Abstract
Background
Dementia is a collective name for different degenerative brain syndromes which, according to Alzheimer's Disease International, affects approximately 35.6 million people worldwide. The latest NICE guideline for dementia highlights the value of diverse treatment options for the different stages and symptoms of dementia including non‐pharmacological treatments. Relevant literature also argues for the value of interventions that acknowledge the complexity of the condition and address the person as a whole, including their physical, emotional, social and cognitive processes. At the same time, there is growing literature that highlights the capacity of the arts and embodied practices to address this complexity. Dance movement therapy is an embodied psychological intervention that can address complexity and thus, may be useful for people with dementia, but its effectiveness remains unclear.
Objectives
To assess the effects of dance movement therapy on behavioural, social, cognitive and emotional symptoms of people with dementia in comparison to no treatment, standard care or any other treatment. Also, to compare different forms of dance movement therapy (e.g. Laban‐based dance movement therapy, Chacian dance movement therapy or Authentic Movement).
Search methods
Searches took place up to March 2016 through ALOIS, Cochrane Dementia and Cognitive Improvement’s Specialized Register, which covers CENTRAL, a number of major healthcare databases and trial registers, and grey literature sources. We checked bibliographies of relevant studies and reviews, and contacted professional associations, educational programmes and experts from around the world.
Selection criteria
We considered randomised controlled trials (RCTs) in any language, including cross‐over design and cluster‐RCTs for inclusion. Studies considered had to include people with dementia, in any age group and in any setting, with interventions delivered by a dance movement therapy practitioner who (i) had received formal training (ii) was a dance movement therapist in training or (iii) was otherwise recognised as a dance movement therapist in the country in which the study was conducted.
Data collection and analysis
The two review authors independently reviewed studies on an abstract/title level and again after reading the full paper, and we independently evaluated methodological quality.
Main results
Of the 102 studies identified through electronic searches and personal communication, after de‐duplication we screened 80 at title/abstract level. We then reviewed 19 full papers, none of which met the inclusion criteria. Although three studies mentioned dance movement therapy as their intervention, they were excluded because they were not delivered by a qualified dance movement therapy practitioner. As a result, no studies were included in this review.
Authors' conclusions
Trials of high methodological quality, large sample sizes and clarity in the way the intervention is put together and delivered are needed to assess whether dance movement therapy is an effective intervention for dementia.
Plain language summary
Is dance movement therapy an effective intervention for dementia? A review of the evidence
Why is this review important?
Dementia currently affects approximately 35.6 million people worldwide and there is an expectation that, as people are growing older, there will be a substantial increase in the number of people affected. Dementia literature argues for the need to address the complexity of the symptoms and work with the person as a whole. It is possible that dance movement therapy, an embodied psychological intervention that uses movement and dance to express and explore emotions, may be useful for people with dementia. However, its effectiveness remains unclear. This is the first review of the effectiveness of dance movement therapy for dementia and will add to the evidence base regarding available non‐pharmacological interventions for dementia.
Who might be interested in this review?
It is expected that this review will be of interest to people affected by dementia and their carers as well as general practitioners, mental health professionals and psychological therapists.
What questions does this review aim to answer?
We asked the following questions. Is dance movement therapy more effective than no treatment or standard care? Is dance movement therapy more effective than any other treatment? How effective are different types of dance movement therapy?
Which studies were included in the review?
We searched databases for all published and unpublished randomised controlled studies of dance movement therapy for dementia up to March 2016, with participants of any age, gender or ethnicity. No study met the inclusion criteria.
What does the evidence from the review tell us?
There was no evidence for or against dance movement therapy as a useful intervention for dementia.
What should happen next?
Well‐designed studies with a large number of participants and well‐defined interventions are needed before we are clear on whether dance movement therapy is an effective intervention for dementia or not.
Background
Description of the condition
Dementia is a collective name for a number of different progressive degenerative brain syndromes that have effects on memory, thinking, behaviour, emotions and social functioning.
People living with dementia may have symptoms such as:
memory loss;
not being able to find the right words or understand what people are saying;
having difficulties in performing what used to be routine tasks;
mood swings and personality changes.
These symptoms limit their ability to communicate with others, may reduce social engagement and, in turn, can lead to apathy, or aggressiveness (Chen 2000), or depression (Lyketsos 2004). Facing cognitive, emotional and social challenges may increase the risk of challenging behaviours such as agitation, wandering or disinhibition related to dementia (Shaji 2009; Krishnamoorthy 2011).
According to Alzheimer's Disease International (ADI 2016), Alzheimer's disease is the most common of these syndromes, followed by vascular dementia, Lewy body dementia and frontotemporal dementia. The same source argues that the different types of dementia affect approximately 35.6 million people worldwide. Furthermore, it is estimated that, as a result of the population growing older, by 2030 there will be 65.7 million people suffering from dementia worldwide, and by 2050 there will be 115.4 million. Although recent studies suggest that populations that were born later in the 20th century have a lower risk of developing dementia than those born earlier (Matthews 2013), dementia remains a major issue for ageing populations with immediate and major impact upon families, services and societies as a whole.
Dementia literature highlights the value of treatment options that address the person as a whole, including their physical, emotional, social, cognitive and spiritual processes (Kitwood 1997). Similarly, the latest NICE guideline (NICE 2006) suggests that different stages and different symptoms of dementia might require different treatment strategies including non‐pharmacological interventions. Furthermore, there is a growing literature that argues for the value of the arts and embodied practices for this population, as being capable of bypassing impairments, connecting with people at a pre‐cognitive level and slowing down the progressive nature of the disease (Palo‐Bengtsson 2002; Verghese 2003; Vink 2003). Dance movement therapy (DMT) is one of these interventions that has been considered a useful intervention for people with dementia (Sandel 1987; Burns 2008; Hayes 2011).
Description of the intervention
DMT is a form of psychotherapy, one of the arts therapies and a treatment option for people with dementia as reported by Hill 1999, Violets‐Gibson 2002, Kowarzik 2004, and Hayes 2011.
DMT is also known as dance therapy, movement therapy, dance movement psychotherapy, movement psychotherapy, dance/movement therapy or dance‐movement therapy. As a profession, in the UK it is regulated by the Association for Dance Movement Psychotherapy UK (ADMP UK) and more recently also from the UK Council of Psychotherapists (UKCP). In Europe, the European Association for Dance Movement Therapy represents national professional Dance Movement Therapy associations, supporting professional development, while in the USA dance/movement therapists receive national certification from the Dance/Movement Therapy Certification Board, an independent affiliate of the American Dance Therapy Association. In the UK, the Association for Dance Movement Psychotherapy UK defines the discipline as follows:
“Dance Movement (Psycho) therapy is the psychotherapeutic use of movement and dance through which a person can engage creatively in a process to further their emotional, cognitive, physical and social integration. It is founded on the principle that movement reflects an individual’s patterns of thinking and feeling. Through acknowledging and supporting clients’ movements, the therapist encourages development and integration of new adaptive movement patterns together with the emotional experiences that accompany such changes” (ADMP UK 2016, p 1).
DMT is regarded as a useful and appropriate intervention for people with a range of conditions, diagnoses and presenting problems, and especially those for whom words can be difficult, those with a cognitive impairment, or who just find it difficult to express and explore their emotions through words (Karkou 2006). This type of therapy can, depending on the group of people who are accessing it, take place in a number of different settings including health services, schools, social services, voluntary organisations, prisons and care homes. Sessions can last from 30 to 90 minutes and often take place weekly at an agreed place and time. Interventions may last from a few weeks to several months, depending on client needs, and can be delivered as one‐to‐one, pair‐ or group‐therapy.
The practice of DMT in the 21st century stems in part from pioneering work that took place in the USA during the middle and latter part of the last century. However, pioneers in other countries also developed approaches that initially were independent of American influences (Payne 1992; Meekums 2008).
Karkou 2006 identifies three main models in the field.
Approaches that rely primarily upon dance/movement engagement and aim to explore specific movement themes and qualities, with or without active movement by the therapist. Examples of these are often, though not exclusively, informed by Rudolf Laban, an early proponent of therapeutic applications of dance movement (Laban 1975).
Approaches that prioritise the non‐verbal interaction between client(s) and therapist. A good example of this is the interactive model developed by the American DMT pioneer Marian Chace, as described by Chaiklin 1986, in which mirroring of movement is a key technique, that is, movement qualities used by the client are reflected back by the therapist and at times other group members.
Approaches that concentrate on movement improvisation associated with a focus on internal experience, in the presence of the therapist. An example of this type of approach is Authentic Movement, a practice developed by the American choreographer Mary Whitehouse (Whitehouse 1979). In this form of DMT, the therapist stays still and observes, using the self as an empathic witness, usually without music to influence the movement.
Meekums 2008 suggests that the feature that marks out contemporary DMT practice is the emphasis on it as a form of psychotherapy. For many therapists, theories relating to the psychodynamic school of thought are used to guide practice (Karkou 2006). For example, Authentic Movement is associated with Jungian psychology (Whitehouse 1979). For others, humanistic approaches are more relevant (Karkou 2006); the interactive model of Marian Chace is an example of an approach that is often closely connected with humanistic thinking. For others, developmental, behavioural or eclectic and integrative models are valued (Karkou 2006). For example, in her work with mothers and young children Meekums used a behavioural approach combined with attachment theory (Meekums 1991). More recently, Meekums suggested an integrative framework based on the symbolic power of the 'movement metaphor’, which transcends such theoretical divisions (Meekums 2002).
In all cases, the therapist is concerned with developing an embodied therapeutic relationship. Within this relationship, the therapist's body may be seen as holding projections from individual clients, or from the group as a whole. These projections may be worked through verbally, or non‐verbally, or both; more or less verbal reflection may take place, depending on the level of cognitive functioning of the participants.
How the intervention might work
DMT may have positive effects for people with dementias that include delaying cognitive deterioration, improving mood and increasing social interaction for a number of reasons such as:
the use of movement as exercise and as dance;
the use of music;
the therapeutic relationship; and
DMT‐specific features.
The use of movement
Since DMT uses the body and encourages movement amongst participants, it is expected that there will be some physiological changes associated with exercise. These are well documented in the generic literature on the physiology of exercise, and include positive effects on cognitive function (Colcombe 2003) as well as in the more recent Cochrane Review on exercise programmes for people with dementia (Forbes 2015).
The dance literature related to this review reveals that some dance forms, such as tango, may have the effect of over‐riding problems in the brain associated with balance and gait in Parkinson's Disease (Hackney 2007; Hackney 2010). Tango has many of the elements also found in a DMT session, including: " . . . frequent movement initiation and cessation, a range of speeds, rhythmic variation . . . " (Hackney 2010; p 682). There is also some research evidence to suggest that those individuals who dance regularly are less likely to develop dementia, demonstrating better memory performance than people who did not engage in any type of exercise in any significant way (Carcel 2012).
It is also possible that the use of dance within the intervention can connect with older people’s experiences of social dancing when younger and the pleasures that this brought, while encouraging people to engage in rhythmic movement and body action, both concepts and associated practices that are extensively used within the discipline (Chaiklin 1986).
The use of music
Although not essential, it is common for dance movement therapists to use music when working with people with dementias. Music of all styles and types can used, often with particular attention to the corresponding rhythm. Studies included in the Cochrane Review by Vink 2003 indicate that music therapy, a discipline closely aligned to DMT, may have some moderate positive effects in reducing behavioural symptoms associated with dementia, stimulating language skills and enhancing social/emotional functioning. However, in a similar way to other systematic reviews that have evaluated emerging treatment options, the authors of the review concluded that the methodological rigour and reporting of findings of these studies was too poor to draw useful conclusions about the value of this intervention. It is also impossible, from a review of music therapy that uses primarily music improvisation, to extrapolate the significance of recorded music as is commonly used within DMT practice.
The therapeutic relationship
As a form of psychotherapy, the therapeutic relationship can be seen as a key agent for change (Norcross 2011; Macaskie 2012). For example, in verbal psychotherapy, and with regard to intersubjective therapeutic relationships in particular, Macaskie 2012 concludes that the relationship is an embodied one, drawing on implicit relational knowing, implicit body memory and embodied participatory sense‐making. Within DMT, embodied relational knowing, body memory and embodied sense‐making are highly developed. Furthermore, empathy, a core component of the therapeutic relationship, is extensively utilised in DMT in the form of a sophisticated understanding and use of kinaesthetic empathy (Meekums 2012). The development of a therapeutic relationship is a key aspect of the work, and its embodied/relational nature in this context is of particular importance when cognition, communication, self‐confidence, self‐identity, self‐worth, orientation in space and time and more, are all under particular threat for the person with dementia. Also, it is accurate to say that, ‘maintaining relationships’ are at the heart of best practice in dementia care. The development of a therapeutic relationship is also one of the main differences between DMT and dance practice.
DMT‐specific features
While DMT participants are encouraged to engage in movement initiation and cessation, rhythmic variation and a range of speeds, they are encouraged to engage in movement that is primarily creative and takes place within an embodied therapeutic relationship, rather than learning steps to music. Additional benefits, therefore, might reasonably be expected beyond those associated with exercise or dance classes.
Karkou 2006 argues that therapeutic change may be related to some of the unique features of DMT specifically: embodiment, creativity and improvisation, movement‐based imagination, the use of symbolic movement and the use of movement as a metaphor. The embodied nature of DMT makes it potentially relevant to those clients for whom body image or body memory may be a particular issue requiring exploration and working through, for example for people who are overweight and have emotional eating patterns (Vaverniece 2012). In the case of dementia, engaging body memories may assist the goals of reminiscence therapy (Woods 2009). Metaphors inherent in symbolic movement offer a way to understand communication (Meekums 2002), and may be important for communication by people with dementia (Young 2011). Creativity and improvised movement work are also seen as enabling participants to develop new ways of being in the world in themselves and in interactions with others (Karkou 2006); this could potentially lead to a better emotional and social life. The value of activating imagination through movement was extensively discussed by Dosamanstes‐Alperson as early as 1981 (Dosamantes‐Alperson 1981), who offers specific guidance on how this can be facilitated and encouraged in a body‐based manner. Furthermore, Meekums 2002 and Karkou 2006 argue that symbols and metaphors can increase emotional distance from distressing memories and feelings, while they can allow for safe explorations that may change cognitions and feelings.
One of the central aspects of DMT for which there is an evidence base relates to the use of non‐verbal communication, and kinaesthetic empathy in particular (Brooks 1989; Berrol 2006; Meekums 2012), which is an important aspect of the therapeutic relationship discussed above. 'Movement mirroring', derived from the Chace approach to DMT mentioned earlier, is a technique extensively used by dance movement therapists as a way of engaging patients and achieving non‐verbal empathy. Within DMT literature, empathic engagement through mirroring is often seen as linked with the activation of mirror neurons in the brain (Rizzolatti 1996; Meekums 2002; Berrol 2006; Gazzola 2006), which fire as a kind of body memory when an individual observes another person engaged in either purposeful movement or emotional expression that is within the repertoire of the observer. However, the significance of mirror neurons within therapeutic kinaesthetic empathy is unclear; emotional engagement through a deliberate attempt to imagine oneself into another's experience appears to be an important additional requirement, used by dance movement therapists alongside their embodied engagement (Meekums 2012). Moreover, mirror neuron activity is associated with watching movements; different processes may be involved in actively mirroring movements, and so while some aspects of kinaesthetic empathy may involve mirror neuron activity, the processes involved in experiencing and conveying empathy are likely to be different.
Further investigation is needed to establish the role of both specific and non‐specific factors in therapeutic change associated with DMT for people with dementia.
Why it is important to do this review
DMT is widely practised around the world in both statutory and non‐statutory sectors with a range of client populations. The current review will add to other completed Cochrane Reviews of studies in DMT that have reviewed research evidence concerning the effects of DMT on schizophrenia, cancer care and depression (Bradt 2011; Ren 2013; Meekums 2015) as well as other systematic reviews that considered the effectiveness of DMT by authors such as Beard 2011, Guzmán‐García 2012, and Koch 2014.
Furthermore, there is a growing need to offer appropriate services to people with dementias who are faced with multiple issues beyond traditional pharmacological treatment. Given that medication focuses primarily on reducing cognitive deterioration, and that there is a growing number of people with dementias, the search for effective interventions that aim to address the person as a whole is particularly timely. Dance movement therapists do insist that they treat the person as a whole, tapping into cognitive areas of functioning but also addressing emotional, social, spiritual and physical aspects. The current review, therefore, will add to existing literature of non‐pharmacological treatment options for dementia, the closest to this review being the reviews on exercise (Forbes 2015), music therapy (Vink 2003) and art therapy (Deshmukh 2014).
Objectives
To assess the effects of dance movement therapy on behavioural, social, cognitive and emotional symptoms of people with dementia in comparison to no treatment, standard care or any other treatment. Also, to compare different forms of dance movement therapy (e.g. Laban‐based dance movement therapy, Chacian dance movement therapy or Authentic Movement).
Methods
Criteria for considering studies for this review
Types of studies
Our review sought to include published or unpublished randomised controlled trials (RCTs) in any language. We also considered cross‐over designs and cluster‐RCTs.
Types of participants
The review aimed to include studies of people who, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5; American Psychiatric Association 2013), International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD‐10; WHO 2010) or other comparable diagnostic criteria, were formally diagnosed as having any type of dementia of any type of severity. Women and men in all age groups and in all settings (e.g. statutory and voluntary organisations, inpatient or outpatient) were considered for inclusion in the review.
Types of interventions
Experimental interventions
We considered interventions delivered by a DMT practitioner who: had received formal training; was a dance movement therapist in training; or was otherwise recognised as a dance movement therapist in the country in which the study was conducted.
We aimed to include both group, individual and family/couple DMT with any number and duration of sessions.
Sessions could include active involvement in dance/movement in the presence of a dance movement therapist, or dance/movement interaction with a dance movement therapist with or without other group members, or both. Dance/movement could be improvisatory or structured. Sessions would have clear therapeutic intent and a clear description of the intervention would be reported or available on request. All approaches to DMT were considered.
We considered the presence or absence of verbal interaction and reflection as a factor to be examined in subgroup analysis. In all cases however, creative movement work would be the main means of working through cognitive, behavioural, emotional or social issues faced by the participants.
Comparators
No treatment or standard care
Other psychological therapies: for example, psychodynamic psychotherapy, humanistic, cognitive behavioural or integrative therapies
Pharmacological interventions: medications such as cholinesterase inhibitors (CgEIs) or memantine
Other interventions: for example, exercise, dance or music
Different types of DMT, as defined above
Types of outcome measures
Primary outcomes
Changes in behaviours often seen as challenging for carers, hereafter called 'challenging behaviours' for the sake of brevity (e.g. wandering, agitation, general restlessness), cognitive functioning, levels of depression and quality of life; examples of tools for assessing each outcome are listed below. We planned to accept all behavioural and psychological tools reported by the authors of the identified primary studies in the same way that Vink did for the Vink 2003 review of music therapy for dementia.
-
Challenging behaviours:
quantitative observational tools specifically designed for an individual study to measure frequency of occurrence of wandering, agitation and general restlessness;
standardised tests such as: Cohen‐Mansfield Agitation Inventory (Cohen‐Mansfield 1989).
-
Cognitive functioning:
the Mini‐Mental State Exam (MMSE) (Folstein 1975);
Alzheimer's Disease Assessment Scale (ADAS‐cog; Rosen 1984).
-
Depression:
Cornell Scale for Depression in Dementia (Alexopoulos 1988).
-
Quality of life:
Quality of Life‐Alzheimer's Disease (QOL‐AD, Logsdson 1999).
If other similar outcome measures were found in the included studies, we would consider them.
Secondary outcomes
Mobility and balance, fatigue, anxiety, social and occupational functioning, economic outcomes (cost‐effectiveness of treatment), treatment or research discontinuation/dropout (as measures of acceptability). We also aimed to consider adverse events, including falls and injuries associated with the intervention. Outcomes were to be included as used within the primary studies.
Search methods for identification of studies
Electronic searches
We searched ALOIS (www.medicine.ox.ac.uk/alois), Cochrane Dementia and Cognitive Improvement’s Specialized Register on 22 March 2016. The search terms used were: "dance*" or "authentic movement" or "movement therap*" or "movement psychot*" or "body psychot*".
ALOIS is maintained by Cochrane Dementia and Cognitive Improvement’s Information Specialist and contains dementia and cognitive improvement studies identified from:
monthly searches of a number of major healthcare databases: MEDLINE, Embase, CINAHL, PsycINFO and LILACS;
monthly searches of a number of trial registers: meta Register of Controlled Trials; Umin Japan Trial Register; WHO portal (which covers ClinicalTrials.gov; ISRCTN; Chinese Clinical trials Register; German Clinical trials register; Iranian Registry of Clinical trials and the Netherlands National Trials Register, plus others);
quarterly search of the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library;
monthly searches of a number of grey literature sources: ISI Web of Knowledge Conference Proceedings; Index to Theses; Australasian Digital Theses.
To view a list of all sources searched for ALOIS see About ALOIS on the ALOIS website.
The Information Specialist ran additional separate searches in many of the above sources to ensure that the most up‐to‐date results were retrieved. The search strategy used for the retrieval of reports of trials from MEDLINE (via the Ovid SP platform) can be seen in Appendix 1.
Searching other resources
We also took the following actions in order to identify published, unpublished and on‐going trials that may not appear in the electronic searches listed above.
We searched the bibliographies of relevant studies and reviews.
We contacted professional associations and educational programmes in DMT from around the world using a standard request form to inform us of Masters‐degree, PhD or independent work that is published or unpublished, completed or ongoing that might meet the inclusion criteria.
We contacted DMT researchers, theoreticians and practitioners who specialise in this area of work, whom we regard as experts in the field.
Data collection and analysis
Selection of studies
In the first instance, the two authors (VK and BM) screened titles and abstracts for inclusion of studies that met the inclusion criteria as discussed in Criteria for considering studies for this review and further specified in Data extraction and management. The two review authors acted independently, assessing different studies' eligibility using the first part of the proforma that can be found in Appendix 2.
We made a final decision only after seeking additional information, where required. There were no substantial disagreements between the two review authors.
Data extraction and management
A proforma specifically designed for this purpose was available to use to extract relevant data from any included studies (see Appendix 2).
Assessment of risk of bias in included studies
In order to identify any risk of bias, we aimed to use the Cochrane 'Risk of bias' tool as presented in Appendix 2 (Higgins 2011a). With the aid of this tool, we intended to make a judgement of 'low risk’, ’high risk’ or ’unclear risk’ of bias for each trial of the following areas:
-
selection bias:
random sequence generation
allocation concealment
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective reporting;
other sources of bias.
Measures of treatment effect
For studies that reported on changes in challenging behaviours (e.g. wandering, agitation, general restlessness), cognitive functioning, depression and quality of life, measured using rating scales presented as dichotomous data, we aimed to summarise data using risk ratios (RR). For continuous outcomes, such as scores from a scale, we aimed to use mean differences (MD).
When studies used different scales to measure the same outcome, we aimed to use the standardised mean difference, calculated using Review Manager 5 (RevMan 5) (RevMan 2014) to summarise outcomes across scales.
In all cases, we would regard endpoint data as a superior method over change scores. This is preferred since data can be skewed in favour of the treatment or the control group where randomisation is inadequate. It is possible that change scores could appear as different when in fact the two end points (control and treatment group) are similar (see, for example, Meekums 2015).
Unit of analysis issues
We were not expecting to find large scale studies, but depending on the type of studies available we aimed to make the following choices:
in the case of cross‐over trials, to use only the first active treatment period;
in studies with multiple arms, to include only the arm with DMT and the control;
in the case of two DMT arms with one single control group, we aimed to consult the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b, chapter 16.5.4).
If the study used cluster randomisation, depending on the data available, we aimed to analyse as per the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b, chapters 16.3.3 to 16.3.7).
Dealing with missing data
If there were missing data in terms of end‐of‐treatment scores, we aimed to either obtain the missing data or find out why data were missing through contacting trialists. We aimed to treat any data that remained unavailable as 'missing at random’ (Higgins 2011b, 16.1.2), and, if end‐of‐treatment scores were missing, to assume that participants had either dropped out of the intervention, died or become too ill to continue. We aimed to calculate the percentage dropout, and cautiously interpret this as a measure of acceptability.
If standard deviations (SD) were missing we aimed to consider the values of other reported measures such as P values, t values, confidence intervals and standard errors. If a sufficient number of studies became available, we aimed to impute a SD. However, in such cases we aimed to make a note of this and perform a sensitivity analysis, as imputed measures may bias towards lack of effect.
For continuous data that remained missing, we planned to report completers' data only. For binary data, we assumed that dropouts had 'no change' and planned to analyse using intention‐to‐treat analysis.
In general terms, we aimed to report all missing data in the risk of bias tables (Appendix 2).
Assessment of heterogeneity
Initially, we planned to examine sources of clinical heterogeneity; studies would only be pooled where the review authors judged that there was sufficient clinical homogeneity. In order to assist our judgement regarding potential sources of clinical heterogeneity, we aimed to summarise studies in terms of participants, settings, method of delivery (that is, group or individual, number of sessions), type of DMT, and reported outcomes.
We planned to assess heterogeneity in the results of the trials by inspection of graphical presentations and by the I2 (Higgins 2003) and Chi2 statistics (Deeks 2011).
We planned to pool studies with I2 statistic values of up to 80% heterogeneity, which may be an acceptable level of heterogeneity for psychological assessments. We then would perform a sensitivity analysis to establish the effects of including studies of lower quality (see Sensitivity analysis).
Assessment of reporting biases
While unlikely at this stage in DMT research, where more than 10 studies addressed the same outcome, we planned to use a funnel plot analysis to examine for publication bias.
Data synthesis
We planned to enter data from all trials included in the review into RevMan 5 software (RevMan 2014). Depending on the outcome of the test for homogeneity, we planned to assess whether we needed to accommodate for heterogeneity by using a random‐effects model to calculate differences between treatment and control groups and pooled estimates.
We planned to perform a meta‐analysis on extracted data if:
there was more than one study with an estimated treatment effect;
the included studies appeared to differ minimally in characteristics and could be investigated for heterogeneity through subgroup analyses;
studies used the same outcome measures;
each study had available data (Deeks 2011; Meekums 2015).
Finally, as it was expected that studies would use different time points for measurement, we planned an initial main analysis based on the final time point. Following this, we planned subgroup analyses if relevant as follows: short follow‐up (up to 14 weeks); moderate follow‐up (15 to 27 weeks) and long follow‐up (28 weeks and over). In cases where the type of intervention, the populations studied or the outcome measures used were very different from one study to another, we planned to include only narrative descriptions of the findings in the review.
Subgroup analysis and investigation of heterogeneity
If possible, we aimed to perform subgroup analyses as follows.
Mode of delivery including group or individual
Actively moving or not actively moving therapist
Presence or absence of verbal interaction
Length of treatment including number of sessions (fewer than 12 sessions versus 12 or more sessions)
Intensity of intervention, to include frequency (weekly or less frequent, bi‐weekly or more frequent) and duration of sessions (one hour or less, more than one hour)
Type of dementia
Severity of dementia (mild, moderate or severe as defined by the trialist)
Participant characteristics including gender (men, women or other, eg. transgender) and age (under 65 years old; 65 years old and over)
Setting (statutory and non‐statutory)
Sensitivity analysis
If relevant, we aimed to perform the following types of sensitivity analysis relating to:
different types of risk of bias, for example high versus low risk studies;
imputed measures versus available case analysis.
Results
Description of studies
There were no included studies.
Results of the search
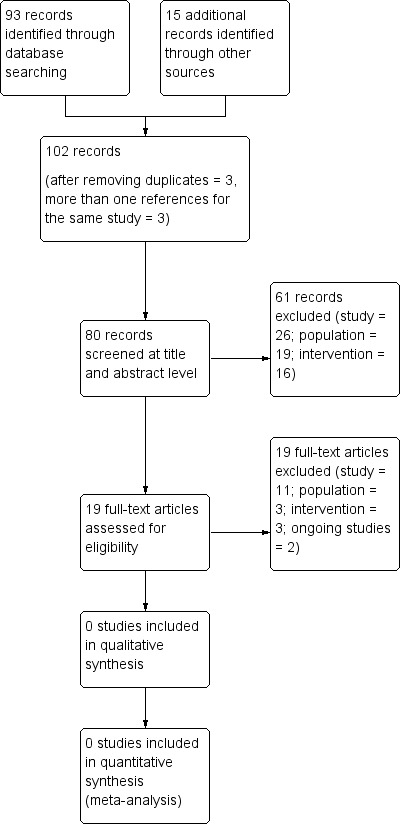
We found 93 studies from electronic searches and 15 from personal communication. After de‐duplication, we considered a total of 102 studies. The number of these studies was reduced to 80 after noise (ie, studies with no relevance to the topic of the review) was excluded (see PRISMA flow chart in Figure 1 (Moher 2009)). The remaining records were screened at a title and abstract level against the pre‐stated inclusion and exclusion criteria, relating to type of study, population and intervention. Nineteen full papers were then reviewed, from which 19 were excluded using the same criteria.
1.
Study flow diagram
Included studies
No study reviewed met all the inclusion criteria.
Excluded studies
At a title and abstract level, from the 80 records considered, we excluded 61 because of the type of study (n = 26), the population (n = 19), the intervention (n = 16),
From the remaining records (19 full papers), we excluded 19 on the basis of the type of study employed (n = 11), the population (n = 3) or the intervention used (n = 3), while two were excluded because they were ongoing studies (n = 2) (see Figure 1). We considered three studies more carefully for inclusion, namely the study by Hokkanen 2008 from Finland, Hwang 2010 from Korea and Hamill 2011 from the UK. We decided that, although these studies referred to the intervention either as DMT (Hokkanen 2008; Hwang 2010) or as having influences from DMT (Hamill 2011), they did not meet one of the main inclusion criteria, that is, the delivery of the intervention by a qualified dance movement therapist. Similarly, there was no suggestion in these studies that the facilitators were either in formal training in the discipline or were seen as DMT practitioners in the country in which the study was conducted. In the case of Hokkanen 2008, although one of the authors of this paper and a qualified dance movement therapist, was involved in the design and offered training to the facilitators of the intervention, qualified nurses provided the intervention. In the case of Hwang 2010, the intervention was designed in consultation with a college professor from a physical education background, an academic from nursing science, one social worker and two physical education trainers for the elderly. The presence of a qualified dance movement therapist was not confirmed in the text. Follow up communication with the authors of both of these studies did not generate any additional information, resulting in our decision to exclude these studies on the basis of intervention. Finally, the study by Hamill 2011 referred to the intervention as integrative influenced by dance therapy next to developmental psychology, body‐oriented theory and neuropsychology but it was provided by a senior clinical psychologist from the Psychotherapy for Older Adults service and a senior nurse from the Dementia Care Team. Although the paper stated that both of these facilitators had been trained in the intervention, had regular supervision and had also had experience in delivering and using psychotherapeutic and psychosocial interventions with older adults who were suffering from a broad range of cognitive impairment, we decided that, since they did not have specific DMT training, this study needed to be excluded.
All three studies reported some positive results for the intervention. Hokkanen 2008 for example, reported on findings from 29 participants suffering from diverse dementias such as Alzheimer’s disease, vascular dementia, and other undefined types of dementia. Statistically significant improvement was found in the DMT intervention (19 participants were involved in this) with regards to the Clock Drawing Test; the DMT group showed opposite trends to the 10 participants of the control group that attended routine nursing activities, that is, standard care. Slight improvement for the DMT group was also found on Mini‐Mental State Examination (MMSE; Folstein 1975) scores and the Picture Description Task.
The Korean study (Hwang 2010) reported results from 18 participants out of the initial 28 selected to participate; 10 of them attended the intervention and eight were part of the control group. It was implied that the control group followed standard care. No difference was reported for the Word List Memory Test between the DMT and the control group, while no results were reported with regards to the use of the Korean version of MMSE. The authors argued that statistically significant differences in cognitive functioning were not found because the control group attended a mass as part of their daily activities in the nursing home: they hypothesised that attending mass may have supported cognitive alertness. Similarly with the Hokkanen 2008 study, however Hwang 2010 focused on measuring cognitive performance, possibly due to a particular emphasis of the intervention on cognitive improvement. Both studies also failed to report on all relevant procedures followed, such as allocation concealment, blinding of the participants and personnel, blinding of outcome assessment, intention‐to‐treat analysis, and omitted reporting of certain findings, indicating high risk of bias.
Slightly different emphasis was apparent in the third study by Hamill 2011. Eleven people with moderate to severe dementia and seven family carers participated in this study. Those not attending in the group became an informal control group. Cognitive improvement was reported for two out of seven participants on the MMSE (Folstein 1975) measure, but unlike the other two studies, quality of life was measured (Quality of Life Scale in Alzheimer’s Disease ‐ QoL‐AD Logsdson 1999) with positive results reported for seven participants. No change was observed on the general health of the participating carers. The risk of bias in this pilot study was also high, particularly with regards to randomisation.
There were also two ongoing studies, Lyons 2015 and Ho Rainbow 2015, both of which were expected to be completed within around two years after the completion of this review. Information sourced for both of these studies suggests that they may meet the inclusion criteria outlined in the protocol of this review. The former (Lyons 2015) was described as a small pilot trial taking place in the UK, while the latter (Ho Rainbow 2015) was a larger study taking place in Hong Kong. We contacted the study authors who confirmed that, during the time of writing this report, they were in the process of recruiting participants.
Risk of bias in included studies
Not relevant
Allocation
Not relevant
Blinding
Not relevant.
Incomplete outcome data
Not relevant
Selective reporting
Not relevant
Other potential sources of bias
Not relevant
Effects of interventions
Not relevant
Discussion
Summary of main results
None of the studies reviewed met the inclusion criteria. Three studies (Hokkanen 2008, Hwang 2010 and Hamill 2011) were considered for inclusion. Closer inspection of these three studies, however, highlighted a failure to meet our criteria with regards to the intervention. Two ongoing studies were identified, a small trial undertaken in the UK by Lyons 2015 and a larger study taking place in Hong Kong by Ho Rainbow 2015. Both of these two studies are expected to be completed within a couple of years after this review was completed.
Overall completeness and applicability of evidence
Not relevant
Quality of the evidence
Not relevant
Potential biases in the review process
One possible area of bias is that, given the low number of published studies, some of the relevant trials may exist in the grey literature. The review authors made extensive efforts to locate all relevant studies, using their professional networks worldwide to search for studies in progress and unpublished studies, in addition to published work located through literature searches. Research in DMT has developed considerably both in methodological quality and quantity over the past two decades, and it is likely therefore that new studies will emerge of relevance to this review in coming years.
There is an assumption that DMT can be identified as a recognisable intervention across the world, playing down cultural variations and differences. It is likely however, that each country defines the field slightly differently in response to legal frameworks, history and training of practitioners, while it adapts to the work environments where this intervention is available and the populations it serves (Karkou 2006). Pioneers in the field also describe such variations as indicated in narrative accounts from different countries, for example, USA (Levy 1992) and UK (Meekums 2008). Our understanding of DMT does not escape cultural biases: we have defined the field through UK, USA and European lenses, but we are certain there are other, albeit equally valid, ways in which DMT can be defined which we have not taken into consideration.
Finally, while it was useful to include dance movement therapists on the research team in order to identify and discuss studies, researcher allegiance could have biased this study. We hope that our prior experience and training in Cochrane Reviews (the two authors have also published the Cochrane Review on DMT for Depression ‐ Meekums 2015) and our experience in academic research and in working in academic institutions have moderated for some inevitable biases.
Agreements and disagreements with other studies or reviews
The review links with Cochrane Reviews of dementia studies in related fields such as exercise (Forbes 2015) and music therapy (Vink 2003), as well as the recent protocol on art therapy (Deshmukh 2014). Although the review on exercise (Forbes 2015) concludes that there is promising evidence that exercise programmes can have a significant impact in improving ability to perform daily activities and possibly in improving cognition in people with dementia, these studies revealed no significant effect on challenging behaviours or depression. It is possible that these areas could be more affected by psychological interventions such as music therapy, art therapy and DMT. However, the Cochrane Review on music therapy (Vink 2003) reported that the methodological quality and the reporting of the included studies were too poor to draw any useful conclusions.
This review also relates to reviews on DMT with three key populations, namely people with schizophrenia, cancer and depression. Although all studies included are limited by methodological flaws and small sample sizes, they also suggest that there is evidence for the effectiveness of DMT in different outcome measures. For example, the Cochrane Review on DMT for schizophrenia by Ren 2013 included just one study of moderate quality that suggested that there might be a positive effect by DMT on negative symptoms of schizophrenia; these symptoms are closely connected to low mood. Bradt 2011 identified two studies with small sample sizes and judged them to be of very low methodological quality, in their Cochrane Review of DMT for people with cancer. Although they found no evidence for an impact of DMT on psychological or mood outcomes, one study, judged to be at a high risk of bias, claimed a positive effect on quality of life and fatigue. Finally, the Cochrane Review on depression (Meekums 2015) included a small subgroup analysis of adults that demonstrated an effect in favour of DMT. A large positive effect was observed for social functioning, but since this was from one study of low methodological quality the result was imprecise. In all cases the need for further studies with high quality and larger sample sizes is advocated before any conclusions can be drawn with clinical significance.
With regards to systematic reviews and meta‐analyses that can be found outside the Cochrane Database of Systematic Reviews, the meta‐analysis by Koch 2014 is an important one in that it covers a large number of DMT and dance studies. Their results suggest that DMT and dance have potential impact on increasing quality of life and decreasing symptoms such as depression and anxiety, with additional effects on subjective well‐being, positive mood, affect and body image. The authors highlight that the heterogeneity of data and the methodological limitations of most studies lead to inconclusive findings. The systematic reviews by Guzmán‐García 2012 and Beard 2011 look at DMT within the context of dancing and arts therapies for dementia respectively. The review by Guzmán‐García 2012 for example, includes four DMT studies of which only Hokkanen 2008 follows an RCT design. The authors conclude that the reviewed studies suggest a decrease in difficult behaviour and at the same time increased enjoyment and social interaction for both residents and staff. The methodological limitations of these studies are, once again, highlighted and explained as closely related to the challenges of this area of research. Finally, the Beard 2011 study includes, amongst others, nine studies in DMT with this population. However, unlike the scope of the current review, in the Beard 2011 review, studies with diverse designs are included, none of which has adopted an RCT design. Beard 2011 concludes that the emphasis of these studies is on the process of the work and in particular on encouraging quality of life, developing a sense of community and supporting interaction. It is therefore, "...far less biomedical..." (Beard 2011, p.11) than for music therapy studies for example. The non‐biomedical ethos of the field may explain why this first Cochrane Review on DMT for dementia has revealed a small number of outcome‐focused studies, a few with an RCT design and none that has met all the relevant criteria.
Authors' conclusions
Implications for practice.
Given the absence of included studies in this review it is not possible to draw any conclusions that can be useful for practice.
Implications for research.
It appears that although there is a growing research literature on the topic, the type of studies completed so far do not meet the pre‐specified criteria for inclusion in this review. Further research in this area is needed that pays attention to why participants, interventions, comparators and outcome measures are used. For example, a clear selection of participants following recognisable screening tools and processes are needed prior to careful randomisation taking place. Thorough descriptions of interventions is also important. For inclusion in future versions of this review, we suggest that the presence and delivery of the intervention by a qualified dance movement therapist, or one in formal training, is an important criterion, next to specific training in the particular intervention used for each study. Furthermore, future research studies need to consider carefully the research design and relevant comparisons to avoid methodological flaws apparent in the design and reporting of studies referred to in this review such as Hwang 2010 and Hokkanen 2008. Identification of relevant primary outcomes will also benefit future studies, avoiding a potentially misplaced attention to either improving or reducing deterioration of cognitive skills only. It is indeed possible that DMT may have an impact on cognition as explored in the Hokkanen 2008 and Hwang 2010 studies. However as a form of psychotherapy, it is more likely that this intervention will have a higher impact on emotional and social aspects as suggested in the qualitative findings from the Hamill 2011 study. Therefore, defining appropriate and relevant primary outcomes and identifying robust measures that address these outcomes should be an important consideration.
The above suggestions are made with an awareness that the area poses methodological challenges as discussed in the review of Guzmán‐García 2012 and further discussed in relevant literature about complex interventions (Campbell 2007; Craig 2008). In the case of DMT, the holistic and person‐centred nature of the intervention, often the context within which studies take place (e.g. care homes for example) and certainly the responses of participants who may find it difficult to either remember or articulate their experiences are all adding to the complexity of research in this area. As a result, guidance offered in the framework for developing and evaluating RCTs for complex interventions by the Medical Research Council 2000 (updated Medical Research Council 2008) or the Agency for Healthcare Research and Quality (Guise 2014) need to be considered carefully in future research in this area.
Acknowledgements
We wish to acknowledge the support by the Higher Education Institutions where the two authors have been based during the writing of this review, namely Edge Hill University and the University of Leeds. We also need to acknowledge the support of Cochrane Dementia and Cognitive Improvement and in particular the Information Specialist of this group for their search through the ALOIS Specialized Register.
Disclaimer
The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Appendices
Appendix 1. MEDLINE search strategy
1. danc*.ti,ab.
2. DTM.ti,ab.
3. "authentic movement*".ti,ab.
4. "movement therap*".ti,ab.
5. "movement psychot*".ti,ab.
6. "body psychot*".ti,ab.
7. "body psychot*".ti,ab.
8. or/1‐7
9. Dance Therapy/
10. 8 or 9
11. exp Dementia/
12. Delirium/
13. Wernicke Encephalopathy/
14. Delirium, Dementia, Amnestic, Cognitive Disorders/
15. dement*.mp.
16. alzheimer*.mp.
17. (lewy* adj2 bod*).mp.
18. deliri*.mp.
19. (chronic adj2 cerebrovascular).mp.
20. ("organic brain disease" or "organic brain syndrome").mp.
21. ("normal pressure hydrocephalus" and "shunt*").mp.
22. "benign senescent forgetfulness".mp.
23. (cerebr* adj2 deteriorat*).mp.
24. (cerebral* adj2 insufficient*).mp.
25. (pick* adj2 disease).mp.
26. (creutzfeldt or jcd or cjd).mp.
27. huntington*.mp.
28. binswanger*.mp.
29. korsako*.mp.
30. or/11‐29
31. 10 and 30
Appendix 2. Sample of data extraction form
Information/data extracted for all relevant studies
General information
'Data extractor'/author ID
Date of extraction
Study ID
Title, author(s), publication details of study
Source if unpublished
Language of publication
Eligibility criteria
Does the study meet the inclusion criteria, and how?
Study design (parallel, controlled trial, randomised controlled trial, systematic allocation)
Participants (diagnosis of dementia)
Interventions (type of dance movement therapy)
Outcomes (changes in cognitive, behavioural, emotional or social scales)
Inclusion? Exclusion? More information needed?
Data extraction for included studies
Study characteristics
Study setting (e.g. country, urban/rural, hospital/clinic/school/charity/community/prison etc)
Participant demographics (e.g. age, gender, socio‐economic status, co‐morbidity; also inclusion/exclusion criteria)
Intervention (interventions delivered by a DMT practitioner; group, individual and family/couple DMT; number and duration of sessions; active involvement in dance/movement with a dance movement therapist; improvisatory or structured dance/movement; therapeutic intent; description of intervention; DMT approach)
Outcome measures used in the study
-
Primary outcome measures that provide scores for changes in:
challenging behaviours
cognitive functioning
depression
quality of life
-
Secondary outcome measures that provide scores for:
mobility and balance
fatigue
anxiety
social and occupational functioning
economic outcomes
treatment or research discontinuation/dropout
adverse events including falls and injuries associated with the intervention
Study results
Source (table, graph, text)
Participants; number of events; percentages, chi2 statistics, risk ratios, for dichotomous outcomes; mean differences or standardised mean differences for continuous outcomes; missing participants
Queries regarding data or methods (to be referred to the study author for further information)
Additional notes
Record of details regarding correspondence with author(s) for additional information or clarification of queries
Ethics of stated conflict of interest
Details of other studies cited in the references
Duplicate publications
Translation required
Risk of bias assessment tool (Higgins 2011)
| Domain | Support for judgement | Review authors’ judgement |
| Selection bias | ||
| Random sequence generation | Describe the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups | Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence |
| Allocation concealment | Describe the method used to conceal the allocation sequence in sufficient detail to determine whether intervention allocations could have been foreseen in advance of, or during, enrolment | Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment |
| Performance bias | ||
| Blinding of participants and personnel: assessments should be made for each main outcome (or class of outcomes) | Describe all measures used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. Provide any information relating to whether the intended blinding was effective | Performance bias due to knowledge of the allocated interventions by participants and personnel during the study |
| Detection bias | ||
| Blinding of outcome assessment: assessments should be made for each main outcome (or class of outcomes) | Describe all measures used, if any, to blind outcome assessors from knowledge of which intervention a participant received. Provide any information relating to whether the intended blinding was effective | Detection bias due to knowledge of the allocated interventions by outcome assessors |
| Attrition bias | ||
| Incomplete outcome data: assessments should be made for each main outcome (or class of outcomes) | Describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. State whether attrition and exclusions were reported, the numbers in each intervention group (compared with total randomised participants), reasons for attrition/exclusions where reported, and any re‐inclusions in analyses performed by the review authors | Attrition bias due to amount, nature or handling of incomplete outcome data |
| Reporting bias | ||
| Selective reporting | State how the possibility of selective outcome reporting was examined by the review authors, and what was found | Reporting bias due to selective outcome reporting |
| Other bias | ||
| Other sources of bias | State any important concerns about bias not addressed in the other domains in the tool. If particular questions/entries were pre‐specified in the review’s protocol, responses should be provided for each question/entry |
Bias due to problems not covered elsewhere in the table |
Checklist into which the tool outlined above will be translated
1. Selection bias
a. Random sequence generation
Was the trial reported as randomised? YES/NO/UNCLEAR Was the method of randomisation appropriate? YES/NO/UNCLEAR YES: randomisation will be rated as appropriate if every participant had an equal chance to be selected for either intervention and if the investigator was unable to predict to which treatment the participant would be assigned. Examples of appropriate randomisation methods include use of: random number table; computer random‐number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing lots; minimisation NO: inappropriate methods include: use of date of birth; sequence generated by a rule e.g. date of admission; patient preference; clinician's judgement; availability of the intervention UNCLEAR: insufficient information provided on which to base judgement
b. Allocation concealment
Was allocation concealment adequate? YES/NO/UNCLEAR YES: allocation concealment will be rated as adequate when the following methods are used: central allocation (e.g. telephone, web‐ or pharmacy‐based randomisation); serially‐numbered, opaque, sealed envelopes; other descriptions with convincing concealment. NO: allocation concealment will be rated as inadequate when the following methods are used: open random allocation schedule, i.e. a list of random numbers; envelopes without safeguards, i.e. unsealed, non‐opaque or not sequentially‐numbered; alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure. UNCLEAR: authors did not report adequately on method of concealment.
2. Blinding of participants and personnel
Was participant and personnel blinding adequate? YES/NO/UNCLEAR YES: adequate blinding will involve blinding of participants and personnel to the allocated interventions during the study. NO: inadequate blinding is implied in studies in which blinding of participants and personnel has not taken place. Please note that for DMT studies, it is highly likely that it will not be possible to blind participants or those providing the DMT interventions. Therefore, it is likely that for this domain DMT studies will be assessed as having inadequate blinding and thus being at a high risk of bias. UNCLEAR: unclear blinding is implied when insufficient information is reported to determine who was blinded, or whether blinding occurred at all.
3. Blinding of outcome assessment
Was discussion of blinding of outcome assessment adequate? YES/NO/UNCLEAR YES: adequate blinding achieved when outcome assessors are unaware of the intervention allocated. NO: inadequate blinding means that outcome assessors are aware of the intervention allocated. UNCLEAR: a judgement of unclear will be used if a study does not address this point.
4. Incomplete outcome data
Were incomplete outcome data adequately considered? YES/NO/UNCLEAR YES: incomplete outcome data will have been adequately considered when: there are no missing outcome data; reasons for missing data are unlikely to be related to the true outcome; missing outcome data are balanced across comparison groups, with similar reasons; plausible effect size (difference in means or standardised difference in means) among missing outcomes is insufficient to have clinically relevant impact on observed effect size; missing data are imputed using appropriate methods. NO: incomplete outcome data will have been inadequately considered when: reasons for missing outcome data are likely to be related to the true outcome, with either imbalance of numbers or reasons for missing data across groups; plausible effect size among missing outcomes is sufficient to induce clinically relevant bias in observed effect size; ’as treated’ analysis performed with substantial departure of the intervention received from that assigned at randomisation; potentially inappropriate application of simple imputation. UNCLEAR: insufficient reporting of attrition or exclusions to permit judgement, e.g. number randomised not stated or no reasons provided for missing data; or the study did not address this outcome.
For continuous data, an intention‐to‐treat (ITT) analysis will be calculated if not presented by the authors of the study.
5. Selective reporting
Was the reporting bias acceptable? YES/NO/UNCLEAR YES: reporting bias will be assessed as acceptable if: the study protocol is available and all pre‐specified outcomes of interest in the review have been reported in the pre‐specified way; or the protocol is not available but it is clear that the published reports include all expected outcomes. NO: reporting bias will be assessed as unacceptable if: not all of the pre‐specified primary outcomes are reported; one or more of these is reported using measurements or analytic methods or subsets of data that were not pre‐specified; one or more of the primary outcomes were not pre‐specified (unless clearly justified, e.g. an unexpected adverse effect); one or more outcomes of interest is reported incompletely and so cannot be entered into meta‐analysis; failure to report results for a key outcome that would be expected from such a study (including adverse outcomes). UNCLEAR: insufficient information provided to make a judgement.
6. Other sources of bias
Were other sources of bias eliminated: YES/NO/UNCLEAR Examples of other risk of bias include: those related to study design; claimed to be fraudulent. Examples of unclear risk of bias include: insufficient rationale or evidence that an identified problem would introduce bias. The above criteria will be used to give each article an overall quality rating of A to C, as follows:
A: low risk of bias ‐ all criteria met. B: moderate risk of bias ‐ one or more of the criteria only partly met. C: high risk of bias ‐ one or more criteria not met.
Studies will not be excluded on the basis of a low quality score.
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abreu 2013 | Study: one single case study was presented |
| ACTRN12614000129684 | Intervention: not about dance therapy but about dance |
| Bräuninger 2014 | Study: survey of practitioners |
| Coaten 2001 | Study: opinion‐based paper |
| Coaten 2002 | Study: opinion‐based paper |
| Coaten 2013 | Study: opinion‐based paper |
| Hamill 2011 | Intervention: the intervention is called integrative, incorporating influences from developmental psychology, body‐oriented theory and neuropsychology next to dance therapy. However, the therapy was provided by a senior clinical psychologist from the Psychotherapy for Older Adults service and a senior nurse from the Dementia Care Team and not from a dance movement therapist. Both therapists had been trained in this intervention with regular supervision and had experience in delivering and using psychotherapeutic and psychosocial interventions with older adults suffering from a broad range of cognitive impairment. |
| Hill 2006 | Study: phenomenological study |
| Hokkanen 2003 | Study: pre‐post pilot study with 4 participants only |
| Hokkanen 2008 | Intervention: although it was suggested that a dance movement therapist offered supervision, qualified nurses offered the intervention |
| Hwang 2010 | Intervention: it was composed in consultation with a college professor from a physical education background, an academic from nursing science, one social worker and two physical education trainers for the elderly; no dance movement therapist was involved in the intervention |
| Ingram 2014 | Study: there was a control group but no randomisation is mentioned. Also there are not references to dementia |
| Newman‐Bluestein 2010 | Study: opinion‐based paper |
| Odell‐Miller (2006) | Population: participants with dementia were fewer than two and were not identified on the basis of dementia |
| Sandel 1995 | Study: not an RCT |
| Song 2012 | Population: the exclusion criteria included dementia or suspected dementia according to the DSM‐IV diagnostic criteria |
| Wilkinson 1998 | Study: no randomisation |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Ho Rainbow ongoing.
| Trial name or title | A 3‐arm RCT on the effects of dance movement intervention and exercises on elderly with early dementia |
| Methods | The participants will be assessed 4 times over the course of 12 months: baseline before randomisation, post intervention (3 months), 6 months from baseline and 12 months from baseline |
| Participants | 201 elderly Chinese individuals with very mild to mild dementia |
| Interventions | Dance movement intervention compared with mild physical exercise and a waiting list. The two intervention groups will receive a 1‐h intervention, twice a week, for 12 weeks |
| Outcomes | The primary outcomes will be compared between assessment points and between groups on neuropsychiatric symptoms, psychosocial well‐being and cognitive and daily functioning. Secondary outcomes will assess the changes in salivary cortisol levels and their relationships with the primary outcome measures |
| Starting date | 2015 |
| Contact information | tinho@nku.hk |
| Notes | We contacted the study authors at the time of writing this review and we were informed that the study was in the stage of recruiting participants |
Lyons ongoing.
| Trial name or title | The value of arts therapies in dementia: a mixed methods trial |
| Methods | Not identified |
| Participants | Thirty participants with very mild to mild dementia |
| Interventions | Dance movement psychotherapy, music therapy and waiting list |
| Outcomes | Quantitatively it will aim to discern what might be a meaningful outcome measure considering different stages of the disease. The possible outcome measures to be used will be CMAI, AD and MIDAS. Qualitative and arts‐based data will also be collected |
| Starting date | 2016/2017 |
| Contact information | lyonsst@edgehill.ac.uk |
| Notes | This is a PhD study that the two authors of this review are supervising. The first phase of the study, which involved a systematic review of the literature on dance movement psychotherapy and music therapy, has been completed |
RCT: randomised controlled trial
Differences between protocol and review
Minor edits on the text for clarity and updates on background literature.
Contributions of authors
Draft of protocol: VK and BM. Develop search strategy and undertake searches: VK and BM in consultation with the Cochrane Dementia and Cognitive Improvement Information Specialist. Data extraction and management: VK and BM. Assessment of quality: VK and BM. Analysis and synthesis: narrative VK and BM.
Sources of support
Internal sources
-
University of Leeds, UK and Edge Hill University, UK.
The two institutions offered support in the form of accessing learning resources
External sources
-
NIHR, UK.
This review was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Dementia and Cognitive Improvement. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
VK is a dance movement psychotherapist registered with the Association for Dance Movement Psychotherapy UK and an active researcher in the field with relevant research activities.
BM is a dance movement psychotherapist registered with the Association for Dance Movement Psychotherapy UK and an active researcher in the field with relevant research activities.
New
References
References to studies excluded from this review
Abreu 2013 {published data only}
- Abreu M, Hartley G. The effects of salsa dance on balance, gait, and fall risk in a sedentary patient with Alzheimer's dementia, multiple comorbidities, and recurrent falls. Journal of Geriatric Physical Therapy 2013;36(2):100‐8. [DOI] [PubMed] [Google Scholar]
ACTRN12614000129684 {published data only}
- We Think You Can Dance! A pilot randomised controlled trial for aged care residents with dementia. In aged care residents with dementia, does a dance program, compared to a music and socialisation program, improve or maintain cognition?. ICTRP/WHO Portal: http://apps.who.int/trialsearch/Trial.aspx?TrialID=ACTRN12614000129684 and on ANZCTR: http://www.anzctr.org.au/ACTRN12614000129684.aspx.
Bräuninger 2014 {published data only}
- Bräuninger I. Dance movement therapy with the elderly: an international internet‐based survey undertaken with practitioners. Body, Movement and Dance in Psychotherapy: An International Journal for Theory, Research and Practice 2014;9(3):138‐53. [DOI: 10.1080/17432979.2014.914977] [DOI] [Google Scholar]
Coaten 2001 {published data only}
- Coaten R. Exploring reminiscence through dance and movement. Journal of Dementia Care 2001;9(5):19‐22. [Google Scholar]
Coaten 2002 {published data only}
- Coaten R. Movement matters: revealing the hidden humanity within dementia through movement, dance and the imagination. Dementia 2002;1(3):386‐92. [Google Scholar]
Coaten 2013 {published data only}
- Coaten R, Newman‐Bluestein D. Embodiment and dementia ‐ dance movement psychotherapists respond. Dementia 2013;12(6):677‐81. [DOI] [PubMed] [Google Scholar]
Hamill 2011 {published data only}
- Hamill M, Smith L, Röhricht F. Dancing down memory lane: circle dancing as a psychotherapeutic intervention in dementia—a pilot study. Dementia 2011;1471(6):709‐24. [Google Scholar]
Hill 2006 {published data only}
- Hill H. Dance therapy as person‐centred cares. In SC Koch and I Braeuninger (Eds), Advances in Dance/Movement Therapy: Theoretical Perspectives and Empirical Findings. Berlin: Logos, 2006. [Google Scholar]
Hokkanen 2003 {published data only}
- Hokkanen L, Rantala L, Remes AM, Harkonen B, Viramo P, Winblad I. Dance/movement therapeutic methods in management of dementia. Journal of the American Geriatrics Society 2003;51(4):576‐7. [DOI] [PubMed] [Google Scholar]
Hokkanen 2008 {published data only}
- Hokkanen L, Rantala L, Remes AM, Harkonen B, Viramo P, Winblad I. Dance and movement therapeutic methods in management of dementia: a randomized, controlled study. Journal of the American Geriatrics Society 2008;56(4):771‐2. [DOI] [PubMed] [Google Scholar]
Hwang 2010 {published data only}
- Hwang HH, Choi YJ. The effects of the dance therapy program through rhythmic exercise on cognitive memory performance of the elderly with dementia. In: Procedings of the 21st Pan‐Asian Congress of Sports and Physical Education. Nanchang, China, 2010; Vol. 4:12‐17.
Ingram 2014 {published data only}
- Ingram T, Hackney ME. Dance your way to better health: Effects of tango dance on mild cognitive impairment in oldest old adults. Journal of general internal medicine. Conference: 37th Annual Meeting of the Society of General Internal Medicine, SGIM 2014 San Diego, CA United States. Conference Start: 20140423 Conference End: 20140426 2104;Conference Publication:S61‐S62. [Google Scholar]
Newman‐Bluestein 2010 {published data only}
- Newman‐Bluestein D, Hill H. Movement as the medium for connection, empathy, playfulness. Journal of Dementia Care 2010;18(5):24‐7. [Google Scholar]
Odell‐Miller (2006) {published data only}
- Odell‐Miller H, Hughes P, Westacott M. An investigation into the effectiveness of the arts therapies for adults with continuing mental health problems. Psychotherapy Research 2006;16(1):122‐39. [Google Scholar]
Sandel 1995 {published data only}
- Sandel S, Hollander AS. Dance/movement therapy with aging populations. In Levy F (Ed), Dance and Other Expressive Art Therapies. New York: Routledge, 1995:113‐43. [Google Scholar]
Song 2012 {published data only}
- Song SW, Kim SH, Ahn YB, Sung‐Goo K. Effect of dance exercise on cognitive function in elderly patients with metabolic syndrome: a pilot study. Obesity facts. Conference: 19th European Congress on Obesity, ECO2012 Lyon France. Conference Start: 20120509 Conference End: 20120512. Conference Publication. 2012:211.
Wilkinson 1998 {published data only}
- Wilkinson N, Srikumar S, Shaw K, Orrell M. Drama and movement therapy in dementia: a pilot study. The Arts in Psychotherapy 1998;25(3):195‐201. [Google Scholar]
References to ongoing studies
Ho Rainbow ongoing {unpublished data only}
- Ho Rainbow TH, Cheung JKK, Chan WC, Cheung IKM, Lam LCW. A 3‐arm randomized controlled trial on the effects of dance movement intervention and exercises on elderly with early dementia. BMC Geriatrics. [DOI] [PMC free article] [PubMed]
Lyons ongoing {unpublished data only}
- Lyons S, Roe B, Meekums B. The value of arts therapies in dementia: a mixed methods trial. Proposal for Phd registration submitted to Edge Hill University, UK.
Additional references
ADI 2016
- Alzheimer's Disease International (ADI). World Alzheimer Report 2010: The global economic impact of dementia. Alzheimer’s Disease International: London 2016.
ADMP UK 2016
- Association of Dance Movement Psychotherapy UK (ADMP UK). What is Dance Movement Psychotherapy?. www.admt.org.uk/whatis.html 2016.
Alexopoulos 1988
- Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell scale for depression in dementia. Biological Psychology 1988;23(3):271‐84. [DOI] [PubMed] [Google Scholar]
American Psychiatric Association 2013
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing., 2013. [Google Scholar]
Beard 2011
- Beard R. Art therapies and dementia care: a systematic review. Dementia 2011;11(5):633‐56. [DOI: 10.1177/1471301211421090] [DOI] [Google Scholar]
Berrol 2006
- Berrol C. Neuroscience meets dance/movement therapy: mirror neurons, the therapeutic process and empathy. The Arts in Psychotherapy 2006;33:302‐15. [Google Scholar]
Bradt 2011
- Bradt J, Goodill SW, Dileo C. Dance/movement therapy for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews 2011, Issue 10. [DOI: 10.1002/14651858.CD007103.pub2] [DOI] [PubMed] [Google Scholar]
Brooks 1989
- Brook D, Stark A. The effects of dance/movement therapy on affect: a pilot study. American Journal of Dance Therapy 1989;11:101‐12. [Google Scholar]
Burns 2008
- Burns J. An interpretive description of patterns of practice of arts therapists working with older people who have dementia in the UK [PhD thesis]. Edinburgh (UK): Queen Margaret University, 2008. [Google Scholar]
Campbell 2007
- Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455‐10.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carcel 2012
- Carcel C, Dasig D, Noble P, Ledesma L, Adapon H, Tuason J. Can ballroom dancing make you smarter? An investigation on its relationship with hippocampal volume and memory performance in older adults. Alzheimer's and dementia 2012 conference: Alzheimer's Association international conference 2012, Vancouver BC, Canada 2012;8(4):142. [Google Scholar]
Chaiklin 1986
- Chaiklin S, Schmais D. The Chace approach to dance therapy. In: Lewis P editor(s). Theoretical Approaches in Dance/Movement Therapy. Vol. 1, Iowa: KIendall/Hunt, 1986:17‐36. [Google Scholar]
Chen 2000
- Chen YL, Ryden MB, Feldt K, Savik K. The relationship between social interaction and characteristics of aggressive, cognitively impaired nursing home residents. American Journal of Alzheimer's Disease 2000;15(1):10‐7. [Google Scholar]
Cohen‐Mansfield 1989
- Cohen‐Mansfield J, Marx MS, Rosenthal AS. A description of agitation in a nursing home. Journal of Gerontology: Medical Sciences 1989;44(3):M77‐M84. [DOI] [PubMed] [Google Scholar]
Colcombe 2003
- Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta‐analytic study. Psychological Science 2003;14(2):125‐30. [DOI] [PubMed] [Google Scholar]
Craig 2008
- Craig P, Dieppe P, Macintyre S, Ritchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655‐10.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Deshmukh 2014
- Deshmukh SR, Holmes J, Cardno A. Art therapy for people with dementia. Cochrane Database of Systematic Reviews 2014, Issue 4. [DOI: 10.1002/14651858.CD011073] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dosamantes‐Alperson 1981
- Dosamantes‐Alperson E. Experiencing in movement therapy. American Journal of Dance Therapy 1981;4(2):33‐44. [Google Scholar]
Folstein 1975
- Folstein MF, Folstein SE, McHigh PR. 'Mini‐Mental State': a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 1975;12:189‐98. [DOI] [PubMed] [Google Scholar]
Forbes 2015
- Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S. Exercise programs for people with dementia. Cochrane Database of Systematic Reviews 2015, Issue 4. [DOI: 10.1002/14651858.CD006489.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gazzola 2006
- Gazzola V, Aziz‐Zadeh L, Keysers C. Empathy and the somatotopic auditory mirror system in humans. Current Biology 2006;16:1824‐9. [DOI] [PubMed] [Google Scholar]
Guise 2014
- Guise JM, Chang C, Viswanathan M, Glick S, Treadwell J, Umscheid C, et al. Systematic Reviews of Complex Multicomponent Health Care Interventions. Research White Paper. Agency for Healthcare Research and Quality (AHRQ) Publication No. 14‐EHC003‐EF. Rockville, MD: AHRQ, 2014. [PubMed] [Google Scholar]
Guzmán‐García 2012
- Guzmán‐García A, Hughes JC, James IA, Rochester L. Dancing as a psychosocial intervention in care homes: a systematic review of the literature. International Journal of Geriatric Psychiatry 2012;28(9):914‐24. [DOI: 10.1002/gps.3913] [DOI] [PubMed] [Google Scholar]
Hackney 2007
- Hackney ME, Kantorovich S, Levin R, Earhart GA. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. Journal of Neurologic Physical Therapy 2007;31(4):173‐9. [DOI] [PubMed] [Google Scholar]
Hackney 2010
- Hackney ME, Earhart GA. Effects of dance on balance and gait in severe Parkinson disease: a case study. Disability and Rehabilitation 2010;32(8):679‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 2011
- Hayes J, Povey S. The Creative Arts in Dementia Care: Practical Person‐Centred Approaches and Ideas. London: Jessica Kingsley, 2011. [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hill 1999
- Hill H. Dance therapy and communication in dementia. Signpost Cardiff Royal Hamadryod Hospital 1999;4(1):13‐4. [Google Scholar]
Karkou 2006
- Karkou V, Sanderson P. Arts Therapies: A Research‐Based Map of the Field. Edinburgh: Elsevier, 2006. [Google Scholar]
Kitwood 1997
- Kitwood T. Dementia Reconsidered. London: Routledge, 1997. [Google Scholar]
Koch 2014
- Koch S, Kunz T, Lykou S, Cruz R. Effects of dance movement therapy and dance on health‐related psychological outcomes: a meta‐analysis. The Arts in Psychotherapy 2014;41:46‐64. [Google Scholar]
Kowarzik 2004
- Kowarzik U. Opening Doors: Dance Movement Therapy with People with Dementia. In: Payne H editor(s). Dance Movement Therapy: Theory, Research and Practice. Hove: Routledge, 2005. [Google Scholar]
Krishnamoorthy 2011
- Krishnamoorthy A, Anderson D. Managing challenging behaviour in older adults with dementia. Progress in Neurology and Psychiatry 2011;15(3):20‐27. [Google Scholar]
Laban 1975
- Laban R. Modern Educational Dance. London: MacDonald Evans, 1975. [Google Scholar]
Levy 1992
- Levy F. Dance/Movement Therapy: A Healing Art. Reston, VA: American Alliance for Health, Physical Education,Recreation and Dance, 1992. [Google Scholar]
Logsdson 1999
- Logsdon RG, Gibbons LE, McCurry SM, Teri L. Quality of life in Alzheimer's disease: patient and caregiver reports. Journal of Mental Health and Aging 1999;5:21‐32. [Google Scholar]
Macaskie 2012
- Macaskie J, Meekums B, Nolan G. Transformational education for psychotherapy and counselling: a relational dynamic approach. British Journal of Guidance & Counselling 2012;41(4):351‐62. [DOI: 10.1080/03069885.2012.726348] [DOI] [Google Scholar]
Matthews 2013
- Matthews FS, Arthur A, Barnes LE, Bond J, Jagger C, Robinson L, et al. A two‐decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. The Lancet 2013;382(9902):1405‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Medical Research Council 2000
- Medical Research Council (MRC). A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health. London: MRC, 2000. [Google Scholar]
Medical Research Council 2008
- Medical Research Council (MRC). Developing and Evaluating Complex Interventions: New Guidance. London: MRC, 2008. [Google Scholar]
Meekums 1991
- Meekums B. Dance movement therapy with mothers and young children at risk of abuse. The Arts in Psychotherapy 1991;18(3):223‐30. [Google Scholar]
Meekums 2002
- Meekums B. Dance Movement Therapy. London: Sage, 2002. [Google Scholar]
Meekums 2008
- Meekums B. Pioneering dance movement therapy in Britain: results of narrative research. The Arts in Psychotherapy 2008;35:99‐106. [Google Scholar]
Meekums 2012
- Meekums B. Kinesthetic Empathy and Movement Metaphor in Dance Movement Psychotherapy. In: Reynolds D, Reason M editor(s). Kinaesthetic Empathy in Creative and Cultural Practices. Bristol: Intellect Publishing, 2012. [Google Scholar]
Meekums 2015
- Meekums B, Karkou V, Nelson EA. Dance movement therapy for depression. Cochrane Database of Systematic Reviews 2015, Issue 2. [DOI: 10.1002/14651858.CD009895] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA Statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2006
- NICE. Dementia: supporting people with dementia and their carers in health and social care. www.nice.org.uk/guidance/cg42 2006. Last updated 2016; Vol. 42.
Norcross 2011
- Norcross JC, Wampold BE. What works for whom: tailoring psychotherapy to the person. Journal of Clinical Psychology: In Session 2011;67:127‐32. [DOI: 10.1002/jclp.20764] [DOI] [PubMed] [Google Scholar]
Palo‐Bengtsson 2002
- Palo‐Bengtsson L, Ekman S‐L. Emotional response to social dancing and walks in persons with dementia. American Journal of Alzheimer’s Disease and Other Dementias 2002;17(3):149‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Payne 1992
- Payne H. Dance Movement Therapy: Theory and Practice. 1st Edition. London: Routledge, 1992. [Google Scholar]
Ren 2013
- Ren J, Xia J. Dance therapy for schizophrenia. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD006868.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rizzolatti 1996
- Rizzolatti G, Fadiga L, Gallese V, Fogassi L. Premotor cortex and the recognition of motor actions. Cognitive Brain Research 1996;3:131‐41. [DOI] [PubMed] [Google Scholar]
Rosen 1984
- Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer's disease. American Journal of Psychiatry 1984;141:1356‐64. [DOI] [PubMed] [Google Scholar]
Sandel 1987
- Sandel S, Johnson DR. Creativity and Hope in the Nursing Home. New York: The Haworth Press, 1987. [Google Scholar]
Shaji 2009
- Shaji KS, George RK, Prince MJ, Jacob KS. Behavioral symptoms and caregiver burden in dementia. Indian Journal of Psychiatry 2009;51(1):45‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaverniece 2012
- Vaverniece I, Majore‐Dusele I, Meekums B, Rasnacs O. Dance movement therapy for obese women with emotional eating: a controlled pilot study. The Arts in Psychotherapy 2012;39:126‐33. [DOI: 10.1016/j.aip.2012.02.004] [DOI] [Google Scholar]
Verghese 2003
- Verghese J, Lipton R, Katz M, Hall C, Derby C, Kuslansky G, et al. Leisure activities and the risk of dementia in the elderly. New England Journal of Medicine 2003;348:2508‐16. [DOI] [PubMed] [Google Scholar]
Vink 2003
- Vink AC, Bruinsma MS, Scholten RJPM. Music therapy for people with dementia. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD003477.pub2] [DOI] [PubMed] [Google Scholar]
Violets‐Gibson 2002
- Violets‐Gibson M. Reawakening the language of the body. The Journal of Dementia Care 2002;10(5):20‐2. [Google Scholar]
Whitehouse 1979
- Whitehouse M. CG Jung and Dance‐Therapy: Two Major Principles. In: Bernstein P L editor(s). Eight Theoretical Approaches in Dance/Movement Therapy. Vol. 1, Iowa: Kendall/Hunt, 1979. [Google Scholar]
WHO 2010
- World Health Organization (WHO). The ICD‐10 Classification of Mental and Behavioural Disorders. 3rd Edition. Geneva: World Health Organisation, 2010. [Google Scholar]
Woods 2009
- Woods B, Spector AE, Jones CA, Orrell M, Davies SP. Reminiscence therapy for dementia. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD001120.pub2] [DOI] [PubMed] [Google Scholar]
Young 2011
- Young TJ, Manthrop C, Howells D, Tullo E. Developing a career communication intervention to support personhood and quality of life in dementia. Ageing and Society 2011;23(07):1003‐25. [Google Scholar]


