Abstract
Background
Physical activity, a balanced diet, avoidance of tobacco exposure, and limited alcohol consumption may reduce morbidity and mortality from non‐communicable diseases (NCDs). Mass media interventions are commonly used to encourage healthier behaviours in population groups. It is unclear whether targeted mass media interventions for ethnic minority groups are more or less effective in changing behaviours than those developed for the general population.
Objectives
To determine the effects of mass media interventions targeting adult ethnic minorities with messages about physical activity, dietary patterns, tobacco use or alcohol consumption to reduce the risk of NCDs.
Search methods
We searched CENTRAL, MEDLINE, Embase, PsycINFO, CINAHL, ERIC, SweMed+, and ISI Web of Science until August 2016. We also searched for grey literature in OpenGrey, Grey Literature Report, Eldis, and two relevant websites until October 2016. The searches were not restricted by language.
Selection criteria
We searched for individual and cluster‐randomised controlled trials, controlled before‐and‐after studies (CBA) and interrupted time series studies (ITS). Relevant interventions promoted healthier behaviours related to physical activity, dietary patterns, tobacco use or alcohol consumption; were disseminated via mass media channels; and targeted ethnic minority groups. The population of interest comprised adults (≥ 18 years) from ethnic minority groups in the focal countries. Primary outcomes included indicators of behavioural change, self‐reported behavioural change and knowledge and attitudes towards change. Secondary outcomes were the use of health promotion services and costs related to the project.
Data collection and analysis
Two authors independently reviewed the references to identify studies for inclusion. We extracted data and assessed the risk of bias in all included studies. We did not pool the results due to heterogeneity in comparisons made, outcomes, and study designs. We describe the results narratively and present them in 'Summary of findings' tables. We judged the quality of the evidence using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology.
Main results
Six studies met the inclusion criteria, including three RCTs, two cluster‐RCTs and one ITS. All were conducted in the USA and comprised targeted mass media interventions for people of African descent (four studies), Spanish‐language dominant Latino immigrants (one study), and Chinese immigrants (one study). The two latter studies offered the intervention in the participants’ first language (Spanish, Cantonese, or Mandarin). Three interventions targeted towards women only, one pregnant women specifically. We judged all studies as being at unclear risk of bias in at least one domain and three studies as being at high risk of bias in at least one domain.
We categorised the findings into three comparisons. The first comparison examined mass media interventions targeted at ethnic minorities versus an equivalent mass media intervention intended for the general population. The one study in this category (255 participants of African decent) found little or no difference in effect on self‐reported behavioural change for smoking and only small differences in attitudes to change between participants who were given a culturally specific smoking cessation booklet versus a booklet intended for the general population. We are uncertain about the effect estimates, as assessed by the GRADE methodology (very low quality evidence of effect). No study provided data for indicators of behavioural change or adverse effects.
The second comparison assessed targeted mass media interventions versus no intervention. One study (154 participants of African decent) reported effects for our primary outcomes. Participants in the intervention group had access to 12 one‐hour live programmes on cable TV and received print material over three months regarding nutrition and physical activity to improve health and weight control. Change in body mass index (BMI) was comparable between groups 12 months after the baseline (low quality evidence). Scores on a food habits (fat behaviours) and total leisure activity scores changed favourably for the intervention group (very low quality evidence). Two other studies exposed entire populations in geographical areas to radio advertisements targeted towards African American communities. Authors presented effects on two of our secondary outcomes, use of health promotion services and project costs. The campaign message was to call smoking quit lines. The outcome was the number of calls received. After one year, one study reported 18 calls per estimated 10,000 targeted smokers from the intervention communities (estimated target population 310,500 persons), compared to 0.2 calls per estimated 10,000 targeted smokers from the control communities (estimated target population 331,400 persons) (moderate quality evidence). The ITS study also reported an increase in the number of calls from the target population during campaigns (low quality evidence). The proportion of African American callers increased in both studies (low to very low quality evidence). No study provided data on knowledge and attitudes for change and adverse effects. Information on costs were sparse.
The third comparison assessed targeted mass media interventions versus a mass media intervention plus personalised content. Findings are based on three studies (1361 participants). Participants in these comparison groups received personal feedback. Two of the studies recorded weight changes over time. Neither found significant differences between the groups (low quality evidence). Evidence on behavioural changes, and knowledge and attitudes typically found some effects in favour of receiving personalised content or no significant differences between groups (very low quality evidence). No study provided data on adverse effects. Information on costs were sparse.
Authors' conclusions
The available evidence is inadequate for understanding whether mass media interventions targeted toward ethnic minority populations are more effective in changing health behaviours than mass media interventions intended for the population at large. When compared to no intervention, a targeted mass media intervention may increase the number of calls to smoking quit line, but the effect on health behaviours is unclear. These studies could not distinguish the impact of different components, for instance the effect of hearing a message regarding behavioural change, the cultural adaptation to the ethnic minority group, or increase reach to the target group through more appropriate mass media channels. New studies should explore targeted interventions for ethnic minorities with a first language other than the dominant language in their resident country, as well as directly compare targeted versus general population mass media interventions.
Keywords: Adult, Humans, Health Behavior, Mass Media, Alcohol Drinking, Alcohol Drinking/prevention & control, Black or African American, Diet, Exercise, Feeding Behavior, Health Promotion, Health Promotion/methods, Hotlines, Hotlines/statistics & numerical data, Interrupted Time Series Analysis, Minority Groups, Minority Groups/education, Primary Prevention, Primary Prevention/education, Randomized Controlled Trials as Topic, Smoking Cessation, Smoking Prevention
Plain language summary
Targeted mass media interventions to encourage healthier behaviours in adult, ethnic minorities
Background and review question
Health authorities and non‐governmental organisations often use mass media interventions (e.g. leaflets, radio and TV advertisements, posters and social media) to encourage healthier behaviours related to physical activity, dietary patterns, tobacco use or alcohol consumption, among others. In this review, we consider the effects of mass media interventions targeted towards ethnic minorities. A targeted intervention is designed for and considers the characteristics of a specific group, ideally providing ethnic minority groups equal opportunities and resources to access information, life skills, and opportunities to make healthier choices. However, we do not know whether targeted mass media strategies are more effective in reaching and influencing ethnic minorities than mass media strategies developed for the general population.
Study characteristics
We found six studies, all from the USA, four of which targeted African Americans and two which targeted Latino or Chinese immigrants. Of the studies, four were experimental (1693 volunteers) and two reported the results of large, targeted campaigns run in whole communities and cities. The evidence is current to August 2016.
Key results
The available evidence is insufficient to conclude whether targeted mass media interventions for ethnic minority groups are more, less or equally effective in changing health behaviours than general mass media interventions. Only one study compared participants' smoking habits and intentions to quit following the receipt of either a culturally adapted smoking advice booklet or a booklet developed for the general population. They found little or no differences in smoking behaviours between the groups.
When compared to no mass media intervention, a targeted mass media intervention may increase the number of calls to smoking quit lines, but the effect on health behaviours is unclear. This conclusion is based on findings from three studies. One study gave participants access to a series of 12 live shows on cable TV with information on how to maintain a healthy weight through diet and physical activity. Compared to women who did not watch the shows, participants reported slightly increased physical activity and some positive changes to their dietary patterns; however, their body weight was no different over time. Two other studies were large‐scale targeted campaigns in which smokers were encouraged to call a quit line for smoking cessation advice. The number of telephone calls from the target population increased considerably during the campaign.
This review also compared targeted mass media interventions versus mass media interventions with added personal interactions. These findings, based on three studies, were inconclusive.
None of the studies reported whether the interventions could have had any adverse effects, such as possible stigmatisation or increased resistance to messages.
Further studies directly comparing targeted mass media interventions with general mass media interventions would be useful. Few studies have investigated the effects of targeted mass media interventions for ethnic minority groups who primarily speak a non‐dominant language.
Quality of the evidence
Our confidence in the evidence of effect on all main outcomes is low to very low. This means that the true effect may be different or substantially different from the results presented in this review. We have moderate confidence in the estimated increase in the number of calls to smoking quit lines.
Summary of findings
Summary of findings for the main comparison. Targeted mass media intervention versus general population mass media intervention for promoting healthy behaviours.
| Comparison 1: targeted mass media intervention versus general population mass media intervention for promoting healthy behaviours | ||||||
| Patient or population: adult, ethnic minority: self‐described Americans of African heritage Setting: volunteers, smokers, USA Intervention: targeted mass media intervention Comparison: general population mass media intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | N of participants (studies) | Quality of the evidence (GRADE)a | Comments | |
| Assumed risk | Corresponding risk | |||||
| General population mass media intervention | Targeted mass media intervention | |||||
| Indicators of behavioural change | ||||||
| Any outcome considered an indicator of change | No study provided data for this outcome. | |||||
| Self‐reported behavioural change | ||||||
| Proportion smoking reduction, 3 months follow‐up |
94% | 95% | — | 255 (1 RCT) | ⊕⊝⊝⊝ Very lowb,c | No effect measures reported by authors. Not significantly different between groups |
| Quit‐attempts, 3 months follow‐up |
— | — | Adjusted OR 1.97 (1.09 to 3.55) in favour of general population mass media intervention | 255 (1 RCT) | ⊕⊝⊝⊝ Very lowb,c | 24‐hour and 7‐day point prevalence abstinence not significantly different between groups |
| Knowledge and attitudes to change | ||||||
| Contemplation ladder to quit smoking (1‐10), 3 months follow‐up | Mean score: 8.2 (SD 2.4) | Mean score: 7.3 (SD 2.6) | — | 255 (1 RCT) |
⊕⊝⊝⊝ Very lowb,c | Difference between group reported at P = 0.01 |
| Adverse effects | ||||||
| Any outcome considered an adverse effect | No study provided data for this outcome. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; OR: odds ratio; SD: standard deviation. | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect. | ||||||
aIn the GRADE assessments for the domain 'directness', we considered the studies directly relevant to the inclusion criteria. Thus, we have not downgraded on this domain. However, the population of interest will be dissimilar in different contexts, relating to characteristics of the ethnic minority group, the country and setting overall. The transferability of results must be considered for each context specifically. bDowngraded one level for unclear risk of bias. cDowngraded two levels for imprecision: Only one, relatively small study.
Summary of findings 2. Targeted mass media intervention for promoting healthy behaviours versus no intervention.
| Comparison 2: targeted mass media intervention for promoting healthy behaviours versus no intervention | ||||||
| Patient or population: adult, ethnic minority group: self‐described Americans of African heritage Setting: volunteers, community setting, USA Intervention: targeted mass media intervention Comparison: no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | N of participants (studies) | Quality of the evidence (GRADE)a | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Targeted mass media intervention | |||||
| Indicators of behavioural change | ||||||
| BMI (kg/m2), 12 months from baseline | 34.4 (SD 8.5)b | Mean difference in change 0.1 (−0.4 to 0.6) | — | 154 (1 RCT) | ⊕⊕⊝⊝ Lowc | Corresponding risk at 3 months: mean difference in change −0.4 (−0.7 to −0.02) |
| Self‐reported behavioural change | ||||||
| Changes in dietary composition, 12 months from baseline | Food habits questionnaire, score on fat behaviours (no scoring scale provided by study authors): 1.0 (SD 0.4) | Mean difference in change −0.2 (−0.3 to ‐0.1) | — | 154 (1 RCT) |
⊕⊝⊝⊝ Very lowc,d | Corresponding risk at 3 months: mean difference in change −0.1 (−0.2 to −0.02) |
| Leisure time physical activity, 12 months from baseline | Physical activity score (no scoring scale provided by study authors): 60.0 (SD 47.0)e | Mean difference in change 12.0 (1.0 to 23.0) | — | 154 (1 RCT) |
⊕⊝⊝⊝ Very lowc,d | Corresponding risk at 3 months: mean difference in change 10.0 (−1.7 to 21.8) |
| Knowledge and attitudes to change | ||||||
| Any measure of knowledge and attitude | No study provided data for this outcome. | |||||
| Adverse effects | ||||||
| Any outcome considered an adverse effect | No study provided data for this outcome. | |||||
| Use of health promotion services (secondary outcome) | ||||||
| Calls to smoking quit lines, during campaign | 18 calls per estimated 10,000 African American smokers in the intervention group versus 0.2 calls in the control communitiesf. | Estimated target population 641,800 (1 RCT) |
⊕⊕⊕⊝ Moderateg,h | — | ||
| Calls to smoking quit lines, during and after campaign | Change from pre‐campaign, calls per month (95% CI) from new pregnant smokers: 8 (1 to 14) first month of campaign, 8 (1 to 14) last month of campaign, 6 (−1 to 12) first month after campaign, 3 (−4 to 10) 4 months after campaign | Population in target city ˜300,000 (1 ITS) | ⊕⊕⊝⊝ Lowi,j | — | ||
| Proportion of calls from target population during campaign | Proportion of calls from African Americans during trial: 82% in intervention and 26% in control communities | Estimated target population 641,800 (1 RCT) |
⊕⊕⊝⊝ Lowg,k | — | ||
| Proportion of calls from target population during and after campaign | Proportion African Americans among pregnant callers: 41% before campaign, 86% during the campaign, 28% after campaign | Population in target city ˜300,000 (1 ITS) | ⊕⊝⊝⊝ Very lowi,k | — | ||
| Costs of the project (secondary outcome) | ||||||
| Programme costs | USD 106,821 for radio advertisements and USD 6744 for television advertisements. No overall costs reported | Estimated target population 641,800 (1 RCT) |
⊕⊕⊝⊝ Lowg,k | — | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; ITS: interrupted time series; RTC: randomised controlled trial; SD: standard deviation. | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect. | ||||||
aIn the GRADE assessments for the domain 'directness', we considered the studies directly relevant to the inclusion criteria. Thus, we have not downgraded on this domain. However, the population of interest will be dissimilar in different contexts, relating to characteristics of the ethnic minority group, the country and setting overall. The transferability of results must be considered for each context specifically. bMean BMI at baseline in comparison group. cDowngraded two levels for imprecision: only one relatively small study. dDowngraded one level for unclear risk of bias. eMean score at baseline in comparison group fMeasures of dispersion not reported. No adjustment for cluster‐randomised design. gDowngraded one level for unclear risk of bias in the largest study. hUnclear precision of estimate and no adjustment for cluster‐randomised design, but substantial effect. Results from ITS study concludes similarly. Therefore, we have not downgraded for imprecision. iGrading of ITS study (observational study) starts at low quality evidence. jResults from RCT study concludes similarly. Therefore, we have not downgraded for imprecision. kDowngraded one level for imprecision.
Summary of findings 3. Targeted mass media intervention versus targeted mass media intervention plus personalised content.
| Comparison 3: targeted mass media intervention versus targeted mass media intervention plus personalised content | ||||||
| Patient or population: adult, ethnic minority groups: Latino immigrants, elderly Chinese immigrants, self‐described Americans of African heritage Setting: volunteers, community setting, USA Intervention: targeted mass media intervention Comparison: media intervention combined with personalised content | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | N of participants (studies) | Quality of the evidence (GRADE)a | Comments | |
| Assumed risk | Corresponding risk | |||||
| Media intervention with personalised content (comparison) | Targeted mass media intervention | |||||
| Indicators of behavioural change | ||||||
| BMI (kg/m2), 12 months from baseline | 34.9 (SD 7.7)b | Mean difference in change 0.4 (−0.1 to 0.8) | — | 286 (1 RCT) | ⊕⊕⊝⊝ Lowc | Two RCTs (643 participants) reported BMI at 3 months. None found significant differences in weight change between study groups |
| Self‐reported behavioural change | ||||||
| Intake meeting target from dietary guidelines, 3 months from baseline | Vegetables: adjusted OR 5.53d (1.96 to 15.58) Fruit: adjusted OR 1.77d (0.99 to 3.15) |
718 (1 RCT) | ⊕⊝⊝⊝ Very lowc,e | — | ||
| Changes in dietary composition, 12 months from baseline | Food habits questionnaire, score on fat behaviours (no scoring scale provided by study authors): 1.0 (SD 0.4)f | Mean difference in change −0.1 (−0.2 to −0.02) | — | 286 (1 RCT) | ⊕⊝⊝⊝ Very lowc,e | Two RCTs (643 participants) reported changes in dietary composition at 3 months. None found significant differences/mean difference in change for energy or dietary fibre intake (study 1) or food habits questionnaire (fat behaviours) (study 2) |
| Weekly physical activity meeting target from guidelines, 3 months from baseline | Adjusted OR 1.27d (0.89 to 1.80) | 718 (1 RCT) | ⊕⊝⊝⊝ Very lowc,e | — | ||
| Leisure time physical activity, 12 months from baseline | Physical activity score (no scoring scale provided by study authors): 68.0 (47.6)f | Mean difference in change 12.9 (3.5 to 22.3) | — | 286 (1 RCT) | ⊕⊝⊝⊝ Very lowc,e | Corresponding risk at 3 months: mean difference in change −2.2 (−12.9 to 8.5) |
| Knowledge and attitudes to change | ||||||
| Knowledge of nutrition and physical activity guidelines | Daily vegetable intake: adjusted OR 12.6d (6.50 to 24.5) Daily fruit intake: adjusted OR 16.2d (5.61 to 46.5) Weekly physical activity: adjusted OR 2.70d (0.31 to 23.2) |
⊕⊝⊝⊝ Very lowc,e | — | |||
| Adverse effects | ||||||
| Any outcome considered an adverse effect | No study provided data for this outcome. | |||||
| Costs of the project (secondary outcome) | ||||||
| Costs per person in each treatment arm | USD 9.00 for targeted newsletters, USD 45.00 individually tailored newsletters, and USD 135 for individually tailored newsletters followed by home visits | 357 (1 RCT) | ⊕⊝⊝⊝ Very lowc,e | — | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial;RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect. | ||||||
aIn the GRADE assessments for the domain 'directness', we considered the studies directly relevant to the inclusion criteria. Thus, we have not downgraded on this domain. However, the population of interest will be dissimilar in different contexts, relating to characteristics of the ethnic minority group, the country and setting overall. The transferability of results must be considered for each context specifically. bMean (SD) BMI at baseline in comparison group. cDowngraded two levels for imprecision: Relatively small studies and few measurement points. dOR > 1 in favour of targeted mass media combined with personalised content (control intervention). Effect estimates adjusted for cluster‐randomised design. eDowngraded one for unclear risk of bias. fMean (SD) score at baseline in comparison group.
Background
Description of the condition
This Cochrane Review explores the effectiveness of targeted mass media interventions in advising ethnic minority groups on preventing non‐communicable diseases (NCDs) through healthier behaviours. Specifically, this review addresses the question of whether or not ethnic minorities will benefit from targeted approaches, which means that interventions are designed to consider characteristics of particular groups (Kreuter 2003).
The most prevalent NCDs (cardiovascular diseases, cancers, chronic respiratory disease, and diabetes) are also the world's leading causes of morbidity and mortality. According to the World Health Organization (WHO), NCDs cause 63% of global deaths, about 40% of which occur in people between 30 and 70 years of age (WHO 2010). The burden of NCDs is a growing public health crisis worldwide, and WHO has called for more actions to prevent disease. Many NCDs share four modifiable, behavioural risk factors: lack of physical activity, poor diet, tobacco use, and excessive consumption of alcohol. Improvements in these behaviours can prevent or delay the onset of disease (Lim 2012). One of the objectives in the WHO Global Action Plan for the Prevention of Noncommunicable Diseases deals with the need to address these four risk factors throughout populations, and mass media campaigns and social marketing initiatives are among the proposed policy options (WHO 2013a).
The WHO Commission on Social Determinants of Health highlighted how "the conditions in which people are born, grow, live, work and age" strongly determine health status and disease patterns within and between populations (CSDH 2008). This picture includes inequities in the morbidity and mortality patterns of NCDs (WHO 2010). In most countries, life expectancy and health status are correlated with social status, as measured by education, occupation, income, or wealth. The underlying forces behind this link include a wide array of unevenly distributed environmental, structural, economic, social, and cultural factors (CSDH 2008). Health inequities are not simply differences between groups, but differences that are considered both avoidable and unjust (Whitehead 1992). The Rio Political Declaration on Social Determinants of Health reaffirmed a global political commitment to reducing health inequities (WHO 2011).
Inequities in health status and disease risk are also associated with ethnic minority status. In many countries, ethnic minority groups tend to have poorer health outcomes than the majority population (Alderete 1999; Nielsen 2010; AHRQ 2013). Genetic variations only partially contribute to differences between ethnic groups in terms of disease patterns (Bhopal 2007). Differences in cultural factors (e.g. beliefs and practices) may influence health status, but social, economic and structural determinants of health during people's lifespans appear to be associated with health inequities between ethnic groups as well (Nazroo 2003; Mulia 2008; Viruell‐Fuentes 2012). Therefore, cultural influences should not be overemphasised as discrete explanatory factors for health inequities (Nazroo 2003; Acevedo‐Garcia 2012). Ethnic minority groups are heterogeneous, having wide‐ranging living conditions within and between countries, with consequently different health statuses and disease risks. The disease patterns of ethnic minorities may converge over time towards those of the majority population. However, health inequities between groups are sufficiently pronounced in many countries to warrant specific public health considerations.
Physical activity levels, dietary habits, tobacco use and alcohol consumption vary between population groups (WHO 2010). In many countries, unhealthy behaviours tend to be more prevalent in disadvantaged groups (Mackenbach 2008), and disparities in health behaviours have recently been shown to increase over time, as more privileged socioeconomic groups adopt healthier behaviours while disadvantaged groups lag behind (Buck 2012). Thus, although behaviours have an element of personal choice, behavioural patterns reveal the influence of the wider determinants of health.
Concern has been raised that public health interventions that have benefited the population overall might have increased inequities. This effect has been observed in public health interventions aimed at voluntary behavioural change in particular (Lorenc 2013). Public health campaigns delivered through mass media or by other means appear to be less effective in socioeconomically disadvantaged groups, whether for smoking cessation (Niederdeppe 2008a; Thomas 2008), physical activity (De Bourdeaudhuij 2011), or dietary factors (Oldroyd 2008; Stockley 2008). On the contrary, structural interventions, such as taxation of tobacco products and alcoholic beverages, appear more likely to reduce differences in health parameters (Lorenc 2013). It is therefore important to identify effective public health strategies that bridge the health gap rather than amplify it.
There are reasons to believe that mass media interventions can be less effective in reaching many ethnic minority groups as well, although few studies have systematically assessed the effects of these campaigns on ethnic minority groups (Niederdeppe 2008b; Durkin 2012; Bala 2013). The health behaviours of ethnic minority groups in different countries could be both more and less healthy than those of the majority population (e.g. the higher prevalence of smokers in some indigenous populations or lower alcohol consumption among Muslim immigrants). However, by describing ethnic minority health in relative terms only, we may fail to consider the absolute magnitude of a health problem or a health need that should guide public health priorities (Bhopal 2007). The Ottawa Charter for Health Promotion declares that equal opportunities and resources to secure "access to information, life skills and opportunities for making healthy choices" are some of the prerequisites for health improvements (WHO 1986). Targeted mass media interventions are possible strategies to better disseminate health promotion messages among ethnic minorities (Webb 2010b; Gould 2013; Nierkens 2013), but their effectiveness has not been established.
There is no internationally agreed‐upon definition of ethnicity, but Bhopal 2007 has summarised some key points: "The concept of ethnicity is complex and implies, according to most accounts, one or more of the following: shared origins or social background; shared culture and traditions which are distinctive, maintained between generations, and lead to a sense of identity and group‐ness; a common language or religious tradition" (Bhopal 2007). Oxford Dictionaries defines an ethnic minority as "a group within a community which has different national or cultural traditions from the main population". Ethnic minority groups are sometimes divided into indigenous populations (SPFII 2004), national ethnic minorities (long‐time residents) (FCNM 2012), and immigrants. Through international migration, most countries gradually become more ethnically diverse. It is important to note that these definitions use social and cultural factors rather than biological ones (physical appearance or genetic differences) to define population groups (Bhopal 2007).
Ethnic minority status is associated with lower socioeconomic status in many countries, but ethnic identity and measures of socioeconomic status have different features. Programmes targeted to ethnic minorities should consider factors such as preferred language; food traditions; different norms, values and knowledge systems; patterns of media use; collective history; and position in the society. Arguably, then, it is appropriate to explore the effectiveness of mass media interventions targeted to ethnic minority groups as distinct from interventions directed at socioeconomically disadvantaged groups.
Description of the intervention
Targeted mass media interventions that promote healthier behaviours to reduce the risk of NCDs in adult ethnic minorities are the subject of this Cochrane Review. Public health authorities, health promotion agencies and non‐governmental organisations (NGOs) are the main providers of health promotion interventions. According to Ferri 2013, most mass media campaigns can be characterised as either information campaigns with messages of warning, empowerment or support, or social marketing campaigns that attempt to correct erroneous normative beliefs, clarify social and legal norms, or set positive role models or social norms. Designers of mass media interventions draw on a wide range of commercial marketing tools and principles. Health promotion campaigns partly overlap with social marketing, using concepts and approaches from marketing to influence behaviours to benefit individuals and communities for the social good (French 2010).
Kreuter 2003 describes a targeted health communication strategy as communication "intended to reach some population subgroup based on characteristics presumed to be shared by the group's members". They distinguish targeted from tailored communication, which is communication adapted to the specific characteristics of an individual. A targeted approach coincides with the principle of audience segmentation in social marketing theory, that is, the identification of meaningful differences among population groups that affect their responses to the promoted action. Thorough knowledge of the target audience is important for developing good combinations of strategic elements and approaches to achieve an intervention's goals (French 2010; MvVey 2010). Targeted communication strategies are only meaningful if the population subgroup is sufficiently homogeneous (Kreuter 2003; Castro 2010). Thus, communication targeted to broadly defined population subgroups, for instance the Latino population in the USA, may fail to recognise subcultures with different history, collective experiences, living conditions and health needs.
Interventions targeting ethnic minority groups should include cultural adaptations that consider "language, culture, and context in such a way that is comparable with the client's cultural patterns, meanings, and values" (Bernal 2009). Common strategies for cultural adaptation of health interventions include gathering information, user input, and feedback from the target group (Netto 2010; Barrera 2013). A targeted approach should also carefully consider ethical aspects to avoid stereotyping and stigmatising. Cultural adaptation strategies have been categorised into surface adjustments and deep, structural‐level adjustments. Surface‐level adjustments involve changing factors such as language, graphics, food, and clothing to match the target audience. Deep, structural‐level adjustments are changes that reflect the cultural, social, historical, environmental, and psychological forces behind behaviours in the target population (Resnicow 1999).
This review includes only health promotion interventions delivered via mass media. Brinn 2010 and Bala 2013 describe mass media as "channels of communication that intend to reach a large number of people without direct person‐to‐person contact". Mass media reach audiences through print material, recordings, broadcast, the Internet, and digital technology. Mass media interventions have the potential to cost effectively reach many people and can spread a message to remote geographical areas or groups that otherwise are difficult to access, or to target certain groups through selected media channels. Mass media channels have diversified quickly in the last couple of decades, including the development of digital communication technology, and national borders now pose fewer constraints on the reach of media channels.
Previous systematic reviews on mass media interventions or campaigns concerning public health issues (smoking cessation, HIV testing, health services utilisation, illicit drug use, mental health‐related stigma) have found that their effects on behavioural outcomes are either inconclusive or exhibit only modest short‐term effects (Grilli 2002; Vidanapathirana 2006; Brinn 2010; Bala 2013; Clement 2013; Ferri 2013). Long‐term effects are generally unclear. Modest effects of mass media interventions on an individual level can still have an important public health impact overall. The population strategy approach to disease prevention, as suggested by Rose 1985, aims to shift the distribution of a risk factor across entire populations. This shift includes the large proportion of the population with only a moderate risk of disease but a significant portion of the total disease burden.
How the intervention might work
The evidence linking increased physical activity, balanced diets, avoidance of tobacco, and limited alcohol consumption to reduced morbidity and mortality from NCDs is well established (WHO 2009; WHO 2010; WHO 2013a; WHO 2013b; WHO 2014). The logic model in Figure 1 (adapted based on Bertrand 2006 and Niederdeppe 2008b) illustrates the possible elements and the relationships by which a targeted mass media intervention can influence these four health‐related behaviours. An additional desired outcome could be that individuals will consult health promotion services, such as smoking cessation assistance or health counselling.
1.
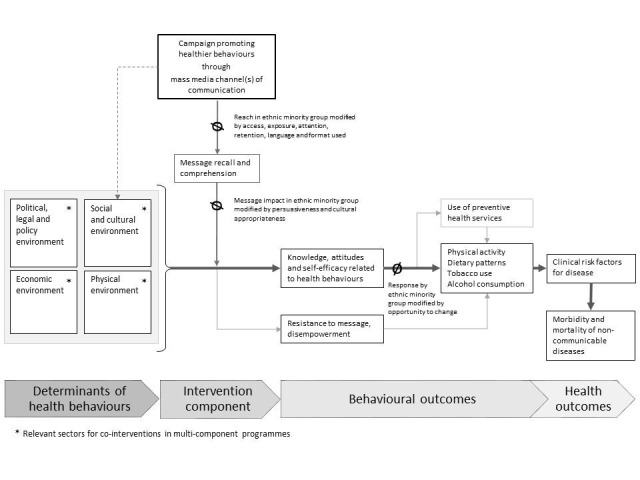
Logic model. Adapted based on Bertrand 2006 and Niederdeppe 2008b
Several theories and models seek to explain health behaviours on the individual level and to determine the most efficient way to influence these behaviours. These theories emphasise that increased knowledge is not sufficient to influence behaviour. Perceived barriers and risks are important moderators of behaviour, while attitudes and self‐efficacy contribute to a person's motivation and competence to act (Brewer 2008). In the logic model, changes in people's knowledge of and attitudes about health behaviours, in addition to self‐efficacy, are the measurable intermediate outcomes of mass media interventions. Contemporary thinking in public health and health promotion acknowledges that social norms, interpersonal interaction and the social and cultural environment influence individual behaviour strongly (Viswanath 2008). People's wider environment – physical, economic, political, legal and policy – may either enable or counteract a certain behaviour (McLeroy 1988; Davis 2014). A basic assumption in this Cochrane Review is that these theories and models are relevant to all population groups.
A mass media intervention can only influence health behaviours if the target audience receives, understands and can recall the message. Based on data and conceptual input (Sorensen 2004; Viswanath 2006; Niederdeppe 2008a), Niederdeppe 2008b has hypothesised that there are three possible sources of differences in response to smoking cessation campaigns that can be traced to socioeconomic status. These three domains probably apply to ethnic minorities as well and may be relevant to consider for targeted mass media interventions, as indicated in the logic model: differences in access, exposure, attention to and retention of the media message; differences in the message's persuasiveness and its motivational response; and differences in opportunities to change in response to the message (Niederdeppe 2008b).
Different media channels might be necessary to reach ethnic minorities, either because conventional media channels are less accessible or not preferred. The language and format of the content (language complexity, illustrations used, skills demonstration) can influence message recall and comprehension. Low health literacy levels, understood as low ability to obtain, process, and understand basic health information, have been identified in many ethnic minority groups and can influence response and compliance with health messages (Berkman 2011). Thus, planners must carefully consider media access, exposure, language and format, attention to and retention of the media message, making these relevant to the targeted ethnic minority group in order to extend the intervention reach.
The second domain relates to the persuasiveness of and motivational response to a message, which could strongly depend on its cultural appropriateness for ethnic minorities. Evidence from health promotion interventions via channels other than mass media have indicated better adherence to a promoted behavioural change when ethnic minorities receive culturally adapted health messages or counselling instead of a standard treatment (Nierkens 2013; Attridge 2014). The four health behaviours in this review relate closely to many markers of ethnic identity. The most obvious ones are dietary patterns and alcohol consumption, but physical activity and smoking patterns may also be closely related to cultural context.
Ethnic minorities might have limited opportunities to change health behaviours, either from a cultural, financial, or structural perspective. Previous reviews on the effect of mass media interventions for smoking cessation indicate that these are more likely to be successful as part of multicomponent programmes with upstream policy support and downstream community‐based activities (Brinn 2010; Bala 2013). Examples of relevant co‐interventions for this Cochrane Review include changes in legislation regarding advertising and taxation of food items, tobacco products, and alcoholic beverages, or changes in available spaces and social arenas for physical activity. Mass media interventions could have an indirect, amplifying effect if family, friends and the wider community adjust their attitudes, norms and behaviours according to the health message. Thus, multicomponent interventions can add benefits to efforts directed at individual change by modifying opportunities to change. Figure 1 indicates relevant sectors for co‐interventions in multicomponent programmes. The logic model also indicates possible unwanted effects of an intervention. Examples of adverse effects are increased resistance to the health promotion message or that the target population will experience more feelings of disempowerment when exposed to a goal they find difficult to achieve.
Why it is important to do this review
Mass media campaigns promoting healthy behaviours are one of several recommended policy options to prevent NCDs (WHO 2009; WHO 2013a), and most countries commonly use them to encourage healthier behaviours (WHO 2009; WHO 2013b; WHO 2014), despite the potentially limited effectiveness. The concern that mass media interventions could widen health inequities warrants more focus on the effect of targeted strategies in population subgroups. It is unclear whether targeted mass media interventions are more effective in changing health behaviours in ethnic minorities than a universal population strategy. This is important to explore, as segmentation of interventions to reach different subgroups may increase programme costs.
The Norwegian Directorate of Health and the Norwegian Cancer Society commissioned a systematic review on this issue to inform public health policy on how to deliver health promotion messages to the growing and increasingly diverse immigrant population. This systematic review has been widened to encompass an international perspective, including a wide focus on ethnic minority groups, as the question may be useful for other national authorities and NGOs as well.
The primary focus of this Cochrane Review is the mode of delivery (mass media intervention) and the strategies used to target such interventions to ethnic minority groups and prevention of NCDs, rather than any of the four specific health behaviours separately. The four behaviours have distinct features and require different messages regarding the suggested action (i.e. to increase physical activity, modify diets, decrease alcohol consumption, or refrain from smoking). At the same time, the behaviours are similar in their focus on preventing negative health outcomes in the future. Thus, the target audience may be less motivated to change ingrained habits in favour of longer‐term – and hence more uncertain – benefits. Our objectives intersect with two Cochrane Reviews on mass media interventions for smoking cessation (Brinn 2010; Bala 2013). Two other systematic reviews have examined the effects of smoking cessation interventions in indigenous populations but are not limited to mass media interventions (Carson 2012a; Carson 2012b). Our objectives include interventions focusing on tobacco use to obtain a full picture of mass media strategies as a means of disseminating health‐promoting messages among ethnic minorities. We gathered additional information on features of these interventions, theoretical frameworks and co‐interventions.
Objectives
Primary
• To determine the effect of mass media interventions targeting adult, ethnic minorities with messages about physical activity, dietary patterns, tobacco use or alcohol consumption to reduce risk of NCDs.
Secondary
• To examine the effect of targeted mass media interventions alone compared to targeted mass media interventions given as part of multi‐component interventions.
Methods
Criteria for considering studies for this review
Types of studies
By definition, mass media communication strategies target large groups of people. Individually randomised controlled trials (RCTs) may be neither the most appropriate nor most feasible study design. Therefore, we included the following study designs and specified features, guided by recommendations from the Effective Practice and Organisation of Care Group (EPOC) review group (EPOC 2016).
RCTs.
Cluster‐RCTs with at least two intervention groups and two control groups.
Non‐RCTs (NRCTs) with at least two intervention sites and two control sites.
Controlled before‐and‐after (CBA) studies with at least two intervention sites and two control sites.
Interrupted‐time‐series (ITS) or repeated measures studies (RMSs) with a clearly defined point in time when the intervention occurred and at least three data points before and three after the intervention.
Types of participants
The population of interest was adults (≥ 18 years) described as being from an ethnic minority group in their country of residence. We use the terms ethnicity and ethnic minorities as described in the Background but did not limit the eligibility of participants to studies using these terms. Different countries and research traditions have dissimilar terminology relating to aspects of ethnicity (Bhopal 2007). Not all use the terms ethnicity and ethnic minorities. We based inclusion on any direct or implicit description by the study authors that the study participants were selected based on ethnic minority characteristics and that the intervention was targeted to such a population group. Examples of applicable terms are indigenous populations, native, aboriginal, racial groups, immigrants, ancestral origin (countries or continents), countries of birth, or specified first language/mother tongue/language preference.
Types of interventions
To be eligible for inclusion, the intervention had to meet all of the following three criteria.
The purpose of the intervention was to promote healthier behaviours related to physical activity, dietary patterns, tobacco use, or alcohol consumption.
The intervention was disseminated via a mass media channel.
The intervention was targeted to an ethnic minority group.
We used the same definition of mass media as in two related Cochrane Reviews (Brinn 2010; Bala 2013): "Mass media is defined here as channels of communication such as television, radio, newspapers, billboards, posters, leaflets or booklets intended to reach large numbers of people and which are not dependent on person‐to‐person contact". In addition, we aimed to include other contemporary mass media channels, such as campaigns delivered through the Internet, social media, and mass distribution through mobile phones. We used the definition by Kreuter 2003 for targeted interventions but did not limit the inclusion to studies using the same terminology.
We included studies that compared the intervention with a general population mass media intervention, no intervention or any other intervention. We included studies that compared targeted mass media interventions alone with targeted mass media interventions delivered as part of multicomponent interventions to explore the secondary research objective.
There were no set requirements on minimum length of intervention.
We excluded the following interventions.
Courses, teaching activities and programmes, interactive self‐help programmes or self‐monitoring services, as these are not considered mass media interventions even though they can be delivered through the Internet, digital applications, or similar media.
Interventions with mass distributed print, audio, or visual material where the content has been tailored/personalised to each individual (i.e. based on answers from questionnaires or similar information sources).
Interventions for patient groups/patient education (including treatment of alcohol dependency and eating disorders), or interventions aimed specifically at relatives of patients.
Types of outcome measures
We did not expect to find any studies of targeted mass media interventions using morbidity or mortality of NCDs as outcome measures, nor clinical risk factors of disease. We intended to examine a number of surrogate endpoints relating to the four specified health behaviours as primary outcomes as relevant, including both objectively measured and self‐reported outcomes.
There was no requirement for a minimum duration of follow‐up for the outcome measures. We intended to present outcomes separately for short‐term (< six months) and long‐term ( ≥ six months) follow‐up.
Primary outcomes
Physiological or clinical parameters that indicate changes in physical activity, dietary intake, use of tobacco, or alcohol consumption
Objective or self‐reported measurements of physical activity, dietary intake, use of tobacco, or alcohol consumption
Measures of knowledge and attitudes concerning physical activity, dietary intake, use of tobacco, or alcohol consumption
Secondary outcomes
Use of health promotion services (for instance smoking quit lines and counselling) or other relevant services
Costs related to the project
Adverse outcomes
Any reported outcome considered an adverse effect, such as measures of participants' resistance to the health promotion message or measures of perceived disempowerment in participants.
Search methods for identification of studies
A research librarian conducted the electronic literature searches.
Electronic searches
We performed a scoping search to identify any systematic reviews in the last five years with a similar primary research objective. We based the search terms on the strategy described in Appendix 1 but with a filter for systematic reviews. We searched the following electronic databases from the beginning of 2009 until September 2014.
Cochrane Database of Systematic Reviews, part of the Cochrane Library (www.thecochranelibrary.com).
Database of Abstracts of Reviews of Effects (DARE), part of the Cochrane Library (www.thecochranelibrary.com).
Health Technology Assessment Database (HTA), part of the Cochrane Library (www.thecochranelibrary.com).
Centre for Reviews and Dissemination (DARE, HTA).
We did not identify any systematic reviews with a similar research objective. As previously described, we are aware of that four Cochrane systematic reviews intersect with the objectives of this Cochrane Review (Brinn 2010; Carson 2012a; Carson 2012b; Bala 2013).
We searched for primary studies without any time limitations or language restrictions on 22 May 2015 and later updated the search to 23 August 2016. We present the search strategies in Appendix 1. We modified the search strategy, subject headings, and syntax to each database and searched the following databases.
Cochrane Central Register of Controlled Trials (CENTRAL; 2016; Issue 7), part of the Cochrane Library.
MEDLINE Ovid (from 1946).
PubMed (from 1946).
Embase Ovid (from 1974).
PsycINFO Ovid (from 1806).
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; from 1981).
ERIC EBSCO (from 1966).
SweMed+ (from 1977).
ISI Web of Science (from 1987).
After merging the databases from each search into the reference management software Endnote 2015, the librarian removed studies retrieved in duplicate.
Searching other resources
We screened related systematic reviews, as found in the scoping search, for relevant primary studies. We also conducted cited reference searches for all included studies using ISI Web of Knowledge and screened their reference lists.
Trial registries
We searched the following websites to 19 October 2016.
WHO International Clinical Trials Search Portal (http://apps.who.int/trialsearch).
ClinicalTrials.gov (http://clinicaltrials.gov).
Grey literature
We searched the following websites to 19 October 2016.
OpenGrey (www.opengrey.eu).
Grey Literature Report (www.greylit.org).
Eldis (www.eldis.org).
Data collection and analysis
Selection of studies
Two review authors screened titles and abstracts independently (AM with either IBL or GEV). We retrieved the full text of all potentially relevant studies. Two review authors (AM with either IBL or GEV) independently assessed these for eligibility using a checklist. At each stage, we resolved any disagreement by discussion or consensus with a third review author. The project group read articles in English, Scandinavian languages and German. Staff members at the Norwegian Institute of Public Health read other languages or considered them for translation. We list the studies excluded based on full‐text assessment in the Characteristics of excluded studies table.
Data extraction and management
We extracted data using a form based on the Data Extraction and Assessment Template from the Cochrane Public Health Group (CPHG). This data extraction form embeds items relating to the PROGRESS‐Plus criteria and the PRISMA‐Equity 2012 Extension (Tugwell 2010; Welch 2012). We revised the form before data extraction. One review author retrieved the specified information and data from the included studies, and another review author checked data extraction. We resolved any disagreements by discussion or consensus with a third review author. We contacted the study authors if key information was missing. We entered the extracted data into RevMan 2014 as appropriate.
When more than one publication referred to the same study, we used the relevant paper with the most comprehensive and clear description of methods and outcome reports from a peer‐reviewed journal as the primary reference. If necessary, we used all papers from one study to extract the relevant information. We contacted investigators in cases of contradiction or incomplete reporting.
In addition to the items from the Data Extraction and Assessment Template, which included descriptions of study details (reference, design), participants, setting, intervention, outcomes, and adverse outcomes, we also extracted the following information when available.
Context of the intervention (sociodemographic, organisational, political, media structure).
Content of the message (health behaviour targeted).
Theoretical basis of the intervention, including message development and framing.
Theoretical basis for how the intervention and message were adapted to the target population.
Media channel(s) used for delivery and frequency of exposure.
Intervention fidelity (whether the intervention was delivered as planned).
Information on the nature and extent of any additional actions given as part of the intervention (co‐interventions).
Intervention costs.
Source of funding.
We present these data in the Characteristics of included studies section.
Assessment of risk of bias in included studies
Two review authors independently assessed the included studies with respect to risk of bias (AM, GEV). We assessed all study designs using the suggested 'Risk of bias' criteria for EPOC reviews (EPOC 2015). There are nine standard criteria for RCTs, cluster‐RCTs, NRCTs, and CBAs: adequate generation of allocation sequence; adequate allocation concealment; similar baseline outcome measurements; similar baseline characteristics; adequate handling of incomplete outcome data; adequate prevention of knowledge of the allocated interventions during the study; adequate protection against contamination; freedom from selective outcome reporting; and other risks of bias. For ITS studies we considered the following criteria: intervention independent of other changes, shape of the intervention effect pre‐specified, intervention unlikely to affect data collection, knowledge of the allocated intervention adequately prevented during the study, incomplete outcome data adequately addressed, study free from selective outcome reporting, and any other risks of bias. We resolved any disagreement in the assessment between the two review authors by discussion. We assessed the likely magnitude and direction of the bias on the findings.
Measures of treatment effect
If possible, we presented continuous outcomes with mean difference and standard deviations. When studies had measured the same outcome using different instruments or scales, we considered combining the outcomes using the standardised mean difference. We did not consider any of the outcomes to be appropriate for such a combination. For dichotomous outcomes, where available from RCTs, cluster‐RCTs, NRCTs, and CBA studies, we intended to present the number of events and number of people in groups as proportions and if appropriate, express effect as relative risk ratio (RR) or odds ratio (OR) with 95% confidence intervals (CIs).
For ITS studies, we present the effect as the difference between the expected value at a given point in time based on the pre‐intervention trend and the expected value at the same point in time based on the postintervention trend. We contacted authors of Kennedy 2013, who provided the original data set for re‐analysis as an ITS for this review as described in EPOC 2013.
We present results from randomised studies, non‐randomised studies and ITS separately, as recommended (Higgins 2011). We present the follow‐up according to our predefined categories: short‐term (< six months) and long‐term ( ≥ six months) follow‐up. Where study authors report several follow‐up times from the same study, we present the longest follow‐up.
Unit of analysis issues
Unit of analysis error can occur if trials based on group allocation to treatment condition (cluster‐RCTs, NRCTs, and CBA studies) have not accounted for the effect of clustering in the statistical analyses. The included cluster‐RCT by Boyd 1998 did not adjust the results for the effect of clustering, while Jih 2016 did. We did not have sufficient information to re‐analyse the data by Boyd 1998. See Appendix 2 for the methods we intended to use.
Dealing with missing data
We consider that incomplete or missing data was not a problem in any of the included studies and thus did not contact any of the authors for such information. See Appendix 2 for the methods we intended to use.
Assessment of heterogeneity
We did not combine data in meta‐analysis and hence did not assess heterogeneity in the results. See Appendix 2 for the methods we intended to use.
Assessment of reporting biases
We planned to generate funnel plots if 10 or more studies reported the same outcome. See Appendix 2 for the methods we intended to use.
Data synthesis
We categorised the included studies according to the intervention, measures and comparisons made. We assessed results for each comparison and collated them separately. If population, study design, intervention, and outcome measures had been similar enough across studies, we could have conducted meta‐analyses using Review Manager 5 (RevMan) software (RevMan 2014). One comparison had only one included study. Otherwise, the interventions, outcome measurements, or study designs differed in ways that did not support meta‐analyses. We based our judgements on the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We considered that one outcome had sufficiently homogeneous populations, interventions, and comparisons to consider a pooled risk ratio, but only one of these two studies reported a measurement of dispersion in the published paper. See Appendix 2 for the methods we intended to use for meta‐analyses. Since meta‐analysis was not appropriate, we present descriptive data in text and tables. Authors of Kennedy 2013 provided data so we could re‐analyse these results as an ITS through segmented time series regression (Ramsay 2003).
Subgroup analysis and investigation of heterogeneity
The included studies did not provide sufficient data for subgroup analyses or investigation of heterogeneity. See Appendix 2 for the methods we intended to use and planned subgroups.
Sensitivity analysis
We intended to perform a sensitivity analysis excluding studies at high risk of bias if there had been a sufficient number of included studies; see Appendix 2.
Summary of findings table
We present the main outcome measures in a 'Summary of findings' table, along with our assessment of the certainty of effect for each outcome using the GRADE methodology (Guyatt 2011). Using GRADE, we reflect on the extent to which we have confidence that the estimates of effect are correct. Our confidence is presented as either high, moderate, low or very low quality evidence. We assess the results for each outcome measure against eight criteria. We consider the first five criteria for possible downgrading of the quality of documentation: study quality (risk of bias), consistency (consistency between studies), directness (the same study participants, intervention, comparator and outcome measures in included studies for the population, measures and outcomes we wanted to study), precision of results, and reporting biases. Results can be upgraded by three criteria: strong or very strong associations between intervention and outcome; large or very large dose‐response effect; and situations where all plausible confounders would have reduced the effect.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
Searches in the electronic databases identified 12,762 unique records (see Figure 2: Study flow diagram). We discovered six additional records through other sources. Based on screening of titles and abstracts, we excluded 12,636 records and retrieved the full text of 132 articles, excluding 124. Six studies (8 articles) were eligible for this review. We did not identify any ongoing studies.
2.
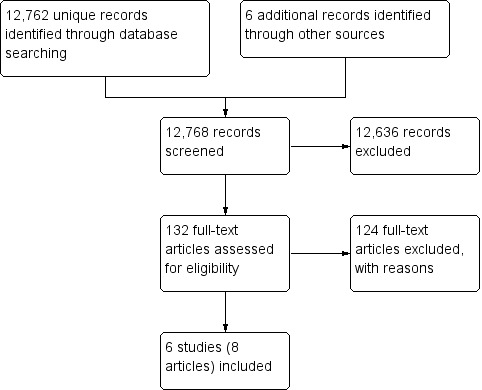
Study flow diagram.
Included studies
Of the included studies, three were individual RCTs (Elder 2005; Webb 2009; Risica 2013), and two were cluster‐RCTs (Boyd 1998; Jih 2016). We obtained the original data from the authors of Kennedy 2013 and were able to re‐analyse this study as an ITS. All of the studies took place in the USA and were published between 1998 and 2016. In four studies, the interventions targeted groups self‐described as Americans of African heritage (Boyd 1998; Webb 2009; Kennedy 2013; Risica 2013), while Elder 2005 targeted Spanish‐language‐dominant Latino immigrants (95% born in Mexico), and Jih 2016, elderly people of Chinese ethnicity (predominantly foreign‐born). Three studies targeted women only (Elder 2005; Kennedy 2013; Risica 2013). In Boyd 1998 and Kennedy 2013, the entire populations of geographically defined areas were potentially exposed to the targeted mass media intervention. The objectives of the interventions were to promote smoking cessation (Boyd 1998; Webb 2009; Kennedy 2013); to encourage dietary changes (particularly regarding fibre and fat intake) (Elder 2005); to promote weight management through modifications to diet and physical activity (Risica 2013); or to increase vegetable intake, fruit intake, and physical activity levels to meet guidelines (Jih 2016). None of the studies examined alcohol intake.
Webb 2009 recruited 261 African American adults who were randomised to receive either a culturally specific smoking cessation booklet or a booklet intended for the general population. The booklet in the intervention arm was culturally adapted using values, communication patterns, statistics, pictures, and other elements considered relevant for the targeted population, and it contained information about smoking and quitting strategies. The booklet used for the control group was identical in format and content and was developed by removing any references to a specific population group and using more general information and graphics.
In Boyd 1998 and Kennedy 2013, the intervention consisted of paid radio advisements, and in Boyd 1998, also some television advertisements, aired repeatedly in two waves that varied from three to six weeks in length. Both studies also included substantial distributions of posters, flyers, and other types of small media. The investigators targeted African American communities by adapting their message, language, and format to the assumed preferences of the group and by user‐testing the intervention with the target population. Advertisements were aired through media channels popular with the target audience or placed in relevant residential areas. The comparator in both studies was no intervention. The main message was to quit smoking and to make use of free telephone smoking cessation information or counselling (quit lines). Calls to this service were also the studies' outcome measurement. Since these studies exposed whole populations to the intervention, the study populations were not fixed. Boyd 1998's targeted mass media intervention was run in seven communities (estimated 310,471 African American smokers), compared to no intervention in seven communities (estimated 331,360 African American smokers). The size of Kennedy 2013's target population was indicated by the 400 births per month among African American women in the catchment area and survey results showing that approximately 40% of pregnant women in this population group were recent smokers.
The study by Risica 2013 gave study participants access to 12, one‐hour live programmes on cable TV over three months, biweekly mailings with printed material corresponding to the shows and, afterwards, four monthly mailings with written material and booster videotapes. The material was culturally adapted based on formative research on the target population. The TV shows had African American female casts, including all experts used. The shows and material contained educational content regarding nutrition and physical activity to improve health and control weight. In total, 71 women received this targeted intervention compared to 82 women on a wait‐list control until the study ended. Another 214 women received both this targeted intervention and the opportunity to engage in personal contact with study staff, either access to a toll‐free number they could use to ask questions during the live‐sharing segments of the shows, and/or weekly telephone support calls with outreach educators. Thus, this study compared the targeted mass media intervention with both a no‐intervention control group and a group receiving the mass media intervention with additional personalised content.
The target mass media intervention in Elder 2005 comprised newsletters in Spanish, mailed to the participants' home (119 women). The targeted newsletters and activity inserts were based on off‐the‐shelf information material developed for the Latino population and contained suggested strategies to change food purchasing, food preparation, and food consumption to reduce the risk of NCDs. This targeted intervention was compared to personalised newsletters and activity inserts in Spanish that were based on baseline questionnaires and specified personal goals. The personalised newsletters (118 women) otherwise focused on the same dietary messages as the targeted materials. A third intervention group (120 women) received both the personalised newsletters and 12 weekly visits by a Spanish‐speeking lay health worker (LHW, called promotora) who reinforced the dietary messages. Similarly, Jih 2016 compared targeted lecture handouts and brochures in 357 participants to the same material delivered through two small‐group, LHW‐facilitated lectures in 361 participants. The main aim was to increase fruit and vegetable intake and physical activity levels to meet guidelines. The researchers developed the lectures and materials using culturally appropriate examples of common foods, relevant physical activities and familiar portion size models for the target group. The lectures were presented in the participants' preferred language (Cantonese, Mandarin, or English).
Figure 3 presents an overview of the strategies that the included studies used to adapt their interventions to the target populations. The strategies are categorised according to the logic model (Figure 1). All of the studies made adaptations to modify message appropriateness, including adapting the message to be culturally appropriate, using selected images or cultural expressions, user‐testing the intervention in the target group, or attempting to address unique barriers and facilitating factors for group change. Two campaigns were implemented in a real context and made adaptations to modify reach by using selected media channels, placing small media in residential areas, distributing outreach packets through community networks, and using people from the target group to convey the media content (Boyd 1998; Kennedy 2013). Two studies presented the mass media interventions in languages that differed from the dominant language of the country (Elder 2005, Jih 2016).
3.
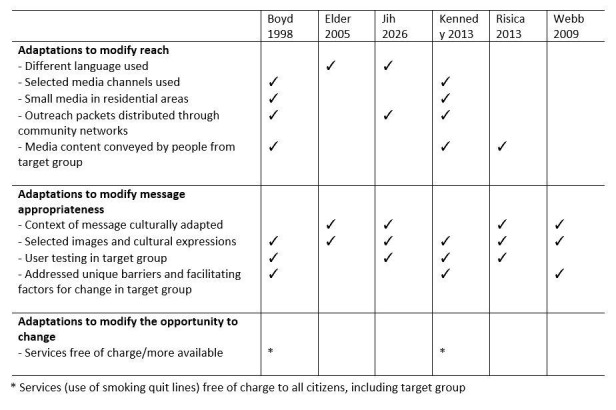
Approaches used in the included studies to target the intervention to the study population, by categories according to logic model.
Three of the included studies received support from the National Cancer Institute (USA) (Boyd 1998; Elder 2005; Risica 2013), and one received funding from both the National Institutes of Health and the National Cancer Institute (Jih 2016). The National Center on Minority Health Disparities, part of the National Institutes of Health (USA), supported Kennedy 2013, and Syracuse University (USA) funded Webb 2009.
Excluded studies
After screening the full texts, we excluded 124 articles (see Characteristics of excluded studies). The main reasons for exclusion were: no mass media intervention or combining the media various forms of personal interaction with the participants; not targeting the intervention to ethnic minorities; or not meeting the inclusion criteria with respect to study design.
Risk of bias in included studies
The Characteristics of included studies table assesses the risk of bias and provides comments for each of the included studies. We used the study‐appropriate risk of bias domains as developed by EPOC 2015, which proposes different domains for assessing ITS studies and the other study designs included in this review. The risk of bias assessment for the ITS study is discussed under the section Other potential sources of bias. Figure 4 and Figure 5 summarise the 'Risk of bias' assessments. These figures present all domains used for both the ITS study and the other study designs but are only filled in for the appropriate categories for each study.
4.
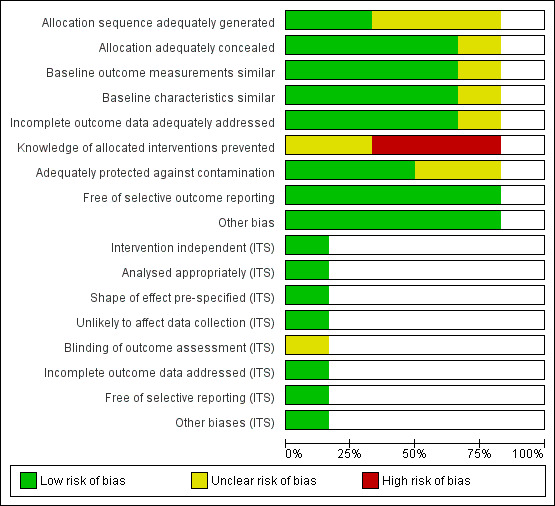
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
5.
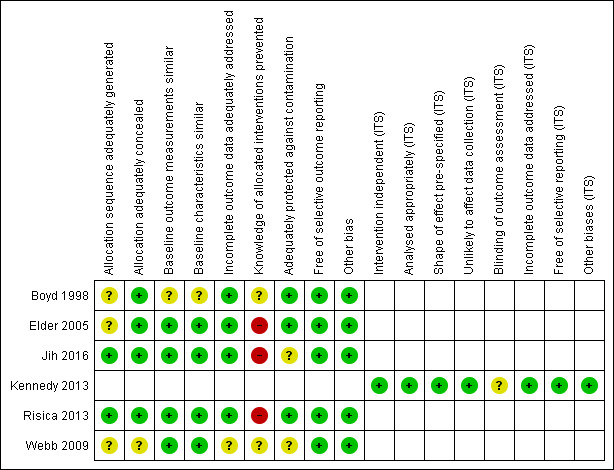
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Two studies reported adequate methods for random sequence allocation (Risica 2013; Jih 2016). Otherwise, the allocation method described in the papers was unclear. We also considered that the method used for allocation concealment in Webb 2009 was at unclear risk of bias. Four studies presented data showing that the groups were similar at baseline with regard to the outcome variables and the participant characteristics (Elder 2005; Webb 2009; Risica 2013; Jih 2016). In Boyd 1998, the communities were matched on selected characteristics before randomisation, but based on the published descriptions we found the distribution of the baseline characteristics to be unclear.
Blinding
It can be difficult to achieve blinding in studies intending to change behaviours. Since most or all the outcomes in Elder 2005, Risica 2013, and Jih 2016 were self‐reported outcomes from non‐blinded studies, we considered these results to be at high risk of bias. In Webb 2009, participants in both study arms received a non‐blinded smoking cessation intervention; we could not tell whether the trial misreported any of the study outcomes with unequal distribution between the groups. Kennedy 2013 reported on a whole‐population mass media campaign, and we considered it to be unclear whether knowledge of the allocated intervention was adequately prevented during the study and in what way this may have biased the findings.
Incomplete outcome data
Loss to follow‐up was unaccounted for in Webb 2009, so we consider the risk of bias to be unclear.
Selective reporting
We found no published study protocols for any of the studies but considered the risk for selective reporting of outcomes to be low in all the studies. This conclusion is based on descriptions in the Methods, expected outcomes reported, and corresponding presentations of results.
Other potential sources of bias
We considered the included studies to be at low risk of other biases.
We re‐analysed Kennedy 2013 as an ITS for this systematic review using the methodology described above. We noted that the second wave of advertisements coincided with a known seasonal increase in call volume and therefore excluded these data from the re‐analysis. We considered the remaining results, as re‐analysed according to the EPOC methods for ITS studies, to be at low risk of bias in all domains except one. As with the study by Boyd 1998, it was unclear whether knowledge of the allocated intervention in Kennedy 2013 (whole population mass media campaign) was adequately prevented during the study and in what way this may have biased the findings.
Effects of interventions
See: Table 1; Table 2; Table 3
Comparison 1: targeted mass media intervention versus general population mass media intervention
See: Table 1.
Only one study assessed the effect of a targeted mass media intervention versus a mass media intervention intended for the general population (Webb 2009).
Primary outcomes
Webb 2009 did not assess any outcomes using indicators of behavioural change but reported several self‐reported measures, including smoking reduction, attempts to quit, 24‐hour point prevalence abstinence and 7‐day point prevalence abstinence. The authors report that they found no significant difference in smoking reduction between the two conditions at the three‐month follow‐up (94% and 95% reported smoking reduction; adjusted OR for quit attempts was 1.97 (95% CI 1.09 to 3.55) in favour of the general population mass media intervention). Knowledge and attitudes toward change were reported as readiness to quit, measured by a 10‐point contemplation ladder (1: no thoughts of quitting; 10: taking action to quit). The mean score was higher in participants who received the mass media intervention intended for the general population compared to the targeted mass media intervention (8.2 points, SD 2.4 versus 7.3 points, SD 2.6, P = 0.01). We considered all effect estimates of these self‐reported behavioural outcome measures to be very low quality evidence as assessed by the GRADE methodology.
Secondary outcomes
The included study did not assess any outcomes on the use of health promotion services or costs of the project.
Adverse outcomes
The included study did not assess any variables measuring adverse outcomes.
Comparison 2: targeted mass media intervention versus no intervention
See: Table 2.
Three studies compared targeted mass media interventions versus no intervention (Boyd 1998; Kennedy 2013; Risica 2013). We could not pool the findings due to differences in outcome measurements and study designs.
Primary outcome
Only one of the included studies reported any of our primary outcomes (Risica 2013). These were: BMI (kg/m2) as an indicator of behavioural change and self‐reported behavioural change using a Food Habits Questionnaire (fat behaviour score) and total leisure activity questionnaire. The included study did not assess knowledge or attitudes toward change.
Changes in BMI were comparable in the two groups 12 months after baseline (longest follow‐up, mean difference in change 0.1 kg/m2, 95% CI −0.4 to 0.6). Fat behaviour scores (no unit described, high scores reflecting high fat intake) were lower in participants who received the targeted mass media intervention compared to the no intervention control group at 12 months (longest follow‐up, mean difference in change −0.2, 95% CI −0.3 to −0.1), while total leisure activity score (no unit described, high scores reflecting more activity) was higher in the intervention group (longest follow‐up, mean difference in change 12.0, 95% CI 1.0 to 23.0). We considered the effect measures based on the outcome BMI to be low quality evidence and the self‐reported behavioural changes to be very low quality evidence.
Secondary outcomes
Two studies reported our secondary outcome: use of health promotion services – in both cases as the number of calls to smoking quit lines (Boyd 1998; Kennedy 2013). During the year of the campaign by Boyd 1998, the quit lines received 558 calls from African American smokers residing in the intervention communities (18 calls per estimated 10,000 African American smokers) compared to 7 calls in the control communities (0.2 calls per estimated 10,000 African American smokers). The proportion of calls from African Americans was 82% of the total number in the experimental communities compared to 26% in the control communities (no measure of dispersion reported). Calls peaked significantly during waves of intense media coverage. We present the re‐analysis of Kennedy 2013 as an ITS for this systematic review in Table 4. During the first and the last month of the campaign, the number of calls from new pregnant women increased by 8 per month (95% CI 1 to 14) over pre‐campaign call rates. Compared to the pre‐campaign monthly call rate, the number was 6 more calls (95% CI −1 to 12) in the first month after the campaign and 3 more calls (95% CI −4 to 10) four months after. The proportion of calls from African American women was 86% during the campaign, compared to 41% before the campaign and 28% after (no measure of dispersion reported). We considered the overall results measured as changes in call volume overall to be moderate quality evidence based on results from the RCT and low quality evidence from the ITS. The change in the proportion of calls from the target population provided low and very low quality evidence from the two respective studies.
1. Re‐analyses of data from Kennedy 2013.
| Outcome | Estimated effect (95% CI)a July 2009 (start of campaign) | Estimated effect October 2009 (last month of campaign) | Estimated effect November 2009 (first month after campaign) | Estimated effect March 2010 (4 months after campaign) |
| Total number of calls | 42 (−115 to 198) | 153 (−8 to 314) | 146 (−13 to 304) | 32 (−148 to 212) |
| Calls from pregnant women | 14 (4 to 25) | 15 (4 to 27) | 8 (−3 to 19) | 7 (−5 to 20) |
| Calls from unique pregnant women | 8 (1 to 14) | 8 (1 to 14) | 6 (−1 to 12) | 3 (−4 to 10) |
| Calls from unique previously unknown pregnant women ('first‐timers') | 6 (1 to 11) | 6 (1 to 10) | 2 (−3 to 6) | 3 (−3 to 8) |
aChange from pre‐campaign call rates.
Kennedy 2013 and Risica 2013 did not report the costs of their projects. Boyd 1998 reported the costs to be USD 106,821 for radio advertisements and USD 6744 for television advertisements but did not mention other costs or required resources overall.
Adverse outcomes
The included studies did not assess any variables measuring adverse outcomes.
Comparison 3: targeted mass media intervention versus targeted media intervention plus personalised content
See: Table 3.
Comparison 3 examined targeted mass media interventions versus targeted media interventions plus personalised content and included data from three studies (Elder 2005; Risica 2013; Jih 2016). Elder 2005 compared a targeted mass media intervention (newsletters based on off‐the‐shelf targeted material) with two intervention arms categorised as media intervention plus personalised content: one arm received individually tailored newsletters, and the other arm received individually tailored newsletters followed by home visits. Risica 2013 had three intervention arms that we categorised as media intervention plus personalised content. The authors reported incomplete delivery of the interactive programme sessions and support calls in these intervention arms; therefore, tor the purpose of this systematic review, we combined the results of these three intervention arms into a single comparison group. Jih 2016 compared a targeted mass media intervention (targeted print material) with a mass media intervention plus personalised content (lectures).
Primary outcomes
Elder 2005 and Risica 2013 reported BMI an as indicator of behavioural change at 3 months and Risica 2013 also at 12 months from baseline. Neither reported any difference in BMI change over time. Mean difference in change between the groups 12 months after baseline was 0.4 kg/m2 (95% CI −0.1 to 0.8) between groups. All three included studies assessed self‐reported behavioural changes. At three months, participants in Jih 2016 who received media interventions plus personalised content had higher odds of adhering to guidelines on vegetable intake than participants who received targeted mass media alone (adjusted OR 5.53, 95% CI 1.96 to 15.58), but there was no difference for fruit intake (adjusted OR 1.77, 95% CI 0.99 to 3.15). Risica 2013 assessed self‐reported behavioural changes using a Food Habits Questionnaire (fat behaviour score) and a total leisure activity questionnaire, as above, while Elder 2005 used a 24‐hour dietary recall interview. Their papers present results for several nutrients and groupings, but in this review we present only the authors' main outcomes: percentage of calories from fat and total dietary fibre (g). Elder 2005 reported no significant differences (P > 0.05) at the end of the intervention between the tailored intervention group and the two comparison groups for either percentage of calories from fat (30.0%, 30.4%, and 29.3%; no measure of dispersion reported) or total dietary fibre (15.6 g, 17.2 g, and 16.1 g; no measure of dispersion reported). In Risica 2013, the participants who received only the targeted mass media intervention had somewhat larger reductions in fat behaviours scores (no unit described, high scores reflecting high fat intake, mean difference in change −0.1, 95% CI −0.2 to −0.02) and greater increases in total leisure activity score (no unit described, high scores reflecting more activity, mean difference in change 12.9, 95% CI 3.5 to 22.3) compared to the groups with additional personalised components after 12 months. In Jih 2016, results indicated no difference in weekly physical activity meeting guidelines (adjusted OR 1.27, 95% CI 0.89 to 1.80). The same study indicated that more participants receiving personalised content had increased knowledge of nutrition guidelines than participants receiving the targeted mass media alone (knowledge of guideline for vegetables, adjusted OR 12.6, 95% CI 6.5 to 24.5, and fruit, adjusted OR 16.2, 95% CI 5.6 to 46.5), but this finding did not hold for knowledge of physical activity guidelines (adjusted OR 2.70, 95% CI 0.31 to 23.2).
We considered the effect measures based on the outcome BMI to be low quality evidence and all self‐reported behavioural changes and knowledge of guidelines to be very low quality evidence.
Secondary outcomes
The included studies did not assess any outcomes concerning the use of health promotion services. Elder 2005 reported that the costs per participant in the three intervention arms were USD 9.00 for targeted newsletters, USD 45.00 individually tailored newsletters, and USD 135 for individually tailored newsletters followed by home visits. Jih 2016 and Risica 2013 did not report project costs.
Adverse outcomes
The included studies did not assess any variables considered adverse outcomes.
Discussion
Summary of main results
Six studies met the inclusion criteria: three RCTs, two cluster‐RCTs, and one ITS. All took place in the USA and consisted of mass media interventions targeting either African Americans (4 studies), Spanish‐language‐dominant Latino immigrants (1 study) or Chinese immigrants (1 study). Furthermore, three targeted women only, and one specifically targeted pregnant women. The interventions addressed physical activity, dietary patterns, or tobacco use, but none addressed alcohol consumption. The studies were diverse with respect to the comparisons made, the outcomes and the study designs. We did not pool data for meta‐analyses.
We categorised the comparisons into three groups: a targeted mass media intervention versus a general mass media intervention; a targeted mass media intervention versus no intervention; and a targeted mass media intervention versus a media intervention plus personalised content.
Only one study compared the relative effects of a culturally targeted mass media intervention and a general mass media intervention on smoking behaviours. The results were inconclusive.
Two studies compared the relative effects of a targeted mass media intervention versus no intervention. The findings suggested that, compared to no intervention, the targeted mass media intervention possibly produced small, short‐term shifts in physical activity and dietary patterns and probably increased calls to smoking quit lines.
Three studies compared a targeted mass media intervention versus a media intervention combined with personalised content. Overall, the results of these studies were too uncertain to conclude whether there were differences between groups with respect to weight changes, dietary changes, or physical activity. Most of the outcomes had either small effects or inconclusive confidence intervals, and the evidence of effect was low to very low quality.
Overall completeness and applicability of evidence
Given the widespread interest in mass media interventions targeting ethnic minority populations with health‐promoting messages regarding physical activity, dietary patterns, tobacco use, or alcohol consumption, the number of relevant studies was small. Only one study, Webb 2009, directly compared the effect of a culturally targeted mass media intervention with the effect of a general mass media intervention using the same format (i.e. smoking cessation advice and general content). The targeting did not involve any change in language use. In the included study, the delivery methods and, therefore, the expected reach were the same between groups. Although this comparison focuses on the value and effectiveness of targeting strategies on their own, the included study only assessed the value of targeting through cultural adaptation. The study was inconclusive regarding the differential effects on smoking behaviours and attitudes. We have very little confidence in the effect estimates and believe that any true effect could be substantially different from the authors' reports. Thus, the evidence is insufficient to conclude whether targeted mass media interventions are more effective than mass media interventions intended for the general population in changing health behaviours among ethnic minority groups.
When comparing the effects of targeted mass media interventions versus no interventions, findings from two large campaigns showed that these probably produce a considerable response, as measured by a surrogate outcome: the use of health promotion services in the form of smoking quit lines (Boyd 1998; Kennedy 2013). These studies did not measure changes in actual smoking behaviours. Calling a smoking quit line may not lead to an actual change in smoking habits or to long‐term smoking cessation. Population‐wide campaigns, such as those reported here (Boyd 1998; Kennedy 2013), may, however, contribute to population changes in attitudes toward smoking, intentions to quit, self‐administered attempts to quit, or use of other health services offering smoking cessation support, thereby providing additional effects through the measured outcomes. Self‐reported changes in behaviours are, when sustained, important outcomes in causal pathways (see Figure 1); however, they are not the ultimate aim, which is to improve health status and decrease the mortality and morbidity of NCDs. The one study in this comparison that measured a physiological indicator of change (BMI), using self‐reported changes in dietary patterns and physical activity, found small effects in the expected direction after three months (the end of the main intervention). The longer‐term effects were more uncertain (Risica 2013). It should be noted that this targeted mass media intervention was relatively high‐intensity, comprising 12, one‐hour live cable TV programmes over three months, with additional mailings over an extended period. The measured effect size was relatively small, and we have low to very low confidence in the effect estimates.
All three studies in this comparison targeted population groups with the same native language as the general population. During the campaigns, these studies also registered smaller or larger increases in call rates in non‐targeted population groups (Boyd 1998; Kennedy 2013). However, the relative shifts in the proportions of callers, as well as the increases in total numbers of calls from the target populations, still indicate that these interventions had specific effects on the intended population group. These results cannot distinguish whether higher responses by the target population were due to the targeting of media content and format, better reach through the targeting of media channels, or both.
Overall, the three studies comparing a targeted mass media intervention with a media intervention plus personalised content were inconclusive (Elder 2005; Jih 2016; Risica 2013). It could be expected that person‐tailored or one‐to‐one intervention content would produce a better response than a mass media intervention alone. In two of these studies (Elder 2005; Risica 2013), all study arms had a relatively high exposure to the intervention, with at least 12 deliveries of mass media content over an extended period. Thus, the intervention groups may not have been sufficiently different to constitute a meaningful comparison.
All six studies in this systematic review were conducted in the USA, and four targeted African American population groups. Only two studies examined the effect of a targeted mass media intervention in a population group with a first language that differed from the national language (Spanish‐dominant Latino immigrants and Chinese immigrants). The current evidence is therefore very limited with respect to different ethnic groups and contexts beyond the USA. Additionally, the cultural gap between the populations considered minorities and majorities may be more or less wide. All of the studies adapted their interventions to the target group by culturally customising the content or format (Figure 3). It is unclear to what extent these adaptations also considered other relevant factors that may characterise the target group, such as gender or socioeconomic status related to income, education, health literacy level, living conditions, or other resources available to the target population. The transferability of the results from this review must be considered for each context specifically.
None of the studies reported or discussed possible adverse effects of the intervention. A targeted mass media intervention can be a means to provide ethnic minority groups with equal opportunities and resources to access information, life skills, and opportunities for making healthier choices; however, by treating the target group differently, targeted efforts may also create a stigma. Drawing attention to the need for additional public health efforts directed toward a particular population subgroup may, in some situations, be considered or experienced as discrimination (Nayar 2014). Different population segments may also experience public health efforts to change personal behaviours as more or less intrusive or unacceptable to their rights to personal freedom. None of the included studies reported resistance to the message or other possible adverse effects as outcomes.
Targeted interventions are considered to be more expensive; however, this may not be universally true. Though the production of a targeted intervention or several adapted versions of the same intervention for different population groups may increase programme costs, the budget upside of a targeted intervention may be the need for fewer or potentially less costly media channels to reach the target group. Furthermore, new digital media channels have significantly changed the picture of media costs. This can make it easier to target specific groups at a low cost, but the new diversity in media markets can also create more 'noise' and increase reach dispersion. Overall, research still needs to explore the cost aspects of targeted interventions.
Quality of the evidence
In the GRADE assessments for the domain 'directness' (Guyatt 2011), we considered the studies directly relevant to the inclusion criteria. Thus, we did not downgrade quality for this domain. The population of interest, and therefore also the directness of these findings, will be dissimilar in different contexts, relating to characteristics of the ethnic minority group, the country, and the overall setting.
Based on the GRADE methodology (Guyatt 2011), we have moderate confidence in the estimated short‐term increase in the number of calls to smoking quit lines. The cluster‐RCT reporting this outcome did not provide measures of dispersion or adjust for effects of the cluster‐randomised design (Boyd 1998). Failing to adjust for cluster effects will overestimate the precision of the effect estimate. However, the study reported a large effect, and additional results from the ITS study had similar conclusions (Kennedy 2013). Otherwise, our confidence in the described effect sizes ranged from low to very low. A low to very low confidence in the evidence means that the true effect can be either different or substantially different from the numbers presented in this review.
Potential biases in the review process
In this review, we focused on the effect of targeted mass media interventions on their own. This means that we have excluded targeted mass media interventions that were combined with any form of personal interaction or feedback (including digital feedback), group sessions, or changes in available resources. We also excluded studies in which a mass media component was part of a complex community intervention involving many intervention activities across several institutions. The only exceptions were studies in which this type of complex intervention served as a comparator for a targeted mass media intervention alone (Elder 2005; Risica 2013; Jih 2016). A boundary that we found difficult to operationalise was the distinction between a mass media intervention and a self‐help programme. We included Webb 2009, where the intervention was a smoking cessation booklet, while we excluded more extensive self‐help programmes with teaching modules and worksheets.
Inclusion criteria regarding study design were based on recommendations from the EPOC group (EPOC 2016). These criteria are well reasoned and include several different study designs but are slightly narrower than those used in other Cochrane Reviews on mass media interventions for smoking cessation. We excluded a few studies that Bala 2013 included, as we used different inclusion criteria regarding study designs; however, we believe that the inclusion of their studies would not have altered our conclusions.
Agreements and disagreements with other studies or reviews
We have not found any other systematic reviews regarding the specific effects of mass media interventions targeting adult ethnic minorities with health promotion messages. One mixed‐methods evidence synthesis identified and assessed the effects of adapted health promotion interventions for ethnic minority populations of African, Chinese, and South Asian origin (Liu 2012). They identified only nine studies (among them Webb 2009, included in our review) directly comparing a culturally adapted health promotion intervention with a standard intervention of equal format, intensity and content. The included studies did not indicate any tendency toward increased effectiveness for culturally adapted interventions. The studies were either inconclusive (k = 5) or found increased effectiveness in the opposite direction of the hypothesis on some outcome variables (k = 3). Only one study found increased effectiveness of the culturally adapted intervention over the standard intervention. All nine studies were conducted in the USA, and eight targeted African Americans. The review authors of Liu 2012 considered that most studies considered in the evidence synthesis were inappropriately designed to establish the effectiveness of the cultural adaptations. Another Cochrane Review, focusing on culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus, found that such education likely improves glycaemic control compared to standard diabetes care. Here, the contexts and the targeted ethnic minority groups were more variable, including several studies of programmes targeting immigrants. Many of the diabetes education programmes in that review were more comprehensive than their standard care counterparts in terms of counselling frequency, personal interaction, and other intervention components (Attridge 2014). Another review found that cultural adaptations resulting in higher‐intensity health promotion interventions appeared to be more effective (Nierkens 2013). However, these reviews also failed to scrutinise the specific effect of the cultural adaptations to the ethnic minority group. Reviews and guidelines increasingly acknowledge ethnic health inequalities and the possibility of differential effects of health promotion interventions (Davidson 2013a). Recommended adaptation strategies can be derived based on current strategies in use; however, there is still little evidence regarding which health promotion interventions are effective for ethnic minority populations (Davidson 2013b).
Of the studies included in our review, three compared targeted mass media interventions to no intervention. Their findings contribute more to the general evidence regarding the effectiveness of mass media interventions addressing health behaviours to reduce the risk of NCDs. In two of the included studies, the interventions were mass media campaigns for smoking cessation. The effectiveness of mass media interventions for smoking cessation is also addressed in two Cochrane Reviews: Bala 2013 in adults and Brinn 2010 in young people (up to age 25). These conclude that there is evidence of some positive effect of these interventions on smoking behaviours, at least in the short term.
Authors' conclusions
Implications for practice.
The evidence is insufficient to determine whether targeted mass media interventions are more effective than mass media interventions intended for the general population for changing health behaviours in ethnic minority populations (based on very low quality evidence; Table 1). It is uncertain whether, compared to no intervention, targeted mass media interventions may slightly improve physical activity and dietary patterns and BMI in the short term (based on the low quality evidence of a small effect for this outcome; Table 2). The intervention may probably increase the number of calls to smoking quit lines during and immediately after campaigns (based on moderate quality evidence; Table 2). The studies in this comparison could not distinguish between the impacts of exposure to an intervention, cultural adaptation to an ethnic minority group, and choice of mass media channels to increase reach to the target group.
Implications for research.
Overall, there is also limited research on targeted mass media interventions physical activity, dietary patterns, and tobacco use. We found no studies fulfilling the inclusion criteria that assessed targeted mass media interventions regarding alcohol consumption.
Further research that is specifically related to the following aspects is necessary.
New studies should be designed to directly compare the effects of targeted versus general mass media interventions with equal intensities and broader frames. If possible, studies should be designed to explore how different components impact intervention effectiveness.
Studies from different contexts, involving different media structures and economic environments, and studies that target populations with a broader range of ethnic minority populations, particularly ethnic minority groups with different first languages than the general population. Studies should consider the impacts of socioeconomic factors, health literacy, and other contextual factors that may modify intervention reach and appropriateness.
Follow‐up times should be longer than the 3 to 12 months presented here, and outcomes related to measurements of behaviours and changes in health status should be prioritised. New studies should report study costs.
The included studies demonstrate that the research objective of this review can be investigated through rigorous study designs, such as individual and cluster‐RCTs, or on a population levels using ITS designs.
Acknowledgements
The study protocol and review have been informed by staff at the Norwegian Institute of Public Health/members of the Cochrane EPOC Group, in particular Marit Johansen (literature search) and Jan Oddgard‐Jensen (data collection and ITS re‐analysis). The Norwegian Directorate of Health and The Norwegian Cancer Society requested the review topic, and provided input on the objectives and framing of the Background section. We would like to thank the authors of Kennedy 2013 for providing the original data to re‐analyse their study as an ITS.
The advisory group members are:
Astrid Austvoll‐Dahlgren, the Norwegian Institute of Public Health;
Rigmor Berg, the Norwegian Institute of Public Health;
Arnfinn Helleve, the Norwegian Directorate of Health;
Jostein Rise, the Norwegian Institute of Public Health;
Hilde Skyvulstad, the Norwegian Directorate of Health;
Ingrid Stenstadvold Ross, the Norwegian Cancer Society.
Appendices
Appendix 1. Search strategies
Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present
Search date: 2016‐08‐23
1 exp communications media/ (266069)
2 consumer health information/ (2624)
3 exp Internet/ (61516)
4 exp marketing/ (32277)
5 (radio or television or "tv" or campaign* or advert* or boards or newspaper* or maga?in* or brochure* or leaflet* or pamphlet* or cinema* or (mass adj (communication or media)) or internet or social media or blog* or facebook or twitter or instagram or podcast* or broadcast* or audiovisual or film* or movie* or ((cell or cellular or mobile) adj (telephone* or phone*))).ti,ab. (320644)
6 (("cd" or "cds" or dvd or dvds or video or videos) adj3 distribut*).ti,ab. (866)
7 or/1‐6 [mass media] (611426)
8 exp drinking behavior/ (64839)
9 exp "tobacco use"/ (133790)
10 exp Food Habits/ (28170)
11 Motor Activity/ (89395)
12 exp exercise/ (144411)
13 exp physical fitness/ (24479)
14 exp sports/ (149201)
15 ((alcohol* adj2 (drink* or consumption)) or (drinking adj5 (behavio?r or habit*)) or nutrition* or diet* or food* or feed* or eating or meal or meals or ((physical or motor) adj5 (activ* or exercis*)) or physical conditioning or running or jogging or swimming or walking or skiing or cycling or climbing or smok* or tobacco* or cigarette*).ti,ab. (1662747)
16 or/8‐15 [behavior] (1895646)
17 Minority Groups/ (11887)
18 Minority Health/ (579)
19 exp Population Groups/ (254763)
20 (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies).ti,ab. (217329)
21 (black or blacks or hispanic* or ((afro or african or asian or latin* or indian) adj1 american*)).ti,ab. (175176)
22 "Emigrants and Immigrants"/ (8064)
23 Refugees/ (7565)
24 cultural diversity/ (10143)
25 exp Human Migration/ (24328)
26 (refugee* or immigrant* or (asyl* adj1 seek*) or foreign* or ethnic* or minorit* or racial* or (multi adj cultural*) or multicultural* or (newly adj arrived) or ((family or families) adj2 reuni*) or resettlement or (cultural adj1 (diversit* or pluralism))).ti,ab. (259123)
27 ((cultural* or language*) and (adapt* or accomodat* or approp* or target* or tailor*)).ti,ab. (40405)
28 or/17‐27 [minorities] (779859)
29 7 and 16 and 28 [mass media, behavior, minorities] (4397)
30 clinical trial.mp. (632942)
31 clinical trial.pt. (505164)
32 random*.mp. (1085945)
33 randomised controlled trial.pt. (428912)
34 controlled clinical trial.pt. (91593)
35 multicenter study.pt. (209949)
36 pragmatic clinical trial.pt. (406)
37 (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or (pre adj5 post)).ti,ab. (86623)
38 ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) adj3 (method* or study or trial or design* or controlled))).ti,ab,hw. (125460)
39 ("time series" or "time points").ti,ab,hw. (82704)
40 (effect or impact or trial or intervention).ti. (1148249)
41 repeated measure*.ti,ab. (34209)
42 ((before adj5 after) or control group*).ti,ab. (638655)
43 (pretest‐posttest study or pretesting or pre‐post tests or quasi experimental design or quasi experimental study or quasi experimental study design or repeated measurement or repeated measurements or repeated measures or time series).kw. (483)
44 Controlled Before‐After Studies/ (182)
45 Non‐Randomized Controlled Trials as Topic/ (77)
46 Interrupted Time Series Analysis/ (206)
47 or/30‐46 (3042682)
48 29 and 47 (1249)
Database: Embase 1974 to 2016 August 24
Search date: 2016‐08‐15
1 exp mass communication/ (429281)
2 consumer health information/ (2891)
3 exp multimedia/ (2863)
4 marketing/ (18599)
5 (radio or television or "tv" or campaign* or advert* or boards or newspaper* or maga?in* or brochure* or leaflet* or pamphlet* or cinema* or (mass adj (communication or media)) or internet or social media or blog* or facebook or twitter or instagram or podcast* or broadcast* or audiovisual or film* or movie* or ((cell or cellular or mobile) adj (telephone* or phone*))).ti,ab. (357025)
6 (("cd" or "cds" or dvd or dvds or video or videos) adj3 distribut*).ti,ab. (1078)
7 or/1‐6 (729956)
8 alcohol consumption/ (93490)
9 exp "tobacco use"/ (257714)
10 smoking cessation/ (45485)
11 exp feeding behavior/ (146067)
12 exp physical activity/ (294347)
13 exp exercise/ (259814)
14 fitness/ (33483)
15 exp sport/ (122407)
16 ((alcohol* adj2 (drink* or consumption)) or (drinking adj5 (behavio?r or habit*)) or nutrition* or diet* or food* or feed* or eating or meal or meals or ((physical or motor) adj5 (activ* or exercis*)) or physical conditioning or running or jogging or swimming or walking or skiing or cycling or climbing or smok* or tobacco* or cigarette*).ti,ab. (2047701)
17 or/8‐16 (2523625)
18 minority health/ (488)
19 exp "ethnic and racial groups"/ (102808)
20 exp "ethnic or racial aspects"/ (194153)
21 exp migration/ (40057)
22 refugee/ (8799)
23 exp population group/ (729630)
24 cultural anthropology/ (50115)
25 (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies).ti,ab. (243376)
26 (black or blacks or hispanic* or ((afro or african or asian or latin* or indian) adj1 american*)).ti,ab. (214006)
27 (refugee* or immigrant* or (asyl* adj1 seek*) or foreign* or ethnic* or minorit* or racial* or (multi adj cultural*) or multicultural* or (newly adj arrived) or ((family or families) adj2 reuni*) or resettlement or (cultural adj1 (diversit* or pluralism))).ti,ab. (312602)
28 ((cultural* or language*) and (adapt* or accomodat* or approp* or target* or tailor*)).ti,ab. (40343)
29 or/18‐28 (1408438)
30 7 and 17 and 29 (9946)
31 random:.tw. (1117293)
32 clinical trial:.mp. (1236961)
33 exp health care quality/ (2371751)
34 Randomized controlled trial/ (417044)
35 Quasi Experimental Study/ (3097)
36 Pretest Posttest Control Group Design/ (267)
37 Time Series Analysis/ (17373)
38 Experimental Design/ (12729)
39 Multicenter Study/ (142496)
40 (effect or impact or trial or intervention).ti. (1404932)
41 (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or (pre adj5 post)).ti,ab. (134214)
42 ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) adj3 (method* or study or trial or design* or controlled))).ti,ab,hw. (230820)
43 ("time series" or "time points").ti,ab,hw. (122771)
44 repeated measure*.ti,ab. (44685)
45 ((before adj5 after) or control group*).ti,ab. (850188)
46 (pretest‐posttest study or pretesting or pre‐post tests or quasi experimental design or quasi experimental study or quasi experimental study design or repeated measurement or repeated measurements or repeated measures or time series).kw. (3215)
47 or/31‐46 (5818497)
48 30 and 47 (3763)
49 limit 48 to embase (3055)
Database: PsycINFO 1806 to July Week 4 2016
Search date: 2016‐08‐25
1 exp mass media/ (36387)
2 exp multimedia/ (24893)
3 exp newspapers/ (2199)
4 exp telecommunications media/ (14503)
5 exp internet/ (25571)
6 exp marketing/ (18275)
7 (radio or television or "tv" or campaign* or advert* or boards or newspaper* or maga?in* or brochure* or leaflet* or pamphlet* or cinema* or (mass adj (communication or media)) or internet or social media or blog* or facebook or twitter or instagram or podcast* or broadcast* or audiovisual or film* or movie* or ((cell or cellular or mobile) adj (telephone* or phone*))).ti,ab. (119163)
8 (("cd" or "cds" or dvd or dvds or video or videos) adj3 distribut*).ti,ab. (71)
9 or/1‐8 (166518)
10 exp Alcohol Drinking Patterns/ (58564)
11 alcohol drinking attitudes/ (2773)
12 tobacco smoking/ (26156)
13 smoking cessation/ (10743)
14 eating behavior/ (9412)
15 food intake/ (13029)
16 food preferences/ (3941)
17 exp physical activity/ (30922)
18 running/ (1661)
19 swimming/ (1521)
20 walking/ (4306)
21 physical fitness/ (3644)
22 exp sports/ (20762)
23 ((alcohol* adj2 (drink* or consumption)) or (drinking adj5 (behavio?r or habit*)) or nutrition* or diet* or food* or feed* or eating or meal or meals or ((physical or motor) adj5 (activ* or exercis*)) or physical conditioning or running or jogging or swimming or walking or skiing or cycling or climbing or smok* or tobacco* or cigarette*).ti,ab. (319950)
24 or/10‐23 (388847)
25 minority groups/ (12258)
26 exp "racial and ethnic groups"/ (107691)
27 ethnic identity/ (13316)
28 immigration/ (17746)
29 exp human migration/ (9348)
30 cross cultural differences/ (46625)
31 (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies).ti,ab. (34290)
32 (black or blacks or hispanic* or ((afro or african or asian or latin* or indian) adj1 american*)).ti,ab. (100887)
33 (refugee* or immigrant* or (asyl* adj1 seek*) or foreign* or ethnic* or minorit* or racial* or (multi adj cultural*) or multicultural* or (newly adj arrived) or ((family or families) adj2 reuni*) or resettlement or (cultural adj1 (diversit* or pluralism))).ti,ab. (161507)
34 ((cultural* or language*) and (adapt* or accomodat* or approp* or target* or tailor*)).ti,ab. (41377)
35 or/25‐34 (339616)
36 9 and 24 and 35 (2227)
37 control*.tw. (567694)
38 random:.tw. (156723)
39 exp treatment/ (657106)
40 experimental design/ (10227)
41 between groups design/ (106)
42 quantitative methods/ (2821)
43 quasi experimental methods/ (142)
44 repeated measures/ (625)
45 time series/ (1658)
46 ("0400" or "0451" or "1800" or "2000").md. (2019250)
47 (pre‐post or "pre test$" or pretest$ or posttest$ or "post test$" or (pre adj5 post)).ti,ab. (43980)
48 ("quasi‐experiment$" or quasiexperiment$ or "quasi random$" or quasirandom$ or "quasi control$" or quasicontrol$ or ((quasi$ or experimental) adj3 (method$ or study or trial or design$ or controlled))).ti,ab,hw. (51501)
49 ("time series" or "time points").ti,ab,hw. (16196)
50 (effect or impact or trial or intervention).ti. (186412)
51 repeated measure*.ti,ab. (13022)
52 ((before adj5 after) or control group*).ti,ab. (108768)
53 or/37‐52 (2630095)
54 36 and 53 (1811)
Database: CINAHL
Search date: 2016‐08‐25
| # | Query | Results |
| S54 | S6 AND S24 AND S35 AND S52 Limiters ‐ Exclude MEDLINE records |
679 |
| S53 | S6 AND S24 AND S35 AND S52 | 2,842 |
| S52 | S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 | 1,307,267 |
| S51 | TI ( effect* or impact* or intervention* or before N5 after or pre N5 post or ((pretest or "pre test") and (posttest or "post test")) or quasiexperiment* or quasi W0 experiment* or evaluat* or "time series" or time W0 point* or repeated W0 measur* ) OR AB ( effect* or impact* or intervention* or before N5 after or pre N5 post or ((pretest or "pre test") and (posttest or "post test")) or quasiexperiment* or quasi W0 experiment* or evaluat* or "time series" or time W0 point* or repeated W0 measur* ) | 741,896 |
| S50 | TI ( randomis* or randomiz* or randomly ) OR AB ( randomis* or randomiz* or randomly ) | 113,421 |
| S49 | (MH "Health Services Research+") | 14,172 |
| S48 | (MH "Multicenter Studies") | 13,763 |
| S47 | (MH "Quasi‐Experimental Studies+") | 8,629 |
| S46 | (MH "Pretest‐Posttest Design+") | 27,255 |
| S45 | (MH "Experimental Studies+") | 171,110 |
| S44 | (MH "Nonrandomized Trials") | 175 |
| S43 | (MH "Intervention Trials") | 6,040 |
| S42 | (MH "Clinical Trials+") | 136,322 |
| S41 | (MH "Randomized Controlled Trials") | 27,706 |
| S40 | PT research | 986,877 |
| S39 | PT clinical trial | 52,803 |
| S38 | PT randomised controlled trial | 30,672 |
| S37 | (MH "Interrupted Time Series Analysis") | 16 |
| S36 | (MH "Controlled Before‐After Studies") | 7 |
| S35 | S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 | 139,789 |
| S34 | TI ( ((cultural* or language*) and (adapt* or accomodat* or approp* or target* or tailor*)) ) OR AB ( ((cultural* or language*) and (adapt* or accomodat* or approp* or target* or tailor*)) ) | 10,727 |
| S33 | TI ( (black or blacks or hispanic* or ((afro or african or asian or latin* or indian) N1 american*)) ) OR AB ( (black or blacks or hispanic* or ((afro or african or asian or latin* or indian) N1 american*)) ) | 23,157 |
| S32 | TI ( (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies) ) OR AB ( (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies) ) | 11,923 |
| S31 | TI ( (refugee* or immigrant* or (asyl* N1 seek*) or foreign* or ethnic* or minorit* or racial* or (multi adj cultural*) or multicultural* or (cultural N1 (diversit* or pluralism))) ) OR AB ( (refugee* or immigrant* or (asyl* N1 seek*) or foreign* or ethnic* or minorit* or racial* or (multi adj cultural*) or multicultural* or (cultural N1 (diversit* or pluralism))) ) | 52,137 |
| S30 | (MH "Cultural Diversity") | 7,341 |
| S29 | (MH "Refugees") | 3,619 |
| S28 | (MH "Emigration and Immigration") | 3,781 |
| S27 | (MH "Immigrants+") | 8,117 |
| S26 | (MH "Ethnic Groups+") | 79,372 |
| S25 | (MH "Minority Groups") | 6,947 |
| S24 | S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 | 327,166 |
| S23 | TI ( ((alcohol* N2 (drink* or consumption)) or (drinking N5 (behavio?r or habit*)) or nutrition* or diet* or food* or feed* or eating or meal or meals or ((physical or motor) N5 (activ* or exercis*)) or physical conditioning or running or jogging or swimming or walking or cycling or climbing or skiing or smok* or tobacco* or cigarette*) ) OR AB ( ((alcohol* N2 (drink* or consumption)) or (drinking N5 (behavio?r or habit*)) or nutrition* or diet* or food* or feed* or eating or meal or meals or ((physical or motor) N5 (activ* or exercis*)) or physical conditioning or running or jogging or swimming or walking or cycling or climbing or skiing or smok* or tobacco* or cigarette*) ) | 230,583 |
| S22 | (MH "Snow Skiing+") | 345 |
| S21 | (MH "Cycling") | 4,947 |
| S20 | (MH "Walking") | 11,426 |
| S19 | (MH "Running+") | 6,847 |
| S18 | (MH "Swimming") | 2,043 |
| S17 | (MH "Physical Activity") | 20,692 |
| S16 | (MH "Exercise+") | 57,782 |
| S15 | (MH "Motor Activity") | 4,381 |
| S14 | (MH "Eating Behavior+") | 15,850 |
| S13 | (MH "Smoking Cessation Programs") | 1,506 |
| S12 | (MH "Smoking Cessation") | 11,297 |
| S11 | (MH "Smoking") | 30,806 |
| S10 | (MH "Tobacco") | 4,366 |
| S9 | (MH "Drinking Behavior+") | 14,793 |
| S8 | (MH "Sports+") | 41,721 |
| S7 | (MH "Physical Fitness+") | 8,921 |
| S6 | S1 OR S2 OR S3 OR S4 OR S5 | 370,846 |
| S5 | (MH "Marketing+") | 16,874 |
| S4 | (MH "Consumer Health Information") | 8,649 |
| S3 | TI ( (("cd" or "cds" or dvd or dvds or video or videos) N3 distribut*) ) OR AB ( (("cd" or "cds" or dvd or dvds or video or videos) N3 distribut*) ) | 72 |
| S2 | TI ( (radio or television or "tv" or campaign* or advert* or boards or newspaper* or magasin* or magazin* or brochure* or leaflet* or pamphlet* or cinema* or ((mass W0 (communication or media)) or internet or social media or blog* or facebook or twitter or instagram or podcast* broadcast* or audiovisual or film* or movie* or ((cell or cellular or mobile) W0 (telephone* or phone*)))) ) OR AB ( (radio or television or "tv" or campaign* or advert* or boards or newspaper* or magasin* or magazin* or brochure* or leaflet* or pamphlet* or cinema* or ((mass W0 (communication or media)) or internet or social media or blog* or facebook or twitter or instagram or podcast* broadcast* or audiovisual or film* or movie* or ((cell or cellular or mobile) W0 (telephone* or phone*)))) ) | 56,745 |
| S1 | MH "Communications Media+" | 327,780 |
Database: SveMed+
Search date: 2016‐08‐25
| 1 | exp:"Communications Media" | 3955 |
| 2 | exp:"Consumer Health Information" | 72 |
| 3 | exp:"internet" | 859 |
| 4 | exp:"Marketing" | 525 |
| 6 | exp:"Drinking Behavior" | 1214 |
| 7 | exp:"Tobacco Use" | 1262 |
| 8 | exp:"Food Habits" | 1398 |
| 9 | exp:"Motor Activity" | 2449 |
| 10 | exp:"Exercise" | 2090 |
| 11 | exp:"physical fitness" | 686 |
| 12 | exp:"sports" | 2477 |
| 13 | exp:"Minority Groups" | 92 |
| 14 | exp:"Minority Health" | 4 |
| 15 | exp:"Population Groups" | 437 |
| 16 | exp:"Emigrants and Immigrants" | 345 |
| 17 | exp:"refugees" | 613 |
| 18 | exp:"Cultural Diversity" | 139 |
| 19 | exp:"human migration" | 857 |
| 20 | #1 OR #2 OR #3 OR #4 | 5088 |
| 21 | #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 | 7219 |
| 22 | #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 | 1852 |
| 23 | #20 AND #21 AND #22 | 5 |
Database: Cochrane Central Register of Controlled Trials
Search date: 2016‐08‐25
| #1 | MeSH descriptor: [Internet] explode all trees | 2580 |
| #2 | MeSH descriptor: [Communications Media] explode all trees | 8714 |
| #3 | MeSH descriptor: [Consumer Health Information] explode all trees | 280 |
| #4 | MeSH descriptor: [Marketing] explode all trees | 412 |
| #5 | radio or television or "tv" or campaign* or advert* or boards or newspaper* or maga?in* or brochure* or leaflet* or pamphlet* or cinema* or internet or social media or blog* or facebook or twitter or instagram or podcast* broadcast* or audiovisual or film* or movie* | 21774 |
| #6 | mass next (communicaton or media) | 549 |
| #7 | (cell or cellular or mobile) next (telephone* or phone*) | 1263 |
| #8 | (("cd" or "cds" or dvd or dvds or video or videos) near/3 distribut*) | 18 |
| #9 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 | 28663 |
| #10 | MeSH descriptor: [Drinking Behavior] explode all trees | 2918 |
| #11 | MeSH descriptor: [Tobacco Use] explode all trees | 188 |
| #12 | MeSH descriptor: [Food Habits] explode all trees | 2012 |
| #13 | MeSH descriptor: [Motor Activity] this term only | 3400 |
| #14 | MeSH descriptor: [Exercise] explode all trees | 16856 |
| #15 | MeSH descriptor: [Physical Fitness] explode all trees | 2456 |
| #16 | MeSH descriptor: [Sports] explode all trees | 11809 |
| #17 | ((alcohol* near/2 (drink* or consumption)) or (drinking near/5 (behavio?r or habit*)) or nutrition* or diet* or food* or feed* or eating or meal or meals or ((physical or motor) near/5 (activ* or exercis*)) or (physical next conditioning) or running or jogging or swimming or walking or skiing or cycling or climbing or smok* or tobacco* or cigarette*) | 146514 |
| #18 | #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 | 153505 |
| #19 | MeSH descriptor: [Minority Groups] explode all trees | 6 |
| #20 | MeSH descriptor: [Population Groups] explode all trees | 6601 |
| #21 | MeSH descriptor: [Minority Health] this term only | 16 |
| #22 | MeSH descriptor: [Emigrants and Immigrants] this term only | 124 |
| #23 | MeSH descriptor: [Refugees] this term only | 80 |
| #24 | MeSH descriptor: [Cultural Diversity] this term only | 79 |
| #25 | MeSH descriptor: [Human Migration] explode all trees | 76 |
| #26 | (refugee* or immigrant* or (asyl* near/1 seek*) or foreign* or ethnic* or minorit* or racial* or (multi next cultural*) or multicultural* or (newly next arrived) or ((family or families) near/2 reuni*) or resettlement or (cultural near/1 (diversit* or pluralism))) | 13000 |
| #27 | indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies | 3574 |
| #28 | black or blacks or hispanic* or ((afro or african or asian or latin* or indian) near/1 american*) | 13802 |
| #29 | ((cultural* or language*) and (adapt* or accomodat* or approp* or target* or tailor*)) | 22085 |
| #30 | #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 | 45204 |
| #31 | #9 and #18 and #30 in Trials | 523 |
Database: Eric via ProQuest
Search date: 2016‐08‐25
(ti((media OR internet OR blog* OR facebook OR twitter OR instagram OR "tv" OR television OR radio OR cinema* OR movie* OR film* OR campaign* OR newspaper* OR magazin* OR magasin* OR phone* OR telephone* OR brochure* OR leaflet* OR pamphlet*) AND (alcohol* OR drinking OR food* OR feed* OR eating OR activity OR exercise OR running OR walking OR jogging OR swimming OR skiing OR cycling OR climbing OR smoking OR tobacco OR cigarette*) AND (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies or black or blacks or hispanic* or afro‐american* or african‐american* or asian‐american* or latin‐american* or indian‐american* or "newly arrived" or "family reunion" or "family reunions" or resettlement or refugee* OR minorit* OR ethnic* OR immigrant* OR cultural) AND (random* OR control* OR pretest OR "pre test" OR posttest OR "post test" OR experiment* OR trial OR effect OR impact OR intervention* OR "time series" OR "repeated measures" OR "repeated measurements" OR "repeated measurement"))) OR (ab((media OR internet OR blog* OR facebook OR twitter OR instagram OR "tv" OR television OR radio OR cinema* OR movie* OR film* OR campaign* OR newspaper* OR magazin* OR magasin* OR phone* OR telephone* OR brochure* OR leaflet* OR pamphlet*) AND (alcohol* OR drinking OR food* OR feed* OR eating OR activity OR exercise OR running OR walking OR jogging OR swimming OR skiing OR cycling OR climbing OR smoking OR tobacco OR cigarette*) AND (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies or black or blacks or hispanic* or afro‐american* or african‐american* or asian‐american* or latin‐american* or indian‐american* or "newly arrived" or "family reunion" or "family reunions" or resettlement or refugee* OR minority* OR ethnic* OR immigrant* OR cultural) AND (random* OR control* OR pretest OR "pre test" OR posttest OR "post test" OR experiment* OR trial OR effect OR impact OR intervention* OR "time series" OR "repeated measures" OR "repeated measurements" OR "repeated measurement"))) 1112
Database: Web of Science
Search date: 2016‐08‐25
("media" OR "internet" OR "blog" OR "facebook" OR "twitter" OR "instagram" OR "tv" OR "television" OR "radio" OR cinema* OR movie* OR film* OR campaign* OR newspaper* OR magazin* OR magasin* OR phone* OR telephone* OR brochure* OR leaflet* OR pamphlet*) AND (alcohol* OR "drinking" OR food* OR feed* OR "eating" OR "activity" OR "exercise" OR "running" OR "walking" OR "jogging" OR "swimming" OR "skiing" OR "cycling" OR "climbing" OR "smoking" OR "tobacco" OR cigarette*) AND (indig* OR aborig* OR native* OR inuit* OR eskimo* OR kalaallit* OR amerind* OR "romany" OR "romanies" OR "gypsies" OR "gipsies" OR "black" OR "blacks" OR hispanic* OR afro‐american* OR african‐american* OR asian‐american* OR latin‐american* OR indian‐american* OR "newly arrived" OR "family reunion" OR "family reunions" OR "resettlement" OR refugee* OR minorit* OR ethnic* OR immigrant* OR cultural*) AND (random* OR "control" OR "pretest" OR "pre test" OR "posttest" OR "post test" OR experiment* OR "trial" OR "effect" OR "impact" OR "intervention" OR "time series" OR "repeated measures" OR "repeated measurements" OR "repeated measurement") 4691
Database: PubMed
Search date: 2016‐08‐25
((((media OR internet OR blog* OR facebook OR twitter OR instagram OR "tv" OR television OR radio OR cinema* OR movie* OR film* OR campaign* OR newspaper* OR magazin* OR magasin* OR phone* OR telephone* OR brochure* OR leaflet* OR pamphlet*) AND (alcohol* OR drinking OR food* OR feed* OR eating OR activity OR exercise OR running OR walking OR jogging OR swimming OR skiing OR cycling OR climbing OR smoking OR tobacco OR cigarette*) AND (indig* or aborig* or native* or inuit* or eskimo* or kalaallit* or amerind* or romany or romanies or gypsies or gipsies or black or blacks or hispanic* or afro‐american* or african‐american* or asian‐american* or latin‐american* or indian‐american* or "newly arrived" or "family reunion" or "family reunions" or resettlement or refugee* OR minorit* OR ethnic* OR immigrant* OR cultural) AND (random* OR control* OR pretest OR "pre test" OR posttest OR "post test" OR experiment* OR trial OR effect OR impact OR intervention* OR "time series" OR "repeated measures" OR "repeated measurements" OR "repeated measurement")))) AND publisher [sb] 206
Database: WHO International Clinical Trials Search Portal
Search date: 2016‐10‐19
Title= (media OR internet OR blog* OR facebook OR twitter OR instagram OR tv OR television OR radio OR cinema* OR movie* OR campaign* OR newspaper* OR magazin* OR magasin* OR phone* OR telephone* OR brochure* OR leaflet* OR pamphlet*) AND (indig* OR aborig* OR native* OR inuit* OR eskimo* OR kalaallit* OR amerind* OR romany OR romanies OR gypsies OR gipsies OR black OR blacks OR hispanic* OR afro‐american* OR african‐american* OR asian‐american* OR latin‐american* OR indian‐american* OR newly arrived OR family reunion OR family reunions OR resettlement OR refugee* OR minorit* OR ethnic* OR immigrant* OR cultural) 15
Database: ClinicalTrials.gov
Search date: 2016‐10‐19
Mass media 147
Database: OpenGrey
Search date: 2016‐10‐19
("media" OR "internet" OR "blog*" OR "facebook" OR "twitter" OR "instagram" OR "tv" OR "television" OR "radio" OR "cinema*" OR "movie*" OR "campaign*" OR "newspaper*" OR "magazin*" OR "magasin*" OR "phone*" OR "telephone*" OR "brochure*" OR "leaflet*" OR "pamphlet*") AND ("alcohol*" OR "drinking" OR "food*" OR "feed*" OR "eating" OR "activity" OR "exercise" OR "running" OR "walking" OR "jogging" OR "swimming" OR "skiing" OR "cycling" OR "climbing" OR "smoking" OR "tobacco" OR "cigarette*") AND("indig*"OR "aborig*"OR "native*"OR "inuit*"OR "eskimo*"OR "kalaallit*"OR "amerind*"OR"romany" OR "romanies" OR "gypsies" OR "gipsies" OR "black" OR "blacks" OR "hispanic*" OR "afro‐american*" OR "african‐american*" OR "asian‐american*" OR "latin‐american*" OR "indian‐american*" OR "newly arrived" OR "family reunion" OR "family reunions" OR "resettlement" OR "refugee*" OR "minorit*" OR "ethnic*" OR "immigrant*" OR "cultural") 192
Database: Grey Literature Report
Search date: 2016‐10‐19
Mass media 92
Television 45
Radio 44
Newspaper 2
Facebook 2
Twitter 5
Instagram 0
Blog 3
Cinema 0
Magazine 26
Brochure 5
Leaflet 0
Pamphlet 4
Phones 33
Telephones 53
Database: Eldis (via Eldis Google development websearch)
Search date: 2016‐10‐19
(media OR internet OR blogs OR facebook OR twitter OR instagram OR tv OR television OR radio OR cinema OR movie OR campaign OR newspaper OR magazines OR magasines OR phones OR telephones OR brochures OR leaflets OR pamphlets) AND (minorities) (limited to Eldis documents) First 100 references were screened.
Appendix 2. Unused methods due to the type of studies or data identified
This appendix describes sections from the review protocol with unused methods (Mosdøl 2015). We could not implement these because of characteristics of the included studies or the available data.
Unit of analysis issues
Unit of analysis error can occur if trials based on group allocation to treatment condition (cluster‐RCTs, NRCTs and CBA studies) have not accounted for the effect of clustering in the statistical analyses. If possible, we will use an estimate of the intra‐cluster correlation coefficient (ICC) derived from the trial and subsequently attempt to re‐analyse the data according to the inflating standard errors method (Higgins 2011). If an ICC is not available, we will attempt to find an appropriate value based on the same/similar outcome from other relevant sources of ICC values. If none of these options is possible, we will report only the point estimate.
Dealing with missing data
We will contact the study authors if the study has incomplete or missing data. If missing data cannot be obtained, we will report this in the 'Risk of bias' table. If there are data missing on the primary outcomes, we will only present the study descriptively. We will note the level of attrition. As far as possible, we will conduct our analysis of randomised trials on an intention‐to‐treat basis.
Assessment of heterogeneity
We will base a first assessment of heterogeneity on the apparent characteristics of the studies regarding the population, intervention, comparison and outcomes. Judgments about whether meta analyses are appropriate will be based on the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). If meta‐analysis is considered meaningful, we will examine the forest plot to look for heterogeneity between studies and use the I2 statistic to quantify it. We will advise caution in the interpretation of those results where there are high levels of unexplained heterogeneity, taking into account that the direction and size of the effects may influence the I2 statistic value.
Assessment of reporting biases
If an outcome is reported in more than 10 studies and a meta analysis has been performed, we will examine the corresponding funnel plot without performing any formal tests. This will guide our assessment of potential small study effects such as publication bias.
Data synthesis
We will sort the included studies according to the intervention, measures and comparisons made. We will assess results for each comparison and collate them separately. If population, study design, intervention and outcome measures are similar enough across studies, we will conduct meta‐analyses using RevMan 2014. If outcomes within a comparison are obtained from several study designs, we will present results from non‐randomised designs separately. Where there is a sufficient number of studies reporting the same outcome with sufficiently homogeneous populations, interventions and comparisons, we will calculate a pooled risk ratio with 95%CIs for dichotomous data. For continuous outcomes, we will calculate the mean difference at follow‐up with 95% CIs, or the standardised mean difference with 95% CIs as appropriate. In the same case for ITS design, we will use the difference between the expected value at one year follow‐up based on the pre‐intervention trend and the expected value at the same point in time based on the postintervention trend. If the differences are not available, we will attempt to re‐analyse using data from graphs or tables through segmented time series regression (Ramsay 2003). We expect that there will be some heterogeneity between populations, interventions and studies, and will therefore use the random effects method in the analyses (Higgins 2011). We will present the meta‐analyses results in both text and forest plots. If meta‐analysis is not considered meaningful/appropriate, we will present descriptive data in text and tables.
Subgroup analysis and investigation of heterogeneity
If there are sufficient data, we will explore subgroup analysis on the primary research objective. We will analyse the comparison by the following criteria: which health behaviour was targeted (physical activity, dietary pattern, tobacco or alcohol), type of media used, whether only one type of mass media or two or more mass media channels were used, and intervention intensity. We will interpret all subgroup analysis carefully.
Sensitivity analysis
If there is a sufficient number of included studies, we will perform a sensitivity analysis excluding studies at high risk of bias.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Boyd 1998.
| Methods |
Study design: cluster‐randomised trial. 14 communities (from 35,600 to 630,000 inhabitants), matched in pairs before randomisation Year of study: 1994‐1995 Intervention period: baseline data collected the year preceding the intervention. Continuous data collection for 15 months. 2 waves of paid advertisements running 6 weeks and 4 weeks in the intervention communities, with some activities (public service announcements (PSAs) and community outreach) throughout the whole period Follow‐up period (postintervention): data collection ended 2 months after last wave of paid advertisement |
|
| Participants |
Country: USA (communities in 4 US regions) Language: English Target population: adult African American smokers Exposure population: broad population exposure in the intervention communities through mass media exposure. Proportion of African American residents ranged from 17% to 42% in the study communities. Estimated number of African American smokers in intervention communities was N = 310,471 and in control communities, N = 331,360. Socioeconomic profile of the communities not reported |
|
| Interventions |
Study objective/aim: to evaluate whether a targeted communications campaign would lead more adult African Americans to call the CIS for smoking cessation resources Control: no intervention Intervention: 10 weeks of paid advisements aired in 2 waves of 6 and 4 weeks (in total 3364 radio and 208 television advertisements) in the intervention communities. Attempts were made to use the advertisements as PSAs (media advertisements in the public interest aired free of charge) particularly during times when interest in smoking cessation was expected (i.e. New Year holiday). Outreach packets containing a 12 min video, posters, and flyers (all mass media components) distributed to the target population (1449 packets distributed). Content of the mass media message: encourage smokers to call the CIS for help to quit smoking; emphasis that the CIS service is free of charge Media channel(s) of dissemination: radio, television, video, posters, and flyers Theoretical basis: no theories specifically mentioned Targeting approach: 6 radio and 1 television advertisements developed using programming formats, language and music adapted to the target population. Messages and advertisements were developed through 3 steps: review of past research on unique quitting motives and barriers in target group; focus groups with target population and 40 individual interviews to identify barriers and facilitators for calling the CIS for help to quit smoking; and pre‐test of intervention material in (new) focus groups with target population and feedback from health communication specialists. Radio and television stations with high African American listenership/viewership identified for placement of advertisements. Outreach packets distributed to leaders and contact persons in community organisations, churches, and social groups in African American communities. |
|
| Outcomes |
Use of health promotion services: calls to the CIS for smoking cessation information and materials by African American adults residing in the intervention and control communities Intervention costs: partial description Adverse outcomes: none reported |
|
| Notes |
Intervention fidelity: the delivery of the intervention assessed through media "target rating points". Range of estimated reach among African Americans in the seven intervention communities 88.0%‐95.5%; with the target audience hearing or seeing an advertisement at estimated frequency of 7.02‐12.60 times in the study communities. Sources of funding: the National Cancer Institute (USA), the Robert Wood Johnson Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation sequence adequately generated | Unclear risk | Allocation method not presented |
| Allocation adequately concealed | Low risk | All clusters randomised at once |
| Baseline outcome measurements similar | Unclear risk | Not presented |
| Baseline characteristics similar | Unclear risk | Not presented. Communities matched in pairs based on number and proportion of population that was African American, income, sex, age, education, population proportion below the poverty line, and proportion of dwellings with telephones |
| Incomplete outcome data adequately addressed | Low risk | This was a population study using routinely collected call data |
| Knowledge of allocated interventions prevented | Unclear risk | Neither participants nor outcome assessors blinded to allocation |
| Adequately protected against contamination | Low risk | Geographically spread communities and non‐overlapping media markets |
| Free of selective outcome reporting | Low risk | Selctive reporting not likely; only few relevant outcomes |
| Other bias | Low risk | Judged low risk, but noted that both the study and the quit line services were funded by the National Cancer Institute. |
Elder 2005.
| Methods |
Study design: RCT Year of study: not stated Intervention period: 12 weeks Follow‐up period (postintervention): immediately postintervention (relevant data at 6 and 12 month follow‐up not published) |
|
| Participants |
Country: USA (San Diego, CA) Language: Spanish Target population: Spanish‐speaking Latino immigrants or Latino American Inclusion criteria: women aged 18‐65 years living in a Spanish‐language dominant household Exclusion criteria: pregnant, on special diet for medical reasons, or planning to leave the area during the study period Participants: intervention 1, N = 119; intervention 2, N = 118; intervention 3, N = 120 Sex: women Socioeconomic characteristics: 95% born in Mexico, 27% with little or no formal education, 27% with some college education, > 50% homemakers, 25% working full‐time. Wide range of family income, 13% with USD 500–USD 1000 per month, 25% with > USD 2501 per month. Low acculturation score. Described by authors as women with low levels of acculturation, income, and education. Other: mean BMI 29.6 kg/m2 ± 5.6 |
|
| Interventions |
Study objective/aim: to assess the effect of person‐tailored nutrition education materials, with or without personal delivery and counselling from lay health advisor(promotora), compared to off‐the‐shelf materials targeted to a Latino population Intervention 1 (study control): targeted mass media intervention The women received 12 weekly Spanish‐language newsletters mailed to the participant's home. These were based on brochures containing information on food purchasing, food preparation, and food consumption from the American Heart Association, American Dietetic Association and the American Cancer Society (off‐the‐shelf materials targeted to a Latino population). Intervention 2: individually‐tailored newsletters The women received 12 weekly individually tailored newsletters and activity inserts mailed to the participant's home. The newsletters were tailored by using the participants' baseline data. They provided feedback on the assessment process, opportunity for personalised goal setting and for dealing with identified barriers. Intervention 3: individually‐tailored newsletters + home visits The women received individually tailored newsletters as for intervention 2 and in addition weekly home visits or telephone calls from promotoras over the 12‐week period. Content of the mass media message: behavioural strategies to reduce dietary fat and to increase fibre, fruit and vegetable intake Media channel(s) of dissemination: newsletters Theoretical basis: none stated for the targeted mass media intervention Targeting approach: material presented in participants' first language (Spanish). Some cultural adaptation of targeted print condition may be assumed (off‐the‐shelf materials targeted to a Latino population by national health organisations), but is not described by authors. Recruitment of Spanish‐speaking Latino participants only |
|
| Outcomes |
Self‐reported behavioural change: energy % calories from fat, dietary fibre intake (g) Intervention costs: partial description Adverse outcomes: none reported |
|
| Notes |
Intervention fidelity: not reported Sources of funding: the National Cancer institute (USA) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation sequence adequately generated | Unclear risk | Block randomisation. Allocation method otherwise not presented |
| Allocation adequately concealed | Low risk | Participants agreed to participate before randomisation. |
| Baseline outcome measurements similar | Low risk | Analyses adjusted for baseline values |
| Baseline characteristics similar | Low risk | Analyses adjusted for baseline values |
| Incomplete outcome data adequately addressed | Low risk | Missing data imputed with baseline values |
| Knowledge of allocated interventions prevented | High risk | Unclear risk for the BMI measurements. High risk for self‐reported behaviours in non‐blinded study |
| Adequately protected against contamination | Low risk | Primary intervention material delivered by mail |
| Free of selective outcome reporting | Low risk | Width of data presented in 3 papers |
| Other bias | Low risk | None considered |
Jih 2016.
| Methods |
Study design: cluster‐RCT. ˜15 participants recruited by each of 58 lay health workers (LHW). LHW‐groups randomised Year of study: August 2010‐September 2013. Intervention period: 2 months Follow‐up period (postintervention): assessment at 6 months (4 months postintervention) |
|
| Participants |
Country: USA (San Francisco, CA) Language: Chinese Target population: Chinese American immigrants Inclusion criteria: self‐identifying as Chinese immigrants (foreign born) or Chinese American; aged 50‐75 years; Cantonese, Mandarin or English speaker; intending to stay in area > 6 months Exclusion criteria: other participants in household, personal history of colorectal cancer (focus of parallel RCT) Participants: intervention 1, N = 360; intervention 2, N = 365 Sex: both, 83% women in intervention group 1, 79% women in intervention group 2 Socioeconomic characteristics: mean 17 years in the US, ˜70% with less education than high school diploma, ˜96% self‐reported spoken English proficiency as 'so‐so', 'poor', or 'not at all'. Wide range of family income Other: mean BMI 24.2 kg/m2 ± 3.4 in intervention group 1; 23.3 kg/m2± 4.0 in intervention group 2 |
|
| Interventions |
Study objective/aim: to evaluate the efficacy of an in‐language intervention of 2 lectures plus printed materials versus printed materials alone on knowledge and adherence to nutrition and physical activity guidelines among older Chinese Americans Intervention 1 (study control): targeted mass media intervention Participants received the printed lecture handouts made for intervention group 2 that focused on culturally appropriate examples of food and physical activity and a Chinese nutrition brochure. Lay health workers (LHW) delivered 2 small group education sessions with follow‐up calls on colorectal cancer (control component). Intervention 2: lectures and targeted mass media intervention Participants received two 60‐90 min lectures, printed lecture handouts and a nutrition brochure about 2 months apart, delivered by an instructor. LHW called about 1 month after each lecture to ask them recall the lecture and remind to attend the next lecture or final assessment. Content of the mass media message: basic nutrition and physical activity education, with focus on recommended daily 5 servings of vegetables and 4 servings of fruit, and ≥ 150 min moderate intensity physical activity weekly Media channel(s) of dissemination: printed information material Theoretical basis: none stated Targeting approach: the lectures were presented in the participants' preferred language (Cantonese, Mandarin, or English). Lectures and material were developed with culturally appropriate examples of common foods, relevant physical activities and familiar portion size models for target group. A community advisory board reviewed the material for cultural and linguistic appropriateness, with subsequent testing in focus groups. |
|
| Outcomes |
Self‐reported behavioural change: self‐reported behaviour meeting guidelines for ≥ 5 servings of vegetables/day, ≥ 5 servings of fruit/day, ≥ 150 minutes moderate physical activity/week Knowledge or attitudes to change: self‐reported knowledge of recommended ≥ 5 servings of vegetables/day, ≥ 5 servings of fruit/day, ≥ 150 minutes moderate physical activity/week Adverse outcomes: none reported |
|
| Notes |
Intervention fidelity: not reported Sources of funding: National Institutes of Health, the National Cancer institute (USA) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation sequence adequately generated | Low risk | Computer‐generated randomisation |
| Allocation adequately concealed | Low risk | LHW‐groups randomised in blocks. Allocation concealed until LHW had recruited all his/her participants |
| Baseline outcome measurements similar | Low risk | Baseline outcome measurement presented without statistical tests; appears balanced |
| Baseline characteristics similar | Low risk | Baseline characteristics presented with statistical tests. Balances apart from small difference in baseline BMI between groups; adjusted in final analysis |
| Incomplete outcome data adequately addressed | Low risk | Small attrition overall, < 1% of sample. 6.5% had missing data for 1 or more covariates |
| Knowledge of allocated interventions prevented | High risk | Self‐reported behavioural change and knowledge in non‐blinded study |
| Adequately protected against contamination | Unclear risk | No discussion of possible contact between participants in different groups |
| Free of selective outcome reporting | Low risk | Few relevant outcome measures; all reported |
| Other bias | Low risk | Analyses adjusted for clustering |
Kennedy 2013.
| Methods |
Study design: interrupted time series study (as re‐analysed for this systematic review) Year of study: 2009‐2011 Intervention period: continuous data collection from March 2009 to June 2011. 2 waves of campaign activities, June‐October 2009 and January‐March 2011 Follow‐up period (postintervention): see intervention period |
|
| Participants |
Country: USA (Richmond, VA) Language: English Target population: pregnant African American smokers Exposure population: full population exposure through media exposure in a city (approximately 200,000 inhabitants). Total target population not known. Approximately 400 births by African American women per month. Interviews indicated that ˜40% of pregnant African American women had smoked the past 3 months. Socioeconomic profile of area not reported |
|
| Interventions |
Study objective/aim: to evaluate the effect of a social marketing campaign aiming to encourage pregnant African American smokers to call telephone counselling Control (pre‐campaign): no intervention Intervention: 3.5 months of paid radio advisements, billboards and bus ads, with estimated 17 million of impressions (i.e. opportunities to hear the campaign messages). In addition, the campaign consisted of other small media, social media content, press coverage, and distribution of campaign‐branded items (tins of mint, lip balm). Outreach workers and frontline clinic and social service agency staff distributed campaign material and reinforced message. A second wave of advertisements starting at New Year 1.5 years after baseline were not re‐analysed for this systematic review. Content of the mass media message: 'One tiny reason to quit' – message from the baby. Encourage pregnant women to quit smoking and make use of free telephone smoking cessation counselling Media channel(s) of dissemination: radio, billboards, bus ads, newspaper ads, Facebook page, press coverage, and campaign‐branded items Theoretical basis: no theories specifically mentioned for development of intervention content, message, or framing. Positive framing chosen based on previous experiences Targeting approach: message concepts were tested for appropriateness and appeal with pregnant African American current and recent smokers, with additional audience testing of creative material. Creative material featuring African American baby. Outreach workers from the African American community were trained to approach pregnant workers with campaign messages and distribute campaign material. Radio ads in the contemporary radio station most popular with young African American adults according to ratings. Billboards in relevant neighbourhoods. Newspaper ads in African American weekly papers |
|
| Outcomes |
Use of health promotion services: all calls to telephone smoking cessation counselling by adults between 18‐45 years in counties in the local broadcast range of the radio station that ran the advertisements Adverse outcomes: none reported |
|
| Notes |
Intervention fidelity: not reported Sources of funding: National Center on Minority Health Dispartities, National Institues of Health (USA) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent (ITS) | Low risk | The second wave of advertisements started at New Year, and thus influenced by the normal increase in calls to quit lines at this time of year. This second wave is not included in the re‐analysed material. |
| Analysed appropriately (ITS) | Low risk | Data re‐analysed for this systematic review according to standards (see Methods section) |
| Shape of effect pre‐specified (ITS) | Low risk | Data re‐analysed for this systematic review according to standards (see Methods section) |
| Unlikely to affect data collection (ITS) | Low risk | Study based on routinely collected call data |
| Blinding of outcome assessment (ITS) | Unclear risk | Unclear if assessors were aware of campaign |
| Incomplete outcome data addressed (ITS) | Low risk | Not relevant |
| Free of selective reporting (ITS) | Low risk | Selctive reporting not likely; only a few relevant outcomes from routinely collected call data |
| Other biases (ITS) | Low risk | No other biases identified |
Risica 2013.
| Methods |
Study design: RCT Year of study: not reported Intervention period: participants had access to 12 weekly cable TV shows and 4 months follow‐up intervention Follow‐up period (postintervention): assessment at 3 months (end of TV shows), 8 months (end of follow‐up intervention) and 12 months (4 months postintervention) |
|
| Participants |
Country: USA (Massachusetts) Language: English Target population: African American women Inclusion criteria: self‐identified as African American or black women, aged 18–70 years, resided in catchment area of the cable TV company, planned to stay in area for ≥ 1 year, access to telephone, television and videocassette recorder (VCR), available to watch the TV programme at its airtime, BMI ≥ 22 kg/m2 Exclusion criteria: pregnant or < 4 months postpartum, physical problems that would prevent mild physical activity, previous history of treatment for eating disorders, unable to speak and read English, participation in other weight‐control research project Participants: control, N = 82; intervention 1, N = 71, Intervention 2, N = 210 (3 intervention arms combined) Sex: women Socioeconomic characteristics: all self‐described African American, black or West Indian/Caribbean ethnicity. 12% foreign‐born. 12% had not completed high school, 40% with college education. 44% in lowest income category. The study paid for cable TV service for participants who could not afford it (19% of participants) Other: 71% obese. Self‐reported hypertension > 25%, diabetes 12%, and on medication for hypertension or heart condition > 25%. |
|
| Interventions |
Study objective/aim: to evaluate the effectiveness of a culturally tailored weight control cable TV programme for black women Control: wait‐list/attention placebo comparison. Biweekly mailings for 12 weeks with other health‐related information. Received all the TV shows as videos and other intervention material after the 12‐month follow‐up (i.e. after final outcome assessment) Intervention 1: participants were given access to 12 one‐hour live programmes on cable TV and printed material corresponding to the shows biweekly by post. After the shows, participants received 4 monthly mailings with written material and booster videotapes including an exercise video. Intervention 2 (combination of 3 study arms): in addition to all intervention content described under intervention 1, participants received either access to a toll‐free number to call during a live sharing part of show; 12 weekly and 4 monthly telephone support calls from a community outreach educator; or both access to call the 'live' sharing and the 16 telephone support calls Content of the mass media message: educational content regarding nutrition and physical activity to improve health and weight control as defined by each woman. Practical cooking demonstration or physical activity breaks. 20 min of each show devoted to a live 'sharing' between social worker, featured guest, and live callers. Media channel(s) of dissemination: cable TV, print material, video Theoretical basis: intervention based on Social Action Theory. Behavioural change, stress reduction and self‐management principles integrated into nutrition and physical activity sections Targeting approach: designed to be culturally appropriate based on formative research with 500 people from the target population. All African American female cast in the TV shows, including all experts; recruited only target population |
|
| Outcomes |
Indicators of behavioural change: BMI (kg/m2), weight (kg) Self‐reported behavioural change: food habits questionnaire (fat behaviours), leisure activity score Adverse outcomes: none reported |
|
| Notes |
Intervention fidelity: random participants were called during shows to monitor who was watching. Calls to live sharing part and support calls logged. At 3 months follow‐up, 69% of participants had watched 7‐12 shows and 57% had read most or all written material. Participants in intervention 2 were more reluctant to call live than expected. < 50% of the planned support calls were completed. Sources of funding: the National Cancer Institute (USA) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation sequence adequately generated | Low risk | After baseline assessment, participants drew an envelope from a container with concealment of allocation. |
| Allocation adequately concealed | Low risk | After baseline assessment, participants drew an envelope from a container with concealment of allocation. |
| Baseline outcome measurements similar | Low risk | Baseline outcome measurements presented and analysed as balanced |
| Baseline characteristics similar | Low risk | Baseline characteristics presented and analysed as balanced |
| Incomplete outcome data adequately addressed | Low risk | ITT analyses conducted |
| Knowledge of allocated interventions prevented | High risk | Unclear risk for the BMI measurements. High risk for self‐reported behaviours in non‐blinded study |
| Adequately protected against contamination | Low risk | Participants reported to be geographically spread |
| Free of selective outcome reporting | Low risk | Results compared with published protocol |
| Other bias | Low risk | None considered |
Webb 2009.
| Methods |
Study design: RCT Year of study: 2006‐2007 Intervention period: 1 mailing of print material Follow‐up period (postintervention): 3 months |
|
| Participants |
Country: USA (Florida) Language: English Target population: African American smokers Inclusion criteria: 18‐65 years old, smoked ≥ 5 cigarettes/day, had permanent mailing address, could read English, wanted to quit smoking within 1 year Exclusion criteria: currently receiving a quit smoking intervention Participants: intervention 1, N =127; intervention 2, N = 128. (The numbers in the participant flow diagram differs from numbers in text: participants randomised to intervention 1, N = 129; intervention 2, N =132). Sex: 56% women Socioeconomic characteristics: 99% African American (3 Hispanic participants), 61% single, 74% completed high school, 47% household income < USD 10,000. Other: mean age: 43 years; mean cigarettes/day: 23, mean years of smoking: 23 |
|
| Interventions |
Study objective/aim: to assess extent to which cultural specificity contributes to the efficacy of written self‐help materials among African American smokers Intervention 1 (control): 1‐2 days after baseline assessment, participants received a non‐culturally specific printed smoking cessation guide Intervention 2: 1‐2 days after baseline assessment, participants received a culturally specific printed smoking cessation guide Content of the mass media message: information about smoking and health, tobacco advertising, secondhand smoke, readiness to quit, quitting strategies, and community efforts Media channel(s) of dissemination: print material Theoretical basis, intervention 1: a non‐culturally specific smoking cessation guide was developed by replacing all culturally specific aspects of the Pathways to freedom smoking cessation guide, while keeping topics and smoking information unchanged. The aim was to create a booklet without attention to any particular ethnic or cultural group. Pictures were changed to cartoons or different ethnicities. Theoretical basis, intervention 2: the Pathways to freedom smoking cessation guide was an established culturally specific guide for African Americans (available from www.cdc.gov/tobacco/quit_smoking/how_to_quit/pathways/pdfs/pathways.pdf). Written at sixth‐grade reading level. Culturally specific elements related to African American values, communication patterns, familial roles, history, statistics specific to African Americans and mobilising the community to fight the tobacco industry. Pictures and testimonials from target group. Stereotypical African American names and colours. |
|
| Outcomes |
Self‐reported behavioural change: quit attempts, smoking reduction, 24‐hour point prevalence abstinence, 7‐day point prevalence abstinence Knowledge or attitudes to change: readiness to quit Adverse outcomes: none reported Reported outcomes not considered relevant for this review: content evaluation measures |
|
| Notes |
Intervention fidelity: not reported Sources of funding: Syracuse University (USA) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation sequence adequately generated | Unclear risk | Allocation method not presented |
| Allocation adequately concealed | Unclear risk | Not reported |
| Baseline outcome measurements similar | Low risk | There was no significant differences on demographics and smoking history |
| Baseline characteristics similar | Low risk | There was no significant differences on demographics and smoking history |
| Incomplete outcome data adequately addressed | Unclear risk | Demographics reported as similar in attrition groups, but ITT analyses not mentioned |
| Knowledge of allocated interventions prevented | Unclear risk | Self‐reported smoking behaviours in non‐blinded study, but assumed similar conditions in both groups. Blinding of assessors not presented |
| Adequately protected against contamination | Unclear risk | Not mentioned |
| Free of selective outcome reporting | Low risk | Main outcome (smoking habits) reported using several different measures |
| Other bias | Low risk | None considered |
BMI: body mass index; CIS: Cancer Information Service; ITT: intention‐to‐treat; LHW: lay health worker; PSA: public service announcement; RCT: randomised controlled trial.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abroms 2014 | Individually tailored text messages. No specific targeting to ethnic minorities |
| Aghi 1984 | Individual counselling available as part of the intervention. Not targeted to ethnic minority |
| Albright 2009 | Not considered a mass media intervention |
| Albright 2012 | Not considered a mass media intervention |
| Alcalay 1999 | Before‐after assessment without control group |
| Bermejo 2012 | Participants attended a group event before receiving the mass media component |
| Block 2004 | Individually tailored content. Unclear targeting to ethnic minority |
| Brady 2010 | Campaign targeted to a patient group |
| Bramley 2005 | Individually tailored text messages based on initial counselling |
| Brimblecombe 2013 | Protocol for a multi‐component store intervention. No relevant outcome measures |
| Brown 2012 | Not considered a mass media intervention |
| Buis 2013 | Retrospective analyses |
| Buller 2008 | Intervention not clearly targeted to ethnic minorities |
| Burger 2003 | Intervention focused on risk communication rather than disease prevention. Study not designed to show effect of a targeted approach |
| Burns 2010 | Assessment of quit line calls from Latino compared to non‐Latino population before and after Spanish‐language campaign |
| Campbell 2004 | Individually tailored newsletters |
| Campbell 2014 | Repeated cross‐sectional surveys. No control group |
| Cantrell 2013 | Experimental study of pictorial versus text‐only tobacco warning labels in different ethnic groups |
| Carlini 2008 | Personal invitation letters to re‐enrol into counselling. Not considered a mass media intervention |
| Cessnun 2011 | The target population is adolescents, secondarily their parents. Not considered a mass media intervention |
| Chang 2010 | Not considered a mass media intervention |
| Chang 2014 | As Chang 2010 |
| Chhichhia 2011 | Not considered a mass media intervention |
| Chung 2014 | Before‐after assessment without control group |
| Collins 2014 | Individually tailored text messages |
| Cummins 2015 | Report on implementation and impact of tobacco quit line counselling services |
| Darity 1997 | Results presented as repeated cross‐sectional surveys. Not relevant study design as analysed |
| Dedier 2014 | Individually tailored automatic telephone coach |
| Dunton 2008 | Individually tailored intervention components |
| Emmons 2003 | Individually tailored intervention components. Not targeted to ethnic minorities |
| Ferguson 2015 | Not any of the specified study designs |
| Fitzgerald 2009 | No impact assessment reported |
| Foster 2014 | Multicomponent store intervention. Mass media components only minor part of intervention. No clear targeting to ethnic minorities |
| Froelicher 2010 | Not considered a mass media intervention |
| Fukuoka 2011 | Individually tailored intervention components |
| Gans 2016 | Multicomponent community intervention. Mass media components only minor part of intervention. No clear targeting to ethnic minorities |
| Gerber 2009 | Not considered a mass media intervention |
| Gerber 2013 | Not considered a mass media intervention |
| Gittelsohn 2012 | Multicomponent store intervention. Mass media components only minor part of complex intervention |
| Gittelsohn 2013 | As Gittelsohn 2012 |
| Glover 2013 | Protocol. Not considered a mass media intervention. Before‐after assessment without control group |
| Graham 2012 | Description of programme development and click‐through rates for different online advertisements |
| Gray 2012 | Protocol. Not considered a mass media intervention |
| Grigg 2008 | Interrupted time series study with 2 data points before the intervention and 2 after |
| Hammerback 2012 | Not considered a mass media intervention. Before‐after assessment without control group |
| Hanson 2012 | Description of programme development and user's opinion of campaign |
| Henderson 2012 | Individually tailored content. Patient education |
| Hind 2010 | Protocol. Study does not evaluate the effect of the mass media component |
| Ho 2008 | Community intervention with many intervention activities involving several institutions. Mass media component smaller part of complex intervention compared to no intervention |
| Houry 2010 | Written information targeted to problem behaviours or life situations, not to ethnic minority characteristics |
| Huang 2015 | Intervention not targeted to ethnic minorities. Not any of the specified study designs |
| Irvine 2004 | Individually tailored, interactive multimedia programme. Unclear targeting to ethnic minorities |
| Ivers 2006 | Content of intervention not identical in the 3 intervention sites |
| Jantz 2002 | Interactive education programme |
| Jason 1988 | The whole population exposed to the mass media component (not described as targeted). Study designed to evaluate the effect of extended community outreach to ethnic minority group |
| Jenkins 1997 | Controlled before‐after study with only 1 intervention site and 1 control site |
| Joseph 2014 | Individually tailored content through interaction and contact with project staff. Mass media component (in control group) not targeted to ethnic minorities |
| Joseph 2015 | Before‐after assessment with no control group |
| Kandula 2014 | Not considered a mass media intervention |
| Kim 2013 | Text messages sent with a possibility to reply and receive answers |
| Kreuter 2004 | Individually tailored women's magazines based on baseline questionnaire |
| Kreuter 2005 | Individually tailored women's magazines based on baseline questionnaire |
| LaChausse 2012 | Intervention not targeted to ethnic minorities. Individual feedback |
| Larsen 2014 | Individually tailored content and counselling. Before‐after without control group |
| Larson 2009 | Community intervention study with many intervention activities on different levels. Time series data with 5 measurement points and gradual implementation of the intervention |
| Lee 2011 | Mass media component (in control group) not targeted to ethnic minorities |
| Li 1984 | Non‐randomised controlled trial with 4 arms. 1 site each for 2 of the arms. Alternating 2 interventions every other week in a third site |
| Linares 2013 | Before‐after assessment without control group |
| Lipkus 1999 | Not considered a mass media intervention |
| Ma 2004 | Description of programme and campaigns. No impact assessment |
| Mackey 2015 | Individually tailored content and counselling. Adapted to characteristics of college life, not ethnicity |
| Magoc 2009 | Individually tailored, interactive computer programme |
| Marin 1990 | Interrupted time series study with 2 data points before the intervention and 2 after |
| Marin 1994 | Interrupted time series study with 2 data points before the intervention and 1 after |
| McAlister 1992 | Non‐randomised controlled trial with 2 intervention sites and 1 control site |
| McDonnell 2011 | Study of a culturally adapted self‐help smoking cessation programme delivered either as an interactive web‐programme or as booklets |
| Mead 2013 | Community intervention with many intervention activities involving several institutions. Mass media component smaller part of complex intervention compared to no intervention |
| Mhurchu 2007 | Pilot study. Description of recruitment and data collection methods |
| Mhurchu 2010 | Nutrition education material tailored to individual shopping preferences in addition to cultural targeting |
| Migneault 2012 | Individually tailored, interactive automatic telephone counselling. Can be considered as patient education |
| Moskowitz 2016 | Not considered a mass media intervention |
| Muñoz 1997 | Study of the effect of adding a mood management programme to a culturally adapted smoking cessation self‐help programme |
| Muñoz 2006 | Describes 4 studies, including 2 RCTs. Smoking cessation programme with individual tailoring |
| Nollen 2007 | Not considered a mass media intervention |
| Orleans 1998 | Participants randomised to different formats of individual telephone counselling |
| Patten 2010 | Not considered a mass media intervention |
| Patten 2012 | Description of a research programme. No impact assessment data presented |
| Pekmezi 2010 | Individually tailored feedback delivered via Internet or print |
| Perez 2009 | Not considered a mass media intervention |
| Reininger 2015 | Multicomponent community intervention. Mass media components only minor part of intervention. Not any of the specified study designs |
| Resnicow 1997 | Not considered a mass media intervention |
| Resnicow 2000 | Not considered a mass media intervention |
| Resnicow 2001 | Not considered a mass media intervention |
| Resnicow 2002 | Not considered a mass media intervention |
| Resnicow 2005 | Not considered a mass media intervention |
| Resnicow 2008 | Not considered a mass media intervention |
| Resnicow 2009 | Individually tailored newsletters |
| Rimmer 2009 | Mass media component (in control group) not targeted to ethnic minorities |
| Romero 2012 | Before‐after assessment without control group |
| Schlundt 2009 | Community intervention study with many intervention activities on different levels. Time series data with 5 measurement points and gradual implementation of the intervention |
| Scisney‐Matlock 2012 | Individually tailored, interactive computer programme with e‐mail feedback |
| Shaikh 2011 | Not considered a mass media intervention |
| Shakeshaft 2014 | Community intervention with many components and intervention activities, including social marketing campaigns. Whole population approach, including aboriginal communities. Not specific targeting to and impact assessment in ethnic minority groups. |
| Sharma 2010 | Description of programme and activities. No impact assessment |
| Shea 1996 | Description of programme and activities. No impact assessment |
| Skewes 2007 | Not considered a mass media intervention |
| Steinberg 2013 | Personal contact with research team through text‐messages and email |
| Stevens 2002 | Before‐after assessment without control group |
| Streja 2014 | The main aim of the study was to reduce secondhand smoke exposure among children with asthma |
| Swartz 2006 | Individually tailored web‐based smoking cessation programme |
| Taylor 2010 | Before‐after assessment without control group |
| Thomas 2010 | Evaluation of intervention without control group |
| Vallone 2011 | Before‐after assessment without control group |
| Webb 2010a | Experimental study of health risk communication with different message content and culturally specific framing |
| Wetter 2007 | Mass media used to create awareness of Spanish‐language smoking cessation services. Study of different formats of quit line counselling |
| Whitehead 2007 | Individually tailored print material |
| Wilson 2005 | Study compares the number of calls to quit line services after different campaigns, including 1 designed for Māori audience. Not relevant study design |
| Wilson 2010 | Cluster‐randomised trial with 3 arms. Only 1 site per arm |
| Wilson 2014 | Individually tailored, interactive computer programme. Feasibility study without control group |
| Withall 2012 | Controlled before‐after study with only 1 intervention site and 1 control site. Not targeted to ethnic minority |
| Wolf 2009 | Not considered a mass media intervention |
| Wright 2013 | Individually tailored automated interactive voice response telephone counselling |
| Zhu 2012 | Not considered a mass media intervention |
Differences between protocol and review
The study protocol states that review authors should use the Cochrane 'Risk of bias' tool for RCTs (Higgins 2011). However, we used the risk of bias criteria proposed for EPOC reviews for all study designs according to the appropriate study specific criteria (EPOC 2015).
Contributions of authors
Annhild Mosdøl (AM), Ingeborg Beate Lidal (IBL), and Gunn Elisabeth Vist (GEV) drafted the protocol. Gyri Hval Straumann (GGS) developed the search strategy. AM, IBL, and GEV screened based title/abstract and full text. AM and GEV did the data extraction, 'Risk of bias' and GRADE assessment. AM wrote most of the review and all authors read and approved last version.
Sources of support
Internal sources
Norwegian Knowledge Centre for the Health Services, Norway.
The Norwegian Institute of Public Health, Norway.
External sources
No sources of support supplied
Declarations of interest
Mosdøl: none known. Lidal: none known. Straumann: none known. Vist: none known.
New
References
References to studies included in this review
Boyd 1998 {published data only}
- Boyd NR, Sutton C, Orleans CT, McClatchey MW, Bingler R, Fleisher L, et al. Quit Today! A targeted communications campaign to increase use of the Cancer Information Service by African American smokers. Preventive Medicine 1998;27(5 part 2):S50‐60. [DOI] [PubMed] [Google Scholar]
Elder 2005 {published data only}
- Baquero B, Ayala GX, Arredondo EM, Campbell NR, Slymen DJ, Gallo L, et al. Secretos de la Buena Vida: processes of dietary change via a tailored nutrition communication intervention for Latinas. Health Education Research 2009;24(5):855‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, Ayala GX, Campbell NR, Slymen D, Lopez‐Madurga ET, Engelberg M, et al. Interpersonal and print nutrition communication for a Spanish‐dominant Latino population: secretos de la buena vida. Health Psychology 2005;24(1):49‐57. [DOI] [PubMed] [Google Scholar]
- Elder JP, Ayala GX, Slymen DJ, Arredondo EM, Campbell NR. Evaluating psychosocial and behavioral mechanisms of change in a tailored communication intervention. Health Education & Behavior 2009;36(2):366‐80. [DOI] [PubMed] [Google Scholar]
Jih 2016 {published data only}
- Jih J, Le G, Woo K, Tsoh JY, Stewart S, Gildengorin G, et al. Educational interventions to promote healthy nutrition and physical activity among older Chinese Americans: a cluster‐randomized trial. American Journal of Public Health 2016;106(6):1092‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kennedy 2013 {published data only}
- Kennedy MG, Genderson MW, Sepulveda AL, Garland SL, Wilson DB, Stith‐Singleton R, et al. Increasing tobacco quitline calls from pregnant African American women: the "one tiny reason to quit" social marketing campaign. Journal of Women's Health 2013;22(5):432‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Risica 2013 {published data only}
- Risica PM, Gans KM, Kumanyika S, Kirtania U, Lasater TM. SisterTalk: final results of a culturally tailored cable television delivered weight control program for Black women. The International Journal of Behavioral Nutrition and Physical Activity 2013;10:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Webb 2009 {published data only}
- Webb MS. Culturally specific interventions for African American smokers: an efficacy experiment. Journal of the National Medical Association 2009;101(9):927‐35. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abroms 2014 {published data only}
- Abroms LC, Boal AL, Simmens SJ, Mendel JA, Windsor RA. A randomized trial of Text2Quit: a text messaging program for smoking cessation. American Journal of Preventive Medicine 2014;47(3):242‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aghi 1984 {published data only}
- Aghi MB, Grupta P, Mehta F. Intervention in the tobacco habits of rural Indian women. World Smoking & Health 1984;9(1):10‐4. [PubMed] [Google Scholar]
Albright 2009 {published data only}
- Albright CL, Maddock JE, Nigg CR. Increasing physical activity in postpartum multiethnic women in Hawaii: results from a pilot study. BMC Women's Health 2009;9(1):Art 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Albright 2012 {published data only}
- Albright CL, Steffen AD, Novotny R, Nigg CR, Wilkens LR, Saiki K, et al. Baseline results from Hawaii's Na Mikimiki Project: a physical activity intervention tailored to multiethnic postpartum women. Women & Health 2012;52(3):265‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alcalay 1999 {published data only}
- Alcalay R, Alvarado M, Balcazar H, Newman E, Ortiz G. Evaluation of a community‐based Latino heart disease prevention program in metropolitan Washington D.C. International Quarterly of Community Health Education 1999;19(3):191‐204. [Google Scholar]
Bermejo 2012 {published data only}
- Bermejo I, Frank F, Kriston L, Walter‐Hamann R, Harter M. Prevention of alcohol‐related disorders in elderly immigrants‐a cluster‐randomized controlled study. European Psychiatry 2012;27(Suppl 1):P422. [Google Scholar]
Block 2004 {published data only}
- Block G, Wakimoto P, Metz D, Fujii ML, Feldman N, Mandel R, et al. A randomized trial of the Little by Little CD‐ROM: demonstrated effectiveness in increasing fruit and vegetable intake in a low‐income population. Preventing Chronic Disease 2004;1(3):A08. [PMC free article] [PubMed] [Google Scholar]
Brady 2010 {published data only}
- Brady TJ, Lam J. Impact of Buenos Dias, artritis, a Spanish health communications campaign promoting physical activity among Spanish‐speaking people with arthritis. Arthritis and Rheumatism 2010;62(Suppl 10):1465. [Google Scholar]
Bramley 2005 {published data only}
- Bramley D, Riddell T, Whittaker R, Corbett T, Lin RB, Wills M, et al. Smoking cessation using mobile phone text messaging is as effective in Maori as non‐Maori. New Zealand Medical Journal 2005;118(1216):74‐83. [PubMed] [Google Scholar]
Brimblecombe 2013 {published data only}
- Brimblecombe J, Ferguson M, Liberato SC, Ball K, Moodie ML, Magnus A, et al. Stores Healthy Options Project in Remote Indigenous Communities (SHOP@RIC): a protocol of a randomised trial promoting healthy food and beverage purchases through price discounts and in‐store nutrition education. BMC Public Health 2013;13:744. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2012 {published data only}
- Brown DL, Conley KM, Resnicow K, Murphy J, Sanchez BN, Cowdery JE, et al. Stroke Health and Risk Education (SHARE): design, methods, and theoretical basis. Contemporary Clinical Trials 2012;33(4):721‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buis 2013 {published data only}
- Buis LR, Hirzel L, Turske SA, Jardins TRD, Yarandi H, Bondurant P. Use of a text message program to raise type 2 diabetes risk awareness and promote health behavior change (part I): assessment of participant reach and adoption. Journal of Medical Internet Research 2013;15(12):e282. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buller 2008 {published data only}
- Buller DB, Woodall WG, Zimmerman DE, Slater MD, Heimendinger J, Waters E, et al. Randomized trial on the 5 a day, the Rio Grande way website, a web‐based program to improve fruit and vegetable consumption in rural communities. Journal of Health Communication 2008;13(3):230‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burger 2003 {published data only}
- Burger J, McDermott MH, Chess C, Bochenek E, Perez‐Lugo M, Pflugh KK. Evaluating risk communication about fish consumption advisories: efficacy of a brochure versus a classroom lesson in Spanish and English. Risk Analysis 2003;23(4):791‐803. [DOI] [PubMed] [Google Scholar]
Burns 2010 {published data only}
- Burns EK, Levinson AH. Reaching Spanish‐speaking smokers: state‐level evidence of untapped potential for QuitLine utilization. American Journal of Public Health 2010;100(Suppl 1):S165‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2004 {published data only}
- Campbell MK, James A, Hudson MA, Carr C, Jackson E, Oates V, et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychology 2004;23(5):492‐502. [DOI] [PubMed] [Google Scholar]
Campbell 2014 {published data only}
- Campbell MA, Finlay S, Lucas K, Neal N, Williams R. Kick the habit: a social marketing campaign by Aboriginal communities in NSW. Australian Journal of Primary Health 2014;20(4):327‐33. [DOI] [PubMed] [Google Scholar]
Cantrell 2013 {published data only}
- Cantrell J, Vallone DM, Thrasher JF, Nagler RH, Feirman SP, Muenz LR, et al. Impact of tobacco‐related health warning labels across socioeconomic, race and ethnic groups: results from a randomized web‐based experiment. PLOS ONE 2013;8(1):e52206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carlini 2008 {published data only}
- Carlini BH, Zbikowski SM, Javitz HS, Deprey TM, Cummins SE, Zhu SH. Telephone‐based tobacco‐cessation treatment. Re‐enrollment among diverse groups. American Journal of Preventive Medicine 2008;35(1):73‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cessnun 2011 {published data only}
- Cessnun K, Dennisuk L, Coutinho A, Sharma S, Shin A, Christiansen K, et al. Environmental change program associated with relative decrease in frequency of carryout/fast food consumption among African American caregivers. FASEB Journal 2011;25:974.15. [Google Scholar]
Chang 2010 {published data only}
- Chang MW, Nitzke S, Brown R. Design and outcomes of a "Mothers In Motion" behavioral intervention pilot study. Journal of Nutrition Education and Behavior 2010;42(3):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chang 2014 {published data only}
- Chang MW, Nitzke S, Brown R, Resnicow K. A community based prevention of weight gain intervention (Mothers In Motion) among young low‐income overweight and obese mothers: design and rationale. BMC Public Health 2014;14:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chhichhia 2011 {published data only}
- Chhichhia P, Khan F A, Kumar E, Young N. Culturally tailored education to South Asian (SA) populations in Auckland successfully promotes early screening and prevention of cardiovascular diseases (CVD) and diabetes. Obesity Research and Clinical Practice 2011;5(Suppl 1):S59. [Google Scholar]
Chung 2014 {published data only}
- Chung A. An online evaluation of a website featuring a brief electronic media e‐health educational intervention to increase fruit and vegetable intake and physical activity among African American mothers and children [PhD thesis]. New York (NY): Teachers College, Columbia University, 2013. [Google Scholar]
Collins 2014 {published data only}
- Collins TC, Dong F, Ablah E, Parra‐Medina D, Cupertino P, Rogers N, et al. Use of text messaging to motivate exercise in Latinos with one or more atherosclerotic risk factors: two pilot studies. Journal of General Internal Medicine 2014;29(1):S245‐6. [Google Scholar]
Cummins 2015 {published data only}
- Cummins SE, Wong S, Bonnevie E, Lee H, Goto CJ, Carrington JM, et al. A multistate Asian‐language tobacco quitline: addressing a disparity in access to care. American Journal of Public Health 2015;105(10):2150‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Darity 1997 {published data only}
- Darity WA, Tuthill RW, Winder AE, Cernada GP, Chen TTL, Buchanan DR, et al. A multi‐city community based smoking research intervention project in the African‐American population. International Quarterly of Community Health Education 1997;17(2):117‐30. [DOI] [PubMed] [Google Scholar]
Dedier 2014 {published data only}
- Dedier JJ, Wright JA, Friedman RH, Heeren T. Randomized controlled trial of a culturally adapted, automated telephone exercise coach to improve physical activity among hypertensive African‐Americans. Journal of General Internal Medicine 2014;29(1):S192‐3. [Google Scholar]
Dunton 2008 {published data only}
- Dunton GF, Robertson TP. A tailored internet‐plus‐email intervention for increasing physical activity among ethnically‐diverse women. Preventive Medicine: An International Journal Devoted to Practice and Theory 2008;47(6):605‐11. [DOI] [PubMed] [Google Scholar]
Emmons 2003 {published data only}
- Emmons KM, Stoddard AM, Gutheil C, Suarez EG, Lobb R, Fletcher R. Cancer prevention for working class, multi‐ethnic populations through health centers: the healthy directions study. Cancer Causes & Control 2003;14(8):727‐37. [DOI] [PubMed] [Google Scholar]
Ferguson 2015 {published data only}
- Ferguson M, Schapira MM, Wileyto EP. Targeted newsletters to promote cancer control in African Americans. Journal of General Internal Medicine 2015;30(2):S263‐S264. [Google Scholar]
Fitzgerald 2009 {published data only}
- Fitzgerald EM, Schweizer E. Using positive social norms marketing to reduce tobacco use by Hispanic/Latino women of child‐bearing age. Kentucky Nurse 2009;57(1):19. [Google Scholar]
Foster 2014 {published data only}
- Foster GD, Karpyn A, Wojtanowski AC, Davis E, Weiss S, Brensinger C, et al. Placement and promotion strategies to increase sales of healthier products in supermarkets in low‐income, ethnically diverse neighborhoods: a randomized controlled trial. American Journal of Clinical Nutrition 2014;99(6):1359‐68. [DOI] [PubMed] [Google Scholar]
Froelicher 2010 {published data only}
- Froelicher ES, Doolan D, Yerger VB, McGruder CO, Malone RE. Combining community participatory research with a randomized clinical trial: the Protecting the Hood Against Tobacco (PHAT) smoking cessation study. Heart & Lung 2010;39(1):50‐63. [DOI] [PubMed] [Google Scholar]
Fukuoka 2011 {published data only}
- Fukuoka Y, Komatsu J, Suarez L, Vittinghoff E, Haskell W, Noorishad T, et al. The mPED randomized controlled clinical trial: applying mobile persuasive technologies to increase physical activity in sedentary women protocol. BMC Public Health 2011;11:933. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gans 2016 {published data only}
- Gans KM, Gorham G, Risica PM, Dulin‐Keita A, Dionne L, Gao T, et al. A multi‐level intervention in subsidized housing sites to increase fruit and vegetable access and intake: rationale, design and methods of the 'Live Well, Viva Bien' cluster randomized trial. BMC Public Health 2016;16:521. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gerber 2009 {published data only}
- Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informatics Journal 2009;15(1):17‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gerber 2013 {published data only}
- Gerber BS, Schiffer L, Brown AA, Berbaum ML, Rimmer JH, Braunschweig CL, et al. Video telehealth for weight maintenance of African‐American women. Journal of Telemedicine & Telecare 2013;19(5):266‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gittelsohn 2012 {published data only}
- Gittelsohn J, He S, Kim E, Delrow B, Pardilla M. Healthy stores intervention associated with psychosocial improvements in adult American Indian consumers. FASEB Journal 2012;26. [Google Scholar]
Gittelsohn 2013 {published data only}
- Gittelsohn J, Kim EM, He S, Pardilla M. A food store‐based environmental intervention is associated with reduced BMI and improved psychosocial factors and food‐related behaviors on the Navajo nation. Journal of Nutrition 2013;143(9):1494‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glover 2013 {published data only}
- Glover M, Bosman A, Wagemakers A, Kira A, Paton C, Cowie N. An innovative team‐based stop smoking competition among Maori and Pacific Island smokers: rationale and method for the study and its evaluation. BMC Public Health 2013;13:1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Graham 2012 {published data only}
- Graham AL, Fang Y, Moreno JL, Streiff SL, Villegas J, Muñoz RF, et al. Online advertising to reach and recruit Latino smokers to an Internet cessation program: impact and costs. Journal of Medical Internet Research 2012;14(4):135‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gray 2012 {published data only}
- Gray LJ, Khunti K, Williams S, Goldby S, Troughton J, Yates T, et al. Let's prevent diabetes: study protocol for a cluster randomised controlled trial of an educational intervention in a multi‐ethnic UK population with screen detected impaired glucose regulation. Cardiovascular Diabetology 2012;11:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grigg 2008 {published data only}
- Grigg M, Waa A, Bradbrook SK. Response to an indigenous smoking cessation media campaign ‐ It's about wh(a)over‐barnau. Australian and New Zealand Journal of Public Health 2008;32(6):559‐64. [DOI] [PubMed] [Google Scholar]
Hammerback 2012 {published data only}
- Hammerback K, Felias‐Christensen G, Phelan EA. Evaluation of a telephone‐based physical activity promotion program for disadvantaged older adults. Preventing Chronic Disease 2012;9:E62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hanson 2012 {published data only}
- Hanson JD, Winberg A, Elliott A. Development of a media campaign on Fetal Alcohol Spectrum disorders for Northern Plains American Indian communities. Health Promotion Practice 2012;13(6):842‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Henderson 2012 {published data only}
- Henderson JA, Chubak J, O'Connell J, Ramos MC, Jensen J, Jobe JB, et al. Design of a randomized controlled trial of a web‐based intervention to reduce cardiovascular disease risk factors among remote reservation‐dwelling American Indian adults with type 2 diabetes. Journal of Primary Prevention 2012;33(4):209‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hind 2010 {published data only}
- Hind D, Scott EJ, Copeland R, Breckon JD, Crank H, Walters SJ, et al. A randomised controlled trial and cost‐effectiveness evaluation of "booster" interventions to sustain increases in physical activity in middle‐aged adults in deprived urban neighbourhoods. BMC Public Health 2010;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ho 2008 {published data only}
- Ho LS, Gittelsohn J, Rimal R, Treuth MS, Sharma S, Rosecrans A, et al. An integrated multi‐institutional diabetes prevention program improves knowledge and healthy food acquisition in northwestern Ontario First Nations. Health Education & Behavior 2008;35(4):561‐73. [DOI] [PubMed] [Google Scholar]
Houry 2010 {published data only}
- Houry D, Hankin A, Smith S, Daugherty J. Effectiveness of a problem‐targeted distribution of informational materials among African‐American women screened in an ED waiting room via a computer‐based system. Academic Emergency Medicine 2010;17(Suppl 1):S164‐5. [Google Scholar]
Huang 2015 {published data only}
- Huang LL, Thrasher JF, Jiang Y, Li Q, Fong GT, Chang Y, et al. Impact of the 'Giving Cigarettes is Giving Harm' campaign on knowledge and attitudes of Chinese smokers. Tobacco Control 2015;24:iv28‐iv34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Irvine 2004 {published data only}
- Irvine AB, Ary DV, Grove DA, Gilfillan‐Morton L. The effectiveness of an interactive multimedia program to influence eating habits. Health Education Research 2004;19(3):290‐305. [DOI] [PubMed] [Google Scholar]
Ivers 2006 {published data only}
- Ivers R, Castro A, Parfitt D, Bailie RS, D'Abbs PH, Richmond RL. Evaluation of a multi‐component community tobacco intervention in three remote Australian aboriginal communities. Australian and New Zealand Journal of Public Health 2006;30(2):132‐6. [DOI] [PubMed] [Google Scholar]
Jantz 2002 {published data only}
- Jantz C, Anderson J, Gould SM. Using computer‐based assessments to evaluate interactive multimedia nutrition education among low‐income predominantly Hispanic participants. Journal of Nutrition Education and Behavior 2002;34(5):252‐60. [DOI] [PubMed] [Google Scholar]
Jason 1988 {published data only}
- Jason LA, Tait E, Goodman D, Buckenberger L, Gruder CL. Effects of a televised smoking cessation intervention among low‐income and minority smokers. American Journal of Community Psychology 1988;16(6):863‐76. [DOI] [PubMed] [Google Scholar]
Jenkins 1997 {published data only}
- Jenkins CN, McPhee SJ, Le A, Pham GQ, Ha N‐T, Stewart S. The effectiveness of a media‐led intervention to reduce smoking among Vietnamese‐American men. American Journal of Public Health 1997;87(6):1031‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Joseph 2014 {published data only}
- Joseph RP, Pekmezi D, Cherrington A, Allison J, Durant N. Lessons learned from implementing 2 Internet‐enhanced physical activity interventions for African American women. Annals of Behavioral Medicine 2014;47(Suppl 1):S129. [Google Scholar]
Joseph 2015 {published data only}
- Joseph RP, Keller C, Adams MA, Ainsworth BE. Print versus a culturally‐relevant Facebook and text message delivered intervention to promote physical activity in African American women: a randomized pilot trial. BMC Women's Health 2015;15(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kandula 2014 {published data only}
- Kandula NR, Dave SS, Patel Y, Seguil PE, Chavez PJD, Kumar S, et al. Translating a heart disease lifestyle intervention for use in south Asian immigrant communities: preliminary results of a pilot randomized controlled trial. Journal of General Internal Medicine 2014;29(Suppl 1):S239. [Google Scholar]
Kim 2013 {published data only}
- Kim BH, Glanz K. Text messaging to motivate walking in older African Americans: a randomized controlled trial. American Journal of Preventive Medicine 2013;44(1):71‐5. [DOI] [PubMed] [Google Scholar]
Kreuter 2004 {published data only}
- Kreuter MW, Skinner CS, Steger‐May K, Holt CL, Bucholtz DC, Clark EM, et al. Responses to behaviorally vs culturally tailored cancer communication among African American women. American Journal of Health Behavior 2004;28(3):195‐207. [DOI] [PubMed] [Google Scholar]
Kreuter 2005 {published data only}
- Kreuter MW, Sugg‐Skinner C, Holt CL, Clark EM, Haire‐Joshu D, Fu Q, et al. Cultural tailoring for mammography and fruit and vegetable intake among low‐income African‐American women in urban public health centers. Preventive Medicine: An International Journal Devoted to Practice and Theory 2005;41(1):53‐62. [DOI] [PubMed] [Google Scholar]
LaChausse 2012 {published data only}
- LaChausse RG. My student body: effects of an Internet‐based prevention program to decrease obesity among college students. Journal of American College Health 2012;60(4):324‐30. [DOI] [PubMed] [Google Scholar]
Larsen 2014 {published data only}
- Larsen BA, Dunsiger S, Hartman S, Nodora J, Pekmezi DW, Marquez B, et al. Activo: assessing the feasibility of designing and implementing a physical activity intervention for Latino men. International Journal of Men's Health 2014;13(1):60‐71. [Google Scholar]
Larson 2009 {published data only}
- Larson CO, Schlundt DG, Patel K, Wang H, Beard K, Hargreaves MK. Trends in smoking among African‐Americans: a description of Nashville's REACH 2010 initiative. Journal of Community Health: The Publication for Health Promotion and Disease Prevention 2009;34(4):311‐20. [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
- Lee RE, Mama SK, Medina A, Orlando ER, McNeill L. SALSA : SAving Lives Staying Active to promote physical activity and healthy eating. Journal of Obesity 2011;2011:436509. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 1984 {published data only}
- Li VC, Coates TJ, Spielberg LA, Ewart CK, Dorfman S, Huster WJ. Smoking cessation with young women in public family planning clinics: the impact of physician messages and waiting room media. Preventive Medicine 1984;13(5):477‐89. [DOI] [PubMed] [Google Scholar]
Linares 2013 {published data only}
- Linares A, Mihos K. Effectiveness of a text message pilot program targeting low‐income Latinos' dietary behaviors. Journal of Nutrition Education & Behavior 2013;45(4 Suppl):s3‐4. [Google Scholar]
Lipkus 1999 {published data only}
- Lipkus IM, Lyna PR, Rimer BK. Using tailored interventions to enhance smoking cessation among African‐Americans at a community health center. Nicotine & Tobacco Research 1999;1(1):77‐85. [DOI] [PubMed] [Google Scholar]
Ma 2004 {published data only}
- Ma GX, Fleisher L, Gonzalez E, Edwards RL. Improving cancer awareness among Asian Americans using targeted and culturally appropriate media: a case study. Home Health Care Management & Practice 2004;17(1):39‐44. [Google Scholar]
Mackey 2015 {published data only}
- Mackey E, Schweitzer A, Hurtado ME, Hathway J, DiPietro L, Lei KY, et al. The feasibility of an e‐mail–delivered Intervention to improve nutrition and physical activity behaviors in African American college students. Journal of American College Health 2015;63(2):109‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Magoc 2009 {published data only}
- Magoc D. The evaluation of a web‐based physical activity intervention in a predominantly Hispanic college population [PhD thesis]. El Paso (TX): The University of Texas at El Paso, 2009:145. [Google Scholar]
Marin 1990 {published data only}
- Marin G, Marin BV, Perez‐Stable EJ, Sabogal F, Otero‐Sabogal R. Changes in information as a function of a culturally appropriate smoking cessation community intervention for Hispanics. American Journal of Community Psychology 1990;18(6):847‐64. [DOI] [PubMed] [Google Scholar]
Marin 1994 {published data only}
- Marin BV, Perez‐Stable EJ, Marin G, Hauck WW. Effects of a community intervention to change smoking behavior among Hispanics. American Journal of Preventive Medicine 1994;10(6):340‐7. [PubMed] [Google Scholar]
McAlister 1992 {published data only}
- McAlister AL, Ramirez AG, Amezcua C, Pulley LV, Stern MP, Mercado S. Smoking cessation in Texas‐Mexico border communities: a quasi‐experimental panel study. American Journal of Health Promotion 1992;6(4):274‐9. [DOI] [PubMed] [Google Scholar]
McDonnell 2011 {published data only}
- McDonnell DD, Kazinets G, Lee HJ, Moskowitz JM. An Internet‐based smoking cessation program for Korean Americans: results from a randomized controlled trial. Nicotine & Tobacco Research 2011;13(5):336‐43. [DOI] [PubMed] [Google Scholar]
Mead 2013 {published data only}
- Mead EL, Gittelsohn J, Roache C, Corriveau A, Sharma S. A community‐based, environmental chronic disease prevention intervention to improve healthy eating psychosocial factors and behaviors in indigenous populations in the Canadian Arctic. Health Education & Behavior 2013;40(5):592‐602. [DOI] [PubMed] [Google Scholar]
Mhurchu 2007 {published data only}
- Mhurchu CN, Blakely T, Wall J, Rodgers A, Jiang Y, Wilton J. Strategies to promote healthier food purchases: a pilot supermarket intervention study. Public Health Nutrition 2007;10(6):608‐15. [DOI] [PubMed] [Google Scholar]
Mhurchu 2010 {published data only}
- Mhurchu NC, Blakely T, Jiang Y, Eyles HC, Rodgers A. Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. American Journal of Clinical Nutrition 2010;91(3):736‐47. [DOI] [PubMed] [Google Scholar]
Migneault 2012 {published data only}
- Migneault JP, Dedier JJ, Wright JA, Heeren T, Campbell MK, Morisky DE, et al. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African‐Americans: a randomized controlled trial. Annals of Behavioral Medicine 2012;43(1):62‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moskowitz 2016 {published data only}
- Moskowitz JM, McDonnell DD, Kazinets G, Lee HJ. Online smoking cessation program for Korean Americans: randomized trial to test effects of incentives for program completion and interim surveys. Preventive Medicine 2016;86:70‐6. [DOI] [PubMed] [Google Scholar]
Muñoz 1997 {published data only}
- Muñoz RF, Marín BV, Posner SF, Pérez‐Stable EJ. Mood management mail intervention increases abstinence rates for Spanish‐speaking Latino smokers. American Journal of Community Psychology 1997;25(3):325‐43. [DOI] [PubMed] [Google Scholar]
Muñoz 2006 {published data only}
- Muñoz RF, Lenert LL, Delucchi K, Stoddard J, Perez JE, Penilla C, et al. Toward evidence‐based Internet interventions: a Spanish/English website for international smoking cessation trials. Nicotine and Tobacco Research 2006;8(1):77‐87. [DOI] [PubMed] [Google Scholar]
Nollen 2007 {published data only}
- Nollen N, Ahluwalia JS, Mayo MS, Richter K, Choi WS, Okuyemi KS, et al. A randomized trial of targeted educational materials for smoking cessation in African Americans using transdermal nicotine. Health Education & Behavior 2007;34(6):911‐27. [DOI] [PubMed] [Google Scholar]
Orleans 1998 {published data only}
- Orleans CT, Boyd NR, Bingler R, Sutton C, Fairclough D, Heller D, et al. A self‐help intervention for African American smokers: tailoring cancer information service counseling for a special population. Preventive Medicine 1998;27(5 part 1):S61‐70. [DOI] [PubMed] [Google Scholar]
Patten 2010 {published data only}
- Patten CA, Windsor RA, Renner CC, Enoch C, Hochreiter A, Nevak C, et al. Feasibility of a tobacco cessation intervention for pregnant Alaska Native women. Nicotine and Tobacco Research 2010;12(2):79‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patten 2012 {published data only}
- Patten CA. Tobacco cessation intervention during pregnancy among Alaska Native women. Journal of Cancer Education 2012;27(1 Suppl):S86‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pekmezi 2010 {published data only}
- Pekmezi DW, Williams DM, Dunsiger S, Jennings EG, Lewis BA, Jakicic JM, et al. Feasibility of using computer‐tailored and internet‐based interventions to promote physical activity in underserved populations. Telemedicine Journal & E‐Health 2010;16(4):498‐503. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perez 2009 {published data only}
- Perez GA. Motivation for Physical Activity in Older Hispanic Women [PhD thesis]. Tempe (AZ): Arizona State University, 2009. [Google Scholar]
Reininger 2015 {published data only}
- Reininger BM, Mitchell‐Bennett L, Lee M, Gowen RZ, Barroso CS, Gay JL, et al. Tu Salud, Sí Cuenta!: Exposure to a community‐wide campaign and its associations with physical activity and fruit and vegetable consumption among individuals of Mexican descent. Social Science & Medicine 2015;143:98‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Resnicow 1997 {published data only}
- Resnicow K, Vaughan R, Futterman R, Weston RE, Royce J, Parms C, et al. A self‐help smoking cessation program for inner‐city African Americans: results from the Harlem health connection project. Health Education & Behavior 1997;24(2):201‐17. [DOI] [PubMed] [Google Scholar]
Resnicow 2000 {published data only}
- Resnicow K, Wallace DC, Jackson A, Digirolamo A, Odom E, Wang T, et al. Dietary change through African American churches: baseline results and program description of the Eat for Life trial. Journal of Cancer Education 2000;15(3):156‐63. [DOI] [PubMed] [Google Scholar]
Resnicow 2001 {published data only}
- Resnicow K, Jackson A, Wang T, De AK, McCarty F, Dudley WN, et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: Results of the Eat for Life trial. American Journal of Public Health 2001;91(10):1686‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Resnicow 2002 {published data only}
- Resnicow K, Jackson A, Braithwaite R, DiIorio C, Blisset D, Rahotep S, et al. Healthy Body/Healthy Spirit: a church‐based nutrition and physical activity intervention. Health Education Research 2002;17(5):562‐73. [DOI] [PubMed] [Google Scholar]
Resnicow 2005 {published data only}
- Resnicow K, Jackson A, Blissett D, Wang T, McCarty F, Rahotep S, et al. Results of the healthy body healthy spirit trial. Health Psychology 2005;24(4):339‐48. [DOI] [PubMed] [Google Scholar]
Resnicow 2008 {published data only}
- Resnicow K, Davis RE, Zhang G, Konkel J, Strecher VJ, Shaikh AR, et al. Tailoring a fruit and vegetable intervention on novel motivational constructs: results of a randomized study. Annals of Behavioral Medicine 2008;35(2):159‐69. [DOI] [PubMed] [Google Scholar]
Resnicow 2009 {published data only}
- Resnicow K, Davis R, Zhang N, Strecher V, Tolsma D, Calvi J, et al. Tailoring a Fruit and Vegetable Intervention on Ethnic Identity: Results of a Randomized Study. Health Psychology 2009;28(4):394‐403. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rimmer 2009 {published data only}
- Rimmer JH, Rauworth A, Wang E, Heckerling PS, Gerber BS. A randomized controlled trial to increase physical activity and reduce obesity in a predominantly African American group of women with mobility disabilities and severe obesity. Preventive Medicine 2009;48(5):473‐9. [DOI] [PubMed] [Google Scholar]
Romero 2012 {published data only}
- Romero Z. An evaluation of a marketing campaign on self‐management skills to enhance Hispanics' propensity to engage in physical activity, better nutritional habits and stress management [PhD thesis]. Denton (TX): Texas Woman's University, 2012. [Google Scholar]
Schlundt 2009 {published data only}
- Schlundt DG, Larson C, Patel K, Beard K, Hargreaves MK. Nashville REACH 2010: Association of community health promotion with population prevalence estimates of BMI, physical activity, and eating behaviors. Diabetes 2009;58. [Google Scholar]
Scisney‐Matlock 2012 {published data only}
- Scisney‐Matlock M, Steigerwalt S, Pressler S, Jamerson K, Ritter N. Wheels‐I computer‐mediated program using dash diet sustains improved BP at 1 year in African American women. Journal of Clinical Hypertension 2012;14. [Google Scholar]
Shaikh 2011 {published data only}
- Shaikh AR, Vinokur AD, Yaroch AL, Williams GC, Resnicow K. Direct and mediated effects of two theoretically based interventions to increase consumption of fruits and vegetables in the Healthy Body Healthy Spirit trial. Health Education & Behavior 2011;38(5):492‐501. [DOI] [PubMed] [Google Scholar]
Shakeshaft 2014 {published data only}
- Shakeshaft A, Doran C, Petrie D, Breen C, Havard A, Abudeen A, et al. The effectiveness of community action in reducing risky alcohol consumption and harm: a cluster randomised controlled trial. PLOS Medicine/Public Library of Science 2014;11(3):e1001617. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharma 2010 {published data only}
- Sharma S, Gittelsohn J, Rosol R, Beck L. Addressing the public health burden caused by the nutrition transition through the Healthy Foods North nutrition and lifestyle intervention programme. Journal of Human Nutrition and Dietetics 2010;23(Suppl 1):120‐7. [DOI] [PubMed] [Google Scholar]
Shea 1996 {published data only}
- Shea S, Basch CE, Wechsler H, Lantigua R. The Washington Heights‐Inwood Healthy Heart Program: a 6‐year report from a disadvantaged urban setting. American Journal of Public Health 1996;86(2):166‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Skewes 2007 {published data only}
- Skewes MC. Utep women kick butt! development, implementation, and evaluation of a web‐based smoking cessation intervention targeted to Hispanic female college students (Texas). Dissertation Abstracts International: Section B: The Sciences and Engineering 2007;67(11B):6727. [Google Scholar]
Steinberg 2013 {published data only}
- Steinberg DM, Levine EL, Askew S, Foley P, Bennett GG. Daily text messaging for weight control among racial and ethnic minority women: randomized controlled pilot study. Journal of Medical Internet Research 2013;15(11):e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stevens 2002 {published data only}
- Stevens W, Thorogood M, Kayikki S. Cost‐effectiveness of a community anti‐smoking campaign targeted at a high risk group in London. Health Promotion International 2002;17(1):43‐50. [DOI] [PubMed] [Google Scholar]
Streja 2014 {published data only}
- Streja L, Crespi CM, Bastani R, Wong GC, Jones CA, Bernert JT, et al. Can a minimal intervention reduce secondhand smoke exposure among children with asthma from low income minority families? Results of a randomized trial. Journal of Immigrant & Minority Health 2014;16(2):256‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Swartz 2006 {published data only}
- Swartz LH, Noell JW, Schroeder SW, Ary DV. A randomised control study of a fully automated internet based smoking cessation programme. Tobacco Control 2006;15(1):7‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2010 {published data only}
- Taylor DM, Chan A, Rae J, Kakegamic C, Fiddler R, Fiddler W, et al. Evaluation of a community‐wide primary stroke prevention program for the remote First Nation community of Sandy Lake. Stroke 2010;41(7):e488‐9. [Google Scholar]
Thomas 2010 {published data only}
- Thomas KB, Hauser K, Rodriguez NY, Quinn GP. Folic acid promotion for Hispanic women in Florida: a vitamin diary study. Health Education Journal 2010;69(3):344‐52. [Google Scholar]
Vallone 2011 {published data only}
- Vallone DM, Niederdeppe J, Richardson AK, Patwardhan P, Niaura R, Cullen J. A national mass media smoking cessation campaign: effects by race/ethnicity and education. American Journal of Health Promotion 2011;25(5 Suppl):S38‐50. [DOI] [PubMed] [Google Scholar]
Webb 2010a {published data only}
- Webb MS, Baker EA, Rodríguez de Ybarra D. Effects of culturally specific cessation messages on theoretical antecedents of behavior among low‐income African American smokers. Psychology of Addictive Behaviors 2010;24(2):333‐41. [DOI] [PubMed] [Google Scholar]
Wetter 2007 {published data only}
- Wetter DW, Mazas C, Daza P, Nguyen L, Fouladi RT, Li YS, et al. Reaching and treating Spanish‐speaking smokers through the National Cancer Institute's Cancer Information Service ‐ a randomized controlled trial. Cancer 2007;109(2):406‐13. [DOI] [PubMed] [Google Scholar]
Whitehead 2007 {published data only}
- Whitehead D, Bodenlos JS, Cowles ML, Jones GN, Brantley PJ. A stage‐targeted physical activity intervention among a predominantly African‐American low‐income primary care population. American Journal of Health Promotion 2007;21(3):160‐3. [DOI] [PubMed] [Google Scholar]
Wilson 2005 {published data only}
- Wilson N, Grigg M, Graham L, Cameron G. The effectiveness of television advertising campaigns on generating calls to a national Quitline by Mãori. Tobacco Control 2005;14(4):284‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2010 {published data only}
- Wilson DK, Trumpeter NN, George SM, Coulon SM, Griffin S, Lee Van Horn M, et al. An overview of the "Positive Action for Today's Health" (PATH) trial for increasing walking in low income, ethnic minority communities. Contemporary Clinical Trials 2010;31(6):624‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2014 {published data only}
- Wilson DK, Alia KA, Kitzman‐Ulrich H, Resnicow K. A pilot study of the effects of a tailored web‐based intervention on promoting fruit and vegetable intake in African American families. Childhood Obesity 2014;10(1):77‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Withall 2012 {published data only}
- Withall J, Jago R, Fox K R. The effect a of community‐based social marketing campaign on recruitment and retention of low‐income groups into physical activity programmes ‐ a controlled before‐and‐after study. Bmc Public Health 2012;12:836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolf 2009 {published data only}
- Wolf RL, Lepore SJ, Vandergrift JL, Basch CE, Yaroch AL. Tailored telephone education to promote awareness and adoption of fruit and vegetable recommendations among urban and mostly immigrant black men: a randomized controlled trial. Preventive Medicine: An International Journal Devoted to Practice and Theory 2009;48(1):32‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wright 2013 {published data only}
- Wright JA, Phillips BD, Watson BL, Newby PK, Norman GJ, Adams WG. Randomized trial of a family‐based, automated, conversational obesity treatment program for underserved populations. Obesity 2013;21(9):E369‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhu 2012 {published data only}
- Zhu SH, Cummins SE, Wong S, Gamst AC, Tedeschi GJ, Reyes‐Nocon J. The effects of a multilingual telephone quitline for Asian smokers: a randomized controlled trial. Journal of the National Cancer Institute 2012;104(4):299‐310. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Acevedo‐Garcia 2012
- Acevedo‐Garcia D, Sanchez‐Vaznaugh EV, Viruell‐Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: a cross‐national framework. Social Science & Medicine 2012;75(12):2060‐8. [DOI] [PubMed] [Google Scholar]
AHRQ 2013
- Agency for Healthcare Research and Quality (AHRQ). 2013 National Healthcare Quality Report. AHRQ Publication No. 14‐0005. Rockville: U.S. Department of Health and Human Services, 2013. [Google Scholar]
Alderete 1999
- Alderete EW. The Health of Indigenous Peoples. WHO/SDE/HSD/99.1. Geneva: World Health Organization, 1999. [Google Scholar]
Attridge 2014
- Attridge M, Creamer J, Ramsden M, Cannings‐John R, Hawthorne K. Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2014, Issue 9. [DOI: 10.1002/14651858.CD006424.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bala 2013
- Bala MM, Strzeszynski L, Topor‐Madry R, Cahill K. Mass media interventions for smoking cessation in adults. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD004704.pub3] [DOI] [PubMed] [Google Scholar]
Barrera 2013
- Barrera M Jr, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. Journal of Consulting and Clinical Psychology 2013;81(2):196‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berkman 2011
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Annals of Internal Medicine 2011;155(2):97‐107. [DOI] [PubMed] [Google Scholar]
Bernal 2009
- Bernal G, Jiménez‐Chafey MI, Domenech Rodríguez MM. Cultural adaptation of treatments: a resource for considering culture in evidence‐based practice. Professional Psychology: Research and Practice 2009;40(4):361‐68. [Google Scholar]
Bertrand 2006
- Bertrand JT, O'Reilly K, Denison J, Anhang R, Sweat M. Systematic review of the effectiveness of mass communication programs to change HIV/AIDS‐related behaviors in developing countries. Health Education Research 2006;21(4):567‐97. [DOI] [PubMed] [Google Scholar]
Bhopal 2007
- Bhopal RS. Ethnicity, Race, and Health in Multicultural Societies; Foundations for Better Epidemiology, Public Health, and Health Care. Oxford: Oxford University Press, 2007. [Google Scholar]
Brewer 2008
- Brewer NT, Rimer BK. Perspectives on health behavior theories that focus on individuals. In: Glanz K, Rimer BK, Viswanath K editor(s). Health Behavior and Health Education. Theory, Research, and Practice. 4th Edition. San Francisco: Jossey‐Bass, 2008:149‐65. [Google Scholar]
Brinn 2010
- Brinn MP, Carson KV, Esterman AJ, Chang AB, Smith BJ. Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews 2010, Issue 11. [DOI: 10.1002/14651858.CD001006.pub2] [DOI] [PubMed] [Google Scholar]
Buck 2012
- Buck D, Frosini F. Clustering of Unhealthy Behaviours Over Time. Implications for Policy and Practice. London: The King's Fund, 2012. [Google Scholar]
Carson 2012a
- Carson KV, Brinn MP, Peters M, Veale A, Esterman AJ, Smith BJ. Interventions for smoking cessation in Indigenous populations. Cochrane Database of Systematic Reviews 2012, Issue 1. [DOI: 10.1002/14651858.CD009046.pub2] [DOI] [PubMed] [Google Scholar]
Carson 2012b
- Carson KV, Brinn MP, Labiszewski NA, Peters M, Chang AB, Veale A, et al. Interventions for tobacco use prevention in Indigenous youth. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD009325.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
Castro 2010
- Castro FG, Barrera M Jr, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence‐based interventions. Annual Reviews of Clinical Psychology 2010;6:213‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clement 2013
- Clement S, Lassman F, Barley E, Evans‐Lacko S, Williams P, Yamaguchi S, et al. Mass media interventions for reducing mental health‐related stigma. Cochrane Database of Systematic Reviews 2013, Issue 7. [DOI: 10.1002/14651858.CD009453.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
CSDH 2008
- Commission on Social Determinants of Health (CSDH). Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization, 2008. [Google Scholar]
Davidson 2013a
- Davidson EM, Liu JJ, Bhopal RS, White M, Johnson MRD, Netto G, et al. Consideration of ethnicity in guidelines and systematic reviews promoting lifestyle interventions: a thematic analysis. European Journal of Public Health 2013;24(3):508‐13. [DOI] [PubMed] [Google Scholar]
Davidson 2013b
- Davidson AM, Liu JJ, Bhopal R, White M, Johnson MRD, Netto G, et al. Behaviour change interventions to improve the health of racial and ethnic minority populations: a tool kit of adaptation approaches. The Milbank Quarterly 2013;91(4):881‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2014
- Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychology Review 2014;8:1‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Bourdeaudhuij 2011
- Bourdeaudhuij I, Simon C, Meester F, Lenthe F, Spittaels H, Lien N, et al. Are physical activity interventions equally effective in adolescents of low and high socio‐economic status (SES): results from the European Teenage project. Health Education Research 2011;26(1):119‐30. [DOI] [PubMed] [Google Scholar]
Durkin 2012
- Durkin S, Brennan E, Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tobacco Control 2012;21(2):127‐38. [DOI] [PubMed] [Google Scholar]
Endnote 2015 [Computer program]
- Thomson Reuters. Endnote. Version X7.3. Philadelphia: Thomson Reuters, 2015.
EPOC 2013
- Effective Practice, Organisation of Care (EPOC). Interrupted time series (ITS) analyses. EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2013. Available from epoc.cochrane.org/epoc‐specific‐resources‐review‐authors.
EPOC 2015
- Effective Practice, Organisation of Care (EPOC). Suggested risk of bias criteria for EPOC reviews. EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2015. Available from epoc.cochrane.org/epoc‐specific‐resources‐review‐authors. Oslo: Norwegian Knowledge Centre for the Health Services.
EPOC 2016
- Effective Practice, Organisation of Care (EPOC). What study designs should be included in an EPOC review? EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2016. Available from epoc.cochrane.org/epoc‐specific‐resources‐review‐authors.
FCNM 2012
- Council of Europe. Framework Convention for the Protection of National Minorities (FCNM) Factsheet. 2012. www.coe.int/en/web/minorities/fcnm‐factsheet (accessed 30 April 2015).
Ferri 2013
- Ferri M, Allara E, Bo A, Gasparrini A, Faggiano F. Media campaigns for the prevention of illicit drug use in young people. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD009287.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
French 2010
- French J, Blair‐Stevens C. Key concepts and principles of social marketing. In: French J, Blair‐Stevens C, MvVey D, Merritt R editor(s). Social Marketing and Public Health. Theory and practice. Oxford: Oxford University Press, 2010:29‐44. [Google Scholar]
Gould 2013
- Gould GS, McEwen A, Watters T, Clough AR, Zwan R. Should anti‐tobacco media messages be culturally targeted for Indigenous populations? A systematic review and narrative synthesis. Tobacco Control 2013;22(4):e7. [DOI] [PubMed] [Google Scholar]
Grilli 2002
- Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD000389] [DOI] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 2011;64(4):380–2. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons, 2011. [Google Scholar]
Kreuter 2003
- Kreuter MK, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. American Journal of Health Behavior 2003;27(Suppl 3):S227‐32. [DOI] [PubMed] [Google Scholar]
Lim 2012
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair‐Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990‐2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2224‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2012
- Liu JJ, Davidson E, Bhopal RS, White M, Johnson MRD, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed‐methods evidence synthesis. Health Technology Assessment 2012;16(44). [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorenc 2013
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. Journal of Epidemiology and Community Health 2013;67(2):190‐3. [DOI] [PubMed] [Google Scholar]
Mackenbach 2008
- Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine 2008;358(23):2468‐81. [DOI] [PubMed] [Google Scholar]
McLeroy 1988
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly 1988;15(4):351‐77. [DOI] [PubMed] [Google Scholar]
Mulia 2008
- Mulia N, Ye Y, Zemore SE, Greenfield TK. Social disadvantage, stress, and alcohol use among black, Hispanic, and white Americans: findings from the 2005 U.S. National Alcohol Survey. Journal of Studies on Alcohol and Drugs 2008;69(6):824‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
MvVey 2010
- McVey D, Walsh L. Generating 'insight' and building segmentations ‐ moving beyond simple targeting. In: French J, Blair‐Stevens C, McVey D, Merritt R editor(s). Social Marketing and Public Health. Theory and Practice. Oxford: Oxford University Press, 2010:97‐122. [Google Scholar]
Nayar 2014
- Nayar US, Stangl AL, Zalduondo B, Brady LM. Reducing stigma and discrimination to improve child health and survival in low‐ and middle‐income countries: Promising approaches and implications for future research. Journal of Health Communication 2014;19:142‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nazroo 2003
- Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. American Journal of Public Health 2003;93(2):277‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Netto 2010
- Netto G, Bhopal R, Lederle N, Khatoon J, Jackson A. How can health promotion interventions be adapted for minority ethnic communities? Five principles for guiding the development of behavioural interventions. Health Promotion International 2010;25(2):248‐57. [DOI] [PubMed] [Google Scholar]
Niederdeppe 2008a
- Niederdeppe J, Fiore MC, Baker TB, Smith SS. Smoking‐cessation media campaigns and their effectiveness among socioeconomically advantaged and disadvantaged populations. American Journal of Public Health 2008;98(5):916‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niederdeppe 2008b
- Niederdeppe J, Kuang X, Crock B, Skelton A. Media campaigns to promote smoking cessation among socioeconomically disadvantaged populations: what do we know, what do we need to learn, and what should we do now?. Social Science & Medicine 2008;67(9):1343‐55. [DOI] [PubMed] [Google Scholar]
Nielsen 2010
- Nielsen SS, Krasnik A. Poorer self‐perceived health among migrants and ethnic minorities versus the majority population in Europe: a systematic review. International Journal of Public Health 2010;55(5):357‐71. [DOI] [PubMed] [Google Scholar]
Nierkens 2013
- Nierkens V, Hartman MA, Nicolaou M, Vissenberg C, Beune EJ, Hosper K, et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. a systematic review. PLOS ONE 2013;8(10):e73373. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oldroyd 2008
- Oldroyd J, Burns C, Lucas P, Haikerwal A, Waters E. The effectiveness of nutrition interventions on dietary outcomes by relative social disadvantage: a systematic review. Journal of Epidemiology and Community Health 2008;62(7):573‐9. [DOI] [PubMed] [Google Scholar]
Oxford Dictionaries
- Oxford Dictionaries. British & World English. Oxford University Press. www.oxforddictionaries.com/ (accessed 30 April 2015).
Ramsay 2003
- Ramsay CR, Matowe L, Grilli R, Grimshaw JM, Thomas RE. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. International Journal of Technology Assessment in Health Care 2003;19(4):613‐23. [DOI] [PubMed] [Google Scholar]
Resnicow 1999
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethnicity & Disease 1999;9(1):10‐21. [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rose 1985
- Rose G. Sick individuals and sick populations. International Journal of Epidemiology 1985;14(1):32‐8. [DOI] [PubMed] [Google Scholar]
Sorensen 2004
- Sorensen G, Barbeau E, Hunt MK, Emmons K. Reducing social disparities in tobacco use: a social‐contextual model for reducing tobacco use among blue‐collar workers. American Journal of Public Health 2004;94(2):230‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
SPFII 2004
- Secretariat of the Permanent Forum on Indigenous Issues (SPFII). The concept of Indigenous peoples. Background paper prepared by the Secretariat of the Permanent Forum on Indigenous Issues. 2004. www.un.org/esa/socdev/unpfii/documents/workshop_data_background.doc. New York: United Nations, (accessed 30 April 2015).
Stockley 2008
- Stockley L, Lund V. Use of folic acid supplements, particularly by low‐income and young women: a series of systematic reviews to inform public health policy in the UK. Public Health Nutrition 2008;11(8):807‐21. [DOI] [PubMed] [Google Scholar]
Thomas 2008
- Thomas S, Fayter D, Misso K, Ogilvie D, Petticrew M, Sowden A, et al. Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tobacco Control 2008;17(4):230‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tugwell 2010
- Tugwell P, Petticrew M, Kristjansson E, Welch V, Ueffing E, Waters E, et al. Assessing equity in systematic reviews: realising the recommendations of the Commission on Social Determinants of Health. BMJ 2010;341:c4739. [DOI] [PubMed] [Google Scholar]
Vidanapathirana 2006
- Vidanapathirana J, Abramson MJ, Forbes A, Fairley C. Mass media interventions for promoting HIV testing: Cochrane systematic review. International Journal of Epidemiology 2006;35(2):233‐4. [DOI] [PubMed] [Google Scholar]
Viruell‐Fuentes 2012
- Viruell‐Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Social Science & Medicine 2012;75(12):2099‐106. [DOI] [PubMed] [Google Scholar]
Viswanath 2006
- Viswanath K, Breen N, Meissner H, Moser RP, Hesse B, Steele WR, et al. Cancer knowledge and disparities in the information age. Journal of Health Communication 2006;11(Suppl 1):1‐17. [DOI] [PubMed] [Google Scholar]
Viswanath 2008
- Viswanath K. Perspectives on models of interpersonal health behavior. In: Glanz K, Rimer BK, Viswanath K editor(s). Health Behavior and Health Education. Theory, Research, and Practice. 4th Edition. San Francisco: Jossey‐Bass, 2008:271‐81. [Google Scholar]
Webb 2010b
- Webb MS, Rodríguez‐Esquivel D, Baker EA. Smoking cessation interventions among Hispanics in the United States: a systematic review and mini meta‐analysis. American Journal of Health Promotion 2010;25(2):109‐18. [DOI] [PubMed] [Google Scholar]
Welch 2012
- Welch V, Petticrew M, Tugwell P, Moher D, O'Neill J, Waters E, et al. PRISMA‐Equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLOS Medicine 2012;9(10):e1001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitehead 1992
- Whitehead M. The concepts and principles of equity and health. International Journal of Health Services 1992;22(3):429‐45. [DOI] [PubMed] [Google Scholar]
WHO 1986
- World Health Organization. The Ottawa Charter for Health Promotion. First International Conference on Health Promotion; 1986 Nov 21; Ottawa. www.who.int/healthpromotion/conferences/previous/ottawa/en/. Ottawa: World Health Organization, (accessed 30 April 2015).
WHO 2009
- World Health Organization. Interventions on Diet and Physical Activity: What Works. Summary Report. Geneva: World Health Organization, 2009. [PubMed] [Google Scholar]
WHO 2010
- World Health Organizaton. Global Status Report on Noncommunicable Diseases 2010. Geneva: World Health Organization, 2010. [Google Scholar]
WHO 2011
- World Health Organization. Rio Political Declaration on Social Determinants of Health. World Conference on Social Determinants of Health, 2011. www.who.int/sdhconference/declaration/en/ (accessed 30 April 2015).
WHO 2013a
- World Health Organization. Global Action Plan for the Prevention of Noncommunicable Diseases 2013‐2020. Geneva: World Health Organization, 2013. [Google Scholar]
WHO 2013b
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2013: Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship. Geneva: World Health Organization, 2013. [Google Scholar]
WHO 2014
- World Health Organization. Global Status Report on Alcohol and Health 2014. Geneva: World Health Organization, 2014. [Google Scholar]
References to other published versions of this review
Mosdøl 2015
- Mosdøl A, Lidal IB, Straumann GH, Vist GE. Targeted mass media interventions promoting healthy behaviours to reduce risk of non‐communicable diseases in adult, ethnic minorities.. Cochrane Database of Systematic Reviews 2015, Issue 5. [DOI: 10.1002/14651858.CD011683] [DOI] [PMC free article] [PubMed] [Google Scholar]


