Abstract
Background
Shoulder pain is a very common symptom. Disorders of the rotator cuff tendons due to wear or tear are among the most common causes of shoulder pain and disability. Magnetic resonance imaging (MRI), magnetic resonance arthrography (MRA) and ultrasound (US) are increasingly being used to assess the presence and size of rotator cuff tears to assist in planning surgical treatment. It is not known whether one imaging method is superior to any of the others.
Objectives
To compare the diagnostic test accuracy of MRI, MRA and US for detecting any rotator cuff tears (i.e. partial or full thickness) in people with suspected rotator cuff tears for whom surgery is being considered.
Search methods
We searched the Cochrane Register of Diagnostic Test Accuracy Studies, MEDLINE, EMBASE, and LILACS from inception to February 2011. We also searched trial registers, conference proceedings and reference lists of articles to identify additional studies. No language or publication restrictions were applied.
Selection criteria
We included all prospective diagnostic accuracy studies that assessed MRI, MRA or US against arthroscopy or open surgery as the reference standard, in people suspected of having a partial or full thickness rotator cuff tear. We excluded studies that selected a healthy control group, or participants who had been previously diagnosed with other specific causes of shoulder pain such as osteoarthritis or rheumatoid arthritis. Studies with an excessively long period (a year or longer) between the index and reference tests were also excluded.
Data collection and analysis
Two review authors independently extracted data on study characteristics and results of included studies, and performed quality assessment according to QUADAS criteria. Our unit of analysis was the shoulder. For each test, estimates of sensitivity and specificity from each study were plotted in ROC space and forest plots were constructed for visual examination of variation in test accuracy. Meta‐analyses were performed using the bivariate model to produce summary estimates of sensitivity and specificity. We were unable to formally investigate potential sources of heterogeneity because of the small number of studies.
Main results
We included 20 studies of people with suspected rotator cuff tears (1147 shoulders), of which six evaluated MRI and US (252 shoulders), or MRA and US (127 shoulders) in the same people. Many studies had design flaws, with the potential for bias, thus limiting the reliability of their findings. Overall, the methodological quality of the studies was judged to be low or unclear. For each test, we observed considerable heterogeneity in study results, especially between studies that evaluated US for the detection of full thickness tears and studies that evaluated MRA for the detection of partial thickness tears. The criteria for a positive diagnostic test (index tests and reference standard) varied between studies.
Meta‐analyses were not possible for studies that assessed MRA for detection of any rotator cuff tears or partial thickness tears. We found no statistically significant differences in sensitivity or specificity between MRI and US for detecting any rotator cuff tears (P = 0.13), or for detecting partial thickness tears (P = 1.0). Similarly, for the comparison between MRI, MRA and US for detecting full thickness tears, there was no statistically significant difference in diagnostic performance (P = 0.7). For any rotator cuff tears, the summary sensitivity and specificity were 98% (95% CI 92% to 99%) and 79% (95% CI 68% to 87%) respectively for MRI (6 studies, 347 shoulders), and 91% (95% CI 83% to 95%) and 85% (95% CI 74% to 92%) respectively for US (13 studies, 854 shoulders). For full thickness tears, the summary sensitivity and specificity were 94% (95% CI 85% to 98%) and 93% (95% CI 83% to 97%) respectively for MRI (7 studies, 368 shoulders); 94% (95% CI 80% to 98%) and 92% (95% CI 83% to 97%) respectively for MRA (3 studies, 183 shoulders); and 92% (95% CI 82% to 96%) and 93% (95% CI 81% to 97%) respectively for US (10 studies, 729 shoulders).
Because few studies were direct head‐to‐head comparisons, we could not perform meta‐analyses restricted to these studies. The test comparisons for each of the three classifications of the target condition were therefore based on indirect comparisons which may be prone to bias due to confounding.
Authors' conclusions
MRI, MRA and US have good diagnostic accuracy and any of these tests could equally be used for detection of full thickness tears in people with shoulder pain for whom surgery is being considered. The diagnostic performance of MRI and US may be similar for detection of any rotator cuff tears. However, both MRI and US may have poor sensitivity for detecting partial thickness tears, and the sensitivity of US may be much lower than that of MRI. The strength of evidence for all test comparisons is limited because most studies were small, heterogeneous and methodologically flawed, and there were few comparative studies. Well designed studies that directly compare MRI, MRA and US for detection of rotator cuff tears are needed.
Keywords: Humans, Arthroscopy, Magnetic Resonance Imaging, Rotator Cuff Injuries, Ultrasonography, Arthrography, Arthrography/methods, Prospective Studies, Rotator Cuff, Rotator Cuff/surgery, Shoulder Pain, Shoulder Pain/etiology, Shoulder Pain/surgery
Plain language summary
Diagnostic tests for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered
This summary of a Cochrane review presents what we know from research about the accuracy of imaging tests to detect tears of the rotator cuff tendons in the shoulder.
The rotator cuff is a group of tendons involved in the positioning and moving of the shoulder joint. The rotator cuff lets people lift their arm and reach overhead. In a lot of people, wear and tear of the rotator cuff tendons is a normal part of ageing and they may not have symptoms. However, many people will develop pain in their shoulder at some point as the tendons degenerate further and tears in the rotator cuff tendons develop. There may also be inflammation of the shoulder tendons or bursa (a sac with internal gliding surfaces that helps the shoulder to move). Often the pain is made worse by sleeping on the affected shoulder and moving the shoulder in certain directions. Often there will be pressure on the tendons by the overlying bone when lifting the arm up. This is called impingement. It may become difficult to use the shoulder in every day activities, sports or work.
If the pain does not go away by itself or with treatments such as steroid injections or physiotherapy, surgery may be performed. Imaging tests such as magnetic resonance imaging (MRI), magnetic resonance arthrography (MRA) and ultrasound (US) are used to assess the presence and size of rotator cuff tears to assist in the planning of the surgery.
Rotator cuff tears can be classified as full or partial thickness tears based on the extent or size of the tears. No test is 100% accurate in identifying tears or assessing their size. The accuracy of the tests is commonly assessed by the sensitivity of the test (the proportion of people who had a tear according to the test, among patients with tears), and specificity (the proportion of people without tears on the test, among patients with no tears).
We searched electronic databases up to February 2011, as well as trial registers, conference proceedings and reference lists of articles, for studies comparing diagnostic tests for people with suspected rotator cuff tears. Our review included 20 studies (1147 shoulders). Many studies had design flaws, which limited the reliability of their findings. We found that MRI, MRA and US may have similar accuracy for detecting the presence of full thickness tears. For identifying any tears (no distinction between partial or full thickness) or identifying partial thickness tears, MRI and US may also have similar accuracy. However, it appears that compared with US, MRI may be more sensitive in identifying partial thickness tears. With these results we can conclude that all three imaging tests (MRI, MRA and US) may help decisions regarding referral for surgery for people with suspected full thickness tears. Information on adverse effects of using these tests was not reported by the included studies.
Summary of findings
Summary of findings'. 'Summary of findings table.
| What is the best imaging modality for rotator cuff tears? | |||||||
| Patient population | Patients with shoulder pain suspected of having a rotator cuff tear for whom surgery is being considered. | ||||||
| Prior testing | Clinical examination. | ||||||
| Settings | Secondary or tertiary care. | ||||||
| Index tests | Magnetic resonance imaging (MRI), magnetic resonance arthroscopy (MRA) and ultrasonography (US). | ||||||
| Reference standard | Arthroscopy and/or open (including mini‐open) surgery findings. | ||||||
| Target condition | Rotator cuff tears: any tear or full or partial thickness tears. | ||||||
| Importance | Imaging tests are usually performed to determine the characteristics of the rotator cuff tears in order to plan surgery. | ||||||
| Included studies | We included 20 (1147 shoulders) prospective accuracy studies that evaluated at least of one of the tests. Six of the 20 studies reported results for 2 tests evaluated in the same patients. |
||||||
| Quality concerns | Patient characteristics and study design were poorly reported. Most of the QUADAS items were scored unclear for many studies. |
||||||
| Limitations | We observed considerable variation in results between studies, especially for US studies. Criteria for test positivity (index tests and reference standard) varied between studies. We could not formally investigate potential sources of heterogeneity due to the number of studies available for each test or because most studies reported the same value for a covariate. Our findings were based on small studies with poor reporting of patient characteristics and study design. Because there were few comparative studies, test comparisons relied on indirect evidence which may be confounded by differences in patient and study design characteristics. No study evaluated MRA, MRI and US in the same population. |
||||||
| Test | Studies | Cases/Shoulders | Summary sensitivity (95% CI) | Summary specificity (95% CI) | Consequences in a cohort of 100 | ||
| Median prevalence% (range)1 | Missed cases2 |
Over treated2 |
|||||
| Any rotator cuff tears | |||||||
| MRI | 6 | 263/347 | 98 (92, 99) | 79 (68, 87) | 80 (34 to 96) | 2 | 4 |
| US | 13 | 626/854 | 91 (83, 95) | 85 (74, 92) | 7 | 3 | |
| MRA3 | 3 | 145/183 | – | – | – | – | |
| Full thickness tears | |||||||
| MRI | 7 | 193/368 | 94 (85, 98) | 93 (83, 97) | 56 (17 to 80) | 3 | 3 |
| US | 10 | 386/729 | 92 (82, 96) | 93 (81, 97) | 4 | 3 | |
| MRA | 3 | 107/183 | 94 (80, 98) | 92 (83, 97) | 3 | 4 | |
| Partial thickness tears | |||||||
| MRI | 6 | 83/347 | 74 (59, 85) | 93 (84, 97) | 14 (3 to 54) | 4 | 6 |
| US | 8 | 121/660 | 52 (33, 70) | 93 (85, 97) | 7 | 6 | |
| MRA3 | 4 | 65/233 | – | – | – | – | |
| Comparisons of the imaging tests for each type of tear | |||||||
| Comparison | Findings | ||||||
| MRIand US for any rotator cuff tears | We did not perform meta‐analysis of MRA studies. The sensitivity of MRA ranged between 72% and 100% and the specificities between 5% and 82% in the three studies. There was a 7% difference in the sensitivities of MRI and US, and a 6% difference in specificities. The differences were not statistically significant (P = 0.13). Given a median prevalence of 80%, 80 out of 100 patients will have any rotator cuff tears. Of the 80 cases, two will be missed if tested using MRI or seven will be missed if tested using US. Of the 20 patients without any rotator cuff tears, four will undergo unnecessary surgery if tested using MRI or three If tested using US. |
||||||
| MRI, US and MRA for full thickness tears | MRA, MRI and US had very similar sensitivities and specificities. There was no evidence to suggest a difference in sensitivity or specificity between the tests (P = 0.7). |
||||||
| MRI and US for partial thickness tears | We did not perform meta‐analysis of MRA studies. The sensitivity of MRA studies ranged between 62% and 80% and the specificities between 47% and 100% in the four studies. Comparing MRI and US, the specificities were found to be similar and despite the large difference in sensitivity (22%), there was no evidence to suggest a difference in sensitivity or specificity between both tests (P = 1.0). Given a median prevalence of 14%, 14 out of 100 patients will have partial thickness tears. Of the 14 cases, two will be missed if tested using MRI but if tested using US, seven will be missed. Of the 20 patients without any rotator cuff tears, four patients will undergo unnecessary surgery if tested using MRI or three patients If tested using US. |
||||||
|
Conclusions: MRI, US and MRA have good diagnostic accuracy for detection of full thickness tears and may perform similarly. The performance of MRI and US may be comparable for detection of partial thickness tears or for detection of any rotator cuff tears. The strength of the evidence for all test comparisons is limited because most studies were small and methodologically flawed, and there were few comparative studies. Well designed studies that directly compare the three tests for detection of rotator cuff tears are needed. There was limited evidence on the best test to diagnose subscapularis tendons tears. | |||||||
1 The median prevalence and range were computed using all the studies that evaluated each target condition. 2 Missed and over treated numbers were computed using the median prevalence for each target condition.
3 Meta‐analyses were not performed for studies that evaluated partial thickness tears and those of any rotator cuff tears because there were few studies and considerable heterogeneity in estimates of sensitivity or specificity.
Background
Target condition being diagnosed
The rotator cuff is composed of the subscapularis, supraspinatus, infraspinatus and teres minor tendons; the long head of the biceps tendon also contributes to the cuff. The role of the rotator cuff is to stabilise the humeral head into the glenoid cavity, preventing the upward migration of the humeral head. The four muscles are recruited during different arm movements. The subscapularis is recruited in internal rotation, the supraspinatus in elevation, and the infraspinatus and teres minor in external rotation (Clark 1992; Favard 2007; Matsen 2008).
Rotator cuff tendinopathy can lead to progressive failure of the rotator cuff, typically progressing from partial to a full thickness tear of the supraspinatus tendon then extending into the infraspinatus tendon or the subscapularis tendon, or both. A review by Lewis 2009 concluded that the pathoaetiology of rotator cuff tears is multifactorial and that tears are correlated with a combination of extrinsic and intrinsic factors, but that more research is necessary to fully understand the aetiology of rotator cuff tears. The extrinsic factors (i.e. those external to the rotator cuff) can be divided into anatomical factors, such as the shape of the acromion (i.e. curved or hooked) and coracoacromial ligament, os acromiale and acromial spurs (Baring 2007; Bigliani 1991; Lewis 2009; Neer 1972; Neer 1983; Nho 2008), and environmental factors including aging, shoulder overuse, smoking, obesity and some metabolic disorders such as diabetes (Chen 2003; Galatz 2006; Harryman 2003; Lewis 2009; Nho 2008; Wendelboe 2004). The intrinsic factors include, among others, repetitive microtrauma, areas of hypoperfusion in the tendons, inflammation and cellular changes in the tendons such as disorganisation of the architecture of collagen (Biberthaler 2003; Levy 2008; Lewis 2009; Nirschl 1989; Rees 2008).
Shoulder pain is very common, with an incidence of 9.5 per 1000 patients in primary care in Cambridge, UK, where amongst them 85% presented with rotator cuff tendinopathy (Ostör 2005). Disorders of the rotator cuff tendons due to either wear or tear are among the most common causes of shoulder pain and disability. In Japan, the prevalence of rotator cuff tears is 20.7% in the general population and 36% in patients with shoulder pain (Yamamoto 2010). More than 4.5 million physician visits occurred and approximately 40,000 inpatient surgeries were performed for rotator cuff problems in the United States in 2002 (Oh 2007).
The diagnosis of rotator cuff tears is mainly based on the patient's history and physical examination. The value of physical examination of the shoulder has been addressed in another Cochrane review (Hanchard 2013). The clinical manifestations vary widely (Duckworth 1999; Matsen 2008). Acute, traumatic full thickness cuff tears may present with sudden onset of weakness during elevation of the arm after a trauma in which the arm has been forced to the side (like a fall with the arm out to the side or on catching a heavy falling object with the arm extended) (Matsen 2008). Chronic degenerative cuff defects may present with progressive pain and weakness, with concomitant loss of active motion. Pain in the lateral area of the shoulder is commonly present at night. Passive motion initially remains full until the pain limits active motion (Baring 2007; Matsen 2008). However, there are many people with degenerative rotator tears who are asymptomatic (Reilly 2006; Zanetti 2000).
Decisions about whether to order a diagnostic test include consideration of whether the results are likely to affect treatment. Plain radiographs of the shoulder may be useful to differentiate rotator tears from osteoarthritis of the glenohumeral or acromioclavicular joints and calcific tendonitis. Ultrasonography (US), magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) are increasingly being used to detect rotator cuff tears, although who orders these tests may vary by setting. In some settings, these tests are mainly ordered by specialists but in other settings they are being ordered by primary care physicians or clinicians (Al‐Shawi 2008; Miller 2008). In the context of specialist care, US or MRI, or both, are usually performed to determine the characteristics of the rotator cuff tears in order to plan surgery. In some settings, however, there has been a significant rise in the number of diagnostic US being performed in primary care. For example, in Australia there has been a more than fourfold increase, from 104,252 in the year 2000 to 2001 to 440,172 in 2008 to 2009 (Medicare Australia 2010). However, the utility of the test to affect treatment in primary care is unknown.
Tears of the rotator cuff can be classified in several ways: duration (acute or chronic), aetiology (traumatic or degenerative) or size (partial or full thickness). Radiologists often describe the size of tear in millimetres or centimetres or descriptively as small, medium, large or massive. All three factors (duration, aetiology and size) influence treatment decisions (Kuhn 2007).
Acute full thickness rotator cuff tears are uncommon and account for less than 10% of all rotator cuff tears. People with acute full thickness tears usually present with a history of acute trauma, such as a fall or dislocation, and immediate pain and weakness. Prompt surgical treatment, ideally within six weeks, is the recommended treatment (Rees 2008). For all other full thickness rotator cuff tears, surgical treatment is usually reserved for those who fail to improve after a period of conservative treatment, although the most effective surgical intervention and its timing remain uncertain (Coghlan 2009; Dunn 2005; Oh 2007; Rees 2008). For example, a delay in surgical repair of a large tear may allow the injured tendon to retract and the muscle to atrophy (Matsen 2008; Oh 2007). On the other hand, asymptomatic tears are common; these are chronic tears that normally do not compromise the function of the shoulder. A recent review reported the prevalence of full thickness tears in 2553 unselected cadavers as 30% (Rees 2008). Furthermore, the pathogenesis and progression to symptomatic tears remains unclear (Rees 2008). In addition, in contrast to acute full thickness tears, symptoms due to acute or chronic partial thickness cuff tears frequently improve with conservative interventions (Matava 2005; Matsen 2008).
While spontaneous healing of a partial thickness tear is unlikely in most cases, the explanation for the ‘cure’ with conservative treatment is due to the likely resolution of the accompanying inflammation over time and may also be related to the residual cuff muscles compensating for the mechanical deficiency of the torn cuff (Fukuda 1996; Fukuda 2003; Matava 2005; Matsen 2008). As with full thickness tears, no simple treatment algorithm for partial thickness rotator cuff tears exists. Surgical treatment, however, is normally indicated for people with persisting symptoms despite conservative treatment and in whom imaging suggests the presence of a partial thickness tear or tears. The ideal timing of surgical intervention also remains unclear (Fukuda 2003; Matava 2005). However, case series and anecdotal evidence suggest that satisfactory results are usually achieved with surgery provided there is a good blood supply to the tendon, contact between the torn ends, absence of retraction and adequate trophic quality of the muscle (Fukuda 2003).
Another recognised category of tears is massive complete tears, in which a large area of the humeral head is uncovered (Wolfgang 1974). Post 1983 defined a massive tear as greater than 5 cm. These tears, which are difficult to repair, are more commonly found in women over 65 years of age and are associated with advanced atrophy, degeneration and progressive fatty infiltration of the rotator cuff muscles (Dines 2007; Gerber 2000). Treatment options for these massive, retracted tears are limited as they are often deemed irreparable. In younger people, tendon transfers may be considered (Neri 2009).
The indications for surgical treatment of rotator cuff tears have not been fully defined. A systematic review of surgical treatment for rotator cuff disease (including tears), which included 14 trials, was unable to draw firm conclusions about the effectiveness of surgery (Coghlan 2009). Nonetheless, the review suggested that there were no significant differences in outcomes between open or arthroscopic surgery and non‐surgical treatment (Coghlan 2009). Many studies have demonstrated that the size of the tear is correlated to the final outcome; partial or small full thickness tears usually have a satisfactory surgical result (Bianchi 2005; Bryant 2002; Fotiadou 2008).
Index test(s)
Currently, US, MRI or MRA are usually performed in patients contemplating surgery for rotator cuff tears to determine the characteristics of the tears. With the improvement of technology, the accuracy of these imaging tests is considered to have improved significantly over time, enabling useful assessment of the size and extent of the rotator cuff tear when planning surgery (Rees 2008).
US is a diagnostic imaging technique used to visualise deep structures of the body by recording the echoes of pulsed ultrasonic waves directed into the tissues and reflected by tissue planes to the transducer. These echoes are converted into 'pictures' of the tissues under examination. Seltzer 1979 was the first to describe ultrasonographic evaluation of rotator cuff diseases. US of the shoulder is utilised in secondary, tertiary and, increasingly, primary healthcare settings to evaluate the integrity of the rotator cuff. It consists of a non‐invasive examination that has practically no adverse effects and allows dynamic visualisation of the tendons during movement of the shoulder (Al‐Shawi 2008). However, operator dependence and a long learning curve are frequently considered to be its limitation (O'Connor 2005; Rutten 2006), principally in view of partial thickness tears for which Le Corroller 2008 described a high interobserver variability.
MRI uses a powerful magnetic field to align the hydrogen atoms of water and other molecules in the body. Pulses of radiofrequency are applied which excite the magnetised atoms. These movements of hydrogen atoms, which vary in different tissues, are captured and the signal can be manipulated to build up an image of the body (Witte 2003). The first article about the use of MRI in the shoulder was published in 1986 (Kneeland 1986). Since then, this technique has been widely used in secondary and tertiary healthcare practice. MRI is a non‐invasive method of imaging that is unique in allowing high resolution images in multiple planes. It is a static examination that may be enhanced by an intra‐articular injection of radiopaque dye (this is called magnetic resonance arthrography). The radiopaque dye acts as contrast material that helps to delineate intra‐articular structures and outline abnormalities. MRA of the shoulder is also useful for assessing the rotator cuff integrity. In comparison with conventional MRI, MRA may improve diagnostic performance in detecting shoulder diseases; however, any potential benefit from MRA must be weighed against the invasiveness and additional discomfort caused by the procedure.
MRI and MRA have some absolute contraindications, such as the presence of intracerebral aneurysm clips, cardiac pacemakers, automatic defibrillators, biostimulators, implanted infusion devices, cochlear implants and metallic orbital foreign bodies (Witte 2003). They are also expensive and time consuming procedures. The strength of the magnet, the sequences used in the examinations and the person (e.g. consultant radiologist, musculoskeletal radiologist or trainee) interpreting and reporting the test may all affect the results.
Summary of diagnostic pathway
The evaluation of patients with suspected rotator cuff tear(s) should initiate with a full history of the patient's complaints and a thorough clinical examination of the shoulder. Decisions for using an imaging diagnostic test may be supported by whether the results are likely to affect treatment. For example, MRI, MRA or US might confirm a possible full thickness tear. The three index tests considered can also be used as triage tests in people suspected of having partial thickness tears. People whose tests were positive can be treated as having partial tears, while people with rotator cuff symptoms whose tests were negative can undergo further diagnostic procedures, such as diagnostic arthroscopy.
Reference tests
The reference tests for diagnosis of rotator cuff tears are invasive. The most common reference test is diagnostic arthroscopy. Arthroscopy is a minimally invasive surgical procedure that involves insertion of an arthroscope, a type of fibre‐optic endoscope, into the joint through a small incision. This allows the surgeon to inspect and probe the articular (joint) and bursal side of the rotator cuff tendons, to assess accurately the rotator cuff insertion (footprint) and to perform a general examination of the shoulder joint in order to identify and treat other potential lesions (Dinnes 2003; Matava 2005). However, limitations associated with diagnostic shoulder arthroscopy include the need for anaesthesia, hospital admission and some interobserver variation in the classification of tears (Kuhn 2007).
Open surgery (including mini‐open) has also been used as a reference test although it is more limited than arthroscopy because joint surface or inferior surface tears are difficult to access and identify using an open approach. Thus open surgery is less accurate than arthroscopy for detecting partial rotator cuff tears.
Rationale
US, MRI and MRA are increasingly being used to assess the presence and size of rotator cuff tears to assist in planning surgical treatment. Improved techniques have resulted in increased reliance on these tests, in place of a separate diagnostic arthroscopy, although arthroscopic examination of the shoulder joint is still commonly performed as part of surgical treatment. US, MRI and MRA are operator and reader dependent. It is not known whether any one test is superior to either of the two others or whether performing US and MRI or US and MRA enhances their value (Swen 1999). It is also not known whether these diagnostic tests provide useful additional information compared with diagnostic arthroscopy, which is an accepted part of the surgical treatment. While, the units costs of MRI and MRA are greater than US, the cost‐effectiveness of the three tests has not been determined.
We identified two relevant systematic reviews with meta‐analyses that assessed diagnostic imaging tests for rotator cuff disease (De Jesus 2009; Dinnes 2003). The literature search in both reviews was restricted to English language only. Dinnes 2003 evaluated the diagnostic accuracy of clinical testing of US, MRI and MRA for detecting rotator cuff tears using both surgical and non‐surgical tests as the reference standard. The authors included 38 studies that assessed the accuracy of US, 29 studies that assessed the accuracy of MRI and 6 studies that assessed the accuracy of MRA and concluded that US or MRI were equivalent for detecting full thickness rotator cuff tears, although MRI was more expensive and US may be better at detecting partial tears. The search date for the review was October 2001. A later review with a search date in September 2007, De Jesus 2009, conducted a meta‐analysis comparing the diagnostic accuracy of US and MRI for rotator cuff tears using surgery as the reference standard. This systematic review included 65 studies but the appraisal of the methodological quality of the included studies was unclear or inadequate. De Jesus 2009 concluded that US is as accurate as MRI for both full and partial thickness rotator cuff tears and also suggested that US may be the most cost‐effective imaging test for detecting rotator cuff tears.
Important technological improvements in US, MRI and MRA have been made since the search dates of both systematic reviews, and new studies evaluating US, MRI and MRA have been published. Our review involves an updated search for diagnostic accuracy studies for rotator cuff tears and will not be restricted to English language publications.
Objectives
To compare the diagnostic test accuracy of magnetic resonance imaging (MRI), magnetic resonance arthrography (MRA) and ultrasonography (US) for detecting any rotator cuff tears (i.e. partial or full thickness) in people with shoulder pain for whom surgery is being considered.
We divided our objectives as follows.
To compare the diagnostic accuracy of US, MRI and MRA for diagnosing any rotator cuff tears (partial or full thickness)
To compare the diagnostic accuracy of US, MRI and MRA for diagnosing full thickness rotator cuff tears (one or more tendons)
To compare the diagnostic accuracy of US, MRI and MRA for diagnosing partial thickness rotator cuff tears
Investigation of sources of heterogeneity
We planned to investigate the following potential sources of heterogeneity:
Type of tear: acute traumatic and chronic degenerative
Type of reference standard: open (including mini‐open) surgery or arthroscopy
Methods
Criteria for considering studies for this review
Types of studies
All diagnostic accuracy studies that compared one or more of the index tests with one or both of the reference tests in patients suspected of having a partial or full thickness rotator cuff tear were included. We only included results from full reports of prospective studies. Studies with an excessively long period of time (i.e. a year or longer) between the index and reference tests were excluded because there is evidence that rotator cuff tears can progress over time (Mall 2010; Melis 2010); however, the rate of progression is not clearly defined.
We included articles in English and languages for which a full translation could be obtained. Non‐English articles where a full translation could not be obtained are cited in the Characteristics of studies awaiting classification but not included in the review.
For studies reported in multiple publications, we included only the most recent or complete report. References to the other publications were cited under the same study identifier.
Participants
We included people with shoulder pain suspected of having a rotator cuff tear for whom surgery was being considered. Studies that included healthy controls or participants who had been previously diagnosed with other specific shoulder pain (e.g. shoulder instability, osteoarthritis, rheumatoid arthritis, frozen shoulder, benign or malignant tumours or referred pain) were excluded. Studies that included participants with shoulder pain, but in which it was unclear if all the participants were suspected of having rotator cuff tears, were also excluded.
Index tests
Studies that assessed the accuracy of US, MRI or MRA were included.
Target conditions
We included studies that evaluated the index tests for detection of at least one of three target conditions:
presence of any rotator cuff tears (partial or full thickness);
presence of full thickness tears;
presence of partial thickness tears.
To standardise classification for this review, rotator cuff tears were dichotomised as absence or presence of any, full and partial thickness tears.
Reference standards
We required arthroscopy or open (including mini‐open) surgery findings to be the reference standards.
Search methods for identification of studies
Electronic searches
We searched relevant computerised databases for eligible diagnostic studies: MEDLINE (PubMed) (1966 to March 2011), EMBASE (Elsevier) (1980 to February 2011), LILACS (Bireme) (1982 to February 2011) and the Cochrane Register of Diagnostic Test Accuracy Studies (February 2011). We also searched DARE (Database of Abstracts of Reviews of Effects), the HTA Database (Health Technology Assessments Database) and the MEDION database (February 2011) for other related diagnostic test accuracy reviews, and we checked the reference lists of those reviews that were relevant for additional studies. We also searched the US Health Services Research Projects in Progress and the UK Clinical Research Network Portfolio Database for ongoing and recently completed studies. When possible, non‐English articles were assessed through translation by a native speaker.
We used a sensitive search strategy as recommended by the Cochrane Collaboration for MEDLINE (PubMed), EMBASE (Elsevier) and LILACS (Bireme) (De Vet 2008). See Appendix 1 for the MEDLINE and EMBASE search strategies.
Searching other resources
We checked the reference lists of articles, reviews and textbooks for relevant primary diagnostic studies and systematic reviews. We handsearched abstracts of the British Elbow and Shoulder Society annual meetings (2005 to July 2011) and American Academy of Orthopaedic Surgeons annual meetings (2005 to July 2011). We also contacted experts in the field.
Data collection and analysis
We used the methods suggested in the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy (Deeks 2009).
Selection of studies
Two review authors (ML and RJ) independently screened the titles and abstracts of retrieved records to identify potentially relevant studies for inclusion. Duplicates were removed and the remaining references were examined. Studies which clearly did not meet the inclusion criteria were excluded, and copies of the full text of potentially relevant references were obtained. ML and RJ independently assessed full text reports and determined inclusion or exclusion of the studies. Any uncertainties or disagreements were resolved by discussion and, when necessary, by adjudication from a third author (RB).
Data extraction and management
Two review authors (ML and RJ) independently collected the available data using a piloted data extraction form without masking of study authors or other identifying information. A third review author (RB) was consulted for resolution of any disagreements. When necessary, we sent requests to study authors for additional information or data. Diagnostic accuracy studies that reported insufficient data for construction of two‐by‐two tables were excluded from the review.
We retrieved the following data.
General information: title, journal, year, publication status, country of study, period of study, primary objective and study design (i.e. prospective versus retrospective and consecutive versus non‐consecutive).
Sample size: number of participants meeting the criteria and total number screened.
Baseline characteristics: baseline diagnosis, age, sex, dominant arm, nature of onset (e.g. traumatic or non‐traumatic), duration of symptoms, prior treatment, inclusion and exclusion criteria.
Target condition as reported.
Index test: description of technique, criteria for positive result, timing of test and expertise of the clinician or technician performing the test.
Reference standard test: description of technique, criteria for positive result, time from index to reference test and expertise of the clinician or technician performing the test.
Adverse effects or complications due to index test(s) and reference standard test(s).
Number of true positives (TP), true negatives (TN), false positives (FP) and false negatives (FN). We extracted data for operational definitions for category of tear (e.g. partial, full or any thickness tears). Multiple outcome categories are often reported for rotator cuff tears: partial thickness tear, full thickness tear and no tears (i.e. three‐by‐three tables). Currently available methods for evaluating diagnostic tests rely on dichotomised disease status. Therefore, for the assessment of each target condition, we dichotomised rotator cuff tears using a strategy based on the options for treatment. To create two‐by‐two tables for partial thickness tears, data for full thickness tears were included with those for no tears. We did not exclude data for any category. We included data for partial thickness tears with those for full thickness tears to create two‐by‐two tables for any tears.
Assessment of methodological quality
The methodological quality of the included studies was assessed independently by two review authors (ML and RJ) and disagreement on study quality was resolved by a third review author (RB). At the same time as data extraction, the methodological quality of selected studies was assessed using a modified version of the QUADAS checklist (Whiting 2003), following the guidelines provided in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy (Reitsma 2009). Appendix 2 explains how we applied the QUADAS items for assessing the included studies.
Statistical analysis and data synthesis
Our unit of analysis was the shoulder. For each test and target condition, estimates of sensitivity and specificity from each study were plotted in receiver operating characteristic (ROC) space and forest plots for visual examination of variation in test accuracy. Where adequate data were available, we conducted meta‐analyses using the bivariate model (Chu 2006; Reitsma 2005). In the bivariate model, the logit‐transformed sensitivities and specificities, and the correlation between them across studies are modelled directly. The model accounts for sampling variability within studies and also accounts for between study variability through the inclusion of random‐effects. In preliminary meta‐analyses for each target condition, we fitted the bivariate model separately for each test. We examined the variance of the random‐effects parameters to consider the magnitude of heterogeneity and to judge whether there were differences in heterogeneity in sensitivities and specificities between tests, before comparing the tests in a single model for formal assessment of comparative accuracy.
Comparative accuracy studies are scarce (Takwoingi 2013). Therefore, whenever possible, we included all studies of US, MRI and MRA (i.e. an indirect comparison) in the main comparative meta‐analysis for each target condition. Due to few studies of MRA and considerable heterogeneity in study results, we only performed pairwise comparisons of MRI and US for detection of partial thickness tears and any tears but compared the three tests for detection of full thickness tears. We compared test accuracy by adding covariate terms for test type to the parameters of the bivariate model to determine which test was superior in terms of sensitivity or specificity or both. The variance coefficients from the preliminary meta‐analysis and summary ROC plot for each test indicated differences in heterogeneity between tests and so we extended the bivariate model to allow the variances of the random‐effects to vary with test type. We assessed the statistical significance of the difference in sensitivity or specificity between tests by using likelihood ratio tests comparing models with and without the covariate terms in the bivariate model. The summary sensitivities and specificities (i.e. average operating points) were plotted on summary ROC plots with corresponding 95% confidence regions. Summary positive and negative likelihood ratios were derived from functions of the bivariate model parameters, with 95% confidence intervals computed using the delta method.
Indirect comparisons of tests are not ideal and are susceptible to bias because other factors, such as participant and study design characteristics, may confound differences between tests. Thus in secondary analyses, we restricted the test comparisons to only studies that evaluated the tests in the same population. Because the studies were few, we were unable to perform meta‐analyses but used linked summary ROC plots where estimates for each of the two tests from each study are joined by a line to illustrate the results. Furthermore, for each target condition, we quantified the difference in sensitivities and specificities between pairs of tests by computing differences in these proportions together with the corresponding 95% CI. Thus we visually and numerically demonstrated the change and consistency of the direction of the change in test performance between the tests. We used the xtmelogit command in Stata version 11.2 (StataCorp, College Station, Texas) to fit the bivariate models.
Investigations of heterogeneity
Heterogeneity was investigated in the first instance through visual examination of forest plots and summary ROC plots. The type of tear and type of reference standard reported in each study were presented on forest plots along with the estimates of sensitivity and specificity. In exploratory analyses, we ordered studies on the forest plots by each of the two covariates in turn and also by sensitivity or specificity to examine the pattern of variation between studies. If there were sufficient data we planned to formally investigate heterogeneity by adding covariates to the bivariate model for each potential source of heterogeneity.
Sensitivity analyses
If there were sufficient studies, we performed sensitivity analyses by comparing results based on all studies with results of subsets of studies that complied (scored 'Yes') with the following methodological quality items of the QUADAS checklist (Whiting 2003).
Representative spectrum
Acceptable reference standard
Acceptable delay between tests
Index test results blinded
Reference standard results blinded
We also investigated the effect of unit of analysis by excluding studies that included both shoulders for any individual.
Results
Results of the search
The search strategy identified 3169 references and the handsearch identified an additional three records (Figure 1). Of these, 2902 were excluded by initial screening of reference titles and abstracts. There were 974 duplicates and 1926 were either not relevant or did not meet the inclusion criteria. We were unable to obtain full text articles for two studies because they were not available from libraries or vendors.
1.
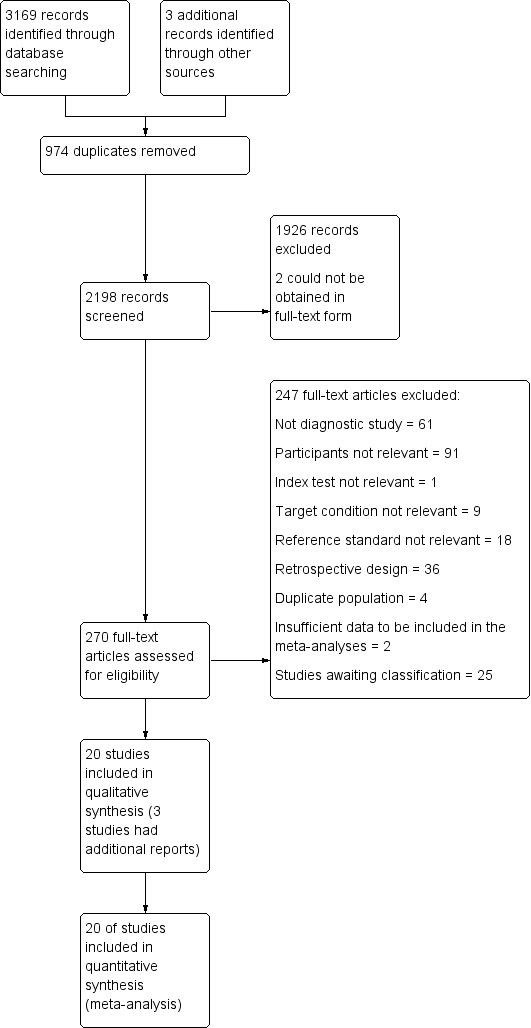
Study flow diagram
Of the 270 potentially eligible studies that were remaining and for which full reports were obtained (192 were reported in English and 78 in a non‐English language), 20 studies met our inclusion criteria and were included in the review. Three of the included studies had additional published data. Two hundred and eighteen studies did not meet our inclusion criteria and were excluded (see Characteristics of excluded studies) and four reported on the same population or a subset of an already excluded study. At the time of publication, we are still awaiting translation of 25 non‐English articles that are potentially relevant based upon their title and abstract; these are listed in Studies awaiting classification. Data from these studies will be added in future updates of this review if the studies are found to be eligible for inclusion.
Among the 20 included studies, six (Iannotti 2005; Kang 2009; Martin‐Hervas 2001; Sipola 2010; Swen 1999; Teefey 2004) evaluated the accuracy of two different tests against the reference standard(s). See the Characteristics of included studies for details of the individual studies.
Methodological quality of included studies
The methodological quality of the 20 included studies was judged to be low or unclear for most categories and is summarised in Figure 2. The quality assessment results for the individual studies can be found in Figure 3 and details are given in the Characteristics of included studies.
2.
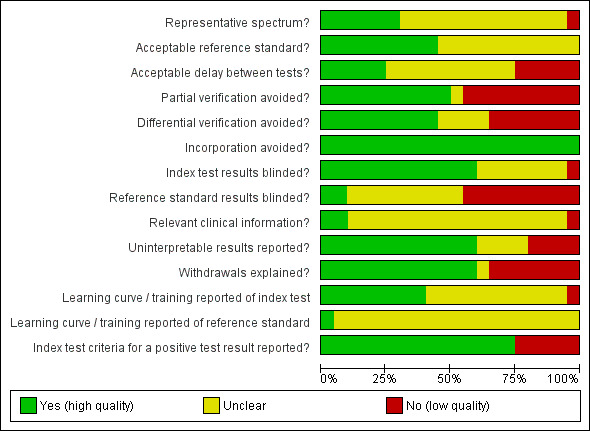
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies
3.
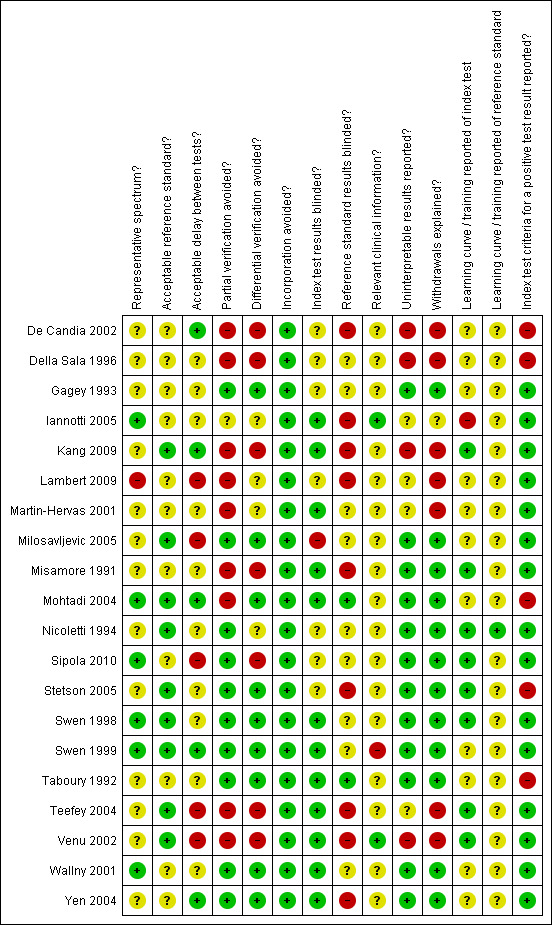
Methodological quality summary: review authors' judgements about each methodological quality item for each included study
The spectrum of participants (item 1) was judged to be representative in only 6 (30%) of the 20 studies. To be judged representative, studies had to be prospective with consecutive recruitment. The setting had to be secondary or tertiary care and the patients had to present with shoulder pain caused by a suspected rotator cuff tear for which surgery was being considered for treatment. Only half of the studies included an appropriate reference standard (item 2) and avoided partial verification (item 4). The majority (more than 50%) of studies poorly described the following QUADAS items: time period between reference standard and index test (item 3), differential verification bias (item 5), reference standard results blinded (item 8), relevant clinical information (item 9), and learning curve and training reported for both the index and reference standard readers (items 12 and 13) (seeAppendix 2 for further explanation of these items). The remaining QUADAS items were well described in 50% to 75% of the included studies: index test results blinded (item 7), un‐interpretable results reported (item 10), withdrawals explained (item 11) and index test criteria for a positive result (item 14). Criteria for test positivity was reported by 15 studies and varied between studies; the criteria are presented in detail in the Characteristics of included studies. As we anticipated in our protocol, the answer for 'incorporation avoided' (item 6) was 'Yes' (no bias) for all included studies.
Findings
Our meta‐analyses were based on indirect comparisons because meta‐analyses of studies that directly compared tests were not possible; there were only six comparative studies. No study directly compared MRA and MRI, or all three modalities in the same patients for any of the target conditions.The summary sensitivities and specificities for the tests are shown in Table 2 for each target condition. For MRA, meta‐analysis was performed only for studies evaluating detection of full thickness tears due to the few studies and the degree of heterogeneity observed on summary ROC plots for studies evaluating partial thickness tears and any rotator cuff tears.
1. Comparison of MRI, US and MRA for detection of any rotator cuff tears (partial or full thickness) using all studies (indirect comparison).
| Index test | Studies | Shoulders | Cases | Summary sensitivity (95% CI) | Summary specificity (95% CI) | LR+ | LR– | Test1 |
| Any rotator cuff tears | ||||||||
| MRI | 6 | 347 | 263 | 98 (92, 99) | 79 (68, 87) | 5 (2, 10) | 0.03 (0.01, 0.11) | P = 0.13 |
| US | 13 | 854 | 626 | 91 (83, 95) | 85 (74, 92) | 6 (3, 12) | 0.11 (0.05, 0.22) | |
| Full thickness tears | ||||||||
| MRI | 7 | 368 | 193 | 94 (85, 98) | 93 (83, 97) | 13 (6, 29) | 0.06 (0.02, 0.16) | P = 0.7 |
| MRA | 3 | 183 | 107 | 94 (80, 98) | 92 (83, 97) | 12 (5, 30) | 0.06 (0.02, 0.23) | |
| US | 10 | 729 | 386 | 92 (82, 96) | 93 (81, 97) | 12 (5, 34) | 0.09 (0.04, 0.20) | |
| Partial tears | ||||||||
| MRI | 6 | 347 | 83 | 74 (59, 85) | 93 (84, 97) | 10 (4, 26) | 0.28 (0.17, 0.48) | P = 1.00 |
| US | 8 | 660 | 121 | 52 (33, 70) | 93 (85, 97) | 8 (3, 19) | 0.52 (0.33, 0.80) | |
1 Likelihood ratio test for evidence of a difference in sensitivity and/or specificity between the tests.
LR+ = positive likelihood ratio; LR– = negative likelihood ratio
Two studies (Iannotti 2005; Milosavljevic 2005) included both shoulders of one and five patients respectively. The remaining studies reported the same number of patients and shoulders, with the exception of Milosavljevic 2005 where this information was missing.
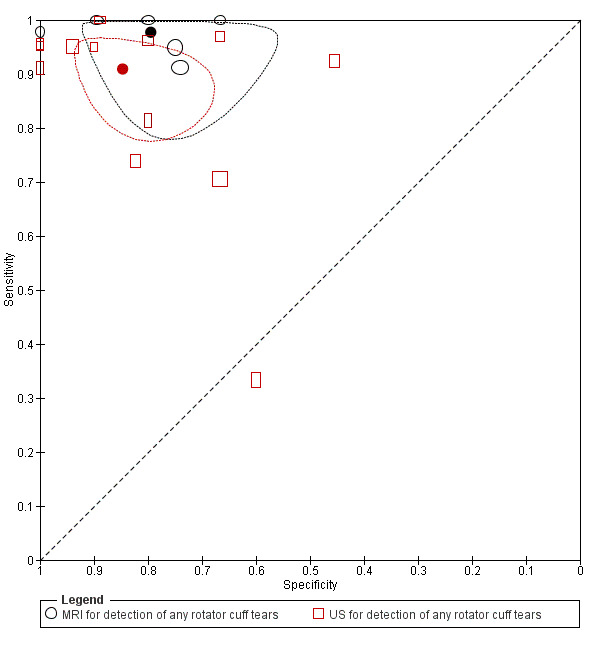
Detection of any rotator cuff tears
Figure 4 shows the forest plots of the sensitivity and specificity estimates for MRI, US and MRA for the 17 studies that assessed any rotator cuff tears.
4.
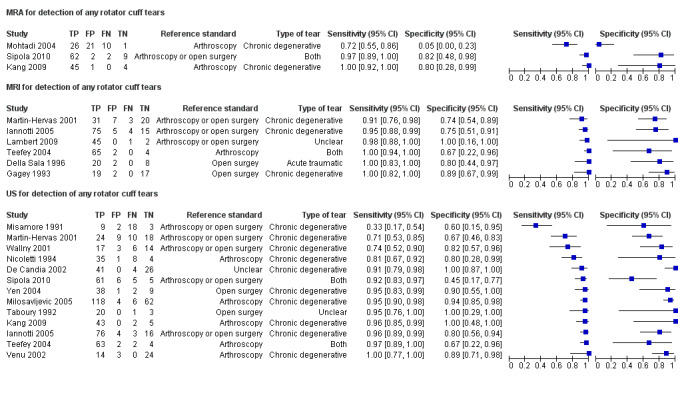
Accuracy of MRA, MRI and US for detecting any rotator cuff tears (forest plot)
Six studies, based on 347 shoulders from 346 patients, assessed the diagnostic accuracy of MRI. The median study size was 55 (range 30 to 99), and the median prevalence of any rotator cuff tear was 73% (range 50% to 96%). The sensitivity of MRI reported in the studies ranged from 91% to 100%, and specificity from 67% to 100%. The summary estimates for the sensitivity and specificity of MRI were 98% (95% CI 92% to 99%) and 79% (95% CI 68% to 87%) respectively. The positive and negative likelihood ratios were 5 (95% CI 2 to 10) and 0.03 (95% CI 0.01 to 0.11) respectively.
Thirteen studies assessed the accuracy of US to detect any rotator cuff tears. The studies included a total of 854 shoulders from 848 patients with a median study size of 50 (range 24 to 190). The prevalence of any rotator cuff tears in the US studies was 80% (range 34% to 92%), and the sensitivities ranged from 33% to 100%, specificities from 45% to 100%. The summary sensitivity and specificity of US were 91% (95% CI 83% to 95%) and 85% (95% CI 74% to 92%) respectively. The positive and negative likelihood ratios were 6 (95% CI 3 to 12) and 0.11 (95% CI 0.05 to 0.22) respectively.
Three studies, based on 183 shoulders from 183 participants, assessed the accuracy of MRA for detection of any rotator cuff tears. The median study size was 58 (range 50 to 75), and the median prevalence was 85% (range 62% to 90%). The sensitivity of MRA ranged from 72% to 100%, and specificity from 5% to 80%. Meta‐analysis was not performed but study specific estimates of sensitivity and specificity were plotted in ROC space with 95% CI in Figure 5.
5.
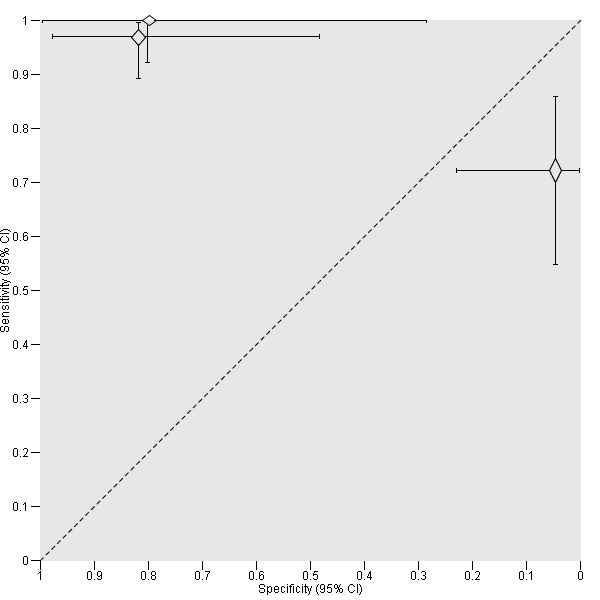
Study estimates of sensitivity and specificity with 95% confidence intervals plotted in ROC space for MRA for the detection of any rotator cuff tears
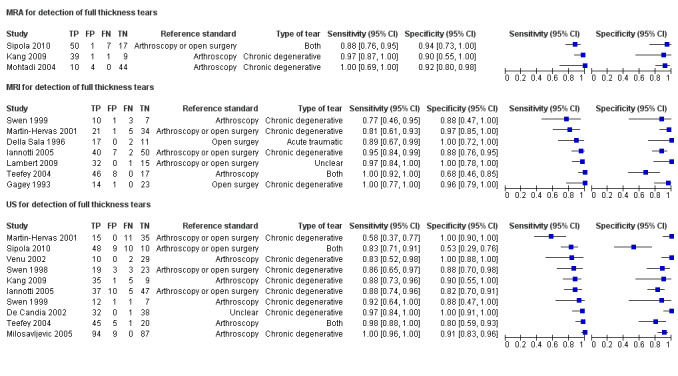
Comparison of MRI and US for detection of any rotator cuff tears
Using the 11 studies that evaluated the accuracy of either MRI or US for detection of any rotator cuff tears, neither test was found to be superior in terms of sensitivity or specificity. Although the sensitivity of MRI was 7% higher than that of US and the specificity of MRI was 6% lower than that of US (Figure 6; Table 2), there was no statistically significant difference between the two tests (P = 0.13). In the analysis restricted to the three studies (231 shoulders from 230 patients) that performed head‐to‐head comparisons of MRI and US within the same patients (Table 3, see Appendix 3 for additional figure), two studies reported higher sensitivity and specificity for MRI compared to US while the other study reported higher sensitivity and specificity for US compared to MRI. For head‐to‐head comparisons of MRA and US, there were only two studies (127 shoulders from 127 patients). Both studies reported higher sensitivity for MRA compared to US but the estimates of specificity were conflicting (Table 4).
6.
Study estimates of sensitivity and specificity, and summary points with 95% confidence regions plotted in ROC space for MRI and US for the detection of any rotator cuff tears
2. Comparison of MRI and US for detection of rotator cuff tears (any, partial or full thickness) limited to studies in which all participants received both MRI and US (direct comparison).
| Study | Cases | Non‐cases | MRI | US | Difference in sensitivity (95% CI) | Difference in specificity (95% CI) | ||
| Sensitivity (95% CI) | Specificity (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | |||||
| Any rotator cuff tears | ||||||||
| Iannotti 2005 | 79 | 20 | 95 (88, 99) | 75 (51, 91) | 96 (89, 99) | 80 (56, 94) | ‐1 (‐8, 5) | ‐5 (‐31, 21) |
| Martin‐Hervas 2001 | 34 | 27 | 91 (76, 98) | 74 (54, 89) | 71 (53, 85) | 67 (46, 83) | 21 (3, 39) | 7 (‐17, 32) |
| Teefey 2004 | 65 | 6 | 100 (94, 100) | 67 (22, 96) | 97 (89, 100) | 67 (22, 96) | 3 (‐1, 7) | 0 (‐53, 53) |
| Full thickness tears | ||||||||
| Iannotti 2005 | 42 | 57 | 95 (84, 99) | 88 (76, 95) | 88 (74, 96) | 82 (70, 91) | 7 (‐5, 19) | 5 (‐8, 18) |
| Martin‐Hervas 2001 | 26 | 35 | 81 (61, 93) | 97 (85, 100) | 58 (37, 77) | 100 (90, 100) | 23 (‐1, 47) | ‐3 (‐8, 3) |
| Swen 1999 | 13 | 8 | 77 (46, 95) | 88 (47, 100) | 92 (64, 100) | 88 (47, 100) | ‐15 (‐42, 12) | 0 (‐32, 32) |
| Teefey 2004 | 46 | 25 | 100 (92, 100) | 68 (46, 85) | 98 (88, 100) | 80 (59, 93) | 2 (‐2, 6) | ‐12 (‐36, 12) |
| Partial thickness tears | ||||||||
| Iannotti 2005 | 37 | 62 | 73 (56, 86) | 90 (80, 96) | 70 (53, 84) | 89 (78, 95) | 3 (‐18, 23) | 2 (‐9, 12) |
| Martin‐Hervas 2001 | 8 | 53 | 50 (16, 84) | 75 (62, 86) | 13 (0, 53) | 68 (54, 80) | 38 (‐4, 79) | 8 (‐10, 25) |
| Teefey 2004 | 19 | 52 | 63 (38, 84) | 98 (90, 100) | 68 (43, 87) | 96 (87, 100) | ‐5 (‐35, 25) | 2 (‐4, 8) |
3. Comparison of MRA and US for detection of rotator cuff tears (any, partial or full thickness) limited to studies in which all patients received both MRI and US (direct comparison).
| Study | Cases | Non‐cases | MRA | US1 | Difference in sensitivity (95% CI) | Difference in specificity (95% CI) | ||
| Sensitivity (95% CI) | Specificity (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | |||||
| Any rotator cuff tears | ||||||||
| Kang 2009 | 45 | 5 | 100 (92, 100) | 80 (28, 99) | 96 (85, 99) | 100 (48, 100) | 4 (‐2, 10) | ‐20 (‐55, 15) |
| Sipola 20102 | 64 | 11 | 97 (89, 100) | 82 (48, 98) | 92 (83, 97) | 45 (17, 77) | 4 (‐3, 12) | 36 (‐0.9, 74) |
| Full thickness tears | ||||||||
| Kang 2009 | 40 | 10 | 97 (87, 100) | 90 (55, 100) | 88 (73, 96) | 90 (55, 100) | 10 (‐1, 21) | 0 (‐26, 26) |
| Sipola 20103 | 57 | 18 | 88 (76, 95) | 94 (73, 100) | 83 (71, 91) | 53 (29, 76) | 5 (‐8, 18) | 42 (17, 67) |
| Partial thickness tears | ||||||||
| Kang 2009 | 5 | 45 | 80 (28, 99) | 96 (85, 99) | 40 (5, 85) | 89 (76, 96) | 40 (‐15, 95) | 7 (‐4, 18) |
| Sipola 20104 | 7 | 68 | 71 (29, 96) | 88 (78, 95) | 13 (0, 53) | 87 (77, 94) | 59 (18, 99) | 1 (‐10, 12) |
1 For the three target conditions, there were 2 additional shoulders for US
2 66 cases for detection of any rotator cuff tears using US
3 8 cases and 69 non‐cases for detection of full thickness tears using US
4 58 cases and 19 non‐cases for detection of partial thickness tears using US
Detection of full thickness rotator cuff tears
The estimates of sensitivity and specificity for the 14 studies that evaluated either MRI, US or MRA for the detection of full thickness rotator cuff tears are shown in Figure 7.
7.
Accuracy of MRA, MRI and US for detecting full thickness rotator cuff tears (forest plot)
Seven studies, based on 368 shoulders from 367 patients, assessed the diagnostic accuracy of MRI. The median study size was 48 (range 21 to 99), and the median prevalence of full thickness rotator cuff tear was 62% (range 37% to 69%). The sensitivities ranged from 77% to 100%, and specificities ranged from 68% to 100%. The summary sensitivity and specificity of MRI were 94% (95% CI 85% to 98%) and 93% (95% CI 83% to 97%) respectively. The positive and negative likelihood ratios were 13 (95% CI 6 to 29) and 0.06 (95% CI 0.02 to 0.16) respectively.
Ten studies (729 shoulders from 723 patients) assessed the accuracy of US to detect full thickness tears. The median study size was 66 (range 21 to 190), and the median prevalence was 48% (range 29% to 80%). Sensitivities ranged from 58% to 100%. Specificities ranged from 53% to 100%. The summary sensitivity and specificity of US were 92% (95% CI 82% to 96%) and 93% (95% CI 81% to 97%) respectively. The positive and negative likelihood ratios were 12 (95% CI 5 to 34) and 0.09 (95% CI 0.04 to 0.20) respectively.
Three studies (the same studies that assessed any rotator cuff tears) assessed the accuracy of MRA to detect full thickness tears with sensitivities ranging from 88% to 100% and specificities ranging from 90% to 94%. The median prevalence was 76% (range 17% to 80%). The summary sensitivity and specificity of MRA were 94% (95% CI 80% to 98%) and 92% (95% CI 83% to 97%) respectively. The positive and negative likelihood ratios were 12 (95% CI 5 to 30) and 0.06 (95% CI 0.02 to 0.23) respectively.
Comparison of MRI, MRA and US for detection of full thickness rotator cuff tears
Based on the 14 studies that assessed the accuracy of MRI, MRA or US for detection of full thickness rotator cuff tears, the summary sensitivities and specificities of MRI, MRA and US were found to be very similar (Figure 8; Table 2). There was no statistically significant difference in sensitivity or specificity (P = 0.7). Four studies (252 shoulders from 251 patients) directly compared MRI and US (Table 3, see Appendix 3 for additional figure) within the same patients, with no consistency among the studies as to which test was superior in terms of either sensitivity or specificity. Two studies (127 shoulders from 127 patients) directly compared MRA and US (Table 4). Both studies reported higher sensitivity for MRA compared to US. One of the two studies also reported a higher specificity while the other study reported no difference.
8.
Study estimates of sensitivity and specificity, and summary points with 95% confidence regions plotted in ROC space for MRA, MRI and US for the detection of full thickness rotator cuff tears
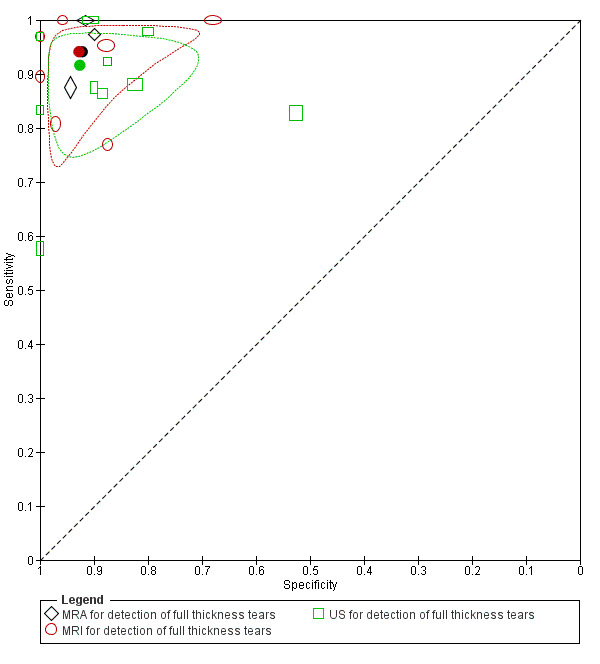
Detection of partial thickness rotator cuff tears
Figure 9 shows the estimates of sensitivity and specificity for the 13 studies that evaluated either MRI, MRA or US for the detection of partial rotator cuff tears.
9.
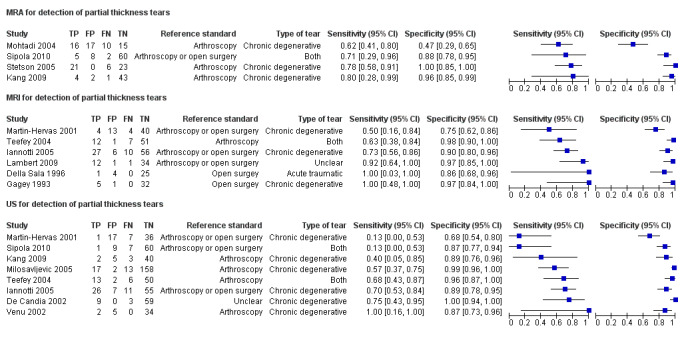
Accuracy of MRI, US and MRA for detecting partial thickness rotator cuff tears (forest plot)
All six studies (347 shoulders from 346 participants) that assessed the accuracy of MRI for the detection of any rotator cuff tears also assessed partial thickness tears. The median prevalence of partial thickness tears was 20% (range 3% to 37%). Sensitivities ranged from 50% to 100% and specificities ranged from 75% to 98%. The summary sensitivity and specificity of MRI were 74% (95% CI 59% to 85%) and 93% (95% CI 84% to 97%) respectively. The positive and negative likelihood ratios were 10 (95% CI 4 to 26) and 0.28 (95% CI 0.17 to 0.48) respectively.
Eight studies (660 shoulders from 654 participants) assessed the accuracy of US to detect partial thickness tears with sensitivities ranging from 13% to 100% and specificities ranging from 68% to 100%. The median prevalence was 14% (range 5% to 37%). The summary sensitivity and specificity of US were 52% (95% CI 33% to 70%) and 93% (95% CI 85% to 97%) respectively. The positive and negative likelihood ratios were 8 (95% CI 3 to 19) and 0.52 (95% CI 0.33 to 0.80) respectively.
Four studies, based on 233 shoulders from 233 participants, assessed the accuracy of MRA to detect partial thickness tears with sensitivities ranging from 62% to 80% and specificities ranging from 47% to 100%. The median prevalence was 27% (range 9% to 54%). Meta‐analysis was not performed but study specific estimates of sensitivity and specificity were plotted in ROC space with 95% CI in Figure 10.
10.
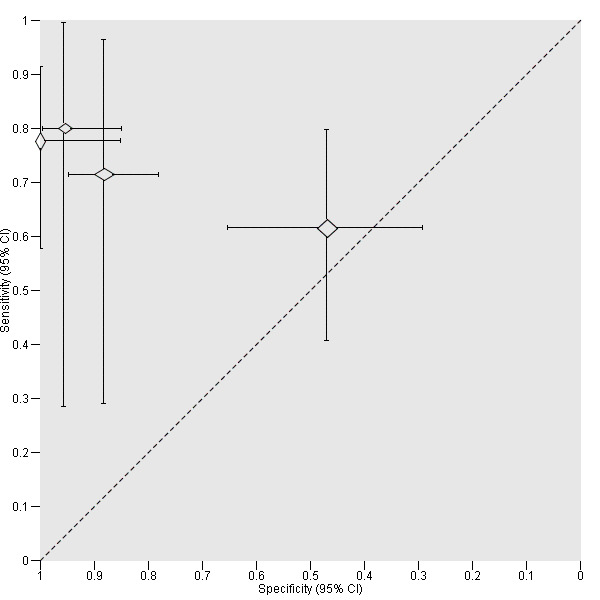
Study estimates of sensitivity and specificity with 95% confidence intervals plotted in ROC space for MRA for the detection of partial thickness rotator cuff tears
Comparison of MRI and US for detection of partial thickness rotator cuff tears
The diagnostic accuracy of MRI and/or US for detecting partial thickness tears was assessed in 11 studies. There was no statistically significant difference in sensitivity or specificity (P = 1.0) (seeTable 2). The individual study estimates of sensitivity and specificity, with summary points and 95% confidence regions, for each test are shown in ROC space (Figure 11). The sensitivities for MRI and US were generally lower for detecting partial thickness tears than for detecting any or full thickness rotator cuff tears. The sensitivity of US for detecting partial thickness tears was only 52% (95% CI 33% to 70%).
11.
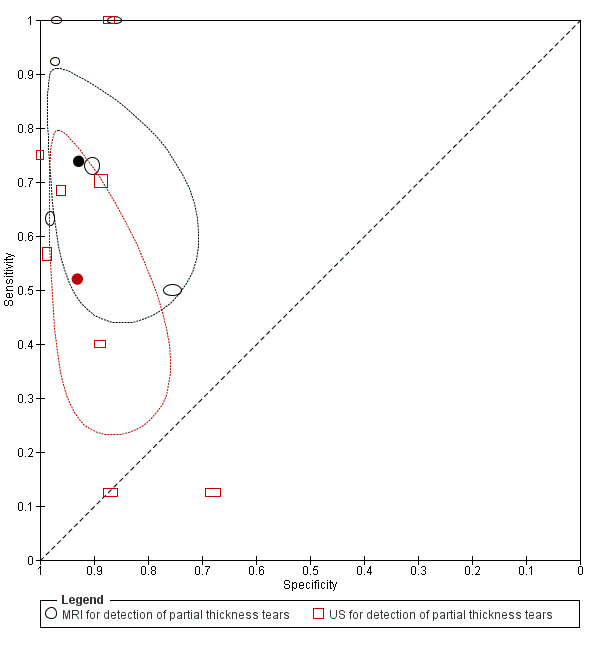
Study estimates of sensitivity and specificity, and summary points with 95% confidence regions plotted in ROC space for MRI and US for the detection of partial thickness rotator cuff tears
The sensitivities and specificities of the three studies that directly compared MRI and US are shown in a ROC space (see Appendix 3 for figure) and differences between the sensitivities and specificities of the tests are presented for each study in Table 3. Two of the studies reported better sensitivity for MRI than US while all three studies reported better specificity for MRI compared to US. Two studies directly compared MRA and US for detection of any rotator cuff tears. Both studies reported better sensitivity and specificity for MRI compared with those of US (Table 4). The same studies also assessed partial thickness tears.
Detection of any subscapularis tendon tears
One study, Mohtadi 2004, assessed the accuracy of MRA for detection of any subscapularis tendon tears, and included 58 shoulders from 58 participants. The study had a prevalence of 33% for subscapularis tendon tears. The sensitivity and specificity of MRA were 79% (95% CI 54% to 94%) and 72% (95% CI 55% to 85%) respectively.
Investigation of heterogeneity
The type of tear and the reference standard used in each study are shown by forest plots for each target condition in Figure 4, Figure 7 and Figure 9. The studies on each plot were ordered according to sensitivity and specificity to demonstrate any pattern in the observed estimates of test accuracy. Based on these descriptive analyses and the magnitude of the variances of the random‐effects parameters, we observed greater variability in sensitivity and specificity across studies of US than across studies of MRI or MRA. We were unable to formally investigate potential sources of heterogeneity because the number of studies available for each test was either inadequate or the same value of a covariate was reported by most studies.
Sensitivity analyses
There were few studies of MRI and MRA, and so we could not perform sensitivity analyses for these tests. We performed sensitivity analyses for US for each of the target conditions. We were only able to investigate the impact of two (acceptable reference standard and index test results blinded) of the five quality items we had specified because few studies scored 'Yes' on the other three items (representative spectrum, acceptable delay between tests, and reference test results blinded). There were small differences in sensitivity and/or specificity (Appendix 4). The largest difference was observed between the summary sensitivity of US for detecting partial thickness tears based of all studies (52%, 95% CI 33% to 70%) and the summary sensitivity (62%, 45% to 77%) based on only studies where the reference standard was acceptable. However, the confidence intervals were comparable and the specificities were similar. The exclusion of studies that did not meet either criteria made no difference to our findings. Two studies included both shoulders for six participants and one study did not report the number of participants so it is unclear whether more than one shoulder was included per participant. We investigated the impact of the unit of analysis on the findings for MRI and US by excluding the three studies, thus assuming the individual as the unit of analysis; the results were found to be consistent with the main analyses based on shoulders.
Discussion
Summary of main results
This review summarised the evidence for the diagnostic accuracy of MRI, MRA and US for detecting rotator cuff tears in people with shoulder pain who were suspected of having a rotator cuff tear and for whom surgery was being considered. These imaging tests are usually carried out to determine the characteristics of the rotator cuff tear in order to plan surgery. We included only prospective accuracy studies that evaluated at least one of the tests. We identified 20 studies (1147 shoulders, 1141 participants), of which six evaluated the accuracy of two of the tests within the same participants (paired comparison).
We found no evidence to suggest differences in the sensitivities and specificities of MRI and US for detecting any rotator cuff tears or partial thickness tears. Similarly, we found no evidence to suggest differences in the sensitivities and specificities of MRI, MRA and US for detecting full thickness tears. The estimates were very similar and the tests demonstrated good discriminatory ability for detecting full thickness tears, with sensitivities and specificities of 92% and above. MRI and US had lower sensitivity for partial thickness tears than for any rotator cuff tears or full thickness tears, with US having a sensitivity of only 52% (95% CI 33% to 70%); this indicates that US may be only marginally better than chance in excluding a partial thickness tear. The specificities of the three tests were generally good except for detection of any rotator cuff tears. The estimates of sensitivity and specificity for any rotator cuff tears suggest that in a population of 100 people with shoulder pain suspected of having a rotator cuff tear and for whom surgery is being considered, if the prevalence was 80%, investigation with MRI may miss two cases (2/80, 3%), while investigation with US may miss seven cases (7/80, 9%). Among patients without a rotator cuff tear (20 out of 100), four patients tested using MRI may have a rotator cuff tear wrongly detected (4/20, 20%) and may undergo unnecessary surgery. A similar number (3/20, 15%) may be over‐treated if US is used. The summary of all results are provided in Table 1.
It is important to emphasise that our review specifically addressed imaging of the rotator cuff by MRI, MRA or US in people with shoulder pain suspected of having a rotator cuff tear and for whom surgery is being considered, and therefore our results are not generalisable to people who present with shoulder pain in primary care where the prevalence of rotator cuff tears may be lower but importantly the prevalence of asymptomatic tears or people with shoulder pain not contemplating surgery could be much higher. Asymptomatic changes in the rotator cuff are common and increase with age and many observed abnormalities might not require specific treatment (Awerbuch 2008). Despite studies continuing to show that primary care practitioners display an over‐reliance upon early imaging for shoulder pain (Buchbinder 2013; Johal 2008; Patel 2011), at the present time, guidelines for the management of shoulder pain in primary care do not advocate imaging for shoulder pain unless there is a suggestion of serious pathology (Bussières 2007; Geraets 2009).
The unit of analysis used in evaluating the diagnostic accuracy of a test is likely to have an impact on the estimates of sensitivity and specificity of the test. Our unit of analysis was the shoulder. However, only six out of 1080 participants had both shoulders included in 19 of the 20 included studies; it was unclear in one study (Martin‐Hervas 2001) whether the number of shoulders was the same as the number of participants. With the exception of Iannotti 2005 and Milosavljevic 2005, the studies reported the same number of participants and shoulders. Both Iannotti 2005 and Martin‐Hervas 2001 compared the accuracy of MRI and US while Milosavljevic 2005 evaluated only US. In sensitivity analyses, we examined the impact of the unit of analysis by excluding the two studies that included both shoulders for any participant and the one study where it was unclear if the number of shoulders was the same as the number of participants. Overall, findings from the sensitivity analyses were consistent with findings from the main analyses.
Strengths and weaknesses of the review
This review was planned and conducted following criteria and methods set out in a published protocol (Lenza 2011). Our results were based on a comprehensive and sensitive literature search that aimed to identify all published studies. We used wide search terms and several electronic databases, not limited by language, and we excluded search filters for diagnostic terms, as they have limited utility (De Vet 2008). Other strengths of this review are our quality assessment of studies and our synthesis of studies with similar methodological features into a meta‐analytic summary based on recommended methods. To increase the applicability and reliability of the summary findings, we included only prospective studies that investigated people with shoulder pain due to a suspected rotator cuff tear and for whom surgery was being considered. We excluded retrospective studies because of their potential for high risk of spectrum and verification bias (Bossuyt 2003; Van der Schouw 1995).
Our review has some limitations. Our findings were based on small studies with poor reporting of participant characteristics and study design. Most of the QUADAS items were scored as unclear for many studies. For example, only 25% of the included studies reported the time interval between the index tests and the reference standard. For some analyses, we observed considerable heterogeneity in sensitivity and/or specificity, which may be due to several factors including variation in the criteria for a positive diagnostic test for both the index tests and the reference standard, technical details of the tests, variation in population, and variation in operator or reader experience. The three diagnostic tests are known to be operator and reader dependent which may account for some of the observed variation between studies, especially for studies of US which were found to be very heterogeneous. We could not formally investigate potential sources of heterogeneity due to the number of studies available for each test or because most studies reported the same covariate value. Our comparative meta‐analyses were based mainly on non‐comparative studies because only a small number of studies made direct comparisons between the tests. Consequently, it is possible that observed differences between tests may be confounded by differences in participant and study design characteristics. It is unclear to what extent these limitations influenced our findings.
An important weakness of this review is that due to resource limitations, 25 potentially eligible studies published in non‐English languages are still awaiting translation. Good quality translation will be required to reliably extract data from these papers due to the complexity of diagnostic accuracy studies.The studies contain more than 2900 participants that could potentially provide data for analyses and they will be considered for inclusion in a future update of the review.
Comparison with existing reviews
We identified six previous systematic reviews of imaging tests to detect rotator cuff tears (De Jesus 2009; Dinnes 2003; Kelly 2009; Ottenheijm 2010; Shahabpour 2008; Smith 2012). Our review limited inclusion to prospective studies whereas the other systematic reviews allowed the inclusion of retrospective studies. Our literature search failed to identify a study (Ruiz Santiago 2000) which was included in the review by Smith 2012. However, this study would not have been eligible for inclusion in our review because arthrography or arthrographic computed tomography was also used as an index test.
Previous reviews reported similar results. De Jesus 2009 compared US with MRI for detecting rotator cuff tears using surgery as the reference standard. De Jesus 2009 included 65 studies and concluded that US was as accurate as MRI for diagnosing both full and partial thickness rotator cuff tears. Dinnes 2003 assessed the diagnostic accuracy of clinical testing, US and MRI for detecting rotator cuff tears using surgical and non‐surgical tests as the reference standard (results also reported in Kelly 2009). Dinnes 2003 concluded that US and MRI were equivalent for detecting full thickness rotator cuff tears, and that MRI may be better at detecting partial thickness tears than US. Shahabpour 2008 also concluded that US and MRI were equivalent for detecting full thickness rotator cuff tears. However, in contrast Shahabpour 2008 concluded that MRA and US may be more accurate at detecting partial thickness tears than MRI. We did not pool MRA studies for detection of partial thickness tears. While our results suggested that MRI may be more sensitive than US, the difference was not statistically significant.
Ottenheijm 2010 assessed the accuracy of US for detecting subacromial diseases in patients presenting in primary and secondary care settings (search date 2001 to June 2010). This systematic review included 23 studies and reported pooled sensitivity and specificity values that were comparable with our results for detecting full thickness tears. Ottenheijm 2010 reported a sensitivity of 95% for detecting full thickness tears compared to 92% (95% CI 82% to 96%) in our systematic review and a specificity of 93% compared with 93% (95% CI 81% to 97%) in our systematic review. However, for detection of partial thickness tears, Ottenheijm 2010 reported a much higher pooled sensitivity of 72% compared with our finding of 52% (95% CI: 33% to 70%). Smith 2012, which included both retrospective and prospective studies, assessed the diagnostic accuracy of MRI and identified 44 studies published up to May 2011. This systematic review reported pooled sensitivity and specificity values that were similar to our results for detecting full thickness tears and partial thickness tears. Smith 2012 reported a pooled sensitivity of 91% (95% CI 86% to 94%) for detecting full thickness tears which was comparable to our result of 94% (95% CI 85% to 98%). Smith 2012 reported a pooled specificity of 97% (95% CI: 96% to 98%) for detecting full thickness tears which is similar to our specificity of 93% (95% CI 83% to 97%). Smith 2012 reported a pooled sensitivity of 80% (95% CI 79% to 84%) for detecting partial thickness tears which is comparable to our sensitivity of 74% (95% CI 59% to 85%); and a pooled specificity of 95% (95% CI 94% to 97%) which is similar to our specificity of 93% (95% CI 84% to 97%). Overall, the results are generally consistent across the different reviews even though there were differences in inclusion criteria and review methods. Despite our study being the most up‐to‐date published systematic review, we included a much smaller number of studies (20 studies) than some of the previous reviews because we restricted our analyses to only prospective studies thus reducing the risk of spectrum and verification bias.
Applicability of findings to the review question
The applicability of our findings is limited because only 30% of the included studies reported an adequately representative spectrum of consecutive patients from secondary or tertiary care. Furthermore, partial verification was avoided in only 50% of the studies. MRI, MRA and US may have similar accuracy for detecting full thickness rotator cuff tears. The sensitivity of both MRI and US for partial thickness rotator cuff tears appeared to be much lower than their sensitivity for any rotator cuff tears or for full thickness tears. While the difference in sensitivity between MRI and US for detecting partial thickness tears was not statistically significant, US showed a much lower sensitivity (52%) than MRI (74%). A sensitivity of 52% suggests that US may not be any better than chance for detecting partial thickness rotator cuff tears. The specificities of the three tests were generally high except for the detection of any rotator cuff tears.
In many countries, US is less time consuming and less expensive and more readily available in secondary and tertiary care than MRI or MRA. Despite MRI and MRA being comparable for detection of full thickness rotator cuff tears, the choice of test may depend upon cost and availability. As the scope of this review was to limited to test accuracy, we were not able to determine if applying any imaging test prior to surgery results in different surgical interventions or benefits in terms of pain relief and shoulder function following surgery.
Authors' conclusions
Implications for practice.
The diagnostic performance of MRI and US depends on the extent (i.e. partial or full thickness) of rotator cuff tears. Our findings suggest that MRI, US and MRA have good diagnostic accuracy and any of these tests could equally be used for detection of full thickness tears in people with shoulder pain for whom surgery is being considered. MRI and US also have good sensitivity for detecting any rotator cuff tears but poor sensitivity for detection of partial thickness tears. The validity and generalisability of our findings are limited because they were based on small, heterogeneous, non‐comparative studies with methodological flaws.
Implications for research.
There is a lack of good quality prospective cohort studies that directly compare the accuracy of MRI, MRA and US shoulder imaging tests for people in secondary and tertiary care, with suspected rotator cuff tears, for whom surgery is being considered. Consequently, further studies are needed in order to evaluate the comparative accuracy of these imaging tests in such circumstances. Future studies should use a blinded design and should limit the amount of time between the index and reference tests as much as possible because there is evidence that rotator cuff tears can progress over time. We suggest that arthroscopy be used as the reference standard test because it is accurate for assessing the articular and bursal side of the rotator cuff. The results of the index test(s) and reference standard should be interpreted by experienced operators.
What's new
| Date | Event | Description |
|---|---|---|
| 3 September 2014 | Amended | Republished (September 2014) to include a Plain Language Summary. |
Acknowledgements
We thank Dr Helen Handoll and Mr Jonathan Rees; and the peer reviewers and contact editors of the Cochrane Diagnostic Test Accuracy Working Group (Dr Rob Scholten, Prof Danielle van der Windt) for helpful feedback at editorial review. We would also like to thank Mrs Lindsey Elstub and Dr Joanne Elliott for their assistance in preparing the review.
We also thank Dr Danielle van der Windt for her useful feedback on the inclusion/exclusion criteria and Robin Christensen for his contribution to the protocol.
Appendices
Appendix 1. Search strategies
MEDLINE (PubMed)
((Ultrasonography [mh] OR ultrasound [tw] OR ultrasonograph* [tw] OR sonograp*[tw] OR us [sh]) OR (Magnetic Resonance Imaging [mh] OR MR imag*[tw] OR magnetic resonance imag* [tw] OR MRI [tw])) AND (Rotator Cuff [mh] OR rotator cuff* [tw] OR musculotendinous cuff* [tw] OR subscapularis [tw] OR supraspinatus [tw] OR infraspinatus OR teres minor [tw]) AND (Rupture [mh:noexp] OR tear* [tw] OR torn [tw] OR thickness [tw] OR lesion* [tw] OR ruptur* [tw] OR injur* [tw])
Total references = 1551
EMBASE (Elsevier)
1 'echography'/de AND [embase]/lim (124208) 2 ultrasound:ab,ti OR ultrasonograph*:ab,ti OR sonograp*:ab,ti AND [embase]/lim (192495) 3 #1 OR #2 (242499) 4 'nuclear magnetic resonance imaging'/de AND [embase]/lim (277184) 5 (('magnetic resonance' OR mr) NEAR/3 imag*):ab,ti AND [embase]/lim (130882) 6 mri:ab,ti AND [embase]/lim (108797) 7 #4 OR #5 OR #6 (311974) 8 'rotator cuff injury'/de OR 'rotator cuff rupture'/de AND [embase]/lim (3561) 9 'rotator cuff'/de AND [embase]/lim (1850) 10 'rotator cuff':ab,ti OR 'musculotendinous cuff':ab,ti OR subscapularis:ab,ti OR supraspinatus:ab,ti OR infraspinatus:ab,ti OR 'teres minor':ab,ti AND [embase]/lim (5679) 11 #9 OR #10 (6120) 12 'rupture'/de AND [embase]/lim (3798) 13 tear*:ab,ti OR torn:ab,ti OR thickness:ab,ti OR lesion*:ab,ti OR ruptur*:ab,ti OR injur*:ab,ti AND [embase]/lim (1001852) 14 #12 OR #13 (1002130) 15 #11 AND #14 (3615) 16 #8 OR #15 (4908) 17 #3 OR #7 (526691) 18 #16 AND #17 (1572)
LILACS (Bireme)
(Mh Ultrasonography OR Tw ultrasound OR Tw ultrasonograph$ OR Tw Sonograp$) OR (Mh Magnetic Resonance Imaging OR (Tw magnetic AND Tw resonance AND Tw imag$) OR Tw MRI) [Words] and Mh Rotator Cuff OR (Tw rotator AND Tw cuff) OR (Tw musculotendinous AND Tw cuff) OR Tw subscapularis OR Tw supraspinatus OR Tw infraspinatus OR (Tw teres AND Tw minor) [Words] and Mh Rupture OR Tw tear$ OR Tw torn OR Tw thickness OR Tw lesion$ OR Tw rupture$ OR Tw injur$ [Words]
Total references = 30
Appendix 2. Assessment of methodological quality: QUADAS and additional items
| Item definition | Item question | Assessment |
| Representative spectrum | 1. Was the spectrum of patients representative of the patients who will receive the test in practice? |
Yes: (a) the setting was secondary or tertiary care AND (b) the population was patients with shoulder pain suspected of a rotator cuff tear for whom surgery is being considered AND (c) the study was prospective AND (d) recruitment was consecutive Unclear: if insufficient information was given on the setting, selection criteria, or selection procedure to make a judgment No: (a) the setting was primary care OR (b) the population was unselected but defined by shoulder pain OR (c) the study was not prospective OR (d) recruitment was not consecutive |
| Acceptable reference standard | 2. Is the reference standard likely to classify the target condition correctly? |
Yes: if the reference standard was arthroscopy or a combination of arthroscopy and open surgery (including mini‐open) Unclear: if the target condition was partial thickness rotator cuff tears and the reference standard was open surgery (including mini‐open) No: not applicable |
| Acceptable delay between tests | 3. Is the time period between reference standard and index test short enough to be reasonably sure that the target condition did not change between the two tests? |
Yes: if the average interval between reference standard and index test was one month or less Unclear: if the interval between tests was not clearly reported No: if the average interval between reference standard and index test was longer than one month |
| Partial verification avoided | 4. Did the whole sample or a random selection of the sample, receive verification using the intended reference standard? |
Yes: If all patients who received the index test went on to receive verification of their disease status using a reference standard (Score 'Yes' even if different reference tests were used) Unclear: if insufficient information was given on relation of index test and reference standard No: if not all the patients who received the index test underwent a reference standard to verify their true disease status |
| Differential verification bias | 5. Did patients receive the same reference standard irrespective of the index test result? |
Yes: if all patients received the same reference standard, regardless of the result of their index test Unclear: If it is unclear whether different reference standards were used No: if the result of the index test influenced the choice of the reference standard |
| Incorporation bias | 6. Was the reference standard independent of the index test (i.e. the index test did not form part of the reference standard)? | Should be considered 'Yes' for all studies because the index test is not part of the reference standard |
| Index test results blinded | 7. Were the index test results interpreted without knowledge of the results of the reference standard? |
Yes: if the person undertaking the index test was blinded to the results of the standard reference Unclear: if insufficient information was given on independent or blind assessment of the index test No: if the results of the reference tests were known to the person undertaking the index tests |
| Reference standard results blinded | 8. Were the reference standard results interpreted without knowledge of the results of the index test? |
Yes: if the reference standard results were performed blind to the results of the index test Unclear: if insufficient information was given on independent or blind assessment of the reference standard No: if the results of the index tests were known to the person interpreting the reference tests |
| Relevant clinical information | 9. Were the same clinical data available when test results were interpreted as would be available when the test is used in practice? |
Yes: if clinical data would normally be available when the test is interpreted in practice and similar data were available when interpreting the index test in the study Unclear: if insufficient information was given to explain which clinical information was available at the time of assessment No: if clinical data were not available when index test(s) was(were) interpreted |
| Uninterpretable results reported | 10. Were uninterpretable/ intermediate test results reported? |
Yes: If the number of uninterpretable test results is stated, or if the number of results reported agrees with the number of patients recruited (indicating no uninterpretable test results) Unclear: if insufficient information was given to permit judgement No: If it states that uninterpretable test results occurred or were excluded and does not report how many |
| Withdrawals explained | 11. Were withdrawals from the study explained? |
Yes: if the number and reasons of all withdrawals from the study were explained (ideally by a flow chart) or if no participants were excluded from the analysis Unclear: if insufficient information was given on the withdrawals No: if not all withdrawals were explained |
| Learning curve / training reported of index test | 12. Had index test operators had appropriate training or experience in musculoskeletal diseases? |
Yes: (a) if the index test(s) executors were radiologists or shoulder surgeons AND (b) if the tests interpreters had experience in diagnostic of musculoskeletal diseases Unclear: if insufficient information was given to permit judgement No: (a) if the index test(s) executors were not radiologists or shoulder surgeons OR (b) if the tests interpreters had no experience in diagnostic of musculoskeletal diseases |
| Learning curve / training reported of reference standard | 13. Had reference standard test operators had appropriate training or experience in shoulder surgery? |
Yes: (a) if the reference standard(s) executors were shoulder surgeons AND (b) if the results interpreters had experience in shoulder diseases Unclear: if insufficient information was given to permit judgement No: (a) if the reference standard(s) executors were not shoulder surgeons OR (b) if the results interpreters had no experience in shoulder diseases |
| Index test / criteria for a positive result | 14. Index test criteria for a positive result reported?? |
Yes: (a) if the study provides a clear definition of a positive test result Unclear: if insufficient information was given to permit judgement No: if no definition is given of a positive test result |
Appendix 3. Additional figures
Summary ROC plot of within study comparisons of MRI and US for detection of any rotator cuff tears (Figure 22)
12.
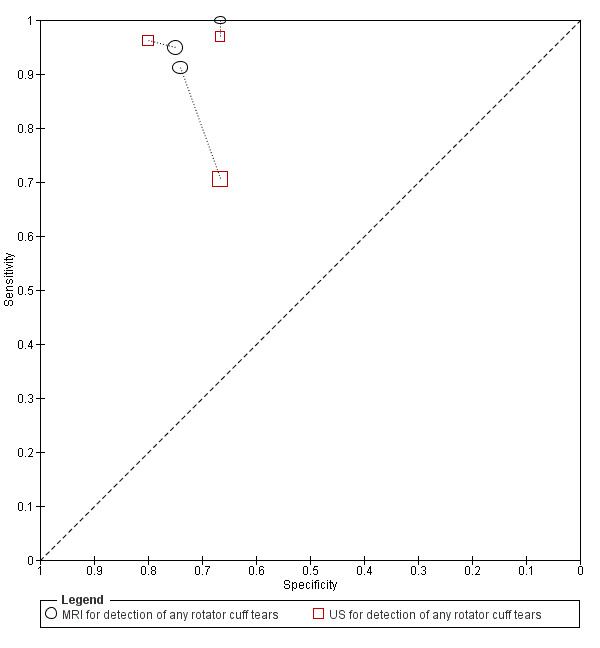
Paired comparison of MRI and US for detection of any rotator cuff tears. Connectling lines link study estimates of sensitivity and specificity for both tests in each study
Summary ROC plot of within study comparisons of MRI and US for detection of full thickness rotator cuff tears (Figure 23)
13.
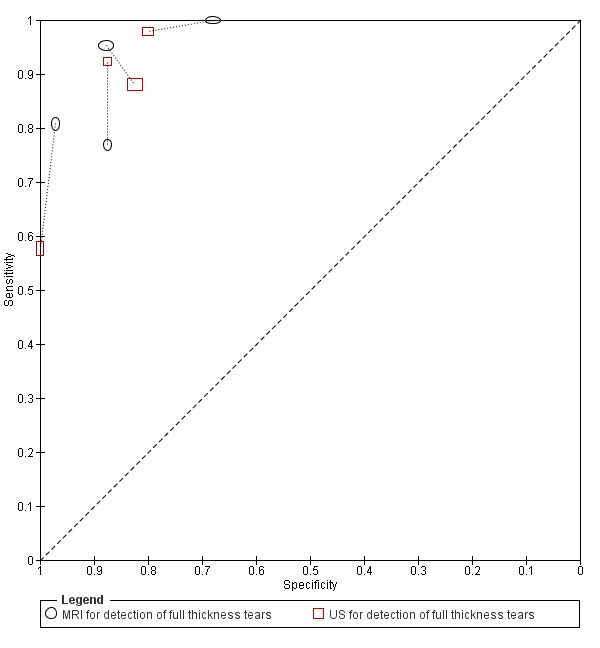
Paired comparison of MRI and US for detection of full thickness rotator cuff tears. Connectling lines link study estimates of sensitivity and specificity for both tests in each study
Summary ROC plot of within study comparisons of MRI and US for detection of partial thickness rotator cuff tears (Figure 24)
14.
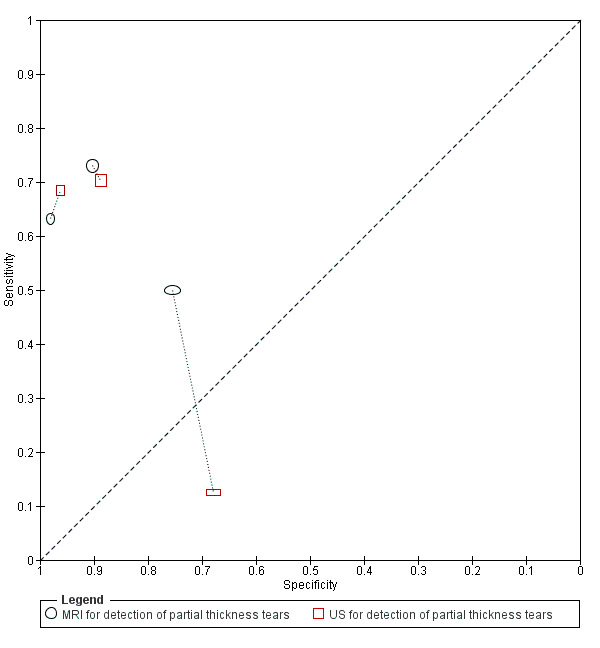
Paired comparison of MRI and US for detection of partial thickness rotator cuff tears. Connectling lines link study estimates of sensitivity and specificity for both tests in each study
Appendix 4. Sensitivity analyses for US studies for detection of rotator cuff tears (any, partial or full thickness)
| Studies | Shoulders | Cases | Summary sensitivity (95% CI) | Summary specificity (95% CI) | LR+ | LR– | |
| Any rotator cuff tears | |||||||
| All studies | 13 | 854 | 626 | 91 (83, 95) | 85 (74, 92) | 6 (3, 12) | 0.11 (0.05, 0.22) |
| Acceptable reference standard | 5 | 400 | 291 | 94 (88, 97) | 91 (82, 95) | 10 (5, 22) | 0.06 (0.03, 0.14) |
| Index test results blinded | 9 | 468 | 348 | 91 (78, 97) | 81 (70, 88) | 5 (2, 10) | 0.11 (0.04, 0.31) |
| Full thickness tears | |||||||
| All studies | 10 | 729 | 386 | 92 (82, 96) | 93 (81, 97) | 12 (5, 34) | 0.09 (0.04, 0.20) |
| Acceptable reference standard | 6 | 421 | 227 | 95 (86, 98) | 91 (85, 95) | 11 (6, 20) | 0.06 (0.02, 0.16) |
| Index test results blinded | 7 | 391 | 201 | 87 (76, 93) | 92 (81, 97) | 11 (5, 26) | 0.14 (0.08, 0.26) |
| Partial tears | |||||||
| All studies | 8 | 660 | 121 | 52 (33, 70) | 93 (85, 97) | 8 (3, 19) | 0.52 (0.33, 0.80) |
| Acceptable reference standard | 4 | 352 | 56 | 62 (45, 77) | 95 (87, 98) | 12 (5, 31) | 0.40 (0.26, 0.61) |
| Index test results blinded | 5 | 322 | 71 | 56 (32, 77) | 87 (78, 93) | 4 (2, 9) | 0.51 (0.28, 0.93) |
Footnotes
Sensitivity analyses performed by excluding studies that scored 'Unclear' or 'No' for each of the two QUADAS criteria listed in the table.
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
1. Test.
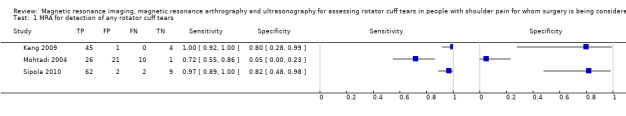
MRA for detection of any rotator cuff tears.
2. Test.
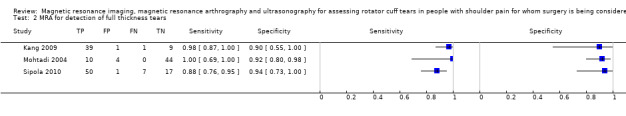
MRA for detection of full thickness tears.
3. Test.
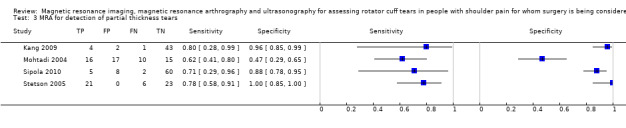
MRA for detection of partial thickness tears.
4. Test.
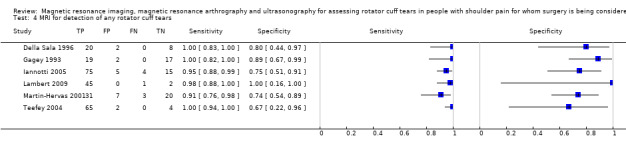
MRI for detection of any rotator cuff tears.
5. Test.
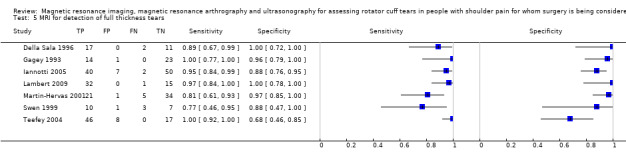
MRI for detection of full thickness tears.
6. Test.
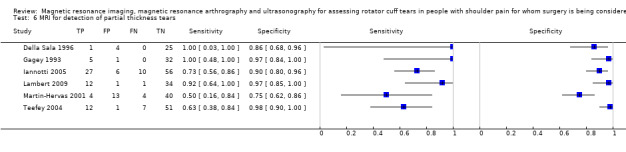
MRI for detection of partial thickness tears.
7. Test.
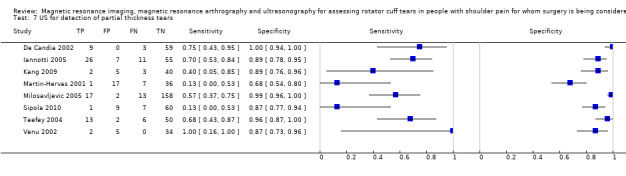
US for detection of partial thickness tears.
8. Test.
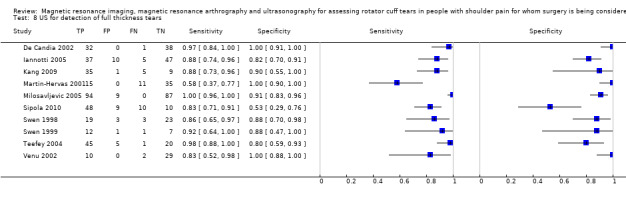
US for detection of full thickness tears.
9. Test.
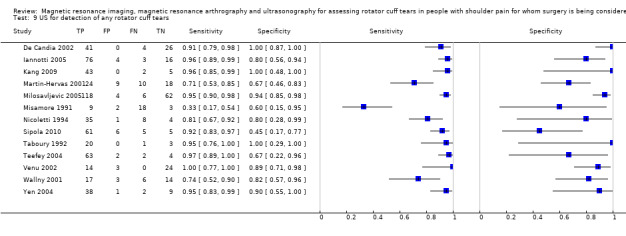
US for detection of any rotator cuff tears.
11. Test.
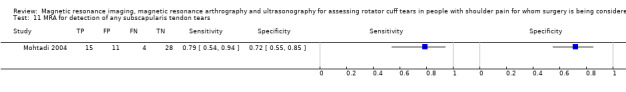
MRA for detection of any subscapularis tendon tears.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
De Candia 2002.
| Clinical features and settings |
Inclusion criteria: Participants with clinical suspicion of rotator cuff tear who underwent surgery Exclusion criteria: Not reported Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Not reported |
|
| Participants |
Place of study: Udine, Italy Period of study: January 2000 to December 2000 Number of participants eligible: 157 participants Number of participants enrolled IT and RS: ‐ US and surgery: 71 participants Data available for analyses: ‐ US and surgery: 71 participants Age (range): 34 to 80 years Male/Female: 31/40 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To determine the values of the US real time compound imaging in the evaluation of supraspinatus tendon in subacromial impingement disease Study design: Prospective, accuracy cohort study Unclear whether consecutive recruitment Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery, unclear whether arthroscopy or open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Scanner: 7 to 12 MHz linear‐array probe applying the soon CT digital algorithm Technique: Images were obtained in static and dynamic evaluations as described in (Martino 1998; Teefey 2000) Patient position: Static evaluation was performed on the patient’s arm in standard position; dynamic evaluation was performed first with the patient’s arm positioned from the internal rotation and extended position to abduction and internal rotation (forearm flexed and the back face of fingertips pointing to the scapula); the second part of the evaluation was performed by moving the patient's arm in adduction and keeping the internal rotation ‐ Criteria for a positive result: Not reported ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Index test was performed on the day before reference standard |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | Part of population of this study was also reported in De Candia 2003 Although De Candia 2003 is more updated than this study, there were no extra data available to be included in the analyses The rotator cuff tears were focused on only supraspinatus tendon tears A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Unclear whether consecutive recruitment |
| Acceptable reference standard? All tests | Unclear | The reference standard was surgery (unclear whether arthroscopy or open surgery) and the target conditions were presence of any rotator cuff tears, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | Yes | Index test was performed on the day before reference standard |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status Of the 157 eligible participants, only 71 (45.2%) underwent to reference standard |
| Differential verification avoided? All tests | No | The result of the index test probably influenced the choice of the reference standard |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Reference standard results blinded? All tests | No | The results of the index tests were probably known to the person interpreting the reference tests |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | No | The results of 86 (54.8%) patients were not reported |
| Withdrawals explained? All tests | No | Some of the eligible patients who entered the study did not complete it and these patients were not accounted for |
| Learning curve / training reported of index test? All tests | Unclear | The interpreters of index tests were two radiologists; however, the training/expertise was not described |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | No | Not reported |
Della Sala 1996.
| Clinical features and settings |
Inclusion criteria: Patients with recent trauma without documented articular bone defect radiologically, shoulder pain and disability persisting after appropriate conservative treatment, clinical examination suggestive of rotator cuff tears and/or impingement Exclusion criteria: Patients with suspected shoulder instability Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Tertiary or secondary |
|
| Participants |
Place of study: Trento, Italy Period of study: January 1993 to December 1994 Number of participants eligible: 80 participants Number of participants enrolled IT and RS: ‐ MRI and open surgery: 30 participants Data available for analyses: ‐ MRI and open surgery: 30 participants Age: mean 50.1 years (range 21 to 71 years) Male/Female: 23/7 Dominant arm: Not reported Nature of onset: Traumatic and chronic injury |
|
| Study design |
Primary objective: Not reported Study design: Unclear whether prospective design. Non‐consecutive recruitment Language: Italian |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Open surgery ‐ Description of technique: Open surgery: as described by Neer 1983 ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): MRI ‐ Description of technique: MRI unit: 1.0 T scanner Sequences and Planes: Spin‐echo T1‐weighted (TR/TE: 786/17) in coronal and sagittal oblique planes; and TR/TE 450/12 in axial plane Patient position: Not reported ‐ Criteria for a positive result: Full‐thickness tears: an increase signal on the T1‐weighted in the entire extension of the rotator cuff Partial thickness tears: an increased signal in not whole extension of the cuff ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | Raw data were given and it was possible to back‐calculate this from the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Insufficient information was given to permit judgement |
| Acceptable reference standard? All tests | Unclear | The reference standard was open surgery and the target conditions were presence of any rotator cuff tears, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status Of the 80 eligible participants, only 30 received the reference standard |
| Differential verification avoided? All tests | No | The result of the index test probably influenced the choice of the reference standard |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | No | The results of 50 (62.5%) patients were not reported |
| Withdrawals explained? All tests | No | Some of the eligible patients who entered the study did not complete it and these patients were not accounted for |
| Learning curve / training reported of index test? All tests | Unclear | Insufficient information was given to permit judgement |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | No | Not reported |
Gagey 1993.
| Clinical features and settings |
Inclusion criteria: Patients with a rotator cuff syndrome resistant to any medical treatment and indication for surgery Exclusion criteria: Not reported Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Tertiary |
|
| Participants |
Place of study: Paris, France Period of study: 15 months period Number of participants eligible: 38 participants Number of participants enrolled IT and RS: ‐ MRI and open surgery: 38 participants Data available for analyses: ‐ MRI and open surgery: 38 participants Age (mean): 47 years Male/Female: 14/24 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To compare the results of the MRI with the open surgery Study design: Prospective accuracy cohort study. Unclear whether consecutive recruitment Language: French |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Visual identification of the tears by the surgeon |
|
| Index and comparator tests |
Index test(s): MRI ‐ Description of technique: MRI unit: 1.5 T surface circular coil Sequences: Spin‐echo T2‐weighted (TR/TE: 2000/25 to 75; TR/TE 1500/25 to 75) and TR/TE 300 to 500/20. Planes: Sagittal and coronal Patient position: Not reported ‐ Criteria for a positive result: Increased signal on T2‐weighted images ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | Mr Jean‐Philippe Regnaux and Mr Ludovic Trinquart kindly translated into English and extracted the data of this study The same population of this study was also reported in Gagey 1991 No two‐by‐two table of the ITs and RS was given, but it was possible to back‐calculate this from the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Insufficient information was given to permit judgement |
| Acceptable reference standard? All tests | Unclear | The reference standard was open surgery and the target conditions were presence of any rotator cuff tears, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | All patients received the same reference standard, regardless of the result of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The number of results reported agrees with the number of patients recruited |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Unclear | Insufficient information was given to permit judgement |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Iannotti 2005.
| Clinical features and settings |
Inclusion criteria: Participants with a clinical diagnosis of rotator cuff symptoms, consisting of pain, decreased function, and/or weakness Exclusion criteria: Not reported Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Tertiary and secondary |
|
| Participants |
Place of study: Cleveland, Ohio, USA Period of study: Not reported Number of participants eligible: 98 participants (99 shoulders) Number of participants enrolled IT and RS: ‐ MRI and arthroscopy or open surgery: 98 participants (99 shoulders) ‐ US and arthroscopy or open surgery: 98 participants (99 shoulders) Data available for analyses: ‐ MRI and arthroscopy or open surgery: 98 participants (99 shoulders) ‐ US and arthroscopy or open surgery: 98 participants (99 shoulders) Age: Not reported Gender: Not reported Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To define the accuracy of US, when performed in an orthopaedic surgeon's office, for the diagnosis of rotator cuff tears Study design: Prospective, consecutive, accuracy cohort study with fully paired direct comparison between MRI and US Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy or open surgery ‐ Description of technique(s): Not reported ‐ Criteria for a positive result: Full thickness tears: a gap in the tendon; the involved tendons were measured with a calibrated probe or ruler, and the total tendon gap was measured in centimetres prior to débridement of the tendon edges Partial thickness tears: on either the bursal or the articular surface was identified as tendon‐fraying and loss of tendon substance The size of the partial thickness tears was measured after débridement of the frayed portions of the tendon |
|
| Index and comparator tests |
Index test(s): MRI and US ‐ Description of technique: MRI MRI unit: 1.5‐T magnet Sequences and Planes: T1 and T2‐weighted image sequences in the sagittal and coronal oblique and axial planes Patient position: Not reported US Scanner: 7.5 MHz transducer Technique: Static and dynamic examinations Images were obtained in transverse plane scans of the biceps tendon; longitudinal and parallel scans of the subscapularis tendon; perpendicular and parallel scans of the supraspinatus and infraspinatus tendons Patient position: Both the patient and the examiner seated on backless stools facing each other The patient positioned the arm at the side with the elbow bent to 90o ‐ Criteria for a positive result: MRI: Full thickness tears: a fluid filled the gap in the tendon on the T2‐weighted sagittal or coronal oblique images Partial thickness tears: an increase signal on the T1‐weighted images, with brighter signal on the T2‐weighted paired image The location of the tear was defined by the tendon(s) involved US: Full thickness tears: a gap in the tendon substance with retraction with increased echogenic signal from the exposed articular cartilage of the humeral head Partial thickness tears: an increase echogenic signal intensity or a focal decrease in the thickness of the tendon or both The location of the tear was defined by the tendon(s) involved ‐ Time from symptoms to index test: Not reported ‐ Time from US to MRI: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Tertiary or secondary care, participants with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive |
| Acceptable reference standard? All tests | Unclear | The reference standard was arthroscopy or open surgery and the target conditions were presence of full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | Unclear | The study did not report how many patients had US and did not proceed to surgery |
| Differential verification avoided? All tests | Unclear | Insufficient information was given to permit judgement |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The study was prospective and the results of the index tests were interpreted before the reference standard |
| Reference standard results blinded? All tests | No | The results of the index tests were known to the person interpreting the reference tests |
| Relevant clinical information? All tests | Yes | The authors had knowledge of history, physical findings and radiographs |
| Uninterpretable results reported? All tests | Unclear | Insufficient information was given to permit judgement |
| Withdrawals explained? All tests | Unclear | Insufficient information was given to permit judgement |
| Learning curve / training reported of index test? All tests | No | Performace of index tests was not by radiologist or surgeon and they had only two training sections |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Kang 2009.
| Clinical features and settings |
Inclusion criteria: Participants with clinical findings of impingement and suspected rotator cuff tear referred for MRA Exclusion criteria: Participants with previous rotator cuff repair, dislocation, previous humeral fracture, and infectious or inflammatory arthritis were excluded from the study Participants who showed clinical improvement while scheduled for surgery and refused it Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Not reported |
|
| Participants |
Place of study: Seoul, Korea Period of study: February 2007 to August 2008 Number of participants eligible: 128 participants Number of participants enrolled IT and RS: ‐ MRA and arthroscopy: 50 participants ‐ 3D‐US and arthroscopy: 50 participants Data available for analyses: ‐ MRA and arthroscopy: 50 participants ‐ 3D‐US and arthroscopy: 50 participants Age: mean 55.6 years (range 22 to 78 years) Male/Female: 32/18 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To compare the diagnostic performance of three‐dimensional (3D) US and MRA for both the detection of supraspinatus tendon tears and the quantification of their size, with arthroscopic findings used as the standard Study design: Prospective, consecutive, accuracy cohort study with fully paired direct comparison between MRA and 3D‐US Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy ‐ Description of technique: In a partial thickness tear or in which the initial arthroscopic findings differed from those reported on the imaging, the rotator cuff was examined from both the articular side and the bursal side Cuff tear size was measured with a calibrated probe using the posterior portal to measure the anterior–posterior dimension and the lateral portal to measure the medial–lateral dimension ‐ Criteria for a positive result: The presence or absence of a full or partial thickness tear was noted at the arthroscopy An estimate of tear size was performed by the location of the medial edge of the tear |
|
| Index and comparator tests |
Index test(s): MRA and 3D‐US ‐ Description of technique: MRA MRI unit: 3.0 T magnet with a dedicated shoulder coil Sequences and Planes: Fat‐suppressed T1‐weighted spin‐echo images (TR/TE, 650 to 750/12) in the transverse plane, sagittal oblique plane and coronal oblique plane. T2‐weighted turbo spin‐echo (TSE) images (4000 to 4500/70) in the sagittal oblique and coronal oblique plane Contrast and procedure: 12 to 15 mL of diluted gadopentetate dimeglumine with a concentration of 2.0 mmol/L The procedure involved direct intra‐articular injection with fluoroscopic guidance Patient position: Supine with the arm in neutral position 3D US Scanner: 8 to 15 MHz with a dedicated 3D‐volume transducer Technique: Images were obtained in longitudinal scans of supraspinatus tendon 3D‐US data were transferred to a separate workstation which was equipped with various post‐processing software that allowed display and interactive analysis of the 3D data In the section mode the volume data were visualised in three orthogonal scan planes, i.e., longitudinal, transverse, and the C‐plane (parallel to the surface of the transducer) Patient position: Patients with the arm in internal rotation, as the patient placed his or her arm on the buttock ‐ Criteria for a positive result: MRA: Full‐thickness tears: the extension of the contrast medium through the entire thickness of the rotator cuff or presence of the contrast medium in the subacromial–subdeltoid bursa or both Partial thickness tears: no communication between the glenohumeral joint and the subacromial–subdeltoid bursa 3D‐US: Full thickness tear: a hypoechoic zone extending through the entire substance of the cuff or segmental or complete loss of rotator cuff substance with visualised tear margins or non‐visualisation of the cuff Partial thickness tear: a focal hypoechoic or anechoic defect in the tendon involving either the bursal or the articular surface and manifesting in both longitudinal transverse planes ‐ Time from symptoms to index test: Not reported ‐ Time from 3D‐US to MRA: The index tests were performed sequentially on the same day beginning with 3D‐US and ending with the MRA ‐ Time from index test to reference standard: mean 24.9 days (range 4 to 99 days |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | The rotator cuff tears were focused on only supraspinatus tendon tears A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Population was patients with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive The care setting was not specified |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target conditions were presence of full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | Yes | The average interval between reference standard and index test was less than one month |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status Of the 128 eligible participants only 50 (39%) underwent to reference standard 16 patients (12.5%) refused surgery as they had improved and it was unclear why the other patients did not receive the reference standard |
| Differential verification avoided? All tests | No | Probably the result of the index test influenced the choice of the reference standard |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The index tests were interpreted before and without knowledge of the reference standard results |
| Reference standard results blinded? All tests | No | The results of the index tests were probably known to the person interpreting the reference tests |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | No | The results of 78 (41%) patients were not reported |
| Withdrawals explained? All tests | No | Some of the eligible patients who entered the study did not complete it and these patients were not accounted for |
| Learning curve / training reported of index test? All tests | Yes | The interpreter of MRA was a musculoskeletal radiologist with 15 years experience The interpreters of US were two radiologists with respectively 5 and 10 years experience performing musculoskeletal US |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Lambert 2009.
| Clinical features and settings |
Inclusion criteria: Not reported Exclusion criteria: Not reported Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Tertiary or secondary |
|
| Participants |
Place of study: Dijon, France Period of study: November 2005 to June 2007 Number of participants eligible: 192 participants Number of participants enrolled IT and RS: ‐ MRI and arthroscopy or open surgery: 48 participants Data available for analyses: ‐ MRI and arthroscopy or open surgery: 48 participants Age (mean): 56 years Gender: Not reported Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To demonstrate the value of 3.0 T MRI for the detection of rotator cuff tendon tears Study design: Prospective, accuracy cohort study Unclear whether consecutive recruitment Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy or open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): MRI ‐ Description of technique: MRI unit: 3.0 T scanner with a shoulder coil Sequences and Planes: Fat suppressed TSE T2‐weighted in three planes (TR/TE 3000/39) A sagittal T1‐weighted sequence to detect fatty muscle atrophy Patient position: Not reported ‐ Criteria for a positive result: Full thickness tears: presence of hyperintense fluid signal with a communication between the glenohumeral joint and subacromial space Partial thickness tears: hyperintense fluid signal or irregularity at the articular or bursal surface of the tendon ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: mean 77.6 days (range 22 to 169 days) |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | No | Unknown why patients had MRI shoulder as included all people who had one at their institution of a period of time November 2005 to June 2007 |
| Acceptable reference standard? All tests | Unclear | The reference standard was shoulder arthroscopy or open surgery and the target condition were presence of any rotator cuff tears, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | No | The average interval between reference standard and index test was 77.6 days |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status. Of the 192 eligible participants, only 48 underwent to reference standard |
| Differential verification avoided? All tests | Unclear | Insufficient information was given to permit judgement |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Reference standard results blinded? All tests | No | The results of the index tests were known to the person interpreting the reference tests |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Unclear | Insufficient information was given to permit judgement |
| Withdrawals explained? All tests | No | Some of the eligible patients who entered the study did not complete it and these patients were not accounted for |
| Learning curve / training reported of index test? All tests | Unclear | Insufficient information was given to permit judgement |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Martin‐Hervas 2001.
| Clinical features and settings |
Inclusion criteria: Patients with shoulder pain and limited movement Exclusion criteria: Patients with claustrophobia, metallic implants, and pacemaker Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Not reported |
|
| Participants |
Place of study: Madrid, Spain Period of study: During 1998 Number of participants eligible: 140 shoulders Number of participants enrolled IT and RS: ‐ MRI and arthroscopy or open surgery: 61 shoulders ‐ US and arthroscopy or open surgery: 72 shoulders Data available for analyses: ‐ MRI and arthroscopy or open surgery: 61 shoulders ‐ US and arthroscopy or open surgery: 61 shoulders Age: Not reported Male/Female: 25/36 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To compare the accuracy of US and MRI in the diagnosis of rotator cuff injuries (focusing on supraspinatus tears) using arthroscopy or open surgery findings as the gold standard Study design: Prospective accuracy cohort study with fully paired direct comparison between US and MRI Unclear whether consecutive recruitment Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy or open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): MRI and US ‐ Description of technique: MRI MRI unit: 0.5 T superconducting magnet Sequences: Spin echo T1‐weighted sequences for coronal and oblique plane images and gradient echo T2*‐weighted sequences for axial and oblique coronal images; when the supraspinatus tendon showed a suggestive increased signal intensity, spin echo T2‐weighted sequences were performed Planes: Axial, oblique coronal and oblique sagittal images Patient position: Patient in a supine position and the arm in a neutral position US Scanner: 7.5 MHz high‐resolution linear electronic transducer Technique and Patient position: Images were obtained in transverse and longitudinal plane scans on the anterior plane of a shoulder with a neutrally rotated humerus to visualise bicipital and subscapularis bursae and axilla Next, sections of the shoulder were performed with internal humeral rotation, and the transducer was moved laterally to visualise the supraspinatus tendon and subacromial bursa The last images were obtained in the posterior plane with the humerus in a neutral position to visualise the infraspinatus and teres minor tendons ‐ Criteria for a positive result: MRI: Full thickness tears: hypersignal on the T1‐ and T2‐weighted images or any irregularity in the borders of the entire thickness of the tendon Partial thickness tears: any irregularity within the tendon or at the bursal or joint surfaces US: Full thickness tears: complete absence of the tendon, focal atrophy, a concave border, liquid‐filled hypoechoic bands, and/or lineal hyperechoic bands Partial thickness tears: heterogeneous tendon with hypoechoic areas (> 3 mm) that do not reach both sides of the tear and an irregular or indented border ‐ Time from symptoms to index test: Not reported ‐ Time from MRI and US: Not reported ‐ Time from index test to reference standard: Less than 6 months |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | The rotator cuff tears were focused on only supraspinatus tendon tears No two‐by‐two table of the ITs and RS was given, but it was possible to back‐calculate this from the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Tertiary or secondary care, participants with suspected of having any rotator cuff tears The study was prospective It was unclear whether consecutive recruitment |
| Acceptable reference standard? All tests | Unclear | The reference standard was arthroscopy or open surgery and the target conditions were presence of any rotator cuff tears, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | Unclear | The interval between tests was not clearly reported |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status |
| Differential verification avoided? All tests | Unclear | Insufficient information was given to permit judgement |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The study was prospective and the results of the index tests were interpreted before the reference standard |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Unclear | Insufficient information was given to permit judgement |
| Withdrawals explained? All tests | No | Some of the eligible patients who entered the study did not complete it and these patients were not accounted for |
| Learning curve / training reported of index test? All tests | Unclear | The interpreter of index test was a musculoskeletal radiologist Experience was not reported |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Milosavljevic 2005.
| Clinical features and settings |
Inclusion criteria: Participants with shoulder symptoms longer than 3 months duration and clinical findings of impingement and suspected rotator cuff tears were referred for US of the shoulder The patients had pain at rest and during motion, the pain‐provoking test was positive, and some patients had weakness of the rotator cuff muscles Exclusion criteria: Not reported Duration of symptoms: Participants with shoulder symptoms longer than 3 months duration Previous treatments: Not reported Care setting: Not reported |
|
| Participants |
Place of study: Uppsala, Sweden Period of study: February 1999 to October 2002 Number of participants eligible: 185 participants (190 shoulders) Number of participants enrolled IT and RS: ‐ US and arthroscopy: 185 participants (190 shoulders) Data available for analyses: ‐ US and arthroscopy: 185 participants (190 shoulders) Age: mean 57 years (range 22 to 78 years) Male/Female: 114/71 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To evaluate the accuracy of high‐resolution shoulder US compared with arthroscopy in a large group of consecutive patients with clinically suspected rotator cuff disease Study design: Prospective consecutive accuracy cohort study Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy ‐ Description of technique: Patient in the beach‐chair position under general anaesthesia Posterior and anterior portal were used The cartilage of the humeral head and the glenoid fossa, the labrum ligament complex, the biceps tendon, the intraarticular portion of the subscapular tendon, and the underside of the rotator cuff were inspected ‐ Criteria for a positive result: In the same manner as for the US findings, i.e. intact cuff, full thickness tears, or partial thickness tears (see below) |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Scanner: 10 MHz linear‐array transducer Technique: All tendons were examined in longitudinal and transversal plane Patient position: Both patient and examiner seated on rotatable chairs without armrests The examiner faced the patient and was seated at the patient’s right side ‐ Criteria for a positive result: Full thickness tears: defect (hypoechoic zone) extending through the entire substance of the cuff; focal, mixed hyper‐ and hypoechoic lesion extending through the entire substance of the cuff; focal thinning with visible margins of the tear; and non‐visualisation of the cuff Partial thickness tears: mixed hyper‐ and hypoechoic focus or a hypoechoic lesion visualised in two orthogonal imaging planes located within the tendon substance but not extending to the surface or with either articular or bursal extension ‐ Time from symptoms to index test: More than 3 months ‐ Time from index test to reference standard: mean 6 months (range 1 day to 18 months) |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Population was patients with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive The care setting was not specified |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target conditions were presence of any rotator cuff tear, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | No | The average interval between reference standard and index test was 6 months |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | All patients received the same reference standard regardless of the result of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | No | When there was disagreement between index test and reference standard findings the results of index test (US) were re‐evaluated to explain discrepancy |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The study was prospective, recruitment was consecutive and results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Unclear | The interpreter of index tests was a radiologist Training and expertise were not described |
| Learning curve / training reported of reference standard? All tests | Unclear | The reference standards were performed by three shoulder surgeons Training and expertise were not described |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Misamore 1991.
| Clinical features and settings |
Inclusion criteria: Participants with symptoms and physical findings consistent with chronic tendinitis or with degeneration or a tear of the rotator cuff Patients who had signs indicating stage II or stage III impingement were included Exclusion criteria: Patients who had an acute injury or who had symptoms for less than one year were excluded Patients were excluded if they had a previous operation on the affected shoulder, if they had any associated disorders of the shoulder (such as arthritis or instability), or if they had cervical radiculopathy or peripheral neuropathy Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Not reported |
|
| Participants |
Place of study: Indianapolis, Indiana, USA Period of study: January 1988 to June 1989 Number of participants eligible: 82 participants Number of participants enrolled IT and RS: ‐ US and arthroscopy or open surgery: 32 participants Data available for analyses: ‐ US and arthroscopy or open surgery: 32 participants Age: mean 47 years (range 35 to 65 years) Male/Female: 26/6 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To compare the accuracy of arthrography compared with US in the evaluation of thirty‐two patients who had a degenerative lesion of the rotator cuff. Study design: Prospective consecutive accuracy cohort study Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of full thickness tears and partial thickness rotator cuff tears Reference standard(s): Shoulder arthroscopy or open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Not reported ‐ Criteria for a positive result: Full thickness tear: an obvious defect localised to the tendon of the rotator cuff was seen or alternatively when there was no echo of the rotator cuff An abnormality of echogenicity alone was not considered to be a tear ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | No two‐by‐two table of the ITs and RS was given, but it was possible to back‐calculate this from the reported summary data for detecting any rotator cuff tears | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Population was patients with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive The care setting was not specified |
| Acceptable reference standard? All tests | Unclear | The reference standard was arthroscopy or open surgery and the target conditions were presence of full and partial thickness tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status Of the 82 eligible participants, 32 patients received the reference standard For 50 patients the symptoms were not severe enough to justify surgery or satisfactory improvement was achieved with conservative treatment |
| Differential verification avoided? All tests | No | Probably the result of the index test influenced the choice of the reference standard |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The index tests were interpreted before and without knowledge of the reference standard results |
| Reference standard results blinded? All tests | No | The results of index tests were probably known to the person interpreting the reference standard |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | Results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | The number and reasons of all withdrawals from the study were explained |
| Learning curve / training reported of index test? All tests | Yes | The interpreters of index tests were radiologists who were skilled in the technique |
| Learning curve / training reported of reference standard? All tests | Unclear | The reference standards were performed by one of the authors (orthopaedic surgeon) |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Mohtadi 2004.
| Clinical features and settings |
Inclusion criteria: Patients with shoulder pain at night or with overhead activity greater than 3 months duration or both A minimum of 3 of the following 6 clinical findings: a painful arc of motion in the scapular plane (60° to 120°) of elevation; pain‐related weakness on resisted elevation in the scapular plane; Neer’s impingement sign; Hawkin’s impingement sign; point of maximal tenderness over the supraspinatus tendon; and positive impingement xylocaine test Failure of conservative management The patients consented to undergo shoulder arthroscopy and subacromial decompression Exclusion criteria: Patients with symptoms of instability Signs of instability Point of maximum tenderness over the acromioclavicular joint Any signs or symptoms consistent with associated cervical spine pathology Previous surgery, arthrography, ultrasound, or MRI Duration of symptoms: More than 3 months of symptoms Previous treatments: Conservative management (nonsteroidal anti‐inflammatory drugs, physiotherapy, home‐based rehabilitation, cortisone injections, and modification of activity) Care setting: Tertiary or secondary |
|
| Participants |
Place of study: Calgary, Alberta, Canada Period of study: 1998 to 2000 Number of participants eligible: 73 participants Number of participants enrolled IT and RS: ‐ Indirect MRA and arthroscopy: 58 participants Data available for analyses: ‐ Indirect MRA and arthroscopy: 58 participants Age: mean 46.2 years (range 21 to 73 years) Male/Female: 43/15 Dominant arm: Not reported Nature of onset: Of these 58 patients, 91.4% reported pain at night and 96.6% reported pain with activity above shoulder level |
|
| Study design |
Primary objective: To determine the diagnostic ability of MRI compared with a reference standard, arthroscopy, in patients presenting with shoulder pain consistent with the signs and symptoms of shoulder impingement Study design: Prospective, consecutive accuracy cohort study Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence full thickness tears and partial thickness supraspinatus tendon tears Presence of any infraspinatus tendon tears Presence of any subscapularis tendon tears Reference standard(s): Shoulder arthroscopy ‐ Description of technique: In accordance with the standardised 15‐point protocol of Snyder classification This included standard posterior and anterior portal examination with subsequent visualisation in the subacromial bursa The subacromial (bursal) examination was not performed All surgeries were videotaped ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): Indirect MRA ‐ Description of technique: MRI unit: 1.5 T with conventional shoulder coil Sequences and Planes: Axial water density (TR/TR 1000/20) and multi‐planar gradient recalled (TR/TE 400/20, flip angle20o) Oblique coronal fast multi‐planar inversion recovery (TR/TE 4600/28, inversion time 150) Oblique coronal post‐gadolinium fat‐saturated T1‐weighted (TR/TE 400/8) and sagittal T1‐weighted (TR/TE 400/8) Contrast and procedure: Intravenous gadolinium administration Patient position: Supine with the arm in a neutral position ‐ Criteria for a positive result: Not reported ‐ Time from symptoms to index test: More than 3 months of symptoms ‐ Time from index test to reference standard: Upon entry into the study patients were scheduled to undergo MRI within 1 week before arthroscopy |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | The analyses of rotator cuff tears were focused on only supraspinatus and subscapularis tendons tears No two‐by‐two table of the ITs and RS was given, but it was possible to back‐calculate this from the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Tertiary or secondary care, participants with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target conditions were presence full thickness tears and partial thickness supraspinatus tendon tears; presence of any infraspinatus tendon tears; presence of any subscapularis tendon tears |
| Acceptable delay between tests? All tests | Yes | Patients were scheduled to undergo MRI within 1 week before arthroscopy |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status Of the 73 eligible participants, eight cancelled the surgery and seven did not undergo MRI within a week and were excluded but their results were not reported |
| Differential verification avoided? All tests | Yes | All patients received the same reference standard regardless of the result of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The index tests were interpreted before and without knowledge of the reference standard results |
| Reference standard results blinded? All tests | Yes | Before and during diagnostic arthroscopy, the surgeon was blinded to the MRI results |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The study was prospective recruitment was consecutive and results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | The number and reasons of all withdrawals from the study were explained |
| Learning curve / training reported of index test? All tests | Unclear | The interpreter of index tests was a musculoskeletal radiologist Training and expertise were not described |
| Learning curve / training reported of reference standard? All tests | Unclear | The reference standards were performed by two experienced orthopaedic surgeons Training and expertise were not described |
| Index test criteria for a positive test result reported? All tests | No | Not reported |
Nicoletti 1994.
| Clinical features and settings |
Inclusion criteria: Patients who had shoulder pain and signs and symptoms of rotator cuff tears with failure of conservative treatment Exclusion criteria: Patients with suspected of instability and neurologic symptoms Duration of symptoms: More than 3 months Previous treatments: Physiotherapy Care setting: Tertiary |
|
| Participants |
Place of study: Sao Paulo, Brazil Period of study: Not reported Number of participants eligible: 48 participants Number of participants enrolled IT and RS: ‐ US and arthroscopy: 48 participants Data available for analyses: ‐ US and arthroscopy: 48 participants Age: mean 48 years (range 19 to 79 years) Male/Female: 16/32 Dominant arm: 65% Nature of onset: Not reported |
|
| Study design |
Primary objective: To evaluate the sensitivity, specificity and accuracy of arthrography and US to detect rotator cuff tears Study design: Unclear whether prospective design Unclear whether consecutive recruitment Language: Portuguese |
|
| Target condition and reference standard(s) |
Target conditions: Presence any rotator cuff tears Reference standard(s): Shoulder arthroscopy ‐ Description of technique: Patient in lateral position with traction in the operative limb The posterior and anterior portals were used to visualise the glenohumeral and subacromial spaces ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Scanner: 5 or 7 MHz linear transducer in real time Technique and Patient position: As described by Crass 1985 ‐ Criteria for a positive result: US signs were: focal or diffuse thinning or non‐visualisation of tendon(s) ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | A two‐by‐two table of the ITs and RS was given which tallied with the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Unclear whether prospective design and consecutive recruitment |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target condition was presence of any rotator cuff tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Unclear | Insufficient information was given to permit judgement |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The number of results reported agrees with the number of patients recruited |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Yes | The interpreter of index tests was a musculoskeletal radiologist |
| Learning curve / training reported of reference standard? All tests | Yes | The reference standards were performed by an experienced shoulder surgeon |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Sipola 2010.
| Clinical features and settings |
Inclusion criteria: Participants with acute or chronic shoulder pain and suspicion of rotator cuff tears Patients who had undergone conservative treatment without sufficient symptom relief Exclusion criteria: Time elapsed between index test and reference standard was more than 12 months Duration of symptoms (pain): mean 21 months (range 2 to 144 months Previous treatments: Conservative treatment including physiotherapy for at least 3 months Care setting: Tertiary or secondary |
|
| Participants |
Place of study: Kuopio, Finland Period of study: Not reported Number of participants eligible: 79 participants Number of participants enrolled IT and RS: ‐ MRA and arthroscopy or open surgery: 75 participants ‐ US and arthroscopy or open surgery: 77 participants Data available for analyses: ‐ MRA and arthroscopy or open surgery: 75 participants ‐ US and arthroscopy or open surgery: 77 participants Age: mean 57 years (range 42 to 76 years) Male/Female: 40/37 Dominant arm: Not reported Nature of onset: The etiology of suspected tear was traumatic in 22% and degenerative in 78% of the participants |
|
| Study design |
Primary objective: To compare the accuracy of US and MRA for the detection and measurement of rotator cuff tears using surgical findings as the standard in a prospective study setting Study design: Prospective, consecutive, accuracy cohort study with fully paired direct comparison between MRA and US Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy or mini‐open ‐ Description of technique: Not reported ‐ Criteria for a positive result: The size and type (partial/full thickness) of tendon tear was determined and measured from anterior to posterior and from lateral to medial dimensions A sterile ruler or a calibrated arthroscopic probe was used to define both the anteroposterior and the mediolateral size of the tear |
|
| Index and comparator tests |
Index test(s): MRA and US ‐ Description of technique: MRA MRI unit: 1.5 T scanner equipped with a flexible surface coil Sequences and Planes: Oblique coronal T1‐weighted spin‐echo (TR/TE 650/20); a T2‐weighted fat‐saturated dual‐echo fast spin‐echo (FSE), 3500/16; oblique sagittal T2‐weighted dual‐echo FSE, 3500/16, 98; axial T2*‐weighted gradient echo two‐dimensional FLASH, 580/15, flip angle 15o; a T1‐weighted fat‐saturated SE, 800/20; T1‐weighted fat‐saturated spin‐echo 800/20 images in the sagittal oblique, coronal oblique and axial planes, and T2‐weighted FSE 4500/96 images in the coronal oblique plane Contrast and procedure: 10 to 20 mL of gadopentetate dimeglumine in a concentration of 469.01 mg/mL was diluted in 250 mL of saline The procedure involved direct intra‐articular injection Patient position: Not reported Seven participants underwent to MRI only (without an intra‐articular contrast) US Scanner: 7.5 MHz linear‐array transducers in real‐time Technique: Images were obtained on the long and short axes of the tendon Patient position: The subscapularis tendon was evaluated with the forearm rotated externally The supraspinatus tendon was assessed with the arm on the ipsilateral side The supraspinatus was assessed with the hand behind the patient’s back (Crass position) or on the waist (modified Crass position) (Crass 1987; Ferri 2005) The infraspinatus tendon was assessed with the patient placed the ipsilateral hand across the chest on top of the contralateral shoulder ‐ Criteria for a positive result: MRA: Full thickness tears: the contrast agent was detected on the MR image throughout the full thickness of the rotator cuff and/or when the contrast agent was detected in the subacromial bursa Partial thickness tears: the contrast agent entered the cuff substance without reaching the subacromial bursa US: Full thickness tears: hypoechoic area or volume loss extended from the bursal surface to the articular surface of the tendon Otherwise the tear was diagnosed as a partial thickness tear ‐ Time from symptoms to index test: mean 21 months (range 2 to 144 months ‐ Time from MRA and US: in the same day ‐ Time from index test to reference standard: mean 2.3 months (range 0 to 9.5 months) |
|
| Follow‐up |
Adverse events due to index test(s): Of the 77 patients, two (3%) could not undergo MRA due to claustrophobia Adverse events due to reference standard test(s): Not reported |
|
| Notes | A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Tertiary or secondary care, participants with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive |
| Acceptable reference standard? All tests | Unclear | The reference standard was arthroscopy or open surgery and the target conditions were presence of any rotator cuff tears, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | No | The average interval between reference standard and index test was 2.3 months |
| Partial verification avoided? All tests | Yes | Only two patients (2.5%) were excluded of study because of delay in surgery 12 months due to medical illness |
| Differential verification avoided? All tests | No | The choice of reference standard (arthroscopy or open surgery) varied between individuals |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The study was prospective, recruitment was consecutive and results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | The number and reasons of all withdrawals from the study were explained |
| Learning curve / training reported of index test? All tests | Yes | The interpreter of MRA was a radiologist who had 1 year of experience in musculoskeletal MRI at the beginning of the study The interpreters of US were three radiologists each with more than 10 years experience in shoulder US |
| Learning curve / training reported of reference standard? All tests | Unclear | The reference standards were performed by three experienced orthopaedic surgeons Training and expertise were not described |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Stetson 2005.
| Clinical features and settings |
Inclusion criteria: Patients with chronic shoulder pain who were suspected of having a rotator cuff abnormality underwent MRA with use of an intra‐articular injection of gadolinium Exclusion criteria: Not reported Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Tertiary or secondary |
|
| Participants |
Place of study: Burbank, California, USA Period of study: During 2 years Number of participants eligible: 50 participants Number of participants enrolled IT and RS: ‐ MRA and arthroscopy: 50 participants Data available for analyses: ‐ MRA and arthroscopy: 50 participants Age: Not reported Gender: Not reported Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To detect partial thickness articular‐sided rotator cuff tears using an intra‐articular injection of gadolinium and MRI Study design: Prospective accuracy cohort Unclear whether consecutive recruitment Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence partial articular‐side thickness tears Reference standard(s): Shoulder arthroscopy ‐ Description of technique: All participants were taken to surgery and underwent a complete 15‐point glenohumeral arthroscopic examination The presence or absence of articular‐sided rotator cuff tears was recorded ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): MRA ‐ Description of technique: MRI unit: 1.5 T scanner. Sequences and Planes: Axial proton‐density‐weighted image with fat suppression, oblique coronal proton‐density‐weighted image, oblique coronal T2‐weighted with fat suppression, oblique sagittal T1‐weighted, and oblique sagittal proton‐density‐weighted image with fat suppression. In addition, axial T1‐weighted with fat suppression, oblique coronal T1‐weighted with fat suppression Contrast and procedure: 1.5 mL of gadolinium with normal saline solution intra‐articularly into the glenohumeral joint under fluoroscopic control Patient position: Supine in neutral position and abduction and external rotation images were also acquired ‐ Criteria for a positive result: Not reported ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | The authors described as false positive the four patients who were incorrectly diagnosed with MRA, as having a full thickness tear, but, at the time of shoulder arthroscopy, they had partial thickness articular‐sided tears To make concordance with our analyses we described these participants as false negative No two‐by‐two table of the ITs and RS was given, but it was possible to back‐calculate this from the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | The study was prospective and the population was participants with shoulder pain and suspected of having any rotator cuff tears. However, it was unclear whether there was consecutive recruitment |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target condition was presence of partial articular‐side rotator cuff tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | All patients received the same reference standard, regardless of the result of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Reference standard results blinded? All tests | No | The results of the index tests were probably known to the person interpreting the reference tests |
| Relevant clinical information? All tests | Unclear | Insufficient information was given to permit judgement |
| Uninterpretable results reported? All tests | Yes | The number of results reported agrees with the number of patients recruited |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Yes | The interpreter of index tests was a fellowship‐trained musculoskeletal radiologist |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | No | Not reported |
Swen 1998.
| Clinical features and settings |
Inclusion criteria: Patients awaiting surgery because of clinically suspected of rotator cuff tears The clinical diagnosis of rotator cuff tears was based on marked difficulty in initiating abduction of the arm with weakness and limitation of movement Lidocaine was injected below the acromion, if after the injection the strength of the rotator cuff was still decreased; this was considered to indicate rotator cuff tears Exclusion criteria: Patients with neurologic origins of the weakness Duration of symptoms: mean 2.3 years (range 0.3 to 10 years) Previous treatments: Not reported Care setting: Not reported, probably tertiary or secondary |
|
| Participants |
Place of study: The Netherlands Period of study: January 1993 to December 1995 Number of participants eligible: 48 participants Number of participants enrolled IT and RS: ‐ US and arthroscopy or open surgery: 48 participants Data available for analyses: ‐ US and arthroscopy or open surgery: 48 participants Age: mean 55 years (range 30 to 76 years) Male/Female: 28/20 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To compare the diagnostic value of US performed by the rheumatologist with that of arthrography by a radiologist for otherwise healthy patients with suspected rotator cuff tears Study design: Prospective consecutive accuracy cohort study Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence full thickness tears Reference standard(s): Shoulder arthroscopy and open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: A full‐thickness was diagnosed if free communication was found between the bursal and humeral sides of the cuff |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Scanner: 7.5 MHz linear array and the 5.0 MHz curved array transducers Technique: The shoulder was examined in the anterior, lateral, and posterior directions, in both the transverse and the longitudinal planes as described by Van Holsbeeck 1991 Patient position: The patients were seated For the anterior approach, the patient’s upper arm was visualised in internal rotation, which was achieved by placing the patient’s hand behind the back ‐ Criteria for a positive result: Full thickness tears: a discontinuity in the rotator cuff extending from the bursal to the humeral side of the rotator cuff ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | A two‐by‐two table of the ITs and RS was given which tallied with the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Tertiary or secondary care Participants with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy or open surgery and the target conditions were presence of full thickness tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | All patients received the same reference standard, regardless of the result of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The study was prospective and the results of the index tests were interpreted before the reference standard |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The study was prospective, recruitment was consecutive and results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Yes | The interpreter of index tests was a rheumatologist with experience in this technique |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Swen 1999.
| Clinical features and settings |
Inclusion criteria: Patients awaiting surgery because of a clinically suspected rotator cuff tears The clinical diagnosis of rotator cuff tears was based on marked difficulty in initiating abduction of the arm with weakness and limitation of movement Lidocaine was injected below the acromion, if after the injection the strength of the rotator cuff was still decreased; this was considered to indicate rotator cuff tears Exclusion criteria: Patients with neurologic origins of the weakness Duration of symptoms: mean 2.3 years (range 0.3 to 8 years) Previous treatments: Not reported Care setting: Not reported Probably tertiary or secondary |
|
| Participants |
Place of study: The Netherlands Period of study: Not reported Number of participants eligible: 21 participants Number of participants enrolled IT and RS: ‐ MRI and arthroscopy: 21 participants ‐ US and arthroscopy: 21 participants Data available for analyses: ‐ MRI and arthroscopy: 21 participants ‐ US and arthroscopy: 21 participants Age (mean/SD): 54/12 years Male/Female: 12/9 Dominant arm: Not reported Nature of onset: In four patients the shoulder complaints could be attributed to trauma |
|
| Study design |
Primary objective: To evaluate the ability of US and MRI to detect full thickness rotator cuff tears in patients with a clinically suspected rotator cuff tears as a solitary non‐inflammatory condition Study design: Prospective, consecutive, accuracy cohort study with fully paired direct comparison between MRI and US Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence full thickness tears Reference standard(s): Shoulder arthroscopy ‐ Description of technique: First the arthroscope was introduced in the glenohumeral joint and then into the subacromial space After introducing the scope into the subacromial space, the bursa was removed to enable examination of the bursal side of the cuff ‐ Criteria for a positive result: A full‐thickness was diagnosed if free communication was found between the bursal and humeral sides of the cuff |
|
| Index and comparator tests |
Index test(s): MRI and US ‐ Description of technique: MRI MRI unit: 1.0T system with a dedicated shoulder coil as receiver Sequences: T1‐weighted (TR/TE 680/15) and a standard T2 coronal spin‐echo sequence (TR/TE 3000/15,105 ms) Planes: Oblique coronal Patient position: Supine position US Scanner: 7.5 MHz linear array and the 5.0 MHz curved array transducers Technique: The shoulder was examined in the anterior, lateral, and posterior directions, in both the transverse and the longitudinal planes as described by Van Holsbeeck 1991 Patient position: The patients were seated For the anterior approach, the patient’s upper arm was visualised in internal rotation, which was achieved by placing the patient’s hand behind the back ‐ Criteria for a positive result: MRI: Full‐thickness tears: a focal, well‐defined area of increased signal intensity on T1‐weighted and T2‐weighted images that extended through the entire thickness of the tendon US: Full‐thickness tears: a discontinuity in the rotator cuff, extending from the bursal to the humeral side of the rotator cuff ‐ Time from symptoms to index test: Not reported ‐ Time from Conventional MRA and 3D isotropic MRA: Not reported ‐ Time from index test to reference standard: MRI and US were performed within 3 weeks before surgery |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | The results of index test were interpreted by two experienced musculoskeletal radiologists The data of only one reader (reader 1) were arbitrarily chosen to be included in our analyses Raw data were given and it was possible to back‐calculate this from the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Tertiary or secondary care, participants with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target condition was presence of full thickness tears |
| Acceptable delay between tests? All tests | Yes | The index tests were performed within 3 weeks of surgery |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | All patients received the same reference standard, regardless of the result of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The study was prospective and the results of the index tests were interpreted before the reference standard |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | No | The interpreters were blinded to history and physical examination |
| Uninterpretable results reported? All tests | Yes | The study was prospective, recruitment was consecutive and results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Unclear | A rheumatologist and a radiologist, both experienced with this test In fact they had different results but this was not examined in this study |
| Learning curve / training reported of reference standard? All tests | Unclear | The reference standards were performed by a single experienced surgeon |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Taboury 1992.
| Clinical features and settings |
Inclusion criteria: Not reported Exclusion criteria: Not reported Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Tertiary |
|
| Participants |
Place of study: Paris, France Period of study: Not reported Number of participants eligible: 24 participants Number of participants enrolled IT and RS: ‐ US and open surgery: 24 participants Data available for analyses: ‐ US and open surgery: 24 participants Age: Not reported Gender: Not reported Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To compare the results of US to open surgery in order to evaluate the characteristics of the rotator cuff tears Study design: Prospective accuracy cohort study Unclear whether consecutive recruitment Language: French |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears Reference standard(s): Open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Scanner: 5 to 10 MHz linear or vectorial short focal probe Technique: Static and dynamic examination of rotator cuff tendons Patient position: Patients seated with the arm in adduction and internal rotation by asking the patients to place their arm behind their back ‐ Criteria for a positive result: Not reported ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | Mr Jean‐Philippe Regnaux and Mr Ludovic Trinquart kindly translated into English and extracted the data of this study A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Unclear whether consecutive recruitment |
| Acceptable reference standard? All tests | Unclear | The reference standard was open surgery and the target condition was presence of any rotator cuff tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | All participants included in the analyses received open surgery, regardless of the results of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The person undertaking the index test was blinded to the results of the standard reference |
| Reference standard results blinded? All tests | Yes | The reference standard results were performed blind to the results of the index test |
| Relevant clinical information? All tests | Unclear | Insufficient information was given |
| Uninterpretable results reported? All tests | Yes | The number of results reported agrees with the number of patients recruited |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Unclear | Insufficient information was given |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given |
| Index test criteria for a positive test result reported? All tests | No | Not reported |
Teefey 2004.
| Clinical features and settings |
Inclusion criteria: Acute or chronic shoulder pain accompanied by a high clinical suspicion of rotator cuff disease Exclusion criteria: Participants with severe claustrophobia, which is a contraindication for magnetic resonance imaging; a previous operation on the shoulder; a humeral fracture; and inflammatory arthritis Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Not reported, probable tertiary or secondary |
|
| Participants |
Place of study: St. Louis, Missouri, USA Period of study: December 1998 and April 2001 Number of participants eligible: 130 participants Number of participants enrolled IT and RS: ‐ MRI and arthroscopy: 71 shoulders ‐ US and arthroscopy: 71 shoulders Data available for analyses: ‐ MRI and arthroscopy: 71 shoulders ‐ US and arthroscopy: 71 shoulders Age: mean 59 (range 31 to 80 years) Male/Female: 41/30 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To compare the diagnostic performances of US and MRI for both the detection of a rotator cuff tear and the quantification of its size, with use of arthroscopic findings as the standard Study design: Prospective, consecutive, accuracy cohort study with fully paired direct comparison between US and MRI Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy ‐ Description of technique: The rotator cuff was examined from both the articular and the bursal side. A tagged suture (number‐1 PDS [polydioxanone]) was placed, during intra‐articular viewing, through the suspected region of the cuff tear to guide arthroscopic bursal imaging ‐ Criteria for a positive result: The presence or absence of a rotator cuff tear and the size and extent of the tear, when present, were recorded. Specifically, the presence or absence of a full thickness tear or of a bursal or articular‐side partial thickness tear and the width (perpendicular to the long axis of the cuff fibres) of any tear that was found were recorded |
|
| Index and comparator tests |
Index test(s): MRI and US ‐ Description of technique: MRI MRI unit: 1.5 T with high field strength with a two‐piece shoulder array coil (54 participants); and with flexible local coils (17 participants) Sequences: Fat‐suppressed, fast‐spin‐echo, proton‐density‐weighted, spin‐echo, or fast‐spin‐echo and transverse, T2‐weighted, fast‐spin‐echo images with or without fat suppression Planes: Oblique coronal and oblique sagittal Patient position: Not reported US Scanner: 7.5 to 9 MHz linear‐array transducer in real‐time Technique and Patient position: As previously described (Teefey 2000). ‐ Criteria for a positive result: MRI: Full thickness tears: complete disruption of all tendon fibres or when the signal within the cuff tendons was isointense compared with fluid on the T2‐weighted images and extended from the articular to the bursal surface on one or more images. Partial thickness tears: fluid‐intensity signal within the tendons was in contact with only one of the surfaces US: Full thickness tears: non‐visualisation of rotator cuff or a focal defect in the rotator cuff created by a variable degree of retraction of the torn tendon ends. Partial thickness tears: minimal flattening of the bursal side of the rotator cuff (bursal‐side tear) or a distinct hypoechoic or mixed hyperechoic and hypoechoic defect visualized in both the longitudinal and the transverse plane at the deep articular side of the rotator cuff (articular‐side tear) ‐ Time from symptoms to index test: Not reported ‐ Time from US and MRI: MRI was performed on the same day as the US for all but three patients, two of whom had the studies six days apart and one of whom had them one day apart ‐ Time from index test to reference standard: mean 56 days (range 2 to 190 days) |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | Part of population (only the participants with full thickness rotator cuff tears) of this study was also reported in Teefey 2005 A two‐by‐two table of the ITs and RS was given, which tallied with the reported summary data with a few discrepancy |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Insufficient information was given to permit judgement |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target condition were presence of any rotator cuff tears, full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | No | The average interval between reference standard and index test was 56 days |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status Of the 130 eligible participants 71 underwent to reference standard |
| Differential verification avoided? All tests | No | The result of the index test probably influenced the choice of the reference standard |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The person undertaking the index test was blinded to the results of the standard reference |
| Reference standard results blinded? All tests | No | The results of the index tests were known to the person interpreting the reference tests |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Unclear | Insufficient information was given to permit judgement |
| Withdrawals explained? All tests | No | Some of the eligible patients who entered the study did not complete it and these patients were not accounted for |
| Learning curve / training reported of index test? All tests | Yes | The interpreter of MRI was one of six radiologists with extensive experience in musculoskeletal magnetic resonance imaging The interpreter of US was one of two radiologists who were very experienced with the technique and who had conducted more than 2500 examinations during a 10‐year period |
| Learning curve / training reported of reference standard? All tests | Unclear | The reference standards were performed by an experienced orthopaedic surgeon |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Venu 2002.
| Clinical features and settings |
Inclusion criteria: Participants with clinical supraspinatus impingement syndrome and failure of clinical improvements with conservative treatment within one year of onset of symptoms Exclusion criteria: Not reported Duration of symptoms: Probably more than one year Previous treatments: Shoulder physiotherapy and sub‐acromial steroid injections Care setting: Not reported |
|
| Participants |
Place of study: Eastbourne, UK Period of study: June 1997 to June 1999 Number of participants eligible: 276 participants Number of participants enrolled IT and RS: ‐ US and arthroscopy: 41 participants Data available for analyses: ‐ US and arthroscopy: 41 participants Age: mean 54 years (range 34 to 79 years) Male/Female: 24/17 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To determine the accuracy of ultrasound compared with arthroscopy in the evaluation of the symptomatic supraspinatus tendon and to identify whether ultrasound diagnosis was helpful in pre‐operative planning Study design: Prospective, consecutive, accuracy cohort study Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of normal tendon, tendinopathy, partial thickness tear, full thickness tear, and rotator cuff rupture Reference standard(s): Shoulder arthroscopy ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Scanner: 5 to 10 MHz using a linear array transducer Technique: Longitudinal and transverse views of the supraspinatus Patient position: Patient probably seated with the shoulder internally rotated to visualise the supraspinatus tendon ‐ Criteria for a positive result: Tendinopathy: thickened and often decreased echogenicity Partial thickness tears: a hypo‐or hyperechoic tendon defect not involving the full thickness of the tendon Full thickness tears: a hypo or hyperechoic tendon defect involving the full thickness of the tendon Rupture: the tendon was absent with often only the retracted proximal tendon visualised ‐ Time from symptoms to index test: More than 1 year ‐ Time from index test to reference standard (mean): 6 months |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | The study reported five categories to classify the tendon (normal tendon, tendinopathy, partial thickness tear, full thickness tear, and rotator cuff rupture) In our analyses we classified the categories ‘normal’ and ‘tendinopathy’ as normal tendon; and ‘full’ and ‘rupture’ as full thickness tear No two‐by‐two table of the ITs and RS was given but it was possible to back‐calculate this from the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Population was patients with suspected of having any rotator cuff tears The study was prospective and recruitment was reported as consecutive The care setting was not specified |
| Acceptable reference standard? All tests | Yes | The reference standard was arthroscopy and the target conditions were presence of normal tendon, tendinopathy, partial thickness tear, full thickness tear, and rotator cuff rupture |
| Acceptable delay between tests? All tests | No | The average interval between reference standard and index test was 6 months |
| Partial verification avoided? All tests | No | Not all the patients who received the index test underwent a reference standard to verify their true disease status Of the 276 eligible participants only 41 (15%) received the reference standard |
| Differential verification avoided? All tests | No | The result of the index test influenced the choice of the reference standard |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The study was prospective and the results of the index tests were interpreted before the reference standard |
| Reference standard results blinded? All tests | No | The surgeon knew the US diagnosis prior to surgery |
| Relevant clinical information? All tests | Yes | Clinical data and plain radiographs were available at the time of performing the US examination |
| Uninterpretable results reported? All tests | No | The results of 235 (85%) patients were not reported |
| Withdrawals explained? All tests | No | Some of the eligible patients who entered the study did not complete it and these patients were not accounted for |
| Learning curve / training reported of index test? All tests | Yes | The interpreters of index tests were two radiologists specialised in shoulder US |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Wallny 2001.
| Clinical features and settings |
Inclusion criteria: Participants suffering from shoulder pain with histories and physical examinations suggestive of rotator cuff lesions Exclusion criteria: Participants with prior shoulder surgery or previous fracture of the humeral head Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Tertiary or secondary |
|
| Participants |
Place of study: Bonn, Germany Period of study: Not reported Number of participants eligible: 40 participants Number of participants enrolled IT and RS: ‐ Two‐dimensional (2D) US and arthroscopy or open surgery: 40 participants ‐ Tree‐dimensional (3D) US and arthroscopy or open surgery: 40 participants Data available for analyses: ‐ 2D US and arthroscopy or open surgery: 40 participants ‐ 3D US and arthroscopy or open surgery: 40 participants Age: mean 54 years (range 38 to 79 years) Male/Female: 25/15 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To determine the validity of 3D US in the diagnosis of rotator cuff lesions Study design: Prospective, consecutive, accuracy cohort study with fully paired direct comparison between 3D US and 2D US Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy or open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): 3‐D US and 2‐D US ‐ Description of technique: Scanner: 10 MHz electronic linear array in broad bandwidth technology, 192 fine pitch elements, frequency ranges: resolution: 4.5 to 13 MHz, penetration: 2.5 to 10 MHz Technique and Patient position: Not reported The region of interest was defined by 2D US before 3D US could be undertaken ‐ Criteria for a positive result: Full thickness tear was defined as: marked thinning, sudden changes of calibre, hyper‐ and/or hypoechoic zones and total absence of the cuff Partial thickness tear was defined as: constituting no more than loss of 1/4 to 1/2 of full thickness of the intact rotator cuff ‐ Time from symptoms to index test: Not reported ‐ Time from 2D US and 3D US: in the same examination ‐ Time from index test to reference standard: Not reported |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | The study reported that the target conditions were presence of any rotator cuff tears, full thickness tears and partial thickness tears Only the data for analysing presence of any rotator cuff tears were available The study reported the data of two different types of US (three‐dimensional and two‐dimensional) Inasmuch as the 2D US examinations are more often used in clinical practice we arbitrarily chose 2D US to be included in our analyses A two‐by‐two table of the ITs and RS was given which tallied with the reported summary data |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Tertiary or secondary care, participants with suspected of having any rotator cuff tears The study was prospective and recruitment was consecutive |
| Acceptable reference standard? All tests | Unclear | The reference standard was arthroscopy or open surgery and the target conditions were presence of full thickness tears and partial thickness tears |
| Acceptable delay between tests? All tests | Unclear | The study did not report the time elapsed between the index tests and reference standard |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | The indication for surgery was based on the results of clinical assessment and an MRI scan but independent of the result of the index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The study was prospective and the results of the index tests were interpreted before the reference standard |
| Reference standard results blinded? All tests | Unclear | Insufficient information was given to permit judgement |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The study was prospective Recruitment was consecutive and results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Unclear | Insufficient information was given to permit judgement |
| Learning curve / training reported of reference standard? All tests | Unclear | The reference standards were performed by a single orthopaedic surgeon |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
Yen 2004.
| Clinical features and settings |
Inclusion criteria: Patients with shoulder pain and suspected of rotator cuff tears Exclusion criteria: Not reported Duration of symptoms: Not reported Previous treatments: Not reported Care setting: Not reported |
|
| Participants |
Place of study: Taiwan, China Period of study: Not reported Number of participants eligible: 50 participants Number of participants enrolled IT and RS: ‐ US and open surgery: 50 Data available for analyses: ‐ US and open surgery: 50 Age: mean 63 years (range 17 to 81 years) Male/Female: 26/24 Dominant arm: Not reported Nature of onset: Not reported |
|
| Study design |
Primary objective: To prospectively compare the US and operative findings of rotator cuff tears Study design: Prospective accuracy cohort study Unclear whether consecutive recruitment Language: English |
|
| Target condition and reference standard(s) |
Target conditions: Presence any rotator cuff tears Reference standard(s): Open surgery ‐ Description of technique: Not reported ‐ Criteria for a positive result: Not reported |
|
| Index and comparator tests |
Index test(s): US ‐ Description of technique: Scanner: 7 MHz linear transducer Technique: Longitudinal, transverse and oblique scans of the tendons were used Patient position: Probably patient seated with the arm in External rotation for scanning the subscapularis tendon Neutral position for the long head of the biceps tendon Internal rotation and with the patient's hand behind the back with extreme internal rotation for the supraspinatus tendon Flexion and adduction for infraspinatus and teres minor tendons ‐ Criteria for a positive result: Six US signs were used: non‐visualisation; Floating bright spots Focal depression Focal thinning Focal hypoechoic cleft Focal heterogeneous hypoechogenicity ‐ Time from symptoms to index test: Not reported ‐ Time from index test to reference standard: within 1 month |
|
| Follow‐up |
Adverse events due to index test(s): Not reported Adverse events due to reference standard test(s): Not reported |
|
| Notes | A two‐by‐two table of the ITs and RS was given which tallied with the reported summary data | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Population was patients with suspected of having any rotator cuff tears The study was prospective It was unclear whether consecutive recruitment |
| Acceptable reference standard? All tests | Unclear | The reference standard was open surgery and the target condition was presence of any rotator cuff tears |
| Acceptable delay between tests? All tests | Yes | The reference standard was performed within 1 month after the index test |
| Partial verification avoided? All tests | Yes | All patients who received the index test went on to receive verification of their disease status using a reference standard |
| Differential verification avoided? All tests | Yes | All patients received the same reference standard regardless of the result of their index test |
| Incorporation avoided? All tests | Yes | The index test did not form part of the reference standard |
| Index test results blinded? All tests | Yes | The index tests were interpreted before and without knowledge of the reference standard results |
| Reference standard results blinded? All tests | No | The results of the index tests were known to the person interpreting the reference tests |
| Relevant clinical information? All tests | Unclear | Not reported |
| Uninterpretable results reported? All tests | Yes | The study was prospective and results were reported for all initially included participants |
| Withdrawals explained? All tests | Yes | No participants were excluded from the analysis |
| Learning curve / training reported of index test? All tests | Unclear | All of the procedures were performed by one sonologist and the findings were interpreted by two or three sonologists in consensus prior to surgery |
| Learning curve / training reported of reference standard? All tests | Unclear | Insufficient information was given to permit judgement |
| Index test criteria for a positive test result reported? All tests | Yes | The study reported the definition of a positive index test result |
<: less than >: more than IT: Index test MHz: Megahertz RS: Reference standard T: Tesla T1‐weighted: Short TR and short TE sequences T2‐weighted: Long TR and long TE sequences TE: Echo time TR: Repetition time
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adams 2010 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Al‐Shawi 2008 | Reference standard not relevant: Arthroscopy or MRI was used as reference standard |
| Aliabadi 1991 | Type of study not relevant: Narrative review |
| Aliprandi 2006 | Participants not relevant: Participants with suspected of chronic or traumatic rotator cuff tear, congenital atraumatic or traumatic glenohumeral instability, traumatic rotator cuff tear and glenohumeral instability, and “frozen shoulder” were enrolled |
| Allmann 1999 | Type of study not relevant: Technique report |
| Ardic 2006 | Reference standard not relevant: MRI was used as reference standard |
| Auethavekiat 2006 | Type of study not relevant: Case report |
| Awerbuch 2008 | Type of study not relevant: Narrative review |
| Balich 1997 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Bencardino 2010 | Type of study not relevant: Narrative review |
| Blanchard 1999a | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Blanchard 1999b | Type of study not relevant: Questionnaire study |
| Blum 1993 | Index test not relevant: Arthrographic computed tomography was used as index test |
| Boisrenoult 1999 | Type of study not relevant: Index test was not compared with reference standard(s) |
| Boorstein 1992 | Type of study not relevant: Narrative review |
| Brandt 1989 | Reference standard not relevant: Arthrography or surgery was used as reference standard |
| Brasseur 1994 | Type of study not relevant: Anatomic description |
| Brenneke 1992 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Bryant 2002 | Type of study not relevant: The purpose of this study was to determine how well the size of rotator cuff tears could be estimated noninvasively by ultrasonography and MRI and how well arthroscopy could detect the size of rotator cuff tears |
| Burk 1989 | Reference standard not relevant: Arthrography or surgery was used as reference standard |
| Chang 2002 | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Chaubal 2007 | Type of study not relevant: Narrative review |
| Chen 1996 | Target condition not relevant: The aim of the study was to determine the MRI findings that are associated with full thickness rotator cuff tears |
| Chiodi 1994 | Participants not relevant: Selective population that all participants had full thickness tears (100% of prevalence) and the study was retrospective and reported non‐consecutive recruitment |
| Chiodi 1995 | Participants not relevant: Selective population that all participants had rotator cuff tears (100% of prevalence) The study also included patients that were reported in Chiodi 1994 |
| Chiou 1999 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Chucair 2008 | Type of study not relevant: Narrative review |
| Chun 2010 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Crass 1987 | Type of study not relevant: Case report |
| Crass 1988 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Cullen 2007 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Cusmano 2000 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| D'Erme 1993 | Reference standard not relevant: Surgery or arthrography was used as reference standard |
| Davidson 2005 | Target condition not relevant: To determine the MRI criteria for predicting rotator cuff tear pattern and method of repair |
| Davis 1991 | Type of study not relevant: Technique report |
| De Muynck 1994 | Reference standard not relevant: Arthrography or arthroscopy or open surgery was used as reference standard |
| Demouy 1993 | Type of study not relevant: Narrative review |
| Deutsch 1997 | Participants not relevant: Selective population, restricted to subscapularis tendon tear (retrospective, so selected out patients with the diagnosis) |
| Dhagat 2002 | Type of study not relevant: Index test (US) was not compared with reference standard(s) |
| Dinter 2008 | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Drakeford 1990 | Participants not relevant: Asymptomatic participants were included |
| El‐Dalati 2005 | Insufficient data to be included in the meta‐analyses |
| El‐Kouba 2010 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Evancho 1988 | Reference standard not relevant: Arthroscopy or arthrography as reference standard |
| Fabis 1999a | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Fabis 1999b | Participants not relevant: The aim was to evaluate US images of rotator cuff integrity after surgical repair |
| Farin 1995 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Farin 1996a | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Farin 1996b | Participants not relevant: Selective population that all participants had full thickness tears (100% of prevalence) and the study was retrospective and reported non‐consecutive recruitment |
| Farley 1992 | Target condition not relevant: The aim of the study was to determine the MRI findings that are associated with full thickness rotator cuff tears |
| Ferrari 2002 | Participants not relevant: Selective population that all participants had full thickness tears (100% of prevalence) and the study reported non‐consecutive recruitment |
| Ferri 2005 | Target condition not relevant: The aim of the study is to assess the accuracy of the Crass and modified Crass positions |
| Flannigan 1990 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Fotiadou 2008 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Frei 2008 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Fritz 1992 | Type of study not relevant: Letter |
| Furtschegger 1988 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Girard 1995 | Type of study not relevant: Narrative review |
| Goergen 1996 | Type of study not relevant: Technique report |
| Goldberg 2003 | Reference standard not relevant: Arthrography findings and clinical examination were used as reference standard |
| Hedtmann 2002 | Type of study not relevant: Narrative review |
| Heijne 2004 | Type of study not relevant: Editorial letter |
| Herold 2006 | Participants not relevant: A history of trauma was reported in 17 (33%) of 51 patients Fourteen (27%) of 51 patients had previous shoulder dislocation, and 36 (71%) presented with clinical signs of impingement |
| Herzog 1997 | Type of study not relevant: Narrative review |
| Herzog 1998 | Type of study not relevant: Narrative review |
| Hodler 1987 | Reference standard not relevant: Arthrography was used as reference standard |
| Hodler 1988 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Hodler 1992 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Hollister 1995 | Target condition not relevant: The aim of the study was to determine the association between bursal and joint effusion (index tests findings) that are associated with rotator cuff tears |
| Homsi 1989 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Horii 1998 | Participants not relevant: Selective population that all participants had full thickness tears (100% of prevalence) and the study was retrospective and reported non‐consecutive recruitment |
| Iannotti 1991 | Participants not relevant: Asymptomatic participants were enrolled |
| Imhoff 1992 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Imhoff 1993 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Imhoff 1996 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Iovane 2001 | Participants not relevant: Selective population that all participants had full thickness tears (100% of prevalence) and the study was retrospective and reported non‐consecutive recruitment |
| Iyengar 2010 | Type of study not relevant: Technique report |
| Jacobson 2003 | Type of study not relevant: Narrative review |
| Jacobson 2004 | Target condition not relevant: The aim of the study was to determine which US signs are important for the diagnosis of a surgically identifiable supraspinatus tendon tear |
| Jaovisidha 1999 | Type of study not relevant: The time elapsed between the index and reference tests was during a 26‐month follow‐up |
| Jeyam 2008 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Jung 2009 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Jung 2010 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Kaneko 1994 | Participants not relevant: A control group without suspected of rotator cuff tears was included |
| Kautzner 2008 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Kelly 2009 | Type of study not relevant: Diagnostic Test Accuracy review |
| Kerkovsky 2008 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Kluger 2003 | Target condition not relevant: The aim of this study was to evaluate the accuracy of MRA and US in millimetres for both width and retraction of full‐thickness rotator cuff tears, and not to detect the tears |
| Kneeland 1987 | Reference standard not relevant: Arthroscopy or arthrography was used as reference standard |
| Kujat 1986 | Type of study not relevant: Technique report |
| Kurol 1991 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Lawson 1991 | Type of study not relevant: Narrative review |
| Lee 2002 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Lipman 1992 | Type of study not relevant: Letter |
| Loew 2000 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Lopez 2007 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Low 1998 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Lucas 1991 | Type of study not relevant: Narrative review |
| Mack 1988 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Magee 2003a | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Magee 2003b | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Magee 2006 | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Magee 2007 | Participants not relevant: Participants with clinical diagnosis of pain or instability or both were enrolled |
| Magee 2009 | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Malvestiti 1997 | Reference standard not relevant: Arthroscopy or MRI or arthrography was used as reference standard |
| Martin 2008 | Type of study not relevant: Technique report |
| Masaoka 1999 | Participants not relevant: Participants who underwent index test after surgery were enrolled |
| Masciocchi 1989 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Meister 2004 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Mendieta‐Sevilla 2009 | Reference standard not relevant: Surgery or MRI or arthrography or rehabilitation was used as reference standard |
| Merl 1996 | Type of study not relevant: Narrative review |
| Middleton 1993 | Type of study not relevant: Letter |
| Miller 2008 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Montrucchio 1997 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Monu 1994 | Participants not relevant: The study included selective participants without rotator cuff tears |
| Moosmayer 2005 | Participants not relevant: Participants with other shoulder complaints, including symptoms from the long head of the biceps muscle were enrolled |
| Moosmayer 2007 | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Morrison 1990 | Reference standard not relevant: Arthrography or arthroscopy or open surgery was used as reference standard |
| Naqvi 2009 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Narbona 2007 | Target condition not relevant: The aim of this study was to detect SLAP lesion in patients with rotator cuff tears |
| Needell 1997 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Nelson 1991 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Nogueira‐Barbosa 2002 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Norregaard 2002 | Participants not relevant: Participants with clinical suspicion of labral or rotator cuff lesion were enrolled |
| Oh 2009 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Oh 2010 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Ostlere 1997 | Type of study not relevant: Narrative review |
| Ozcakar 2005 | Type of study not relevant: Letter |
| Paavolainen 1994 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Palmer 1993 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Palmer 1994 | Type of study not relevant: Narrative review |
| Parsa 1997 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Pattee 1988 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Patten 1994 | Reference standard not relevant: Arthroscopy, arthrography and non‐surgical therapy were used as reference standard |
| Peetrons 1986 | Type of study not relevant: Index test was not compared with reference standard(s). |
| Pfirrmann 1999 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Pfirrmann 2004 | Participants not relevant: Asymptomatic participants were included |
| Pigeau 1992 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Poey 1990 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Porcellini 1994 | Reference standard not relevant: Surgery or arthrography was used as reference standard |
| Prendergast 1992 | Type of study not relevant: Narrative review |
| Quinn 1995 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Rafii 1990 | Participants not relevant: Asymptomatic participants were included |
| Read 1998 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Recht 1993 | Type of study not relevant: Narrative review. |
| Recht 1994 | Type of study not relevant: Narrative review. |
| Reinus 1995 | Participants not relevant: Participants with shoulder pain; however, it was unclear if all participants had suspected of having rotator cuff tears. |
| Roberts 1998 | Reference standard not relevant: MRI or arthrography was used as reference standard. |
| Roberts 2001 | Participants not relevant: Participants with other shoulder complaints, including adhesive capsulitis and osteoarthritis were enrolled. |
| Robertson 1995 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Rouaud 1989 | Type of study not relevant: Index test (US) was not compared with reference standard(s) |
| Rubin 1997 | Type of study not relevant: Letter |
| Rutten 2010a | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Rutten 2010b | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears. |
| Sahin‐Akyar 1998 | Participants not relevant: Participants with rotator cuff tear and other disorders were enrolled |
| Sartoris 1992 | Type of study not relevant: Narrative review |
| Sasaki 1990 | Participants not relevant: Asymptomatic participants were included |
| Schneider 2003 | Insufficient data to be included in the meta‐analyses |
| Schreinemachers 2009 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Schultz 1994 | Type of study not relevant: Letter |
| Seeger 1988 | Type of study not relevant: The study did not describe the comparison between the index test and the reference standard |
| Sheah 2009 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Shellock 1996 | Type of study not relevant: Narrative review |
| Shellock 2001 | Participants not relevant: The authors reported that participants with suspected of ‘shoulder pathology’ were included, probable included participants with suspected of rotator cuff tears and shoulder instability |
| Shiv 1990 | Type of study not relevant: Index test (US) was not compared with reference standard(s) |
| Singer 1995 | Type of study not relevant: Index test was not compared with reference standard(s) |
| Singson 1996 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Skib 1998 | Type of study not relevant: Letter |
| Soble 1989 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Sonin 1996 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Sonnabend 1997 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Soto Araiza 1998 | Reference standard not relevant: Surgery or MRI was used as reference standard |
| Steinbach 2000 | Type of study not relevant: Narrative review |
| Strauss 1998 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Suder 1994 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Sunde 2001 | Type of study not relevant: Letter |
| Sunde 2008 | Type of study not relevant: Letter |
| Taboury 1995 | Participants not relevant: Selective population that all participants had full thickness tears (100% of prevalence) and the study was retrospective and reported non‐consecutive recruitment |
| Takagishi 1993 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Takagishi 1996 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Teefey 2000 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Teefey 2009 | Type of study not relevant: Case report |
| Theodoropoulos 2010 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Tirman 1994 | Participants not relevant: Selective population of five professional throwing athletes were evaluated; and, these participants had other shoulder complaints, including instability |
| Torstensen 1999 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Touzard 1991 | Reference standard not relevant: Surgery or arthrography was used as reference standard |
| Toyoda 2005 | Participants not relevant: Selective population that all participants had full thickness tears (100% of prevalence) and the study was retrospective and reported non‐consecutive recruitment |
| Traughber 1992 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Traughber 1996 | Type of study not relevant: Letter |
| Traughber 2006 | Type of study not relevant: Letter |
| Tuite 1994 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Tuite 1995 | Participants not relevant: It was unclear if all participants were suspected of having rotator cuff tears; furthermore, the study reported that part of participants of Tuite 1994 were included Thus, participants with other shoulder complaints, including instability were enrolled |
| Tuite 1998 | Participants not relevant: It was unclear if all participants were suspected of having rotator cuff tears; furthermore, the study reported that part of participants of Tuite 1994 were included Thus, participants with other shoulder complaints, including instability were enrolled |
| Tuite 2001 | Participants not relevant: It was unclear if all participants were suspected of having rotator cuff tears; probable the study included participants with shoulder instability |
| Turrin 1997 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Vahlensieck 2001 | Type of study not relevant: Letter |
| Van Dyck 2009 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Van Holsbeeck 1995 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Van Moppes 1995 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Vander Maren 1995 | Participants not relevant: Participants with shoulder pain were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Vanecek 2000 | Type of study not relevant: Narrative review |
| Waldt 2007 | Participants not relevant: Participants with symptomatic shoulder; however, it was unclear if all participants were suspected of having rotator cuff tears |
| Wallny 1999 | Type of study not relevant: Technique report The study described an index to improve the accuracy of diagnosis of chronic rotator cuff tears |
| Walz 2007 | Target condition not relevant: The aim of this study was a description of delamination tears of the supraspinatus, subscapularis, infraspinatus or teres minor tendons, as well as for mention of partial or full thickness tears |
| Wang 1994 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Weinstabl 1988 | Type of study not relevant: Technique report |
| Wiener 1993 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Wilson 1994 | Type of study not relevant: Letter |
| Wnorowski 1997 | Participants not relevant: Participants with shoulder problems were enrolled; however, it was unclear if all participants were suspected of having rotator cuff tears The study reported that in the majority of the participants the primary diagnosis was unclear after the clinical evaluation |
| Wu 2003 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Yagci 2001 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Yamakawa 2001 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Yeh 2003 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
| Yeu 1994 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Zehetgruber 2002 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Ziegler 2004 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Zlatkin 1989 | This was a retrospective study with a possible risk of spectrum and verification bias |
| Zlatkin 2004 | Participants not relevant: Participants with other shoulder complaints, including instability were enrolled |
Characteristics of studies awaiting classification [ordered by study ID]
Engebretsen 1994.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 41 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 25 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ Norwegian article The information was collected from titles and abstracts that were reported in English |
Farin 1990.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 301 participants Number of participants enrolled IT and RS: ‐ US and surgery: 66 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Guo 2000.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 53 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 53 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Open surgery or arthroscopy |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ Chinese article The information was collected from titles and abstracts that were reported in English |
Habermeyer 1984.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 49 participants Number of participants enrolled IT and RS: ‐ US and surgery: 17 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears Reference standard(s): Open surgery |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Hedtmann 1995.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 4172 participants Number of participants enrolled IT and RS: ‐ US and surgery: 1227 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears Reference standard(s): Open surgery |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Heininger‐Biner 2000.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 88 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 88 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Kayser 2005.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 239 participants Number of participants enrolled IT and RS: ‐ US and surgery: 239 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Kenn 2000.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 40 participants Number of participants enrolled IT and RS: ‐ US and surgery: 40 participants ‐ MRI and surgery: 40 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI and US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Kumagai 1991.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 30 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 30 participants ‐ MRA and surgery: 30 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI and MRA |
| Follow‐up | |
| Notes | Awaiting translation ‐ Japanese article The information was collected from titles and abstracts that were reported in English |
Kumagai 1992.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 115 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: unclear |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ Japanese article The information was collected from titles and abstracts that were reported in English |
Kumagai 1995.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 94 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 21 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of full thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ Japanese article |
Labanauskaite 2002.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 31 participants Number of participants enrolled IT and RS: ‐ US and surgery: 31 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ Lithuanian article The information was collected from titles and abstracts that were reported in English |
Manych 2007.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 275 participants Number of participants enrolled IT and RS: ‐ MRA and surgery: 197 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy |
| Index and comparator tests | Index test(s): MRA |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Nagamori 1995.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 45 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 45 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ Japanese article The information was collected from titles and abstracts that were reported in English |
Qu 2008.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 57 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 57 participants ‐ MRA and surgery: 57 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy |
| Index and comparator tests | Index test(s): MRI and MRA |
| Follow‐up | |
| Notes | Awaiting translation ‐ Chinese article The information was collected from titles and abstracts that were reported in English |
Rudolph 2000.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 63 participants Number of participants enrolled IT and RS: ‐ MRA and surgery: 32 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Sakuragi 1989.
| Clinical features and settings | |
| Participants |
Number of participants eligible: unclear number of participants Number of participants enrolled IT and RS: ‐ US and surgery: unclear number of participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ Japanese article The information was collected from titles and abstracts that were reported in English |
Sasaki 1991.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 30 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 15 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ Japanese article The information was collected from titles and abstracts that were reported in English |
Schedel 1990.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 30 participants Number of participants enrolled IT and RS: ‐ US and surgery: unclear number of participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Schroder 2003.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 80 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 80 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Open surgery or shoulder arthroscopy |
| Index and comparator tests | Index test(s): MRI |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Sell 1992.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 37 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: unclear number of participants ‐ US and surgery: unclear number of participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Open surgery or shoulder arthroscopy |
| Index and comparator tests | Index test(s): MRI and US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Sperner 1993.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 375 participants Number of participants enrolled IT and RS: ‐ US and surgery: 375 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Open surgery |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Vahlensieck 1996.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 25 participants Number of participants enrolled IT and RS: ‐ MRI and surgery: 25 participants ‐ US and surgery: 25 participants ‐ MRA and surgery: 25 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy |
| Index and comparator tests | Index test(s): MRI, US and MRA |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected by titles and abstracts that were reported in English |
Wallny 2000.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 25 participants Number of participants enrolled IT and RS: ‐ US and surgery: 25 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Surgery Unclear whether arthroscopy or open surgery |
| Index and comparator tests | Index test(s): US |
| Follow‐up | |
| Notes | Awaiting translation ‐ German article The information was collected from titles and abstracts that were reported in English |
Wang 2009.
| Clinical features and settings | |
| Participants |
Number of participants eligible: 40 participants Number of participants enrolled IT and RS: ‐ MRA and surgery: 40 participants |
| Study design | |
| Target condition and reference standard(s) |
Target conditions: Presence of any rotator cuff tears, full thickness tears and partial thickness tears Reference standard(s): Shoulder arthroscopy |
| Index and comparator tests | Index test(s): MRA |
| Follow‐up | |
| Notes | Awaiting translation ‐ Chinese article The information was collected from titles and abstracts that were reported in English |
IT: index test RS: reference standard MRI: magnetic resonance imaging MRA: magnetic resonance arthrography US: ultrasound
Differences between protocol and review
We only included studies of participants suspected of having rotator cuff tears. Studies that reported results of people who had been previously diagnosed with, or suspected of having, other specific shoulder diagnoses were excluded. If it was unclear whether or not all participants were suspected of having rotator cuff tears, we also excluded these studies
Inasmuch as there is no set time point beyond which it is known that rotator cuff tears progress, we accepted studies in which the time between the index test and the reference standard test was up to a year (rather than six months as specified in the protocol).
We included the MEDION database in our search strategy.
We restricted our analyses to prospective studies and excluded retrospective studies because of the high risk of spectrum and verification biases in these studies.
We made an amendment in the assessment of methodological quality – item seven (index test results blinded). We removed “if the study was retrospective” as a reason to say No because we included only prospective studies.
We made an amendment in the assessment of methodological quality ‐ item eight (reference standard results blinded). We excluded “if the study was retrospective” as a reason to say No because it was covered by the first part of the sentence.
We included in the assessment of methodological quality table an additional generic quality item assessing whether or not the criteria for a positive index test result was reported.
We used the bivariate model for meta‐analysis instead of the hierarchical summary ROC (HSROC) model. Given the available information, we assumed a common threshold was applicable but with heterogeneity around this common threshold due to variation in interpretation in practice. Therefore we consider the bivariate model and the estimation of summary points (with 95% confidence regions) appropriate for summarising the results of the review.
We conducted sensitivity analyses to examine the effect of unit of analysis.
Contributions of authors
All authors contributed to the development of the review and commented on and approved the final version. The guarantor of this review is Mario Lenza.
Sources of support
Internal sources
Universidade Federal de São Paulo, Brazil.
-
The Parker Institute, Denmark.
The Parker Institute: Musculoskeletal Statistics Unit is supported by grants from The Oak Foundation
Teesside University, UK.
-
Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Monash University, Australia.
In kind support
-
Cabrini Institute, Cabrini Hospital, Malvern, Victoria, Australia.
In kind support
External sources
No sources of support supplied
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
De Candia 2002 {published data only}
- Candia A, Doratiotto S, Paschina E, Segatto E, Pelizzo F, Bazzocchi M. Real‐time compound sonography of the rotator‐cuff: evaluation of artefact reduction and image definition. Radiologia Medica 2003;105(4):308‐14. [PubMed] [Google Scholar]
- Candia A, Doratiotto S, Pelizzo F, Paschina E, Bazzocchi M. Real time compound ultrasound of the shoulder. Radiology and Oncology 2002;36(4):319‐25,+336. [Google Scholar]
Della Sala 1996 {published data only}
- Della Sala SW, Bianchini G. Magnetic resonance in the study of the painful shoulder. The surgical comparison in 30 consecutive cases [La Risonanza Magnetica nello studio della spalla dolorosa. Raffronto chirurgico in 30 casi consecutivi]. Radiologia Medica 1996;91(4):348‐55. [PubMed] [Google Scholar]
Gagey 1993 {published data only}
- Gagey N, Desmoineaux P, Gagey O, Idy‐Peretti I, Mazas F. Contribution of MRI to the preoperative evaluation of rotator cuff tears [Apport de l'IRM dans le bilan pre‐chirurgical des lesions de la coiffe des rotateurs]. Revue de Chirurgie Orthopedique et Reparatrice de l Appareil Moteur 1991;77(8):521‐9. [PubMed] [Google Scholar]
- Gagey N, Desmoineaux P, Gagey O, Idy‐Peretti I, Mazas F. MRI in the pre‐operative evaluation of lesions of the rotator cuff [Apport de l'IRM dans le bilan pre‐chirurgical des lesions de la coiffe des rotateurs]. Journal de Radiologie 1993;74(1):39‐46. [PubMed] [Google Scholar]
Iannotti 2005 {published data only}
- Iannotti JP, Ciccone J, Buss DD, Visotsky JL, Mascha E, Cotman K, et al. Accuracy of office‐based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. Journal of Bone and Joint Surgery. American Volume 2005;87(6):1305‐11. [DOI] [PubMed] [Google Scholar]
Kang 2009 {published data only}
- Kang CH, Kim SS, Kim JH, Chung KB, Kim YH, Oh YW, et al. Supraspinatus tendon tears: Comparison of 3D US and MR arthrography with surgical correlation. Skeletal Radiology 2009;38(11):1063‐9. [DOI] [PubMed] [Google Scholar]
Lambert 2009 {published data only}
- Lambert A, Loffroy R, Guiu B, Mejean N, Lerais JM, Cercueil JP, et al. Rotator cuff tears: value of 3.0T MRI [Perforations de la coiffe des rotateurs: intérêt de l’IRM 3,0T]. Journal de Radiologie 2009;90(5 Pt 1):583‐8. [DOI] [PubMed] [Google Scholar]
Martin‐Hervas 2001 {published data only}
- Martin‐Hervas C, Romero J, Navas‐Acien A, Reboiras JJ, Munuera L. Ultrasonographic and magnetic resonance images of rotator cuff lesions compared with arthroscopy or open surgery findings. Journal of Shoulder and Elbow Surgery 2001;10(5):410‐5. [DOI] [PubMed] [Google Scholar]
Milosavljevic 2005 {published data only}
- Milosavljevic J, Elvin A, Rahme H. Ultrasonography of the rotator cuff: a comparison with arthroscopy in one‐hundred‐and‐ninety consecutive cases. Acta Radiologica 2005;46(8):858‐65. [DOI] [PubMed] [Google Scholar]
Misamore 1991 {published data only}
- Misamore GW, Woodward C. Evaluation of degenerative lesions of the rotator cuff. A comparison of arthrography and ultrasonography. Journal of Bone and Joint Surgery. American Volume 1991;73(5):704‐6. [PubMed] [Google Scholar]
Mohtadi 2004 {published data only}
- Mohtadi NG, Vellet AD, Clark ML, Hollinshead RM, Sasyniuk TM, Fick GH, et al. A prospective, double‐blind comparison of magnetic resonance imaging and arthroscopy in the evaluation of patients presenting with shoulder pain. Journal of Shoulder and Elbow Surgery 2004;13(3):258‐65. [DOI] [PubMed] [Google Scholar]
Nicoletti 1994 {published data only}
- Nicoletti SJ, Moura L. Rotator cuff disease: do ultrasonography and pneumoarthrography increase diagnostic reliability of the physical examination for supraspinatus lesion detection? [Lesöes do manguito rotator: a ultra‐sonografia e a pneumoartrografia aumentam a capacidade diagnóstica do exame físico, para a detecçäo das roturas do supra‐espinhal?]. Revista Brasileira de Ortopedia 1994;29(9):656‐60. [Google Scholar]
Sipola 2010 {published data only}
- Sipola P, Niemitukia L, Kroger H, Hofling I, Vaatainen U. Detection and quantification of rotator cuff tears with ultrasonography and magnetic resonance imaging ‐ A prospective study in 77 consecutive patients with a surgical reference. Ultrasound in Medicine and Biology 2010;36(12):1981‐9. [DOI] [PubMed] [Google Scholar]
Stetson 2005 {published data only}
- Stetson WB, Phillips T, Deutsch A. The use of magnetic resonance arthrography to detect partial‐thickness rotator cuff tears. Journal of Bone and Joint Surgery. American Volume 2005;87(Suppl 2):81‐8. [DOI] [PubMed] [Google Scholar]
Swen 1998 {published data only}
- Swen WA, Jacobs JW, Neve WC, Bal D, Bijlsma JW. Is sonography performed by the rheumatologist as useful as arthrography executed by the radiologist for the assessment of full thickness rotator cuff tears?. Journal of Rheumatology 1998;25(9):1800‐6. [PubMed] [Google Scholar]
Swen 1999 {published data only}
- Swen WA, Jacobs JW, Algra PR, Manoliu RA, Rijkmans J, Willems WJ, et al. Sonography and magnetic resonance imaging equivalent for the assessment of full‐thickness rotator cuff tears. Arthritis and Rheumatism 1999;42(10):2231‐8. [DOI] [PubMed] [Google Scholar]
Taboury 1992 {published data only}
- Taboury J. Ultrasonography of the shoulder: diagnosis of rupture of tendons of the rotator muscles [Echographie de l'epaule. Diagnostic de rupture des tendons des muscles rotateurs]. Annales de Radiologie 1992;35(3):133‐40. [PubMed] [Google Scholar]
Teefey 2004 {published data only}
- Teefey SA, Middleton WD, Payne WT, Yamaguchi K. Detection and measurement of rotator cuff tears with sonography: Analysis of diagnostic errors. American Journal of Roentgenology 2005;184(6):1768‐73. [DOI] [PubMed] [Google Scholar]
- Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears: comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy‐one consecutive cases. Journal of Bone and Joint Surgery. American Volume 2004;86(4):708‐16. [PubMed] [Google Scholar]
Venu 2002 {published data only}
- Venu KM, Howlett DC, Garikipati R, Anderson HJ, Bonnici AV. Evaluation of the symptomatic supraspinatus tendon ‐ A comparison of ultrasound and arthroscopy. Radiography 2002;8(4):235‐40. [Google Scholar]
Wallny 2001 {published data only}
- Wallny TA, Schild RL, Schulze Bertelsbeck D, Hansmann ME, Kraft CN. Three‐dimensional ultrasonography in the diagnosis of rotator cuff lesions. Ultrasound in Medicine and Biology 2001;27(6):745‐9. [DOI] [PubMed] [Google Scholar]
Yen 2004 {published data only}
- Yen CH, Chiou HJ, Chou YH, Hsu CC, Wu JJ, Ma HL, et al. Six surgery‐correlated sonographic signs for rotator cuff tears: Emphasis on partial‐thickness tear. Clinical Imaging 2004;28(1):69‐76. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adams 2010 {published data only}
- Adams CR, Schoolfield JD, Burkhart SS. Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy 2010;26(11):1427‐33. [DOI] [PubMed] [Google Scholar]
Aliabadi 1991 {published data only}
- Aliabadi P. Imaging evaluation of rotator cuff tears. Rheumatic Disease Clinics of North America 1991;17(3):795‐7. [PubMed] [Google Scholar]
Aliprandi 2006 {published data only}
- Aliprandi A, Fausto A, Quarenghi M, Modestino S, Randelli P, Sardanelli F. One‐shot CT and MR arthrography of the shoulder with a mixture of iodinated and paramagnetic contrast agents using arthroscopy as a gold standard [Artro‐TC e artro‐RM di spalla con unica iniezione di una mistura di mezzi di contrasto iodato e paramagnetico. Valutazione dei risultati con gold standard artroscopico]. Radiologia Medica 2006;111(1):53‐60. [DOI] [PubMed] [Google Scholar]
Allmann 1999 {published data only}
- Allmann KH, Schafer O, Hauer M, Winterer J, Laubenberger J, Reichelt A, et al. Indirect MR arthrography of the unexercised glenohumeral joint in patients with rotator cuff tears. Investigative Radiology 1999;34(6):435‐40. [DOI] [PubMed] [Google Scholar]
Al‐Shawi 2008 {published data only}
- Al‐Shawi A, Badge R, Bunker T. The detection of full thickness rotator cuff tears using ultrasound. Journal of Bone and Joint Surgery. British Volume 2008;90(7):889‐92. [DOI] [PubMed] [Google Scholar]
Ardic 2006 {published data only}
- Ardic F, Kahraman Y, Kacar M, Kahraman MC, Findikoglu G, Yorgancioglu ZR. Shoulder impingement syndrome: Relationships between clinical, functional, and radiologic findings. American Journal of Physical Medicine and Rehabilitation 2006;85(1):53‐60. [DOI] [PubMed] [Google Scholar]
Auethavekiat 2006 {published data only}
- Auethavekiat P, Michet CJ Jr. Images in clinical medicine. Rotator‐cuff tear. New England Journal of Medicine 2006;354(19):e20. [DOI] [PubMed] [Google Scholar]
Awerbuch 2008 {published data only}
- Awerbuch MS. The clinical utility of ultrasonography for rotator cuff disease, shoulder impingement syndrome and subacromial bursitis. Medical Journal of Australia 2008;188(1):50‐3. [DOI] [PubMed] [Google Scholar]
Balich 1997 {published data only}
- Balich SM, Sheley RC, Brown TR, Sauser DD, Quinn SF. MR imaging of the rotator cuff tendon: Interobserver agreement and analysis of interpretive errors. Radiology 1997;204(1):191‐4. [DOI] [PubMed] [Google Scholar]
Bencardino 2010 {published data only}
- Bencardino JT, Beltran LS. Pain related to rotator cuff abnormalities: MRI findings without clinical significance. Journal of Magnetic Resonance Imaging 2010;31(6):1286‐99. [DOI] [PubMed] [Google Scholar]
Blanchard 1999a {published data only}
- Blanchard TK, Bearcroft PW, Constant CR, Griffin DR, Dixon AK. Diagnostic and therapeutic impact of MRI and arthrography in the investigation of full‐thickness rotator cuff tears. European Radiology 1999;9(4):638‐42. [DOI] [PubMed] [Google Scholar]
Blanchard 1999b {published data only}
- Blanchard TK, Bearcroft PW, Maibaum A, Hazelman BL, Sharma S, Dixon AK. Magnetic resonance imaging or arthrography for shoulder problems: A randomised study. European Journal of Radiology 1999;30(1):5‐10. [DOI] [PubMed] [Google Scholar]
Blum 1993 {published data only}
- Blum A, Boyer B, Regent D, Simon JM, Claudon M, Mole D. Direct coronal view of the shoulder with arthrographic CT. Radiology 1993;188(3):677‐81. [DOI] [PubMed] [Google Scholar]
Boisrenoult 1999 {published data only}
- Boisrenoult P, Gagey O. Second consultation and MR imaging diagnosis of full‐thickness tears of the rotator cuff, including subscapularis [Les ruptures transfixiantes de la coiffe des rotateurs. Deuxième consultation: Diagnostic lésionnel par l'imagerie]. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur 1999;85(SUPPL. II):97‐9. [Google Scholar]
Boorstein 1992 {published data only}
- Boorstein JM, Kneeland JB, Dalinka MK, Iannotti JP, Suh JS. Magnetic resonance imaging of the shoulder. Current Problems in Diagnostic Radiology 1992;21(1):5‐27. [DOI] [PubMed] [Google Scholar]
Brandt 1989 {published data only}
- Brandt TD, Cardone BW, Grant TH, Post M, Weiss CA. Rotator cuff sonography: a reassessment. Radiology 1989;173(2):323‐7. [DOI] [PubMed] [Google Scholar]
Brasseur 1994 {published data only}
- Brasseur JL, Lazennec JY, Tardieu M, Richard O, Roger B, Grenier P. Dynamic ultrasonography of the shoulder for tears of the rotator cuff [Echographie dynamique de l'épaule dans le conflit antéro‐supérieur]. Revue d'Imagerie Medicale 1994;6(11):629‐31. [Google Scholar]
Brenneke 1992 {published data only}
- Brenneke SL, Morgan CJ. Evaluation of ultrasonography as a diagnostic technique in the assessment of rotator cuff tendon tears. American Journal of Sports Medicine 1992;20(3):287‐9. [DOI] [PubMed] [Google Scholar]
Bryant 2002 {published data only}
- Bryant L, Shnier R, Bryant C, Murrell GA. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. Journal of Shoulder and Elbow Surgery 2002;11(3):219‐24. [DOI] [PubMed] [Google Scholar]
Burk 1989 {published data only}
- Burk DL Jr, Karasick D, Kurtz AB, Mitchell DG, Rifkin MD, Miller CL, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. American Journal of Roentgenology 1989;153(1):87‐92. [DOI] [PubMed] [Google Scholar]
Chang 2002 {published data only}
- Chang CY, Wang SF, Chiou HJ, Ma HL, Sun YC, Wu HD. Comparison of shoulder ultrasound and MR imaging in diagnosing full‐thickness rotator cuff tears. Clinical Imaging 2002;26(1):50‐4. [DOI] [PubMed] [Google Scholar]
Chaubal 2007 {published data only}
- Chaubal NG. Ultrasonography of shoulder [rotator cuff]. Indian Journal of Radiology and Imaging 2007;17(3):209‐14. [Google Scholar]
Chen 1996 {published data only}
- Chen JD, Jim YF, Chang CY. MR imaging of rotator cuff impingement: correlation with full‐thickness rotator cuff tear. Zhonghua Yi Xue Za Zhi (Taipei) 1996;58(3):198‐204. [PubMed] [Google Scholar]
Chiodi 1994 {published data only}
- Chiodi E, Morini G. Lesions of the rotatory cuff: diagnostic validity of echography. Surgical findings [Le lesioni della cuffia dei rotatori: validita diagnostica dell'ecografia al riscontro chirurgico]. Radiologia Medica 1994;88(6):733‐5. [PubMed] [Google Scholar]
Chiodi 1995 {published data only}
- Chiodi E, Morini G. Chronic shoulder pain. Ultrasonography versus surgery [Spalla dolorosa cronica. Ecografia e chirurgia a confronto]. Radiologia Medica 1995;89(5):600‐3. [PubMed] [Google Scholar]
Chiou 1999 {published data only}
- Chiou HJ, Chou YH, Wu JJ, Hsu CC, Tiu CM, Chang CY. High‐resolution ultrasonography of the musculoskeletal system: Analysis of 369 cases. Journal of Medical Ultrasound 1999;7(4):212‐8. [Google Scholar]
Chucair 2008 {published data only}
- Chucair AE. Utility of ultrasound in the study of the musculotendinous pathology of the upper limb: comparison with other methods: part 2 [Ultrasonografía en el estudio de la patología musculotendinosa del miembro superior: comparación con otros métodos: parte 2]. Revista Argentina de Ultrasonido 2008;7(2):111‐20. [Google Scholar]
Chun 2010 {published data only}
- Chun KA, Kim MS, Kim YJ. Comparisons of the various partial‐thickness rotator cuff tears on MR arthrography and arthroscopic correlation. Korean Journal of Radiology 2010;11(5):528‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crass 1987 {published data only}
- Crass JR, Craig EV, Feinberg SB. The hyperextended internal rotation view in rotator cuff ultrasonography. Journal of Clinical Ultrasound 1987;15(6):416‐20. [DOI] [PubMed] [Google Scholar]
Crass 1988 {published data only}
- Crass JR, Craig EV, Bretzke C, Feinberg SB. Ultrasonography of the rotator cuff. Radiographics 1985;5(6):941‐53. [DOI] [PubMed] [Google Scholar]
- Crass JR, Craig EV, Feinberg SB. Ultrasonography of rotator cuff tears: A review of 500 diagnostic studies. Journal of Clinical Ultrasound 1988;16(5):313‐27. [DOI] [PubMed] [Google Scholar]
- Crass JR, Craig EV, Thompson RC, Feinberg SB. Ultrasonography of the rotator cuff: Surgical correlation. Journal of Clinical Ultrasound 1984;12(8):487‐91. [DOI] [PubMed] [Google Scholar]
Cullen 2007 {published data only}
- Cullen DM, Breidahl WH, Janes GC. Diagnostic accuracy of shoulder ultrasound performed by a single operator. Australasian Radiology 2007;51(3):226‐9. [DOI] [PubMed] [Google Scholar]
Cusmano 2000 {published data only}
- Cusmano F, Pedrazzini M, Uccelli M, Ferrozzi F, Bassi S, Corradi M, et al. Rotator cuff rupture. Diagnostic imaging [Rottura della cuffia dei rotatori. Diagnostica per immagini]. Acta Biomed Ateneo Parmense 2000;71(6):217‐26. [PubMed] [Google Scholar]
D'Erme 1993 {published data only}
- D'Erme M, Cupis V, Maria M, Barbiera F, Maceroni P, Lasagni MP. Echography, magnetic resonance and double‐contrast arthrography of the rotator cuff. A prospective study in 30 patients [L'ecografia, la risonanza magnetica e l'artrografia con doppio mezzo di contrasto della cuffia dei rotatori. Studio prospettico in 30 pazienti]. Radiologia Medica 1993;86(1‐2):72‐80. [PubMed] [Google Scholar]
Davidson 2005 {published data only}
- Davidson JF, Burkhart SS, Richards DP, Campbell SE. Use of preoperative magnetic resonance imaging to predict rotator cuff tear pattern and method of repair. Arthroscopy 2005;21(12):1428. [DOI] [PubMed] [Google Scholar]
Davis 1991 {published data only}
- Davis SJ, Teresi LM, Bradley WG, Ressler JA, Eto RT. Effect of arm rotation on MR imaging of the rotator cuff. Radiology 1991;181(1):265‐8. [DOI] [PubMed] [Google Scholar]
Demouy 1993 {published data only}
- Demouy EH, Kaneko K. Rotator cuff disease: The role of plain film and MRI. Postgraduate Radiology 1993;13(4):223‐31. [Google Scholar]
De Muynck 1994 {published data only}
- Muynck M. Sonography in the diagnosis of rotator cuff ruptures. European Journal of Physical Medicine and Rehabilitation 1994;4(4):130‐3. [Google Scholar]
Deutsch 1997 {published data only}
- Deutsch A, Altchek DW, Veltri DM, Potter HG, Warren RF. Traumatic tears of the subscapularis tendon: Clinical diagnosis, magnetic resonance imaging findings, and operative treatment. American Journal of Sports Medicine 1997;25(1):13‐22. [DOI] [PubMed] [Google Scholar]
Dhagat 2002 {published data only}
- Dhagat P, Singh H, Sharma V. Spectrum of rotator cuff injuries on ultrasound. Asian Oceanian Journal of Radiology 2002;7(2):99‐103. [Google Scholar]
Dinter 2008 {published data only}
- Dinter DJ, Lehmann LJ. Questions related with our inclusion criteria [personal communication]. Email to: D Dinter and L Lehmann 10 July 2011.
- Dinter DJ, Martetschlager F, Busing KA, Schonberg SO, Scharf HP, Lehmann LJ. Shoulder injuries in overhead athletes: utility of MR arthrography [Schulterverletzungen des Uberkopfsportlers: Wertigkeit der MR‐Arthrografie]. Sportverletz Sportschaden 2008;22(3):146‐52. [DOI] [PubMed] [Google Scholar]
Drakeford 1990 {published data only}
- Drakeford MK, Quinn MJ, Simpson SL, Pettine KA. A comparative study of ultrasonography and arthrography in evaluation of the rotator cuff. Clinical Orthopaedics and Related Research 1990;(253):118‐22. [PubMed] [Google Scholar]
El‐Dalati 2005 {published data only}
- El‐Dalati G, Castellarin G, Martone E, Ricci M, Vecchini E, Caffarri S, et al. Standard sonography and arthrosonography in the study of rotator cuff tears. Radiologia Medica 2005;110(5‐6):616‐22. [PubMed] [Google Scholar]
El‐Kouba 2010 {published data only}
- El‐Kouba G, Huber TA, Freitas JRW, Steglich V, Ayzemberg H, AMS. Comparison of complementary exams in the diagnosis of rotator cuff injuries [Comparação dos exames complementares no diagnóstico das lesões do manguito rotador]. Revista Brasileira de Ortopedia 2010;45(5):418‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Evancho 1988 {published data only}
- Evancho AM, Stiles RG, Fajman WA, Flower SP, Macha T, Brunner MC, et al. MR imaging diagnosis of rotator cuff tears. American Journal of Roentgenology 1988;151(4):751‐4. [DOI] [PubMed] [Google Scholar]
Fabis 1999a {published data only}
- Fabis J, Synder M. The sensitivity and specificity of sonographic examination in detection of rotator cuff tear [Czulosc i swoistosc badania ultrasonograficznego w diagnostyce uszkodzenia pierscienia rotatorow]. Chirurgia Narzadów Ruchu I Ortopedia Polska 1999;64(1):19‐23. [PubMed] [Google Scholar]
Fabis 1999b {published data only}
- Fabis J. Ultrasonographic evaluation of the rotator cuff after its surgical reconstruction [Ultrasonograficzna ocena pierscienia rotatorow po jego chirurgicznej rekonstrukcji]. Chirurgia Narzadów Ruchu I Ortopedia Polska 1999b;64(5):527‐31. [PubMed] [Google Scholar]
Farin 1995 {published data only}
- Farin PU, Jaroma H. Acute traumatic tears of the rotator cuff: value of sonography. Radiology 1995;197(1):269‐73. [DOI] [PubMed] [Google Scholar]
Farin 1996a {published data only}
- Farin PU, Kaukanen E, Jaroma H, Vaatainen U, Miettinen H, Soimakallio S. Site and size of rotator‐cuff tear. Findings at ultrasound, double‐contrast arthrography, and computed tomography arthrography with surgical correlation. Investigative Radiology 1996;31(7):387‐94. [DOI] [PubMed] [Google Scholar]
Farin 1996b {published data only}
- Farin P, Jaroma H. Sonographic detection of tears of the anterior portion of the rotator cuff (subscapularis tendon tears). Journal of Ultrasound in Medicine 1996;15(3):221‐5. [DOI] [PubMed] [Google Scholar]
Farley 1992 {published data only}
- Farley TE, Neumann CH, Steinbach LS, Jahnke AJ, Petersen SS. Full‐thickness tears of the rotator cuff of the shoulder: diagnosis with MR imaging. American Journal of Roentgenology 1992;158(2):347‐51. [DOI] [PubMed] [Google Scholar]
Ferrari 2002 {published data only}
- Ferrari FS, Governi S, Burresi F, Vigni F, Stefani P. Supraspinatus tendon tears: Comparison of US and MR arthrography with surgical correlation. European Radiology 2002;12(5):1211‐7. [DOI] [PubMed] [Google Scholar]
Ferri 2005 {published data only}
- Ferri M, Finlay K, Popowich T, Stamp G, Schuringa P, Friedman L. Sonography of full‐thickness supraspinatus tears: Comparison of patient positioning technique with surgical correlation. American Journal of Roentgenology 2005;184(1):180‐4. [DOI] [PubMed] [Google Scholar]
Flannigan 1990 {published data only}
- Flannigan B, Kursunoglu‐Brahme S, Snyder S, Karzel R, Pizzo W, Resnick D. MR arthrography of the shoulder: comparison with conventional MR imaging. American Journal of Roentgenology 1990;155(4):829‐32. [DOI] [PubMed] [Google Scholar]
Fotiadou 2008 {published data only}
- Fotiadou AN, Vlychou M, Papadopoulos P, Karataglis DS, Palladas P, Fezoulidis IV. Ultrasonography of symptomatic rotator cuff tears compared with MR imaging and surgery. European Journal of Radiology 2008;68(1):174‐9. [DOI] [PubMed] [Google Scholar]
- Vlychou M. Questions related with our inclusion criteria [personal communication]. Email to: M Vlychou 19 July 2011.
- Vlychou M, Dailiana Z, Fotiadou A, Papanagiotou M, Fezoulidis IV, Malizos K. Symptomatic partial rotator cuff tears: diagnostic performance of ultrasound and magnetic resonance imaging with surgical correlation. Acta Radiologica 2009;50(1):101‐5. [DOI] [PubMed] [Google Scholar]
Frei 2008 {published data only}
- Frei R, Chladek P, Trc T, Kopecny Z, Kautzner J. Arthroscopic evaluation of ultrasonography and magnetic resonance imaging for diagnosis of rotator cuff tear. Ortopedia Traumatologia Rehabilitacja 2008;10(2):111‐4. [PubMed] [Google Scholar]
Fritz 1992 {published data only}
- Fritz RC, Stoller DW. Fat‐suppression MR arthrography of the shoulder. Radiology 1992;185(2):614‐5. [DOI] [PubMed] [Google Scholar]
Furtschegger 1988 {published data only}
- Furtschegger A, Resch H. Value of ultrasonography in preoperative diagnosis of rotator cuff tears and postoperative follow‐up. European Journal of Radiology 1988;8(2):69‐75. [PubMed] [Google Scholar]
Girard 1995 {published data only}
- Girard JM, Garcia J. MRI of the shoulder [IRM de l'épaule]. Radiologie ‐ Journal du CEPUR 1995;15(3):32‐7. [Google Scholar]
Goergen 1996 {published data only}
- Goergen SK, Bradley WG Jr, Liu J, Tam JK, Dubin MD, Pema PJ, et al. Improving the diagnostic accuracy of MR in the detection of infraspinatus tendon injuries. Journal of Computer Assisted Tomography 1996;20(5):829‐33. [DOI] [PubMed] [Google Scholar]
Goldberg 2003 {published data only}
- Goldberg JA, Bruce WJ, Walsh W, Sonnabend DH. Role of community diagnostic ultrasound examination in the diagnosis of full‐thickness rotator cuff tears. ANZ Journal of Surgery 2003;73(10):797‐9. [DOI] [PubMed] [Google Scholar]
Hedtmann 2002 {published data only}
- Hedtmann A, Fett H. Ultrasound diagnosis of the rotator cuff [Schultersonographie bei Subakromialsyndromen mit Erkrankungen und Verletzungen der Rotatorenmanschette]. Der Orthopäde 2002;31(3):236‐46. [PubMed] [Google Scholar]
Heijne 2004 {published data only}
- Heijne A. Magnetic resonance imaging of the shoulder. Acta Radiologica 2004;45(5):489‐90. [DOI] [PubMed] [Google Scholar]
Herold 2006 {published data only}
- Herold T, Bachthaler M, Hamer OW, Hente R, Feuerbach S, Fellner C, et al. Indirect MR arthrography of the shoulder: use of abduction and external rotation to detect full‐ and partial‐thickness tears of the supraspinatus tendon. Radiology 2006;240(1):152‐60. [DOI] [PubMed] [Google Scholar]
Herzog 1997 {published data only}
- Herzog RJ. Magnetic resonance imaging of the shoulder. Journal of Bone and Joint Surgery. American Volume 1997;79(6):934‐53. [Google Scholar]
Herzog 1998 {published data only}
- Herzog RJ. Magnetic resonance imaging of the shoulder. Instructional Course Lectures 1998;47:3‐20. [PubMed] [Google Scholar]
Hodler 1987 {published data only}
- Hodler J, Gerber C, Terrier F. Sonography of the rotator cuff [Die Sonographie der Rotatorenmanschette]. Schweizerische Zeitschrift fur Sportmedizin 1987;35(1):5‐11. [PubMed] [Google Scholar]
Hodler 1988 {published data only}
- Hodler J, Fretz CJ, Terrier F, Gerber C. Rotator cuff tears: Correlation of sonographic and surgical findings. Radiology 1988;169(3):791‐4. [DOI] [PubMed] [Google Scholar]
Hodler 1992 {published data only}
- Hodler J, Kursunoglu‐Brahme S, Snyder SJ, Cervilla V, Karzel RP, Schweitzer ME, et al. Rotator cuff disease: Assessment with MR arthrography versus standard MR imaging in 36 patients with arthroscopic confirmation. Radiology 1992;182(2):431‐6. [DOI] [PubMed] [Google Scholar]
Hollister 1995 {published data only}
- Hollister MS, Mack LA, Patten RM, Winter TC 3rd, Matsen FA 3rd, Veith RR. Association of sonographically detected subacromial/subdeltoid bursal effusion and intraarticular fluid with rotator cuff tear. American Journal of Roentgenology 1995;165(3):605‐8. [DOI] [PubMed] [Google Scholar]
Homsi 1989 {published data only}
- Homsi C, Ferreira Filho AA, Padula FM, Stump X, Zoppi Filho A, Bolliger Neto R. Comparative study between ultrasonography and arthrography of the shoulder in rotator cuff tears [Estudo comparativo entre a ultra‐sonografia e a artrografia do ombro nas lesöes do manguito rotador]. Revista Brasileira de Ortopedia 1989;24(11/12):379‐82. [Google Scholar]
Horii 1998 {published data only}
- Horii M, Takubo Y, Yamaguchi J, Kurokawa M, Kubo T, Hirasawa Y. The diagnostic usefulness of magnetic resonance imaging for a partial‐ thickness rotator cuff tear. Journal of Orthopaedic Surgery (Hong Kong) 1998;6(1):53‐8. [Google Scholar]
Iannotti 1991 {published data only}
- Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. Journal of Bone and Joint Surgery. American Volume 1991;73(1):17‐29. [PubMed] [Google Scholar]
Imhoff 1992 {published data only}
- Imhoff A, Hodler J. Arthroscopy and MRT of the shoulder ‐ a comparative retrospective analysis [Arthroskopie und MRT an der Schulter ‐ eine vergleichende retrospektive Analyse]. Zeitschrift für Orthopädie und ihre Grenzgebiete 1992;130(3):188‐96. [DOI] [PubMed] [Google Scholar]
Imhoff 1993 {published data only}
- Imhoff AB, Hodler J, Perrenoud A. Possibilities of shoulder arthroscopy in comparison with magnetic resonance tomography and arthro‐computerized tomography [Moglichkeiten der Schulterarthroskopie im Vergleich zur Magnetresonanz‐Tomographie und Arthro‐Computertomographie]. Zeitschrift für Unfallchirurgie und Versicherungsmedizin 1993;86(1):4‐17. [PubMed] [Google Scholar]
Imhoff 1996 {published data only}
- Imhoff AB, Hodler J. Correlation of MR imaging, CT arthrography, and arthroscopy of the shoulder. Bulletin of the Hospital for Joint Diseases 1996;54(3):146‐52. [PubMed] [Google Scholar]
Iovane 2001 {published data only}
- Iovane A, Midiri M, Bartolotta TV, Carcione A, Lagalla R. Normal anatomy and pathological conditions of subscapular muscle: US findings compared with surgery [Anatomia normale e quadri patologici del muscolo sotoscapolare. Confronto tra ecografia e chirurgia]. Radiologia Medica 2001;101(4):260‐4. [PubMed] [Google Scholar]
Iyengar 2010 {published data only}
- Iyengar JJ, Burnett KR, Nottage WM, Harwin SF. The abduction external rotation (ABER) view for MRI of the shoulder. Orthopedics 2010;33(8):562‐5. [DOI] [PubMed] [Google Scholar]
Jacobson 2003 {published data only}
- Jacobson JA. Sonography of the shoulder. Applied Radiology 2003;32(9):19‐25. [Google Scholar]
Jacobson 2004 {published data only}
- Jacobson JA, Lancaster S, Prasad A, Holsbeeck MT, Craig JG, Kolowich P. Full‐thickness and partial‐thickness supraspinatus tendon tears: value of US signs in diagnosis. Radiology 2004;230(1):234‐42. [DOI] [PubMed] [Google Scholar]
Jaovisidha 1999 {published data only}
- Jaovisidha S, Jacobson JA, Lenchik L, Resnick D. MR imaging of rotator cuff tears: Is there a diagnostic benefit of shoulder exercise prior to imaging. Clinical Imaging 1999;23(4):249‐53. [DOI] [PubMed] [Google Scholar]
Jeyam 2008 {published data only}
- Jeyam M, Funk L, Harris J. Are shoulder surgeons any good at diagnosing rotator cuff tears using ultrasound?: A comparative analysis of surgeon vs radiologist. International Journal of Shoulder Surgery 2008;2(1):4‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jung 2009 {published data only}
- Jung JY, Yoon YC, Yi SK, Yoo J, Choe BK. Comparison study of indirect MR arthrography and direct MR arthrography of the shoulder. Skeletal Radiology 2009;38(7):659‐67. [DOI] [PubMed] [Google Scholar]
Jung 2010 {published data only}
- Jung JY, Jee WH, Chun HJ, Ahn MI, Kim YS. Magnetic resonance arthrography including ABER view in diagnosing partial‐thickness tears of the rotator cuff: accuracy, and inter‐ and intra‐observer agreements. Acta Radiologica 2010;51(2):194‐201. [DOI] [PubMed] [Google Scholar]
Kaneko 1994 {published data only}
- Kaneko K, DeMouy EH, Brunet ME. MR evaluation of rotator cuff impingement: Correlation with confirmed full‐thickness rotator cuff tears. Journal of Computer Assisted Tomography 1994;18(2):225‐8. [DOI] [PubMed] [Google Scholar]
Kautzner 2008 {published data only}
- Kautzner J, Smetana P, Krotka I, Kos P, Frei R, Trc T. Shoulder joint disorder: Correlation of findings by arthroscopy and magnetic resonance imaging [Korelace patologických nalezu ramenniho kloubu pomocí artroskopie versus nukleární magnetickou rezonancí]. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca 2008;75(3):190‐5. [PubMed] [Google Scholar]
Kelly 2009 {published data only}
- Kelly AM, Fessell D. Ultrasound compared with magnetic resonance imaging for the diagnosis of rotator cuff tears: a critically appraised topic. Seminars in Roentgenology 2009;44(3):196‐200. [DOI] [PubMed] [Google Scholar]
Kerkovsky 2008 {published data only}
- Kerkovsky M, Sprlakova‐Pukova A, Uher T, Vojtanik P, Rouchal M. Role of ultrasonography in the diagnosis of shoulder joint injury [Význam UZ vyšetření v diagnostice poranění ramenního kloubu]. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca 2008;75(3):167‐72. [PubMed] [Google Scholar]
Kluger 2003 {published data only}
- Kluger R, Mayrhofer R, Kroner A, Pabinger C, Partan G, Hruby W, et al. Sonographic versus magnetic resonance arthrographic evaluation of full‐thickness rotator cuff tears in millimeters. Journal of Shoulder and Elbow Surgery 2003;12(2):110‐6. [DOI] [PubMed] [Google Scholar]
Kneeland 1987 {published data only}
- Kneeland JB, Middleton WD, Carrera GF, Zeuge RC, Jesmanowicz A, Froncisz W, et al. MR imaging of the shoulder: diagnosis of rotator cuff tears. American Journal of Roentgenology 1987;149(2):333‐7. [DOI] [PubMed] [Google Scholar]
Kujat 1986 {published data only}
- Kujat R, Wippermann BW, Gebel M. Sonography of the shoulder in rotator cuff defects. Technic and clinical value [Schultersonographie bei Rotatorendefekten. Technik und Aussagen]. Der Unfallchirurg 1986;89(9):398‐401. [PubMed] [Google Scholar]
Kurol 1991 {published data only}
- Kurol M, Rahme H, Hilding S. Sonography for diagnosis of rotator cuff tear. Comparison with observations at surgery in 58 shoulders. Acta Orthopaedica Scandinavica 1991;62(5):465‐7. [DOI] [PubMed] [Google Scholar]
Lawson 1991 {published data only}
- Lawson TL, Middleton WD. MRI and ultrasound evaluation of the shoulder. Acta Orthopaedica Belgica 1991;57 Suppl 1:62‐9. [PubMed] [Google Scholar]
Lee 2002 {published data only}
- Lee SY, Lee JK. Horizontal component of partial‐thickness tears of rotator cuff: imaging characteristics and comparison of ABER view with oblique coronal view at MR arthrography initial results. Radiology 2002;224(2):470‐6. [DOI] [PubMed] [Google Scholar]
Lipman 1992 {published data only}
- Lipman JK. Shoulder magnetic resonance imaging. Western Journal of Medicine 1992;156(3):299. [PMC free article] [PubMed] [Google Scholar]
Loew 2000 {published data only}
- Loew R, Kreitner KF, Runkel M, Zoellner J, Thelen M. MR arthrography of the shoulder: comparison of low‐field (0.2 T) vs high‐field (1.5 T) imaging. European Radiology 2000;10(6):989‐96. [DOI] [PubMed] [Google Scholar]
Lopez 2007 {published data only}
- Lopez M. Rotator cuff. Correlation between magnetic resonance imaging and arthroscopy [Manguito rotador. Correlacion entre resonancia magnetica nuclear y artroscopia]. Artroscopía (Buenos Aires) 2007;14(2):91‐5. [Google Scholar]
Low 1998 {published data only}
- Low R, Kreitner KF, Runkel M, Zollner J, Thelen M. Low‐field MR arthrography of the shoulder: Early results using an open 0.2 T MR system [Niederfeld MR‐Arthrographie der Schulter: Erste Ergebnisse mit einem offenen 0,2T MR‐System]. RoFo Fortschritte auf dem Gebiete der Rontgenstrahlen und der Neuen Bildgebenden Verfahren 1998;168(4):316‐22. [DOI] [PubMed] [Google Scholar]
Lucas 1991 {published data only}
- Lucas C, Duvauferrier R, Korvin B, Thomazeau H, Lelievre N, Ramee A. MRI of the shoulder [IRM de l'épaule]. Feuillets de Radiologie 1991;31(1):68‐76. [Google Scholar]
Mack 1988 {published data only}
- Mack LA, Gannon MK, Kilcoyne RF, Matsen RA 3rd. Sonographic evaluation of the rotator cuff. Accuracy in patients without prior surgery. Clinical Orthopaedics and Related Research 1988;(234):21‐7. [PubMed] [Google Scholar]
- Mack LA, Matsen FA 3rd, Kilcoyne RF, Davies PK, Sickler ME. US evaluation of the rotator cuff. Radiology 1985;157(1):205‐9. [DOI] [PubMed] [Google Scholar]
Magee 2003a {published data only}
- Magee T, Shapiro M, Williams D, Ramnath RR, Simon J. Usefulness of the simultaneous acquisition of spatial harmonics technique during MRI of the shoulder. American Journal of Roentgenology 2003;181(4):961‐4. [DOI] [PubMed] [Google Scholar]
Magee 2003b {published data only}
- Magee T, Shapiro M, Williams D. Comparison of high‐field‐strength versus low‐field‐strength MRI of the shoulder. American Journal of Roentgenology 2003;181(5):1211‐5. [DOI] [PubMed] [Google Scholar]
Magee 2006 {published data only}
- Magee T, Williams D. 3.0‐T MRI of the supraspinatus tendon. American Journal of Roentgenology 2006;187(4):881‐6. [DOI] [PubMed] [Google Scholar]
Magee 2007 {published data only}
- Magee T. Can isotropic fast gradient echo imaging be substituted for conventional T1 weighted sequences in shoulder MR arthrography at 3 tesla?. Journal of Magnetic Resonance Imaging 2007;26(1):118‐22. [DOI] [PubMed] [Google Scholar]
Magee 2009 {published data only}
- Magee T. 3‐T MRI of the shoulder: Is MR arthrography necessary?. American Journal of Roentgenology 2009;192(1):86‐92. [DOI] [PubMed] [Google Scholar]
Malvestiti 1997 {published data only}
- Malvestiti O, Mariani C, Scorsolini A, Ratti F, Ferraris G, Columbaro G. Subacromial impingement syndrome and rotator cuff tear. Ultrasonography of 140 cases [Sindrome da conflitto sotto‐acromiale e lesioni della cuffia dei rotatori. Esperienza ecografica in 140 casi]. Radiologia Medica 1997;94(1‐2):37‐42. [PubMed] [Google Scholar]
Martin 2008 {published data only}
- Martin D, Jeer PJ, Kalairajah Y, Falworth M, Zadow S, Simmons N. Air bubble saline arthrosonography in imaging rotator cuff tears. Orthopedics 2008;31(2):140‐2. [DOI] [PubMed] [Google Scholar]
Masaoka 1999 {published data only}
- Masaoka S, Hashizume H, Senda M, Nishida K, Nagoshi M, Inoue H. Ultrasonographic analysis of shoulder rotator cuff tears. Acta Medica Okayama 1999;53(2):81‐9. [DOI] [PubMed] [Google Scholar]
Masciocchi 1989 {published data only}
- Masciocchi C, Barile A, Fascetti E, Gallucci M, Beomonte Zobel B, Laconi MM, et al. Magnetic resonance of the shoulder: technique, anatomy and clinical results [Risonaza magnetica della spalla: tecnica, anatomia e risultati clinici]. Radiologia Medica 1989;78(5):485‐91. [PubMed] [Google Scholar]
Meister 2004 {published data only}
- Meister K, Thesing J, Montgomery WJ, Indelicato PA, Walczak S, Fontenot W. MR arthrography of partial thickness tears of the undersurface of the rotator cuff: An arthroscopic correlation. Skeletal Radiology 2004;33(3):136‐41. [DOI] [PubMed] [Google Scholar]
Mendieta‐Sevilla 2009 {published data only}
- Mendieta‐Sevilla SR, Lourdes Munoz‐Carlin M, Canto‐Vera R, Gonzalez‐Perez CE, Trejo‐Trejo JS, Torres‐Zavala A. Evaluation with ultrasound and arthro‐ultrasonography of complete rotator cuff rupture [Evaluacion por ultrasonido y artroultrasonografia de la ruptura completa del manguito de los rotadores]. Revista de Investigacion Clinica; Organo del Hospital de Enfermedades de la Nutricion 2009;61(1):33‐40. [PubMed] [Google Scholar]
Merl 1996 {published data only}
- Merl T, Weinhardt H, Ottl G, Lenz M, Riel KA. Diagnostic imaging of the shoulder joint in impingement [Bildgebende Diagnostik des Schultergelenkes bei Impingement]. Rontgenpraxis; Zeitschrift fur radiologische Technik 1996;49(1):8‐11. [PubMed] [Google Scholar]
Middleton 1993 {published data only}
- Middleton WD. Sonographic detection and quantification of rotator cuff tears. American Journal of Roentgenology 1993;160(1):109‐10. [DOI] [PubMed] [Google Scholar]
Miller 2008 {published data only}
- Miller D, Frost A, Hall A, Barton C, Bhoora I, Kathuria V. A 'one‐stop clinic' for the diagnosis and management of rotator cuff pathology: Getting the right diagnosis first time. International Journal of Clinical Practice 2008;62(5):750‐3. [DOI] [PubMed] [Google Scholar]
Montrucchio 1997 {published data only}
- Montrucchio E, Iovane A, Midiri M, Finazzo M, Tona G, Lagalla R. Normal anatomy and pathologic features of the supraspinatus muscle: comparison between ultrasonography and surgery. Analysis of the potential sources of diagnostic errors [Anatomia normale e quadri patologici del muscolo sovraspinato: confronto tra ecografia e chirurgia. Analisi delle possibili fonti di errore diagnostico]. Radiologia Medica 1997;93(4):342‐7. [PubMed] [Google Scholar]
Monu 1994 {published data only}
- Monu JU, Pruett S, Vanarthos WJ, Pope TL Jr. Isolated subacromial bursal fluid on MRI of the shoulder in symptomatic patients: correlation with arthroscopic findings. Skeletal Radiology 1994;23(7):529‐33. [DOI] [PubMed] [Google Scholar]
Moosmayer 2005 {published data only}
- Moosmayer S, Smith HJ. Diagnostic ultrasound of the shoulder ‐ a method for experts only? Results from an orthopedic surgeon with relative inexpensive compared to operative findings. Acta Orthopaedica 2005;76(4):503‐8. [DOI] [PubMed] [Google Scholar]
Moosmayer 2007 {published data only}
- Moosmayer S, Heir S, Smith HJ. Sonography of the rotator cuff in painful shoulders performed without knowledge of clinical information: results from 58 sonographic examinations with surgical correlation. Journal of Clinical Ultrasound 2007;35(1):20‐6. [DOI] [PubMed] [Google Scholar]
Morrison 1990 {published data only}
Naqvi 2009 {published data only}
- Naqvi GA, Jadaan M, Harrington P. Accuracy of ultrasonography and magnetic resonance imaging for detection of full thickness rotator cuff tears. International Journal of Shoulder Surgery 2009;3(4):94‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Narbona 2007 {published data only}
- Narbona P. Superior labrum anterior‐posterior lesions in rotator cuff rupture. Efficacy of clinical and imaging findings [Diagnostico de la lesion SLAP en las rupturas del manguito rotador. Eficacia del examen fisico y de la resonancia magnetica nuclear sin contraste]. Artroscopía (Buenos Aires) 2007;14(2):96‐101. [Google Scholar]
Needell 1997 {published data only}
- Needell SD, Zlatkin MB. Comparison of fat‐saturation fast spin echo versus conventional spin‐ echo MRI in the detection of rotator cuff pathology. Journal of Magnetic Resonance Imaging 1997;7(4):674‐7. [DOI] [PubMed] [Google Scholar]
Nelson 1991 {published data only}
- Nelson MC, Leather GP, Nirschl RP, Pettrone FA, Freedman MT. Evaluation of the painful shoulder. A prospective comparison of magnetic resonance imaging, computerized tomographic arthrography, ultrasonography, and operative findings. Journal of Bone and Joint Surgery. American Volume 1991;73(5):707‐16. [PubMed] [Google Scholar]
Nogueira‐Barbosa 2002 {published data only}
- Nogueira‐Barbosa MH, Volpon JB, Elias Júnior J, Muccillo G. Diagnostic imaging of shoulder rotator cuff lesions [Diagnóstico por imagem nas rupturas do manguito rotador]. Acta Ortopedica Brasileira 2002;10(4):31‐9. [Google Scholar]
Norregaard 2002 {published data only}
- Norregaard J, Krogsgaard MR, Lorenzen T, Jensen EM. Diagnosing patients with longstanding shoulder joint pain. Annals of the Rheumatic Diseases 2002;61(7):646‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oh 2009 {published data only}
- Oh DK, Yoon YC, Kwon JW, Choi SH, Jung JY, Bae S, et al. Comparison of indirect isotropic MR arthrography and conventional MR arthrography of labral lesions and rotator cuff tears: a prospective study. American Journal of Roentgenology 2009;192(2):473‐9. [DOI] [PubMed] [Google Scholar]
Oh 2010 {published data only}
- Oh JH, Kim JY, Choi JA, Kim WS. Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: comparison with magnetic resonance imaging with arthroscopic correlation. Journal of Shoulder and Elbow Surgery 2010;19(1):14‐20. [DOI] [PubMed] [Google Scholar]
Ostlere 1997 {published data only}
- Ostlere SJ. Imaging the rotator cuff ‐ A practical approach. Imaging 1997;9(2):89‐93. [Google Scholar]
Ozcakar 2005 {published data only}
- Ozcakar L, Vanderstraeten G, Parlevliet T. Sonography and visualizing rotator cuff injuries in older people. Journal of the American Geriatrics Society 2005;53(10):1840‐1. [DOI] [PubMed] [Google Scholar]
Paavolainen 1994 {published data only}
- Paavolainen P, Ahovuo J. Ultrasonography and arthrography in the diagnosis of tears of the rotator cuff. Journal of Bone and Joint Surgery. American Volume 1994;76(3):335‐40. [DOI] [PubMed] [Google Scholar]
Palmer 1993 {published data only}
- Palmer WE, Brown JH, Rosenthal DI. Rotator cuff: Evaluation with fat‐suppressed MR arthrography. Radiology 1993;188(3):683‐7. [DOI] [PubMed] [Google Scholar]
Palmer 1994 {published data only}
- Palmer WE. Imaging options for suspected rotator cuff disorder. American Journal of Roentgenology 1994;163(4):990‐1. [DOI] [PubMed] [Google Scholar]
Parsa 1997 {published data only}
- Parsa M, Tuite M, Norris M, Orwin J. MR imaging of rotator cuff tendon tears: comparison of T2*‐weighted gradient‐echo and conventional dual‐echo sequences. American Journal of Roentgenology 1997;168(6):1519‐24. [DOI] [PubMed] [Google Scholar]
Pattee 1988 {published data only}
- Pattee GA, Snyder SJ. Sonographic evaluation of the rotator cuff: correlation with arthroscopy. Arthroscopy 1988;4(1):15‐20. [DOI] [PubMed] [Google Scholar]
Patten 1994 {published data only}
- Patten RM, Spear RP, Richardson ML. Diagnostic performance of magnetic resonance imaging for the diagnosis of rotator cuff tears using supplemental images in the oblique sagittal plane. Investigative Radiology 1994;29(1):87‐93. [DOI] [PubMed] [Google Scholar]
Peetrons 1986 {published data only}
- Peetrons P, Delmotte S, Stehman M, Peetrons A. Lesions of the rotator cuff: the specific value of echography [Lesions de la coiffe des rotateurs: apport specifique de l'echographie]. Acta Orthopaedica Belgica 1986;52(6):703‐16. [PubMed] [Google Scholar]
Pfirrmann 1999 {published data only}
- Pfirrmann CW, Zanetti M, Weishaupt D, Gerber C, Hodler J. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology 1999;213(3):709‐14. [DOI] [PubMed] [Google Scholar]
Pfirrmann 2004 {published data only}
- Pfirrmann CW, Schmid MR, Zanetti M, Jost B, Gerber C, Hodler J. Assessment of fat content in supraspinatus muscle with proton MR spectroscopy in asymptomatic volunteers and patients with supraspinatus tendon lesions. Radiology 2004;232(3):709‐15. [DOI] [PubMed] [Google Scholar]
Pigeau 1992 {published data only}
- Pigeau I, Doursounian L, Sokolow C, Valenti P, Djermag Y, Maigne JY, et al. Contribution of gradient‐echo MRI in the study of subacromial pathology: correlation between surgery and arthrography [Apport de l'IRM par echo de gradient dans l'etude de la pathologie sous‐acromiale: correlation chirurgicale et arthrographique]. Annales de Radiologie 1992;35(3):143‐9. [PubMed] [Google Scholar]
Poey 1990 {published data only}
- Poey C, Fajadet P, Pages M, Chaffai MA, Lassoued S, Maquin P, et al. MRI in subacromial pathology. Report of 20 cases [IRM dans la pathologie sous‐acromiale. A propos de 20 observations]. Journal de Radiologie 1990;71(8‐9):457‐66. [PubMed] [Google Scholar]
Porcellini 1994 {published data only}
- Porcellini G, Campi F, Nicolo F, Vottari S, Valbonesi C, Arcangeli E. Rotator cuff rupture in the shoulder impingement syndrome. Echography and arthrography: 2 diagnostic methods compared [Rottura della cuffia dei rotatori nella sindrome da attrito della spalla. Ecografia e artrografia: due metodiche diagnostiche a confronto]. Radiologia Medica 1994;88(5):564‐8. [PubMed] [Google Scholar]
Prendergast 1992 {published data only}
- Prendergast N, Rafii M. Magnetic resonance imaging of the shoulder joint. Current Opinion in Radiology 1992;4(6):70‐6. [PubMed] [Google Scholar]
Quinn 1995 {published data only}
- Quinn SF, Sheley RC, Demlow TA, Szumowski J. Rotator cuff tendon tears: Evaluation with fat‐suppressed MR imaging with arthroscopic correlation in 100 patients. Radiology 1995;195(2):497‐500. [DOI] [PubMed] [Google Scholar]
Rafii 1990 {published data only}
- Rafii M, Firooznia H, Sherman O, Minkoff J, Weinreb J, Golimbu C, et al. Rotator cuff lesions: signal patterns at MR imaging. Radiology 1990;177(3):817‐23. [DOI] [PubMed] [Google Scholar]
Read 1998 {published data only}
- Read JW, Perko M. Shoulder ultrasound: diagnostic accuracy for impingement syndrome, rotator cuff tear, and biceps tendon pathology. Journal of Shoulder and Elbow Surgery 1998;7(3):264‐71. [DOI] [PubMed] [Google Scholar]
Recht 1993 {published data only}
- Recht MP, Resnick D. Magnetic resonance‐imaging studies of the shoulder. Diagnosis of lesions of the rotator cuff. Journal of Bone and Joint Surgery. American Volume 1993;75(8):1244‐53. [DOI] [PubMed] [Google Scholar]
Recht 1994 {published data only}
- Recht MP, Resnick D. Magnetic resonance imaging studies of the shoulder: diagnosis of lesions of the rotator cuff. Instructional Course Lectures 1994;43:483‐92. [PubMed] [Google Scholar]
Reinus 1995 {published data only}
- Reinus WR, Shady KL, Mirowitz SA, Totty WG. MR diagnosis of rotator cuff tears of the shoulder: value of using T2‐weighted fat‐saturated images. American Journal of Roentgenology 1995;164(6):1451‐5. [DOI] [PubMed] [Google Scholar]
Roberts 1998 {published data only}
- Roberts CS, Galloway KP, Honaker JT, Hulse G, Seligson D. Sonography for the office screening of suspected rotator cuff tears: early experience of the orthopedic surgeon. American Journal of Orthopedics 1998;27(7):503‐6. [PubMed] [Google Scholar]
Roberts 2001 {published data only}
- Roberts CS, Walker JA 2nd, Seligson D. Diagnostic capabilities of shoulder ultrasonography in the detection of complete and partial rotator cuff tears. American Journal of Orthopedics 2001;30(2):159‐62. [PubMed] [Google Scholar]
Robertson 1995 {published data only}
- Robertson PL, Schweitzer ME, Mitchell DG, Schlesinger F, Epstein RE, Frieman BG, et al. Rotator cuff disorders: interobserver and intraobserver variation in diagnosis with MR imaging. Radiology 1995;194(3):831‐5. [DOI] [PubMed] [Google Scholar]
Rouaud 1989 {published data only}
- Rouaud JP, Dufour D, Caroit M. Echography in simple shoulder pain [L'echographie dans les epaules douloureuses simples]. Revue du Rhumatisme et des Maladies Osteo‐Articulaires 1989;56(12):805‐7. [PubMed] [Google Scholar]
Rubin 1997 {published data only}
- Rubin DA. Not‐so‐fast MR imaging of the rotator cuff. American Journal of Roentgenology 1997;168(4):1112‐3. [DOI] [PubMed] [Google Scholar]
Rutten 2010a {published data only}
- Rutten MJ, Jager GJ, Kiemeney LA. Ultrasound detection of rotator cuff tears: observer agreement related to increasing experience. American Journal of Roentgenology 2010;195(6):W440‐6. [DOI] [PubMed] [Google Scholar]
Rutten 2010b {published data only}
- Rutten MJ, Spaargaren GJ, Loon T, Waal Malefijt MC, Kiemeney LA, Jager GJ. Detection of rotator cuff tears: the value of MRI following ultrasound. European Radiology 2010;20(2):450‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sahin‐Akyar 1998 {published data only}
- Sahin‐Akyar G, Miller TT, Staron RB, McCarthy DM, Feldman F. Gradient‐echo versus fat‐suppressed fast spin‐echo MR imaging of rotator cuff tears. AJM. American Journal of Roentgenology 1998;171(1):223‐7. [DOI] [PubMed] [Google Scholar]
Sartoris 1992 {published data only}
- Sartoris DJ. Diagnosing shoulder pain: What's the best imaging approach?. Physician and Sportsmedicine 1992;20(9):151‐6,159‐62,164. [DOI] [PubMed] [Google Scholar]
Sasaki 1990 {published data only}
- Sasaki M, Ehara S, Nakasato T, Tamakawa Y, Kuboya Y, Sugisawa M, et al. MR of the shoulder with a 0.2‐T permanent‐magnetic unit. American Journal of Roentgenology 1990;154(4):777‐8. [DOI] [PubMed] [Google Scholar]
Schneider 2003 {published data only}
- Schneider TL, Schmidt‐Wiethoff R, Drescher W, Fink B, Schmidt J, Appell HJ. The significance of subacromial arthrography to verify partial bursal‐side rotator cuff ruptures. Archives of Orthopaedic and Trauma Surgery 2003;123(9):481‐4. [DOI] [PubMed] [Google Scholar]
Schreinemachers 2009 {published data only}
- Schreinemachers SA, Hulst VP, Willems WJ, Bipat S, Woude HJ. Detection of partial‐thickness supraspinatus tendon tears: is a single direct MR arthrography series in ABER position as accurate as conventional MR arthrography?. Skeletal Radiology 2009;38(10):967‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schultz 1994 {published data only}
- Schultz E. What is the significance on increased signal within the rotator cuff on T2‐weighted images in the coronal oblique plane?. American Journal of Roentgenology 1994;163(2):472. [DOI] [PubMed] [Google Scholar]
Seeger 1988 {published data only}
- Seeger LL, Gold RH, Bassett LW, Ellman H. Shoulder impingement syndrome: MR findings in 53 shoulders. American Journal of Roentgenology 1988;150(2):343‐7. [DOI] [PubMed] [Google Scholar]
Sheah 2009 {published data only}
- Sheah K, Bredella MA, Warner JJ, Halpern EF, Palmer WE. Transverse thickening along the articular surface of the rotator cuff consistent with the rotator cable: identification with MR arthrography and relevance in rotator cuff evaluation. American Journal of Roentgenology 2009;193(3):679‐86. [DOI] [PubMed] [Google Scholar]
Shellock 1996 {published data only}
- Shellock FG, Stoller D, Crues JV. MRI of the shoulder: a rational approach to the reporting of findings. Journal of Magnetic Resonance Imaging 1996;6(1):268‐70. [DOI] [PubMed] [Google Scholar]
Shellock 2001 {published data only}
- Shellock FG, Bert JM, Fritts HM, Gundry CR, Easton R, Crues JV, et al. Evaluation of the rotator cuff and glenoid labrum using a 0.2‐Tesla extremity magnetic resonance (MR) system: MR results compared to surgical findings. Journal of Magnetic Resonance Imaging 2001;14(6):763‐70. [DOI] [PubMed] [Google Scholar]
Shiv 1990 {published data only}
- Shiv VK, Marya SK, Taneja K, Mehrotra G, Mittal SK, Bhargava SK. Sonographic evaluation of rotator cuff injuries. Indian Journal of Radiology and Imaging 1990;44(3):197‐200. [Google Scholar]
Singer 1995 {published data only}
- Singer B, Cotten A, Chastanet P. Ultrasonography of the rotator cuff [Échographie de la coiffe des rotateurs]. Radiologie ‐ Journal du CEPUR 1995;15(5):11‐9. [Google Scholar]
Singson 1996 {published data only}
- Singson RD, Hoang T, Dan S, Friedman M. MR evaluation of rotator cuff pathology using T2‐weighted fast spin‐echo technique with and without fat suppression. American Journal of Roentgenology 1996;166(5):1061‐5. [DOI] [PubMed] [Google Scholar]
Skib 1998 {published data only}
- Skib RA. Magnetic resonance imaging assessment of the rotator cuff: is it really accurate?. Arthroscopy 1998;14(6):656‐8. [DOI] [PubMed] [Google Scholar]
Soble 1989 {published data only}
- Soble MG, Kaye AD, Guay RC. Rotator cuff tear: clinical experience with sonographic detection. Radiology 1989;173(2):319‐21. [DOI] [PubMed] [Google Scholar]
Sonin 1996 {published data only}
- Sonin AH, Peduto AJ, Fitzgerald SW, Callahan CM, Bresler ME. MR imaging of the rotator cuff mechanism: comparison of spin‐echo and turbo spin‐echo sequences. American Journal of Roentgenology 1996;167(2):333‐8. [DOI] [PubMed] [Google Scholar]
Sonnabend 1997 {published data only}
- Sonnabend D, Hughes HJ, Giuffre B, Farrell R. Ultrasound assessment of shoulder pathology. Surgery of the shoulder. 6th International Congress, Helsinki, Finland. 1995:13–7.
- Sonnabend DH, Hughes JS, Giuffre BM, Farrell R. The clinical role of shoulder ultrasound. Australian and New Zealand Journal of Surgery 1997;67(9):630‐3. [DOI] [PubMed] [Google Scholar]
Soto Araiza 1998 {published data only}
- Soto Araiza G, Arredondo Estrada JH, Onofre Castillo J, Arredondo Galán JH, Padilla Dieste A, Garza Montemayor M, et al. Ultrasound of the painful shoulder: study of 42 patients [El ultrasonido en el hombro doloroso: estudio de 42 pacientes]. Revista Mexicana de Radiología 1998;52(4):163‐7. [Google Scholar]
Steinbach 2000 {published data only}
- Steinbach LS, Gunther SB. Magnetic resonance imaging of the rotator cuff. Seminars in Roentgenology 2000;35(3):200‐16. [DOI] [PubMed] [Google Scholar]
Strauss 1998 {published data only}
- Strauss J, Krause D, Holtzmann P, Gonzalves M, Maillefert JF, Tavernier C. Correlations and discordante observations MRI versus arthroscopy in shoulder cuff tears [Correlations et analyse de discordances – IRM – Arthroscopie dans les ruptures de coiffe de l’epaule]. Rhumatologie 1998;50(8):266‐73. [Google Scholar]
Suder 1994 {published data only}
- Suder PA, Hougaard K, Frich LH, Rasmussen OS, Lundorf E. Intraarticular findings in the chronically painful shoulder. A study of 32 posttraumatic cases. Acta Orthopaedica Scandinavica 1994;65(3):339‐43. [DOI] [PubMed] [Google Scholar]
Sunde 2001 {published data only}
- Sunde P, Edenberg J. Diagnosis of rotator cuff injury [Diagnostikk av rotatorcuffskade]. Tidsskrift for Den Norske Laegeforening 2001;121(18):2203. [PubMed] [Google Scholar]
Sunde 2008 {published data only}
- Sunde P, Tariq R. Ultrasound ‐ a good alternative to MR in shoulder problems [Ultralyd ‐ et godt alternativ til MR ved skulderlidelser]. Tidsskrift for Den Norske Laegeforening 2008;128(7):842. [PubMed] [Google Scholar]
Taboury 1995 {published data only}
- Taboury J. Ultrasonography of the tendons of the rotator cuffs of the shoulder [Etude echographique des tendons des muscles rotateurs de l'epaule]. Annales de Radiologie 1995;38(5):275‐9. [PubMed] [Google Scholar]
Takagishi 1993 {published data only}
- Takagishi K, Itoman M, Araki T, Nishimura A, Yamamoto M, Ikeda T. MR imaging of recurrent dislocation and impingement syndrome of the shoulder. Journal of Orthopaedic Surgery 1993;1(1):99‐101. [Google Scholar]
Takagishi 1996 {published data only}
- Takagishi K, Makino K, Takahira N, Ikeda T, Tsuruno K, Itoman M. Ultrasonography for diagnosis of rotator cuff tear. Skeletal Radiology 1996;25(3):221‐4. [DOI] [PubMed] [Google Scholar]
Teefey 2000 {published data only}
- Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff: A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. Journal of Bone and Joint Surgery. American Volume 2000;82(4):498‐504. [PubMed] [Google Scholar]
Teefey 2009 {published data only}
- Teefey SA, Petersen B, Prather H. Shoulder ultrasound vs MRI for rotator cuff pathology. PM & R : The Journal of Injury, Function, and Rehabilitation 2009;1(5):490‐5. [DOI] [PubMed] [Google Scholar]
Theodoropoulos 2010 {published data only}
- Theodoropoulos JS, Andreisek G, Harvey EJ, Wolin P. Magnetic resonance imaging and magnetic resonance arthrography of the shoulder: Dependence on the level of training of the performing radiologist for diagnostic accuracy. Skeletal Radiology 2010;39(7):661‐7. [DOI] [PubMed] [Google Scholar]
Tirman 1994 {published data only}
- Tirman PF, Bost FW, Steinbach LS, Mall JC, Peterfy CG, Sampson TG, et al. MR arthrographic depiction of tears of the rotator cuff: benefit of abduction and external rotation of the arm. Radiology 1994;192(3):851‐6. [DOI] [PubMed] [Google Scholar]
Torstensen 1999 {published data only}
- Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. Journal of Shoulder and Elbow Surgery 1999;8(1):42‐5. [DOI] [PubMed] [Google Scholar]
Touzard 1991 {published data only}
- Touzard RC, Pigeau I, Doursounian L, Maigne JY, Vadrot D. Contribution of echogradient magnetic resonance imaging in the study of subacromial diseases. Surgical and arthrographic correlations [Apport de l'IRM par echo de gradient dans l'etude de la pathologie sous‐acromiale. Correlation chirurgicale et arthrographique]. Chirurgie 1991;117(7):569‐76. [PubMed] [Google Scholar]
Toyoda 2005 {published data only}
- Toyoda H, Ito Y, Tomo H, Nakao Y, Koike T, Takaoka K. Evaluation of rotator cuff tears with magnetic resonance arthrography. Clinical Orthopaedics and Related Research 2005;(439):109‐15. [DOI] [PubMed] [Google Scholar]
Traughber 1992 {published data only}
- Traughber PD, Goodwin TE. Shoulder MRI: arthroscopic correlation with emphasis on partial tears. Journal of Computer Assisted Tomography 1992;16(1):129‐33. [PubMed] [Google Scholar]
Traughber 1996 {published data only}
- Traughber P, Czech M. Accuracy of fat‐suppressed MR imaging of the shoulder for detection of partial‐thickness rotator cuff tears. Radiology 1996;198(1):293. [DOI] [PubMed] [Google Scholar]
Traughber 2006 {published data only}
- Traughber PD, Merandi S, Traughber KA. MR arthrography is not proven to be preferred baseline MRI examination. American Journal of Roentgenology 2006;186(1):265‐6. [DOI] [PubMed] [Google Scholar]
Tuite 1994 {published data only}
- Tuite MJ, Yandow DR, DeSmet AA, Orwin JF, Quintana FA. Diagnosis of partial and complete rotator cuff tears using combined gradient echo and spin echo imaging. Skeletal Radiology 1994;23(7):541‐5. [DOI] [PubMed] [Google Scholar]
Tuite 1995 {published data only}
- Tuite MJ, Yandow DR, Smet AA, Orwin JF, Quintana FA. Effect of field of view on MR diagnosis of rotator cuff tears. Skeletal Radiology 1995;24(7):495‐8. [DOI] [PubMed] [Google Scholar]
Tuite 1998 {published data only}
- Tuite MJ, Turnbull JR, Orwin JF. Anterior versus posterior, and rim‐rent rotator cuff tears: prevalence and MR sensitivity. Skeletal Radiology 1998;27(5):237‐43. [DOI] [PubMed] [Google Scholar]
Tuite 2001 {published data only}
- Tuite MJ, Asinger D, Orwin JF. Angled oblique sagittal MR imaging of rotator cuff tears: comparison with standard oblique sagittal images. Skeletal Radiology 2001;30(5):262‐9. [DOI] [PubMed] [Google Scholar]
Turrin 1997 {published data only}
- Turrin A, Cappello A, Mauri M, Zambelloni M. Echography of the shoulder with the patient supine in the diagnosis of rotator cuff rupture [L'ecografia della spalla con paziente supino nella diagnosi della rottura della cuffia dei rotatori]. Radiologia Medica 1997;94(3):170‐5. [PubMed] [Google Scholar]
Vahlensieck 2001 {published data only}
- Vahlensieck M. On: Indirect MR arthrography in the diagnosis rotator cuff injuries [Zu: Indirekte MR‐Arthrographie in der Diagnostik von Rotatorenmanschettenlasionen]. ROFO. Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 2001;173(2):161. [DOI] [PubMed] [Google Scholar]
Vander Maren 1995 {published data only}
- Vander Maren C, Shahabpour M, Willems S, Vande Berg B, Handelberg F, Malghem J. The value of MRI in the evaluation of lesions of the supraspinous muscle. Multicentric retrospective study of 66 records [Interet de l'I.R.M. dans le bilan lesionnel du supra‐epineux. Etude multicentrique retrospective de 66 dossiers]. Acta Orthopaedica Belgica 1995;61 Suppl 1:8‐13. [PubMed] [Google Scholar]
Van Dyck 2009 {published data only}
- Dyck P, Gielen JL, Veryser J, Weyler J, Vanhoenacker FM, Glabbeek F, et al. Tears of the supraspinatus tendon: assessment with indirect magnetic resonance arthrography in 67 patients with arthroscopic correlation. Acta Radiologica 2009;50(9):1057‐63. [DOI] [PubMed] [Google Scholar]
Vanecek 2000 {published data only}
- Vanecek I, Kasparek R. Ultrasonographic examination of the rotator cuff of the shoulder: our eight‐year experience [Ultrasonograficke vysetreni rotatorove manzety ramenniho kloubu ‐ nase osmilete zkusenosti]. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca 2000;67(5):316‐23. [PubMed] [Google Scholar]
Van Holsbeeck 1995 {published data only}
- Holsbeeck MT, Kolowich PA, Eyler WR, Craig JG, Shirazi KK, Habra GK, et al. US depiction of partial‐thickness tear of the rotator cuff. Radiology 1995;197(2):443‐6. [DOI] [PubMed] [Google Scholar]
Van Moppes 1995 {published data only}
Waldt 2007 {published data only}
- Waldt S, Bruegel M, Mueller D, Holzapfel K, Imhoff AB, Rummeny EJ, et al. Rotator cuff tears: assessment with MR arthrography in 275 patients with arthroscopic correlation. European Radiology 2007;17(2):491‐8. [DOI] [PubMed] [Google Scholar]
Wallny 1999 {published data only}
- Wallny T, Wagner UA, Prange S, Schmitt O, Reich H. Evaluation of chronic tears of the rotator cuff by ultrasound. A new index. Journal of Bone and Joint Surgery. British Volume 1999;81(4):675‐8. [DOI] [PubMed] [Google Scholar]
Walz 2007 {published data only}
- Walz DM, Miller TT, Chen S, Hofman J. MR imaging of delamination tears of the rotator cuff tendons. Skeletal Radiology 2007;36(5):411‐6. [DOI] [PubMed] [Google Scholar]
Wang 1994 {published data only}
- Wang YM, Shih TT, Jiang CC, Su CT, Huang KM, Hang YS, et al. Magnetic resonance imaging of rotator cuff lesions. Journal of the Formosan Medical Association 1994;93(3):234‐9. [PubMed] [Google Scholar]
Weinstabl 1988 {published data only}
- Weinstabl R, Gritzmann N, Hertz H. Significance of ultrasonography in the diagnosis of shoulder pathology [Stellenwert der Sonographie in der pathologischen Schulterdiagnostik]. Zeitschrift fur Unfallchirurgie, Versicherungsmedizin und Berufskrankheiten 1988;81(3):157‐64. [PubMed] [Google Scholar]
Wiener 1993 {published data only}
- Wiener SN, Seitz WH Jr. Sonography of the shoulder in patients with tears of the rotator cuff: accuracy and value for selecting surgical options. American Journal of Roentgenology 1993;160(1):103‐7. [DOI] [PubMed] [Google Scholar]
Wilson 1994 {published data only}
- Wilson AJ. Is shoulder arthrography considered an acceptable alternative to MR imaging in the evaluation of rotator cuff tears?. American Journal of Roentgenology 1994;162(6):1495. [DOI] [PubMed] [Google Scholar]
Wnorowski 1997 {published data only}
- Wnorowski DC, Levinsohn EM, Chamberlain BC, McAndrew DL. Magnetic resonance imaging assessment of the rotator cuff: Is it really accurate?. Arthroscopy 1997;13(6):710‐9. [DOI] [PubMed] [Google Scholar]
Wu 2003 {published data only}
- Wu HP, Dubinsky TJ, Richardson ML. Association of shoulder sonographic findings with subsequent surgical treatment for rotator cuff injury. Journal of Ultrasound in Medicine 2003;22(2):155‐61. [DOI] [PubMed] [Google Scholar]
Yagci 2001 {published data only}
- Yagci B, Manisali M, Yilmaz E, Ozkan M, Ekin A, Ozaksoy D, et al. Indirect MR arthrography of the shoulder in detection of rotator cuff ruptures. European Radiology 2001;11(2):258‐62. [DOI] [PubMed] [Google Scholar]
Yamakawa 2001 {published data only}
- Yamakawa S, Hashizume H, Ichikawa N, Itadera E, Inoue H. Comparative studies of MRI and operative findings in rotator cuff tear. Acta Medica Okayama 2001;55(5):261‐8. [DOI] [PubMed] [Google Scholar]
Yeh 2003 {published data only}
- Yeh LR, Kuen‐Huang Chen C, Lai PH. MR arthrographic evaluation of the shoulder: Comparison of neutral position and ABER position. Chinese Journal of Radiology 2003;28(4):209‐16. [Google Scholar]
Yeu 1994 {published data only}
- Yeu K, Jiang CC, Shih TT. Correlation between MRI and operative findings of the rotator cuff tear. Journal of the Formosan Medical Association 1994;93(2):134‐9. [PubMed] [Google Scholar]
Zehetgruber 2002 {published data only}
- Zehetgruber H, Lang T, Wurnig C. Distinction between supraspinatus, infraspinatus and subscapularis tendon tears with ultrasound in 332 surgically confirmed cases. Ultrasound in Medicine and Biology 2002;28(6):711‐7. [DOI] [PubMed] [Google Scholar]
Ziegler 2004 {published data only}
- Ziegler DW. The use of in‐office, orthopaedist‐performed ultrasound of the shoulder to evaluate and manage rotator cuff disorders. Journal of Shoulder and Elbow Surgery 2004;13(3):291‐7. [DOI] [PubMed] [Google Scholar]
Zlatkin 1989 {published data only}
- Zlatkin MB, Iannotti JP, Roberts MC, Esterhai JL, Dalinka MK, Kressel HY, et al. Rotator cuff tears: diagnostic performance of MR imaging. Radiology 1989;172(1):223‐9. [DOI] [PubMed] [Google Scholar]
Zlatkin 2004 {published data only}
- Zlatkin MB, Hoffman C, Shellock FG. Assessment of the rotator cuff and glenoid labrum using an extremity MR system: MR results compared to surgical findings from a multi‐center study. Journal of Magnetic Resonance Imaging 2004;19(5):623‐31. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Engebretsen 1994 {published data only}
- Engebretsen L, Craig EV, Fritts HM. Evaluation of the rotator cuff with magnetic tomography [Evaluering av skulderens rotatormuskulatur med magnettomografi]. Tidsskrift for Den Norske Laegeforening 1994;114(6):682‐3. [PubMed] [Google Scholar]
Farin 1990 {published data only}
- Farin P, Danner R, Jaroma H. The sonography of rotator cuff ruptures. The correlation of the sonographic, arthrographic and intraoperative findings in rotator cuff ruptures [Sonographie der Rotatorenmanschettenruptur. Korrelation sonographischer, arthrographischer und intraoperativer Befunde bei Rotatorenmanschettenrupturen]. ROFO. Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 1990;153(6):711‐5. [DOI] [PubMed] [Google Scholar]
Guo 2000 {published data only}
- Guo A, Fujita K, Mizuno K. Diagnostic value of arthrography and MRI in rotator cuff tears. Zhonghua Wai Ke Za Zhi [Chinese Journal of Surgery] 2000;38(4):263‐5. [PubMed] [Google Scholar]
Habermeyer 1984 {published data only}
- Habermeyer P, Mayer R, Mayr B. Comparison of arthrography, computer tomography and ultrasonography in diagnosis of rotator cuff lesions [Vergleichende Diagnostik der Rotatoren‐verletzung durch Arthrographie, Computertomographie und Sonographie]. Zeitschrift fur Unfallchirurgie, Versicherungsmedizin und Berufskrankheiten 1984;77(3):121‐9. [PubMed] [Google Scholar]
Hedtmann 1995 {published data only}
- Hedtmann A, Fett H. Ultrasonography of the shoulder in subacromial syndromes with disorders and injuries of the rotator cuff [Schultersonographie bei Subakromialsyndromen mit Erkrankungen und Verletzungen der Rotatorenmanschette]. Der Orthopäde 1995;24(6):498‐508. [PubMed] [Google Scholar]
Heininger‐Biner 2000 {published data only}
- Heininger‐Biner K, Muller M, Hertel R. Diagnosis of rotator cuff rupture: correlation of clinical findings and magnetic resonance tomography with intraoperative findings [Diagnostik der Rotatorenmanschettenruptur: Korrelation des klinischen Befundes und der Magnetresonanztomographie mit dem intraoperativen Befund]. Zeitschrift fur Orthopadie und Ihre Grenzgebiete 2000;138(6):478‐80. [DOI] [PubMed] [Google Scholar]
Kayser 2005 {published data only}
- Kayser R, Hampf S, Pankow M, Seeber E, Heyde CE. Validity of ultrasound examinations of disorders of the shoulder joint [Validitat der sonographischen Untersuchung des Schultergelenkes ‐ Prospektive, randomisierte und doppelt blinde, arthroskopisch kontrollierte Studie an 239 Fallen]. Ultraschall in der Medizin 2005;26(4):291‐8. [DOI] [PubMed] [Google Scholar]
Kenn 2000 {published data only}
- Kenn W, Hufnagel P, Muller T, Gohlke F, Bohm D, Kellner M, et al. Arthrography, ultrasound and MRI in rotator cuff lesions: a comparison of methods in partial lesions and small complete ruptures [Arthrographie, Ultraschall und MRT bei Rotatorenmanschettenlasionen ‐ ein Methodenvergleich bei Partiallasionen und kleinen kompletten Rupturen]. RoFo. Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 2000;172(3):260‐6. [DOI] [PubMed] [Google Scholar]
Kumagai 1991 {published data only}
- Kumagai H, Mikasa M, Tanaka Y, Hashimoto S. MR arthrography with intraarticular Gd‐DTPA in the diagnosis of rotator cuff tears. Japanese Journal of Clinical Radiology 1991;36(4):455‐60. [Google Scholar]
Kumagai 1992 {published data only}
- Kumagai H. MR imaging of rotator cuff tears. Nippon Igaku Hoshasen Gakkai Zasshi 1992;52(2):172‐81. [PubMed] [Google Scholar]
Kumagai 1995 {published data only}
- Kumagai H, Ito H, Kubo A. Comparison between T2*‐ and T2‐weighted images in diagnosing rotator cuff tears. Nippon Igaku Hoshasen Gakkai Zasshi 1995;55(3):133‐7. [PubMed] [Google Scholar]
Labanauskaite 2002 {published data only}
- Labanauskaite G. Usefulness of ultrasonography in the diagnosis of rotator cuff tears [Ultragarsinio tyrimo reiksme diagnozuojant peties sanario rotatoriu plysimus]. Medicina 2002;38(2):131‐4. [PubMed] [Google Scholar]
Manych 2007 {published data only}
- Manych M. MR arthrography enables accurate diagnosis of partial‐thickness rotator cuff tears [MR‐Arthrographie ermöglicht zuverlässige Diagnose]. RoFo. Fortschritte auf dem Gebiet der Rontgenstrahlen und der Bildgebenden Verfahren 2007;179(9):886. [Google Scholar]
Nagamori 1995 {published data only}
- Nagamori M, Okamura K, Usui M, Ishii S. Usefulness of MR imaging for rotator cuff tear. Hokkaido Journal of Orthopedic and Traumatic Surgery 1995;38(2):6‐9. [Google Scholar]
Qu 2008 {published data only}
- Qu N, Yao WW, Yang SX, Lu ZH. MR imaging diagnosis of shoulder joint injury. Chinese Journal of Radiology 2008;42(3):236‐41. [Google Scholar]
Rudolph 2000 {published data only}
- Rudolph J, Lorenz M, Schroder R, Sudkamp NP, Felix R, Maurer J. Indirect MR arthrography in the diagnosis of rotator cuff lesions [Indirekte MR‐Arthrographie in der Diagnostik von Rotatorenmanschettenlasionen]. RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 2000;172(8):686‐91. [PubMed] [Google Scholar]
Sakuragi 1989 {published data only}
- Sakuragi K. Morphological and clinical study of shoulder joint diseases by ultrasonography. Journal of the Japanese Orthopaedic Association 1989;63(11):1330‐42. [PubMed] [Google Scholar]
Sasaki 1991 {published data only}
- Sasaki T, Saito Y, Tarusawa K, Saikawa Y, Yodono H, Takekawa S, et al. MRI of the rotator cuff injury. Japanese Journal of Clinical Radiology 1991;36(4):461‐7. [Google Scholar]
Schedel 1990 {published data only}
- Schedel H, Hilbertz T, Fink U, Mayr B, Lehrberger K, Theermann R. Use of digital subtraction arthrography in lesions of the rotator cuff ‐‐ comparison with ultrasound [Einstz der Digitalen‐Subtraktions‐Arthrographie bei Lasionen der Rotatorenmanschette ‐ Vergleich mit Ultraschall]. Digitale Bilddiagnostik 1990;10(1):30‐5. [PubMed] [Google Scholar]
Schroder 2003 {published data only}
- Schroder RJ, Bostanjoglo M, Kaab M, Herzog H, Hidajat N, Rottgen R, et al. Accuracy of routine MRI in lesions of the supraspinatus tendon ‐ comparison with surgical findings [Treffsicherheit der nativen und kontrastverstarkten MRT im Routineeinsatz bei Supraspinatussehnenrupturen ‐ Vergleich mit operativen Ergebnissen]. RoFo. Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 2003;175(7):920‐8. [DOI] [PubMed] [Google Scholar]
Sell 1992 {published data only}
- Sell S, Konig H, Gutsche I, Kusswetter W. Nuclear magnetic resonance tomography and sonography in diagnosis of lesions of the rotator cuff [Die Kernspintomographie und Sonographie in der Diagnostik von Lasionen der Rotatorenmanschette]. Sportverletz Sportschaden 1992;6(1):20‐3. [DOI] [PubMed] [Google Scholar]
Sperner 1993 {published data only}
- Sperner G, Resch H, Golser K, Lener M, Seykora P. The value of sonography in ruptures of the rotator cuff [Die Wertigkeit der Sonographie bei Rupturen der Rotatorenmanschette]. Der Unfallchirurg 1993;96(3):119‐23. [PubMed] [Google Scholar]
Vahlensieck 1996 {published data only}
- Vahlensieck M, Sommer T. Indirect MR arthrography of the shoulder. An alternative to direct MR arthrography? [Indirekte MR‐Arthrographie der Schulter. Alternative zur direkten MR‐Arthrographie?]. Der Radiologe 1996;36(12):960‐5. [DOI] [PubMed] [Google Scholar]
Wallny 2000 {published data only}
- Wallny T, Schild RL, Perlick L, Schultz Bertelsbeck D, Schmitt O. Three‐dimensional ultrasound evaluation of the rotator cuff. Preliminary results of clinical application [Die dreidimensionale Ultraschalluntersuchung der Rotatorenmanschette. Erste Ergebnisse in der klinischen Anwendung]. Ultraschall in der Medizin 2000;21(4):180‐5. [DOI] [PubMed] [Google Scholar]
Wang 2009 {published data only}
- Wang YL, Guo XG, Cheng LQ, Wei M, Xu X, Ma L. MR image‐guided anterior direct arthrography of the shoulder. Zhongguo Gu Shang 2009;22(9):665‐7. [PubMed] [Google Scholar]
Additional references
Baring 2007
- Baring T, Emery R, Reilly P. Management of rotator cuff disease: specific treatment for specific disorders. Best Practice and Research. Clinical Rheumatology 2007;21(2):279‐94. [DOI] [PubMed] [Google Scholar]
Bianchi 2005
- Bianchi S, Martinoli C, Abdelwahab IF. Ultrasound of tendon tears. Part 1: general considerations and upper extremity. Skeletal Radiology 2005;34(9):500‐12. [DOI] [PubMed] [Google Scholar]
Biberthaler 2003
- Biberthaler P, Wiedemann E, Nerlich A, Kettler M, Mussack T, Deckelmann S, et al. Microcirculation associated with degenerative rotator cuff lesions. In vivo assessment with orthogonal polarization spectral imaging during arthroscopy of the shoulder. Journal of Bone and Joint Surgery. American Volume 2003;85‐A(3):475‐80. [PubMed] [Google Scholar]
Bigliani 1991
- Bigliani LU, Ticker JB, Flatow EL, Soslowsky LJ, Mow VC. The relationship of acromial architecture to rotator cuff disease. Clinics in Sports Medicine 1991;10(4):823‐38. [PubMed] [Google Scholar]
Bossuyt 2003
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou Paul P, Irwig LM, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ 2003;326(7379):41‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buchbinder 2013
- Buchbinder R, Staples MP, Shanahan EM, Roos JF. General practitioner management of shoulder pain in comparison with rheumatologist expectation of care and best evidence: an Australian national survey. Public Library of Science one 2013;8(4):e61243. [DOI: 10.1371/journal.pone.0061243] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bussières 2007
- Bussières AE, Peterson C, Taylor JA. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults‐‐an evidence‐based approach: introduction. Journal of Manipulative and Physiological Therapeutics 2007;30(9):617‐83. [DOI] [PubMed] [Google Scholar]
Chen 2003
- Chen AL, Shapiro JA, Ahn AK, Zuckerman JD, Cuomo F. Rotator cuff repair in patients with type I diabetes mellitus. Journal of Shoulder and Elbow Surgery 2003;12(5):416‐21. [DOI] [PubMed] [Google Scholar]
Chu 2006
- Chu H, Cole SR. Bivariate meta‐analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. Journal of Clinical Epidemiology 2006;59(12):1331‐2; author reply 1332‐3. [DOI] [PubMed] [Google Scholar]
Clark 1992
- Clark JM, Harryman DT 2nd. Tendons, ligaments, and capsule of the rotator cuff: gross and microscopic anatomy. Journal of Bone and Joint Surgery. American Volume 1992;74(5):713‐25. [PubMed] [Google Scholar]
Coghlan 2009
- Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD005619.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Crass 1985
- Crass JR, Craig EV, Bretzke C, Feinberg SB. Ultrasonography of the rotator cuff. Radiographics 1985;5(6):941‐53. [DOI] [PubMed] [Google Scholar]
De Candia 2003
- Candia A, Doratiotto S, Paschina E, Segatto E, Pelizzo F, Bazzocchi M. Real‐time compound sonography of the rotator‐cuff: evaluation of artefact reduction and image definition. Radiologia Medica 2003;105(4):308‐14. [PubMed] [Google Scholar]
De Jesus 2009
- Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta‐analysis. American Journal of Roentgenology 2009;192(6):1701‐7. [DOI] [PubMed] [Google Scholar]
De Vet 2008
- Vet HCW, Eisinga A, Riphagen II, Aertgeerts B, Pewsner D. Chapter 7: Searching for Studies. In: Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 0.4 [updated September 2008]. The Cochrane Collaboration, 2008. Available from: http://srdta.cochrane.org/handbook‐dta‐reviews.
Deeks 2009
- Deeks JJ, Bossuyt PM, Gatsonis C (editors). Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0.0. The Cochrane Collaboration, 2009. Available from: http://srdta.cochrane.org/ (accessed November 2010).
Dines 2007
- Dines DM, Moynihan DP, Dines J, McCann P. Irreparable rotator cuff tears: what to do and when to do it; the surgeon's dilemma. Journal of Bone and Joint Surgery. American Volume 2006;88(10):2294‐302. [DOI] [PubMed] [Google Scholar]
Dinnes 2003
- Dinnes J, Loveman E, McIntyre L, Waugh N. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Health Technology Assessment (Winchester, England) 2003;7(29):1‐166. [DOI] [PubMed] [Google Scholar]
Duckworth 1999
- Duckworth DG, Smith KL, Campbell B, Matsen FA 3rd. Self‐assessment questionnaires document substantial variability in the clinical expression of rotator cuff tears. Journal of Shoulder and Elbow Surgery 1999;8(4):330‐3. [DOI] [PubMed] [Google Scholar]
Dunn 2005
- Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF, et al. Variation in orthopaedic surgeons' perceptions about the indications for rotator cuff surgery. Journal of Bone and Joint Surgery. American Volume 2005;87(9):1978‐84. [DOI] [PubMed] [Google Scholar]
Favard 2007
- Favard L, Bacle G, Berhouet J. Rotator cuff repair. Joint, Bone, Spine: Revue du Rhumatisme 2007;74(6):551‐7. [DOI] [PubMed] [Google Scholar]
Fukuda 1996
- Fukuda H, Hamada K, Nakajima T, Yamada N, Tomonaga A, Goto M. Partial‐thickness tears of the rotator cuff. A clinicopathological review based on 66 surgically verified cases. International Orthopaedics 1996;20(4):257‐65. [DOI] [PubMed] [Google Scholar]
Fukuda 2003
- Fukuda H. The management of partial‐thickness tears of the rotator cuff. Journal of Bone and Joint Surgery. British Volume 2003;85(1):3‐11. [DOI] [PubMed] [Google Scholar]
Gagey 1991
- Gagey N, Desmoineaux P, Gagey O, Idy‐Peretti I, Mazas F. Contribution of MRI to the preoperative evaluation of rotator cuff tears [Apport de l'IRM dans le bilan pre‐chirurgical des lesions de la coiffe des rotateurs]. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur 1991;77(8):521‐9. [PubMed] [Google Scholar]
Galatz 2006
- Galatz LM, Silva MJ, Rothermich SY, Zaegel MA, Havlioglu N, Thomopoulos S. Nicotine delays tendon‐to‐bone healing in a rat shoulder model. Journal of Bone and Joint Surgery. American Volume 2006;88(9):2027‐34. [DOI] [PubMed] [Google Scholar]
Geraets 2009
- Geraets JJ, Jongh AC, Boeke AJ, Buis PA, Spinnewijn WE, Geijer RM, et al. Summary of the practice guideline for shoulder complaints from the Dutch College of General Practitioners. Nederlands Tijdschrift voor Geneeskunde 2009;153:A164. [PubMed] [Google Scholar]
Gerber 2000
- Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. Journal of Bone and Joint Surgery. American Volume 2000;82(4):505‐15. [DOI] [PubMed] [Google Scholar]
Hanchard 2013
- Hanchard NCA, Lenza M, Handoll HHG, Takwoingi Y. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD007427.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harryman 2003
- Harryman DT 2nd, Hettrich CM, Smith KL, Campbell B, Sidles JA, Matsen FA 3rd. A prospective multipractice investigation of patients with full‐thickness rotator cuff tears: the importance of comorbidities, practice, and other covariables on self‐assessed shoulder function and health status. Journal of Bone and Joint Surgery. American Volume 2003;85‐A(4):690‐6. [PubMed] [Google Scholar]
Johal 2008
- Johal P, Martin D, Broadhurst N. Managing shoulder pain in general practice ‐ assessment, imaging and referral. Australian Family Physician 2008;37(4):263‐5. [PubMed] [Google Scholar]
Kneeland 1986
- Kneeland JB, Carrera GF, Middleton WD, Campagna NF, Ryan LM, Jesmanowicz A, et al. Rotator cuff tears: preliminary application of high‐resolution MR imaging with counter rotating current loop‐gap resonators. Radiology 1986;160(3):695‐9. [DOI] [PubMed] [Google Scholar]
Kuhn 2007
- Kuhn JE, Dunn WR, Ma B, Wright RW, Jones G, Spencer EE, et al. Interobserver agreement in the classification of rotator cuff tears. American Journal of Sports Medicine 2007;35(3):437‐41. [DOI] [PubMed] [Google Scholar]
Le Corroller 2008
- Corroller T, Cohen M, Aswad R, Pauly V, Champsaur P. Sonography of the painful shoulder: role of the operator's experience. Skeletal Radiology 2008;37(11):979‐86. [DOI] [PubMed] [Google Scholar]
Lenza 2011
- Lenza M, Buchbinder R, Christensen R, Hanchard NCA, Faloppa F. Magnetic resonance imaging versus ultrasonography for assessing rotator cuff tears in patients with shoulder pain for whom surgery is being considered. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD009020] [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2008
- Levy O, Relwani J, Zaman T, Even T, Venkateswaran B, Copeland S. Measurement of blood flow in the rotator cuff using laser Doppler flowmetry. Journal of Bone and Joint Surgery. British Volume 2008;90(7):893‐8. [DOI] [PubMed] [Google Scholar]
Lewis 2009
- Lewis JS. Rotator cuff tendinopathy. British Journal of Sports Medicine 2009;43(4):236‐41. [DOI] [PubMed] [Google Scholar]
Mall 2010
- Mall NA, Kim HM, Keener JD, Steger‐May K, Teefey SA, Middleton WD, et al. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. Journal of Bone and Joint Surgery. American Volume 2010;92(16):2623‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martino 1998
- Martino F, Mocci A, Rizzo A, Dicandia V, Strada A, Macarini L, et al. Echography of the supraspinatus tendon: forced passive adduction maneuver [Ecografia del tendine sopraspinoso: manovra di adduzione passiva forzata]. Radiologia Medica 1998;95(4):298‐3. [PubMed] [Google Scholar]
Matava 2005
- Matava MJ, Purcell DB, Rudzki JR. Partial‐thickness rotator cuff tears. American Journal of Sports Medicine 2005;33(9):1405‐17. [DOI] [PubMed] [Google Scholar]
Matsen 2008
- Matsen FA 3rd. Clinical practice. Rotator‐cuff failure. New England Journal of Medicine 2008;358(20):2138‐47. [DOI] [PubMed] [Google Scholar]
Medicare Australia 2010
- Medicare Australia. Medicare Item Reports: Medicare Australia. https://www.medicareaustralia.gov.au/statistics/mbs_item.shtml (accessed 10 May 2010).
Melis 2010
- Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clinical Orthopaedics and Related Research 2010;468(6):1498‐505. [DOI] [PMC free article] [PubMed] [Google Scholar]
Neer 1972
- Neer CS 2nd. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. Journal of Bone and Joint Surgery. American Volume 1972;54(1):41‐50. [PubMed] [Google Scholar]
Neer 1983
- Neer CS 2nd. Impingement lesions. Clinical Orthopaedics and Related Research 1983;(173):70‐7. [PubMed] [Google Scholar]
Neri 2009
- Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. Journal of Shoulder and Elbow Surgery 2009;18(5):808‐18. [DOI] [PubMed] [Google Scholar]
Nho 2008
- Nho SJ, Yadav H, Shindle MK, Macgillivray JD. Rotator cuff degeneration: etiology and pathogenesis. American Journal of Sports Medicine 2008;36(5):987‐93. [DOI] [PubMed] [Google Scholar]
Nirschl 1989
- Nirschl RP. Rotator cuff tendinitis: basic concepts of pathoetiology. Instructional Course Lectures 1989;38:439‐45. [PubMed] [Google Scholar]
O'Connor 2005
- O'Connor PJ, Rankine J, Gibbon WW, Richardson A, Winter F, Miller JH. Interobserver variation in sonography of the painful shoulder. Journal of Clinical Ultrasound 2005;33(2):53‐6. [DOI] [PubMed] [Google Scholar]
Oh 2007
- Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clinical Orthopaedics and Related Research 2007;(455):52‐63. [DOI] [PubMed] [Google Scholar]
Ostör 2005
- Ostör AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL. Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology 2005;44(6):800‐5. [DOI] [PubMed] [Google Scholar]
Ottenheijm 2010
- Ottenheijm RP, Jansen MJ, Staal JB, Bruel A, Weijers RE, Bie RA, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: a systematic review and meta‐analysis. Archives of Physical Medicine and Rehabilitation 2010;91(10):1616‐25. [DOI] [PubMed] [Google Scholar]
Patel 2011
- Patel S, Hossain FS, Colaco HB, El‐Husseiny M, Lee MH. The accuracy of primary care teams in diagnosing disorders of the shoulder. Journal of Evaluation in Clinical Practice 2011;17(1):118‐22. [DOI] [PubMed] [Google Scholar]
Post 1983
- Post M, Silver R, Singh M. Rotator cuff tear. Diagnosis and treatment. Clinical Orthopaedics and Related Research 1983;(173):78‐91. [PubMed] [Google Scholar]
Rees 2008
- Rees JL. The pathogenesis and surgical treatment of tears of the rotator cuff. Journal of Bone and Joint Surgery. British Volume 2008;90(7):827‐32. [DOI] [PubMed] [Google Scholar]
Reilly 2006
- Reilly P, Macleod I, Macfarlane R, Windley J, Emery RJ. Dead men and radiologists don't lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Annals of the Royal College of Surgeons of England 2006;88(2):116‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reitsma 2005
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. Journal of Clinical Epidemiology 2005;58(10):982‐90. [DOI] [PubMed] [Google Scholar]
Reitsma 2009
- Reitsma JB, Rutjes AWS, Whiting P, Vlassov VV, Leeflang MMG, Deeks JJ. Chapter 9: Assessing methodological quality. Deeks JJ, Bossuyt PM, Gatsonis C (editors), Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0.0. The Cochrane Collaboration 2009. Available from: http://srdta.cochrane.org/.
Ruiz Santiago 2000
- Ruiz Santiago F, Ortega Herrera R, López Milena G, Moreno Gayá M, Cañadillas Barea L. Correlation of different imaging diagnostic methods in rotator cuff rupture. Rehabilitacion 2000;34:139–46. [Google Scholar]
Rutten 2006
- Rutten MJ, Jager GJ, Blickman JG. From the RSNA refresher courses: US of the rotator cuff: pitfalls, limitations, and artifacts. Radiographics 2006;26(2):589‐604. [DOI] [PubMed] [Google Scholar]
Seltzer 1979
- Seltzer SE, Finberg HJ, Weissman BN, Kido DK, Collier BD. Arthrosonography: gray‐scale ultrasound evaluation of the shoulder. Radiology 1979;132(2):467‐8. [DOI] [PubMed] [Google Scholar]
Shahabpour 2008
- Shahabpour M, Kichouh M, Laridon E, Gielen JL, Mey J. The effectiveness of diagnostic imaging methods for the assessment of soft tissue and articular disorders of the shoulder and elbow. European Journal of Radiology 2008;65(2):194‐200. [DOI] [PubMed] [Google Scholar]
Smith 2012
- Smith TO, Daniell H, Geere JA, Toms AP, Hing CB. The diagnostic accuracy of MRI for the detection of partial‐ and full‐thickness rotator cuff tears in adults. Magnetic Resonance Imaging 2012;30(3):336‐46. [DOI] [PubMed] [Google Scholar]
Takwoingi 2013
- Takwoingi Y, Leeflang MM, Deeks JJ. Empirical evidence of the importance of comparative studies of diagnostic test accuracy. Annals of Internal Medicine 2013;158(7):544‐54. [DOI] [PubMed] [Google Scholar]
Teefey 2005
- Teefey SA, Middleton WD, Payne WT, Yamaguchi K. Detection and measurement of rotator cuff tears with sonography: Analysis of diagnostic errors. American Journal of Roentgenology 2005;184(6):1768‐73. [DOI] [PubMed] [Google Scholar]
Van der Schouw 1995
- Schouw YT, Dijk R, Verbeek AL. Problems in selecting the adequate patient population from existing data files for assessment studies of new diagnostic tests. Journal of Clinical Epidemiology 1995;48(3):417‐22. [DOI] [PubMed] [Google Scholar]
Van Holsbeeck 1991
- Holsbeeck M, Introcaso JH. Sonography of the shoulder. In: Holsbeeck M, Introcaso JH editor(s). Musculoskeletal ultrasound. St. Louis: Mosby, 1991:265‐84. [Google Scholar]
Wendelboe 2004
- Wendelboe AM, Hegmann KT, Gren LH, Alder SC, White GL Jr, Lyon JL. Associations between body‐mass index and surgery for rotator cuff tendinitis. Journal of Bone and Joint Surgery. American Volume 2004;86‐A(4):743‐7. [DOI] [PubMed] [Google Scholar]
Whiting 2003
- Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Medical Research Methodology 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Witte 2003
- Witte DH. Magnetic Resonance Imaging in Orthopaedics. In: Canale ST editor(s). Campbell's Operative Orthopaedics. 10th Edition. Philadelphia: Mosby, 2003:123‐64. [Google Scholar]
Wolfgang 1974
- Wolfgang GL. Surgical repair of tears of the rotator cuff of the shoulder. Factors influencing the result. Journal of Bone and Joint Surgery. American Volume 1974;56(1):14‐26. [PubMed] [Google Scholar]
Yamamoto 2010
- Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, et al. Prevalence and risk factors of a rotator cuff tear in the general population. Journal of Shoulder and Elbow Surgery 2010;19(1):116‐20. [DOI] [PubMed] [Google Scholar]
Zanetti 2000
- Zanetti M, Jost B, Hodler J, Gerber C. MR imaging after rotator cuff repair: full‐thickness defects and bursitis‐like subacromial abnormalities in asymptomatic subjects. Skeletal Radiology 2000;29(6):314‐9. [DOI] [PubMed] [Google Scholar]


