Abstract
Introduction
More than one-third of Oklahomans live in rural counties, and 63 of Oklahoma's 77 counties are classified as health professional shortage areas, where telemedicine would be beneficial. In response to this need, in 2012, the Colleges of Nursing and Allied Health at the University of Oklahoma Health Sciences Center implemented a sequence of interprofessional learning experiences to prepare nurse practitioner, physical therapy, and occupational therapy students in team-based geriatric care using telehealth technologies.
Methods
The sequence included modules on interprofessional competencies, a simulated patient case, and clinical experiences. This publication includes instructional materials and evaluation tools for replicating this sequence.
Results
Student responses to the guided reflection exercise provided a snapshot of their thoughts and reactions during this learning activity. Overall, their reflections suggested that they were highly motivated and actively thinking about how to work together effectively as a team to care for their standardized patient.
Discussion
This case is most applicable for educators who own telehealth equipment; however, a telehealth patient encounter could be simulated with other technologies.
Keywords: Geriatrics, Interprofessional, Telehealth
Educational Objectives
By the end of this learning activity, students should be able to:
-
1.
Practice working together effectively as a team to plan care for a geriatric patient using telehealth equipment.
-
2.
Identify the most important aspects of patient history and/or assessment that each discipline would perform.
-
3.
Actively communicate as an effective member of an interprofessional health care team.
-
4.
Demonstrate knowledge of how to conduct patient care using telehealth technology.
Introduction
For more than 2 decades, a growing body of evidence has demonstrated that care provided by highly functioning interprofessional teams results in better utilization of health care resources and improved patient outcomes.1–3 The key to teaching health science professionals how to practice quality team-based care is thought to be educating students together in what is termed interprofessional education (IPE).4,5
The goal of IPE is to teach students the skills related to the four core competencies for collaborative practice: values/ethics, roles/responsibilities, communication, and teams/teamwork.6 However, due to the multidimensional nature of the learning experience, implementing and evaluating the effectiveness of IPE programs has proven to be challenging.7,8 For example, the values/ethics competency includes a fairly broad set of skills and behaviors, such as putting the patient's needs first, respecting the cultural differences of others, and keeping abreast of one's own discipline.6 Acquiring basic knowledge about these competencies through casual contact with other disciplines, such as attending lectures together in mixed groups, is not sufficient.9,10 Students need to learn team-based patient care by learning how to provide it through activities in which they can practice it.11
In response to this need, the University of Oklahoma Health Sciences Center's Colleges of Nursing and Allied Health developed a three-phase curriculum in which nurse practitioner (NP), physical therapy (PT), and occupational therapy (OT) students were given the opportunity to learn together and then put their knowledge into practice as health care teams. The simulated case study described below and the instructional materials (see the appendices) represent phase two of the project during which students worked together to care for a standardized patient (SP). In the third and final phase, students provided care for a real patient at different clinical sites.
Geriatric care was chosen as the population focus of the curriculum because it was complementary to the disciplines involved. In addition, telehealth technology was used because 37% of Oklahomans live in rural counties, and 63 of Oklahoma's 77 counties are classified as health professional shortage areas where telemedicine would be beneficial. The first cohort of students began working through the curriculum in the 2013 spring semester, and two subsequent cohorts were enrolled in the 2013 and 2014 fall semesters, respectively.
Methods
This learning activity was designed as a multiphased learning experience and includes an SP encounter to teach interprofessional teamwork skills and the effective use of telehealth in geriatric patient care. This case is most applicable for educators who own telehealth equipment; however, a telehealth patient encounter could be simulated with other technologies. We used a Polycom HDX 7000 telemedicine cart equipped with a GenCam, telephonic stethoscope, and ENT scope. Additionally, iPad 4s were used in this learning activity, although a suitable tablet computer would suffice. Connections were made using the Polycom RealPresence app.
Three weeks prior to the date assigned for their SP encounter, facilitators should provide students with the case (Appendix A), the student instructional packet (Appendix C), and the Interdisciplinary Geriatric Assessment (IGA) form (Appendix D). Facilitators should provide participating faculty with the case, the student instructional packet, the IGA form, and the faculty guide (Appendix B) at this time as well.
In a typical SP or OSCE encounter, a single student interacts with a live actor who has been hired and trained to portray a predetermined clinical case.12,13 Often, the SP evaluates the student using a checklist that is limited to yes/no or done/not done/not done correctly ratings on specific clinical skills, such as physical examination, patient provider communication, or patient education. In this instance, however, a multidisciplinary team of students interacted with an SP, and the focus of the SP encounter was less on clinical skills and more on team functioning. An overview of how to replicate this learning activity is provided in the Table.
Table. Time Line for Interprofessional Standardized Patient (SP) Learning Activity.
| Time Line | Activity Description |
|---|---|
| >3 weeks prior to simulation | Faculty assign students to interprofessional teams of four or five members and provide the case scenario and other preliminary materials, and students attend a face-to-face orientation to the telemedicine cart. |
| <2 weeks prior to simulation | As instructed, students meet together as a team to engage in the first phase of the learning activity: preplanning. See the student instructional packet (Appendix C) for details describing what students are to do during this phase. |
| 30 minutes | Student teams interact with their assigned SP in a simulated clinical exam room using telehealth equipment. One student from each team participates from a distant location, connecting with an iPad or suitable tablet computer. |
| 20 minutes | Students engage in interprofessional care planning as a team after their SP encounter. |
| 20 minutes | Students receive feedback from their SP and are debriefed by faculty who observed the encounter and care planning. |
| <2 weeks after simulation | Within 24 hours after the simulated patient encounter, students receive an e-mail to complete an online guided reflection exercise. Students complete the reflection voluntarily within 2 weeks. |
Please note that at least one of the students is assigned to participate from a distant location using an iPad or tablet computer. The distant participant connects to a telehealth cart or substitute equipment while the other students in each group interact directly with the SP and use the telehealth cart equipment.
During the debriefing phases, faculty should provide a safe educational atmosphere, offer verbal feedback, promote communication among team members, and encourage students to reflect, self-observe, and self-assess. Faculty should wrap up with nonjudgmental lessons learned. Faculty who participate in this learning activity should observe students during the SP encounter and make handwritten notes for reference during the debriefing segment.
Qualitative and quantitative data were collected to evaluate the learning experience. The guided reflection exercise was based on previous work by Zimmerman14 and provided students with the opportunity to engage in self- and team-performance appraisal. There were 10 questions total; answers to the following seven questions were the most useful:
-
1.
As I look back on our interprofessional team interaction with Mrs. Smith, I believe that we should have had additional time on …
-
2.
If I felt anxious, nervous, or frustrated during our interaction with Mrs. Smith, it was because I …
-
3.
If I found myself distracted during our interaction with Mrs. Smith by noise, activity, or by lack of concentration, I …
-
4.
If Mrs. Smith was a real patient, my impression of the potential consequences of our team's performance was …
-
5.
My reaction to what I liked about our interprofessional standardized patient experience …
-
6.
My reaction to what I did not like about our interprofessional standardized patient experience …
-
7.
Other strategies I used during our interprofessional standardized patient experience were …
Student reflection responses were analyzed using qualitative document and script analysis techniques in order to explore what students focused on during the learning activity. Analysis of the reflections was open-ended, and themes were allowed to emerge naturally.
Students' attitudes toward telehealth technology were assessed with 26 items of the Telemedicine Acceptance Questionnaire (TAQ),15 which was administered before and after the simulated learning activity. The survey assessed perceived usefulness of telemedicine with 13 items (e.g., “The use of telemedicine could help me to evaluate and monitor my patients more rapidly”), perceived ease of use with three items (e.g., “I think that I could easily learn how to use telemedicine”), and perceived subjective norm with four items (e.g., “Most of my patients will welcome the fact that I use telemedicine”). Six items were discarded because of psychometric concerns. Items were scored on a 7-point Likert scale from totally disagree (−3) to totally agree (3). Internal consistencies for the three scales at Time 1 and Time 2 were satisfactory, with alphas of .97 and .97 (perceived usefulness), .89 and .83 (perceived ease of use), and .82 and .89 (perceived subjective norm). Paired-sample t tests were conducted to compare students' pre- and posttest attitudes.
In accordance with the human subjects rules for informed consent, students' completion of the guided reflection exercise and the TAQ was voluntary.
Participants
A total of 86 out of 137 (62.8%) of the students participating in the simulated patient encounter completed the guided reflection exercise. Out of these, 29 (66%) were NP students, 42 (67%) were PT students, and 15 (50%) were OT students.
A total of 85 students (29 NP students, 20 OT students, and 36 PT students) completed the attitudes toward telehealth survey before and after the simulated patient encounter; the response rate was 62%. On average, NP students were 37.4 years old (SD = 9.4 years), whereas the mean ages of OT and PT students were 24.7 years (SD = 2.6 years) and 27.1 years (SD = 4.5 years), respectively. The majority of students were female (75.6%) and Caucasian (81.4%).
NP students were licensed registered nurses in the second semester of the first year of their advanced practice program. Some had worked in clinical settings for several years and were experienced with patient interaction, but none had had didactic coursework with PT and OT students during their undergraduate or postgraduate training. In contrast, PT and OT students were enrolled in the third semester of their respective professional programs and had participated in an ongoing integrated curriculum in which they shared foundational science, assessment, and intervention coursework together. All three programs are graduate programs. None of the students had experience with telehealth. Further, the use of simulation, including SPs, had not been widely used as a teaching technique within the respective programs.
Results
Student responses to the guided reflection exercise provided a snapshot of their thoughts and reactions during this learning activity. Overall, their reflections suggested that they were highly motivated and actively thinking about how to work together effectively as a team to care for their SP. While the majority of students' statements (50%) expressed confidence in the care their teams had provided, 29% noted concerns. Disciplines differed in the level of confidence. NP students felt the most confident, while PT students were the least. Furthermore, PTs most often voiced concerns about the care provided, while OT students were the least likely to express concerns.
Three themes emerged in regard to these concerns. The first was the importance of establishing rapport with the SPs. Second was remaining patient-centered despite distractions. Third was mitigating the effects of telehealth on these efforts. Rapport, sometimes called the therapeutic relationship,16 focuses on improving patient trust and communication through empathy-based clinician behaviors and techniques, such as positive body language and avoidance of medical jargon. Reflection quotes suggest that the students were focused more on the medical aspects of the case and felt they neglected the emotional state of their SP. “We provided safe comprehensive care to the patient, however … we may not have shown as much emotional concern as she desired,” an NP student stated. “We focused more on medical aspects of the case, and not as much on the individual patient as we should have. The patient could easily have been feeling overwhelmed and overlooked by our team,” a PT student said. “We had no chance to gain [the patient's] trust and we made her feel more uncomfortable,” an OT student said.
Students were actively working to filter out distractions as they endeavored to put the patient's needs first. “I continued to make direct eye contact to let her know I was listening and not completely distracted from extraneous noise, etc.,” an NP student said. “I tried to maintain eye contact with the patient, and block out the variables that were causing a lack of concentration,” said a PT student. “When [I was] distracted, I focused my attention back to the patient by looking directly at her as she answered other member's questions. I was able to focus on her [the patient's] response as well as make observations about her movements and facial expressions,” an OT student stated.
However, students struggled to mitigate the impact of the telehealth equipment on their efforts to establish rapport with their SP. “I didn't feel anxious or frustrated with Mrs. Smith. I felt frustrated with technology not working (connecting with distance provider and using accessory cameras),” said an NP student. “I was attending via the telehealth component. I found it was harder to interact and find my place as a health care provider because I wasn't present in the room with the patient,” said a PT student. “I tried to empathize with the patient so that she could feel a connection with me even though I was [not] in the room with her,” said an OT student who was on an iPad.
Potential changes in the attitudes toward telemedicine were assessed by comparing student scores before and after the SP activity. All students were affected by the use of telehealth technology so that differences between the students who were on site with the patient and the remote team member were not analyzed.
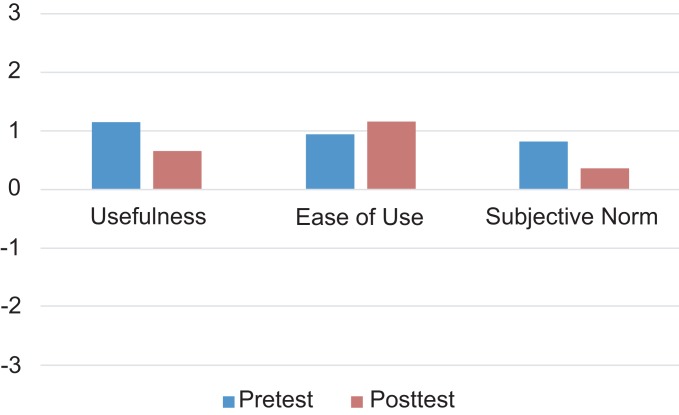
Figure 1 depicts the mean values of perceived usefulness, perceived ease of use, and perceived subjective norm for telemedicine. Overall, attitudes toward telemedicine were slightly positive, with mean values around 1 (tend to agree), but significantly declined between pretest (M = 0.97, SD = 0.86) and posttest (M = 0.73, SD = 0.94; t(84) = 2.29, p = .024). While perceived usefulness (pretest: M = 1.14, SD = 0.98; posttest: M = 0.64, SD = 1.16; t(84) = 3.81, p < .001) and perceived subjective norm significantly declined between pretest (M = 0.82, SD = 0.84) and posttest (M = 0.37, SD = 1.09; t(84) = 3.26, p = .002), perceived ease of use improved marginally (pretest: M = 0.96, SD = 1.09; posttest: M = 1.17, SD = 1.04; t(84) = −1.85, p = .067). This indicates that the telehealth equipment was easier to use than students had expected; however, they also found it less useful, and they were less convinced that others expected them to use it after the SP encounter.
Figure 1. Pre- and posttest mean attitudes towards telehealth.
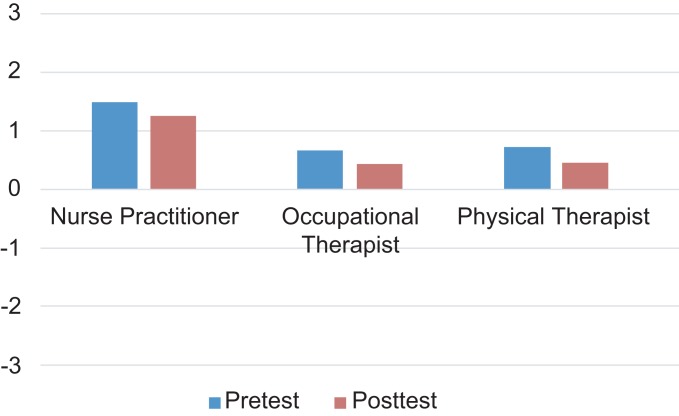
Figure 2 depicts the mean attitudes toward telehealth for the NP, OT, and PT students separately. Disciplines differed significantly before (F2,82 = 9.53, p < .001) and after (F2,82 = 8.28, p = .001) the simulated patient encounter. NP students had the most positive attitudes toward telemedicine and differed significantly from PT and OT students. This may indicate that students with more clinical experience either can better evaluate the benefits of telemedicine or feel less overwhelmed when using it.
Figure 2. Pre- and posttest mean attitudes by discipline.
Discussion
Team-based patient care requires students to learn knowledge and skills needed for collaborative practice. These skills cannot be developed through lectures and casual encounters with other disciplines but instead require learning activities in which interprofessional student teams can practice them. This publication describes the experiences with a learning activity in which NP, OT, and PT students practiced interprofessional geriatric patient care using telehealth technology. Qualitative reflection responses and quantitative survey data were analyzed to evaluate the learning experience and to assess potential changes in attitudes towards telehealth technology.
Qualitative data reveal that most students felt confident in the care their team had provided. However, they also noted that they had focused more on the medical aspects of the case and felt that they had neglected the emotional state of their patient. This indicates that they understood the importance of active communication to establish rapport with their simulated patient as well as with their health care team. They also understood that team-based patient care requires them to set aside their traditional discipline-specific assessment methods to elicit input from their team members. The telehealth technology further increased the complexity of the learning situation and impaired the communication between on-site team members and the SP.
Quantitative data indicate that students had slightly positive attitudes towards patient care using telehealth technology before the learning activity. After the exercise, attitudes remained overall positive but significantly declined. Interestingly, students found the technology easier to use than anticipated but evaluated it as less useful and did not think that others expected them to use it. The data also reveal significant differences between disciplines, with NP students being more positive compared to OT and PT students. The NP students were licensed registered nurses who had worked in clinical settings for several years and were experienced with patient interaction. This experience might have helped them to focus on the important aspects of the task and see the potential of telehealth in serving patients who otherwise would not receive medical care, resulting in more positive attitudes about telehealth. In contrast, both the PT and OT students were enrolled in the third semester of their respective professional programs, had less clinical experience, and held less positive views of telehealth.
The data also indicate that this learning activity could be strengthened by providing students with more background about the case and strategies to offset the potentially negative impacts of computer-mediated communication during telehealth-based patient care. Visual cues especially differ between virtual and face-to-face encounters, such as persons appearing larger than life on a screen and not being in the same place at the same time, thus losing the sense of personal connection established by physical presence. Students could have been given additional opportunities to familiarize themselves with the telehealth equipment before the SP encounter to help them focus on the patient instead of the technology. Being able to better concentrate on the patient could also help students acknowledge the benefits of telemedicine by providing better care for patients, especially in rural areas classified as health professional shortage areas.
Appendices
A. Mrs Anh Kha Smith Case Study.pdf
B. Faculty Guide.docx
C. Student Instructional Packet.docx
D. Mrs Anh Kha Smith IGA Form.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number D09HP25024, Advanced Nursing Education Grants, in the amount of $1,116,906. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by, HRSA, HHS, or the U.S. Government.
Ethical Approval
This publication contains data obtained from human subjects and received ethical approval.
References
- 1.Institute of Medicine. Crossing the Quality Chasm. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 2.Institute of Medicine. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Baker DP, Gustafson S, Beaubien JM, Salas E, Barach P. Medical team training programs in health care. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation. Rockville, MD: Agency for Healthcare Research and Quality; 2005:253–267. [PubMed] [Google Scholar]
- 4.Blue AV, Mitcham M, Smith T, Raymond J, Greenberg R. Changing the future of health professions: embedding interprofessional education within an academic health center. Acad Med. 2010;85(8):1290–1295. http://dx.doi.org/10.1097/ACM.0b013e3181e53e07 [DOI] [PubMed] [Google Scholar]
- 5.Hammick M, Freeth D, Koppel I, Reeves S, Barr H. A best evidence systematic review of interprofessional education: BEME Guide no. 9. Med Teach. 2007;29(8):735–751. http://dx.doi.org/10.1080/01421590701682576 [DOI] [PubMed] [Google Scholar]
- 6.Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, DC: Interprofessional Education Collaborative; 2011. [Google Scholar]
- 7.Valentine MA, Nembhard IM, Edmondson AC. Measuring teamwork in health care settings: a review of survey instruments. Med Care. 2015;53(4):e16–e30. [DOI] [PubMed] [Google Scholar]
- 8.Deutschlander S, Mallinson S. Measuring behaviour as outcome of interprofessional interventions: are you willing to collaborate or are you collaborating? J Res Interprof Pract Educ. 2014;4(2):179. [Google Scholar]
- 9.Hall P. Interprofessional teamwork: professional cultures as barriers. J Interprof Care. 2005;19(suppl 1):188–196. http://dx.doi.org/10.1080/13561820500081745 [DOI] [PubMed] [Google Scholar]
- 10.Curran VR, Sharpe D, Forristall J, Flynn K. Attitudes of health sciences students towards interprofessional teamwork and education. Learn Health Soc Care. 2008;7(3):146–156. http://dx.doi.org/10.1111/j.1473-6861.2008.00184.x [Google Scholar]
- 11.Sargeant J, Loney E, Murphy G. Effective interprofessional teams: contact is not enough to build a team. J Contin Educ Health Prof. 2008;28(4):228–234. [DOI] [PubMed] [Google Scholar]
- 12.Downing SM, Yudkowsky R. Assessment in Health Professional Education. New York, NY: Routledge; 2009. [Google Scholar]
- 13.Wallace P. Coaching Standardized Patients: For Use in the Assessment of Clinical Competence. New York, NY: Springer Publishing Co; 2007. [Google Scholar]
- 14.Zimmerman BJ. Investigating self-regulation and motivation: historical background, methodological developments, and future prospects. Am Educ Res J. 2008;45(1):166–183. http://dx.doi.org/10.3102/0002831207312909 [Google Scholar]
- 15.Gagnon MP, Orruno E, Asua J, Abdeljelil AB, Emparanza J. Using a modified technology acceptance model to evaluate healthcare professionals' adoption of a new telemonitoring system. Telemed J E Health. 2012;18(1):54–59. http://dx.doi.org/10.1089/tmj.2011.0066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leach MJ. Rapport: a key to treatment success. Complement Ther Clin Pract. 2005;11(4):262–265. http://dx.doi.org/10.1016/j.ctcp.2005.05.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Mrs Anh Kha Smith Case Study.pdf
B. Faculty Guide.docx
C. Student Instructional Packet.docx
D. Mrs Anh Kha Smith IGA Form.docx
All appendices are peer reviewed as integral parts of the Original Publication.