Abstract
Background
Endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) are tests used in the diagnosis of common bile duct stones in patients suspected of having common bile duct stones prior to undergoing invasive treatment. There has been no systematic review of the accuracy of EUS and MRCP in the diagnosis of common bile duct stones using appropriate reference standards.
Objectives
To determine and compare the accuracy of EUS and MRCP for the diagnosis of common bile duct stones.
Search methods
We searched MEDLINE, EMBASE, Science Citation Index Expanded, BIOSIS, and Clinicaltrials.gov until September 2012. We searched the references of included studies to identify further studies and of systematic reviews identified from various databases (Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment (HTA), Medion, and ARIF (Aggressive Research Intelligence Facility)). We did not restrict studies based on language or publication status, or whether data were collected prospectively or retrospectively.
Selection criteria
We included studies that provided the number of true positives, false positives, false negatives, and true negatives for EUS or MRCP. We only accepted studies that confirmed the presence of common bile duct stones by extraction of the stones (irrespective of whether this was done by surgical or endoscopic methods) for a positive test, and absence of common bile duct stones by surgical or endoscopic negative exploration of the common bile duct or symptom free follow‐up for at least six months for a negative test, as the reference standard in people suspected of having common bile duct stones. We included participants with or without prior diagnosis of cholelithiasis; with or without symptoms and complications of common bile duct stones, with or without prior treatment for common bile duct stones; and before or after cholecystectomy. At least two authors independently screened abstracts and selected studies for inclusion.
Data collection and analysis
Two authors independently collected the data from each study. We used the bivariate model to obtain pooled estimates of sensitivity and specificity.
Main results
We included a total of 18 studies involving 2366 participants (976 participants with common bile duct stones and 1390 participants without common bile duct stones). Eleven studies evaluated EUS alone, and five studies evaluated MRCP alone. Two studies evaluated both tests. Most studies included patients who were suspected of having common bile duct stones based on abnormal liver function tests; abnormal transabdominal ultrasound; symptoms such as obstructive jaundice, cholangitis, or pancreatitis; or a combination of the above. The proportion of participants who had undergone cholecystectomy varied across studies. Not one of the studies was of high methodological quality. For EUS, the sensitivities ranged between 0.75 and 1.00 and the specificities ranged between 0.85 and 1.00. The summary sensitivity (95% confidence interval (CI)) and specificity (95% CI) of the 13 studies that evaluated EUS (1537 participants; 686 cases and 851 participants without common bile duct stones) were 0.95 (95% CI 0.91 to 0.97) and 0.97 (95% CI 0.94 to 0.99). For MRCP, the sensitivities ranged between 0.77 and 1.00 and the specificities ranged between 0.73 and 0.99. The summary sensitivity and specificity of the seven studies that evaluated MRCP (996 participants; 361 cases and 635 participants without common bile duct stones) were 0.93 (95% CI 0.87 to 0.96) and 0.96 (95% CI 0.90 to 0.98). There was no evidence of a difference in sensitivity or specificity between EUS and MRCP (P value = 0.5). From the included studies, at the median pre‐test probability of common bile duct stones of 41% the post‐test probabilities (with 95% CI) associated with positive and negative EUS test results were 0.96 (95% CI 0.92 to 0.98) and 0.03 (95% CI 0.02 to 0.06). At the same pre‐test probability, the post‐test probabilities associated with positive and negative MRCP test results were 0.94 (95% CI 0.87 to 0.97) and 0.05 (95% CI 0.03 to 0.09).
Authors' conclusions
Both EUS and MRCP have high diagnostic accuracy for detection of common bile duct stones. People with positive EUS or MRCP should undergo endoscopic or surgical extraction of common bile duct stones and those with negative EUS or MRCP do not need further invasive tests. However, if the symptoms persist, further investigations will be indicated. The two tests are similar in terms of diagnostic accuracy and the choice of which test to use will be informed by availability and contra‐indications to each test. However, it should be noted that the results are based on studies of poor methodological quality and so the results should be interpreted with caution. Further studies that are of high methodological quality are necessary to determine the diagnostic accuracy of EUS and MRCP for the diagnosis of common bile duct stones.
Keywords: Humans; Cholangiopancreatography, Magnetic Resonance; Cholangiopancreatography, Magnetic Resonance/standards; Endosonography; Endosonography/standards; Choledocholithiasis; Choledocholithiasis/diagnosis; Choledocholithiasis/diagnostic imaging; Sensitivity and Specificity
Plain language summary
Endoscopic ultrasound versus magnetic resonance cholangiopancreatography for the diagnosis of common bile duct stones
Background
Bile, produced in the liver and stored temporarily in the gallbladder, is released into the small bowel on eating fatty food. The common bile duct (CBD) is the tube through which bile flows from the gallbladder to the small bowel. Stones in the CBD (CBD stones) are usually formed in the gallbladder before migration into the bile duct. They can obstruct the flow of bile leading to jaundice (yellowish discolouration of skin, whites of the eyes, and dark urine), infection of the bile (cholangitis), and inflammation of the pancreas (pancreatitis), which can be life threatening. Various diagnostic tests can be performed for the diagnosis of CBD stones. Depending upon the availability of resources, these stones are removed endoscopically (usually the case) or may be removed as part of the operation performed to remove the gallbladder (it is important to remove the gallbladder since the stones continue to form in the gallbladder and can cause recurrent problems). Prior to removal, invasive tests such as endoscopic retrograde cholangiopancreatography (ERCP) or intraoperative cholangiography (IOC) can be performed to detect CBD stones. However, before performing such invasive tests to diagnose CBD stones, non‐invasive tests such as endoscopic ultrasound (EUS) (using ultrasound attached to the endoscope) and magnetic resonance cholangiopancreatography (MRCP) are used to identify people at high risk of having CBD stones so that only those at high risk can be subjected to further tests.
Study characteristics
We performed a thorough search for studies that reported the accuracy of EUS or MRCP in the diagnosis of CBD stones. We included a total of 18 studies involving 2532 participants. Eleven studies evaluated EUS alone, five studies evaluated MRCP alone, and two studies evaluated both tests. A total of 1537 participants were included in the 13 studies that evaluated EUS and 995 participants were included in the seven studies that evaluated MRCP. Most studies included patients who were suspected of having CBD stones based on abnormal blood tests, abnormal ultrasound, or symptoms such as jaundice or pancreatitis, or a combination of the above. The proportion of participants who had undergone previous gallbladder removal varied across studies.
Key results
Based on an average sensitivity of 95% for EUS, on average 95 out of 100 people with CBD stones will be detected while the remaining 5 people will be missed and will not receive appropriate treatment. The average number of people with CBD stones detected using EUS may vary between 91 and 97 out of 100 people. The average specificity of 97% for EUS means that on average 97 out of 100 people without CBD stones will be identified as not having CBD stones; 3 out of 100 would be false positives and would not receive appropriate treatment. The average number of false positives could vary between 1 and 6 out of 100 people. For MRCP, an average sensitivity of 93% means that on average 93 out of 100 people with CBD stones will be detected while the remaining 7 people will be missed and will not receive appropriate treatment. The average number of people with CBD stones detected using MRCP may vary between 87 and 96 out of 100 people. With an average specificity of 96% for MRCP, 96 out of 100 people without CBD stones will be identified as not having CBD stones; 4 out of 100 would be false positives and would not receive appropriate treatment. The average number of false positives could vary between 2 and 10 out of 100 people. This means that some people with CBD stones can be missed by EUS and MRCP. Although most people with a negative EUS or MRCP do not need to undergo further invasive tests, in the presence of persistent symptoms further testing with MRCP if the patient had undergone EUS or EUS if the patient had undergone MRCP, ERCP, or IOC may be indicated. There is little to choose between EUS and MRCP in terms of diagnostic accuracy.
Quality of evidence
All the studies were of low methodological quality, which may undermine the validity of our findings.
Future research
Further studies of high methodological quality are necessary.
Summary of findings
Summary of findings'. 'Performance of endoscopic ultrasound and magnetic resonance cholangiopancreatography for diagnosis of common bile stones.
| Population | Patients suspected of having common bile duct stones based on symptoms, liver function tests, and ultrasound | ||||
| Settings | Secondary and tertiary care setting in different parts of the world | ||||
| Index tests | Endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) | ||||
| Reference standard | Endoscopic or surgical extraction of stones in patients with a positive index test result or clinical follow‐up (minimum 6 months) in patients with a negative index test result | ||||
| Target condition | Common bile duct stones | ||||
| Number of studies | A total of 18 studies were included. Thirteen studies (686 cases, 1537 participants) evaluated EUS and 7 studies (361 cases, 996 participants) evaluated MRCP. Two of the studies evaluated both tests in the same patients | ||||
| Methodological quality concerns | All the studies were of poor methodological quality; most studies were at high risk of bias or gave high concern about applicability across all domains of quality assessment, or both | ||||
| Pre‐test probability1 | Test | Summary sensitivity (95% CI) | Summary specificity (95% CI) | Positive post‐test probability (95% CI)2 | Negative post‐test probability (95% CI)3 |
| 0.14 | EUS | 0.95 (0.91 to 0.97) | 0.97 (0.94 to 0.99) | 0.85 (0.72 to 0.93) | 0.01 (0.01 to 0.02) |
| MRCP | 0.93 (0.87 to 0.96) | 0.96 (0.89 to 0.98) | 0.79 (0.61 to 0.90) | 0.01 (0.01 to 0.02) | |
| 0.30 | EUS | 0.95 (0.91 to 0.97) | 0.97 (0.94 to 0.99) | 0.94 (0.87 to 0.97) | 0.02 (0.01, 0.04) |
| MRCP | 0.93 (0.87 to 0.96) | 0.96 (0.89 to 0.98) | 0.90 (0.80 to 0.96) | 0.03 (0.02, 0.06) | |
| 0.41 | EUS | 0.95 (0.91 to 0.97) | 0.97 (0.94 to 0.99) | 0.96 (0.92 to 0.98) | 0.03 (0.02, 0.06) |
| MRCP | 0.93 (0.87 to 0.96) | 0.96 (0.89 to 0.98) | 0.94 (0.87 to 0.97) | 0.05 (0.03 to 0.09) | |
| 0.48 | EUS | 0.95 (0.91 to 0.97) | 0.97 (0.94 to 0.99) | 0.97 (0.93, 0.99) | 0.05 (0.03 to 0.08) |
| MRCP | 0.93 (0.87 to 0.96) | 0.96 (0.89 to 0.98) | 0.95 (0.90 to 0,98) | 0.06 (0.04 to 0.11) | |
| 0.68 | EUS | 0.95 (0.91 to 0.97) | 0.97 (0.94 to 0.99) | 0.99 (0.97 to 0.99) | 0.10 (0.06 to 0.16) |
| MRCP | 0.93 (0.87 to 0.96) | 0.96 (0.89 to 0.98) | 0.98 (0.95 to 0.99) | 0.13 (0.08 to 0.23) | |
| Comparison of the diagnostic accuracy of EUS and MRCP: at pre‐test probabilities of 14%, 41%, and 68%, out of 100 people with positive EUS, common bile duct stones will be present in 85, 96, and 99 people respectively; while out of 100 people with positive MRCP, common bile duct stones will be present in 79, 94, and 98 people. For the same pre‐test probabilities, out of 100 people with negative EUS, common bile duct stones will be present in 1, 3, and 10 people respectively; while out of 100 people with negative MRCP, common bile duct stones will be present in 1, 5, and 13 people respectively. | |||||
| Conclusions: the performance of EUS and MRCP appears to be comparable for diagnosis of common bile duct stones. The strength of the evidence for the test comparison was weak because the studies were methodologically flawed, and only two studies made head‐to‐head comparisons of EUS and MRCP. | |||||
1 The pre‐test probability (proportion with common bile duct stones out of the total number of participants) was computed for each included study. These numbers represent the minimum, lower quartile, median, upper quartile and the maximum values from the 18 studies.
2Post‐test probability of common bile duct stones in people with positive index test results.
3Post‐test probability of common bile duct stones in people with negative index test results.
Background
Biliary stones are conglomerates of precipitated bile salts that form in the gallbladder or the common bile duct. The common bile duct carries bile from the liver to the duodenum (first part of the small intestine). The term 'gallstones' generally refers to the stones in the gallbladder while the term 'common bile duct stones' refers to stones in the common bile duct. Common bile duct stones may form inside the common bile duct (primary common bile duct stones), or they may form in the gallbladder and migrate to the common bile duct (secondary common bile duct stones) (Williams 2008). A significant proportion of patients presenting with common bile duct stones may be asymptomatic (Sarli 2000). In some patients the stones pass silently into the duodenum, and in others the stones cause clinical symptoms like biliary colic, jaundice, cholangitis, or pancreatitis (Caddy 2006). The prevalence of gallstone disease in the general population is about 6% to 15%, with a higher prevalence in females (Barbara 1987; Loria 1994). Only 2% to 4% of people with gallstones become symptomatic with biliary colic (pain), acute cholecystitis (inflammation), obstructive jaundice, or gallstone pancreatitis in a year (Attili 1995; Halldestam 2004), and removal of the gallbladder is recommended in people with symptomatic gallstones (Gurusamy 2010). Among patients who undergo laparoscopic cholecystectomy (removal of the gallbladder) for symptomatic gallstones, 3% to 22% of patients also have concomitant common bile duct stones (Arnold 1970; Lill 2010; Yousefpour Azary 2011).
Common bile duct stones present in multiple ways. Central and right sided upper abdominal pain is a common presentation (Anciaux 1986; Roston 1997). Jaundice, caused by an impacted stone in the common bile duct leading to obstruction of bile passage into the duodenum, is another presentation. It may subsequently resolve if the common bile duct stone passes spontaneously into the duodenum. This happens in 54% to 73% of patients with common bile duct stones in whom cholecystectomy is performed for gallstones (Tranter 2003; Lefemine 2011). Another, more dangerous, complication of common bile duct stones is acute cholangitis. Cholangitis is clinically defined by Charcot's triad which includes elevated body temperature, pain under the right ribcage, and jaundice (Raraty 1998; Salek 2009). Acute cholangitis is caused by an ascending bacterial infection of the common bile duct and the biliary tree along with biliary obstruction. This complication is present in 2% to 9% of patients admitted for gallstone disease (Saik 1975; Tranter 2003) and a mortality of approximately 24% is recorded (Salek 2009). Common bile duct stones may also cause acute pancreatitis, accounting for 33% to 50% of all patients with acute pancreatitis (Corfield 1985; Toh 2000). Acute pancreatitis is usually a self‐limiting disease and is generally sufficiently treated by conservative measures in its mild form (Neoptolemos 1988). However, a more severe pancreatitis may evolve in approximately 27% to 37% of patients with common bile duct stone induced pancreatitis, with mortality around 6% to 9% (Mann 1994; Toh 2000).
Suspicion of common bile duct stones can be investigated by laboratory liver function tests (Barkun 1994) or imaging tests like abdominal ultrasound (Ripolles 2009). Further testing may include endoscopic ultrasound (EUS) (Aljebreen 2008), magnetic resonance cholangiopancreatography (MRCP) (Stiris 2000), endoscopic retrograde cholangiopancreatography (ERCP) (Geron 1999), and intraoperative cholangiography (IOC) (Fiore 1997). Currently, these are the recommended tests for diagnosis of common bile duct stones. Of these tests, IOC can only be done during an operation as the test requires surgical cannulation of the common bile duct during cholecystectomy. The other tests may be used before or after cholecystectomy. Usually the first diagnostic tests that most patients undergo are liver function tests and abdominal ultrasound. Invasive diagnostic tests are usually reserved for patients with suspected common bile duct stones based on non‐invasive diagnostic tests, or when therapeutic measures are necessary (Freitas 2006).
Conventional computed tomogram (CT scan), CT cholangiogram, laparoscopic ultrasound, and ERCP guided intraductal ultrasound are of limited use for diagnosing common bile duct stones (Maple 2010).
Target condition being diagnosed
Common bile duct stones. We did not differentiate the target condition with respect to common bile duct stone size, degree of common bile duct obstruction, and the presence or absence of symptoms.
Index test(s)
MRCP uses a high magnetic field to cause fluctuations of tissues at a molecular level. These minute fluctuations are then registered by the receiver as differences in frequencies of fluctuation for the different types of tissues. This information is then combined using computer software to generate high‐resolution pictures of the scanned area. A common bile duct stone is seen as a hypointense round or oval area of low signal in the hyperintense common bile duct (Stiris 2000; RadiologyInfo 2011).
Endoscopic ultrasound combines endoscopy (a flexible tube used to visualise the food‐pipe and stomach) with ultrasound. A forward‐viewing or side‐viewing endoscope with an ultrasound transducer is introduced in the duodenum by visual control, and then high‐frequency sound waves are used to inspect the tissues that are in the proximity. Seeing a hyperechoic round or oval structure within the common bile duct is considered a positive test (Fickling 2003; Aljebreen 2008).
Clinical pathway
Figure 1 illustrates a diagnostic pathway. Patients that are at risk of having common bile duct stones or are suspected of having common bile duct stones (such as patients with gallbladder stones or patients that show symptoms and signs of obstructive jaundice or pancreatitis) will undergo liver function tests and abdominal ultrasound as the first step. An abdominal ultrasound is usually available by the time the person is at risk or is suspected of having common bile duct stones. Usually a combination of both tests is used as triage tests before further testing is done in the second step, but these can be used as the definitive diagnostic tests to carry out a therapeutic option (for example endoscopic or surgical common bile duct exploration) (Williams 2008; ASGE Standards of Practice Commitee 2010). MRCP or EUS are tests in the second step of the diagnostic pathway, which are used as optional triage tests prior to tests used in the third step of the diagnostic pathway; but they can also be used as definitive diagnostic tests to carry out a therapeutic option, that is, some people attempt extraction of stones irrespective of the ERCP or IOC findings. MRCP and EUS are not usually combined since the positive or negative results of one or the other is usually accepted for further clinical decision making, without taking into consideration the results of liver function tests or transabdominal ultrasound, as it is generally believed that MRCP and EUS have better diagnostic accuracy than liver function tests or transabdominal ultrasound. ERCP and IOC are used in the third step of the diagnostic pathway. Both tests are done just before the therapeutic intervention. Therapeutic interventions, such as endoscopic or surgical stone extraction, can then be undertaken during the same session. ERCP is done before endoscopic sphincterotomy and removal of common bile duct stones using a Dormia basket or balloon during the same endoscopic session (Prat 1996; Maple 2010), and IOC is done before surgical common bile duct exploration and removal of common bile duct stones using surgical instruments during an operation for cholecystectomy (Targarona 2004; Freitas 2006; Chen 2007; Williams 2008; ASGE Standards of Practice Commitee 2010; Kelly 2010).
1.
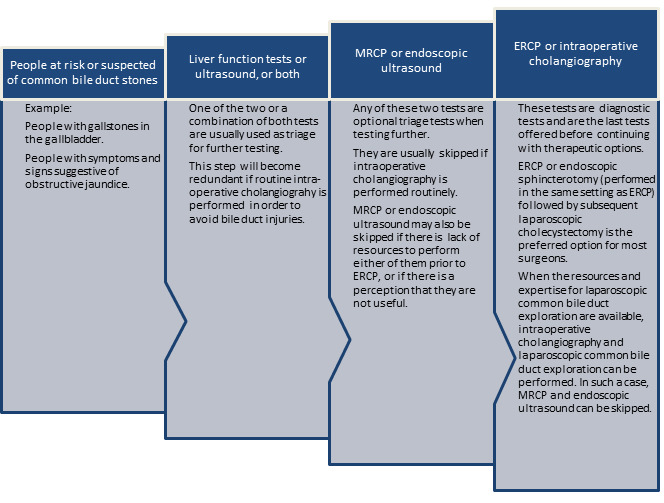
The diagnostic pathway for diagnosis of common bile duct stones. Note that ultrasound is generally performed in all patients at risk or suspected of common bile duct stones.
Abbreviations MRCP: magnetic resonance cholangiopancreatography ERCP: endoscopic retrograde cholangiopancreatography
MRCP and EUS can be considered as add‐on tests in patients with a positive transabdominal ultrasound or liver function tests. Although most patients can undergo either MRCP or EUS, with the choice between the tests being determined by the preference of the surgeon, EUS is the only add‐on test possible in patients with contra‐indications to magnetic resonance imaging such as claustrophobic patients and patients with cardiac pacemakers (Magnetic Resonance Imaging 2011) while MRCP is the only add‐on test possible in patients with Roux‐en‐Y gastric anastomosis since EUS cannot reach the desired location (Wilson 2010).
Implications of negative tests
In general, patients with negative tests in one step do not undergo further testing. For example, a person with no suggestion of common bile duct stones on liver function tests and ultrasound will not undergo further testing for common bile duct stones. Similarly, persons having no suggestion of common bile duct stones on MRCP or EUS will not undergo further testing for common bile duct stones, and persons with no suggestion of common bile duct stones on ERCP or IOC will not undergo common bile duct clearance. Individuals with a false negative test result can develop complications of common bile duct stones such as cholangitis and pancreatitis but the natural history of such patients with negative tests in terms of the frequency with which these complications develop is not known. However, it is generally recommended that common bile duct stones are removed when they are identified because of the serious complications associated with their presence (Williams 2008). Although this practice is not evidence‐based, this shows the perception among hepato‐pancreato biliary surgeons and gastroenterologists that it is important not to miss common bile duct stones.
Prior test(s)
Ultrasound and liver function tests are usually used prior to EUS and MRCP (see Figure 1).
Role of index test(s)
EUS and MRCP are employed as add‐on tests in the second step of the diagnostic pathway. If positive, the tests are followed by diagnostic tests in the third step of the diagnostic pathway. If negative, the diagnosis of common bile duct stones is ruled out and further invasive testing is not performed.
Alternative test(s)
There are no alternative tests to EUS and MRCP that are in routine clinical use at the second step of the diagnostic pathway. CT cholangiography and intravenous cholangiography may be used in the second step of the diagnostic pathway but are not used routinely. A small proportion of surgeons use postoperative endoscopic sphincterotomy for management of common bile duct stones. In persons in whom postoperative sphincterotomy is used for management of common bile duct stones, IOC may be considered as an alternative to EUS and MRCP.
Rationale
There are several other benign and malignant conditions that may present in a similar manner to common bile duct stones. Benign (non‐cancerous) causes of obstructive jaundice include primary sclerosing cholangitis (Penz‐Osterreicher 2011), primary biliary cirrhosis (Hirschfield 2011), chronic pancreatitis (Abdallah 2007), autoimmune pancreatitis (Lin 2008), inflammatory strictures of the common bile duct (Krishna 2008), and strictures of the common bile duct caused by prior instrumentation (Lillemoe 2000; Tang 2011). Malignant (cancerous) causes of obstructive jaundice include cholangiocarcinoma (Siddiqui 2011), cancer of the ampulla of Vater as well as other periampullary cancers (Hamade 2005; Choi 2011; Park 2011), and carcinoma of the pancreas (Singh 1990; Kalady 2004). It is important to differentiate between the causes of obstructive jaundice in order to initiate appropriate treatment. The correct diagnosis of common bile duct stones is an essential contribution to this differentiation.
Common bile duct stones are responsible for a range of complications. Common bile duct stones lead to pancreatitis in about 33% to 50% of the patients who have them (Corfield 1985; Toh 2000) and cause mortality in about 6% to 9% of these patients (Mann 1994; Toh 2000). Acute cholangitis appears in 2% to 9% of patients admitted for gallstone disease, with mortality around 24% (Salek 2009). Therefore, it is important to diagnose common bile duct stones in order to treat patients and prevent such complications.
The preferred option for the treatment of common bile duct stones is currently endoscopic sphincterotomy (ES) with balloon trawling followed by laparoscopic cholecystectomy (Ludwig 2001; Spelsberg 2009). Other options include open cholecystectomy with open common bile duct exploration, laparoscopic cholecystectomy with laparoscopic common bile duct exploration, and laparoscopic cholecystectomy with ES (Hong 2006; Dasari 2013). It has been found that approximately half of patients with jaundice, abnormal liver function tests, and common bile duct dilation on ultrasound do not actually have common bile duct stones (Hoyuela 1999) and, therefore, these patients undergo invasive procedures unnecessarily. Accurate diagnosis of common bile duct stones may avoid unnecessary procedures and the complications associated with these procedures. Invasive tests can result in complications; for example, endoscopic retrograde cholangiopancreatography with endoscopic sphincterotomy (ERCP‐ES) can have life‐threatening complications such as pancreatitis (Gurusamy 2011). Accurate diagnosis of common bile duct stones using non‐invasive tests can avoid these complications.
Currently, there are no Cochrane reviews of studies assessing the accuracy of different tests for diagnosing common bile duct stones. This review is one of three reviews evaluating the diagnostic accuracy of different tests in the diagnosis of common bile duct stones and will help in the development of an evidence‐based algorithm for diagnosis of common bile duct stones.
Objectives
To determine and compare the accuracy of EUS and MRCP for the diagnosis of common bile duct stones.
Secondary objectives
To investigate variation in the diagnostic accuracy of EUS and MRCP according to the following potential sources of heterogeneity.
Studies at low risk of bias versus those with unclear or high risk of bias (as assessed by the QUADAS‐2) tool (Table 2).
Full text publications versus abstracts (this may indicate publication bias if there is an association between the results of the study and the study reaching full publication) (Eloubeidi 2001).
Prospective versus retrospective studies.
Symptomatic versus asymptomatic common bile duct stones (the presence of symptoms may increase the pre‐test probability). Symptomatic patients are defined as patients showing upper right quadrant abdominal pain, jaundice, acute cholangitis or acute pancreatitis (Anciaux 1986; Roston 1997; Raraty 1998; Toh 2000; Tranter 2003).
Prevalence of common bile duct stones in each included study. The prevalence of common bile duct stones in the population analysed by each included study may vary and cause heterogeneity. Prevalence may also change with the presence of patients with comorbidities that would predispose them to common bile duct stones such as primary sclerosing cholangitis, Caroli's disease, hypercholesterolaemia, sickle cell anaemia, and sphincter of Oddi dysfunction.
Proportion of patients with previous cholecystectomy. Cholecystectomy may cause dilatation of the common bile duct (Benjaminov 2013) and subsequently change the accuracy of the index test, particularly imaging modalities.
Proportion of patients with common bile duct strictures (only for index tests that use contrast material, as strictures may prevent contrast material from filling the common bile duct completely and, therefore, change the accuracy of the index test).
1. Application of the QUADAS‐2 tool for assessing methodological quality of included studies.
| Domain 1: Patient sampling | Signalling question | Signalling question | Signalling question | Risk of bias | Concerns for applicability |
| Patient sampling | Was a consecutive or random sample of patients enrolled? | Was a case‐control design avoided? | Did the study avoid inappropriate exclusions? | Could the selection of patients have introduced bias? | Were there concerns that the included patients and setting did not match the review question? |
| Yes: all consecutive patients or random sample of patients with suspected common bile duct stones were enrolled No: selected patients were enrolled Unclear: this was not clear form the report |
Yes: case‐control design was avoided. No: case‐control design was not avoided Unclear: this was not clear from the report. |
Yes: the study avoided inappropriate exclusions (i.e., difficult to diagnose patients) No: the study excluded patients inappropriately Unclear: this was not clear from the report |
Low risk: 'yes' for all signalling questions High risk: 'no' or 'unclear' for at least one signalling question |
Low concern: the selected patients represent the patients in whom the tests will be used in clinical practice (please see diagnostic pathway (Figure 1) High concern: there was high concern that patient selection was performed in a such a way that the included patients did not represent the patients in whom the tests will be used in clinical practice |
|
| Domain 2: Index test | |||||
| Index test(s) | Were the index test results interpreted without knowledge of the results of the reference standard? | If a threshold was used, was it pre‐specified? | Could the conduct or interpretation of the index test have introduced bias? | Were there concerns that the index test, its conduct, or interpretation differ from the review question? | |
| Yes: index test results were interpreted without knowledge of the results of the reference standard No: index test results were interpreted with knowledge of the results of the reference standard Unclear: this was not clear from the report |
Not applicable | Low risk: 'yes' for all signalling questions High risk: 'no' or 'unclear' for at least one of the two signalling questions |
High concern: there was high concern that the conduct or interpretation of the index test differs from the way it is likely to be used in clinical practice Low concern: there was low concern that the conduct or interpretation of the index test differs from the way it is likely to be used in clinical practice |
||
| Domain 3: Reference standard | |||||
| Target condition and reference standard(s) | Was the reference standard likely to correctly classify the target condition? | Were the reference standard results interpreted without knowledge of the results of the index tests? | Could the reference standard, its conduct, or its interpretation have introduced bias? | Were there concerns that the target condition as defined by the reference standard does not match the review question? | |
| Yes: all patients underwent the acceptable reference standard No: if all patients did not undergo an acceptable reference standard. Such studies will be excluded from the review Unclear: if the reference standard that the patients underwent was not stated. Such studies will be excluded from the review |
Yes: reference standard results were interpreted without knowledge of the results of the index test No: reference standard results were interpreted with the knowledge of the results of the index test Unclear: this was not clear from the report |
Low risk: 'yes' for all signalling questions High risk: 'no' or 'unclear' for at least one of the two signalling questions |
Low concern: patients underwent endoscopic or surgical exploration for common bile duct stone High concern: all patients did not undergo endoscopic or surgical exploration for common bile duct stone |
||
| Domain 4: Flow and timing | |||||
| Flow and timing | Was there an appropriate interval between index test and reference standard? | Did all patients receive the same reference standard? | Were all patients included in the analysis? | Could the patient flow have introduced bias? | |
| Yes: the interval between index test and reference standard was shorter than or equal to four weeks (arbitrary choice) No: the interval between index test and reference standard was longer than four weeks Unclear: this was not clear from the report |
Yes: all patients underwent endoscopic or surgical exploration for common bile duct stone irrespective of the index test results No: patients underwent endoscopic or surgical exploration if the index test results were positive and underwent clinical follow‐up for at least 6 months if the index test results were negative Unclear: this was not clear from the report. Such studies were excluded |
Yes: all patients meeting the selection criteria (selected patients) were included in the analysis, or data on all the selected patients were available so that a 2 x 2 table including all selected patients could be constructed No: not all patients meeting the selection criteria were included in the analysis or the 2 x 2 table could not be constructed using data on all selected patients Unclear: this was not clear from the report |
Low risk: 'yes' for all signalling questions High risk: 'no' or 'unclear' for at least one signalling question |
Methods
Criteria for considering studies for this review
Types of studies
We included studies providing cross‐sectional information comparing one or more of the index tests against a reference standard in the appropriate patient population (see Participants). We included studies irrespective of language or publication status, or whether data were collected prospectively or retrospectively. We planned to include comparative studies in which EUS and MRCP were performed in the same study population, either by giving all patients both index tests or by randomly allocating patients to receive MRCP or EUS. We planned to exclude diagnostic case‐control studies if there were at least four cross‐sectional or comparative studies.
Participants
Patients at risk or suspected of having common bile duct stones with or without prior diagnosis of cholelithiasis; with or without symptoms and complications of common bile duct stones or with or without prior treatment for common bile duct stones; and before or after cholecystectomy.
Index tests
Endoscopic ultrasound (EUS) and magnetic resonance retrograde cholangiopancreatography (MRCP).
Target conditions
Common bile duct stones.
Reference standards
We accepted the following reference standards.
For test positives, we accepted confirmation of a common bile duct stone by extraction of the stone (irrespective of whether this was done by surgical or endoscopic methods).
For test negatives, we acknowledged that there was no way of being absolutely sure that there were no common bile duct stones. However, we accepted negative results by surgical or endoscopic negative exploration of the common bile duct, or symptom‐free follow‐up for at least six months as the reference standard. Surgical or endoscopic exploration is adequate but it is not commonly used in patients with negative index tests because of its invasive nature. Therefore, we accepted follow‐up as a less adequate reference test. Negative exploration of the common bile duct is likely to be a better reference standard than follow‐up for at least six months since most stones already present in the common bile duct are likely to be identified and extracted in this fashion. Six months is an arbitrary choice but we anticipated that most common bile duct stones will manifest during this period.
Search methods for identification of studies
Electronic searches
We searched MEDLINE via PubMed (January 1946 to September 2012), EMBASE via OvidSP (January 1947 to September 2012), Science Citation Index Expanded via Web of Knowledge (January 1898 to September 2012), BIOSIS via Web of Knowledge (January 1969 to September 2012), and Clinicaltrials.gov (September 2012). The search strategies are shown in Appendix 1. We used a common search strategy for the three reviews of which this review is one. The other two reviews assess the diagnostic accuracy of transabdominal ultrasound, liver function tests, ERCP, and IOC (Gurusamy 2015a; Gurusamy 2015b). We also identified systematic reviews from the Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment (HTA), Medion, and ARIF (Aggressive Research Intelligence Facility) databases in order to search their reference lists (please see searching other resources).
Searching other resources
We searched the references of the included studies and systematic reviews related to the topic to identify further studies. We also searched for additional articles related to the included studies by performing the 'related search' function in MEDLINE (PubMed) and EMBASE (OvidSP) and a 'citing reference' search (search the articles which cited the included articles) (Sampson 2008) in Science Citation Index Expanded and EMBASE (OvidSP).
Data collection and analysis
Selection of studies
Three authors (VG and DH or GP) searched the references independently for identification of relevant studies. We obtained full texts for the references that at least one of the authors considered relevant. Two review authors (VG and DH or GP) assessed the full text articles independently. Any differences in study selection were arbitrated by KG. We selected the studies that met the inclusion criteria for data extraction. We included abstracts if sufficient data to create a 2 x 2 table were provided.
Data extraction and management
Two authors (KG and VG) independently extracted the following data from each included study.
First author of report.
Year of publication of report.
Study design (prospective or retrospective; cross‐sectional studies or randomised clinical trials).
Inclusion and exclusion criteria for individual studies.
Total number of patients.
Number of males and females.
Mean age of the participants.
Tests carried out prior to index test.
Index test.
Reference standard.
Number of true positives, false positives, true negatives, and false negatives.
We sought further information on the diagnostic test accuracy data and assessment of methodological quality (please see Assessment of methodological quality) from the authors of the studies, if necessary. We resolved any differences between the review authors by discussion till a consensus was reached. We extracted the data excluding participants with indeterminate results but recorded the number of indeterminates and the reference standard results of the patients with indeterminate results.
Assessment of methodological quality
We adopted the quality assessment of diagnostic accuracy studies assessment tool (QUADAS‐2) (Whiting 2006; Whiting 2011) for assessment of the methodological quality of included studies as described in Table 2. We considered studies classified at low risk of bias and low concern regarding applicability to the review question as studies at low risk of bias. Any differences in the methodological quality assessments were resolved by discussion between the review authors until a consensus was reached. We sought further information from study authors in order to accurately assess the methodological quality of the included studies.
Statistical analysis and data synthesis
To visually explore between study variation in the performance of each test, we plotted estimates of sensitivity and specificity from each study on forest plots and in receiver operating characteristic (ROC) space. Because our focus of inference was summary points, we used the bivariate model (Reitsma 2005; Chu 2006) to jointly summarise the sensitivity and specificity of each test. This model accounts for between study variability in estimates of sensitivity and specificity through the inclusion of random effects for the logit sensitivity and logit specificity parameters of the bivariate model.
Using all available studies (that is, an indirect comparison), we compared the diagnostic accuracy of EUS and MRCP by including covariate terms for test type in the bivariate model to estimate differences in the sensitivity and specificity of the two tests. We also allowed the variances of the random effects and their covariance to depend on test type thus allowing the variances to differ between tests. We used likelihood ratio tests to compare the fit of different models, and we also compared the estimates of sensitivity and specificity between models to check the robustness of our assumptions about the variances of the random effects. If studies that evaluated EUS and MRCP in the same study population were available, we planned to also perform a direct head‐to‐head comparison by limiting the test comparison to such studies. Meta‐analyses were performed using the xtmelogit command in Stata version 13 (Stata‐Corp, College Station, Texas, USA).
We created a table of pre‐test probabilities (using the observed median and range of prevalence from the included studies) against post‐test probabilities. The post‐test probabilities were calculated using these pre‐test probabilities and the summary positive and negative likelihood ratios were derived by using the Stata _diparm command and functions of the parameter estimates from the bivariate model that we fitted to estimate the summary sensitivities and specificities.
Investigations of heterogeneity
We visually inspected forest plots of sensitivity and specificity, and summary ROC plots to investigate the potential sources of heterogeneity as stated in the Secondary objectives. Where possible given the number of included studies, we planned to formally explore heterogeneity by adding each potential source of heterogeneity listed above as a covariate in the bivariate model (meta‐regression with one covariate at a time).
Sensitivity analyses
Exclusion of participants with uninterpretable results can result in an overestimation of diagnostic test accuracy (Schuetz 2012). In practice, uninterpretable test results will generally be considered as test negatives. Therefore, we planned to perform sensitivity analyses by including uninterpretable test results as test negatives, if sufficient data were available.
Assessment of reporting bias
As described in the Investigations of heterogeneity section, we planned to investigate whether the sensitivity and specificity of the tests differed between studies that were published as full texts and those that were available only as abstracts.
Results
Results of the search
We identified a total of 22,789 references through electronic searches of MEDLINE (n = 8292), EMBASE (n = 10,029), Science Citation Index Expanded and Biosis (n = 4276), and DARE and HTA in the Cochrane Library (n = 192). One additional reference was identified by searching other sources. We excluded 5866 duplicates and 16,718 clearly irrelevant references through reading abstracts. We assessed the remaining 206 references for eligibility by reading the full texts of the publications. We excluded 188 full text articles. The main reasons for exclusion were inappropriate reference standards and lack of data to construct the 2 x 2 tables needed for meta‐analyses. The list of excluded studies and reasons for exclusion are listed in the Characteristics of excluded studies table. We included a total of 18 studies. We were able to obtain additional information from the authors of two of the studies (Prat 1996; Montariol 1998). The flow of studies through the selection process is shown in Figure 2.
2.
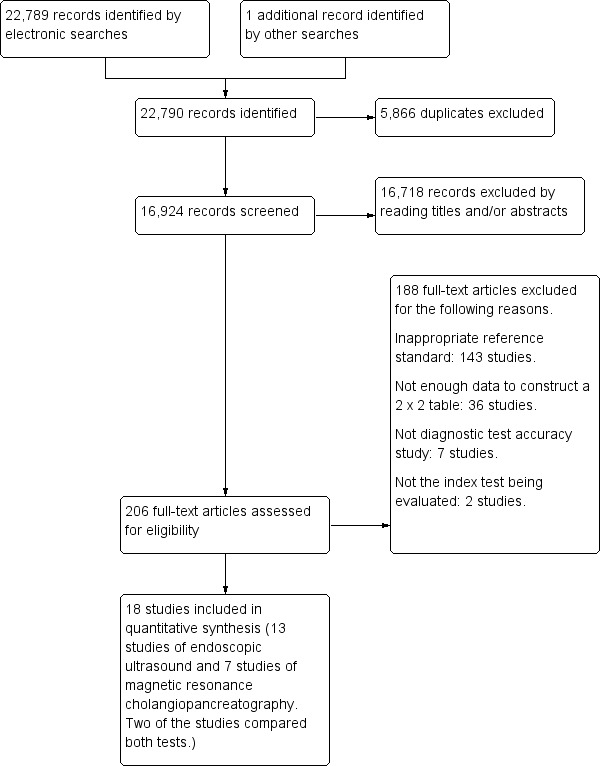
Flow of studies through the screening process.
Characteristics of included studies
The characteristics of the included studies are summarised in the Characteristics of included studies table. We included a total of 18 studies involving 2366 participants in this systematic review. EUS was evaluated by 13 studies involving 1537 participants (686 participants with common bile duct stones and 851 participants without common bile duct stones), and MRCP was evaluated by seven studies involving 996 participants (361 cases and 635 participants without common bile duct stones). The median pre‐test probability of common bile duct stones was 0.41, or 41%. The minimum pre‐test probability of common bile duct stones in the studies was 0.14, and the maximum pre‐test probability was 0.68. Fifteen (Prat 1996; Norton 1997; Canto 1998; Montariol 1998; De Ledinghen 1999; Liu 2001; Boraschi 2002; Jendresen 2002; Kohut 2002; Buscarini 2003; Gautier 2004; Guarise 2005; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007) of the 18 included studies were full text publications. Ten studies (Canto 1998; Montariol 1998; De Ledinghen 1999; Liu 2001; Fazel 2002; Jendresen 2002; Kohut 2002; Buscarini 2003; Gautier 2004; Choo 2012) were prospective studies, one study (Ang 2012) was a retrospective study, and it was unclear whether the remaining studies were prospective or retrospective (Prat 1996; Norton 1997; Boraschi 2002; Guarise 2005; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007). Ten studies (Prat 1996; Norton 1997; Canto 1998; De Ledinghen 1999; Boraschi 2002; Fazel 2002; Kohut 2002; Buscarini 2003; Fernandez‐Esparrach 2007; Ang 2012) included patients who were suspected of having common bile duct stones based on abnormal liver function tests; abnormal transabdominal ultrasound; symptoms such as obstructive jaundice, cholangitis, or pancreatitis; or a combination of the above. One study (Liu 2001) included only patients with pancreatitis and another study (Ney 2005) included patients with abnormal liver function tests or ultrasound but excluded those with symptoms. One study (Montariol 1998) excluded patients with abnormal liver function tests, abnormal transabdominal ultrasound, or symptoms; and one study (Choo 2012) included only patients with a positive intraoperative cholangiogram. Three studies (Gautier 2004; Guarise 2005; Miletic 2006) reported that they performed the test in patients with suspected common bile duct stones but the reasons for suspicion were not stated. The reason for performing the test was not stated in the remaining study (Jendresen 2002). Six studies (Norton 1997; Canto 1998; Montariol 1998; Boraschi 2002; Jendresen 2002; Ney 2005) included participants who had not undergone previous cholecystectomy. In one study (Choo 2012) all the participants had undergone cholecystectomy, while in three studies (Prat 1996; Liu 2001; Buscarini 2003) 8% to 75% of participants had undergone cholecystectomy. The proportion of participants who had undergone cholecystectomy was not stated in the remaining studies. The proportion of patients with common bile duct strictures was not stated in any of the studies.
The criteria for a positive EUS varied between the studies that reported their criteria. While the studies used hyperechoic shadowing inside the common bile duct as the main criterion (Norton 1997; Canto 1998; Montariol 1998; De Ledinghen 1999; Liu 2001; Kohut 2002; Buscarini 2003; Ney 2005; Fernandez‐Esparrach 2007), some studies stipulated that these shadows should have acoustic shadowing (Canto 1998; Montariol 1998; Kohut 2002; Ney 2005) and should be mobile (Ney 2005). The criteria for a positive MRCP were signal defects within the common bile duct, defined variably as foci or rounded and oval in some studies (De Ledinghen 1999; Boraschi 2002; Jendresen 2002; Gautier 2004; Guarise 2005; Fernandez‐Esparrach 2007).
Methodological quality of included studies
The methodological quality of the included studies is summarised in Figure 3 and Figure 4. Not one of the included studies was of high methodological quality. Regarding applicability concerns, none of the studies were of low concern in all three domains.
3.
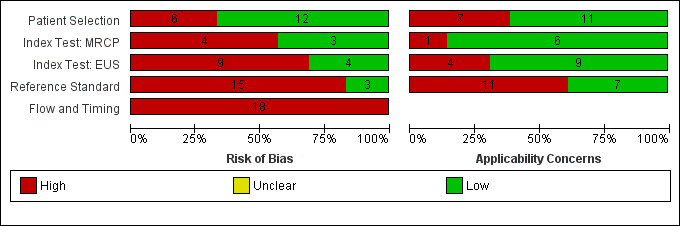
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies. Each bar shows the number of studies in each category. The index test domain was evaluated separately for each test. Of the 18 included studies, 7 studies evaluated MRCP and 13 studies evaluated EUS; the numbers do not add up to 18 because two of the studies evaluated both tests.
4.
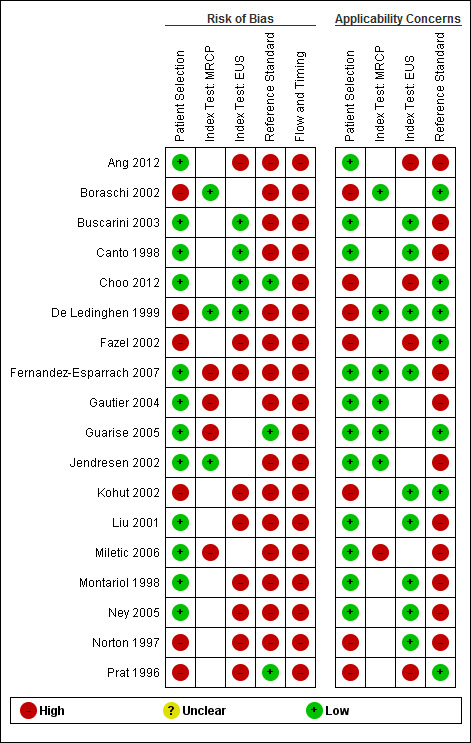
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study. In the index test domain, the empty white cell indicates that the study did not evaluate the test.
Patient selection domain
In the patient selection domain, 12 studies (Canto 1998; Montariol 1998; Liu 2001; Jendresen 2002; Buscarini 2003; Gautier 2004; Guarise 2005; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007; Ang 2012; Choo 2012) had low risk of bias. Eleven studies (Canto 1998; Montariol 1998; Liu 2001; Jendresen 2002; Buscarini 2003; Gautier 2004; Guarise 2005; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007; Ang 2012) had low applicability concerns. The remaining studies were at high risk of bias and were of high concern for applicability because patient recruitment was unclear (Norton 1997; De Ledinghen 1999; Boraschi 2002; Fazel 2002; Kohut 2002), participants were excluded inappropriately (Prat 1996), or there were concerns that the participants did not match the types of participants that will undergo these tests in routine clinical practice (Choo 2012).
Index test domain
In the index test domain, seven studies had low risk of bias; four were EUS only studies (Prat 1996; Canto 1998; Buscarini 2003; Choo 2012), two (Boraschi 2002; Jendresen 2002) were MRCP only studies, and one (De Ledinghen 1999) evaluated both EUS and MRCP. The remaining studies were at high risk of bias because it was not clear whether the index test results were interpreted without knowledge of the reference standard results. Thirteen studies were of low concern for applicability; seven (Norton 1997; Canto 1998; Montariol 1998; Liu 2001; Kohut 2002; Buscarini 2003; Ney 2005) were EUS only studies, four (Boraschi 2002; Jendresen 2002; Gautier 2004; Guarise 2005) were MRCP only studies, and two (De Ledinghen 1999; Fernandez‐Esparrach 2007) were studies of both EUS and MRCP. The remaining studies (Prat 1996; Boraschi 2002; Fazel 2002; Gautier 2004; Guarise 2005; Miletic 2006; Ang 2012; Choo 2012) were of high concern for applicability because the criteria for a positive test were not stated.
Reference standard domain
In the reference standard domain, three studies (Prat 1996; Guarise 2005; Choo 2012) had low risk of bias. The remaining studies were at high risk of bias because it was either not clear whether the reference standards were interpreted without knowledge of the index test results (Norton 1997; Canto 1998; De Ledinghen 1999; Liu 2001; Boraschi 2002; Fazel 2002; Kohut 2002; Buscarini 2003; Gautier 2004; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007; Ang 2012) or it was clear that the reference standards were interpreted with the knowledge of the index test results (Montariol 1998; Jendresen 2002). Seven studies (Prat 1996; De Ledinghen 1999; Boraschi 2002; Fazel 2002; Kohut 2002; Guarise 2005; Choo 2012) gave low concern about applicability. The remaining 11 studies (Norton 1997; Canto 1998; Montariol 1998; Liu 2001; Jendresen 2002; Buscarini 2003; Gautier 2004; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007; Ang 2012) were of high concern because endoscopic or surgical clearance of the common bile duct was achieved in patients with a positive test and clinical follow‐up was performed in patients with a negative test.
Flow and timing domain
In the flow and timing domain, all 18 studies were at high risk of bias for the following reasons. Six studies (De Ledinghen 1999; Boraschi 2002; Fazel 2002; Guarise 2005; Fernandez‐Esparrach 2007; Ang 2012) did not report the time interval between the index test and reference standard, and 11 studies (Norton 1997; Canto 1998; Montariol 1998; Liu 2001; Jendresen 2002; Buscarini 2003; Gautier 2004; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007; Ang 2012) did not use the same reference standard since endoscopic or surgical clearance of the common bile duct was achieved in patients with a positive test and clinical follow‐up was performed in patients with a negative test. It was not clear whether all the patients were included in the analysis in six studies (Norton 1997; Canto 1998; Fazel 2002; Kohut 2002; Ang 2012; Choo 2012), while some patients were excluded from the analysis in nine studies (Prat 1996; Montariol 1998; De Ledinghen 1999; Boraschi 2002; Buscarini 2003; Gautier 2004; Guarise 2005; Miletic 2006; Fernandez‐Esparrach 2007).
Findings
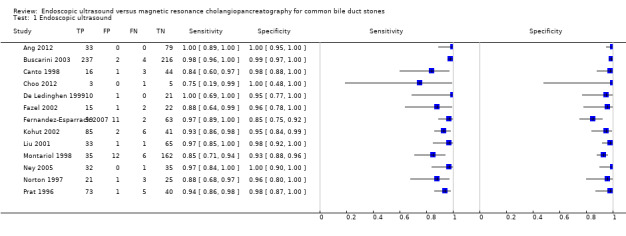
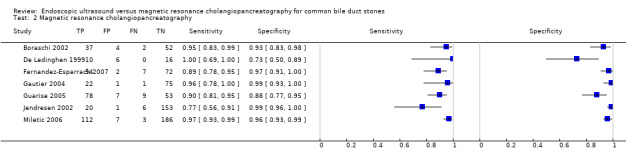
The results are summarised in Table 1, Figure 5, and Figure 6.
5.
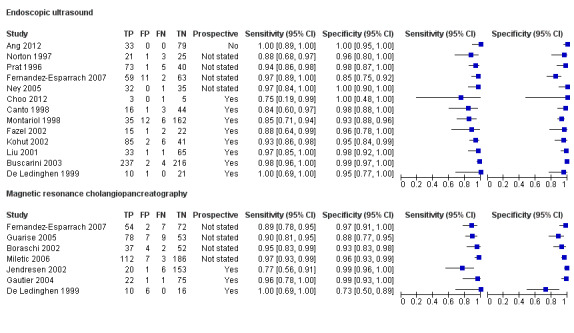
Forest plot of endoscopic ultrasound and magnetic resonance cholangiopancreatography for diagnosis of common bile duct stones. The plot shows study specific estimates of sensitivity and specificity (with 95% confidence intervals). The studies are ordered according to study design (prospective or not), sensitivity and study identifier; FN = false negative; FP = false positive; TN = true negative; TP = true positive.
6.
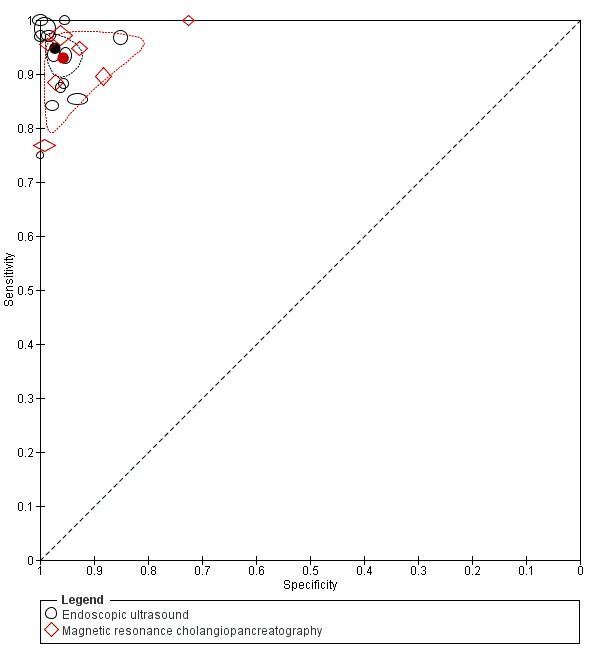
Summary ROC plot of endoscopic ultrasound and magnetic resonance cholangiopancreatography for diagnosis of common bile duct stones. For each test, each symbol represents the pair of sensitivity and specificity from a study and the symbol is scaled according to the sample size of the study. The solid circles represent the summary sensitivity and specificity for each test. Each summary point is surrounded by a 95% confidence region.
Endoscopic ultrasound (EUS)
The sensitivities of the 13 studies ranged between 0.75 and 1.00, and the specificities ranged between 0.85 and 1.00 (Figure 5). The summary sensitivity (95% CI) and summary specificity (95% CI) were 0.95 (95% CI 0.91 to 0.97) and 0.97 (95% CI 0.94 to 0.99). The summary positive and negative likelihood ratios were 34.4 (95% CI 15.2 to 78.1) and 0.05 (95% CI 0.03 to 0.09). At the median pre‐test probability of common bile duct stones of 41%, the post‐test probabilities (with 95% CI) associated with positive and negative tests were 0.96 (95% CI 0.92 to 0.98) and 0.03 (95% CI 0.02 to 0.06) respectively. At the minimum pre‐test probability of 14%, the post‐test probabilities associated with positive and negative tests were 0.85 (95% CI 0.72 to 0.93) and 0.01 (95% CI 0.01 to 0.02). At the maximum pre‐test probability of 68%, the post‐test probabilities associated with positive and negative tests were 0.99 (95% CI 0.97 to 0.99) and 0.10 (95% CI 0.06 to 0.16).
Magnetic resonance cholangiopancreatography (MRCP)
The sensitivities ranged between 0.77 and 1.00, and the specificities ranged between 0.73 and 0.99 (Figure 5). The summary sensitivity (95% CI) and summary specificity (95% CI) were 0.93 (95% CI 0.87 to 0.96) and 0.96 (95% CI 0.89 to 0.98). The summary positive and negative likelihood ratios were 21.7 (95% CI 9.3 to 50.7) and 0.07 (95% CI 0.04 to 0.14). At the median pre‐test probability of common bile duct stones of 41%, the post‐test probabilities associated with positive and negative tests were 0.94 (95% CI 0.87 to 0.97) and 0.05 (95% CI 0.03 to 0.09). At the minimum pre‐test probability of 14%, the post‐test probabilities associated with positive and negative tests were 0.79 (95% CI 0.61 to 0.90) and 0.01 (95% CI 0.01 to 0.02). At the maximum pre‐test probability of 68%, the post‐test probabilities associated with positive and negative tests were 0.98 (95% CI 0.95 to 0.99) and 0.13 (95% CI 0.08 to 0.23).
Endoscopic ultrasound (EUS) versus magnetic resonance cholangiopancreatography (MRCP)
Only two studies (De Ledinghen 1999; Fernandez‐Esparrach 2007) performed EUS and MRCP in the same participants and so we were unable to perform a direct comparison. We performed an indirect comparison of EUS and MRCP (Figure 6). There was no evidence of a difference in sensitivity or specificity between EUS and MRCP (P value = 0.5).
Investigation of sources of heterogeneity
We were unable to formally explore potential sources of heterogeneity for MRCP because there were only seven studies. For EUS, we found no evidence of a difference in sensitivity or specificity between full text publications (10 studies) and abstracts (3 studies) (P value = 0.5). The prevalence of common bile duct stones in the studies of EUS ranged between 16% and 63%. There was no evidence of an effect of prevalence on test performance (P value = 0.5).
We were unable to explore the effect of the following potential sources of heterogeneity.
Studies at low risk of bias versus those at unclear or high risk of bias: the analysis could not be performed because all the studies were of low methodological quality.
Prospective studies versus retrospective studies: eight studies were prospective, one was retrospective and four studies did not provide this information.
Symptomatic versus asymptomatic participants: this information was available in five studies only (Norton 1997; Montariol 1998; Buscarini 2003; Ney 2005; Choo 2012). All participants in these studies were symptomatic.
Proportion of patients with common bile duct strictures: the information was not available in any of the studies.
Proportion of patients with previous cholecystectomy: four studies did not include patients with previous cholecystectomy and five studies included between 8% and 100% of such patients.
Sensitivity analyses
Endoscopic ultrasound (EUS)
Two studies (Prat 1996; Buscarini 2003) reported participants with uninterpretable results together with their reference standard results. Five studies (Prat 1996; Montariol 1998; De Ledinghen 1999; Buscarini 2003; Fernandez‐Esparrach 2007) reported uninterpretable results but did not provide the corresponding reference standard results. We did not perform sensitivity analyses because data were sparse.
Magnetic resonance cholangiopancreatography (MRCP)
None of the studies reported participants with uninterpretable results for whom the reference standard results were available and so we did not perform sensitivity analyses. Six studies (De Ledinghen 1999; Boraschi 2002; Gautier 2004; Guarise 2005; Miletic 2006; Fernandez‐Esparrach 2007) reported participants with uninterpretable results for whom the reference standard results were not available.
Discussion
Summary of main results
The results are summarised in Table 1. We included 13 studies that evaluated the diagnostic accuracy of EUS and seven studies that evaluated the diagnostic accuracy of MRCP. The summary sensitivity and specificity of EUS were 0.95 (95% CI 0.91 to 0.97) and 0.97 (95% CI 0.94 to 0.99). The summary sensitivity and specificity of MRCP were 0.93 (95% CI 0.87 to 0.96) and 0.96 (95% CI 0.89 to 0.98). Sensitivity and specificity did not differ significantly between the two tests. The median pre‐test probability of common bile duct stones from the included studies was 41%. This proportion is higher than in the general population (Barbara 1987; Loria 1994) or in the population of patients undergoing cholecystectomy for gallbladder stones (Arnold 1979; Lill 2010; Yousefpour Azary 2011). This is probably due to the fact that EUS and MRCP are performed as triage tests in the second step of the diagnostic pathway, and only preselected patients with abnormal liver function tests or abnormal abdominal ultrasound, or both, were included in these studies. The probability of common bile duct stones in such a selected population has been reported to be about 36% (Rahman 2010), which is similar to the pre‐test probability in this review. For a pre‐test probability of 41%, the median observed in this review, the post‐test probabilities associated with positive and negative EUS were 0.96 (95% CI 0.92 to 0.98) and 0.03 (95% CI 0.02 to 0.06). At the same pre‐test probability, the post‐test probabilities associated with positive and negative MRCP were 0.94 (95% CI 0.87 to 0.97) and 0.05 (95% CI 0.03 to 0.09).
The choice of whether to use MRCP or EUS will be based on the availability and expertise to perform these tests, and whether patients can tolerate the procedure. For example, MRCP may not be suitable for people with cardiac pacemakers or claustrophobia. Endoscopic ultrasound may not be suitable for people who have undergone gastric bypass procedures, including Roux‐en‐Y anastomosis for various indications such as cancer and obesity surgery. The proportion of people with such contra‐indications to the tests is likely to be low and it is very unlikely that both tests will be unsuitable in the same person.
Strengths and weaknesses of the review
We conducted a thorough literature search and included full text publications and abstracts without any language restrictions. The use of diagnostic test accuracy filters may lead to the loss of some studies (Doust 2005) and so we did not use any diagnostic test accuracy filters. Two authors independently identified and extracted data from the studies, potentially decreasing errors related to single data extraction (Buscemi 2006). To avoid potential bias due to the use of an inadequate reference standard, we restricted the studies to those with appropriate reference standards.
The major limitation in the review process was our inability to formally explore all the potential sources of heterogeneity, as planned, because of limited data. Factors such as the proportion of participants with previous cholecystectomy may affect test accuracy but this information was not fully available. It was also not possible to perform a direct comparison of the tests because only two studies performed both tests in the same patients. Therefore, the evidence relies on an indirect test comparison which is prone to confounding and may give different results compared to a more reliable direct comparison (Takwoingi 2013). Endoscopic or surgical extraction was used in all participants in only seven studies (Prat 1996; De Ledinghen 1999; Boraschi 2002; Fazel 2002; Kohut 2002; Guarise 2005; Choo 2012). In the remaining 11 studies endoscopic or surgical clearance of the common bile duct was achieved in patients with a positive index test and clinical follow‐up was performed in patients with a negative index test (Norton 1997; Canto 1998; Montariol 1998; Liu 2001; Jendresen 2002; Buscarini 2003; Gautier 2004; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007; Ang 2012). This may result in overestimation of diagnostic accuracy although there was no evidence that this was the case. However, we acknowledge that even the best reference standard of endoscopic or surgical extraction of common bile duct stones can result in misclassification and hence an alteration in diagnostic accuracy if one or more stones reach the small bowel without the knowledge of the person who performed the common bile duct stone extraction. The use of different reference standards may also reflect the belief of the study authors about the probability of participants harbouring common bile duct stones. It is quite possible that in studies in which surgical or endoscopic clearance was performed in all participants (Prat 1996; De Ledinghen 1999; Boraschi 2002; Fazel 2002; Kohut 2002; Guarise 2005; Choo 2012) included participants were at greater risk of having common bile duct stones because of their symptoms (that is, they were more symptomatic) compared to the study in which participants with a positive index test underwent surgical or endoscopic extraction of stones and participants with a negative index test were followed up clinically (Norton 1997; Canto 1998; Montariol 1998; Liu 2001; Jendresen 2002; Buscarini 2003; Gautier 2004; Ney 2005; Miletic 2006; Fernandez‐Esparrach 2007; Ang 2012). This was not evident from pre‐test probabilities of common bile duct stones in studies in which all participants underwent endoscopic or surgical extraction compared to those in which participants received different reference standards.
The major limitation of the included studies was that none of the studies were of good methodological quality. There was a high proportion of studies at high risk of bias and with high concern regarding applicability in all the four domains of the QUADAS‐2 tool. This makes the validity of the results questionable. We considered endoscopic or surgical extraction of common bile duct stones in all participants as a better reference standard than a combination of extraction of common bile duct stones in participants with a positive index test and clinical follow‐up in those with a negative index test. However, we acknowledge that even this ideal reference standard can result in misclassification and hence an alteration in diagnostic test accuracy if one or more stones reach the small bowel without the knowledge of the person performing the extraction. Despite these shortcomings, these studies provide the best available evidence on the topic.
There are other published systematic reviews on diagnostic accuracy of EUS and MRCP for common bile duct stones (Mark 2002; Verma 2006; Ledro‐Cano 2007; McMahon 2008). The summary sensitivity of EUS in these systematic reviews ranged from 90% to 93%, and specificity ranged from 96% to 99%. The summary sensitivity of MRCP ranged from 85% to 87% and specificity ranged from 93% to 95%. In general, in spite of differences in the methods used, the summary sensitivities and specificities appear broadly similar between these reviews and the current review.
Applicability of findings to the review question
Most of the participants included in the review had prior abnormal transabdominal ultrasound or liver function tests or were symptomatic, and so the findings of this review are only applicable to such people. The diagnostic accuracy in asymptomatic people with normal ultrasound and liver function tests may be different. The methods of EUS and MRCP that were used in the included studies have not changed considerably over time and so the results from old studies (the earliest publication included in this review was in 1996 for EUS and 1999 for MRCP) are still applicable. The reference standard that we used in this review is a reliable reference standard and so the findings are applicable to the review question. However, it should be noted that the tests were performed in secondary or tertiary centres and our findings are therefore applicable only in this setting. The decision to use these tests as triage tests prior to confirmation with invasive tests in a state‐funded health system is dependent upon a formal cost‐utility analysis, which is beyond the scope of this review.
In this review, we have assessed the diagnostic test accuracy of EUS and MRCP in the diagnosis of common bile duct stones. The diagnostic accuracy of these tests for the diagnosis of other conditions such as benign or malignant biliary stricture and periampullary tumours have not been assessed in this review.
Authors' conclusions
Implications for practice.
Both EUS and MRCP have high diagnostic accuracy for detection of common bile duct stones. People with positive EUS or MRCP should undergo endoscopic or surgical extraction of common bile duct stones, and those with negative EUS or MRCP do not need further invasive tests. However, further investigations will be indicated if symptoms persist. The two tests are similar in terms of diagnostic accuracy; the choice of which test to use will be informed by availability and contra‐indications to each test. However, it should be noted that the results are based on studies that are of poor methodological quality and so the results should be interpreted with caution.
Implications for research.
Further studies of high methodological quality are necessary. Future research should be conducted in a prospective manner as close as possible to the clinical setting in which EUS and MRCP would be used. Such research should use appropriate reference standards and should not use ERCP or IOC as the reference standards because neither of these tests are 100% accurate (Gurusamy 2015a). We acknowledge that differential verification cannot always be avoided if endoscopic sphincterotomy and extraction of stones are used as the reference standard because of the complications associated with this procedure (Gurusamy 2011). Surgical exploration of the common bile duct is a major surgical procedure and cannot be undertaken lightly. Based on these considerations, persons with a positive test are likely to undergo endoscopic sphincterotomy and extraction of stones or surgical exploration of the common bile duct while those with a negative test are likely to be followed up. Such persons should be followed up for at least six months to ensure that they do not develop the symptoms of common bile duct stones. Future studies should avoid any inappropriate exclusions to ensure that true diagnostic accuracy can be determined. Long‐term follow‐up of patients with negative tests will help in understanding the implications of false negative results and will aid clinical decision making.
Both EUS and MRCP involve additional costs. Whether these additional costs are offset by avoiding unnecessary invasive testing in a state‐funded healthcare system has to be investigated in formal cost‐effectiveness analysis.
Notes
This review is based on a common protocol which needed to be split in to three reviews (Giljaca 2013).
Acknowledgements
We thank the Cochrane Hepato‐Biliary Group (CHBG) and Cochrane Diagnostic Test Accuracy Working Group for their help in the development of this systematic review. We are grateful to Dimitrinka Nikolova and Christian Gluud of the CHBG for their advice during preparation of this review. We also thank Sarah Louise Klingenberg of the CHBG for her assistance with searches and obtaining articles, and Bosa Licul of the University of Rijeka Medical School Library Services for her help in obtaining some of the articles.
Contact Editors; Agostino Colli, Italy; Dario Conte, Italy.
This project was funded by the National Institute for Health Research.
Disclaimer of the Department of Health: 'The views and opinions expressed in the review are those of the authors and do not necessarily reflect those of the National Institute for Health Research (NIHR), National Health Services (NHS), or the Department of Health'.
Appendices
Appendix 1. Search strategies
| Database | Period of Search | Search Strategy |
| MEDLINE (PubMed) | 1946 until September 2012 | (((bile duct[tiab] or biliary[tiab] OR CBD[tiab]) AND (stone[tiab] OR stones[tiab] OR calculus[tiab] OR calculi[tiab])) OR choledocholithiasis[tiab] OR cholelithiasis[tiab] OR "Choledocholithiasis"[Mesh] OR "Common Bile Duct Calculi "[MESH] OR "Cholelithiasis "[MESH]) AND (CT[tiab] OR tomodensitometry[tiab] OR MRI[tiab] OR NMRI[tiab] OR zeugmatogra*[tiab] OR ((computed[tiab] OR computerised[tiab] OR computerized[tiab] OR magneti*[tiab] OR MR[tiab] OR NMR[tiab] OR proton[tiab]) AND (tomogra*[tiab] OR scan[tiab] OR scans[tiab] OR imaging[tiab] OR cholangiogra*[tiab])) OR "Tomography, X‐Ray Computed"[Mesh] OR "Magnetic Resonance Imaging"[Mesh] OR echogra*[tiab] OR ultrason*[tiab] OR ultrasound[tiab] OR EUS[tiab] OR "Ultrasonography"[Mesh] OR "Endosonography"[Mesh] OR cholangiogra*[tiab] OR cholangio?pancreatogra*[tiab] OR cholangiosco*[tiab] OR choledochosco*[tiab] OR ERCP[tiab] OR MRCP[tiab] OR "Cholangiography"[Mesh] OR "Cholangiopancreatography, Magnetic Resonance"[Mesh] OR liver function test[tiab] OR liver function tests[tiab] OR "Liver Function Tests"[Mesh]) |
| EMBASE (OvidSP) | 1947 until September 2012 | 1. (((bile duct or biliary or CBD) adj5 (stone or stones or calculus or calculi)) or choledocholithiasis or cholelithiasis).tw. 2. exp common bile duct stone/ or exp bile duct stone/ or exp cholelithiasis/ 3. 1 or 2 4. (CT or tomodensitometry or MRI or NMRI or zeugmatogra* or ((computed or computerised or computerized or magneti* or MR or NMR or proton) adj5 (tomogra* or scan or scans or imaging or cholangiogra*))).tw. 5. exp computer assisted tomography/ 6. exp nuclear magnetic resonance imaging/ 7. (echogra* or ultrason* or ultrasound or EUS).tw. 8. exp ultrasound/ 9. (cholangiogra* or cholangio?pancreatogra* or cholangiosco* or choledochosco* or ERCP or MRCP).tw. 10. exp cholangiography/ 11. (liver function test or liver function tests).tw. 12. exp liver function test/ 13. 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 14. 3 and 13 |
| Science Citation Index Expanded (ISI Web of Knowledge) | 1898 until September 2012 | #1 TS=(((bile duct or biliary OR CBD) AND (stone OR stones OR calculus OR calculi)) OR choledocholithiasis OR cholelithiasis) #2 TS=(CT OR tomodensitometry OR MRI OR NMRI OR zeugmatogra* OR ((computed OR computerised OR computerized OR magneti* OR MR OR NMR OR proton) AND (tomogra* OR scan OR scans OR imaging OR cholangiogra*))) #3 TS=(echogra* OR ultrason* OR ultrasound OR EUS) #4 TS=(cholangiogra* OR cholangio?pancreatogra* OR cholangiosco* OR choledochosco* OR ERCP OR MRCP) #5 TS=(liver function test OR liver function tests) #6 #5 OR #4 OR #3 OR #2 #7 #1 AND #6 |
| BIOSIS (ISI Web of Knowledge) | 1969 until September 2012 | #1 TS=(((bile duct or biliary OR CBD) AND (stone OR stones OR calculus OR calculi)) OR choledocholithiasis OR cholelithiasis) #2 TS=(CT OR tomodensitometry OR MRI OR NMRI OR zeugmatogra* OR ((computed OR computerised OR computerized OR magneti* OR MR OR NMR OR proton) AND (tomogra* OR scan OR scans OR imaging OR cholangiogra*))) #3 TS=(echogra* OR ultrason* OR ultrasound OR EUS) #4 TS=(cholangiogra* OR cholangio?pancreatogra* OR cholangiosco* OR choledochosco* OR ERCP OR MRCP) #5 TS=(liver function test OR liver function tests) #6 #5 OR #4 OR #3 OR #2 #7 #1 AND #6 |
| Clinicaltrials.gov | September 2012 | (bile duct) OR CBD OR choledocholithiasis OR cholelithiasis |
| Database of Abstracts of Reviews of Effects (DARE) and Health Technology Assessment (HTA) in The Cochrane Library (Wiley) |
September 2012 | #1 (((bile duct or biliary or CBD) NEAR/5 (stone OR stones OR calculus OR calculi)) OR choledocholithiasis OR cholelithiasis):ti,ab,kw #2 MeSH descriptor Choledocholithiasis explode all trees #3 (#1 OR #2) #4 (CT OR tomodensitometry OR MRI OR NMRI OR zeugmatogra* OR ((computed OR computerised OR computerized OR magneti* OR MR OR NMR OR proton) NEAR/5 (tomogra* OR scan OR scans OR imaging OR cholangiogra*))):ti,ab,kw #5 MeSH descriptor Tomography, X‐Ray Computed explode all trees #6 MeSH descriptor Magnetic Resonance Imaging explode all trees #7 (echogra* OR ultrason* OR ultrasound OR EUS):ti,ab,kw #8 MeSH descriptor Ultrasonography explode all trees #9 MeSH descriptor Endosonography explode all trees #10 (cholangiogra* OR cholangio?pancreatogra* OR cholangiosco* OR choledochosco* OR ERCP OR MRCP):ti,ab,kw #11 MeSH descriptor Cholangiography explode all trees #12 MeSH descriptor Cholangiopancreatography, Magnetic Resonance explode all trees #13 (liver function test OR liver function tests):ti,ab,kw #14 MeSH descriptor Liver Function Tests explode all trees #15 (#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14) #16 (#3 AND #15) |
| Medion (www.mediondatabase.nl/) | September 2012 | We will conduct four separate searches of the abstract using the terms: bile duct CBD choledocholithiasis cholelithiasis |
| ARIF (www.birmingham.ac.uk/research/activity/mds/projects/HaPS/PHEB/ARIF/databases/index.aspx) | September 2012 | (bile duct) OR CBD OR choledocholithiasis OR cholelithiasis |
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
| Test | No. of studies | No. of participants |
|---|---|---|
| 1 Endoscopic ultrasound | 13 | 1537 |
| 2 Magnetic resonance cholangiopancreatography | 7 | 996 |
1. Test.
Endoscopic ultrasound.
2. Test.
Magnetic resonance cholangiopancreatography.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ang 2012.
| Study characteristics | |||
| Patient sampling | Type of study: retrospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 112 Females: not stated Age: 61 years Presentation: Inclusion criteria Patients with a high clinical probability of CBD stone defined as following 1. Recent episode of acute cholangitis 2. Acute gallstone pancreatitis with cholestatic liver function test 3. Cholestatic jaundice 4. Alkaline phosphatase elevation > 2‐fold 5. Dilated CBD Setting: secondary care (Department of Gastroenterology, Singapore) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: not stated Performed by: not stated Criteria for positive diagnosis: not stated | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic extraction of stones in patients with positive EUS and clinical follow‐up minimum 6 months in patients with negative EUS Technical specifications: not applicable Performed by: endoscopists and clinicians Criteria for positive diagnosis: endoscopic extraction of stones in patients with positive EUS and clinical follow‐up minimum 6 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | Unclear | ||
| High | |||
Boraschi 2002.
| Study characteristics | |||
| Patient sampling | Type of study: unclear whether prospective or retrospective study Consecutive or random sample: unclear | ||
| Patient characteristics and setting | Sample size: 97 Females: 56 (58.9%) Age: 63 years Presentation: Inclusion criteria 1. Elevation of biochemical parameters of cholestasis (alkaline phosphatase, gamma glutamyl transpeptide, aspartate aminotransferase, alanine aminotransferase, and bilirubin) 2. Clinical or enzymatic pancreatitis 3. Common bile duct size at least 6.5 mm at ultrasound Setting: secondary care (Italy) | ||
| Index tests | Index test: magnetic resonance cholangiopancreatography Technical specifications: 0.5 T magnet; GE Performed by: two experienced radiologists jointly Criteria for positive diagnosis: foci of intraluminal signal void on T2‐weighted sequences | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: attempted endoscopic, laparoscopic or surgical extraction of CBD stones Technical specifications: not applicable Performed by: endoscopists and surgeons Criteria for positive diagnosis: presence or absence of stones during endoscopic or surgical clearance | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: 2 (2.1%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| High | High | ||
| DOMAIN 2: Index Test MRCP | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Buscarini 2003.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 459 Females: 283 (61.7%) Age: 66 years Presentation: Inclusion criteria Patients with suspected choledocholithiasis based on one of the following criteria: 1. History of biliary‐type colicky pain or recent cholangitis, and a history of jaundice 2. Recent acute pancreatitis 3. Serum bilirubin and/or alkaline phosphatase or 7‐glutamyl transpeptidase or aminotransferases more than twice the upper normal limit, or both 4. Dilatation of the intrahepatic or extrahepatic bile ducts (> 7 mm) or a suspicion of choledocholithiasis on transabdominal US or CT, or both Exclusion criteria: 1. Any factor that rendered the patient unsuitable for treatment of choledocholithiasis 2. Previous gastrectomy 3. Patients with a definite transabdominal ultrasound diagnosis of choledocholithiasis Setting: secondary care (Gastroenterology Department in Italy) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: GF‐UM20; Olympus; 7.5 to 12 MHz probe Performed by: endoscopist with at least 3 years' experience Criteria for positive diagnosis: echo‐rich structures, possibly moving within the bile duct, with or without acoustic shadowing | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 7 months in patients with negative EUS Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 7 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard were available: 4 (0.8%) Number of patients who were excluded from the analysis: 22 (4.3%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Canto 1998.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 64 Females: 42 (65.6%) Age: 53 years Presentation: Inclusion criteria Patients with suspected choledocholithiasis based on two or more of the following: 1. Right upper quadrant or epigastric pain 2. Abnormal serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), serum alkaline phosphatase, or total bilirubin 3. History of acute pancreatitis 4. Recent or current acute cholangitis 5. Biliary dilatation on transabdominal US or CT 6. Choledocholithiasis diagnosed by US, CT, or endoscopic retrograde cholangiopancreatography previously performed at another institution Exclusion criteria 1. Haemodynamically unstable patients Setting: secondary care (Gastroenterology Department, USA) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: EU‐M20; Olympus; 7.5 MHz probe Performed by: experienced endosonographer Criteria for positive diagnosis: a reproducible hyperechoic focus within the extrahepatic bile duct with associated acoustic shadowing | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 12 months in patients with negative EUS Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 12 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | Unclear | ||
| High | |||
Choo 2012.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 9. Females: 8 (88.8%) Age: 37 years Presentation: Inclusion criteria Patients who had positive intraoperative cholangiogram Setting: secondary care (Department of Gastroenterology, USA) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: not stated Performed by: physician Criteria for positive diagnosis: not stated | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: attempted endoscopic extraction of stones in all patients Technical specifications: not applicable Performed by: endoscopist Criteria for positive diagnosis: presence or absence of stones during endoscopic clearance | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | High | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Low | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| High | |||
De Ledinghen 1999.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: unclear | ||
| Patient characteristics and setting | Sample size: 43 Females: 25 (58.1%) Age: 61 years Presentation: Inclusion criteria Patients with clinical or biochemical signs of choledocholithiasis according to the following criteria: 1. Combination of epigastric or right upper quadrant pain with fever or jaundice 2. One or two of the previous signs together with an elevation of serum alkaline phosphatase level or an elevation of serum gamma glutamyl transpeptidase or transaminase level more than the upper limit of normal 3. Acute pancreatitis 4. Unexplained cholestasis defined by an elevation of serum alkaline phosphatase level and an elevation of serum gamma glutamyl transpeptidase level to more than two times the upper limit of normal Exclusion criteria 1. Long‐term daily alcohol intake exceeded 80 g 2. Taking a hepatotoxic drug 3. Serum hepatitis B or C antibodies were present Setting: secondary care (Hepatogastroenterology Department, France) | ||
| Index tests | Index test: magnetic resonance cholangiopancreatography
Technical specifications: 1 T magnet; Siemens
Performed by: two experienced radiologists jointly
Criteria for positive diagnosis: a round, oval, or multifaceted area of signal void (hypointensity) was present within the lumen of the hyperintense bile duct Index test: endoscopic ultrasound Technical specifications: GF EUM20; Olympus Performed by: not stated Criteria for positive diagnosis: a hyperechoic structure within the common bile duct sometimes associated with an acoustic shadow |
||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: attempted endoscopic or surgical extraction of stones in all patients Technical specifications: not applicable Performed by: endoscopists and surgeons Criteria for positive diagnosis: presence or absence of stones during endoscopic or surgical clearance | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: 11 (25.6%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| High | High | ||
| DOMAIN 2: Index Test MRCP | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Fazel 2002.
| Study characteristics | |||
| Patient sampling | Type of study: unclear whether prospective or retrospective study Consecutive or random sample: unclear | ||
| Patient characteristics and setting | Sample size: 40 Females: not stated Age: not stated Presentation: Inclusion criteria Patients with suspicion of biliary stone disease on the basis of symptoms and signs suggestive of choledocholithiasis (biliary colic, abnormal liver function tests, or abnormal transabdominal ultrasound) Setting: care setting not stated, USA | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: not stated Performed by: not stated Criteria for positive diagnosis: not stated | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: attempted endoscopic extraction of stones in all patients Technical specifications: not applicable Performed by: endoscopists and surgeons Criteria for positive diagnosis: presence or absence of stones during endoscopic or surgical clearance | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| High | High | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| High | |||
Fernandez‐Esparrach 2007.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 159 Females: 74 (46.5%) Age: 68 years Presentation: Inclusion criteria 1. Unexplained common bile duct dilation in standard US, independently of clinical symptoms 2. Non‐dilated common bile duct and a high probability of having choledocholithiasis (cholangitis, jaundice, non‐severe pancreatitis, alkaline phosphatase < twice the upper normal limit or increased gamma glutamyl transferase, alanine aminotransferase or aspartate aminotransferase Exclusion criteria 1. Acute severe biliary pancreatitis Setting: secondary care (Gastroenterology and Surgery Departments, Spain) | ||
| Index tests | Index test: magnetic resonance cholangiopancreatography
Technical specifications: 1.5 T magnet; Siemens
Performed by: not stated
Criteria for positive diagnosis: a round, oval, or multifaceted area of signal void (hypointensity) was present inside the lumen of the hyperintense bile duct Index test: endoscopic ultrasound Technical specifications: GF UM20 or GF UM160; Olympus Performed by: not stated Criteria for positive diagnosis: visualisation of one or more hyperechoic images inside the common bile duct with or without acoustic shadow |
||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up of minimum 6 months in patients with negative EUS Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up of minimum 6 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: 24 (15.1%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test MRCP | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Gautier 2004.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 108 Females: 58 (53.7%) Age: 59 years Presentation: Inclusion criteria Patients with suspected common bile duct stones Exclusion criteria 1. Patients with a contraindication for magnetic resonance imaging (pacemaker, intraocular metallic implant) 2. Initial differential or positive diagnosis of CBDS had been established on the basis of ultrasound or computed tomography Setting: secondary care (Radiology Department, France) | ||
| Index tests | Index test: magnetic resonance cholangiopancreatography Technical specifications: 1.5 T magnet; Siemens Performed by: two radiologists interpreted the scan independently and in the case of discrepancy, a third radiologist made the final decision Criteria for positive diagnosis: low intensity intraductal signal surrounded by a high intensity liquid signal | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic or surgical extraction of stones or clinical follow‐up of minimum 6 months Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic, surgical extraction of stones, clinical follow‐up of minimum 6 months | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: 9 (8.3%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test MRCP | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Guarise 2005.
| Study characteristics | |||
| Patient sampling | Type of study: unclear whether prospective or retrospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 170 Females: not stated Age: not stated Presentation: Inclusion criteria Patients who underwent magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography for clinically suspected biliary disease Setting: secondary care (Radiology Department, Italy) | ||
| Index tests | Index test: magnetic resonance cholangiopancreatography Technical specifications: 1.5 T magnet; Siemens Performed by: two radiologists with experience in gastrointestinal disease Criteria for positive diagnosis: a rounded and oval signal defect within the bile duct in at least two projections and located in the dependent portion of the duct | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic extraction of stones in all patients Technical specifications: not applicable Performed by: endoscopists (the images were interpreted as consensus with radiologist) Criteria for positive diagnosis: endoscopic extraction of stones in all patients | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: 23 (13.5%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test MRCP | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Low | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Jendresen 2002.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 180 Females: 129 (71.7%) Age: not stated Presentation: Inclusion criteria Patients with symptomatic cholelithiasis Setting: secondary care (Surgery, Surgical Gastroenterology, and Radiology Departments, Denmark) | ||
| Index tests | Index test: magnetic resonance cholangiopancreatography Technical specifications: Gyroscan T5‐NT Powertrack 1000; Phillips Performed by: one radiologist Criteria for positive diagnosis: areas of low signal in the surrounding signal‐intense bile | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic extraction of stones or clinical follow‐up of minimum 6 months Technical specifications: not applicable Performed by: endoscopists and clinicians Criteria for positive diagnosis: endoscopic extraction of stones or clinical follow‐up of minimum 6 months | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test MRCP | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | Yes | ||
| High | |||
Kohut 2002.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: unclear | ||
| Patient characteristics and setting | Sample size: 134 Females: 109 (81.3%) Age: 57 years Presentation: Inclusion criteria Patients suspected of having common bile duct stones based on the following features 1. Biliary colic with elevated levels of biochemical values (bilirubin, transaminases, alkaline phosphatase, g‐glutamyl transpeptidase), and enlarged bile ducts (> 7 mm in patients with gallbladder in situ or > 9 mm in post‐cholecystectomy patients) or suspicion of bile duct stones on conventional ultrasound, done currently or in the previous 6 months Exclusion criteria 1. Patients with suspicion of biliary or pancreatic malignancy on CT scan 2. Current acute biliary pancreatitis or cholangitis, or both Setting: secondary care (Gastroenterology Departments, Poland) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: FG 32 UA; Pentax Performed by: not stated Criteria for positive diagnosis: single or multiple hyperechoic structures within the biliary tree with acoustic shadowing were found | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: attempted endoscopic or surgical extraction of stones in all patients Technical specifications: not applicable Performed by: endoscopists and surgeons Criteria for positive diagnosis: presence or absence of stones during endoscopic or surgical clearance | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| High | High | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| High | |||
Liu 2001.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 100 Females: 49 (49.0%) Age: 61 years Presentation: Inclusion criteria 1. Patients presenting with acute pancreatitis Exclusion criteria 1. Known diagnosis of recurrent pancreatitis related to chronic alcoholism or hyperlipidaemia 2. Post‐endoscopic retrograde cholangiopancreatography pancreatitis when performed for reasons other than suspected biliary stones Setting: secondary care (Surgery Department, Hong Kong, China) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: GF‐UM20 or JF‐UM20; Olympus; 7.5 MHz probe Performed by: endoscopist Criteria for positive diagnosis: a persistent echogenic focus with or without posterior acoustic shadowing was considered a biliary stone, microlithiasis, or sludge | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic extraction of stones in patients with positive EUS and clinical follow‐up of minimum 12 months in patients with negative EUS Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic extraction of stones in patients with positive EUS and clinical follow‐up of minimum 12 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | Yes | ||
| High | |||
Miletic 2006.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 337 Females: 174 (51.6%) Age: 65 years Presentation: Inclusion criteria Patients with suspected CBD stones undergoing magnetic resonance cholangiopancreatography Setting: secondary care (Croatia) | ||
| Index tests | Index test: magnetic resonance cholangiopancreatography Technical specifications: 0.5 T magnet; Shimadzu Performed by: two radiologists interpreted the scan independently and arrived at a consensus Criteria for positive diagnosis: not stated | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic or surgical extraction of stones in patients and clinical follow‐up of minimum 12 months in patients with negative endoscopic retrograde cholangiopancreatography Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic or surgical extraction of stones in patients and clinical follow‐up of minimum 12 months in patients with negative endoscopic retrograde cholangiopancreatography | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: 29 (8.6%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test MRCP | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Montariol 1998.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 240 Females: 171 (71.3%) Age: 57 years Presentation: Inclusion criteria 1. Patients with symptomatic cholelithiasis, scheduled for elective cholecystectomy or emergency operations within 48 hours for acute cholecystitis Exclusion criteria 1. Cholelithiasis was asymptomatic 2. Preoperative risk of CBD stones was less than 5% 3. Patients had symptomatic choledocholithiasis defined as combination of clinical symptoms (pancreatic pain and jaundice), biochemical abnormalities (serum aminotransferase, alkaline phosphatase or γ‐glutamyl transpeptidase levels more than twice normal values, serum bilirubin levels >50 µmol/L, and serum amylase and lipase levels more than fourfold and threefold, respectively), and morphologic features (presence of hyperechoic image in the CBD on ultrasonography Setting: secondary care (Surgery Departments, France) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: EUM3 and EUM20; Olympus; 7.5 MHz probe Performed by: experienced and selected operators Criteria for positive diagnosis: stones were described as hyperechoic images in the different parts of the CBD, identified because of their acoustic shadow and usually mobile spontaneously or with changing positions | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: surgical extraction of stones in patients with positive EUS and clinical follow‐up of minimum 12 months in patients with negative EUS Technical specifications: not applicable Performed by: surgeons and clinicians Criteria for positive diagnosis: surgical extraction of stones in patients with positive EUS and clinical follow‐up of minimum 12 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: 25 (10.4%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| High | |||
Ney 2005.
| Study characteristics | |||
| Patient sampling | Type of study: prospective study Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 68 Females: 49 (72.1%) Age: 57 years Presentation: Inclusion criteria 1. Dilated CBD (> 7 mm on conventional ultrasound) and/or hepatic biochemical parameter abnormalities (AST > 2 times normal; elevated alkaline phosphatase) Exclusion criteria 1. Jaundiced or had clinical signs of cholangitis 2. Acute pancreatitis 3. Unequivocal evidence of CBD stones on US or CT scans or magnetic resonance cholangiopancreatography Setting: secondary care (Surgery Department, Brazil) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: GIF‐UM20; Olympus; 7.5 or 12 MHz probe Performed by: not stated Criteria for positive diagnosis: stones were defined as mobile hyperechoic spots with an acoustic shadow | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 11 months in patients with negative EUS Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 11 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | Yes | ||
| High | |||
Norton 1997.
| Study characteristics | |||
| Patient sampling | Type of study: unclear whether prospective or retrospective study Consecutive or random sample: unclear | ||
| Patient characteristics and setting | Sample size: 50 Females: 34 (68.0%) Age: 63 years Presentation: Inclusion criteria Patients with proven symptomatic gallstone disease and suspected bile duct stones because of the presence of at least one of the following features 1. Dilated (greater than 7 mm) bile duct on abdominal ultrasonography 2. Clinical jaundice 3. Gallstone pancreatitis 4. Deranged liver function Setting: secondary care (Surgery Department, United Kingdom) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: GF‐UM 20; Olympus Performed by: not stated Criteria for positive diagnosis: stones were recognized by their hyperechoic image and the acoustic shadow commonly produced | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 6 months in patients with negative EUS Technical specifications: not applicable Performed by: endoscopists, surgeons, and clinicians Criteria for positive diagnosis: endoscopic or surgical extraction of stones in patients with positive EUS and clinical follow‐up minimum 6 months in patients with negative EUS | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: not stated Number of patients who were excluded from the analysis: not stated | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| High | High | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | Unclear | ||
| High | |||
Prat 1996.
| Study characteristics | |||
| Patient sampling | Type of study: prospective Consecutive or random sample: consecutive patients | ||
| Patient characteristics and setting | Sample size: 121 Females: 69 (57.0%) Age: 70 years Presentation: Inclusion criteria 1. Strong suspicion of choledocholithiasis as determined by a combination of clinical symptoms (history of biliary colic, pancreatic pain, fever, jaundice), biochemical abnormalities (raised serum aminotransferases, alkaline phosphatase, or gamma‐glutamyl transpeptidase more than twice the normal value, serum bilirubin above 50 (micromol/L), and morphological features (common bile duct dilated to more than 8 mm in patients with the gallbladder in situ and 10 mm in patients with previous cholecystectomy, or the presence of a hyperechoic image in the common bile duct). 2. Endoscopic treatment would be chosen for the treatment of the stones Exclusion criteria 1. Patients younger than 50 who had not had cholecystectomy 2. Patients who declined to take part Setting: secondary care (Gastroenterology Department, France) | ||
| Index tests | Index test: endoscopic ultrasound Technical specifications: GIF‐EUM20; Olympus; 7.5 and 12 MHz probe Performed by: one of two experts in EUS Criteria for positive diagnosis: not stated | ||
| Target condition and reference standard(s) | Target condition: common bile duct stones Reference standard: attempted endoscopic extraction of stones in all patients Technical specifications: not applicable Performed by: endoscopists and surgeons Criteria for positive diagnosis: presence or absence of stones during endoscopic clearance | ||
| Flow and timing | Number of indeterminates for whom the results of reference standard was available: 1 (0.8%) Number of patients who were excluded from the analysis: 1 (0.8%) | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| High | High | ||
| DOMAIN 2: Index Test EUS | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| High | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Low | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| High | |||
EUS: endoscopic ultrasound. MRCP: magnetic resonance cholangiopancreatography.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adamek 1998 | Not enough data for 2 x 2 table |
| Agapov 2006 | Review of literature |
| Ahn 1998 | Inappropriate reference standard |
| Ainsworth 2003 | Not enough data for 2 x 2 table |
| Al‐Jiffry 2010 | Inappropriate reference standard |
| Alcaraz 2000 | Inappropriate reference standard |
| Alhayaf 2008 | Inappropriate reference standard |
| Aljebreen 2008 | Inappropriate reference standard |
| Amouyal 1994 | Inappropriate reference standard |
| Anderloni 2012 | Not enough data for 2 x 2 table |
| Anderloni 2012a | Not enough data for 2 x 2 table |
| Ang 2007 | Inappropriate reference standard |
| Ang 2007a | Inappropriate reference standard |
| Aube 2005 | Inappropriate reference standard |
| Aubertin 1996 | Inappropriate reference standard |
| Aubertin 1996a | Inappropriate reference standard |
| Basile 2000 | Inappropriate reference standard |
| Becker 1997 | Inappropriate reference standard |
| Berdah 2001 | Inappropriate reference standard |
| Bhatt 2005 | Not enough data for 2 x 2 table |
| Bilgin 2012 | Inappropriate reference standard |
| Boboev 2012 | Inappropriate reference standard |
| Bodula 2011 | Inappropriate reference standard |
| Bokobza 1988 | Review article |
| Boraschi 1999 | Inappropriate reference standard |
| Brisbois 2001 | Inappropriate reference standard |
| Calle 2006 | Inappropriate reference standard |
| Calvo 2002 | Inappropriate reference standard |
| Canto 1995 | Not enough data for 2 x 2 table |
| Catalano 2000 | Inappropriate reference standard |
| Cervi 2000 | Inappropriate reference standard |
| Chak 1999 | Inappropriate index test |
| Chan 1996 | Not enough data for 2 x 2 table |
| Chan 2010 | Inappropriate reference standard |
| Chandra 2010 | Not enough data for 2 x 2 table |
| Chavez‐Valencia 2009 | Inappropriate reference standard |
| Chen 2003 | Inappropriate reference standard |
| Chen 2012 | Editorial |
| Chowdhury 1999 | Inappropriate reference standard |
| Coakley 2002 | Review article |
| Contractor 2004 | Inappropriate reference standard |
| Dalton 2005 | Inappropriate reference standard |
| Danaci 2002 | Inappropriate reference standard |
| Dancygier 1995 | Not enough data for 2 x 2 table |
| De Waele 2007 | Inappropriate reference standard |
| del Pozo 2011 | Not enough data for 2 x 2 table |
| Demartines 2000 | Inappropriate reference standard |
| Denis 1993 | Inappropriate reference standard |
| Derodra 1986 | Letter to editor |
| Di Angelo 2010 | Not enough data for 2 x 2 table |
| Di Angelo 2011 | Not enough data for 2 x 2 table |
| Dittrick 2005 | Inappropriate reference standard |
| Duchmann 1999 | Not enough data for 2 x 2 table |
| Dwerryhouse 1998 | Inappropriate reference standard |
| Eshghi 2008 | Inappropriate reference standard |
| Familiari 2004 | Inappropriate reference standard |
| Fernandez 2001 | Inappropriate reference standard |
| Filippone 2003 | Inappropriate reference standard |
| Galvao 2007 | Inappropriate reference standard |
| Griffin 2003 | Inappropriate reference standard |
| Gul 2010 | Inappropriate reference standard |
| Gupta 2008 | Inappropriate reference standard |
| Hasan 2010 | Inappropriate reference standard |
| Hayashi 2002 | Not enough data for 2 x 2 table |
| Ho 1999 | Inappropriate reference standard |
| Hochwald 1998 | Inappropriate reference standard |
| Holzknecht 1998 | Inappropriate reference standard |
| Hrabar 2009 | Inappropriate reference standard |
| Hussein 2002 | Inappropriate reference standard |
| Isomoto 1998 | Inappropriate reference standard |
| Ito 2001 | Inappropriate reference standard |
| Janssen 2008 | Not enough data for 2 x 2 table |
| Karakan 2009 | Inappropriate reference standard |
| Kats 2003 | Inappropriate reference standard |
| Kausar 2005 | Not enough data for 2 x 2 table |
| Ke 2004 | Inappropriate reference standard |
| Kejriwal 2004 | Inappropriate reference standard |
| Kim 2002 | Inappropriate reference standard |
| Kim 2005 | Inappropriate reference standard |
| Kohut 2003 | Not enough data for 2 x 2 table |
| Kondo 2005 | Inappropriate reference standard |
| Lachter 2000 | Inappropriate reference standard |
| Laghi 1998 | Inappropriate reference standard |
| Laokpessi 2001 | Inappropriate reference standard |
| Le Rhun 1999 | Inappropriate reference standard |
| Lee 1996 | Inappropriate reference standard |
| Lee 2010 | Inappropriate reference standard |
| Leytens 2001 | Inappropriate reference standard |
| Liessi 1996 | Inappropriate reference standard |
| Lim 2003 | Inappropriate reference standard |
| Liu 1999 | Inappropriate reference standard |
| Liu 2005 | Inappropriate reference standard |
| Lomanto 1997 | Inappropriate reference standard |
| Lomas 1999 | Inappropriate reference standard |
| Lundorf 2000 | Inappropriate reference standard |
| Magnuson 1997 | Inappropriate reference standard |
| Magnuson 1999 | Inappropriate reference standard |
| Makary 2005 | Inappropriate reference standard |
| Maurea 2009 | Not enough data for 2 x 2 table |
| Meduri 1998 | Inappropriate reference standard |
| Mendler 1998 | Inappropriate reference standard |
| Meroni 2004 | Inappropriate reference standard |
| Miao 2008 | Not enough data for 2 x 2 table |
| Mirbagheri 2005 | Inappropriate reference standard |
| Mofidi 2008 | Inappropriate reference standard |
| Moon 2005 | Inappropriate reference standard |
| Morera 2006 | Inappropriate reference standard |
| Morris‐Stiff 2009 | Inappropriate reference standard |
| Munir 2004 | Inappropriate reference standard |
| Musella 1998 | Inappropriate reference standard |
| Nandalur 2008 | Inappropriate reference standard |
| Nau 2011 | Inappropriate reference standard |
| Nebiker 2009 | Inappropriate reference standard |
| Neri 2000 | Inappropriate reference standard |
| Norero 2008 | Inappropriate reference standard |
| Okaniwa 2002 | Inappropriate reference standard |
| Palazzo 1995 | Inappropriate reference standard |
| Palazzo 1998 | Overview article |
| Palmucci 2010 | Inappropriate reference standard |
| Pamos 1998 | Inappropriate reference standard |
| Pamos 2003 | Inappropriate reference standard |
| Pavone 1996 | Inappropriate reference standard |
| Pavone 1996a | Inappropriate reference standard |
| Pavone 1996b | Inappropriate reference standard |
| Pavone 1997 | Inappropriate reference standard |
| Pavone 1997a | Not enough data for 2 x 2 table |
| Polkowski 2001 | Not enough data for 2 x 2 table |
| Pomakov 2007 | Inappropriate reference standard |
| Pozo 2010 | Not enough data for 2 x 2 table |
| Pulpeiro 2000 | Inappropriate reference standard |
| Puri 2012 | Not enough data for 2 x 2 table |
| Rahman 2010 | Inappropriate reference standard |
| Regan 1996 | Inappropriate reference standard |
| Regan 1996a | Not enough data for 2 x 2 table |
| Regan 1998 | Inappropriate reference standard |
| Reinhold 1998 | Inappropriate reference standard |
| Roig 1995 | Not enough data for 2 x 2 table |
| Roig 1995a | Not enough data for 2 x 2 table |
| Rudowicz‐Pietruszewska 2002 | Inappropriate reference standard |
| Sabbagh 2000 | Not enough data for 2 x 2 table |
| Sajewicz 2006 | Inappropriate reference standard |
| Sakai 2007 | Not enough data for 2 x 2 table |
| Salmeron 1994 | Inappropriate reference standard |
| Saruc 2001 | Inappropriate reference standard |
| Scaffidi 2009 | Inappropriate reference standard |
| Scheiman 2001 | Inappropriate reference standard |
| Schmidt 2012 | Inappropriate reference standard |
| Seifert 2004 | Inadequate index test |
| Shafiq 2003 | Not enough data for 2 x 2 table |
| Shamiyeh 2005 | Inappropriate reference standard |
| Shanmugam 2005 | Inappropriate reference standard |
| Shim 1995 | Inappropriate reference standard |
| Simeone 1997 | Inappropriate reference standard |
| Skorka 1982 | Inappropriate reference standard |
| Soto 1996 | Inappropriate reference standard |
| Soto 2000 | Inappropriate reference standard |
| Soto 2000a | Inappropriate reference standard |
| Sotoudehmanesh 2007 | Not enough data for 2 x 2 table |
| Sperlongano 2005 | Not enough data for 2 x 2 table |
| Srinivasa 2010 | Inappropriate reference standard |
| Stevens 1996 | Inappropriate reference standard |
| Stiris 2000 | Inappropriate reference standard |
| Sugiyama 1997 | Inappropriate reference standard |
| Sugiyama 1998 | Inappropriate reference standard |
| Sverrisson 2012 | Not enough data for 2 x 2 table |
| Taylor 2002 | Inappropriate reference standard |
| Tennoe 1999 | Inappropriate reference standard |
| Topal 2003 | Inappropriate reference standard |
| Tripathi 2002 | Inappropriate reference standard |
| Uehara 1998 | Inappropriate reference standard |
| Urban 2002 | Inappropriate reference standard |
| Vaishali 2004 | Inappropriate reference standard |
| Valji 1996 | Inappropriate reference standard |
| Varghese 1999 | Inappropriate reference standard |
| Varghese 2000 | Inappropriate reference standard |
| Vazquez‐Sequeiros 2005 | Inappropriate reference standard |
| Vazquez‐Sequeiros 2011 | Inappropriate reference standard |
| Verma 2006 | Systematic review |
| Watanabe 2003 | Inappropriate reference standard |
| Wehrmann 2009 | Inappropriate reference standard |
| Wierzbicka‐Paczos 1999 | Not enough data for 2 x 2 table |
| Wong 2012 | Inappropriate reference standard |
| Zaheer 2011 | Not enough data for 2 x 2 table |
| Zaydan 2009 | Inappropriate reference standard |
| Zhang 2012 | Inappropriate reference standard |
| Zhi 2002 | Not enough data for 2 x 2 table |
| Zidi 1997 | Not enough data for 2 x 2 table |
| Zidi 1999 | Inappropriate reference standard |
Differences between protocol and review
We used the statistical package Stata instead of SAS to fit the bivariate models.
We performed one main analysis. In this analysis indeterminate test results were excluded. The planned sensitivity analyses were considered inappropriate because of sparse data.
Author order changed: Vanja Giljaca, Kurinchi Selvan Gurusamy, Yemisi Takwoingi, David Higgie, Goran Poropat, Davor Stimac, Brian R Davidson.
Contributions of authors
KSG designed the search strategies. VG wrote the first draft review. VG, GP and DH independently evaluated references for inclusion in this review. VG and KSG independently extracted data from included studies and assessed the methodological quality of included studies. YT and KSG performed the analysis, critically commented on the interpretation of the results, and revised sections of the review. DS and BRD critically commented on the review.
Sources of support
Internal sources
University College London, UK.
External sources
-
University of Rijeka ‐ Medical Faculty, Croatia.
TransMedRi project, EU FP7 REGPOT‐2010‐5 programme (grant agreement No. 256686)
National Institute of Health Research, UK.
Declarations of interest
Vanja Giljaca: none. Kurinchi S Gurusamy: none. David Higgie: none. Goran Poropat: none. Davor Stimac is a co‐author in one of included studies (Miletic 2006). Davor Stimac is not affiliated with Shimadzu, Siemens, or Olympus. Brian R Davidson: none. Yemisi Takwoingi: none.
New
References
References to studies included in this review
Ang 2012 {published data only}
- Ang TL, Liew SFAP, Ang D, Kwek A, Fock KM, Teo EK. EUS‐Guided ERCP in patients with negative cross sectional imaging but high clinical probability of choledocholithiasis. Gastrointestinal Endoscopy 2012; Vol. 1:AB203.
Boraschi 2002 {published data only}
Buscarini 2003 {published data only}
Canto 1998 {published data only}
Choo 2012 {published data only}
- Choo L, Mishra G, Conway J, Evans JA. Prospective single blinded study of endoscopic ultrasound prior to endoscopic retrograde cholangio‐pancreatography for patients with a positive intra‐operative cholangiogram. Gastrointestinal Endoscopy 2012; Vol. 1:AB203.
De Ledinghen 1999 {published data only}
Fazel 2002 {published data only}
- Fazel A, Catalano MF, Quadri A, Geenen JE. A comparison of the diagnostic accuracy of EUS and ERCP in identifying common bile duct stones. Gastrointestinal Endoscopy 2002; Vol. 55, issue 5:AB246.
Fernandez‐Esparrach 2007 {published data only}
- Fernandez‐Esparrach G, Gines A, Sanchez M, Pages M, Pellise M, Fernandez‐Cruz L, et al. Comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the diagnosis of pancreatobiliary diseases: A prospective study. American Journal of Gastroenterology 2007;102(8):1632‐9. [DOI] [PubMed] [Google Scholar]
Gautier 2004 {published data only}
Guarise 2005 {published data only}
- Guarise A, Baltieri S, Mainardi P, Faccioli N. Diagnostic accuracy of MRCP in choledocholithiasis. La Radiologia Medica 2005; Vol. 109, issue 3:239‐51. [PubMed]
Jendresen 2002 {published data only}
Kohut 2002 {published data only}
Liu 2001 {published data only}
Miletic 2006 {published data only}
Montariol 1998 {published data only}
- Montariol T, Msika S, Charlier A, Rey C, Bataille N, Hay JM, et al. Diagnosis of asymptomatic common bile duct stones: Preoperative endoscopic ultrasonography versus intraoperative cholangiography ‐ a multicenter, prospective controlled study. Surgery 1998; Vol. 124, issue 1:6‐13. [PubMed]
Ney 2005 {published data only}
- Ney MV, Maluf‐Filho F, Sakai P, Zilberstein B, Gama‐Rodrigues J, Rosa H. Echo‐endoscopy versus endoscopic retrograde cholangiography for the diagnosis of choledocholithiasis: the influence of the size of the stone and diameter of the common bile duct. Arquivos de Gastroenterologia 2005; Vol. 42, issue 4:239‐43. [DOI] [PubMed]
Norton 1997 {published data only}
- Norton SA, Alderson D. Prospective comparison of endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in the detection of bile duct stones. British Journal of Surgery 1997; Vol. 84, issue 10:1366‐9. [PubMed]
Prat 1996 {published data only}
References to studies excluded from this review
Adamek 1998 {published data only}
- Adamek HE, Albert J, Weitz M, Breer H, Schilling D, Riemann JF. A prospective evaluation of magnetic resonance cholangiopancreatography in patients with suspected bile duct obstruction. Gut 1998;43(5):680‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Agapov 2006 {published data only}
- Agapov VK, Romanov VA, Aleksandrov BA, Aslibekov MA. The application of endoscopic ultrasonography in diagnostics of choledocholithiasis. [Russian]. Voenno‐Meditsinskii Zhurnal 2006; Vol. 327, issue 3:41‐3. [PubMed]
Ahn 1998 {published data only}
- Ahn T, Matsumoto M, Ueda S, Fukui H. Diagnostic usefulness of magnetic resonance cholangiopancreatography (MRCP) in comparison with retrograde cholangiopancreatography (ERCP) for cholelithiasis. [Japanese]. Nippon Rinsho (Japanese Journal of Clinical Medicine) 1998; Vol. 56, issue 11:2923‐7. [PubMed]
Ainsworth 2003 {published data only}
Alcaraz 2000 {published data only}
- Alcaraz MJ, Morena EJ, Polo A, Ramos A, Cal MA, Mandly AG. A comparative study of magnetic resonance cholangiography and direct cholangiography. Revista Espanola de Enfermedades Digestivas 2000; Vol. 92, issue 7:433‐8. [PubMed]
Alhayaf 2008 {published data only}
- Alhayaf N, Lalor E, Bain V, McKaigney J, Sandha GS. The clinical impact and cost implication of endoscopic ultrasound on use of endoscopic retrograde cholangiopancreatography in a Canadian university hospital. Canadian Journal of Gastroenterology 2008; Vol. 22, issue 2:138‐42. [DOI] [PMC free article] [PubMed]
Aljebreen 2008 {published data only}
Al‐Jiffry 2010 {published data only}
- Al‐Jiffry B, El‐Fateh A. The use of MRCP in choledocholithiasis to reduce the incidence of negative ERCP. HPB 2010; Vol. 12:415‐6.
Amouyal 1994 {published data only}
Anderloni 2012 {published data only}
- Anderloni A, Ballare M, Galeazzi M, Pagliarulo M, Andorno S, Piano M. The clinical impact of early endoscopic ultrasound (EUS) in suspected choledocholithiasis: A prospective pilot study. Digestive and Liver Disease 2012; Vol. 44:S182.
Anderloni 2012a {published data only}
- Anderloni A, Galeazzi M, Ballare M, Pagliarulo M, Andorno S, Piano M. Assessment of the utility of early endoscopic ultrasound (EUS) in the evaluation of acute biliary pancreatitis (ABP): A prospective pilot study. Digestive and Liver Disease 2012; Vol. 44:S76.
Ang 2007 {published data only}
- Ang TL, Ming FK, Kiong TE. A prospective study of the impact of clinical parameters and EUS in the management of suspected choledocholithiasis. Journal of Gastroenterology and Hepatology 2007; Vol. 22:A220.
Ang 2007a {published data only}
Aube 2005 {published data only}
Aubertin 1996 {published data only}
- Aubertin JM, Levoir D, Becheur H, Bouillot JL, Bloch F, Petite JP. Prospective comparison of preoperative endosonography and intraoperative cholangiography during laparoscopic cholecystectomy in patients with common bile duct stone risk. Gastroenterology 1996; Vol. 110, issue 4:A446.
Aubertin 1996a {published data only}
Basile 2000 {published data only}
- Basile L, Pezzoto C, Roubicek D, Tempra A, Laborda Molteni J. Magnetic resonance cholangiopancreatography: comparative study with direct cholangiography. [Spanish]. Acta Gastroenterologica Latinoamericana 2000; Vol. 30, issue 5:487‐90. [PubMed]
Becker 1997 {published data only}
Berdah 2001 {published data only}
Bhatt 2005 {published data only}
- Bhatt C, Shah PS, Prajapati HJ, Modi J. Comparison of diagnostic accuracy between USG and MRCP in biliary and pancreatic pathology. Indian Journal of Radiology and Imaging 2005; Vol. 15, issue 2:177‐81.
Bilgin 2012 {published data only}
- Bilgin M, Toprak H, Burgazli M, Bilgin SS, Chasan R, Erdogan A, et al. Diagnostic value of dynamic contrast‐enhanced magnetic resonance imaging in the evaluation of the biliary obstruction. Scientific World Journal 2012; Vol. 2012:731089. [DOI] [PMC free article] [PubMed]
Boboev 2012 {published data only}
- Boboev B. [Usefulness of endoscopic ultrasonography in the diagnosis of choledocholithiasis and inflammatory biliary strictures]. Vestnik Khirurgii Imeni I. I. Grekova 2012; Vol. 171, issue 3:39‐41. [0042‐4625: (Print)] [PubMed]
Bodula 2011 {published data only}
- Bodula A, Pazurek M, Wozniak B, Biernacki R, Antosik‐Biernacka A, Winter K, et al. Comparison of magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography in the diagnosis of pancreatobiliary diseases. [Polish]. Przeglad Gastroenterologiczny 2011; Vol. 6, issue 3:187‐94.
Bokobza 1988 {published data only}
- Bokobza B, Leblanc I, Michot F, Bouvier P, Teniere P. Peroperative investigations during surgery for biliary lithiasis. Endoscopy and ultrasonography. [French]. Revue Francaise de Gastro‐Enterologie 1988; Vol. 24, issue 236:729‐31.
Boraschi 1999 {published data only}
Brisbois 2001 {published data only}
- Brisbois D, Plomteux O, Nchimi A, Hock D, Dupont P, Delforge M, et al. Value of MRCP for detection of choledocholithiasis in symptomatic patients: One‐year experience with a standardized high resolution breath‐hold technique. [French]. Journal Belge de Radiologie 2001; Vol. 84, issue 6:258‐61. [PubMed]
Calle 2006 {published data only}
- Calle G, Hastier P, Chevalier P, Bataille L, Dumas R, Demarquai JF, et al. Cholangiography by magnetic resonance for detection of cholelithiasis: comparison with endoscopic retrograde cholangiography, operative cholangiography and percutaneous cholangiography. [Spanish]. Revista de Gastroenterologia del Peru 2006; Vol. 26, issue 2:115‐24. [PubMed]
Calvo 2002 {published data only}
Canto 1995 {published data only}
- Canto M, Chak A, Sivak MV, Blades E, Stellato T. Endoscopic ultrasonography (EUS) versus cholangiography for diagnosing extrahepatic biliary stones ‐ a prospective, blinded study in precholecystectomy and postcholecystectomy patients. Gastrointestinal Endoscopy 1995; Vol. 41, issue 4:391.
Catalano 2000 {published data only}
- Catalano MF, Sial SH, Geenen JE, Hogan WJ. Endoscopic ultrasonography versus endoscopic retrograde cholangiopancreatography in the evaluation of patients with suspected choledocholithiasis. Gastrointestinal Endoscopy 2000; Vol. 51, issue 4:AB187.
Cervi 2000 {published data only}
Chak 1999 {published data only}
Chan 1996 {published data only}
Chan 2010 {published data only}
- Chan C, Cho SS, Bell CJ, Norton ID. EUS immediately prior to planned ERCP is a valuable strategy for the management of intermediate probability choledocholithiasis. Gastrointestinal Endoscopy 2010; Vol. 71, issue 5:AB281.
Chandra 2010 {published data only}
- Chandra N, Hodgekiss CH, Gupta PK, Mee AS. Do patients presenting with obstructive symptoms, abnormal LFTS and gallstones on USS require a MRCP before an ERCP?. Gastroenterology 2010; Vol. 1:S212.
Chavez‐Valencia 2009 {published data only}
- Chavez‐Valencia V, Espinosa‐Ortega H, Espinoza‐Peralta D, Arce‐Salinas C. [Diagnostic performance of biliary ultrasound vs. magnetic resonance cholangiogram in patients with recurrent biliary obstruction]. Revista de Gastroenterología de México 2009; Vol. 74, issue 4:329‐33. [0375‐0906: (Print)] [PubMed]
Chen 2003 {published data only}
- Chen RC, Lin KY, Lii JM, Yang MT, Chen WT, Tu HY, et al. MR cholangiopancreatography: Prospective comparison of 3‐dimensional turbo spin echo and single‐shot turbo spin echo with ERCP. Journal of the Formosan Medical Association 2003; Vol. 102, issue 3:172‐7. [PubMed]
Chen 2012 {published data only}
Chowdhury 1999 {published data only}
- Chowdhury A, Bourke MJ, Valiozis I, Williams SJ, Peduto A, Markson G, et al. Magnetic resonance cholangiography (MRC) versus endoscopic retrograde cholangio‐pancreaticography (ERCP) in the diagnosis of bile duct stones & strictures. Gastrointestinal Endoscopy 1999; Vol. 49, issue 4:AB154.
Coakley 2002 {published data only}
Contractor 2004 {published data only}
- Contractor QQ, Karkaria AK, Contractor TQ, Dubian MK. Impact of magnetic resonance cholangiography on endoscopic therapy before and after laparoscopic cholecystectomy. Indian Journal of Gastroenterology 2004; Vol. 23, issue 1:8‐11. [PubMed]
Dalton 2005 {published data only}
- Dalton SJ, Balupuri S, Guest J. Routine magnetic resonance cholangiopancreatography and intra‐operative cholangiogram in the evaluation of common bile duct stones. Annals of the Royal College of Surgeons of England 2005; Vol. 87, issue 6:469‐70. [DOI] [PMC free article] [PubMed]
Danaci 2002 {published data only}
- Danaci M, Polat V, Kamali A, Belet U, Incesu L, Ozen N, et al. Magnetic resonance cholangiography and ultrasonography in the diagnosis of choledocholithiasis. [Turkish]. Ondokuz Mayis Universitesi Tip Dergisi 2002; Vol. 19, issue 3:195‐201.
Dancygier 1995 {published data only}
- Dancygier H. Endoscopic ultrasonography in extrahepatic obstructive jaundice. Acta Endoscopica 1995; Vol. 25, issue 5:511‐8.
del Pozo 2011 {published data only}
Demartines 2000 {published data only}
Denis 1993 {published data only}
- Denis BJ, Bas V, Goudot C, Frederic M, Bigard MA, Gaucher P. Accuracy of endoscopic ultrasonography (EUS) for diagnosis of common bile‐duct stones (CBDS). Gastroenterology 1993; Vol. 104, issue 4:A358.
Derodra 1986 {published data only}
- Derodra J. Predictive ability of choledocholithiasis indicators. Annals of Surgery 1986; Vol. 203, issue 3:335. [PMC free article] [PubMed]
De Waele 2007 {published data only}
Di Angelo 2010 {published data only}
- Angelo IT, Prochazka V, Holinka M, Konecny M, Zapletalova J. Sensitivity, specificity and predictive value of choledocholithiasis by EUS and ERCP. Gastrointestinal Endoscopy 2010; Vol. 71, issue 5:AB293.
Di Angelo 2011 {published data only}
- Angelo IT, Prochazka V, Holinka M, Zapletalova J. Endosonography versus endoscopic retrograge cholangiopancreatography in diagnosing extrahepatic biliary obstruction. Biomedical Papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia 2011; Vol. 155, issue 4:339‐46. [DOI] [PubMed]
Dittrick 2005 {published data only}
- Dittrick G, Lamont JP, Kuhn JA, Mallat D. Usefulness of endoscopic ultrasound in patients at high risk of choledocholithiasis. Proceedings (Baylor University. Medical Center) 2005; Vol. 18, issue 3:211‐3. [0899‐8280: (Print)] [DOI] [PMC free article] [PubMed]
Duchmann 1999 {published data only}
- Duchmann JC, Benkirane A, Herve E, Barbare JC, Latrive JP, Messerschmitt C. Endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography performed during the same anesthesia session. [French]. Gastroenterologie Clinique et Biologique 1999; Vol. 23, issue 10:1028‐32. [PubMed]
Dwerryhouse 1998 {published data only}
Eshghi 2008 {published data only}
- Eshghi F. Routine magnetic resonance cholangiography compared to intra‐operative cholangiography in patients with suspected common bile duct stones. Journal of Medical Sciences 2008; Vol. 8, issue 1:98‐101. [PubMed]
Familiari 2004 {published data only}
- Familiari LT. MRCP vs ERCP: A comparative study in diagnosis of common bile duct stones. Gastrointestinal Endoscopy 2004; Vol. 59, issue 5:AB198.
Fernandez 2001 {published data only}
- Fernandez E, Falco J, Martin J, Brullet E, Campo R, Espinos J, et al. A prospective, comparative study of magnetic resonance cholangiopancreatography and direct cholangiography in the diagnosis of biliary diseases. [Spanish]. Radiologia 2001; Vol. 43, issue 3:99‐104.
Filippone 2003 {published data only}
- Filippone A, Ambrosini R, Fuschi M, Marinelli T, Pinto D, Maggialetti A. Clinical impact of MR cholangiopancreatography in patients with biliary disease. [Italian, English]. Radiologia Medica 2003; Vol. 105, issue 1‐2:27‐35. [PubMed]
Galvao 2007 {published data only}
- Galvao do Amaral PC, Azaro Filho E, Marques de Menezes Ettinger JE, Cunha AG, Cangussu HC, Correa Lima MD, et al. Common bile duct investigation in patients with mild biliary pancreatitis. When and how? A prospective analysis of 48 patients. Hepato‐Gastroenterology 2007; Vol. 54, issue 77:1323‐5. [PubMed]
Griffin 2003 {published data only}
Gul 2010 {published data only}
- Gul H, Waheed S, Orakzai R, Nawaz M, Saddique U, Roghani IS. Utility of magnetic resonance Cholangiopancreatography in the evaluation of biliary tract obstruction. Journal of Medical Sciences 2010; Vol. 18, issue 2:97‐100.
Gupta 2008 {published data only}
- Gupta T, Anwar S, Mesenas S. Endoscopic ultrasound (EUS) for choledocholithiasis: accuracy and cost benefit analysis. Journal of Gastroenterology and Hepatology 2008; Vol. 23:A143.
Hasan 2010 {published data only}
- Hasan DI, Almassry HN. Magnetic resonance cholangiopancreatography in conjunction with 3D for assessment of different biliary obstruction causes. Egyptian Journal of Radiology and Nuclear Medicine 2010; Vol. 41, issue 4:483‐9.
Hayashi 2002 {published data only}
- Hayashi T, Maguchi H, Takahashi K, Katanuma A, Tanaka Y, Yoshida A, et al. Diagnosis of biliary stones by endoscopic ultrasound and intraductal ultrasonography. Gastrointestinal Endoscopy 2002; Vol. 56, issue 4:S128.
Ho 1999 {published data only}
- Ho JT, Yap CK. Magnetic resonance cholangiopancreatography: value of using the half‐Fourier acquisition single‐shot turbo spin‐echo (HASTE) sequence. Annals of the Academy of Medicine, Singapore 1999; Vol. 28, issue 3:366‐70. [PubMed]
Hochwald 1998 {published data only}
Holzknecht 1998 {published data only}
Hrabar 2009 {published data only}
- Hrabar D, Gomercic M, Duvnjak M, Ljubicic N, Pavic T, Nikolic M. Endoscopic ultrasonography in the diagnosis of choledocholithiasis. Acta Medica Croatica 2009; Vol. 63 Suppl 3:5‐9. [PubMed]
Hussein 2002 {published data only}
Isomoto 1998 {published data only}
- Isomoto I, Koshiishi T, Fukuda T, Hayashi K. Diagnosis of common bile duct stones by MR imaging, mainly MR cholangiopancreatography. [Japanese]. Nihon Igaku Hoshasen Gakkai Zasshi 1998; Vol. 58, issue 11:566‐71. [PubMed]
Ito 2001 {published data only}
- Ito K, Fujita N, Noda Y, Kobayashi G, Kimura K, Tada T, et al. Clinical efficacy of magnetic resonance cholangiopancreatography in the diagnosis of biliary tract diseases. [Japanese]. Japanese Journal of Gastroenterology 2001; Vol. 98, issue 10:1164‐73. [PubMed]
Janssen 2008 {published data only}
Karakan 2009 {published data only}
Kats 2003 {published data only}
Kausar 2005 {published data only}
- Kausar A, Kaushik VY, Chang D, Chadwick M. Role of endoscopic ultrasound following normal ultrasound and/or magnetic resonance imaging in patients suspected of biliary calculus disease. Gut 2005; Vol. 54:A72.
Ke 2004 {published data only}
- Ke ZW, Zheng CZ, Li JH, Yin K, Chen DL, Hu MG, et al. Evaluation of magnetic resonance cholangiography in patients with suspected common bile duct stones before laparoscopic cholecystectomy. [Chinese]. World Chinese Journal of Digestology 2004; Vol. 12, issue 9:2143‐6.
Kejriwal 2004 {published data only}
Kim 2002 {published data only}
Kim 2005 {published data only}
Kohut 2003 {published data only}
- Kohut M, Nowak A, Nowakowska‐Dulawa E, Marek T, Kaczor R. Endosonography with linear array instead of endoscopic retrograde cholangiography as the diagnostic tool in patients with moderate suspicion of common bile duct stones. World Journal of Gastroenterology 2003; Vol. 9, issue 3:612‐4. [DOI] [PMC free article] [PubMed]
Kondo 2005 {published data only}
- Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, et al. Detection of common bile duct stones: Comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical‐computed‐tomographic cholangiography. European Journal of Radiology 2005; Vol. 54, issue 2:271‐5. [DOI] [PubMed]
Lachter 2000 {published data only}
Laghi 1998 {published data only}
- Laghi A, Pavone P, Catalano C, Broglia L, Messina A, Panebianco V, et al. MR Cholangiopancreatography (MRCP) in the evaluation of bilio‐pancreatic diseases. [Italian]. Chirurgia 1998; Vol. 11, issue 5:305‐10.
Laokpessi 2001 {published data only}
Lee 1996 {published data only}
- Lee DWH, Chan YL, Chan ACW, Lam WWM, Chung SCS, Sung JY, et al. Magnetic resonance cholangiography can replace endoscopic retrograde cholangiography for the diagnosis of common bile duct stones. Gastrointestinal Endoscopy 1996; Vol. 43, issue 4:381.
Lee 2010 {published data only}
Le Rhun 1999 {published data only}
- Rhun M. Magnetic resonance cholangiography and diagnosis of choledocolithiasis. [French]. Hepato‐Gastroenterology 1999; Vol. 6, issue 3:231‐2.
Leytens 2001 {published data only}
- Leytens JWA, Proosdij MP, Koster K, Eeftinck Schattenkerk M, Ziedses des Plantes BG, Hazenberg HJA, et al. Magnetic resonance cholangiopancreatography: A sensitive and specific method of examination in presumption of choledocholithiasis. [Dutch]. Nederlands Tijdschrift voor Geneeskunde 2001; Vol. 145, issue 10:478‐82. [PubMed]
Liessi 1996 {published data only}
- Liessi G, Cesari S, Dell'Antonio C, Avventi P, Spaliviero B, Butini R, et al. Cholangiopancreatography with magnetic resonance. Clinical use of a new "inversion‐recovery" sequence. [Italian]. La Radiologia Medica 1996; Vol. 92, issue 3:252‐6. [PubMed]
Lim 2003 {published data only}
- Lim KP, Khan AL, Kirk HJ, Deans H, Koruth M. A prospective comparison of endoscopic retrograde cholangiography with magnetic resonance cholangiography in choledocholithiasis. British Journal of Surgery 2003; Vol. 90:94.
Liu 1999 {published data only}
- Liu TH, Consorti ET, Kawashima A, Ernst RD, Black CT, Greger Jr PH, et al. The efficacy of magnetic resonance cholangiography for the evaluation of patients with suspected choledocholithiasis before laparoscopic cholecystectomy. American Journal of Surgery 1999; Vol. 178, issue 6:480‐4. [DOI] [PubMed]
Liu 2005 {published data only}
- Liu CL, Fan ST, Lo CM, Tso WK, Wong Y, Poon RTP, et al. Comparison of early endoscopcic ultrasonography and endoscopic retrograde cholangiopancreatography in the management of acute biliary pancreatitis: A prospective randomized study. Clinical Gastroenterology and Hepatology 2005; Vol. 3, issue 12:1238‐44. [DOI] [PubMed]
Lomanto 1997 {published data only}
Lomas 1999 {published data only}
Lundorf 2000 {published data only}
- Lundorf E, Sorensen JS, Wara P, Kruse A. MR‐cholangiography in patients suspected with choledochus calculi. [Danish]. Ugeskrift for Laeger 2000; Vol. 162, issue 17:2436‐8. [PubMed]
Magnuson 1997 {published data only}
- Magnuson TH, Regan F, Ahrendt SA, Schaefer DC, Bender JS. Magnetic resonance cholangiography compared to ultrasound and other clinical criteria in the preoperative prediction of choledocholithiasis. Gastroenterology 1997; Vol. 112, issue 4:A1456.
Magnuson 1999 {published data only}
Makary 2005 {published data only}
- Makary MA, Duncan MD, Harmon JW, Freeswick PD, Bender JS, Bohlman M, et al. The role of magnetic resonance cholangiography in the management of patients with gallstone pancreatitis. Annals of Surgery 2005; Vol. 241, issue 1:119‐24. [DOI] [PMC free article] [PubMed]
Maurea 2009 {published data only}
Meduri 1998 {published data only}
- Meduri B, Aubert A, Chiche R, Fritsch J. Laparoscopic cholecystectomy and common bile duct stones: value of preoperative endoscopic ultrasonography and endoscopic retrograde cholangiography. Gastroenterologie Clinique et Biologique 1998; Vol. 22, issue 10:759‐65. [PubMed]
Mendler 1998 {published data only}
Meroni 2004 {published data only}
- Meroni E, Bisagni P, Bona S, Fumagalli U, Zago M, Rosati R, et al. Pre‐operative endoscopic ultrasonography can optimise the management of patients undergoing laparoscopic cholecystectomy with abnormal liver function tests as the sole risk factor for choledocholithiasis: a prospective study. Digestive and Liver Disease 2004; Vol. 36, issue 1:73‐7. [DOI] [PubMed]
Miao 2008 {published data only}
- Miao L, Fan ZN, Ji GZ, Wen W, Wang X, Xiong GY, et al. Comparative study of ultrasonography, magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography in common duct stones. [Chinese]. Chinese Journal of Surgery 2008; Vol. 46, issue 19:1465‐7. [PubMed]
Mirbagheri 2005 {published data only}
- Mirbagheri SA, Mohamadnejad M, Nasiri J, Vahid AA, Ghadimi R, Malekzadeh R. Prospective evaluation of endoscopic ultrasonography in the diagnosis of biliary microlithiasis in patients with normal transabdominal ultrasonography. Journal of Gastrointestinal Surgery 2005; Vol. 9, issue 7:961‐4. [DOI] [PubMed]
Mofidi 2008 {published data only}
Moon 2005 {published data only}
Morera 2006 {published data only}
Morris‐Stiff 2009 {published data only}
- Morris‐Stiff G, Al‐Allak A, Frost B, Lewis WG, Puntis MC, Roberts A. Does endoscopic ultrasound have anything to offer in the diagnosis of idiopathic acute pancreatitis?. JOP: Journal of the Pancreas 2009; Vol. 10, issue 2:143‐6. [PubMed]
Munir 2004 {published data only}
- Munir K, Bari V, Yaqoob J, Khan DB, Usman MU. The role of magnetic resonance cholangiopancreatography (MRCP) in obstructive jaundice. Journal of the Pakistan Medical Association 2004; Vol. 54, issue 3:128‐32. [0030‐9982: (Print)] [PubMed]
Musella 1998 {published data only}
Nandalur 2008 {published data only}
Nau 2011 {published data only}
- Nau PN, Cowgill S, Ellison E, Melvin W, Muscarella P. Diagnostic accuracy of magnetic resonance cholangiopancreatography in patients with suspected choledocholithiasis. HPB 2011; Vol. 13:48.
Nebiker 2009 {published data only}
Neri 2000 {published data only}
- Neri V, Ambrosi A, Lauro G, Melino R, Valentino TP. Role of ERCP, MRCP and laparoscopic exploration of common biliary duct. E.A.E.S: Proceedings of the 8th International Congress of the European Association for Endoscopic Surgery. E.A.E.S., 2000:167‐71.
Norero 2008 {published data only}
- Norero E, Norero B, Huete A, Pimentel F, Cruz F, Ibanez L, et al. Accuracy of magnetic resonance cholangiopancreatography for the diagnosis of common bile duct stones. [Spanish]. Revista Medica de Chile 2008; Vol. 136, issue 5:600‐5. [PubMed]
Okaniwa 2002 {published data only}
- Okaniwa S, Nakamura Y, Matsuo K, Horigome N, Kaneko G, Miyakawa M. Usefulness of endoscopic ultrasonography in detecting bile duct stones. Gastrointestinal Endoscopy 2002; Vol. 56, issue 4:S127.
Palazzo 1995 {published data only}
Palazzo 1998 {published data only}
- Palazzo L. [Lithiasis of the common bile duct: endoscopic ultrasonography. Results and indications]. Gastroentérologie Clinique et Biologique 1998; Vol. 22, issue 5 Suppl:B7‐B16. [0399‐8320: (Print)] [PubMed]
Palmucci 2010 {published data only}
- Palmucci S, Mauro LA, Scola S, Incarbone S, Bonanno G, Milone P, et al. Magnetic resonance cholangiopancreatography and contrast‐enhanced magnetic resonance cholangiopancreatography versus endoscopic ultrasonography in the diagnosis of extrahepatic biliary pathology. La Radiologia Medica 2010; Vol. 115, issue 5:732‐46. [DOI] [PubMed]
Pamos 1998 {published data only}
- Pamos S, Rivera P, Canelles P, Quiles F, Orti E, Cuquerella J, et al. [Magnetic resonance cholangiopancreatography (MRCP) versus endoscopic retrograde cholangiopancreatography (ERCP): diagnostic usefulness]. Gastroenterology & Hepatology 1998; Vol. 21, issue 4:174‐80. [0210‐5705: (Print)] [PubMed]
Pamos 2003 {published data only}
- Pamos S, Benages A, Medina E, Martinez Sanjuan V. Prospective evaluation of magnetic resonance cholangiopancreatography in patients with biliary disease: comparative study with conventional ultrasonography and endoscopic retrograde cholangiopancreatography diagnostic algorithm. Digestive and Liver Disease 2003; Vol. 35, issue 3:186‐92. [DOI] [PubMed]
Pavone 1996 {published data only}
- Pavone P, Laghi A, Catalano C, Broglia L, Fiocca F, Passariello R. Non‐invasive evaluation of the biliary tree with magnetic resonance cholangiopancreatography: Initial clinical experience. Italian Journal of Gastroenterology 1996; Vol. 28, issue 2:63‐9. [PubMed]
Pavone 1996a {published data only}
- Pavone P, Laghi A, Catalano C, Broglia L, Panebianco V, Messina A, et al. [Lithiasis of the common bile duct: the role of cholangiography and magnetic resonance]. Radiologia Medica 1996; Vol. 91, issue 4:420‐3. [0033‐8362: (Print)] [PubMed]
Pavone 1996b {published data only}
- Pavone P, Laghi A, Catalano C, Panebianco V, Messina A, Pirillo S, et al. [Cholangiography with magnetic resonance in the diagnosis of main common bile duct calculi in candidates to laparoscopic cholecystectomy]. Radiologia Medica 1996; Vol. 92, issue 6:748‐51. [0033‐8362: (Print)] [PubMed]
Pavone 1997 {published data only}
Pavone 1997a {published data only}
- Pavone P, Laghi A, Panebianco V, Catalano C, Passariello R. MR cholangiopancreatography: technique, indications and clinical results. [Italian]. Radiologia Medica 1997; Vol. 94, issue 6:632‐41. [PubMed]
Polkowski 2001 {published data only}
- Polkowski M, Regula J, Tilszer A, Rupinski M, Wronska E, Butruk E. Endosonography instead of endoscopic retrograde cholangiography in patients with low‐to‐moderate probability of bile duct stones ‐ A randomised, prospective comparison of two management strategies. [Polish]. Gastroenterologia Polska 2001; Vol. 8, issue 3:269‐76.
Pomakov 2007 {published data only}
- Pomakov OA, Mehboob S. Incidental bile duct stones diagnosed by EUS. American Journal of Gastroenterology 2007; Vol. 102:S177‐8.
Pozo 2010 {published data only}
- Pozo DD, Tabernero S, Poves E. Usefulness of endoscopic ultrasonography in patients with low clinical suspicion of biliary disease. Gastrointestinal Endoscopy 2010; Vol. 71, issue 5:AB287.
Pulpeiro 2000 {published data only}
- Pulpeiro JR, Armesto V, Lopez‐Roses L, Lancho A, Gonzalez A. Comparison between magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP). [Spanish]. Radiologia 2000; Vol. 42, issue 3:175‐81.
Puri 2012 {published data only}
- Puri R, Sud R, Thandassery RB. EUS versus ERC in patients with moderate risk of common bile duct stones. Gastrointestinal Endoscopy 2012; Vol. 1:AB197‐8.
Rahman 2010 {published data only}
- Rahman R, Ju J, Shamma's J, Goebel S, Sundaram U. Correlation between MRCP and ERCP findings at a tertiary care hospital. The West Virginia Medical Journal 2010; Vol. 106, issue 5:14‐9. [PubMed]
Regan 1996 {published data only}
Regan 1996a {published data only}
Regan 1998 {published data only}
Reinhold 1998 {published data only}
Roig 1995 {published data only}
- Roig MVP, Espinosa RG, Rodero DR. Risk of common bile‐duct stones ‐ selective criteria for preoperative ercp or intraoperative cholangiography in laparoscopic cholecystectomy. British Journal of Surgery 1995; Vol. 82:15.
Roig 1995a {published data only}
- Roig MVP, Espinosa RG, Rodero DR. Risk of common bile‐duct stones ‐ selective criteria for preoperative ERCP or intraoperative cholangiography in laparoscopic cholecystectomy. British Journal of Surgery 1995; Vol. 82:15.
Rudowicz‐Pietruszewska 2002 {published data only}
- Rudowicz‐Pietruszewska B, Sasiadek M, Jamrozik‐Kruk Z. MRCP with mid‐field unit versus ERCP ‐ Comparison of 88 cases. [Polish]. Gastroenterologia Polska 2002; Vol. 9, issue 1:51‐8.
Sabbagh 2000 {published data only}
- Sabbagh L, Velasco B, Hani A, Gutierrez O, Jaramillo C, Sanmiguel C, et al. A prospective evaluation of endoscopic ultrasonography reliability for choledocholithiasis and pancreatic involvement diagnosis in acute pancreatic. Gastrointestinal Endoscopy 2000; Vol. 51, issue 4:AB246.
Sajewicz 2006 {published data only}
- Sajewicz Z, Wozniak‐Stolarska B, Salomon A, Poniewierka E, Kempinski R. The use of endoscopic ultrasonography in the diagnosis of the causes of common bile duct dilation. Advances in Clinical and Experimental Medicine 2006; Vol. 15, issue 2:293‐5.
Sakai 2007 {published data only}
- Sakai Y, Tsuyuguchi T, Tsuchiya S, Sugiyama H, Miyakawa K, Ebara M, et al. Diagnostic value of MRCP and indications for ERCP. Hepato‐Gastroenterology 2007; Vol. 54, issue 80:2212‐5. [PubMed]
Salmeron 1994 {published data only}
- Salmeron M, Simon JF, Houdart R, Lemann M, Johanet H. Endoscopic ultrasonography (EUS) versus invasive methods for the diagnosis of common bile‐duct stones (CBDS). Gastroenterology 1994; Vol. 106, issue 4:A357.
Saruc 2001 {published data only}
- Saruc M, Tarhan S, Aydede H, Can M, Erhan Y, Ersoz G, et al. Magnetic resonance cholangiopancreatography versus endoscopic retrograde cholangiopancreatography in the diagnosis of common bile duct stones. Turkish Journal of Gastroenterology 2001; Vol. 12, issue 4:263‐6.
Scaffidi 2009 {published data only}
- Scaffidi MG, Luigiano C, Consolo P, Pellicano R, Giacobbe G, Gaeta M, et al. Magnetic resonance cholangio‐pancreatography versus endoscopic retrograde cholangio‐pancreatography in the diagnosis of common bile duct stones: A prospective comparative study. Minerva Medica 2009; Vol. 100, issue 5:341‐7. [PubMed]
Scheiman 2001 {published data only}
- Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, Chey WD, et al. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? A prospective trial and cost analysis. American Journal of Gastroenterology 2001; Vol. 96, issue 10:2900‐4. [DOI] [PubMed]
Schmidt 2012 {published data only}
Seifert 2004 {published data only}
Shafiq 2003 {published data only}
- Shafiq K, Thomas E, Brett B, Jamieson C. Evaluating MRC against ERCP in the assessment of bile duct stones. Gut 2003; Vol. 52:A25.
Shamiyeh 2005 {published data only}
Shanmugam 2005 {published data only}
Shim 1995 {published data only}
Simeone 1997 {published data only}
- Simeone A, Carriero A, Armillotta M, Marano R, Maio G, Scarabino T, et al. Choledocholithiasis: semeiotic and diagnostic accuracy of cholangiography with magnetic resonance. [Italian]. La Radiologia Medica 1997; Vol. 93, issue 5:561‐6. [PubMed]
Skorka 1982 {published data only}
- Skorka B, Preuss HJ, Baldauf K. Informative value and validity of pre‐, per‐ and postoperative radiological bile‐duct diagnostics. [German]. Zeitschrift fur Arztliche Fortbildung 1982; Vol. 76, issue 1‐2:24‐9.
Soto 1996 {published data only}
Soto 2000 {published data only}
Soto 2000a {published data only}
- Soto JA, Barish MA, Alvarez O, Medina S. Detection of choledocholithiasis with MR cholangiography: Comparison of three‐dimensional fast spin‐echo and single‐ and multisection half‐Fourier rapid acquisition with relaxation enhancement sequences. Radiology 2000; Vol. 215, issue 3:737‐45. [DOI] [PubMed]
Sotoudehmanesh 2007 {published data only}
- Sotoudehmanesh R, Kolahdoozan S, Asgari AA, Dooghaei‐Moghaddam M, Ainechi S. Role of endoscopic ultrasonography in prevention of unnecessary endoscopic retrograde cholangiopancreatography ‐ A prospective study of 150 patients. Journal of Ultrasound in Medicine 2007; Vol. 26, issue 4:455‐60. [DOI] [PubMed]
Sperlongano 2005 {published data only}
- Sperlongano P, Pisaniello D, Viscovo L, Falco M, Parmeggiani D, Piatto A, et al. Efficacy of magnetic resonance cholangiopancreatography in detecting common bile duct lithiasis: our experience. Chirurgia Italiana 2005; Vol. 57, issue 5:635‐40. [PubMed]
Srinivasa 2010 {published data only}
- Srinivasa S, Sammour T, McEntee B, Davis N, Hill AG. Selective use of magnetic resonance cholangiopancreatography in clinical practice may miss choledocholithiasis in gallstone pancreatitis. Canadian Journal of Surgery 2010; Vol. 53, issue 6:403‐7. [PMC free article] [PubMed]
Stevens 1996 {published data only}
- Stevens PD, Lightdale CJ, Chabot JA, Green PHR, Stein JA, Siegel LM, et al. Endoscopic ultrasound in patients with suspected common bile duct stones before laparoscopic cholecystectomy. Gastrointestinal Endoscopy 1996; Vol. 43, issue 2:13.
Stiris 2000 {published data only}
Sugiyama 1997 {published data only}
Sugiyama 1998 {published data only}
Sverrisson 2012 {published data only}
- Sverrisson IP, Bjornsson ES, Ivarsson B, Jonsson HM, Hannesson P, Blondal S. The value of magnetic resonance cholangio‐pancreatography (MRCP) in patients suspected to have choledocholithiasis. Scandinavian Journal of Gastroenterology 2012; Vol. 47:S68.
Taylor 2002 {published data only}
Tennoe 1999 {published data only}
- Tennoe B, Stiris MG, Dullerud R, Lunde OC, Aadland E. Magnetic resonance tomography of biliary and pancreatic ducts. [Norwegian]. Tidsskrift for den Norske Laegeforening 1999; Vol. 119, issue 22:3252‐6. [PubMed]
Topal 2003 {published data only}
Tripathi 2002 {published data only}
- Tripathi RP, Batra A, Kaushik S. Magnetic resonance cholangiopancreatography: evaluation in 150 patients. Indian Journal of Gastroenterology 2002; Vol. 21, issue 3:105‐9. [PubMed]
Uehara 1998 {published data only}
- Uehara H, Caro L, Cerisoli C, Ghigliani M. Usefulness of endoscopic ultrasound (EUS) in the diagnosis of choledocholithiasis. Gastrointestinal Endoscopy 1998; Vol. 47, issue 4:AB155.
Urban 2002 {published data only}
Vaishali 2004 {published data only}
Valji 1996 {published data only}
- Valji A, Rawat B, Loewy J, Pfeifer J, Keith R. MRI cholangiography is highly predictive for choledocholithiasis. Gastroenterology 1996; Vol. 110, issue 4:A1424.
Varghese 1999 {published data only}
- Varghese JC, Farrell MA, Courtney G, Osborne H, Murray FE, Lee MJ. A prospective comparison of magnetic resonance cholangiopancreatography with endoscopic retrograde cholangiopancreatography in the evaluation of patients with suspected biliary tract disease. Clinical Radiology 1999; Vol. 54, issue 8:513‐20. [DOI] [PubMed]
Varghese 2000 {published data only}
Vazquez‐Sequeiros 2005 {published data only}
- Vazquez‐Sequeiros E, Boixeda‐Miquel D, Moreira‐Vicente V, Garcia‐Plaza A. Patients with suspicion for bile duct stones and negative MRI cholangiography: EUS to the rescue?. Gastrointestinal Endoscopy 2005; Vol. 61, issue 5:AB304.
Vazquez‐Sequeiros 2011 {published data only}
- Vazquez‐Sequeiros E, Tamargo FGP, Boixeda‐Miquel D, Milicua JM. Diagnostic accuracy and therapeutic impact of endoscopic ultrasonography in patients with intermediate suspicion of choledocholithiasis and absence of findings in magnetic resonance cholangiography. Revista Espanola de Enfermedades Digestivas 2011; Vol. 103, issue 9:464‐71. [DOI] [PubMed]
Verma 2006 {published data only}
Watanabe 2003 {published data only}
- Watanabe M, Sugano S, Yamamoto K, Kobayashi M, Sumino Y. Diagnosis of choledocholithiasis using magnetic resonance cholangiopancreatography (MRCP) 0.5T single‐slice 2D‐fast advanced spin echo (FASE). Journal of the Medical Society of Toho University 2003; Vol. 50, issue 3:233‐41.
Wehrmann 2009 {published data only}
Wierzbicka‐Paczos 1999 {published data only}
- Wierzbicka‐Paczos E, Butkiewicz J. Endoscopic ultrasonography in the diagnosis of unexplained extrahepatic cholestasis. [Polish]. Polski Merkuriusz Lekarski 1999; Vol. 7, issue 40:175‐9. [PubMed]
Wong 2012 {published data only}
- Wong HP, Chiu YL, Shiu BH, Ho LC. Preoperative MRCP to detect choledocholithiasis in acute calculous cholecystitis. Journal of Hepato‐Biliary‐Pancreatic Sciences 2012; Vol. 19, issue 4:458‐64. [1868‐6982: (Electronic)] [DOI] [PMC free article] [PubMed]
Zaheer 2011 {published data only}
- Zaheer A, Anwar MM, Donohoe CL, O'Keeffe S, Mushtaq H, Barry Kelleher T, et al. EUS significantly reduces the burden of ERCP and accurately predicts CBD stones in patients with suspected biliary obstruction: Consecutive analysis of 418 patients. Gastrointestinal Endoscopy 2011; Vol. 1:AB328‐9.
Zaydan 2009 {published data only}
- Zaydan RA, Muslim OT. Is endoscopic ultrasonography mandatory prior to endoscopic retrograde cholangiopancreatography in patients at high risk of choledocholithiasis?. Gastrointestinal Endoscopy 2009; Vol. 69, issue 2:S264.
Zhang 2012 {published data only}
- Zhang ZY, Wang D, Ni JM, Yu XR, Zhang L, Wu WJ, et al. Comparison of three‐dimensional negative‐contrast CT cholangiopancreatography with three‐dimensional MR cholangiopancreatography for the diagnosis of obstructive biliary diseases. European Journal of Radiology 2012; Vol. 81, issue 5:830‐7. [DOI] [PubMed]
Zhi 2002 {published data only}
- Zhi FC, Yan ZQ, Li XL, Zhu JX, Chen CL, Zhang XL, et al. Prospective study of diagnostic value of magnetic resonance cholangiopancreatography versus endoscopic retrograde cholangiopancreatography in cholangiopancreatic diseases. Chinese Journal of Digestive Diseases 2002; Vol. 3, issue 3:124‐6.
Zidi 1997 {published data only}
- Zidi S, Prat F, LeGuen O, Frouge C, Pelletier G. Magnetic resonance cholangiography (MRCP) in biliary stone disease. A prospective controlled study. Gastroenterology 1997; Vol. 112, issue 4:A529.
Zidi 1999 {published data only}
- Zidi SH, Prat F, Guen O, Rondeau Y, Rocher L, Fritsch J, et al. Use of magnetic resonance cholangiography in the diagnosis of choledocholithiasis: Prospective comparison with a reference imaging method. Gut 1999; Vol. 44, issue 1:118‐22. [DOI] [PMC free article] [PubMed]
Additional references
Abdallah 2007
- Abdallah AA, Krige JEJ, Bornman PC. Biliary tract obstruction in chronic pancreatitis. HPB 2007;9(6):421‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anciaux 1986
- Anciaux ML, Pelletier G, Attali P, Meduri B, Liguory C, Etienne JP. Prospective study of clinical and biochemical features of symptomatic choledocholithiasis. Digestive Diseases and Sciences 1986;31(5):449‐53. [DOI] [PubMed] [Google Scholar]
Arnold 1970
- Arnold DJ, Zollinger RW, Bartlett RM, Telesz W, King RG, Strait J, et al. 28621 cholecystectomies in Ohio. Results of a survey in Ohio hospitals by the gallbladder survey committee, Ohio Chapter, American College of Surgeons. American Journal of Surgery 1979;119(6):714‐7. [DOI] [PubMed] [Google Scholar]
Arnold 1979
- Arnold DJ, Zollinger RW, Bartlett RM, Telesz W, King RG, Strait J, et al. 28621 cholecystectomies in Ohio. Results of a survey in Ohio hospitals by the gallbladder survey committee, Ohio Chapter, American College of Surgeons. American Journal of Surgery 1979;119(6):714‐7. [DOI] [PubMed] [Google Scholar]
ASGE Standards of Practice Commitee 2010
- Maple JT, Ben‐Menachem T, Anderson MA, Appalaneni V, Banerjee S, ASGE Standards of Practice Commitee 2010. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointestinal Endoscopy 2010;71(1):1‐9. [DOI] [PubMed] [Google Scholar]
Attili 1995
- Attili AF, Santis A, Capri R, Repice AM, Maselli S. The natural history of gallstones: The GREPCO experience. The GREPCO group. Hepatology 1995;21(3):655‐60. [DOI] [PubMed] [Google Scholar]
Barbara 1987
- Barbara L, Sama C, Morselli Labate AM, Taroni F, Rusticali AG, Festi D, et al. A population based study on the prevalence of gallstone disease: the Sirmione study. Hepatology 1987;7(5):913‐7. [DOI] [PubMed] [Google Scholar]
Barkun 1994
- Barkun AN, Barkun JS, Fried GM, Ghitulescu G, Steinmetz O, Pham C, et al. Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. Annals of Surgery 1994;220(1):32‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benjaminov 2013
- Benjaminov F, Leichtman G, Naftali T, Half EE, Konikoff FM. Effects of age and cholecystectomy on common bile duct diameter as measured by endoscopic ultrasonography. Surgical Endoscopy 2013;27(1):303‐7. [DOI] [PubMed] [Google Scholar]
Buscemi 2006
- Buscemi N, Hartling L, Vandermeer B, Tjosvold L, Klassen TP. Single data extraction generated more errors than double data extraction in systematic reviews. Journal of Clinical Epidemiology 2006;59(7):697‐703. [DOI] [PubMed] [Google Scholar]
Caddy 2006
- Caddy GR, Tham DC. Gallstone disease: symptoms, diagnosis and endoscopic management of common bile duct stones. Best Practice & Research. Clinical Gastroenterology 2006;20(6):1085‐101. [DOI] [PubMed] [Google Scholar]
Chen 2007
- Chen YK, Pleskow DK. SpyGlass single‐operator peroral cholangiopacreatoscopy system for the diagnosis and therapy of bile duct disorders: a clinical feasibility study (with video). Gastrointestinal Endoscopy 2007;65(6):832‐41. [DOI] [PubMed] [Google Scholar]
Choi 2011
- Choi SB, Kim W, Song TJ, Suh SO, Kim YC, Choi SY. Surgical outcomes and prognostic factors for ampulla of Vater cancer. Scandinavian Journal of Surgery 2011;100(2):92‐8. [DOI] [PubMed] [Google Scholar]
Chu 2006
- Chu H, Cole SR. Bivariate meta‐analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. Journal of Clinical Epidemiology 2006;59(12):1331‐2. [DOI] [PubMed] [Google Scholar]
Corfield 1985
- Corfield AP, Cooper MJ, Williamson RCN. Acute pancreatitis: a lethal disease of increasing incidence. Gut 1985;26(7):724‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dasari 2013
- Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, et al. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database of Systematic Reviews 2013, Issue 9. [DOI: 10.1002/14651858.CD003327.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Doust 2005
- Doust JA, Pietrzak E, Sanders S, Glasziou PP. Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. Journal of Clinical Epidemiology 2005;58(5):444‐9. [DOI] [PubMed] [Google Scholar]
Eloubeidi 2001
- Eloubeidi MA, Wade SB, Provenzale D. Factors associated with acceptance and full publication of GI endoscopic research originally published in abstract form. Gastrointestinal Endoscopy 2001;53(3):275‐82. [DOI] [PubMed] [Google Scholar]
Fickling 2003
- Fickling WE, Wallace MB. Endoscopic ultrasound and upper gastrointestinal disorders. Journal of Clinical Gastroenterology 2003;36(2):103‐10. [DOI] [PubMed] [Google Scholar]
Fiore 1997
- Fiore NF, Ledniczky G, Wiebke EA, Broadie TA, Pruitt AL, Goulet RJ, et al. An analysis of perioperative cholangiography in one thousand laparoscopic cholecystectomies. Surgery 1997;122(4):817‐23. [DOI] [PubMed] [Google Scholar]
Freitas 2006
- Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standard for diagnosis and management. World Journal of Gastroenterology 2006;12(20):3162‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Geron 1999
- Geron N, Reshef R, Shiller M, Kniaz D, Eitan A. The role of endoscopic retrograde cholangiopancreatography in the laparoscopic era. Surgical Endoscopy, Ultrasound and Interventional Techniques 1999;13(5):452‐6. [DOI] [PubMed] [Google Scholar]
Gurusamy 2010
- Gurusamy KS, Davidson BR. Surgical treatment of gallstones. Gastroenterology Clinics of North America 2010;39(2):229‐44, viii. [DOI] [PubMed] [Google Scholar]
Gurusamy 2011
- Gurusamy K, Sahay SJ, Burroughs AK, Davidson BR. Systematic review and meta‐analysis of intraoperative versus preoperative endoscopic sphincterotomy in patients with gallbladder and suspected common bile duct stones. British Journal of Surgery 2011;98(7):908‐16. [DOI] [PubMed] [Google Scholar]
Gurusamy 2015a
- Gurusamy KS, Giljaca V, Higgie D, Poropat G, Stimac D, Davidson BR. Endoscopic retrograde cholangiopancreatography versus intraoperative cholangiography for diagnosis of common bile duct stones. Cochrane Database of Systematic Reviews 2015, Issue 2. [DOI: 10.1002/14651858.CD010339] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gurusamy 2015b
- Gurusamy KS, Giljaca V, Higgie D, Poropat G, Stimac D, Davidson BR. Ultrasound versus liver function tests for diagnosis of common bile duct stones. Cochrane Database of Systematic Reviews 2015, Issue 2. [DOI: 10.1002/14651858.CD011548] [DOI] [PMC free article] [PubMed] [Google Scholar]
Halldestam 2004
- Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. British Journal of Surgery 2004;91(6):734‐8. [DOI] [PubMed] [Google Scholar]
Hamade 2005
- Hamade AM, Al‐Bahrani AZ, Owera AMA, Hamoodi AA, Abid GH, Bani Hani OI, et al. Therapeutic, prophylactic, and preresection applications of laparoscopic gastric and biliary bypass for patients with periampullary malignancy. Surgical Endoscopy 2005;19(10):1333‐40. [DOI] [PubMed] [Google Scholar]
Hirschfield 2011
- Hirschfield GM, Gershwin ME. Primary biliary cirrhosis: one disease with many faces. Israel Medical Association Journal 2011;13(1):55‐9. [PubMed] [Google Scholar]
Hong 2006
- Hong DF, Xin Y, Chen DW. Comparison of laparoscopic cholecystectomy combined with intraoperative endoscopic sphincterotomy and laparoscopic exploration of the common bile duct for cholecystocholedocholithiasis. Surgical Endoscopy and Other Interventional Techniques 2006;20(3):424‐7. [DOI] [PubMed] [Google Scholar]
Hoyuela 1999
- Hoyuela C, Cougat E, Pretcha P, Collera P, Espinos J, Marco C. Must ERCP be routinely performed if choledocholithiasis is suspected?. Digestive Surgery 1999;16(5):411‐4. [DOI] [PubMed] [Google Scholar]
Kalady 2004
- Kalady MF, Peterson B, Baillie J, Onaitis MW, Abdul‐Wahab OI, Howden JK, et al. Pancreatic duct strictures: identifying risk of malignancy. Annals of Surgical Oncology 2004;11(6):581‐8. [DOI] [PubMed] [Google Scholar]
Kelly 2010
- Kelly MD. Results of laparoscopic bile duct exploration via choledochotomy. ANZ Journal of Surgery 2010;80(10):694‐8. [DOI] [PubMed] [Google Scholar]
Krishna 2008
- Krishna RP, Kumar A, Singh RK, Sikora S, Saxena R, Kapoor VK. Xanthogranulomatous inflammatory strictures of extrahepatic biliary tract: presentation and surgical management. Journal of Gastrointestinal Surgery 2008;12(5):836‐41. [DOI] [PubMed] [Google Scholar]
Ledro‐Cano 2007
- Ledro‐Cano D. Suspected choledocholithiasis: endoscopic ultrasound or magnetic resonance cholangio‐pancreatography? A systematic review. European Journal of Gastroenterology & Hepatology 2007;19:1007‐11. [DOI] [PubMed] [Google Scholar]
Lefemine 2011
- Lefemine V, Morgan RJ. Spontaneous passage of common bile duct stones in jaundiced patients. Hepatobiliary and Pancreatic Diseases International 2011;10(2):209‐13. [DOI] [PubMed] [Google Scholar]
Lill 2010
- Lill S, Rantala A, Pekkala E, Sarparanta H, Huhtinen H, Rautava P, et al. Elective laparoscopic cholecystectomy without routine intraoperative cholangiography: a retrospective analysis of 1101 consecutive cases. Scandinavian Journal of Surgery 2010;99(4):197‐200. [DOI] [PubMed] [Google Scholar]
Lillemoe 2000
- Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Campbell KA, Talamini MA, et al. Postoperative bile duct strictures: management and outcome in the 1990s. Annals of Surgery 2000;232(3):430‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lin 2008
- Lin LF, Huang PT, Ho KS, Tung JN. Autoimmune chronic pancreatitis. Journal of the Chinese Medical Association 2008;71(1):14‐22. [DOI] [PubMed] [Google Scholar]
Loria 1994
- Loria P, Dilengite MA, Bozzzoli M, Carubbi F, Messora R, Sassatelli R, et al. Prevalence rates of gallstone disease in Italy. The Chianciano population study. European Journal of Epidemiology 1994;10(2):143‐50. [DOI] [PubMed] [Google Scholar]
Ludwig 2001
- Ludwig K, Kockerling F, Hohenberger W, Lorenz D. Surgical therapy for cholecysto‐/choledocholithiasis. Results of a Germany‐wide questionnaire sent to 859 clinics including 123,090 cholecystectomies [Die chirurgische Therapie der cholecysto‐/choledocholithiasis. Ergenbisse einer deutschlandweiten Umfrage an 859 Kliniken mit 123.090 cholecystektomien]. Der Chirurg 2001;72(10):1170‐8. [DOI] [PubMed] [Google Scholar]
Magnetic Resonance Imaging 2011
- What is an MRI scan and what can it do?. Drug and Therapeutics Bulletin 2011;49(12):141‐4. [DOI] [PubMed] [Google Scholar]
Mann 1994
- Mann DV, Hershman MJ, Hittinger R, Glazer G. Multicentre audit of death from acute pancreatitis. British Journal of Surgery 1994;81(6):890‐3. [DOI] [PubMed] [Google Scholar]
Maple 2010
- Maple JT, Ben‐Menachem T, Anderson MA, Appalaneni V, Banerjee S, ASGE Standards of Practice Commitee 2010. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointestinal Endoscopy 2010;71(1):1‐9. [DOI] [PubMed] [Google Scholar]
Mark 2002
- Mark DH, Flamm CR, Aronson N. Evidence‐based assessment of diagnostic modalities for common bile duct stones. Gastrointestinal Endoscopy 2002;56(6 Suppl):S190‐4. [DOI] [PubMed] [Google Scholar]
McMahon 2008
- McMahon CJ. The relative roles of magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound in diagnosis of common bile duct calculi: a critically appraised topic. Abdominal Imaging 2008;33:6‐9. [DOI] [PubMed] [Google Scholar]
Neoptolemos 1988
- Neoptolemos JP, London NJ, James D, Carr‐Locke DL, Bailey IA, Fossard DP. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet 1988;2(8618):979‐83. [DOI] [PubMed] [Google Scholar]
Park 2011
- Park SY, Park CH, Cho SB, Lee WS, Kim JC, Cho CK, et al. What is appropriate procedure for preoperative biliary drainage in patients with obstructive jaundice awaiting pancreaticoduodenectomy. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2011;21(5):344‐8. [DOI] [PubMed] [Google Scholar]
Penz‐Osterreicher 2011
- Penz‐Osterreicher M, Osterreicher CH, Trauner M. Fibrosis in autoimmune and cholestatic liver disease. Best Practices & Research. Clinical Gastroenterology 2011;25(2‐4):245‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
RadiologyInfo 2011
- RadiologyInfo.org. What is magnetic resonance cholangiopancreatography (MRCP)?. www.radiologyinfo.org/en/info.cfm?pg=mrcp (accessed on 27 February 2014).
Raraty 1998
- Raraty MG, Finch M, Neoptolemos JP. Acute cholangitis and pancreatitis secondary to common duct stones: management update. World Journal of Surgery 1998;22(11):1155‐61. [DOI] [PubMed] [Google Scholar]
Reitsma 2005
- Reitsma JB, Glas AS, Rutjes AWS, Scholten RJPM, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. Journal of Clinical Epidemiology 2005;58(10):982‐90. [DOI] [PubMed] [Google Scholar]
Ripolles 2009
- Ripolles T, Ramirez‐Fuentes C, Martinez‐Perez MJ, Delgado F, Blanc E, Lopez A. Tissue harmonic sonography in the diagnosis of common bile duct stones: a comparison with endoscopic retrograde cholangiography. Journal of Clinical Ultrasound 2009;37(9):501‐6. [DOI] [PubMed] [Google Scholar]
Roston 1997
- Roston AD, Jacobson IM. Evaluation of the pattern of liver tests and yield of cholangiography in symptomatic choledocholithiasis: a prospective study. Gastrointestinal Endoscopy 1997;45(5):394‐9. [DOI] [PubMed] [Google Scholar]
Saik 1975
- Saik RP, Greenburg AG, Farris JM, Peksin GW. Spectrum of cholangitis. American Journal of Surgery 1975;130(2):143‐50. [DOI] [PubMed] [Google Scholar]
Salek 2009
- Salek J, Livote E, Sideridis K, Bank S. Analysis of risk factors predictive of early mortality and urgent ERCP in acute cholangitis. Journal of Clinical Gastroenterology 2009;43(2):171‐5. [DOI] [PubMed] [Google Scholar]
Sampson 2008
- Sampson M, Shojania KG, McGowan J, Daniel R, Rader T, Iansavichene AE, et al. Surveillance search techniques identified the need to update systematic reviews. Journal of Clinical Epidemiology 2008;61(8):755‐62. [DOI] [PubMed] [Google Scholar]
Sarli 2000
- Sarli L, Costi R, Gobbi S, Sansebastiano G, Roncoroni L. Asymptomatic bile duct stones: selection criteria for intravenous cholangiography and/or endoscopic retrograde cholangiography prior to laparoscopic cholecystectomy. European Journal of Gastroenterology & Hepatology 2000;12(11):1175‐80. [PubMed] [Google Scholar]
Schuetz 2012
- Schuetz GM, Schlattmann P, Dewey M. Use of 3x2 tables with an intention to diagnose approach to assess clinical performance of diagnostic tests: meta‐analytical evaluation of coronary CT angiography studies. BMJ (Clinical Research Edition) 2012;345:e6717. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siddiqui 2011
- Siddiqui AA, Sreenarasimhaiah J, Lara LF, Harford W, Lee C, Eloubeidi MA. Endoscopic ultrasound‐guided transduodenal placement of a fully covered metal stent for palliative biliary drainage in patients with malignant biliary obstruction. Surgical Endoscopy 2011;25(2):549‐55. [DOI] [PubMed] [Google Scholar]
Singh 1990
- Singh SM, Londmire WP, Reber HA. Surgical palliation for pancreatic cancer: the UCLA experience. Annals of Surgery 1990;212(2):132‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spelsberg 2009
- Spelsberg FW, Nusser F, Huttl TK, Obeidat FW, Lang RA, Jauch KW, et al. Management of cholecysto‐ and choledocholithiasis‐survey and analysis of 16 615 cholecystectomies and common bile duct explorations in Bavaria. Zentralblatt fur Chirurgie 2009;134(2):120‐6. [DOI] [PubMed] [Google Scholar]
Takwoingi 2013
- Takwoingi Y, Leeflang MM, Deeks JJ. Empirical evidence of the importance of comparative studies of diagnostic test accuracy. Annals of Internal Medicine 2013;158(7):544‐54. [DOI] [PubMed] [Google Scholar]
Tang 2011
- Tang S, Singh S, Singh S. Sphincterotome stricturoplasty for long ampullary stenoses and benign biliary strictures (with video). Surgical Endoscopy 2011;25(4):1313‐8. [DOI] [PubMed] [Google Scholar]
Targarona 2004
- Targarona EM, Bendahan GE. Management of common bile duct stones: controversies and future perspectives. HPB 2004;6(3):140‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Toh 2000
- Toh SKC, Phillips S, Johnson CD. A prospective audit against national standards of the presentation and management of acute pancreatitis in the south of England. Gut 2000;46(2):239‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tranter 2003
- Tranter SE, Thompson MH. Spontaneous passage of bile duct stones: frequency of occurrence and relation to clinical presentation. Annals of the Royal College of Surgeons of England 2003;85(3):174‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting 2006
- Whiting PF, Weswood ME, Rutjes AWS, Reitsma JB, Bossuyt PNM, Kleijnen J. Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Medical Research Methodology 2006;6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, TQ‐2 group. QUADAS‐2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529‐36. [DOI] [PubMed] [Google Scholar]
Williams 2008
- Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the management of common bile duct stones (CBDS). Gut 2008;57(7):1004‐21. [DOI] [PubMed] [Google Scholar]
Wilson 2010
- Wilson JA, Hoffman B, Hawes RH, Romagnuolo J. EUS in patients with surgically altered upper GI anatomy. Gastrointestinal Endoscopy 2010;72(5):947‐53. [DOI] [PubMed] [Google Scholar]
Yousefpour Azary 2011
- Yousefpour Azary S, Kalbasi H, Setayesh A, Mousavi M, Hashemi A, Khodadoostan M, et al. Predictive value and main determinants of abnormal features of intraoperative cholangiography during cholecystectomy. Hepatobiliary and Pancreatic Diseases International 2011;10(3):308‐12. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Giljaca 2013
- Giljaca V, Gurusamy KS, Vaughan J, Stimac D, Davidson BR. Tests for diagnosis of common bile duct stones. Cochrane Database of Systematic Reviews 2013, Issue 1. [DOI: 10.1002/14651858.CD010339] [DOI] [PMC free article] [PubMed] [Google Scholar]


