a treatment for osteoarthritis. Curr Opin Rheumatol. 2005;17:634–640. doi: 10.1097/01.bor.0000171214.49876.38. [DOI] [PubMed] [Google Scholar]
- 26.Wu G. Zhao F. Zhou X. Wei L. Improvement of isokinetic knee extensor strength and reduction of postural sway in the elderly from long-term t'ai chi exercise. Arch Phys Med Rehabil. 2002;83:1364–1369. doi: 10.1053/apmr.2002.34596. [DOI] [PubMed] [Google Scholar]
- 27.Tseng SC. Liu W. Finley M. McQuade K. Muscle activation profiles about the knee during t'ai-chi stepping movement compared to the normal gait step. J Electromyogr Kinesiol. 2007;17:372–380. doi: 10.1016/j.jelekin.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Christou EA. Yang Y. Rosengren KS. Taiji training improves knee extensor strength and force control in older adults. J Gerontol A Biol Sci Med Sci. 2003;58:763–766. doi: 10.1093/gerona/58.8.m763. [DOI] [PubMed] [Google Scholar]
- 29.Qin L. Au S. Choy W, et al. Regular t'ai chi chuan exercise may retard bone loss in postmenopausal women: A case–control study. Arch Phys Med Rehabil. 2002;83:1355–1359. doi: 10.1053/apmr.2002.35098. [DOI] [PubMed] [Google Scholar]
- 30.Goerres GW. Hauselmann HJ. Seifert B, et al. Patients with knee osteoarthritis have lower total hip bone mineral density in the symptomatic leg than in the contralateral hip. J Clin Densitom. 2005;8:484–487. doi: 10.1385/jcd:8:4:484. [DOI] [PubMed] [Google Scholar]
- 31.Arden NK. Crozier S. Smith H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis Rheum. 2006;55:610–615. doi: 10.1002/art.22088. [DOI] [PubMed] [Google Scholar]
- 32.Wayne PM. Kiel DP. Krebs DE, et al. The effects of t'ai chi on bone mineral density in postmenopausal women: A systematic review. Arch Phys Med Rehabil. 2007;88:673–680. doi: 10.1016/j.apmr.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 33.Yarasheski KE. Campbell JA. Kohrt WM. Effect of resistance exercise and growth hormone on bone density in older men. Clin Endocrinol. 1997;47:223–229. doi: 10.1046/j.1365-2265.1997.2461060.x. [DOI] [PubMed] [Google Scholar]
- 34.Dornemann TM. McMurray RC. Renner JB. Anderson JJB. Effects of high-intensity resistance exercise on bone mineral density and muscle strength of 40-50-year-old women. J Sports Med Phys Fitness. 1997;37:246–251. [PubMed] [Google Scholar]
- 35.Zehnacker CH. Bemis-Dougherty A. Effect of weighed exercise on bone mineral density in postmenopausal women: A systematic review. J Geriatr Phys Ther. 2007;30:79–88. doi: 10.1519/00139143-200708000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Wu G. Millon D. Joint kinetics during t'ai chi gait and normal walking gait in young and elderly t'ai chi chuan practitioners. Clin Biomech (Bristol, Avon) 2008;23:787–795. doi: 10.1016/j.clinbiomech.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Wu G. Hitt J. Ground contact characteristics of t'ai chi gait. Gait Posture. 2005;22:32–39. doi: 10.1016/j.gaitpost.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 38.Liu-Ambrose T. Khan KM. Eng JJ, et al. Balance confidence improves with resistance or agility training: Increase is not correlated with objective changes in fall risk and physical abilities. Gerontology. 2004;50:373–382. doi: 10.1159/000080175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Legters K. Fear of falling. Phys Ther. 2002;82:264–272. [PubMed] [Google Scholar]
- 40.Liu-Ambrose T. Khan KM. Donaldson MG, et al. Falls-related self-efficacy is independently associated with balance and mobility in older women with low bone mass. J Gerontol A Biol Sci Med Sci. 2006;61:832–838. doi: 10.1093/gerona/61.8.832. [DOI] [PubMed] [Google Scholar]
- 41.Zhang JG. Ishikawa-Takata K. Yamazaki H, et al. The effects of t'ai chi chuan on physiological function and fear of falling in the less robust elderly: An intervention study for preventing falls. Arch Gerontol Geriatr. 2006;42:107–116. doi: 10.1016/j.archger.2005.06.007. [DOI] [PubMed] [Google Scholar]