Abstract
Background
To limit long‐term sick leave and associated consequences, insurers, healthcare providers and employers provide programmes to facilitate disabled people's return to work. These programmes include a variety of coordinated and individualised interventions. Despite the increasing popularity of such programmes, their benefits remain uncertain. We conducted a systematic review to determine the long‐term effectiveness of return‐to‐work coordination programmes compared to usual practice in workers at risk for long‐term disability.
Objectives
To assess the effects of return‐to‐work coordination programmes versus usual practice for workers on sick leave or disability.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 11), MEDLINE, Embase, CINAHL and PsycINFO up to 1 November 2016.
Selection criteria
We included randomised controlled trials (RCTs) that enrolled workers absent from work for at least four weeks and randomly assigned them to return‐to‐work coordination programmes or usual practice.
Data collection and analysis
Two review authors independently screened titles, abstracts and full‐text articles for study eligibility; extracted data; and assessed risk of bias from eligible trials. We contacted authors for additional data where required. We conducted random‐effects meta‐analyses and used the GRADE approach to rate the quality of the evidence.
Main results
We identified 14 studies from nine countries that enrolled 12,568 workers. Eleven studies focused on musculoskeletal problems, two on mental health and one on both. Most studies (11 of 14) followed workers 12 months or longer. Risk of bias was low in 10 and high in 4 studies, but findings were not sensitive to their exclusion.
We found no benefits for return‐to‐work coordination programmes on return‐to‐work outcomes.
For short‐term follow‐up of six months, we found no effect on time to return to work (hazard ratio (HR) 1.32, 95% confidence interval (CI) 0.93 to 1.88, low‐quality evidence), cumulative sickness absence (mean difference (MD) −16.18 work days per year, 95% CI −32.42 to 0.06, moderate‐quality evidence), the proportion of participants at work at end of the follow‐up (risk ratio (RR) 1.06, 95% CI 0.86 to 1.30, low‐quality evidence) or on the proportion of participants who had ever returned to work, that is, regardless of whether they had remained at work until last follow‐up (RR 0.87, 95% CI 0.63 to 1.19, very low‐quality evidence).
For long‐term follow‐up of 12 months, we found no effect on time to return to work (HR 1.25, 95% CI 0.95 to 1.66, low‐quality evidence), cumulative sickness absence (MD −14.84 work days per year, 95% CI −38.56 to 8.88, low‐quality evidence), the proportion of participants at work at end of the follow‐up (RR 1.06, 95% CI 0.99 to 1.15, low‐quality evidence) or on the proportion of participants who had ever returned to work (RR 1.03, 95% CI 0.97 to 1.09, moderate‐quality evidence).
For very long‐term follow‐up of longer than 12 months, we found no effect on time to return to work (HR 0.93, 95% CI 0.74 to 1.17, low‐quality evidence), cumulative sickness absence (MD 7.00 work days per year, 95% CI −15.17 to 29.17, moderate‐quality evidence), the proportion of participants at work at end of the follow‐up (RR 0.94, 95% CI 0.82 to 1.07, low‐quality evidence) or on the proportion of participants who had ever returned to work (RR 0.95, 95% CI 0.88 to 1.02, low‐quality evidence).
We found only small benefits for return‐to‐work coordination programmes on patient‐reported outcomes. All differences were below the minimal clinically important difference (MID).
Authors' conclusions
Offering return‐to‐work coordination programmes for workers on sick leave for at least four weeks results in no benefits when compared to usual practice. We found no significant differences for the outcomes time to return to work, cumulative sickness absence, the proportion of participants at work at end of the follow‐up or the proportion of participants who had ever returned to work at short‐term, long‐term or very long‐term follow‐up. For patient‐reported outcomes, we found only marginal effects below the MID. The quality of the evidence ranged from very low to moderate across all outcomes.
Plain language summary
Effect of return‐to‐work coordination programmes for workers on sick leave
What is the aim of this review?
The aim of this review was to compare the effect of return‐to‐work coordination programmes to usual practice in workers on sick leave or disability.
Key messages
We found that return‐to‐work coordination programmes had no effects compared to usual practice on return‐to‐work outcomes. These outcomes were time to return to work, cumulative sickness absence, the proportion of workers at work at the end of the follow‐up and the proportion who had ever returned to work. We found no benefits in the short term, long term or very long term.
We found only small benefits in patient‐reported outcomes. All these effects were smaller than the so‐called minimal clinically important difference.
What was studied in the review?
Returning long‐term sick‐leave workers back to work is important for society, employers and certainly for workers themselves. Possible interventions for this purpose are return‐to‐work coordination programmes, also described as case management or collaborative care. These programmes involve a number of health professionals collaborating with the workers to help them overcome their incapacity to work. Return‐to‐work coordination programmes vary in duration and design. In general, they include an assessment of the obstacles impeding a return to work and an individualised plan to eliminate barriers and return workers to employment. Treatment components may include counselling, physical or occupational therapy, and specialist care.
Return‐to‐work coordination programmes require substantial resources. However, it is uncertain how effective they are.
What are the main results of the review?
We included 14 randomised controlled trials involving 12,568 workers with musculoskeletal or mental health problems. Workers had to be on sick leave for a minimum of four weeks.
At short‐term follow‐up of six months, return‐to‐work coordination programmes may make little or no difference to time to return to work (low‐quality evidence), probably make little or no difference to cumulative sickness absence (moderate‐quality evidence), may make little or no difference to the proportion of participants at work at end of the follow‐up (low‐quality evidence). Finally, we are uncertain whether the programmes improve the proportion of participants who had ever returned to work as the quality of the evidence has been assessed as very low.
At long‐term follow‐up of 12 months, return‐to‐work coordination programmes may make little or no difference to time to return to work, cumulative sickness absence or the proportion of participants at work at end of the follow‐up (all low‐quality evidence) and they probably make little or no difference to the proportion of participants who had ever returned to work (moderate‐quality evidence).
At very long‐term follow‐up of longer than 12 months, return‐to‐work coordination programmes may make little or no difference to time to return to work (low‐quality evidence), probably make little or no difference to cumulative sickness absence (moderate‐quality evidence), and may make little or no difference to the proportion of participants at work at end of the follow‐up and to the proportion of participants who had ever returned to work (both low‐quality evidence).
We found only small benefits in patient‐reported outcomes including pain, ability to function, depression and anxiety. All these effects were smaller than the so‐called minimal clinically important difference.
As we found so much low‐ and very low‐quality evidence it means that new research is likely to change the results.
How up‐to‐date is this review?
We searched scientific literature until 1 November 2016.
Summary of findings
Summary of findings for the main comparison. Return to work coordination programmes compared to usual practice for improving return to work in workers on sick leave.
| Return to work coordination programmes compared to usual practice for improving return to work in workers on sick leave | |||||
| Patient or population: workers on sick leave Intervention: return‐to‐work coordination programmes Comparison: usual practice | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with usual practice | Risk with return‐to‐work coordination programmes | ||||
| Time to return to work ‐ short‐term follow‐up: 6 months |
— | — | HR 1.32 (0.93 to 1.88) | 161 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b |
| Time to return to work ‐ long‐term follow‐up: 12 months |
— | — | HR 1.25 (0.95 to 1.66) | 1935 (6 RCTs) | ⊕⊕⊝⊝ Lowb,c |
| Time to return to work ‐ very long‐term follow‐up: more than 12 months | — | — | HR 0.93 (0.74 to 1.17) | 474 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b |
| Cumulative sickness absence in work days ‐ short‐term follow‐up: 6 months | The mean cumulative sickness absence was 79.14 work days | The mean cumulative sickness absence in the intervention group was 16.18 work days lower (32.42 lower to 0.06 higher) | — | 113 (1 RCT) | ⊕⊕⊕⊝ Moderateb |
| Cumulative sickness absence in work days ‐ long‐term follow‐up: 12 months |
The mean cumulative sickness absence was 144 work days | The mean cumulative sickness absence in the intervention group was 14.84 work days lower (38.56 lower to 8.88 higher) | — | 1339 (6 RCTs) | ⊕⊕⊝⊝ Lowb,c |
| Cumulative sickness absence in work days ‐ very long‐term follow‐up: more than 12 months |
The mean cumulative sickness absence was 466 work days | The mean cumulative sickness absence in the intervention group was 7 work days higher (15.17 lower to 29.17 higher) | — | 8052 (1 RCT) | ⊕⊕⊕⊝ Moderateb |
| Proportion at work at end of the follow‐up ‐ short‐term follow‐up: 6 months | 53 per 100 | 56 per 100 (46 to 69) | RR 1.06 (0.86 to 1.30) | 1388 (5 RCTs) | ⊕⊕⊝⊝ Lowa,b |
| Proportion at work at end of the follow‐up ‐ long‐term follow‐up: 12 months |
60 per 100 | 64 per 100 (59 to 69) | RR 1.06 (0.99 to 1.15) | 3061 (5 RCTs) | ⊕⊕⊝⊝ Lowa,b |
| Proportion at work at end of the follow‐up ‐ very long‐term follow‐up: more than 12 months |
53 per 100 | 49 per 100 (43 to 56) | RR 0.94 (0.82 to 1.07) | 815 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b |
| Proportion who had ever returned to work ‐ short‐term follow‐up: 6 months |
57 per 100 | 49 per 100 (36 to 68) | RR 0.87 (0.63 to 1.19) | 675 (4 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c |
| Proportion who had ever returned to work ‐ long‐term follow‐up: 12 months | 69 per 100 | 71 per 100 (67 to 75) | RR 1.03 (0.97 to 1.09) | 3822 (8 RCTs) | ⊕⊕⊕⊝ Moderateb |
| Proportion who had ever returned to work ‐ very long‐term follow‐up: more than 12 months |
75 per 100 | 71 per 100 (66 to 77) | RR 0.95 (0.88 to 1.02) | 938 (3 RCTs) | ⊕⊕⊝⊝ Lowa,b |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; OR: odds ratio. | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
a Downgraded 1 level for risk of bias (attrition bias, reporting bias). b Downgraded 1 level for imprecision (confidence interval encloses negative and positive effect or population size less than 400). c Downgraded 1 level for inconsistency (substantial heterogeneity).
Background
Description of the condition
Most industrialised countries recognise long‐term sick leave as an increasing public health problem (Canadian Human Rights Commission 2007; Henderson 2005; OECD 2010), which affects society through loss of productivity and work disability claims (Arends 2012). NICE 2009 defines long‐term sick leave as an absence from work for at least four weeks.
Statistics from the Organisation for Economic Co‐operation and Development (OECD) countries show that 5.7% of the working age population (20 to 64 years of age) received disability benefits in 2010 (OECD 2014 a), ranging from 0.6% to 10.4% across countries. Mental health problems were the leading causes for sick leave, followed by musculoskeletal disorders (Arends 2012; Henderson 2005). For workers, long‐term sick leave implies health risks as well as occupational, social and economic deprivation (Henderson 2005; OECD 2003).
The duration of sick leave and the likelihood to return to work have an inverse relationship: being sick‐listed for six months or longer resulted in an 80% chance of remaining off work for five years (Waddell 2006). Once on disability benefits, people tend not to go back to work; they rather move onto another benefit or retire (OECD 2010).
Description of the intervention
To limit long‐term sick leave and associated consequences, insurers, healthcare providers and employers may provide special programmes that facilitate workers' return. These programmes run under a variety of names, such as case management, integrated or collaborative care, or return‐to‐work coordination programmes. They differ widely in content, set‐up and duration, and their components include a variety of interventions, such as occupational therapy, physiotherapy, psychological therapy, medical interventions, workplace ergonomics, education and social therapy. All components are individually adjusted to the worker's needs.
Despite increasing popularity, there is limited evidence regarding the short‐ and long‐term effectiveness and cost‐effectiveness of return‐to‐work programmes (Berchtold 2006; Hofmarcher 2007; NICE 2009; Palmer 2012).
How the intervention might work
Return‐to‐work programmes identify barriers that may prevent workers from successfully returning to work and assess their strengths and limitations. A designated coordinator then provides the worker with individually tailored interventions to overcome these barriers (Craig 2013).
Possible barriers are:
physical (e.g. a painful joint due to osteoarthritis, chronic obstructive lung disease);
mental (e.g. low resilience due to depression or a personality disorder);
functional (e.g. low endurance, minor flexibility to adapt to new situations, restricted range of motion);
workplace‐related (elements of the workplace may be unsuitable, e.g. lack of job autonomy); and
psychosocial (e.g. interpersonal problems with the supervisor, challenging family situation, burdening financial situation).
Early multidisciplinary interventions seem appropriate and promising ways to return people to work (Department for Work and Pensions 2013; Hoefsmit 2012).
Effective return‐to‐work coordination programmes depend on good communication between the various stakeholders (i.e. workers and their families, employers, supervisors, healthcare providers, and insurers) and on smooth coordination of the various components included in the programme. The return‐to‐work coordinator plays a pivotal role by ensuring communication and a joint understanding regarding expectations for all stakeholders (IWH 2007). Face‐to‐face contact between the worker and the return‐to‐work coordinator favours an optimal selection and implementation of the return‐to‐work interventions and intensifies the worker's accountability to the programme.
Why it is important to do this review
Long‐term sick leave results in serious consequences for individuals and other stakeholders as well as for the society at large. Return‐to‐work coordination programmes may respond to this challenge, but they represent complex and costly interventions requiring substantial human and financial resources. The sparse and heterogeneous evidence on their effectiveness calls for an investigation into their impact.
We published a former version of this review (Schandelmaier 2012). The importance and timeliness of the subject required an update with a new search for relevant studies.
Objectives
To assess the effects of return‐to‐work coordination programmes versus usual practice for workers on sick leave or disability.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) irrespective of their language of publication. We included studies reported as full text, those published as abstract only and unpublished data.
Types of participants
We included studies in adults of working age (16 to 65 years) who:
were on full‐ or part‐time sick leave continuously for at least four weeks or were receiving long‐term disability benefits; and
were employed at the time of sick‐listing.
At least 80% of the participants in a study had to fulfil both criteria. We included studies irrespective of the cause of sick leave or disability, the setting or the benefit scheme (e.g. private or government provider).
Types of interventions
Experimental intervention
We included trials comparing return‐to‐work coordination programmes to usual practice. No uniform definition of return‐to‐work coordination programmes exists. We defined such programmes as follows.
The objective is to promote return to work.
The return‐to‐work coordinator(s) and the affected worker have at least one face‐to‐face contact.
The process starts with an assessment of the worker's needs and leads to an individually tailored return‐to‐work plan.
The implementation of the return‐to‐work plan is managed by the return‐to‐work coordinator(s).
In our definition, 'individually tailored' implies a personalised set of actions directed at the worker, the employer, the workplace, or other factors in the return‐to‐work process. Adjustment to the needs of the worker within a pre‐defined action, such as individually tailored physical therapy, was not sufficient to meet the criterion. Consequently, the return‐to‐work plan had to allow for more than one possible action.
We included studies where public or private insurers offered return‐to‐work coordination programmes to people on sick leave due to impaired health ('in‐house programmes'). In addition, we considered return‐to‐work coordination programmes that could be contracted by insurers ('commissioned programmes'). We assumed that both have comparable effects as long as they share the goal of returning to work.
We excluded employer‐initiated return‐to‐work coordination programmes. Such programmes encounter fewer barriers in implementing workplace‐directed interventions than insurers or third‐party return‐to‐work coordinators and are typically not available for smaller companies.
Control intervention
We classified the level of support for the control groups as low, moderate or high. To get a better understanding of what usual practice in the different countries entailed, we contacted all authors and asked them to provide additional information.
We classified usual practice by a healthcare provider (e.g. a general practitioner or a physical therapist or other generally accessible rehabilitation professionals) as a low level of support. We classified conventional case management (e.g. as provided by the municipality or the insurer), usual sickness guidance by an occupational practitioner or a brief clinical intervention as a moderate level of support. We classified a clinical intervention in addition to a conventional case management as a high level of support.
Types of outcome measures
Primary outcomes
Our primary outcome of interest was return to work, which was measured in studies using several descriptive outcomes. We included studies that reported at least one of the following.
Time to return to work.
Cumulative sickness absence.
Proportion at work at end of the follow‐up.
Proportion ever returned to work.
Since almost all of the included studies reported on the outcome 'proportion of participants who had ever returned to work', we added it post hoc. This outcome captures workers who returned to work (for a defined time span) during the follow‐up time, regardless of whether they stayed at work or took sick leave again.
We further considered whether the individual returned to:
full‐time or part‐time work; and
the former or a modified occupation.
Secondary outcomes
If included studies provided data on patient‐reported outcomes, we collected the following.
Physical, mental, social or overall functioning.
Pain, depression and anxiety.
Quality of life.
Satisfaction of patients, employers, and social insurance organisations.
Search methods for identification of studies
Electronic searches
We conducted a systematic literature search to identify published and unpublished trials that could be eligible for inclusion in this review. We developed a search strategy for PubMed and then adapted it for use in the other electronic databases (Appendix 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5). In order to avoid language bias, we used our international network to assess all non‐English language papers for potential inclusion in our review.
We searched the following electronic databases from their inception to 1 November 2016.
MEDLINE via PubMed (including the 'related citations' feature).
Embase.
CINAHL.
PsycINFO.
Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 11).
Searching other resources
We scanned the bibliographies of all eligible trials and other relevant publications, including reviews and meta‐analyses. For relevant publications that were listed in the Web of Science, we scanned citing articles with the 'times cited' feature.
Data collection and analysis
Selection of studies
Three authors (SS, NV, RK) independently screened the titles and abstracts of all identified citations and acquired full‐text articles that at least one author deemed potentially eligible. Subsequently, two authors (SS, NV) independently assessed the full‐text articles for eligibility; we resolved disagreements through discussion or by arbitration with a third author (RK). We identified and excluded duplicates and collated multiple reports of the same study so that each study rather than each report was the unit of interest. For details of excluded studies see Characteristics of excluded studies.
We recorded the selection process to complete a PRISMA flow diagram (Moher 2009). For details see Figure 1.
1.
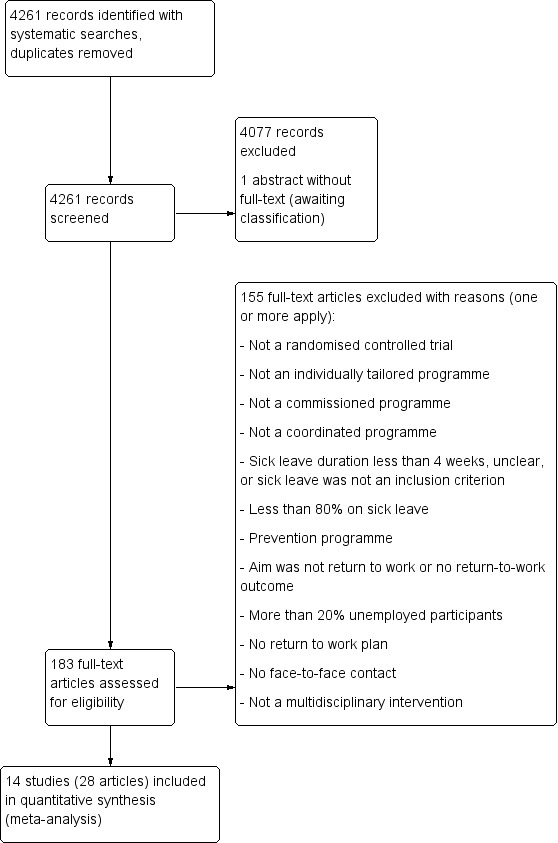
PRISMA Study flow diagram
Data extraction and management
Using a standardised form, we extracted the following data.
Characteristics of study design.
Setting.
Participants.
Study eligibility criteria.
Intervention details.
Outcomes.
Funding sources and stated conflicts of interest.
Two pairs of authors (SS, JB, SE, NV) independently extracted data and resolved disagreement by discussion or by arbitration with a third author (RK). If information was insufficient or uncertain for data extraction, we contacted the study authors for clarification.
One author (NV) transferred data into the Cochrane statistical software, Review Manager 5 (RevMan 2014); another author (TZ) cross‐checked the transferred data.
Assessment of risk of bias in included studies
Two authors (SS, NV) independently assessed all included studies for risk of bias using the Cochrane tool for assessing risk of bias (Higgins 2011). We referred to a third author (RK) to resolve disagreements. We evaluated the following risk of bias domains (Higgins 2011).
Sequence generation.
Allocation concealment.
Blinding.
Incomplete outcome data.
Selective outcome reporting.
Other sources of bias.
We further assessed cluster‐RCTs for recruitment bias and appropriate statistical analysis (Higgins 2011).
We modified the Cochrane tool for assessing risk of bias (Higgins 2011): the response options of 'definitely yes' and 'probably yes' conferred low risk of bias, while the response options of 'definitely no' and 'probably no' conferred high risk of bias (Akl 2012). We graded each potential source of bias as high, low or unclear and provided a quote from the study report together with a justification for our judgment in the 'Risk of bias' table. We considered random sequence generation, allocation concealment, selective outcome reporting and incomplete outcome data to be key domains. We judged a study to be at high risk of bias when we judged one or more key domains to be at high risk of bias. Conversely, we judged a study to have a low risk of bias when we judged low risk of bias for all key domains. We summarised the risk of bias judgments across different studies for each of the domains listed.
We assessed blinding of outcome assessment and completeness of data for return‐to‐work outcomes and patient‐reported outcomes separately. We judged studies to be at high risk of attrition bias if they had more than 15% losses to follow‐up for return‐to‐work outcomes.
We summarised and presented the results of our risk of bias assessment in Figure 2 and Figure 3 as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Where information on risk of bias related to unpublished data or correspondence with the author, we noted this in the 'Risk of bias' tables.
2.
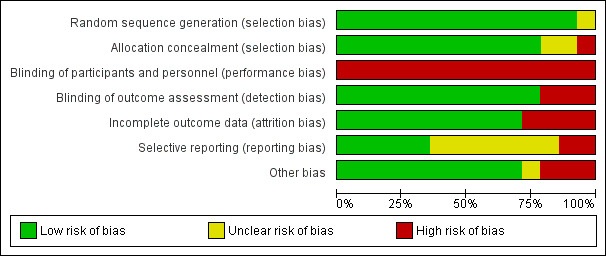
Risk of bias graph: review author's judgements about each risk of bias item presented as percentages across all included studies.
3.
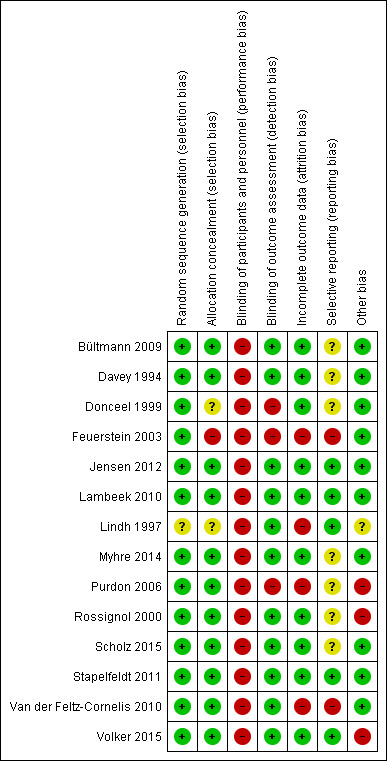
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Assessment of bias in conducting the systematic review
We conducted the review according to our published protocol (Vogel 2015), reporting any deviations in the section Differences between protocol and review.
Measures of treatment effect
We entered outcome data for each study into the data tables in RevMan 2014 to calculate the treatment effects. We expressed dichotomous outcomes as risk ratios (RRs) and time‐to‐event outcomes as hazard ratios (HRs). We calculated absolute effects through risk differences (RDs). We recalculated sickness absence days in work days where necessary. For patient‐reported outcomes presented in different units, we transformed them into units on the scale of the most familiar instrument before pooling mean differences (MDs) (Thorlund 2011).
We used the minimal clinically important difference (MID) to improve the interpretation of patient‐reported outcomes (Johnston 2010). If studies reported only effect estimates and their 95% confidence intervals (CIs) or standard errors, we entered these data into RevMan 2014 using the generic inverse variance method. If studies with time‐to‐event outcomes failed to report HRs, we extracted individual patient data from survival curves, verified the extracted data by comparing the original plot with the plot derived from the extracted data, and then calculated the HRs and associated 95% CIs.
We considered longer‐lasting return to work to be the most important outcome. If we detected varying measures of return to work, we concentrated on the one that expressed long‐term outcome best. If available, we focused on outcomes with at least four weeks of lasting return to work, even if a longer interval might be more meaningful.
Unit of analysis issues
In the case of cluster‐RCTs, we followed the methods in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For studies that employed a cluster‐randomised design and that reported sufficient data to be included in the meta‐analysis but did not make an allowance for the design effect, we calculated the design effect based on a fairly large assumed intracluster correlation (ICC) of 0.10. We based this assumption of 0.10 being a realistic estimate by analogy on studies about implementation research (Campbell 2001).
Dealing with missing data
We contacted study authors to obtain data missing from their reports when necessary. If we could not obtain essential information within a reasonable time, we judged the respective risk of bias domain to be unclear. If we could not obtain numerical outcome data such as standard deviations (SD) or correlation coefficients, we calculated them from other available statistics such as P values according to the methods described in Higgins 2011. In case of missing values, we analysed the available data without imputations as a complete case analysis (Higgins 2011).
Assessment of heterogeneity
We assessed clinical homogeneity of the results of the included studied based on similarity of intervention, participants, outcome and follow‐up. We followed the algorithm provided by (Verbeek 2012). We considered participants as similar when they were of working age and on sick leave for at least four weeks. In the presence of statistical heterogeneity, we investigated differences between workers with musculoskeletal diseases and workers with mental health problems.
We considered interventions as similar when they were multidisciplinary return‐to‐work interventions tailored to the needs of the sick‐listed worker (as stated in Criteria for considering studies for this review). We considered outcome measures as similar when they reported on time to return to work, cumulative sickness absence, proportion of participants at work at a specific time point or proportion who had ever returned to work. We regarded short‐term (up to 6 months), long‐term (6 to 12 months) and very long‐term (longer than 12 months) follow‐up times as different.
We assessed heterogeneity by visual inspection of forest plots and by using the I² statistic. We then quantified the degree of heterogeneity as follows (Higgins 2011).
0% to 40% might not be important.
30% to 60% may represent moderate heterogeneity.
50% to 90% may represent substantial heterogeneity.
75% to 100% considerable heterogeneity.
In the presence of substantial heterogeneity and sufficient number of studies, we conducted subgroup analyses as described below (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
We tried to prevent reporting bias by searching across multiple databases and by including articles irrespective of their language. If we detected multiple articles on the same study, we extracted data only once. We assessed publication bias by funnel plots (Higgins 2011).
Data synthesis
We pooled data using the generic inverse variance method in RevMan 2014 according to Higgins 2011. If sufficient data were available, we performed a meta‐analysis. Since it is implausible that the true effect is the same in all considered studies, we considered a random‐effects model more appropriate for meta‐analyses. All our estimates include 95% CIs. For analyses not available within RevMan 2014, we used the R software (R 2015).
We expressed pooled effects of dichotomous outcomes as RRs and time‐to‐event outcomes as HRs. We calculated illustrative RDs by using the median baseline risk. We pooled effects of continuous outcomes as differences between group means (MDs). For patient‐reported outcomes, we calculated the proportion of patients who experienced an improvement greater than the MID ('substantial improvement') and pooled the RD (Thorlund 2011). If available, we used baseline‐adjusted effect estimates.
Subgroup analysis and investigation of heterogeneity
We planned to conduct subgroup analyses to detect different effects if we found at least 10 studies in a meta‐analysis. We specified the following a priori hypotheses for possible subgroup differences.
Methodology: trials with high risk of bias show larger effects.
Intervention: effects increase with return‐to‐work coordination programmes starting earlier (within three months) in the course of sick leave.
Intervention: effects increase with the involvement of the employers.
Controls: effects decrease with the intensity of support for the control group (ranging from no support to other form of return‐to‐work coordination programmes).
We were unable to carry out subgroup analyses; no meta‐analyses included 10 or more studies.
Sensitivity analysis
We performed a sensitivity analysis to test the robustness of our results by omitting studies with a high risk of bias.
Reaching conclusions
We based our conclusions only on findings from the quantitative synthesis of included studies for this review. We considered the different return‐to‐work outcomes as measurements of the same concept and based our conclusion on all of them. We avoided making recommendations for practice based on more than just the evidence, such as values and available resources. Our implications for research suggest priorities for future research and outline the remaining uncertainties in the area.
Summary of findings table
We used the GRADE approach as described in Higgins 2011 and present the quality of the evidence in the Table 1.
Results
Description of studies
Results of the search
We identified 14 relevant RCTs and included them in our meta‐analyses. Figure 1 illustrates the details of the search.
Included studies
Study design
All of the 14 included studies were RCTs with a parallel design. Three studies were cluster‐RCTs (Donceel 1999; Van der Feltz‐Cornelis 2010; Volker 2015). See Characteristics of included studies for further details.
Participants
We included 12,568 participants, 30% of whom were women. The range of participants per study was 50 to 8050 with a median of 220 participants. The mean age was 41.8 years. Eleven studies enrolled workers with musculoskeletal health problems, two enrolled workers with mental health problems (Van der Feltz‐Cornelis 2010; Volker 2015), and one study investigated both (Purdon 2006). Twelve studies included only employed participants, Davey 1994 included 96% employed participants, and Scholz 2015 included 93% employed participants. Workers in all studies were on sick leave: in seven studies they were on partial or full sick leave (Feuerstein 2003; Jensen 2012; Lambeek 2010; Myhre 2014; Scholz 2015; Stapelfeldt 2011; Volker 2015), while the rest of the studies included only workers on full sick leave. In five studies the length of work absence was shorter than three months (Bültmann 2009; Donceel 1999; Jensen 2012; Rossignol 2000; Stapelfeldt 2011); in four studies, longer than three months (Davey 1994; Lambeek 2010; Lindh 1997; Myhre 2014); in three studies, from 1 to 6 months (Feuerstein 2003; Purdon 2006; Volker 2015); and in one study, from 1 to 11 months (Van der Feltz‐Cornelis 2010). Scholz 2015 did not provide data, but the inclusion of participants with severe accidents made a sick leave duration of at least four weeks plausible. For further details see Characteristics of included studies.
Setting
Recruitment procedures took place from June 1995 to August 2011; this information was missing in four studies. Most of the studies took place in Europe, in: Belgium (Donceel 1999), Denmark (Bültmann 2009; Jensen 2012; Stapelfeldt 2011), the Netherlands (Lambeek 2010; Van der Feltz‐Cornelis 2010; Volker 2015), Norway (Myhre 2014), Sweden (Lindh 1997), Switzerland (Scholz 2015), and the UK (Davey 1994; Purdon 2006). Rossignol 2000 was in Canada, and Feuerstein 2003 was in the USA. For details of the recruitment procedures see Characteristics of included studies.
Experimental intervention
Although the return‐to‐work coordination programmes differed in structure, components, team members and duration, all included a tailored, multidisciplinary, coordinated intervention with an individual assessment and a return‐to‐work plan.
A variety of specialists were involved in the interventions, most often an occupational physician, a general practitioner or physician, a mental health specialist, a physical or occupational therapist, and a social worker. For further information see Table 2 and Characteristics of included studies. The duration of the return‐to‐work coordination programmes varied substantially. Some studies delivered the programme tailored to the worker's needs, others until successful return to work or for a defined period. Heterogeneous reporting precluded a descriptive summary (e.g. total number of weeks, median number of weeks, range of weeks). For details see Characteristics of included studies.
1. Involved disciplines in the intervention groups.
| Occupational or rehabilitation physician | General practitioner | (Occupational) physiotherapist | Psychologist, psychiatrist, psychotherapist | Occupational therapist | Social worker | Chiropractor | Other | |
| Bültmann 2009 | X | — | X | X | — | X | X | — |
| Davey 1994 | X | — | X | X | X | — | — | — |
| Donceel 1999 | X (social insurance physician) | X | — | — | — | — | — | Other healthcare personnel, social insurance agent |
| Feuerstein 2003 | — | — | — | — | — | — | — | “[E].g. supervisor, injury compensation specialist, medical providers, claims examiner” |
| Jensen 2012 | X | X | X | — | X | X | — | — |
| Lambeek 2010 | X | — | X | — | X | — | — | Medical specialist |
| Lindh 1997 | X | — | X | X | X | X | — | Nurse, vocational counsellor |
| Myhre 2014 | X | — | X | — | — | — | — | Case worker, medical specialist, group discussions, lecturer |
| Purdon 2006 | — | — | X | X | — | — | X | Podiatrists, osteopaths and dieticians |
| Rossignol 2000 | X | — | X | — | — | — | X | — |
| Scholz 2015 | X (insurance physician) | X | X | — | X | — | — | Outpatient care provider, inpatient care provider, other care provider |
| Stapelfeldt 2011 | X | X | X | — | X | X | — | — |
| Van der Feltz‐Cornelis 2010 | X | X | — | X | — | — | — | — |
| Volker 2015 | X | X | — | X | — | — | — | Web‐based eHealth Modules |
X = involved discipline
The study coordinator contacted and enlisted the involvement of the employer in eight studies (Bültmann 2009; Feuerstein 2003; Jensen 2012; Lambeek 2010; Myhre 2014; Purdon 2006; Scholz 2015; Stapelfeldt 2011). One study reported no direct contact but described workplace accommodations as needed (Rossignol 2000). In five studies the employer was not involved in the intervention.
In five studies the intervention started less than three months after inclusion (Bültmann 2009; Donceel 1999; Jensen 2012; Rossignol 2000; Stapelfeldt 2011), while in four studies it started later than three months (Davey 1994; Lambeek 2010; Lindh 1997; Myhre 2014). In four studies the start of the intervention ranged from one to six months after inclusion, while the final study did not provide information.
Control intervention
We classified five studies as using a control intervention with a low level of support (Davey 1994; Donceel 1999; Lindh 1997; Purdon 2006; Rossignol 2000), while seven provided a moderate level of support (Bültmann 2009; Feuerstein 2003; Lambeek 2010; Myhre 2014; Scholz 2015; Van der Feltz‐Cornelis 2010; Volker 2015), and two studies offered a high level of support (Jensen 2012; Stapelfeldt 2011).
One study performed at two sites used the pre‐existing intervention at each site: either a brief or a comprehensive multidisciplinary intervention (Myhre 2014). However, authors showed similar effects for these treatment programmes.
Outcomes
Primary outcomes
Nine studies retrieved the primary outcomes on return to work from administrative data (Bültmann 2009; Feuerstein 2003; Jensen 2012; Lindh 1997; Myhre 2014; Rossignol 2000; Scholz 2015; Stapelfeldt 2011; Volker 2015). Two studies used a combination of administrative data and self‐report (Lambeek 2010; Van der Feltz‐Cornelis 2010). Other studies used a semi‐structured interview in combination with information from claims files (Davey 1994), a standardised questionnaire (Donceel 1999), or a face‐to‐face survey (Purdon 2006).
Nine studies reported on time to return to work (Donceel 1999; Feuerstein 2003; Jensen 2012; Lambeek 2010; Myhre 2014; Rossignol 2000; Stapelfeldt 2011; Van der Feltz‐Cornelis 2010; Volker 2015), 7 studies reported on cumulative sickness absence (Bültmann 2009; Jensen 2012; Lambeek 2010; Myhre 2014; Scholz 2015; Stapelfeldt 2011; Volker 2015), 7 studies reported on the proportion of participants at work at end of the follow‐up (Bültmann 2009; Davey 1994; Donceel 1999; Jensen 2012; Lindh 1997; Purdon 2006; Van der Feltz‐Cornelis 2010), and 12 studies reported on the proportion of participants who had ever returned to work (Davey 1994; Donceel 1999; Feuerstein 2003; Jensen 2012; Lambeek 2010; Lindh 1997; Myhre 2014; Purdon 2006; Rossignol 2000; Stapelfeldt 2011; Van der Feltz‐Cornelis 2010; Volker 2015).
Definitions of return to work varied: eight studies used full‐time return to work (i.e. suspension of sickness benefits) (Donceel 1999; Feuerstein 2003; Jensen 2012; Lambeek 2010; Myhre 2014; Purdon 2006; Stapelfeldt 2011; Van der Feltz‐Cornelis 2010), and four studies applied full and partial return to work (Davey 1994; Lindh 1997; Rossignol 2000; Scholz 2015). Two studies reported data on full and partial return to work separately (Bültmann 2009; Volker 2015).
Six studies reported successful return to work without additional specification (Bültmann 2009; Davey 1994; Donceel 1999; Feuerstein 2003; Lindh 1997; Scholz 2015). Eight studies defined lasting return to work for at least two days (Rossignol 2000), two weeks (Purdon 2006), four weeks (Jensen 2012; Lambeek 2010; Stapelfeldt 2011; Van der Feltz‐Cornelis 2010; Volker 2015), or five weeks (Myhre 2014).
Secondary outcomes
Included studies also collected data on patient‐reported outcomes. We analysed secondary outcomes on pain (Bültmann 2009; Feuerstein 2003; Jensen 2012; Lambeek 2010; Myhre 2014; Purdon 2006; Rossignol 2000), overall function (Bültmann 2009; Jensen 2012; Lambeek 2010; Myhre 2014; Purdon 2006; Rossignol 2000), physical function (Feuerstein 2003; Jensen 2012; Lambeek 2010; Purdon 2006; Rossignol 2000), mental function (Feuerstein 2003; Jensen 2012; Purdon 2006), social function (Jensen 2012; Purdon 2006), depression (Davey 1994; Myhre 2014; Van der Feltz‐Cornelis 2010; Volker 2015), and anxiety (Davey 1994; Myhre 2014; Volker 2015).
We found insufficient data for meta‐analyses on quality of life and on the satisfaction of workers, employers or social insurance organisations.
Follow‐up
We regarded a follow‐up of up to 6 months as short‐term (Davey 1994; Rossignol 2000; Van der Feltz‐Cornelis 2010); between 6 and 12 months, as long‐term (Bültmann 2009; Donceel 1999; Lambeek 2010; Myhre 2014; Purdon 2006; Stapelfeldt 2011; Volker 2015); and more than 12 months, as very long‐term (Feuerstein 2003 (16 months); Jensen 2012 (24 months); Lindh 1997 (60 months); Scholz 2015 (72 months)). Duration of follow‐up times ranged from 3 to 72 months.
Excluded studies
We assessed 183 full text articles and excluded 155 for not meeting our inclusion criteria. See Characteristics of excluded studies for details.
Risk of bias in included studies
Risk of bias varied across studies (Figure 2). We judged 10 studies to be at low risk of bias (Bültmann 2009; Davey 1994; Donceel 1999; Jensen 2012; Lambeek 2010; Myhre 2014; Rossignol 2000; Scholz 2015; Stapelfeldt 2011; Volker 2015). We judged four studies to be at high risk of bias based on lack of allocation concealment (Feuerstein 2003), incomplete outcome data (Feuerstein 2003; Lindh 1997; Purdon 2006; Van der Feltz‐Cornelis 2010), and selective outcome reporting (Feuerstein 2003; Van der Feltz‐Cornelis 2010). See Figure 3 for details.
Allocation
Eleven studies reported concealed allocation and suitable methods of randomisation; we judged them to be at low risk of selection bias. Feuerstein 2003 omitted allocation concealment, so we judged the study to be at high risk of selection bias. Donceel 1999 and Lindh 1997 reported no concealment; we judged them to be at unclear risk of selection bias.
Blinding
We judged all studies to be at high risk of bias, acknowledging that successful blinding towards the intervention may be very challenging or not feasible at all. All but three studies succeeded in blinded outcome assessment by using administrative data on return to work (Donceel 1999;Feuerstein 2003;Purdon 2006) (see Types of outcome measures).
Incomplete outcome data
We found high risk of attrition bias for four studies (Feuerstein 2003; Lindh 1997; Purdon 2006; Van der Feltz‐Cornelis 2010).
Selective reporting
Two studies were at high risk of reporting bias. Feuerstein 2003 did not publish return‐to‐work outcomes but provided (incomplete) data on request. Van der Feltz‐Cornelis 2010 did not pre‐specify return to work as a primary outcome: it changed from 'level of functioning' in the protocol to 'time until return to work for at least four weeks'. They did not report the level of functioning.
Other potential sources of bias
We judged two studies to have a potential source of bias because of low adherence among participants (Purdon 2006; Volker 2015), while one study had baseline imbalances between the groups (Rossignol 2000).
Effects of interventions
See: Table 1
Return‐to‐work coordination programmes versus usual practice
We compared return‐to‐work coordination programmes to usual practice. See Table 1 for the effects of the intervention for all outcomes and the GRADE assessment of quality of the evidence per outcome.
Primary outcomes
Time to return to work
Based on nine studies, we found no significant differences in the Hazard Ratios (HR) of time to return to work (Analysis 1.1, Figure 4).
1.1. Analysis.
Comparison 1 Return‐to‐work outcomes, Outcome 1 Time to return to work.
4.
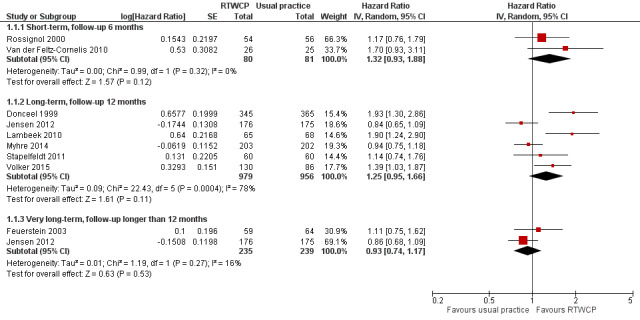
Forest plot of comparison: time to return to work. RTWCP = return‐to‐work coordination programmes
The HR at short‐term follow‐up was 1.32 (95% CI 0.93 to 1.88, two studies, low quality evidence, low heterogeneity). The HR at long‐term follow‐up was 1.25 (95% CI 0.95 to 1.66, six studies, low quality evidence, substantial heterogeneity). The HR at very long‐term follow‐up was 0.93 (95% CI 0.74 to 1.17, two studies, low quality evidence, low heterogeneity).
Cumulative sickness absence
Based on seven studies, we found no significant differences in cumulative sickness absence (Analysis 1.3, Figure 5).
1.3. Analysis.
Comparison 1 Return‐to‐work outcomes, Outcome 3 Cumulative sickness absence in work days.
5.
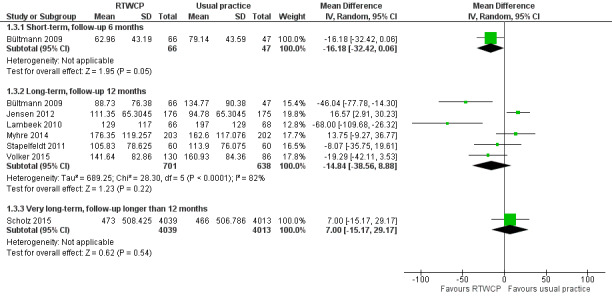
Forest plot of comparison: cumulative sickness absence in work days. RTWCP = return‐to‐work coordination programmes
The Mean Difference (MD) at short‐term follow‐up was 16.18 work days per year lower (95% CI −32.42 to 0.06, one study, moderate quality evidence). The MD at long‐term follow‐up was 14.84 work days per year lower (95% CI −38.56 to 8.88, six studies, low quality evidence, substantial heterogeneity). The MD at very long‐term follow‐up was 7.00 work days per year higher (95% CI −15.17 to 29.17, one study, moderate quality evidence).
Proportion of participants at work at end of the follow‐up
Based on seven studies, we found no significant differences in the proportion of participants at work at end of the follow‐up (Analysis 1.4, Figure 6).
1.4. Analysis.
Comparison 1 Return‐to‐work outcomes, Outcome 4 Proportion at work at end of the follow‐up.
6.
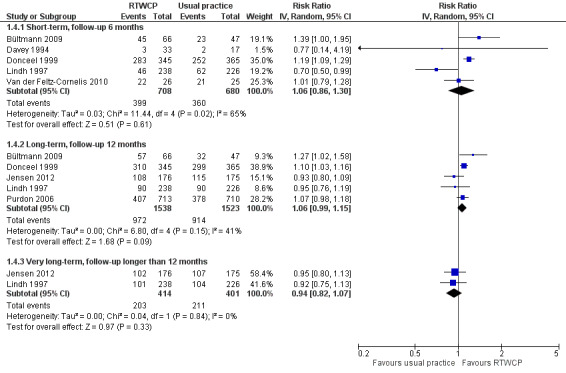
Forest plot of comparison: proportion at work at end of the follow‐up. RTWCP = return‐to‐work coordination programmes
The Risk Ratio (RR) at short‐term follow‐up was 1.06 (95% CI 0.86 to 1.30, five studies, low quality evidence, substantial heterogeneity). The RR at long‐term follow‐up was 1.06 (95% CI 0.99 to 1.15, five studies, low quality evidence, moderate heterogeneity). The RR at very long‐term follow‐up was 0.94 (95% CI 0.82 to 1.07, two studies, low quality evidence, low heterogeneity).
The absolute effect for the intervention versus control was 4 in 100 more individuals returning to work at short‐term follow‐up (95% CI 8 fewer to 16 more), 4 in 100 more at long‐term follow‐up (95% CI 2 fewer to 9 more), and 3 in 100 fewer at very long‐term follow‐up (95% CI 10 fewer to 3 more).
Proportion of participants who had ever returned to work
Based on 12 studies, we found no significant differences in the proportion of participants who had ever returned to work (Analysis 1.6, Figure 7).
1.6. Analysis.
Comparison 1 Return‐to‐work outcomes, Outcome 6 Proportion who had ever returned to work.
7.
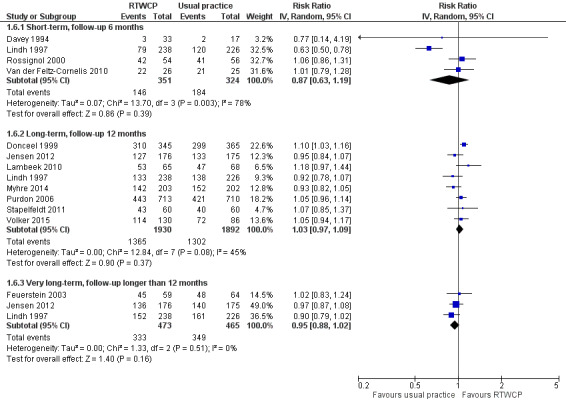
Forest plot of comparison: proportion who had ever returned to work. RTWCP = return‐to‐work coordination programmes
The RR at short‐term follow‐up was 0.87 (95% CI 0.63 to 1.19, four studies, very low quality evidence, substantial heterogeneity). The RR at long‐term follow‐up was 1.03 (95% CI 0.97 to 1.09, eight studies, moderate quality evidence, moderate heterogeneity). The RR at very long‐term follow‐up was 0.95 (95% CI 0.88 to 1.02, three studies, low quality evidence, low heterogeneity).
The absolute effect for the intervention versus control was 6 in 100 fewer individuals having ever returned to work for any time period at short‐term follow‐up (95% CI 19 fewer to 8 more), 2 in 100 more at long‐term follow‐up (95% CI 2 fewer to 6 more), and 4 in 100 fewer at very long‐term follow‐up (95% CI 10 fewer to 1 more).
Sensitivity analyses
For the primary outcomes, we conducted sensitivity analyses for studies at high risk of bias and cluster‐RCTs.
Omitting studies at high risk of bias revealed a significant difference in the proportion of participants working at end of the short‐term follow‐up (RR 1.20, 95% CI 1.10 to 1.30; Analysis 1.5). We found no significant changes for the time to return to work (Analysis 1.2), cumulative sickness absence (no high risk af bias studies), or the proportion of participants who had ever returned to work (Analysis 1.7)
1.5. Analysis.
Comparison 1 Return‐to‐work outcomes, Outcome 5 Proportion at work at end of the follow‐up, sensitivity analysis (low risk of bias studies only).
1.2. Analysis.
Comparison 1 Return‐to‐work outcomes, Outcome 2 Time to return to work, sensitivity analysis (low risk of bias studies only).
1.7. Analysis.
Comparison 1 Return‐to‐work outcomes, Outcome 7 Proportion who had ever returned to work, sensitivity analysis (low risk of bias studies only).
For cluster‐RCTs (Donceel 1999; Van der Feltz‐Cornelis 2010; Volker 2015), we calculated the design effect based on an ICC of 0.10. We found no relevant changes in the effect estimates or CIs.
Subgroup analysis and investigation of heterogeneity
In the presence of substantial heterogeneity, we wanted to conduct subgroup analyses according to our a priori hypotheses; however, we found too few studies in each subgroup to compare them in meaningful subgroup analyses.
Heterogeneity was substantial for time to return to work at long‐term follow‐up (I² = 78%; Analysis 1.1), cumulative sickness absence at a long‐term follow‐up (I² = 82%; Analysis 1.3), the proportion of participants at work at the end of short‐term follow‐up (I² = 65%; Analysis 1.4), and for the proportion who had ever returned to work at short‐term follow‐up (I² = 78%; Analysis 1.6).
Eliminating high risk of bias studies resolved heterogeneity for the proportion at work and the proportion who had ever returned to work. Eliminating two outliers, both clearly in favour for return‐to‐work coordination programmes (Donceel 1999; Lambeek 2010), reduced heterogeneity for time to return to work to a moderate level, even though these programmes showed no obvious differences to other studies. Heterogeneity for cumulative sickness absence at a long‐term follow‐up remained substantial and unexplained: even if we just analysed Jensen 2012 and Stapelfeldt 2011, two studies within the identical setting, identical recruitment procedure and identical interventions, heterogeneity remained moderate (I² = 59%).
Secondary outcomes
Pain
Seven studies reported on pain, and we found a significant MD and Risk Difference (RD) for long‐term follow‐up. However, the difference was not clinically important (Minimally Important Difference (MID) = −10.0 points on a 0 to 100 scale).
The MD at short‐term follow‐up was −4.76 points (95% CI −14.89 to 5.36, four studies, low quality evidence); at long‐term follow‐up, −2.98 points (95% CI −5.33 to −0.63, six studies, moderate quality evidence); and at very long‐term follow‐up, −7.20 points (95% CI −15.76 to 1.36, one study, very low quality evidence; Analysis 2.1).
2.1. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 1 Pain ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0.
The proportion of participants in the intervention group whose pain improved substantially was 3% (95% CI 0% to 6%) at long‐term follow‐up and not significantly different from control at short‐term (RD −3%, 95% CI −11% to 5%) or very long‐term follow‐up follow‐up (RD −2%, 95% CI −11% to 7%; Analysis 2.2).
2.2. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 2 Pain ‐ pooled RDs of workers with an improvement greater than the MID of 10.0.
Overall function
Six studies reported on overall function, and we found a significant MD at short‐term follow‐up and no significant RDs. The effect did not reach the MID of 10 points on a 0 to 100 scale.
The MD at short‐term follow‐up was 8.13 points (95% CI 3.95 to 12.32, three studies, moderate quality evidence) and at long‐term follow‐up, 2.74 points (95% CI −0.15 to 5.64, five studies, moderate quality evidence; Analysis 2.3).
2.3. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 3 Overall function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0.
The proportion of participants in the intervention group whose overall function improved substantially was not significantly different from control (RD 16%, 95% CI −4% to 37% and RD 0%, 95% CI −9% to 9%, respectively; Analysis 2.4).
2.4. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 4 Overall function ‐ pooled RDs of workers with an improvement greater than the MID of 10.0.
Physical function
Five studies reported on physical function, but we found no significant MDs or RDs (MID = 8.4 points on a 0 to 100 scale).
The MD at short‐term follow‐up was 3.47 points (95% CI −3.26 to 10.20, three studies, low quality evidence); at long‐term follow‐up, 2.19 points (95% CI −2.29 to 6.67, four studies, very low quality evidence); and at very long‐term follow‐up, 1.85 points (95% CI −2.25 to 5.95, one study, very low quality evidence; Analysis 2.5).
2.5. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 5 Physical function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 8.4.
The proportion of participants in the intervention group whose physical function improved substantially was not significantly different from control (short‐term: RD 3%, 95% CI −7% to 13%; long‐term: RD 1%, 95% CI −2 to 3%; very long‐term: RD 0%, 95% CI −2% to 2%; Analysis 2.6).
2.6. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 6 Physical function ‐ pooled RDs of workers with an improvement greater than the MID of 8.4.
Social function
Two studies reported on social function, and we found no significant MDs or RDs (MID = 11.7 points on a 0 to 100 scale).
The MD at long‐term follow‐up was 2.84 points (95% CI −0.09 to 5.77, two studies, low quality evidence; Analysis 2.7).
2.7. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 7 Social function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 11.7.
The proportion of participants in the intervention group whose social function improved substantially was not significantly different from control (RD 1%, 95% CI −2% to 4%; Analysis 2.8).
2.8. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 8 Social function ‐ pooled RDs of workers with an improvement greater than the MID of 11.7.
Mental function
Three studies reported on mental function. We found a significant MD at long‐term and very long‐term follow‐up and no significant RDs (MID = 7.3 points on a 0 to 100 scale).
The MD at short‐term follow‐up was 1.85 points (95% CI −2.67 to 6.37, one study, very low quality evidence); at long‐term follow‐up, 3.14 points (95% CI 1.16 to 5.11, three studies, moderate quality evidence); and at very long‐term follow‐up, 6.09 points (95% CI 0.56 to 11.63, one study, very low quality evidence; Analysis 2.9).
2.9. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 9 Mental function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 7.3.
The proportion of participants in the intervention group whose mental function improved substantially was not significantly different from control (short‐term: RD 0%, 95% CI −1% to 1%; long‐term: RD 0%, 95% CI −1% to 1%; and very long‐term: RD 0%, 95% CI −1% to 1%; Analysis 2.10).
2.10. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 10 Mental function ‐ pooled RDs of workers with an improvement greater than the MID of 7.3.
Depression
Four studies reported on depression, but we found no significant MDs or RDs (MID = 5.0 on a 0 to 27 scale).
The MD at short‐term follow‐up was 0.37 points (95% CI −2.81 to 3.55, three studies, low quality evidence) and for long‐term follow‐up, 0.00 points (95% CI −1.07 to 1.07, two studies, moderate quality evidence; Analysis 2.11).
2.11. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 11 Depression ‐ scale 0 to 27 (higher score indicates deterioration) ‐ MID 5.0.
The proportion of participants in the intervention group that experienced substantial change in depression was not significantly different from control (short term: RD 3%, 95% CI −7% to 12%; and long term: RD 1%, 95% CI −4% to 6%; Analysis 2.12).
2.12. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 12 Depression ‐ pooled RDs of workers with an improvement greater than the MID of 5.0.
Anxiety
Three studies reported on anxiety, but we found no significant MDs or RDs (MID = 4.0 on a 0 to 21 scale).
The MD at short‐term follow‐up was −0.02 points (95% CI −3.24 to 3.21, two studies, low quality, P = 0.99) and for long‐term follow‐up, 0.97 points (95% CI −0.17 to 2.12, two studies, moderate quality, P = 0.1; Analysis 2.13).
2.13. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 13 Anxiety ‐ scale 0 to 21 (higher score indicates deterioration) ‐ MID 4.0.
The proportion of participants in the intervention group that experienced substantial change in anxiety was not significantly different from control (short term: RD −1%, 95% CI −8% to 7 and long‐term: RD 2%, 95% CI −3% to 8%; Analysis 2.14).
2.14. Analysis.
Comparison 2 Patient‐reported outcomes, Outcome 14 Anxiety ‐ pooled RDs of workers with an improvement greater than the MID of 4.0.
Discussion
Summary of main results
We included 14 RCTs comparing return‐to‐work coordination programmes to usual practice. Very low‐ to moderate‐quality evidence suggests no benefits on return‐to‐work outcomes.
For the outcomes time to return to work, cumulative sickness absence, proportion of participants working at end of the follow‐up and proportion who had ever returned to work, we found no significant differences at short‐term (6 months), long‐term (12 months) or very long‐term (longer than 12 months) follow‐up.
Omitting high risk of bias studies showed a significantly higher proportion of participants returning to work at short‐term follow‐up but there were no relevant changes for any other outcome.
Regarding the patient‐reported outcomes, we found no differences greater than the MID. The quality of the evidence ranged from very low to moderate.
Overall completeness and applicability of evidence
We performed an extensive literature search without language restriction and screened almost 4000 records. Furthermore, the review authors contributed with their professional expertise in the field of work disability and insurance medicine to find ongoing or unpublished studies. Risk of selection bias is therefore low. However, we found only two studies in workers with common mental health problems.
We identified studies from nine different countries, reflecting a broad variety of healthcare systems. Differences in the healthcare systems and benefit schemes of each country might have an additional effect on the return‐to‐work outcome.
Quality of the evidence
We included 14 RCTs with more than 12,500 workers. We considered this a large number of participants.
The risk of bias was low in 10 studies and high in 4 studies because of reporting bias, attrition bias or detection bias. None of the studies blinded participants or personnel, but most studies retrieved return‐to‐work data through administrative databases (11 of 14).
According to the GRADE system, the quality of the evidence was very low to moderate through the different outcomes. Besides high risk of attrition or reporting bias, we downgraded the quality of evidence for inconsistency (substantial heterogeneity) and imprecision (a confidence interval spanning a negative and positive effect or a small population size).
Potential biases in the review process
At least two authors independently performed all subjective steps in the review process. We reported on individual studies, not articles, to prevent reporting bias, but we extracted data from all related articles. Funnel plots (not shown) did not suggest the presence of publication bias. If required, we recalculated sickness absence into work days to pool the MD or recalculated SDs from studies when only P values or standard errors were given. If studies reported no time‐to‐event outcomes, we extracted data from survival curves and verified it by comparing the original plot with the plot derived from the extracted data, and then calculated the HRs and associated 95% CIs.
Due to methodological considerations we included only RCTs and excluded non‐RCTs. We already knew we had an adequate number of RCTs because of our previous non‐Cochrane version of this review (Schandelmaier 2012). Furthermore, we decided to exclude studies without at least one face‐to‐face contact and employer‐initiated programmes, which were not our focus. However, we did not have to exclude studies solely for these reasons.
It is challenging to compare multidisciplinary programmes that allow for different interventions, in different intensities, with different support for the control group. However, we tried to choose appropriate inclusion and exclusion criteria. Unfortunately, we did not find enough data to explore further heterogeneity by means of subgroup analyses.
Agreements and disagreements with other studies or reviews
In the previous version of this review (Schandelmaier 2012), we found significant effects for all four of the return‐to‐work outcomes in favour for return‐to‐work coordination programmes. Our new search identified five additional publications: all of them with low risk of bias, a follow‐up ranging from 12 months to 72 months, and moderate to high support for the control group. Thus, we conclude that the quality of research as well as the quality of usual practice has improved.
Other reviews on interventions facilitating return to work have different foci but partly overlap regarding the included studies. In summary, they give no clear recommendations regarding return‐to‐work coordination programmes.
Recently, Van Vilsteren 2015 investigated workplace interventions to prevent disability in workers on sick leave. Especially for workers with musculoskeletal disorders, they found evidence that workplace interventions reduce time to first return to work and cumulative duration of sickness absence. For time to lasting return to work, they found only low‐quality evidence for workplace interventions.
Nieuwenhuijsen 2014 analysed interventions to improve return to work in people with depression. Moderate‐quality evidence suggested that adding a work‐directed intervention to a clinical intervention reduced the number of days on sick leave compared to a clinical intervention alone. For adults with adjustment disorders, Arends 2012 found that cognitive behavioural therapy did not significantly reduce time to partial or full return to work compared with no treatment. For problem‐solving therapy, they found a significant effect on partial return to work after one year compared to non‐guideline based care, but there was no significant effect on time to full return to work.
Palmer 2012 completed a systematic review regarding the effectiveness of community‐ and workplace‐based interventions to reduce sickness absence and job loss. They concluded that most interventions, especially in large and high‐quality studies, show small beneficial effects. No intervention was clearly superior to another, but effort‐intensive interventions were less effective than simple programmes. Clayton 2011 reviewed studies with an individual focus to return people with disabilities and long‐term illnesses back to work. Personal advisors and individual case management helped some participants back to work, but authors concluded that existing programmes must be modified and extended for the more complex needs of those workers further from the labour market. Kuoppala 2008 found that return‐to‐work programmes decreased long sick leaves but not the proportion who returned to work. They emphasised the benefit of involving the workplace in rehabilitation efforts.
Authors' conclusions
Implications for practice.
This review found very low‐ to moderate‐quality evidence that return‐to‐work coordination programmes compared to usual practice do not facilitate return to work. We found no significant differences in our return‐to‐work outcomes at any follow‐up time point. Very low‐ to moderate‐quality evidence suggests no substantial impact on patient‐reported outcomes.
One fairly large, well‐designed study contributed data on more than 8000 participants over 72 months and provides moderate‐quality evidence suggesting no beneficial effect on cumulative sickness absence. On the other hand, we found two nearly identical studies (same setting and interventions, different participants): Stapelfeldt 2011 favoured return‐to‐work coordination programmes, and Jensen 2012 favoured usual practice, even if the results were not significant. These findings challenge the formulation of definitive implications for practice.
Implications for research.
Future studies should investigate lasting return to work for at least four weeks. A longer interval might be even more meaningful. It is not sufficient to report only whether return to work occurred or not; outcomes should capture relapse into sick leave as well.
More studies with a long‐term and very long‐term follow‐up will help to evaluate lasting benefits. A more detailed description of the intervention in both the control and the intervention group are necessary to distinguish the extent to which groups are different from one another. To improve the replicability of interventions, the Template for Intervention Description and Replication (TIDieR) checklist and guide ought to be used (Hoffmann 2014). Furthermore, monitoring additional healthcare utilisation would allow for better comparability.
There is a need for more studies on workers with mental health problems, as we already know that this will be a rising concern in the future (OECD 2014 b).
Furthermore, even if coordinated return‐to‐work programmes are not necessarily employer‐initiated, we believe it is essential to integrate the workplace as much as possible in the return‐to‐work process. Future studies should investigate and report more details on the extent and relevance of employers' involvement.
Acknowledgements
We would like to thank all the authors providing us additional material and information and who patiently answered our questions. We are grateful to Gordon Guyatt for his indispensable support. Furthermore, we thank Mohsen Mousavi, who contributed to the protocol and helped to draft the review.
We thank Jani Ruotsalainen, Managing Editor, Cochrane Work Group for providing administrative and logistical support for the planning of the current review, and Kaisa Neuvonen, Trials Search Co‐ordinator, Cochrane Work Group, for developing and testing the search strategies.
We would also like to thank the Cochrane Work Group's Coordinating Editor Jos Verbeek, Managing Editor Jani Ruotsalainen, the Central Editorial Unit's Senior Editor Toby Lasserson, Editors Deirdre FitzGerald, Anneli Ojajärvi, and Kaisa Neuvonen; and external peer referees Juha Liira, David Bruinvels, Ute Bültmann and Doug Gross for their comments. Last but not least, we thank Joey Kwong for copy‐editing the protocol and Meggan Harris for copy editing the review.
Appendices
Appendix 1. MEDLINE search strategy
1. "absenteeism"[tw]
2. "sick days"[tw]
3. "illness days"[tw]
4. "sick listed"[tw]
5. ("long term"[tw] OR "absence"[tw] OR "leave"[tw]) AND ("disability"[tw] OR "sickness"[tw] OR "sick"[tw])
6. ("benefit"[tw] OR "benefits"[tw] OR "pension"[tw] OR "pensions"[tw]) AND ("claimant"[tw] OR "claimants"[tw] OR "claim"[tw] OR "claims"[tw])
7. "work disablement"[tw]
8. "work disability"[tw]
9. "working disability"[tw]
10. "work absence"[tw]
11. ("injured"[tw] OR "injury"[tw] OR "accident"[tw] OR "sickness"[tw] OR "sick"[tw] OR "disability"[tw] OR "disabled"[tw] OR "disablement"[tw] OR "invalid"[tw] OR "invalidity"[tw] OR "absent"[tw] OR "absence"[tw]) AND ("worker"[tw] OR "workers"[tw] OR "employee"[tw] OR "employees"[tw])
12. ("sickness"[tw] OR "disability"[tw] OR "disabled"[tw] OR "disablement"[tw] OR "invalid"[tw] OR "invalidity"[tw] OR "absent"[tw] OR "absence"[tw] OR "out of work"[tw] OR "social security"[tw] OR "social insurance"[tw]) AND ("benefit"[tw] OR "benefits"[tw] OR "beneficiaries"[tw] OR "beneficiary"[tw] OR "claimant"[tw] OR "claimants"[tw] OR "claim"[tw] OR "claims"[tw] OR "pension"[tw] OR "pensions"[tw] OR "pensioners"[tw] OR "pensioner"[tw] OR "compensation"[tw] OR "compensations"[tw])
13. "Insurance, disability"[tw]
14. "disability insurance"[tw]
15. ("workman's"[tw] OR "workman"[tw] OR "workmans"[tw] OR "workmen's"[tw] OR "workmen"[tw] OR "workmens"[tw] OR "worker's"[tw] OR "worker"[tw] OR "workers"[tw]) AND ("compensation"[tw] OR "compensations"[tw])
16. "case management"[tw]
17. "case manager"[tw]
18. "absence management"[tw]
19. "assertive community treatment"[tw]
20. "management programme"[tw]
21. "management program"[tw]
22. ("project"[tw] OR "programme"[tw] OR "program"[tw] OR "model"[tw] OR "interview"[tw] OR "interviews"[tw] OR "plan"[tw] OR "measure"[tw] OR "measures"[tw] OR "intervention"[tw] OR "interventions"[tw] OR "rehabilitation"[tw] OR "management"[tw]) AND ("co ordinator"[tw] OR "coordinator"[tw] OR "coordination"[tw] OR "co ordination"[tw] OR "coordinated"[tw] OR "co ordinated"[tw] OR "multidisciplinary"[tw] OR "multi disciplinary"[tw] OR "multi professional"[tw] OR "multiprofessional"[tw] OR "multimodal"[tw] OR "multi modal"[tw] OR "integrated"[tw] OR "patient centred"[tw] OR "patient focused"[tw] OR "individual"[tw] OR "individually"[tw] OR "face to face"[tw] OR "one on one"[tw] OR "in person"[tw] OR "personal"[tw] OR "personally"[tw] OR "customized"[tw] OR "customised"[tw] OR "tailored"[tw] OR "on the job"[tw] OR "work focused"[tw] OR "work related"[tw] OR "workplace"[tw] OR "work location"[tw] OR "work‐site"[tw] OR "work place"[tw] OR "job site"[tw] OR "worksite"[tw] OR "occupational"[tw] OR "vocational"[tw] OR "return to work"[tw] OR "return to work" [mesh] OR "counselling"[tw] OR "reintegration"[tw])
23. "rehabilitation"[tw] AND ("project"[tw] OR "programme"[tw] OR "program"[tw] OR "plan"[tw] OR "model"[tw] OR "measure"[tw] OR "measures"[tw] OR "intervention"[tw] OR "interview"[tw] OR "interviews"[tw] OR "intervention"[tw] OR "interventions"[tw] OR "management"[tw])
24. "randomized controlled trial"[pt]
25. "controlled clinical trial"[pt]
26. "randomized"[tiab]
27. "randomised"[tiab]
28. "randomly"[tiab]
29. "trial"[ti]
30. "clinical trials as topic"[mesh: noexp]
31. OR / 1 ‐ 15
32. OR / 16 ‐ 23
33. OR / 24 ‐ 30
34. AND / 31 – 33
Appendix 2. EMBASE search strategy
(("absenteeism" OR "sick days" OR "illness days" OR "sick listed" OR (("long term" OR "absence" OR "leave" ) NEAR/3 ("disability" OR "sickness" OR "sick")) OR (("benefit" OR "benefits" OR "pension" OR "pensions") AND ("claimant" OR "claimants" OR "claim" OR "claims")) OR "work disablement" OR "work disability" OR "working disability" OR "work absence" OR (("injured" OR "injury" OR "accident" OR "sickness" OR "sick" OR "disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence") AND ("worker" OR "workers" OR "employee" OR "employees")) OR (("sickness" OR "disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence" OR "out of work" OR "social security" OR "social insurance") NEAR/3 ("benefit" OR "benefits" OR "beneficiaries" OR "beneficiary" OR "claimant" OR "claimants" OR "claim" OR "claims" OR "pension" OR "pensions" OR "pensioners" OR "pensioner" OR "compensation" OR "compensations")) OR "Insurance, disability" OR "disability insurance" OR (("workman?s" OR "workman" OR "workmans" OR "workmen?s" OR "workmen" OR "workmens" OR "worker?s" OR "worker" OR "workers") Near/3 ("compensation" OR "compensations"))) AND ("case management" OR "case anager" OR "absence management" OR "assertive community treatment" OR "management programme" OR "management program" OR (("project" OR "programme" OR "program" OR "model" OR "interview" OR "interviews" OR "plan" OR "measure" OR "measures" OR "intervention" OR "interventions" OR "rehabilitation" OR "management") NEAR/3 ("co ordinator" OR "coordinator" OR "coordination" OR "co ordination" OR "coordinated" OR "co ordinated" OR "multidisciplinary" OR "multi disciplinary" OR "multi professional" OR "multiprofessional" OR "multimodal" OR "multi modal" OR "integrated" OR "patient centred" OR "patient focused" OR "individual" OR "individually" OR "face to face" OR "one on one" OR "in person" OR "personal" OR "personally" OR "customized" OR "customised" OR "tailored" OR "on the job" OR "work focused" OR "work related" OR "workplace" OR "work location" OR "work‐site" OR "work place" OR "job site" OR "worksite" OR "occupational" OR "vocational" OR "return to work" OR "counselling" OR "reintegration")) OR (("project" OR "programme" OR "program" OR "plan" OR "model" OR "measure" OR "measures" OR "intervention" OR "interview" OR "interviews" OR "intervention" OR "interventions" OR "management") NEAR/3 "rehabilitation"))):ti:ab:de AND ([controlled clinical trial]/lim OR [randomized controlled trial]/lim OR "randomized":ti:ab OR "randomly":ti:ab OR "trial":ti OR "controlled clinical trial":de OR "single blind procedure":de OR "double blind procedure":de OR "triple blind procedure":de OR (doubl* next blind*):ti:ab OR (singl* next blind*):ti:ab OR (assign*):ti:ab OR (allocate*):ti:ab OR (volunteer*):ti:ab) AND [embase]/lim
Appendix 3. CINAHL search strategy
TX (("absenteeism" OR "sick days" OR "illness days" OR "sick listed" OR (("long term" OR "absence" OR "leave") AND ("disability" OR "sickness" OR "sick")) OR (("benefit" OR "benefits" OR "pension" OR "pensions") AND ("claimant" OR "claimants" OR "claim" OR "claims")) OR "work disablement" OR "work disability" OR "working disability" OR "work absence" OR (("injured" OR "injury" OR "accident" OR "sickness" OR "sick" OR "disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence") AND ("worker" OR "workers" OR "employee" OR "employees")) OR (("sickness" OR "disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence" OR "out of work" OR "social security" OR "social insurance") AND ("benefit" OR "benefits" OR "beneficiaries" OR "beneficiary" OR "claimant" OR "claimants" OR "claim" OR "claims" OR "pension" OR "pensions" OR "pensioners" OR "pensioner" OR "compensation" OR "compensations")) OR "Insurance, disability" OR "disability insurance" OR (("workman?s" OR "workman" OR "workmans" OR "workmen?s" OR "workmen" OR "workmens" OR "worker?s" OR "worker" OR "workers") AND ("compensation" OR "compensations"))) AND ("case management" OR "case manager" OR "absence management" OR "assertive community Treatment" OR "management programme" OR "management program" OR (("project" OR "programme" OR "program" OR "model" OR "interview" OR "interviews" OR "plan" O "measure" OR "measures" OR "intervention" OR "interventions" OR "rehabilitation" OR "management") AND ("co ordinator" OR "coordinator" OR "coordination" OR "co ordination" OR "coordinated" OR "co ordinated" OR "multidisciplinary" OR "multi disciplinary" OR "multi professional" OR "multiprofessional" OR "multimodal" OR "multi modal" OR "integrated" OR "patient centred" OR "patient focused" OR "individual" OR "individually" OR "face to face" OR "one on one" OR "in person" OR "personal" OR "personally" OR "customized" OR "customised" OR "tailored" OR "on the job" OR "work focused" OR "work related" OR "workplace" OR "work location" OR "work‐site" OR "work place" OR "job site" OR "worksite" OR "occupational" OR "vocational" OR "return to work" OR "counselling" OR "reintegration")) OR (("project" OR "programme" OR "program" OR "plan" OR "model" OR "measure" OR "measures" OR "intervention" OR "interview" OR "interviews" OR "intervention" OR "interventions" OR "management" ) AND "rehabilitation"))) AND (TI (randomly OR randomi?ed OR trial) OR AB (randomly OR randomi?ed))
Appendix 4. PsycINFO search strategy
(("absenteeism" OR "sick days" OR "illness days" OR "sick listed" OR (("long term" OR "absence" OR "leave" ) ADJ3 ("disability" OR "sickness" OR "sick")) OR (("benefit" OR "benefits" OR "pension" OR "pensions") AND ("claimant" OR "claimants" OR "claim" OR "claims")) OR "work disablement" OR "work disability" OR "working disability" OR "work absence" OR (("injured" OR "injury" OR "accident" OR "sickness" OR "sick" OR "disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence") AND ("worker" OR "workers" OR "employee" OR "employees")) OR (("sickness" OR "disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence" OR "out of work" OR "social security" OR "social insurance") ADJ3 ("benefit" OR "benefits" OR "beneficiaries" OR "beneficiary" OR "claimant" OR "claimants" OR "claim" OR "claims" OR "pension" OR "pensions" OR "pensioners" OR "pensioner" OR "compensation" OR "compensations")) OR "Insurance, disability" OR "disability insurance" OR (("workman?s" OR "workman" OR "workmans" OR "workmen?s" OR "workmen" OR "workmens" OR "worker?s" OR "worker" OR "workers") Adj3 ("compensation" OR "compensations"))) AND ("case management" OR "case manager" OR "absence management" OR "assertive community Treatment" OR "management programme" OR "management program" OR (("project" OR "programme" OR "program" OR "model" OR "interview" OR "interviews" OR "plan" OR "measure" OR "measures" OR "intervention" OR "interventions" OR "rehabilitation" OR "management") ADJ3 ("co ordinator" OR "coordinator" OR "coordination" OR "co ordination" OR "coordinated" OR "co ordinated" OR "multidisciplinary" OR "multi disciplinary" OR "multi professional" OR "multiprofessional" OR "multimodal" OR "multi modal" OR "integrated" OR "patient centred" OR "patient focused" OR "individual" OR "individually" OR "face to face" OR "one on one" OR "in person" OR "personal" OR "personally" OR "customized" OR "customised" OR "tailored" OR "on the job" OR "work focused" OR "work related" OR "workplace" OR "work location" OR "work‐site" OR "work place" OR "job site" OR "worksite" OR "occupational" OR "vocational" OR "return to work" OR "counselling" OR "reintegration")) OR (("project" OR "programme" OR "program" OR "plan" OR "model" OR "measure" OR "measures" OR "intervention" OR "interview" OR "interviews" OR "intervention" OR "interventions" OR "management") ADJ3 "rehabilitation"))).tw. AND ("random*".ti,ab. OR "trial".ti.)
Appendix 5. CENTRAL search strategy
("Absenteeism" OR "sick leave" OR "sick absence" OR "sickness absence" OR "sick listed" OR ("long term" AND ("sickness" OR "sick")) OR "sickness benefit" OR "sickness benefits" OR (("benefit" OR "benefits" OR "pension" OR "pensions") AND ("claimant" OR "claimants" OR "claim" OR "claims")) OR "work disablement" OR "working disablement" OR "work disability" OR "working disability" OR (("injured" OR "injury" OR "accident" OR "sickness" OR "sick" OR "disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence" ) AND ("worker" OR "workers" OR "employee" OR "employees")) OR (("disability" OR "disabled" OR "disablement" OR "invalid" OR "invalidity" OR "absent" OR "absence" OR "out of work" OR "Social Security" OR "Insurance OR Disability" ) AND ("benefit" OR "benefits" OR "beneficiaries" OR "beneficiary" OR "claimant" OR "claimants" OR "claim" OR "claims" OR "pension" OR "pensions" OR "pensioners" OR "pensioner"))) AND ("case management" OR "case management" OR "case manager" OR "absence management" OR "assertive community Treatment" OR "management programmme" OR "management program" OR (("project" OR "programme" OR "program" OR "Model" OR "interview" OR "interviews" OR "plan" OR "measure" OR "measures" OR "intervention" OR "interventions" OR "rehabilitation" OR "rehabilitation" OR "management") AND ("co ordinator" OR "coordinator" OR "coordination" OR "co ordination" OR "coordinated" OR "co ordinated" OR "multidisciplinary" OR "multi disciplinary" OR "multi professional" OR "multiprofessional" OR "multimodal" OR "multi modal" OR "integrated" OR "patient centred" OR "patient focused" OR "individual" OR "individually" OR "face to face" OR "one on one" OR "in person" OR "personal" OR "personally" OR "customized" OR "customised" OR "tailored" OR "on the job" OR "work focused" OR "work related" OR "workplace" OR "occupational" OR "vocational" OR "return to work" OR "counselling" OR "reintegration")) OR (("project" OR "programme" OR "program" OR "plan" OR "Model" OR "measure" OR "measures" OR "intervention" OR "interview" OR "interviews" OR intervention OR interventions OR "management") AND "rehabilitation"))
Data and analyses
Comparison 1. Return‐to‐work outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 9 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term, follow‐up 6 months | 2 | 161 | Hazard Ratio (Random, 95% CI) | 1.32 [0.93, 1.88] |
| 1.2 Long‐term, follow‐up 12 months | 6 | 1935 | Hazard Ratio (Random, 95% CI) | 1.25 [0.95, 1.66] |
| 1.3 Very long‐term, follow‐up longer than 12 months | 2 | 474 | Hazard Ratio (Random, 95% CI) | 0.93 [0.74, 1.17] |
| 2 Time to return to work, sensitivity analysis (low risk of bias studies only) | 7 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term, follow‐up 6 months | 1 | 110 | Hazard Ratio (Random, 95% CI) | 1.17 [0.76, 1.79] |
| 2.2 Long‐term, follow‐up 12 months | 6 | 1935 | Hazard Ratio (Random, 95% CI) | 1.25 [0.95, 1.66] |
| 2.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Hazard Ratio (Random, 95% CI) | 0.86 [0.68, 1.09] |
| 3 Cumulative sickness absence in work days | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Short‐term, follow‐up 6 months | 1 | 113 | Mean Difference (IV, Random, 95% CI) | ‐16.18 [‐32.42, 0.06] |
| 3.2 Long‐term, follow‐up 12 months | 6 | 1339 | Mean Difference (IV, Random, 95% CI) | ‐14.84 [‐38.56, 8.88] |
| 3.3 Very long‐term, follow‐up longer than 12 months | 1 | 8052 | Mean Difference (IV, Random, 95% CI) | 7.0 [‐15.17, 29.17] |
| 4 Proportion at work at end of the follow‐up | 7 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Short‐term, follow‐up 6 months | 5 | 1388 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.86, 1.30] |
| 4.2 Long‐term, follow‐up 12 months | 5 | 3061 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.99, 1.15] |
| 4.3 Very long‐term, follow‐up longer than 12 months | 2 | 815 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.82, 1.07] |
| 5 Proportion at work at end of the follow‐up, sensitivity analysis (low risk of bias studies only) | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Short‐term, follow‐up 6 months | 3 | 873 | Risk Ratio (IV, Random, 95% CI) | 1.20 [1.10, 1.30] |
| 5.2 Long‐term, follow‐up 12 months | 3 | 1174 | Risk Ratio (IV, Random, 95% CI) | 1.08 [0.94, 1.23] |
| 5.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.80, 1.13] |
| 6 Proportion who had ever returned to work | 12 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Short‐term, follow‐up 6 months | 4 | 675 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.63, 1.19] |
| 6.2 Long‐term, follow‐up 12 months | 8 | 3822 | Risk Ratio (IV, Random, 95% CI) | 1.03 [0.97, 1.09] |
| 6.3 Very long‐term, follow‐up longer than 12 months | 3 | 938 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.88, 1.02] |
| 7 Proportion who had ever returned to work, sensitivity analysis (low risk of bias studies only) | 8 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Short‐term, follow‐up 6 months | 2 | 160 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.86, 1.31] |
| 7.2 Long‐term, follow‐up 12 months | 6 | 1935 | Risk Ratio (IV, Random, 95% CI) | 1.04 [0.96, 1.11] |
| 7.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.87, 1.08] |
Comparison 2. Patient‐reported outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0 | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term, follow‐up 6 months | 4 | 427 | Mean Difference (IV, Random, 95% CI) | ‐4.76 [‐14.89, 5.36] |
| 1.2 Long‐term, follow‐up 12 months | 6 | 2319 | Mean Difference (IV, Random, 95% CI) | ‐2.98 [‐5.33, ‐0.63] |
| 1.3 Very long‐term, longer than 12 months | 1 | 80 | Mean Difference (IV, Random, 95% CI) | ‐7.20 [‐15.76, 1.36] |
| 2 Pain ‐ pooled RDs of workers with an improvement greater than the MID of 10.0 | 7 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term, follow‐up 6 months | 4 | Risk Difference (Random, 95% CI) | ‐0.03 [‐0.11, 0.05] | |
| 2.2 Long‐term, follow‐up 12 months | 6 | Risk Difference (Random, 95% CI) | ‐0.03 [‐0.06, ‐0.00] | |
| 2.3 Very long‐term, longer than 12 months | 1 | Risk Difference (Random, 95% CI) | ‐0.02 [‐0.11, 0.07] | |
| 3 Overall function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0 | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Short‐term, follow‐up 6 months | 3 | 295 | Mean Difference (IV, Random, 95% CI) | 8.13 [3.95, 12.32] |
| 3.2 Long‐term, follow‐up 12 months | 5 | 2235 | Mean Difference (IV, Random, 95% CI) | 2.74 [‐0.15, 5.64] |
| 4 Overall function ‐ pooled RDs of workers with an improvement greater than the MID of 10.0 | 6 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 4.1 Short‐term, follow‐up, 6 months | 3 | Risk Difference (Random, 95% CI) | 0.16 [‐0.04, 0.37] | |
| 4.2 Long‐term, follow‐up 12 months | 5 | Risk Difference (Random, 95% CI) | 0.00 [‐0.09, 0.09] | |
| 5 Physical function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 8.4 | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Short‐term, follow‐up 6 months | 3 | 336 | Mean Difference (IV, Random, 95% CI) | 3.47 [‐3.26, 10.20] |
| 5.2 Long‐term, follow‐up 12 months | 4 | 1860 | Mean Difference (IV, Random, 95% CI) | 2.19 [‐2.29, 6.67] |
| 5.3 Very long‐term, follow‐up longer than 12 months | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 1.85 [‐2.25, 5.95] |
| 6 Physical function ‐ pooled RDs of workers with an improvement greater than the MID of 8.4 | 5 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 6.1 Short‐term, follow‐up 6 months | 3 | Risk Difference (Random, 95% CI) | 0.03 [‐0.07, 0.13] | |
| 6.2 Long‐term, follow‐up 12 months | 4 | Risk Difference (Random, 95% CI) | 0.01 [‐0.02, 0.03] | |
| 6.3 Very long‐term, follow‐up longer than 12 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.02, 0.02] | |
| 7 Social function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 11.7 | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Long‐term, follow‐up 12 months | 2 | 1636 | Mean Difference (IV, Random, 95% CI) | 2.84 [‐0.09, 5.77] |
| 8 Social function ‐ pooled RDs of workers with an improvement greater than the MID of 11.7 | 2 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 8.1 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.01 [‐0.02, 0.04] | |
| 9 Mental function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 7.3 | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Short‐term, follow‐up 6 months | 1 | 125 | Mean Difference (IV, Random, 95% CI) | 1.85 [‐2.67, 6.37] |
| 9.2 Long‐term, follow‐up 12 months | 3 | 1737 | Mean Difference (IV, Random, 95% CI) | 3.14 [1.16, 5.11] |
| 9.3 Very long‐term, follow‐up longer than 12 months | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 6.09 [0.56, 11.63] |
| 10 Mental function ‐ pooled RDs of workers with an improvement greater than the MID of 7.3 | 3 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 10.1 Short‐term, follow‐up 6 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.01, 0.01] | |
| 10.2 Long‐term, follow‐up 12 months | 3 | Risk Difference (Random, 95% CI) | 0.00 [‐0.01, 0.01] | |
| 10.3 Very long‐term, follow‐up longer than 12 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.01, 0.01] | |
| 11 Depression ‐ scale 0 to 27 (higher score indicates deterioration) ‐ MID 5.0 | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Short‐term, follow‐up 6 months | 3 | 252 | Mean Difference (IV, Random, 95% CI) | 0.37 [‐2.81, 3.55] |
| 11.2 Long‐term, follow‐up 12 months | 2 | 420 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐1.07, 1.07] |
| 12 Depression ‐ pooled RDs of workers with an improvement greater than the MID of 5.0 | 4 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 12.1 Short‐term, follow‐up 6 months | 3 | Risk Difference (Random, 95% CI) | 0.03 [‐0.07, 0.12] | |
| 12.2 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.01 [‐0.04, 0.06] | |
| 13 Anxiety ‐ scale 0 to 21 (higher score indicates deterioration) ‐ MID 4.0 | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Short‐term, follow‐up 6 months | 2 | 208 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐3.24, 3.21] |
| 13.2 Long‐term, follow‐up 12 months | 2 | 420 | Mean Difference (IV, Random, 95% CI) | 0.97 [‐0.17, 2.12] |
| 14 Anxiety ‐ pooled RDs of workers with an improvement greater than the MID of 4.0 | 3 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 14.1 Short‐term, follow‐up 6 months | 2 | Risk Difference (Random, 95% CI) | ‐0.01 [‐0.08, 0.07] | |
| 14.2 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.02 [‐0.03, 0.08] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bültmann 2009.
| Methods |
Design: RCT, parallel, 2 arms Country: Denmark Sample size: 119 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: April 2004 to April 2005 Method of recruitment: 4 participating municipalities, invitation to an information meeting Follow‐up: 3, 6, 12 months |
|
| Participants |
Health problem: low back pain, neck pain, musculoskeletal disorders Age in years: mean 43.7 (SD 11.3) Female in %: 55 Intervention group: 68 participants Control group: 51 participants Inclusion criteria: absent from work 4‐12 weeks, aged 18‐65 years, understanding and speaking Danish, reimbursement request indicating low back pain or musculoskeletal disorders as the main cause of sick leave Exclusion criteria: mental health disorders, alcohol or drug addiction, pregnancy, quit their job or had been fired before randomisation Duration and type of sick leave: 1‐3 months, mean 39.3 days (SD 20.9); full sick leave Type of sick leave compensation: employer paid according to public sickness benefit scheme |
|
| Interventions |
Intervention: coordinated and tailored work rehabilitation Components of intervention:
Team: occupational physician, occupational physiotherapist, chiropractor, psychologist, social worker Involvement of the employer: yes Providers of intervention: rehabilitation team, experience and training not reported Theoretical basis: Canadian multidisciplinary work rehabilitation programme (i.e. the Sherbrooke model, Loisel 2002) Duration: maximum 3 months Control: conventional case management as provided by the municipality; same information about the study and the same (follow‐up) questionnaires, no additional assessment or action |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation without stratification |
| Allocation concealment (selection bias) | Low risk | Concealed (author information) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 participants withdrew their consent after randomisation; for the rest complete data on return‐to‐work outcomes, 33% loss to follow‐up on patient‐related outcomes, non‐response analysis: “A non‐response analysis revealed that nonrespondents in both groups and at both time points were more likely to be men. Moreover, in the CTWR [coordinated and tailored work rehabilitation] group, non‐respondents at 3 month follow‐up tended to have less vocationally education and more sickness absence hours. Otherwise, non‐respondents in both groups did not differ significantly from respondents with respect to other sociodemographic, health status, and work absence variables tested at 3 and 12 months follow‐up.” (p. 86) |
| Selective reporting (reporting bias) | Unclear risk | No study protocol published, “pain intensity last week” was considered to be less relevant and was not reported (author information) |
| Other bias | Low risk | No indications of other sources of bias |
Davey 1994.
| Methods |
Design: RCT, parallel, 2 arms Country: Scotland, North‐East England Sample size: 50 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: not reported Method of recruitment: the 4 participating insurance companies identified potential clients from the personal injury claims files, invitation by letter Follow‐up: 6, 12 months (after 6 months: intervention for both groups, therefore only 6 months follow‐up data analysed) |
|
| Participants |
Health problem: injuries likely to result in absence from work of 6 months or more Age in years: mean 39.4, range 18‐61 Female in %: 18 Intervention group: 33 participants Control group: 17 participants Inclusion criteria: residents in Scotland or North‐East England, aged 16‐65 years, in the labour market at the time of injury, injuries likely to result in absences from work ≥ 6 months and/or permanent disability Exclusion criteria: people with catastrophic injuries Duration and type sick leave: median 20 months, mean 21 months, range 3‐50 months; full sick leave Type of sick leave compensation: personal injury insurance (private insurance) |
|
| Interventions |
Intervention: rehabilitation coordinator service Components of intervention:
Team: physiotherapist, psychologist, consultant in rehabilitation medicine, occupational therapist Involvement of the employer: no Providers of intervention: a physiotherapist as coordinator with experience in care coordination, 3‐month induction programme Theoretical basis: Chamberlain 1991, Thornicroft 1991 Duration: 6 months Control: no restrictions; the intervention group received help for 12 months, beginning immediately after the initial assessment, while the control group had no contact with the coordinator for 6 months, then received help for 6 months between their 6 and 12 month reassessments |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Concealed in sequentially numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up, complete data at 6 months |
| Selective reporting (reporting bias) | Unclear risk | Unclear, insufficient information |
| Other bias | Low risk | No indications of other sources of bias |
Donceel 1999.
| Methods |
Design: RCT, parallel, 2 arms Country: Belgium Sample size: 710 in 60 clusters Unit of allocation: cluster Unit of analysis: individuals Date of recruitment: October 1996 to June 1997 Method of recruitment: patients of all medical advisors of Christian Sickness Fund who introduced a claim for benefits after surgery for disc herniation Follow‐up: 6, 12 months |
|
| Participants |
Health problem: surgery for disc herniation Age in years: mean 39.2 Female in %: 35 Intervention group: 345 participants (30 medical advisors) Control group: 365 participants (30 medical advisors) Inclusion criteria: absent from work before surgery < 1 year, aged 15‐64 years, worker Exclusion criteria: self‐employment Duration and type of sick leave: 2‐2.5 months; full sick leave Type of sick leave compensation: a claim for benefits after surgery for disc herniation |
|
| Interventions |
Intervention: new guideline for medical advisers Components of intervention: intervention guidelines for the medical adviser:
Team: general practitioner, social insurance agent, social insurance physician, other healthcare personnel (not reported) Involvement of the employer: no Providers of intervention: 30 medical advisers (social insurance physicians), experience and training not reported Theoretical basis: a number of rehabilitation guidelines Duration: as long as participant is on disability benefit Control: medical practice as in the past; focus on corporal damage, few rehabilitation efforts |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement): none |
|
| Notes | Each medical advisor was responsible for a specific region, baseline characteristics of medical advisors not reported (unit of randomisation) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | No concealment of allocation reported (usually not relevant in cluster randomised trials, as all clusters are randomised at once) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding, but participants were probably not aware of the intervention, case mangers were not blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blind for return‐to‐work outcomes Unclear if blind for patient related outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | Low risk | No indications of other sources of bias, recruitment‐bias implausible: participants were blind during recruitment process, no analysis of cluster effect reported |
Feuerstein 2003.
| Methods |
Design: RCT, parallel, 2 arms Country: USA Sample size: 205 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: July 1999 to December 2000 Method of recruitment: invitation by letter from the medical director of the Office of Worker's Compensation Programs Follow‐up: 4, 10, 16 months |
|
| Participants |
Health problem: work‐related upper extremity disorder Age in years: mean 46 (SD 8.6) Female in %: 78 Intervention group: initial number of participants not reported; 58 participants answered the patient satisfaction questionnaire Control group: initial number of participants not reported; 73 participants answered the patient satisfaction questionnaire Inclusion criteria: aged 18‐65 years, accepted single worker's compensation claim according to work‐related upper extremity disorder, no claims in the previous 2 years, claims adjudicated and accepted as work‐related within 90 days of filing (only those still out of work or on modified duty at the time of claim adjudication were eligible) Exclusion criteria: none Duration and type of sick leave: 1‐6 months; full‐ and part‐time sick leave Type of sick leave compensation: claims of the US Department of Labor's Office of Worker's Compensation Programs |
|
| Interventions |
Intervention: integrated case management Components of intervention:
Team: “e.g. supervisor, injury compensation specialist, medical providers, claims examiner” (p. 383 Shaw 2001) Involvement of the employer: yes Providers of intervention: 32 nurse case managers: 2 years experience providing case management service, 2‐day training in ergonomic assessment and workplace accommodations, problem‐solving approach, experience in coordination of medical care Theoretical basis: Shaw 2001 Duration: 4 months, variable Control: usual practice; 33 nurse case managers, focus on medical care, no training in a structured protocol |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | Return‐to‐work data was not published, but provided by one of the authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “[P]articipants were randomly assigned” (p. 805) |
| Allocation concealment (selection bias) | High risk | No concealed allocation (author information) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Probably not blind for return‐to‐work outcomes Probably not blind for patient related outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 40% losses to follow‐up for return‐to‐work outcomes, 36%‐61% losses to follow‐up for patient‐reported outcomes (author information) |
| Selective reporting (reporting bias) | High risk | Return‐to‐work outcomes not published, one author provided outcomes as far as possible |
| Other bias | Low risk | No indications of other sources of bias |
Jensen 2012.
| Methods |
Design: RCT, parallel, 2 arms with 2 subgroups Subgroups: those with influence on the planning of their own work and no perceived risk of losing job and/or being a work injury claimant; those without influence on the planning of their own work or feeling at risk of losing job and not a work injury claimant Country: Denmark Sample size: 351 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: November 2004 to June 2007 Method of recruitment: referred by their general practitioner, recruited at the Spine Center Follow‐up: 12, 24 months |
|
| Participants |
Health problem: low back pain Age in years: mean 42.0 (SD 10.5) Female in %: 52 Intervention group: 176 participants Control group: 175 participants Inclusion criteria: absent from work for 3‐16 weeks, aged 16‐60 years, ability to read and speak Danish Exclusion criteria: unemployed, continuing or progressive symptoms indicating plans for surgery, surgery in the spine within the past 12 months, diagnosis of specific back disease (e.g. tumour), diagnosis of primary psychiatric disease, pregnancy, known substance abuse Duration and type of sick leave: range 3‐16 weeks; full‐ and part‐time sick leave Type of sick leave compensation: municipalities, financed by tax payers |
|
| Interventions |
Intervention: multidisciplinary intervention (same as Stapelfeldt 2011) Components of intervention:
Team: specialist of social medicine, a rheumatologist, a physiotherapist, a social worker, and an occupational therapist Involvement of the employer: yes Providers of intervention: 3 case managers; experience and training not reported Theoretical basis: Canadian multidisciplinary work rehabilitation programme (i.e. the Sheerbrooke model, Loisel 2002) Duration: median 18 weeks Control: municipality case management and brief intervention:
Same control group interventions as Stapelfeldt 2011 and Myhre 2014 (without municipality case management) |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | The proportion at work at end of the follow‐up was reported to 'last job' or 'modified job or training'; we analysed the proportion returned to last job followed by a sensitivity analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block‐randomisation |
| Allocation concealment (selection bias) | Low risk | Allocation was carried out by a secretary |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not possible; only the first clinical examination was carried out double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Author information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete data for return‐to‐work outcomes; for patient‐reported outcomes 39% losses to follow‐up after 12 months |
| Selective reporting (reporting bias) | Low risk | Study protocol published; all outcomes reported; after 24 months no reporting of patient‐reported outcomes |
| Other bias | Low risk | No indications of other sources of bias |
Lambeek 2010.
| Methods |
Design: RCT, parallel, 2 arms Country: Netherlands Sample size: 134 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: November 2005 to April 2007 Method of recruitment: in each hospital a competent hospital employee identified the source population weekly from the computerised patient record system, invitation by mail Follow‐up: 3, 6, 12 months |
|
| Participants |
Health problem: non‐specific chronic low back pain Age in years: mean 46.2 (SD 9.1) Female in %: 42 Intervention group: 66 participants Control group: 68 participants Inclusion criteria: aged 18‐65 years, low back pain > 12 weeks, visited an outpatient clinic in one of the participating hospitals, absent or partially absent from work, paid employment or self‐employed (> 8 hours/week) Exclusion criteria: absent from work > 2 years, temporarily work for an employment agency without detachment, lumbar spine surgery in the past 6 weeks or surgery or invasive examinations within 3 months, serious psychiatric or cardiovascular illness, specific low back pain (due to infection, tumour, osteoporosis, rheumatoid arthritis, fracture or inflammatory process), pregnancy Duration and type of sick leave: mean 22 weeks; full‐ and part‐time sick leave Type of sick leave compensation: employer is responsible for 2 years (is obliged to have a company insurance) |
|
| Interventions |
Intervention: integrated care Components of intervention:
Team: clinical occupational physician, patients occupational physician, general practitioner, medical specialist, occupational therapist, physiotherapist Involvement of the employer: yes Providers of intervention: 2 case managers (occupational physicians), 2 days training programme Theoretical basis: not reported Duration: 67 calender days (SD 32) Control: usual practice; guidance from health professionals, average 0.2 visits to case managers |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | EQ‐5D scores by author information | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random‐sequence table |
| Allocation concealment (selection bias) | Low risk | Opaque, sequentially numbered, and sealed coded envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 13% losses to follow‐up for return‐to‐work outcomes, 7% losses to follow‐up for patient‐reported outcomes, missing outcome data balanced in numbers across groups, with similar reasons for missing outcome data and plausible effect size among missing data (assuming a smaller effect in same direction) not enough to introduce clinically relevant bias) |
| Selective reporting (reporting bias) | Low risk | Study protocol published, all outcomes reported |
| Other bias | Low risk | No indications of other sources of bias |
Lindh 1997.
| Methods |
Design: RCT, parallel, 2 arms with 2 subgroups Subgroups: Swedes; immigrants Country: Sweden Sample size: 611 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: not reported Method of recruitment: 7 social insurance offices in Gotenburg reported cases reaching a continuous sick leave of 90 days; invitation by letter Follow‐up: 3 months intervals up to 60 months |
|
| Participants |
Health problem: non‐specific chronic musculoskeletal pain Age in years: mean 39.5, range 20‐55 Female in %: 62 Intervention group: 351 participants Control group: 296 participants Inclusion criteria: absent from work < 180 days sick listed in the preceding 2 years, age < 56 years Exclusion criteria: ongoing rehabilitation, partial sick leave, pregnancy Duration and type of sick leave: 3 months or more; full sick leave Type of sick leave compensation: sick benefit through the Swedish social insurance system |
|
| Interventions |
Intervention: multidisciplinary rehabilitation programme Components of intervention: outpatient regime with:
Team: rehabilitation physician, nurse, physical therapist, psychotherapist, psychologist, occupational therapist, social worker, vocational counsellor Involvement of the employer: no Providers of intervention: rehabilitation team, experience and training not reported Theoretical basis: not reported Duration: individually Control: usual practice; physical therapy and other rehabilitation measures |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement): none |
|
| Notes | No information about attrition after randomisation Contradicting information, whether time point 0 in the graph corresponds to time of randomisation or sick listing (we assumed randomisation) Contradicting information between figures and text Since follow‐up was much longer than in other studies, we analysed the data on the 24 months follow‐up and conducted a sensitivity analysis using 60 months outcome. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No method reported |
| Allocation concealment (selection bias) | Unclear risk | No concealment reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High level of attrition directly after randomisation: 77 (24%) in the intervention group returned to work between randomisation and first visit; to correct for possible selection bias a similar proportion in the control group was randomly excluded A further 80 patients never received the study intervention because of their doctor's refusal (n = 24), other rehabilitation (n = 38), withdraw (n = 11) or other (n = 7); these 80 patients were included in the analysis (intention‐to‐treat), it seems plausible that further patients were lost to follow‐up after the intervention started |
| Selective reporting (reporting bias) | Low risk | Results presented in subgroups (Swedes and immigrants), we extracted return‐to‐work rates from graphs and recombined subgroups |
| Other bias | Unclear risk | Unclear |
Myhre 2014.
| Methods |
Design: RCT, parallel, 2 arms Country: Norway Sample size: 405 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: August 2009 to August 2011 Method of recruitment: patients referred for diagnostic consideration or multidisciplinary treatment of neck and/or back pain were screened for eligibility at their first consultation at the outpatient clinic Follow‐up: 4, 12 months |
|
| Participants |
Health problem: neck pain (10%) and low back pain (90%) Age in years: mean 40.59 (SD 9.86) Female in %: 46 Intervention group: 203 participants Control group: 202 participants Inclusion criteria: absent from work 4‐52 weeks, employed or self‐employed Exclusion criteria: need for surgical treatment, cauda equina syndrome, symptomatic spinal deformities, osteoporosis with fractures, inflammatory rheumatic diseases, pregnancy, legal labour disputes, insufficient Norwegian language skills, cardiac/pulmonary/metabolic disease with functional restrictions, mental disorders. Duration and type of sick leave: mean 112 days (IQR 71‐182); full‐ and part‐time sick leave Type of sick leave compensation: sickness benefits, a work assessment allowance pension, or a disability pension from the Norwegian Labour and Welfare Administration |
|
| Interventions |
Intervention: work‐focused intervention Components of intervention:
Team: physician, physical therapist, case worker, medical specialist, group discussions, lecturer Involvement of the employer: yes Providers of intervention: caseworkers, experience and training not reported Theoretical basis: not reported Duration: 3 weeks Control: usual practice:
|
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | Secondary outcomes from Marchand 2015; authors provided additional outcome data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “An independent statistician generated a random block sequence stratified by hospital.” (p. 2001) |
| Allocation concealment (selection bias) | Low risk | Concealed (author information) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up for return‐to‐work outcomes, 26% losses to follow‐up for patient‐reported outcomes “Patients lost to follow‐up at 12 months had higher baseline disability scores (mean difference 3.60, p = 0.018), reported higher baseline pain (mean difference 0.52, p = 0.039) and higher baseline FABQ‐P scores (mean difference 1.57, p =0.015). There were also a significantly higher number of men, smokers, patients with a foreign mother tongue, and patients with low education in patients lost to follow‐up. The response rate was 74% at the 12‐month follow‐up. There were a similar number of patients lost to follow‐up in both groups” (Marchand 2015; p. 5) |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | Low risk | No indications of other sources of bias |
Purdon 2006.
| Methods |
Design: RCT, parallel, 4 arms Country: United Kingdom Sample size: 1423 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: April 2003 for 2 years Method of recruitment: potential clients spoke with the central telephone contact centre, brief explanation of the trial, check for eligibility Follow‐up: 20‐36 weeks |
|
| Participants |
Health problem: any condition likely to result in a 50% chance to return to work (musculoskeletal, mental and behavioural problems, injuries) Age in years: mean 44.0 Female in %: 57 Intervention group: 571 (weighted: 713 participants) Control group: 458 (weighted: 710 participants) Inclusion criteria: absent from work 6‐26 weeks, employed/self‐employed and working for > 16 hours/week, living and working within one of the pilot areas Exclusion criteria: not be within 18 weeks of planned retirement Duration and type of sick leave: 1.5‐6 months; full sick leave Type of sick leave compensation: 30.4% incapacity benefit, rest unclear |
|
| Interventions |
Intervention: job retention and rehabilitation Components of intervention:
Team: psychologist, psychotherapist, physical therapist, podiatrists, chiropractors, osteopaths, dieticians Involvement of the employer: yes Providers of intervention: case managers, experience and training not reported Theoretical basis: not reported Duration: 20 to 36 weeks Control: usual practice; no systematic aid, low levels of work support |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | Authors presented data only for the weighted numbers of patients: “These unequal numbers per group inevitably leads to some concerns that the randomisation groups may not be strictly balanced: to address this a thorough non‐response analysis has been carried out and the data has been weighted to help minimise any non‐response bias.” (p. 2) Return to work was reported for at least 2 weeks, 6 weeks or 13 weeks: due to the limited follow‐up of 20‐36 weeks, we disregarded the 13 weeks outcome which most participants probably could not achieve in this timeframe; to ensure the longest follow‐up, we used the data for the 2 weeks outcome and conducted sensitivity analyses using 6 and 13 weeks outcome |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome survey for return‐to‐work outcomes with risk of recall in both groups Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High rates of non‐response (20% intervention group, 35% control group) |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | High risk | Low compliance (88% received return‐to‐work‐plan, 72% of those followed the plan), probably bias through weighting: “The weighting strategy could have introduced bias into the impact estimates. A comparison . . . showed that . . . the estimates have not been affected substantially. We conclude that the weighting has not distorted the measurement of the impact in a way that adversely affects the comparison of the randomisation groups or the interpretation of the estimates.” (p. 142) |
Rossignol 2000.
| Methods |
Design: RCT, parallel, 2 arms Country: Canada Sample size: 110 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: June 1995 to December 1996 Method of recruitment: invitation by letter and by telephone to all consecutive cases eligible for inclusion in the computer system of Quebec Worker's Compensation Board in Montreal office Follow‐up: 3, 6 months |
|
| Participants |
Health problem: any work‐related injury to the middle or lower vertebral column, not surgery or multiple injuries Age in years: mean 37.6 (SD 10.1) Female in %: 28 Intervention group: 54 participants Control group: 56 participants Inclusion criteria: absent from work 4‐8 weeks from the date of filing a claim, compensation for any work‐related injury to the thoracic, lumbar, and/or sacral portions of the vertebral column Exclusion criteria: history of compensation for the back in the previous year or history of spinal surgery at any time in the past, multiple injuries involving sites other than mid‐ or lower spine, workers with claims labelled as a recurrent by the Quebec Worker's Compensation Board or in litigation at the time of recruitment, pregnancy, no communication in French or in English Duration and type of sick leave: cumulative 40 days of absence from work; full sick leave Type of sick leave compensation: Quebec Worker's Compensation Board (public insurance) |
|
| Interventions |
Intervention: programme for coordination of primary health care (CORE) Components of intervention:
Team: treating physician, chiropractor, physiotherapist Involvement of the employer: no direct contact, but workplace accommodations on occasion Providers of intervention: a team of 2 primary care physicians and a nurse, experience and training not reported Theoretical basis: clinical guideline for the management of back pain Duration: until return to work Control: usual practice; instruction to continue with their treating physician |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Consecutively numbered sealed envelopes, allocation was probably concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | For return‐to‐work outcomes, no attrition according to author, for patient related outcomes 18% missing data, “The number of nonreturned questionnaires at 6 months was relatively large but equal in both groups, and the baseline functional scores were similar to those who returned their questionnaire” (p. 256), plausible effect size among missing data (assuming a smaller effect in same direction), not enough to introduce clinically relevant bias (as the observed effects for patient‐reported outcomes were clearly beneficial) |
| Selective reporting (reporting bias) | Unclear risk | Healthcare satisfaction only incompletely reported |
| Other bias | High risk | Some baseline imbalances between the groups: fewer men in the CORE group (66.7% vs. 76.8%), more subjects with a history of compensation for back pain in the CORE group (42.6% vs. 28.6%) and more subjects with disabling back pain in the previous month in the CORE group (27% vs. 8.9%) |
Scholz 2015.
| Methods |
Design: quasi‐RCT, parallel, 2 arms Country: Switzerland Sample size: 8050 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: 2002 to 2006 Method of recruitment: cases covered by the Swiss National Accident Insurance Fund (which includes occupational and non‐occupational accident insurance, and insurance for the unemployed) and registered within 12 months of the accident where eligible for randomisation Follow‐up: 12, 24, 36, 48, 60, 72 months |
|
| Participants |
Health problem: severe accidents, occupational and non‐occupational Age in years: mean 40.21 Female in %: 18 Intervention group: 4039 participants (unweighted: 3863) Control group: 4013 participants (unweighted: 4187) Inclusion criteria: medical complexity, difficulties with return to work, risk of permanent disability Exclusion criteria: no coverage by the Swiss compulsory accident insurance, cases registered more than 12 months after accident, patients with occupational diseases Duration and type of sick leave: no information about duration of sick leave, at least 4 weeks seemed plausible; full‐ and part‐time sick leave Type of sick leave compensation: Swiss National Accident Insurance Fund (public insurance) |
|
| Interventions |
Intervention: intensive case management Components of intervention: highly structured approach with defined steps:
Team: independent physician, insurance physician, outpatient care provider, inpatient care provider, physiotherapist, ergotherapist, other care provider Involvement of the employer: yes Providers of intervention: case manager, “specially trained” Theoretical basis: not reported Duration: as long as considered appropriate, average 21.9 months (median 18 months) Control: standard case management:
|
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement):
|
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random procedure based on custom software |
| Allocation concealment (selection bias) | Low risk | Concealed (author information) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind (author information) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | Low risk | No indications of other sources of bias |
Stapelfeldt 2011.
| Methods |
Design: RCT, parallel, 2 arms with 2 subgroups Subgroups: 1) those with influence on the planning of their own work and no perceived risk of losing job and/or being a work injury claimant, 2) those without influence on the planning of their own work or feeling at risk of losing job and not a work injury claimant Country: Denmark Sample size: 120 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: August 2007 to July 2008 Method of recruitment: referred by their general practitioner, recruited at the Spine Center Follow‐up: 12 months |
|
| Participants |
Health problem: low back pain Age in years: mean 40.7 (SD 10.0) Female in %: 58 Intervention group: 60 participants Control group: 60 participants Inclusion criteria: absent from work for 3‐16 weeks, aged 16‐60 years, ability to read and speak Danish Exclusion criteria: unemployed, continuing or progressive symptoms indicating plans for surgery, surgery in the spine within the past 12 months, diagnosis of specific back disease (e.g. tumour), diagnosis of primary psychiatric disease, pregnancy, known substance abuse Duration and type of sick leave: range 3‐16 weeks; full‐ and part‐time sick leave Type of sick leave compensation: municipalities, financed by taxpayers (public insurance) |
|
| Interventions |
Intervention: multidisciplinary intervention (same as Jensen 2012) Components of intervention: brief intervention like control group; case management containing:
Team: specialist of social medicine, a rheumatologist, a physiotherapist, a social worker and an occupational therapist Involvement of the employer: yes Providers of intervention: 3 case managers; experience and training not reported Theoretical basis: Canadian multidisciplinary work rehabilitation programme (i.e. the Sherbrooke model, Loisel 2002) Duration: median 18 weeks Control: municipality case management and brief intervention:
Same control group interventions as Jensen 2012 and Myhre 2014 (without municipality case management) |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement): none |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated block‐randomisation |
| Allocation concealment (selection bias) | Low risk | Allocation was carried out by a secretary |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not possible, only the first clinical examination was carried out double blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Author information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete data for return‐to‐work outcomes |
| Selective reporting (reporting bias) | Low risk | Study protocol published; all outcomes reported |
| Other bias | Low risk | No indications of other sources of bias |
Van der Feltz‐Cornelis 2010.
| Methods |
Design: RCT, parallel, 2 arms Country: Netherlands Sample size: 60 in 24 clusters Unit of allocation: cluster Unit of analysis: individuals Date of recruitment: not reported, duration 3 years Method of recruitment: recruitment of occupational physicians and consultant psychiatrists in cooperation with ArboNed and Arbounie (2 companies providing company medical care; together they cover almost half of the working population in the Netherlands); recruitment of patients who visited an occupational physician within the past 6 months, selected from the medical files, invitation by letter Follow‐up: 3, 6 months |
|
| Participants |
Health problem: anxiety, depression, somatoform disorder Age in years: mean 42, range 24‐59 Female in %: 58 Intervention group: 29 participants (12 occupational physicians) Control group: 31 participants (12 occupational physicians) Inclusion criteria: absent from work > 6 weeks, a positive screen on either the Patient Health Questionnaire or the Whitely Index, no plan to return to work within another 6 weeks Exclusion criteria: suicidal, addicted to drugs or alcohol, psychotic, suffering from dementia, insufficient knowledge of the Dutch language, involved in a legislative procedure for unemployment compensation or on sick leave > 52 weeks Duration and type of sick leave: mean 144 days, range 1‐46 (conflicting information to inclusion criteria); full sick leave Type of sick leave compensation: government |
|
| Interventions |
Intervention: psychiatric consultation model Components of intervention:
Team: occupational physician, consulting psychiatrist, and in some cases the general practitioner Involvement of the employer: no Providers of intervention: 12 occupational physicians, training in diagnosis and treatment of mental disorders, consulted by 2 psychiatrists trained in improvement of work functioning Theoretical basis: Van der Feltz‐Cornelis 1996 Duration: until return to work Control: usual practice; care from occupational physicians and mental healthcare professionals |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | Baseline characteristics of the occupational physicians not reported (unit of randomisation) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Consecutive envelopes, the sequence was concealed until interventions were assigned by an independent blinded research assistant |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 18% losses to follow‐up for return‐to‐work outcomes, 27% losses to follow‐up for patient‐reported outcomes |
| Selective reporting (reporting bias) | High risk | Primary outcome was not pre‐specified: changed from “level of functioning” in the protocol to “time until RTW for at least 4 weeks”; reasons for change of primary outcomes were not discussed in final report; “level of functioning” not reported |
| Other bias | Low risk | No indications of other sources of bias; no indication of design effect: “As this is a cluster randomized trial, a correction for possible doctor variance (practices) was made. It was shown that it did not make any difference to the effect size which doctor gave the treatment. Apparently the effect of the intervention stands for itself.” (p. 383) |
Volker 2015.
| Methods |
Design: RCT, parallel, 2 arms Country: Netherlands Sample size: 220 in 12 clusters Unit of allocation: cluster Unit of analysis: individuals Date of recruitment: not reported Method of recruitment: screening of sick‐listed employees visiting their occupational physician, invitation by letter and telephone Follow‐up: 3, 6, 9, 12 months |
|
| Participants |
Health problem: common mental disorders Age in years: 44.46 (SD 10.04) Female in %: 59 Intervention group: 131 participants (32 occupational physicians) Control group: 89 participants (30 occupational physicians) Inclusion criteria: absent from work 4‐26 weeks, aged ≥18 years, screened positive (score ≥ 10) on either the scale of the Patient Health Questionnaire 9, Patient Health Questionnaire 15 or the Generalised Anxiety Disorder Questionnaire Exclusion criteria: insufficient knowledge of the Dutch language, pregnancy, involved in legal action against their employer, no Internet access Duration and type of sick leave: 4‐26 weeks, median 73 days (intervention group) and 70 days (control group); full‐ and part‐time sick leave Type of sick leave compensation: government |
|
| Interventions |
Intervention: e‐health module embedded in Collaborative Occupational health care (ECO) Components of intervention: the ECO intervention included
Team: occupational physician, general practitioner, mental health professional Additional resource: Return@Work eHealth module, email decision aid for the occupational physician Involvement of the employer: no Providers of intervention: 29 occupational physicians at Arbo Vitale (a large occupational health service) and one occupational physician at GGz Breburg (a large mental health service employer); half a day training on sickness guidance, the e‐health module and contact to other stakeholders Theoretical basis: none Duration: not reported (up to 16 sessions) Control: usual practice with contact to occupational physician, general practitioner and mental health professional, contact to other healthcare professionals not restricted (same utilisation as in intervention group) |
|
| Outcomes |
Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
|
|
| Notes | Authors provided additional data for secondary outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | “The research assistants and the participants were blind to the allocation when assessing the eligibility of sick‐listed employees for participating in this study.” (p. 3) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2% losses to follow‐up for return‐to‐work outcomes “For the self‐reported secondary outcomes, follow‐up questionnaires were returned by 158 of 220 participants (71.8%) at 3 months, 158 participants (71.8%) at 6 months, 137 participants (62.3%) at 9 months, and 131 participants (59.5%) at 12 months. At 9 months, the loss to follow‐up rate was significantly higher in the ECO condition (44.3%, 58/131) than in the CAU condition (28%, 25/89, P=.02). However, the participants who did return the questionnaire at 9 months did not differ significantly at baseline on sickness absence duration, depression, somatization, or anxiety symptoms from the participants who did not return the questionnaire. This was the case in the ECO condition and in the control condition. From these results, we concluded that there was no evidence for selective dropout in this study.” (p. 7) |
| Selective reporting (reporting bias) | Low risk | Study protocol published, all outcomes reported |
| Other bias | High risk | Low adherence to intervention: “in the intervention group, 31 participants (23.7%) never logged in at Return@Work. Of the 100 participants who did log in at Return@Work, 10.0% (10/100) did not finish the introduction (which included information about Return@Work and a questionnaire). The mean number of total log‐ins of the 90 participants who finished the introduction and actually started Return@Work was 7.8 (SD 6.1). Furthermore, 40% (36/90) of the participants minimally completed half of the modules of Return@Work.” (p. 11) no indication of a cluster effect: “The results, however, showed that there was no evidence of a clustering effect at the level of occupational physician regions (P = 0.92).” (p. 9) |
IQR: interquartile range; SD: standard deviation; SF‐12/36: 12/36‐item Short Form Health Survey.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abásolo 2005 | Not a commissioned programme, not an individually tailored programme |
| Abásolo 2007 | Not a commissioned programme, not an individually tailored programme |
| Alaranta 1986 | Not a commissioned programme, not an individually tailored programme |
| Alaranta 1994 | Not a commissioned programme, not an individually tailored programme |
| Andersen 2015 | Sick leave was not inclusion criteria |
| Anema 2007 | Sick leave less than 4 weeks |
| Arnetz 2003 | Sick leave duration unclear |
| Bakker 2007 | Not a commissioned programme, not an individually tailored programme |
| Berg 2011 | Sick leave less than 4 weeks |
| Bergström 2012 | Not an individually tailored programme |
| Bethge 2010 | Sick leave was not an inclusion criterion |
| Bethge 2011 | Not an individually tailored programme |
| Beutel 2005 | Not a commissioned programme, not an individually tailored programme |
| Bishop 2014 | Only vocational advice service |
| Bjorneklett 2013 | Not an individually tailored programme, less than 80% on sick leave |
| Blonk 2006 | Not an individually tailored programme, duration of sick leave unclear |
| Bohman 2011 | Prevention programme |
| Bonde 2005 | Sick leave less than 4 weeks |
| Bouwsma 2014 | Sick leave less than 4 weeks |
| Braathen 2007 | Not an individually tailored programme |
| Brendbekken 2016 | Not coordinated |
| Brouwers 2006 | Not an individually tailored programme |
| Buijs 2009 | Not an RCT |
| Busch 2011 | Not an individually tailored programme |
| Byrne 1993 | Aim was not return to work |
| Carlsson 2013 | Sick leave less than 4 weeks |
| Cheadle 1999 | Sick leave was not an inclusion criterion |
| Cheng 2007 | Not an individually tailored programme |
| De Boer 2004 | Prevention programme |
| De Boer 2007 | Prevention programme |
| De Buck 2005 | Prevention programme |
| Della‐Posta 2006 | Unemployed participants, not an individually tailored programme |
| Demir 2014 | Not an individually tailored programme, no return‐to‐work plan |
| Demoulin 2010 | Not an individually tailored programme |
| Dibbelt 2006 | Not a commissioned programme, not an individually tailored programme |
| Drews 2007 | Not an RCT |
| Du Bois 2012 | Advice only |
| Ektor‐Andersen 2008 | Sick leave less than 4 weeks |
| Ellis 2010 | Investigates self‐management |
| Elvsåshagen 2009 | Not an individually tailored programme |
| Eshoj 2001 | Less than 80% on sick leave |
| Fimland 2014 | Not an individually tailored programme |
| Frey 2008 | Unemployed participants |
| Fritz 2003 | Sick leave less than 4 weeks, no individually tailored programme |
| Gatchel 2003 | Not a controlled design |
| Greitemann 2006 | Not a commissioned programme, not an individually tailored programme |
| Haldorsen 1998 | No face‐to‐face contact, not an individually tailored programme |
| Haldorsen 2002 | No face‐to‐face contact, not an individually tailored programme |
| Hees 2013 | Not an individually tailored programme |
| Henchoz 2010 | Not an individually tailored programme |
| Hlobil 2007 | Not an individually tailored programme |
| Hoverstad 1994 | Prevention programme |
| Hubbard 2013 | No face‐to‐face contact, aim was to assess the feasibility of the programme |
| Huppe 2006 | Sick leave less than 4 weeks |
| Indahl 1998 | Not an individually tailored programme |
| Jensen 1995 | Sick leave duration unclear, no commissioned programme |
| Jensen 2013 | Not an RCT |
| Johansson 1998 | Sick leave less than 4 weeks |
| Jousset 2004 | Not an individually tailored programme |
| Karlson 2010 | Not an RCT |
| Karrholm 2006 | No prospective design |
| Karrholm 2008 | No prospective design |
| Kimbrough 2010 | Not an RCT |
| Kirby 2004 | Not an individually tailored programme |
| Kittel 2008 | Not a commissioned programme, not an individually tailored programme |
| Klaber Moffett 2004 | Not an individually tailored programme |
| Knapp 2015 | Not coordinated, no return‐to‐work plan |
| Knight 1994 | Prevention programme |
| Kornfeld 2000 | More than 20% unemployed participants |
| Kyes 1999 | Not an RCT |
| Lai 2007 | Not an RCT |
| Lamb 2007 | Aim was not return to work; participants not on sick leave |
| Lerner 2015 | Participants not on sick leave |
| Li 2006 | Aim was not return to work |
| Li‐Tsang 2008 | Control group received the intervention after 3 weeks |
| Linden 2014 | Not an individually tailored programme; participants not on sick leave |
| Lindström 1992 | Not a commissioned programme, not an individually tailored programme |
| Lindström 1995 | Not a commissioned programme, not an individually tailored programme |
| Linton 1989 | Sick leave less than 4 weeks |
| Loisel 2002 | Sick leave was 4 weeks during 1 year |
| Magnussen 2007 | Not an individually tailored programme |
| Mallon 2008 | Not an individually tailored programme |
| Marhold 2001 | Not an individually tailored programme |
| Marnetoft 1999 | No prospective design, more than 20% unemployed participants |
| Marnetoft 2000 | No prospective design, more than 20% unemployed participants |
| Martin 2013 | Quasi‐randomised trial, more than 20% unemployed participants |
| Matchar 2008 | Less than 80% on sick leave |
| McCluskey 2006 | Not an RCT |
| Meijer 2006 | Not an individually tailored programme |
| Mitchell 1994 | Not an individually tailored programme |
| Mortelmans 2006 | Not an RCT |
| Netterstrom 2013 | Not an individually tailored programme |
| Nilsson 1996 | More than 20% unemployed participants |
| Noordik 2013 | Sick leave less than 4 weeks |
| Norrefalk 2007 | Not an individually tailored programme |
| Ntsiea 2015 | Not an individually tailored programme |
| Nystuen 2006 | Not an individually tailored programme |
| Odeen 2013 | Prevention programme |
| Okpaku 1997 | Unemployed participants |
| Pedersen 2015 | Not an individually tailored programme, no return‐to‐work plan |
| Peters 1999 | Health promotion programme |
| Petit 2014 | Not all participants on sick leave |
| Ponzer 2000 | Sick leave less than 4 weeks |
| Poulsen 2014 | More than 20% unemployed participants |
| Raftery 2013 | Study protocol, no multidisciplinary intervention, not individually tailored |
| Rebergen 2007 | Sick leave less than 4 weeks |
| Rebergen 2009a | Sick leave less than 4 weeks |
| Rebergen 2009b | Sick leave less than 4 weeks |
| Roche 2007 | Not an individually tailored programme |
| Rolving 2014 | Study protocol, not an individually tailored programme |
| Ross 2006 | Not a commissioned programme, not an individually tailored programme |
| Rost 2004 | Not a commissioned programme; more than 20% unemployed participants |
| Rupp 1996 | More than 20% unemployed participants |
| Sacks 2008 | Unemployed participants |
| Salazar 2010 | Evaluation study |
| Scheer 1995 | Not an RCT |
| Schene 2007 | Not an individually tailored programme |
| Schultz 2008 | Not an RCT |
| Shete 2012 | Participants not on sick leave |
| Shu‐Kei 2007 | Not an individually tailored programme |
| Sjöström 2012 | Not an RCT |
| Skouen 2002 | No face‐to‐face contact, not an individually tailored programme |
| Skouen 2006 | No face‐to‐face contact, not an individually tailored programme |
| Stapelfeldt 2015 | Not an RCT |
| Steenstra 2003 | Sick leave less than 4 weeks |
| Steenstra 2006 | Sick leave less than 4 weeks |
| Steenstra 2007 | Sick leave less than 4 weeks |
| Steenstra 2009 | Sick leave less than 4 weeks |
| Streibelt 2008 | No controlled design |
| Streibelt 2014 | Multidisciplinary rehabilitation for both groups |
| Sundberg 2009 | Aim was not return to work |
| Svendsen 2014 | Not an individually tailored programme |
| Tamminga 2013 | Not a coordinated programme |
| Tamminga 2016 | Not an individually tailored programme |
| Thunnissen 2008 | Not a commissioned programme, more than 20% unemployed participants, sick leave duration unclear |
| Van Beurden 2012 | Not an RCT |
| Van Beurden 2015 | Sick leave less than 4 weeks |
| Van der Klink 2003 | Not an individually tailored programme, sick leave less than 4 weeks |
| Van Oostrom 2008 | Sick leave duration 2‐8 weeks |
| Van Oostrom 2010 | Sick leave duration 2‐8 weeks |
| Varekamp 2011 | Other outcomes |
| Vermeulen 2010 | Unemployed participants |
| Vermeulen 2011 | More than 20% unemployed participants |
| Vidor 2014 | Not an individually tailored programme |
| Vissers 2008 | Study was not conducted |
| Vlasveld 2013 | Not an individually tailored programme |
| Vonk Noordegraaf 2014 | Sick leave less than 4 weeks |
| Wang 2007 | No face‐to‐face contact, participants not on sick leave |
| Westman 2010 | Sick leave less than 4 weeks, less than 80% on sick leave |
| Whitehurst 2007 | Not a commissioned programme, not an individually tailored programme |
| Willert 2011 | Less than 80% on sick leave |
| Yassi 1995 | No prospective design, not an individually tailored programme |
| Zaman 2016 | Not an individually tailored programme, sick leave duration unclear |
| Zhang 1994 | Unemployed participants |
| Østerås 2009 | Not an individually tailored programme |
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
Norén 2015.
| Methods |
Design: RCT, parallel, 2 arms Country: Sweden Sample size: unknown Method of recruitment: patients at high risk for long‐term sick leave are identified within primary care Follow‐up: unknown |
| Participants | Patients at high risk for long‐term sick leave |
| Interventions |
Intervention: standard care and return‐to‐work coordination (individually adapted patient coaching and coordination
of rehabilitation activities, workplace efforts and health care) Control: standard care |
| Outcomes | Cumulative sickness absence Average sick‐claim rates |
| Notes | Some inclusion and exclusion criteria not verifiable, poster presentation, no full‐text available |
Differences between protocol and review
We planned to consider follow‐up times of short‐term (up to three months) and long‐term (closest to 12 months) as different. As it turned out, we found some studies with a follow‐up time extending considerably longer than 12 months and therefore changed our classification: we regarded a last follow‐up to 6 months as short‐term, between 6 and 12 months as long‐term and longer than 12 months as very long‐term.
Almost all studies (12 of 14) measured return to work using the outcome proportion who had ever returned to work. Study authors seem to regard this outcome as important, so we added it post hoc as a primary outcome.
To make it easier to understand the results, we calculated absolute effects using risk differences.
We did not pre‐specify the number of studies required for subgroup analyses, but we described the need to have a sufficient number of studies. We decided 10 studies per meta‐analysis was sufficient.
We classified the level of support for the control group as low, moderate or high to get a better understanding of the usual practice. However, we could not use this classification for subgroup analyses. We did not find enough studies to conduct subgroup analyses at all.
We intended to perform subgroup analyses according to the lengths of history of sick leave of participants and the intensity of return‐to‐work coordination programmes. We did not find enough information to conduct these analyses.
Contributions of authors
Drafting the manuscript: NV, SS, RK, SE, JB, WB.
Coordinating the manuscript: NV.
Developing search strategies: SS, RK.
Writing the manuscript: NV, SS, TZ, SE, WB, JB, RK.
Sources of support
Internal sources
-
EbIM, Evidence‐based Insurance Medicine, University of Basel Hospital, Basel, Switzerland.
Salary for Nicole Vogel, Wout de Boer and Regina Kunz
External sources
No sources of support supplied
Declarations of interest
Regina Kunz: EbIM, Evidence‐based Insurance Medicine at the University Hospital in Basel, is funded in part by donations from public insurance companies and a consortium of private insurance companies without restrictions on how the donations are used.
Nicole Vogel: None known.
Stefan Schandelmaier: None known.
Thomas Zumbrunn: employer received payment for the statistical analyses he conducted for the publication on which this review is based.
Shanil Ebrahim: None known.
Wout de Boer: None known.
Jason Busse: acts as a consultant to Prisma Health Canada, a private incorporated company funded by employers and insurers that consults on and manages long‐term disability claims.
New
References
References to studies included in this review
Bültmann 2009 {published data only}
- Bültmann U, Sherson D, Olsen J, Hansen CL, Lund T, Kilsgaard J. Coordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders. Journal of Occupational Rehabilitation 2009;19(1):81‐93. [DOI] [PubMed] [Google Scholar]
Davey 1994 {published data only}
- Davey CA. The Implementation and Evaluation of a Rehabilitation Co‐ordinator Service for Personal Injury Claimants. Edinburgh: University of Edinburgh, 1994. [Google Scholar]
Donceel 1999 {published data only}
- Donceel P, Du Bois M, Lahaye D. Return to work after surgery for lumbar disc herniation. A rehabilitation‐oriented approach in insurance medicine. Spine 1999;24(9):872‐6. [DOI] [PubMed] [Google Scholar]
Feuerstein 2003 {published and unpublished data}
- Feuerstein M, Huang GD, Ortiz JM, Shaw WS, Miller VI, Wood PM. Integrated case management for work‐related upper‐extremity disorders: impact of patient satisfaction on health and work status. Journal of Occupational and Environmental Medicine 2003;45(8):803‐12. [DOI] [PubMed] [Google Scholar]
Jensen 2012 {published data only}
- Jensen C, Jensen OK, Nielsen CV. Sustainability of return to work in sick‐listed employees with low‐back pain. Two‐year follow‐up in a randomized clinical trial comparing multidisciplinary and brief intervention. BMC Musculoskeletal Disorders 2012;13:156. [DOI: 10.1186/1471-2474-13-156] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lambeek 2010 {published data only}
- Lambeek LC, Mechelen W, Knol DL, Loisel P, Anema JR. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ 2010;340:c1035. [DOI: 10.1136/bmj.c1035] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lindh 1997 {published data only}
- Lindh M, Lurie M, Sann H. A randomized prospective study of vocational outcome in rehabilitation of patients with non‐specific musculoskeletal pain: A multidisciplinary approach to patients identified after 90 days of sick‐leave. Scandinavian Journal of Rehabilitation Medicine 1997;29(2):103‐12. [PubMed] [Google Scholar]
Myhre 2014 {published and unpublished data}
- Myhre K, Marchand GH, Leivseth G, Keller A, Bautz‐Holter E, Sandvik L, et al. The effect of work‐focused rehabilitation among patients with neck and back pain: a randomized controlled trial. Spine 2014;39(24):1999‐2006. [DOI] [PubMed] [Google Scholar]
Purdon 2006 {published data only}
- Purdon S, Stratford N, Taylor R, Natarajan L, Bell S, Wittenburg D. Impacts of the job retention and rehabilitation pilot. Leeds: Department for Work and Pensions. 2006. Research Report No 342.
Rossignol 2000 {published data only}
- Rossignol M, Abenhaim L, Seguin P, Neveu A, Collet JP, Ducruet T, et al. Coordination of primary health care for back pain. A randomized controlled trial. Spine 2000;25(2):251‐8; discussion 258‐9. [DOI] [PubMed] [Google Scholar]
Scholz 2015 {published data only}
- Scholz SM, Andermatt P, Tobler BL, Spinnler D. Work incapacity and treatment costs after severe accidents: standard vs. intensive case management in a 6‐year randomized controlled trial. Journal of Occupational Rehabilitation 2016;26(3):319‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stapelfeldt 2011 {published and unpublished data}
- Stapelfeldt CM, Christiansen DH, Jensen OK, Nielsen CV, Petersen KD, Jensen C. Subgroup analyses on return to work in sick‐listed employees with low back pain in a randomised trial comparing brief and multidisciplinary intervention. BMC Musculoskeletal Disorders 2011;12:112. [DOI: 10.1186/1471-2474-12-112] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van der Feltz‐Cornelis 2010 {published data only}
- Feltz‐Cornelis CM, Hoedeman R, Jong FJ, Meeuwissen JA, Drewes HW, Laan NC, et al. Faster return to work after psychiatric consultation for sicklisted employees with common mental disorders compared to care as usual. A randomized clinical trial. Journal of Neuropsychiatric Disease and Treatment 2010;6:375‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Volker 2015 {published and unpublished data}
- Volker D, Zijlstra‐Vlasveld MC, Anema JR, Beekman AT, Brouwers EP, Emons WH, et al. Effectiveness of a blended web‐based intervention on return to work for sick‐listed employees with common mental disorders: results of a cluster randomized controlled trial. Journal of Medical Internet Research 2015;17(5):e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Abásolo 2005 {published data only}
- Abásolo L, Blanco M, Bachiller J, Candelas G, Collado P, Lajas C, et al. A health system program to reduce work disability related to musculoskeletal disorders. Annals of Internal Medicine 2005;143(6):404‐14. [DOI] [PubMed] [Google Scholar]
Abásolo 2007 {published data only}
- Abásolo L, Carmona L, Hernandez‐Garcia C, Lajas C, Loza E, Blanco M, et al. Musculoskeletal work disability for clinicians: time course and effectiveness of a specialized intervention program by diagnosis. Arthritis & Rheumatology 2007;57(2):335‐42. [DOI] [PubMed] [Google Scholar]
Alaranta 1986 {published data only}
- Alaranta H, Hurme M, Einola S, Kallio V, Knuts LR, Törmä T. Rehabilitation after surgery for lumbar disc herniation: results of a randomized clinical trial. International Journal of Rehabilitation Research 1986;9(3):247‐57. [DOI] [PubMed] [Google Scholar]
Alaranta 1994 {published data only}
- Alaranta H, Rytokoski U, Rissanen A, Talo S, Ronnemaa T, Puukka P, et al. Intensive physical and psychosocial training program for patients with chronic low back pain. A controlled clinical trial. Spine 1994;16(12):1339‐49. [DOI] [PubMed] [Google Scholar]
Andersen 2015 {published data only}
Anema 2007 {published data only}
- Anema JR, Steenstra IA, Bongers PM, Vet HC, Knol DL, Loisel P, et al. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine 2007;32(3):291‐8. [DOI] [PubMed] [Google Scholar]
Arnetz 2003 {published data only}
- Arnetz BB, Sjogren B, Rydehn B, Meisel R. Early workplace intervention for employees with musculoskeletal‐related absenteeism: a prospective controlled intervention study. Journal of Occupational and Environmental Medicine 2003;45(5):499‐506. [DOI] [PubMed] [Google Scholar]
Bakker 2007 {published data only}
- Bakker IM, Terluin B, van‐Marwijk HWJ, Windt DAWM, Rijmen F, van MW, et al. A cluster‐randomised trial evaluating an intervention for patients with stress‐related mental disorders and sick leave in primary care. PLOS Clinical Trials 2007;2(6):e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berg 2011 {published data only}
- Berg SK, Svendsen JH, Zwisler AD, Pedersen BD, Preisler P, Siersbaek‐Hansen L, et al. COPE‐ICD: a randomised clinical trial studying the effects and meaning of a comprehensive rehabilitation programme for ICD recipients ‐design, intervention and population. BMC Cardiovascular Disorders 2011;11:33. [DOI: 10.1186/1471-2261-11-33] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergström 2012 {published data only}
- Bergström C, Jensen I, Hagberg J, Busch H, Bergstrom G. Effectiveness of different interventions using a psychosocial subgroup assignment in chronic neck and back pain patients: a 10‐year follow‐up. Disability and Rehabilitation 2012;34(2):110‐8. [DOI] [PubMed] [Google Scholar]
Bethge 2010 {published data only}
- Bethge M, Herbold D, Trowitzsch L, Jacobi C. Return to work following work‐related orthopaedic rehabilitation: a cluster randomized trial. Rehabilitation 2010;49(1):2‐12. [DOI] [PubMed] [Google Scholar]
Bethge 2011 {published data only}
- Bethge M, Herbold D, Trowitzsch L, Jacobi C. Work status and health‐related quality of life following multimodal work hardening: a cluster randomised trial. Journal of Back and Musculoskeletal Rehabilitation 2011;24(3):161‐72. [DOI] [PubMed] [Google Scholar]
Beutel 2005 {published data only}
- Beutel ME, Zwerenz R, Bleichner F, Vorndran A, Gustson D, Knickenberg RJ. Vocational training integrated into inpatient psychosomatic rehabilitation‐‐short and long‐term results from a controlled study. Disability and Rehabilitation 2005;27(15):891‐900. [DOI] [PubMed] [Google Scholar]
Bishop 2014 {published data only}
- Bishop A, Wynne‐Jones G, Lawton SA, Windt D, Main C, Sowden G, et al. Rationale, design and methods of the Study of Work and Pain (SWAP): a cluster randomised controlled trial testing the addition of a vocational advice service to best current primary care for patients with musculoskeletal pain (ISRCTN 52269669). BMC Musculoskeletal Disorders 2014;15:232. [DOI: 10.1186/1471-2474-15-232] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjorneklett 2013 {published data only}
- Bjorneklett HG, Rosenblad A, Lindemalm C, Ojutkangas ML, Letocha H, Strang P, et al. A randomized controlled trial of support group intervention after breast cancer treatment: results on sick leave, health care utilization and health economy. Acta Oncologica 2013;52(1):38‐47. [DOI] [PubMed] [Google Scholar]
Blonk 2006 {published data only}
- Blonk RWB, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: a comparison of two cognitive behavioural interventions in cases of work‐related psychological complaints among the self‐employed. Work and Stress 2006;20(2):129‐44. [Google Scholar]
Bohman 2011 {published data only}
- Bohman TM, Wallisch L, Christensen KB, Stoner B, Pittman A, Reed B, et al. Working Well ‐ the Texas demonstration to maintain indenpendence and employment: 18‐month outcomes. Journal of Vocational Rehabilitation 2011;34(2):97‐106. [Google Scholar]
Bonde 2005 {published data only}
- Bonde JP, Rasmussen MS, Hjøllund H, Svendsen SW, Kolstad HA, Jensen LD, et al. Occupational disorders and return to work: a randomized controlled study. Journal of Rehabilitation Medicine 2005;37(4):230‐5. [DOI] [PubMed] [Google Scholar]
Bouwsma 2014 {published data only}
- Bouwsma EV, Anema JR, Vonk Noordegraaf A, Knol DL, Bosmans JE, Schraffordt Koops SE, et al. The cost effectiveness of a tailored, web‐based care program to enhance postoperative recovery in gynecologic patients in comparison with usual care: protocol of a stepped wedge cluster randomized controlled trial. JMIR Research Protocols 2014;3(2):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Braathen 2007 {published data only}
- Braathen TN, Veiersted KB, Heggenes J. Improved work ability and return to work following vocational multidisciplinary rehabilitation of subjects on long‐term sick leave. Journal of Rehabilitation Medicine 2007;39(6):493‐9. [DOI] [PubMed] [Google Scholar]
Brendbekken 2016 {published data only}
- Brendbekken R, Eriksen HR, Grasdal A, Harris A, Hagen EM, Tangen T. Return to work in patients with chronic musculoskeletal pain: multidisciplinary intervention versus brief intervention: a randomized clinical trial. Journal of Occupational Rehabilitation 2016; Vol. 27, issue 1:82‐91. [DOI: 10.1007/s10926-016-9634-5] [DOI] [PMC free article] [PubMed]
Brouwers 2006 {published data only}
- Brouwers EP, Tiemens BG, Terluin B, Verhaak PF. Effectiveness of an intervention to reduce sickness absence in patients with emotional distress or minor mental disorders: a randomized controlled effectiveness trial. General Hospital Psychiatry 2006;28(3):223‐9. [DOI] [PubMed] [Google Scholar]
Buijs 2009 {published data only}
- Buijs PC, Lambeek LC, Koppenrade V, Hooftman WE, Anema JR. Can workers with chronic back pain shift from pain elimination to function restore at work? Qualitative evaluation of an innovative work related multidisciplinary programme. Journal of Back and Musculoskeletal Rehabilitation 2009;22(2):65‐73. [DOI] [PubMed] [Google Scholar]
Busch 2011 {published data only}
- Busch H, Bodin L, Bergstrom G, Jensen IB. Patterns of sickness absence a decade after pain‐related multidisciplinary rehabilitation. Pain 2011;152(8):1727‐33. [DOI] [PubMed] [Google Scholar]
Byrne 1993 {published data only}
- Byrne DM, Drury J, Mackay RC, Robinson S, Faranda C, MacAdam DB. Evaluation of the efficacy of an instructional programme in the self‐management of patients with asthma. Journal of Advanced Nursing 1993;18(4):637‐46. [DOI] [PubMed] [Google Scholar]
Carlsson 2013 {published data only}
- Carlsson L, Englund L, Hallqvist J, Wallman T. Early multidisciplinary assessment was associated with longer periods of sick leave: a randomized controlled trial in a primary health care centre. Scandinavian Journal of Primary Health Care 2013;31(3):141‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheadle 1999 {published data only}
- Cheadle A, Wickizer TM, Franklin G, Cain K, Joesch J, Kyes K, et al. Evaluation of the Washington State Workers' Compensation Managed Care Pilot Project II: medical and disability costs 639. Medical Care 1999;37(10):982‐93. [DOI] [PubMed] [Google Scholar]
Cheng 2007 {published data only}
- Cheng AS, Hung LK. Randomized controlled trial of workplace‐based rehabilitation for work‐related rotator cuff disorder. Journal of Occupational Rehabilitation 2007;17(3):487‐503. [DOI] [PubMed] [Google Scholar]
De Boer 2004 {published data only}
- Boer AG, Beek JC, Durinck J, Verbeek JH, Dijk FJ. An occupational health intervention programme for workers at risk for early retirement; a randomised controlled trial. Occupational and Environmental Medicine 2004;61(11):924‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Boer 2007 {published data only}
- Boer AG, Burdorf A, Duivenbooden C, Frings‐Dresen MH. The effect of individual counselling and education on work ability and disability pension: a prospective intervention study in the construction industry. Occupational and Environmental Medicine 2007;64(12):792‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Buck 2005 {published data only}
- Buck PD, le CS, Hout WB, Peeters AJ, Ronday HK, Westedt ML, et al. Randomized comparison of a multidisciplinary job‐retention vocational rehabilitation program with usual outpatient care in patients with chronic arthritis at risk for job loss. Arthritis & Rheumatology 2005;53(5):682‐90. [DOI] [PubMed] [Google Scholar]
Della‐Posta 2006 {published data only}
- Della‐Posta C, Drummond PD. Cognitive behavioural therapy increases re‐employment of job seeking worker's compensation clients. Journal of Occupational Rehabilitation 2006;16(2):223‐30. [DOI] [PubMed] [Google Scholar]
Demir 2014 {published data only}
- Demir S, Dulgeroglu D, Cakci A. Effects of dynamic lumbar stabilization exercises following lumbar microdiscectomy on pain, mobility and return to work. European Journal of Physical and Rehabilitation Medicine 2014;50(6):627‐40. [PubMed] [Google Scholar]
Demoulin 2010 {published data only}
- Demoulin C, Grosdent S, Capron L, Tomasella M, Somville PR, Crielaard JM, et al. Effectiveness of a semi‐intensive multidisciplinary outpatient rehabilitation program in chronic low back pain. Joint Bone Spine 2010;77(1):58‐63. [DOI] [PubMed] [Google Scholar]
Dibbelt 2006 {published data only}
- Dibbelt S, Greitemann B, Büschel C. Long‐term efficiency of orthopedic rehabilitation in chronic back pain‐‐the integrative orthopedic psychosomatic concept (IopKo) [Nachhaltigkeit orthopädischer Rehabilitation bei chronischen Rückenschmerzen ‐ Das Integrierte orthopädisch‐psychosomatische Behandlungskonzept (IopKo)]. Die Rehabilitation 2006;45(6):324‐35. [DOI] [PubMed] [Google Scholar]
Drews 2007 {published data only}
- Drews B, Nielsen CV, Rasmussen MS, Hjort J, Bonde JP. Improving motivation and goal setting for return to work in a population on sick leave: a controlled study. Scandinavian Journal of Public Health 2007;35(1):86‐94. [DOI] [PubMed] [Google Scholar]
Du Bois 2012 {published data only}
- Du Bois M, Donceel P. Guiding low back claimants to work: a randomized controlled trial. Spine 2012;37(17):1425‐31. [DOI] [PubMed] [Google Scholar]
Ektor‐Andersen 2008 {published data only}
- Ektor‐Andersen J, Ingvarsson E, Kullendorff M, Orbaek P. High cost‐benefit of early team‐based biomedical and cognitive‐behaviour intervention for long‐term pain‐related sickness absence. Journal of Rehabilitation Medicine 2008;40(1):1‐8. [DOI] [PubMed] [Google Scholar]
Ellis 2010 {published data only}
- Ellis N, Johnston V, Gargett S, MacKenzie A, Strong J, Battersby M, et al. Does self‐management for return to work increase the effectiveness of vocational rehabilitation for chronic compensated musculoskeletal disorders? Protocol for a randomised controlled trial. BMC Musculoskeletal Disorders 2010;11:115. [DOI: 10.1186/1471-2474-11-115] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elvsåshagen 2009 {published data only}
- Elvsåshagen H, Tellnes G, Abdelnoor MH. Does early intervention by a specialist in physical medicine and rehabilitation reduce the duration of long term sick leave among persons with musculoskeletal diseases? [Gir tidlig vurdering og behandling hos spesialist i fysikalskmedisin og rehabilitering reduksjon i langtidsfravær hossykmeldte med muskel‐ og skjelettsykdommer?]. Norsk Epidemiologi 2009;19(2):219‐22. [Google Scholar]
Eshoj 2001 {published data only}
- Eshoj P, Tarp U, Nielsen CV. Effect of early vocational intervention in a rheumatological outpatient clinic‐‐a randomized study. International Journal of Rehabilitation Research 2001;24(4):291‐7. [DOI] [PubMed] [Google Scholar]
Fimland 2014 {published data only}
- Fimland MS, Vasseljen O, Gismervik S, Rise MB, Halsteinli V, Jacobsen HB, et al. Occupational rehabilitation programs for musculoskeletal pain and common mental health disorders: study protocol of a randomized controlled trial. BMC Public Health 2014;14:368. [DOI: 10.1186/1471-2458-14-368] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frey 2008 {published data only}
- Frey WD, Azrin ST, Goldman HH, Kalasunas S, Salkever DS, Miller AL, et al. The mental health treatment study. Psychiatric Rehabilitation Journal 2008;31:306‐12. [DOI: 10.2975/31.4.2008.306.312] [DOI] [PubMed] [Google Scholar]
Fritz 2003 {published data only}
- Fritz JM, Delitto A, Erhard RE. Comparison of classification‐based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine 2003;28(13):1363‐71. [DOI] [PubMed] [Google Scholar]
Gatchel 2003 {published data only}
- Gatchel RJ, Polatin PB, Noe C, Gardea M, Pulliam C, Thompson J. Treatment‐ and cost‐effectiveness of early intervention for acute low‐back pain patients: a one‐year prospective study. Journal of Occupational Rehabilitation 2003;13(1):1‐9. [DOI] [PubMed] [Google Scholar]
Greitemann 2006 {published data only}
- Greitemann B, Dibbelt S, Büschel C. Multidisciplinary orthopedic rehabilitation program in patients with chronic back pain and need for changing job situation ‐‐ long‐term effects of a multimodal, multidisciplinary program with activation and job development [Integriertes Orthopädisch‐Psychosomatisches Konzept zur medizinischen Rehabilitation von Patienten mit chronischen Schmerzen des Bewegungsapparates ‐ Langfristige Effekte und Nachhaltigkeit eines multimodalen Programmes zur Aktivierung und beruflichen Umorientierung]. Zeitschrift für Orthopädie und ihre Grenzgebiete 2006;144(3):255‐66. [DOI] [PubMed] [Google Scholar]
Haldorsen 1998 {published data only}
- Haldorsen EM, Kronholm K, Skouen JS, Ursin H. Multimodal cognitive behavioral treatment of patients sicklisted for musculoskeletal pain: a randomized controlled study. Scandinavian Journal of Rheumatology 1998;27(1):16‐25. [DOI] [PubMed] [Google Scholar]
Haldorsen 2002 {published data only}
- Haldorsen EM, Grasdal AL, Skouen JS, Risa AE, Kronholm K, Ursin H. Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment, and extensive multidisciplinary treatment for long‐term sick‐listed employees with musculoskeletal pain. Pain 2002;95(1‐2):49‐63. [DOI] [PubMed] [Google Scholar]
Hees 2013 {published data only}
- Hees HL, Vries G, Koeter MW, Schene AH. Adjuvant occupational therapy improves long‐term depression recovery and return‐to‐work in good health in sick‐listed employees with major depression: results of a randomised controlled trial. Occupational and Environmental Medicine 2013;70(4):252‐60. [DOI] [PubMed] [Google Scholar]
Henchoz 2010 {published data only}
- Henchoz Y, Goumoens P, So AK, Paillex R. Functional multidisciplinary rehabilitation versus outpatient physiotherapy for non specific low back pain: randomized controlled trial. Swiss Medical Weekly 2010;140:w13133. [DOI: 10.4414/smw.2010.13133] [DOI] [PubMed] [Google Scholar]
Hlobil 2007 {published data only}
- Hlobil H, Uegaki K, Staal JB, de‐Bruyne MC, Smid T, van MW. Substantial sick‐leave costs savings due to a graded activity intervention for workers with non‐specific sub‐acute low back pain. European Spine Journal 2007;16(7):919‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoverstad 1994 {published data only}
- Hoverstad T, Koefoed G, Gudding IH. Intervention against sick‐leave in an industrial company. Tidsskrift for den Norske lægeforening 1994;114(11):1317‐20. [PubMed] [Google Scholar]
Hubbard 2013 {published data only}
- Hubbard G, Gray NM, Ayansina D, Evans JM, Kyle RG. Case management vocational rehabilitation for women with breast cancer after surgery: a feasibility study incorporating a pilot randomised controlled trial. Trials 2013;14:175. [DOI: 10.1186/1745-6215-14-175] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huppe 2006 {published data only}
- Huppe A, Glaser‐Moller N, Raspe H. Offering multidisciplinary medical rehabilitation to workers with work disability due to musculoskeletal disorders: results of randomized controlled trial [Trägerübergreifendes Projekt zur Früherkennung von Rehabilitationsbedarf bei Versicherten mit muskuloskelettalen Beschwerden durch Auswertung von Arbeitsunfähigkeitsdaten: Ergebnisse einer randomisierten, kontrollierten Evaluationsstudie]. Gesundheitswesen 2006;68(6):347‐56. [DOI] [PubMed] [Google Scholar]
Indahl 1998 {published data only}
- Indahl A, Haldorsen EH, Holm S, Reikeras O, Ursin H. Five‐year follow‐up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine 1998;23(23):2625‐30. [DOI] [PubMed] [Google Scholar]
Jensen 1995 {published data only}
- Jensen I, Nygren A, Gamberale F, Goldie I, Westerholm P, Jonsson E. The role of the psychologist in multidisciplinary treatments for chronic neck and shoulder pain: a controlled cost‐effectiveness study. Scandinavian Journal of Rehabilitation Medicine 1995;27(1):19‐26. [PubMed] [Google Scholar]
Jensen 2013 {published data only}
- Jensen AG. A two‐year follow‐up on a program theory of return to work intervention. Work (Reading, MA) 2013;44(2):165‐75. [DOI] [PubMed] [Google Scholar]
Johansson 1998 {published data only}
- Johansson C, Dahl J, Jannert M, Melin L, Andersson G. Effects of a cognitive‐behavioral pain‐management program. Behaviour Research and Therapy 1998;36(10):915‐30. [DOI] [PubMed] [Google Scholar]
Jousset 2004 {published data only}
- Jousset N, Fanello S, Bontoux L, Dubus V, Billabert C, Vielle B, et al. Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study. Spine 2004;29(5):487‐93. [DOI] [PubMed] [Google Scholar]
Karlson 2010 {published data only}
- Karlson B, Jonsson P, Palsson B, Abjornsson G, Malmberg B, Larsson B, et al. Return to work after a workplace‐oriented intervention for patients on sick‐leave for burnout‐‐a prospective controlled study. BMC Public Health 2010;10:301. [DOI: 10.1186/1471-2458-10-301] [DOI] [PMC free article] [PubMed] [Google Scholar]
Karrholm 2006 {published data only}
- Karrholm J, Ekholm K, Jakobsson B, Ekholm J, Bergroth A, Schuldt K. Effects on work resumption of a co‐operation project in vocational rehabilitation. Systematic, multi‐professional, client‐centred and solution‐oriented co‐operation. Disability and Rehabilitation 2006;28(7):457‐67. [DOI] [PubMed] [Google Scholar]
Karrholm 2008 {published data only}
- Karrholm J, Ekholm K, Ekholm J, Bergroth A, Ekholm KS. Systematic co‐operation between employer, occupational health service and social insurance office: a 6‐year follow‐up of vocational rehabilitation for people on sick‐leave, including economic benefits. Journal of Rehabilitation Medicine 2008;40(8):628‐36. [DOI] [PubMed] [Google Scholar]
Kimbrough 2010 {published data only}
- Kimbrough E, Lao L, Berman B, Pelletier KR, Talamonti WJ. An integrative medicine intervention in a Ford Motor Company assembly plant. Journal of Occupational and Environmental Medicine 2010;52(3):256‐7. [DOI] [PubMed] [Google Scholar]
Kirby 2004 {published data only}
- Kirby S, Riley R. Compulsory work‐focused interviews for inactive benefit claimants: an evaluation of the British ONE pilots. Labour Economics 2004;11(4):415‐29. [Google Scholar]
Kittel 2008 {published data only}
- Kittel J, Karoff M. Improvement of worklife participation through vocationally oriented cardiac rehabilitation? Findings of a randomized control group study. Rehabilitation 2008;47(1):14‐22. [DOI] [PubMed] [Google Scholar]
Klaber Moffett 2004 {published data only}
- Klaber Moffett JA, Carr J, Howarth E. High fear‐avoiders of physical activity benefit from an exercise program for patients with back pain. Spine 2004;29(11):1167‐72; discussion 73. [DOI] [PubMed] [Google Scholar]
Knapp 2015 {published data only}
Knight 1994 {published data only}
- Knight KK, Goetzel RZ, Fielding JE, Eisen M, Jackson GW, Kahr TY, et al. An evaluation of Duke university's LIVE FOR LIFE health promotion program on changes in worker absenteeism. Journal of Occupational and Environmental Medicine 1994;36(5):533‐6. [PubMed] [Google Scholar]
Kornfeld 2000 {published data only}
- Kornfeld R, Rupp K. The net effects of the Project NetWork return‐to‐work case management experiment on participant earnings, benefit receipt, and other outcomes. Social Security Bulletin 2000;63(1):12‐33. [PubMed] [Google Scholar]
Kyes 1999 {published data only}
- Kyes KB, Wickizer TM, Franklin G, Cain K, Cheadle A, Madden C, et al. Evaluation of the Washington State Workers' Compensation Managed Care Pilot Project I: medical outcomes and patient satisfaction. Medical Care 1999;37(10):972‐81. [DOI] [PubMed] [Google Scholar]
Lai 2007 {published data only}
- Lai HS, Chan CC. Implementing a pilot work injury management program in Hong Kong. Journal of Occupational Rehabilitation 2007;17(4):712‐26. [DOI] [PubMed] [Google Scholar]
Lamb 2007 {published data only}
- Lamb SE, Gates S, Underwood MR, Cooke MW, Ashby D, Szczepura A, et al. Managing Injuries of the Neck Trial (MINT): design of a randomised controlled trial of treatments for whiplash associated disorders. BMC Musculoskeletal Disorders 2007;8:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lerner 2015 {published data only}
- Lerner D, Adler DA, Rogers WH, Chang H, Greenhill A, Cymerman E, et al. A randomized clinical trial of a telephone depression intervention to reduce employee presenteeism and absenteeism. Psychiatric Services 2015;66(6):570‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2006 {published data only}
- Li EJ, Li‐Tsang CW, Lam CS, Hui KY, Chan CC. The effect of a "training on work readiness" program for workers with musculoskeletal injuries: a randomized control trial (RCT) study. Journal of Occupational Rehabilitation 2006;16(4):529‐41. [DOI] [PubMed] [Google Scholar]
Linden 2014 {published data only}
- Linden M, Muschalla B, Hansmeier T, Sandner G. Reduction of sickness absence by an occupational health care management program focusing on self‐efficacy and self‐management. Work (Reading, MA) 2014;47(4):485‐9. [DOI] [PubMed] [Google Scholar]
Lindström 1992 {published data only}
- Lindström I, Ohlund C, Eek C, Wallin L, Peterson LE, Fordyce WE, et al. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant‐conditioning behavioral approach. Physical Therapy 1992;72(4):279‐90. [DOI] [PubMed] [Google Scholar]
Lindström 1995 {published data only}
- Lindström I, Ohlund C, Nachemson A. Physical performance, pain, pain behavior and subjective disability in patients with subacute low back pain. Scandinavian Journal of Rehabilitation Medicine 1995;27(3):153‐60. [PubMed] [Google Scholar]
Linton 1989 {published data only}
- Linton SJ, Bradley LA, Jensen I, Spangfort E, Sundell L. The secondary prevention of low back pain: a controlled study with follow‐up. Pain 1989;36(2):197‐207. [DOI] [PubMed] [Google Scholar]
Li‐Tsang 2008 {published data only}
- Li‐Tsang CW, Li EJ, Lam CS, Hui KY, Chan CC. The effect of a job placement and support program for workers with musculoskeletal injuries: a randomized control trial (RCT) study. Journal of Occupational Rehabilitation 2008;18(3):299‐306. [DOI] [PubMed] [Google Scholar]
Loisel 2002 {published data only}
- Loisel P, Lemaire J, Poitras S, Durand MJ, Champagne F, Stock S, et al. Cost‐benefit and cost‐effectiveness analysis of a disability prevention model for back pain management: a six year follow up study. Occupational and Environmental Medicine 2002;59(12):807‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Magnussen 2007 {published data only}
- Magnussen L, Strand LI, Skouen JS, Eriksen HR. Motivating disability pensioners with back pain to return to work‐‐a randomized controlled trial. Journal of Rehabilitation Medicine 2007;39(1):81‐7. [DOI] [PubMed] [Google Scholar]
Mallon 2008 {published data only}
- Mallon TM, Cloeren M, Firestone LM, Burch HC. Contract case managers prove cost effective in federal workers' compensation programs. Military Medicine 2008;173(3):253‐8. [DOI] [PubMed] [Google Scholar]
Marhold 2001 {published data only}
- Marhold C, Linton SJ, Melin L. A cognitive‐behavioral return‐to‐work program: effects on pain patients with a history of long‐term versus short‐term sick leave. Pain 2001;91(1‐2):155‐63. [DOI] [PubMed] [Google Scholar]
Marnetoft 1999 {published data only}
- Marnetoft SU, Selander J, Bergroth A, Ekholm J. Vocational rehabilitation‐‐early versus delayed. The effect of early vocational rehabilitation compared to delayed vocational rehabilitation among employed and unemployed, long‐term sick‐listed people. International Journal of Rehabilitation Research 1999;22(3):161‐170. [PubMed] [Google Scholar]
Marnetoft 2000 {published data only}
- Marnetoft SU, Selander J. Multidisciplinary vocational rehabilitation focusing on work training and case management for unemployed sick‐listed people. International journal of rehabilitation research 2000;23(4):271‐9. [DOI] [PubMed] [Google Scholar]
Martin 2013 {published data only}
- Martin MH, Nielsen MB, Madsen IE, Petersen SM, Lange T, Rugulies R. Effectiveness of a coordinated and tailored return‐to‐work intervention for sickness absence beneficiaries with mental health problems. Journal of Occupational Rehabilitation 2013;23(4):621‐30. [DOI] [PubMed] [Google Scholar]
Matchar 2008 {published data only}
- Matchar DB, Harpole L, Samsa GP, Jurgelski A, Lipton RB, Silberstein SD, et al. The headache management trial: a randomized study of coordinated care. Headache 2008;48(9):1294‐310. [DOI] [PubMed] [Google Scholar]
McCluskey 2006 {published data only}
- McCluskey S, Burton AK, Main CJ. The implementation of occupational health guidelines principles for reducing sickness absence due to musculoskeletal disorders. Occupational Medicine 2006;56(4):237‐42. [DOI] [PubMed] [Google Scholar]
Meijer 2006 {published data only}
- Meijer EM, Sluiter JK, Heyma A, Sadiraj K, Frings‐Dresen MH. Cost‐effectiveness of multidisciplinary treatment in sick‐listed patients with upper extremity musculoskeletal disorders: a randomized, controlled trial with one‐year follow‐up. International Archives of Occupational and Environmental Health 2006;79(8):654‐64. [DOI] [PubMed] [Google Scholar]
Mitchell 1994 {published data only}
- Mitchell RI, Carmen GM. The functional restoration approach to the treatment of chronic pain in patients with soft tissue and back injuries. Spine 1994;19(6):633‐42. [DOI] [PubMed] [Google Scholar]
Mortelmans 2006 {published data only}
- Mortelmans AK, Donceel P, Lahaye D, Bulterys S. Does enhanced information exchange between social insurance physicians and occupational physicians improve patient work resumption? A controlled intervention study. Occupational and Environmental Medicine 2006;63(7):495‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Netterstrom 2013 {published data only}
- Netterstrom B, Friebel L, Ladegaard Y. Effects of a multidisciplinary stress treatment programme on patient return to work rate and symptom reduction: results from a randomised, wait‐list controlled trial. Psychotherapy and Psychosomatics 2013;82(3):177‐86. [DOI] [PubMed] [Google Scholar]
Nilsson 1996 {published data only}
- Nilsson I, Von BL. An attempt to work rehabilitation after long sick‐leave. Work (Reading, MA) 1996;7(3):183‐9. [DOI] [PubMed] [Google Scholar]
Noordik 2013 {published data only}
- Noordik E, Klink JJ, Geskus RB, Boer MR, Dijk FJ, Nieuwenhuijsen K. Effectiveness of an exposure‐based return‐to‐work program for workers on sick leave due to common mental disorders: a cluster‐randomized controlled trial. Scandinavian Journal of Work, Environment & Health 2013;39(2):144‐54. [DOI] [PubMed] [Google Scholar]
Norrefalk 2007 {published data only}
- Norrefalk JR, Linder J, Ekholm J, Borg K. A 6‐year follow‐up study of 122 patients attending a multiprofessional rehabilitation programme for persistent musculoskeletal‐related pain. International Journal of Rehabilitation Research 2007;30(1):9‐18. [DOI] [PubMed] [Google Scholar]
Ntsiea 2015 {published data only}
- Ntsiea MV, Aswegen H, Lord S, Olorunju S S. The effect of a workplace intervention programme on return to work after stroke: a randomised controlled trial. Clinical Rehabilitation 2015;29(7):663–73. [DOI] [PubMed] [Google Scholar]
Nystuen 2006 {published data only}
- Nystuen P, Hagen KB. Solution‐focused intervention for sick listed employees with psychological problems or muscle skeletal pain: a randomised controlled trial [ISRCTN39140363]. BMC Public Health 2006;6:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Odeen 2013 {published data only}
- Odeen M, Ihlebaek C, Indahl A, Wormgoor ME, Lie SA, Eriksen HR. Effect of peer‐based low back pain information and reassurance at the workplace on sick leave: a cluster randomized trial. Journal of Occupational Rehabilitation 2013;23(2):209‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Okpaku 1997 {published data only}
- Okpaku S, Anderson KH, Sibulkin AE, Butler JS, Bickman L. The effectiveness of a multidisciplinary case management. Psychiatric Rehabilitation Journal 1997;20(3):34‐41. [Google Scholar]
Pedersen 2015 {published data only}
- Pedersen P, Søgaard HJ, Labriola M, Nohr EA, Jensen C. Effectiveness of psychoeducation in reducing sickness absence and improving mental health in individuals at risk of having a mental disorder: a randomised controlled trial. BMC Public Health 2015;15:763. [DOI: 10.1186/s12889-015-2087-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peters 1999 {published data only}
- Peters K, Carlson J. Worksite stress management with high‐risk maintenance workers: a controlled study. International Journal of Stress Management 1999;6(1):21‐44. [Google Scholar]
Petit 2014 {published data only}
- Petit A, Roche‐Leboucher G, Bontoux L, Dubus V, Ronzi Y, Roquelaure, Y, et al. Effectiveness of three treatment strategies on occupational limitations and quality of life for patients with non‐specific chronic low back pain: is a multidisciplinary approach the key feature to success? Study protocol for a randomized controlled trial. BMC Musculoskeletal Disorders 2014;15(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ponzer 2000 {published data only}
- Ponzer S, Molin U, Johansson SE, Bergman B, Törnkvist H. Psychosocial support in rehabilitation after orthopedic injuries. The Journal of Trauma 2000;48(2):273‐9. [DOI] [PubMed] [Google Scholar]
Poulsen 2014 {published data only}
- Poulsen OM, Aust B, Bjorner JB, Rugulies R, Hansen JV, Tverborgvik T, et al. Effect of the Danish return‐to‐work program on long‐term sickness absence: results from a randomized controlled trial in three municipalities. Scandinavian Journal of Work, Environment & Health 2014;40(1):47‐56. [DOI] [PubMed] [Google Scholar]
Raftery 2013 {published data only}
- Raftery MN, Murphy AW, O'Shea E, Newell J, McGuire BE. Effectiveness of a cognitive behavioural therapy‐based rehabilitation programme (Progressive Goal Attainment Program) for patients who are work‐disabled due to back pain: study protocol for a multicentre randomised controlled trial. Trials 2013;14:290. [DOI: 10.1186/1745-6215-14-290] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rebergen 2007 {published data only}
- Rebergen DS, Bruinvels DJ, Beek AJ, van MW. Design of a randomized controlled trial on the effects of counseling of mental health problems by occupational physicians on return to work: the CO‐OP‐study. BMC Public Health 2007;7:183. [DOI: 10.1186/1471-2458-7-183] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rebergen 2009a {published data only}
- Rebergen DS, Bruinvels DJ, Bezemer PD, Beek AJ, van MW. Guideline‐based care of common mental disorders by occupational physicians (CO‐OP study): a randomized controlled trial. Journal of Occupational and Environmental Medicine/American College of Occupational and Environmental Medicine 2009;51(3):305‐12. [DOI] [PubMed] [Google Scholar]
Rebergen 2009b {published data only}
- Rebergen DS, Bruinvels DJ, van‐Tulder MW, Beek AJ, van MW. Cost‐effectiveness of guideline‐based care for workers with mental health problems. Journal of Occupational and Environmental Medicine 2009;51(3):313‐22. [DOI] [PubMed] [Google Scholar]
Roche 2007 {published data only}
- Roche G, Ponthieux A, Parot SE, Jousset N, Bontoux L, Dubus V, et al. Comparison of a functional restoration program with active individual physical therapy for patients with chronic low back pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2007;88(10):1229‐35. [DOI] [PubMed] [Google Scholar]
Rolving 2014 {published data only}
- Rolving N, Oestergaard LG, Willert MV, Christensen FB, Blumensaat F, Bunger C, Nielsen CV. Description and design considerations of a randomized clinical trial investigating the effect of a multidisciplinary cognitive‐behavioural intervention for patients undergoing lumbar spinal fusion surgery. BMC Musculoskeletal Disorders 2014;15(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ross 2006 {published data only}
- Ross RH, Callas PW, Sargent JQ, Amick BC, Rooney T. Incorporating injured employee outcomes into physical and occupational therapists' practice: a controlled trial of the Worker‐Based Outcomes Assessment System. Journal of Occupational Rehabilitation 2006;16(4):607‐29. [DOI] [PubMed] [Google Scholar]
Rost 2004 {published data only}
- Rost K, Smith JL, Dickinson M. The effect of improving primary care depression management on employee absenteeism and productivity. A randomized trial. Medical Care 2004;42(12):1202‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rupp 1996 {published data only}
- Rupp K, Wood M, Bell SH. Targeting people with severe disabilities for return‐to‐work: the Project NetWork demonstration experience. Journal of Vocational Rehabilitation 1996;7(1):63‐91. [Google Scholar]
Sacks 2008 {published data only}
- Sacks S, McKendrick K, Sacks JY, Banks S, Harle M. Enhanced outpatient treatment for co‐occurring disorders: main outcomes. Journal of Substance Abuse Treatment 2008;34(1):48‐60. [DOI] [PubMed] [Google Scholar]
Salazar 2010 {published data only}
- Salazar MK. Evaluation of a case management program. Summary and integration of findings. American Association of Occupational Health Nurses 2010;47(9):416‐23. [PubMed] [Google Scholar]
Scheer 1995 {published data only}
- Scheer SJ, Radack KL, O'Brien DR Jr. Randomized controlled trials in industrial low back pain relating to return to work. Part 1. Acute interventions. Archives of Physical Medicine and Rehabilitation 1995;76(10):966‐73. [DOI] [PubMed] [Google Scholar]
Schene 2007 {published data only}
- Schene AH, Koeter MW, Kikkert MJ, Swinkels JA, McCrone P. Adjuvant occupational therapy for work‐related major depression works: randomized trial including economic evaluation. Psychological Medicine 2007;37(3):351‐62. [DOI] [PubMed] [Google Scholar]
Schultz 2008 {published data only}
- Schultz IZ, Crook J, Berkowitz J, Milner R, Meloche GR, Lewis ML. A prospective study of the effectiveness of early intervention with high‐risk back‐injured workers‐‐a pilot study. Journal of Occupational Rehabilitation 2008;18(2):140‐51. [DOI] [PubMed] [Google Scholar]
Shete 2012 {published data only}
- Shete KM, Suryawanshi P, Gandhi N. Management of low back pain in computer users: a multidisciplinary approach. Journal of Craniovertebral Junction and Spine 2012;3(1):7‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shu‐Kei 2007 {published data only}
- Shu‐Kei C. Job coach model for occupational shoulder soft tissue injuries rehabilitation. Dissertation Abstracts International. Vol. 68, Hong Kong: Chinese University of Hong Kong, 2007. [Google Scholar]
Sjöström 2012 {published data only}
- Sjöström R, Asplund R, Alricsson M. Back to work: evaluation of a multidisciplinary rehabilitation program with emphasis on mental symptoms; A two‐year follow up. Journal of multidisciplinary healthcare 2012;5:145‐51. [DOI: 10.2147/JMDH.S32372] [DOI] [PMC free article] [PubMed] [Google Scholar]
Skouen 2002 {published data only}
- Skouen JS, Grasdal AL, Haldorsen EM, Ursin H. Relative cost‐effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long‐term sick leave: randomized controlled study. Spine 2002;27(9):901‐9. [DOI] [PubMed] [Google Scholar]
Skouen 2006 {published data only}
- Skouen JS, Grasdal A, Haldorsen EM. Return to work after comparing outpatient multidisciplinary treatment programs versus treatment in general practice for patients with chronic widespread pain. European Journal of Pain 2006;10(2):145‐52. [DOI] [PubMed] [Google Scholar]
Stapelfeldt 2015 {published data only}
- Stapelfeldt CM, Labriola M2 Jensen AB, Andersen NT, Momsen AM, Nielsen CV. Municipal return to work management in cancer survivors undergoing cancer treatment: a protocol on a controlled intervention study. BMC Public Health 2015;15:720. [DOI: 10.1186/s12889-015-2062-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Steenstra 2003 {published data only}
- Steenstra IA, Anema JR, Bongers PM, de‐Vet HC, van MW. Cost effectiveness of a multi‐stage return to work program for workers on sick leave due to low back pain, design of a population based controlled trial [ISRCTN60233560]. BMC Musculoskeletal Disorders 2003;4:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steenstra 2006 {published data only}
- Steenstra IA, Anema JR, van‐Tulder MW, Bongers PM, de‐Vet HC, van MW. Economic evaluation of a multi‐stage return to work program for workers on sick‐leave due to low back pain. Journal of Occupational Rehabilitation 2006;16(4):557‐78. [DOI] [PubMed] [Google Scholar]
Steenstra 2007 {published data only}
- Steenstra IA, Anema JR, Bongers PM, Vet‐de HC, Knol DL, Loisel P, et al. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine 2007;32(3):299‐300. [DOI] [PubMed] [Google Scholar]
Steenstra 2009 {published data only}
- Steenstra IA, Knol DL, Bongers PM, Anema JR, Mechelen W, Vet HC. What works best for whom? An exploratory, subgroup analysis in a randomized, controlled trial on the effectiveness of a workplace intervention in low back pain patients on return to work. Spine 2009;34(12):1243‐9. [DOI] [PubMed] [Google Scholar]
Streibelt 2008 {published data only}
- Streibelt M, Blume C, Thren K, Müller FW. Economic evaluation of medically occupationally orientated rehabilitation in patients with musculoskeletal disorders‐‐a cost‐benefit analysis from the perspective of the German statutory pension insurance scheme [Ökonomische Evaluation einer medizinisch‐beruflich orientierten Maßnahme bei Patienten mit muskuloskeletalen Erkrankungen ‐ Eine Kosten‐Nutzen‐Analyse aus Rentenversicherungsperspektive]. Die Rehabilitation 2008;47(3):150‐7. [DOI] [PubMed] [Google Scholar]
Streibelt 2014 {published data only}
- Streibelt M, Bethge M. Effects of intensified work‐related multidisciplinary rehabilitation on occupational participation: a randomized‐controlled trial in patients with chronic musculoskeletal disorders. International Journal of Rehabilitation Research 2014;37(1):61‐6. [DOI] [PubMed] [Google Scholar]
Sundberg 2009 {published data only}
- Sundberg T, Petzold M, Wändell P, Rydén A, Falkenberg T. Exploring integrative medicine for back and neck pain ‐ a pragmatic randomised clinical pilot trial. BMC Complementary and Alternative Medicine 2009;9:33. [DOI: 10.1186/1472-6882-9-33] [DOI] [PMC free article] [PubMed] [Google Scholar]
Svendsen 2014 {published data only}
- Svendsen SW, Christiansen DH, Haahr JP, Andrea LC, Frost P. Shoulder function and work disability after decompression surgery for subacromial impingement syndrome: a randomised controlled trial of physiotherapy exercises and occupational medical assistance. BMC Musculoskeletal Disorders 2014;15:215. [DOI: 10.1186/1471-2474-15-215] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tamminga 2013 {published data only}
- Tamminga SJ, Verbeek JH, Bos MM, Fons G, Kitzen JJ, Plaisier PW, et al. Effectiveness of a hospital‐based work support intervention for female cancer patients ‐ a multi‐centre randomised controlled trial. PLOS ONE 2013;8(5):e63271. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tamminga 2016 {published data only}
- Tamminga SJ, Hoving JL, Frings‐Dresen MH, Boer AG. Cancer@Work — a nurse‐led, stepped‐care,e‐health intervention to enhance the return to work of patients with cancer: study protocol for a randomized controlled trial. Trials 2016;17:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thunnissen 2008 {published data only}
- Thunnissen M, Duivenvoorden H, Busschbach J, Hakkaart‐van Roijen L, Tilburg W, Verheul R, et al. A randomized clinical trial on the effectiveness of a reintegration training program versus booster sessions after short‐term inpatient psychotherapy. Journal of Personality Disorders 2008;22(5):483‐95. [DOI] [PubMed] [Google Scholar]
Van Beurden 2012 {published data only}
- Beurden KM, Vermeulen SJ, Anema JR, Beek AJ. A participatory return‐to‐work program for temporary agency workers and unemployed workers sick‐listed due to musculoskeletal disorders: a process evaluation alongside a randomized controlled trial. Journal of Occupational Rehabilitation 2012;22(1):127‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Beurden 2015 {published data only}
- Beurden KM, Klink JJ, Brouwers EP, Joosen MC, Mathijssen JJ, Terluin B, et al. Effect of an intervention to enhance guideline adherence of occupational physicians on return‐to‐work self‐efficacy in workers sick‐listed with common mental disorders. BMC Public Health 2015;15:796. [DOI: 10.1186/s12889-015-2125-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van der Klink 2003 {published data only}
- Klink JJ, Blonk RW, Schene AH, van‐Dijk FJ. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occupational and Environmental Medicine 2003;60(6):429‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Oostrom 2008 {published data only}
- Oostrom SH, Anema JR, Terluin B, Vet HC, Knol DL, van MW. Cost‐effectiveness of a workplace intervention for sick‐listed employees with common mental disorders: design of a randomized controlled trial. BMC Public Health 2008;8:12. [DOI: 10.1186/1471-2458-8-12] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Oostrom 2010 {published data only}
- Oostrom SH, Mechelen W, Terluin B, Vet HC, Knol DL, Anema JR. A workplace intervention for sick‐listed employees with distress: results of a randomised controlled trial. Occupational and Environmental Medicine 2010;67(9):596‐602. [DOI] [PubMed] [Google Scholar]
Varekamp 2011 {published data only}
- Varekamp I, Verbeek JH, Boer A, Dijk FJ. Effect of job maintenance training program for employees with chronic disease ‐ a randomized controlled trial on self‐efficacy, job satisfaction, and fatigue. Scandinavian Journal of Work, Environment & Health 2011;37(4):288‐97. [DOI] [PubMed] [Google Scholar]
Vermeulen 2010 {published data only}
- Vermeulen SJ, Anema JR, Schellart AJ, van MW, Beek AJ. Cost‐effectiveness of a participatory return‐to‐work intervention for temporary agency workers and unemployed workers sick‐listed due to musculoskeletal disorders: design of a randomised controlled trial [Protocol]. BMC Musculoskeletal Disorders 2010;11:60. [DOI: 10.1186/1471-2474-11-60] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vermeulen 2011 {published data only}
- Vermeulen SJ, Anema JR, Schellart AJ, Knol DL, Mechelen W, Beek AJ. A participatory return‐to‐work intervention for temporary agency workers and unemployed workers sick‐listed due to musculoskeletal disorders: results of a randomized controlled trial. Journal of Occupational Rehabilitation 2011;21(3):313‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vidor 2014 {published data only}
- Vidor C, Leroyer A, Christophe V, Seillier M, Foncel J, Maele J, et al. Decrease social inequalities return‐to‐work: development and design of a randomised controlled trial among women with breast cancer. BMC Cancer 2014;14:267. [DOI: 10.1186/1471-2407-14-267] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vissers 2008 {published data only}
- ISRCTN31632033. The efficacy and predicting variables of a multidisciplinary disability resolution (MDR) program for CFS patients receiving long term disability benefits from income protection insurers. www.isrctn.com/ISRCTN31632033 (first received 4 April 2006).
Vlasveld 2013 {published data only}
- Vlasveld MC, Feltz‐Cornelis CM, Ader HJ, Anema JR, Hoedeman R, Mechelen W, et al. Collaborative care for sick‐listed workers with major depressive disorder: a randomised controlled trial from the Netherlands Depression Initiative aimed at return to work and depressive symptoms. Occupational and Environmental Medicine 2013;70(4):223‐30. [DOI] [PubMed] [Google Scholar]
Vonk Noordegraaf 2014 {published data only}
- Vonk Noordegraaf A, Anema JR, Mechelen W, Knol DL, Baal WM, Kesteren PJ, et al. A personalised eHealth programme reduces the duration until return to work after gynaecological surgery: results of a multicentre randomised trial. BJOG: An International Journal of Obstetrics and Gynaecology 2014;121(9):1127‐35; discussion 36. [DOI] [PubMed] [Google Scholar]
Wang 2007 {published data only}
- Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA 2007;298(12):1401‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Westman 2010 {published data only}
- Westman A, Linton SJ, Ohrvik J, Wahlén P, Theorell T, Leppert J. Controlled 3‐year follow‐up of a multidisciplinary pain rehabilitation program in primary health care. Disability and Rehabilitation 2010;32(4):307‐16. [DOI] [PubMed] [Google Scholar]
Whitehurst 2007 {published data only}
- Whitehurst DG, Lewis M, Yao GL, Bryan S, Raftery JP, Mullis R, et al. A brief pain management program compared with physical therapy for low back pain: results from an economic analysis alongside a randomized clinical trial. Arthritis & Rheumatology 2007;57(3):466‐73. [DOI] [PubMed] [Google Scholar]
Willert 2011 {published data only}
- Willert MV, Thulstrup AM, Bonde JP. Effects of a stress management intervention on absenteeism and return to work‐results from a randomized wait‐list controlled trial. Scandinavian Journal of Work, Environment & Health 2011;37(3):186‐95. [DOI] [PubMed] [Google Scholar]
Yassi 1995 {published data only}
- Yassi A, Tate R, Cooper JE, Snow C, Vallentyne S, Khokhar JB. Early intervention for back‐injured nurses at a large Canadian tertiary care hospital: an evaluation of the effectiveness and cost benefits of a two‐year pilot project. Occupational Medicine 1995;45(4):209‐14. [DOI] [PubMed] [Google Scholar]
Zaman 2016 {published data only}
- Zaman AG, Tytgat KM, Klinkenbijl JH, Frings‐Dresen MH, Boer AG. Design of a multicentre randomized controlled trial to evaluate the effectiveness of a tailored clinical support intervention to enhance return to work for gastrointestinal cancer patients. BMC Cancer 2016;16:303. [DOI: 10.1186/s12885-016-2334] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 1994 {published data only}
- Zhang M, Yan H, Phillips MR. Community‐based psychiatric rehabilitation in Shanghai. Facilities, services, outcome, and culture‐specific characteristics. The British Journal of Psychiatry. Supplement 1994;165(24):70‐9. [PubMed] [Google Scholar]
Østerås 2009 {published data only}
- Østerås N, Gulbrandsen P, Benth JS, Hofoss D, Brage S. Implementing structured functional assessments in general practice for persons with long‐term sick leave: a cluster randomised controlled trial. BMC Family Practice 2009;10:31. [DOI: 10.1186/1471-2296-10-31] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Norén 2015 {published data only}
- Norén AM, Bengtner J, Landström S, Sjöberg E. Rehabilitation coordination for return to work, as extended role for health professionals ‐ results from a randomized controlled trial. Health Professionals in Rheumatology Abstracts 2015;SAT0646‐HPR:1337. [Google Scholar]
Additional references
Akl 2012
- Akl EA, Sun X, Busse JW, Johnston BC, Briel M, Mulla S, et al. Specific instructions for estimating unclearly reported blinding status in randomized trials were reliable and valid. Journal of Clinical Epidemiology 2012;65(3):262‐7. [DOI] [PubMed] [Google Scholar]
Arends 2012
- Arends I, Bruinvels DJ, Rebergen DS, Nieuwenhuijsen K, Madan I, Neumeyer‐Gromen A, et al. Interventions to facilitate return to work in adults with adjustment disorders. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD006389.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berchtold 2006
- Berchtold P, Hess K. Evidenz für Managed Care: Europäische Literaturanalyse unter besonderer Berücksichtigung der Schweiz: Wirkung von Versorgungssteuerung auf Qualität und Kosteneffektivität. Vol. Arbeitsdokument des Obsan 16, Neuchâtel: Schweizerisches Gesundheitsobservatorium, 2006. [Google Scholar]
Campbell 2001
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391‐9. [DOI] [PubMed] [Google Scholar]
Canadian Human Rights Commission 2007
- Canadian Human Rights Commission. A Guide for Managing the Return to Work. Minister of Public Works and Government Services 2007. www.chrc‐ccdp.ca/eng/content/guide‐managing‐return‐work (accessed 10 October 2014).
Chamberlain 1991
- Chamberlain R, Rapp CA. A decade of case management: a methodological review of outcome research. Community Mental Health Journal 1991;27(3):171‐88. [DOI] [PubMed] [Google Scholar]
Clayton 2011
- Clayton S, Bambra C, Gosling R, Povall S, Misso K, Whitehead M. Assembling the evidence jigsaw: insights from a systematic review of UK studies of individual‐focused return to work initiatives for disabled and long‐term ill people. BMC Public Health 2011;11:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Craig 2013
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. International Journal of Nursing Studies 2013;50(5):587‐92. [DOI] [PubMed] [Google Scholar]
Department for Work and Pensions 2013
- Department for Work and Pensions. Working for a healthier tomorrow: work and health in Britain. July 2013. Available from www.gov.uk/government/publications/working‐for‐a‐healthier‐tomorrow‐work‐and‐health‐in‐britain.
Henderson 2005
- Henderson M, Glozier N, Holland Elliott K. Long term sickness absence. BMJ 2005;330(7495):802‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hoefsmit 2012
- Hoefsmit N, Houkes I, Nijhuis FJ. Intervention characteristics that facilitate return to work after sickness absence: a systematic literature review. Journal of Occupational Rehabilitation 2012;22(4):462‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI: 10.1136/bmj.g1687] [DOI] [PubMed] [Google Scholar]
Hofmarcher 2007
- Hofmarcher MM, Oxley H, Rusticelli E. Improved health system performance through better care coordination. December 2007. OECD Health Working Papers, No. 30, OECD Publishing, Paris. Available from www.oecd‐ilibrary.org/social‐issues‐migration‐health/improved‐health‐system‐performance‐through‐better‐care‐coordination_246446201766.
IWH 2007
- Institute for Work & Health. Seven 'principles' for successful return to work. www.iwh.on.ca/seven‐principles‐for‐rtw (accessed 8 December 2014).
Johnston 2010
- Johnston BC, Thorlund K, Schunemann HJ, Xie F, Murad MH, Montori VM, et al. Improving the interpretation of quality of life evidence in meta‐analyses: the application of minimal important difference units. Health and Quality of Life Outcomes 2010;8:116. [DOI: 10.1186/1477-7525-8-116] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuoppala 2008
- Kuoppala J, Lamminpää A. Rehabilitation and work ability: a systematic literature review. Journal of Rehabilitation Medicine 2008;40(10):796–804. [DOI] [PubMed] [Google Scholar]
Marchand 2015
- Marchand GH, Myhre K, Leivseth G, Sandvik L, Lau B, Bautz‐Holter E, et al. Change in pain, disability and influence of fear‐avoidance in a work‐focused intervention on neck and back pain: a randomized controlled trial. BMC Musculoskeletal Disorders 2015;16(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Journal of Clinical Epidemiology 2009;62(10):1006‐12. [DOI] [PubMed] [Google Scholar]
NICE 2009
- National Institute for Health and Care Excellence. Managing long‐term sickness and incapacity for work. NICE guidelines [PH19]. 2009 March. Available from www.nice.org.uk/guidance/PH19.
Nieuwenhuijsen 2014
- Nieuwenhuijsen K, Faber B, Verbeek JH, Neumeyer‐Gromen A, Hees HL, Verhoeven AC, et al. Interventions to improve return to work in depressed people. Cochrane Database of Systematic Reviews 2014, Issue 12. [DOI: 10.1002/14651858.CD006237.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
OECD 2003
- Organisation for Economic Cooperation and Development (OECD). Transforming disability into ability: policies to promote work and income security for disabled people. 2003 February. OECD Publishing, Paris. Available from www.oecd‐ilibrary.org/content/book/9789264158245‐en. [DOI: ]
OECD 2010
- Organisation for Economic Cooperation and Development (OECD). Sickness, Disability and Work: Breaking the Barriers: A Synthesis of Findings across OECD Countries. 2010 November. OECD Publishing, Paris. Available from www.oecd‐ilibrary.org/social‐issues‐migration‐health/sickness‐disability‐and‐work‐breaking‐the‐barriers_9789264088856‐en. [DOI: ]
OECD 2014 a
- Organisation for Economic Cooperation and Development (OECD). Economic Policy Reforms 2014: Going for Growth Interim Report. 2014 February. OECD Publishing, Paris. Available from www.oecd‐ilibrary.org/economics/economic‐policy‐reforms‐2014_growth‐2014‐en. [DOI: ]
OECD 2014 b
- Organisation for Economic Cooperation and Development (OECD). Making Mental Health Count. The Social and Economic Costs of Neglecting Mental Health Care. July 2014. OECD Health Policy Studies, OECD Publishing, Paris. Available from www.oecd.org/els/health‐systems/Focus‐on‐Health‐Making‐Mental‐Health‐Count.pdf.
Palmer 2012
- Palmer KT, Harris EC, Linaker C, Barker M, Lawrence W, Cooper C, et al. Effectiveness of community‐ and workplace‐based interventions to manage musculoskeletal‐related sickness absence and job loss: a systematic review. Rheumatology 2012;51(2):230‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
R 2015 [Computer program]
- R Core Team. R: A language and environment for statistical computing. Version 3.2.0. Vienna: R Foundation for Statistical Computing, 2015.
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Shaw 2001
- Shaw WS, Feuerstein M, Lincoln AE, Miller VI, Wood PM. Case management services for work related upper extremity disorders. Integrating workplace accommodation and problem solving. AAOHN Journal 2001;49(8):378‐89. [PubMed] [Google Scholar]
Thorlund 2011
- Thorlund K, Walter SD, Johnston BC, Furukawa TA, Guyatt GH. Pooling health‐related quality of life outcomes in meta‐analysis ‐ a tutorial and review of methods for enhancing interpretability. Research Synthesis Methods 2011;2(3):188‐203. [DOI] [PubMed] [Google Scholar]
Thornicroft 1991
- Thornicroft G. The concept of case management for long term mental illness. International Review of Psychiatry 1991;3(1):125‐32. [Google Scholar]
Van der Feltz‐Cornelis 1996
- Feltz‐Cornelis CM, Wijkel D, Verhaak PF, Collijn DH, Huyse FJ, Dyck R. Psychiatric consultation for somatizing patients in the family practice setting: a feasibility study. The International Journal of Psychiatry in Medicine 1996;26(2):223‐39. [DOI] [PubMed] [Google Scholar]
Van Vilsteren 2015
- Vilsteren M, Oostrom SH, Vet HCW, Franche RL, Boot CRL, Anema JR. Workplace interventions to prevent work disability in workers on sick leave. Cochrane Database of Systematic Reviews 2015, Issue 10. [DOI: 10.1002/14651858.CD006955.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Verbeek 2012
- Verbeek J, Ruotsalainen J, Hoving JL. Synthesizing study results in a systematic review. Scandinavian Journal of Work Environment & Health 2012;38(3):282‐90. [DOI] [PubMed] [Google Scholar]
Waddell 2006
- Waddell G, Burton AK. Is work good for your health & well‐being? Commissioned by the Department for Work and Pensions. Published by TSO (The Stationery Office). 2006. Available from www.gov.uk/government/uploads/system/uploads/attachment_data/file/214326/hwwb‐is‐work‐good‐for‐you.pdf.
References to other published versions of this review
Schandelmaier 2012
- Schandelmaier S, Ebrahim S, Burkhardt SC, Boer WE, Zumbrunn T, Guyatt GH, et al. Return to work coordination programmes for work disability: a meta‐analysis of randomised controlled trials. PLOS ONE 2012;7(11):e49760. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vogel 2015
- Vogel N, Schandelmaier S, Zumbrunn T, Ebrahim S, Boer WEL, Mousavi SM, et al. Return to work coordination programmes for improving return to work in workers on sick leave. Cochrane Database of Systematic Reviews 2015, Issue 3. [DOI: 10.1002/14651858.CD011618] [DOI] [PMC free article] [PubMed] [Google Scholar]


