Abstract
Background
Currently, the two most common surgical techniques for approaching the vas during vasectomy are the incisional method and the no‐scalpel technique. Whereas the conventional incisional technique involves the use of a scalpel to make one or two incisions, the no‐scalpel technique uses a sharp‐pointed, forceps‐like instrument to puncture the skin. The no‐scalpel technique aims to reduce adverse events, especially bleeding, bruising, hematoma, infection and pain and to shorten the operating time.
Objectives
The objective of this review was to compare the effectiveness, safety, and acceptability of the incisional versus no‐scalpel approach to the vas.
Search methods
In February 2014, we searched the computerized databases of CENTRAL, MEDLINE, POPLINE and LILACS. We looked for recent clinical trials in ClinicalTrials.gov and the International Clinical Trials Registry Platform. Previous searches also included in EMBASE. For the initial review, we searched the reference lists of relevant articles and book chapters.
Selection criteria
Randomized controlled trials and controlled clinical trials were included in this review. No language restrictions were placed on the reporting of the trials.
Data collection and analysis
We assessed all titles and abstracts located in the literature searches and two authors independently extracted data from the articles identified for inclusion. Outcome measures included safety, acceptability, operating time, contraceptive efficacy, and discontinuation. We calculated Peto odds ratios (OR) with 95% confidence intervals (CI) for the dichotomous variables.
Main results
Two randomized controlled trials evaluated the no‐scalpel technique and differed in their findings. The larger trial demonstrated less perioperative bleeding (OR 0.49; 95% CI 0.27 to 0.89) and pain during surgery (OR 0.75; 95% CI 0.61 to 0.93), scrotal pain (OR 0.63; 95% 0.50 to 0.80), and incisional infection (OR 0.21; 95% CI 0.06 to 0.78) during follow up than the standard incisional group. Both studies found less hematoma with the no‐scalpel technique (OR 0.23; 95% CI 0.15 to 0.36). Operations using the no‐scalpel approach were faster and had a quicker resumption of sexual activity. The smaller study did not find these differences; however, the study could have failed to detect differences due to a small sample size as well as a high loss to follow up. Neither trial found differences in vasectomy effectiveness between the two approaches to the vas.
Authors' conclusions
The no‐scalpel approach to the vas resulted in less bleeding, hematoma, infection, and pain as well as a shorter operation time than the traditional incision technique. No difference in effectiveness was found between the two approaches.
Plain language summary
Scalpel or no‐scalpel approach to the vas
Vasectomy is a surgical method used in men to cut or tie the vas deferens. The vas is a tube that delivers sperm from the testicles. The purpose of vasectomy is to provide permanent birth control. Usually the operation involves cutting the skin of the scrotum with a scalpel. A newer technique uses a sharp instrument to puncture the skin instead. The intent is to have fewer problems with bleeding, bruising, and infection. This review looked at whether the no‐scalpel approach to the vas worked as well as the scalpel method. It also studied any side effects of the methods and whether the men liked the method.
In February 2014, we did a computer search for studies comparing the no‐scalpel approach to the vas with the scalpel method. We included randomized controlled trials in any language. For the initial review, we also looked at reference lists of articles and book chapters.
We found two trials that looked at the no‐scalpel approach to the vas. The trials had somewhat different results. The larger trial showed the no‐scalpel method led to less bleeding, infection, and pain during and after the procedure. The no‐scalpel approach required less time for the operation and had a faster return to sexual activity. The smaller study did not show these differences. However, the study may have been too small and many men dropped out. The two methods did not differ in the numbers of men who became sterile.
Background
Currently, the two most common surgical techniques for approaching the vas during vasectomy are the incisional method and the no‐scalpel technique (Schwingl 2000). Whereas the conventional incisional technique involves the use of a scalpel to make one or two incisions (each 1 to 2 cm in length), the no‐scalpel technique uses a sharp, pointed, forceps‐like instrument to puncture the scrotum. The no‐scalpel technique, which was developed in China, aims to reduce adverse events, especially hematomas, bleeding, bruising, infection and pain, and to shorten the operating time. This method generally requires more training and skill than the conventional incisional method (RCOG 2004).
While adverse events following vasectomy are relatively uncommon (PIP 1992), men may experience bleeding, bruising, infection, acute and chronic pain after the procedure (RCOG 2004). The method of incision used to approach the vas can affect the occurrence of vasectomy‐related adverse events. The method of vas occlusion, though, is thought to be a stronger determinant of effectiveness than the method used to approach the vas (Goldstein 2002; RCOG 2004).
Evaluation of the relative effectiveness, safety and acceptability of these two approaches to the vas during vasectomy is vital to inform the decision making of both health service providers and clients. Ideally, choice of incision method for vasectomy should be based on the best available evidence from randomized controlled trials.
Objectives
The objective of this review was to compare the effectiveness, safety, acceptability and costs of scalpel versus no‐scalpel incision for vasectomy. The review does not address methods of occluding the vas, as that is the subject of another Cochrane review (Cook 2007).
Methods
Criteria for considering studies for this review
Types of studies
We included only randomized controlled trials in this review. No language restrictions were placed on the reporting of the trials.
Types of participants
Men of reproductive age undergoing vasectomy for sterilization.
Types of interventions
We examined two techniques for the approach to the vas for vasectomy: the no‐scalpel and the incisional method.
Types of outcome measures
We focused on clinically relevant outcome measures. We excluded studies evaluating possible long‐term vasectomy side effects (e.g., cancer, cardiovascular disease) or physiopathological outcomes only.
Primary outcomes
Post‐vasectomy adverse events including, but not limited to, the following: hematoma, scrotal abscess, wound infection, local pain and tenderness, reaction to suture material, bleeding, epididymo‐orchitis, chronic testicular/scrotal pain, congestive epidydymitis and vasovagal episodes.
Secondary outcomes
Operating time
Pain during surgery
Time to resumption of intercourse
Rates for azoospermia (no sperm detected) at post‐vasectomy follow‐up visits
Time to azoospermia
Pregnancy (contraceptive failure)
Incidence of recanalization
Incidence of repeat vasectomy
Cost analysis
Consumer acceptability measures
Provider acceptability measures.
Search methods for identification of studies
Electronic searches
In February 2014, we conducted computerized searches of the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE using PubMed, POPLINE and LILACS. In addition, we searched for recent clinical trials through ClinicalTrials.gov and the International Clinical Trials Registry Platform (ICTRP). The strategies are given in Appendix 1. The earlier strategies, which also included EMBASE, are shown in Appendix 2.
Searching other resources
For the initial review, we obtained relevant randomized and controlled trials from a search of publications describing vasectomy techniques for male sterilization. We searched the reference lists of all identified studies for additional, previously unidentified trials. Relevant book chapters and review articles were searched for all relevant trials. In addition, we attempted to find unpublished randomized controlled trials through personal communication with experts.
Data collection and analysis
Selection of studies
Two authors assessed the titles and abstracts from our literature search and evaluated copies of all possibly relevant articles to determine eligibility. Discrepancies were resolved by discussion.
Data extraction and management
Two authors independently collected the data under unblinded conditions (Berlin 1997). In addition to the outcome measures, we systematically extracted data on the following variables: loss to follow up, study duration, location of health care setting, experience level and number of surgeons, age of the men, total number of men included, inclusion and exclusion criteria, and method of vas occlusion. Discrepancies were resolved by discussion or by consulting a third author. When necessary, we contacted the authors of the trials to seek additional information. Correct entry of the data was verified by one other author.
Assessment of risk of bias in included studies
We assessed the methodological quality of the eligible articles as per Higgins 2005. The assessment of the validity of studies focused on the method of generating the allocation sequence, the use and method of allocation concealment, the use and method of blinding, exclusion of participants after randomization and loss to follow up.
Data synthesis
We calculated Peto odds ratios with 95% confidence intervals for dichotomous variables using the RevMan software. If the data did not permit entry into RevMan, we qualitatively described the findings in the text.
Results
Description of studies
After evaluation of the abstracts from the searches, we excluded articles that clearly were not randomized or controlled trials or did not focus on interventions or outcomes included in this review. We retrieved copies of 55 potentially relevant trials, of which two met the inclusion criteria (Sokal 1999; Christensen 2002). We excluded six reports (Black 1989; Nirapathpongporn 1990; Black 2003; Chen 2004; Chen 2005; Song 2006). No new studies have been found since the review was first published.
The two eligible studies compared similar interventions but differed in their timing and nature of post‐operative evaluations, including the evaluation of sterility. They also differed in operator experience with the no‐scalpel technique. No surgeon in the Christensen 2002 trial had substantial experience with the technique while some (3/8) in the Sokal 1999 trial were experienced with the method.
Christensen 2002 compared vasectomy with bilateral incision versus vasectomy with no‐scalpel approach to the vas. Outcome measures included vasectomy success (defined as azoospermia at three months post‐operation), duration of procedure, pain and discomfort immediately following the procedure using visual analog scales, adverse events, need for second doctor's assistance, and conversion to a different type of procedure. Participants were mailed a survey regarding pain and wound problems after one month, and they were to return after three months for semen analysis for establishing azoospermia. Semen analysis methods were not described.
Sokal 1999 compared vasectomy (small segment of the vas excised and ligated both ends) using a no‐scalpel incision versus vasectomy with a standard incision (i.e., a double vertical incision used in Guatemala and Semarang, Indonesia and a single vertical incisions in the remaining sites). Safety was the primary outcome measure. Other measures were ease of use, duration of procedure and sterility (defined as absence of live spermatozoa). A second measure of vasectomy effectiveness (i.e., failure) was determined at the surgeons' discretion without standardized criteria between centers. Participants were to return between 3 and 15 days for post‐operative evaluation and at 10 weeks for semen analysis. Semen analysis methods were not described. The vas occlusion technique in most cases was ligation (99.8% for the no‐scalpel and 99.6% for the standard incision group). Excision of the vas segment was completed for most participants (99.7% for the no‐scalpel and 99.9% for the incision group) and ligation of both ends of the vas was performed in 99.7% of all vasectomies. Sutures were used for wound closure in 2.2% of no‐scalpel and 28.9% of standard incision procedures.
Risk of bias in included studies
Christensen 2002 was a small (N=100) randomized controlled trial using sealed, sequentially‐numbered envelopes. Blinding was not reported for the outcome assessors or participants. Two randomization envelopes were opened by mistake (both for no‐scalpel arm) and were not replaced. One post‐randomization exclusion was reported (no‐scalpel arm) for a case with high testis due to inability to perform vasectomy under local anesthetic. Two men assigned to the no‐scalpel group were converted to bilateral incision during the procedure but, consistent with intent‐to‐treat principle, they were analyzed according to their randomized group (i.e., not treatment group). The study had a high loss to follow up at the one‐month survey (13%) and at the three‐month assessment for azoospermia (74%), which could have biased the study results greatly.
Sokal 1999 conducted a large randomized controlled trial (N=1429) using randomly‐generated numbers, and opaque, sealed envelopes to conceal the allocation process. Although the outcome assessor was blinded as to the group assignments, the participant blinding was unclear. After randomization, 35 men failed to receive their assigned type of incision due to allocation errors (N=17) or intraoperative obstacles (N=8). The primary analysis included participants with protocol violations, random allocation errors or technical failures (except for the exclusion of one technical failure that used different approaches on each vas). However, the analysis groups were based on the treatment received instead of the randomized assignment (N=705 for the no‐scalpel group and N=723 for the standard incision group). The follow‐up rates were about 77% for short‐term (at 15 days post‐vasectomy) and 91% for long‐term (after 15 days post‐vasectomy).
Both trials were conducted by non‐profit organizations.
Effects of interventions
Although the smaller study did not find any significant difference in perioperative bleeding (Christensen 2002), the no‐scalpel group in the larger trial (Sokal 1999) was half as likely to bleed during surgery as the scalpel group (OR 0.49; 95% CI 0.27 to 0.89). Furthermore, both studies found less hematoma during follow up for the men who received the no‐scalpel technique than those who had the standard incision (OR 0.23; 95% CI 0.15 to 0.36).
Christensen 2002 reported that the median operating times for the no‐scalpel and incisional groups (20 and 24 minutes, respectively) were not significantly different, but provided only the P value without any measure of the precision of the estimates. In contrast, the larger trial of Sokal 1999 showed that the no‐scalpel technique required less surgery time. The no‐scalpel group was more likely to have an operation time of 6 minutes or less (OR 2.37; 95% CI 1.92 to 2.91) and less likely to be 11 minutes or longer in duration (OR 0.56; 95% CI 0.43 to 0.73) than the incisional group (Sokal 1999). The 6 and 11 minute cut points, though, were selected post hoc.Christensen 2002 did not find significant differences between groups in perioperative difficulties (i.e., tight ductus, difficulty in identifying the ductus, hydrocele testis, need for assistance from a second operator). However, Sokal 1999 reported more difficulty isolating the vas (OR 1.80; 95% CI 1.18 to 2.76), short scrotum or thin deferens, and adhesions for this group compared to the scalpel group despite the shorter operation time with the no‐scalpel approach. The no‐scalpel group, though, was less likely to have (unspecified) equipment difficulties than the scalpel group (OR 0.28; 95% CI 0.10 to 0.77) (Sokal 1999). No statistically significant differences were observed for difficulty entering the scrotum, closing the incision, occluding the vas, difficulties due to fatty, adipose or fibrous tissue, chronic infection, pain or patient restlessness (only P value was provided) (Sokal 1999).
The no‐scalpel group was less likely to report perioperative pain than the incisional group (OR 0.75; 95% CI 0.61 to 0.93) in the larger trial (Sokal 1999). In contrast, the smaller study found no differences in visual analog scale scores for perioperative pain or discomfort between the two groups (Christensen 2002). Similarly, no differences in the reporting during follow up of general pain, scrotal pain or pain at ejaculation was found for the smaller study (Christensen 2002). In the larger trial (Sokal 1999), the no‐scalpel group was less likely to report scrotal pain (OR 0.63; 95% CI 0.50 to 0.80) than the standard incision group. The no‐scalpel group in the larger trial (Sokal 1999) also had less incisional infection during follow up than the scalpel group (OR 0.21; 95% CI 0.06 to 0.78). The smaller trial found no statistically significant difference in infection or wound problems (Christensen 2002). Pain or tenderness was the most common long‐term (i.e., at least 15 days post‐operation) side effect reported in Sokal 1999, but the outcome did not differ significantly between groups. Three men in each group in this trial required hospitalization during the follow‐up period, of which three complications appeared to be vasectomy‐related. Sokal 1999 also found a quicker resumption of sexual intercourse among the no‐scalpel than the incision group (P < 0.05 from Kaplan‐Meier survival estimate in article). In addition, nearly 90% of the participants in both groups reported that they were 'satisfied' or 'very satisfied' with the procedure.
In the smaller trial (Christensen 2002), microscopic analysis of resected tissue showed sufficient bilateral vasectomy from 98/99 surgeries. The exception was one case of vasectomy with bilateral incision, in which the operators had difficulty identifying the right‐sided ductus deferens during the surgery, and the microscopic analysis afterwards showed missing material. Only 26 of 99 patients (13 in each group) adhered to the study protocol of returning to provide semen samples at three months post‐operation. Two cases in the scalpel group and three cases in the no‐scalpel group were determined to be insufficient vasectomy. The larger trial (Sokal 1999) found similar rates of vasectomy success for the two groups whether measured as sterility (i.e., azoospermia) (OR 0.94; 95% CI 0.50 to 1.76) or the center‐specific evaluation of vasectomy failure (OR 0.87; 95% CI 0.37 to 2.07). The authors did not find evidence of interaction by clinical sites, and they also found almost identical results when they repeated the analysis using a per‐protocol population (i.e., excluding the 108 men with protocol violations, random allocation errors or technical failures).
Discussion
Men who received the no‐scalpel method in the Sokal 1999 trial had less bleeding, hematoma, infection and pain during surgery and follow up, but they had more surgical difficulties than those who had the incisional method. Despite having more surgical difficulties (i.e., short scrotum or thin deferens, adhesions and difficulties isolating the vas), the no‐scalpel group required a shorter operation time. Men who had the no‐scalpel technique also had a quicker resumption of sexual activity. These findings are consistent with results from large, non‐randomized studies that have documented fewer hematomas and infection, as well as a shorter operation time, with the no‐scalpel than with the scalpel approach (Nirapathpongporn 1990; Li 1991). The results are also consistent with the Labrecque 2004 review of this topic. The favorable results with the no‐scalpel technique are predicated upon good training, which should be standard for all surgical services.
In contrast, the Christensen 2002 trial reported few differences between the two approaches to the vas. The authors hypothesized that the lack of demonstrable benefits with the no‐scalpel technique in their study could have been due to operator inexperience with the method. Methodological differences between the two studies also could account for the inconsistencies. The Christensen 2002 trial was small (N=100) and could have been underpowered to detect differences. Furthermore, the trial had a high loss to follow up, which could have biased the results.
Neither trial found a difference between groups in vasectomy success. The rates in the Christensen 2002 trial are unreliable, though, because most participants (74%) failed to return at the three‐month post‐vasectomy visit to give a semen sample. The authors calculated an inaccurate azoospermia estimate by using the total number of randomized men as the denominator. The tacit assumption that the men who did not return for the three‐month follow‐up visit were azoospermic is untenable. Given the low follow‐up rate, we did not calculate an estimate of the relative effectiveness of the two methods for this trial. Furthermore, the authors did not report the vas occlusion techniques used despite their potential effect on the effectiveness of the procedure. Sokal 1999 had higher follow‐up rates for the 10‐week semen analysis (87%), and did not find a difference in the measures of sterility and vasectomy failure for the two groups.
Authors' conclusions
Implications for practice.
Compared to the traditional incision technique, the no‐scalpel approach to the vas resulted in less bleeding, hematoma, pain during or after the procedure, and infection, as well as a shorter operation time and a more rapid resumption of sexual activity. Although no difference in vasectomy effectiveness was found between the two approaches, the sample sizes might have been too small to detect actual differences.
Implications for research.
Since these results are based on one large trial, the evidence would be stronger if confirmed by a second trial. Effectiveness data were limited; however, the effectiveness of vasectomy is largely determined by the method of vas occlusion rather than the approach to the vas. The interpretation of future studies would be strengthened by the standardization of follow‐up protocols and statistical analysis methods. Researchers could also contribute by comparing the costs of the scalpel versus no‐scalpel techniques.
Feedback
Scalpel versus no‐scalpel incision for vasectomy
Summary
In their Implications for practice and Implications for research sections, the authors state: Although no difference in vasectomy effectiveness was found between the two approaches, the sample sizes might have been too small to detect actual differences.
Effectiveness is still unknown because the sample sizes might have been too small. Additional well‐conducted randomized trials would help answer this question. The interpretation of future studies would be strengthened by evaluation of vasectomy success and failure?
These statements are irrelevant to the No‐scalpel vasectomy approach to the vas. No‐scalpel vasectomy ( NSV ) is unfortunately a misnomer. NSV is exclusively a technique to approach and and extrude the vas out of the scrotum and has nothing to do with the occlusive and/or contraceptive efficacy/effectiveness of vasectomy which is determined by the occlusion technique performed ( e.g. ligation with suture material or metal clibs, excision of a vas segment, folding back of a vas segment, intraluminal cautery, and/or fascial interposition ). The authors should help correct this misunderstanding about vasectomy techniques for the sake of the health professional community and the general population.
I suggest they revise all statements implying any relation between NSV and vasectomy occlusive and/or contraceptive effectiveness and they clarify the two steps of vasectomy: 1) approaching/extruding the vas which has essentially no impact on success or failure of vasectomy, and 2) occluding the vas which determines vasectomy occlusive and contraceptive efficacy/effectiveness.
December 7, 2006
Reply
We thank Dr. Labrecque for his thoughtful comments. We agree that the no‐scalpel method is an approach to the vas and not a vasectomy method. The review generally refers to the no‐scalpel method or the no‐scalpel approach to the vas. The Abstract had an unfortunate typo in the Objective. We have edited the Abstract objective for consistency with the main text.
In the Background section, paragraph 2 notes that the method of occlusion was likely to be more important to effectiveness than the approach to vas. Paragraph 3 includes efficacy as one issue important to "inform the decision making of both health service providers and clients". The Cochrane Collaboration focuses on examining the best available evidence. Cochrane reviews help inform decision‐making, and consumers of such information are generally interested in effectiveness. Both Christensen 2002 and Sokal 1999 addressed effectiveness in their reports. In this review, effectiveness was a secondary outcome. Therefore, we have now decreased the emphasis on effectiveness in the Conclusions ( abstract and main text ) as well as in the last paragraph of the Discussion. We also edited the Plain Language Summary so it is consistent with these changes. In the conclusions ( Implications for research ), we have now restated the Background information about the occlusion method being more important than the approach to the vas.
January 10, 2007
Contributors
Michel Labrecque Laval University Quebec Canada
What's new
| Date | Event | Description |
|---|---|---|
| 8 February 2017 | Amended | Error corrected in Effects of interventions section, which now reads: the no‐scalpel group in the larger trial... was half as likely to bleed during surgery as the scalpel group (OR 0.49; 95% CI 0.27 to 0.89) |
| 27 February 2014 | Review declared as stable | Searches were updated; no new trials found. |
History
Protocol first published: Issue 2, 2003 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 13 October 2011 | New search has been performed | Searches were updated; no new trials found. |
| 9 March 2009 | New search has been performed | Updated searches; added searches of clinical trials databases. No new trials were found. |
| 15 April 2008 | Amended | Converted to new review format. |
| 9 January 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
From FHI 360:
Carol Manion assisted with the literature searches.
David Grimes and David Sokal reviewed the initial manuscript.
Florence Carayon helped with the searches and reviewed the search results in 2014.
Thanks to Dr Hugo Andreini, for advising us of an error in the text in the Effects of interventions section. The error was corrected and the amended review was republished in February 2017.
Appendices
Appendix 1. Search strategy 2014
CENTRAL (2011 to 21 Feb 2014)
vasectomy [in title, abstract, or keywords]
MEDLINE via PubMed (01 Jun 2011 to 21 Feb 2014)
(((sterilization, sexual AND (male OR men)) OR vasectomy) NOT (animal NOT human)) AND (Clinical Trial[ptyp])
POPLINE (2011 to 25 Feb 2014)
Keyword: Vasectomy
Filter by keywords: Research report
LILACS (2011 to 21 Feb 2014)
(men OR male OR hombres OR homens OR masculino) AND (sterilization, sexual OR esterilizacao sexual OR esterilizacion sexual) or vasectomy OR vasecomia [Words]
ClinicalTrials.gov (01 Jun 2011 to 18 Feb 2014)
Search term: vasectomy
ICTRP (01 Jun 2011 to 25 Feb 2014)
vasectomy (general search)
Appendix 2. Previous search strategies
2011
CENTRAL (2009 to 13 Oct 2011)
vasectomy [in title, abstract, or keywords]
MEDLINE via PubMed (Mar 2009 to 13 Oct 2011)
(((sterilization, sexual AND (male OR men)) OR vasectomy)) AND ((clinical trials OR random allocation OR double‐blind method OR single‐blind method OR research design OR comparative study OR evaluation studies OR follow‐up studies OR prospective studies OR intervention studies OR evaluation studies OR randomized controlled trial[pt] OR controlled clinical trial[pt] OR clinical trial[pt] OR ((singl* OR doubl* OR tripl* OR trebl*) AND (blind OR mask)) OR random OR latin square OR control* OR prospectiv* OR volunteer) NOT (animal NOT human))
POPLINE (13 Oct 2011 and past five years)
(clinical trials / comparative studies) & ((vas occlusion / vas ligation / vasectomy / male sterilization) NOT vas reanastomosis)
LILACS (13 Oct 2011)
(men OR male OR hombres OR homens OR masculino) AND (sterilization, sexual OR esterilizacao sexual OR esterilizacion sexual) [Words] or vasectomy OR vasecomia [Words] and 2009 OR 2010 OR 2011 [Country, year publication]
ClinicalTrials.gov (13 Oct 2011)
vasectomy
ICTRP (13 Oct 2011)
vasectomy
2009
CENTRAL (24 Feb 2009)
vasectomy [in title, abstract, or keywords]
MEDLINE via PubMed (06 Mar 2009)
(((sterilization, sexual AND (male OR men)) OR vasectomy)) AND ((clinical trials OR random allocation OR double‐blind method OR single‐blind method OR research design OR comparative study OR evaluation studies OR follow‐up studies OR prospective studies OR intervention studies OR evaluation studies OR randomized controlled trial[pt] OR controlled clinical trial[pt] OR clinical trial[pt] OR ((singl* OR doubl* OR tripl* OR trebl*) AND (blind OR mask)) OR random OR latin square OR control* OR prospectiv* OR volunteer) NOT (animal NOT human))
EMBASE (06 Mar 2009)
((((vasectomy OR male(w)sterilization OR (vas AND excision) OR ((vas(w)irrigation) OR (fascial AND interposition) OR (suture ligature(w)vas) OR (vas AND irrigation) OR (open‐ended AND vas) OR (surgical(w)clips AND vas) OR (electrocautery AND vas) OR (chemical(w)occlusion AND vas)) AND ((method OR methods) OR technique OR techniques))) AND human) NOT vasovasostomy
POPLINE (06 Mar 2009)
(clinical trials / comparative studies) & ((vas occlusion / vas ligation / vasectomy / male sterilization) NOT vas reanastomosis)
LILAC (06 Mar 2009)
(men OR male OR hombres OR homens OR masculino) AND (sterilization, sexual OR esterilizacao sexual OR esterilizacion sexual) [Words] or vasectomy OR vasecomia [Words] and 2006 OR 2007 OR 2008 OR 2009 [Country, year publication]
ClinicalTrials.gov (Feb 2009)
vasectomy
ICTRP (Feb 2009)
vasectomy
Data and analyses
Comparison 1. No‐scalpel versus standard incision.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Perioperative bleeding | 2 | 1534 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.59 [0.33, 1.04] |
| 2 Hematoma during follow up | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.15, 0.36] |
| 3 Operating time <=6 minutes | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.37 [1.92, 2.91] |
| 4 Operating time >=11 min | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.56 [0.43, 0.73] |
| 5 Perioperative difficulty in identifying ductus | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.54 [0.05, 5.30] |
| 6 Perioperative difficulty in isolating the vas | 1 | 1421 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.80 [1.18, 2.76] |
| 7 Perioperative equipment difficulties (unspecified) | 1 | 1456 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.10, 0.77] |
| 8 Perioperative need for assistance from second operator | 1 | 99 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.77 [0.67, 4.70] |
| 9 Perioperative pain | 1 | 1428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.75 [0.61, 0.93] |
| 10 Pain during follow up | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.43, 2.52] |
| 11 Pain or tenderness during long‐term follow up | 1 | 1272 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.46, 1.32] |
| 12 Scrotal pain during follow up | 2 | 1179 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.66 [0.52, 0.83] |
| 13 Pain at ejaculation during follow up | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.94 [0.49, 129.15] |
| 14 Infection during follow up | 2 | 1182 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.34 [0.13, 0.90] |
| 15 Wound problems during follow up | 1 | 86 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.51 [0.18, 1.47] |
| 16 Sterility | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.94 [0.50, 1.76] |
| 17 Vasectomy failure | 1 | 1239 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.37, 2.07] |
1.1. Analysis.
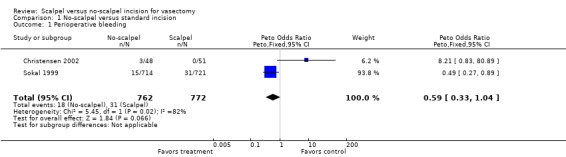
Comparison 1 No‐scalpel versus standard incision, Outcome 1 Perioperative bleeding.
1.2. Analysis.
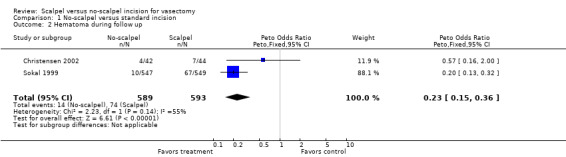
Comparison 1 No‐scalpel versus standard incision, Outcome 2 Hematoma during follow up.
1.3. Analysis.
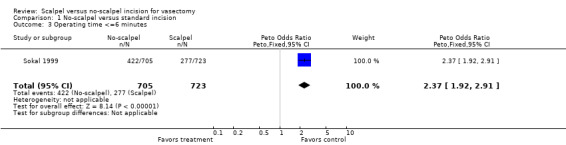
Comparison 1 No‐scalpel versus standard incision, Outcome 3 Operating time <=6 minutes.
1.4. Analysis.
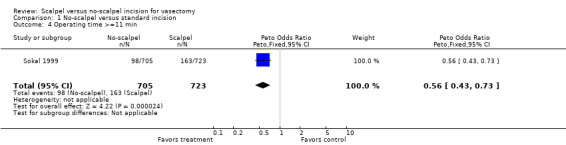
Comparison 1 No‐scalpel versus standard incision, Outcome 4 Operating time >=11 min.
1.5. Analysis.
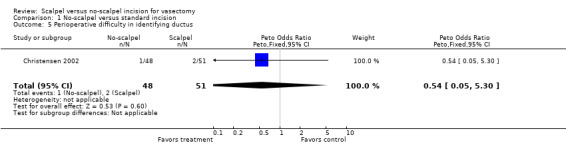
Comparison 1 No‐scalpel versus standard incision, Outcome 5 Perioperative difficulty in identifying ductus.
1.6. Analysis.
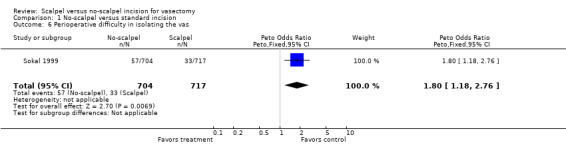
Comparison 1 No‐scalpel versus standard incision, Outcome 6 Perioperative difficulty in isolating the vas.
1.7. Analysis.
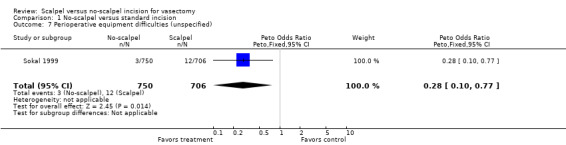
Comparison 1 No‐scalpel versus standard incision, Outcome 7 Perioperative equipment difficulties (unspecified).
1.8. Analysis.
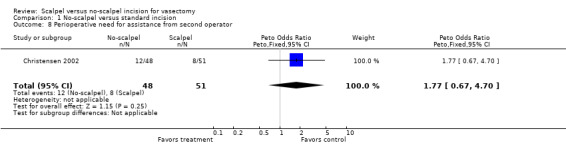
Comparison 1 No‐scalpel versus standard incision, Outcome 8 Perioperative need for assistance from second operator.
1.9. Analysis.
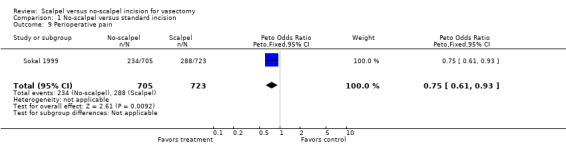
Comparison 1 No‐scalpel versus standard incision, Outcome 9 Perioperative pain.
1.10. Analysis.
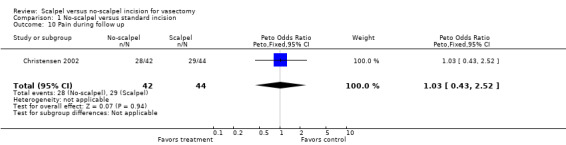
Comparison 1 No‐scalpel versus standard incision, Outcome 10 Pain during follow up.
1.11. Analysis.
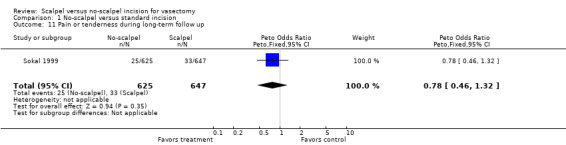
Comparison 1 No‐scalpel versus standard incision, Outcome 11 Pain or tenderness during long‐term follow up.
1.12. Analysis.
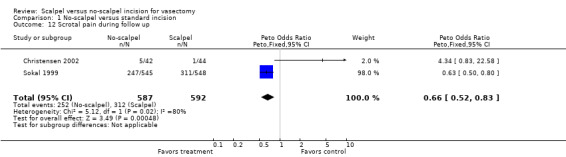
Comparison 1 No‐scalpel versus standard incision, Outcome 12 Scrotal pain during follow up.
1.13. Analysis.
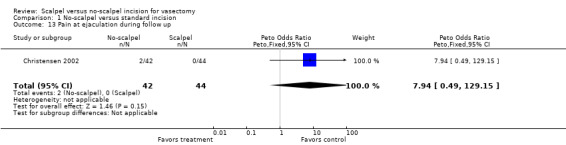
Comparison 1 No‐scalpel versus standard incision, Outcome 13 Pain at ejaculation during follow up.
1.14. Analysis.
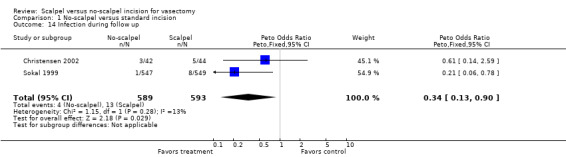
Comparison 1 No‐scalpel versus standard incision, Outcome 14 Infection during follow up.
1.15. Analysis.
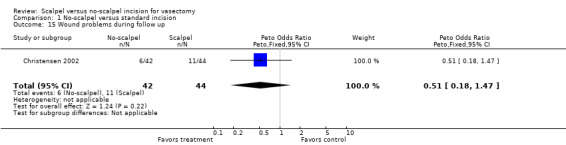
Comparison 1 No‐scalpel versus standard incision, Outcome 15 Wound problems during follow up.
1.16. Analysis.
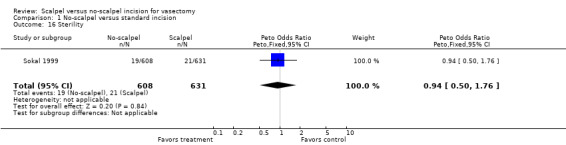
Comparison 1 No‐scalpel versus standard incision, Outcome 16 Sterility.
1.17. Analysis.
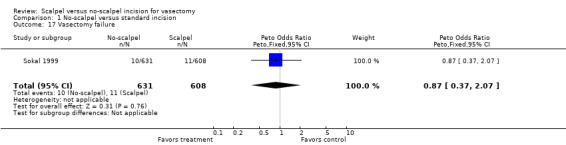
Comparison 1 No‐scalpel versus standard incision, Outcome 17 Vasectomy failure.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Christensen 2002.
| Methods | Randomization by marking 102 sheets with one of the methods (51 for each arm), which were sealed in sequentially‐numbered envelopes. Blinding was not reported for outcome assessor or the participants. Two randomization envelopes were opened by mistake (both for no‐scalpel arm) and were not replaced. One post‐randomization exclusion was reported (no‐scalpel arm) due to inability to perform vasectomy under local anesthetic because of a high testis. Two men assigned to no‐scalpel were converted to bilateral incision during the procedure. High lost to follow‐up rate for the one‐month survey (7 men in the incisional group and 7 men in the no‐scalpel group; 13%) and for the 3‐month assessment for azoospermia (13 men in each group; 74%). | |
| Participants | 100 participants aged 31 to 44 years at one site in Denmark from July 1998 to January 2000. The inclusion and exclusion criteria were not stated. | |
| Interventions | Vasectomy with bilateral incision (N=51) versus vasectomy with no‐scalpel approach to the vas (N=49). The methods of vas occlusion and anesthesia were not stated. | |
| Outcomes | The outcome measures included vasectomy success as defined as azoospermia at 3 months, duration of procedure, pain and discomfort (measured with Visual Analog Scales immediately following the procedure), adverse events, need for assistance from another doctor and conversion to another type of procedure. Participants were sent a survey at 1 month regarding pain and wound problems. Participants were to return at 3 months for semen analysis to establish azoospermia. Postoperatively, the resected tissues were sent for microscopic evaluation of the vasectomy. Semen analysis methods were not described. | |
| Notes | The paper was reported in Danish and translated into English. None of the 8 operators (senior resident or fellow) had substantial experience in the no‐scalpel technique. Training was limited to a viewing of an instructional video and one supervised procedure. Only one surgeon performed more than 10 no‐scalpel vasectomies in the trial. Analysis was according to intent‐to‐treat principle exception for one post‐randomization exclusion (due to inability to perform either procedure). The authors reported a priori sample size calculation, but it was based on unrealistic numbers (i.e., 80% power to detect a 19% difference in effect rates between groups at the 5% alpha level). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Sokal 1999.
| Methods | Randomized controlled trial using randomly generated numbers. Allocation concealment by opaque, sealed envelopes. Outcome evaluator blinded. Participant blinding unclear. Few men lost to follow up or excluded following randomization. Participants with protocol violations, random allocation errors or technical failure were included in the primary analysis. | |
| Participants | 1429 participants at 8 sites in 5 countries (Brazil, Guatemala, Indonesia, Sri Lanka, Thailand) from March 1988 to August 1991. The age range was not stated. Inclusion criteria were men in good health requesting vasectomy who were 21 years of age or greater. Some local eligibility criteria applied, such as in the Brazil site men were 30 to 40 years of age, had 2 live children, an 8th grade education and minimum monthly income, while Sri Lanka participants had to have 2 or more living children. Exclusion criteria included a history of excessive pain or swelling, abnormality or congenital anomaly and previous injury to or operation on the scrotum or testes, including any previous sterilization. | |
| Interventions | Vasectomy (small segment of the vas excised and ligated both ends) using a no‐scalpel incision (N=715) versus vasectomy (same technique) with a single or double vertical incision (N=714). Method of anesthesia was not stated. | |
| Outcomes | The primary outcome measure was safety. Secondary measures were ease of use, duration of procedure and effectiveness (sterility). Participants were to return between 3 and 15 days for post‐operative evaluation and at 10 weeks for semen analysis. Absence of live spermatozoa was considered proof of sterility. Failures were determined at surgeon discretion and criteria were not standardized among centers. Participants were encouraged to return whenever they had a problem related to surgery and until semen analysis showed no live spermatozoa or sterilization was declared. | |
| Notes | All 8 operators (general surgeons and urologists) had experience with the standard vasectomy technique while 3 had experience with the no‐scalpel technique. Inexperienced surgeons were trained in the no‐scalpel technique before the study. Analysis was not according to intent‐to‐treat principle since groups were based on treatment received (and not randomly‐assigned vasectomy method). The authors report a posteriori sample size calculation that had low power (65%) to detect a 3% difference in effect rates between the two groups at the 5% alpha level. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Black 1989 | Not a randomized controlled trial. |
| Black 2003 | Not a randomized controlled trial since treatment group was based on patient preference for date of operation. |
| Chen 2004 | Compared two no‐scalpel methods. |
| Chen 2005 | Duplicate publication of Chen 2004; compared two no‐scalpel methods. |
| Nirapathpongporn 1990 | Not a randomized controlled trial. |
| Song 2006 | Compared no‐scalpel method with intra‐vas device. |
Contributions of authors
A Pun and L Cook did the data abstraction. L Lopez reviewed the literature searches for the initial review, and updated the review from 2009 to 2014. All authors were involved in the review development and edited the initial manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
-
U.S. Agency for International Development, USA.
Support for conducting the review and updates at FHI 360 (through 2011)
-
National Institute of Child Health and Human Development, USA.
Support for conducting the review and updates at FHI 360 (through 2014)
Declarations of interest
L Lopez is employed at FHI 360 (formerly known as Family Health International) where one of the included trials was conducted (Sokal 1999). She was not involved in that trial.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Christensen 2002 {published data only}
- Christensen P, Al‐Aqidi OA, Jensen FS, Dorflinger T. Vasectomy. A prospective, randomized trial of vasectomy with bilateral incision versus the Li vasectomy [Vasektomi. Et prospektivt, randomiseret studie af vasektomi med dobbeltsidig incision vs. vasektomi a.m. Li]. Ugeskr Laeger 2002;164:2390‐4. [PubMed] [Google Scholar]
Sokal 1999 {published data only}
- Sokal D, McMullen S, Gates D, Dominik R. A comparative study of the no scalpel and standard incision approaches to vasectomy in 5 countries. The Male Sterilization Investigator Team. Journal of Urology 1999;162:1621‐5. [PubMed] [Google Scholar]
References to studies excluded from this review
Black 1989 {published data only}
- Black TR, Gates DS, Lavely K, Lamptey P. The percutaneous electrocoagulation vasectomy technique‐‐a comparative trial with the standard incision technique at Marie Stopes House, London. Contraception 1989;39:359‐68. [DOI] [PubMed] [Google Scholar]
Black 2003 {published data only}
- Erratum to Black 2003 article. Journal of Family Planning and Reproductive Health Care 2003; Vol. 29:159.
- Black T, Francome C. Comparison of Marie Stopes scalpel and electrocautery no‐scalpel vasectomy techniques. Journal of Family Planning and Reproductive Health Care 2003;29:32‐4. [DOI] [PubMed] [Google Scholar]
Chen 2004 {published data only}
- Chen KC. A novel instrument‐independent no‐scalpel vasectomy ‐ a comparative study against the standard instrument‐dependent no‐scalpel vasectomy. International Journal of Andrology 2004;27:222‐7. [DOI] [PubMed] [Google Scholar]
Chen 2005 {published data only}
- Chen KC, Peng CC, Hsieh HM Chiang HS. Simply modified no‐scalpel vasectomy (percutaneous vasectomy) ‐ a comparative study against the standard no‐scalpel vasectomy. Contraception 2005;71:153‐6. [DOI] [PubMed] [Google Scholar]
Nirapathpongporn 1990 {published data only}
- Nirapathpongporn A, Huber DH, Krieger JN. No‐scalpel vasectomy at the King's birthday vasectomy festival. Lancet 1990;335:894‐5. [DOI] [PubMed] [Google Scholar]
Song 2006 {published data only}
- Song L, Gu Y, Lu W, Liang X, Chen Z. A phase II randomized controlled trial of a novel male contraception, an intra‐vas device. International Journal of Andrology 2006;29(4):489‐95. [DOI] [PubMed] [Google Scholar]
Additional references
Berlin 1997
- Berlin JA. Does blinding of readers affect the results of meta‐analyses? University of Pennsylvania Meta‐analysis Blinding Study Group. Lancet 1997;350:185‐6. [DOI] [PubMed] [Google Scholar]
Cook 2007
- Cook LAA, Vliet HAAM, Lopez LM, Pun A, Gallo MF. Vasectomy occlusion techniques for male sterilization. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD003991] [DOI] [PubMed] [Google Scholar]
Goldstein 2002
- Goldstein M. Surgical management of male infertility and other scrotal disorders. In: Walsh PC, Retik AB, Vaughan ED, Wein AJ editor(s). Campbell's Urology. Eighth. Philadelphia: W.B. Saunders Co., 2002:1532‐1587. [Google Scholar]
Higgins 2005
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. www.cochrane.dk/cochrane/handbook/hbook.htm. John Wiley & Sons, Ltd, (accessed 1 June 2005).
Labrecque 2004
- Labrecque M, Dufresne C, Barone MA, St‐Hilaire K. Vasectomy surgical techniques: a systematic review. BioMed Central Medicine 2004:2. Available through the World Wide Web at http://www.biomedcentral.com/1741‐7015/2/21. [DOI] [PMC free article] [PubMed]
Li 1991
- Li SQ, Goldstein M, Zhu J, Huber D. The no‐scalpel vasectomy. Journal of Urology 1991;145:341‐4. [DOI] [PubMed] [Google Scholar]
PIP 1992
- Population Information Programme. Vasectomy: new opportunities. Population Reports 1992;Series D(No. 5):2‐6. [Google Scholar]
RCOG 2004
- Royal College of Obstetricians and Gynaecologists. Male and Female Sterilisation. Evidence‐Based Guideline No. 4. London: RCOG Press, 2004. [Google Scholar]
Schwingl 2000
- Schwingl PJ, Guess HA. Safety and effectiveness of vasectomy. Fertility and Sterility 2000;73:923‐36. [DOI] [PubMed] [Google Scholar]


