Abstract
BACKGROUND
Pneumonia, the commonest lower respiratory tract infection, can result in respiratory and non-respiratory complications. Few studies have reported on the prevalence of many complications.
OBJECTIVES
Identify the prevalence of 18 complications of pneumonia and compare complication rates by age group and type of pneumonia. Identify most prevalent comorbidities, the effect of the number of comorbidities on the presence of complications, and the association between specific comorbidities and specific complications.
DESIGN
Retrospective, cross-sectional prevalence study.
SETTING
Tertiary care center in Riyadh.
PATIENTS AND METHODS
The target population were patients aged 17 years and older, of different nationalities and both genders, diagnosed with pneumonia during the period of 2010 to 2017. Selection was by stratified sampling by year of admission.
MAIN OUTCOME MEASURES
Complications of pneumonia.
SAMPLE SIZE
800.
RESULTS
Complications were observed in 427 patients (53.4%). The complications were respiratory in 258 patients (32%), sepsis and septic shock in 186 (23%), cardiac in 125 (16%), neurological in 5 (0.6%), and cholestatic jaundice in 2 (0.3%). Pleural effusion was the commonest complication, observed in 230 patients. There was a significant difference (P<.001) between the complication rates in older patients compared to younger (60% as compared to 41%). For the type of pneumonia, there was a significant difference (P<.001) between community-acquired pneumonia and hospital-acquired pneumonia in the presence of complications (OR=2.41, 95% CI for OR=1.66, 3.49). The number of comorbidities was significantly associated with the presence of complications (P=.001) for those with multiple comorbidities (46% for patients with no comorbid illnesses versus 68% in patients with three or more comorbidities).
CONCLUSION
These results suggest that Saudi Arabia needs to establish better prevention and intervention programs, especially for the high-risk groups identified in this study: older patients, patients with hospital-acquired pneumonia and patients with two or more comorbidities.
LIMITATIONS
Retrospective design and single-centered.
Pneumonia is the most common lower respiratory tract infection and a leading cause of morbidity and mortality worldwide.1 Pneumonia can result in both respiratory and non-respiratory complications. The respiratory complications include abscess, pleurisy, acute respiratory distress syndrome (ARDS), and parapneumonic effusion. Pneumonia is the most common single cause of ARDS.2 A study published in 1990 stated that approximately 10% of patients who have primary pneumonia that required ICU admission had ARDS.3 Moreover, parapneumonic effusion is a common complication that accounts for approximately 35% to 40% of 1.3 million patients hospitalized with pneumonia in the United States each year.4
Non-respiratory complications include sepsis, septic shock, cholestatic jaundice, cardiac, and neurological complications. In a case report, two of three patients admitted to respiratory care unit with severe life-threatening hemoptysis and septic shock as a complication of community-acquired Staphylococcus aureus pneumonia, deteriorated to death.5 Cholestasis can occur as a complication of infections and sepsis in hospitalized patients. In another case report, a 35-year-old male presented with a cholestatic picture with no obvious cause other than an acute infection with mycoplasma pneumonia. After receiving IV antibiotics, he showed significant improvement in his overall clinical condition.6 Moreover, out of seventeen articles that reported cardiac complications, the incidence rates were heart failure (14.1%), acute coronary syndrome (5.3%), and cardiac arrhythmia (4.7%).7 Neurological complications of sudden onset can also manifest in patients with mycoplasma pneumonia such as Guillain-Barré syndrome, encephalitis, meningitis, acute cerebellar ataxia, and peripheral neuropathy.8
One study conducted in Saudi Arabia reported that the point prevalence of community-acquired pneumonia (CAP) in hospitalized patients was 30.3% with a peak prevalence in patients over 50 years, while the point prevalence of hospital-acquired pneumonia (HAP) was 4.4%.9 Another study that included 567 pneumonia patients with a mean (SD) age of 42.7 (21.9) years showed that 2.3% experienced non-fatal complications and 6% died due to pneumonia.10 The aim of this study was to identify the prevalence of complications of pneumonia, and the prevalence of common diseases associated with pneumonia complications, among inpatients at a tertiary care hospital in Saudi Arabia. This would be helpful in reducing the occurrence of pneumonia complications in admitted patients.
PATIENTS AND METHODS
This study design was a retrospective cross-sectional descriptive study that was conducted in King Abdulaziz Medical City, Riyadh, Saudi Arabia. The pulmonary department is one of the busiest departments in KAMC, with an average of 6–10 consultations/day. The first pulmonary rehabilitation in Saudi Arabia was established there. The target population was hospitalized patients aged 17 years and older, of different nationalities and both genders, who were diagnosed with pneumonia during the period of 2010 to 2017 and followed up at KAMC. No exclusion criteria were specified. The sampling frame included a list of all pneumonia patients aged 17 years and older. Stratified sampling by year of study of pneumonia onset was used to obtain a sample of patients distributed over the years from 2010 to 2017. From each year, 100 patients were selected randomly. Pneumonia was diagnosed on the basis of suggestive history, compatible physical findings, and new infiltrates on a chest radiograph that was not due to any other causes. Approval of the research was obtained from the of Institutional Review Board (SP17/349/R).
The data contained no personal information on the participants. A retrospective chart review was conducted in which the investigators reviewed paper and electronic charts to extract the data. Variables included patient demographics (age, gender, nationality), past medical history (smoking, respiratory problems, diabetes mellitus, immunosuppressive therapy, cystic fibrosis, and chronic kidney diseases), and the complications (related to cardiovascular system, central nervous system, and respiratory system). The independent variables were age, gender, nationality, past medical history, and initial treatment. The outcome variables were the respiratory and non-respiratory complications of pneumonia.
Data entry was managed using the MS Excel, and the data was analyzed using IBM SPSSversion 21 (Armonk, NY: IBM Corp., United States). The results are presented as descriptive statistics (mean and standard deviation for numerical variables and as frequencies and percentages for the categorical variables). The chi-square test was used to analyze the relationship between categorical variables and the presence of complications. The data was presented with a 95% confidence interval, and a P value <.05 was statistically significant.
RESULTS
The study sample consisted of 800 patients with pneumonia who were admitted over an 8-year period. The demographics of the patients and associated comorbidities are summarized in Table 1. The highest number of comorbid illnesses in a patient was five, which was seen in two patients. Complications were observed in 427 (53%), while 373 (47%) did not develop any complications according to the patient record files. The 18 types of complications identified are shown in Table 2. Pleural effusion was the most commonly encountered complication 230 (29%) followed by sepsis 183 (23%). Some patients had more than one respiratory complication, 245 had only one complication, 12 had two complications, and one had three complications. Table 3 shows the relationship between the age groups and the presence of specific complications; the difference was statistically significant for unilateral pleural effusion (P=.03) being lower in the 46-to-65 year age group (9%) as compared to the 17-to-45 year (16%) and >65 year (17%) age groups. Bilateral pleural effusion was more common in the >65 year age group (17%) as compared to the younger age groups (P=.03). Heart failure was more common in the two older age groups as compared to 2% in the 17-to-45 year age group (P=.007), while sepsis was significantly higher (P<.001) in the >65 year age group (28%) as compared to the two younger age groups. Acute respiratory distress (P=.18) and septic shock (P=.12) were not significantly related to age even though they were among the common complications. Table 4 presents the associations between specific complications and type of pneumonia. Among the complications that were assessed, unilateral pleural effusion (P=.048), heart failure (P=.02), sepsis (P<.001), septic shock (P=.002), and encephalitis (P=.001) were significantly more likely in HAP than CAP patients. Acute respiratory distress disease was seen in 14% of CAP and 19% of HAP (P=.07), and bilateral pleural effusion was seen in 14% of CAP and 14% of HAP (P=.80). The same analysis for Table 4 was applied to the subgroup of patients (n=82) who were taking immunosuppressant therapy. For the complications that statistically significantly different, septic shock (HAP 19%, CAP 20%) and unilateral pleural effusion (HAP 14%, CAP 16%) were similar to the CAP and HAP percentages in the overall group. The percentage was slightly different for the following complications: sepsis (HAP 33%, CAP 28%), heart failure (HAP 0%, CAP 5%), bilateral pleural effusion (HAP 19%, CAP 12%) and ARDS (HAP 14%, CAP 21%). However, these differences were not statistically significant within the group taking immunosuppressant therapy (P>.05).
Table 1.
Demographic and clinical characteristics of the patients (N=800).
| Characteristics | n (%) |
|---|---|
|
| |
| Age (years) | |
| 17–45 | 128 (16) |
| 46–65 | 212 (27) |
| >65 | 460 (58) |
| Gender | |
| Male | 373 (47) |
| Female | 427 (53) |
| Nationality | |
| Saudi | 794 (99) |
| Non-Saudi | 6 (1) |
| Comorbid illness | |
| Diabetes mellitus | 530 (66) |
| Chronic kidney disease | 175 (22) |
| Cystic fibrosis | 1 (0.1) |
| Chronic obstructive pulmonary disease | 154 (19) |
| Asthma | 236 (30) |
| Lung cancer | 30 (4) |
| Other risk factors | |
| Smoker | 101 (13) |
| Immunosuppressant therapy | 82 (10) |
Table 2.
The prevalence of complications in patients with pneumonia (N=800).
| Complication | n (%) |
|---|---|
|
| |
| Respiratory complications | 258 (32) |
| Sepsis | 183 (23) |
| Cardiac complications | 125 (16) |
| Acute respiratory distress | 118 (15) |
| Pleural effusion | |
| Unilateral | 120 (15) |
| Bilateral | 110 (14) |
| Septic shock | 94 (12) |
| Heart failure | 75 (9) |
| Arrhythmias | 52 (6.5) |
| Bronchiectasis | 22 (3) |
| Pleurisy | 10 (1.3) |
| Acute coronary syndrome | 8 (1) |
| Empyema | 8 (1) |
| Neurological complications | 5 (0.6) |
| Encephalitis | 5 (0.6) |
| Encephalitis | 5 (0.6) |
| Pulmonary abscess | 2 (0.3) |
| Endocarditis | 2 (0.3) |
| Cholestatic jaundice | 2 (0.3) |
| Pericarditis | 1 (0.1) |
| Myocarditis | 1 (0.1) |
Table 3.
Association between age groups and specific complications.
| Complication | Age groups | P value | ||
|---|---|---|---|---|
| 17 to 45 years (n=128) | 46 to 65 years (n=212) | > 65 years (n=460) | ||
|
| ||||
| Acute respiratory distress | 13 (10%) | 29 (14%) | 76 (17%) | .18 |
| Unilateral pleural effusion | 20 (16%) | 20 (9%) | 80 (17%) | .03 |
| Bilateral pleural effusion | 14 (11%) | 20 (9%) | 76 (17%) | .03 |
| Heart failure | 3 (2%) | 19 (9%) | 53 (12%) | .007 |
| Sepsis | 17 (13%) | 37 (18%) | 129 (28%) | <.001 |
| Septic shock | 10 (8%) | 21 (10%) | 63 (14%) | .12 |
Table 4.
Association between type of pneumonia and specific complications.
| Complication | Type of pneumonia* | P value | |
|---|---|---|---|
| CAP (n=640) | HAP (n=160) | ||
|
| |||
| Acute respiratory distress disease | 87 (14%) | 31 (19%) | .07 |
| Unilateral pleural effusion | 88 (14%) | 32 (20%) | .048 |
| Bilateral pleural effusion | 87 (14%) | 23 (14%) | .80 |
| Heart failure | 52 (8%) | 23 (14%) | .02 |
| Sepsis | 123 (19%) | 60 (38%) | <.001 |
| Septic shock | 64 (10%) | 30 (19%) | .002 |
| Encephalitis | 1 (0.2%) | 4 (3%) | .001 |
CAP: Community acquired pneumonia, HAP: Hospital acquired pneumonia
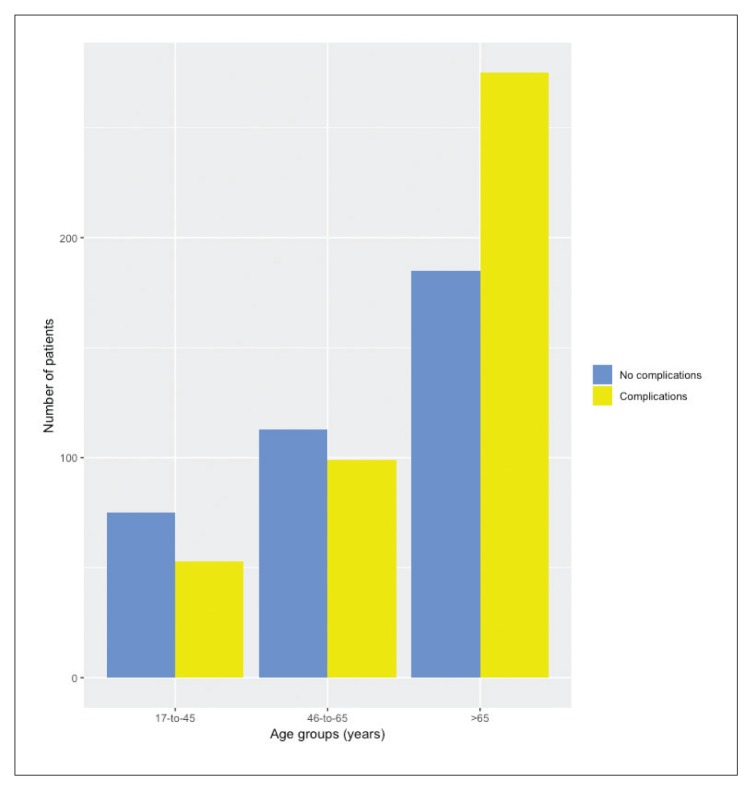
There was a significant difference (P<.001) between CAP and HAP patients in terms of complications. Among the 160 patients who were diagnosed with HAP, the majority (n=112, 70%) had complications, while of the 640 diagnosed with CAP, 314 (49%) had complications (OR=2.41, 95% CI: 1.66, 3.49). Patients older than 65 years of age were more likely (P<.001) to develop any complication (60%) as compared to the younger age groups of 17-to-45 years (41%) and 46-to-65 years (47%) (Figure 1).
Figure 1.
Presence of complications by age groups.
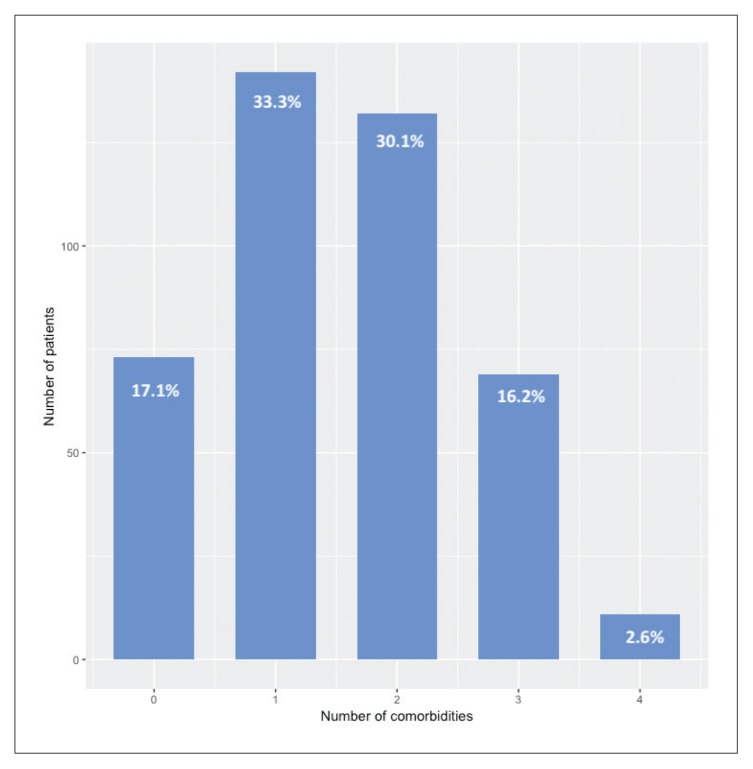
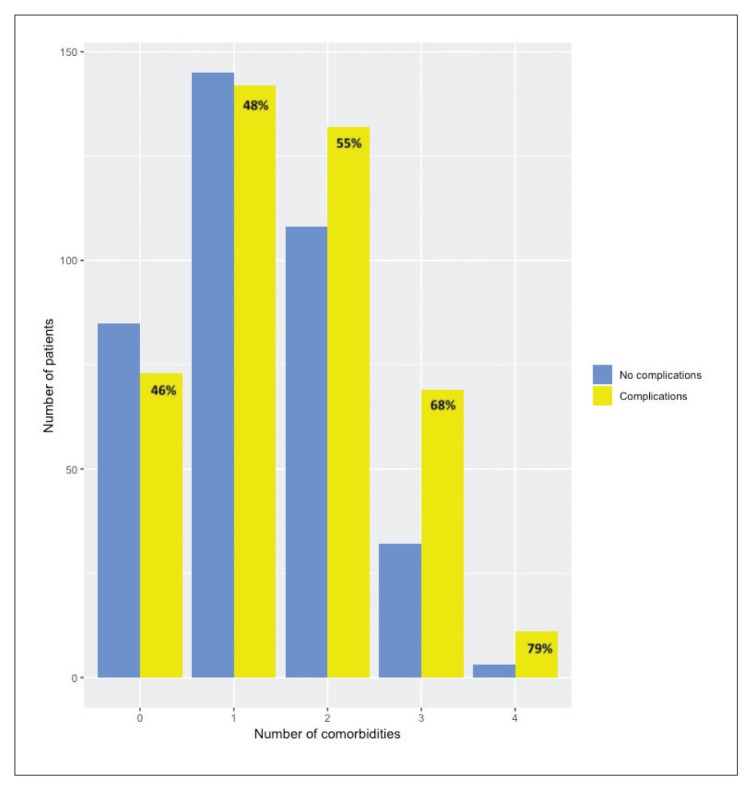
While there were relatively few patients with complications who had two or more comorbidities (Figure 2), there were more patients with comorbidities among patients with complications compared with patients without complications. Patients with no comorbid illnesses had a complication rate of 46%, which was similar to patients with only one comorbid illness (48%) as compared to 55% (P=.9) in patients with two comorbid illnesses (P=.6) and 68% in patients with three or more comorbid illnesses (P=.002) (pairwise comparisons with Bonferroni correction) (Figure 3). Among all the comorbid illnesses that were included in this study, diabetes mellitus was most common (n=530, 66%). Of those 530 patients, 295 (56%) had complications. The second most common comorbid illness in this study was asthma 236 (30%), and of these, 131 (56%) developed complications. The incidence of complications with other comorbid illnesses was chronic kidney disease (62%), chronic obstructive pulmonary disease (64%), and lung cancer (70%). There were 82 patients with pneumonia on immunosuppressant therapy and 48 (59%) of those patients had complications. In addition, 101 pneumonia patients were smokers, and among these 59 (58%) developed complications. There was some association between specific comorbid illnesses with certain complications (data not shown). Patients with chronic kidney disease were more likely to have heart failure (17%) as compared to those who did not have the illness (7%) (P<.001). Also, patients with chronic obstructive pulmonary disease were more likely to have acute respiratory distress disease (23%) as compared to those who did not have the illness (13%) (P=.002).
Figure 2.
Frequency of comorbidities among patients with complications (n=427).
Figure 3.
Frequency of comorbidities among patients with (n=427) and without complications (n=373). Percentages are portion with complications for each number of comorbidities (two patients had 5 comorbidities) (0 vs 1: P=.9; 0 vs 2, P=.6; 0 vs 3, P=.002).
Multiple logistic regression identified risk factors associated with the development of any complication in the pneumonia patients (Table 5). The risk factors significantly associated with the presence of any complication included age >65 years (OR=1.73, 95% CI: 1.08, 2.78), being immunocompromised (OR=4.35, 95% CI: 1.7, 11.14), and having HAP (OR=2.42, 95% CI: 1.65, 3.56). There was no relationship identified with any of the comorbid conditions nor with being a smoker or being on immunosuppressant therapy.
Table 5.
Multiple logistic regression of risk factors for presence of any complication.
| n | Wald | Sig. | Exp(B) | 95% CI for EXP(B) | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
|
| ||||||
| Age category (years) | ||||||
| 17–45 | 128 | 10.35 | .006 | |||
| 46–65 | 212 | 0.05 | 0.82 | 1.06 | 0.64 | 1.76 |
| >65 | 460 | 5.24 | .02 | 1.73 | 1.08 | 2.78 |
| Gender | ||||||
| Male | 373 | 1.00 | ||||
| Female | 427 | 0.28 | 0.60 | 1.09 | 0.80 | 1.49 |
| Presence of comorbidities | ||||||
| Diabetes mellitus | 530 | 0.001 | 0.98 | 1.004 | 0.70 | 1.43 |
| Chronic kidney disease | 175 | 2.47 | 0.12 | 1.35 | 0.93 | 1.95 |
| Chronic obstructive pulmonary disease | 154 | 2.70 | 0.10 | 1.40 | 0.94 | 2.09 |
| Asthma | 236 | 0.91 | 0.34 | 1.17 | 0.85 | 1.63 |
| Other risk factors | ||||||
| Smoker | 101 | 1.38 | 0.24 | 1.33 | 0.82 | 2.16 |
| Immunocompromised | 34 | 9.36 | .002 | 4.35 | 1.70 | 11.14 |
| Immunosuppressant therapy | 82 | 0.04 | 0.83 | 1.06 | 0.63 | 1.76 |
| Type of pneumonia | ||||||
| Community acquired | 640 | 1.00 | ||||
| Hospital acquired | 160 | 20.20 | <.001 | 2.42 | 1.65 | 3.56 |
| Constant | 9.89 | <.001 | 0.51 | |||
Omnibus tests of model coefficients: Chi-square=62.892, df=11, P<.001; −2 log likelihood: 1042.496; Cox and Snell R Square: .076; Nagelkerke R square: .101
DISCUSSION
This study investigated 18 complications of pneumonia that were grouped into respiratory, cardiac, neurological, sepsis and septic shock, and cholestatic jaundice. Complications were observed in 53% of the patients in this study. This is contrary to the national data documented in the literature, in which the prevalence of complications of pneumonia in a study conducted in Al-Qassim was only 8%.10 Our study revealed that the most prevalent complications were respiratory complications, sepsis and septic shock. The most common complications were pleural effusion, sepsis, acute respiratory distress, and septic shock. The prevalence of complications was highest among older age group (>65 years).
Respiratory failure, meningitis, pleural effusion, and empyema are the most common complications of pneumococcal pneumonia in one review.11 The results of the present study are consistent with findings in a review by Marrie, except for meningitis and empyema, which were rare complications in this study. This discrepancy may be because other studies included pneumococcal pneumonia only as it is the most common type, while our study included all types of pneumonia. Cardiac complications were seen in 16% of the patients which is somewhat similar to results from other studies.7
Also, our findings are consistent with findings of Kaplan et al who found that CAP is a frequent cause of hospital admissions and mortality among elderly patients, with a five-fold increase in incidence and two-fold increases in mortality as age increased from 65–69 years to older than 90 years.12 This association between complications and old age can be attributed to many factors including functional status, tube feeding, comorbidities, and use of multiple medications. A functional status assessment for the elderly should be incorporated with a pneumonia assessment to reduce the risk of complications. This is supported by the findings of the literature, which concluded that functional status was an independent predictor of short- and long-term mortality in hospitalized CAP elderly patients.13
In this study, the number of patients diagnosed with CAP was much higher than the patients with HAP. However, the complication rate was higher among patients with HAP compared to CAP. These findings are matched with the results of a study done by Rothberg et al, which revealed that the case-fatality is greater with HAP since they were more likely to have a principal diagnosis of sepsis and respiratory failure than CAP patients.14 This can be explained by numerous influencers such as the different organisms that cause HAP, immune status, comorbidities, and current use of medication. In addition, patients with HAP are more likely to require ICU admission.
The rate of comorbidities in our patients (54%) correspondend to that seen in a national study conducted in Al-Qassim (54%).10 However, higher rates were noticed in the western region of Saudi Arabia (68%).15 Our study investigated these comorbidities, and concluded that diabetes mellitus, chronic kidney disease, chronic obstructive pulmonary disease, asthma, and illnesses that require immunosuppressant therapy were associated with more risk of complications, as >50% of patients who had at least one comorbid illness had complications. The association between diabetes mellitus and pneumonia complications was expected, as it was reported in earlier literature. One study investigated the association between fasting hyperglycemia and pneumonia complication rates among elderly patients revealed that complication rates were greater among patients with mild and severe hyperglycemia compared to the normal group.16 These results are consistent with our findings since diabetes mellitus had the highest frequency.
The high prevalence of complications emphasizes the need to modify existing interventions and preventive methods especially for high risk groups. For example, the Saudi Thoracic Society pneumococcal vaccination guidelines - 2016 should be more implemented and reinforced, as it comprehensively addresses the susceptible Saudi population.17 Moreover, measuring severity and mortality risk through different scoring systems like Sepsis-related Organ Failure Assessment (SOFA)18 and APACHE score19 should be carried out repetitively and extensively in all high-risk groups identified in this study. Our results can be used as a baseline to test the efficacy of newly implemented assessment and intervention programs.
In this study, there are some limitations that needs to be recognized. First, the authors ruled out all the confounding factors while collecting data pre-existing comorbidities that can lead to the same complication of the pneumonia. Clinical judgment was the only measure used in deciding which confounding factors to ignore, as no other measure be applied. Second, the study design was a retrospective cross-sectional study. Third, the study included only one center in the capital city of Saudi Arabia, which does not reflect the whole region. Also, data on mortality was not collected, which could help in the prediction of seriousness and prognosis of the complications of pneumonia patients. Nevertheless, the present study has many strengths. First, the large sample size provided a good assessment of the prevalence of complications. Second, the different age groups included provided a good estimate of the susceptible population by age.
In conclusion, our study showed that respiratory complications, sepsis, and septic shock were the most prevalent complications of pneumonia. Older age group, HAP cases and those with two or more comorbidities were associated with higher rates of complication. The presence of these complications can lead to longer hospital stays, poor quality of life, more ICU admissions, and more hospital resources use. These findings highlight the need for better prevention and intervention programs. Moreover, the health authorities should address the knowledge gap by educating patients and health care workers about following sterile methods and practicing good hygiene to reduce transmission of infection and to prevent the development of HAP.
Footnotes
Funding: None.
CONFLICT OF INTEREST: None.
REFERENCES
- 1.Kumar P, Clark M. Kumar & Clark’s clinical medicine. 1st ed. Edinburgh: Saunders; 2002. pp. 833–9. [Google Scholar]
- 2.Bauer T, Ewig S, Rodloff A, Muller E. Acute respiratory distress syndrome and pneumonia: A comprehensive review of clinical data. Clin Infect Dis. 2006;43(6):748–56. doi: 10.1086/506430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niederman M, Fein A. Sepsis syndrome, the adult respiratory distress syndrome, and nosocomial pneumonia. A common clinical sequence. Clin Chest Med. 1990;11(4):633–56. [PubMed] [Google Scholar]
- 4.Grijalva C, Zhu Y, Nuorti J, Griffin M. Emergence of parapneumonic empyema in the USA. Thorax. 2011;66(8):663–8. doi: 10.1136/thx.2010.156406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boussaud VR, Parrot A, Mayaud C, Wislez M, Antoine M, Picard CM, et al. Life-threatening hemoptysis in adults with community-acquired pneumonia due to Panton-Valentine leukocidin-secreting Staphylococcus aureus. Intensive Care Med. 2003;29:1840–3. doi: 10.1007/s00134-003-1918-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grullich C, Baumert T, Blum H. Acute Mycoplasma pneumoniae Infection Presenting as Cholestatic Hepatitis. J Clin Microbiol. 2003;41(1):514–5. doi: 10.1128/JCM.41.1.514-515.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corrales-Medina VF, Suh KN, Rose G, Chirinos JA, Doucette S, Cameron DW, et al. Cardiac Complications in Patients with Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis of Observational Studies. PLoS Med. 2011 Jun 28;8(6):e1001048. doi: 10.1371/journal.pmed.1001048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gücüyener K, Şimşek F, Yilmaz Ö, Serdaroğlu A. Methyl-prednisolone in neurologic complications of Mycoplasma pneumonia. Indian J Pediatr. 2000;67(6):467–9. doi: 10.1007/BF02859473. [DOI] [PubMed] [Google Scholar]
- 9.Abubakar A, Malik M, Pebody R, Elkholy A, Khan W, Bellos A, et al. Burden of acute respiratory disease of epidemic and pandemic potential in the WHO Eastern Mediterranean Region: A literature review. East Mediterr Health J. 2016 Oct 2;22(7):513–26. [PubMed] [Google Scholar]
- 10.Kurashi N, al-Hamdan A, Ibrahim E, al-Idrissi H, al-Bayari T. Community acquired acute bacterial and atypical pneumonia in Saudi Arabia. Thorax. 1992;47(2):115–8. doi: 10.1136/thx.47.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marrie T. Pneumococcal pneumonia: epidemiology and clinical features. Semin Respir Infect. 1999;14(3):227–36. [PubMed] [Google Scholar]
- 12.Kaplan V, Angus D, Griffin M, Clermont G, Scott Watson R, Linde-Zwirble W. Hospitalized community-acquired pneumonia in the elderly. Am J Respir Crit Care Med. 2002;165(6):766–72. doi: 10.1164/ajrccm.165.6.2103038. [DOI] [PubMed] [Google Scholar]
- 13.Torres O, Muñoz J, Ruiz D, Ris J, Gich I, Coma E, et al. Outcome Predictors of Pneumonia in Elderly Patients: Importance of Functional Assessment. J Am Geriatr Soc. 2004;52(10):1603–9. doi: 10.1111/j.1532-5415.2004.52492.x. [DOI] [PubMed] [Google Scholar]
- 14.Rothberg M, Haessler S, Lagu T, Lindenauer PK, Pekow PS, Priya A, et al. Outcomes of patients with healthcare-associated pneumonia: Worse disease or sicker patients? Infect Control Hosp Epidemiol. 2014;35(S3):S107–15. doi: 10.1086/677829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Dabbagh AA, El-Deeb HA, El-Zamzamy MM, Reheem AMA, El-Tahawy AT, Al-Bagdadi TM. The radiological manifestations of lower respiratory tract infections in the Western Province of the Kingdom of Saudi Arabia. Saudi Med J. 1989;10(1):42–7. [Google Scholar]
- 16.Castellanos M, Szerszen A, Saifan C, Zigelboym I, Khoueiry G, Abi Rafeh N, et al. Fasting hyperglycemia upon hospital admission is associated with higher pneumonia complication rates among the elderly. Int Arch Med. 2010;3(1):16. doi: 10.1186/1755-7682-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alharbi NS, Al-Barrak AM, Al-Moamary MS, Zeitouni MO, Idrees MM, Al-Ghobain MO, et al. The Saudi Thoracic Society pneumococcal vaccination guidelines-2016. Ann Thorac Med. 2016;11(2):93–102. doi: 10.4103/1817-1737.177470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 19.Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med. 1981;9(8):591–7. doi: 10.1097/00003246-198108000-00008. [DOI] [PubMed] [Google Scholar]