Abstract
Background
The term anchorage in orthodontic treatment refers to methods of controlling unwanted tooth movement. This is provided either by anchor sites within the mouth, such as the teeth and the palate, or from outside the mouth (headgear). Recently, new methods of providing anchorage have been developed using orthodontic implants which are surgically inserted into the bone in the mouth. This is termed surgical anchorage. This is an update of a Cochrane review first published in 2007.
Objectives
To assess the effects of surgical anchorage techniques compared to conventional anchorage in the prevention of unwanted tooth movement in patients undergoing orthodontic treatment by evaluating the mesiodistal movement of upper first molar teeth. A secondary objective was to compare the effects of one type of surgical anchorage with another.
Search methods
We searched the Cochrane Oral Health Group's Trials Register (to 28 October 2013), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2013, Issue 9), MEDLINE via OVID (1946 to 28 October 2013) and EMBASE via OVID (1980 to 28 October 2013). We handsearched key international orthodontic and dental journals, and searched the trial database ClinicalTrials.gov and the World Health Organization (WHO) International Clinical Trials Registry Platform for ongoing and unpublished studies.
Selection criteria
Randomised controlled trials comparing surgical anchorage with conventional anchorage in orthodontic patients. Trials comparing two types of surgical anchorage were also included.
Data collection and analysis
At least two review authors independently and in duplicate extracted data and carried out risk of bias assessments. We contacted study authors to clarify aspects of study design and conduct, and to obtain unreported data.
Main results
Fourteen new studies were added in this update resulting in a total of 15 studies reporting data from 561 randomised patients. The studies were conducted in Europe, India, China, South Korea and the USA. The age range of patients was commonly restricted to adolescents or young adults, however the participants of two studies were from a much wider age range (12 to 54 years). The distribution of males and females was similar in eight of the studies, with a predominance of female patients in seven studies.
Eight studies were assessed to be at high overall risk of bias; six studies at unclear risk of bias; one study at low risk of bias.
Ten studies with 407 randomised and 390 analysed patients compared surgical anchorage with conventional anchorage for the primary outcome of mesiodistal movement of upper first molars. We carried out a random‐effects model meta‐analysis for the seven studies that fully reported this outcome. There was strong evidence of an effect of surgical anchorage on this outcome. Compared with conventional anchorage, surgical anchorage was more effective in the reinforcement of anchorage by 1.68 mm (95% confidence interval (CI) ‐2.27 mm to ‐1.09 mm; seven studies, 308 participants analysed) with moderate quality of evidence (one study at high overall risk of bias, five studies at unclear risk of bias, one study at low risk of bias). This result should be interpreted with some caution, however, as there was a substantial degree of heterogeneity for this comparison. There was no evidence of a difference in overall duration of treatment between surgical and conventional anchorage (‐0.15 years; 95% CI ‐0.37 years to 0.07 years; three studies, 111 analysed patients) with low quality of evidence (one study at high overall risk of bias and two studies at unclear risk of bias). Information on patient‐reported outcomes such as pain and acceptability was limited and inconclusive.
When direct comparisons were made between two types of surgical anchorage, there was a lack of evidence to suggest that any one technique was better than another.
No included studies reported adverse effects.
Authors' conclusions
There is moderate quality evidence that reinforcement of anchorage is more effective with surgical anchorage than conventional anchorage, and that results from mini‐screw implants are particularly promising. While surgical anchorage is not associated with the inherent risks and compliance issues related to extraoral headgear, none of the included studies reported on harms of surgical or conventional anchorage.
Keywords: Adolescent; Adult; Child; Female; Humans; Male; Middle Aged; Young Adult; Dental Implantation, Endosseous; Tooth Movement Techniques; Extraoral Traction Appliances; Molar; Orthodontic Anchorage Procedures; Orthodontic Anchorage Procedures/methods; Orthodontic Brackets; Orthodontic Brackets/adverse effects; Randomized Controlled Trials as Topic
Plain language summary
Reducing unwanted movement of teeth during treatment with orthodontic braces, comparing surgically placed implants as stabilisers (anchors) with other conventional methods
Review question
This review, produced by the Cochrane Oral Health Group, seeks to assess the effects of using implants surgically placed in bone in the mouth in order to stabilise (anchor) teeth during treatment with orthodontic braces and compares implants with the use of conventional methods. It also assesses the effects of different surgical anchorage techniques.
Background
Orthodontic treatment is used to correct crooked or sticking out teeth by moving the affected teeth into the correct position. The teeth are straightened by using a brace. Sometimes unwanted movement of other teeth is caused by the use of a brace and this is controlled by what is known as anchorage, or methods for stabilising these teeth. Conventionally anchorage sites are inside the mouth (intraoral) using teeth for example, or alternatively from outside the mouth (extraoral) using headgear devices attached to the head or neck. Sometimes when devices such as headgear are used there are issues with patients being reluctant to wear them, or they have been reported to cause injuries.
As an alternative to these conventional methods, surgical techniques have been developed to put mini‐screws or other types of implants into bone in the mouth to provide a firm structure for anchorage (stabilisation) to prevent the unwanted movement of teeth during orthodontic treatments.
These types of devices have become increasingly popular, however their effects have not been fully evaluated.
Study characteristics
The evidence on which this review is based was correct as of 28 October 2013. This is an update to an existing review, which included one study. Fifteen studies were included in this review involving data from 561 participants. The studies were conducted in Europe, India, China, South Korea and the USA. Most took place in university settings or training hospitals and one in a specialist orthodontic practice. Most studies contained a similar number of males and females, however there were more females than males in five studies and only females in two. The age range varied from adolescents and young adults to adults up to the age of 54 years. All participants in the studies needed a course of orthodontic treatment with additional anchorage control. None of the studies reported adverse effects.
Key results
When surgically implanted anchorage devices were compared to conventional anchorage devices, they were better in providing stabilisation for preventing unwanted movement in teeth during orthodontic treatment. There was limited information on patient‐reported outcomes such as pain and how acceptable the devices were found to be. No information was reported on adverse events.
Quality of the evidence
The quality of the evidence for the important outcomes in this review ranged from moderate to low quality. The main shortcomings of all of the studies were related to issues with their design and the way they were carried out, with insufficient and low quality reporting of the study methods and outcomes.
Summary of findings
Summary of findings for the main comparison. Surgical anchorage compared to conventional anchorage for patients undergoing orthodontic treatment.
| Surgical anchorage compared to conventional anchorage for patients undergoing orthodontic treatment | ||||||
| Patient or population: patients undergoing orthodontic treatment Settings: orthodontic clinics in university settings or specialist practice Intervention: surgical anchorage (mini‐screw or mid‐palatal implant) Comparison: conventional anchorage | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional anchorage | Surgical anchorage | |||||
| Mesiodistal movement of the upper first permanent molar | The mean mesiodistal movement of the upper first permanent molar ranged across control groups from 1.47 to 3.22 mm | The mean mesiodistal movement of the upper first permanent molar in the intervention groups was 1.68 mm lower (2.27 to 1.09 lower) | 308 (7 studies) | ⊕⊕⊕⊝ moderate1, 2 | Lower scores indicates less movement (greater reinforcement of anchorage). A change of 1.5 mm or greater is clinically important | |
| Duration of overall treatment (months) | The mean duration of overall treatment was 2.23 years (SD 0.62) | The mean duration of overall treatment (months) in the intervention group was 0.15 years shorter (0.37 years shorter to 0.07 years longer) | 111 (3 studies) | ⊕⊕⊝⊝ low3,4 | Lower scores indicate a shorter duration of overall treatment Duration estimated using a standardised mean difference of –0.25 (‐0.62 to 0.12)5 |
|
| Adverse events | This outcome was unreported in all included studies | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; SD: standard deviation | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 7 studies at overall high (1), unclear (5) and low (1) risk of bias. Substantial heterogeneity I2 78% although mean difference (MD) of 6/7 studies in favour of surgical intervention
2 Outcome incompletely reported in 2 additional studies at overall high risk of bias (both studies reported in favour of surgical anchorage) and not reported in 1 study at overall high risk of bias
3 Small studies likely underpowered; imprecision of result
4 2 studies at unclear risk of bias, 1 study at high risk of bias
5 Representative study to re‐express standardised mean difference in years (Chesterfield 2007)
Background
Description of the condition
Many children and adolescents present for orthodontic treatment with crooked or prominent teeth. Treatment to align the teeth is conventionally provided using fixed orthodontic appliances, with the extraction of teeth and the use of either an intra‐ or extraoral appliance to provide support to the molar teeth (anchorage reinforcement) as the fixed appliance aligns the anterior teeth (Mitchell 2001).
Anchorage in orthodontics is defined as the prevention of unwanted tooth movement. Traditionally this may be provided from anchor sites within the mouth (intraoral anchorage) or from outside the mouth (extraoral anchorage) (Mitchell 2001). Intraoral anchor sites include teeth or other oral structures. Extraoral anchorage is achieved with headgear, using the back of the head or the neck.
Intraoral anchorage can be supplemented by securing teeth together by means of metal wires, such as transpalatal arches or lingual arches. Anchorage may also be supplemented by using elastic traction to the opposing arch. This is termed intermaxillary anchorage (Mitchell 2001).
While extraoral anchorage may be a more effective method of preventing anchor tooth movement than intraoral methods, there are concerns about patient compliance with headgear (Cureton 1993) and issues over patient safety. For example, Samuels has described a range of soft tissue and eye injuries associated with headgear (Samuels 1996). In a few cases this has resulted in the loss of an eye (Booth‐Mason 1988; Samuels 1994; Samuels 1996). A related Cochrane systematic review has assessed the effects of conventional distalis ing appliances developed to overcome the limitations of headgear (Jambi 2013).
Another method of reinforcing anchorage has been developed using surgical techniques. For example, Gainsforth and Higley suggested the use of metallic screws as anchors as long ago as 1945 (Gainsforth 1945). Melsen experimented with anchorage from wires passed through the zygomatic arch in cases where posterior teeth were absent or of poor quality (Melsen 1998). A recent development has been the modification of dental implants in which devices are surgically inserted into the alveolar bone where they become osseointegrated (Kanomi 1997). This new technique could have an important role in orthodontic treatment as it may offer the possibility of circumventing most of the shortcomings of traditional anchorage methods.
Description of the intervention
All surgical techniques for reinforcing anchorage use the bone as the anchor site, which is considered a solid, stable structure. Types of surgical anchorage include mini‐screw implants, mini‐plates and mid‐palatal implants (Prabhu 2006). The mini‐screw implant is a modification of screws used for fixation of maxillofacial fractures. Although they have varying lengths and diameters, they are generally smaller than maxillofacial fixation screws hence the term 'mini'. Another type of implant is placed in the bone in the middle of the palate and these are called mid‐palatal implants.
Both these types of implants can be placed by the orthodontist or the oral surgeon. The anchorage device can be placed before the start of treatment, at the beginning or during the space closure phase of treatment.
How the intervention might work
As the surgical anchorage device is fixed to the bone it is proposed that it provides a stable point from which anchorage can be provided. The implants provide stability either by mechanical retention (mini‐plates), osseointegration (mid‐palatal implants), or both (mini‐screw implants) (Prabhu 2006).
Why it is important to do this review
The two most common conventional methods of providing anchorage reinforcement have been headgear and palatal arches. Surgical anchorage has the following potential advantages over conventional anchorage reinforcement.
Active compliance by the wearer is eliminated.
Surgical appliances are not associated with the injuries that can result from wearing conventional anchorage appliances.
Absolute anchorage may be provided.
Recently the use of surgical anchorage has become increasingly popular with what may be considered to be lack of high level evidence to underpin its use. A systematic review with formal quality assessment to standardised criteria is needed to evaluate the effects of these types of surgical anchorage techniques.
This is an update of a Cochrane review first published in 2007.
Objectives
The primary objective of this review was to assess the effects of surgical anchorage techniques compared to conventional anchorage in the prevention of unwanted tooth movement in patients undergoing orthodontic treatment by evaluating the mesiodistal movement of upper first molar teeth. A secondary objective was to compare the effects of one type of surgical anchorage with another.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel group, randomised, controlled trials in which surgically assisted anchorage reinforcement techniques were used during orthodontic treatment. There was no restriction on language of publication. Where studies were reported in abstract form, the literature was searched for the full publication. Split‐mouth trials were excluded because the nature of orthodontic treatment precludes both sides of the mouth from being independent of each other.
Types of participants
Patients of any age undergoing orthodontic treatment with fixed appliances and requiring surgical or conventional anchorage.
Types of interventions
Mid‐palatal implants, onplants, mini‐screw implants, spider screws, titanium plates and zygomatic wires were considered under the term surgically assisted means of reinforcing anchorage.
The control group included patients with anchorage supported by conventional means including headgear, chin caps, face masks, transpalatal arches (including Nance buttons), lingual arches and interarch elastics.
We also included studies comparing two methods of surgically assisted anchorage.
Types of outcome measures
The primary outcome measure was the mesiodistal movement of upper first molars (in mm). The secondary outcome measures were residual overjet, success or failure of the anchorage device, duration of active treatment, duration of space closure, number of visits, patient perceptions (pain and discomfort), acceptability of the anchorage device, adverse effects and economic factors.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
the Cochrane Oral Health Group's Trials Register (to 28 October 2013) (Appendix 1);
the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2013, Issue 9) (Appendix 2);
MEDLINE via OVID (1946 to 28 October 2013) (Appendix 3);
EMBASE via OVID (1980 to 28 October 2013) (Appendix 4).
No restrictions were placed on the language or date of publication when searching the electronic databases.
Detailed search strategies were developed for each database. Individual search strategies were based on the search strategy developed for MEDLINE (Appendix 3) but revised appropriately for each database. The MEDLINE search used a combination of controlled vocabulary and free text terms in conjunction with the Cochrane highly sensitive search strategy for identifying reports of randomised controlled trials (RCTs) (as published in box 6.4.c in the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0, updated March 2011) (Higgins 2011). The search of EMBASE was linked to the Cochrane Oral Health Group filter for identifying RCTs.
Searching other resources
Handsearching
The following journals have been identified for handsearching for this review. Journal issues that had not already been searched as part of the Cochrane Oral Health Group's journal handsearching programme (see the Cochrane Masterlist for journals searched to date) were handsearched:
American Journal of Orthodontics and Dentofacial Orthopedics (2005 to January 2013);
The Angle Orthodontist (2007 to January 2013);
Clinical Implant Dentistry and Related Research (2003 to December 2012);
Clinical Oral Implant Research (2001, 2003 to December 2012);
European Journal of Orthodontics (2006 to December 2012);
International Journal of Oral and Maxillofacial Implants (2004 to December 2012);
Journal of Orthodontics (formerly British Journal of Orthodontics) (2008 to December 2012);
Journal of Dental Research (1999 to 2000, 2004 to January 2013);
Journal of Dentistry (2004 to December 2012);
Journal of Clinical Orthodontics (1991 to December 2012);
Orthodontics and Craniofacial Research (2000 to November 2012) (Clinical Orthodontics and Research (1998 to 2001));
Seminars in Orthodontics (2005 to December 2012).
Grey literature and trial registries
In addition to contacting authors, we approached manufacturers of implant products used in orthodontics and asked them to provide us with information concerning unpublished or ongoing studies.
We also checked the bibliographies of potentially relevant clinical trials for references to trials published outside the handsearched journals. In addition, non‐Cochrane systematic reviews were checked for potentially relevant studies.
Trial registries were searched to identify ongoing studies. The most recent search for all trial registries was October 2013. We searched the following:
World Health Organization (WHO) International Clinical Trials Registry Platform;
the International Federation of Pharmaceutical Manufacturers & Associations (IFMPA) clinical trials portal (http://clinicaltrials.ifpma.org/clinicaltrials/no_cache/en/clinical‐trial‐advanced‐search/index.htm) (Appendix 6);
Current Controlled Trials (isrctn.org) (Appendix 7).
Data collection and analysis
Selection of studies
At least two review authors independently examined the titles and abstracts of identified studies; any report that was clearly not relevant was excluded. We retrieved full text documents of potentially relevant studies and assessed them for eligibility according to the criteria for considering studies for this review. We resolved any disagreements by open discussion, occasionally arbitrated by an independent assessor. If information was unclear in study reports on study eligibility, we contacted the study investigators. Final decisions on study inclusion were made through discussion.
There were no language restrictions on the studies to be retrieved. Where the report was in a language other than English, a translation was sought.
Data extraction and management
We developed and piloted a more detailed data extraction form for use in this update. It contained information on methods, participants, interventions, primary and secondary outcomes and reported results. Data extraction was performed independently and in duplicate by three review authors. One form was used as the master form and any additions were added to it as appropriate. We resolved disagreements by discussion.
When we found that there was incomplete reporting of data, we contacted the study authors in an attempt to obtain the data.
Assessment of risk of bias in included studies
We used the Cochrane risk of bias tool to assess the potential bias of the studies. This was done independently and in duplicate by two review authors as part of the data extraction process. We investigated six specific domains: sequence generation, allocation concealment, blinding of the outcome assessor, incomplete outcome data, selective outcome reporting and 'other bias'. Blinding of patients and operators was considered unfeasible due to the nature of the interventions, however there was potential for assessment and detection bias.
For selective reporting we considered both selective reporting of outcomes and selective reporting of study data. Where the primary outcome of this review was not reported but could reasonably have been expected to be recorded and reported then the study was judged to be at high risk of bias for this domain. Where the protocol of the primary study was not available then the study was judged to be at unclear risk of bias because of the uncertainty about reporting all intended outcomes. Selective reporting of study data, such as incomplete reporting of summary statistics, was considered high risk only in relation to the primary outcome. The overall judgement on risk of bias in this domain was given according to the highest risk of bias identified.
For each study, each domain was assessed as being at low, high or unclear risk of bias as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Higgins 2011). Additional information provided by the authors of the primary studies was taken into account where appropriate. A risk of bias table was completed for each included study. These results were also presented graphically.
The overall risk of bias for each study was assessed as follows: low risk of bias if all domains were low, unclear if one or more was unclear, and high if one or more domain was high.
Measures of treatment effect
For dichotomous outcomes, the estimate of effect was expressed as risk ratio (RR); for continuous outcomes, the estimate of effect was expressed as the mean difference (MD) if studies reported an outcome using the same scales or standardised mean difference (SMD) if studies reported an outcome using different scales. The 95% confidence interval (95% CI) was calculated alongside the effect estimate. Where insufficient information was reported to enable these effect measures to be calculated a narrative report of the summary measures was provided.
Unit of analysis issues
When we identified the reporting of outcomes at multiple time points, the most common or clinically relevant time point or both were used for data extraction.
Dealing with missing data
Where data were not available in the printed report, or where the data were unclear, we contacted the corresponding author of the study to obtain the missing data. No studies were excluded on the basis of missing data and no imputations were carried out for missing data.
Assessment of heterogeneity
Clinical heterogeneity was assessed on the basis of the participants and the interventions in each study. A meta‐analysis was undertaken when there were studies with sufficient similarities in the participants, interventions and outcomes. Statistical heterogeneity was assessed using the Chi2 test for heterogeneity (P value < 0.1) and the I2 statistic. The I2 values range from 0% (may not be important) to 100% (considerable heterogeneity). The importance of the observed value of I2 depends on: (i) magnitude and direction of effects and (ii) strength of evidence for heterogeneity (for example P value from the Chi2 test) (Higgins 2011).
Assessment of reporting biases
Publication bias was not assessed in this review.
Data synthesis
We carried out a random‐effects model meta‐analysis when there were more than three studies and pooling of the data was clinically and statistically appropriate. In meta‐analyses with two or three studies, a fixed‐effect model analysis was undertaken.
In multi‐arm studies with more than two intervention groups, only single pairwise comparisons were made. When we identified studies with multiple groups that were all relevant, clinically similar intervention and control groups were combined into a single intervention or control group respectively. For continuous outcomes, we combined means and standard deviations using the formulae described in the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (Higgins 2011). For dichotomous outcomes, both the sample sizes and the numbers of people with events were summed across groups.
For comparisons where a meta‐analysis could not be carried out, we provided a narrative reporting of the summary measures and treatment effects.
Subgroup analysis and investigation of heterogeneity
We undertook a meta‐analysis comparing all types of surgical anchorage to all types of conventional anchorage for the planned outcomes found in the studies. In addition, subgroup analysis was carried out to investigate the effects of different types of surgical anchorage appliances compared to conventional anchorage.
Sensitivity analysis
Sensitivity analyses were not undertaken.
Presentation of main results
A summary of findings table was developed for the primary outcomes of this review using the GRADE profiler software. The quality of the evidence was assessed with reference to the overall risk of bias of the included studies, the directness of the evidence, the inconsistency of the results, the precision of the estimates, the risk of publication bias and the magnitude of the effect. The quality of the evidence was categorised as high, moderate, low or very low for the primary outcomes of mesiodistal movement, duration of overall treatment and adverse events.
Results
Description of studies
Results of the search
The initial search strategy for the original review was undertaken in November 2004. We identified 157 records of which 147 were rejected after examination of the titles and abstracts. Ten studies were selected for more detailed evaluation of the full publications. None fulfilled the criteria for inclusion. One trial (Chesterfield 2007) meeting the inclusion criteria was identified through personal contact with the authors whilst the review was in preparation.
The search was last updated in October 2013 and the results are presented graphically (Figure 1). We identified a total of 423 records from electronic resources and 9 from other resources. After removing duplicates, 291 records remained of which 238 were excluded after examination of the titles and abstracts. Most of these were excluded because the interventions were clearly not relevant or the studies were not randomised controlled trials.
1.
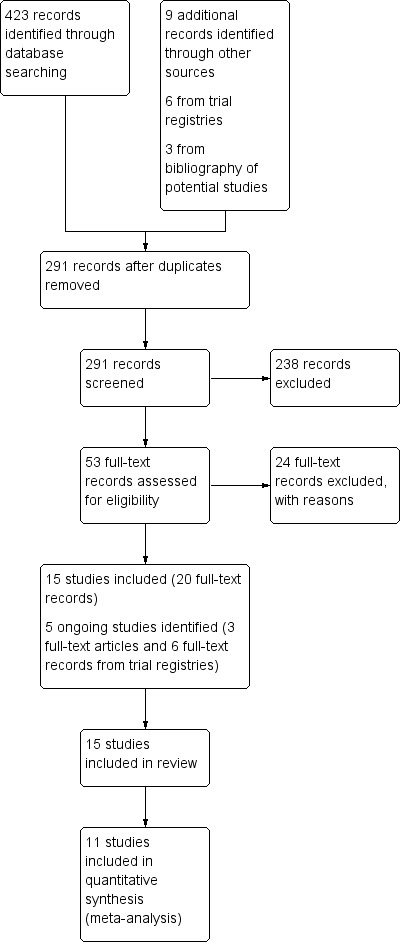
Study flow diagram.
We assessed 53 full text records for eligibility. Fifteen studies, involving data from 543 analysed participants, were included in this review. Five ongoing studies were identified: Bearn 2008 (ISRCTN 29710460; UKCRN ID 7460); Biavati/ Migliorati 2011 (ClinicalTrials.gov: NCT01717417); Jung 2007 (ISRCTN 97142521); Miller 2009 (ClinicalTrials.gov: NCT01025141); Sandler 2008 (ClinicalTrials.gov: NCT00995436).
Included studies
The last published version of this review included one study (Chesterfield 2007) which compared mid‐palatal implants versus headgear in patients with Class II Division 1 malocclusions deemed to have an 'absolute anchorage' requirement. This study with 47 participants analysed was assessed as at low risk of bias. The present update has added 14 studies. A total of 15 studies with 561 randomised patients (543 analysed patients) were included in this update. Summary details of the studies are given in the Characteristics of included studies table.
Characteristics of the trial settings
Fifteen studies involving data from 543 analysed participants were included in this review: 13 were two‐arm studies, one a three‐arm study (Turkoz 2011) and one a four‐arm study (Feldmann 2007). Thirteen trials were conducted in university settings or training hospitals with patients attending a dental clinic, the Lehnen 2011 study was conducted in a specialist orthodontic practice, and the setting of the Maddalone 2010 study was not stated. Seven trials were carried out in European countries (Borsos 2008; Borsos 2012; Chesterfield 2007; Feldmann 2007; Lehnen 2011; Maddalone 2010; Turkoz 2011), three were carried out in India (Basha 2010; Sharma 2012; Upadhyay 2008), three in China (Liu 2009; Ma 2008; Shi 2008), one in South Korea (Bechtold 2013) and one in the USA (Jackson 2008). Fourteen studies were single‐centre trials and one (Chesterfield 2007) was carried out in two centres.
Characteristics of participants
Seven studies recruited adolescent children (Borsos 2008; Borsos 2012; Chesterfield 2007; Feldmann 2007; Lehnen 2011; Sharma 2012; Turkoz 2011) and six studies recruited young adults (Basha 2010; Bechtold 2013; Liu 2009; Ma 2008; Shi 2008; Upadhyay 2008). Two studies included adults up to the age of 48 years (Jackson 2008) and 54 years (Maddalone 2010).
The gender distribution was comparable in most of the trials (Borsos 2008; Borsos 2012; Feldmann 2007; Jackson 2008; Lehnen 2011; Ma 2008; Turkoz 2011). However, there was a clear dominance of female patients in five studies (Bechtold 2013; Chesterfield 2007; Liu 2009; Sharma 2012; Shi 2008) and two studies recruited only female participants (Basha 2010; Upadhyay 2008). The gender distribution was not reported in one study (Maddalone 2010).
Characteristics of the interventions
Ten studies compared the effects of surgical anchorage to conventional anchorage, three studies compared mid‐palatal implants to conventional anchorage (Borsos 2012; Chesterfield 2007; Feldmann 2007), and seven studies compared mini‐screw implants to conventional anchorage (Basha 2010; Liu 2009; Ma 2008; Maddalone 2010; Sharma 2012; Shi 2008; Upadhyay 2008).
The direct comparisons of surgical interventions were: early and delayed loading of the same mini‐screw implants (Borsos 2008; Jackson 2008); pre‐drilling and self drilling mini‐screw implants (Lehnen 2011; Turkoz 2011); and single and dual mini‐screw implants (Bechtold 2013).
Characteristics of the outcomes
Additional Table 2 provides a summary of all of the outcomes relevant to this review as reported by each study.
1. Outcomes found in each of the included studies.
| STUDY |
Basha 2010 |
Bechtold 2013a |
Borsos 2008a |
Borsos 2012 |
Chesterfield 2007 |
Feldmann 2007 |
Jackson 2008a |
Lehnen 2011a |
Liu 2009 |
Ma 2008 |
Maddalone 2010 |
Sharma 2012 |
Shi 2008 | Turkoz 2011a |
Upadhyay 2008 |
| OUTCOME | |||||||||||||||
| Mesial movement of upper first molar | yes | yes | no | yes | yes | yes | no | no | yes | no | yes | yes | yes | no | yes |
| Residual overjet at the end of treatment | no | no | no | no | no | no | no | no | no | no | no | no | no | no | no |
| Success/failure of anchorage device | yes | yes | yes | no | yes | yes | yes | no | no | no | yes | no | no | yes | yes |
| Duration of active treatment | no | no | no | yes | yes | no | no | no | yes | no | no | no | no | no | no |
| Duration of space closure | yes | yes | no | yes | no | no | no | no | no | no | no | no | no | no | yes |
| Number of visits | no | no | no | no | yes | no | no | no | no | no | no | no | no | no | no |
| Patient perception (pain/discomfort) | no | no | no | no | yes | yes | no | yes | no | no | no | no | no | no | no |
| Acceptability | no | no | no | no | no | yes | no | no | no | no | no | no | no | no | no |
| Adverse effects | no | no | no | no | no | no | no | no | no | no | no | no | no | no | no |
| Economic factors | no | no | no | no | no | no | no | no | no | no | no | no | no | no | no |
aThese studies compared 2 types of surgical anchorage
Studies comparing surgical anchorage to conventional anchorage
The primary outcome for this comparison was the movement of the upper first molar in a mesial or distal direction. This was measured at different time points:
when anchorage reinforcement was no longer needed (Chesterfield 2007);
at the end of levelling and alignment and at the end of space closure (including and excluding the levelling and alignment phase) (Feldmann 2007);
from the start of treatment to the end of space closure (Sharma 2012);
at the end of space closure or canine retraction (not including levelling and alignment) (Basha 2010; Borsos 2012; Upadhyay 2008);
at the start and end of active orthodontic treatment (Borsos 2012; Liu 2009; Shi 2008);
from the beginning of space closure to four months later (Maddalone 2010).
All studies measured molar movement on lateral cephalometric radiographs except for Maddalone 2010 in which molar movement was measured clinically using the head of the mini‐screw implant as a reference point.
No studies reported on residual overjet at the end of treatment.
Treatment 'success' was reported in five studies (Basha 2010; Chesterfield 2007; Feldmann 2007; Maddalone 2010; Upadhyay 2008); duration was reported in five studies, as duration of the course of orthodontic treatment (Borsos 2012; Chesterfield 2007; Liu 2009) or space closure (Basha 2010; Borsos 2012; Upadhyay 2008). The number of visits was reported in one study (Chesterfield 2007).
Two studies (Chesterfield 2007; Feldmann 2007) reported on patient perception in terms of pain and discomfort and acceptability.
No studies reported on adverse effects and economic evaluation.
One study (Ma 2008) did not report any of the outcomes of interest to this review.
Studies comparing two types of surgical anchorage
One study (Bechtold 2013) reported on the primary outcome of movement of the upper first molar in a mesial or distal direction at the end of space closure. No studies reported on the residual overjet at the end of treatment.
Four studies reported on the success of the anchorage device as defined by histologic bone‐implant contact (Borsos 2008) and implant stability (Bechtold 2013; Jackson 2008; Turkoz 2011).
One study reported on the duration (space closure (Bechtold 2013)). No studies reported on the number of visits.
Patient perception was reported in one study (Lehnen 2011).
Acceptability, economic factors and adverse effects were not reported in any of the studies.
Excluded studies
Summary details are given in the Characteristics of excluded studies table. We contacted the corresponding authors of five studies to enquire about issues relating to study eligibility. In four studies replies indicated that the allocation of the interventions in the studies was not random; there was no reply from the author of the fifth study. After examination of full text records we excluded 24 records for the following reasons:
not truly randomised or not a randomised controlled trial (RCT) (confirmed following contact with the authors (Gelgor 2007; Lee 2011; Upadhyay 2008‐2; Upadhyay 2012)) (n = 13);
surgical anchorage was not included as an intervention (n = 6);
randomisation did not occur between two types of anchorage reinforcement (n = 2);
split‐mouth study (Garfinkle 2008) (n = 1);
trial with a single trial arm (n = 1);
no fixed appliance in the duration of the trial (Schatzle 2009) (n = 1).
Ongoing studies
Summary details are given in the Characteristics of ongoing studies table.
We identified five ongoing studies: four studies are comparing surgical anchorage to conventional anchorage (Bearn 2008; Biavati/ Migliorati 2011; Miller 2009; Sandler 2008), and one is comparing two types of surgical anchorage (early and delayed loading of Orthosystem type II implants) (Jung 2007). The number of participants recruited ranges from 45 to 124. All studies are recruiting males and females; one study is recruiting adolescents aged from 12 to 17 years only (Sandler 2008) and two studies are recruiting growing and non‐growing participants (Biavati/ Migliorati 2011; Miller 2009); the age of participants in the remaining trials is not stated. Two are three‐arm trials comparing mini‐screw implants to headgear and transpalatal arches (Bearn 2008; Sandler 2008) and the remaining are two‐arm trials comparing mini‐screw implants to conventional anchorage. Four of these studies measure anchorage loss as a primary outcome; it is not clear if the remaining study measures this outcome as part of assessing treatment efficacy (Miller 2009). Secondary outcomes include success of the anchorage device, peer assessment rating (PAR) index, American Board of Orthodontics (ABO) scores, patient perception, treatment process, soft tissue health, root resorption, bone quality, amount of extraction space closure, angle classification of canines and parallelism of the dental axis.
Risk of bias in included studies
The overall risk of bias assessments for all the included studies are shown in Figure 2 and Figure 3. Eight studies (Basha 2010; Borsos 2008; Feldmann 2007; Jackson 2008; Lehnen 2011; Ma 2008; Maddalone 2010; Turkoz 2011) were assessed as at high risk of bias overall, and in six studies (Bechtold 2013; Borsos 2012; Liu 2009; Sharma 2012; Shi 2008; Upadhyay 2008) the overall risk of bias was unclear. One study (Chesterfield 2007) was assessed as at overall low risk of bias.
2.
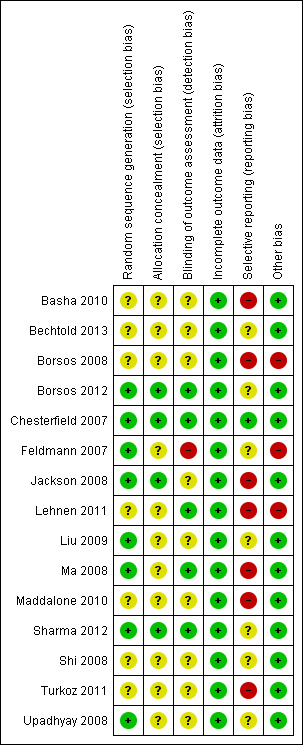
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
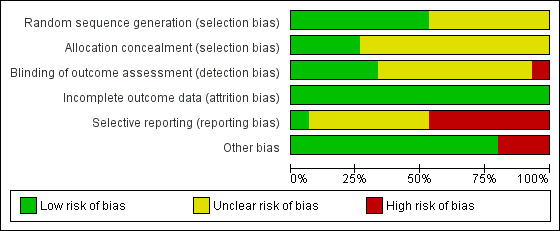
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Four studies clearly reported the method of sequence generation and allocation concealment (Borsos 2012; Chesterfield 2007; Jackson 2008; Sharma 2012) and were assessed as at low risk of selection bias. Four studies clearly reported the method of random sequence generation but allocation concealment was unclear (Feldmann 2007; Liu 2009; Ma 2008; Upadhyay 2008). In seven studies the methods of both random sequence generation and allocation concealment were unclear and these studies were assessed as at unclear risk of selection bias.
Blinding
It is not always possible to blind the clinician and the patient to the intervention in studies assessing the effects of orthodontic appliances. It is sometimes possible to carry out blinded outcome assessment. We assessed five studies at low risk of detection bias (study level), where the implant type was concealed or obscured (Borsos 2012; Chesterfield 2007; Sharma 2012) and assessment of the outcome was carried out by individuals not associated with the study (Chesterfield 2007; Lehnen 2011; Ma 2008; Sharma 2012).
We assessed one study (Feldmann 2007) at high risk of detection bias as the orthodontic appliances were clearly visible in the radiographs being measured.
We assessed nine studies at unclear risk of detection bias due to the lack of reporting of methods used to ensure blinded outcome assessment (Basha 2010; Bechtold 2013; Borsos 2008; Jackson 2008; Liu 2009; Maddalone 2010; Shi 2008; Turkoz 2011) or it was unclear if there was an attempt to mask the intervention on the radiographs (Upadhyay 2008).
Incomplete outcome data
This domain was assessed on a study level. All 15 studies were at low risk of attrition bias either because all randomised patients were accounted for or there were a small number of drop‐outs.
All randomised patients were accounted for in the analysis in nine studies (Basha 2010; Bechtold 2013; Borsos 2008; Borsos 2012; Lehnen 2011; Liu 2009; Ma 2008; Maddalone 2010; Sharma 2012). In six studies the number of post‐randomisation drop‐outs was small or unrelated to the intervention or the outcome or both (Chesterfield 2007; Feldmann 2007; Jackson 2008; Shi 2008; Turkoz 2011; Upadhyay 2008).
Selective reporting
We were able to locate a published protocol for only one study (Chesterfield 2007). All intended outcomes were reported in the full trial paper except for 'inflammation of the peri‐implant tissues'. Correspondence with the authors confirmed that this was a change from the protocol and this outcome was not measured. We assessed this study as at low risk of reporting bias.
We assessed five studies as at high risk of reporting bias through lack of reporting of the primary outcome of this review (Borsos 2008; Jackson 2008; Lehnen 2011; Ma 2008; Turkoz 2011). In four of these studies the objective of the trial was not to investigate the effects on anchorage but to provide alternatives in the way they are used clinically (Borsos 2008; Jackson 2008; Lehnen 2011; Turkoz 2011). Two studies (Basha 2010; Maddalone 2010) that were assessed at high risk of reporting bias incompletely reported the molar movement outcome (standard deviations omitted). We did not consider incomplete reporting of secondary outcomes as a criterion for an assessment of high risk of reporting bias (Borsos 2008; Feldmann 2007; Lehnen 2011; Upadhyay 2008).
We could not locate published protocols for seven studies (Bechtold 2013; Borsos 2012; Feldmann 2007; Liu 2009; Sharma 2012; Shi 2008; Upadhyay 2008); these were assessed at unclear risk of reporting bias.
Other potential sources of bias
Two studies were assessed at high risk of other potential sources of bias due to the use of restricted randomisation in unblinded studies conducted in single centres. Two single‐centre studies used fixed‐size block randomisation with a relatively small block size of four to six (Borsos 2008; Feldmann 2007) and unclear methods of allocation concealment. In such instances it is possible to predict future treatment allocation with relative accuracy.
One study (Lehnen 2011) was assessed at high risk of other potential sources of bias due to differences in the methods of pain relief (injection techniques) given in the same appointment.
In all other studies included in this review no other potential sources of bias were identified.
Effects of interventions
See: Table 1
For the purposes of analysis, the comparisons were as follows:
trials comparing surgical anchorage to conventional anchorage;
trials comparing two types of surgical anchorage (head to head trials).
Additional Table 2 lists the presence or absence in the primary studies of the outcomes that are relevant to this review.
Comparison of surgical anchorage to conventional anchorage
Ten studies with 407 randomised and 390 analysed patients compared a type of surgical anchorage to a type of conventional anchorage (Basha 2010; Borsos 2012; Chesterfield 2007; Feldmann 2007; Liu 2009; Ma 2008; Maddalone 2010; Sharma 2012; Shi 2008; Upadhyay 2008). Summary results are presented in the Table 1.
Primary outcome
Mesiodistal movement of the upper first molar teeth
Seven studies (Borsos 2012; Chesterfield 2007; Feldmann 2007; Liu 2009; Sharma 2012; Shi 2008; Upadhyay 2008) with 308 analysed patients were included in a random‐effects model meta‐analysis of surgical anchorage versus conventional anchorage for mesiodistal movement of upper first molar teeth (Figure 4). The conventional anchorage methods included headgear, transpalatal arches, banding of second molars, and application of differential moments. There was strong evidence in favour of surgical anchorage on this outcome, with an overall mean difference (MD) of ‐1.68 mm in molar movement (95% confidence interval (CI) ‐2.27 to ‐1.09). There was a substantial amount of heterogeneity (Tau2 = 0.44; Chi2 = 27.37, degrees of freedom (df) = 6, P value < 0.001; I2 = 78%). The range of effects within the confidence interval comprised only beneficial effects of surgical anchorage that were of clinical importance. However, these results should be interpreted with caution due to the high level of heterogeneity.
4.
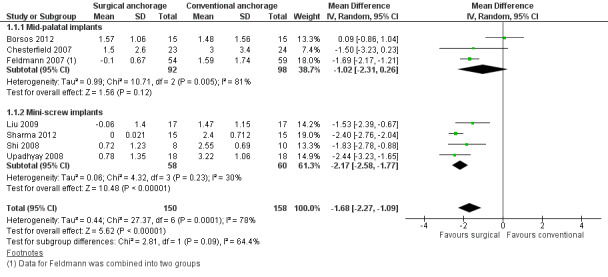
Forest plot of comparison: 1 Surgical anchorage versus conventional anchorage, outcome: 1.1 Mesiodistal movement of the upper first permanent molar.
We then analysed the data according to type of surgical intervention. For mid‐palatal implants (three studies, 190 patients analysed) there was an overall MD of ‐1.02 mm in molar movement favouring surgical anchorage (95% CI ‐2.31 to 0.26; Tau2 = 0.99; Chi2 = 10.71, df = 2, P value = 0.005; I2 = 81%); for the mini‐screw implants (four studies, 118 patients analysed) there was an overall MD of ‐2.17 mm in molar movement favouring surgical intervention (95% CI ‐2.58 to ‐1.77; Tau2 = 0.06; Chi2 = 4.32, df = 3, P value = 0.23; I2 = 30%).
There was some evidence of a difference in effect according to subgroup (P value = 0.09), with a greater and more precise effect estimate for the meta‐analysis of mini‐screw implants than the mid‐palatal implants. Moreover, there was greater consistency of results for the mini‐screw subgroup with all included trials showing evidence of a favourable effect of mini‐screws.
We were unable to include three studies in the meta‐analysis due to incomplete reporting of this outcome (Basha 2010; Ma 2008; Maddalone 2010). Two of these studies (Basha 2010; Maddalone 2010) did not report standard deviations for the surgical implant arm of the trial. Both studies reported a result in favour of surgical anchorage for mesiodistal movement of the upper first molar. The mean anchorage loss was 1.73 mm (standard deviation (SD) 0.43) in the conventional anchorage group and 0 mm in the surgical anchorage (mini‐screw) group (Basha 2010). One study (Ma 2008) did not report mesiodistal movement.
Secondary outcomes
Success of anchorage device
Five studies reported on the success of surgical anchorage compared to conventional anchorage (Basha 2010; Chesterfield 2007; Feldmann 2007; Maddalone 2010; Upadhyay 2008). The number of successes, the definition of success and the types of anchorage devices used in each of these studies are summarised in Additional Table 3. Due to the variability in the definition of this outcome measure and incomplete outcome reporting we did not pool the results of these studies.
2. Success rates of surgical appliances.
| Study | Type of anchorage device | Definition of success/failure | Success rate |
| Basha 2010 | Mini‐implants | Loosening of the mini‐screw implants and subsequently replaced | 71.43% (10/14) |
| Transpalatal arch | Success not measured | N/A | |
| Chesterfield 2007 | Orthosystem mid‐palatal implant | Orthodontic failure: failure after orthodontic loading, patients did not end up with implant‐assisted anchorage | 91.30% (21/23) |
| Headgear | Patient did not end up with headgear/headgear did not provide sufficient anchorage | 87.50% (21/24) |
|
| Feldmann 2007 | Nobel‐Biocare onplant | Successful anchorage comprises anchorage loss of less than 1 mm, no failures of osseointegration or failures during anchorage system placement, and no drop‐outs after the treatment started | 82.76% (24/29) |
| Orthosystem mid‐palatal implant | 93.33% (28/30) |
||
| Headgear | 46.67% (14/30) |
||
| Palatal arch | 27.59% (8/29) |
||
| Maddalone 2010 | Mini‐screw implant | Loosening of the mini‐implant | 84.21% (16/19) |
| Elastomeric chains or NiTi springs | Success not measured | N/A | |
| Upadhyay 2008 | Mini‐screw implant | Success: complete stability throughout the retraction phase Failure: loose and subsequently replaced |
93.05% (67/72) |
| Conventional anchorage | Success not measured | N/A |
Two studies provided complete data comparing the success of surgical anchorage to that of conventional anchorage (Chesterfield 2007; Feldmann 2007). The results of these studies were not pooled due to substantial clinical differences in the definitions of success of the anchorage devices but are reported as a narrative (Additional Table 3). In the first study (47 patients analysed), the success of the anchorage device was high in both study arms, with a 91% success rate for surgical anchorage and 88% success rate for conventional anchorage (Chesterfield 2007). With surgical anchorage (Orthosystem mid‐palatal) reasons for failures were: failure after orthodontic loading, patients did not end up with implant‐assisted anchorage. With conventional anchorage (headgear) reasons for failures were: patients did not end up with headgear, or headgear did not provide sufficient anchorage. In the second study (118 patients analysed) the proportion of successful outcomes was greater in the combined surgical anchorage groups than in the combined conventional anchorage groups (Feldmann 2007). Reasons for failure with surgical anchorage (Nobel Biocare onplants and Orthosystem implants) were: failure of osseointegration, technical problems with the implants, discontinuation of treatment due to poor oral hygiene, and anchorage loss more than 1 mm. Reasons for failure with conventional anchorage (headgear and palatal arches) were: anchorage loss of more than 1 mm, patients discontinued headgear, or headgear did not provide sufficient anchorage.
Three studies reported the success of the surgical anchorage arm of the study only (Basha 2010; Maddalone 2010; Upadhyay 2008), again with variability in definitions of success and failure.
Five studies did not report this outcome (Borsos 2012; Liu 2009; Ma 2008; Sharma 2012; Shi 2008).
Duration of active treatment
The duration of the complete course of orthodontic treatment was reported in three studies (Borsos 2012; Chesterfield 2007; Liu 2009) with 111 analysed patients. The mean duration of active treatment was reported differently in the three studies: in days (Borsos 2012), months (Liu 2009), and years (Chesterfield 2007). Results of a fixed‐effect model meta‐analysis of overall treatment time (Figure 5) indicated that the treatment time was 0.25 standard units shorter on average with surgical anchorage than with conventional anchorage (standardised mean difference (SMD) ‐0.25; 95% CI ‐0.62 to 0.12 ). Heterogeneity was negligible for this comparison (Chi2 = 0.63, df = 2, P value = 0.73; I2 = 0%). We re‐expressed the SMD in years using the summary standard deviations of the Chesterfield study for interpretation; overall treatment time was 0.15 years shorter with surgical anchorage than conventional anchorage (95% CI ‐0.37 to 0.07). The range of effects contained within the confidence interval included both no effect of the intervention and some effect. There was not strong evidence that surgical anchorage reduced treatment time compared with conventional anchorage.
5.
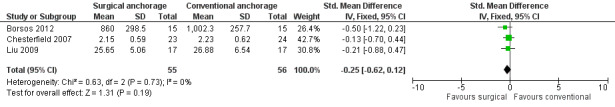
Forest plot of comparison: 1 Surgical anchorage versus conventional anchorage, outcome: 1.2 Duration of overall treatment.
Duration of space closure
The duration of space closure was reported in three studies (Basha 2010; Borsos 2012; Upadhyay 2008) with 80 analysed participants. The mean duration of space closure was reported differently in the three studies, in days (Basha 2010; Borsos 2012) and months (Upadhyay 2008). Results of a fixed‐effect meta‐analyses (Figure 6) indicated that duration of space closure was 0.09 standard units shorter with surgical anchorage than conventional anchorage (SMD ‐0.09; 95% CI ‐0.54 to 0.35). There was a moderate amount of heterogeneity for this outcome (Chi2 = 3.64, df = 2, P value = 0.16; I2 = 45%). We re‐expressed the SMD in days using the summary standard deviations of the Borsos 2012 study for interpretation: time to space closure was 12 days shorter with surgical anchorage than conventional anchorage (95% CI ‐72 to 47). The range of effects contained within the confidence interval include both no effect of the intervention and some effect. There was not strong evidence that surgical anchorage reduced the time to space closure compared with conventional anchorage.
6.
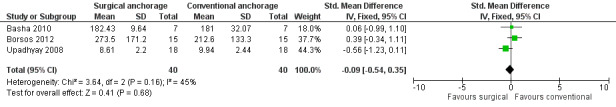
Forest plot of comparison: 1 Surgical anchorage versus conventional anchorage, outcome: 1.3 Duration of space closure (months).
Number of visits
One study (Chesterfield 2007) with 47 analysed patients reported the number of visits taken to complete the course of orthodontic treatment. This did not include the time taken for surgical placement and osseointegration of the mid‐palatal implants. The mean number of visits required to complete orthodontic treatment was 26.21 (SD 7.41) for surgical anchorage and 19.2 (SD 4.58) for conventional anchorage. On average, seven visits less were needed to complete orthodontic treatment with conventional anchorage than with surgical anchorage (MD 7.01; 95% CI 3.47 to 10.55).
Patient perception
Pain
Patient‐reported pain during anaesthetic injection, following surgery or extraction, in the evening after surgery or extraction and one week following surgery or extraction in relation to the anchorage device was reported by one study (Feldmann 2007). The results of the visual analogue scale (VAS) for pain are summarised in Additional Table 4. "The first evening after the intervention, groups A (surgical anchorage) (P value = 0.002) and C (conventional anchorage) (P value = 0.007) had significantly more pain intensity compared to group B (surgical anchorage). The difference in pain intensity between onplant installation and premolar extraction was not significant. One week after the interventions, pain intensity was still significantly higher in group C (conventional anchorage) compared to group B (surgical anchorage) who had undergone installation of an Orthosystem implant (P value = 0.001). Differences between groups A (surgical anchorage) and B (surgical anchorage) were not significant."
3. Pain perception reported by the Feldmann 2007 studya.
|
Pain during anaesthetic injection Median (range) |
Pain during surgery/extraction Median (range) |
Pain on the evening after surgery/extraction Median (range) |
Pain 1 week after surgery/extraction Median (range) |
|
| Nobel‐Biocare onplant | 15 (0‐72) | 3 (0‐14) | 38 (0‐100) | 3 (0‐13) |
| Orthosystem implant | 16 (0‐84) | 3 (0‐16) | 5 (0‐90) | 0 (0‐5) |
| Extraction group (headgear and palatal arch) | 10 (0‐55) | 4 (0‐28) | 28 (0‐100) | 5 (0‐50) |
aPain was self reported on a visual analogue scale (VAS) from 0 to 100 with 'no pain' and 'worst imaginable pain' at the endpoints of the scale
Self reported questionnaires assessing patient‐reported pain on a VAS from 0 to 100 were also administered throughout the orthodontic treatment (from start of treatment until the first visit after retention). Pain in the three anchorage groups peaked on day 2 after the start of treatment. Values for medians and interquartile ranges (IQR) were as follows: 46.0 (IQR 16.0 to 76.5) for the surgical anchorage group, 43.8 (IQR 14.3 to 62.3) for headgear, and 57.0 (IQR 34.5 to 72) for palatal arches.
Discomfort
Discomfort in relation to the anchorage device was reported in two studies (Chesterfield 2007; Feldmann 2007) with 47 and 113 patients analysed, respectively.
When discomfort was assessed in relation to placement of the anchorage device (Feldmann 2007) the results followed a similar pattern to the pain assessed in the same study. The most severe discomfort was experienced on the evening after surgery with the Nobel‐Biocare onplants (median 33, IQR 0 to 96) and the evening after extractions (median 21, IQR 0 to 88). There was still a degree of discomfort with the Orthosystem mid‐palatal implants the evening after surgery (median 14, IQR 0 to 98), however the most severe discomfort experienced with this type of anchorage was during the anaesthetic injection (median 22, IQR 0 to 96). The results of the VAS for discomfort are summarised in Additional Table 5.
4. Discomfort reported by the Feldmann 2007 studya.
|
Discomfort during anaesthetic injection Median (range) |
Discomfort during surgery/extraction Median (range) |
Discomfort on the evening after surgery/extraction Median (range) |
Discomfort 1 week after surgery/extraction Median (range) |
|
| Nobel‐Biocare onplant | 17 (0‐93) | 7 (0‐60) | 33 (0‐96) | 5 (0‐49) |
| Orthosystem implant | 22 (0‐96) | 13 (0‐84) | 14 (0‐98) | 0 (0‐7) |
| Extraction group (headgear and palatal arch) | 13 (0‐59) | 7 (0‐50) | 21 (0‐88) | 3 (0‐26) |
a Discomfort was self reported on a visual analogue scale (VAS) from 0 to 100 with 'no discomfort' and 'worst imaginable discomfort' at the endpoints of the scale
Data were extracted from graphs
Discomfort was also assessed throughout orthodontic treatment on self reported questionnaires that assessed discomfort on a VAS from 0 to 100. Discomfort, expressed as tension from jaws and teeth and soreness from the appliance, in the three anchorage groups peaked on day 2 (no data reported).
In the Chesterfield 2007 study, patients randomised to receive implants were asked to indicate through a self reported questionnaire the grade they would assign to the surgery from 1 (totally comfortable) to 6 (very uncomfortable), immediately after implant placement and on removal of the implant: "75% of the respondents scored between 4 and 6 ‐ i.e. at the comfortable end of the scale for implant placement ‐ and no patient scored 1 indicating that the placement of implants was generally acceptable." These results were repeated over the first three days. On implant removal "40% scored 5, 40% scored 3, and 20% scored 1, indicating that implant removal was slightly less comfortable than implant placement."
Patient acceptability
One study (Feldmann 2007) reported on patient acceptability in terms of limitations to activities of daily life. The study narratively reported that "..limitations in daily life and jaw function were throughout the trial low to moderate and with no differences between anchorage groups." In terms of the impact of orthodontic treatment on the patient's mood and appearance the study further reported "Assessment of how much orthodontic treatment affected the patient's mood and appearance peaked at the first rescheduled visit after 6 weeks (overall median = 14.0; median = 99.0) and with no differences between groups."
Other secondary outcomes
Residual overjet, adverse effects and economic factors were not reported by any of the included studies.
Comparison of two types of surgical anchorage
Primary outcomes
2.1. Analysis.
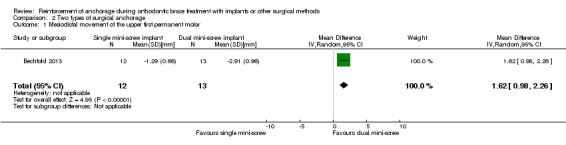
Comparison 2 Two types of surgical anchorage, Outcome 1 Mesiodistal movement of the upper first permanent molar.
The primary outcome of mesiodistal movement of molars was reported in only one study (Bechtold 2013) with 25 patients analysed, which reported an MD of 1.62 mm (95% CI 0.98 to 2.26) in favour of a dual mini‐screw implant over a single mini‐screw implant.
Secondary outcomes
2.2. Analysis.
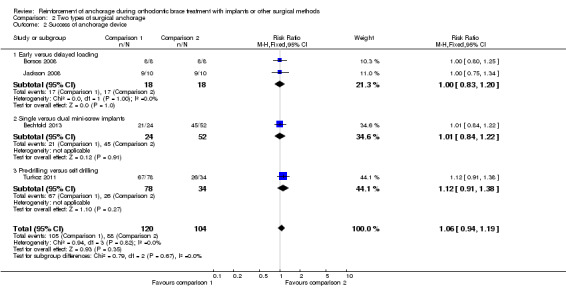
Comparison 2 Two types of surgical anchorage, Outcome 2 Success of anchorage device.
Success of early versus delayed loading
Two studies with 36 patients analysed compared the success of early versus delayed loading of mini‐screw implant anchorage (Borsos 2008; Jackson 2008). Rates of success were high as all 16 implants (in 16 patients) were successful whether loading was early or delayed (Borsos 2008): loading was successful for 9 out of 10 patients in the early loaded group, and 9 out of 10 patients in the delayed loaded group (Jackson 2008) (risk ratio (RR) 1.00; 95% CI 0.83 to 1.20).
Success of single versus dual mini‐screw implants
One study with 25 patients (76 implants) compared the success of single versus dual mini‐ screw implants (Bechtold 2013). Results were reported at the implant level with a similar proportion of successes in the two groups (21/24 successes with the single mini‐ screw implants and 45/52 successes with the dual mini‐ screw implants; RR 1.01; 95% CI 0.84 to 1.22). This confidence interval result should be interpreted with caution as results were reported on an implant level rather than a patient level and were therefore subject to unit of analysis error.
Success of pre‐drilled versus self drilling implants
One study with 62 patients (112 implants) compared the success of pre‐drilled versus self drilling implants (Turkoz 2011). Results were reported at the implant level with similar proportion of successes in the two groups (26/34 successes with the self drilling implants and 67/78 successes with the pre‐drilled implants; RR 1.12; 95% CI 0.91 to 1.38). This confidence interval result should be interpreted with caution as results were reported on an implant level rather than a patient level and were therefore subject to unit of analysis error.
Duration of space closure
A single study (Bechtold 2013) compared the duration of space closure with single versus dual mini‐screw implants. Space closure (months) was quicker, on average, by just over two months in the single mini‐screw implant group than in the dual mini‐screw implant group (MD ‐2.19 months; 95% CI ‐6.35 to 1.97) although this was not statistically significant.
Patient perception
Pain
A single study (Lehnen 2011) with 30 analysed patients compared patient pain perception between the pre‐drilling and self drilling mini‐screw implant groups. Patients were asked: "How would you describe the pain on insertion" and a response was collected on a scale from 0 to 4, where 0 indicated no pain and 4 indicated a high level of pain. On average, self reported pain was less for patients in the pre‐drilling group (n = 15; mean 0.73 (SD 1.1); median 0.00 (IQR 0 to 3)) compared to patients in the self drilling group (n = 15; mean 1.87 (SD 1.13); median 2.0 (IQR 0 to 4)).
Other secondary outcomes
The outcomes of residual overjet, duration of overall treatment, number of visits, adverse effects and economic factors were not reported by these studies.
Discussion
Summary of main results
This is a substantial update with an additional 14 studies added to the single study of the initial review published in 2007.
Comparison of surgical anchorage to conventional anchorage
Mesiodistal movement of upper molar teeth
The last published version of this review included only one study and the results were inconclusive. The small amount of information available to compare surgical anchorage (a single study of surgical anchorage using a mid‐palatal implant) with conventional anchorage did not indicate that the mesiodistal movement of the upper first permanent molar differed in the two groups.
The results from this updated review indicate that there is some evidence that surgical methods of reinforcing orthodontic anchorage are more effective than conventional methods such as headgear and other intraoral devices in reinforcing anchorage during orthodontic brace treatment. The pooled mean difference in mesiodistal movement was 1.68 mm and whilst this difference may seem small it is clinically significant. This is also important when we consider that there are published reports of risk with the use of extraoral devices. As a result, the use of surgical anchorage has clear advantages over other methods of reinforcing anchorage.
Since the development of the protocol for this review current practice has moved towards the adoption of specific types of surgical anchorage, the most common of which is the mini‐screw implant. Hence a post hoc subgroup analysis was undertaken to further investigate the effects of different individual types of surgical anchorage, mid‐palatal implants and mini‐screw implants. Whilst the overall effects favoured surgical anchorage for both subgroups, the mean difference in mesiodistal movement was smaller, and thus more favourable, for mini‐screw implants than conventional anchorage (headgear and palatal arches).
Secondary outcomes
The effects on the secondary outcomes of the review were less certain due to limited reporting of these outcomes and variability in the clinical definitions of outcomes, which precluded synthesis. Both methods of anchorage were successful. There was not strong evidence that surgical anchorage reduced treatment time or duration of space closure when compared to conventional anchorage. There was very little evidence on patient‐reported outcomes such as pain, discomfort and acceptability. Importantly, no studies reported on residual overjet at the end of treatment, adverse effects and economic factors.
Comparison of two types of surgical anchorage
The direct comparisons of surgical interventions were from two small studies of early and delayed loading of the same mini‐screw implants, two studies comparing pre‐drilling and self drilling mini‐screw implants, and one study comparing single and dual mini‐screw implants. Results from these studies did not indicate that the proportion of successes were different between these pairwise comparisons of surgical interventions.
Only one study reported on the primary outcome of movement of the upper first molar in a mesial or distal direction, and no studies reported on residual overjet at the end of treatment. One study reported on the duration of space closure. The number of visits, acceptability, economic factors and adverse effects were not reported in any of the studies.
Overall completeness and applicability of evidence
The primary objective of the review was to assess the effects of surgical anchorage techniques compared to conventional anchorage in the prevention of unwanted tooth movement in orthodontic patients, by evaluating the mesiodistal movement of upper first molar teeth. Ten studies, conducted principally in a dental hospital setting, in locations across Europe, Asia and the USA contributed information to the evaluation of this outcome. Participants were adolescents and younger and older adults. The overall risk of bias for the included studies was high or unclear, with only one study assessed as at low risk of bias. The pooled estimate of effect showed a mean difference in favour of surgical anchorage, which was of clinical importance. However, this result should be interpreted with caution due to the associated high level of heterogeneity of the pooled studies and the inclusion of only mini‐screw and mid‐palatal implants as surgical interventions.
A secondary objective was to compare the effects of one type of surgical anchorage with another. This was assessed in five studies where applicability of the evidence to the review question was good. The overall risk of bias for the included studies was high or unclear. The surgical interventions were diverse and this precluded the calculation of a pooled estimate of effect.
Whilst the updated review comprised 15 included studies the amount of information contributing to the primary and secondary outcomes varied substantially. Hence only the effects of the primary outcome mesiodistal movement for surgical anchorage techniques compared to conventional anchorage techniques can be estimated with any degree of certainty. The implications of this finding are discussed further in the sections Implications for practice and Implications for research.
Quality of the evidence
SeeFigure 2, Figure 3, Table 1
The body of evidence reporting the primary outcome was moderate according to the GRADE approach due to limitations in the design and conduct of the studies. One study was at low risk of bias and one was at high risk of bias due to the lack of blinding of outcome assessment. A further two were at an unclear risk of bias because we could not locate the protocol of the primary study leading to uncertainty in the reporting of all intended outcomes; all other risk of bias domains were at low risk of bias in these two studies. The remaining studies were at an unclear risk of bias mainly because the concealment of the allocation sequence was not reported.
We assessed the quality of evidence for the additional outcome of duration of treatment as low due to limitations in design, the conduct of the studies, and to imprecision of results from the two small studies providing data for this outcome.
We assessed the studies in this review as having varying risks of bias. The evidence for the main outcomes of mesiodistal movement, duration of treatment and adverse events were from studies at overall high and unclear risks of bias. Only one small study was assessed to have an overall low risk of bias. No information on the remaining outcome, adverse events, was reported.
Selective reporting was evident for many of the included studies as expected cephalometric and clinical outcomes were not reported or were reported incompletely. Where possible, we contacted the authors for additional information on aspects of study design or outcome data. Any additional information that was obtained was included in the review.
Orthodontic treatment is a long and sometimes painful process. The number of studies reporting patient‐reported outcomes of relevance to the review, such as pain and acceptability, was small and the quality of the reported outcomes was poor. This is a definite limitation of the review.
Potential biases in the review process
We found it difficult to agree a single appropriate endpoint to measure anchorage loss a priori (seeImplications for research). In addition, the subgroup analysis which looked at the effects of different types of surgical anchorage compared to conventional anchorage was not pre‐determined but was driven by the types of studies found. The results of this post hoc analysis should be interpreted with caution.
We decided not to pool the results of outcomes with different clinical definitions (e.g. success of anchorage), but to present the results of the individual studies as a narrative.
Agreements and disagreements with other studies or reviews
The results of this review are in agreement with other systematic reviews on the topic, which have less rigorous methodology. The inclusion criteria for these reviews have often allowed a large variation in study design, including retrospective studies. These reviews either assessed a variety of surgical anchorage devices or were specifically interested in mini‐screw implants. The most common outcome that was investigated in these reviews was the success or failure of the anchorage device, followed by anchorage loss (molar movement). Mini‐screw implants were found to have success rates of 83.3% (Crismani 2010), 87.7% (Papadopoulos 2011), 86.5% (Papageorgiou 2012) and 61% to 100% (Tsui 2012). Mini‐plates and palatal implants had success rates of 91.4% to 100% and 74% to 93.3%, respectively. In addition, the Li 2011 review reported more distal movement with the mid‐palatal implants, onplants and mini‐screw implants. Reported anchorage loss was in agreement with this review. The mean difference in distal molar movement favoured mini‐screw implants over conventional anchorage in the Papadopoulos 2011 review (MD ‐2.4 mm; 95% confidence interval ‐2.9 to ‐1.8).
Authors' conclusions
Implications for practice.
The last published version of this review included a single study and concluded that the objectives of the review were not met because little evidence was identified for assessment. It was also suggested that mid‐palatal implants may be an acceptable alternative to headgear reinforced anchorage in orthodontic anchorage.
From this update there is some evidence of moderate quality to suggest that surgical anchorage is more effective than conventional anchorage in the reinforcement of anchorage during orthodontic brace treatment, and that results from mini‐screw implants are particularly promising. Importantly, surgical anchorage is not associated with the inherent risks and compliance issues related to headgear. There was no evidence of a difference in duration of treatment between surgical and conventional anchorage.
When direct comparisons were made between two types of surgical anchorage, there was a lack of evidence to suggest that any one technique was better than another.
Implications for research.
Current evidence on the effectiveness of surgical anchorage is based on randomised trials with varying levels of bias. In particular, methods to reduce the potential for selection bias should be undertaken and reported. Only two of the included studies (Chesterfield 2007; Feldmann 2007) reported calculating the sample size. Future research should ensure that an adequate sample size is achieved.
A wide age range of patients could possibly benefit from surgical anchorage. However, including a wide age range in a single study is discouraged because it is known that growing patients respond differently to orthodontic treatment when compared to non‐growing patients. In addition, studies should address both patient and clinician acceptability of the surgical appliances as important changes to policies can be made as a result of such trials. These could include adding this type of treatment to the syllabus of training orthodontists or providing this treatment as part of government or insured health care or both.
Outcomes should consider an appropriate start and endpoint to measure molar movement as a function of assessing orthodontic anchorage. It was difficult to agree an appropriate endpoint for measurement of anchorage loss before undertaking the review; a decision was made to use the most common endpoint(s). Anchorage control is required in all phases of orthodontic treatment and this was reflected in the endpoints reported in the studies of this review. Points at which anchorage loss was measured included at the end of the levelling and alignment phase, the end of space closure (including or excluding the previous alignment phase or both), the end of anchorage (when the anchorage device was no longer needed) and the end of treatment. A consensus on the most important endpoint could possibly be achieved by conducting qualitative research; this could be part of an overall design to reach a consensus on outcomes relevant to anchorage devices. Important considerations would be the clinical relevance of the endpoint, an occasion when the biggest difference is likely to occur, or the objectivity of the endpoint or both. For example, choosing 'end of anchorage' as an endpoint is likely to be the point where maximum movement of the molars is achieved, however it is a somewhat subjective time point. Conversely, the end of treatment is a more objective time point however, the effects of the anchorage devices may be neutralised or further reinforced in an attempt to achieve the ideal occlusion at the end of treatment.
Studies should also focus on relevant outcomes rather than reporting routine cephalometric analysis. Studies included in this review and the ongoing studies have reported a variety of relevant outcomes. A single study would need large resources and adequate time to investigate all relevant outcomes and time points, therefore it is recommended that consensus be reached on the most important outcomes and how they may be investigated and reported. Areas for research include determining the best size and shape of the implant as well as the type of material to use. Other areas of comparison are immediate versus delayed, and static versus dynamic loading. It is also important to assess patient perception and acceptability. Appropriate outcomes from such research should include anchorage loss, failure rates, financial costs, assessment of discomfort and related quality of life issues. The outcome of success poses a particular challenge when comparing surgical and conventional anchorage. This was previously discussed in a related Cochrane review (Jambi 2013). It is difficult to find a definition for success that applies to both surgical and conventional anchorage. The recommendation is to define success according to treatment objectives. For example, an appliance would be successful in orthodontic anchorage if it achieves at least no loss of anchorage (0 mm molar movement) or gain of anchorage (distal molar movement).
What's new
| Date | Event | Description |
|---|---|---|
| 4 August 2014 | New search has been performed | Searches updated to October 2013. |
| 4 August 2014 | New citation required and conclusions have changed | Substantial update with different authors, inclusion criteria, search strategy, citations and conclusions. 14 new studies were added to the single study in the last published version of the review. |
History
Protocol first published: Issue 1, 2005 Review first published: Issue 3, 2007
| Date | Event | Description |
|---|---|---|
| 11 January 2008 | Amended | Converted to new review format. |
Acknowledgements
Thanks are due to Anne Littlewood, Trials Search Co‐ordinator for the Cochrane Oral Health Group, for carrying out the searches for this review.
We would also like to acknowledge Chunjie Li, Lecturer at the Department of Oral & Maxillofacial Surgery, West China College of Stomatology, Sichuan University, for his translation support for the Shi 2008 study.
Appendices
Appendix 1. Cochrane Oral Health Group's Trials Register search strategy
From December 2012, searches were conducted in the Cochrane Oral Health Group's Trials Register via the Cochrane Central Register of Controlled Studies, using the search strategy below:
#1 (orthodontic*:ti,ab) AND (INREGISTER) #2 (((dental and implant*) or (oral and implant*) or (titanium and implant*) or (palatal and implant*) or (endosseous and implant*)):ti,ab) AND (INREGISTER) #3 (osseointegrat*:ti,ab) AND (INREGISTER) #4 ("titanium plate*":ti,ab) AND (INREGISTER) #5 ("zygoma* wire*":ti,ab) AND (INREGISTER) #6 ((miniscrew* or "mini screw*" or mini‐screw* or microscrew* or "micro screw*" or micro‐screw* or spiderscrew* or "spider screw*" or spider‐screw*) :ti,ab) AND (INREGISTER) #7 ((surgical* or surgery):ti,ab) AND (INREGISTER) #8 (onplant*:ti,ab) AND (INREGISTER) #9 ("temporary anchorage device*":ti,ab) AND (INREGISTER) #10 (TAD:ti,ab) AND (INREGISTER) #11 (#2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10) AND (INREGISTER) #12 (anchor*) AND (INREGISTER) #13 (#1 and #11 and #12) AND (INREGISTER)
Previous searches were conducted in the Cochrane Oral Health Group's Trials Register using the Procite software and the search strategy below:
(orthodontic* and anchor*)
Appendix 2. CENTRAL search strategy
#1 MeSH descriptor Orthodontics explode all trees #2 orthodontic* in All Text #3 (#1 or #2) #4 MeSH descriptor Dental implants explode all trees #5 MeSH descriptor Dental Implantation explode all trees #6 ((dental in All Text near/4 implant* in All Text) or (oral in All Text near/4 implant* in All Text) or (titanium in All Text near/4 implant* in All Text) or (palatal in All Text near/4 implant* in All Text) or (endosseous in All Text near/4 implant* in All Text)) #7 osseointegration in All Text #8 "titanium plate*" in All Text #9 "zygoma* wire*" in All Text #10 (mini‐screw* in All Text or "mini screw*" in All Text or mini‐screw* in All Text or microscrew* in All Text or "micro screw*" in All Text or micro‐screw* in All Text or spiderscrew* in All Text or "spider screw*" in All Text or spider‐screw* in All Text) #11 (surgical* in All Text or surgery in All Text) #12 onplant* in All Text #13 "temporary anchorage device*" in All Text #14 TAD in Title, Abstract or Keywords #15 (#4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14) #16 MeSH descriptor Orthodontic Anchorage Procedures this term only #17 anchor* in All Text #18 (#16 or #17) #19 (#3 and #15 and #18)
Appendix 3. MEDLINE via OVID search strategy
exp Orthodontics/
orthodontic$.mp.
or/1‐2
exp Dental Implants/
exp Dental Implantation/
((dental adj4 implant$) or (oral adj4 implant$) or (titanium adj4 implant$) or (palatal adj4 implant$) or (endosseous adj4 implant$)).mp.
osseointegration.mp.
"titanium plate$".mp.
"zygoma$ wire$".mp.
(mini‐screw$ or "mini screw$" or mini‐screw$ or microscrew$ or "micro screw$" or micro‐screw$ or spiderscrew$ or "spider screw$" or spider‐screw$).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
(surgical$ or surgery).mp.
onplant$.mp.
"temporary anchorage device".mp.
TAD.ti,ab.
or/4‐14
Orthodontic Anchorage Procedures/
anchor$.mp.
or/16‐17
3 and 15 and 18
Cochrane search filter for MEDLINE via OVID:
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. EMBASE via OVID search strategy
exp Orthodontics/
orthodontic$.mp.
or/1‐2
exp Dental Implants/
exp Dental Implantation/
((dental adj4 implant$) or (oral adj4 implant$) or (titanium adj4 implant$) or (palatal adj4 implant$) or (endosseous adj4 implant$)).mp.
osseointegration.mp.
"titanium plate$".mp.
"zygoma$ wire$".mp.
(mini‐screw$ or "mini screw$" or mini‐screw$ or microscrew$ or "micro screw$" or micro‐screw$ or spiderscrew$ or "spider screw$" or spider‐screw$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name]
(surgical$ or surgery).mp.
onplant$.mp.
"temporary anchorage device".mp.
TAD.ti,ab.
or/4‐14
Orthodontic Anchorage Procedures/
anchor$.mp.
or/16‐17
3 and 15 and 18
Filter for EMBASE via OVID:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. ANIMAL/ or NONHUMAN/ or ANIMAL EXPERIMENT/ 16. HUMAN/ 17. 16 and 15 18. 15 not 17 19. 14 not 18
Appendix 5. Clinicaltrials.gov search strategy
The Clinicaltrials.gov website was searched by topic selecting mouth and tooth diseases. All records under 'malocclusion' and 'Malocclusion Angle Class II' were searched. In addition, an advanced keyword search using the following 'search terms' and 'interventions' was conducted:
Orthodontic AND anchorage OR Temporary AND anchorage OR Surgical AND anchorage | mini‐screws OR mini‐screws OR micro‐screws OR microscrews OR spiderscrews OR spider AND screws OR titanium AND plates OR miniplates OR zygoma AND wire
Appendix 6. IFMPA search strategy
This was searched by using the following terms from the 'site language': 'orthodontic procedure' and 'dental braces complication'.
Appendix 7. Current Controlled Trials search strategy
The Current Controlled Trials website was searched by using the following keywords individually: dental, orthodontic, mini‐implant, mini‐screw implant, surgical anchorage and headgear.
Data and analyses
Comparison 1. Surgical anchorage versus conventional anchorage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mesiodistal movement of the upper first permanent molar | 7 | 308 | Mean Difference (IV, Random, 95% CI) | ‐1.68 [‐2.27, ‐1.09] |
| 1.1 Mid‐palatal implants | 3 | 190 | Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐2.31, 0.26] |
| 1.2 Mini‐screw implants | 4 | 118 | Mean Difference (IV, Random, 95% CI) | ‐2.17 [‐2.58, ‐1.77] |
| 2 Duration of overall treatment | 3 | 111 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.62, 0.12] |
| 3 Duration of space closure (months) | 3 | 80 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.54, 0.35] |
| 4 Number of visits | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 7.01 [3.47, 10.55] |
1.1. Analysis.
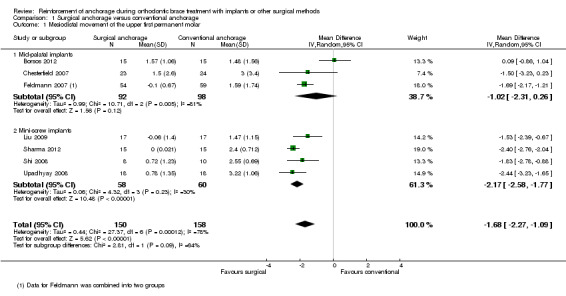
Comparison 1 Surgical anchorage versus conventional anchorage, Outcome 1 Mesiodistal movement of the upper first permanent molar.
1.2. Analysis.
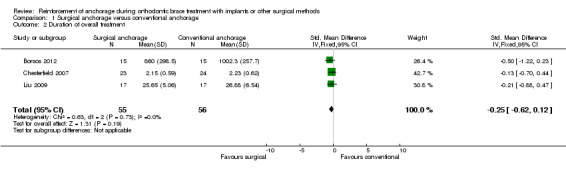
Comparison 1 Surgical anchorage versus conventional anchorage, Outcome 2 Duration of overall treatment.
1.3. Analysis.
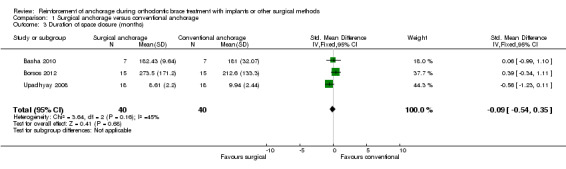
Comparison 1 Surgical anchorage versus conventional anchorage, Outcome 3 Duration of space closure (months).
1.4. Analysis.
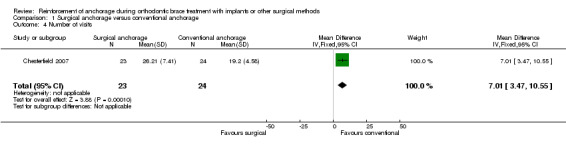
Comparison 1 Surgical anchorage versus conventional anchorage, Outcome 4 Number of visits.
Comparison 2. Two types of surgical anchorage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mesiodistal movement of the upper first permanent molar | 1 | 25 | Mean Difference (IV, Random, 95% CI) | 1.62 [0.98, 2.26] |
| 2 Success of anchorage device | 4 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.94, 1.19] |
| 2.1 Early versus delayed loading | 2 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.83, 1.20] |
| 2.2 Single versus dual mini‐screw implants | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.84, 1.22] |
| 2.3 Pre‐drilling versus self drilling | 1 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.91, 1.38] |
| 3 Duration of space closure | 1 | 25 | Mean Difference (IV, Random, 95% CI) | ‐2.19 [‐6.35, 1.97] |
2.3. Analysis.
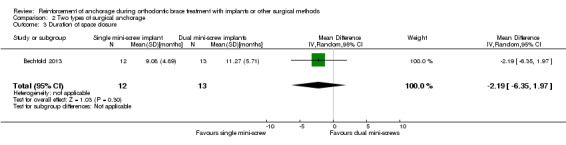
Comparison 2 Two types of surgical anchorage, Outcome 3 Duration of space closure.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Basha 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
‐ measured in mm on cephalometric radiographs by calculating the difference in the distance between pterygoid vertical to maxillary molar ‐ measured from the start of space closure until the end of space closure
|
|
| Notes | A pre‐adjusted edgewise appliance with an MBT prescription and a 0.022 x 0.028 inch slot was used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A comparative study consisting of 14 patients (all females) randomised into 2 groups" Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment is not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were accounted for in the analysis |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Bechtold 2013.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Subjects were randomly allocated to either group A …. or group B" Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not addressed |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were accounted for |
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Borsos 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | The main outcome of this study was the histological evaluation of the bone‐implant contact after treatment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly assigned to treatment groups in groups of four at a 1:1 ratio" Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not addressed |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were accounted for |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk | Fixed size blocks were used in a small single‐centre unblinded trial. This may make it possible to predict future assignments |
Borsos 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Both groups were treated with Alexander brackets with a 0.018 x 0.025 inch slots | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote from paper: "...the allocation was carried out by using randomised blocks of six" Quote from correspondence: "We used block randomisation with blocks of six. So we had to wait, until a group of six patients were collected, then we carried out a randomisation. This was repeated five times. In practice, this means that you have to wait until six patients are collected ‐ meeting the inclusion criteria and are willing to participate in the study. As every patient, taken up to our Department, also the participants got a card number, when he first presented themselves. At the randomisation one will be drawn from the 20 possible blocks (closed envelopes), in all of which the two (A and B) groups are represented equally. The selected block would be assigned to the patients based on their card sequence number. (For example: we have six patients with card numbers 2, 4, 6, 7, 9, 12 and block 4 (AABBA) is selected – than patient 2, 4, 12 are candidates in group A and patient 6, 7, 9 in group B)" |
| Allocation concealment (selection bias) | Low risk | Quote from correspondence: "They were 20 pieces standard size postal envelopes stamped on the sealing. They were stored in the drawer of the head of the department in his closed office. Chief dental nurse was drawing and opening the envelopes (only one at once) in the presence of two witnesses (me and the head of dep.)" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote from paper: "...the cephalometric analysis was carried out anonymously, using an opaque marker in the approximate position of an implant in both groups" |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were accounted for |
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Chesterfield 2007.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
‐ measured in mm on cephalometric radiographs using the Pancherz analysis between T1 (treatment start) and T2 (end of anchorage reinforcement) ‐ measured at the end of anchorage (when the anchorage device was no longer needed)
‐ questionnaire in which the patients were asked to indicate the grade they would assign to the surgery on a six 6‐point scale where 1 was totally uncomfortable and 6 was comfortable ‐ questionnaire was administered at 3 time points: immediately after placement of the palatal implant, 3 days after placement and upon removal of the palatal implant |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...randomisation carried out by using computer‐generated random numbers in a block design" |
| Allocation concealment (selection bias) | Low risk | Quote: "..randomisation carried out by using computer‐generated random numbers in a block design by a researcher unconnected with the recruitment of most patients" Quote: "...allocation was concealed in consecutively numbered, sealed opaque envelopes, which were opened after the patient and parent agreed to enter the trial" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quotes:
|
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk |
|
| Selective reporting (reporting bias) | Low risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Feldmann 2007.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
‐ measured in mm on cephalometric radiographs using Bjork and Pancherz analyses ‐ measured at the end of levelling and alignment (start of space closure) and at the end of space closure (including and excluding the levelling and alignment phase) ‐ data included in this review were from the end of space closure excluding the levelling and alignment phase
‐ comparisons were made between Nobel Biocare onplants, Orthosystem mid‐palatal implants and conventional anchorage (headgear and palatal arches combined) ‐ self reported on a VAS from 0 to 100 where 'no pain/discomfort' and 'worst imaginable pain/discomfort' were the endpoints of the scale ‐ assessed at 4 time points, during the anaesthetic injection, during surgery/extractions, the evening after surgery/extractions and 1 week after surgery ‐ pain in the first 2 groups was related to mid‐palatal implant placement and in the third group related to premolar extractions
‐ daily activities included leisure time, speech, ability to take a big bite, ability to chew hard and soft food, the ability to chew against resistance, schoolwork, drinking, laughing, yawning, kissing, in addition to how the orthodontic treatment affected mood and appearance ‐ comparisons were made between the surgical anchorage group (Nobel Biocare onplants and Orthosystem implants combined), headgear and palatal arches ‐ self reported on a VAS from 0 to 100, or a 4‐point scale ‐ there were multiple time points; at the start of treatment, each day for a week after the start of treatment, 6 weeks into treatment, after levelling and alignment, after space closure, and 6 weeks into retention |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The allocation sequence was computer generated by a statistician at..." Quote: "the patients were randomised in blocks of 4 and stratified by sex into 1 of 4 groups" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The allocation sequence was ..., and concealed in envelopes until randomization" Comment: not stated whether envelopes were opaque and sequentially numbered |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessment was not blinded because the appliances were visible on the radiographs |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | At the end of space closure the following drop‐outs were reported:
|
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | High risk | Fixed size blocks were used in a single‐centre unblinded trial. This may make it possible to predict future assignments |
Jackson 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes | Clinical success of the palatal implant defined as the ability to use the implant in the course of orthodontic treatment | |
| Notes | The main study outcome was implant stability, not success of anchorage device. The duration of this study was 8 weeks, and the definition for clinical success of the mini‐screw implants was the ability to use the implant in the course of orthodontic treatment. An endpoint of 8 weeks after mini‐screw implant placement does not represent a course of orthodontic treatment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "All patients in the study were randomised to either immediately loaded or non loaded treatments using the method of randomly permuted blocks" Quote: "The randomization scheme was generated by using the web site Randomization.com" |
| Allocation concealment (selection bias) | Low risk | Quote: "Third party volunteer sealed the treatment assignment for each participant in a brown envelope, which was open immediately prior to placement of the midpalatal implant" Quote: "Group designation obtained by randomization was revealed to the primary investigator on the day of the surgery" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not addressed |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | 1 patient dropped out from the immediate loading group due to failure of the implant |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Lehnen 2011.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | The questionnaire was administered by an interviewer and had a total of 11 questions:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the patients were divided at random into two groups of the same size while aiming for equal gender distribution" Quote: "the first injection quadrant was chosen at random" Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "the interviewer was neither involved in the clinical procedure nor informed about it" |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All 30 participants answered the questionnaires completely |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk | There was no wash‐out period in the second randomisation, both injection techniques were given in the same appointment |
Liu 2009.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "they were randomly assigned to two groups with the aid of a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not addressed |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were included in the analysis |
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Ma 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes | No outcomes concerned with this review were reported | |
| Notes | Pre‐adjusted straight wire appliances were used with an MBT prescription | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The subjects were randomly divided (RandA1.0 Software, Planta Medical Technology and Development Co. Ltd, Beijing, China) into two equal groups" |
| Allocation concealment (selection bias) | Unclear risk | Not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Tracing, superimposition, and measurement were undertaken manually by two examiners who did not participate in the study design" Comment: blinding of outcome assessment probably achieved because the radiographs were taken before and immediately after treatment; at these points of treatment, the appliances are not fixed inside the mouth, and hence do not show on the radiographs |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients accounted for |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Maddalone 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Information for this study was obtained from a Google translation of the manuscript reporting the study The method of measurement of molar movement used the head of the mini‐screw implants and the canines as a reference, it is unknown if the implant is a stable reference point |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Translated quote: "The items were assigned randomly to two groups of study: 19 were treated with distalisation…" Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not addressed |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were analysed |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Sharma 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
‐ the distance between the pterygoid vertical plane (PTV) and the centroid point on the upper first molar was used to determine the position of the upper first molar ‐ the difference between the pre‐treatment and post‐canine retraction position was used to determine mesial molar movement |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Each subject was assigned a computer‐generated random number. When a total of 30 had been recruited they were arranged in ascending order according to their assigned random number. The first patient of the arranged number list was assigned to group A, the next to group B. This was carried out alternatively until all the..." |
| Allocation concealment (selection bias) | Low risk | Quote: "the random numbers were generated using EPI Info 6 software (Centers for Disease Control and Prevention [CDC] Atlanta, GA, USA) by a faculty member independent from the study" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "the mini‐screw implant or TPA was removed to avoid observer bias and a post‐canine retraction cephalometric radiograph was taken" Quote: "All pre‐ and post‐treatment cephalometric radiographs were hand traced by one investigator (DC) who was masked as to the details of the study" |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were accounted for in the analysis |
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Shi 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes | Molar mesiodistal movement on lateral cephalometric radiographs; U6‐PTV (distance from mesiobuccal apex of the upper first molar to PTV) | |
| Notes | The full text article is in Chinese; this information was obtained from a translation of the article | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not addressed |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | There were 2 drop‐outs in the mini‐screw implant group; due to loss of implants |
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Turkoz 2011.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
‐ failure was recorded when there was significant mobility that could not sustain the orthodontic force ‐ this was assessed before loading, 1 month after loading and overall |
|
| Notes | Success and failure reported by implant and not by participant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Sixty‐two adolescent patients were randomly assigned to three groups" Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not addressed |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk | All randomised patients were analysed |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | Low risk | Study appears to be free of other sources of bias |
Upadhyay 2008.
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Straight wire appliance was used with Roth prescription | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the subjects were randomly divided into 2 groups" Quote: "the allocation sequence, which was generated by the statistician on this project using computer‐generated random numbers" Quote: "A restricted randomizations method was used in blocks of 10 to ensure that equal numbers of patients were allocated to each treatment group" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The principal investigator (M.U.) was blinded to the allocation sequence" Comment:
|
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "measurement analysis of the cephalogram was performed blindly" Quote: "One faculty member (K.N.) examined all 72 cephalograms. The same faculty member conducted the measurement analysis of the cephalograms and was unaware of the objectives of the study" Quote: "All data were entered into computer databases by research assistants, who were also blinded to the treatment group" Comment: the faculty member examining the radiographs could have seen the intervention on the radiograph if there was no attempt to mask it, even if they were unaware of the study objectives |
| Incomplete outcome data (attrition bias) mesial movement of upper first maxillary molar | Low risk |
|
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Low risk | There was en masse retraction in the mini‐implant group and sequential retraction in the conventional group; however this would bias the results towards underestimating the effects of the mini‐implants |
RCT = randomised controlled trial; SD = standard deviation; VAS = visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Altug‐Atac 2008 | Interventions did not include a type of surgical anchorage |
| Baxmann 2010 | Randomisation does not occur between 2 types of anchorage reinforcement |
| Bondemark 2005 | Interventions did not include a type of surgical anchorage |
| Chen 2008 | This study is not a randomised controlled trial as confirmed after translation of this article |
| Cheng 2004 | Randomisation does not occur between 2 different types of anchorage reinforcement |
| Deguchi 2008 | This study is not a randomised controlled trial |
| Garfinkle 2008 | This is a split‐mouth study |
| Gelgor 2007 | This study is not a randomised controlled trial, as confirmed by author correspondence |
| Gollner 2009 | This study is not a randomised trial |
| Kadioglu 2008 | This study is not a randomised controlled trial |
| Lee 2011 | This study is not a randomised controlled trial, as confirmed by author correspondence |
| Melsen 2007 | Interventions do not include a type of surgical anchorage |
| Moon 2008 | There was only a single intervention |
| Motoyoshi 2007 | This study is not a randomised controlled trial |
| Palagi 2010 | Interventions did not include a type of surgical anchorage |
| Papadopoulos 2010 | Interventions do not include a type of surgical anchorage |
| Polat‐Ozsoy 2011 | Interventions do not include a type of surgical anchorage |
| Schatzle 2009 | This study did not include patients undergoing orthodontic treatment with fixed appliances |
| Thiruvenkatachari 2008 | This study is not a randomised controlled trial |
| Upadhyay 2008‐2 | This study is not a randomised controlled trial, as confirmed by author correspondence |
| Upadhyay 2012 | This study is not a randomised controlled trial, as confirmed by author correspondence |
| Wiechmann 2007 | This study is not a randomised controlled trial |
| Wilmes 2009 | This study is not a randomised controlled trial |
| Zhou 2009 | This study is a prospective controlled trial. However, there is no indication that randomisation was carried out. Correspondence address for the authors could not be found to confirm |
Characteristics of ongoing studies [ordered by study ID]
Bearn 2008.
| Trial name or title | What is the most effective method for providing orthodontic anchorage? A randomised clinical trial of headgear, AbsoAnchor mini‐screws, palatal arch |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | 16 July 2008 |
| Contact information | Dr Roberta Littleford
University of Dundee, Tayside Clinical Trials Unit, Ninewells Hospital & Medical School, Research & Development Office, Level 2 Residency Block, Dundee, Scotland, DD1 9SY, United Kingdom Telephone: +44 (0)1382 740376 r.littleford@dundee.ac.uk |
| Notes |
Biavati/ Migliorati 2011.
| Trial name or title | Three dimensional movement analysis of maxillary impacted canine using TADs: a randomized clinical trial |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | September 2011 |
| Contact information | Doctor Marco Migliorati Orthodontics Department, Dental School, Genoa University, Genoa, Italy, 16100 Telephone: +39 3383825781 marco.migliorati@gmail.com |
| Notes |
Jung 2007.
| Trial name or title | Early loading of palatal implants (Ortho‐type II) a prospective multicentre randomised controlled clinical trial |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | December 2006 |
| Contact information | BA Jung Department of Orthodontics, University Medical Center Mainz, Augustusplatz 2, 55131 Mainz, Germany brjung@uni‐mainz.de |
| Notes | The results reported at this point in time are an interim analysis involving 41 participants and reporting the outcome success of anchorage device. The trial is still ongoing |
Miller 2009.
| Trial name or title | Study of the efficacy of skeletal anchorage (mini‐screw) compared to dental anchorage during orthodontic treatment |
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Starting date | February 2009 |
| Contact information | Bretonneau Hospital, Paris, France, 75018 |
| Notes |
Sandler 2008.
| Trial name or title | Efficiency and effectiveness of 3 methods of anchorage reinforcement in orthodontics |
| Methods |
|
| Participants | 75 participants, both male and female eligible, age range from 12‐17 years |
| Interventions |
|
| Outcomes |
|
| Starting date | July 2008 |
| Contact information | Not known |
| Notes | This study is now completed, and data will be reported when this review is updated |
RCT = randomised controlled trial
Differences between protocol and review
The inclusion criteria were changed as follows.
Quasi‐randomised studies were no longer eligible for the review.
To coincide with recent advancements in measurement techniques, studies in which measurements were made on superimposed digital models were also considered eligible for the review.
The electronic search strategy was amended by the Cochrane Oral Health Group's Trials Search Co‐ordinator to include additional terms (endosseous, temporary anchorage device, TAD, orthodontic anchorage procedures).
The handsearch was expanded to include relevant journals on oral implants.
The search for unpublished studies was expanded to include trial registries.
Subgroup analysis was carried out to further investigate the effects of different types of surgical anchorage. This was a post hoc analysis as we did not expect to find multiple trials investigating surgical anchorage.
Contributions of authors
Amendment of methodology: Safa Jambi (SJ), supervised by Kevin O'Brien (KOB).
Searching other resources: SJ.
Examination of titles and abstracts: Safa Jambi (SJ), Jonathan Sandler (JPS), KOB.
Retrieval and examination of full text reports: SJ, JPS.
Final decisions on study inclusion: SJ, JPS, KOB, Tanya Walsh (TW).
Development of data collection forms: SJ.
Piloting of data collection forms, data extraction and management: SJ, JPS.
Risk of bias assessment: SJ, JPS, KOB, TW.
Data synthesis: SJ, TW.
Writing the review: SJ, KOB, TW.
The original version of this review was jointly conceived and designed by Richard M Skeggs and Philip E Benson.
Sources of support
Internal sources
The University of Manchester, UK.
External sources
-
The Ministry of Higher Education/Taiba University, Saudi Arabia.
This review was undertaken as part of a PhD at The University of Manchester and funded by the government of Saudi Arabia.
-
Cochrane Oral Health Group Global Alliance, UK.
All reviews in the Cochrane Oral Health Group are supported by Global Alliance member organisations (British Association of Oral Surgeons, UK; British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; British Society of Periodontology, UK; Canadian Dental Hygienists Association, Canada; Mayo Clinic, USA; National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Royal College of Surgeons of Edinburgh, UK) providing funding for the editorial process (http://ohg.cochrane.org/).
-
National Institute for Health Research (NIHR), UK.
CRG funding acknowledgement: The NIHR is the largest single funder of the Cochrane Oral Health Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Declarations of interest
Two of the authors of this review, Philip E Benson and Jonathan Sandler, were involved as authors in one of the included studies (Chesterfield 2007); and Jonathan Sandler was involved in one of the ongoing studies (Sandler 2008). Decisions on study inclusion, data extraction and risk of bias assessments for these studies were and will be performed independently of these authors.
Safa Jambi, Tanya Walsh, Richard M Skeggs, Kevin D O'Brien: no interests to declare.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Basha 2010 {published data only (unpublished sought but not used)}
- Basha AG, Shantaraj R, Mogegowda SB. Comparative study between conventional en‐masse retraction (sliding mechanics) and en‐masse retraction using orthodontic micro implant. Implant Dentistry 2010;19(2):128‐36. [DOI] [PubMed] [Google Scholar]
Bechtold 2013 {published data only}
- Bechtold TE, Kim JW, Choi TH, Park YC, Lee KJ. Distalization pattern of the maxillary arch depending on the number of orthodontic miniscrews. The Angle Orthodontist 2013;83(2):266‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borsos 2008 {published data only}
- Borsos G, Rudzki‐Janson I, Stockmann P, Schlegel KA, Végh A. Immediate loading of palatal implants in still‐growing patients: a prospective, comparative, clinical pilot study. Journal of Orofacial Orthopedics 2008;69(4):297‐308. [DOI] [PubMed] [Google Scholar]
Borsos 2012 {published data only}
- Borsos G, Jianu R, Vegh A. Comparison of bone‐borne and tooth tissue‐borne anchorage during the maxillary canine retraction in growing patients. TMJ 2011;61(1‐2):98‐101. [Google Scholar]
- Borsos G, Voko Z, Gredes T, Kunert‐Keil C, Vegh A. Tooth movement using palatal implant supported anchorage compared to conventional dental anchorage. Annals of Anatomy 2012;194(6):556‐60. [DOI] [PubMed] [Google Scholar]
Chesterfield 2007 {published and unpublished data}
- Benson P, Tinsley D, O'Dwyer J, Majumder A, Doyle P, Sandler P. Mid‐palatal implants versus headgear for orthodontic anchorage ‐ A randomised clinical trial: cephalometric results. American Journal of Orthodontics and Dentofacial Orthopedics 2007;132(5):606‐15. [DOI] [PubMed] [Google Scholar]
- Sandler J, Benson P, Doyle P, Majumder A, O'Dwyer J, Speight P, et al. Palatal implants are a good alternative to headgear: a randomized trial. American Journal of Orthodontics and Dentofacial Orthopedics 2008;133(1):51‐7. [DOI] [PubMed] [Google Scholar]
Feldmann 2007 {published data only}
- Feldmann I. Evidence‐based evaluation of anchorage capacity and patients' perception. Swedish Dental Journal 2007;Suppl 191:1‐132. [PubMed] [Google Scholar]
- Feldmann I, Bondemark L. Anchorage capacity of osseointegrated and conventional anchorage systems: A randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2008;133(3):339.e19‐339.e28. [DOI] [PubMed] [Google Scholar]
- Feldmann I, List T, Bondemark L. Orthodontic anchoring techniques and its influence on pain, discomfort, and jaw function‐‐a randomized controlled trial. European Journal of Orthodontics 2012;34(1):102‐8. [DOI] [PubMed] [Google Scholar]
- Feldmann I, List T, Feldmann H, Bondemark L. Pain intensity and discomfort following surgical placement of orthodontic anchoring units and premolar extraction. The Angle Orthodontist 2007;77(4):578‐85. [DOI] [PubMed] [Google Scholar]
Jackson 2008 {published data only}
- Jackson A, Lemke R, Hatch J, Salome N, Gakunga P, Cachran D. A comparison of stability between delayed versus immediately loaded orthodontic palatal implants. Journal of Esthetic and Restorative Dentistry 2008;20(3):174‐85. [DOI] [PubMed] [Google Scholar]
Lehnen 2011 {published data only}
- Lehnen S, McDonald F, Bourauel C, Baxmann M. Patient expectations, acceptance and preferences in treatment with orthodontic mini‐implants. A randomly controlled study. Part I: insertion techniques. Journal of Orofacial Orthopedics 2011;72(2):93‐102. [DOI] [PubMed] [Google Scholar]
Liu 2009 {published data only}
- Liu YH, Ding WH, Liu J, Li Q. Comparison of the differences in cephalometric parameters after active orthodontic treatment applying mini‐screw implants or transpalatal arches in adult patients with bialveolar dental protrusion. Journal of Oral Rehabilitation 2009 Sep;36(9):687‐95. [DOI] [PubMed] [Google Scholar]
Ma 2008 {published data only (unpublished sought but not used)}
- Ma J, Wang L, Zhang W, Chen W, Zhao C, Smales RJ. Comparative evaluation of micro‐implant and headgear anchorage used with a pre‐adjusted appliance system. European Journal of Orthodontics 2008;30(3):283‐7. [DOI] [PubMed] [Google Scholar]
Maddalone 2010 {published data only}
- Maddalone M, Ferrari M, Stanizzi A, Barrilla S, Arrigoni P. Use of miniscrew implants in orthodontic distal movement [Utilizzo delle miniviti nelle meccaniche ortodontiche di distalizzazione]. Dental Cadmos 2010;78(8):97‐105. [Google Scholar]
Sharma 2012 {published data only}
- Sharma M, Sharma V, Khanna B. Mini‐screw implant or transpalatal arch‐mediated anchorage reinforcement during canine retraction: a randomized clinical trial. Journal of Orthodontics 2012;39(2):102‐10. [DOI] [PubMed] [Google Scholar]
Shi 2008 {published data only}
- Shi Y‐T, Ping Y, Shan L‐H, Song J‐S, Qiu Z‐X. Stability of mini‐implant during orthodontic treatment as anchorage. Zhongguo Zuzhi Gongcheng Yanjiu Yu Linchuang Kang Fu (Journal of Clinical Rehabilitative Tissue Engineering Research) 2008;12(26):5109‐12. [Google Scholar]
Turkoz 2011 {published data only}
- Turkoz C, Atac MS, Tuncer C, Balos Tuncer B, Kaan E. The effect of drill‐free and drilling methods on the stability of mini‐implants under early orthodontic loading in adolescent patients. European Journal of Orthodontics 2011;33(5):533‐6. [DOI] [PubMed] [Google Scholar]
Upadhyay 2008 {published and unpublished data}
- Upadhyay M, Yadav S, Nagaraj K, Patil S. Treatment effects of mini‐implants for en‐masse retraction of anterior teeth in bialveolar dental protrusion patients: A randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2008;134(1):18‐29. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Altug‐Atac 2008 {published data only}
Baxmann 2010 {published data only}
- Baxmann M, McDonald F, Bourauel C, Jager A. Expectations, acceptance, and preferences regarding microimplant treatment in orthodontic patients: A randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2010;138(3):250.e1‐250.e10; discussion 250‐1. [DOI] [PubMed] [Google Scholar]
Bondemark 2005 {published data only}
- Bondemark L, Karlsson I. Extraoral vs intraoral appliance for distal movement of maxillary first molars: a randomized controlled trial. The Angle Orthodontist 2005;75(5):699‐706. [DOI] [PubMed] [Google Scholar]
Chen 2008 {published data only}
- Chen WJ, Li QY, Gong AX, Hu F, Gu YJ. Comparison between J‐hook and micro‐implant anchorage in the treatment of patients with bimaxillary protrusion. Zhonghua Kouqiang Yixue Zazhi (Chinese Journal of Stomatology) 2008;43(2):83‐6. [PubMed] [Google Scholar]
Cheng 2004 {published data only}
- Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini‐implants used for orthodontic anchorage. The International Journal of Oral and Maxillofacial Implants 2004;19(1):100‐6. [PubMed] [Google Scholar]
Deguchi 2008 {published data only}
- Deguchi T, Murakami T, Kuroda S, Yabuuchi T, Kamioka H, Takano‐Yamamoto T. Comparison of the intrusion effects on the maxillary incisors between implant anchorage and J‐hook headgear. American Journal of Orthodontics and Dentofacial Orthopedics 2008;133(5):654‐60. [DOI] [PubMed] [Google Scholar]
Garfinkle 2008 {published and unpublished data}
- Garfinkle J, Cunningham Jr L, Beeman C, Kluemper G, Hicks E, Kim M. Evaluation of orthodontic mini‐implant anchorage in premolar extraction therapy in adolescents. American Journal of Orthodontics and Dentofacial Orthopedics 2008;133(5):642‐53. [DOI] [PubMed] [Google Scholar]
Gelgor 2007 {published and unpublished data}
Gollner 2009 {published data only}
- Gollner P, Jung BA, Kunkel M, Liechti T, Wehrbein H. Immediate vs. conventional loading of palatal implants in humans. Clinical Oral Implants Research 2009;20(8):833‐7. [DOI] [PubMed] [Google Scholar]
Kadioglu 2008 {published data only}
Lee 2011 {published and unpublished data}
- Lee KJ, Park YC, Hwang CJ, Kim YJ, Choi TH, Yoo HM, et al. Displacement pattern of the maxillary arch depending on mini‐screw position in sliding mechanics. American Journal of Orthodontics and Dentofacial Orthopedics 2011;140(2):224‐32. [DOI] [PubMed] [Google Scholar]
Melsen 2007 {published data only}
- Melsen B, Enemark E. Effect of cervical anchorage studied by the implant method (Transactions of the European Orthodontic Society 1969). European Journal of Orthodontics 2007;29:i102‐6. [PubMed] [Google Scholar]
Moon 2008 {published data only}
Motoyoshi 2007 {published data only}
- Motoyoshi M, Yoshida T, Ono A, Shimizu N. Effect of cortical bone thickness and implant placement torque on stability of orthodontic mini‐implants. International Journal of Oral and Maxillofacial Implants 2007;22(5):779‐84. [PubMed] [Google Scholar]
Palagi 2010 {published data only}
- Palagi LM, Sabrosa CE, Gava EC, Baccetti T, Miguel JA. Long‐term follow‐up of dental single implants under immediate orthodontic load. The Angle Orthodontist 2010 Sep;80(5):807‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Papadopoulos 2010 {published data only}
- Papadopoulos MA, Melkos AB, Athanasiou AE. Noncompliance maxillary molar distalization with the first class appliance: a randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2010;137(5):586.e1‐586.e13; discussion 586‐7. [DOI] [PubMed] [Google Scholar]
Polat‐Ozsoy 2011 {published data only}
- Polat‐Ozsoy O, Arman‐Ozcirpici A, Veziroglu F, Cetinsahin A. Comparison of the intrusive effects of miniscrews and utility arches. American Journal of Orthodontics and Dentofacial Orthopedics 2011;139(4):526‐32. [DOI] [PubMed] [Google Scholar]
Schatzle 2009 {published data only}
- Schatzle M, Mannchen R, Balbach U, Hammerle CH, Toutenburg H, Jung RE. Stability change of chemically modified sandblasted/acid‐etched titanium palatal implants. A randomized‐controlled clinical trial. Clinical Oral Implants Research 2009;20(5):489‐95. [DOI] [PubMed] [Google Scholar]
Thiruvenkatachari 2008 {published data only}
- Thiruvenkatachari B, Pavithranand A, Rajasigamani K, Kyung HM. Comparison and measurement of the amount of anchorage loss of the molars with and without use of implant anchorage during canine retraction. American Journal of Orthodontics and Dentofacial Orthopedics 2008;35(2):128. [DOI] [PubMed] [Google Scholar]
Upadhyay 2008‐2 {published and unpublished data}
- Upadhyay M, Yadav S, Patil S. Mini‐implant anchorage for en‐masse retraction of maxillary anterior teeth: A clinical cephalometric study. American Journal of Orthodontics and Dentofacial Orthopedics 2008;134(6):803‐10. [DOI] [PubMed] [Google Scholar]
Upadhyay 2012 {published and unpublished data}
- Upadhyay M, Yadav S, Nagaraj K, Uribe F, Nanda R. Mini‐implants vs fixed functional appliances for treatment of young adult Class II female patients: a prospective clinical trial. The Angle Orthodontist 2012;82(2):294‐303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiechmann 2007 {published data only (unpublished sought but not used)}
- Wiechmann D, Meyer U, Buchter A. Success rate of mini‐ and micro‐implants used for orthodontic anchorage: a prospective clinical study. Clinical Oral Implant Research 2007;18:263‐7. [DOI] [PubMed] [Google Scholar]
Wilmes 2009 {published data only}
- Wilmes B, Olthoff G, Drescher D. Comparison of skeletal and conventional anchorage methods in conjunction with pre‐operative decompensation of a skeletal class III malocclusion. Journal of Orofacial Orthopedics 2009;70(4):297‐305. [DOI] [PubMed] [Google Scholar]
Zhou 2009 {published data only}
- Zhou H‐X, Wang Z‐Q, Huang C‐H, Yu X‐H. Comparison of micro‐implant screw anchorage at various implant areas. Zhongguo Zuzhi Gongcheng Yanjiu Yu Linchuang Kang Fu (Journal of Clinical Rehabilitative Tissue Engineering Research) 2009;13(26):5181‐4. [Google Scholar]
References to ongoing studies
Bearn 2008 {published and unpublished data}
- What is the most effective method for providing orthodontic anchorage? A randomised clinical trial of headgear, AbsoAnchor mini‐screws, palatal arch. Ongoing study 16 July 2008.
Biavati/ Migliorati 2011 {published data only}
- Three dimensional movement analysis of maxillary impacted canine using TADs: a randomized clinical trial. Ongoing study September 2011.
Jung 2007 {published data only}
- Jung B, Wehrbein H, Hopfenmuller W, Harzer W, Gedrange T, Deidrich P, et al. Early loading of palatal implants (ortho‐type II) a prospective multicenter randomized controlled clinical trial. Trials 2007;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung BA, Harzer W, Gedrange T, Kunkel M, Moergel M, Diedrich P, et al. Spectrum of indications for palatal implants in treatment concepts involving immediate and conventional loading. Journal of Orofacial Orthopedics 2010;71(4):273‐80. [DOI] [PubMed] [Google Scholar]
- Jung BA, Harzer W, Wehrbein H, Gedrange T, Hopfenmüller W, Lüdicke G, et al. Immediate versus conventional loading of palatal implants in humans: a first report of a multicenter RCT. Clinical Oral Investigations 2011;15(4):495‐502. [DOI] [PubMed] [Google Scholar]
Miller 2009 {published data only}
- Study of the efficacy of skeletal anchorage (mini‐screw) compared to dental anchorage during orthodontic treatment. Ongoing study February 2009.
Sandler 2008 {published and unpublished data}
- Efficiency and effectiveness of 3 methods of anchorage reinforcement in orthodontics. Ongoing study July 2008.
Additional references
Booth‐Mason 1988
- Booth‐Mason S, Birnie D. Penetrating eye injury from orthodontic headgear ‐ a case report. European Journal of Orthodontics 1988;10(2):111‐4. [DOI] [PubMed] [Google Scholar]
Crismani 2010
- Crismani AG, Bertl MH, Celar AG, Bantleon HP, Burstone CJ. Miniscrews in orthodontic treatment: review and analysis of published clinical trials. American Journal of Orthodontics and Dentofacial Orthopedics 2010;137(1):108‐13. [DOI] [PubMed] [Google Scholar]
Cureton 1993
- Cureton SL, Regennitter FJ, Yancey JM. Clinical versus quantitative assessment of headgear compliance. American Journal of Orthodontics and Dentofacial Orthopedics 1993;104(3):277‐84. [DOI] [PubMed] [Google Scholar]
Gainsforth 1945
- Gainsforth BL, Higley LB. A study of orthodontic anchorage possibilities in basal bone. American Journal of Orthodontics and Oral Surgery 1945;31:406‐16. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Jambi 2013
- Jambi S, Thiruvenkatachari B, O'Brien KD, Walsh T. Orthodontic treatment for distalising upper first molars in children and adolescents. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD008375.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kanomi 1997
- Kanomi R. Mini‐implant for orthodontic anchorage. Journal of Clinical Orthodontics 1997;31(11):763‐7. [PubMed] [Google Scholar]
Li 2011
- Li F, Hu HK, Chen JW, Liu ZP, Li GF, He SS, et al. Comparison of anchorage capacity between implant and headgear during anterior segment retraction. The Angle Orthodontist 2011;81(5):915‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Melsen 1998
- Melsen B, Petersen JK, Costa A. Zygoma ligatures: an alternative form of maxillary anchorage. Journal of Clinical Orthodontics 1998;32(3):154‐8. [PubMed] [Google Scholar]
Mitchell 2001
- Mitchell L. An Introduction to Orthodontics. 2nd Edition. Oxford, UK: Oxford University Press, 2001. [Google Scholar]
Papadopoulos 2011
- Papadopoulos MA, Papageorgiou SN, Zogakis IP. Clinical effectiveness of orthodontic miniscrew implants: a meta‐analysis. Journal of Dental Research 2011;90(8):969‐76. [DOI] [PubMed] [Google Scholar]
Papageorgiou 2012
- Papageorgiou SN, Zogakis IP, Papadopoulos MA. Failure rates and associated risk factors of orthodontic miniscrew implants: a meta‐analysis. American Journal of Orthodontics and Dentofacial Orthopedics 2012;142(5):577‐95. [DOI] [PubMed] [Google Scholar]
Prabhu 2006
- Prabhu J, Cousley RR. Current products and practice: bone anchorage devices in orthodontics. Journal of Orthodontics 2006;33(4):288‐307. [DOI] [PubMed] [Google Scholar]
Samuels 1994
- Samuels RH, Jones ML. Orthodontic facebow injuries and safety equipment. European Journal of Orthodontics 1994;16(5):385‐94. [DOI] [PubMed] [Google Scholar]
Samuels 1996
- Samuels RH, Willner F, Knox J, Jones ML. A national survey of orthodontic facebow injuries in the UK and Eire. British Journal of Orthodontics 1996;23(1):11‐20. [DOI] [PubMed] [Google Scholar]
Tsui 2012
- Tsui WK, Chua HD, Cheung LK. Bone anchor systems for orthodontic application: a systematic review. International Journal of Oral and Maxillofacial Surgery 2012;41(11):1427‐38. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Skeggs 2005
- Skeggs R, Benson P. Surgical reinforcement of anchorage during orthodontic brace treatment. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD005098] [DOI] [PMC free article] [PubMed] [Google Scholar]
Skeggs 2007
- Skeggs RM, Benson PE, Dyer F. Reinforcement of anchorage during orthodontic brace treatment with implants or other surgical methods. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD005098.pub2] [DOI] [PubMed] [Google Scholar]


