Abstract
Background
Hospital environments have recently received renewed interest, with considerable investments into building and renovating healthcare estates. Understanding the effectiveness of environmental interventions is important for resource utilisation and providing quality care.
Objectives
To assess the effect of hospital environments on adult patient health‐related outcomes.
Search methods
We searched: the Cochrane Central Register of Controlled Trials (last searched January 2006); MEDLINE (1902 to December 2006); EMBASE (January 1980 to February 2006); 14 other databases covering health, psychology, and the built environment; reference lists; and organisation websites. This review is currently being updated (MEDLINE last search October 2010), see Studies awaiting classification.
Selection criteria
Randomised and non‐randomised controlled trials, controlled before‐and‐after studies, and interrupted times series of environmental interventions in adult hospital patients reporting health‐related outcomes.
Data collection and analysis
Two review authors independently undertook data extraction and 'Risk of bias' assessment. We contacted authors to obtain missing information. For continuous variables, we calculated a mean difference (MD) or standardized mean difference (SMD), and 95% confidence intervals (CI) for each study. For dichotomous variables, we calculated a risk ratio (RR) with 95% confidence intervals (95% CI). When appropriate, we used a random‐effects model of meta‐analysis. Heterogeneity was explored qualitatively and quantitatively based on risk of bias, case mix, hospital visit characteristics, and country of study.
Main results
Overall, 102 studies have been included in this review. Interventions explored were: 'positive distracters', to include aromas (two studies), audiovisual distractions (five studies), decoration (one study), and music (85 studies); interventions to reduce environmental stressors through physical changes, to include air quality (three studies), bedroom type (one study), flooring (two studies), furniture and furnishings (one study), lighting (one study), and temperature (one study); and multifaceted interventions (two studies). We did not find any studies meeting the inclusion criteria to evaluate: art, access to nature for example, through hospital gardens, atriums, flowers, and plants, ceilings, interventions to reduce hospital noise, patient controls, technologies, way‐finding aids, or the provision of windows. Overall, it appears that music may improve patient‐reported outcomes such as anxiety; however, the benefit for physiological outcomes, and medication consumption has less support. There are few studies to support or refute the implementation of physical changes, and except for air quality, the included studies demonstrated that physical changes to the hospital environment at least did no harm.
Authors' conclusions
Music may improve patient‐reported outcomes in certain circumstances, so support for this relatively inexpensive intervention may be justified. For some environmental interventions, well designed research studies have yet to take place.
Keywords: Adult; Humans; Health Facility Environment; Interior Design and Furnishings; Outcome and Process Assessment, Health Care; Air Pollution, Indoor; Inpatients; Inpatients/psychology; Lighting; Music; Music/psychology; Odorants; Randomized Controlled Trials as Topic; Temperature
Plain language summary
Sensory environment on health‐related outcomes of hospital patients
The hospital environment (such as sounds, pictures, aromas, design, air quality, furnishings, architecture, and layout), may have an impact on the health of patients within it. This review aims to summarise the best available evidence on hospital environments, in order to help people involved in the design of hospital environments make decisions that will benefit patients' health.
The review identified 102 relevant studies, 85 of which were on the use of music in hospital. Other environmental aspects considered were: aromas (two studies), audiovisual distractions (five studies), decoration (one study), air quality (three studies), bedroom type (one study), flooring (two studies), furniture and furnishings (one study), lighting (one study), temperature (one study), and multiple design changes (two studies). No studies meeting the inclusion criteria were found to evaluate: art, access to nature for example through hospital gardens, atriums, flowers, and plants, ceilings, interventions to reduce hospital noise, patient controls, technologies, way‐finding aids, or the provision of windows.
Overall, it appears that music in hospital may help improve patient‐reported outcomes such as anxiety; however, there is less evidence to support the use of music for physiological outcomes (such as reducing heart rate and blood pressure) and for reducing the use of medications. For other aspects of hospital environments, there are not very many well designed studies to help with making evidence‐based design decisions. The studies that have been included in this review show that physical changes made to 'improve' the hospital environment on the whole do no harm.
Background
The International Academy for Design and Health held its 7th World Congress in 2011, highlighting the growing multinational interest in environmental design that promotes health. A reform on a global scale is underway to make hospitals much more than places to go and receive treatment; hospitals are now being conceptualised as places that have the potential to positively impact health through being restorative, healing environments (Dilani 2001). The World Health Organization (WHO) highlights the important role of the environment in the health process, and calls for action towards creating supportive environments ('Ottowa' 2004). In accordance with this movement, international organisations such as The Centre for Health Design (CHD) have been established ('CHD' 2009). CHD's mission is 'to transform healthcare environments for a healthier, safer world through design research, education and advocacy'.
Other initiatives have been stimulated by the US‐based Society for the Arts in Healthcare ('SAH' 2009), which attempts to advance arts as an integral component in health care, and the UK‐based Medical Architecture Research Unit (Etheridge 2008), which provides research, consultancy, and training, with a vision to "explore the interface between health service organisational culture and the built environment response". Research into, and implementation of 'healing' healthcare environments is also being carried out in Japan (Cooper 2002; Takayanagi 2004), and across Europe (Pelikan 2001).
In the Middle East, various major investment projects have been supporting a rapid growth in the hospital sector (News 2004) and the hospital industry in the United States has been going through a major building boom with billions more dollars being spent on replacing or renovating old facilities (Babwin 2002). In the United Kingdom, the Private Finance Initiative (PFI) has prompted a renewed interest in hospital design, investing billions of pounds into the biggest new hospital building programme in the history of the NHS (Milburn 2001). Investments such as these have provided an opportunity for hospitals to be considered as 'therapeutic environments' (Gesler 2004), spurring on initiatives such as the UK‐based scheme in which the Kings Fund and the Department of Health offer grants to health authorities to enhance the environment ('Kings Fund' 2009).
Some argue that this expenditure is a waste of resources (Lipley 2001), whilst others have highlighted the lack of 'evidence‐based practice' when it comes to hospital design (Frumkin 2003). Schemes set up to enhance the hospital environment are sometimes not evaluated on the grounds that it is too logistically complex (Comer 1982), or by simply stating that the effects are obvious (Parker 2000). There is some empirical evidence in support of creating better environments in care facilities however, and researchers are finding that changes to the physical environment can positively influence patient outcomes (Devlin 2003; Rubin 1996). In an invitation‐only conference entitled 'Designing the 21st Century Hospital: serving patients and staff', held by the Robert Wood Johnson Foundation ('Webcast' 2004), Craig Zimring and Roger Ulrich referred to a literature review they had conducted, finding over 600 studies on the effects of the hospital environment on patients, families and staff (Ulrich 2004a, later updated: Ulrich 2008). In their presentation of the research, Zimring and Ulrich emphasised the evidence mainly in terms of quantity and consistency of findings. Following the presentations, delegates discussed how worthwhile applying quality criteria to the current evidence would be, such as in a Cochrane systematic review.
Description of the intervention
The environment can be altered in endless ways. Some environmental changes may be detrimental to health (Thompson 2000), further exemplifying the need for using evidence‐based design. As a framework for assessing the evidence on hospital design, the literature could be considered in terms of whether it regards: (1) aspects that are added to the environment as positive distracters (such as art and music); and (2) aspects of the environment that are changed to reduce stressors (such as light, noise or air quality).
In this review, we are interested in elements of the sensory environment; that is, aspects of the hospital surroundings that can be seen, touched, smelt, or heard (such as the building design and layout, decor, furniture and furnishings, air quality and aromas/odours, and noises/sounds). In this review we utilise the phrase 'sensory environment' to define the hospital characteristics under study; in the literature, other terms are utilised such as 'healing environments', 'supportive environments', and 'health‐promoting environments'. We have opted for a less directive phrase as we are interested in determining which environmental factors have positive, negative, and neutral effects on the health of individuals.
How the intervention might work
Sensory environments have been advocated on the basis of their perceived ability to reduce anxiety, lower blood pressure, improve postoperative outcomes, reduce the need for pain medication, and shorten the hospital stay (Ulrich 1992); good design has also been implicated to improve quality of sleep (Hewitt 2002; Marberry 2002), reduce hospital acquired infections (Ulrich 2004b), and improve staff retention and well‐being (Neuberger 2003; Marberry 2002; Gross 1998). Theories underpinning these effects are wide‐ranging and stem from a variety of perspectives, for example: Attention Restorative Theory (a 'functionalist‐evolutionary' model; Kaplan 1989); a 'psycho‐evolutionary' model (Ulrich 1983) and the Biophilia Hypothesis (Ulrich 1993a); Henry's model of neuro‐endocrine responses (Parsons 1991, which incorporates the ideas of the 'Fight or Flight' response to environmental stressors and Selye's model of stress and disease, 'General Adaptation Syndrome'); the Intake‐Reject Hypothesis (Lacey 1974), a controversial hypothesis which has implications for distraction therapies; the 'Gate Control Theory' (Melzack 1965) and the 'Neuromatrix Theory' of pain (Melzack 1999); and the Broaden‐and‐Build model (Fredrickson 2000), which offers a premise for creating environments which help cultivate positive emotions. We will not go into a full explanation and debate of all these theories here, but suffice is to say that although there are some disparities between these explanatory models, and some sit controversially within their fields, they complement each other on the general principles that removing environmental stressors, and using the environment to calm, distract, and elicit positive emotions may have positive implications for health.
Why it is important to do this review
Clearly this is a broad and complex area of study, with the 'environment' being considered as an intervention influencing health‐related outcomes; nevertheless, it is imperative that the evidence‐base for sensory environments is assessed systematically, to ensure that patients are provided with the best possible opportunity to recover and that the system remains cost‐effective.
Objectives
To assess the effect of the sensory hospital environment on adult patient health‐related outcomes.
Methods
Criteria for considering studies for this review
Types of studies
In this area of research it may often be very difficult to conduct a Randomised Controlled Trial (RCT) due to the nature of the intervention and logistical complexities. Therefore, this review included a variety of study designs: RCTs, (non‐randomised) Controlled Clinical Trials (CCTs), Controlled Before and After studies (CBAs), and Interrupted Time Series (ITS). To be included in the review, a CBA had to have two intervention sites and two concurrent control sites with outcomes measured both before and after the intervention was implemented. An ITS had to have at least three data collection points before the intervention, and at least a further three data collection points after the intervention. All studies must have been conducted prospectively.
Types of participants
The review included adults attending hospital as in‐patients, day hospital or out‐patients. Studies were included if over 90% of the participants were over 18. Both elective and non‐elective patients were included in the review. We have included all diagnoses including psychiatric patients (Gross 1998).
Where possible, studies were characterised by the type of hospital visit, where 90% of participants was considered as a cut‐off point for inclusion in a specific category. In‐patients were classed as those that required a hospital bed and required an overnight stay for tests or surgery; day‐patients were patients that required a hospital bed for specialised observation or health care for a limited number of hours of the day, but did not need to stay overnight; out‐patients were people who were referred to see a hospital consultant for a specialist opinion or examination and did not require a hospital bed.
Types of interventions
The review incorporated studies that investigated any aspect(s) of the sensory environment. Interventions were those that altered the environment by one or a mixture of the following ways.
(1) Providing positive distracters to complement the treatment already being administered. Positive distracters are elements of the sensory environment; they do not include therapies (such as bright light therapy), which are received instead of orthodox treatments. Patients could be offered a choice of distraction but we did not include instances when patients were actively involved in creating a distraction (e.g. creating a work of art). Positive distracters included:
aromas/scents (different aromas/patient choice of aroma versus none);
viewing artwork (comparing different styles/patient choice of art versus no art);
viewing performance art (versus none);
audiovisual distractions, such as television/video (absent versus present/differences between content/patient choice of content);
decoration (colour of walls etc.);
music (versus no music, different styles of music, or other environmental comparison);
access to nature, for example via atriums, gardens, window views, or indoor planting (versus no access to nature, other views or urban retreats).
(2) Reducing environmental stressors by implementing physical changes. We have not included changes that are made to policy (e.g. ensuring multi‐bed rooms are unisex). Physical changes to the sensory environment include:
noise‐reducing aids (e.g. sound‐absorbing ceiling tiles versus regular);
way‐finding aids (e.g. colour‐zoned areas, landmarks);
patient controls (e.g. access to lighting and ventilation controls);
lighting (e.g. natural versus fluorescent);
people/privacy (e.g. open versus closed wards, decentralised nurse stations).
(3) Multi‐faceted interventions: Some studies manipulate many variables and as such span across the above three broad categories of environmental interventions (such as when a whole ward is redesigned; Leather 2003). We have included these studies in the review provided they were not confounded with non‐environmental changes, such as changes to policy.
We excluded studies from the review if the intervention was not clearly defined (to the extent that it could be replicated). In order to meet this requirement, studies must have, where applicable, either:
provided the manufacturing details of the intervention being assessed, if appropriate;
provided pictures or diagrams, if appropriate;
provided a detailed description of the objective properties of the intervention, (e.g. an intervention of colour change needs to describe the specific hue; simply stating 'blue' is not specific enough);
provided a contact from which more detailed information could be sought.
All studies were carried out in a hospital setting. A hospital was defined (Ward 2008) as a health facility that:
provides communal care where there is an expectation that this care is time limited;
provides overnight accommodation;
provides nursing and personal care;
provides for people with illness and disability.
This definition includes hospices.
Studies may have been conducted in any area of the hospital grounds, such as general wards, specialist wards (e.g. Intensive Care Units), waiting rooms, common areas, and gardens.
Types of outcome measures
This review included all validated health‐related patient outcomes reported in the research. Outcomes of interest included validated measures of: anxiety; pain; length of hospital stay; patients' satisfaction; quality of sleep; aggression and mood; physiological outcomes; medication utilisation; hospital‐acquired infections; and mortality. We included a broad range of outcomes since the environment may affect many aspects of a patient's physical and psychological health and different interventions may be applicable to some outcomes and not others. When summarising the results of studies, we have reported up to five relevant outcomes for each comparison and grouped the remaining reported outcomes for that intervention under a heading "other outcomes".
Search methods for identification of studies
Electronic searches
We searched databases covering the fields of health, medicine, psychology and architecture. To identify possible studies, a strategy for MEDLINE was developed using relevant MeSH terms and text words (dates searched 1902 to December 2006; Appendix 1). This strategy was adapted for other databases searched. These included: the Cochrane Central Register of Controlled Trials (CENTRAL; last searched January 2006; Appendix 2); EMBASE (January 1980 to February 2006; Appendix 3); Royal College of Nursing/British Nursing Index (BNI; January 1985 to August 2005; Appendix 4); PsycINFO (January 1806 to December 2006; Appendix 5); Construction and Building Abstracts (CBA; January 1985 to August 2005; Appendix 6); Royal Institute of British Architects (RIBA) library online catalogue (last searched December 2005; Appendix 7); InformeDesign (last searched January 2005; Appendix 8); NHS Estates Knowledge and Information Portal (Architecture in Healthcare Database; complete database searched November 2004); Avery Index to Architectural Periodicals (January 1996 to December 2001; Appendix 9); Cumulative Index to Nursing and Allied Health Literature (CINAHL; January 1982 to August 2005; Appendix 10); Web of Science (January 1970 to January 2006; Appendix 11); Applied Social Sciences Index and Abstracts (ASSIA; January 1987 to December 2004; Appendix 12); UK National Research Register (last searched February 2006; Appendix 13); Architecture Publication Index (January 1978 to March 2002; Appendix 14); Turning Research Into Practice (TRIP) database plus (last searched January 2006; Appendix 15); and Zetoc (The British Library's Electronic Table of Contents; last searched January 2006; Appendix 16). This review is currently being updated (MEDLINE last search October 2010; Appendix 17), see Studies awaiting classification.
Searching other resources
We reviewed reference lists of relevant articles, sourced grey literature from relevant organisations' web pages (e.g. Centre for Health Design, NHS Estates and Facilities Division), and contacted researchers for further information and other potential studies.
Data collection and analysis
Selection of studies
One review author (AD) conducted the initial search (Trials Search Co‐ordinator 'JM' conducted the EMBASE search). The initial search of databases retrieved 78,480 'hits'; these were screened for relevance and the majority of deleted records were double‐checked by a second review author. After screening, 15,140 titles were recorded on the main review database. Two review authors (AD/RS/DW/TD/EG) independently screened the studies obtained from the initial search. Each title was rated as 'hit' (maybe eligible), 'unsure' (probably not eligible) or 'reject' (not to be assessed further). Any disagreement with regard to eligibility was resolved through a third review author and discussion where necessary. We obtained full‐text (English and non‐English) papers for the 'hits' and abstracts for the 'unsures'. All abstracts (2029 total) were assessed independently by two review authors (AD/RS/DW/TD/EG) and rated as 'hit', 'unsure', or 'reject'. We then obtained full‐text papers (524 total) for 'hits' and 'unsures' and these were assessed for inclusion by at least two review authors. We discussed full‐text papers rated as 'unsure' in group meetings. A final corpus of 102 studies was selected for inclusion in the review (see Figure 1 for a flow diagram of the study process).
1.
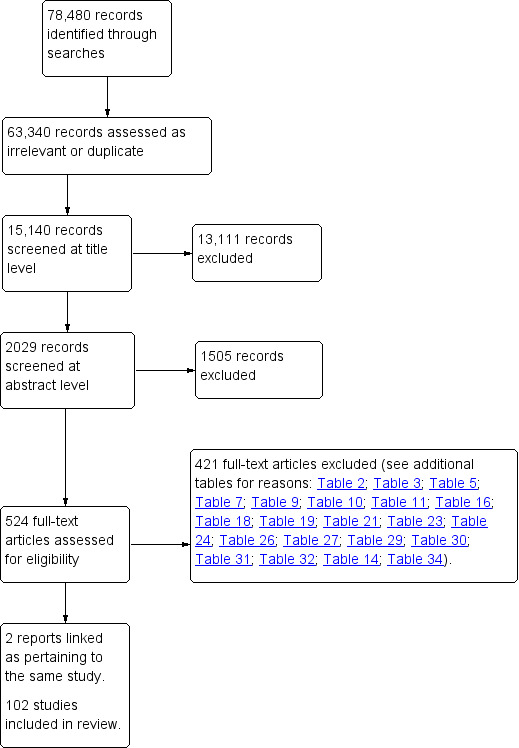
Study flow diagram.
Data extraction and management
Two review authors undertook data extraction independently, using a modified version of the EPOC data collection checklist (AD/DG/HM/RS/DW/TD/EG). Any disagreements were resolved through discussion between review authors.
Assessment of risk of bias in included studies
Retrieved studies were independently evaluated for risk of bias by two review authors (AD/DG/HM/RS/DW/TD/EG), using the criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). For studies where there was difference of opinion a consensus was reached through discussion between review authors.
Data synthesis
The results section is structured alphabetically by intervention (and control) with multi‐intervention studies (e.g. whole ward redesign) being grouped as a separate category. Where appropriate, we have summarised the results of each intervention against different types of control (e.g. other form of environment, standard care) separately; this is because the effectiveness of interventions will vary depending on the comparison, and it may not be appropriate to combine all different types of control group together. Outcomes for individual interventions are looked at in turn and the heterogeneity of the studies explored.
For continuous variables, we calculated a mean difference (MD) for identical measures, or standardized mean difference (SMD), where different techniques were used to measure the same outcome domain, with 95% confidence intervals (CI) for each study. For dichotomous variables, we calculated a risk ratio (RR) with 95% CI. We used sensitivity analyses to explore the influence of risk of bias ('similarities at baseline'; 'sequence generation'; 'concealment of allocation'; 'completeness of data'; and 'blinding of healthcare personnel'), and the influence of deciding to include individual studies that were ambiguous as to whether they met the inclusion criteria.
Where statistical analyses were inappropriate or unfeasible, a discursive account of the results is presented with supporting tables. When it was appropriate to combine the studies, we used a random‐effects model of meta‐analysis. We have presented continuous data that were reported using medians and ranges in tables only.
Subgroup analysis and investigation of heterogeneity
We identified the presence of statistical heterogeneity by visually examining the forest plots, and using the I2 test for heterogeneity (where it was considered that: 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; 75% to 100% represents considerable heterogeneity). The importance of the observed value of I2 was evaluated in conjunction with (i) magnitude and direction of effects and (ii) strength of evidence for heterogeneity (i.e. P value from the Chi2 test). We explored heterogeneity qualitatively (based on the characteristics listed below), and with subgroup analyses (where appropriate).
Heterogeneity was explored based on:
case mix (reason for hospitalisation; psychiatric/non‐psychiatric);
hospital visit characteristics (in‐patient/out‐patient/day‐patient; area of hospital studied);
geography (countries in which studies were undertaken).
To aid interpretation, we have presented the findings for anxiety from studies on music in subgroups (this decision was made post‐hoc and is based on the following rationale); Given the temporal dependence of anxiety as a transitional state (Spielberger 1983), the studies have been grouped according to the methodological criteria of when the musical intervention was provided, i.e. according to whether music was provided in the waiting period prior to a medical procedure (and hence the outcome of anxiety was obtained after the music intervention but before the medical procedure), or if music was provided throughout a medical procedure (anxiety was measured after both the music and medical procedure), or music was provided in the post‐operative period, or in an intensive care environment. We have displayed Chi2 tests assessing subgroup differences where appropriate (i.e. when the data presented in each subgroup is independent).
Results
Description of studies
Overall, 102 studies have been included in this review; one study was published twice on the same population but with different outcomes reported (Barnason 1995/1996) and two studies (Barnason 1995/1996 ; Lembo 1998) explored more than one type of intervention. Environmental interventions explored were: those that provided positive distracters to complement healthcare treatment already being administered, to include aromas (two studies), audiovisual distractions (five studies), decoration (one study), music (85 studies); those that reduced environmental stressors by implementing physical changes, to include studies on air quality (three studies), bedroom type (one study), flooring (two studies), furniture and furnishings (one study), lighting (one study), and temperature (one study);and multifaceted interventions (two studies). No studies meeting the inclusion criteria were found to evaluate: art, access to nature for example through hospital gardens, atriums, flowers, and plants, ceilings, interventions to reduce hospital noise, patient controls, technologies, way‐finding aids, or the provision of windows.
Studies awaiting assessment
We have two studies published in Korean, which we have not yet been able to assess due to translation difficulties (Hur 2005; Son 2006), one ongoing study (Characteristics of ongoing studies), and a further 66 studies awaiting assessment which are part of an ongoing update of this review (Studies awaiting classification).
Risk of bias in included studies
A summary of risk of bias judgements for all studies can be seen in Figure 2. A narrative description for each intervention type is given below.
2.
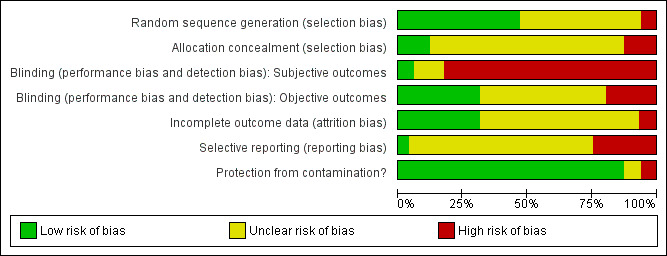
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Effects of interventions
Providing positive distracters
Aromas
Description of studies on aromas:
One RCT (Graham 2003) and one CCT (Holmes 2002) have been included on the use of aromas in the hospital (Table 1). These studies investigated the use of aromas in 328 patients overall; in Graham 2003 it is unclear how many participants there are per group, and Holmes 2002 is a cross‐over trial of 15 psychiatric patients. The overall mean age was 65.64 years old, with 169 males and 159 females included in the studies. Studies were conducted in Australia and England. Patient groups assessed were those undergoing radiotherapy treatment, and psychiatric in‐patients in a psychogeriatric ward.
1. Aromas: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes |
| Graham 2003 | RCT; 3 parallel groups. | DESCRIPTION: 313 patients undergoing radiotherapy, in Australia. NUMBERS: Unclear how many patients per group. AGE, mean (range): 65 (33‐90) years old. GENDER (male/female): 163/150. ETHNICITY: not described. INCLUSION CRITERIA: If a course of eight or more fractions of radiotherapy was prescribed. EXCLUSION CRITERIA: not described. | FRAGRANT PLACEBO: Patients were administered the carrier oil with low‐grade essential oils. The carrier oil was sweet almond cold‐pressed pure vegetable oil. The low‐grade fractionated oils (lavender, bergamot, and cedarwood) were of unknown purity (supplied by Naturistics, Hornsby, Australia). These fractionated oils were diluted with the carrier oil in a ratio of 1:2. NON‐FRAGRANT PLACEBO: Patients were administered the carrier oil only: sweet almond cold‐pressed pure vegetable oil. PURE ESSENTIAL OIL: 100% pure essential oils of lavender, bergamot, and cedarwood were administered in a ratio of 2:1:1 (supplied by "In Essence"). All patients were administered their study treatment via a necklace with a plastic‐backed paper bib, donned before radiotherapy treatment each day and removed after exiting the treatment bunker. Three drops of oil were applied to the bib. Typical duration lasted 15‐20 minutes. Patients were seated in waiting areas segregated according to study arm allocation to avoid cross‐exposure. | ANXIETY, DEPRESSION, and FATIGUE: Measured via the Hospital Anxiety and Depression Scale (HADS), and the Somatic and Psychological Health Report (SPHERE), which is composed of the General Health Questionnaire (GHQ) and Symptoms of Fatigue and Anergia (SOFA) scales. In a multivariate analysis: There were significantly fewer patients with anxiety >7 in the non‐fragrant placebo arm than both the essential oil (Odds ratio = 2.6, 95% CI = 1.1 to 6.1), and fragrant placebo (Odds ratio = 2.8, 95% CI = 1.1 to 6.7) groups. There were no significant differences between groups in depression scores, the General Health Questionnaire, and fatigue scale. |
| Holmes 2002 | CCT; Cross‐over trial, 2 conditions. | DESCRIPTION: 15 psychiatric inpatients in the communal area of a long‐stay hospital psychogeriatric ward for patients with behavioural problems, in England. NUMBERS: 15 patients; cross‐over trial. AGE, mean (SD): 79.0 (6.3) years old. GENDER (male/female): 6/9. ETHNICITY: not described. INCLUSION CRITERIA: International classification of disease (ICD)‐10 diagnostic criteria for severe dementia; evidence of agitated behaviour‐ defined as scoring > 3 on the Pittsburgh Agitation Scale at some point each day over the period of a week. EXCLUSION CRITERIA: none described. | LAVENDER: The communal area of the unit was diffused with a standard concentration of lavender oil (2%), using three aroma‐streams for a period of two hours between the period of 4pm and 6pm. PLACEBO: The communal area of the unit was diffused with water, using three aroma‐streams for a period of two hours between the period of 4pm and 6pm. A total of five treatments and five placebo trials were carried out for each patient over a period of two weeks. | AGITATION: Measured on the 16‐point Pittsburgh Agitation Scale by a blinded observer for the final hour of each two hour study period. Outcomes are presented as median scores for each patient in each condition. 9 patients showed an improvement with lavender. 5 patients showed no change with lavender. 1 patient showed a worsening of condition with lavender. Wilcoxon Signed‐Ranks test, P = 0.016 Of the 4 patients with Alzheimer's disease, 3 improved and 1 showed no change; of the 7 patients with vascular dementia, 5 improved and 2 showed no change; of the 3 patients with Dementia with Lewy Bodies, 2 showed no change and 1 worsened; the 1 patient with Fronto‐temporal lobe dementia improved. |
SD: standard deviation
Fragrances were administered via a necklace with a plastic‐backed paper bib (Graham 2003) and an aroma‐stream in the communal area (Holmes 2002). One study had three comparison groups (Graham 2003). Fragrances evaluated were: low‐grade fractionated oils (combination of lavender, bergamot, and cedarwood, diluted with a carrier oil), 100% pure essential oil (combination of lavender, bergamot, and cedarwood), and lavender oil (2%). Control conditions were: sweet almond cold‐pressed pure vegetable oil only; and water.
Outcomes assessed were: anxiety, depression, fatigue, and agitation.
We have tabulated 15 excluded studies (Table 2).
2. Aromas: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Anderson 2004 | Intervention |
| Burns 2000a | Study design |
| Burns 2000b | Study design |
| Burns 2002 | Study design |
| Bykov 2003a | Setting and population |
| Girard 2004 | Editorial |
| Hudson 1995 | Study design |
| Hudson 1996 | Outcomes |
| Itai 2000 | Study design |
| Kane 2004 | Data unsuitable for cross‐over study |
| Kirkpatrick 1998 | Commentary |
| Lehrner 2000 | Setting |
| Louis 2002 | Setting |
| Redd 1994 | Aromas administered via nasal cannula, judged to be too invasive to constitute an 'environmental' intervention. |
| Tate 1997 | Intervention; outcome not validated |
Risk of bias in included studies on aromas:
One RCT and one CCT were included on hospital aromas. Methods of group assignment were via telephone contact to a data management centre (Graham 2003; adequacy unclear), and alternate days (Holmes 2002). Concealment of allocation is adequate in Graham 2003. Blinding (of patients, physicians, and outcome assessment) was attempted in Graham 2003. In this study 9% of patients in the non‐fragrant placebo group believed they had received pure essential oil, 25% in the fragrant placebo group believed they had received pure essential oil, and 24% in the pure essential oil group believed they had received the pure essential oil. Holmes 2002 blinded the outcome assessor to study group (through the use of nose callipers), although in this study it was not feasible to blind patients to the scent on the ward. Completeness of outcome data was satisfactory in the studies (> 80% complete). Graham 2003 did not report withdrawals and drop‐outs, and in Holmes 2002 there were no withdrawals. It is unclear whether or not there is selective outcome reporting in either study. Protection against contamination could not be achieved in Holmes 2002 as this was a cross‐over trial, however, for the other study, this was not a problem.
Findings from studies on aromas:
Anxiety
One study on patients undergoing radiotherapy treatment, measured the outcome anxiety on the Hospital Anxiety and Depression (HAD) scale (Graham 2003). Graham 2003 reports a multivariate analysis, in which there were significantly fewer anxious patients (cases were classified as anxious when scoring > 7) in the non‐fragrant placebo group (13%), than in both the essential oil group (25%), odds ratio (OR) = 2.6 (95% confidence interval (CI) 1.1 to 6.1), and fragrant placebo group (23%), OR = 2.8 (95% CI 1.1 to 6.7).
Other outcomes
Graham 2003 found no strong evidence of effects for depression, fatigue, and general health (data insufficient for extraction) between any of the three groups.
Findings from non‐randomised studies:
Holmes 2002 investigated agitation using the Pittsburgh Agitation Scale (PAS) in a psychogeriatric ward communal area (N = 15, cross‐over study) and reports a significant effect (Wilcoxon Signed‐Ranks test P value 0.016) in favour of the lavender oil aroma‐stream group (median PAS score = 3, range = 1 to 7) versus diffused water (median PAS score = 4, range 3 to 7).
Art
Description of studies on art:
No studies have been included on the use of art in hospital. We have tabulated 16 excluded studies (Table 3).
3. Art: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Bower 1995 | Qualitative report |
| Breslow 1993 | Descriptive article |
| De Jong 1972 | Participants |
| Finkelstein 1971 | Intervention interactive |
| Finlay 1993 | Qualitative report |
| Green 1994 | News article |
| Guillemin 2000 | Qualitative |
| Homicki 2004 | Descriptive article |
| Litch 2006 | Narrative article |
| Mellor 2001 | Commentary |
| Palmer 1999 | No group comparisons presented, unable to obtain further details from authors |
| Staricoff 2001 | Study design |
| Staricoff 2003a | Study design (part of same study as Staricoff 2001) |
| Ulrich 1993b | Conference abstract, unable to obtain further details from author |
| Wikström 1992 | Setting |
| Wikström 1993 | Setting |
Audiovisual distractions
Description of studies on audiovisual distractions:
Five RCTs were conducted on audiovisual distractions (Table 4; NB. two articles report on Barnason 1995/1996; although the articles report differently on the choices of audiovisual distractions made available to the intervention group, the patient demographics and study designs are identical). These studies result in a total sample of 387 participants (Audiovisual group = 144, Control group = 243). Included patients had a mean age of 53.92 years old (range = 18 to 90), with 231 males and 156 females. Four studies were conducted in the USA and one was conducted in China. Three studies were carried out during endoscopy interventions, one was conducted during dressing changes for burns, and one during the post‐operative period.
4. Audiovisual: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Barnason 1995/1996 | RCT; 3 parallel groups. | DESCRIPTION: 96 in‐patients in the cardiovascular ICU and progressive care units having undergone elective coronary artery bypass grafting, in USA. NUMBERS: Music group = 33, Music + video group = 29, Scheduled rest group = 34. AGE, mean (SD): 67 (9.9) years old. GENDER (male/female): 65/31. ETHNICITY: White = 96 (100%) INCLUSION CRITERIA: Orientated to person, time and place; speak and read English; 19 years or older; extubated within 12 hours of surgery; removal of intra‐aortic balloon pump within 12 hours of surgery. EXCLUSION CRITERIA: Currently using one of the intervention techniques; major hearing deficit. | MUSIC GROUP: Choice of 5 tapes: 'Country Western Instrumental' or 'Fresh Aire' by Mannheim Steamroller, 'Winter into Spring' by George Winston, or 'Prelude' or 'Comfort Zone' by Steven Halpern. Played via headphones for 30 minutes. MUSIC + VIDEO GROUP: Barnason 1995 states: Choice of 2 Steven Halpern tapes: 'Summer Wind' or 'Crystal Suite'. Each is 30 minutes of soft instrumental with visual imaging. Zimmerman 1996 states: Choice of three 30 minute videocassettes by Pioneer Artist ('Water's Path', 'Western Light', or 'Winter'). SCHEDULED REST: 30 minutes of rest in bed or chair, visitors and staff requested not to disturb. 2 x 30 min intervention periods during afternoons of post‐operative days 2 and 3. Lights dimmed. | Barnason 1995 reports: STATE ANXIETY: measured using STAI at three time‐points: pre‐operatively, before intervention on 2nd post‐operative day, and after intervention on 3rd post‐operative day. ANXIETY: taken using NRS before and after each intervention session. PHYSIOLOGICAL: HR (bpm) and BP (mm Hg) taken using the Kendall BP Monitor (Model 8200)‐ not enough data presented for extraction. MOOD: Measured using a NRS‐ not a validated outcome. Zimmerman 1996 reports: PAIN: Pain was measured with a 10‐point VRS before and after each session, and with the McGill Pain Questionnaire (scores are given for the subscales and the present pain index rating scale) administered once prior to the first session, and once after the second session. SLEEP: Measured with the Richards‐Campbell Sleep Questionnaire (RSQ), administered between 7am and 9am on the third post‐operative day. | Data extracted for state anxiety (STAI measure). Pain data are extracted for the end values on the VRS. Patients in the music group showed a significant improvement in mood after the 2nd intervention when controlling for pre‐intervention mood rating. No differences between groups were found for anxiety on either data collection tool. Physiological measures did not differ between groups, however there were significant differences over time (regardless of group), indicating a generalised relaxation response. Authors conclude that although no intervention was overwhelmingly superior, all groups demonstrated a relaxation response. |
| Diette 2003 | RCT; 2 parallel groups. | DESCRIPTION: 80 in‐patients and out‐patients undergoing FB in Mariland, USA. NUMBERS: Bedscapes group = 41, Control = 39 patients. AGE, mean (range): Bedscapes = 52.3 (21‐88); Control = 55.3 (30‐90). GENDER (Male/Female): Bedscapes = 16/25; Control = 22/17. ETHNICITY (White/African‐American): Bedscapes = 25/16; Control = 28/11. INCLUSION CRITERIA: 18 years or older, undergoing FB. EXCLUSION CRITERIA: Non‐English speaker, contact isolation, presence of encephalopathy or significant alteration in mental status, sensory deficits that preclude use of visual/auditory aid. | BEDSCAPES GROUP: Countryside river scene with associated sounds of nature played through headphones. Intervention available before, during, and after FB procedure. The scene was mounted by the bedside in the recovery area and on the ceiling in the procedure room. CONTROL GROUP: standard care. | ANXIETY: State anxiety via STAI; PAIN: Pain control during procedure measured by VRS. Values presented as % with good/excellent pain control. Due to unclear missing data (> 10%), it is unclear how many people this represents. ABILITY TO BREATHE: (poor to excellent) rating scale. Validity unclear. SATISFACTION WITH CARE: Ratings of: willingness to return, privacy, safety, overall rating of facility. Validity unclear. Outcomes obtained via a follow‐up survey administered on the second day following the procedure. Out‐patients completed form and returned it by mail. In‐patients forms were collected from their hospital room. | SDs for anxiety have been estimated from P value of a t‐test. Adverse events: 1 patient in the treatment group urinated on the bronchoscopy table. The patient felt that this had occurred because of hearing sounds of running water. |
| Lee 2004a | RCT; 3 parallel groups. | DESCRIPTION: 157 day‐patients undergoing colonoscopy in an Endoscopy Suite in Hong Kong, China. NUMBERS: Visual distraction = 52 patients, Audiovisual distraction = 52 patients, Control group = 53 patients. AGE, mean (SD): Visual distraction = 45.6 (10.2), Audiovisual distraction = 48.8 (11.3), Control group = 46.3 (11.4). GENDER (male/female): Visual distraction = 25/27, Audiovisual = 27/25, Control group = 23/30. ETHNICITY: not described. INCLUSION CRITERIA: Undergoing elective day‐case colonoscopy. EXCLUSION CRITERIA: History of allergy to propofol and/or alfentanil. Receive a colectomy. | VISUAL DISTRACTION: Eyetreck system (olympus) with preset home made movie (mainly scenic views), patient wears earphones but with no sound. AUDIOVISUAL DISTRACTION: Same as visual distraction with the addition of classical music played through earphones. CONTROL: Standard care. All groups received PCS using a mixture of propofol and alfentanil. | PAIN: scored using 10 cm VAS; SATISFACTION: measured using 10 cm VAS; Willingness to repeat procedure (using 10 cm VAS); ANALGESICS: Dose of PCS consumed; PHYSIOLOGICAL: Hypotensive episodes; Oxygen desaturation; RECOVERY TIME: nurse assessed | |
| Lembo 1998 | RCT; 3 parallel groups. | DESCRIPTION: 37 patients undergoing flexible sigmoidoscopy in Calfornia, USA. NUMBERS: Audiovisual group = 13, audio alone group = 12, control group = 12. AGE, mean (SD): Audiovisual group = 58 (7), Audio alone group = 60 (8), Control group = 59 (7) years old. GENDER: Male = 37 (100%). ETHNICITY: not described. INCLUSION CRITERIA: Undergoing routine screening flexible sigmoidoscopy. EXCLUSION CRITERIA: none described. | AUDIOVISUAL: Virtual‐i glasses, personal display system showing an ocean shoreline with corresponding sounds (via headphones) AUDIO ALONE: Sounds of the ocean shoreline only played via headphones. CONTROL: No intervention, standard care. | DISCOMFORT: Measured via VAS which asked patients to rate their level of abdominal discomfort from faint to severly intense. STRESS SYMPTOMS: Measured 6 subscales (arousal, stress, anxiety, anger, fatigue, and attention) using 12 VAS. | Data for discomfort entered as pain scores. Data extracted for review on anxiety and anger. Arousal and attention not considered health‐related outcomes. There was no difference between groups on the stress and fatigue subscales, data not reported for extraction. |
| Miller 1992 | RCT; 2 parallel groups. | DESCRIPTION: 17 in‐patients undergoing burns care treatment and dressings change in a Burn Special Care Unit, Cincinnati, USA. NUMBERS: Audiovisual group = 9, Control group = 8. AGE, mean: Audiovisual group = 40.9, Control group = 27.8 GENDER (male/female): Audiovisual group = 9/0, Control group = 7/1. ETHNICITY (white/black): Audiovisual group = 8/1, Control group = 7/1. INCLUSION CRITERIA: 10‐40% body surface burn; expected length of stay >/= 1 week; Adult patients, 18 years or older. EXCLUSION CRITERIA: Substance abuse disorder; unable to see/or hear; psychotic; under 18 years old; cannot understand English; mentally retarded; disorientated; multiple trauma injuries. | AUDIOVISUAL GROUP: "Muralvision" (Muralvision Studios, Inc., Eugene, Ore.)‐ on a bedside television, video programmes composed of scenic beauty (ocean, desert, forest, flowers, waterfalls, and wildlife) with accompanying music. CONTROL GROUP: Standard care. Participants were exposed to their treatment group on 10 occasions during dressing change. | PAIN: Measured via the McGill Pain Questionnaire, with the Pain Rating Index and Present Pain Intensity scales. ANXIETY: Measured via the STAI. Outcomes were measured within 2 minutes at the end of each dressing change. Outcomes are reported as the overall means and standard errors for the 10 dressing changes. | For data extraction in the review, change scores from baseline were calculated and associated estimated standard deviations, using the F statistics provided. |
SD: standard deviation; STAI: State Trait Anxiety Inventory; VAS: visual analogue scale
Audiovisual interventions were all nature‐based, with Diette 2003 consisting of a static "photomural" of nature and the remaining being video‐based (Lee 2004a and Lembo 1998 used video eye glasses, and Barnason 1995/1996 and Miller 1992 used a bedside television). Diette 2003 and Lembo 1998 played nature sounds which corresponded to the visual distraction, and Barnason 1995/1996, Lee 2004a, and Miller 1992 played accompanying music. Three studies had more than one control group. Control groups consisted of: standard care alone (N = 4; Diette 2003; Lee 2004a; Lembo 1998; Miller 1992), visual distraction alone (N = 1; Lee 2004a), audio distraction alone (N = 2; Barnason 1995/1996; Lembo 1998), and scheduled rest (N = 1; Barnason 1995/1996).
Outcomes investigated were: Anxiety (N = 4), patient‐reported pain (N = 5), heart rate (N = 1), blood pressure (N = 1), sedation medication requirement (N = 1), sleep (N = 1), satisfaction (N = 1), hypotensive episodes (N = 1), oxygen desaturation (N = 1), recovery time (N =1), anger (N =1), stress (N = 1), and fatigue (N = 1).
We have tabulated 16 excluded studies on audiovisual distractions (Table 5).
5. Audiovisual: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Allen 1989 | Intervention |
| Egger 1981 | Study design |
| Friedman 1992 | Study design |
| Hoffman 2000 | Intervention‐ interactive virtual reality |
| Hoffman 2001 | Intervention‐ interactive virtual reality |
| Holden 1992 | Intervention‐ patient education video |
| Martin 1999 | Inadequate information provided (Ulrich study) |
| Oyama 2000 | Intervention interactive |
| Pruyn 1998 | Unclear validity of outcomes |
| Schneider 2003 | Intervention interactive |
| Schneider 2004 | Intervention interactive |
| Schofield 2000 | Intervention‐ snoezelen |
| Singer 2000 | Population, < 90% over 18 years old. |
| Tse 2003 | Setting |
| Ulrich 2003 | Setting |
| Wint 2002 | Participants not adults |
Below, we summarise findings for the following comparisons:
Audiovisual distraction versus audio distraction (music)
Audiovisual distraction versus scheduled rest
Audiovisual distraction versus standard care alone
Audiovisual distraction versus visual distraction
Visual distraction versus standard care alone
Risk of bias in included studies on audiovisual distractions:
Five RCTs were included on audiovisual distractions. For Lembo 1998 and Miller 1992, the method of randomisation is unclear; Lee 2004a allocated patients via a computer‐generated list; Barnason 1995/1996 drew lots; and Diette 2003 allocated patients according to clinic day (which was randomised to intervention and control). Of the five included studies, it is unclear if concealment of allocation was used in four studies, and it was not used in one (Barnason 1995/1996 ). Lee 2004a reports blinding of recovery nurses (who assessed some outcomes) to patient allocation, and blinding of the endoscopists to two patient groups (but not to the standard care group). In the remaining studies blinding of healthcare personnel was not possible. Only Lee 2004a was judged to address incomplete outcome data, and the others remain unclear. Lee 2004a reported withdrawals and drop‐outs (eight patients; unclear from which groups), the reasons for which appear unrelated to the interventions, and Barnason 1995/1996 reports that all participants completed the study. Barnason 1995/1996 and Diette 2003 have been judged to be at risk of selective outcome reporting, whilst the remaining studies are unclear. All studies offered protection against contamination.
Findings from studies on audiovisual distraction versus audio distraction (music):
Anxiety
Two studies (Barnason 1995/1996; Lembo 1998) reported on the outcome anxiety (audiovisual group = 42, audio group = 45). Although both studies showed no strong evidence that the intervention had an effect (both individually and when combined: standardised mean difference (SMD) −0.24, 95% CI −1.05 to 0.56, P Value = 0.55), when combined they demonstrate moderate statistical heterogeneity (I2 = 65.6%, Chi2 = 2.91, df = 1, P value = 0.09; Analysis 1.1).
1.1. Analysis.
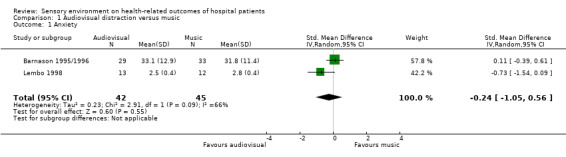
Comparison 1 Audiovisual distraction versus music, Outcome 1 Anxiety.
Exploring the heterogeneity of studies on anxiety:
With only two studies, it is difficult to explore the reasons for heterogeneity in terms of methodological and clinical differences. Both studies are subject to risk of bias; neither study had adequate allocation concealment and in Barnason 1995/1996 allocation concealment was not used. Additionally, Lembo 1998 was a very small study with no power calculation. Both studies were conducted in the USA and used video visual images. Barnason 1995/1996 was conducted on post‐operative patients and Lembo 1998 was conducted on patients undergoing an endoscopic procedure.
Pain
Two studies (Barnason 1995/1996; Lembo 1998) reported on the outcome pain (audiovisual group = 42, audio group = 45). With one small study (N = 25) in favour of audiovisual distraction (Lembo 1998: SMD −1.72, 95% CI −2.66 to −0.78), and the other (N = 62) showing no strong evidence that the intervention had an effect (Barnason 1995/1996: SMD 0.20, 95% CI −0.30 to 0.70), the studies combine with considerable statistical heterogeneity (I2 = 92%; Analysis 1.2), so we have not pooled these studies in a meta‐analysis.
1.2. Analysis.
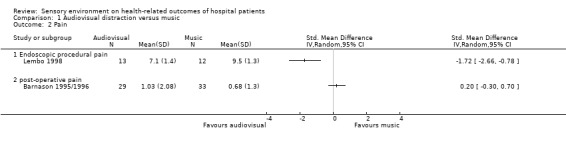
Comparison 1 Audiovisual distraction versus music, Outcome 2 Pain.
Exploring the heterogeneity of studies on pain:
The comparison of Barnason 1995/1996 with Lembo 1998 has already been assessed for the outcome anxiety above.
Heart rate
Studies with insufficient data for extraction:
One study (Barnason 1995/1996; audiovisual N = 29, music N = 33) collected data on heart rate and reported that there was no strong evidence that the intervention had an effect.
Blood pressure
Studies with insufficient data for extraction:
One study (Barnason 1995/1996; audiovisual N = 29, music N = 33) collected data on blood pressure and reported that there was no strong evidence that the intervention had an effect.
Other outcomes
Lembo 1998 additionally reported on anger and fatigue (data insufficient for extraction). This study (audiovisual group = 13, audio group = 12) found the audiovisual group to have significantly lower anger scores (mean difference (MD) −0.40 points on a 10‐point visual analogue scale (VAS), 95% CI −0.68 to −0.12, P value = 0.005) and no difference in fatigue ratings. Barnason 1995/1996 (audiovisual = 29, music = 33) collected data on sleep quality to find no strong evidence that the intervention had an effect (MD 0.40 on the Richards‐Campbell Sleep Questionnaire, 95% CI −0.71 to 1.51, P value = 0.48).
Findings from studies on audiovisual distraction versus scheduled rest:
Anxiety
One study (Barnason 1995/1996) reported on anxiety (audiovisual group N = 29, scheduled rest N = 34) and found no strong evidence for an intervention effect (MD −1.60 points on the State Trait Anxiety Inventory (STAI), 95% CI −8.74 to 5.54, P value = 0.66).
Pain
One study (Barnason 1995/1996) reported on pain (audiovisual group N = 29, scheduled rest group N = 34) and found no strong evidence for an intervention effect (MD 0.15 points on a 10 point verbal rating scale (VRS), 95% CI −0.82 to 1.12, P value = 0.76).
Heart rate
Studies with insufficient data for extraction:
One study (Barnason 1995/1996; audiovisual N = 29, scheduled rest N = 34) collected data on heart rate and found no strong evidence for an intervention effect.
Blood pressure
Studies with insufficient data for extraction:
One study (Barnason 1995/1996; audiovisual N = 29, scheduled rest N = 34) collected data on blood pressure and found no strong evidence for an intervention effect.
Other outcomes
One study (Barnason 1995/1996 reported on sleep quality (audiovisual group N = 29, scheduled rest group N = 34) and found scores to significantly favour the audiovisual group (MD 1.57 on the Richards‐Campbell Sleep Questionnaire, 95% CI 0.47 to 2.67, P value = 0.005).
Findings from studies on audiovisual distraction versus standard care alone:
Anxiety
Three studies reported on anxiety (audiovisual group = 63, standard care group = 59). The largest of these studies (Diette 2003; N = 80) showed no strong evidence that the intervention had an effect, whilst the smaller two studies (Lembo 1998; Miller 1992) have significant findings favouring audiovisual distraction. When combined these studies show considerable statistical heterogeneity (I2 = 93%; Analysis 2.1) so we have not pooled these studies in a meta‐analysis.
2.1. Analysis.
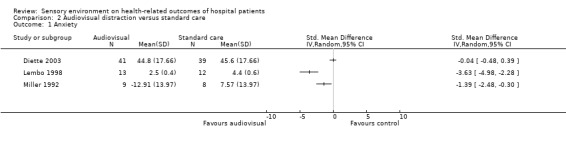
Comparison 2 Audiovisual distraction versus standard care, Outcome 1 Anxiety.
Exploring the heterogeneity of studies on anxiety:
With few studies it is difficult to explore reasons for heterogeneity. All three studies are subject to risk of bias with unclear allocation concealment. Other than the size and quality of the individual studies, a further explanation for the differences in findings could be that the intervention Diette 2003 utilised was a static picture, whereas the other studies utilised video. All studies were conducted in the USA, with two (Diette 2003; Lembo 1998) being conducted on endoscopy patients and the other being conducted on patients undergoing burns dressing changes.
Pain
Three studies (Lee 2004a; Lembo 1998; Miller 1992) reported sufficient information for extraction on pain (Analysis 2.2). Although all three studies were significantly in favour of audiovisual distraction for pain relief, there is considerable heterogeneity between study effect estimates (I2 = 93%), therefore we have not pooled these studies in a meta‐analysis.
2.2. Analysis.
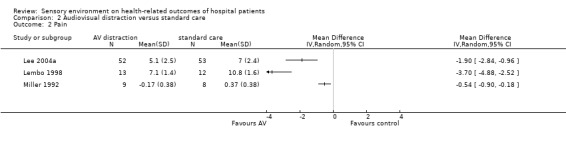
Comparison 2 Audiovisual distraction versus standard care, Outcome 2 Pain.
Exploring the heterogeneity of studies on pain:
With few studies it is difficult to explore reasons for heterogeneity. All three studies are subject to risk of bias, with unclear allocation concealment. All three studies used a video audiovisual distraction. Two were conducted in patients undergoing an endoscopic procedure and one (Miller 1992) was conducted during burns dressing changes. Two were conducted in the USA and one (Lee 2004a) was conducted in China.
Studies with insufficient data for extraction:
Diette 2003 also reported on pain scores; this study, which used static pictures also found a significant effect for pain in favour of patients who received an audiovisual distraction.
Sedation medication requirements
Lee 2004a reported on propofol requirement in patients undergoing an endoscopy procedure in China. This study found that those who received an audiovisual distraction (N = 52) required significantly less sedation medication than those who received standard care (N = 53), MD −0.37 mg/kg (95% CI −0.58 to −0.16, P value = 0.0005).
Other outcomes
Other health‐related outcomes reported were recovery time (Lee 2004a), oxygen desaturation episodes (Lee 2004a), hypotensive episodes (Lee 2004a), satisfaction (Lee 2004a), anger (Lembo 1998), and fatigue (Lembo 1998). Outcomes (each from just one study) favouring audiovisual distraction were anger (MD −2.20 cm on a 10 cm VAS, 95% CI −2.63 to −1.77, P value < 0.00001) and satisfaction (MD 2.30 cm on a 10 cm VAS, 95% CI 1.28 to 3.32, P value < 0.00001). There is no strong evidence of an intervention effect for recovery time, oxygen desaturation episodes, hypotensive episodes, or fatigue.
Findings from studies on audiovisual distraction versus visual distraction:
Pain
Lee 2004a found that audiovisual distraction (N = 52) is significantly better than visual distraction alone (N = 52) at reducing patient‐reported pain (MD −1.10 cm on a 10 cm VAS, 95% CI −2.01 to −0.19, P value = 0.02).
Sedation medication requirements
Lee 2004a found that audiovisual distraction (N = 52) is significantly better than visual distraction alone (N = 52) at reducing sedation medication requirements (MD −0.36 mg/kg, 95% CI −0.62 to −0.10, P value = 0.006).
Other outcomes
Lee 2004a also reported on recovery time, satisfaction, episodes of oxygen desaturation, and episodes of hypertension. For these outcomes there is no strong evidence that audiovisual distraction was more effective than visual distraction alone.
Findings from studies on visual distraction versus standard care alone:
Pain
Lee 2004a found no significant difference for patient‐reported pain (MD −0.80 cm on a 10 cm VAS, 95% CI −1.68 to 0.08, P value = 0.07) between a visual distraction group (N = 52) and standard care (N = 53).
Sedation medication requirements
Lee 2004a found no significant difference for sedation medication (propofol) requirements (MD −0.01 mg/kg, 95% CI −0.28 to 0.26, P value = 0.94) between a visual distraction group (N = 52) and standard care (N = 53).
Other outcomes
Lee 2004a found that patients allocated to a visual distraction group (N = 52) were significantly more satisfied (MD 2.10 cm on a 10 cm VAS, 95% CI 1.08 to 3.12, P value < 0.0001) than those allocated to standard care (N = 53).
Decoration
Description of studies on decoration:
One RCT on hospital décor has been included in the review (Table 6; Edge 2003). In this study there were 39 participants overall; 13 patients were assigned to beige rooms, 10 to purple, nine to green, and seven to orange. In Edge 2003 participants' ages ranged from 26 to 89 years old (average unknown), with 20 males and 19 females. The study was conducted in the USA on patients in a cardiac care unit.
6. Decoration: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Edge 2003 | RCT; 4 parallel groups. | DESCRIPTION: 39 in‐patients (10 post‐operative for cardiac surgery, 29 undergoing cardiac observations) in a cardiac care unit in Florida, USA. NUMBERS: Beige = 13, Purple = 10, Green = 9, Orange = 7. AGE: 26 to 89 years old. GENDER (male/female): 20/19. ETHNICITY: not described. INCLUSION CRITERIA: Admitted to unit between February and March 2003. EXCLUSION CRITERIA: Colour blind; non‐English speaking; not able to understand or confused. | BEIGE: Walls remained original colour of beige (similar to Sherwin Williams colour SW6658) in four rooms. PURPLE: Wall at foot of bed painted purple (SW6556) in two rooms. GREEN: Wall at foot of bed painted green (SW6451) in two rooms. ORANGE: Wall at foot of bed painted orange (SW6346) in two rooms. Otherwise rooms were of same decor and intervention colours were co‐ordinated with colours already present in the rooms (e.g. on bed curtains). Artwork was removed from the rooms. Rooms were double occupancy with western outlook. Curtains were combination of orange, yellow, green, blue, and purple. Laminate countertops were green, and floors were orange and green. Furniture was neutral shades of white, grey, or beech wood. | ANXIETY: Measured via STAI on day of discharge (after 2 to 5 days in hospital). Presented as mean (SD). No significant differences reported. LENGTH OF STAY: Extracted from patient notes by researcher (days). No SDs presented. No significant differences reported. PAIN MEDICATION REQUESTS: Extracted from patient notes by researcher. Presented as number of patients making requests and number of requests made (no SDs presented), subgrouped by first day, middle days, and final day. No significant differences reported. | Partients in this study were not approached for informed consent until Day 3 of the study. |
STAI: State Trait Anxiety Inventory
The intervention colours were painted on to one wall at the foot of the patient beds, and were colour co‐ordinated with the rest of the room (e.g. with the colours in the curtains). Colour descriptors were: beige (original room colour, similar to Sherwin Williams colour SW6658), purple (SW6556), green (SW6451), and orange (SW6346).
Health‐related outcomes assessed were: anxiety, pain medication requests, and length of stay.
Twelve excluded studies have been tabulated on decoration (Table 7).
7. Decoration: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Becker 1980 | Outcomes not validated |
| Cooper 1989 | Qualitative report |
| Dickinson 1995 | Setting |
| Hewawasam 1996 | Study design |
| Hussian 1987 | Study design |
| Jacobs 1974 | Participants |
| Knobel 1985 | Descriptive article |
| Namazi 1989 | Study design |
| Rabin 1981 | Descriptive article |
| Rice 1980 | Outcomes |
| Steer 1975 | Counfounding |
| Steffes 1985 | Staffing confound |
Risk of bias in included studies on decoration:
In the one RCT (Edge 2003) on decoration, participants were randomly assigned by administrative staff, but the method is unclear, and concealment of allocation was not used. Blinding of group allocation was not possible. Length of stay and pain medication requests were obtained from patient records, and subjective anxiety assessment was not blinded. The study is small, but of the consenting participants completeness of data was achieved. The author does give a description of withdrawals, drop‐outs, and non‐consenting patients (participants were approached for consent after allocation). Overall 11 patients were not included in the study for reasons seemingly unrelated to the intervention (Table 6), and one of whom was withdrawn by the researcher because she felt the patient was falsely answering the questions on anxiety (because the patient feared that high anxiety would affect her length of stay). This study is at risk of selective outcome reporting. It is likely that there was adequate protection against contamination.
Findings from studies on decoration:
Anxiety
Studies with insufficient data for extraction:
Edge 2003 found no strong evidence of an effect between groups for the outcome anxiety.
Pain medication requests
Studies with insufficient data for extraction:
Edge 2003 found no strong evidence of an effect between groups for the outcome pain medication requests.
Length of stay
Studies with insufficient data for extraction:
Edge 2003 found no strong evidence of an effect between groups for the outcome length of stay.
Music
Description of studies on music:
The 85 included RCTs investigating music (Table 8), resulted in a total sample of 6061 patients. Including two cross‐over trials (of 24 and 20 participants respectively; Davis‐Rollans 1987; Wong 2001). There were 2980 patients allocated to music, and 3124 allocated to a control (leaving one unknown case due to poor reporting in Taylor 1998). Patient characteristics were not reported in all of the studies; however, based on the 69 studies that reported information on mean age (details for 1108 participants remain unknown), the mean population age was 53.82 years old (range 14 to 99 years old; NB. > 90% of participants were 18 or older). Based on the 71 studies that reported information on gender, there were 2874 males and 2642 females included in the review (545 unknown cases). Studies were conducted in 16 different countries, predominantly the USA (N = 43) and China (N = 10). Five studies were conducted in each of Sweden and Canada, four in Germany, three in each of England and Taiwan, two in each of Australia, Japan, Turkey, and India, and one in each of Spain, Austria, Thailand, Slovenia, and Poland (NB. one study was carried out in two countries). The use of music was investigated in patients waiting for medical procedures (N = 13), undergoing endoscopic examinations (N = 12), undergoing percutaneous or surgical medical interventions (N = 34), undergoing non‐invasive medical procedures (N = 6), during labor (N = 1), post‐surgery (N = 7), in coronary care or intensive care environments (N = 10), or in ward environments (N = 2).
8. Music [RCT]: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Allen 2001 | RCT; 2 parallel groups. | DESCRIPTION: 40 day‐patients undergoing ophthalmic surgery in New York, USA. NUMBERS: 20 patients in each group. AGE, mean (range): Music group = 74 (51‐87), Control group = 77 (64‐88) years old. GENDER (male/female): Music group = 5/15, Control group = 5/15. ETHNICITY: not described. INCLUSION CRITERIA: Ambulatory surgical patients scheduled on the rosters of two ophthalmic surgeons. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Patient choice of 22 types of music (e.g. soft hits, classical guitar, chamber music, folk music, popular singers from 1940's and 1950's), played via headphones throughout pre‐operative, surgical, and post‐operative periods. CONTROL GROUP: Standard care. | PHYSIOLOGICAL: HR and BP measured via Propaq Monitor (Protocol Systems, Inc., Beaverton, OR) every 5 minutes during pre‐operative, surgical, and post‐operative period. Averages for the last three recorded measures within each time period were used for analysis in the paper. For purposes of review, data is extracted for the mean post‐operative scores only. COGNITIVE APPRAISAL: Two Likert scales used to measure questions on coping and stress, validity unclear. Not extracted for review. | |
| Andrada 2004 | RCT; 2 parallel groups. | DESCRIPTION: 118 out‐patients undergoing colonoscopy in a Digestive Endoscopy Unit in Spain. NUMBERS: Music group = 63 patients, Control group = 55 patients. AGE, mean (SD): Music group = 46 (14.22), Control = 49 (13.88). GENDER (Male/Female): Music group = 31/32, Control group = 28/27. ETHNICITY: not specified. INCLUSION CRITERIA: 18‐75 years old, scheduled for ambulatory examination. EXCLUSION CRITERIA: anacusis or significant bilateral hearing loss, senile dementia, cognitive disorders, acute or chronic confusional syndromes, treatment with anxiolytic medication in 72 hours prior to examination. | MUSIC GROUP: Series of classical tracks (e.g. Bach, Grieg, Mozart, Delibe, Faure, and Mendelssohn) played via headphones during procedure. CONTROL GROUP: Wore headphones but did not receive music throughout the procedure. | ANXIETY: State anxiety measure pre and post procedure using the STAI; Reported as post ‐ pre difference with 95% CI. ABNORMAL EVENTS: BP, capillary oxygen saturation, and HR were monitored using a Datex‐Ohmeda 3800 pulse oximeter and Nissei KTJ‐20 sphygmomanometer. Abnormal events arising from these parameters e.g. hypoxaemia, hypotension, hypertension, bradycardia, and tachycardia were recorded. | There were no significant differences between groups regarding abnormal events. This data has not been extracted for the review. |
| Argstatter 2006 | RCT; 3 parallel groups. | DESCRIPTION: 83 in‐patients undergoing cardiac catheterization in Germany. NUMBERS: Music group = 28, Control group = 27, Coaching group excluded from review. There are some discrepancies as to reported numbers in the paper, which also states there were 28 people in the control group. AGE, mean (SD) [range]: Music group = 65.8 (8.4) [49‐83], Control group = 67.5 (14.0) [28‐83]. GENDER (male/female): Music group = 16/12, Control group = 15/12. ETHNICITY: not described. INCLUSION CRITERIA: Patients were undergoing cardiac catheterization for the first or second time. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Music was played via headphones, which were worn half on so patients could still hear the medical personnel, during the cardiac catheterization. A music therapist was present only to control the volume. Music played was "Entspannung" [relaxation] by Markus Rummel, composed specially for relaxation. CONTROL GROUP: Standard care. This group did not have the addition of a music therapist present during the cardiac catheterization. COACHING GROUP: Excluded from review. | ANXIETY: Measured via the STAI before and after cardiac catheterization. Unclear whether post measurements were taken on the following day after cardiac catheterization. PHYSIOLOGICAL: BP and Pulse are reported as pre‐ and post‐measurements. Unclear how measurements were obtained. SUBJECTIVE MUSIC QUESTIONNAIRE: excluded from review. | |
| Ayoub 2005 | RCT; 3 parallel groups. | DESCRIPTION: 90 patients undergoing urological surgery with spinal anaesthesia and PCS in Connecticut (USA) and Beirut (Lebonon). NUMBERS: Music group = 31, White noise = 31, Operating room noise = 28. AGE, mean (SD): Music group = 55 (12), White noise = 54 (12), OR noise = 57 (10) years old. GENDER (male/female): Music group = 28/3, White noise = 29/2, OR noise = 24/4. ETHNICITY: Unclear, although 36 recruited in USA, and 54 recruited in Lebonon. INCLUSION CRITERIA: 18‐60 years old; ASA status I‐III (although Table1 states music group had a classification of V). EXCLUSION CRITERIA: On psychiatric medications; a history of affective disorders. | MUSIC GROUP: Patients brought own music from home. WHITE NOISE: Delivered by SoundSpa Acoustic Relaxation Machine. OR NOISE: Delivered by mini‐amplifier speaker via occlusive headphones. This Radio Shack (R) has mini‐microphone for voice acquisition. All groups wore occlusive headphones. | PROPOFOL REQUIREMENTS: Recorded as mg/kg/min and % of patients not using any propofol. Unclear if data presented are the SDs, and if the data presented as mg/kg/min is based on the total N or % of patients who used propofol. Observers Assessment of Alertness/Sedation Scale (OAA/S): Data not presented. PACU LENGTH OF STAY. (not primary outcome)‐ unclear whether the numbers presented are mean and SD. | Data not extracted for meta‐analysis. |
| Bally 2003 | RCT; 2 parallel groups. | DESCRIPTION: 107 patients undergoing diagnostic coronary angiography or a percutaneous intervention procedure, in Ontario, Canada. NUMBERS: Music group = 56 patients, Control group = 51 patients. AGE, mean (SD): Music group = 59 (11), Control group = 58 (11). GENDER (Male/Female): at enrolment: Music group = 34/24, Control group = 30/25. ETHNICITY: not specified. INCLUSION CRITERIA: 1st time diagnostic coronary angiography or a percutaneous intervention procedure, speak and read English, cognitively orientated. EXCLUSION CRITERIA: major auditory deficits. | MUSIC GROUP: patient selected music (classical, soft rock, relaxation, country, own/other) played via headphones before, during, and after procedure, continued as the patient desired. CONTROL GROUP: standard care (no music). | ANXIETY: State Anxiety via STAI pre and post procedure; PAIN INTENSITY: measured via 100mm VAS pre and post procedure (data extracted); PAIN RATING: measured via VRS pre and post procedure; APICAL HR (bpm): measured via cardiac monitor; BP (mm Hg): measured via pressure dynamometer and arterial pressure monitoring; HR and BP were taken at 4 points: (1) baseline; (2) after sheath insertion; (3) end of procedure; (4) after procedure, before sheath removal. Not enough information provided for data extraction of HR and BP. | See Cepeda 2006 for details on music for pain relief. |
| Barnason 1995/1996 | RCT; 3 parallel groups. | DESCRIPTION: 96 in‐patients in the cardiovascular ICU and progressive care units having undergone elective coronary artery bypass grafting, in USA. NUMBERS: Music group = 33, Music+video group = 29, Scheduled rest group = 34. AGE, mean (SD): 67 (9.9) years old. GENDER (male/female): 65/31. ETHNICITY: White = 96 (100%) INCLUSION CRITERIA: Orientated to person, time and place; speak and read English; 19 years or older; extubated within 12 hours of surgery; removal of intra‐aortic balloon pump within 12 hours of surgery. EXCLUSION CRITERIA: Currently using one of the intervention techniques; major hearing deficit. | MUSIC GROUP: Choice of 5 tapes: 'Country Western Instrumental' or 'Fresh Aire' by Mannheim Steamroller, 'Winter into Spring' by George Winston, or 'Prelude' or 'Comfort Zone' by Steven Halpern. Played via headphones for 30 minutes. MUSIC + VIDEO GROUP: Barnason 1995 states: Choice of 2 Steven Halpern tapes: 'Summer Wind' or 'Crystal Suite'. Each is 30 minutes of soft instrumental with visual imaging. Zimmerman 1996 states: Choice of three 30 minute videocassettes by Pioneer Artist ('Water's Path', 'Western Light', or 'Winter'). SCHEDULED REST: 30 minutes of rest in bed or chair, visitors and staff requested not to disturb. 2 x 30 min intervention periods during afternoons of post‐operative days 2 and 3. Lights dimmed. | Barnason 1995 reports: STATE ANXIETY: measured using STAI at three time‐points: pre‐operatively, before intervention on 2nd post‐operative day, and after intervention on 3rd post‐operative day. ANXIETY: taken using NRS before and after each intervention session. PHYSIOLOGICAL: HR (bpm) and BP (mm Hg) taken using the Kendall BP Monitor (Model 8200)‐ not enough data presented for extraction. MOOD: Measured using a NRS‐ not a validated outcome. Zimmerman 1996 reports: PAIN: Pain was measured with a 10‐point VRS before and after each session, and with the McGill Pain Questionnaire (scores are given for the subscales and the present pain index rating scale) administered once prior to the first session, and once after the second session. SLEEP: Measured with the Richards‐Campbell Sleep Questionnaire (RSQ), administered between 7am and 9am on the third post‐operative day. | Data extracted for state anxiety (STAI measure).
Patients in the music group showed a significant improvement in mood after the 2nd intervention when controlling for pre‐intervention mood rating. No differences between groups were found for anxiety on either data collection tool. Physiological measures did not differ between groups, however there were significant differences over time (regardless of group), indicating a generalised relaxation response.
Authors conclude that although no intervention was overwhelmingly superior, all groups demonstrated a relaxation response. See Cepeda 2006 for details on music for pain relief. |
| Binnings 1987 | RCT; 2 parallel groups. | DESCRIPTION: 20 patients undergoing regional anaesthesia in North Carolina, USA. NUMBERS: 10 patients in each group. AGE: Not stated. GENDER: Not stated. ETHNICITY: Not stated. INCLUSION CRITERIA: Patients scheduled for regional anaesthesia, 18‐65 years old. EXCLUSION CRITERIA: Taking tranquilizers or psychoactive medication. | NATURE TAPES: choice of sounds of birds, the ocean, a lagoon, or deeply resonant chimes, played for the duration of the surgery. CONTROL: standard care. | STATE ANXIETY: STAI administered pre‐operatively and one hour post‐operatively to calculate the change score. SEDATION MEDICATION: amount of Methohexital (mg) and Fentanyl (cc) administered by the anaesthetist was recorded. The anaesthetist was instructed to administer as much sedation as needed for a safe and comfortable experience with regional anaesthesia. Data extracted for Fentanyl for analysis ( P < 0.025 for differences between groups for both medications in favour of nature sounds). | Scores given for state anxiety are outside of the normal range for this questionnaire (20‐80). Method of calculating scores is not described. SDs calculated from t‐values presented for the difference in means between groups. |
| Blankfield 1995 | RCT; 3 parallel groups. | DESCRIPTION: 95 in‐patients undergoing coronary artery bypass (n = 92) or valvular heart surgery (n = 3) in Ohio, USA. NUMBERS: Music group = 32, Control group = 29, therapeutic suggestions = 34. AGE, mean (SD): Music group = 60 (10.4), Control group = 65 (7.8) years old. GENDER (male/female): Music group = 23/9, Control group = 21/8. ETHNICITY (White/other): Music group = 30/2, Control group = 27/2. INCLUSION CRITERIA: All coronary artery bypass patients. EXCLUSION CRITERIA: Impaired hearing, poor comprehension of English. | TAPED THERAPEUTIC SUGGESTIONS: excluded from review. MUSIC GROUP: Listened to "Dreamflight II" by Herb Ernst intraoperatively and for 30 minutes twice daily during post‐operative period. CONTROL GROUP: Listened to a blank tape intraoperatively (to blinded surgeon), and received no tape during the post‐operative period. | POST‐OPERATIVE STAY (days); Data extracted for analyses. SURGICAL INTENSIVE CARE UNIT STAY (days); Data not entered into analyses as accounted for by postoperative stay score (no significant differences). MORPHINE USAGE (mg); MEPERIDINE USAGE (mg); MORPHINE EQUIVELENTS (mg): combined morphine/meperidine usage, where the use of 10 mg of meperidine was considered equivalent to 1 mg morphine. ORAL NARCOTICS (total number of pills); DEPRESSION: 7‐item depression scale, unclear validity/reliability. Questionnaire given approximately one month after discharge. ACTIVITIES OF DAILY LIVING (10‐item scale), Questionnaire given approximately one month after discharge; CARDIAC SYMPTOM SCALE (7‐item scale), unclear validity/reliability. Questionnaire given approximately one month after discharge. | See Cepeda 2006 for details on music for pain relief. |
| Broscious 1999 | RCT: 3 parallel groups. | DESCRIPTION: 156 in‐patients undergoing chest tube removal after open heart surgery in Virginia, USA. NUMBERS: Music group = 70 patients, White noise = 36 patients, Control group = 50 patients. AGE, mean (SD): 66.35 (9.7) year old. GENDER (male/female): Music group = 53/17, White noise = 22/14, Control group = 32/18. ETHNICITY (White/Asian/Hispanic/Other): 152/1/1/2. INCLUSION CRITERIA: Ability to read and understand English, haemodynamic stability, no prior untoward response to music. EXCLUSION CRITERIA: Psychiatric history. | MUSIC GROUP: Patients preselected music they would prefer to hear from a library of 10 pre‐recorded music cassettes with no lyrics. Cassettes were produced by students in a music therapy programme under the supervision of a music therapist. Patients listened to the music via headphones for 10 minutes prior to and then during chest tube removal. WHITE NOISE: Pre‐recorded tape selected by the investigator. Patients listened to the tape via headphones for 10 minutes prior to and then during chest tube removal. CONTROL: Not explicit, presumably standard care with no headphones. | PAIN INTENSITY: Measured using a 10 cm NRS at 3 time points: (1) 10 minutes prior to chest tube removal, (2) immediately after chest tube removal, (3) 15 minutes after chest tube removal. HR and BP: measured every 5 minutes from 10 minutes prior to chest tube removal to 15 minutes afterwards. Physiological measurements were taken with a Hewlett‐Packard Component Monitoring System or a DINAMAP. | Report states that 18 participants had missing physiological data. Unclear from which groups these belonged, so for purposes of data extraction, it has been assumed that 6 participants were missing from each group. See Cepeda 2006 for details on music for pain relief. |
| Buffum 2006 | RCT; 2 parallel groups. | DESCRIPTION: 170 pre‐operative patients to undergo vascular angiography in California, USA. NUMBERS: Music group = 89, Control group = 81. AGE, mean (SD): 66.8 (9.95) years old. GENDER (male/female): 166/4. ETHNICITY: not described. INCLUSION CRITERIA: undergoing vascular angiography of the abdomen or lower extremities; 18 years or older; English speaking; read and write a 5th grade level; able to sign consent; interested in participating. EXCLUSION CRITERIA: Documented diagnosis of active psychosis or dementia; unable to consent; could not listen to music for 15 minutes prior to procedure. | MUSIC GROUP: Selection of 5 categories (classical, jazz, rock, country western, easy listening), played via headphones for 15 minutes prior to angiography. Patients could continue to listen to music during the angiography after collection of outcomes. CONTROL GROUP: 15 minute wait period. These participants were allowed to listen to music during the angiography after the study outcome measures had been taken. | ANXIETY: Measured via STAI before and after 15 minute study period. VITAL SIGNS: Unclear how data collected. | |
| Cadigan 2001 | RCT; 2 parallel groups. | DESCRIPTION: 140 in‐patients in the cardiac units with intravascular sheaths or an intra‐aortic balloon pump (IABP) in place, in USA. NUMBERS: Music group = 75 patients, Control group = 65 patients. AGE, mean (SD): Music group = 62 (11.4), Control group = 62.5 (14). GENDER (Male/Female): Music group = 56/19, Control group = 44/21. ETHNICITY: not specified. INCLUSION CRITERIA: read and speak English, haemodynamic stability, received an intravascular sheath or IABP. EXCLUSION CRITERIA: psychiatric illness, hearing deficits (not enhanced with an assistive device), documented confusional state. | MUSIC GROUP: 30 minutes of music through headphones. Mixture of symphonic music and nature sounds selected by the researchers. Same music played to all those in the music group. CONTROL GROUP: standard care. | PAIN PERCEPTION: measured via 10 mm VAS pre‐ and post‐intervention. HR (bpm): determined from a 1 minute readout of electrocardiogram; BP: measured via noninvasive automatic oscillometric BP cuff or transduced arterial wave form; RR (breaths per minute): measured via auscultation with stethoscope over chest for 1 minute; PERIPHERAL SKIN TEMPERATURE: taken from index finger with 'Dermatemp' hand‐held infrared thermographic scanner; MOOD: measure by the Profile of Mood States (POMS) short form questionnaire. | See Cepeda 2006 for details on music for pain relief. |
| Cepeda 1998 | RCT; 2 parallel groups. | DESCRIPTION: 193 day‐patients undergoing lithotripsy for renal stones (America). NUMBERS: Music group = 97, Control group = 96 patients. AGE, mean (SD): Music group = 40.7 (12.1), Control group = 41.0 (11.4). GENDER (male/female): Music group = 48/49, Control group = 47/49. ETHNICITY: not described. INCLUSION CRITERIA: 15‐65 years old, undergoing first lithotripsy for renal stones. EXCLUSION CRITERIA: Serum creatinine exceeded 1.5 mg/dl. | MUSIC GROUP: Music of type preferred by patient played via headphones, starting 10 minutes prior to procedure and continuing until 10 minutes after lithotripsy is complete. Patients wore additional ear protectors to protect patients from the noise of the lithotriptor. CONTROL GROUP: Wore headphones with ear protectors however the music (of patient preference) did not begin until the lithotripsy and study primary outcomes data collection had completed. Music was played for 10 minutes at the conclusion of the procedure. | PAIN INTENSITY: rated verbally every 5 minutes throughout the lithotripsy on a NRS (0‐10). ALFENTANIL REQUIREMENT: "registered" (mg). QUALITY OF ANALGESIA: rated by anaesthesiologist on a 4‐point scale (excellent to bad), 10 minutes after procedure conclusion. SIDE EFFECTS: evaluated throughout procedure and in the PACU: respiratory depression, bradycardia, level of consciousness, nausea, pruritis. PATIENT SATISFACTION WITH ANALGESIA: patient rated before leaving the PACU on a VRS, and indicated if they would accept same technique for future treatments. | See Cepeda 2006 for details on music for pain relief. |
| Chan 2003 | RCT; 2 parallel groups. | DESCRIPTION: 220 female out‐patients undergoing colposcopy in China. NUMBERS: Music group = 112 patients, Control group = 108. AGE, median (range): Music group = 40 (20‐61), Control group = 38.5 (19‐65). GENDER: All patients were female. ETHNICITY: All patients were Chinese. INCLUSION CRITERIA: 18‐65 years old, presenting for initial colposcopy, read and understand Chinese. EXCLUSION CRITERIA: previous experience of colposcopy, mental impairment, pregnant. | MUSIC GROUP: CD compilation of slow‐rhythm music (instrumental ballad). Patients could choose to listen to any song(s) within the compilation. Music played through speakers during the examination. Prior to onset of study women attending the clinic were surveyed on musical preferences to inform compilation disc. CONTROL GROUP: standard care, no music. | ANXIETY: State anxiety via Chinese version of STAI measured pre and post colposcopy; PAIN INTENSITY: measured via 10 cm VAS. | See Cepeda 2006 for details on music for pain relief. |
| Chan 2006 | RCT; 2 parallel groups. | DESCRIPTION: 43 in‐patients undergoing application of a C‐clamp (which applies pressure to stop bleeding when sheaths are removed after percutaneous coronary interventions), in an ICU, Hong Kong, China. NUMBERS: Music group = 20, Control group = 23. AGE: 32.6% of participants were 75+, age ranged from 35 upwards. GENDER (male/female): Music group = 16/4, Control group = 15/8. ETHNICITY: not described. INCLUSION CRITERIA: Diagnosis of MI, acute coronary syndrome, or coronary artery disease; conscious and alert; able to communicate, read, and write; able to speak Cantonese. EXCLUSION CRITERIA: hearing deficit; history of psychiatric illness; neurological disorders; dying; unable to give informed consent. | MUSIC GROUP: 3 choices of soft, slow music without lyrics (slow rhythmic songs, Chinese slow rhythmic music, Western slow rhythmic music). Music played via headphones during the application of the C‐clamp (approximately 45 minutes). CONTROL GROUP: No music, standard care. | VITAL SIGNS: BP, HR, RR, and oxygen saturation, recorded at baseline, 15, 30, and 45 minutes via a bedside monitor. PAIN: Measured via the Universal Pain Assessment Tool (a NRS). | Outcomes extracted for end time‐point only.
This paper states that missing values (unclear how many) were replaced with the group mean. It is unclear from the data presented if these are the raw values, or those that have been adjusted (which may potentially bias the results by lowering the variance and exaggerating group differences). For this reason we have removed this study in sensitivity analyses. See Cepeda 2006 for details on music for pain relief. |
| Chang 2005 | RCT; 2 parallel groups. | DESCRIPTION: 64 patients undergoing cesarean section in Taiwan. NUMBERS: 32 patients per group. AGE, mean (SD): Music group = 30.31 (4.16), Control group = 32.31 (4.48) years old. GENDER: Female = 64 (100%) . ETHNICITY: Taiwanese. INCLUSION CRITERIA: Women scheduled to receive cesarean section; married, between 20 and 40 years old; pregnancies gone to term with planned cesarean births; underwent spinal or epidural anaesthesia; newborns normal singletons with an Apgar score >/= 7 at 5 minutes. EXCLUSION CRITERIA: not stated. | MUSIC GROUP: Choice of western classical, new age, or Chinese religious music, played via headphones. Participants listened to music for at least 30 minutes from start of anaesthesia to end of surgery. Volume low enough to allow mutual conversation with the researcher. CONTROL GROUP: Unaware they had not had the opportunity to listen to music. They received the researchers' attendance and casual conversation. | ANXIETY: measured via a 10 cm VAS, researcher filled it in after asking participant to indicate how they were feeling. PHYSIOLOGICAL MEASURES: Oxygen saturation (measured via NONIN MODEL 9500 pulse oximeter), temperature of finger (measured via biofeedback system DT‐002), RR, pulse, and BP measured via Hewllett Packard 78352A. BIRTH SATISFACTION: measured via the satisfaction of cesarean delivery scale (SCDS) designed for the present study. Data not extracted. Anxiety & physiological measures taken pre‐surgery, post neonatal contact, and after completion of skin suture. Data extracted for end time‐points only. | |
| Chlan 1995 | RCT; 2 parallel groups. | DESCRIPTION: 20 in‐patients receiving mechanical ventilation in private patient room areas in critical care units in Midwest USA. NUMBERS: Music group = 11, Control group = 9. AGE, mean: Music group = 64.2, Control group = 55.7 years old. GENDER (male/female): 13/7. ETHNICITY: not described. INCLUSION CRITERIA: mechanically ventilated patients; alert; mentally competent; haemodynamically stable; able to sign consent form; adequate hearing. EXCLUSION CRITERIA: Documented mental incompetence; haemodynamically unstable; comatose; uncorrected impaired hearing. | MUSIC GROUP: Selection of classical music played for 30 minutes via headphones. Patients instructed to close eyes and concentrate on the music. CONTROL GROUP: Wore headphones with no music. Instructed to close eyes and rest for 30 minutes. For both groups lights were dimmed and/or doors closed. Experiment took place during late afternoon or early evening. | MOOD: Short‐form POMS. PHYSIOLOGICAL: HR (bedside ECG monitor), RR (observation for 1 minute), Oxygen saturation (pulse oximetry with finger probe), airway pressure (dial on ventilator), and BP (indwelling arterial lines, automatic BP monitor, or mercury sphygmomanometer and stethoscope), were measured before, and at 5 minute intervals during and 5 minutes after the intervention for both groups. | No SDs are presented for the post‐intervention physiological outcomes. Significant differences were found for HR and RR in favour of music. Other variables did not differ significantly. |
| Chlan 1998 | RCT; 2 parallel groups. | DESCRIPTION: 54 in‐patients receiving mechanical ventilation in one of 4 Intensive Care Units, USA. NUMBERS: 27 patients in each group. AGE, mean (SD): Music group = 57.3 (14.5); Control = 56.8 (18.6). GENDER (Male/Female): 22/32. ETHNICITY (White/Black/Native American): 50/3/1. INCLUSION CRITERIA: ventilator dependent, alert, mentally competent, adequate hearing, English as primary language. EXCLUSION CRITERIA: receiving continuous intravenous sedation. | MUSIC GROUP: choice of non‐lyric tapes 60‐80 bpm, classical, new age, country western, religious, and easy listening (30 mins). CONTROL GROUP: rest period (30 mins). Both groups received an enhanced environment by closing the blinds, placing a "do not disturb" sign on door, dimming the lights, and instructed to lie quietly and close eyes. | ANXIETY: State anxiety via short form STAI (6 items); RR (observation); HR (bedside cardiac monitor). Insufficient data for RR and HR data extraction. | Due to the lack of clarity over withdrawals and drop‐outs, it is unclear how many people were analysed in each group for the outcome anxiety. The degrees of freedom stated (49) suggests 51 observations were made, and we have assumed that N = 25 in the music group and N = 26 in the control group, based on the descriptions given for 3 of the withdrawals in the paper. |
| Chlan 2000 | RCT; 2 parallel groups. | DESCRIPTION: 64 out‐patients undergoing flexible sigmoidoscopy (FS) in Midwest USA. NUMBERS: Music group = 30 patients; Control group = 34 patients. AGE, mean (SD): Overall = 54.6 (11.5) years old. GENDER (Male/Female):20/44 ETHNICITY (White/African‐American/Hispanic): 62/1/1. INCLUSION CRITERIA: any adult out‐patient scheduled to undergo a nurse‐endoscopist performed screening FS, English as primary language, adequate or corrected hearing, mental competence. EXCLUSION CRITERIA: mentally incompetent (i.e. Alzheimers), uncorrected hearing impairment, English not primary language. | MUSIC GROUP: choice of music (classical, country‐western, new‐age, easy listening, pop, rock, religious, jazz, era‐specific, motion picture soundtracks), played via headphones during FS procedure. Patients instructed to concentrate on music and that the investigator would meet with them afterwards to discuss their experiences. CONTROL GROUP: routine care consisting of nurse‐endoscopist speaking to the patient at various times throughout the procedure. Patients were informed that the investigator will meet with them afterwards to discuss their experiences. | ANXIETY: State anxiety measured via STAI DISCOMFORT: Intensity of discomfort measured via NRS (entered into review as pain scores). SATISFACTION: Satisfaction measured via VRS FUTURE COMPLIANCE: Perceived future compliance measured via VRS | |
| Chui 2003 | RCT; 2 parallel groups. | DESCRIPTION: 68 pre‐operative patients undergoing extracorporeal shock wave lithotripsy (ESWL) in Taiwan. NUMBERS: Music group = 34 patients, Control group = 34 patients. AGE (range): 23‐72 years old. GENDER (male/female): 57/11. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: listened to natural music via headphones for 5 minutes prior to ESWL. CONTROL GROUP: Headphones without music for 5 minutes. All participants lay on the operating table and rested in the dark alone. Then experimental conditions were implemented and the outcome measures were taken, all prior to ESWL procedure. | BLOOD PRESSURE: Method of data collection unclear. HEART RATE VARIABILITY: Measured via an electrocardiogram (ECG). A number of measures derived, including RR intervals, low frequency (LF) and high frequency (HF) bands, converted into total power (LF nu; HF nu) and the LF/HF ratio. Heart rate variability data showed positive changes in favour of the music group. | |
| Colt 1999 | RCT; 2 parallel groups. | DESCRIPTION: 60 in‐patients and out‐patients undergoing flexible fibreoptic bronchoscopy (FB) in California, USA. NUMBERS: Music group = 30 patients; Control group = 30 patients. AGE, mean (SD): Music group = 49 (18); Control group = 56 (13) years. GENDER (Male/Female): Music group = 20/10; Control group = 19/11. ETHNICITY (Caucasian/Hispanic/Black/Asian): 37/11/10/2. INCLUSION CRITERIA: All in‐patients and out‐patients referred for diagnostic FB. EXCLUSION CRITERIA: under 18 years old, unable to speak and understand English, unable to give consent, in need of ICU hospitalisation, significantly hearing impaired, impaired mental status, receiving known anxiolytic or sedative medication. | MUSIC GROUP: "Relax" (Expansion Records, Manchester, UK) consisting of piano improvisations (60bpm), played via headphones during FB procedure. CONTROL GROUP: silence whilst wearing headphones during FB procedure. | ANXIETY: State and Trait anxiety measure via STAI. | |
| Cooke 2005 | RCT; 3 parallel groups. | DESCRIPTION: 180 pre‐operative day patients scheduled for day surgery in Australia. NUMBERS: 60 participants in each group. AGE, median (range): Music group = 53 (19‐99), Placebo group = 58 (18‐83), Control group = 56 (18‐87) years old. GENDER (male/female): 30/30 in each group. ETHNICITY: not described. INCLUSION CRITERIA: Day surgery patients. EXCLUSION CRITERIA: < 18 years old; undergoing eye surgery requiring eye drops which could affect vision; had pre‐operative sedatives; did not like music; hearing‐impaired; difficulty wearing headphones; could not read and write English; had a pre‐operative waiting time anticipated as < 45 minutes. | MUSIC GROUP: Choice of classical, jazz, country & western, new age, easy‐listening, and "other" mostly by contemporary artists. Music played for 30 minutes via headphones. PLACEBO GROUP: Patients wore headphones without any music for 30 minutes. CONTROL GROUP: Routine care. | ANXIETY: State anxiety measured via STAI. | 95% Confidence Intervals are presented in the paper based on logarithmically transformed scores. Standard deviations were calculated by first back‐translating data to a log scale before utilising the CIs to estimate the SDs. Data entered into the review analysis are expressed as the natural log. |
| Cruise 1997 | RCT; 4 parallel groups. | DESCRIPTION: 121 patients undergoing elective cataract extraction in Canada. NUMBERS: Music = 32, OR noise = 30, White noise = 29 (Relaxing Suggestions, N = 30, excluded from review). AGE, mean: Music = 70.8, OR noise = 68.3, White noise = 73.6 years old. GENDER (male/female): Music = 8/24, OR noise = 12/18, White noise = 12/17. ETHNICITY: not described. INCLUSION CRITERIA: none described. EXCLUSION CRITERIA: On sedative or psychotropic drugs; hearing impairment. | MUSIC GROUP: Classical music accompanied by soothing sounds of nature, played via headphones intra‐operatively. OR NOISE: Playback of a previously recorded cataract operation, played via headphones intra‐operatively. WHITE NOISE: Played via headphones intra‐operatively. RELAXING SUGGESTIONS: Excluded from review. | ANXIETY: Measured via STAI before and after surgery. VITAL SIGNS: BP, HR, and RR recorded before and after the retrobulbar block, and at 15 minute intervals thereafter until procedure completion. SATISFACTION: Unclear validity, not included in review. | Data reporting unclear. Cannot extract SDs. No differences between groups are reported for anxiety, DBP, HR and RR. SBP did differ between groups over time, where music and white noise groups increased more after the retrobulbar block than the OR noise group, and then the OR noise group decreased more over the course of the operation than both the music and white noise group. Exact differences between groups are unclear. |
| Daub 1988 | RCT; 3 parallel groups. | DESCIPTION: 90 pre‐operative in‐patients waiting for dental restoration surgery under general anaesthesia, or orthopedic surgery, in Germany. NUMBERS: 30 patients in each group. AGE: 15‐65 years old. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: 15‐65 years old; German speaking (1st language). EXCLUSION CRITERIA: Malignant diseases; expecting operations of uncertain outcome. | MUSIC GROUP: listened to 45 minutes of music pre‐operatively. Choice of music arranged the evening before surgery. 11 patients chose classical, 19 chose pop music. NO MEDICATION: Patients received no premedication and no music. MEDICATION: Received 1‐2 ml Thalamonal. Excluded from review. | ANXIETY: Measure via STAI and a tick‐box anxiety scale tailored for the clinic. There was a significant decrease in state anxiety from pre‐treatment to post‐treatment in the music group (change score = 2.2). There was no significant change in anxiety for the 'no medication' control group (change score = 0.633). Other outcomes not included. | Not enough information for data extraction. |
| Davis‐Rollans 1987 | RCT; Cross‐over study. | DESCRIPTION: 24 in‐patients with MI (N = 12) and other cardiac conditions (N=12) in a Critical Care Unit, Ontario, Canada. NUMBERS: Cross‐over study of 24 patients. AGE, mean (range): 62 (45‐75) years old. GENDER (male/female): 19/5. ETHNICITY: not described. INCLUSION CRITERIA: Willingness to listen to music; Asymptomatic for 6 hours prior to data collection; Stable vital signs; Physician's approval to participate. EXCLUSION CRITERIA: Pace‐maker; Hearing deficit; Use of a ventilator; Asian or Middle Eastern cultural background [rationale: "tonal systems differ from that of Western (European) music"]. | MUSIC: 3 pieces each lasting approximately 12 minutes played in randomised Latin square design via headphones. a) Symphony no.6 by Beethoven; b) Eine Kleine Nachtmusik by Mozart; and c) The Moldau by Smetana. CONTROL: ICU noise as heard through silent headphones. Order of receiving conditions was randomised, each condition lasted 42 minutes. | PSYCHOLOGIC: Questionnaire not fully validated (content validity only). Not extracted for review. PHYSIOLOGICAL: HR (median values used) and heart rhythm (clinical categorisation) measured via electrocardiography. RR measured via Brush‐Gould bellows pneumograph and Hewlett‐Packard 4 channel FM tape recorder. Each session began with a 5 minute baseline data collection period. | Significant order effects for HR variability (P = 0.03) and heart rhythm (ectopy). HR varied when different music pieces were played (P = 0.04) regardless of order. Individual patient data presented for HR during music and control periods. Data extracted for review and paired t‐test reveals no significant difference between groups (MD = 0.847, 95% CI = ‐1.42, 3.11, P = 0.447), music and control significantly correlated (r = 0.942). Data entered with adjusted standard deviations. No significant differences are reported for RR between music and control periods. |
| Domar 2005 | RCT; 3 parallel groups. | DESCRIPTION: 143 out‐patients (93 included in present review) undergoing screening mammography in a clinic of a tertiary care hospital in Massachusetts, USA. NUMBERS: Music group = 47, Control group = 46 patients. AGE, mean (SD): Music group = 51.7 (10.9), Control group = 53.1 (11.6). GENDER: all patients were female. ETHNICITY (white/black/other): Music group = 91/7/2, Control group = 80/13/7. INCLUSION CRITERIA: Scheduled for screening mammography. EXCLUSION CRITERIA: unable to read and speak English, current psychiatric diagnosis, brought own tape player and planned to listen to an audiotape during mammography, pain or anxiety medication taken before procedure. Additionally stated "women who have a history of breast cancer do not undergo screening, so they were not eligible for the study". | RELAXATION GROUP: excluded from review, as taped instructions constitute a psychological therapy. MUSIC GROUP: choice of classical, jazz, or soft rock, played via headphones whilst in the waiting room and during the examination. CONTROL GROUP: blank tape played via headphones, whilst in the waiting room and during the examination. | ANXIETY: recorded before and after study period using the STAI, and at the end of the study with a Likert scale (1‐10) asking to rate level of anxiety felt during the procedure. PAIN: recorded after procedure using the McGil Pain Questionnaire, and a Likert scale (1‐10) asking to rate pain felt during the procedure. | Investigator identified a possible floor effect. See Cepeda 2006 for details on music for pain relief (this study is not yet included in Cepeda 2006). |
| Elliot 1994 | RCT; 3 parallel groups. | DESCRIPTION: 56 in‐patients with unstable angina pectoris or acute MI at coronary care unit in Australia. NUMBERS: Music group = 19, Control group = 19, muscle relaxation not included in review. AGE, average = 60.6 years old. GENDER (male/female): 40/16. ETHNICITY (Australian/Other): 47/9. INCLUSION CRITERIA: Patients admitted to the coronary care unit with provisional medical diagnoses of unstable angina pectoris or acute MI. EXCLUSION CRITERIA: none further described. | MUSIC GROUP: Received two or three 30‐minute sessions of light classical music (Bonny,Music Rx) played via headphones. CONTROL GROUP: two or three sessions of 30 minutes uninterrupted rest. MUSCLE RELAXATION: Excluded from review. | ANXIETY: Measured at pre and post test with three psychologic scales, 1) STAI, 2) Hospital Anxiety and Depression Scale, and 3) Linear Analogue Anxiety Scale (VAS). STAI scores extracted for review. PHYSIOLOGICAL: HR (measured digitally by bedside cardiac monitors) and BP (measured via sphygmomanometer) were observed 7 times at the routine observation times in the coronary care unit (not directly before and after intervention period). | |
| Ezzone 1998 | RCT; 2 parallel groups. | DESCRIPTION: 33 in‐patients undergoing bone marrow transplant chemotherapy, in Columbus, USA. NUMBERS: Music group = 16, Control group = 17. AGE, median (range): Music group = 36.9 (21‐49), Control group = 40.3 (14‐61). GENDER (male/female): Music group = 11/5, Control group = 8/9. ETHNICITY: not described. INCLUSION CRITERIA: Patients receiving treatment with autologous or allogeneic transplant; a preparative regimen consisting of busulfan and cyclophosphamide or busulfan, etoposide, and cyclophosphamide with all dosages calculated on body weight; the pharmacologic protocol for control of nausea and vomiting consisting of IV ondansetron 0.15 mg/kg every six hours around the clock starting 30 minutes before and continuing for 24 hours after the preparative regimen. Additional antiemetics were limited to IV lorazepam 1‐2 mg or promethazine 12.5‐25 mg every four to six hours as needed for breakthrough nausea and vomiting. EXCLUSION CRITERA: none described. | MUSIC GROUP: Listened to 45 minute recording of self‐selected music via headphones at 6, 9, and 12 hours after the start of each infusion as an adjunct to antiemetic therapy. A variety of music selections was available and patients were encouraged to bring their favourite music. CONTROL GROUP: Standard care. | NAUSEA: Measured on a VAS in the pictorial form of a thermometer (questionable validity). Mean (range) at 8‐hour follow‐up, 1st dose of Cytoxan: Music group = 50 (0‐90), Control group = 54.4 (0‐100) Mean (range) at 8‐hour follow‐up, 2nd dose of Cytoxan: Music group = 29.6 (0‐95), Control group = 59.3 (0‐100). VOMITING: Instances of vomiting were defined as the oral expulsion of gastric contents or as retching, the act of vomiting without expulsion of gastric contents. For data analysis, the authors considered the occurrence of 5 instances of retching within one minute as a vomiting episode. Mean (range) episodes at 8‐hour follow‐up, 1st dose: Music group = 0.69 (0‐4), Control group = 1.73 (0‐6) Mean (range) episodes at 8‐hour follow‐up, 2nd dose: Music group = 0.31 (0‐2), Control group = 0.94 (0‐2). | Data not in sufficient detail for extraction. The music group had significantly less nausea and vomiting than the control group (Mann‐Whitney U test, P < 0.017 for both comparisons). |
| Ferguson 2004 | RCT; 2 parallel groups. | DESCRIPTION: 11 patients undergoing range‐of‐motion exercises as part of acute care rehabilitation for burns, Virginia, USA. NUMBERS: Music group = 5, Control group = 6. AGE, mean (range, SD): Music group = 45.4 (22‐75, 19.3), Control group = 38.3 (18‐57, 16.3). GENDER (male/female) %: Music group = 92/8, Control group = 46/54. (Note: Can not sensibly convert % to number of patients ‐data unclear) ETHNICITY (African American/White) %: Music group = 58/42, Control group = 0/100 INCLUSION CRITERIA: English‐speaking; partial‐thickness or deeper burns crossing at least one major joint; scored 100% on a cognitive screening tool. EXCLUSION CRITERIA: No further criteria described. | MUSIC GROUP: Choice of 6 cassette tapes (Lifescapes series) that met the guidelines for music in medical settings. Music was played during the range‐of‐motion exercises. CONTROL GROUP: No music played during the range‐of‐motion exercises. The number of repetitions and type of exercise (active, active‐assistive, or passive) were based on the needs of each patient. Both groups were treated in the patient's room with the door closed and "do not disturb" sign posted. Lights were turned on and the television was turned off. | PAIN: Measured via VAS before and after rehabilitation exercises. There was a statistically significant increase in pain from pre‐treatment to post‐treatment in both groups (P = 0.04). There was no significant difference between groups (P = 0.38). ANXIETY: Measured via STAI before and after rehabilitation exercises. The mean pre‐treatment and post‐treatment state anxiety scores were greater for the control group (P = 0.04). VITAL SIGNS: BP, HR, and RR measured before and after rehabilitation exercises using either the Hewlett‐Packard Component Monitoring System or the Dinamap 8100 Portable Vital Signs Monitor. There were no significant differences between groups (systolic BP: P = 0.30, diastolic BP: P = 0.84, HR: P = 0.29, RR: P = 0.54). RR did increase in both groups from baseline (P <0.01). | Data not in sufficient detail for extraction. See Cepeda 2006 for details on music for pain relief. |
| Gaberson 1991 | RCT (post‐test only); 3 parallel groups. | DESCRIPTION: 15 pre‐operative patients in the waiting room for elective same‐day surgery in Pittsburgh, USA. NUMBERS: Music group = 5, Control group = 5, Humour group = 5 (excluded from review). AGE (range): 23‐76 years old. GENDER (male/female): 6/9. ETHNICITY: not described. INCLUSION CRITERIA: 21 years old and over; admitted for same‐day elective surgical procedures; EXCLUSION CRITERIA: Can not speak, understand, and read English; Hearing loss; Surgery for diagnostic procedures; Taken anti‐anxiety medication with 24 hours of operation. | HUMOUR GROUP: excluded from review. MUSIC GROUP: Listened to 'Omni Suite' by Steven Bergman (tranquil music) via headphones for 20 minutes in the waiting room. CONTROL GROUP: Standard care. | ANXIETY: Measured via a VAS after the intervention period. | |
| Gaberson 1995 | RCT (post‐test only); 3 parallel groups. | DESCRIPTION: 46 pre‐operative patients scheduled for same‐day surgery in Pittsburgh, USA. NUMBERS: Music group = 16 patients, Control group = 15 patients, Humour group = 15 patients (excluded from review); AGE, mean (SD): Music group = 51.75 (17.18), Control group = 47.07 (19.07) years old. GENDER (male/female): 19/27 ETHNICITY: not described. INCLUSION CRITERIA: 21 years and older; scheduled for elective surgical procedures. EXCLUSION CRITERIA: Can not speak, read, and understand English; Hearing loss; Undergoing diagnostic procedure; Taken medications with anti‐anxiety effects within past 24 hours; presenting with ear pathology. | HUMOUR GROUP: excluded from review. MUSIC GROUP: listened to tranquil music via earphones for 20 minutes after admission to surgery unit and before scheduled procedure. CONTROL GROUP: 20 minute waiting period (standard care). | ANXIETY: Measure post‐intervention via VAS. | |
| Ganidagli 2005 | RCT; 2 parallel groups. | DESCRIPTION: 50 pre‐operative patients to undergo septorhinoplastic surgery in Turkey. NUMBERS: Music group = 25, Control group = 25 patients. AGE, mean (SD): Music group = 31 (9), Control group = 29 (9) years old. GENDER (male/female): Music group = 14/11, Control group = 15/10. ETHNICITY: not described. INCLUSION CRITERIA: ASA I‐II; 18‐60 years old; scheduled to undergo septorhinoplastic surgery. EXCLUSION CRITERIA: 4 patients excluded as observer blinding unsuccessful due to technical problems with tape player. | MUSIC GROUP: Patients brought own CD or tape from home, those who forgot were provided with a 'suitable replacement', played via headphones during pre‐operative period, as patients were being sedated. CONTROL GROUP: Blank tape/CD played via headphones during pre‐operative sedation period. All patients asked to bring music from home in case they were allocated to the music group. | "modified" OAA/S: not included in review. BI‐SPECTRAL INDEX (BIS): Time (seconds) to reach BIS value of 60 (hypnotic end point of anaesthesia). BIS values were monitored (A‐2000, Aspect Medical Systems Inc) and the average scores calculated at 10 minute intervals from baseline to 50 minutes. Data extracted for time to reach BIS 60 value (end‐point). PROPOFOL: induction dose of propofol (mg) recorded. Time to eyelash reflex: not included in review. | |
| Guo 2005 | RCT; 2 parallel groups. | DESCRIPTION: 93 in‐patients scheduled for laparoscope surgery, in Beijing, China. NUMBERS: Music group = 48 patients; Control group = 45. AGE, mean (SD) years: Music group = 40.90 (10.94); Control group = 40.69 (9.94). GENDER (male/female): Music group = 20/28; Control group = 19/26. ETHNICITY: Not stated. INCLUSION CRITERIA: Consenting patients. EXCLUSION CRITERIA: Hearing problems; cancer patients; no clear outcome from laparoscopy. | MUSIC GROUP: Choice of 6 types of music (Western classical; light; pop; folk; folksong; opera) with 30 minutes listening time. Patients listened to music via headphones 1‐2 hours before their operation, whilst lying in bed. CONTROL GROUP: Had headphones with no music for 30 minutes 1‐2 hours prior to operation. | ANXIETY: Measured via STAI before and after intervention period. BP, HR, GALVANIC SKIN RESPONSE: Measured before intervention, at 10 and 20 minutes after, and at 4 hours after. Unclear what time point the data in the table reflects. SALIVA CORTISOL: Measured before and 2‐3 minutes after intervention. | |
| Harikumar 2006 | RCT; 2 parallel groups. | DESCRIPTION: 78 patients undergoing colonoscopy in Kerala, India. NUMBERS: Music group = 38, Control group = 40 AGE: not described. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: Scheduled for elective colonoscopy; 15‐60 years old. EXCLUSION CRITERIA: Hard of hearing; overt or borderline psychiatric illness; cardiopulmonary morbidity. | MUSIC GROUP: Choice of 6 tapes played via headphones during colonoscopy. Selection of: popular film songs (based on carnatic classical ragas), classical music, devotional songs, folk songs, soft instrumental music, bioacoustics (soft instrumental music with nature sounds). CONTROL GROUP: Wore headphones but were not played music. | SEDATION: Dose of midazolam (2 mg given on demand). DURATION OF PROCEDURE; RECOVERY TIME: Defined as when patient orientated in time, place, and person, and can serially subtract 6 from 100, as assessed by recovery room nurse; PAIN SCORE: 0‐10 visual analogue scale (UNCLEAR if patient or nurse rated); DISCOMFORT SCORE: 0‐10 visual analogue scale (UNCLEAR if patient or nurse rated); WILLINGNESS TO REPEAT PROCEDURE: Method of data collection not described. Data insufficient for extraction. | Data reported as median and range.
Controls received significantly more midazolam:
Music group = 4 (0‐6) mg
Control group = 5 (0‐8) mg
Duration of procedure did not differ between groups:
Music group = 28 (14‐50) minutes
Control group = 33 (17‐58) minutes
Recovery time was significantly longer in controls:
Music group = 10 (0‐28) minutes
Control group = 20 (0‐20) minutes. See Cepeda 2006 for details on music for pain relief (this study is not yet included in Cepeda 2006). |
| Hayes 2003 | RCT; 2 parallel groups. | DESCRIPTION: 198 out‐patients awaiting gastrointestinal procedures (colonoscopy or esophagogastroduodenoscopy [EGD]) in California, USA. NUMBERS: Music group = 100, Control group = 98. AGE, mean (SD): 61 (10.5) years old. GENDER (male/female): 193/5. ETHNICITY: not described. INCLUSION CRITERIA: Undergoing colonoscopy or EGD for the 1st time; 18 years or older; English speaking; Able to read at 5th grade level; able to sign the study consent. EXCLUSION CRITERIA: Actively psychotic or has dementia; could not listen to music for 15 minutes prior to procedure. | MUSIC GROUP: Patient selected music (classical, rock, jazz, country western, easy listening) for 15 minutes prior to medical procedure. Were allowed to continue listening to music after outcome measures were taken. CONTROL GROUP: No music for a 15 minute wait, were given the opportunity to listen to music during their procedure. | ANXIETY: state anxiety measured via STAI. PHYSIOLOGICAL MEASURES: BP and pulse were recorded before and after the 15‐minute intervention period, however details of methods unclear. | This study has questionable clinical relevance: "To avoid introducing more anxiety with the explanation of the [gastrointestinal] procedure, the consent process for the [gastrointestinal] procedure was delayed until after the patients completed the music study". |
| Heitz 1992 | RCT; 3 parallel groups. | DESCRIPTION: 60 in‐patients who have undergone surgery with general anaesthesia, in a PACU in Iowa, USA. NUMBERS: 20 participants per group. AGE, mean (SE): Music group = 46 (3), Control group = 52 (3), Headphones only group = 54 (4) years old. GENDER (male/female): Music group = 2/18, Control group = 1/19, Headphones only group = 1/19. ETHNICITY: not described. INCLUSION CRITERIA: >19 years old; Undergoing a thyroidectomy, parathyroidectomy, or unilateral modified radical mastectomy; Intact hearing; No drug abuse; No psychiatric history; class I‐III ASA status. EXCLUSION CRITERIA: none further described. | MUSIC GROUP: Choice of three instrumental tapes: Calm classical (e.g. Bach, Debussy, Pachelbel), Stimulative classical (e.g. Strauss, Tschaikovsky), and calm popular music (e.g. piano solos by George Winston, guitar solos by William Ackerman and Steve Halpern). Patients decided which music they would like to listen to in the PACU in the pre‐operative visit. Played via headphones until discharge from PACU. CONTROL GROUP: No headphone, no music (standard care). HEADPHONES ONLY GROUP: Wore headphones but heard no music. Patients wore headphones until discharge from the PACU. | PAIN: Measured via 10cm VAS every 15 minutes while in the PACU. MORPHINE REQUIREMENT: Patients received 0.025 mm/kg IV morphine every 5 minutes as necessary for pain control. Total requirement and time until initial analgesic was needed after leaving the PACU were recorded. PHYSIOLOGICAL MEASURES: BP and HR were monitored with an ECG and Noninvasive BP machine (Spacelabs, Redmond, WA). RR was monitored by counting the rate for 1 minute. BP, HR, and RR were recorded every 15 minutes whilst in the PACU. LENGTH OF STAY: Length of stay in the PACU was recorded. FOLLOW‐UP QUESTIONNAIRE: not included in review (not validated). | Data insufficient for extraction.
There was no significant differences between groups in:
Pain scores; Morphine requirement; BP; HR; RR; Length of stay.
After leaving the PACU patients in the music group (mean = 6.5 hours) waited significantly longer than the headphones only group (mean = 3.5 hours) before initially requiring analgesic. Patients in the control group waited for 4.5 hours (not significant). See Cepeda 2006 for details on music for pain relief. |
| Ikonomidou 2004 | RCT; 2 parallel groups. | DESCRIPTION: 55 day‐patients undergoing laparoscopic sterilization or laparoscopic tubal dyeing as part of a fertility programme in Sweden. NUMBERS: Music group = 29, Control group = 26. AGE, median (range): Music group = 34 (25‐45), Control group = 34 (22‐42) years old. GENDER: Female = 55 (100%). ETHNICITY: not described. INCLUSION CRITERIA: ASA rating 1‐2; 25‐45 years old (does not tally with baseline characteristics); scheduled to undergo gynaecologic laparoscopy under general anaesthesia. EXCLUSION CRITERIA: ASA rating > 2; psychiatric disorder; history of drug/alcohol abuse; neurological disease; 1st language not Swedish; chronic pain problems; analgesic medication taken within the last week; allergy to any of the planned perioperative medications; past complications during anaesthesia or surgery; additionally 5 patients were excluded from analysis due to "extended surgery or various technical problems on the ward" | MUSIC GROUP: Panpipe music played via headphones for 30 minutes pre‐operatively and 30 minutes post operatively. CONTROL GROUP: Blank disc and headphones for 30 minutes pre‐ and post‐operatively. | PHYSIOLOGICAL MEASURES: RR, BP, and HR, were measured by an attending nurse blinded to group allocation, before and after each 30 minute session (pre‐ and post‐surgery). PAIN: Pain was measured post‐operatively using a VAS. Pain medication ("cumulative opioid consumption") was also recorded, units unclear. WELLBEING: Measured pre‐ and post‐ each 30 minute session using a VAS with end‐points marked "calm" and "very anxious". For purposes of review this data is considered as the outcome ANXIETY. | Sensitivity analyses conducted using data extracted for pre‐operative and post‐operative scores for anxiety, RR, BP, and HR.
Findings reported in the paper cannot be replicated using the data provided in the table, leading to concerns over either the validity of information provided or selective outcome reporting (due to the multiple ways data could have been analysed). For this reason the study has been removed in sensitivity analyses. See Cepeda 2006 for details on music for pain relief. |
| Jacobson 1999 | RCT; 3 parallel groups. | DESCRIPTION: 110 in‐patients and out‐patients undergoing IV catheter insertion in Southwestern public and private hospitals, USA. NUMBERS: (Saline group = 38 patients), Music group = 36 patients, Control group = 36 patients. AGE, mean (SD): overall = 53 (14) years old. GENDER (male/female): 58/52 ETHNICITY (Caucasian/Black/Hispanic): 74/25/11. INCLUSION CRITERIA: 18 years and older, English speaking, vision and hearing in tact, medical orders for peripheral IV therapy. EXCLUSION CRITERIA: cognitive, neurological, or motor impairment. | SALINE GROUP: excluded from review as confounding non‐environmental intervention. MUSIC GROUP: choice of 11 compact discs representing different music styles (e.g. jazz, country). CONTROL GROUP: standard care. | PAIN INTENSITY: measured via 100mm VAS. PAIN DISTRESS: measured via 100mm VAS. INSERTION DIFFICULTY: Difficulty of IV catheter insertion via 100mm VAS. IV catheter insertion difficulty checklist (12 items to identify factors contributing to difficulty). Patients filled out the pain scores and the investigator rated the insertion difficulty immediately after IV insertion or failed IV insertion attempt. | See Cepeda 2006 for details on music for pain relief. Insertion difficulty is not included in the present review as a health‐related outcome. |
| Kliempt 1999 | RCT; 3 parallel groups. | DESCRIPTION: 76 in‐patients undergoing surgery with general anaesthetic, in Sidcup, UK. NUMBERS: Music group = 25, Control group = 26, Binaural beats group = 25. AGE, mean: Music group = 48.7, Control group = 46.9, Binaural Beats group = 41.8 GENDER (male/female): Music group = 9/16, Control group = 9/17, Binaural beats group = 15/10. ETHNICITY: not described. INCLUSION CRITERIA: ASA 1‐2; Aged 18‐76 years old; Scheduled for general surgical operations under general anaesthesia. EXCLUSION CRITERIA: Disliked classical music; knew the Monroe Institute or knew about Hemi‐Sync (Binaural Beats) music; suffered from known malignancy; hearing impairment; mentally impaired; used regular pain killers, tranquillisers, or antihypertensive medicines; known alcoholic or drug user; history of epilepsy or mental illness; were pregnancy; scheduled for operation involving the head or neck area; were not suitable for the standardised anaesthetic technique. | MUSIC GROUP: Classical music ('Adagio' Karajan, Deutsche Grammophon, 445 282‐4). Played via headphones during surgery. CONTROL GROUP: Blank tape via headphones during surgery. BINAURAL BEATS GROUP: Hemispheric sychronisation through binaural beats, played via headphones during surgery. (Not included in review). | FENTANYL REQUIIREMENTS: This served as an indication of the adequacy of nociception control provided during the operation. Fentanyl (ųg) was given intravenously if intra‐operative BP or HR increased by 20% or more above baseline values for more than 5 minutes. | See Cepeda 2006 for details on music for pain relief. |
| Koch 1998a | RCT; 2 parallel groups. | DESCRIPTION: 34 out‐patients undergoing urologic procedures using spinal anaesthesia, USA. NUMBERS: Music group = 19, Control group = 15. AGE, mean (SD): Music group = 54 (15), Control group = 53 (12) years old. GENDER (male/female): Music group = 16/3; Control group = 13/2. ETHNICITY: Not described. INCLUSION CRITERIA: Unpremedicated with ASA status 1‐3. EXCLUSION CRITERIA: Not stated. | MUSIC GROUP: All patients requested to bring their favourite CD to hospital on morning of surgery. A suitable substitution was provided to those who did not have access to their favourite CD. Music played via occlusive headphones intraoperatively. CONTROL GROUP: As with music group, patients were asked to bring their favourite CD to the hospital. Patients in the control group did not listen to music nor did they wear headphones. They were exposed to the operating room noise (standard care). | BP (mm Hg), HR (bpm), PROPOFOL REQUIREMENTS (mg/min): recorded every 10 minutes for duration of surgery; PACU LENGTH OF STAY (min). | See Cepeda 2006 for details on music for pain relief. |
| Koch 1998b | RCT; 2 parallel groups. | DESCRIPTION: 43 patients undergoing lithotripsy, USA. NUMBERS: Music group = 21, Control group = 22. AGE, mean (SD): Music group = 54 (15), Control group = 53 (12) years old. GENDER (male/female): Music group = 17/4, Control group = 10/12. ETHNICITY: Not described. INCLUSION CRITERIA: ASA status 1‐3; scheduled for lithotripsy treatment of renal calculi using the Dornier 3 or 4 lithotripter. EXCLUSION CRITERIA: None described. | MUSIC GROUP: Patients brought own music from home to listen to via occlusive headphones during surgery. CONTROL GROUP: Standard care. Also brought in own music in case of allocation to other group. | BP (mm Hg), HR (bpm), ALFENTANIL REQUIREMENTS: recorded every 15 mins. PAIN SCORE: Self‐report VAS recorded every 15 minutes intraoperatively. Insufficient information for extraction of: PACU length of stay, desaturation rate, level of sedation, self‐report sedation. | See Cepeda 2006 for details on music for pain relief. |
| Korunka 1992 | RCT; 3 parallel groups. | DESCRIPTION: 163 in‐patients undergoing hysterectomy in Vienna, Austria. NUMBERS: Music group = 55, Control group = 53. AGE, mean (SD): Music group = 44.9 (7.6), Control group = 46.8 (8.4) years old. GENDER: Female = 163 (100%). ETHNICITY: not described. INCLUSION CRITERIA: All women scheduled for hysterectomy. EXCLUSION CRITERIA: Cardiovascular disease; psychological problems; risk of cancer in uterus. | MUSIC GROUP: Patient choice of classical (Bach), Entertainment ("Musik zum Träumen" [Music for Dreaming]), or Relaxation (Oliver Shanti "Rainbow Way"). Played via headphones for 45 minutes beginning at the start of the operation (at the abdominal incision). POSITIVE SUGGESTIONS: Excluded from review. CONTROL: Recording of OR noise played via headphones. | PAIN: Pain intensity measured via 10 cm VAS once a day for 5 days. There were no differences between groups. Post‐operative pain measured via a multidimensional pain scale (with 6 subscales). Significant differences were found between the music and control group (control scores consistently higher than music on all subscales). Data presented in graphs‐ UNCLEAR. MEDICATION: Time of request and dose of pain medications was recorded. Patients could request up to 4 more doses of medication. Patients in the music group had reduced pain medication compared to controls. Outcomes missing for 23 participants (unclear which groups): Time to first medication administration, mean (SD): Music = 211 (240), Control = 118 (154) minutes. Overall pain medication dose, mean (SD): Music = 197 (138), Control = 291 (175) uG/K. Length of stay, mean (SD): Music = 8.52 (2.0), Control = 10.20 (3.8) days. | Where means and SDs are presented (for length of stay), there are missing data from 23 participants so it is unclear how many people are in each group. See Cepeda 2006 for details on music for pain relief. |
| Kotwal 1998 | RCT; 2 parallel groups. | DESCRIPTION: 104 patients undergoing gastrointestinal endoscopy in India. NUMBERS: Music group = 54, Control group = 50 patients. AGE: not described. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Classical Indian instrumental music played for 10 minutes prior to procedure and then throughout the procedure. CONTROL GROUP: no music, standard care. | PHYSIOLOGICAL OUTCOMES: BP, HR, and RR measured at beginning of the consultation and at the end of the procedure. Methods unclear. Data presented as change scores. ATTITUDE: a 3‐point VRS was used to assess willingness to undergo procedure again‐ data not extracted for review. | |
| Kwekkeboom 2003 | RCT; 3 parallel groups. | DESCRIPTION: 58 patients undergoing noxious medical procedures (e.g. tissue biopsy, vascular port placement) at an oncology clinic in Midwestern USA. NUMBERS: Music group = 24, Control group = 20, Distraction group = 14 (excluded from review). AGE, mean (SD): Music group = 51.96 (15.21), Control group = 53.30 (17.83) years old. GENDER, (male/female): Music group = 9/15, Control group = 7/13. ETHNICITY (white/other): Music group = 21/3, Control group = 20/0. INCLUSION CRITERIA: Treated by one particular surgeon. EXCLUSION CRITERIA: Unable to read/write English; incapable of completing questionnaires independently or with minor assistance from researcher. | MUSIC GROUP: Patient choice from selection of CDs (pop, rock, easy listening, classical, religious hymns, jazz or blues, country), listened via headphones prior to and during procedure. CONTROL GROUP: Standard care. Asked to rest quietly prior to and during procedure. DISTRACTION GROUP: Excluded from review. Book on tape with quiz post‐treatment. | PAIN: Pain intensity measured via a NRS prior to treatment, during treatment (retrospectively), and post treatment. ANXIETY: State anxiety measured via STAI pre‐ and post‐procedure. CONTROL: Perceived control over pain and anxiety was measured via a NRS post‐procedure. Data not extracted for review (compound question not validated). | Values provided are adjusted scores (from analysis of covariance), adjusted for baseline scores, medications, and gender. Numbers reported as SDs in the text although too small so assumed to be the standard errors, which reflect the non‐significant findings described. See Cepeda 2006 for details on music for pain relief |
| Lee 2002 | RCT; 3 parallel groups. | DESCRIPTION: 165 out‐patients undergoing elective colonoscopy in Hong Kong, China. NUMBERS: 55 patients per group. AGE, median (interquartile range): Music + PCS = 54 (46‐68); PCS alone = 47 (39‐67). GENDER (Male/Female): Music + PCS = 33/22; PCS alone = 29/26. ETHNICITY: not specified. INCLUSION CRITERIA: Scheduled for elective out‐patient colonoscopy, 16‐75 years old. EXCLUSION CRITERIA: none stated. | MUSIC ALONE: excluded from review as no appropriate control (i.e. music with no PCS). MUSIC + PCS: music played via headphones, patients offered a choice of classical, jazz, popular (Chinese or English), and Chinese opera. Patient controlled sedation administered via pump. PCS ALONE: patient controlled sedation via pump with no music or headphones. | PAIN SCORE: 10 mm VAS; SATISFACTION: 10 mm VAS; WILLINGNESS TO REPEAT SEDATION: (not included as health‐related outcome in review); PAIN MEDICATION: Dose of propofol (mg/kg) ‐ patient‐controlled sedation. EPISODES OF HYPERTENSION: systolic BP < 90 mm Hg, observed by blinded assessor (4 vs. 6 episodes in 'music + PCS' and 'PCS alone' groups respectively‐ unclear if numbers are independent). EPISODES OF OXYGEN DESATURATION: Oxygen saturation < 90%, observed by blinded assessor (no events observed). RECOVERY TIME: Assessed every 5 minutes by independent (blinded) recovery nurse until patient was orientated to person, time, and place, and able to serially subtract 7 from 100. Results presented as median and interquartile range. | See Cepeda 2006 for details on music for pain relief. |
| Lee 2005 | RCT; 2 parallel groups. | DESCRIPTION: 64 in‐patients on mechanical ventilation in an Intensive Care Unit in Hong Kong, China. NUMBERS: 32 patients per group. AGE, mean (SD): Music group = 70.6 (15.1); Control group = 68.3 (15.6). GENDER (Male/Female): Music group = 25/7; Control = 21/11. ETHNICITY: not stated. INCLUSION CRITERIA: alert, able to obey commands, able to hear, haemodynamic stability, undergoing mechanical ventilation with self‐triggering modes. EXCLUSION CRITERIA: psychiatric illness. | MUSIC GROUP: Choice of Chinese classical music, religious music (Buddhist and Christian), Western classical, natural sounds with slow beats. Played via headphones. CONTROL GROUP: Headphones without music. All patients instructed to close eyes. The lights were dimmed and the curtains were closed for all patients. Intervention and control periods lasted for 30 minutes. | ANXIETY: State anxiety using Chinese STAI ‐short version (6 items). Participants responded to questions by holding up corresponding number of fingers. RR; HR; BP; All measure taken before and after 30 minute intervention/control period. | |
| Lembo 1998 | RCT; 3 parallel groups. | DESCRIPTION: 37 patients undergoing flexible sigmoidoscopy in Calfornia, USA. NUMBERS: Audiovisual group = 13, audio alone group = 12, control group = 12. AGE, mean (SD): Audiovisual group = 58 (7), Audio alone group = 60 (8), Control group = 59 (7) years old. GENDER: Male = 37 (100%). ETHNICITY: not described. INCLUSION CRITERIA: Undergoing routine screening flexible sigmoidoscopy. EXCLUSION CRITERIA: none described. | AUDIOVISUAL: Virtual‐i glasses, personal display system showing an ocean shoreline with corresponding sounds (via headphones) AUDIO ALONE: Sounds of the ocean shoreline only played via headphones. CONTROL: No intervention, standard care. | DISCOMFORT: Measured via VAS which asked patients to rate their level of abdominal discomfort from faint to severely intense. STRESS SYMPTOMS: Measured 6 subscales (arousal, stress, anxiety, anger, fatigue, and attention) using 12 VAS. | Data extracted for review on anxiety and anger. Arousal and attention not considered health‐related outcomes. There was no difference between groups on the stress and fatigue subscales, data not reported for extraction. |
| Lepage 2001 | RCT; 2 parallel groups. | DESCRIPTION: 50 in‐patients and out‐patients undergoing non‐oncologic surgery under spinal anaesthesia in Canada. NUMBERS: 25 patients per group. AGE, mean (SD): Music group = 37.8 (12.6), Control group = 38.9 (8.6) years old. GENDER (male/female): Music group = 15/10, Control group = 16/9. ETHNICITY: not described. INCLUSION CRITERIA: ASA I or II; scheduled to undergo non‐oncologic surgery under spinal anaesthesia. EXCLUSION CRITERIA: Parturients; patients experiencing mental illness; documented hearing loss; taking drugs likely to influence mood or haemodynamic status. | MUSIC GROUP: Choice of pop, jazz, classical, and new age played via non‐occlusive headset. Patients received the music prior to, during and after surgery. CONTROL GROUP: standard care (no music). | PCS: Amount of midazolam consumed during the perioperative period was recorded. Data extracted for total midazolam consumed (mg). ANXIETY: Measured via STAI and VAS at four time points. Data presented in graph form and estimated readings of end scores taken from this. PHYSIOLOGICAL DATA: BP, HR, and RR collected in study although data not presented for extraction. There were no significant differences between groups on any of these measures. | Estimated anxiety data extracted. Physiological data not presented: n.s. |
| Lueders Bolwerk 1990 | RCT; 2 parallel groups. | DESCRIPTION: 35 in‐patients in one of 5 Intensive Care Units having had an acute myocardial infarction, Midwestern USA. NUMBERS: Music group = 17 patients, Control group = 18 patients. AGE, mean (range): Music group = 61 (36‐79), Control group = 56.3 (33 to 78). GENDER (male/female): Music group = 11/6, Control group = 16/2. ETHNICITY: not described. INCLUSION CRITERIA: Anxious patients (STAI state anxiety score ≥ 40), medical diagnosis of MI, within 48 hours of hospitalisation, patients understood they had had a "heart attack". EXCLUSION CRITERIA: Class 4 MI patient (physiologically unstable). | MUSIC GROUP: 3 sessions of music listening on 1st, 2nd, and 3rd day (or 2nd‐4th day) of hospitalisation. Music session consisted of listening to 3 pieces of music each session: Bach's 'Largo', Beethoven's 'Largo', and Dubussy's 'Prelude to the Afternoon Faun'. Each session lasted approximately 22 minutes. CONTROL GROUP: standard care, received no music sessions. | STATE ANXIETY: measured with the STAI at two time points: (1) during the first 48 hours of admission, and (2) on the 3rd or 4th day of hospitalisation. For the music group, these measurements were taken prior to the first music session and at the end of the 3rd music session. | |
| Mandle 1990 | RCT; 3 parallel groups. | DESCRIPTION: 45 patients undergoing femoral angiography in Boston, USA. NUMBERS: Music group = 14 patients, Control group = 16 patients, Relaxation tape group = 15 patients (excluded from review). AGE: not described. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: Peripheral vascular disease undergoing femoral angiography. EXCLUSION CRITERIA: not described. | RELAXATION TAPE: Progressive muscle relaxation. Excluded from review. MUSIC TAPE: Contemporary instrumental music ("Music for Airports" by Brian Eno, EG Music, New York, 1978). CONTROL GROUP: Blank tape. Participants instructed to listen to the tape throughout the entire procedure. | STATE ANXIETY: Measured via STAI immediately pre‐ and post‐procedure. PAIN: Measured using the pain rating index and the pain intensity scale of the McGill Pain Questionnaire. Pain intensity data extracted for review. NURSE RATINGS: Nurses rated the degree of pain and anxiety exhibited by each patient during the procedure on a 7‐point scale. Data not included in review. MEDICATION REQUESTS: A record of kept of the amount of Fentanyl Citrate (ųg) and Diazepam consumed. VITAL SIGNS: BP and HR were measured however no data presented. No significant differences reported. | See Cepeda 2006 for details on music for pain relief. |
| Masuda 2005 | RCT; 2 parallel groups. | DESCRIPTION: 44 post‐operative in‐patients in an Orthopaedic Department, Japan. NUMBERS: 22 patients per group. AGE, mean (SD): Music group = 67.1 (4.8), Control group = 70.8 (7.7) years old. GENDER (male/female): Music group = 9/13, Control group = 9/13. ETHNICITY: not described. INCLUSION CRITERIA: Over 60 years old; undergone surgical treatment of any kind, with general or spinal anaesthesia, in the Orthopaedic Department between April 2001 and November 2002; were required to be on post‐operative bed rest for one week or less in a private room. EXCLUSION CRITERIA: cardiovascular disease; hypertension; mental illness. | MUSIC GROUP: Choice of: Western classical music, Gagaku (Japanese traditional court music), Noh songs, or Enka. All participants choose Enka (a melodramatic and representative genre of Japanese popular songs, usually about sad aspects of life, irrecoverable destiny, and desertion by a lover, sung with a slow tempo), which is popular among elderly Japanese people. There were 10 Enka CDs to choose from. Music played via headphones for 20 minutes whilst lying in bed. CONTROL GROUP: No headphones or music. | PAIN: Measured via 10 cm VAS and the Wong/Baker Faces Pain Rating Scale (includes 6 categories of facial expressions ranging from '0, a happy smiling face' and '5, a tearful face'). VITAL SIGNS: HR and BP measured via an automatic sphygmomanometer. SKIN TEMPERATURE: Taken at the palmar centre point of the tip of the middle finger with a thermograph. Room temperature was adjusted with an air conditioner and monitored thermographically. Skin and room temperature had to be stable for 5 minutes before beginning the experiment. Patients kept their hands on top of the bed quilts. SKIN BLOOD FLOW: measured using a laser type skin blood flow analysis system (FLO‐C1, Omega Wave Co., Ltd.) with a skin contact probe taped the palmar centre point of the tip of the index finger. This device measures blood flow, blood mass, and blood velocity. Outcome measures recorded at baseline, and at 10 and 20 minutes. | See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). |
| McRee 2003 | RCT; 4 parallel groups. | DESCRIPTION: 52 in‐patients undergoing various surgical procedures in USA. NUMBERS: 13 patients in each group. AGE, mean (SD): 43.08 (13.1) years old. GENDER (male/female): 19/33. ETHNICITY: not described. INCLUSION CRITERIA: At least 18 years old; Read English; Low‐risk surgical patients (determined by pre‐operative assessment by anaesthesia provider on the ASA scale). EXCLUSION CRITERIA: Not described. Demographic information detailed includes information from study groups excluded from this review. Demographic characteristics were similar between groups. | MASSAGE THERAPY: excluded from review. MASSAGE AND MUSIC: excluded from review. MUSIC ONLY GROUP: compilation of soft piano music selected by investigator. played for 30 minutes pre‐operatively. CONTROL GROUP: Standard care, waited in the waiting room. | STATE ANXIETY: measured via the short‐form STAI‐6 in the PACU (after surgical procedure). VITAL SIGNS: BP and pulse (measured pre‐operatively, intraoperatively, and post‐operatively) measured using automatic monitoring equipment. End time‐points extracted for analysis. HORMONES: Established post‐operatively. Cortisol measured by a chemiluminescent immunoassay, and prolactin measured with a two‐site sandwich antibody assay. Blood was sent to a regional laboratory for processing. PAIN CONTROL: amount and frequency of analgesia administered, was measured in the recovery room. Data not presented although states no significant differences. | See Cepeda 2006 for details on music for pain relief (study not included in Cepeda 2006). |
| Mennegazzi 1991 | RCT; 2 parallel groups. | DESCRIPTION: 38 emergency department admissions undergoing laceration repair in Pittsburgh, USA. NUMBERS: 19 patients per group. AGE, mean (SD): Music group = 24.4 (5.1), Control group = 25.9 (7.5) years old. GENDER (male/female): Music group = 13/6, Control group = 8/11. ETHNICITY: not described. INCLUSION CRITERIA: All patients presenting to the emergency department for laceration repair. EXCLUSION CRITERIA: Laceration repair secondary to more serious medical condition; under 18 years old; received analgesics in the field; alcohol or substance intoxication. | MUSIC GROUP: Listened to music via headset. Choice of 50 styles and artists to choose from. CONTROL GROUP: Standard care. | ANXIETY: State anxiety measured via STAI before and after laceration repair. SDs presented in graphical format. Estimated figures extracted for purposes of review. PAIN: Measured via VAS after laceration repair. Estimated SDs extracted from graph. PHYSIOLOGICAL: HR, BP, RR data collected before and after laceration repair by nurses although methods of data collection unclear. | SDs for pain and anxiety are estimates from graphs. See Cepeda 2006 for details on music for pain relief. |
| Migneault 2004 | RCT; 2 parallel groups. | DESCRIPTION: 30 patients undergoing surgery with general anaesthesia, Canada. NUMBERS: 15 patients per group. AGE, mean (SD): Music group = 46.3 (12.1), Control group = 52.2 (9.1) years old. GENDER: All female. ETHNICITY: Not described. INCLUSION CRITERIA: ASA grade I‐III, 18‐70 years old, scheduled for abdominal hysterectomy, hysterosalpingo‐oophorectomy, or salpingo‐oophorectomy under general anaesthesia. EXCLUSION CRITERIA: Auditory problems, uncontrolled hypertension, Raynaud syndrome, hormonal dysfunction (adrenal, pituitary, or thyroid), steroid use, cocaine abuse, established diagnosis of severe anxiety disorder. | MUSIC GROUP: Selected a CD preoperatively from a choice of 4: classical, jazz, new‐age, popular piano music. Selected listening volume. Anesthesiologist started CD once patients were anaesthetised. Music played via headphones. CONTROL GROUP: Also selected music prior to surgery. Wore headphones during surgery however no music was played. The CD player was covered in both groups to blind the investigator. At the end of wound closure and after the last intraoperative blood sample was drawn, the CD was stopped and the headphones removed. | Repeated measures observations (4 time points)‐ T1: immediately after arterial line insertion, T2: 5 min after peritoneal incision, T3: at skin closer, T4: 30 min after arrival in the recovery area. STRESS HORMONES: Epinephrine, norepinephrine, cortisol and adrenocorticotropic hormone. PHYSIOLOGICAL OBSERVATIONS: Arterial BP; and HR. MORPHINE: Total administered via PCA for the first 24 post‐operative hours (mg). ADVERSE EVENTS: Six patients in the music group versus two patients in the control group needed rescue medication for hypertensive episodes (P value = 0.13). | Data extracted for end time points only. See Cepeda 2006 for details on music for pain relief |
| Mullooly 1998 | RCT; 2 parallel groups. | DESCRIPTION: 28 post‐operative in‐patients who have undergone elective abdominal hysterectomy, USA. NUMBERS: 14 patients in each group. AGE, mean (range): 47 (37 to 57) years old. GENDER: Female = 28 (100%). ETHNICITY (White/other): 25/3 INCLUSION CRITERIA: undergoing elective abdominal hysterectomy. EXCLUSION CRITERIA: History of drug abuse; psychiatric disorder; potential malignant neoplasm; experience with use of relaxation techniques. | MUSIC GROUP: Four easy listening selections (out of an original 10) were selected by nursing graduate students to be harmonious, pleasant, and calming. Patients listened to music for 10 minutes via headphones and were requested to close eyes on the first and second post‐operative day. CONTROL GROUP: Standard care. | PAIN: measured via VAS on first and second post‐operative day (pre and post 10 minute intervention period). ANXIETY: measured via a NRS (with VRS) pre‐ and post‐intervention period on first and second day. | Outcomes extracted for 2nd post‐operative day as only 6 and 5 outcome measures were obtained for the intervention and control group on the 1st post‐operative day (all 28 participants completed the 2nd day of testing). See Cepeda 2006 for details on music for pain relief. |
| Nilsson 2001 | RCT; 3 parallel groups. | DESCRIPTION: 90 (58 included in present review) in‐patients undergoing elective hysterectomy in Sweden. NUMBERS: Music group = 30, Control group = 28 patients. AGE, mean (SD): Music group = 51 (8.1), Control group = 50 (8.2) years old. GENDER: Female = 90 (100%), (58 included in review). ETHNICITY: not described. INCLUSION CRITERIA: ASA I‐III, scheduled for elective abdominal hysterectomy via lower abdominal incision, good understanding of Swedish. EXCLUSION CRITERIA: Hearing impairment, alcohol or drug abuse, psychiatric or memory disorder. | MUSIC GROUP: relaxing music accompanied by sea waves (ref: Uneståhl L‐E. Avslappningmusik. Träningsprogram för kropp och själ. [Relaxation music. Training programme for body and soul]. Örebro, Sweden Veje International AB: 1970). Played through headphones from time of skin incision to time of wound closure. MUSIC +THERAPEUTIC SUGGESTIONS: Excluded from review. CONTROL: playback of previously recorded operation. Played through headphones from time of incision to time of wound closure. | PAIN INTENSITY: 10‐point VAS used every hour for the first 24 post‐operative hours, and every 3 hours after that until the patient felt no pain. Data presented as group mean score of patients' median score. POST‐OPERATIVE ANALGESIA: This was recorded from the amount of patient controlled analgesia used. MOBILISATION: Estimated as time from the end of surgery to the time the patient could sit, stand, and walk without assistance. Recorded by the patient in a patient diary. POST‐OPERATIVE FATIGUE, WELLBEING, AND NAUSEA: Graded on individual VRS by the patient in a diary on the day of surgery, the day after surgery and at discharge from the hospital. | Data extracted for responses given on the day of surgery. See Cepeda 2006 for details on music for pain relief. |
| Nilsson 2003a | RCT; 3 parallel groups. | DESCRIPTION: 151 day patients undergoing surgery of varicose veins or inguinal hernia repair under general anaesthesia, in Sweden. NUMBERS: Intra‐operative music = 51, Post‐operative music = 51, Control = 49 patients. AGE, mean (SD): Intra‐operative music = 54 (14.5), Post‐operative music = 53 (14.7), Control = 54 (12.2) years. GENDER (male/female): Intra‐operative music = 39/12, Post‐operative music = 35/16, Control = 33/16. ETHNICITY: not described. INCLUSION CRITERIA: Good understanding of Swedish, ASA I‐II, 21 to 85 years old, scheduled for day‐case surgery of varicose veins or inguinal hernia repair under general anaesthesia. EXCLUSION CRITERIA: Hearing impairment, drug abuse, psychiatric or memory disorder. | INTRA‐OPERATIVE MUSIC GROUP: Music played via headphones from end of induction of anaesthesia until wound dressing via headphones. Music was soft instrumental comprising 7 melodies of a new‐age synthesizer. Post‐operatively, in the PACU, patients were exposed for 1 hour to a blank (silent) disc via headphones. POST‐OPERATIVE MUSIC GROUP: Exposed to blank disc intra‐operatively via headphones, and the same music as above for 1 hour post‐operatively in the PACU, via headphones. CONTROL GROUP: Blank disc both intra‐operatively and post‐operatively. | PAIN INTENSITY: Post‐operatively on a NRS (0 to10), every 30 minutes for 2 hours in the PACU. MORPHINE REQUIREMENTS: Total amount of post‐operative morphine requirements in the PACU recorded from patient records (mg). ANXIETY: Recorded pre‐operatively, after 1hour in the PACU, at discharge, at home in the evening of the day of surgery, days 1 and 2 following surgery in the morning and evening, on a NRS (0 to 10). FATIGUE: Using a NRS (0 to10), recorded after 1 hour in the PACU, at discharge, at home in the evening of the day of surgery, days 1 and 2 after surgery in the evening. NAUSEA: Using a NRS (0 to10), recorded after 1 hour in the PACU, at discharge, at home in the evening of the day of surgery, days 1 and 2 after surgery in the morning and evening. NIGHT SLEEP: Recorded in the morning on the 1st and 2nd day after surgery on a NRS. SATISFACTION: patient NRS rating (0 to10) of peri‐operative care. | Anxiety and fatigue not presented in enough detail. Findings on night sleep not reported at all. See Cepeda 2006 for details on music for pain relief. |
| Nilsson 2003b | RCT; 3 parallel groups. | DESCRIPTION: 182 (125 included in present review) day patients undergoing surgery for varicose veins or inguinal hernia repair under general anaesthesia, from two hospitals in Sweden. NUMBERS: Music group = 62, Control group = 63 patients. AGE, mean (SD): Music group = 53 (14.1), Control group = 52 (13.2) years old. GENDER (male/female): Music group = 44/18, Control group = 48/15. ETHNICITY: not described. INCLUSION CRITERIA: Good understanding of Swedish, ASA I‐II, scheduled for day care surgery of varicose veins or open inguinal hernia repair under general anaesthesia. EXCLUSION CRITERIA: Hearing impairment, drug abuse, known psychiatric or memory disorder. | MUSIC GROUP: Soft classical music via headphones which allow conversation to take place. Played on auto‐reverse from the time of arrival at the PACU until the patient wanted to stop listening. CONTROL GROUP: Blank tape (silence). Played from time of arrival at the PACU until the patient wanted to stop listening. MUSIC + THERAPEUTIC SUGGESTIONS: excluded from review due to psychological intervention. | PAIN INTENSITY: taken every 30 minutes until patient reports a pain level of ≤ 3 on a VAS (0 to 10). Data presented as the mean of median scores in 120 minutes. MORPHINE REQUIREMENT (mg): taken from the patient records. ANXIETY: recorded using the STAI, pre‐operatively at the hospital, and post‐operatively at home on the day of the surgery. SYMPTOMS: well‐being, nausea, headache, fatigue, and urinary problems recorded using VRSs post‐operatively at home in the evening of the day of the surgery. | There was a significant difference in the length of time patients listened to their allocated tape.
Music group = 117.0 (50.6) minutes
Blank tape group = 80.2 (44.9) minutes. See Cepeda 2006 for details on music for pain relief. |
| Nilsson 2005 | RCT; 3 parallel groups. | DESCRIPTION: 75 day patients undergoing surgery of open Lichtenstein inguinal hernia repair, in Sweden. NUMBERS: 25 patients in each group. AGE, mean (SD): Intra‐operative music = 55 (14.7), Post‐operative music = 56 (16.8), Control = 57 (11.6) years. GENDER: 24 males per group, 1 female per group. ETHNICITY: not described. INCLUSION CRITERIA: ASA grade I‐II, scheduled for day care surgery between 8 and 11.30am of open Lichtenstein inguinal hernia repair under general anaesthesia. EXCLUSION CRITERIA: Hearing impairment, diabetes mellitus, treatment with corticosteroids. | INTRA‐OPERATIVE MUSIC GROUP: exposed to new‐age synthesizer music during operation, and a sham (silent) CD for 1 hour post‐operatively in the PACU. POST‐OPERATIVE MUSIC GROUP: exposed to sham (silent) CD intra‐operatively, and new‐age synthesizer music for 1 hour post‐operatively in PACU. CONTROL GROUP: Exposed to sham (silent) CD both intra‐operatively and for 1 hour post‐operatively. All patients wore headphones throughout. Intra‐operative headphones were occlusive to block out other sounds; post‐operative headphones allowed conversation between patients and staff. Intra‐operative period ran from end of anaesthesia induction to after wound dressing at the end of the surgery. | PAIN: assessed by NRS (0 to 10), 30 minutes before anaesthesia and 1 hour after admission to PACU. ANXIETY: same as pain score. BP, HR, and OXYGEN SATURATION: assessed at same time points as pain, using a digital BP monitor and pulse oximetry. MORPHINE REQUIREMENTS: total amount used in the PACU was recorded (mg). SERUM CORTISOL, BLOOD GLUCOSE LEVELS, and SERUM IgA LEVELS: taken at 5 time points: 30 minutes prior to anaesthesia, at the end of surgery after wound dressing, and at the 1st, 2nd, and 3rd hour after arrival at the PACU. Not enough data presented for extraction. | Data extracted for post‐operative music group versus control group. See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). |
| Nowobilski 2005 | RCT; 2 parallel groups. | DESCRIPTION: 36 in‐patients with bronchial asthma, in Poland. NUMBERS: 18 patients per group. AGE, mean (SD): Music group = 44.9 (15.9), Control group = 47.4 (13.4) years old. GENDER (male/female): 13/23. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Underwent 10 day rehabilitation programme, including 45 minutes each day of: exercise of breath control, correction of respiratory pattern, training of diaphragm and additional respiratory muscles, plus an additional 15 minutes of music listening (C.M. Weber "Adagio"; J.S. Bach "Air on a G‐string"; V.A. Mozart "Andante z Divertimenta D‐dur"). CONTROL GROUP: Underwent 10 day rehabilitation programme, including 45 minutes each day of: exercise of breath control, correction of respiratory pattern, training of diaphragm and additional respiratory muscles. Did not receive additional music listening. | ANXIETY: Measured via the STAI at baseline and after the 10th session. There was no significant difference between groups: F (1,34) = 0.37, P value = 0.55 DYSPNEA: Measured via the Borg dyspnoea scale at baseline and after the 10th session. There was no significant difference between groups: F (1, 32) = 1.02, P value = 0.32 | Data not provided in sufficient detail for extraction. |
| Padmanabhan 2005 | RCT; 3 parallel groups. | DESCRIPTION: 104 day‐patients scheduled for elective surgical procedures (gynaecology, general surgery, urology) in a Day Surgery Unit in England. NUMBERS: Music + binaural beat = 35 patients, Music only = 34 patients, Control = 35 patients. AGE: not described. GENDER (male/female): Music+binaural beat = 12/23, Music only = 12/22, Control = 15/20. ETHNICITY: not described. INCLUSION CRITERIA: Scheduled to undergo elective surgery with general anaesthetic. EXCLUSION CRITERIA: History of epilepsy, < 16 years old, history of profound deafness. | MUSIC + BINAURAL BEAT: taken to a quiet environment pre‐operatively and asked to listen to music with their eyes closed; 30 minute soundtrack (Holosync Solution, 'Awakening Prologue', Centerpointe Research Institute, Beaverton, OR) which produces binaural beats (through two similar pure tones being presented separately to each other). MUSIC ONLY: taken to a quiet environment pre‐operatively and asked to listen to music with eyes closed; Identical soundtrack to above without the added tones. CONTROL: standard care, allowed to read or watch television for 30 minutes pre‐operatively. | STATE ANXIETY: measured via the STAI before and after intervention period. Results converted to percentages instead of presenting STAI score. | It is unclear if > 90% of participants are 18 years old or over. Data extracted for music only group versus control group. Confidence intervals have been used to estimate standard deviations for purposes of review. |
| Palakanis 1994 | RCT; 2 parallel groups. | DESCRIPTION: 50 out‐patients undergoing flexible sigmoidoscopy in Maryland, USA. NUMBERS: 25 patients per group. AGE, mean (range): Music group = 55 (22 to 76), Control group = 49 (20 to 79). GENDER (male/female): Music group = 17/8, Control group = 20/5. ETHNICITY: not described. INCLUSION CRITERIA: scheduled for out‐patient flexible sigmoidoscopy. No patients were taking anxiolytic medications. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Choice of 20 tapes (classical/country‐western/popular/rhythm and blues/gospel) played via headphones throughout the procedure. CONTROL GROUP: Standard care. | ANXIETY: Measured via STAI. An analysis of variance identified a significant difference between groups (P < 0.002): Music group = 25.24 Control group = 31.48 PHYSIOLOGICAL: BP and HR measured via Dinamap Model 845XT before and during the procedure (at full insertion of the sigmoidoscope). Paper reports significantly less change in HR and mean arterial BP for the music group. Mean HR: Music group: Before = 86 bpm; During = 84 bpm Control group: Before = 75 bpm; During = 80 bpm Mean arterial BP: Music group: Before = 111; During = 110 mm Hg Control group: Before = 104; During = 115 mm Hg | No SDs reported. Insufficient data for extraction. |
| Phumdoung 2003 | RCT; 2 parallel groups. | DESCRIPTION: 110 in‐patients giving birth for the first time (to a singleton fetus), in Southern Thailand. NUMBERS: 55 in each group. AGE (mean, SD): 24 (3) years old. GENDER: Female = 110 (100%). ETHNICITY: not described. INCLUSION CRITERIA: Married primiparas, 20 to 30 years old, with a singleton fetus, received antenatal care from the 2nd trimester, been in the latent phase of labour for no more than 10 hours, normal fetal heart rate, cephalic presentation, vertical lie, 38 to 42 weeks gestation with estimated fetal weight of 2500 to 4000 grams. EXCLUSION CRITERIA: Received analgesic medication, difficulty hearing the spoken word, induced labour, infections, HIV, asthma, previous negative reaction to music, had a spontaneous membrane rupture for longer than 20 hours, history of psychiatric problems, major antipsychotic medications. | MUSIC: patient choice of western music without lyrics, including synthesizer, harp, piano, orchestra, and jazz (60‐80 bpm). Patients listened to their choice via headphones for the first 3 hours of the active phase of labour, starting when cervical dilation was 3 or 4 cm with uterine contraction of 30 to 60 seconds. Women could stop listening to music for 10 minutes if they wished. CONTROL: No music or headphones, but were told that they would receive music at a later time during labour, after all the pain measurements had been taken. | PAIN SENSATION: measured using 100 mm VAS at four time points‐ once at the start of the study before the treatment period, and then every hour for 3 hours. PAIN DISTRESS: measured in the same manner as pain sensation. There was a small ceiling effect reported in the second hour for 4% of controls, and in the 3rd hour for 7% of controls and 5% of the music group. | See Cepeda 2006 for details on music for pain relief. |
| Schiemann 2002 | RCT; 2 parallel groups. | DESCRIPTION: 119 patients undergoing diagnostic endoscopy in Germany. NUMBERS: Music group = 59, Control group = 60 AGE, mean (SD): Music group = 52.3 (13.9), Control group = 55.8 (13.5) years old. GENDER (male/female): Music group = 25/34, Control group = 33/27. ETHNICITY: not described. INCLUSION CRITERIA: 18 to 80 years old. EXCLUSION CRITERIA: History of partial colectomy, gastrectomy, or hysterectomy; Impassable colonic stenosis due to a tumour, chronic inflammatory bowel disease, or diverticulitis. | MUSIC GROUP: Played Radio Arabella (105.2 MHz) throughout the procedure. This is a well‐known regional broadcasting company in Munich, and plays various trends of pop, rock, soul, and 'Deutsche Schlager' music, specialising in 'oldies'. CONTROL GROUP: Standard care. | SEDATION & ANALGESIA: Number of patients requiring midazolam and pethidine, and amount administered. It is unclear from the report if sedation is an outcome measure or baseline characteristic. TIME: Examination time and number of colonoscopies prematurely aborted due to pain were recorded. OXYGEN: Number of patients requiring oxygen supplementation was recorded. | See Cepeda 2006 for details on music for pain relief. |
| Schneider 2001 | RCT; 2 parallel groups. | DESCRIPTION: 30 patients undergoing cerebral angiography in Hannover, Germany. NUMBERS: 15 patients per group. AGE, mean (range): Music group = 42.1 (26‐58), Control group = 44.3 (25 to 59) years old. GENDER (male/female): 14/16. ETHNICITY: not described. INCLUSION CRITERIA: Undergoing cerebral angiography for the first time. EXCLUSION CRITERIA: hypertension; cardiac dysrhythmia; anaemia; endocrine disease; psychiatric problems; infections; use of sedative, anxiolytic, or illegal drugs. | MUSIC GROUP: Choice of nine tapes (international pop, German pop, oldies, meditation, rock, techno, instrumental, classic, and traditional). Played via stereo speakers throughout the angiogram; patients could adjust the volume. CONTROL GROUP: No music (standard care). | ANXIETY: Measured via STAI the evening before the angiography and during the angiography. ENDOCRINE: Cortisol and catecholamines were taken through an indwelling IV catheter four times: 1) before placing patient on the angiographic table, 2) before giving local anaesthetic, 3) after the first angiographic run, and 4) before returning to bed. PHYSIOLOGICAL: BP and HR were measured continuously every 5 minutes by a non‐invasive system. | Data not sufficient for extraction. There were no significant differences between groups in anxiety or HR. BP decreased significantly in music group but remained constant in the control group. The control group had a significant increase in cortisol over the angiogram. Cortisol remained constant in the music group. There were no differences between groups in adrenaline and noradrenaline levels. |
| Sendelbach 2006 | RCT; 2 parallel groups. | DESCRIPTION: 86 post‐operative in‐patients who have undergone cardiac surgery, in cardiovascular units, Midwest USA. NUMBERS: Music group = 50, Control group = 36 AGE, mean (SD): Music group = 62.3 (14.8), Control group = 64.7 (11.4). GENDER (male/female): music group = 31/19, Control group = 29/7. ETHNICITY: not described. INCLUSION CRITERIA: Scheduled for non‐emergent coronary artery bypass and/or valve replacement surgeries. EXCLUSION CRITERIA: Non‐English speaking; intubated; physician‐documented psychiatric disorder. | MUSIC GROUP: Participants advised to clear minds and allow muscles to relax. They were given a choice of easy listening, classical, or jazz music, played via headphones, for 20 minutes whilst participant remained in bed. Music qualities were: no dramatic changes, consonance, instrumental, 60 to 70 bpm. The environment was made conducive to rest. CONTROL GROUP: 20 minute rest period. Advised to rest in bed and a comfortable position was encouraged. No relaxation suggestions were given. Interventions were for 20 minutes, two times a day, in the morning and evening, of the post‐operative days 1 to 3. | HR: Recorded on bedside monitor. No differences between groups. BP: Recorded on bedside monitor or with BP cuff. No differences between groups. ANXIETY: Recorded with short form state anxiety scale. Significantly lower in the music group. PAIN: Recorded on an NRS. Significantly lower in the music group. OPIOD REQUIREMENT: No differences between groups. | Paper only reports data for the first 3 sessions due to missing data. SDs obtained from authors (unpublished). Data extracted for morning session of the first post‐operative day. See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). |
| Smith 2001 | RCT; 2 parallel groups. | DESCRIPTION: 42 male out‐patients undergoing radiation therapy in a Veterans Affairs Hospital in Southeastern USA. NUMBERS: Music group = 19 patients, Control group = 23 patients AGE: mean (range): Music group = 62.2 (39‐78), Control group = 63.4 (44 to 80). GENDER: Not described. ETHNICITY: Caucasian/African‐American/Hispanic/Other: Music group = 11/4/4/0, Control group = 20/1/1/1. INCLUSION CRITERIA: Expected to receive at least 5 weeks of radiation therapy; 18 years or older; Able to read and understand English. EXCLUSION CRITERIA: Hearing impaired; overtly psychotic; previous diagnosis of anxiety or currently taking anxiolytic medications; participating in a radiation therapy setup that precludes the use of headphones. | MUSIC GROUP: Patient choice of rock and roll, big band, country and western, classical, easy listening, Spanish, religious. Four to six tapes were available in each category. Each patient could choose one category for the duration of the study. Patients listened via headphones to the music before and during the radiation simulation appointment, and during daily radiation treatments for the duration of course of therapy. CONTROL GROUP: Standard care. | STATE ANXIETY: measured using the STAI at 5 time points: (1) time of evaluation; (2) post simulation appointment; (3) end of first week of treatment; (4) end of third week of treatment; and (5) end of the fifth week or end of radiation therapy. | Data extracted for end time point. Standard deviations derived from P value of a t‐test. |
| Smolen 2002 | RCT; 2 parallel groups. | DESCRIPTION: 32 out‐patients undergoing colonoscopy, USA. NUMBERS: 16 patients in each group. AGE, mean (SD): Music group = 58.63 (13.64), Control group = 61. 06 (9.48) years old. GENDER (male/female): Music group = 10/6, Control group = 7/9. ETHNICITY: Not described. INCLUSION CRITERIA: Scheduled for ambulatory colonoscopy with an admitting diagnosis of personal history of colorectal cancer, colon polyps, long‐standing ulcerative colitis, or significant family histories of colorectal neoplasia; 18 years and older; conscious, orientated; able to read, write, and speak English; evidenced haemodynamic stability by BP between 90 to 160 mm Hg systolic and 50 to 95 mm Hg diastolic. EXCLUSION CRITERIA: Taking anti‐anxiety or anti‐depressant medication; unable to engage in verbal conversation throughout the procedure and into the recovery phase. | MUSIC GROUP: Patient choice of classical, jazz, pop rock, easy listening, played via headphones throughout pre‐sedation and procedure. CONTROL GROUP: Standard care. | SEDATION REQUIREMENTS (mg). Amount of Versed and Demerol administered was recorded (not a primary outcome). STATE ANXIETY: measured using STAI before and after the procedure. HR (bpm) and BP (mm Hg): measured using Critikon Model SNK9935 at four time points: on admission, 5 minutes after medication, 5 minutes after procedure, and immediately before discharge. Data presented in graphs, not extracted as unclear what lines represent (e.g. SD or 95% CI). | State anxiety data extracted from graph in article, bars taken as standard errors and converted into SD. |
| Staricoff 2003f | RCT; 2 parallel groups. | DESCRIPTION: 17 in‐patients with HIV/AIDS staying in the HIV/AIDS ward, London, UK. NUMBERS: Music group = 8, Control group = 9. AGE: not described. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: Clinicians performed clinical assessment of hospitalised patients and sent a list of nominated patients to the study personnel for randomisation. No further details given. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Attended a live music concert played in the public area on the hospital ground floor. Unclear what type of music was played. CONTROL GROUP: Remained on the ward, where they could not hear the music. | LEVELS OF CD4 AND CD8 LYMPHOCYTES (cells/mm3): measured within one hour before and after the study period. There was no difference in the number of CD4 cells before and after the concert in either group. Paper reports that the number of CD8 cells increased in the music group, and remained unchanged in the control group. Table of results suggest that CD8 cells decreased in the control group and increased in the music group. Change score (post‐pre): Music group (n = 8) = 77 Control group (n = 9) = −78 Paper reports a t‐test to show statistical significance (P value = 0.01, 95% CI 40 to 269). Estimated SDs (not reported) = 150 | Data insufficient detail. |
| Tang 1993 | RCT; 2 parallel groups. | DESCRIPTION: 120 in‐patients undergoing surgery with epidural anaesthesia in Taiwan. NUMBERS: 60 patients in each group. AGE, mean (SD) years: Music group = 42.18 (11.82); Control group = 41.92 (14.22). GENDER (male/female): Music group = 26/34; Control group = 32/28. ETHNICITY: not stated. INCLUSION CRITERIA: To undergo surgery with epidural anaesthesia; ASA grade I‐II. EXCLUSION CRITERIA: Patients who wish to switch study group. Patients who request tranquillisers. | MUSIC GROUP: Walkman music via headphones. Choice of 5 types (Manderin pop song, local Taiwanese folksong, Western, Classical, Buddhist hymn). Music played throughout operation. CONTROL GROUP: No music, standard care. | Subjective feelings of anxiety and sedation: Method of assessment unclear (data EXCLUDED from review). HR (bpm) and BP (mm Hg): Repeated measures (7 time points). Outcomes reported as means and SD taken at baseline and 20 minutes into operation. | |
| Taylor 1998 | RCT; 3 parallel groups. | DESCRIPTION: 61 in‐patients who have had an elective abdominal hysterectomy using general anaesthesia in Arizona, USA. NUMBERS: Unclear how many participants assigned to each group. AGE, mean (SD): Music group = 40.7 (7.29); Headphones only group = 43.3 (7.79); Control = 34.6 (6.13). The control group were significantly younger than the intervention groups. GENDER: Female = 61 (100%). ETHNICITY: not specified. INCLUSION CRITERIA: All patients scheduled for elective abdominal hysterectomies using general anaesthesia. EXCLUSION CRITERIA: hearing or visually impaired, unable to communicate in English. | MUSIC GROUP: patient choice brought from home or from selection provided (classical; jazz; light rock; country; rock and roll; easy listening; gospel), played via headphones. HEADPHONES ONLY GROUP: headphones without music were used to block out unpleasant sounds in the PACU. CONTROL GROUP: No headphones or music, standard care. Interventions took place post‐operatively in the PACU. | PAIN INTENSITY: Two measures used: a 9‐inch VAS, and a 10‐point NRS. Measures were taken every 15 minutes for the duration of PACU stay (unspecified). Results of VAS are reported as a mean value for each group; results of NRS are reported as mean rating at 1 hour and at discharge from PACU. | See Cepeda 2006 for details on music for pain relief. |
| Taylor‐Piliae 2002 | RCT; 3 parallel groups. | DESCRIPTION: 30 pre‐operative in‐patients scheduled to undergo cardiac catheterization (CC) in Hong Kong, China. NUMBERS: 15 patients in each group. AGE, mean (SD): music group = 56.9 (10.3), control group = 65 (6.9). GENDER (Male/Female): Music group = 12/3, Control group = 11/4. ETHNICITY: Chinese = 30 (100%). INCLUSION CRITERIA: admitted for CC, ethnic Chinese, literate in Chinese, 35 to 75 years old. EXCLUSION CRITERIA: diagnosed mental illness, major hearing difficulties, life threatening or concomitant major illness (e.g. renal failure/cancer). | SENSORY INFORMATION: excluded from review. MUSIC GROUP: Instrumental music without words, choice of new age, Chinese instrumental, or classical music. CONTROL GROUP: standard care. The study period was 1 hour before CC and lasted for 15 to 20 minutes. | STATE ANXIETY: measured via STAI before and after intervention period; MOOD: measured via POMS questionnaire. UNCERTAINTY: measured via Mishel's Uncertainty in Illness Scale. HR (bpm) taken manually for 1 minute by researcher. RR recorded manually for 1 minute by researcher. Outcomes were collected at: (T0) baseline, (T1) after the study intervention (pre‐procedure), and (T2) approximately 1 hour after cardiac catheterization. | Outcomes extracted for T1 ‐ after the study intervention but before cardiac catheterization, as the study has been categorised in the "pre‐procedure" subgroup. |
| Triller 2006 | RCT; 2 parallel groups. | DESCRIPTION: 200 patients undergoing flexible bronchoscopy in Slovenia. NUMBERS: Music group = 93, Control group = 107. AGE, mean (SD): Music group = 58.6 (14.9), Control group = 59.6 (14.5) years old. GENDER (male/female): Music group = 64/29, Control group = 77/30. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Easy listening and relaxation ambient music selected by the investigator, started immediately after the beginning of the procedure and stopped when the procedure is over. CONTROL GROUP: Standard care. Bronchoscopist team asked not to communicate aloud with each other during the procedure. | PHYSIOLOGICAL: HR and BP recorded before and after the procedure, method of data collection not described. FEELINGS: Overall feelings during the procedure were measured using a VAS. This outcome was not extracted for the review due to questionable validity. | |
| Tsuchiya 2003 | RCT; 2 parallel groups. | DESCRIPTION: 59 in‐patients undergoing elective laparoscopic cholecystectomy in an operating theatre in Japan. NUMBERS: Nature sounds = 29, Control = 30. AGE, mean (SD): Nature sounds = 65 (10), Control = 66 (9) years old. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: ASA grade I‐II, scheduled for elective laparoscopic cholecystectomy. EXCLUSION CRITERIA: angina; essential hypertension; auditory perception complications. | NATURE SOUNDS: Patients were played their choice of nature sounds via headphones throughout operation, after induction of anaesthesia until the last suture of surgery. CONTROL: Patients wore dummy headphones so were exposed to the operating theatre noise. They were not played nature sounds during operation, after induction of anaesthesia until the last suture of surgery. All patients choose a set of sounds they felt to be calming and comforting in the pre‐operative period. These sounds included familiar Japanese environmental sounds including: sounds of a ripple, a small stream, a soft wind, and a twitter. They all listened to their selected sounds via headphones to determine a comfortable volume. All participants listened to sounds for at least 30 minutes to familiarise themselves with them, prior to operation. | PHYSIOLOGICAL MEASURES: BP and HR was recorded through 'non‐invasive' methods using the Philips patient monitoring system for anaesthesia [unpublished]. Outcomes were measured pre‐anaesthesia, at the start of surgery, at gallbladder removal, at the end of surgery, at extubation, at the end of anaesthesia, and in the PACU. Patients in the control group had higher BP and HR at extubation than those in the nature sounds group (P value < 0.05). All other time‐points were non‐significant. EXPERIENCE OF ANAESTHESIA: Unclear validity, 10‐point VAS from 'acceptable' to 'not acceptable'. | Data insufficient detail for extraction. Authors unable to provide means and SDs for physiological measures. |
| Twiss 2006 | RCT; 2 parallel groups. | DESCRIPTION: 60 in‐patients undergoing coronary artery bypass graft or vascular surgery, in the OR and ICU, Florida, USA. NUMBERS: Music group = 30, Control group = 30. AGE, mean (SD): Music group = 72.6 (2.1), Control group = 75.1 (3.4) years old. GENDER (male/female): Music group = 10/20, Control group = 10/20. ETHNICITY: not described. INCLUSION CRITERIA: Orientated to person, time, and place on admission; not currently using music therapy intervention; able to hear music played with the CD player; available the night before surgery to meet with investigator and take the baseline STAI. EXCLUSION CRITERIA: It is UNCLEAR if patients < 65 years old were excluded. | MUSIC GROUP: Choice of 6 discs played during surgery and post‐operatively. Family encouraged to bring in additional music choices post‐operatively. Music selection from Prescriptive Music Inc., ('Clarity'‐ melodies from classical motion pictures; 'Timeless'‐ heartfelt originals, 'Towards'‐ piano improvisation, 'Interlude'‐ piano music by Mozart, 'Universe'‐ synthesized compositions, 'Essence'‐ cello and piano). CONTROL GROUP: Standard care. | ANXIETY: Measured via the STAI on the 3rd post‐operative day. INTUBATION TIME: Recorded in minutes. | |
| Voss 2004 | RCT; 3 parallel groups. | DESCRIPTION: 61 post‐operative in‐patients following open heart surgery undergoing 30 minutes chair rest, in the surgical intensive care unit of a rural Midwestern hospital, USA. NUMBERS: Music group = 19, rest group = 21, control group = 21. AGE, mean (SD): 63 (13) years old. GENDER (male/female): 39/22. ETHNICITY (White/American Indian): 52/8. INCLUSION CRITERIA: 1st post‐operative day following open heart surgery. Morning chair rest ordered. At least 18 years old. No major hearing deficit. Stable condition. Alert, orientated, able to follow commands. Read/write/understand English. EXCLUSION CRITERIA: Femoral arterial sheath remained in place after surgery. | MUSIC GROUP: Instructed to listen and follow music and allow it to distract and relax. Played through headphones. 6 choices: synthesizer, harp, piano, orchestra ,slow jazz, flute. 30 second excerpts provided for choice. Phone unplugged, blinds closed, lights dimmed and door closed. Do not disturb sign placed on door. REST GROUP: Phone unplugged, blinds closed, lights dimmed and door closed. Do not disturb sign placed on door. CONTROL GROUP: Activity as normal. | ANXIETY: Anxiety about chair rest measured via 100 mm VAS. PAIN SENSATION: measured via 100 mm VAS. PAIN DISTRESS: measured via 100 mm VAS. | Change scores extracted for anxiety. See Cepeda 2006 for details on music for pain relief (study not included in Cepeda 2006). |
| Wang 2002 | RCT; 2 parallel groups. | DESCRIPTION: 93 pre‐surgical out‐patients, to undergo elective surgery (ear‐nose‐throat; orthopedics; plastics; or other general minor surgery), in USA. NUMBERS: Music group = 48, Control group = 45. AGE, mean (SD): Music group = 44 (11), Control group = 41 (11) years old. GENDER (male/female): Music group = 56/44, Control group = 61/39. ETHNICITY (White/African‐American/Other): Music group = 38/8/2, Control group = 37/6/2. INCLUSION CRITERIA: Aged 18 to 65 years old; ASA grade 1 to 3; Scheduled to undergo anaesthesia and elective out‐patient surgery. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Music played for 30 minutes via headphones prior to surgery in a hospital isolation room. Participants brought their own choice of music from home. CONTROL GROUP: Wore headphones but did not listen to any music or white noise. In hospital isolation room. Condition lasted 30 minutes. No hospital personnel were allowed in the room during the experiment. The experimenter waited outside the room. Persons accompanying the participant were allowed in the room, and participants were allowed to read and converse during the experiment. | ANXIETY: Measured via STAI before and after experiment. HR: Measured via Biolog monitoring system. BP: Method of measurement unclear. SKIN CONDUCTANCE: Continually monitored with a Biolog ambulatory recording system (Model 3992/2). HORMONES: Plasma catecholamines (cortisol, epinephrine, and norepinephrine) were obtained before and after experimental condition via blood sampling. Outcomes were obtained through radioimmunoassay then through high‐performance liquid chromatography and an electrochemical detector. | Outcomes are expressed as a percentage of the baseline score (mean and SD). |
| White 1992 | RCT; 2 parallel groups. | DESCRIPTION: 40 in‐patients in acute care unit for acute myocardial infarction in Midwest USA. NUMBERS: 20 patients per group. AGE, mean (SD): 55.7 (7.57) years old. GENDER (male/female): 29/11. ETHNICITY (Euro‐American/African‐American): 36/4. INCLUSION CRITERIA: Stable condition; confirmed diagnosis of acute MI; State anxiety > 40; Alert and orientated; Able to read and write English. EXCLUSION CRITERIA: Interrupted during the study. | MUSIC GROUP: listened to 4 adagios selected by the investigator for 25 minutes. Primarily string composition, low‐pitched, simple and direct musical rhythm, tempo approximately 60 bpm. Played via headphones. CONTROL GROUP: received 25 minutes of uninterrupted rest. | ANXIETY: state anxiety measured via STAI. HR and RR measured by auscultation for 30 seconds. | |
| White 1999 | RCT; 3 parallel groups. | DESCRIPTION: 45 in‐patients who had an acute MI, in private rooms in an ICU in Midwest USA. NUMBERS: 15 patients per group. AGE: mean = 63 years old. GENDER (male/female): Music group = 13/2, Rest group = 10/5, Control group = 11/4. ETHNICITY (African‐American/White/Hispanic): Music group = 2/13/0, Rest group = 4/10/1, Control group = 2/12/1. INCLUSION CRITERIA: Confirmed acute MI within previous 72 hours; haemodynamic condition stable enough for participation (determined by nurse); alert and orientated; primary cardiac rhythm originating from the sinoatrial node. EXCLUSION CRITERIA: Receiving mechanical ventilation. | MUSIC GROUP: Experimenter selected classical music, played via headphones. Asked to assume a comfortable position in bed, lights lowered, telephones unplugged, curtains drawn, doors closed, advised to clear mind and let muscles relax. 20 minutes. REST GROUP: 20 minutes uninterrupted rest (experimenter outside door). Asked to assume comfortable position in bed, lights lowered, telephones unplugged, curtains drawn, doors closed, advised to clear mind and let muscles relax. CONTROL GROUP: activities as normal (standard care). | PHYSIOLOGICAL: HR (chart extraction), RR (auscultation with a stethoscope for 30 seconds), BP (non‐invasive automatic oscillometric BP cuff), measured pre, immediately post and at 1 and 2 hours post the intervention period. Heart rate variability determined using power spectral analysis and fast Fourier transform from 3 hours of continuous electrocardiographic data (30 minutes pre to 2 hours post intervention period). ANXIETY: Measured via state portion of STAI pre and immediately post intervention. | Data presented as mean and SE. SEs converted into SDs for purposes of review. Data extracted for measures immediately after 20 minute intervention period. Data extracted for HR, RR, BP, and anxiety, for purposes of review. Data not extracted for Rate pressure product or high‐frequency HR. |
| Winter 1994 | RCT; 2 parallel groups. | DESCRIPTION: 50 day patients scheduled for elective same‐day surgery of gynaecological procedures (e.g. exploratory laparoscopies, laparoscopic tubal ligation, ovarian cysts excision, and intrauterine device removal), in New Jersey, USA. NUMBERS: Music group = 31 patients, Control group = 19 patients. AGE, mean (SD): Music = 37 (8), Control = 37 (8). GENDER: Female = 50 (100%). ETHNICITY: not stated. INCLUSION CRITERIA: Not described. EXCLUSION CRITERIA: Not described. | MUSIC GROUP: Choice of classical, country, jazz, popular, or show music, played via headphones. CONTROL GROUP: Standard care. The intervention period took place in the surgical holding area prior to the patients' gynaecological procedure. Pre‐operative stay in holding area was 50 (+/‐ 20) minutes. | ANXIETY: State and trait anxiety via STAI on entry and exit of holding area. Results reported as Mean +/‐ SEM. BP and HR: Taken on arrival in the surgical holding area and again just before going to the Operating Room (secondary outcomes). | Anxiety data presented as mean and SEs. SEs converted into SDs for purposes of review. |
| Wong 2001 | RCT; cross‐over study (2 allocation groups). | DESCRIPTION: 20 ventilator‐dependent in‐patients in an ICU in Hong Kong, China. NUMBERS: Music group = 20 patients, Scheduled rest = 20 patients (cross‐over design). AGE, mean (SD): 58.25 (15.53) years old. GENDER (male/female): 15/5. ETHNICITY: Chinese = 20 (100%). INCLUSION CRITERIA: Chinese; understand Cantonese or English; 18 to 85 years old; alert, mentally competent; without hearing problems; able to communicate by holding up fingers in response to researchers' questions; undergoing mechanical ventilation with self‐triggering; haemodynamically stable. EXCLUSION CRITERIA: Receiving any continuous intravenous analgesia; receiving any inotropic support; enrolled in previous similar studies. | MUSIC GROUP: Choice of 7 cassettes (Chinese folk song; Chinese instrumental music; Chinese music with western instruments; Buddhist music; Western classic; Western movie music; piano music). Participants instructed to close eyes and focus on the flow of the music. SCHEDULED REST GROUP: Dimmed lights, drawn curtains (if in cubicle) or closed door (if in single room). Instructed to close eyes and rest. Interventions lasted 30 minutes with an interval of at least 6 hours between the two interventions. Visitors were allowed to stay during the experimental and control interventions. | STATE ANXIETY: short‐form STAI, patients held up appropriate number of fingers in response to questions. Taken before and after each intervention. RR: breaths per minute counted via observation. BP (mm Hg): measured with the means of indwelling arterial lines recorded on the bedside cardiac monitor. RR and BP recorded every 5 minutes during intervention periods (7 measurement points). | This cross‐over study has not reported patient‐specific differences between the two intervention measurements. Therefore, the data has been extracted as if it is independent groups (as there was not enough data to calculate a correlation coefficient). |
| Yang 2003 | RCT; 2 parallel groups. | DESCRIPTION: 39 patients undergoing eye operations with anaesthetics and analgesics in China. NUMBERS: Music group = 19 patients; Control group = 20. AGE, mean years: Music group = 39; Control group = 37. GENDER: Male = 39 (100%). ETHNICITY: not stated. INCLUSION CRITERIA: 18 to 60 years old, with a baseline anxiety score of more than 40. EXCLUSION CRITERIA: not stated. | MUSIC GROUP: Given a choice of 3 musical styles (pop, light, classical) with each type including 4 songs. Patients were asked to listen to the music 2 to 3 times the night before the operation and relax (not clear if patients were in‐patients). Patients then listened to the music throughout their operation. CONTROL GROUP: Were given a pre‐operative visit but were not given a music tape. These patients received standard care during their operation. | ANXIETY: STAI presented as change scores. DEPRESSION: Self‐rating Depression Scale (SDS) presented as change scores. CONCERN / WORRY: via VAS (0 to 10) taken before, during, and after surgery. BI: Bispectral Index measured via EEG. | |
| Yung 2003 | RCT; 2 parallel groups. | DESCRIPTION: 66 pre‐operative surgical patients in the OR holding area in Hong Kong, China. NUMBERS: 33 patients in each group. AGE, mean (range): 64.7 (21 to 89) years old. GENDER: Male = 66 (100%). ETHNICITY: Chinese = 66 (100%). INCLUSION CRITERIA: Volunteer surgical patients; 50 to 80 years old (this does not reflect age range provided in table); comprehend written and verbal instructions; have prior surgical experience. EXCLUSION CRITERIA: auditory impairment; received preoperative sedation; cardiac and respiratory disease; history of hypertension. | MUSIC GROUP: Slow music played via headphones for 20 minutes pre‐operatively. Participants had a choice of 3 tapes‐ Chinese instrumental, Western instrumental, or Western and Chinese slow songs. CONTROL GROUP: Standard care. | ANXIETY: State anxiety measured via C‐STAI pre‐ and post‐intervention period. PHYSIOLOGICAL: BP and HR measured with an automated monitor (Dinamap 1846‐SX) before and after intervention period. RR measured through observing the number of chest movements. | |
| Zhang 2005 | RCT; 2 parallel groups. | DESCRIPTION: 110 in‐patients undergoing abdominal hysterectomy in China. NUMBERS: 55 patients in each group. AGE, mean (SD): Music group = 41 (5) years old; Control group = 41 (3) years old. GENDER: Female = 110 (100%). ETHNICITY: not described. INCLUSION CRITERIA: ASA I‐II; scheduled for elective total abdominal hysterectomy under spinal‐epidural anaesthesia. EXCLUSION CRITERIA: Hearing impairment; drug abuse; known psychiatric disorders or memory disorders. | MUSIC GROUP: Patient choice of music they felt to be calming and comforting, played via headphones intraoperatively, from 6 minutes before skin incision and 1 minute before the loading dose of anaesthesia to wound closure CONTROL GROUP: Wore headphones without sound or music. | PHYSIOLOGICAL: BP, HR, Bispectral Index recorded at 10‐minute intervals during surgery. Results reported as baseline and mean score during surgery (during target sedation period). SEDATION: Level of alertness graded using the OAA/S at 10‐minute intervals. Time to sedation (OAA/S score = 3) reported (mins). PROPOFOL: amount of intra‐operative propofol (mg) recorded. SATISFACTION: patient's satisfaction with the peri‐operative care measured using a 10 cm VAS one day after surgery. SERUM INTERLEUKIN‐6: measured at 3 time intervals (before, immediately after, and 1 hour after intervention). Determined using radioimmunoassay kits. | See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). |
| Zimmerman 1988 | RCT; 3 parallel groups. | DESCRIPTION: 75 in‐patients with suspected myocardial infarction in a coronary care unit in Midwest USA. NUMBERS: 25 participants in each group. AGE, mean: Music group = 65, Control group = 72, White noise group = 59. Overall mean (range) = 65 (34 to 92) years old. GENDER (male/female): 49/26 ETHNICITY: White = 75 (100%). INCLUSION CRITERIA: Orientated to person, place, and time; English speaking; > 19 years old; Stable condition. EXCLUSION CRITERIA: Hearing deficit; Health professional background. | MUSIC GROUP: 30 minutes of self‐selected music choice of instrumental tapes: Halpern relaxation tape, classical music, country and western. Played via headphones. WHITE NOISE GROUP: 30 minutes of white noise played via headphones. CONTROL GROUP: Standard care. Were told the study was for gaining information about new admissions. Asked to lay quietly in bed for 30 minutes. The music and white noise groups were told the tapes were to relax them. | ANXIETY: state anxiety measured via STAI PHYSIOLOGICAL: BP and HR measured via an automatic monitor (Kendall Co., Model 8200). Skin temperature monitored by a digital thermometer (No. 865; Omega Engineering Inc.). | |
| Zimmerman 1989 | RCT; 2 parallel groups. | DESCRIPTION: 40 in‐patients with chronic cancer pain in acute care, Midwestern USA. NUMBERS: 20 patients per group. AGE, mean (range): 60 (34 to 79) years old. GENDER (male/female): 16/24. ETHNICITY (white/other): 39/1. INCLUSION CRITERIA: orientation to person time and space; English speaking; 19 years or older; ability to consent verbally and in writing; experiencing pain for > 6months; receiving a scheduled (e.g. every 3 or 4 hours round‐the‐clock) pain medication; free of major hearing deficit. EXCLUSION CRITERIA: no further criteria described. | MUSIC GROUP: Choice of 10 relaxing instrumental tapes. Participants without a preference were given a Halpern antifrantic tape. The researcher suggested to the participant that the music would help them relax and reduce their pain. Participants listened to the music for 30 minutes via headphones. Participants lay on their beds and the lights were dimmed. CONTROL GROUP: Patients lay on their beds for 30 minutes with the lights dimmed. | PAIN: Measured before and after 30 minute test period via McGill Pain Questionnaire (Pain Rating Index, Number of Words Chosen, and Present Pain Index). Additionally, pain intensity was measured via a 10 mm [sic] VAS. | See Cepeda 2006 for details on music for pain relief. |
BP: blood pressure; HR: heart rate; PACU: post‐operative care unit; POMS: Profile of Mood States; RR: respiration rate; SD: standard deviation; STAI: State Trait Anxiety Inventory; VAS: visual analogue scale; VRS: verbal rating scale;
Typically the music intervention consisted of the patient choosing from a selection of music compilations offered by the researcher (N = 46). Some studies asked the patient to bring music from home to listen to (N = 7), whilst others offered a fixed condition chosen by the researcher (N = 32), with three of these being sounds of nature as opposed to music. Studies utilised a variety of comparison groups (with 11 studies utilising two comparison groups): standard care alone (N = 52); blank tape/headphones only (N = 25); white noise (N = 4); pre‐recorded operating room noise (N = 4); restful environment (N = 9); and audiovisual distraction (N = 2). Given that the type of comparison may influence the size or direction of treatment effect, each comparison is dealt with separately in the review.
Studies investigated the use of music on: patient‐reported anxiety (N = 52), patient‐reported pain (N = 32, see the Cochrane review Cepeda 2006, which has overlapping scope), blood pressure (N = 43), heart rate (N = 45), respiration rate (N = 20), pain‐medication requirements (N = 23, see also Cepeda 2006), anxiolytic medication requirements (N = 5), peripheral skin temperature (N = 4), skin conductance (N = 2), oxygen saturation (N = 5), requirement of oxygen supplementation (N = 1), lung function (N = 1), blood flow (N = 1), heart rate variability (N = 1), bispectral index (N = 3), stress hormones (N = 6), mood (N = 4), depression (N = 1), sleep quality (N = 2), headache (N = 1), fatigue (N = 4), urinary problems (N = 1), well‐being (N = 2), nausea (N = 5), uncertainty (N = 1), satisfaction (N = 5), length of stay (N = 8), time to mobilisation (N = 1), induction time of sedation (N = 1), activities of daily living (N = 1), and interleukins (N = 1).
We do not report on music for pain in this review since it has already been covered elsewhere (Cepeda 2006).
We have tabulated 138 excluded studies on music (Table 9;, Table 10, Table 11), including 24 CCTs which were excluded following review by our contact editor (Table 9; see section on 'Differences between protocol and review').
9. Music [CCT]: Characteristics of post‐hoc exclusions (non‐randomised studies).
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Augustin 1996 | CCT; 2 parallel groups; Allocated by alternation; Blinding: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: NOT DONE; Outcomes obtained for >80% of patients: UNCLEAR; Groups similar at baseline: DONE; Protection against contamination: UNCLEAR; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 42 pre‐operative patients scheduled for ambulatory surgery in a Midwestern city hospital, USA. NUMBERS: 21 patients per group. AGE, mean (range): 47 (18‐73) years old. GENDER (Male/Female): 25/17 ETHNICITY: All Caucasian. INCLUSION CRITERIA: Any patient scheduled for ambulatory surgery who is over 15 years old. EXCLUSION CRITERIA: Cognitive disability/delay; scheduled for cataract removal; hearing impairment; received a pre‐operative sedative; received colon preparation; lack sufficient time to participate. | MUSIC GROUP: Choice of 20 tapes (classical, environmental, new age, country‐western, general easy listening), played via headphones whilst resting in recliner chairs. Intervention lasted 15‐30 minutes depending on how long patient had left before surgery. CONTROL GROUP: Standard care‐ not offered music. Activities were not monitored, friends and family may have been present, rooms contained magazines and a television. | PHYSIOLOGICAL MEASURES: measured using "standard noninvasive technology" before and after the intervention period. RR (non‐significant): Music group = 15.10 (2.28) Control group = 16.00 (1.75) BP (Non‐significant): Music group: Systolic = 126.00 (15.47), Diastolic = 78.90 (12.54). Control group: Systolic = 130.50 (17.14), Diastolic = 83.90 (9.45). HR (Mean difference = ‐5.90, 95% CI = ‐11.56, ‐0.24): Music group = 67.20 (8.87) Control group = 73.10 (9.83). ANXIETY: State anxiety measured using the STAI before and after intervention period. Non‐significant: Music group = 35.38 (9.44) Control group = 33.42 (9.62) | |
| Binek 2003 | CCT; 2 parallel groups; Allocated by alternation; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: UNCLEAR; Outcomes obtained for >80% of participants: UNCLEAR; Groups similar at baseline: demographics‐ DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 301 outpatients and inpatients undergoing colonoscopy or esophagogastroduodenoscopy (EGD) in Switzerland. NUMBERS: Music group = 151, Control group = 150. AGE, mean: 59 years old. GENDER (male/female): 173/128. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: Inability to answer questions due to severe illness, impaired consciousness, impaired hearing, and emergency interventions. | MUSIC GROUP: Patients could choose between "light" and "classical" music which was played in the background during the examination. CONTROL GROUP: Standard care. | GENERAL EVALUATION: Not extracted for review. PAIN SENSATION: Measured via 100mm VAS. No significant difference. Music group: Mean (SD) = 7.66 (2.40), Control group: Mean (SD) = 7.86 (2.45). TOLERANCE OF PROCEDURE: Not extracted for review. ROOM AMBIENCE: Not extracted for review. SEDATION: Amount of midazolam and pethidine received was recorded, no significance difference between groups. Pethidine: Music group = 36.07 (18.88) Control group = 37.10 (18.18) Midazolam: Music group = 3.01 (1.46) Control group = 2.76 (1.37) | Paper reports outcomes as medians. Authors provided means and standard deviations on request for purposes of review. |
| Brunges 2003 | CCT; 2 parallel groups; Allocation method: UNCLEAR; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: UNCLEAR; Unit of allocation same as unit of analysis: UNCLEAR; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 44 pre‐operative in‐patients in the holding area before total joint replacement, in Florida, USA. NUMBERS: Graph depicts 22 patients in the music group and 21 patients in the control group (one person missing). AGE, range: 39‐81 years old. GENDER (male/female): 23/21 ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Listened to music via headphones for a minimum of 30 minutes in the pre‐operative holding area. Music consisted of music‐enhanced nature sounds (sea, thunder, rainstorms, wind, and waterfalls). CONTROL GROUP: Standard care. | The paper provides descriptive statistics only. EPINEPHRINE: Sampled via indwelling catheter lines. Results given as a range: Music group = 5‐10 mcg Control group = 8‐32 mcg LENGTH OF STAY: Presented in a bar chart. Means and SDs derived from the bar chart (NB. Two participants in the control group stayed for > 7 days, to calculate the mean and SD for this group, it was assumed these participants stayed for 7 days, thus providing a conservative estimate of the mean and SD): Music group (n = 22) = 4.14 (0.83) days Control group (n = 21) = 4.76 (1.18) days A t‐test on this derived data provides a P value of 0.052 (95% CI = ‐1.25 to 0.01). | |
| Dubois 1995 | CCT; 2 parallel groups; Allocated by medical record number (odd numbers were assigned to music, even numbers assigned to control); Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: DONE; Groups similar at baseline: demographics‐ DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: DONE (3 patients refused music). | DESCRIPTION: 49 out‐patients undergoing bronchoscopy, USA. NUMBERS: Music group = 21, Control group = 28. AGE, mean (SD): Music group = 56 (14), Control group = 54 (17) years old. GENDER (male/female): Music group = 12/9, Control group = 16/12. ETHNICITY: not described. INCLUSION CRITERIA: Bronchoscopy patients; understand English. EXCLUSION CRITERIA: none stated. | MUSIC GROUP: Played new wave music 'Reflections of Passion' by Yanni, via headphones for the duration of bronchoscopy procedure. CONTROL GROUP: Standard care. | PHYSIOLOGICAL: Methods of obtaining data unclear. There were no significant differences between groups on any of the physiological parameters. Oxygen saturation: Music group = 92 (5) Control group = 93 (3) HR: Music group = 104 (19) Control group = 101 (22) BP: Music group: systolic BP = 154 (27), diastolic BP = 89 (13) Control group: systolic BP = 152 (24), diastolic BP = 95 (24) COMFORT: Measured via 'Borg Scale', validity unclear. MEDICATION INTAKE: Amount of midazolam consumed did not differ between groups. Music group = 2.81 (1.58) mg Control group = 3.19 (2.12) mg. | |
| Dzhuraeva 1989 | CCT; 2 parallel groups; Method of allocation: UNCLEAR; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: UNCLEAR; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 158 inpatients with cardiovascular and respiratory illnesses participating in a therapeutic exercise programme, in the Republic of Uzbekistan. NUMBERS: unclear how many patients per group. There were 69 cardiovascular patients, and 89 respiratory patients included in the study. AGE: 30‐55 years old. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Were played classical and pop music during the two week exercise programme. CONTROL GROUP: Were not played music during the exercise programme. The exercise programme was tailored to the physical and functional readiness of the participants, with the same protocol applied to both the music and control groups. Respiratory patients received additional training on breathing when stationary and during exercise. | PULSE: Assessed increase in pulse rate during exercise in the first and second weeks of the exercise programme. Method of data collection unclear. In week one, the music group worked harder, as demonstrated by increased pulse. Cardiovascular patients: Music group = 50.3 (2.89); Control group = 33.1 (1.54) Respiratory patients: Music group = 58.1 (1.66); Control group = 47.2 (1.93) In week two, the clinical groups showed more similar patterns, and the music group had adapted better to the exercise. Cardiovascular patients: Music group = 30.3 (4.12); Control group = 40.5 (3.07) Respiratory patients: Music group = 34.1 (2.23); Control group = 43.2 (2.86) OBSERVATIONS: Complaints, sweating, skin colour, respiration, co‐ordination. Details unclear. Cardiovascular patients adapted better to the exercise in week one with music, as compared to respiratory patients who showed greater unpleasant reactions, disruptive breathing patterns, and sweating. By the second week of exercise, respiratory patients in the music group were demonstrating better adaptation to exercise than controls. | Authors conclude that cardiovascular patients should use music from the 1st week of exercise, and respiratory patients should use music from the 2nd week of exercise for better adaptation. |
| Evans 1994 | CCT; 2 parallel groups; Allocated systematically (3 to music group then 1 to control group); Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Power calculation: NOT DONE; Outcomes obtained for > 80% of participants: DONE; Groups similar at baseline: Trait anxiety ‐ DONE, other characteristics‐ UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 24 pre‐operative day surgery patients waiting for surgery under general anaesthesia, in Texas, USA. NUMBERS: Music group = 18, Control group = 6. AGE, mean (SD): Music group = 52.67 (11.74), Control group = 43.50 (7.56) years old. GENDER (male/female): Music group = 8/10, Control group = 1/5. ETHNICITY: not described. INCLUSION CRITERIA: Read and speak English; Scheduled for endoscopic cholecystectomy, herniorrhaphy, or appendectomy under general anaesthesia. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Choice of "easy listening" music selections recorded by the medical staff played via headphones for 20 minutes pre‐operatively. CONTROL GROUP: Standard care. Both groups were encouraged to close their eyes or cover them with a cloth. | ANXIETY: Measured via the STAI and a VAS. There was no significant difference between groups on either measure. STAI: Music group = 33.2 Control group = 34.0 BP: Method of measurement UNCLEAR. There was no significant difference between groups: Music group: Systolic BP = 125.6 (13.2), Diastolic = 79.8 (12.6) Control group: Systolic BP = 128.5 (22.7), Diastolic = 74.5 (8.0) PULSE: Method of measurement UNCLEAR. There was no significant difference between groups: Music group = 75 (12.8) Control group = 78 (6.9) | |
| Guétin 2005 | CCT; 2 parallel groups; Allocated by month of admission; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: NOT DONE; Power calculation: DONE; Outcomes obtained for >80% of participants: DONE; Groups similar at baseline: DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: DONE (3 from music group, 2 from control group). | DESCRIPTION: 65 in‐patients undergoing rehabilitation (physiotherapy, balneotherapy, re‐education, and physical exercise) for lower back pain, France. NUMBERS: Music group = 33, Control group = 32. AGE: not described. GENDER (male/female): Music group = 16/17, Control group = 16/16. ETHNICITY (French/European/African): Music group = 28/2/3, Control group = 28/2/2. INCLUSION CRITERIA: 30‐70 years old; speak and read French; not cognitively impaired; diagnosis of lower back pain for > 6 months. EXCLUSION CRITERIA: deafness; epilepsy around auditory stimuli; infectious/inflammatory back pain. | MUSIC GROUP: Music provided for first 4 days of 12 day hospitalisation. Music played for 20 minutes in the afternoon after physical therapy via headphones in a silent room. Patients were given a choice of music, with each choice arranged to have progressive relaxation with re‐awakening period at the end. CONTROL GROUP: Received physical therapy alone, with no music sessions. | PAIN: Measured via VAS at baseline, day 5, and day 12, plus immediately pre and post therapy sessions. Day 5 outcomes did not significantly differ between groups: Music group = 3.7 (2.7), Control group = 4.0 (2.0). DEPRESSION/ANXIETY: Measured via the Hospital Anxiety and Depression (HAD) scale (scores from 0‐21 with higher scores indicating more depression/anxiety). Paper reports the music group had significantly reduced scores from baseline to Day 5 on depression and anxiety when compared to the control group: Depressoin (change score): Music group = ‐2.1 (3.0), Control group = 0.6 (2.4) Anxiety (change score): Music group = ‐3.5 (3.7), Control group = 2.5 (9.4) FUNCTIONAL ABILITY: Measure with the Oswestry index (scores from 0‐50 with higher scores indicating more disability). Paper reports that music group had significantly reduced scores from baseline to Day 5 when compared to the control group: Music group = ‐11.8 (17.8), Control group = ‐2.5 (9.4) | |
| Hamel 2001 | CCT; 2 parallel groups; Allocated via alternation; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: DONE; Outcomes obtained for > 80% of participants: NOT DONE; Groups similar at baseline: gender‐ DONE, outcomes ‐ NOT DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: DONE (36 left prior to completing the STAI, 2 disliked music, 2 did not want to retake STAI). | DESCRIPTION: 101 in‐patients and out‐patients waiting for cardiac catheterizations in a cardiac telemetry unit, USA. NUMBERS: Music group = 51, Control group = 50. AGE, range: 43‐74. GENDER (male/female): Music group = 34/17, Control group = 29/21. ETHNICITY: not described. INCLUSION CRITERIA: Orientated to person, place and time; read and speak English; free of hearing deficit. EXCLUSION CRITERIA: none stated. | MUSIC GROUP: Listened to 20 minutes of 'Trance‐Zendance' by Halpern. Played via headphones prior to cardiac catheterization. CONTROL GROUP: Standard care. | ANXIETY: Measured via STAI pre‐ and post‐ 20‐minute intervention period. There was a significant difference in anxiety scores in favour of the music group: Music group = 37.84 (9.82) Control group = 44.34 (10.99) HR: Measured manually by counting heart beats from the radial artery or automatically with a Marquette Component Monitor. There were no significant differences between groups on HR: Music group = 64.43 (12.00) Control group = 67.56 (19.43) BP: Measured via an automatic noninvasive oscillometric cuff, or using a sphygmomanometer auscultating over brachial artery. Paper reports a significant increase in systolic BP in the control group from baseline. There was not a significant difference between groups post‐treatment. Music group: Systolic BP = 133.53 (19.79), Diastolic BP = 72.78 (10.91) Control group: Systolic BP = 139.72 (21.61), Diastolic BP = 75.52 (11.94) | |
| Haun 2001 | CCT; 2 parallel groups; Allocated via alternation; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: NOT DONE; Outcomes obtained for >80% of participants: UNCLEAR; Groups similar at baseline: demographics ‐ DONE, outcomes ‐ UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 20 pre‐operative patients scheduled for breast biopsy in a holding area in Kentucky, USA. NUMBERS: 10 patients in each group. AGE, mean (SD): Music group = 39.7 (13.2), Control group = 37.2 (12.7) years old. GENDER: 100% female. ETHNICITY: not described. INCLUSION CRITERIA: none described. EXCLUSION CRITERIA: Hearing impairment; history of cancer surgery; hypertension; cardiac disease; pulmonary disease; on medication for any of the above conditions; excluded by attending surgeon. | MUSIC GROUP: Choice from selection of "new age" music listened to via headphones for 20 minutes pre‐operatively. No other music types were offered and patients' preferences were not solicited. CONTROL GROUP: Standard care. Family members encouraged to be with both groups once nursing staff had completed all necessary pre‐operative care. | ANXIETY: Measured via the STAI pre‐ and post‐ 20‐minute study period. Significant difference found in favour of music group: Music group = 32.8 (7.0) Control group = 46.6 (9.3) PHYSIOLOGICAL: BP and HR measured via Spacelab monitor immediately pre‐ and post‐ 20‐minute study period. RR measured via experimenter observation. No differences observed between groups for BP and HR. A significant difference was observed in favour of music group for RR. BP: Music group: Systolic BP = 118.0 (14.3), Diastolic BP = 69.0 (10.4) Control group: Systolic BP = 121.7 (15.9), Diastolic BP = 71.2 (10.6) HR: Music group = 77.4 (16.0); Control group = 79.7 (13.6) RR: Music group = 16.4 (2.1); Control group = 18.4 (2.1) | |
| Heiser 1997 | CCT; 2 parallel groups; Patients matched for gender and age; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Power calculation: NOT DONE; Outcomes obtained for >80% of participants: NOT DONE; Groups similar at baseline: Gender and age‐ DONE, outcome measures‐ UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: DONE for 15 patients (anaesthesia care providers unable to adhere to the intraoperative anaesthesia study protocol for 6 patients, 8 patients had incomplete data, 1 patient who had denied alcohol abuse preoperatively admitted this postoperatively). A further 9 patients were not included in analysis, presumably due to matched pairing, although this is UNCLEAR. | DESCRIPTION: 34 in‐patients undergoing elective lumbar microdiscectomy procedures consented to participate (although only 10 analysed), Kentucky, USA. NUMBERS: Music group = 5 patients analysed, Control group = 5 patients analysed. AGE, mean (range): Original 34 participants = 38 (23‐59) years old. GENDER (male/female): 21/13. ETHNICITY: not described. INCLUSION CRITERIA: ASA status I‐II; scheduled for elective lumbar microdiscectomy procedures. EXCLUSION CRITERIA: History of substance abuse; psychological disorders; > 40% over ideal body weight; had incurred lumbar spine injuries with other traumatic injuries; history of chronic pain. | MUSIC GROUP: Participants had a choice of 3 cassettes (country, instrumental, classical), with music 60‐80 bpm, played via headphones at a volume pre‐selected by participants. Music began 30 minutes before the end of the surgery and continued without interruption for one hour in PACU. CONTROL GROUP: Also selected preferred music and checked sound level pre‐operatively, but were not played any music during surgery or in the PACU. | No data reported in paper. The paper reports there were no differences between the two groups on any of the outcome measures. ANALGESICS: Amount of IV morphine sulfate administered. PAIN and ANXIETY: Measured via VAS. | |
| Kaempf 1989 | CCT; 2 parallel groups; Allocation by alternative weeks; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: NOT DONE; Power calculation: NOT DONE; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 33 out‐patients awaiting arthroscopic procedures in Philadelphia, USA. NUMBERS: UNCLEAR, paper states that recruitment continued until there were at least 15 patients in each group. AGE: not described. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: 18 years or older; understand written and verbal instructions. EXCLUSION CRITERIA: received sedation prior to arriving in the holding area. | MUSIC GROUP: 20 minutes of classical music (tape 3 of Music Rx, developed by Bonny), played via audiocassette played placed 1 foot away during the waiting period. CONTROL GROUP: Standard care. | BP: Measured via a Dinamap monitor before and after the 20 minute study period. There were no significant differences between the groups. Standard deviations are not provided. Music group: Systolic BP = 122.3 mm Hg, Diastolic BP = 73.1 mm Hg. Control group: Systolic BP = 124.6 mm Hg, Diastolic BP = 74.7 mm Hg. RR: Method of measurement unclear. There was a significant difference in favour of the music group (P = 0.047). No standard deviations provided. Music group = 15.2 Control group = 19.0 ANXIETY: Measured via STAI before and after intervention period. There was no significant difference between the groups. No standard deviations provided. Music group = 32.7 Control group = 35.8 | |
| Lee 2004b | CCT; 2 parallel groups; Allocation by day of procedure; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: NOT DONE; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: Physiological measures (DONE), STAI (NOT DONE). Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 113 pre‐operative day patients undergoing cytoscopy, cauterisation, or endoscopy, in China (Hong Kong).NUMBERS: Music group = 58, Control group = 55.AGE, mean (SD): Music group = 50.0 (15.5), Control group = 51.9 (14.4) years old.GENDER (male/female): Music group = 31/27, Control group = 27/28.ETHNICITY: not described.INCLUSION CRITERIA: 18 years or older; undertaking noninvasive day procedures with regional or local anaesthetic.EXCLUSION CRITERIA: Cognitive disability; hearing impairment; received preoperative sedatives; received a colon preparation; pre‐existing co‐morbid illness; did not have sufficient time to participate. | MUSIC GROUP: Choice of eastern and western style easy listening music and Chinese pop music (10 CDs and 10 mini‐discs) played via headphones in reclining chairs for 20‐40 minutes pre‐operatively.CONTROL GROUP: Undertook usual pre‐procedural relaxing activities (e.g. reading, watching TV) in the waiting room. | STATE ANXIETY: Measured via STAI pre‐ and post‐intervention period. Only the music group had a significant drop in anxiety. Post‐intervention scores:Music group = 42.5 (5.7) Control group = 46.4 (6.5) PHYSIOLOGICAL OUTCOMES: Measured via "standard non‐invasive instruments" pre‐ and post‐intervention period. There were no significant differences between groups.BP scores: Music group: Systolic BP = 124.2 (21.1), Diastolic BP = 70.0 (10.8) Control group: Systolic BP = 129.4 (25.6), Diastolic BP = 72.0 (11.1) PULSE scores: Music group = 71.1 (10.4) Control group = 70.1 (8.6) RR:Music group = 16.6 (1.0) Control group = 16.7 (1.0) | |
| Metera 1975a | CCT; 2 groups (non‐parallel), intervention group was cross‐over (2 types of music played in same order for all participants), control group may have been recruited post‐hoc (UNCLEAR). Allocation method: Participants appear to have been recruited to intervention group first, and control participants recruited after‐ UNCLEAR. Blinding of group allocation: NOT DONE Blinded assessment of outcomes: UNCLEAR if automated; Power calculation: UNCLEAR; Outcomes obtained for >80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: NOT DONE‐ cross‐over in music group. DONE for control group. Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 45 patients with disease of the lungs or chest being treated at the Department of Chest Surgery in Zakopane, Poland. NUMBERS: Music group = 30, Control group = 15. AGE, mean (range): Music group = 34 (19‐62) years old, Control group not described. GENDER (male/female): Music group = 25/5, Control group not described. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Cross‐over study. Music was played via headphones. Patients were played Debussy's 3rd part of Bergamasque Suite (Clair de Lune) on the piano (soothing music), and then Bartok's Wonderful Mandarin (nerve racking/exciting music). First, there was a 3‐minute rest in the recumbent position then, before, in between, and after each musical piece was a 3‐minute pause. CONTROL GROUP: Received no music. No specific treatment/surgery was being given to any participants during the experiment. | Parameters were measured at 5 time points in the music group: 1) Following 3‐min rest; 2) Following soothing music; 3) Following 3‐min pause; 4) Following exciting music; 5) Following 3‐min pause. Parameters were measured at 4‐time points in the control group (to follow same time scale as the music group)‐ a final 5th measurement was not taken for the control group. Paper states "No statistically significant differences were found in any of these parameters between the experimental and the control group". RESPIRATORY RATE: No significant differences within the music group. TIDAL VOLUME: Within the music group there was significant differences between the 1st and 2nd measurements (639 ml and 527 ml) only. MINUTE VENTILATION: Within the music group there was a significant difference (P <0.1) [sic] between the 1st and 2nd measurements (11l and 8.9l). Measurements during exciting music showed a rise in MV almost to the initial value (4th measurement = 10.6l). MINUTE OXYGEN CONSUMPTION: Within the music group there was a significant decrease between the 1st and 2nd measurements (315 ml and 282 ml). There was an increase of 60 ml during the exciting music (significance unclear). BASAL METABOLIC RATE: Within the music group there was a significant decrease between the 1st and 2nd measurements (42% and 24 %). Exciting music increased BMR to 53.5% ("significant even at P < 0.1" [sic]). HEART RATE: No significant differences within the music group. | Data not sufficient for extraction. No SDs reported. Paper reports significance as P < 0.1. Data for control group reported in line graphs only. |
| Metera 1975b | CCT; 2 groups (non‐parallel), intervention group was cross‐over (2 types of music played in same order for all participants), control group may have been recruited post‐hoc (UNCLEAR). Allocation method: Participants appear to have been recruited to intervention group first, and control participants recruited after‐ UNCLEAR. Blinding of group allocation: NOT DONE Blinded assessment of outcomes: UNCLEAR if automated; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: NOT DONE‐ cross‐over in music group. DONE for control group. Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 45 patients with disease of the lungs or chest being treated at the Department of Chest Surgery in Zakopane, Poland. NUMBERS: Music group = 30, Control group = 15. AGE, mean: Music group = 34 years old, Control group not described. GENDER (male/female): Music group = 25/5, Control group not described. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Cross‐over study. Music was played via headphones. Patients were played Debussy's 3rd part of Bergamasque Suite (Clair de Lune) on the piano (soothing music), and then Bartok's finale of the Wonderful Mandarin (nerve racking/exciting music). First there was a 3‐minute rest in the recumbent position, then a 3‐minute pause before the first musical piece. After the first piece of music, there was a 4‐minute pause before the second musical piece was played. CONTROL GROUP: Received no music. No specific treatment/surgery was being given to the patients during the experiment. | Parameters of airway resistance were measured at three time points in both groups: 1) Following 3‐min rest; 2) Following relaxing music; 3) Following exciting music. AIRWAY RESISTANCE: Tests were carried out using a Godart Pulmotest. The maximum forced one‐second expiration curve, maximum mid‐expiratory flow rate, first phase of forced expiratory volume, and the inspiration/expiration time ratio, were analysed. There were no significant differences between the control and music group. There were no significant differences between conditions within the music group. | Data not sufficient for extraction. Appears to be same participants in Metera 1975a (mean age and gender distribution of music group is the same). |
| Mok 2003 | CCT; 2 parallel groups; Allocated by alternation (weeks) Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: Physiological outcomes (DONE‐ automated), C‐STAI (NOT DONE); Unit of allocation same as unit of analysis: NOT DONE; Power calculation: DONE; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 80 patients undergoing minor surgery in a day‐surgery ward in China. NUMBERS: 40 patients per group. AGE, range: 18‐70. GENDER, (male/female): Music group = 7/33, Control group = 8/32. ETHNICITY: not described. INCLUSION CRITERIA: 18 years or older; consenting; comprehend written and oral instruction. EXCLUSION CRITERIA: hearing impairment; received preoperative sedative; cardiac disease; history of hypertension. | MUSIC GROUP: Choice of 3 types of music with slow rhythms: classical music (concertos and sonatas), contemporary popular music (e.g. "The heart will go on"), Chinese popular music (e.g. "Night plane"). Music had 45 minutes running time and played via headphones for duration of surgery. CONTROL GROUP: Standard care. | ANXIETY: measured via C‐STAI post‐surgery. Patients were asked to fill out the questionnaire by thinking retrospectively over procedure. Mean difference = ‐25.40, 95% CI = ‐29.28, ‐21.52 Music group = 31.83 (4.97) Control group = 57.23 (11.50) PHYSIOLOGICAL MEASURES: HR and BP measured via an automated portable HR monitor. Music group had 3 intra‐operative readings taken and the paper reports the mean scores, the control group readings taken post‐operatively only. Data not suitable for comparison. | |
| Moss 1987 | CCT; 2 parallel groups; Allocation method UNCLEAR ("groups were divided by gender and chosen by convenience"); Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: NOT DONE; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 17 day‐patients undergoing arthroscopic surgery, USA. NUMBERS: Music group = 9, Control group = 8 patients. AGE: 20‐40 years old. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: admitted for scheduled arthroscopic surgery under general anaesthesia. EXCLUSION CRITERIA: none stated. | MUSIC GROUP: Choice of 4 musical tapes (classical tapes from 'Music Rx', Bonny; popular tapes from 'Music Rx'; New Age tape by Steven Halpern called "Dawn"; easy listening selections assembled by investigator). Music played via headset and auto‐reverse cassette player. From administration of pre‐operative medication to PACU. Participants were told to restart the music if they desired after their return to the ambulatory surgery unit. CONTROL GROUP: standard care. | ANXIETY: state anxiety measured via STAI approximately 2 hours post‐operatively. Non‐significant. Music group = 32.60 (8.73) Control group = 29.80 (8.73) | SDs are estimated from the t‐value. |
| Schuster 1985 | CCT; 2 parallel groups; Allocation method: UNCLEAR; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: UNCLEAR if data collection procedure automated. Unit of allocation same as unit of analysis: UNCLEAR; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: NOT DONE: BP. Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 63 patients undergoing dialysis, Florida, USA. NUMBERS: Music group = 31, Control group = 32. AGE (range): 22‐81 years old. GENDER (male/female): 24/39. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: Choice of classical, pop, rock, jazz, country/western, gospel, easy listening, swing, and bluegrass played via headphones during dialysis treatment. Music was played for 1 hour beginning 30 minutes after the onset of dialysis treatment, there then was an hour of no music, followed by another hour of music. CONTROL GROUP: Standard care. | BP: Measured after each hour of dialysis treatment. BP was recorded daily from each patient's chart for a 2‐week baseline period and a 3‐week treatment period. The two groups did not significantly differ on systolic and diastolic BP readings for onset through final readings during the treatment period. NURSE RATINGS: Not validated. ATTITUDE SURVEY: Not validated. | Data not sufficient for extraction. |
| Staricoff 2003b | CCT; 2 parallel groups; Allocation method: UNCLEAR; Blinding of group allocation: UNCLEAR (this is one of a series of studies. It states at beginning of document that blinding was carried out where possible but unclear where or how this was achieved). Blinded assessment of outcomes: UNCLEAR; Unit of allocation same as unit analysis: UNCLEAR; Power calculation: NOT DONE; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 88 pregnant women attending a high‐risk antenatal clinic, London, UK. NUMBERS: Music group = 54, Control group = 34. AGE: not described. GENDER: 100% female. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | MUSIC GROUP: One or two musicians playing in one corner of the waiting room with the chairs arranged in a semi‐circle around them. Harp, clarinet, or guitar were preferred, violin and cello not welcomed. Does not explain in depth what was played. CONTROL GROUP: No live music. | BP: Obtained by the clinician (method unclear) at the beginning of the consultation (after the waiting room experience). There was no significant difference between the groups. Systolic BP: Live music (n = 54), mean (SD) = 115 (13) Control group (n = 34) mean (SD) = 118 (16) Diastolic BP: Live music = 70 (11) Control group = 72 (11) | This is one of a series of studies. Two more studies were conducted in the antenatal clinic that do not need inclusion criteria for the review due to the study design (before and after). |
| Szeto 1999 | CCT; 2 parallel groups; Allocation method UNCLEAR ("a quasi‐experimental design was used"); Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: NOT DONE; Outcomes obtained for > 80% of participants: NOT DONE; Groups similar at baseline: DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: DONE (3 control participants could not compete procedure as sent for their operation). | DESCRIPTION: 9 in‐patients waiting for elective surgery in a theatre holding area, China. NUMBERS: Music group = 6, Control group = 3. AGE, mean (range): 58 (21‐89). GENDER: not described. ETHNICITY: 100% Chinese INCLUSION CRITERIA: 18 years or older; understand written and verbal instructions; no hearing impairment; not received any pre‐medication sedation; consented to participate. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Choice of: slow rhythmical songs; Chinese slow rhythmical music; Western slow rhythmical music. Played via headphones for 20 minutes pre‐operatively. CONTROL GROUP: Standard care. | BP: Measured via a calibrated Dinamap BP monitor before and after 20 minute study period. No significant differences between groups. Music group (N = 6): Systolic BP = 143.83 (31.25), Diastolic BP = 80.83 (9.07). Control group (N = 3): Systolic BP = 144.00 (16.09), Diastolic BP = 75.33 (7.02). ANXIETY: Measured via C‐STAI pre‐ and post‐treatment. Paper reports a significant difference (Wilcoxon Signed‐Rank test) in favour of the music group after the 20 minute study period. Music group (N = 6) = 33.33 (6.38) Control group (N = 3) = 46.33 (4.73) TENSION: Measured via the Subjective Unit of Tension Scale (a NRS) pre‐ and post‐treatment. No significant differences between groups. Music group (N=6) = 1.67 (1.63) Control group (N=3) = 3.00 (2.00) | |
| Tanabe 2001 | CCT; 3 parallel groups; Allocation method: alternation; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: DONE; Outcomes obtained for > 80% of participants: DONE; Groups similar at baseline: Pain‐ DONE, demographics‐ UNCLEAR; Protection against contamination: NOT DONE; Description of withdrawals and drop‐outs: DONE (75 exclusions detailed). | DESCRIPTION: 76 patients presenting to an emergency department with minor musculoskeletal trauma, in Midwest USA. NUMBERS: Music group = 24, Standard Care = 28, Ibuprofen = 24 (excluded from review). AGE mean (SD): 41 (17.54) years old. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: 18 years or older; chief complaint of minor extremity trauma distal to and including the knee or elbow. EXCLUSION CRITERIA: analgesics administered prior to arrival; injury occurred more than 24 hours earlier; pain rating 3 or less; unable to speak English; unable to use pain scales; lacerations; sensitivity to cold; Raynaud's phenomenon; rheumatoid arthritis to the affected joint. | MUSIC GROUP: Provided with a Walkman tape player and choice of music (classical, country, rock, pop, and jazz), or were allowed to listen to the radio if they preferred. Patients also received standard care. STANDARD CARE: Consisted of ide, elevation, and immobilization of the affected extremity. IBUPROFEN: Excluded from review. | PAIN: Pain intensity measured at 0, 30, and 60 minutes via 10‐point NRS. There was no statistical differences between groups at any time interval. All groups showed significant improvement from baseline. Mean pain ratings: Music group: 0 min = 6.46; 30 min = 5.75; 60 min = 5.83 Standard care: 0 min = 6.57, 30 min = 5.61; 60 min = 5.57 SATISFACTION: Measured via VRS and a non‐validated yes/no question. There were no differences between groups on either measure. | No SDs provided. |
| Tse 2005 | CCT; 2 parallel groups; Allocation method: Mondays = experimental group, Thursdays = control group. Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: NOT DONE; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 57 post‐operative in‐patients who have undergone elective nasal surgery. NUMBERS: Music group = 27, Control group = 30. AGE, mean (SD): Music group = 39.2 (14.4), Control group = 40.6 (14.5). GENDER (male/female): Music group = 11/16, Control group = 13/17. ETHNICITY: 100% Chinese. INCLUSION CRITERIA: scheduled for functional endoscopic sinus surgery or turbinectomy. EXCLUSION CRITERIA: History of mental disturbance; had undergone previous major surgery; opioid dependent; hearing problem; history of hypertension. | MUSIC GROUP: Choice of Chinese and Western various music types and patients encouraged to bring music of their own choice. Listened for 30 minutes on four occasions: post‐operatively (T1), again 4 hours later (T2), on the first post‐operative day at 8am (T3) and again at noon (T4). CONTROL GROUP: Standard care. | PAIN: Measured via VRS at baseline and after each intervention session. Music group gave significantly lower pain ratings at all four time points. T4 data: Music group = 1.04 (0.28) Control group = 4.07 (0.33). SYSTOLIC BP: Measurement method unclear. Significant differences at all four time points in favour of music group. T4 data: Music group = 113.67 (11.28) mm Hg Control group = 132.37 (18.68) mm Hg HR: Measurement method unclear. Significant differences at all four time points in favour of music group. T4 data: Music group = 74.52 (5.99) bpm Control group = 81.57 (7.61) bpm PAIN MEDICATION: Number of paracetamol tablets taken, and dose of diclofenac sodium was recorded four hours after surgery and at 8am on the first post‐operative day. Significant differences were found in favour of the music group at both time points for paracetamol intake, and at the first time point only for diclofenac sodium intake. 8am on first post‐operative day data: Music group: Paracetamol intake = 2.15 (2.41) tablets, Diclofenac Sodium = 0.04 (0.19). Control group: Paracetamol intake = 5.43 (2.00), Diclofenac Sodium = 0.20 (0.41). | |
| Williamson 1992 | CCT; 2 parallel groups; Method of allocation: alternation; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: DONE; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: demographics‐ DONE; Protection against contamination: DONE; Description of withdrawals and dropouts: DONE (4 patients refused to listen to ocean sounds after first night). | DESCRIPTION: 60 post‐operative in‐patients after coronary artery bypass graft in a progressive care area, USA. NUMBERS: 30 patients per group. AGE, mean (SD): Sounds = 58.6 (7.72), Control group = 58.3 (9.31) years old. GENDER (male/female): Sounds = 21/9, Control group = 24/6. ETHNICITY: not described. INCLUSION CRITERIA: presenting for elective coronary artery bypass graft surgery; 21‐69 years old; were not retained in the ICU for longer than 3 days after surgery; did not have to return to surgery; were not placed on the intra‐aortic balloon pump; did not receive any surgery other than bypass grafting. EXCLUSION CRITERIA: Documented sleep disorder; were having repeat coronary artery bypass graft surgery; taking tricyclic antidepressants regularly within 1 month of surgery; could not hear sounds played softly at bedside; experimental group participants did not complete 3 nights of listening to ocean sounds; chest pleural tube in place beyond the 2nd night post‐transfer to progressive care unit. | SOUNDS GROUP: Marsona Sound Conditioner (providing white noise in the form of rain, ocean waves, or a waterfall). 56/60 patients chose ocean sounds. Sounds were played at the bedside throughout the night (switched on between 20.30 and 21.00 hours). Sounds played for 3 nights. CONTROL GROUP: No sounds. | SLEEP: Pre‐test evaluated for patients on their usual sleep at home, data collected on admission, prior to surgery. Assessed on the fourth day post‐transfer for the quality of sleep the previous night. Measured via the Richards‐Campbell Sleep Questionnaire, which includes VAS for sleep depth, latency to sleep onset, awakening, return to sleep, quality of sleep, and a total sleep score. No SDs reported. The sound group reported significantly deeper sleep than controls: Sound group: Pre‐test = 49, Post‐test = 56 Control group: Pre‐test = 66, Post‐test = 35 There was no significant difference between groups in falling asleep: Sound group: Pre‐test = 68, Post‐test = 71 Control group: Pre‐test = 62, Post‐test = 60 The sounds group reported being awake significantly less in the night: Sound group: Pre‐test = 68, Post‐test = 65 Control group: Pre‐test = 69, Post‐test = 51 The sounds group returned to sleep significantly faster than controls: Sound group: Pre‐test = 63, Post‐test = 68 Control group: Pre‐test = 61, Post‐test = 51 The sounds group reported significantly better quality of sleep than controls: Sounds group: Pre‐test = 71, Post‐test = 69 Control group: Pre‐test = 67, Post‐test = 46 The total sleep score was significantly better in the sound group: Sounds group: Pre‐test = 64, Post‐test = 66 Control group: Pre‐test = 65, Post‐test = 48 | |
| Wolowicka 1989 | CCT; 2 parallel groups; Allocation method: UNCLEAR; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: UNCLEAR; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 50 patients undergoing surgery with local anaesthetic, Poland. NUMBERS: Music group = 30, Control group = 20. AGE: not described. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: none described. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Played music before during and after surgery. Patients chose music from a selection of instrumental tapes (music was soft, bright, avoiding high‐pitched sounds, classical). CONTROL GROUP: Standard care. | ANXIETY: Measured via STAI the day before and directly after surgery in the recovery room. Music group: pre‐surgery = 38, post‐surgery = 36. Control group: pre‐surgery = 46, post‐surgery = 43. On the second and third day after surgery anxiety was lower in the music group. No statistical analyses reported. | Data not in sufficient detail for extraction. |
| Yamanaka 2003 | CCT; 2 parallel groups; Allocation method: Day of week; Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: NOT DONE; Unit of allocation same as unit of analysis: NOT DONE; Power calculation: UNCLEAR; Outcomes obtained for > 80% of participants: UNCLEAR; Groups similar at baseline: UNCLEAR; Protection against contamination: DONE; Description of withdrawals and drop‐outs: NOT DONE. | DESCRIPTION: 57 in‐patients undergoing surgery with local anaesthetic, Japan. NUMBER: Music group = 34, Control group = 23. AGE, mean (range): Music group = 45.3 (18‐75), Control group = 38.2 (15‐79) years old. GENDER (male/female): Music group = 12/22, Control group = 6/17. ETHNICITY: not described. INCLUSION CRITERIA: Consenting participants during the period May to July. EXCLUSION CRITERIA: none described. | MUSIC GROUP: Were played a set piece (by Elgar) from when they entered the theatre to the end of surgery. CONTROL GROUP: Standard care. | ANXIETY: Measured via STAI before and after surgery. Participants were requested to think back to how they felt during surgery in the post‐treatment questionnaire. Authors group findings into those who demonstrated a reduction in anxiety (from pre to post), those who showed no change, and those who showed an increase in anxiety. They then used Chi‐square to assess the differences between music and control groups. This analysis showed no difference between groups. | |
| Yung 2002 | CCT; 3 parallel groups; Allocation method: UNCLEAR, paper states it was a quasi‐experimental design. Blinding of group allocation: NOT DONE; Blinded assessment of outcomes: Anxiety‐ NOT DONE, BP and HR‐ automated; Unit of allocation same as unit of analysis: DONE; Power calculation: NOT DONE; Outcomes obtained for > 80% of participants: DONE; Groups similar at baseline: DONE; Protection against contamination: DONE; Description of withdrawals and drop‐outs: DONE (description of 12 exclusions and no withdrawals). | DESCRIPTION: 30 pre‐operative patients waiting for transurethral resection of the prostate, in a theatre holding area, Hong Kong, China. NUMBERS: 10 patients in each group. AGE, mean (SD): Music group = 65.2 (10.15), Control group = 70.9 (6.49). GENDER: 100% male. ETHNICITY: 100% Chinese. INCLUSION CRITERIA: Comprehend oral and written instructions. EXCLUSION CRITERIA: Cardiac disease; history of hypertension; received pre‐operative sedation. | MUSIC GROUP: 20 minutes of slow rhythm soft music played pre‐operatively via headphones. Choice of three tapes that had been judged by a panel of 3 musicians (slow rhythm songs, Chinese slow rhythm music, Western slow rhythm music). No nurse presence. CONTROL GROUP: No nurse or music present. NURSE PRESENCE: Excluded from review. | PHYSIOLOGICAL: BP and HR recorded on an automated BP monitor (Dinamap 1846‐SX) before and after 20 minute study period. Paper reports no significant differences between groups (Kruskal‐Wallis test) BP: Music group: Systolic BP = 126.5 (18.03), Diastolic BP = 73.9 (10.83) Control group: Systolic BP = 138.8 (19.61), Diastolic BP = 81.0 (10.71) HR: Music group = 72.2 (12.32) Control group = 79.3 (11.26) ANXIETY: Measured via the C‐STAI before and after 20 minute study period. Paper reports no significant differences between groups (Kruskal‐Wallis test): Music group = 37.6 (7.41) Control group = 37.7 (7.27) |
BP: blood pressure; HR: heart rate; RR: respiration rate; STAI: State Trait Anxiety Inventory; VAS: visual analogue scale
10. Music [A‐M]: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Abramson 1966 | No data presented‐ summary paper |
| Bampton 1997 | Validity of outcomes |
| Beck 1991 | Setting |
| Boeke 1988 | Validity of outcomes |
| Bonke 1982 | Outcomes not reported for relevant groups; data collection methods unclear. |
| Bozcuk 2006 | Study design |
| Browning 2001 | Intervention provided outside of hospital |
| Byers 1997 | Study design |
| Bykov 2003b | Setting and population |
| Cai 2001a | Intervention |
| Cai 2001b | Intervention |
| Ceccio 1984 | Intervention‐ relaxation technique |
| Chikamori 2004 | Intervention |
| Clair 1994 | Questionable validity of outcome, relevant data not presented |
| Clair 2006 | Setting |
| Clark 1998 | Setting |
| Cooper 1991 | Qualitative report |
| Courtright 1990 | Outcome measure |
| Cunningham 1997 | Outcomes |
| Davis 1992 | Setting |
| De l'Etoile 2002 | Intervention |
| Denney 1997 | Setting |
| Dritsas 2004 | Intervention not well defined |
| Durham 1986 | Intervention provided during education programme |
| Eisenman 1995 | Study design |
| Escher 1993 | Music therapist confound; group differences in timing of data collection |
| Fauerbach 2002 | Intervention included coaching of participants |
| Ferguson 1997 | Setting not hospital |
| Fox 1986 | Study design |
| Frank 1985 | Study design |
| Fratianne 2001 | Intervention interactive music therapy |
| Frid 1981 | Interventions not suitable for inclusion |
| Good 1995 | Invention group provided 20mins coaching. |
| Good 1998 | Intervention group provided reinforcement and training‐ bias |
| Good 1999 | Intervention group provided coaching on relaxing |
| Good 2001 | Secondary analysis of previous study |
| Good 2002 | Secondary analysis of previous study |
| Good 2005 | Secondary analysis of previous study |
| Götell 2002 | Setting; qualitative |
| Götell 2003 | Qualitative |
| Guzzetta 1989 | Relaxation (psychological) technique use with intervention |
| Harris 1992 | Outcomes not health‐related |
| Haythornthwaite 2001 | Intervention‐ taught techniques |
| Helmes 2006 | Outcomes |
| Hooper 1992 | Case study |
| Hsu 1998 | Intervention not well defined |
| Huffman 1994 | Intervention not well defined |
| Janelli 1997 | Policy confound (restraints use) |
| Janelli 1998 | Policy confound (restraints use) |
| Janelli 2000 | Policy confound (restraints use) |
| Janelli 2002 | Outcome measure |
| Janelli 2004 | Outcome measure |
| Janiszewski 1980 | Study design |
| Jarvis 1979 | Conference abstract‐ not enough detail |
| Jonas 1988 | Study design |
| Kaiming 1997 | Intervention not well defined |
| Kane 2004 | Data unsuitable for cross‐over study |
| Kim 2005 | Setting |
| Kimata 2003 | Setting |
| Kopp 1991 | Intervention not well defined |
| Kumar 1992 | Validity of outcomes |
| Kwon 2006 | Study design‐ selection of participants by matching, different wards assigned to different conditions. |
| Lai 1999 | Unable to clarify discrepancies in data with author |
| Lai 2005 | Setting |
| Lai 2006 | Setting; Duplicate |
| Laurion 2003 | Intervention began before admission |
| Lazaroff 2000 | Unclear methods and data |
| Leão 2004 | Study design |
| Locsin 1979 | Intervention not well described (CCT) |
| Locsin 1981 | Intervention not well described (CCT) |
| McCaffrey 2004 | Outcomes not validated/reliable |
| Mellgren 1967 | Study design |
| Mihara 2005 | Lack of information |
| Miluk‐Kolasa 1994 | Confounding |
| Miluk‐Kolasa 1996 | Intervention not well described |
| Miluk‐Kolasa 2002 | Intervention not well described |
| Moss 1988 | Intervention not well described, no data presented (CCT) |
| Murrock 2002 | Setting |
11. Music [N‐Z]: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Norberg 1986 | Study design |
| Prensner 2001 | Study design |
| Ragneskog 1996 | Setting |
| Rakshy 1997 | Inappropriate methods and analysis |
| Routhieaux 1997 | Outcomes not patient‐related |
| Salmore 2000 | Intervention |
| Sármány 2006 | Patients allocated retrospectively to music or control, depending on whether or not they had noticed or heard any music playing (unpublished information). |
| Satoh 1983 | Intervention not well described |
| Schuhl 1985 | Data collection tool not validated |
| Sherratt 2004 | Outcomes not validated |
| Shertzer 2001 | Policy change‐ staff asked to remain quiet on intervention days |
| Sidorenko 2000a | Therapy as treatment |
| Siedliecki 2006 | Setting |
| Spintge 2000 | Overview‐ insufficient detail |
| Spitzer 2005 | Music not well described; cross‐over trial with and with‐out vibration |
| Standley 1992 | Setting |
| Staricoff 2003a | Study design |
| Staricoff 2003c | Study design |
| Staricoff 2003d | Study design |
| Staricoff 2003e | Study design |
| Steelman 1990 | Intervention not well defined |
| Stermer 1998 | Outcomes not validated |
| Stone 1989 | Study design |
| Strauser 1997 | Setting |
| Swinford 1987 | Intervention |
| Thorgaard 2004 | Outcomes not validated |
| Thorgaard 2005 | Study design |
| Tierney 1978 | Study design; outcomes |
| Uedo 2004 | Insufficient information (intervention and data) |
| Updike 1987 | Study design |
| Updike 1990 | Study design |
| Vollert 2002 | Test (not clinical) situation, healthy controls |
| Vollert 2003 | Setting |
| Walther‐Larsen 1988 | Intervention not well defined; validity of outcomes unclear |
| Yilmaz 2003 | Inappropriate control‐ drugs |
| Zhong 2005 | Duplicate study (Lee 2005) |
Below, we summarise findings for the following comparisons.
Music versus blank tape/headphones alone
Music versus pre‐recorded operating room noise
Music versus scheduled rest
Music versus standard care alone
Music versus white noise
Risk of bias in included studies on music:
Of the 85 RCTs, method of randomisation was unclear in 42 studies. The remaining studies allocated participants to groups via a computer‐generated sequence (N = 19), a table of random numbers (N = 11), drawing lots (N = 9), or coin flips (N = 4). Reporting of allocation concealment was poor with only 11 of 85 studies reporting adequate allocation concealment. Five RCTs had inadequate allocation concealment and 69 studies remain unclear. Blinding to group allocation was achieved in some studies that utilised a control condition involving headphones. Blinding of healthcare personnel and/or the data collector was reported in 20 studies, and double‐blinding of patients and staff was achieved in four studies which investigated the use of music during surgery with general anaesthesia. For studies comparing music to standard care, blinding to group allocation was not possible. Blinded assessment of patient‐reported outcomes was generally not possible for music interventions. Other outcomes, such as physiological measures, were reported as automated in 12 studies. Blinded assessment of at least one outcome was achieved in 16 studies. For 43 studies, no blinding or automation of any outcome measure was achieved, and in six studies it was unclear whether any of the outcomes were blinded or automated. The remaining studies had outcomes rated as a mixture of 'not done' and 'unclear' for blinded assessment. Completeness of data (i.e. outcomes obtained for > 80% of participants) was also poorly reported, with 49 studies scoring as 'done' on this measure (31 were unclear). Five RCTs had incomplete (< 80%) data for at least one outcome measure. Reporting of withdrawals and drop‐outs was not done in the majority of studies (N = 47). In the 38 studies which did report withdrawals and drop‐outs, attrition ranged from zero to 33 participants per study, amounting to 235 withdrawals. Only 22 studies specified from which groups participants withdrew, and overall in these instances the music and control groups had similar attrition (43 and 49 participants respectively; missing information on 143 withdrawals). When studies are weighted according to final sample size, four RCTs arise as outliers in the number of withdrawals (Broscious 1999; Korunka 1992; Phumdoung 2003; Twiss 2006). Korunka 1992 withdrew 23 participants due to missing data (unclear from which groups), and reasons for the withdrawals (N = 92) from the other three studies are largely unrelated to the intervention itself.
Protection against contamination did not appear to be a problem for most studies (N = 80). Two RCTs were cross‐over designs so this could not be achieved. Three RCTs had unclear protection against contamination.
Findings from studies on music versus blank tape/headphones alone:
Anxiety
Eleven RCTs reported sufficient data for extraction on the outcome anxiety (with a total sample of 891 participants: 455 in the music group, and 436 in the control group; Analysis 3.1). Four studies investigated music in the pre‐procedure period (Cooke 2005; Guo 2005; Ikonomidou 2004; Wang 2002), four during a medical procedure (Andrada 2004; Colt 1999; Domar 2005; Mandle 1990), three post‐operatively (Ikonomidou 2004; Nilsson 2003b; Nilsson 2005), and one in the intensive care unit (Lee 2005). Ikonomidou 2004 investigated the use of music in the same patients both pre‐operatively and post‐operatively. Andrada 2004 reports change scores and as such it is inappropriate to combine the data of this study in a meta‐analyses where we are using the standardised mean difference (SMD).
3.1. Analysis.
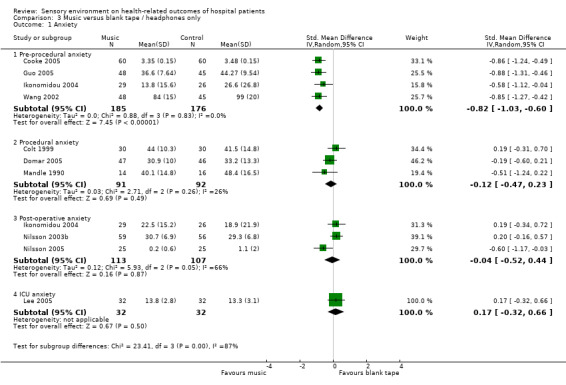
Comparison 3 Music versus blank tape / headphones only, Outcome 1 Anxiety.
Studies conducted in the pre‐procedure period were fairly homogenous (I2 = 0%) and were in favour of the use of music as compared with headphones only (SMD −0.82, 95% CI −1.03 to −0.60, P value < 0.00001). This translates into a mean difference of approximately −9.58 points (95% CI −12.04 to −7.02) on the State Trait Anxiety Inventory (assuming an SD of 11.64; Millar 1995), approximately −23.2 mm (95% CI −29.2 to −17.0) on a 100 mm VAS (assuming an SD of 28.35; Millar 1995), or approximately −3.8 points (95% CI −4.7 to −2.7) on the Hospital Anxiety and Depression scale (assuming an SD of 4.59; Millar 1995).
Studies conducted during medical procedures were also fairly homogenous (I2 = 26%), however, once combined these studies (with 91 and 92 participants in the music and headphones groups respectively) show no strong evidence of an effect when comparing music with headphones alone (SMD −0.12, 95% CI −0.47 to 0.23, P value = 0.49). Not included in this estimate is Andrada 2004 (with 63 and 55 participants in the music and headphones groups respectively); this study showed a significant difference in change scores (MD −5.08, 95% CI −9.04 to −1.12). If Andrada 2004 were to be included in the analysis, it is likely therefore to increase the heterogeneity and modify the effect estimate somewhat in favour of the music group.
Studies conducted during the post‐operative period showed no strong evidence of an effect on average, however these studies, which straddle the line of no effect, have substantial statistical heterogeneity (I2 = 66%). The one study conducted in the intensive care unit also showed no strong evidence of an effect between groups (SMD 0.17, 95% CI −0.32 to 0.66, P value = 0.50).
Due to the observed differences between subgroups, we have not combined all studies in a meta‐analysis, which would reveal substantial heterogeneity (I2 = 74% or 76%, depending on whether the pre‐procedure or post‐procedure data from Ikonomidou 2004 are used).
Exploring the heterogeneity of studies on anxiety:
Conducting a sensitivity analyses to remove studies with higher risk of bias (removing those with unclear or inadequate allocation concealment) leaves just two studies (Cooke 2005; Lee 2005), one of which has findings in favour of music (Cooke 2005: SMD −0.86, 95% CI −1.24 to −0.49) and the other found no strong evidence for an intervention effect (Lee 2005: SMD 0.17, 95% CI −0.32 to 0.66).
Grouping the studies by reason for hospitalisation (seven studies = surgery, two studies = endoscopy, one study = non‐invasive intervention, and one study = ICU), or geographical location (four studies = USA, three studies = Sweden, two studies = China, one study = Spain,and one study = Australia) does not help explain the heterogeneity. All studies were conducted on non‐psychiatric populations.
A post‐hoc analysis shows that four studies (Cooke 2005; Domar 2005; Guo 2005; Lee 2005) provided patients with a choice of music to listen to (I2 = 81.2%), one asked patients to bring music from home (Wang 2002), and the remaining six (five without Andrada 2004) provided set pieces of music to listen to (I2 = 64%, 52%, or 62%, depending on whether the pre‐procedure, post‐procedure, or no data from Ikonomidou 2004 are included). Grouping the studies in this way does little to explain the heterogeneity.
Studies with insufficient data for extraction:
One other RCT also investigated anxiety (Nilsson 2003a); this study was conducted in 151 day patients undergoing surgery with general anaesthetic. This study found no strong evidence of an effect between groups (which were either played music intra‐operatively only, post‐operatively only, or not at all) for anxiety. This finding is in concordance with the studies outlined above that were also conducted in the post‐operative period or during surgery.
Heart rate
Eight RCTs reported sufficient data for extraction on the outcome heart rate (Analysis 3.2). Davis‐Rollans 1987 is a cross‐over study (with 24 participants) presenting individual patient data. The standard deviations for this study have been adjusted to account for the correlation co‐efficient. When combined these studies include 519 participants (music group = 276, control group = 267) with consistent findings (I2 = 0%), showing no strong evidence of an intervention effect (MD 0.40 bpm, 95% CI −1.02 to 1.82, P value = 0.58). A sensitivity analysis conducted without Davis‐Rollans 1987 (495 participants, music group = 252, control group = 243), does little to alter the overall results (I2 = 0%, MD −0.04 bpm, 95% CI −1.86 to 1.95, P value = 0.96).
3.2. Analysis.
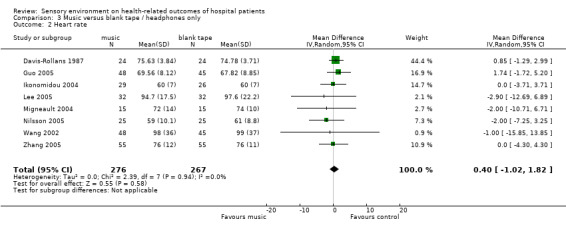
Comparison 3 Music versus blank tape / headphones only, Outcome 2 Heart rate.
Studies with insufficient data for extraction:
Four other RCTs also investigated heart rate (Chlan 1995; Heitz 1992; Mandle 1990; Tsuchiya 2003). These studies included 149 participants (music group = 74, control group = 75). Chlan 1995 reported that the findings were significantly in favour of the music group; however this was a small study with only 11 participants in the music group and nine in the control group. Tsuchiya 2003 also reported a significant difference in favour of the music group at one time point (at extubation), however five other time points (start of surgery, at gallbladder removal, at the end of surgery, at the end of anaesthesia, and in the post‐operative care unit (PACU) demonstrated no strong evidence of an effect. The remaining two studies showed no strong evidence of an effect between groups. These findings typically support the findings of the RCTs reported above.
Blood pressure
Eight RCTs reported sufficient data for extraction on the outcome blood pressure (Analysis 3.3). Of these studies, seven reported systolic blood pressure (music group = 271, control group = 262 participants), six reported diastolic blood pressure (music group = 242, control group = 236 participants), and one reported arterial blood pressure (15 participants per group). The studies are statistically homogenous (I2 = 0%), and demonstrate no strong evidence that music (when compared with headphones only/blank tape) can help reduce systolic blood pressure (MD −0.40 mm Hg, 95% CI −2.48 to 1.67, P value = 0.70), diastolic blood pressure (MD −0.35 mm Hg, 95% CI −2.08 to 1.39, P value = 0.69), or arterial blood pressure (MD 4.00 mm Hg, 95% CI −5.33 to 13.33, P value = 0.40).
3.3. Analysis.
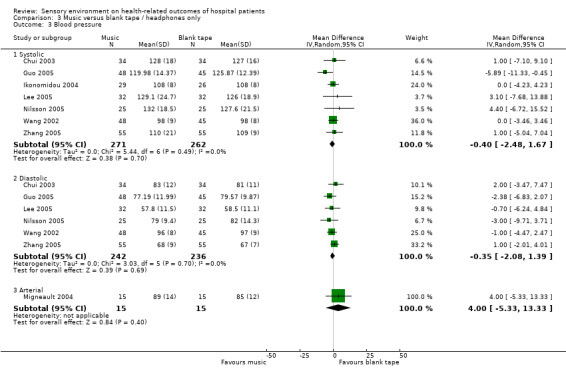
Comparison 3 Music versus blank tape / headphones only, Outcome 3 Blood pressure.
Studies with insufficient data for extraction:
Four other RCTs also investigated blood pressure (Chlan 1995; Heitz 1992; Mandle 1990; Tsuchiya 2003). These studies all found no strong evidence of an effect between groups, apart from Tsuchiya 2003 who found that the control group had significantly higher blood pressure at extubation than the music group. In Tsuchiya 2003, five other time points (as described in the findings for heart rate) did not demonstrate any evidence of an effect. These findings are in concordance with the RCTs described above.
Respiration rate
Two RCTs (Lee 2005; Ikonomidou 2004) reported sufficient data for extraction on the outcome respiration rate (Analysis 3.4). Combined, these studies investigated music on 119 participants (music group = 61, control group = 58). With low heterogeneity (I2 = 13.0%), these studies are in favour of music (MD −1.72 breaths/min, 95% CI −3.00 to −0.44, P value = 0.008). However, there are multiple ways to extract and analyse the data presented in these studies (see Analysis 3.4), and given the concerns of risk of bias and the data presented in Ikonomidou 2004 (see Table 8), it can be concluded that there is no strong evidence for an effect of music on respiration rate when compared to blank tape/headphones alone.
3.4. Analysis.
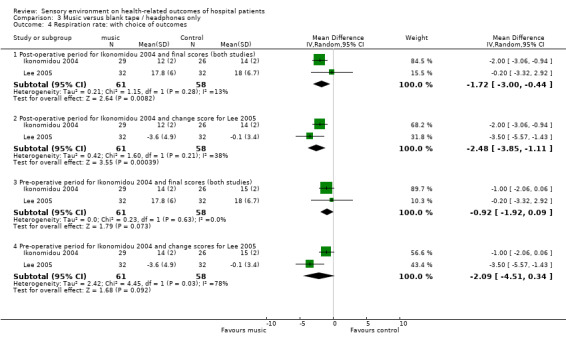
Comparison 3 Music versus blank tape / headphones only, Outcome 4 Respiration rate: with choice of outcomes.
Studies with insufficient data for extraction:
Three other RCTs also investigated respiration rate (Chlan 1995; Davis‐Rollans 1987; Heitz 1992). One small study, Chlan 1995 (with 11 participants in the music group and nine in the control group), reports significant findings in favour of music. Heitz 1992 (N = 40), and Davis‐Rollans 1987 (cross‐over of 24 participants) reported no strong evidence for an effect. These findings further contribute to the conclusion reported above that there is currently no strong evidence to support the use of music for reducing respiration rate when compared to a blank tape or headphones alone.
Anxiolytic medication requirements
One RCT reported sufficient data for extraction on the outcome anxiolytic medication requirements (Mandle 1990). In this study of 30 patients (music group = 14, control group = 16), there was no strong evidence for an effect between groups on diazepam consumption (MD −0.50 mg, 95% CI −2.08 to 1.08, P value = 0.53).
Studies with insufficient data for extraction:
One other RCT also investigated anxiolytic medication requirements (Harikumar 2006). This study of 78 participants (music group = 38, control group = 40) reports that the control group received significantly more midazolam than the music group.
Other outcomes
Some studies reported on other outcomes (Table 12). For this set of outcomes, significant differences were found in favour of music for well‐being and induction time of sedation. No strong evidence of an intervention effect was found for abnormal events, activities of daily living, airway pressure, bispectral index, fatigue, headache, interleukins, mood, nausea, skin conductance, stress hormones, and urinary problems. Mixed evidence was found for heart rate variability characteristics, length of stay, oxygen saturation, and satisfaction. It should be noted that for many of these outcomes, only one or two studies are reported and in cases there is a high risk of bias.
12. Other outcomes: Music versus blank tape/headphones only.
| Outcome | Detailed RCTs (N) | Participants (N) | Heterogeneity (%) | Results | Other RCTs | Participants (N) | Findings |
| Oxygen saturation | N = 1 Nilsson 2005 | Total = 50 Music = 25 Control = 25 | N/A | MD 1.60, 95% CI 0.05 to 3.15, P value = 0.04 In favour of music. | N = 1 Chlan 1995 | Total = 20 Music = 11 Control = 9 | No significant difference between groups. |
| Airway pressure | None | N/A | N/A | N/A | N = 1 Chlan 1995 | Total = 20 Music = 11 Control = 9 | No significant differences between groups. |
| Skin conductance | N = 2 Wang 2002; Guo 2005 | Total = 186 Music = 96 Control = 90 | I2 = 81.7% (one study significant, one study non‐significant) | SMD 0.13, 95% CI −0.55 to 0.80, P value = 0.71 (Analysis 3.5). | None | N/A | N/A |
| Heart rate variability (RR intervals, low and high frequency bands, total power, low/high frequency ratio) | None | N/A | N/A | N/A | N = 1 Chui 2003 | Total = 68 Music = 34 Control = 34 | Heart rate variability data (high frequency power, logarithm of low frequency, and high/low frequency ratio) showed significant positive changes in the music group but not control group. Other variables (RR intervals, low and high frequency bands, low frequency power, and logarithm of high frequency) were non‐significant. |
| Bispectral index (mean, time to reach BIS 60) | N = 2 Ganidagli 2005; Zhang 2005 | Total = 160 Music = 80 Control = 80 | N/A (studies reported different outcomes) | Bispectral index: MD 1.00, 95% CI −1.27 to 3.27, P value = 0.39; Time to reach BIS 60: MD −5.00, 95% CI −15.55 to 5.55, P value = 0.35 | None | N/A | N/A |
| Stress hormones (Cortisol, epinephrine, norepinephrine, adrenocorticotropic hormone‐ ACTH) | N = 3 Migneault 2004; Wang 2002; Guo 2005 | Total = 216 Music = 111 Control = 105 | Cortisol I2 = 51.8% (3 studies) Others I2 = 0% (2 studies) ACTH, N/A (1 study) | Cortisol: SMD −0.32, 95% CI 0.73 to 0.09, P value = 0.13;
Epinephrine: SMD −0.02, 95% CI −0.38 to 0.33, P value = 0.91;
Norepinephrine: SMD −0.08, 95% CI −0.44 to 0.27, P value = 0.64;
ACTH: SMD −0.44, 95% CI −1.17 to 0.28, P value = 0.23 (Analysis 3.6) |
N = 1 Nilsson 2005 | Total = 75 Intra‐operative music = 25 Post‐operative music = 25 Control = 25 | No differences in cortisol levels at any time between groups. Change scores at 2 hours post‐operatively were significantly greater in the post‐operative music group than control. Blood glucose levels did not differ between groups at any time. |
| Mood | N = 1 Chlan 1995 | Total = 20 Music = 11 Control = 9 | N/A | MD −8.50, 95% CI −18.55 to 1.55, P value = 0.10 | None | N/A | N/A |
| Abnormal events (hypoxaemia, hypotension, hypertension, bradycardia, tachycardia, respiratory depression, pruritis) | N = 1 Andrada 2004 | Total = 118 Music = 63 Control = 55 | N/A | Cardio‐respiratory incidents = 0; Oxygen desaturation = 0; Arterial hypertension = 1 control; Arterial hypotension = 2 control; Bradycardia = 3 music, 2 control; Tachycardia = 1 music, 1 control. | N = 1 Cepeda 1998 | Total = 193 Music = 97 Control = 96 | Vomiting (Intra‐operatively/PACU): Music = 0/0%, Control = 2.2/0%
Pruritus (Intra‐operatively/PACU): Music = 26.6/27.6%, Control = 26.1/26.1%
Bradycardia (intra‐operatively/PACU): Music = 0/0%, Control = 2.3/0% Unclear missing data as presented in % values. |
| Headache | N = 1 Nilsson 2003b | Total = 115 Music = 59 Control = 56 | N/A | MD 0.00, 95% CI −0.15 to 0.15, P value = 1.00 | None | N/A | N/A |
| Fatigue | N = 1 Nilsson 2003b | Total = 115 Music = 59 Control = 56 | N/A | MD −0.30, 95% CI −0.78 to 0.18, P value 0.22 | N = 1 Nilsson 2003a | Total = 151 Intra‐operative music = 51 Post‐operative music = 51 Control = 49 | There were no significant differences between groups. |
| Urinary problems | N = 1 Nilsson 2003b | Total = 115 Music = 59 Control = 56 | N/A | MD −0.10, 95% CI −0.40 to 0.20, P value = 0.51 | None | N/A | N/A |
| Well‐being | N = 1 Nilsson 2003b | Total = 115 Music = 59 Control = 56 | N/A | MD 0.30, 95% CI 0.02 to 0.58, P value = 0.03 in favour of music group. | None | N/A | N/A |
| Nausea | N = 2 Nilsson 2003b; Cepeda 1998 | Total = 308 Music = 156 Control = 152 | N/A (different methods of measurement) | MD −0.20, 95% CI −0.50 to 0.10, P value = 0.19 OR 0.82, 95% CI 0.35 to 1.93, P value = 0.64 | N = 1 Nilsson 2003a | Total = 151 Intra‐operative music = 51 Post‐operative music = 51 Control = 49 | There were no significant differences between groups. |
| Satisfaction | N = 1 Zhang 2005 | Total = 110 Music = 55 Control = 55 | N/A | MD 1.60, 95% CI 1.29 to 1.91, P value < 0.00001 in favour of music group | N = 2 Cepeda 1998; Nilsson 2003a | Total = 344 Intra‐operative music = 148 Post‐operative music = 51 Control = 145 | There were no significant differences between groups. |
| Length of stay | N = 1 Blankfield 1995 | Total = 61 Music = 32 Control = 29 | N/A | MD 0.00, 95% CI −0.99 to 0.99, P value = 1.00 | N = 2 Harikumar 2006; Heitz 1992 | Total = 118 Music = 58 Control= 60 | Harikumar 2006 reports that recovery time was significantly longer (difference in medians = 10 minutes) in the control group. Heitz 1992 reports no significant differences between groups. |
| Activities of daily living | N = 1 Blankfield 1995 | Total = 61 Music = 32 Control = 29 | N/A | MD −0.30, 95% CI −2.63 to 2.03, P value 0.80 | None | N/A | N/A |
| Serum interleukins (IL‐6) | N = 1 Zhang 2005 | Total = 110 Music = 55 Control = 55 | N/A | MD −7.40, 95% CI −22.61 to 7.81, P value = 0.34 | None | N/A | N/A |
| Induction time of sedation (minutes) | N = 1 Zhang 2005 | Total 110 Music = 55 Control = 55 | N/A | MD −6.00, 95% CI −10.49 to −1.51, P value = 0.009 in favour of music. | None | N/A | N/A |
CI: confidence interval; MD: mean difference; SMD: standardised mean difference; PACU: post‐operative care unit; RR: respiration rate
Findings from studies on music versus pre‐recorded operating room noise:
Anxiety
Studies with insufficient data for extraction:
One RCT investigated anxiety (Cruise 1997; N = 62) and found no strong evidence for an intervention effect.
Heart rate
Studies with insufficient data for extraction:
One RCT investigated heart rate (Cruise 1997; N = 62) to find no strong evidence for an intervention effect.
Blood pressure
Studies with insufficient data for extraction:
One RCT investigated blood pressure (Cruise 1997; N = 62). This study found no strong evidence for an intervention effect on diastolic blood pressure. However, significant differences were observed for systolic blood pressure; in this study systolic blood pressure was unexpectedly increased in the music group (but not significantly in the operating room noise group) immediately after retrobulbar block, and at 15 and 30 minutes after the retrobulbar block the music group had higher systolic blood pressure than the operating room noise group (which decreased over the course of the surgery).
Respiration rate
Studies with insufficient data for extraction:
One RCT investigated respiration rate (Cruise 1997; N = 62) to find no strong evidence for an intervention effect.
Other outcomes
Other outcomes reported for the comparison music versus operating theatre noise were: length of stay (Ayoub 2005; Korunka 1992); time to mobilisation (Nilsson 2001); nausea (Nilsson 2001); fatigue (Nilsson 2001); and well‐being (Nilsson 2001). The two studies that reported length of stay have differing findings (Korunka 1992 reports results significantly in favour of music, whereas Ayoub 2005 reports no strong evidence for an effect), however these studies can not be combined in a meta‐analysis due to insufficient data for extraction. Nilsson 2001 found that those who received music were faster to mobilise to a sitting position than the control group however there was no difference between groups in the time it took to stand and walk. For the patient‐reported outcomes (fatigue, nausea, and well‐being) Nilsson 2001 found no strong evidence of an effect.
Findings from studies on music versus scheduled rest:
Anxiety
Eight RCTs (Barnason 1995/1996; Chlan 1998; Elliot 1994; Sendelbach 2006; Voss 2004; White 1992; White 1999; Wong 2001) investigated music versus scheduled rest for anxiety (Analysis 4.1). These studies (music =189, control = 187), which individually are either non‐significant or in favour of music, have substantial heterogeneity (I2 = 82%), and therefore we have not pooled the data.
4.1. Analysis.
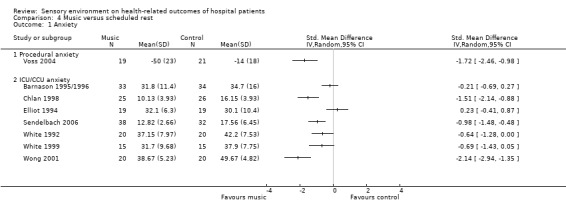
Comparison 4 Music versus scheduled rest, Outcome 1 Anxiety.
Exploring the heterogeneity of studies on anxiety:
One study (Barnason 1995/1996) did not use allocation concealment, however removing this study in a sensitivity analysis does little to reduce the heterogeneity (I2 = 80%). Studies were all conducted in either intensive, critical, or coronary care units (in Voss 2004 patients were undergoing chair rest in a Surgical Intensive Care Unit), and on non‐psychiatric populations. Six of the studies were conducted in the USA (I2 = 71%) and the other two were conducted in Australia (Elliot 1994) and China (Wong 2001).
A post‐hoc subgroup analysis of the three studies which played patients in the intervention group set pieces of music (I2 = 58%; Elliot 1994; White 1992; White 1999), and the remaining studies which offered patients a choice of music from a selection (I2 = 84%; Barnason 1995/1996; Chlan 1998; Sendelbach 2006; Voss 2004; Wong 2001), does little to explain the heterogeneity.
Heart rate
Four studies (Elliot 1994; Sendelbach 2006; White 1992; White 1999) reported sufficient data for extraction on heart rate (Analysis 4.2). These studies demonstrated little statistical heterogeneity (I2 = 0%), and overall (music group = 94, control group = 86) found no strong evidence of an effect between groups (MD −2.76 bpm, 95% CI −6.65 to 1.13, P value = 0.16).
4.2. Analysis.
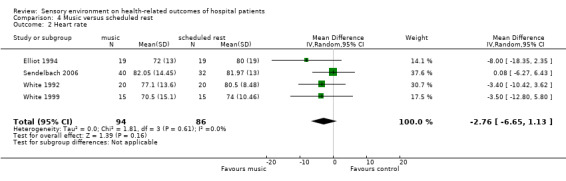
Comparison 4 Music versus scheduled rest, Outcome 2 Heart rate.
Studies with insufficient data for extraction:
Two other RCTs also reported on heart rate (Barnason 1995/1996; Chlan 1998). Barnason 1995/1996 (music group = 33, control group = 34) found no strong evidence of an effect between groups, and Chlan 1998 (music group = 27, control group = 27) reports a significant effect in favour of music for heart rate reduction.
Blood pressure
Three studies (Elliot 1994; Sendelbach 2006; White 1999) reported systolic blood pressure (music group = 74, control group = 66), two studies (Elliot 1994; Sendelbach 2006) reported diastolic blood pressure (music group = 59, control group = 51), and one study (Wong 2001) reported arterial blood pressure (music group = 20, control group = 20). It is possible that this outcome is subject to selective outcome reporting (as it could be expected that studies would have collected both systolic and diastolic blood pressure data). For each outcome, studies demonstrated little statistical heterogeneity (I2 = 0%; Analysis 4.3). Combined findings for systolic blood pressure showed no strong evidence of an effect (MD −1.51 mm Hg, 95% CI −6.65 to 3.63, P value = 0.56), but for diastolic blood pressure the findings were favour of music (MD −5.29 mm Hg, 95% CI −8.78 to −1.79, P value = 0.003). The one study that assessed arterial blood pressure showed no strong evidence of an effect (MD −4.75 mm Hg, 95% CI −13.98 to 4.48, P value = 0.31).
4.3. Analysis.
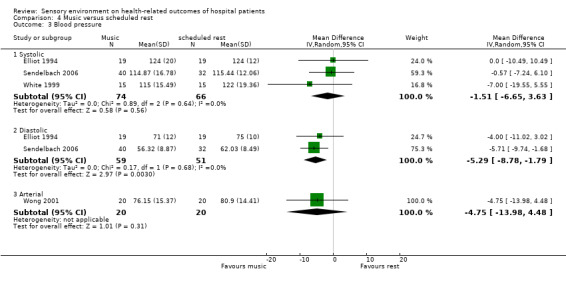
Comparison 4 Music versus scheduled rest, Outcome 3 Blood pressure.
Studies with insufficient data for extraction:
One study (Barnason 1995/1996; music group = 33, control group = 34) also assessed blood pressure and found no strong evidence of an effect.
Respiration rate
Three RCTs (White 1992; White 1999; Wong 2001) measuring respiration rate (music group = 55, control group = 55), when combined (I2 = 0%) found a significant difference (MD −2.04 breaths/min, 95% CI −3.43 to −0.66, P value = 0.004) in favour of the music group (Analysis 4.4).
4.4. Analysis.
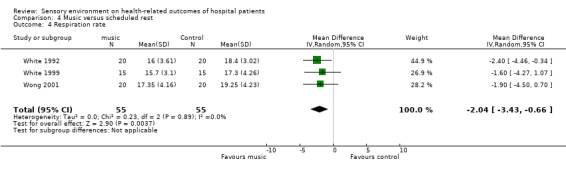
Comparison 4 Music versus scheduled rest, Outcome 4 Respiration rate.
Studies with insufficient data for extraction:
Chlan 1998 also reported on respiration rate, and this study (with 27 patients in each group) also reported a significant effect in favour of the music group for respiration rate over the course of the experiment.
Other outcomes
One study also reported on sleep quality (Barnason 1995/1996; music group = 33, control group = 34) and found no strong evidence of an intervention effect (MD 1.17 points on the Richards‐Campbell Sleep Questionnaire, 95% CI 0.00 to 2.34, P value = 0.05).
Findings from studies on music versus standard care alone:
Anxiety
Twenty‐nine RCTs reporting sufficient data for extraction (with a total sample size of 1812 participants: music group = 916, control group = 896), investigated the use of music versus standard care alone for the reduction of anxiety (Analysis 5.1). Nine studies provided music in the waiting period prior to a medical procedure (Buffum 2006; Cooke 2005; Gaberson 1991; Gaberson 1995; Hayes 2003; Padmanabhan 2005; Taylor‐Piliae 2002; Winter 1994; Yung 2003), 15 studies provided the music throughout a medical procedure (Argstatter 2006; Bally 2003; Binnings 1987; Chan 2003; Chang 2005; Chlan 2000; Kwekkeboom 2003; Lembo 1998; Lepage 2001; McRee 2003; Mennegazzi 1991; Smith 2001; Smolen 2002; Voss 2004; Yang 2003), and five studies investigated the use of music in the post‐operative period or in an intensive care environment (Lueders Bolwerk 1990; Mullooly 1998; Twiss 2006; White 1999; Zimmerman 1988).
5.1. Analysis.
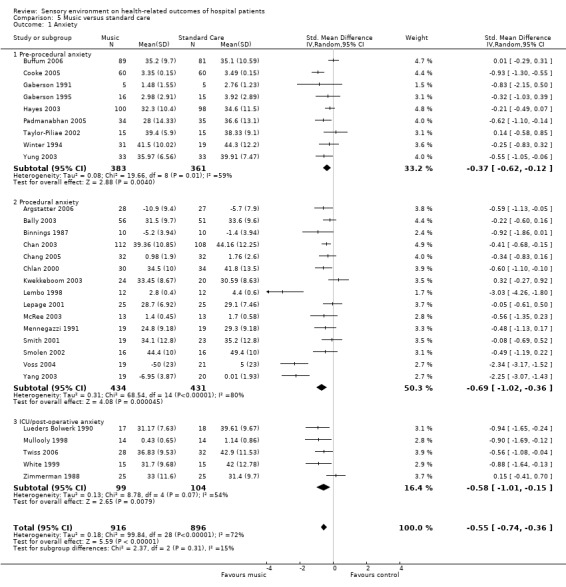
Comparison 5 Music versus standard care, Outcome 1 Anxiety.
In a random‐effects analysis, all three subgroups showed average treatment effects in favour of music (pre‐procedural SMD −0.37, 95% CI −0.62 to −0.12; procedural SMD −0.69, 95% CI −1.02 to −0.36; ICU/post‐operative SMD −0.58, 95% CI −1.01 to −0.15), as did the subgroups combined (SMD −0.55, 95% CI −0.74 to −0.36). Individual studies generally point in favour of music, or show no difference between groups. However, as indicated by the Chi2 statistics in the analysis, heterogeneity is present; the subgroups contain moderate to substantial heterogeneity (pre‐procedural anxiety I2 = 59.3%, procedural anxiety I2 = 79.6%, ICU/post‐operative anxiety I2 = 54.5%), as do all the studies combined (total I2 = 72.0%). A funnel plot of the studies indicates there may be some evidence of publication bias, with a lack of small studies with small treatment effects (Figure 3).
3.
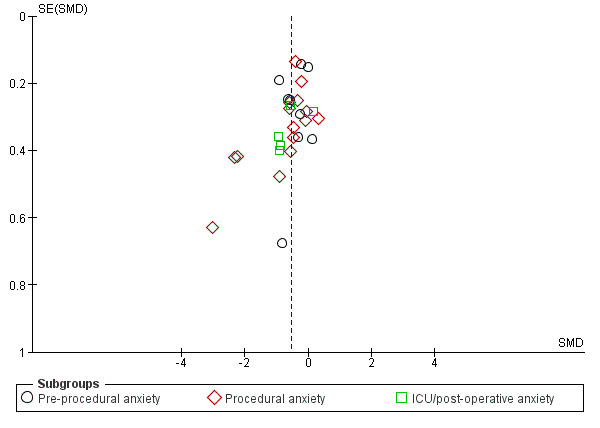
Funnel plot of comparison: 5 Music versus standard care, outcome: 5.1 Anxiety.
Exploring the heterogeneity of studies on anxiety:
Removing all studies with unclear concealment of allocation from the analysis, as well as Voss 2004 in which there were significant differences at baseline for the outcome anxiety, leaves 5 studies (Bally 2003; Chan 2003; Cooke 2005; Smith 2001; Twiss 2006), which combine with moderate heterogeneity (I2 = 56.5%), to estimate a slightly lower, average treatment effect (SMD) of −0.46 (95% CI −0.74 to −0.19) in favour of music.
Sub‐grouping studies into reason for hospitalisation (surgery or percutaneous interventions (n = 20); endoscopic procedures (n = 5; Chan 2003; Chlan 2000; Hayes 2003; Lembo 1998; Smolen 2002); coronary care (n = 3; Lueders Bolwerk 1990; White 1999; Zimmerman 1988); and radiation therapy (n = 1; Smith 2001), yields largely heterogeneous groupings (I2 = 73.2%, 79.9%, and 73.7%, respectively), so does not appear an appropriate variable to explain the heterogeneity between studies. All studies included in this comparison were carried out on non‐psychiatric populations. The majority of studies were conducted in the USA (n = 19), four in China (Chan 2003; Taylor‐Piliae 2002; Yang 2003; Yung 2003), two in Canada (Bally 2003; Lepage 2001), one in each of Taiwan (Chang 2005), Germany (Argstatter 2006), England (Padmanabhan 2005), and Australia (Cooke 2005). The two Canadian studies showed no strong evidence of a treatment effect (SMD −0.16, 95% CI −0.48 to 0.15, I2 = 0%), whereas studies from other locations achieved mixed results, favouring music overall but with substantial heterogeneity. It is likely therefore that location has little to do with the size of treatment effects for this comparison.
A post‐hoc subgroup analysis of all studies according to whether patients were provided with a choice of music or were provided with a set piece(s) selected by the researcher, suggests that providing patients with set pieces increases the average effect size. Nine studies (Argstatter 2006; Binnings 1987; Gaberson 1991; Gaberson 1995; Lembo 1998; Lueders Bolwerk 1990; McRee 2003; Padmanabhan 2005; White 1999) with some heterogeneity (I2 = 49.9%) provided set pieces (SMD −0.83, 95% CI −1.19 to −0.47, P value < 0.00001), and the remaining 20 studies (I2 = 74.8%) offered patients a choice of music (SMD −0.45, 95% CI −0.66 to −0.23, P value < 0.00001). The five studies listed above with adequate allocation concealment however, all offered patients a choice of music from the researchers' selection, which may confound the observation made here.
Studies with insufficient data for extraction:
A further five RCTs investigated music versus standard care for anxiety. One study conducted during the waiting period before a medical procedure favoured music (Daub 1988), in line with the findings above. Four studies investigated the use of music during a procedure (non‐invasive/rehabilitation = Ferguson 2004 and Nowobilski 2005; endoscopic = Palakanis 1994; percutaneous = Schneider 2001). Two of these studies (with 36 and 30 participants respectively) found no differences between groups (Nowobilski 2005; Schneider 2001). One study with 50 participants found significant differences in favour of music (Palakanis 1994), and one also favoured music (Ferguson 2004; with 11 participants) although the control group were also more anxious at baseline. These mixed results reflect the heterogeneity observed in the meta‐analysis above.
Heart rate
Twenty‐one RCTs reporting sufficient data for extraction (with a total sample size of 1653 participants: 838 in the intervention group, and 815 in the control) investigated the use of music versus standard care on heart rate. The studies combine with substantial heterogeneity (I2 = 60%; Analysis 5.2). In a random‐effects analysis, the average treatment effect is estimated to be −2.72 bpm (95% CI −4.70 to −0.74, P value = 0.007).
5.2. Analysis.
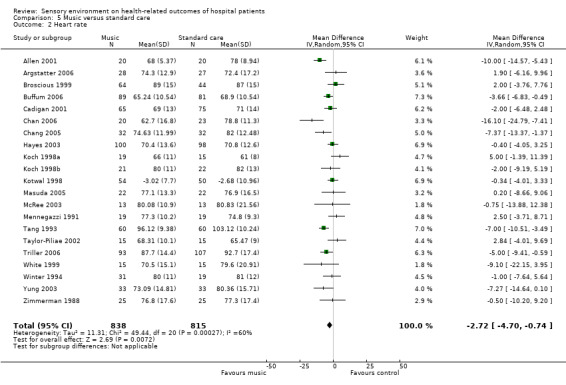
Comparison 5 Music versus standard care, Outcome 2 Heart rate.
Exploring the heterogeneity of studies on heart rate:
Whereas for most studies allocation concealment is unclear, one study (Allen 2001) definitely did not use allocation concealment. Removing this study in a sensitivity analysis removes some of the heterogeneity (resulting in I2 = 52.1%) and reduces the overall effect size somewhat (MD −2.25 bpm, 95% CI −4.14 to −0.36, P value = 0.02). One study (White 1999) included a restful environment for the intervention group. Removing this study from the analysis, so all remaining studies are of music alone, increases the heterogeneity (I2 = 60.9%).
Sub‐grouping studies by type of procedure: pre‐procedure (N = 4), non‐invasive (N = 1), endoscopic (N = 2), percutaneous/surgical (N = 11), post‐operative (N = 1), and in care unit after myocardial infarction (N = 2), resolves some of the heterogeneity issue. The four pre‐procedure studies (Hayes 2003; Taylor‐Piliae 2002; Winter 1994; Yung 2003) fairly consistently (I2 = 26.7%) conclude that there is no strong evidence for an effect of music for reducing heart rate during this period (MD −1.07 bpm, 95% CI −4.44 to 2.30, P value = 0.53). The one study conducted during non‐invasive procedures (lithotripsy; Koch 1998b) also found no strong evidence of an effect. The two studies (Kotwal 1998; Triller 2006) conducted during endoscopic procedures had mixed findings (I2 = 60.6%), as did the 11 studies conducted during percutaneous interventions (I2 = 73.1%). One study on post‐operative patients (Masuda 2005, MD 0.20 bpm, 95% CI −8.66 to 9.06), and two studies (White 1999; Zimmerman 1988) conducted on patients recovering from myocardial infarction (I2 = 6.9%, MD −3.65 bpm, 95% CI −11.76 to 4.47) also found no strong evidence of an effect. The heterogeneity largely exists amongst the studies carried out during invasive procedures (endoscopic and percutaneous), with other procedures finding no strong evidence of an effect.
Studies were mostly conducted in the USA (N = 12), whilst some were conducted in China (N = 3), Taiwan (N = 2), India (N = 1), Japan (N =1), Slovenia (N = 1), and Germany (N = 1). Although there is some heterogeneity amongst the 12 USA studies (I2 = 53.0%), most of this can be explained by Allen 2001; the only study that did not use allocation concealment. Removing Allen 2001 from this subgroup reduces the heterogeneity (to I2 = 2.1%) and results in a mean difference of −0.97 bpm (95% CI −2.65 to 0.70, P value = 0.26), showing no strong evidence of an effect. The three studies conducted in China (Chan 2006; Taylor‐Piliae 2002; Yung 2003) show mixed findings (I2 = 82.8%), whereas the two studies conducted in Taiwan (Chang 2005; Tang 1993) were consistently (I2 = 0%) in favour of music (MD −7.09, 95% CI −10.13 to −4.06). Studies from India (Kotwal 1998), Japan (Masuda 2005), and Germany (Argstatter 2006) showed no strong evidence of an effect, whereas the study conducted in Slovenia (Triller 2006) did favour music.
A post‐hoc exploration can group studies according to whether patients were provided a choice of music (N = 13), asked to bring music from home (N = 2; Koch 1998a; Koch 1998b), or provided with set pieces (N = 6; Argstatter 2006; Cadigan 2001; Kotwal 1998; McRee 2003; Triller 2006; White 1999). The set piece subgroup has little statistical heterogeneity (I2 = 0%), and overall shows no strong evidence of an effect (MD −2.03 bpm, 95% CI −4.25 to 0.19, P value = 0.07). Moderate heterogeneity exists (I2 = 50.9%) between the two studies which asked patients to bring music from home. Together these two studies also show no strong evidence of an effect (MD 1.70 bpm, 95% CI −5.15 to 8.55, P value = 0.63). And, although favouring music for the reduction of heart rate (MD −3.54 bpm, 95% CI −6.25 to −0.84, P value = 0.01), the patient choice group has substantial statistical heterogeneity (I2 = 67.5%).
Studies with insufficient data for extraction:
Seven other RCTs also collected data on heart rate. Two studies investigated music during endoscopic procedures (Palakanis 1994; Smolen 2002), and with study sample sizes of 50 and 32 patients respectively, were in favour of music. Three studies (of 107, 50, and 30 participants) were conducted during percutaneous interventions (Bally 2003; Lepage 2001; Schneider 2001) and showed no strong evidence of an effect. One study conducted in the post‐operative period (Heitz 1992, with 60 participants) found no strong evidence of an effect, in line with the findings above. And one study was conducted during rehabilitative exercises (Ferguson 2004); patients in this study were undergoing different forms of exercise and rehabilitation (passive and active), making it unclear as to the appropriate direction of findings (i.e. if the aim of using music is for patients to work harder, then an increase in heart rate would be appropriate, but if the aim was to decrease stress, then a decrease in heart rate would be appropriate). This study of only 11 participants found no strong evidence of an effect.
Blood pressure
Eighteen RCTs reported sufficient information for assessment of the outcome systolic blood pressure (Allen 2001; Argstatter 2006; Broscious 1999; Buffum 2006; Cadigan 2001; Chan 2006; Chang 2005; Hayes 2003; Koch 1998a; Koch 1998b; Kotwal 1998; Masuda 2005; McRee 2003; Mennegazzi 1991; Triller 2006; White 1999; Winter 1994; Zimmerman 1988), 17 reported diastolic blood pressure (Allen 2001; Argstatter 2006; Broscious 1999; Buffum 2006; Cadigan 2001; Chan 2006; Chang 2005; Hayes 2003; Koch 1998a; Koch 1998b; Kotwal 1998; Masuda 2005; McRee 2003; Mennegazzi 1991; Triller 2006; Winter 1994; Zimmerman 1988), and two reported arterial blood pressure (Tang 1993; Yung 2003) (Analysis 5.3). Again, this outcome is subject to the risk of selective outcome reporting. The total sample size of the studies that measured systolic blood pressure was 1437 (730 in the intervention group and 707 in the control), with studies combining to show substantial statistical heterogeneity (I2 = 67%). All but one (White 1999) of these studies also reported diastolic blood pressure (overall N = 1407; intervention group = 715, control group = 692). For this outcome there was less statistical heterogeneity (I2 = 50%), and the overall findings showed no strong evidence of an effect (MD −0.97 mm Hg, 95% CI −2.58 to 0.63, P value = 0.23). There were 186 participants in the two studies that assessed arterial blood pressure (93 in the intervention group and 93 in the control group), and these studies were consistently (I2 = 0%) in favour of the music group for reduction of blood pressure (MD −9.86 mm Hg, 95% CI −12.06 to −7.65, P value < 0.00001).
5.3. Analysis.
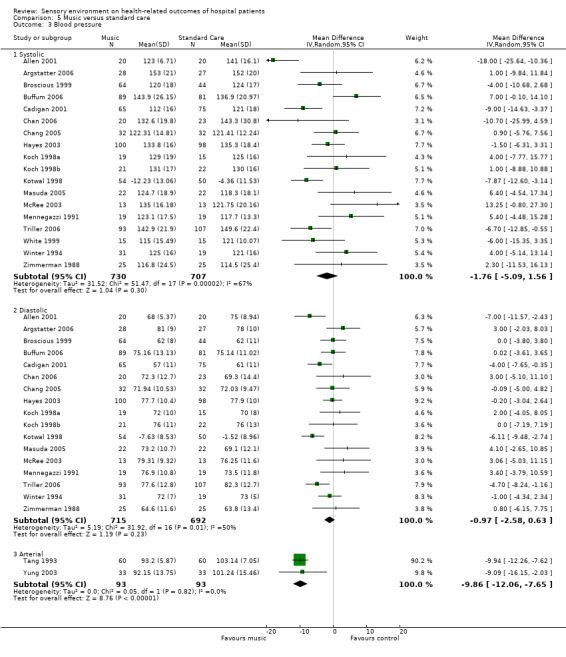
Comparison 5 Music versus standard care, Outcome 3 Blood pressure.
Exploring the heterogeneity of studies on blood pressure:
In one study allocation concealment was definitely not used (Allen 2001). This study had the largest treatment effect in favour of music of all the studies that reported on systolic and diastolic blood pressure. Removing this study in a sensitivity analysis reduces the heterogeneity between studies (systolic blood pressure I2 = 55%, diastolic blood pressure I2 = 42%), and the combined effects continue to demonstrate no strong evidence of an effect (systolic blood pressure: MD −0.93 mm Hg, 95% CI −3.90 to 2.04, P value = 0.54; diastolic blood pressure: MD −0.66 mm Hg, 95% CI −2.20 to 0.87, P value = 0.40).
Ten studies were conducted on patients undergoing surgical/percutaneous procedures (Allen 2001; Argstatter 2006; Broscious 1999; Cadigan 2001; Chan 2006; Chang 2005; Koch 1998a; McRee 2003; Mennegazzi 1991; Tang 1993), two were conducted on patients undergoing endoscopic procedures (Kotwal 1998; Triller 2006), four were conducted during the waiting period before a medical procedure (Buffum 2006; Hayes 2003; Winter 1994; Yung 2003), two were conducted on patients in coronary or intensive care units (White 1999; Zimmerman 1988), one was conducted during a non‐invasive medical procedure (Koch 1998b), and one was conducted on post‐operative patients (Masuda 2005). Moderate heterogeneity exists in the nine studies conducted during percutaneous/surgical procedures measuring systolic and diastolic blood pressure (Systolic I2 = 74%; Diastolic I2 = 51%), attributable largely to Allen 2001. Overall, these studies show no strong evidence of an effect (Systolic MD −2.57 mm Hg, 95% CI −8.36 to 3.21, P value = 0.38; Diastolic MD −0.31 mm Hg, 95% CI −2.83 to 2.22, P value = 0.81). The two studies conducted during endoscopic procedures had little statistical heterogeneity (systolic and diastolic I2 = 0%) and were in favour of music for reducing systolic and diastolic blood pressure (Systolic MD −7.44 mm Hg, 95% CI −11.18 to −3.69, P value = 0.0001; Diastolic MD −5.44 mm Hg, 95% CI −7.88 to −3.00, P value < 0.0001). The studies in patients receiving music during the waiting period showed no strong evidence of an effect for systolic or diastolic blood pressure (Systolic MD 2.53 mm Hg, 95% CI −3.09 to 8.15, P value = 0.38 [I2 = 51%]; Diastolic MD −0.39 mm Hg, 95% CI −2.25 to 1.47, P value = 0.68 [I2 = 0%]), as did the studies conducted in coronary care units (Systolic MD −3.40 mm Hg, 95% CI −11.14 to 4.35, P value = 0.39 [I2 = 0%]; Diastolic MD 0.80 mm Hg, 95% CI −6.15 to 7.75, P value = 0.82 [Zimmerman 1988]). The studies conducted during non‐invasive procedures and during the post‐operative period also showed no strong evidence of an effect for systolic and diastolic blood pressure. Of the studies that measured arterial blood pressure (both significantly in favour of music), one was conducted on percutaneous/surgical patients and one was conducted during the waiting period.
Twelve of the studies that measured blood pressure were conducted in the USA (Allen 2001; Broscious 1999; Buffum 2006; Cadigan 2001; Hayes 2003; Koch 1998a; Koch 1998b; McRee 2003; Mennegazzi 1991; White 1999; Winter 1994; Zimmerman 1988). Two were conducted in China (Chan 2006; Yung 2003), two in Taiwan (Chang 2005; Tang 1993), and one in each of Germany (Argstatter 2006), India (Kotwal 1998), Japan (Masuda 2005), and Slovenia (Triller 2006). For the outcome systolic blood pressure there is substantial heterogeneity between the studies conducted in the USA (I2 = 73%), largely attributable to Allen 2001. For the studies that measured arterial blood pressure with positive findings, one was conducted in China, and one was conducted in Taiwan.
One study (White 1999), which reported on systolic blood pressure, incorporated a restful environment for those in the music group. Removing this study in a sensitivity analysis (so all remaining studies compare music alone to standard care), does little to change the statistical heterogeneity (I2 = 69%). Twelve studies offered participants a selection of music to choose from (Allen 2001; Broscious 1999; Buffum 2006; Chan 2006; Chang 2005; Hayes 2003; Masuda 2005; Mennegazzi 1991; Tang 1993; Winter 1994; Yung 2003; Zimmerman 1988), two requested patients to bring their own music from home (Koch 1998a; Koch 1998b), and six played participants set pieces selected by the investigators (Argstatter 2006; Cadigan 2001; Kotwal 1998; McRee 2003; Triller 2006; White 1999. For the outcome systolic blood pressure, grouping studies in this way does little to explain the heterogeneity (choice from selection: systolic I2 = 71%, diastolic I2 = 24%; music from home: systolic I2 = 0%, diastolic I2 = 0%; set pieces: systolic I2 = 52%, diastolic I2 = 66%). The two studies which requested participants to bring their own music from home produced consistent results showing no strong evidence of effect (systolic MD 2.24 mm Hg, 95% CI ‐5.33 to 9.81, P value = 0.56; diastolic MD 1.17 mm Hg, 95% CI −3.46 to 5.80, P value = 0.62), however, these studies were conducted by the same investigators and are likely to have many other similarities.
Studies with insufficient data for extraction:
Seven other RCTs collected data on blood pressure (Bally 2003; Ferguson 2004; Heitz 1992; Lepage 2001; Palakanis 1994; Schneider 2001; Smolen 2002). Within these studies, sample sizes range from 11 to 107 participants (mean = 48.57, SD = 30.50, median = 50). There is plausible risk of bias in these studies that raises some doubt about the results; only two studies were judged as having adequate allocation concealment (Bally 2003; Palakanis 1994). Studies were based in the USA (Ferguson 2004; Heitz 1992; Palakanis 1994; Smolen 2002), Canada (Bally 2003; Lepage 2001), and Germany (Schneider 2001). All studies offered patients a choice of music from a selection. Findings from these studies generally mirror those of the RCTs described above. Three studies were conducted during percutaneous/surgical interventions (Bally 2003; Lepage 2001; Schneider 2001), with one (Schneider 2001) reporting a significant drop in blood pressure from pre‐ to post‐treatment in the music group and no change in the control group (the other two studies showed no strong evidence of an effect). Two studies were conducted on patients undergoing endoscopic examinations (Palakanis 1994; Smolen 2002), and both reported significant findings favouring the music group. Ferguson 2004 was conducted on patients undergoing non‐invasive "range‐of‐motion" exercises with non‐significant findings. And Heitz 1992 was conducted in the post‐operative period, reporting no difference between groups.
Respiration rate
Nine RCTs reported sufficient information for data extraction on respiration rate. When combined these studies had an overall sample of 644 patients (322 in each group), and the study findings were heterogeneous (I2 = 80%; Analysis 5.4), so have not been pooled.
5.4. Analysis.
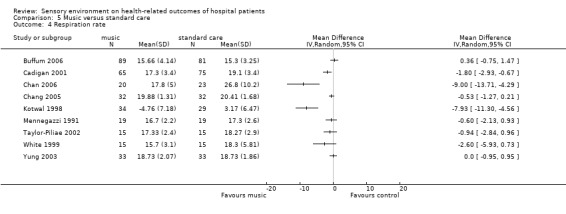
Comparison 5 Music versus standard care, Outcome 4 Respiration rate.
Exploring the heterogeneity of studies on respiration rate:
The quality of studies was mixed, with only one (Taylor‐Piliae 2002) reporting adequate concealment of allocation.
Five studies (Cadigan 2001; Chan 2006; Chang 2005; Mennegazzi 1991; Yung 2003) were conducted on patients undergoing percutaneous or surgical procedures (I2 = 78%), two studies (Buffum 2006; Taylor‐Piliae 2002) were conducted during the waiting period (I2 = 25%; MD −0.05 breaths per minute, 95% CI −1.24 to 1.13, P value = 0.93), one study (Kotwal 1998) was conducted during endoscopic procedures (favouring music), and one study (White 1999) was conducted in a coronary care unit (non‐significant findings).
Four studies were conducted in the USA (I2 = 64%), three in China (I2 = 85%), one in Taiwan, and one in India; grouping studies in this way does little to explain the heterogeneity.
One study (White 1999) incorporated a restful environment for the music group. Removing this study in a sensitivity analysis so that all remaining studies compare music alone to standard care does little to change the findings (I2 = 82%). Three studies exposed participants to set pieces of music (Cadigan 2001; Kotwal 1998; White 1999) and the remaining six studies offered participants a choice of music from a selection. Sub‐grouping studies in this way leaves 68% heterogeneity in the patient choice group (MD −0.60 breaths per minute, 95% CI −1.57 to 0.36, P value = 0.22) and 82% in the set pieces group. Much of the statistical heterogeneity in this set of studies is contributed by the significant findings of Chan 2006 and Kotwal 1998, however none of the clinical or methodological differences explored above explain these findings.
Studies with insufficient data for extraction:
Three other RCTs (Ferguson 2004; Heitz 1992; Lepage 2001) also collected data on respiration rate. Sample sizes were 11, 60 (with two control groups), and 50, respectively. Within these studies there is plausible bias which raises some doubt about the results. None of the studies had adequate allocation concealment. One study (Heitz 1992) reported that healthcare professionals were partially blinded to group allocation. This study had a third 'headphones only' group so nurses were not aware if those wearing headphones were actually receiving music, but they could recognise who was allocated to the standard care alone group. No studies reported a power calculation. None of the studies had clear completeness of dataset. Ferguson 2004 had different baseline characteristics between groups. None of the studies reported on withdrawals and drop‐outs. The studies (conducted during non‐invasive procedures, percutaneous interventions, and post‐operatively) all offered patients a choice of music from a selection and showed no difference between groups.
Anxiolytic medication requirements
Three RCTs reported sufficient data for extraction on the use of anxiolytic medications requirements (Analysis 5.5). These studies investigated 201 participants (music group = 100, control group = 101) and show considerable statistical heterogeneity (I2 = 91%) and for this reason have not been pooled. Two of the studies (Lepage 2001; Smolen 2002) report findings in favour of music, and one larger study reports no difference between groups (Schiemann 2002).
5.5. Analysis.
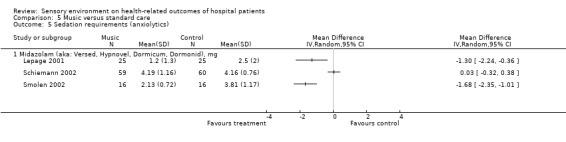
Comparison 5 Music versus standard care, Outcome 5 Sedation requirements (anxiolytics).
Exploring the heterogeneity of studies on anxiolytic medication requirements:
In all three studies allocation concealment is unclear, blinding of group allocation is not done, power calculations are not reported, and withdrawals and drop‐outs are not reported. All studies offer adequate protection against contamination and report that groups were similar at baseline. The two studies with positive outcomes (Lepage 2001; Smolen 2002) have unclear completeness of data, whereas the study with non‐significant findings (Schiemann 2002) did report completeness of dataset. Schiemann 2002 and Smolen 2002 were conducted on patients undergoing endoscopic procedures, and Lepage 2001 was conducted in patients undergoing percutaneous interventions. The studies with positive results were conducted in the USA and Canada, and study with non‐significant findings was conducted in Germany. The two studies with positive outcomes (Lepage 2001; Smolen 2002) offered patients in the intervention group a choice of music (I2 = 0%, MD −1.55 mg, 95% CI −2.10 to −1.00, P value < 0.00001). The study with non‐significant findings (Schiemann 2002, MD 0.03 mg, 95% CI −0.32 to 0.38) played patients in the intervention group set pieces of music. It is unclear in Schiemann 2002 if midazolam consumption is an outcome measure or baseline characteristic; this may provide an alternative explanation for the non‐significant findings in this study. From these observations, it is difficult to draw conclusions as to the explanation for the statistical heterogeneity.
Other outcomes
A number of studies reported on additional outcomes which we have summarised in Table 13. For this set of outcomes, apart from fatigue and uncertainty, significant differences in favour of music were found for most patient‐reported outcomes (mood, anger, depression, nausea, and satisfaction). Groups did not differ however, on most physiological outcomes (skin temperature, oxygen saturation, blood flow, bispectral index, lung function, requirement for oxygen supplementation). Findings for the outcome cortisol are mixed, and there was no strong evidence of an effect for other stress hormones (prolactin and catecholamines). Significant differences in favour of the music group were found for intubation time and length of stay (although another study at higher risk of bias, with insufficient data for extraction, was non‐significant). It should be noted that few studies reported on each of these outcomes (for 10 of the 16 outcomes only one study is included), and in some cases the risk of bias in studies is high.
13. Other outcomes: Music versus Standard Care.
| Outcome | Detailed RCTs (N) | Participants (N) | Heterogeneity (%) | Results | Other RCTs | Participants (N) | Findings | Comments |
| Skin temperature | N = 4 Cadigan 2001; Chang 2005; Masuda 2005; Zimmerman 1988. | Total = 298 Music = 144 Control = 154 | I2 = 0% | SMD 0.15, 95% CI −0.08 to 0.37, P value = 0.21; No difference between groups. (Analysis 5.6) | None | N/A | N/A | |
| Oxygen saturation | N = 3 Chan 2006; Chang 2005; Koch 1998b. | Total = 150 Music = 73 Control = 77 | I2 = 79%; 1 significant study and 2 non‐significant studies. | MD −0.71% 95% CI −1.75 to 0.32, P value = 0.17; No difference between groups. (Analysis 5.7) | None | N/A | N/A | |
| Requirement for oxygen supplementation | N = 1 Schiemann 2002 | Total = 119 Music = 59 Control = 60 | N/A | OR 0.49, 95% CI 0.09 to 2.79, P value = 0.42; No difference between groups. | None | N/A | N/A | |
| Blood flow characteristics | N = 1 Masuda 2005 | Total = 44 Music = 22 Control = 22 | N/A | Blood flow: MD −2.40 ml/min/100g, 95% CI −7.45 to 2.65, P value = 0.35; Blood mass: MD 3.90 (relative value), 95% CI −4.67 to 12.47, P value = 0.37; Blood velocity: MD 0.29 KHz, 95% CI −0.11 to 0.69, P value = 0.15; No difference between groups. | None | N/A | N/A | |
| Bispectral index | N = 1 Yang 2003 | Total = 39 Music = 19 Control = 20 | N/A | MD 0.22 BIS value, 95% CI −0.76 to 1.20, P value = 0.66; No significant difference between groups. | None | N/A | N/A | It is unclear if this study meets the review inclusion criteria. Music group may have received intervention prior to coming to hospital. |
| Lung Function: (dyspnoea, tidal volume, minute ventilation, oxygen consumption, airway resistance). | None | N/A | N/A | N/A | N = 1 Nowobilski 2005 | Total = 36 Music = 18 Control = 18 | No significant differences. | |
| Stress hormones (Cortisol, Prolactin). | N = 1 McRee 2003 | Total = 26 Music = 13 Control = 13 | N/A | Cortisol: MD 7.29, 95% CI −7.37 to 21.95, P value = 0.33; Prolactin: MD −2.50, 95% CI −33.58 to 28.58, P value = 0.87; No difference between groups. | N = 1 Schneider 2001 | Total = 30 Music = 15 Control = 15 | Cortisol significantly increased in the control group and remained unchanged in the music group. Catecholamines were non‐significant. | |
| Mood | N = 2 Taylor‐Piliae 2002; Cadigan 2001. | Total = 170 Music = 80 Control = 90 | I2 = 0% | MD −1.18, 95% CI −2.17 to −0.19, P value = 0.02 in favour of music group. (Analysis 5.8) | None | N/A | N/A | |
| Anger | N = 1 Lembo 1998 | Total = 24 Music = 12 Control = 12 | N/A | MD −1.80, 95% CI −2.26 to −1.34, P value < 0.00001 in favour of music group. | None | N/A | N/A | |
| Depression | N = 1 Yang 2003 | Total = 39 Music = 19 Control = 20 | N/A | MD −3.29, 95% CI −4.99 to −1.59, P value = 0.0001 in favour of music group. | None | N/A | N/A | It is unclear if this study meets the review inclusion criteria. Music group may have received intervention prior to coming to hospital. |
| Fatigue | None | N/A | N/A | N/A | N= 1 Lembo 1998 | Total = 24 Music = 12 Control = 12 | No significant difference between groups. | |
| Uncertainty | N = 1 Taylor‐Piliae 2002 | Total = 30 Music = 15 Control = 15 | N/A | MD −3.53, 95% CI −12.15 to 5.09, P value = 0.42; No difference between groups. | None | N/A | N/A | |
| Satisfaction | N = 2 Lee 2002; Chlan 2000. | Total = 174 Music = 85 Control = 89 | I2 = 0% | MD 0.46, 95% CI 0.16 to 0.76, P value = 0.003 in favour of music (Analysis 5.9). | None | N/A | N/A | |
| Nausea | None | N/A | N/A | N/A | N = 1 Ezzone 1998 | Total = 33 Music = 16 Control = 17 | The paper reports that the music group had significantly less nausea and vomiting than the control group (Mann‐Whitney U test, P < 0.017). | |
| Length of stay | N = 2 Koch 1998a; Schiemann 2002. | Total = 153 Music = 78 Control = 75 | I2 = 0% | MD −6.00 minutes, 95% CI −10.72 to −1.28, P value = 0.01 in favour of music group (Analysis 5.10). | N = 1 Heitz 1992 | Total = 60 Music = 20 Standard care = 20 Headphones only = 20 | Findings were non‐significant. | |
| Intubation time | N = 1 Twiss 2006 | Total = 60 Music = 28 Control = 32 | N/A | MD −200.20 minutes, 95% CI −391.03 to −9.37, P value = 0.04 in favour of music group. | None | N/A | N/A |
CI: confidence interval; MD: mean difference; SMD: standardised mean difference
Findings from studies on music versus white noise:
Anxiety
One RCT reported sufficient data for extraction on anxiety (Zimmerman 1988). In this study of 50 participants (music group = 25, control group = 25), there was no strong evidence of an effect (MD 0.90 points on the state anxiety scale of the STAI, 95% CI −5.78 to 7.58, P value = 0.79).
Studies with insufficient data for extraction:
One other RCT (music group = 32, control group = 29) also investigated anxiety (Cruise 1997). This study also found no strong evidence of an effect.
Heart rate
Two RCTs reported sufficient data for extraction on the outcome heart rate (Broscious 1999; Zimmerman 1988; Analysis 6.1). When combined, these studies (music group = 89, control group = 55) with statistical homogeneity (I2 = 0%), show no strong evidence of an effect (MD 4.67 bpm, 95% CI −0.76 to 10.10, P value = 0.09).
6.1. Analysis.
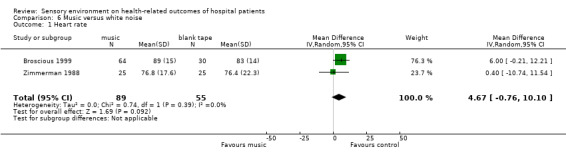
Comparison 6 Music versus white noise, Outcome 1 Heart rate.
Studies with insufficient data for extraction:
One other RCT (music group = 32, control group = 29) also investigated heart rate (Cruise 1997) and also found no strong evidence of an effect.
Blood pressure
Two RCTs reported sufficient data for extraction on the outcome blood pressure (Analysis 6.2), both of which reported systolic and diastolic blood pressure (music group = 89, control group = 55). These studies were homogenous for the outcome systolic blood pressure (I2 = 0%), finding no strong evidence of an effect (MD −1.80 mm Hg, 95% CI −8.59 to 5.00, P value = 0.60). Although the findings for diastolic blood pressure also showed no difference between groups, the two studies show considerable statistical heterogeneity (I2 = 78%).
6.2. Analysis.
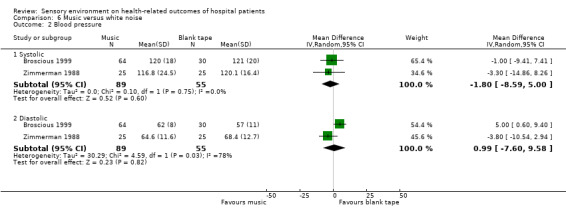
Comparison 6 Music versus white noise, Outcome 2 Blood pressure.
Studies with insufficient data for extraction:
One other RCT (music group = 32, control group = 29) also investigated blood pressure (Cruise 1997) and found no difference in both systolic and diastolic blood pressure between the music and white noise groups.
Respiration rate
Studies with insufficient data for extraction:
One RCT investigated respiration rate (Cruise 1997). This study (music group = 32, control group = 29) found no differences between groups.
Other outcomes
Other outcomes investigated were skin temperature (Zimmerman 1988; N = 50) and length of stay (Ayoub 2005; N = 62). For both these outcomes the findings showed no strong evidence of an effect.
Access to nature
Description of studies on providing access to nature:
There are no studies on provision of access to nature included in the review; We have tabulated five excluded studies (Table 14).
14. Access to nature: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| DeSchriver 1990 | Setting |
| Morsley 1999 | Commentary |
| Rice 1980 | Outcomes |
| Siegman‐Igra 1986 | Study design |
| Ulrich 1984 | Study design‐ retrospective matched pairs |
Reducing environmental stressors by implementing physical changes
Air quality
Description of studies on air quality:
We included one RCT (Lohner 1979) and two CCTs (Engelhart 2003; Whyte 1969) on hospital air quality (Table 15). Engelhart 2003 reports numbers in terms of patient bed‐days (not number of patients), and in this study there were 6000 bed‐days (1200 bed‐days in the intervention group and 4800 in the control group). In the remaining studies there were 1771 participants, 824 in the intervention groups, and 947 in the control groups. Based on the data of 1771 patients reported in two of the studies (Lohner 1979; Whyte 1969; and assuming that reported "average" age is the mean), patients were on average 38.2 years old (ranging from at least 13 to at least 74 years old). Gender is not reported in Engelhart 2003. In the remaining two studies there were 815 males and 956 females included. Studies were conducted in Germany, Belgium, and Scotland. Patient groups included those in haematology‐oncology units, those undergoing treatment for acute leukaemia or bone marrow aplasia, and post‐operative patients in a surgical unit (urological surgery/general surgery).
15. Air quality: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Engelhart 2003 | CCT; 2 parallel groups. | DESCRIPTION: In‐patients, predominantly with leukaemia, multiple myeloma, and malignant non‐Hodgkins lymphoma, admitted to the haematology‐oncology unit in Bonn, Germany. NUMBERS: Over one year there was 4800 bed days in the control group, and 1200 bed days in the air filtration group. GENDER: not described. AGE: not described. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | AIR FILTRATION: 3 rooms (single or double) were fitted with portable air filtration units (NSA model 7100A/B Environment Air System, National Safety Association Ltd., Memphis, USA). These units have a 95% filtering capacity for particles > 0.3 micrometers. They have two settings (high/low). Flow rate: High = 168, Low = 112 cubic m/hr. Noise: High = 57, Low = 55 dB(A). Patients were advised to keep windows closed as much as possible and run the unit on the high setting. CONTROL: Standard care, no air filtration units. All rooms were naturally ventilated with no HEPA filtration. They were on the 1st floor surrounded by forest. Patients instructed to keep windows closed during periods of neutropenia, wear masks when leaving the room, avoid showering, and use sterile water during other applications. Regular policies for aspergillus prevention included daily disinfection of horizontal surfaces, prohibiting potted plants and flower arrangements within the whole unit. | INVASIVE ASPERGILLOSIS: Counts of cases (confirmed and suspected) were achieved via ward liaison, targeted chart reviews, and consultation with medical staff. One confirmed case, and four suspected cases were recorded (5 per 4800 bed days). All were allocated to control areas. No cases were recorded in rooms with air filtration (0 per 1200 bed days). This difference was not significant (Fisher's Exact, P value = 0.33). AIR SAMPLING: not a patient outcome. | Compliance to the air filtration units was low; they were generally run on low due to the noise generated, and sometimes stopped during the night. |
| Lohner 1979 | RCT; 2 parallel groups. | DESCRIPTION: 45 inpatients undergoing treatment for acute leukaemia or bone marrow aplasia, in Belgium. NUMBERS: Isolation group = 24, Control group = 21. AGE, mean (range): Isolation group = 44.8 (17 to 72), Control group = 46.4 (13 to 74) years old. GENDER (male/female): Isolation group = 16/8, Control group = 14/7. ETHNICITY: not described. INCLUSION CRITERIA: During induction treatment of acute leukaemia or during bone marrow aplasia regardless of its origin. All were treated at the Institut Jules Bordet between May 1973 and April 1977. EXCLUSION CRITERIA: none described. | ISOLATION: Patients were isolated in a laminar air flow room. The isolation unit consisted of a normal bed enclosed in a plastic tent. The area available for the patient was about 5 sq metres. Air was pumped vertically through high‐efficiency filters positioned on the ceiling. All procedures on the patient were done through plastic gloves on the sides of the tent. All items entering the unit were either gas or steam sterilized, passing through locks irradiated by ultraviolet light. The tent was only opened when absolutely necessary. Any person approaching the isolated patients wore sterile boots, gloves, gown, and mask. Patients remained in isolation until either the bone marrow showed haematologic remission or myeloid proliferation and maturation. The study period ended when the patient was no longer in isolation. CONTROL: Patients were kept in single rooms during the entire hospitalisation period. Patients left the rooms only for special examinations, such as radiologic or isotopic investigations. All patients received oral non‐absorbable antibiotics, and sterile food and liquid. Unclear if cleaning protocols of patients were identical for both groups. | BACTERIAL INFECTIONS: Fungal cultures of stools were performed at least once a week. Data is reported as a count of the number of patients in which suppression of bacterial growth from stool cultures was achieved. Cultures were also obtained from the nose, gingiva, throat, ear, and axilla. Results report the number of days with infection (per 1000 days with severe neutropenia). MORTALITY: A count is provided of the number of fatal infections. REMISSION: A count is provided of the number of patients in complete and "partial" remission. Data extracted for complete remission. ADVERSE EVENTS: The paper reports on a number of people removed from isolation due to poor psychologic tolerance. | |
| Whyte 1969 | CCT; 2 parallel groups. | DESCRIPTION: 1726 in‐patients residing in the wards of a surgical unit (urological surgery/general surgery), in Scotland, UK. NUMBERS: Open plan wards = 926, Closed ward = 800. AGE, average: Open plan wards = 38, Closed ward = 38 years old. GENDER (male/female): Open plan wards = 417/509, Closed ward = 368/432. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | OPEN WARDS: Two wards (one male, one female) with natural ventilation (and no mechanical ventilation). The male ward had partitioned 4‐6 bedded bays, housing a total of 28 beds, and female ward was completely open plan with 29 beds. CLOSED WARD: One mixed gender ward divided into rooms (four 5‐bed male rooms, and five 4‐bed female rooms, plus 4 single rooms for either gender as required). This ward was air‐conditioned, with the air filtered, humidified, and heated or cooled. Temperature in the ward area was maintained at 20 degrees celsius and the relative humidity of 55%. Patient rooms had approximately 7‐8 air changes per hour. Two thirds of the ward air was re‐circulated through high‐efficiency filters. | STAPHYLOCOCCUS AUREUS (Staph. aureus): Nasal acquisition of Staph. aureus was monitored via swabs taken on admission, and then every Monday and Thursday thereafter. Data reported as the number of acquisitions, and the rate per 100 patient‐week. The number of tetracycline‐resistant strains of Staph. aureus and delayed acquisitions was also determined. WOUND SEPSIS: A wound was regarded as infected (1) when pus was visible to the naked eye, or (2) if a fluid exudate was present and pathogenic bacteria were isolated from it. |
Intervention groups included: isolation curtains with high‐efficiency particulate air (HEPA) filtration (Lohner 1979); single or double rooms with portable air filtration units (Engelhart 2003); and a closed ward with air conditioning, partially HEPA filtered (Whyte 1969). Comparison groups were with conventional airflow, which included mechanical and natural ventilation, and rooms of varying sizes.
Outcomes assessed were: invasive aspergillosis, mortality, remission, bacterial infections, and wound sepsis.
We have tabulated 31 excluded studies on air quality (Table 16).
16. Air quality: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Alberti 2001 | Study design |
| Azer 1971 | Setting |
| Baird 1969 | Outcomes |
| Bodey 1969 | Study design (no control) |
| Bodey 1971 | Study design (matched pairs) |
| Choctaw 1984 | Policy confound (sterile versus clean attire) |
| Chow 2005 | Study design (computer modelling) |
| Dekker 1994 | Confounding |
| Demling 1978 | Patients‐ mix of adults and children, data inseparable |
| Freireich 1975 | Preliminary report of Rodriguez 1978; policy confound |
| Friberg 1999 | Sham operations |
| Friberg 2003 | One patient health‐related outcome reported (surgical site infections), but not enough detail on how it was assessed or if it was noted on an 'ad hoc' basis. |
| Gundermann 1974 | Not patient outcomes |
| Lai 2001 | Study design |
| Legg 1970 | Not patient outcomes; test scenario |
| Lidwell 1969 | Not patient outcomes; test scenario |
| Lidwell 1975 | Study design |
| Lidwell 1982 | Some relevant subgroups within study however cannot separate data (number of re‐operations in each subgroup). Additionally, there are discrepancies in reporting with Lidwell 1984 with 185 patients switching subgroups. |
| Lidwell 1984 | Same study as Lidwell 1982. Non‐transparant reporting of findings‐ data not usable. Discrepancies between Lidwell 1982 and Lidwell 1984. |
| Lowbury 1971 | Population‐ age |
| Lowbury 1978 | Preliminary report of Lidwell 1982 and Lidwell 1984 |
| May 1984 | Study design |
| Passweg 1998 | Retrospective study; population (age) |
| Petersen 1987 | Policy (decontamination) changes |
| Qian 2006 | Mock setting |
| Rodriguez 1978 | Policy confounding |
| Schimpff 1975 | Policy confounding |
| Sherertz 1987 | Study design |
| Steingold 1963 | Study design |
| Whyte 1968 | Not patient outcomes |
| Yates 1973 | Policy confounding |
Below, we summarise findings for the following comparisons.
Air conditioned closed ward versus naturally ventilated open ward
Laminar airflow (High Efficiency Particulate Air filter) versus conventional airflow
Portable air filtration unit versus standard care
Risk of bias in included studies on air quality:
We included one RCT (Lohner 1979) and two CCTs (Engelhart 2003; Whyte 1969) on air quality. Method of sequence generation and allocation concealment was unclear in two studies (Engelhart 2003; Lohner 1979), and allocation was by day of the week in Whyte 1969. Blinding of group allocation was not done in any study, although it is unclear if outcome assessments were automated or blinded in Lohner 1979 and Whyte 1969. Completeness of outcome data is unclear throughout. No studies reported withdrawals and drop‐outs. Protection against contamination was adequate in all studies. The reliability of outcome measures (case counts of invasive aspergillosis) is unclear in Engelhart 2003.
Findings from studies on air quality. Air conditioned closed ward versus naturally ventilated open ward:
Infection
Whyte 1969 (air conditioned wards = 800, naturally ventilated open wards = 929) found no strong evidence of an effect for number of septic episodes, presence of resistant bacteria, and acquisitions of Staphylococcus aureus.
Findings from studies on air quality. Laminar airflow (High Efficiency Particulate Air filter) versus conventional airflow:
Infection
Studies with insufficient data for extraction:
Lohner 1979 reports that the number of infections and cases of septicaemia were not different between groups. Lohner 1979 reports that days of infection and treatment with antibiotics were significantly more frequent (P value < 0.05) in the conventional airflow group (however the table contradicts the text, and it is unclear how the counts were standardised as the number of study days varied between groups).
Mortality
Lohner 1979 reported mortality data (laminar airflow group = 7/24, conventional airflow group = 5/21), showing no strong evidence of an effect (risk ratio (RR) 1.23, 95% CI 0.46 to 3.29, P value = 0.69).
Remission
Lohner 1979 reported "complete remission" data (laminar airflow group = 5/24, conventional airflow group = 3/21), showing no strong evidence of an effect (RR 1.46 , 95% CI 0.40 to 5.38, P value = 0.57).
Adverse events
Lohner 1979 reported that 10 patients were removed from the laminar airflow room due to "poor psychologic tolerance of confinement after an average confinement period of 18.6 days (range 15 to 23 days)". One further patient with schizophrenia was removed after 59 days in the laminar airflow room.
Findings from studies on air quality. Portable air filtration unit versus standard care:
Infection
The overall incidence of invasive aspergillosis between groups in Engelhart 2003 showed no strong evidence of an effect (portable air filtration unit = zero infections per 1200 patient‐days, standard care five infections per 4800 patient‐days, P value = 0.33).
Bedroom type
Description of studies on bedroom types:
One CCT (Lidwell 1971) has been included (Table 17), which assesses different bedroom types (e.g. open versus closed rooms). Lidwell 1971 reported data in patient‐weeks (not number of patients), and 3327 patient‐weeks were assessed (open rooms = 2750 patient‐weeks, closed single rooms = 577 patient‐weeks). Participant age is described to an extent in Lidwell 1971 (57% of patients were under 60 years old, and 43% were over 60 years old), but no details are given on participant gender. The study was conducted in the UK on in‐patients in two medical wards.The open rooms were partitioned into four‐bed bays (six bays on each of two wards), each with three proper walls and a fourth low dividing wall opening on to the corridor. The closed rooms were single‐bed rooms (five rooms on each of two wards) based on the same two wards as the open rooms.The outcome 'acquisition of Staphylococcus aureus' was assessed. We have tabulated 42 excluded studies (Table 18) on bedroom type.
17. Bedroom type: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Lidwell 1971 | CCT; 2 parallel groups. | DESCRIPTION: 3327 patient‐weeks were analysed. Participants were in‐patients on one of two medical wards in the UK. NUMBERS: Open wards = 2750 patient‐weeks, Closed single rooms = 577 patient‐weeks. AGE: under 60 years = 57%, Over 60 years = 43%. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | OPEN WARD: Two identical wards each containing 6 four‐bed rooms, which opened up on to the corridor. The four‐bed rooms each had three proper walls with the fourth side being open to the corridor except for low dividing walls (3 ft.) on each side of the entrance. SINGLE‐BED ROOMS: The same two wards as above each had five single rooms, each proper rooms with four walls to divide them from the rest of the ward. There was no mechanical ventilation in these rooms. | PATIENT NASAL AQUISITION OF STAPHYLOCOCCUS AUREUS: A nasal swab was taken from patients as soon as possible after arriving on the ward (within 3 days). Subsequently a swab was taken from each patient on a set day of the week. STAFF NASAL AQUISITION: Not included in review. AIR CONTAMINATION: Not included in review. | Ratio of nasal carriage rates in single rooms to 4‐bed bays: All strains = 1:2 Tetracycline resistant strains = 1:4 Ratio of nasal acquisition rates in single rooms to 4‐bed bays: All strains = 1:1 Tetracycline resistant strains = 1:3 |
18. Bedroom type: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Armstrong 1984 | Review article |
| Burke 1977 | Participants (age) |
| Chaudhury 2003 | Cross‐sectional survey and qualitative interviews |
| Dekker 1994 | Confounding |
| Dolce 1985 | Retrospective study |
| Duckworth 1988 | Policy changes |
| Freireich 1975 | Preliminary report of Rodriguez 1978; policy confound |
| Gabor 2003 | Healthy participants received intervention |
| Hahn 1995 | Study design |
| Harmankaya 2002 | Study design |
| Hendrich 2004 | Study design |
| Herr 2003 | Study design, outcomes |
| Ittelson 1970 | Study design |
| Janssen 2000 | Outcome measure |
| Janssen 2001 | Participants |
| Kaldenberg 1999 | Study design |
| Kibbler 1998 | Study design; confounding |
| Kulik 1996 | Intervention |
| Leigh 1972 | Study design |
| Levine 1973 | Confounding |
| Lewis 1999 | Study 1: inappropriate control; Study 2: intervention |
| Lidwell 1966 | Study design |
| May 1984 | Study design |
| McConnell 2005 | Study design; unclear intervention |
| Miller 1998 | Participants; Study design |
| Morgan 1998 | Setting |
| Mulin 1997 | Study design |
| Nauseef 1981 | Policy changes |
| Parker 1965 | Patients‐ 38% <10 years old |
| Preston 1981 | Study design |
| Ribas‐Mundo 1981 | Intervention (non‐environmental changes) |
| Rodriguez 1978 | Policy confounding |
| Schimpff 1975 | Policy confounding |
| Shooter 1963 | Policy change |
| Silini 2002 | Study design |
| Thompson 2002 | Study design |
| Walsh 1989 | Policy changes |
| Wilkins 1988 | Study design |
| Williams 1962 | Study design |
| Williams 1969 | Study design‐ no control |
| Wood 1977 | Validity of outcomes |
| Yates 1973 | Policy confounding |
Risk of bias in included studies on bedroom types:
The one included CCT (Lidwell 1971) had unclear methods of sequence generation and allocation concealment was not done. Blinding of outcome assessors was unclear. Completeness of dataset was unclear. Withdrawals and drop‐outs were not described. There were insufficient data provided for extraction giving rise to a risk of reporting bias. It is unclear if there was protection against contamination.
Findings from studies on bedroom types:
Infection
Non‐randomised studies and studies with insufficient data for extraction:
Lidwell 1971 found that patients in single rooms (opening off the general ward area and not mechanically ventilated) acquired strains of Staphylococcus aureus from other patients at almost the same rate (23.9/1000 weeks) as patients in divided four‐bed bays (24.1/1000 weeks).
Ceilings
Description of studies on ceilings:
There are no studies on ceilings included in the review. We have tabulated two excluded studies (Table 19), which we excluded due to not meeting our study design and participant inclusion criteria.
19. Ceilings: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Berg 2001 | Participants (students) |
| Hagerman 2005 | Study design |
Flooring
Description of studies on flooring:
We included two RCTs, including one cross‐over trial of 58 patients, on flooring in hospitals (Table 20). These two studies included 112 elderly adults exposed to carpeted floor (N = 86) and vinyl floor (N = 84). The mean age of participants was 79.39 years old. The gender of participants in the cross‐over trial (Willmott 1986) is not described; however there were 10 males and 44 females in the other trial (Donald 2000). Both studies were conducted in England. One study was carried out in an elderly care rehabilitation ward (Donald 2000), and the other study states "elderly hospital in‐patients" (Willmott 1986).
20. Flooring: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes |
| Donald 2000 | RCT; 2 x 2 design (2 x flooring, 2 x therapy). | DESCRIPTION: 54 in‐patients in an elderly care rehabilitation ward, in England. NUMBERS: Linoleum floor = 26, Carpeted floor = 28. AGE, mean: Linoleum floor = 82.75, Carpeted floor = 83.20 GENDER (male/female): Linoleum floor = 8/18, Carpeted floor = 2/26. ETHNICITY: not described. INCLUSION CRITERIA: All patients admitted for rehabilitation. EXCLUSION CRITERIA: none described. | LINOLEUM FLOOR: Patient admitted to one of two four‐bed bays with latex vinyl square tile flooring. CARPETED FLOOR: Patient admitted to one of two four‐bed bays with hospital‐duty flotex (Flotex® 200). This carpet was chosen because it has no pile facilitating bacterial build‐up; it also reduces the movement of equipment satisfactorily when the brakes are applied, but still enables easy wheeling of beds, chairs and commodes. Patients were also allocated to either routine physiotherapy or additional exercises (stratified by flooring type). Outcomes relating to these groups are excluded from the review. | NUMBER OF FALLERS: obtained from the accident report forms. NUMBER OF FALLS: obtained from the accident report forms. INDEPENDENCE: obtained from the Barthel index. LENGTH OF STAY: not enough data for extraction, no difference reported between groups. |
| Willmott 1986 | RCT, cross‐over design, 2 conditions. | DESCRIPTION: 58 elderly hospital patients in England. NUMBERS: 58 patients (cross‐over) AGE: mean = 76.05 years old. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: not described. EXCLUSION CRITERIA: not described. | CARPETED CORRIDOR: Each patient walked along the corridor towards a staff member standing 15 m ahead. Chalk marks were drawn at an interval of 10 m. REFLECTIVE VINYL TILED CORRIDOR: Each patient walked along the corridor towards a staff member standing 15 m ahead. Chalk marks were drawn at an interval of 10 m. | GAIT SPEED and STEP LENGTH: The number of steps taken was counted from the time the patient crossed the first chalk line until the distal line was crossed by the leading forefoot, and elapsed time was measured by a stopwatch. Patient specific differences not reported. Study reports significant differences on both outcomes in favour of the carpeted floor. Gait speed (m/s): Carpet = 0.48 (0.19), Vinyl = 0.40 (0.17) Step length (cm): Carpet = 33.72 (12.01), Vinyl = 29.50 (12.32) |
Carpeted floors were heavy‐duty Flotex® 200, with no pile (Donald 2000) and in Willmott 1986 it was described as a carpeted corridor. Vinyl floors were latex vinyl square tiles in Donald 2000, and a reflective vinyl tiled corridor in Willmott 1986.
Outcomes assessed were: number of fallers, number of falls, independence, length of stay, gait speed, and step length.
We have tabulated seven excluded studies on flooring (Table 21), and one ongoing study (Characteristics of ongoing studies).
21. Flooring: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Anderson 1982 | Paediatric hospital |
| Buemi 1995 | Study design; outcomes |
| Cheek 1971 | Qualitative |
| Hewawasam 1996 | Study design |
| Hussian 1987 | Study design |
| Skoutelis 1993 | Study design |
| Thorne 1963 | Qualitative evaluation |
Risk of bias in included studies on flooring:
Included in the review was one parallel RCT (Donald 2000), with randomisation conducted via envelopes stratified by patient risk of falling (using a scale designed by the researcher), and one cross‐over RCT (Willmott 1986) with an unclear method of sequence generation. Donald 2000 was a factorial design including two types of physical therapy as well as the two flooring types. Concealment of allocation was unclear in both studies. Blinding of group allocation in both studies was not possible. Completeness of dataset was achieved in Donald 2000 for the outcomes of interest in this review, but it is unclear in Willmott 1986. Willmott 1986 does not describe any withdrawals and drop‐outs. Donald 2000 describes 22 withdrawals and drop‐outs by allocation group (Table 20), which were mostly (N = 13) due to non‐compliance with the therapy related outcome measures (not included in review), as well as death (N = 6), and patient transfer (N = 3). Both studies are at risk of selective outcome reporting bias. Neither study offered protection against contamination.
Findings from studies on flooring:
Number of fallers and falls
Donald 2000 found that the number of people who fell on carpeted floor (N = 7 of 28 people, fell altogether 10 times) was greater than on linoleum floor (N = 1 person of 26, fell once) but this showed no strong evidence of an effect.
Independence
Donald 2000 found no strong evidence of an effect between carpeted flooring (mean improvement = 1.1, SD 3.4) and linoleum flooring (mean improvement = 2.9, SD 3.3) groups in Barthel score (MD 1.80, reported P value = 0.08).
Length of stay
Studies with insufficient data for extraction:
Donald 2000 reported no strong evidence of an effect between linoleum flooring and carpeted flooring groups on length of stay.
Gait speed
Studies with insufficient data for extraction:
In a cross‐over trial of 58 patients, Willmott 1986 found that gait speed was significantly faster on carpet than vinyl (P value < 0.0005).
Step length
Studies with insufficient data for extraction:
In a cross‐over trial of 58 patients, Willmott 1986 found that step length was significantly greater on carpet than vinyl (P value < 0.0005).
Furniture and furnishings
Description of studies on furniture and furnishings:
One RCT has been included on hospital furniture (Table 22; Wilber 2005). This study was of 132 elderly out‐patients (66 assigned to a reclining chair, and 66 assigned to the standard gurney). Patients were 65 years or older (mean = 77.5 years old), including 55 males and 77 females. The study was conducted in the USA on patients admitted to an emergency department.
22. Furniture and furnishings: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Wilber 2005 | RCT; 2 parallel groups. | DESCRIPTION: 132 elderly out‐patients admitted to the emergency department, in Ohio, USA. NUMBERS: Chair group = 66, Gurney group = 66. AGE, mean (SD): Chair group = 77 (7.2), Gurney group = 78 (6.7) years old. GENDER (male/female): Chair group = 28/38, Gurney group = 27/39. ETHNICITY: not described. INCLUSION CRITERIA: Ambulatory outpatients; 65 years or older; able to sit upright, transfer, and engage in normal conversation. EXCLUSION CRITERIA: Refused participation; too ill to participate (as determined by the Emergency Department attending physician); unable to follow the instructions to remain in the chair or gurney and use the call light for any transfers (determined by the study nurse). | CHAIR GROUP: Remained on the gurney until initial physician and nursing evaluations complete. Patients were then assisted to a reclining chair. Patients were told "it is now time to move to the chair" and if they asked why, they were told they had the option of now moving to the chair. Patients were assisted to a position of comfort. Patients can sit on the reclining chairs with the hips and knees flexed. GURNEY GROUP: Remained on the gurney (the Emergency Department bed) throughout. The gurney has a thin foam mattress. Patients were assisted to a position of comfort. | PAIN: "The study nurse specifically instructed patients to rate pain associated with the gurney, rather than other sources." Measured on a NRS at three time points (time 0 = baseline; time 1 = one hour after randomisation; time 2 = two hours after randomisation). This outcome was dichotomised as favourable outcome (yes/no). A favourable outcome was considered as the patient having no pain at time 0 or time 1, or a decrease in pain from time 0 to time 1. An unfavourable outcome was defined as an increase in pain from time 0 to time 1, or no change in pain score if the patient complained of pain at time 0. SATISFACTION: Satisfaction with the gurney or chair was measured on a VAS at the time of discharge or after two hours (which ever came first). | SDs for satisfaction were estimated from the 95% confidence interval (1.4, 2.8), assuming 66 patients per group. Data extracted for pain at T1 for completeness of data. Results were slightly more pronounced at T2. |
The chair group were assisted to a reclining chair where they could sit with their hips and knees flexed. The gurney group remained on a gurney (the Emergency Department bed), which has a thin foam mattress. Both groups were assisted to a position of comfort.
Outcomes assessed were pain and satisfaction.
A Cochrane systematic review has already been conducted to include studies on beds, mattresses, overlays, and cushions (Cullum 2008), and their influence on the incidence and prevention of pressure sores. This review on support surfaces (Cullum 2008) includes the secondary outcomes of patient comfort, as well as costs, durability, reliability, and acceptability of the devices assessed. Fifty‐two randomised controlled trials are included in Cullum 2008, and these will not be re‐assessed here. A further three studies evaluating pressure‐relieving mattresses were identified by the present review, which either have not been assessed (Beldon 2002), or do not include the primary outcomes of Cullum 2008 (Grindley 1996; Pring 1998). These studies have been omitted from the present review, since it is felt that including them without duplicating the work of Cullum 2008, will provide an unrepresentative view of the literature.
In total, we have tabulated 19 excluded studies (Table 23).
23. Furniture and furnishings: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Baldwin 1985 | Outcomes and policy changes |
| Beldon 2002 | Other systematic review in this area (Cullum 2008) |
| Cooper 1998 | Other systematic review in this area (Cullum 2008) |
| Davies 1980 | Study design |
| Dubbs 2003 | Not a research study |
| Gray 2000 | Other systematic review in this area (Cullum 2008) |
| Grindley 1996 | Other systematic review in this area (Cullum 2008) |
| Hanger 1999 | Study design |
| Holahan 1972 | Test (not clinical) situation, policy change |
| Larsson 1991 | Study design |
| Mayer 1991 | Study design‐ inappropriate data |
| Nixon 2006 | Other systematic review in this area (Cullum 2008) |
| Okada 1986 | Not health‐related outcomes |
| Peterson 1977 | Outcomes (validity and relevance) |
| Pring 1998 | Other systematic review in this area (Cullum 2008) |
| Schott 1999 | Policy change |
| Sommer 1958 | Study design |
| Sherertz 1985 | Intervention |
| Williams 1962 | Policy changes with cleaning of blankets |
Risk of bias in included studies on furniture and furnishings:
We included one parallel RCT (Wilber 2005), with randomisation conducted via a random numbers table, and sealed numbered packets (adequate allocation concealment). Patients were not aware of the true nature of the study but blinding of healthcare professionals was not done. Outcomes were patient‐reported, and we have judged these to be assessed blindly. Completeness of outcome data was achieved at 'time 1' (one hour after randomisation), but not 'time 2' (two hours after randomisation). A description of withdrawals and drop‐outs is reported (N = 28), and these were all due to being discharged before outcomes could be assessed. It is unclear whether the study is at risk of selective outcome reporting. Protection against contamination was not done.
Findings from studies on furniture and furnishings:
Pain
Wilber 2005 found that significantly more people in the chair group (64/66) had a favourable pain outcome compared with those in the gurney group (50/66), (RR 0.78, 95% CI 0.68 to 0.90, P value = 0.0007).
Satisfaction
Wilber 2005 (chair group = 66, gurney group = 66) found that participants in the chair group were significantly more satisfied than those in the gurney (MD −2.10 points on a 10 point numerical rating scale, 95% CI −2.80 to −1.40, P value < 0.00001).
Hospital noise
Description of studies on hospital noise:
There are no studies on interventions for hospital noise reduction included in our review. Our search revealed 23 reports that investigated hospital noise, and possible interventions to reduce this. None of these reports have been included in the review (Table 24).
24. Hospital noise: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Aaron 1996 | No intervention‐ observational study |
| Baker 1987 | No intervention |
| Baker 1992 | No intervention |
| Baker 1993a | No intervention |
| Baker 1993b | Review article |
| Bame 1995 | Study design |
| Biley 1994 | Review article |
| Buemi 1995 | Study design; outcomes |
| Falk 1973 | No intervention |
| Gabor 2003 | No intervention in patients |
| Gast 1989 | Study design |
| Grumet 1994 | Discussion article |
| Haddock 1994 | Study design |
| Harrison 1989 | Study design |
| Haslam 1970 | Study design |
| Hilton 1976 | Study design |
| Hilton 1985 | No intervention |
| Kam 1994 | Review article |
| Lamont 1975 | No intervention |
| Lan‐Ping 2000 | Policy confound |
| Moore 1998 | Policy change |
| Pimentel‐Souza 1996 | Study design (cross‐sectional, no intervention) |
| Yinnon 1992 | Study design |
Lighting
Description of studies on lighting:
We included one CCT on hospital lighting conditions (Table 25; Walch 2005), resulting in a total sample of 89 patients (intervention group = 44, control group = 45). Mean age of the sample was 58.84 years old. There were 43 males and 46 females. The study was conducted in the USA on post‐operative patients.
25. Lighting: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Walch 2005 | CCT; 2 parallel groups. | DESCRIPTION: 89 post‐operative in‐patients recovering from elective cervical and lumbar spinal surgeries in single patient rooms, Pittsburgh, USA. NUMBERS: Bright room = 44, Dim room = 45. AGE, mean (SD): Bright room = 60.1 (13.7), Dim room = 57.6 (13.4) years old. GENDER (male/female): Bright room = 25/19, Dim room = 18/27. ETHNICITY (Caucasian/other): Bright room = 42/2, Dim room = 40/5. INCLUSION CRITERIA: undergoing elective cervical and lumbar spinal surgery. Admitted to single‐occupancy room. EXCLUSION CRITERIA: Discharge on day after surgery; history of major depression or use of antidepressant medications. | BRIGHT ROOM: On west side of the corridor. Received approximately 46% more natural sunlight than dim rooms (received on average 73,537 lux‐hours per day). DIM ROOM: On east side of the corridor. The light to these rooms was blocked due to an adjacent building approximately 25 meters away (received on average 50,410 lux‐hours per day). Rooms were of the same configuration and size. No attempt was made to control patient usage of window blinds and room lighting. | ANALGESIC CONSUMPTION: obtained via chart extraction and standardised to morphine equivalent mg/hr. PAIN: Recorded on post‐operative day one and on the day of discharge via McGill Pain Questionnaire. On discharge those in the bright rooms reported less pain although this was not significant (P value = 0.058). DEPRESSION: The Centre for Epidemiological Studies Depression Scale on first and last post‐operative day. There were no differences between groups. ANXIETY: Measured using the POMS anxiety scale on first and last post‐operative day. There were no differences between groups. STRESS: Measured using the Perceived Stress Scale on first and last post‐operative day. Patients in the bright rooms reported significantly less stress on day of discharge (P value = 0.035). | Analgesic consumption data extracted for entire LOS mg/hr. |
POMS: Profile of Mood States
The study investigated the effects of sunlight availability in the patients' rooms (as controlled by the aspect of the patients' rooms, e.g. east versus west facing). Rooms were classified as bright or dim and according to the report did not systematically differ in any other way.
Outcomes assessed were: analgesic consumption, pain, anxiety, stress, and depression.
We have tabulated 13 excluded studies on lighting (Table 26).
26. Lighting: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Beauchemin 1996 | Retrospective study |
| Beauchemin 1998a | Duplicate of Beauchemin 1998b |
| Beauchemin 1998b | Retrospective study |
| Benedetti 2001 | Retrospective study |
| Diffey 1988 | Study design |
| Fox 1986 | Study design |
| Harrison 1989 | Study design |
| Kolanowski 1990 | Setting |
| Rosenthal 1985 | Intervention |
| Satlin 1992 | Intervention |
| Sheperd 2001 | Study design |
| Van Someren 1997 | Setting; Study design |
| Veitch 2001 | Literature review |
Risk of bias in included studies on lighting:
One CCT (Walch 2005, where patients were allocated according to room availability) was included on lighting. Allocation concealment was not used. This study reports that healthcare professionals (assessing outcomes) were blinded to group allocation, and that patients were unaware of the study intervention, however, it is unclear how this was achieved, particularly when light readings were being taken in patient rooms. Completeness of outcome data was achieved on the day of surgery and the first and second post‐operative days, but not for the third to fifth post‐operative days (as patients were discharged). All patients included in the study were analysed on an intention‐to‐treat basis, and attrition was determined by length of stay in the ward. It is unclear if the study is at risk of selective outcome reporting. It is likely that patients were protected against contamination (as they stayed in single‐occupancy rooms) although no attempt was made to control patients' use of window blinds or overhead lighting, which may have affected their exposure.
Findings from studies on lighting:
Anxiety
Findings from non‐randomised studies:
Walch 2005 (N used in analysis: bright room = 29, dim room = 30) found no strong evidence for an effect for the outcome anxiety (MD 0.80 points on the Profile of Mood States (POMS) anxiety scale, 95% CI −0.56 to 2.16, P value = 0.25).
Pain
Findings from non‐randomised studies:
Walch 2005 (N used in analysis: bright room = 29, dim room = 30) found no strong evidence for an effect for the outcome pain (MD −1.30 points on the McGill Pain Questionnaire, 95% CI −2.58 to −0.02, reported P value = 0.058).
Pain medication requirement
Findings from non‐randomised studies:
Walch 2005 (bright room = 44, dim room = 45) found that patients in sunnier rooms consumed less analgesics (MD −0.90 mg/hr, 95% CI −1.80 to 0.00, reported P value = 0.047).
Other outcomes
Findings from non‐randomised studies:
Walch 2005 also reported on depression (MD 0.60 points on the Centre for Epidemiological Studies Depression Scale (CES‐D), 95% CI −1.95 to 3.15, P value = 0.64) showing no strong evidence for an effect, and perceived stress (MD −3.40 points on the Perceived Stress Scale (PSS), 95% CI −6.43 to −0.37, P value = 0.03), which favoured the patients residing in sunnier rooms.
Patient controls
Description of studies on patient controls:
There are no included studies on the provision of patient controls (no excluded studies have been tabulated). Some of the studies included for music interventions offered patients an element of choice over their 'music' environment, and we have explored this through subgroup analyses.
Technologies
Description of studies on technologies:
There are no studies on technologies included in the review. We have tabulated three excluded studies (Table 27) on alarm systems.
27. Technologies: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Gaffney 1986 | Setting; study design |
| Nelson Negley 1990 | Setting; outcomes |
| Tideiksaar 1993 | Intervention |
Temperature
Description of studies on temperature:
One CCT (Table 28; Frank 1992) investigated the use of ambient room temperature in 97 patients (63 patients had an operation in a warm operating room and 34 patients had an operation in a cold operating room). Participants were 64.5 (range = 35 to 94) years old, and gender is not described. The study was conducted in the USA on surgical in‐patients.
28. Temperature: Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes |
| Frank 1992 | CCT; 2 parallel groups. | DESCRIPTION: 97 surgical in‐patients undergoing lower extremity vascular reconstruction in an ORa in Maryland, USA. NUMBERS: Warm OR = 63, Cold OR = 34. AGE, mean (SD) [range]: 64.5 (1.1) [35 to 94] years old. GENDER: not described. ETHNICITY: not described. INCLUSION CRITERIA: Scheduled for lower extremity vascular reconstruction. EXCLUSION CRITERIA: not described. | WARM OR: Patient underwent operation in one of a group of ORs with the ambient room temperature maintained at 24.5 (0.4) degrees Celsius. COLD OR: Patient underwent operation in an OR with an ambient room temperature maintained at 21.3 (0.3) degrees Celsius. This room was maintained as such because it was also used for cardiac surgery with hypothermic cardiopulmonary bypass. All rooms had non‐recirculating airflow an no laminar flow system. Patients in each group were also randomised to receive general anaesthesia or epidural anaesthesia. | ORAL TEMPERATURE: Measured with an electronic digital thermometer, pre‐operatively (before being transported to the OR), immediately post‐operatively, on arrival at the ICU, and every hour for 24 hours. Intraoperative decrease in temperature: Warm OR (General Anaesthesia), [n = 30] = 1.0 (1.09) Warm OR (Epidural Anaesthesia) [n = 33] = 1.0 (1.15) Cold OR (General Anaesthesia) [n = 21] = 1.8 (0.92) Cold OR (Epidural Anaesthesia) [n = 13] = 0.8 (0.72) Ambient room temperature did not influence rewarming rate. |
aOR = Operating Room.
Intervention and control groups were: warm operating room of 24.5 ºc and cold operating room of 21.3 ºc.
Outcomes assessed were: re‐warming rate and oral temperature.
We have tabulated five excluded studies on temperature (Table 29).
29. Temperature: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Ansari 1969 | Study design |
| Hashiguchi 2005 | Study design |
| Morris 1970 | Study design |
| Plourde 1997 | Intervention‐ temperature of equipment not ambient room temperature |
| Wyon 1968 | Staff outcomes |
Risk of bias in included studies on temperature:
The included CCT (Frank 1992) used hospital scheduling rules and room availability to allocate patients to groups (allocation concealment not used), within these groups patients were also randomised to receive general or epidural anaesthesia. Oral temperature was measured with an electronic thermometer, but no blinding of group allocation was reported. Completeness of outcome data is reported for oral temperature (this is unclear for the outcome 'shivering'). However, the paper does not give a description of withdrawals and drop‐outs. It is unclear if the study is at risk of selective outcome reporting. Groups were protected against contamination.
Findings from studies on temperature:
Oral temperature
Findings from non‐randomised studies:
Frank 1992 found, that for patients undergoing operations with general anaesthesia, those assigned to warm operating rooms had less temperature loss than those assigned to colder rooms (MD −0.80 ºc, 95% CI −1.35 to −0.25, P value = 0.005). This difference was not apparent in patients undergoing operations with an epidural anaesthetic (MD 0.20 ºc, 95% CI −0.35 to 0.75, P value = 0.48).
Ward layout
Description of studies on ward layout:
There are no studies on ward layout included in the review; We have tabulated 10 excluded studies (Table 30).
30. Ward layout: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Baldwin 1985 | Not health‐related outcomes; policy changes |
| Barlas 2001 | Not health‐related outcomes; query validity |
| Elmståhl 1997 | Not a hospital setting |
| Good 1978 | Qualitative |
| Karro 2005 | Design; outcomes |
| Kim 1997 | Not health‐related outcome |
| Lomas 1987 | Outcomes |
| McKendrick 1976 | Study design |
| Pattison 1996 | Confounding staffing differences |
| Wilson 1983 | Qualitative; participants |
Wayfinding
Description of studies on wayfinding:
There are no studies on wayfinding interventions included in the review; We have tabulated eight excluded studies (Table 31).
31. Wayfinding: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Butler 1993 | Setting |
| Carpman 1983 | Study design |
| Dickinson 1995 | Setting |
| Mayer 1991 | Study design‐ inappropriate data |
| Passini 1998 | No intervention; comparison with healthy controls |
| Watanabe 1997 | Not health‐related outcomes; conversation confounding |
| Weisman 1981 | Setting |
| Wright 1993 | Participants not patients |
Windows
Description of studies on windows:
There are no included studies on the provision of windows included in the review. Three excluded studies have been tabulated (Table 32).
32. Windows: Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Keep 1980 | Study design |
| Verderber 1983 | Study design, validity of outcomes |
| Wilson 1972 | Study design‐ retrospective |
Multifaceted interventions
Whole unit design
Description of studies on whole unit design:
Two CCTs with multifaceted interventions have been included in the review (Table 33; Kasmar 1968; Vaaler 2005). In these two studies there were 171 psychiatric participants. Kasmar 1968 does not make clear how many participants were assigned to each group (details of 115 participants are unknown), however in Vaaler 2005 there were 31 participants in a refurbished wing, and 25 in the traditional wing. Participants in Kasmar 1968 were aged 16 to 66 years old, it is unclear how many participants were under 18 years old (34% were aged 16 to 22 years), or if indeed this study should be excluded in the review for this reason. Participants in Vaaler 2005 were on average 37.07 years old. Overall, there were 84 males and 87 females included in the studies, with one conducted in the USA (Kasmar 1968) and the other in Norway (Vaaler 2005). One study was conducted in an out‐patient psychiatric treatment room (Kasmar 1968) and one in an in‐patient seclusion area (Vaaler 2005).
33. Whole unit design (multifaceted): Characteristics of included studies.
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| Kasmar 1968 | CCT; 8 parallel groups (2 x rooms, 2 x psychiatrists, 2 x time of data collection). | DESCRIPTION: 115 applicants for out‐patient psychiatric treatment at the Neuropsychiatric Institute, Los Angeles, USA. NUMBERS: UNCLEAR how many patients per group. AGE: 16 to 66 years old, UNCLEAR if > 90% were 18 years old; 34% of patients were aged 16 to 22 years old. GENDER (male/female): 56/59. ETHNICITY: White = 115 (100%). INCLUSION CRITERIA: The patients had neither interacted or seen the psychiatrist previously. EXCLUSION CRITERIA: none described. | 'BEAUTIFUL ROOM': Carpeted in burnt‐yellow carpeting and contained an abstract picture on one wall, a floor‐sized artificial plant, a wooden waste‐basket, and indirect lighting provided by a contemporary desk lamp. The room was neat and well kept.'UGLY ROOM': Carpetless, with beige asphalt floor tiling, overhead fluorescent lighting and was unkempt, with work papers strewn over the furniture and an overflowing grey metal wastebasket and ashtray. Both rooms were windowless offices of identical size (6 x 8 x 8 feet), wall covering, and colour. The furniture was the same (brown metal desks with beige formica tops, green leatherette desk chairs, and green and yellow leatherette side chairs. The offices varied only in decor. | ROOM RATINGS: not included in review. PATIENT PERCEPTIONS OF PSYCHIATRIST: not included in review. MOOD RATINGS: Recorded via the "Psychiatric Outpatient Mood Scale" [This scale is known as Profile of Mood States, POMS]. No significant differences were found in the rated mood state for the main variables of room, psychiatrist, or patient age or gender.There was a significant interaction (P value < 0.05) of 'psychiatrist x age x sex' on factor 5 (fatigue‐inertia), which the authors evaluate as a chance finding. | Data not presented in enough detail for extraction. |
| Vaaler 2005 | CCT; 2 parallel groups. | DESCRIPTION: 56 psychiatric in‐patients in the seclusion area of an acute psychiatric ward in Norway. NUMBERS: Refurbished wing = 31, Traditional wing = 25. AGE, mean (SD): Refurbished wing = 37.7 (15.5), Traditional wing = 36.3 (16.5) years old. GENDER (male/female): Refurbished wing = 17/14, Traditional wing = 11/14. ETHNICITY: not described.INCLUSION CRITERIA: Admitted to the seclusion area of the ward. EXCLUSION CRITERIA: Contagious diseases; dementia; mental retardation; autism to an extensive degree; does not speak Norwegian or English. | REFURBISHED WING: Redecorated and refurbished with the aim of looking, as much as security permitted, like an ordinary Norwegian home: Wainscoting walls, colourful wallpaper and paintings, lowered ceilings, multiple lighting spots, tasteful curtains, wardrobes, chairs, flowers, personal items, Italian ceramic‐tiled bathroom. TRADITIONAL WING: Had been refurbished 4 years prior to the study with: sparse furniture, walls in grey colours, lacking pictures, no window curtains, single lamps in the ceilings 4 m high, bathroom with grey, laminated paint all over, and patient rooms with a single bed and a chair of metal tubes. Rooms were well kept and had a few signs of damage. | SYMPTOMS AND PSYCHOPATHOLOGY: Scored on the Positive And Negative Syndrome Scale (PANSS) for schizophrenia, with the time criterion of the last 24 hours. Scale has scores for total, positive, negative, and general symptoms. Assessed on admittance, day 3, and at discharge from seclusion. SYMPTOMS AND FUNCTION: Assessed on the Global Assessment of Function Scale‐ split version (GAF‐S). Assessed on admittance, day 3, and at discharge from seclusion. BEHAVIOUR: Assessed on the Brøset Violence Checklist (BVC). This is a 6‐item observer rated scale scoring behaviours that predict imminent violence in psychiatric inpatients. Violent or threatening incidents were recorded with Staff Observation Aggression Scale‐ Revised (SOAS‐R). Assessed on admittance, day 3, and at discharge from seclusion. LENGTH OF STAY. | Data extracted for change from baseline (beginning and end time‐points only).PANSS score for 'total' extracted for review. No significant difference was found on any of the subscales. |
Interventions were a 'beautiful room', neat and well‐kept, with burnt‐yellow carpeting, abstract picture, artificial plant, wooden waste‐basket, and indirect lighting provided by a contemporary desk lamp (Kasmar 1968), and a refurbished wing (Vaaler 2005), which was redecorated and refurbished to look like a Norwegian home, with wainscoting walls, colourful wallpaper and paintings, lowered ceilings, multiple lighting spots, "tasteful" curtains, wardrobes, chairs, flowers, personal items, and an Italian ceramic tiled bathroom. Control areas were an 'ugly room' (Kasmar 1968), which was carpetless, beige asphalt floor tiling, overhead fluorescent lighting, unkempt, with work papers strewn over the furniture and an overflowing grey metal wastebasket and ashtray, and a 'traditional wing' (Vaaler 2005), which at four years old was well kept with few signs of damage, had sparse furniture, grey walls, lacking pictures, no window curtains, single lamps in the 4 m‐high ceilings, bathrooms with grey, laminated paint, and patient rooms with a single bed and metal‐tubed chair.
Health‐related outcomes assessed by the studies were: mood ratings, psychiatric symptoms and psychopathology, function, violent behaviour, and length of stay.
We have tabulated 61 excluded studies (Table 34) on whole unit design.
34. Whole unit design (multifaceted): Characteristics of excluded studies.
| Study ID | Reason for exclusion |
| Alvermann 1979 | Descriptive article |
| Anthony Williams | Descriptive article |
| Bame 1993 | Study design |
| Barker 2005 | Descriptive article |
| Berlet 1979 | No intervention |
| Birdsong 1990 | No intervention |
| Christenfeld 1989 | CBA‐ Control sites and 'before' sites not clearly defined |
| Connell 1996 | Review article |
| Coulson 1997 | Setting |
| Counsell 2000 | Policy confound |
| Covinsky 1998 | Policy confound |
| Davidson 1971 | Study design |
| Dennis 1988 | Descriptive article |
| Devlin 1992 | Study design |
| Donchin 2002 | Review article |
| Dracup 1988 | Review article |
| Freeman 1987 | Study design |
| Greenberg 1992 | Descriptive article |
| Gurr 1997 | Descriptive case study |
| Hahn 1995 | Study design |
| Harvey 1998 | Review article |
| Harwood 1992 | Study design |
| Holahan 1973 | Outcomes |
| Holahan 1976 | Outcomes |
| Hyde 1989 | Qualitative; setting |
| Ingham 1997 | Setting |
| Jastremski 1998 | Literature review |
| Kovach 1997 | Setting |
| Laitinen 1994 | Intervention |
| Lawson 2000 | Study design (same study as Lawson 2003) |
| Lawson 2002 | Study design (same study as Lawson 2003) |
| Lawson 2003 | Study design (before‐and‐after no contemporaneous control) |
| Lawton 1970 | Study design |
| Leather 2003 | Study design (before‐and‐after no contemporaneous control) |
| Liebowitz 1979 | Study design |
| Martin 1998 | Policy confound |
| McLaughlin 1976 | Qualitative study |
| McGonagle 2002 | Study design |
| McNaughton 2005 | Study design |
| Meyer 1994 | No intervention |
| Middelboe 2001 | Confounding |
| Noskin 2001 | Literature review |
| Notelovitz 1978 | Study design |
| Oberle 1990 | Study design |
| Okamoto 2002 | Study design |
| Olsen 1984 | Outcomes; unclear study design |
| Palmer 1998 | Policy confound |
| Pattison 1996 | Confounding staffing differences |
| Rubin 1998 | Literature review |
| Rudy 1995 | Intervention (care delivery systems) |
| Shirani 1986 | Study design |
| Smith 1974 | Follow‐up study (Smylie 1971, Davidson 1971); study design |
| Smylie 1971 | Study design |
| Stahler 1984 | Study design (gender differences) |
| Swan 2003 | Study design |
| Tyerman 1980 | Unclear intervention/control |
| Vietri 2004 | Study design |
| Walker 1989 | Qualitative interviews |
| Weber 1996 | Overview article |
| Whitehead 1984 | Study design |
| Winkel 1986 | Descriptive case studies |
Risk of bias in included studies on whole unit design:
Two CCTs are included on whole unit design. In Kasmar 1968, participants were assigned to one of eight conditions (two x room types, two x psychiatrists, two x time of data collection). For the purposes of this review, this study has been classified as a CCT (non‐randomised) as although there was an element of randomisation (method not described), it appears that participants were not randomly allocated to room type, as this was dependent on the previous allocation. The paper states that psychiatrist and room type were matched. In Kasmar 1968, allocation concealment is unclear. Blinding of healthcare personnel and assessment of outcomes was not done (and not feasible), and it is unclear if there was completeness of dataset and there is no description of withdrawals and drop‐outs. This study is at risk of selective outcome reporting. Protection against contamination seems likely.
In Vaaler 2005, patients were admitted to the wing with fewest patients, or (if there were even numbers of patients on each wing) to the wing which did not receive the last patient. Allocation concealment was not used. No blinding was possible in this study. It is unclear whether data was obtained for > 80% of participants. In Vaaler 2005, participants were not asked for consent due to their condition and all admitted patients were included apart from one with senile dementia. It is unclear if there were any withdrawals or drop‐outs. It is unclear if this study is at risk of selective outcome reporting. It is unclear if patients were retained to their wing, or if there was possible contamination.
Findings from studies on whole unit design:
Mood Ratings
Studies with insufficient data for extraction:
Kasmar 1968 found no strong evidence of an effect on mood between groups exposed to a 'beautiful room' or an 'ugly room'.
Psychiatric symptoms
Findings from non‐randomised controlled trials:
Vaaler 2005 found no strong evidence of an effect between a refurbished wing group and a traditional wing group in psychiatric symptoms (MD −7.60 points on the Positive And Negaitve Syndrome Scale (PANSS), 95% CI −16.81 to 1.61, P value = 0.11).
Symptoms and function
Findings from non‐randomised controlled trials:
Vaaler 2005 found no strong evidence of an effect between a refurbished wing group and a traditional wing group in function (MD −1.00 points, 95% CI −5.75 to 3.75, P value = 0.68) or symptoms (MD −2.00 points, 95% CI −8.69 to 4.69, P value = 0.56), as measured by the Global Assessment of Function Scale ‐split version (GAF‐S).
Violence
Findings from non‐randomised controlled trials:
Vaaler 2005 found no strong evidence of an effect between a refurbished wing group and a traditional wing group in violence (MD −0.04 points on the Brøset Violence Checklist, 95% CI −0.69 to 0.61, P value = 0.90).
Length of stay
Findings from non‐randomised controlled trials:
Vaaler 2005 found no strong evidence of an effect for length of stay between a refurbished wing group and a traditional wing group (MD −1.80 days, 95% CI −6.18 to 2.58, P value = 0.42).
Discussion
Summary of main results
Providing positive distracters
We found studies for a number of interventions which could be used as positive distractions in hospital environments. These interventions included: music, audiovisual distractions, visual distractions, decoration, and aromas. Studies reported on a variety of health‐related outcomes, and here we will focus on patient‐reported anxiety and pain, anxiolytic and pain medication requirements, blood pressure, heart rate, and respiration rate. In general, the findings support the use of music for reduction of patient‐reported anxiety, particularly in the pre‐procedure period which was favourable compared with both standard care and blank headphones. For use during medical procedures, music was preferable to standard care but there was no strong evidence of an effect when music was compared with a blank tape with headphones (note, we have not statistically assessed the difference between the comparison of 'music versus standard care' and 'music versus blank tape with headphones'). This may imply that it is the reduction of unpleasant noise, rather than the addition of music, which accounts for significant findings when music is compared with standard care, or that the studies using standard care as a control group were at higher risk of bias (as healthcare personnel were not blinded to study groups). Alternatively, the attention associated with providing patients with a blank tape and headphones may explain why this is just as effective as providing music. Some studies reported on anxiolytic medication requirements, but these findings did not always parallel the findings for patient‐reported anxiety. For physiological measures (heart rate, blood pressure, and respiration rate), findings are less positive. On these outcomes mixed results are obtained when comparing music with standard care. However, as with some of the findings for anxiety, when comparing music to blank tape (or headphones), studies tend to show no strong evidence of an effect. Only one study (comparing music with pre‐recorded operating room noise) found music to increase systolic blood pressure, and all other outcomes reported by all studies, if not positively in favour of music, demonstrated that the addition of music did not do any harm. Evidence on music for pain relief is reported in Cepeda 2006.
It is unclear whether patients should be provided with a choice of music or provided with set pieces. For some outcomes and comparisons, set pieces seem preferable, whereas for others a choice of music appears preferable. This may reflect that it is not 'having a choice' which is most important but rather the 'content' of the music that makes the difference. The geographical location of studies does not appear to influence the heterogeneity of the findings so it appears that patients may react similarly to music interventions regardless of location. In this review, we have not explored the relationship between musical content and country of study, or how the content of music relates to the study findings.
There were fewer studies that investigated the use of audiovisual distractions. Three audiovisual studies had mixed results (showing positive findings and no difference) for anxiety compared with standard care. A number of explanations may explain these differences, including the type of audiovisual distraction (the dynamic distractions were positive and the static distraction showed no strong evidence of an effect). The studies on audiovisual distraction for patient‐reported pain were all positively in favour of audiovisual distraction (compared with standard care) but to different degrees. One study reporting on sedation medication requirements had results in the same positive direction as the patient‐reported pain findings. Two studies had heterogeneous findings for audiovisual distraction versus audio distraction for pain. Audiovisual distraction was no better than audio alone for anxiety, heart rate, and blood pressure.
One study compared audiovisual distraction with visual distraction alone on the outcomes pain and pain medications, and found audiovisual distraction to be preferable. One study found that audiovisual distraction was no better than scheduled rest for anxiety, pain, blood pressure and heart rate. The one study included on decoration had small study groups and found no difference between groups on anxiety, pain medication and length of stay. One study on aromas reported a positive effect for anxiety, whilst another found improvements in agitation levels. One study found no strong evidence of aroma effects for depression, fatigue, and general health.
On the whole, it appears that some positive distractions in hospital may prove worthwhile for improving patient‐reported outcomes such as pain and anxiety, however, the benefit of these interventions for physiological outcomes (heart rate, blood pressure, and respiration rate) has less support. It is also unclear if the benefits that positive distractions may have for patient‐reported outcomes translate directly in to reduced medication usage.
Reducing environmental stressors by implementing physical changes
Included in the review are studies that looked at lighting, air quality, temperature, bedroom types, flooring, and furniture; each reporting on a range of relevant outcomes.
Patient rooms facing directions which allow more sunlight in were found to be no different than darker rooms for reducing anxiety and pain (one study reporting on each). However, pain medication requirement was found to be less in sunnier rooms (findings from one study), as was perceived stress.
There was no strong evidence of an effect of air quality, as controlled by various air conditioning systems, on various measures of infection (number of infections, cases of septicaemia, incidence of invasive aspergillosis, number of septic episodes, presence of resistant bacteria, and acquisitions of Staphylococcus aureus), mortality, or remission. Additionally one study reported that there were cases of poor psychologic tolerance of confinement in a laminar air flow room. One study on temperature of operating theatres found that warmer rooms were beneficial for patients under general anaesthesia but made no difference to those with epidural anaesthesia in terms of temperature loss.
One study included on single‐ and multi‐bed rooms found no difference between room types on infection rates. Two studies were included on flooring and each investigated different outcomes. One study found no difference between carpet and linoleum for number of falls and fallers, independence, and length of stay. However, elderly people had a faster gait and longer stride on carpeted floor compared to vinyl. One study included on furniture, found reclining chairs to produce less patient‐reported pain and more satisfaction than hospital gurneys.
These studies represent a diverse range of physical modifications that could be made to hospital environments. There are few studies included for each intervention, and many of the studies included are at unclear or high risk of bias. Some environmental interventions appear to have positive effects, whilst others provide no strong evidence of an effect and may even indicate harmful effects.
Multifaced interventions
Two studies conducted on psychiatric populations found no differences between environments. This finding is important as it suggests that providing sparsely decorated and furnished rooms for psychiatric populations is not necessary for the control of psychiatric symptoms, and providing a pleasant environment at least does not do any harm.
Overall completeness and applicability of evidence
The majority of studies included in this review explored the use of music. Few studies were found to meet the inclusion criteria for other forms of environmental intervention. The inclusion criteria were broad, making the review applicable to all types of adult patients attending hospital for any reason. The downside to this inclusiveness means that much heterogeneity exists between the studies, so interpretation and application of the findings requires that attention is paid to the specific scenarios in which the included studies were conducted. There were a number of environmental interventions which were searched for but no studies meeting the methodological criteria were found. This means there are gaps in the evidence for interventions on: art, nature, ceilings, windows, and layout. It is sometimes argued that it is too logistically complex to conduct studies with good methodological designs on environmental interventions, however, this review has demonstrated that it is possible (as some studies have been included), however, for some interventions these types of studies have yet to take place.
To assist with the manageability of the review process, the inclusion criteria for this review was limited to the hospital setting; other evidence exists pertaining to, for example, dentists, nursing and care home environments, which has not been systematically assessed by this review. Furthermore, it is possible that the hospital environment may also impact on staff, having more indirect effects on patient care and outcomes; this evidence is currently lacking however, as summarised in another Cochrane systematic review focusing on the effects of the healthcare environment on staff outcomes (Tanja‐Dijkstra 2011).
Studies included in this review have a wide geographical spread, covering Australasia, North America, Asia, and Europe. There are no studies included from Africa or South America, and the transferability of the findings of this review to low‐to‐middle‐income countries is unknown. Heterogeneity between included studies was not easily explained by geographical location implying that this factor may not be so important (i.e. the findings are transferable across the locations assessed).
We have not undertaken to formally include economic evaluations as part of this review. For the majority of interventions pertaining to the sensory hospital environment, the evidence‐base for effectiveness is limited due to lack of studies and poorly rated studies, this should not be confused however with evidence of no effect; it may be cost‐effective to implement changes to the sensory environment, however this is not known and more robust evidence of effectiveness is required.
Quality of the evidence
The quality of the evidence is quite varied. Much of the evidence was rated poorly due to a lack of clarity in the reporting as opposed to definitively being at high risk of bias (although this could have also been the case). A number of non‐randomised controlled trials were found, and we did not summarise these for music interventions since there were many randomised trials conducted in this area. However, we have reported on non‐randomised controlled trials for other interventions where the body of evidence is much smaller. Whereas sometimes the approach of not randomly allocating patients to groups is understandable for logistical reasons (e.g. when patient allocation is dictated by hospital room availability); in other cases there is no real valid reason why randomisation could not have been used (instead of for example, alternate days).
Potential biases in the review process
Searching for studies in this area has proved particularly problematic, which is partially due to fact that many words associated with environmental interventions are used in other contexts with different meanings (for example, "art", "floor", "ventilation"), resulting in searches with very low specificity. It is hoped that, most importantly, the sensitivity of the search has been maximised through the wide range of sources searched, however, there is no way to guarantee the capture of all relevant studies. The review does now require updating and 69 studies are listed in Studies awaiting classification from an updated search. It is possible that once further relevant studies have been incorporated into the review findings, that the conclusions may change. All stages of selecting, appraising, and collecting data from studies in this review have been conducted independently by at least two people, in order to minimise bias and improve the robustness of decisions. The protocol for this review was written prior to the release of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008), and we have tried to align the review with the updated guidance, which has involved deviating somewhat from the original protocol (See: Differences between protocol and review).
This review set out with a very broad question; in particular, including all "health‐related outcomes" may be seen as problematic as with multiple analyses there is higher potential for an analysis to be significant by chance alone. This issue, which is a problem related to random error as opposed to bias, is further manifested amongst individual studies, some of which contain multiple tests and many outcomes. We have handled this issue by reporting up to five relevant outcomes for each comparison and grouping the remaining reported outcomes for that intervention under a heading "other outcomes"; where only a minority of studies have reported an outcome, this is also highlighted in the text, so users of this review should be particularly wary of chance findings in these circumstances.
Agreements and disagreements with other studies or reviews
There have been a series of other reviews conducted in this area, although the foci of these reviews are not directly comparable to the inclusion and exclusion criteria of this current review. A number of reviews have been published (including in the grey literature) covering a broad range of environmental interventions (Dijkstra 2010; Ulrich 2004a and Ulrich 2008; Van den Berg 2005).
Ulrich 2004a conducted a review on "the role of the physical environment in the hospital" on patient (of all ages) and staff outcomes, which was later revised and updated (Ulrich 2008). The updated narrative review places more emphasis on the quality of studies than the original, however, the criteria against which studies were assessed is not clear ("each study was evaluated in terms of its research design and methods and whether the journal was peer‐reviewed"). The findings additionally draw on a range of evidence (excluding non‐English language studies), including qualitative studies, surveys, other literature reviews, and observational studies, and including indirect evidence (e.g. surface and air contamination levels as a proxy for hospital‐acquired infections which in turn is linked to reduced length of stay, and studies conducted in non‐hospital settings), and multifaceted interventions which have an element of environmental modification.
A series of interventions are advocated in Ulrich 2008, which are not supported by the present review either through lack of evidence or interpretation of the findings. These include the following.
Access to nature (e.g. large windows, art, and technological audio‐visual distractions) for pain, stress (but with limited evidence on nature art), length of stay, and satisfaction. Some of the studies reported to favour nature in Ulrich 2008 were included under audiovisual distractions in the present review (as the studies assessed pictures and sounds rather than real‐life nature and the findings do not support the use of nature per se due to the choice of comparison groups).
Daylight for pain (with limited evidence) and depression (drawing on a number of studies which utilised bright light treatment for depression, which were not included in the present review), and length of stay. The non‐significant findings (Walch 2005: pain and anxiety) highlighted in the present review are over‐interpreted by Ulrich 2008 as favouring sunnier rooms.
Single‐occupancy rooms for infection rates, reduction of stress, and improvement of sleep.
Rooms with better air quality, easy‐to‐clean surfaces, alcohol‐based hand‐rub dispensers in accessible locations, and carefully maintained water systems for reduction of infection rates.
Limited indirect evidence around the influence of noise, lighting, and acuity‐adaptable single patient rooms on medical errors.
Sound‐absorbing ceiling tiles and eliminating or reducing noise sources (e.g. adopting a noiseless paging system) for sleep.
In line with the current review, Ulrich 2008 found no conclusive evidence linking environmental interventions with reduced falls, and states there is little research assessing wayfinding systems on healthcare outcomes. Ulrich 2008 also assessed outcomes related to speech privacy and confidentiality, communication and social support for patients and family, and staff‐related outcomes, which were not covered in the present review. On the whole, compared to the present review, Ulrich 2008 is a more inclusive review, with the resulting conclusions reporting more confidently on the positive impact that hospital environments may have on patient outcomes. The present review has more stringent inclusion criteria and assessment of risk of bias and as such does not draw the same degree of positive conclusions.
Van den Berg 2005 reviewed studies on nature, daylight, fresh air, and quiet in healthcare settings. Van den Berg 2005 included a range of healthcare settings (including non‐clinical settings), age groups, and staff and patient health outcomes. Van den Berg 2005 took a more systematic approach than Ulrich 2004a by setting out the inclusion and exclusion criteria, and relating the findings to a methodological critique and relevance. Like the present review, Van den Berg 2005 concludes that there is insufficient evidence to support the use of hospital gardens for improved clinical outcomes. Van den Berg 2005 concludes that there is sufficient evidence that viewing nature can reduce stress and pain and that there is solid evidence that ventilation of fresh air is associated with improved health (these conclusions are not fully supported by the present review). Van den Berg 2005 reports that there is weak evidence to support the use of indoor plants (the present review included no studies of this nature) and that there is weak and inconclusive evidence for the health benefits of daylight (concurring with the present review findings). Van den Berg 2005 concludes that there is some evidence to support the promotion of quiet in healthcare settings, and this is supported in part by the present review, the findings of which suggest that the provision of music may reduce the impact of stressful noise.
Dijkstra 2006 also reviewed the evidence in this area. The inclusion/exclusion criteria of Dijkstra 2006 differ from the current review although there is some overlap in the studies included in each. Dijkstra 2006 only includes two studies on music and one on ocean sounds, but also includes studies that did not meet the methodological inclusion criteria of the present review. Dijkstra 2006 included more studies on multifaceted interventions, which did not meet the criteria of the present review; from these studies Dijkstra 2006 concludes that there is support for the notion that the environment impacts upon patient well‐being. With regard to single environmental interventions, the need for further research is suggested. Dijkstra 2006 did not incorporate any meta‐analyses, and included evidence on televisions, seating arrangements, and layout which did not meet the criteria for the present review. Despite these differences, in very broad terms, the overall conclusions (that there is a general lack of high quality evidence for many environmental interventions) are similar.
Authors' conclusions
Implications for practice.
The studies included in this review demonstrate that the addition of selected music to the hospital setting, at least does no harm, and may have a beneficial effect in certain circumstances (possibly by way of reducing unpleasant noise), particularly for patient‐reported outcomes such as anxiety. There is less evidence to support or refute other environmental changes for patient‐related health outcomes. Although the evidence generally supports the premise that environmental interventions do not do any harm (but see conclusions on air quality studies), this does not imply that the benefits of implementing environmental interventions will outweigh the costs.
Implications for research.
There are already many studies reporting on the effects of listening to music in hospital; Further exploration could be made into the impact of music genre, tempo, volume, personal choice, cultural and sociological influences, and underlying mechanisms, to further explore some of the heterogeneity of effects summarised in this review.
It is sometimes argued that it is too logistically complex to conduct studies with good methodological designs on environmental interventions. This review has demonstrated that it is possible to conduct research with good methodological designs (as some studies have been included) however for many environmental interventions these types of studies have yet to take place. The scale of interventions clearly influences the logistical complexity of conducting studies in this field, and the time it takes to organise and run such research; for example, it is easier to allocate patients to receive a music intervention than it is to administer a more permanent environmental structure (such as windows, floors, and ward layout) as an intervention in a research study. However, ongoing research is exploring the feasibility of researching large‐scale environmental interventions (e.g. flooring) using a more rigorous research design (NCT00817869). Future research efforts in the field should focus on improved methodological design to reduce the risk of bias, and improved reporting. Assessing the effectiveness of environmental interventions is important in order that resources are focused appropriately, and that patients are provided with the best opportunity to be well.
Feedback
Comment from Kass, 20 August 2014
Summary
I have composed music designed for mental health with improvement in concentration and emotional well being for those under stress, employment , businesses, hospitals and doctors offices. Anecdotally there has been uniform success. I invite you to cdbaby.com, A Voice From heaven. We are looking for joint projects to use the music in a setting for better outcomes
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
Reply
Thank you for your comment and interest in our review. You may have noted that our review includes many (85) studies assessing the effects of music. As well, there are approximately 40 systematic reviews related to the effects music and music therapy in the Cochrane Database of Systematic Reviews – those co‐authored by Joke Bradt may particularly interest you. With this in mind, researchers of future studies in the area need to carefully consider what they will add to the evidence base. Our review’s section ‘Implications for research’ suggests some avenues of research in the field. In addition, any future research should aim to minimise bias (i.e. by addressing the risk of bias criteria used in Cochrane Reviews), and especially, to consider which outcomes to include. Since many music studies include a plethora of outcomes (and risk reporting only the significant ones), we would like to see studies specify in advance the outcomes they plan to measure, and report on all of these, regardless of the direction of the results. Understandably, the outcomes of choice may differ depending on the population studied, but we would advise future research to consider both patient‐reported and physiologically measured outcomes; the current evidence seems to suggest that though music may improve patient‐reported outcomes, this may not translate into measurable physiological effects. As in all research, transparency and conduct of the highest standard matters most, regardless of affiliation or any vested interest in the results. We wish you well in your partner search and hope you find a suitable opportunity to empirically assess the effectiveness of your music.
Contributors
Feedback (comment) from:
Fred Kass, JD, BA, Fred Kass Law, VP and musical director MartinKassMedia
Response to feedback (comment) from:
Amy Drahota, Derek Ward and Andrew Herxheimer
What's new
| Date | Event | Description |
|---|---|---|
| 13 November 2014 | Feedback has been incorporated | Minor amendment |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 3, 2012
| Date | Event | Description |
|---|---|---|
| 20 October 2008 | Amended | Converted to new review format. |
| 30 November 2004 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Protocol and review support: Sasha Shepperd, Alain Mayhew, Laura McAuley, Phil Alderson, Andy Oxman, Jeremy Grimshaw.
Elizabeth Galloway contributed to writing the protocol, screening citations, abstracts, and full reports. Faridah Nanfuka contributed to the extraction of data for the 'Risk of bias' tool, the updated search, and screening citations.
Search strategy support: Roisin Gwyer (subject specialist librarian), Ian Mayfield (subject specialist librarian), Andy Barrow (subject specialist librarian), Janet Wilmot (inter‐library loans), Jessie McGowan (Trials Search Co‐ordinator), Michelle Fiander (Trials Search Co‐ordinator).
Foreign language support: Diane Gal (Portuguese); Lucy Birchwood (French); Sabine Quandte and Monja Knoll (German); Janine Givati‐Teerling and Aldert Vrij (Dutch); Katarzyna Zinken (Polish); Lyuda Wade (Russian); John Wong (Chinese); Endre Kadar (Hungarian); Tomoko Yamashita (Japanese).
Financial Support: The Dunhill Medical Trust (Registered research charity) provided the salary of AD for a separately funded project of which this review formed part.
Appendices
Appendix 1. MEDLINE search strategy
#1. explode "Psychophysiology‐" / all SUBHEADINGS in MIME,MJME,PT #2. #1 not reaction time #3. explode "Hospitalization‐" / all SUBHEADINGS in MIME,MJME,PT #4. explode "Hemodynamic‐Phenomena" / all SUBHEADINGS in MIME,MJME,PT #5. explode "Analgesics‐" / all SUBHEADINGS in MIME,MJME,PT #6. explode "Pain‐" / all SUBHEADINGS in MIME,MJME,PT #7. "Patient‐Satisfaction" / all SUBHEADINGS in MIME,MJME,PT #8. explode "Emotions‐" / all SUBHEADINGS in MIME,MJME,PT #9. explode "Aggression‐" / all SUBHEADINGS in MIME,MJME,PT #10. "Sleep‐Deprivation" / all SUBHEADINGS in MIME,MJME,PT #11. ( (anxiety) in AB )or( (anxiety) in TI ) #12. ( (stress) in AB )or( (stress) in TI ) #13. ( (heart rate) in AB )or( (heart rate) in TI ) #14. ( (blood pressure) in AB )or( (blood pressure) in TI ) #15. ( (pain) in AB )or( (pain) in TI ) #16. ( (cortisol) in AB )or( (cortisol) in TI ) #17. ( (physiological) in AB )or( (physiological) in TI ) #18. ( (analgesi*) in AB )or( (analgesi*) in TI ) #19. ( (anaesthe*) in AB )or( (anaesthe*) in TI ) #20. ( (length near stay) in AB )or( (length near stay) in TI ) #21. ( (recovery near time) in AB )or( (recovery near time) in TI ) #22. ( (days near recovery) in AB )or( (days near recovery) in TI ) #23. ( (hospital acquired infection?) in AB )or( (hospital acquired infection?) in TI ) #24. ( (hospital associated infection?) in AB )or( (hospital associated infection?) in TI ) #25. OR/#2‐#24 #26. explode "Art‐" / all SUBHEADINGS in MIME,MJME,PT #27. explode "Color‐" / all SUBHEADINGS in MIME,MJME,PT #28. "Acoustic‐Stimulation" / all SUBHEADINGS in MIME,MJME,PT #29. "Color‐Therapy" / all SUBHEADINGS in MIME,MJME,PT #30. "Music‐Therapy" / all SUBHEADINGS in MIME,MJME,PT #31. "Aromatherapy‐" / all SUBHEADINGS in MIME,MJME,PT #32. ( (television) in AB )or( (television) in TI ) #33. "Music‐" / all SUBHEADINGS in MIME,MJME,PT #34. ( (distraction) in AB )or( (distraction) in TI ) #35. OR/#26‐#34 #36. #35 NOT massage #37. explode "Architecture‐" / all SUBHEADINGS in MIME,MJME,PT #38. ( (healing design?) in AB )or( (healing design?) in TI ) #39. ( (therapeutic design?) in AB )or( (therapeutic design?) in TI ) #40. ( (restorative design?) in AB )or( (restorative design?) in TI ) #41. ( (healing environment?) in AB )or( (healing environment?) in TI ) #42. ( (therapeutic environment?) in AB )or( (therapeutic environment?) in TI ) #43. ( (restorative environment?) in AB )or( (restorative environment?) in TI ) #44. "Environment‐Design" / all SUBHEADINGS in MIME,MJME,PT #45. explode "Facility‐Design‐and‐Construction" / all SUBHEADINGS in MIME,MJME,PT #46. explode "Health‐Facility‐Environment" / all SUBHEADINGS in MIME,MJME,PT #47. "Air‐Conditioning" / all SUBHEADINGS in MIME,MJME,PT #48. "Temperature‐" / WITHOUT SUBHEADINGS in MIME,MJME,PT #49. "Lighting‐" / all SUBHEADINGS in MIME,MJME,PT #50. "Heating‐" / all SUBHEADINGS in MIME,MJME,PT #51. "Humidity‐" / all SUBHEADINGS in MIME,MJME,PT #52. "Ventilation‐" / all SUBHEADINGS in MIME,MJME,PT #53. ( (natural light*) in AB )or( (natural light*) in TI ) #54. ( (fluorescent light*) in AB )or( (fluorescent light*) in TI ) #55. ( (temperature near room) in AB )or( (temperature near room) in TI ) #56. explode "Sound‐" / all SUBHEADINGS in MIME,MJME,PT #57. "Socioenvironmental‐Therapy" / all SUBHEADINGS in MIME,MJME,PT #58. "Milieu‐Therapy" / all SUBHEADINGS in MIME,MJME,PT #59. OR/#37‐#58 #60. #36 OR #59 #61. "Ecology‐" / all SUBHEADINGS in MIME,MJME,PT #62. explode "Environmental‐Health" / all SUBHEADINGS in MIME,MJME,PT #63. ( (nature near view?) in AB )or( (nature near view?) in TI ) #64. ( (nature near access) in AB )or( (nature near access) in TI ) #65. ( (garden*) in AB )or( (garden*) in TI ) #66. ( (window*) in AB )or( (window*) in TI ) #67. ( (plants) in AB )or( (plants) in TI ) #68. ( (sanctuary) in AB )or( (sanctuary) in TI ) #69. ( (horticultur*) in AB )or( (horticultur*) in TI ) #70. ( (landscape?) in AB )or( (landscape?) in TI ) #71. ( (urban) in AB )or( (urban) in TI ) #72. ( (flowers) in AB )or( (flowers) in TI ) #73. ( (biophilia) in AB )or( (biophilia) in TI ) #74. OR/#61‐#73 #75. #60 OR #74 #76. #25 AND #75 #77. COMMENT‐ in PT #78. #76 NOT #77 #79. CHILD in AGE #80. CHILD‐PRESCHOOL in AGE #81. INFANT in AGE #82. INFANT‐NEWBORN in AGE #83. OR/#79‐#82 #84. #78 NOT #83
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1. MeSH descriptor Aromatherapy, this term only in MeSH products #2. MeSH descriptor Music Therapy, this term only in MeSH products #3. MeSH descriptor Music, this term only in MeSH products #4. MeSH descriptor Television, this term only in MeSH products #5. MeSH descriptor Art, this term only in MeSH products #6. distraction in Record Title or distraction in Abstract or distraction in Keywords in CENTRAL #7. virtual NEXT reality in All Fields in CENTRAL #8. MeSH descriptor Paintings, this term only in MeSH products #9. (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8) #10. MeSH descriptor Architecture explode all trees in MeSH products #11. MeSH descriptor Environment Design, this term only in MeSH products #12. MeSH descriptor Health Facility Environment explode all trees in MeSH products #13. MeSH descriptor Patient Isolation, this term only in MeSH products #14. MeSH descriptor Air Conditioning, this term only in MeSH products #15. MeSH descriptor Lighting, this term only in MeSH products #16. MeSH descriptor Ventilation explode all trees in MeSH products #17. MeSH descriptor Noise, this term only in MeSH products #18. MeSH descriptor Odors, this term only in MeSH products #19. (#10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18) #20. MeSH descriptor Nature, this term only in MeSH products #21. window NEAR view in All Fields in CENTRAL #22. flower in Record Title or flower in Abstract in CENTRAL #23. garden OR gardens in Record Title or garden OR gardens in Abstract in CENTRAL #24. urban NEAR view in Abstract in CENTRAL #25. (#20 OR #21 OR #22 OR #23 OR #24) #26. (#9 OR #19 OR #25) #27. MeSH descriptor Patients, this term only in MeSH products #28. MeSH descriptor Inpatients, this term only in MeSH products #29. MeSH descriptor Outpatients, this term only in MeSH products #30. MeSH descriptor Hospitals explode all trees in MeSH products #31. *patient in All Fields in CENTRAL #32. (#27 OR #28 OR #29 OR #30 OR #31) #33. (#26 AND #32)
Appendix 3. EMBASE search strategy
1 art therapy/ or music therapy/ (1291) 2 art therap$.tw. (353) 3 music therap$.tw. (403) 4 (colour therap$ or color therap$).tw. (6) 5 exp sensory stimulation/ (30083) 6 acoustic stimulation.tw. (700) 7 environmental planning/ (2100) 8 exp microclimate/ (9265) 9 ((multisensory or multi‐sensory or sensory or therapeutic or restorative or healing) adj2 (environment$ or design)).tw. (1968) 10 hospital design/ (584) 11 environmental temperature/ (5443) 12 milieu therap$.tw. (108) 13 ((environmental or ambient) adj2 (design or feature$ or stimuli)).tw. (1952) 14 illumination/ (3967) 15 exp sound related phenomena/ or temperature/ (83594) 16 landscaping/ (361) 17 ((environmental or ambient) adj2 (design or feature$ or stimuli)).tw. (1952) 18 performance art.tw. (9) 19 odor/ (5456) 20 television/ (2667) 21 noise reduction/ (2754) 22 (fluorescent light$ or natural light$).tw. (893) 23 way finding aid$.tw. (0) 24 (household plant$ or garden$).tw. (2533) 25 or/1‐24 (147174) 26 hospitalization/ (44105) 27 exp physiology/ (20990) 28 exp physiology/ (20990) 29 exp anxiety/ (36236) 30 exp stress/ (68252) 31 exp analgesics/ (306913) 32 "length of stay"/ (16390) 33 anesthetic recovery/ (3435) 34 recovery time.tw. (3669) 35 (days adj2 recovery).tw. (2119) 36 patient satisfaction/ (24987) 37 exp emotions/ (101670) 38 exp aggression/ (21101) 39 Hospital Infection/ (17731) 40 sleep deprivation/ (2865) 41 or/26‐40 (586558) 42 25 and 41 (10061) 43 hospital patient/ (12716) 44 (hospital patient$ or inpatient$ or in‐patient$).tw. (2213126) 45 43 or 44 (2214656) 46 42 and 45 (1796) 47 randomized controlled trial/ (103293) 48 (randomised or randomized).tw. (161851) 49 experiment$.tw. (613741) 50 (time adj series).tw. (5256) 51 (pre test or pretest or post test or posttest).tw. (5718) 52 impact.tw. (156384) 53 intervention?.tw. (184862) 54 chang$.tw. (1004161) 55 evaluat$.tw. (931758) 56 effect?.tw. (1849257) 57 compar$.tw. (1620320) 58 or/47‐57 (4264846) 59 46 and 58 (1252) 60 from 59 keep 1‐1000 (1000) 61 from 59 keep 1001‐1252 (252)
Appendix 4. BNI search strategy
#43 #41 not #42(4372 records) #42 "designing questionnaires" or "questionnaire design"(23 records) #41 #39 not #40(4391 records) #40 "learning environment"(74 records) #39 #37 not #38(4461 records) #38 (UNDERGRADUATE) or (UNDERGRADUATES)(309 records) #37 #35 not #36(4477 records) #36 (SCHOOL) or (SCHOOL‐AGE) or (SCHOOL‐AGED) or (SCHOOL‐BASED) or (SCHOOL‐HEALTH) or (SCHOOL‐HEALTH‐SERVICES) or (SCHOOL‐NURSING)(2370 records) Searches and results below from saved search history BNI #35 (DESIGN) or (ARCHITECTURE) or ((DISTRACTION) or (DISTRACTIONS) or (DISTRACTORS)) or ((SENSES) or (SENSES‐)) or ((MUSIC) or (MUSIC‐VIDEO)) or (MUSIC‐BASED) or (MUSIC‐VIDEO) or ((TELEVISION) or (TELEVISIONS)) or (SENSORY‐STIMULATING) or (SENSORY‐STIMULATION) or (SENSORY‐CALMING) or (COLOURFUL) or (COLOUR) or (ART) or (AROMATIC) or (AROMATHERAPY) or (RETREAT) or (REFUGE) or (FLOWERS) or (SANCTUARY) or (PLANTS) or (( window )not( "window of" )not( "time window" )) or (( windows )not( time windows )not( "windows of" )) or (GARDEN) or (GARDENS) or (( #22 )not( research designs )not( study designs )) or (( designs )not( quantitative designs )not( qualitative designs )) or (( #20 )not( "their nature" )) or (( #19 )not( "human nature" )) or (( nature )not( "nature of" )not( "the nature" )) or (NOISE) or (( light )not( "in light" )) or (ENVIRONMENT‐FRIENDLY) or ((ENVIRONMENT) or (ENVIRONMENT‐FRIENDLY) or (ENVIRONMENTS))(4533 records) #34 AROMATIC(2 records) #33 AROMATHERAPY(203 records) #32 RETREAT(23 records) #31 REFUGE(10 records) #30 FLOWERS(23 records) #29 SANCTUARY(12 records) #28 PLANTS(23 records) #27 ( window )not( "window of" )not( "time window" )(29 records) #26 ( windows )not( time windows )not( "windows of" )(8 records) #25 GARDEN(31 records) #24 GARDENS(14 records) #23 ( #22 )not( research designs )not( study designs )(40 records) #22 ( designs )not( quantitative designs )not( qualitative designs )(60 records) #21 ( #20 )not( "their nature" )(83 records) #20 ( #19 )not( "human nature" )(85 records) #19 ( nature )not( "nature of" )not( "the nature" )(87 records) #18 NOISE(164 records) #17 ( light )not( "in light" )(423 records) #16 ENVIRONMENT‐FRIENDLY(2 records) #15 (ENVIRONMENT) or (ENVIRONMENT‐FRIENDLY) or (ENVIRONMENTS)(1421 records) #14 DESIGN(1044 records) #13 ARCHITECTURE(14 records) #12 (DISTRACTION) or (DISTRACTIONS) or (DISTRACTORS)(51 records) #11 (SENSES) or (SENSES‐)(153 records) #10 (MUSIC) or (MUSIC‐VIDEO)(278 records) #9 MUSIC‐BASED(2 records) #8 MUSIC‐VIDEO(1 records) #7 (TELEVISION) or (TELEVISIONS)(116 records) #6 SENSORY‐STIMULATING(1 records) #5 SENSORY‐STIMULATION(1 records) #4 SENSORY‐CALMING(1 records) #3 COLOURFUL(4 records) #2 COLOUR(68 records) #1 ART(528 records)
Appendix 5. PsycINFO search strategy
1."Noise‐Levels‐Work‐Areas" in MJ, MN 2.temperature near room 3.fluorescent light* 4.natural light* 5."Relaxation‐Therapy" in MJ, MN 6."Holistic‐Health" in MJ, MN 7.explode "Facility‐Environment" in MJ, MN 8."Environmental‐Planning" in MJ, MN 9.explode "Therapeutic‐Environment" in MJ, MN 10.explode "Architecture‐" in MJ, MN 11.restorative adj environment? 12.therapeutic adj environment? 13.healing adj environment? 14.healing adj design? 15.therapeutic adj design? 16.restorative adj design? 17."Milieu‐Therapy" in MJ, MN 18."Auditory‐Stimulation‐+" in MJ, MN 19."Olfactory‐Stimulation" in MJ, MN 20."Television‐Viewing" in MJ, MN 21."Visual‐Stimulation‐+" in MJ, MN 22."Illumination‐" in MJ, MN 23."Color‐" in MJ, MN 24.explode "Arts‐" in MJ, MN 25.explode "Creative‐Arts‐Therapy" in MJ, MN 26."Recreation‐Therapy" in MJ, MN 27."Distraction‐" in MJ, MN 28.plant? 29.flora? 30.window* 31.biophilia 32.garden* in AB 33.refuge 34.nature near view? 35.retreat 36.nature near access 37.flower? 38.urban 39.landscape? 40.horticultur* 41.sanctuary 42.or/1‐41 43.OUTPATIENT in PO 44.INPATIENT in PO 45.or/43‐44 46.42 and 45
Appendix 6. Construction and Building Abstracts search strategy
1. hospital* 2. hospice* 3. patient* 4. or/1‐2 5. 4 and 3
Appendix 7. RIBA search strategy
1. NAME OF BUILDING "hospice$" 2. NAME OF BUILDING "hospital$" 3. 1 or 2
Appendix 8. InformeDesign search strategy
All records retrieved listed under: Health Care: 1. Health Care ‐General (15) 2. Intensive Care/Acute Care (8) 3. Laboratory (1) 4. Long Term Care/Nursing Home (29) 5. Outpatient Treatment (4) 6. Rehabilitation (1) 7. Ambulatory Care (1) 8. Clinic (4) 9. Emergency Room (2) 10. Examination Room (2) 11. Hospice Care (1) 12. Hospital (11) Occupants: 1. Patient (41)
Appendix 9. Avery search strategy
S1: BIK= "hospital*" S2: BIK= "hospice*" S3: BIK= "interior" AND "design" S4: BIK= "alterations" S5: BIK= "additions" S6: BIK= "patient*" S7: BIK= "children*" S8: S1 or S2 or S6 S9: S3 or S4 or S5 S10: S8 and S9 S11:S10 not S7
Appendix 10. CINAHL search strategy
#29 (("Middle‐Age" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or (("Aged‐80‐and‐Over" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Aged‐Hospitalized" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Frail‐Elderly" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Aged‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Adult‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE))) and (#23 not #24)(1864 records) #28 ("Middle‐Age" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or (("Aged‐80‐and‐Over" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Aged‐Hospitalized" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Frail‐Elderly" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Aged‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Adult‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE))(220395 records) #27 "Middle‐Age" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(103161 records) #26 ("Aged‐80‐and‐Over" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Aged‐Hospitalized" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Frail‐Elderly" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Aged‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Adult‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE)(201374 records) #25 #23 not #24(8865 records) #24 Military‐Personnel in MJ(987 records) #23 #17 not #22(8873 records) #22 (explode "Education‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or (explode "Schools‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Hospitals‐Pediatric" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or (("Halfway‐Houses" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Residential‐Facilities" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Nursing‐Homes" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE))(198593 records) #21 explode "Education‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(191546 records) #20 explode "Schools‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(10865 records) #19 "Hospitals‐Pediatric" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(1412 records) #18 ("Halfway‐Houses" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Residential‐Facilities" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Nursing‐Homes" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE)(7018 records) #17 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16(11986 records) #16 ("Patients'‐Rooms" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Patient‐Bedside" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE)(293 records) #15 ("Air‐Conditioning" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Temperature‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Lighting‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Laminar‐Air‐Flow" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Ventilation" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Heating‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Environment‐Controlled" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Humidity‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE)(1750 records) #14 ("Hospital‐Design‐and‐Construction" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Facility‐Design‐and‐Construction" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Floors‐and‐Floorcoverings" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE)(1327 records) #13 "Architectural‐Accessibility" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(478 records) #12 "Interior‐Design‐and‐Furnishings" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(842 records) #11 ("Distraction‐Iowa‐NIC" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Distraction‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE)(209 records) #10 "Aromatherapy‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(635 records) #9 "Noise‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(1112 records) #8 "Sensation‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(497 records) #7 "Natural‐Environment" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(65 records) #6 "Music‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(1527 records) #5 "Television‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(1436 records) #4 "Socioenvironmental‐Therapy" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(286 records) #3 "Sensory‐Stimulation" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(383 records) #2 "Color‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE(484 records) #1 ("Art‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE) or ("Signage‐" / all TOPICAL SUBHEADINGS / all AGE SUBHEADINGS in DE)(1508 records)
Appendix 11. Web of Science search strategy
1. TS=aromatherapy 2. TS=music 3. TI=(art OR arts) 4. TS=television* 5. TS=virtual reality 6. TS=distraction therapy 7. TI=layout* 8. TS=patient isolation 9. TS=air conditioning 10. TI=noise 11. TS=garden* 12. TS=architectur* 13. TI=(design* SAME hospital) 14. TI=(design* SAME ward*) 15. TI=(design* SAME environment*) 16. TS=(ventilation NOT mechanical) 17. TS=(daylight OR artificial light* OR natural light* OR fluorescent light* OR florescent light*) 18. #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 19. TS=((hospital* OR ward* OR patients) NOT (pediat* OR paediat* OR child* OR neonatal OR newborn* OR dentist* OR snoezelen OR SAD OR seasonal affective disorder OR pathology)) 20. #19 AND #18
Appendix 12. ASSIA search strategy
1.NOISE in DE 2.BEDROOMS in DE 3.ENVIRONMENTAL ROOMS in DE 4.PRACTICE ROOMS in DE 5.WAITING ROOMS in DE 6.ROOMMATES in DE 7.ROOM ARRANGEMENTS in DE 8.ARTIFICIAL LIGHT in DE 9.BRIGHTNESS in DE 10.DAYLIGHT in DE 11.HOLISTIC MEDICINE in DE 12.AROMATHERAPY in DE 13.ESSENTIAL OILS in DE 14.SNOEZELEN APPROACH in DE 15.ENVIRONMENTAL ASPECTS in DE 16.BUILT ENVIRONMENT in DE 17.FACILITATING ENVIRONMENT in DE 18.GROUP ENVIRONMENT in DE 19.NOISY ENVIRONMENT in DE 20.PSYCHOLOGICAL ENVIRONMENT in DE 21.PSYCHOSOCIAL ENVIRONMENT in DE 22.STRESSFUL ENVIRONMENT in DE 23.URBAN ENVIRONMENT in DE 24.WINDOWS in DE 25.MULTISENSORY ROOMS in DE 26.INTERIOR DESIGN in DE 27.ARCHITECTURE in DE 28.AESTHETICS in DE 29.MUSIC THERAPY in DE 30.MILIEU THERAPY in DE 31.NATURAL PHENOMENA in DE 32.PERSON‐ENVIRONMENT FIT in DE 33.ENVIRONMENTAL PSYCHOLOGY in DE 34.REFUGE in DE 35.RETREATS in DE 36.HORTICULTURE in DE 37.PLANTS in DE 38.URBAN AREAS in DE 39.NATURAL LANDSCAPES in DE 40.URBAN LANDSCAPES in DE 41.SANCTUARIES in DE 42.NATURE in DE 43.DANCERS in DE 44.MUSICIANS in DE 45.SINGERS in DE 46.PROFESSIONAL DANCERS in DE 47.PERFORMING ARTS in DE 48.ARTS in DE 49.CONCERTS in DE 50.ART in DE 51.DANCING in DE 52.MUSIC in DE 53.MULTIMODAL THERAPY in DE 54.THEATRE in DE 55.BACKGROUND MUSIC in DE 56.BLUES MUSIC in DE 57.CLASSICAL MUSIC in DE 58.COUNTRY MUSIC in DE 59.DANCE MUSIC in DE 60.DRUMMING in DE 61.FOLK MUSIC in DE 62.JAZZ in DE 63.MELODIES in DE 64.MOTETS in DE 65.OPERA in DE 66.ORCHESTRAS in DE 67.POP MUSIC in DE 68.ROCK MUSIC in DE 69.SALSA MUSIC in DE 70.SINGING in DE 71.SONGS in DE 72.HEAVY METAL MUSIC in DE 73.PUNK ROCK MUSIC in DE 74.HIP HOP MUSIC in DE 75.INDIE MUSIC in DE 76.RAP MUSIC in DE 77.RAVE MUSIC in DE 78.REGGAE MUSIC in DE 79.CONTEMPORARY ART in DE 80.DRAWINGS in DE 81.PAINTINGS in DE 82.POSTMODERN ART in DE 83.PUBLIC ART in DE 84.IMPRESSIONISTIC PAINTINGS in DE 85.NATURE PAINTINGS in DE 86.PORTRAITS in DE 87.COLOUR in DE 88.TELEVISION in DE 89.ANIMATION in DE 90.CABLE TELEVISION in DE 91.DIGITAL TELEVISION in DE 92.LIVE TELEVISION in DE 93.LOCAL TELEVISION in DE 94.SATELLITE TELEVISION in DE 95.DISTRACTORS in DE 96.DISTRACTION in DE 97.or/1‐96 98.OUTPATIENT CLINICS in DE 99.HOSPICES in DE 100.MINOR INJURIES UNITS in DE 101.PERIOPERATIVE CARE in DE 102.POSTOPERATIVE CARE in DE 103.ACCIDENT AND EMERGENCY DEPARTMENTS in DE 104.BURNS UNITS in DE 105.CHEST PAIN UNITS in DE 106.COMMUNITY HOSPITALS in DE 107.DAY HOSPITALS in DE 108.DISTRICT GENERAL HOSPITALS in DE 109.DRUG DEPENDENCY UNITS in DE 110.FIELD HOSPITALS in DE 111.GENERAL PRACTITIONER HOSPITALS in DE 112.GERIATRIC HOSPITALS in DE 113.INTENSIVE CARE UNITS in DE 114.LEARNING DISABILITY HOSPITALS in DE 115.LONG TERM HOSPITALS in DE 116.MAGNET HOSPITALS in DE 117.MATERNITY HOSPITALS in DE 118.MATERNITY UNITS in DE 119.MILITARY HOSPITALS in DE 120.MISSION HOSPITALS in DE 121.NEUROSURGICAL UNITS in DE 122.NIGHT HOSPITALS in DE 123.OPERATING THEATRES in DE 124.ORTHOPAEDIC UNITS in DE 125.OUTPATIENT DEPARTMENTS in DE 126.PARTIAL HOSPITALIZATION PROGRAMMES in DE 127.PRIVATE HOSPITALS in DE 128.PSYCHIATRIC HOSPITALS in DE 129.SPECIAL HOSPITALS in DE 130.STROKE UNITS in DE 131.TEACHING HOSPITALS in DE 132.TRUST HOSPITALS in DE 133.HOSPITALS in DE 134.or/98‐133 135.97 and 134
Appendix 13. National Research Register search strategy
AROMATHERAPY single term (MeSH) ‐ 38 hits MUSIC single term (MeSH) ‐ 19 hits MUSIC THERAPY single term ‐ 35 hits TELEVISION single term (MeSH) ‐ 14 hits PAINTINGS single term (MeSH) ‐ 2 hits ART single term (MeSH) ‐ 13 hits distraction:ti ‐ 36 hits distracting:ti ‐ 1 hits virtual NEXT reality ‐ 35 hits ARCHITECTURE explode tree 1 (MeSH) ‐ 28 hits ENVIRONMENT DESIGN single term (MeSH) ‐ 15 hits HEALTH FACILITY ENVIRONMENT explode all trees (MeSH) ‐ 30 hits PATIENT ISOLATION single term (MeSH) ‐ 8 hits AIR CONDITIONING single term (MeSH) ‐ 3 hits LIGHTING single term (MeSH) ‐ 7 hits VENTILATION single term (MeSH) ‐ 6 hits NOISE single term (MeSH) ‐ 15 hits ODORS single term (MeSH) ‐ 5 hits NATURE single term (MeSH) ‐ 0 hits window NEXT view ‐ 0 hits window NEXT views ‐ 0 hits flowers:ti ‐ 0 hits garden:ti ‐ 2 hits gardens:ti ‐ 0 hits urban NEAR view ‐ 3 hits nature NEAR views ‐ 14 hits nature:ti ‐ 187 hits aromatherapy ‐ 54 hits music ‐ 97 hits television ‐ 36 hits art:ti ‐ 63 hits environment:ti ‐ 310 hits milieu ‐ 29 hits patient NEXT isolation ‐ 11 hits Ventilation ‐ 841 hits Aromas ‐ 0 hits Aroma ‐ 7hits Noise ‐ 159 hits Smell ‐ 46 hits Smells ‐ 2 hits Odours ‐ 9 hits Odour ‐ 23 hits Odors ‐ 5 hits Odor ‐ 0 hits Air NEXT conditioning ‐ 4 hits Lighting ‐ 21 hits Lights ‐ 15 hits Bedroom ‐ 6 hits Bedrooms ‐ 0 hits Architecture ‐ 95 hits Layout ‐ 14 hits Ward NEXT design ‐ 3 hits Wayfinding ‐ 3 hits Signage ‐ 1 hit Signs ‐ 77 hits Carpets ‐ 2 hits Flooring ‐ 0 hits Floors ‐ 5 hits Windows ‐ 58 hits Patients NEXT rooms ‐ 39 hits
Appendix 14. Architecture Publication Index search strategy
Select types of records you wish to search: PERIODICAL ARTICLES Now select the range you require: ALL YEARS
Search terms: All fields: patient*
Appendix 15. Turning Research Into Practice (TRIP) search strategy
Free text terms searched in the "title" field only:
aromatherapy OR music OR art OR arts OR television* OR "distraction therapy" OR "virtual reality" OR architectur* OR design* OR environment* OR layout* OR "patient isolation" OR "air conditioning" OR light* OR noise OR ventilation AND hospital* OR garden* OR decoration OR distracting
Appendix 16. Zetoc search strategy
Search conducted with "general search" (journals and conferences). Search terms entered in "title" field only.
1. aromatherapy patients (16) 2. music patients (153) 3. Music hospital* (37) 4. Hospital* arts (19) 5. art patients (190) 6. Arts patients (15) 7. television patients (5) 8. distraction therapy (15) 9. virtual reality patients (26) 10. Architectur* hospital* (102) 11. hospital design (312) 12. Design hospitals (62) 13. Hospital environment (389) 14. Ward layout* (2) 15. Ward environment* (61) 16. Ward design* (28) 17. Patient isolation (196) 18. Air conditioning hospital* (18) 19. Air conditioning patients (2) 20. Light* hospital* (92) 21. Lighting patients (5) 22. Ventilation Hospital* (108) 23. Noise hospital* (48) 24. Noise patients (70) 25. Garden* hospital* (23)
Appendix 17. MEDLINE updated search strategy
1. (randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or placebo.ab. or clinical trials as topic.sh. or randomly.ab. or trial.ti. (721440) 2. exp animals/ not humans.sh. (3584268) 3. 1 not 2 [Cochrane RCT Filter 6.4.d Sens/Precision Maximizing] (668537) 4. intervention?.ti. or (intervention? adj6 (clinician? or collaborat$ or community or complex or DESIGN$ or doctor? or educational or family doctor? or family physician? or family practitioner? or financial or GP or general practice? or hospital? or impact? or improv$ or individuali?e? or individuali?ing or interdisciplin$ or multicomponent or multi‐component or multidisciplin$ or multi‐disciplin$ or multifacet$ or multi‐facet$ or multimodal$ or multi‐modal$ or personali?e? or personali?ing or pharmacies or pharmacist? or pharmacy or physician? or practitioner? or prescrib$ or prescription? or primary care or professional$ or provider? or regulatory or regulatory or tailor$ or target$ or team$ or usual care)).ab. (111007) 5. (hospital$ or patient?).hw. and (study or studies or care or health$ or practitioner? or provider? or physician? or nurse? or nursing or doctor?).ti,hw. (600947) 6. demonstration project?.ti,ab. (1669) 7. (pre‐post or "pre test$" or pretest$ or posttest$ or "post test$" or (pre adj5 post)).ti,ab. (45565) 8. (pre‐workshop or post‐workshop or (before adj3 workshop) or (after adj3 workshop)).ti,ab. (411) 9. trial.ti. or ((study adj3 aim?) or "our study").ab. (424292) 10. (before adj10 (after or during)).ti,ab. (293973) 11. ("quasi‐experiment$" or quasiexperiment$ or "quasi random$" or quasirandom$ or "quasi control$" or quasicontrol$ or ((quasi$ or experimental) adj3 (method$ or study or trial or design$))).ti,ab,hw. [ML] (80883) 12. ("time series" adj2 interrupt$).ti,ab,hw. [ML] (541) 13. (time points adj3 (over or multiple or three or four or five or six or seven or eight or nine or ten or eleven or twelve or month$ or hour? or day? or "more than")).ab. (5878) 14. pilot.ti. (27972) 15. Pilot projects/ [ML] (63517) 16. (clinical trial or controlled clinical trial or multicenter study).pt. [ML] (559118) 17. (multicentre or multicenter or multi‐centre or multi‐center).ti. (21501) 18. (random$ or controlled).ti,ab. (781142) 19. (control adj3 (area or cohort? or compare? or condition or design or group? or intervention? or participant? or study)).ab. not (controlled clinical trial or randomized controlled trial).pt. [ML] (312893) 20. "comment on".co. or systematic review.ti. or literature review.ti. or randomized controlled trial.pt. [ML] (328972) 21. exp animals/ not humans.sh. [ML] (3584268) 22. *experimental design/ or *pilot study/ or quasi experimental study/ [EM] (16120) 23. ("quasi‐experiment$" or quasiexperiment$ or "quasi random$" or quasirandom$ or "quasi control$" or quasicontrol$ or ((quasi$ or experimental) adj3 (method$ or study or trial or design$))).ti,ab. [EM] (80883) 24. ("time series" adj2 interrupt$).ti,ab. [EM] (541) 25. (or/4‐19) not (or/20‐21) [EPOC Methods Filter ML 1.8] (1961926) 26. or/4‐10,13‐14,17‐18,22‐24 [EPOC Methods Filter EM 1.8] (2092621) 27. Patients' Rooms/ (1753) 28. exp Patients/ or (patient? or inpatient?).ti. (1068697) 29. ward?.ti,ab. (32686) 30. or/27‐29 [Patients or Ward] (1095079) 31. "Hospital Design and Construction"/ (7608) 32. Environment design/ or "facility design and construction"/ or architectural accessibility/ or "floors and floorcoverings"/ or "interior design and furnishings"/ (13827) 33. Environment, Controlled/ or Air conditioning/ or Heating/ or Humidity/ or Lighting/ or Temperature/ or Ventilation/ or Noise/ (202220) 34. exp hospitals/ or Hospital units/ or exp Hospital Departments/ or exp Ambulatory Care Facilities/ or Health Facilities/ or exp hospitals, teaching/ or Hospices/ or Health Facility Environment/ (319293) 35. (or/32‐33) and 34 (4473) 36. 31 or 35 [Hosp Design/Hosp Envir] (11394) 37. ((healing or therapeutic) adj2 environment?).ti,ab. (630) 38. protected environment.ti,ab. [may not search this in ab in EMBASE] (187) 39. Music therapy/ or aromatherapy/ (2197) 40. Sensory Art Therapies/ or color therapy/ or art therapy/ or Acoustic Stimulation/ or complementary therapies/ (41150) 41. (patient? distraction or distraction therapy or distraction therapies).ti. (6) 42. Art/ or Color/ or Music/ (28488) 43. Sunlight/ or Plants/ or Gardening/ (68743) 44. (garden? or solarium? or (plants adj2 (indoor? or ornament$ or decorat$)) or natural environment? or landscaping).ti,ab. (8345) 45. (room? and (colo?r? or decoration? or design? or layout? or lighting or temperature)).ti. (2611) 46. or/37‐45 [Healing Env/Sensory Stimulus/Therapies] (150325) 47. exp Patients/ and Anxiety/ (1095) 48. anxiety/pc or (Anxiety and hospital$).hw. or (anxiety and hospital$).ti. [formerly anxiety pc only] (5230) 49. ((pre‐operative or post‐operative) adj2 (anxiety or psycholo$)).ti,ab. (130) 50. ((inpatient? or patient?) adj3 psycholog$).ab. (4076) 51. ((adverse event? or adverse effect) adj3 (reduc$ or decreas$)).ti,ab. (866) 52. ((inpatient? or patient?) and (anxiety or comfort or discomfort or distraction? or pain level? or (reduc$ adj2 pain))).ti. (3738) 53. ((inpatient? or patient?) adj3 (anxiety or comfort or discomfort or distraction? or (reduc$ adj pain))).ab. (12950) 54. (intraoperative complications/ or Postoperative Complications/) and "prevention & control".fs. (41374) 55. (perioperative care/ or intraoperative care/ or postoperative care/ or preoperative care/) and methods.fs. (35519) 56. (intraoperative complications/ or Postoperative Complications/) and "prevention & control".fs. and patient?.ti,hw. (5917) 57. (intraoperative complications/pc or Postoperative Complications/pc) and adverse effects.fs. (8845) 58. (patient? adj5 distraction?).ab. (709) 59. ((agitation or agitated) adj5 (patient? or inpatient?)).ti,ab. (1345) 60. or/47‐59 [Patient Anxiety] (100687) 61. (exp diagnostic techniques, surgical/ or exp Surgical Procedures, Operative/) and anxiety/ (3543) 62. (intraoperative complications/ or Postoperative Complications/ or perioperative care/ or intraoperative care/ or postoperative care/ or Preoperative care/) and Anxiety/ (970) 63. (exp diagnostic techniques, surgical/ or exp Surgical Procedures, Operative/ or intraoperative complications/ or Postoperative Complications/ or perioperative care/ or intraoperative care/ or postoperative care/ or Preoperative care/) and 60 (80582) 64. or/61‐63 [Anxiety & Procedures] (82717) 65. exp Vital signs/ and music.ti,hw. (251) 66. ((Hospital$ or preoperat$ or postoperat$ or an?esthe$ or pain or prean?esth$ or sedation or blood pressure or heart rate or respiration or ward? or inpatient?) and (aromatherap$ or music)).ti,hw. (1221) 67. (Hospital$ or preoperat$ or postoperat$ or an?esthe$ or pain or prean?esth$ or sedation or blood pressure or heart rate or respiration or ward? or inpatient?).ti,ab,hw. and (diversion$ adj2 (therapy or therapies or intervention?)).ti,ab. (17) 68. (Hospital$ or preoperat$ or postoperat$ or an?esthe$ or pain or prean?esth$ or sedation or blood pressure or heart rate or respiration or ward? or inpatient?).ti,ab,hw. and (distraction adj (therapy or therapies)).ti,ab. (16) 69. ((environmental or patient? or inpatient? or outpatient? or out‐patient?) adj surrounding?).ti,ab. (53) 70. or/65‐69 [Keywords/Misc combine with filters only] (1308) 71. 60 and (or/35‐36) [Anxiety & Hosp Design/Interior Enviro] (93) 72. 30 and 35 [Patients/Rooms & Hosp Design/Interior Enviro] (738) 73. 30 and 46 [Patients/Rooms & Healing Enviro] (4163) 74. 46 and 60 [Healing Env & Anxiety] (540) 75. 60 and 64 and (or/36,46) [Patient Anxiety & Procedures & Hosp Design/Envir] (225) 76. 70 or 71 or 72 or 73 or 74 or 75 (6121) 77. 76 and 3 [RCT Results] (716) 78. 76 and 25 [EPOC FIlter 1.8 Results] (2516)
Data and analyses
Comparison 1. Audiovisual distraction versus music.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety | 2 | 87 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐1.05, 0.56] |
| 2 Pain | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Endoscopic procedural pain | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 post‐operative pain | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Audiovisual distraction versus standard care.
Comparison 3. Music versus blank tape / headphones only.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Pre‐procedural anxiety | 4 | 361 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.82 [‐1.03, ‐0.60] |
| 1.2 Procedural anxiety | 3 | 183 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.47, 0.23] |
| 1.3 Post‐operative anxiety | 3 | 220 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.52, 0.44] |
| 1.4 ICU anxiety | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.32, 0.66] |
| 2 Heart rate | 8 | 543 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐1.02, 1.82] |
| 3 Blood pressure | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Systolic | 7 | 533 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐2.48, 1.67] |
| 3.2 Diastolic | 6 | 478 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐2.08, 1.39] |
| 3.3 Arterial | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 4.0 [‐5.33, 13.33] |
| 4 Respiration rate: with choice of outcomes | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Post‐operative period for Ikonomidou 2004 and final scores (both studies) | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐1.72 [‐1.00, ‐0.44] |
| 4.2 Post‐operative period for Ikonomidou 2004 and change score for Lee 2005 | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐2.48 [‐3.85, ‐1.11] |
| 4.3 Pre‐operative period for Ikonomidou 2004 and final scores (both studies) | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.92, 0.09] |
| 4.4 Pre‐operative period for Ikonomidou 2004 and change scores for Lee 2005 | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐2.09 [‐4.51, 0.34] |
| 5 Skin conductance | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Stress hormones | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Cortisol | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.73, 0.09] |
| 6.2 Epinephrine | 2 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.38, 0.33] |
| 6.3 Norepinephrine | 2 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.44, 0.27] |
| 6.4 Adrenocorticotropic hormone (ACTH) | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.17, 0.28] |
3.5. Analysis.
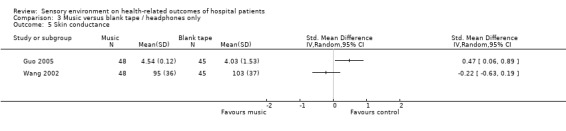
Comparison 3 Music versus blank tape / headphones only, Outcome 5 Skin conductance.
3.6. Analysis.
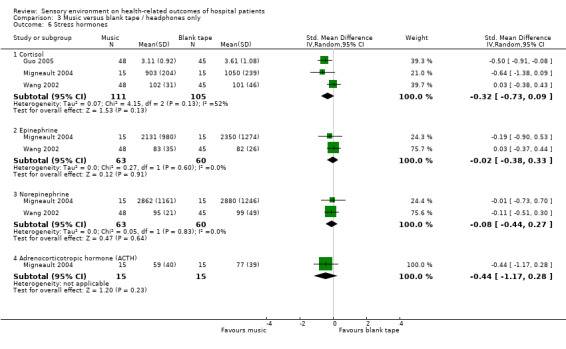
Comparison 3 Music versus blank tape / headphones only, Outcome 6 Stress hormones.
Comparison 4. Music versus scheduled rest.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety | 8 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Procedural anxiety | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 ICU/CCU anxiety | 7 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Heart rate | 4 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.76 [‐6.65, 1.13] |
| 3 Blood pressure | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Systolic | 3 | 140 | Mean Difference (IV, Random, 95% CI) | ‐1.51 [‐6.65, 3.63] |
| 3.2 Diastolic | 2 | 110 | Mean Difference (IV, Random, 95% CI) | ‐5.29 [‐8.78, ‐1.79] |
| 3.3 Arterial | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐4.75 [‐13.98, 4.48] |
| 4 Respiration rate | 3 | 110 | Mean Difference (IV, Random, 95% CI) | ‐2.04 [‐3.43, ‐0.66] |
Comparison 5. Music versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety | 29 | 1812 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.74, ‐0.36] |
| 1.1 Pre‐procedural anxiety | 9 | 744 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.62, ‐0.12] |
| 1.2 Procedural anxiety | 15 | 865 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.02, ‐0.36] |
| 1.3 ICU/post‐operative anxiety | 5 | 203 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.01, ‐0.15] |
| 2 Heart rate | 21 | 1653 | Mean Difference (IV, Random, 95% CI) | ‐2.72 [‐4.70, ‐0.74] |
| 3 Blood pressure | 20 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Systolic | 18 | 1437 | Mean Difference (IV, Random, 95% CI) | ‐1.76 [‐5.09, 1.56] |
| 3.2 Diastolic | 17 | 1407 | Mean Difference (IV, Random, 95% CI) | ‐0.97 [‐2.58, 0.63] |
| 3.3 Arterial | 2 | 186 | Mean Difference (IV, Random, 95% CI) | ‐9.86 [‐12.06, ‐7.65] |
| 4 Respiration rate | 9 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Sedation requirements (anxiolytics) | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Midazolam (aka: Versed, Hypnovel, Dormicum, Dormonid), mg | 3 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Peripheral skin temperature | 4 | 298 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.08, 0.37] |
| 7 Oxygen saturation | 3 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.75, 0.32] |
| 8 Mood state | 2 | 170 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐2.17, ‐0.19] |
| 9 Satisfaction | 2 | 174 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.16, 0.76] |
| 10 Length of stay / Examination time | 2 | 153 | Mean Difference (IV, Random, 95% CI) | ‐6.00 [‐10.72, ‐1.28] |
5.6. Analysis.
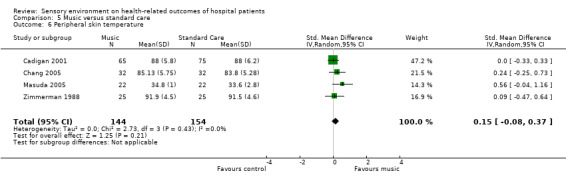
Comparison 5 Music versus standard care, Outcome 6 Peripheral skin temperature.
5.7. Analysis.
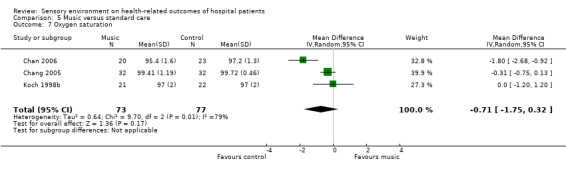
Comparison 5 Music versus standard care, Outcome 7 Oxygen saturation.
5.8. Analysis.
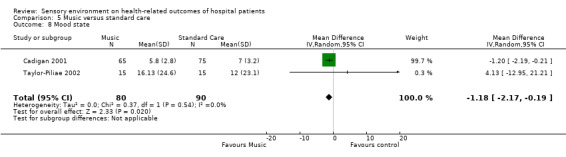
Comparison 5 Music versus standard care, Outcome 8 Mood state.
5.9. Analysis.
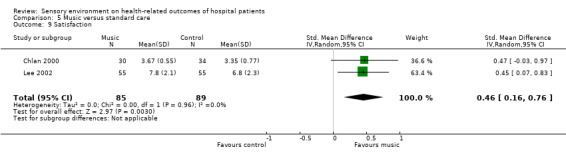
Comparison 5 Music versus standard care, Outcome 9 Satisfaction.
5.10. Analysis.
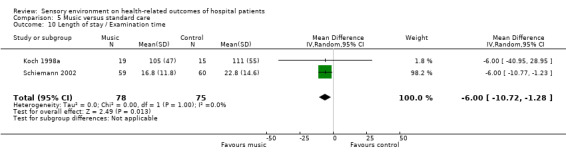
Comparison 5 Music versus standard care, Outcome 10 Length of stay / Examination time.
Comparison 6. Music versus white noise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Heart rate | 2 | 144 | Mean Difference (IV, Random, 95% CI) | 4.67 [‐0.76, 10.10] |
| 2 Blood pressure | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Systolic | 2 | 144 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐8.59, 5.00] |
| 2.2 Diastolic | 2 | 144 | Mean Difference (IV, Random, 95% CI) | 0.99 [‐7.60, 9.58] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allen 2001.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘‘Patients were sequentially selected from the patient rosters of two ophthalmic surgeons. [...] On each day data collection surgeons were randomly assigned to have their patients in the experimental or control group.’’ Method of randomisation not stated. |
| Allocation concealment (selection bias) | High risk | "Office assistants were unaware of the study prepared patient rosters. On each day data collection surgeons were randomly assigned to have their patients in the experimental or control group. Patients were then approached in the waiting room and asked to participate in the study." Patients approached after allocation. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Not extracted for review (validity of measurement scales unclear). |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Automated measurement of physiological data via Propaq Monitor. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. Physiological outcomes reported for all included patients. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Music allocated on an individual basis via headphones. |
Andrada 2004.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subsequently, patients were divided randomly into the experimental group or the control group by the flip of a coin." |
| Allocation concealment (selection bias) | High risk | Patients were randomised after consent by the flip of a coin. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of their group allocation. "During the procedure, patients did not inform either the explorer of assistant whether they belonged to the experiemental group or the control group." |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Patients aware of their group allocation. "During the procedure, patients did not inform either the explorer of assistant whether they belonged to the experiemental group or the control group." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Description of withdrawals and drop‐outs: 3 patients excluded as had taken anxiolytic drugs within 72 hours prior to procedure. Missing data unclear. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Music allocated to individuals via headphones. |
Argstatter 2006.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not descibed. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear whether measurements of physiological outcomes were automated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Description of withdrawals and drop‐outs: 7 patients were excluded due to incomplete outcome data. Outcomes reported for > 80% of participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Music allocated to individuals via headphones. |
Ayoub 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomized into three groups." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | "The research team consisted of a nonblinded member who randomized participants and administered the intervention" Allocation concealment not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Low risk | "An external power switch was connected to the opaque box and power was temporarily turned off before each OAA/S was determined to assure blindness of the outcomes assessor". |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "Vital signs [...], propofol consumption, and OAA/S score were documented every 5 min by the blinded researcher". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Individuals allocated to groups and all wore headphones. |
Bally 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients who consented were immediately randomized [...] by selecting a randomly generated group number [...]" |
| Allocation concealment (selection bias) | Low risk | "randomly generated group number sealed in an opaque envelope" |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Outcome assessors aware of group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "113 (87.6%) agreed to participate [...].We have complete data on 107 patients. Six patients (4 controls, 2 experimental) were not included because the procedure was cancelled after their enrolment or they could not complete all the questionnaires because of complications." |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and BP. |
| Protection from contamination? | Low risk | Individuals allocated to the music group listened via headphones. |
Barnason 1995/1996.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 or Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The researcher randomly assigned subjects to one of the three intervention groups by drawing lots" |
| Allocation concealment (selection bias) | High risk | "After written consent was obtained from the subject, the researcher randomly assigned subjects [...]. A slip of paper was drawn out of the box before requesting participation. If the subject consented to participate, the slip of paper was thrown away; if the subject did not agree to participate, the slip of paper was put back in the box." |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Physiological data not described in enough detail for use in review. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "All participants enrolled in the study participated in both sessions". Missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: BP and HR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Binnings 1987.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients who met the study criteria were assigned to the control or experimental groups by using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear if the anaesthetist was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Blankfield 1995.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned to one of three groups." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Length of stay and narcotics usage ‐blinding unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "100 patients were enrolled. Two patients who died in hospital were excluded from the final data analysis. Three patients whose hospitalization following surgery lasted longer 14 days were also excluded from the final data analysis." Data presented for 95 remaining participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Broscious 1999.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by drawing lots in a blinded fashion. |
| Allocation concealment (selection bias) | Low risk | Randomised by drawing lots in a blinded fashion. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | HR and BP automated measurement with Hewlett‐Packard Component Monitoring System or a DINAMAP. Healthcare staff removing chest tubes were blinded to which tape patients were listening to. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 participants withdrew (reasons and group allocation not described), 3 participants had cancelled surgery, 11 had chest tube removal prior to baseline data collection, 3 participants were suffering from confusion, 9 had an unstable condition preventing chest tube removal, 2 had equipment failure, and one person died. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Buffum 2006.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were assigned using a table of random numbers to either group" |
| Allocation concealment (selection bias) | Unclear risk | "Patients who consented to participate were then given a number that had been preassigned [...]. Patients became aware of their assigned group after they signed the consent." No description of whether the person recruiting patients knew the assignments in advance. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | "The patients and staff were not blinded to assignment" |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | "The patients and staff were not blinded to assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "A total of 190 persons were recruited, 20 refused, and 170 persons completed the study." Does not describe if the 20 refusals occurred before or after randomisation, or reasons for refusal. Data reported for 170 participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Cadigan 2001.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomized to either the treatment or control group by means of a table of random numbers." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Outcome assessors aware of group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Cepeda 1998.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly allocated by the nurse to two groups using a computer‐generated list" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Unclear if patients were aware of the difference between the two groups. Patients in the control group were played music after the outcome measures had been taken, for 10 minutes at the conclusion of the procedure. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Anaesthesiologist blinded to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "There were no drop‐outs." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Chan 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The subjects were randomly assigned to either a music or no‐music group by the research nurse using a computer‐generated random number series [...]" |
| Allocation concealment (selection bias) | Low risk | "computer‐generated random number series contained within closed opaque envelopes." |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Objective outcomes not addressed by this study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "all subjects completed the STAI form again and assessed their degree of pain" "220 women were entered into the trial and all of them completed the study" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Chan 2006.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Forty six participants were included in the study, using a random digit generated by research randomizer (Research Randomizer 2005)." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear if physiological outcome measures were automated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Three participants in the music group expressed a dislike of the music that they had chosen. They refused to continue to participate and their data were withdrawn from the analysis" "Missing values were replaced by the group mean" Amount of missing data values not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Chang 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly allocated to experimental and control groups." Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients in the control group were not aware they had not had the opportunity to listen to music. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Physiological outcomes were measured via automated system. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 withdrew from the music group for the following reasons:"(a) lost interest (n = 2), (b) received nitrous oxide or sedative (n=2), (c) had a newborn with imperforate anus (n = 1) or had failure of local anesthesia (n = 1)" 6 withdrew from the control group for the following reasons: "(a) had emergency caesarean section (n = 2) and (b) received nitrous oxide or sedative (n = 4)" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Unclear risk | Interventions administered on an individual basis. |
Chlan 1995.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Each subject was randomized." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Physiological measures recorded via range of means, some automated others not. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR, BP, and RR. |
| Protection from contamination? | Unclear risk | Interventions administered on an individual basis. |
Chlan 1998.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "With use of a table of random numbers, subjects were randomized to either a control group or to an experimental group" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Respiration rate measured via observation. Outcome assessor not blinded. Heart rate measured via bedside monitor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Among the 54 subjects who signed consent forms, two withdrew after instrument administration for personal reasons. Three subjects withdrew at various times during the assigned treatment conditions, two in the experimental group and one from the control group. Reasons given for with‐drawal were personal (i.e., tired of lying still or were too anxious) or, in one instance, because the subject was scheduled for a diagnostic test." |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Chlan 2000.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects who consented to participate in the study were randomized by a coin‐flip to either an experimental condition or control condition" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. "All subjects completed the NRS‐discomfort instrument, followed by the state anxiety scale" ‐implies no missing data. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Chui 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "They were randomly assigned to experimental [...] and control [...] group" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | This study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Method of collecting blood pressure data not described. Unclear if automated. Heart rate variability measured via electrocardiogram (ECG). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Colt 1999.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "using a random‐numbers table" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data in tables presented for all included participants. Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Cooke 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated list was used for permuted block random assignment" |
| Allocation concealment (selection bias) | Low risk | "A biostatistician and research assistant who did not participate in data collection conducted the randomization procedures and prepared sequentially numbered sealed envelopes containing the random assignment for each consenting patient" |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "there were no drop‐outs" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Cruise 1997.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was by patients selecting from a bag one of four different tapes in a blinded fashion" |
| Allocation concealment (selection bias) | Low risk | "Randomization was by patients selecting from a bag one of four different tapes in a blinded fashion" |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear if outcome assessor of vital signs was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR, BP, and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Daub 1988.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety. |
| Protection from contamination? | Low risk | Intervention administered on an individual basis. |
Davis‐Rollans 1987.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "With the use of a Latin square design, the three musical selections (A, B, C) were randomly assigned to be presented to the patients in one of three different orders. Whether patients listened to either the music or the control period first was also randomly varied." Method of random sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Questionairre not fully validated; not extracted for review. Patients aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Automated recording of heart rate and respiratory rate, but data then determined from graphs by investigator ("the taped waveforms were off the scale because of a malfunction of the indicator needle"). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: RR. |
| Protection from contamination? | High risk | Cross‐over study. Duration of wash‐out period unclear. "The patients were continuously monitored for two 42‐minute periods in the same day." |
Diette 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The unit of assignment to intervention or control status was an entire day of FB procedures. The allocation schedule was generated by having a study member place equal numbers of intervention and control assignments in opaque envelopes. Each day at 4:00 PM, two other study members (not those who filled the envelopes) opened one of the envelopes to determine the next day’s assignment.’’ |
| Allocation concealment (selection bias) | Unclear risk | No information is given on concealment of allocation for patients. However “bronchoscopists could not know the assignment at the time that they scheduled their patients’’ |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | For this intervention, it was not possible to blind patients. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | The study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. Paper reports more than 10% of data for the outcome pain was missing (unclear exactly how much data was missing), and an imputation algorithm was used. Analyses were repeated with and without imputation, and the results were similar in both. Other outcomes had no more than 10% missing data; for these outcomes, missing values were substituted with the median (for ordinal and continuous outcomes) or mode (for nominal outcomes). |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Pain. |
| Protection from contamination? | Low risk | Interventions administered for an entire day. |
Domar 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were then randomized, according to a computer‐generated random‐numbers table" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Six subjects withdrew consent before randomization for the following reasons: one was late for a meeting, one did not want to be in a control group, one stated that reading the questions made her “feel depressed,” one changed her mind, one did not have enough time before being called in for the mammography, and one did not like the wording of the consent form. A seventh subject was not included in data analysis because she later reported that she did indeed have a current psychiatric illness, thus making her ineligible." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Donald 2000.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 20 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Pre‐stratification of patients was achieved by a simple nine‐question risk score [...] This was designed empirically by one of us (KP), and had face validity, but has not been subjected to any other validation. This provided a score from 0 (low risk) to 9 (high risk), and was used to stratify patients into low (0‐2), medium (3‐4) or high (>4) perceived risk of falling prior to randomization. Using randomized envelopes for each risk group, patients were assigned to a floor group (carpet or vinyl) and a physiotherapy group [...]." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Study was not blinded. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Linoleum floor‐ 1 patient died, 2 were transferred, 7 did not comply with repeated therapy‐related outcome measurements; Carpet floor‐ 5 died, 1 patient was transferred, 6 patients did not comply with repeated therapy‐related outcome measurements. There is not a problem with the flooring‐related outcomes (falls) in this study, but 40% missing data for therapy‐related outcomes (not included in review). |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: length of stay. |
| Protection from contamination? | High risk | "two patients allocated to carpet were nursed on vinyl becasue they required side‐rooms" |
Edge 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 6 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly placed in the hospital rooms by the hospital administration upon their admission to the hospital" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | High risk | Patients were recruited into the study on their final day of hospital stay (after they had been allocated to a room). |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Length of stay and drug requests objectively recorded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Eleven patients who were approached could not be used in the study. Three patients explained that they would just prefer not to participate. Two of the patients were considered legally colorblind. [...] One patient was extremely confused and could not understand the information being explained to him. [...] One patient felt uncomfortable with having the principal investigator examine his medical records [...]. One patient was considered extremely depressed by the nurse manager and was not approached to participate in the study and two patients could not speak English [...]. Lastly, one patient was extremely nervous and worried that the anxiety test would reveal that that she should have to stay in the hospital for an extended amount of time. It was therefore the researcher’s opinion that she altered her answers on the test to make it appear as though she had no anxiety in her life." It is unclear from which rooms withdrawals came. Data of remaining included patients appears complete. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, pain medication, and length of stay. |
| Protection from contamination? | Low risk | Patients assigned to individual rooms. |
Elliot 1994.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The study was a randomized, controlled trial." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Blood pressure was nurse‐assessed (not blinded). Heart rate was automated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and dropouts not described. Data presented for all included participants. "The study examined the anxiety of 56 patients. [...] Fifty‐six subjects completed the study." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Engelhart 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 15 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Cases of Invasive aspergillosis were recorded as suspected or proven. Staff would have been aware of intervention. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Staff would have been aware of presence or absence of portable air filtration units. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. It is unclear if outcome data are complete. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Intervention assigned to patient rooms. |
Ezzone 1998.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were assigned randomly." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Unclear who assessed vomiting. There was no blinding of healthcare personnel, patients, or researchers. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Three control group patients were dropped from the study because measurements were not taken at baseline or at a minimum of four of the other six data collection points. A fourth patient requested to learn relaxation therapy in addition to the music and therefore was not included. An additional two patients in the music intervention group were dropped from the study because they did not listen to music at the prescribed time intervals." (15% of participants withdrawn). Outcomes were obtained for >80% of included participants at 8 hours follow‐up but not at 16 hours follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Ferguson 2004.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomly assigned." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Vital signs measurement automated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR, BP, and RR. |
| Protection from contamination? | Unclear risk | Interventions administered on an individual basis. |
Frank 1992.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 28 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Assignment to rooms was not controlled or formally randomized but was based on scheduling rules and OR availability" |
| Allocation concealment (selection bias) | High risk | Rule‐based system. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Unclear level of blinding for assessment of outcomes. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear level of blinding for assessment of outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Participants assigned to rooms on individual basis. |
Gaberson 1991.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were assigned randomly to one of the three groups." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | WIthdrawals and drop‐outs not described. Data reported for all 15 included participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Gaberson 1995.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Each research assistant randomly assigned subjects by lottery to one of three groups" Method of randomisation not clearly described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, dropouts, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Ganidagli 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "they were assigned, using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | All patients wore headphones. "no hospital personnel were allowed to communicate with the patient. [...] scores were measured [...] by a blinded observer. To test observer blinding, the observer was asked whether he recognized the patient's group at any stage during the study period. [...] four patients were excluded because of failure in observer blinding after a technical problem." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Four patients (three in the music and one in the control group) were excluded from the study because of technical problems related to the music player." Missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Graham 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Random assignment [...]” Method of randomisation not described. |
| Allocation concealment (selection bias) | Low risk | “Random assignment was conducted by telephone to a separate data management centre. Patients and physicians were blinded to product allocation.” |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Blinding was not done for non‐fragrant 'placebo' group, but was done for the pure essential oil and fragrant placebo groups. Although patients were not told their group allocation, only 9% of the non‐fragrant placebo group believed they had received the essential oil, compared to 25% of the fragrant placebo and 24% of the pure essential oil (P = 0.006). Therefore the non‐fragrant 'placebo' was not a true placebo control. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | The study did not assess this outcome. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Withdraws or dropouts: “The reason for not receiving the full number of possible aromatherapy treatments included research assistant illness and absence, failure to complete the planned radiotherapy course, and withdraw from receiving aromatherapy. Of the 313 patients who were randomly assigned, 285, 286, and 295 completed baseline, HADS anxiety (HADSA), HADS depression (HADSD), and SPHERE questionnaire, respectively providing 91% to 94% questionnaire compliance for analysis of these scores. There was no significant difference in missing data by allocated arms.” |
| Selective reporting (reporting bias) | Unclear risk | There may be a risk of bias from selective outcome reporting, given that the results are presented as the proportion of participants whose score on an ordinal variable exceeded a cut‐off point (> 7); the data could instead have been reported as mean and SD. Normative data for the HAD suggest ≤7 is normal, 8 to 10 is borderline, and ≥11 may indicate clinically relevant anxiety (Millar 1995); this presents a rationale for the cut‐off. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Guo 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation via computer generated list. |
| Allocation concealment (selection bias) | High risk | Not done. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Automated outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 5 in the control group and 2 in the music group were excluded after moving to other room. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Harikumar 2006.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were allocated into two groups using computer‐generated random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Recovery room nurse who was "unaware of the group allocation" assessed time to recovery. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, dropouts, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiolytic medication |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Hayes 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomized using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | "Patients were unaware of their group assignment until they signed the consent form" Unclear if person recruiting patients had allocation concealment. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear if measurement of physiological outcomes was automated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Two hundred persons were enrolled and two were dropped due to incomplete data" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Heitz 1992.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The subjects were randomly placed into three groups." Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | BP and HR monitored via automated machine. RR measured via counting rate for 1 minute. "The nurse caring for the subject was partially blinded and only knew whether the subject had headphones, but did not know which subjects received music." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing data not described. "A total of 60 subjects were studied, 20 in each study group. An additional three patients consented but were excluded. Two patients were non‐complaint with the study protocol and one patient had extended surgery." |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR, BP, and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Holmes 2002.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | “The communal area of the unit was diffused [...], on alternate days [...].” |
| Allocation concealment (selection bias) | High risk | Not described‐ although CCT design means the sequence was predictable. |
| Blinding (performance bias and detection bias) Subjective outcomes | Low risk | Agitation measured by "an experienced independent blinded (using nose callipers prior to entry onto the ward) rater, unaware of the study design" |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | The study did not address this outcome. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Fifteen patients were recruited [...]. For each subject 10 total PAS scores were obtained." Results were obtained from all the patients that were recruited and therefore it is indicated that there were no dropouts or withdrawals. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | High risk | Cross‐over trial. |
Ikonomidou 2004.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were assigned randomly." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "The CDs were unmarked, and the content was unknown to the nurse starting the CD player. [...] All were told [...] that the investigators were to remain blinded as to which CD was used. [...] HR, noninvasive BP, mid RR were measured by an attending nurse who was unaware of the CD's content." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Five patients ‐ three from M group and two from C group ‐ were excluded from the calculations because of extended surgery or various technical problems on the ward" |
| Selective reporting (reporting bias) | High risk | Reports systolic blood pressure but not diastolic blood pressure. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Jacobson 1999.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects wishing to participate were assigned to 1 of the 3 treatment groups by a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "One subject withdrew after consenting, but before data collection." Group allocation or reason not described. Data described for all included participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Kasmar 1968.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 33 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The Ss were randomly assigned to the eight experimental conditions‐with the one constraint that the experimental room randomly assigned to one E‐S pair dictate the room to be used by the other E‐S pair. Within that constraint, time of ratings by Ss was randomized." ("E‐S pair" refers to psychiatrist‐participant pair). This has been interpreted to mean that although 'time of data collection' is reported as randomised, the variable 'room' was not randomly allocated, as it was dependent on the previous allocation. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Study was not blinded. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: mood. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Kliempt 1999.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "One of three numbered but unlabelled tapes was randomly assigned to the patient by computer‐generated random number table. The randomisation was stratified according to estimated length of stay (less than 2 days and more than this)." |
| Allocation concealment (selection bias) | Unclear risk | Unclear if the person recruiting patients was aware of the randomisation schedule. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Study did not address subjective outcomes |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Fentanyl requirements: "throughout the study, the anaesthetist remained unaware of the nature of the tape" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Eighty‐three of these gave their informed consent but seven later revoked this in the induction room" Description of reasons and group allocation not given. Data presented on all remaining included participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Koch 1998a.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomized into either control or a music group using a Table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | This study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | "Thus, the observer was not blinded to group assignment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Two patients were removed from the study secondary to the need for general anaesthesia and inadvertent departure from the study design." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Koch 1998b.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned." Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear if physiological measures were automated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and dropouts not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Korunka 1992.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States that participants were randomly assigned but does not say how the sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Low risk | Patients were unaware of which study group they were in. Intervention took place during surgery. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Clinical staff and experimenter were blinded to study groups. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Sämtliche Patientinnen (N = 163) konnten in die Auswertung aufgenommen werden. Von 23 Patientinnen liegt kein vollständiges Protokoll des Analgetikaverbrauchs in der Aufwachphase vor. Die Auswertung des Analgetikaverbrauchs bezieht sich daher auf eine Stichprobe von n = 140." All 163 patients were included in the analysis. However, there is incomplete data on analgesic consumption for 23 patients, so this outcome is based on 140 patients (unclear how many patients per group). |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions were administered on an individual basis. |
Kotwal 1998.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear how physiological outcomes were measured and if these were automated. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawals and dropouts not described. "Blood pressure and heart rate were recorded in all the patients in the music as well as without music group. Respiratory rate was recorded in 34 and 29 patients in the music and without music group respectively." (RR measured for < 80% of participants) |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Kwekkeboom 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was completed within categories of procedures [...] to ensure that the different types of procedures were distributed equally among the three study groups" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | This study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Data from two participants were excluded from analyses because experimental conditions had been contaminated. One participant assigned to the distraction group had an unusually long wait on the procedure table and requested music in addition to the distraction stimulus. One participant assigned to the control group was exposed to music when the surgeon requested that it be played while he was in the room" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Two participants were excluded due to "contamination" |
Lee 2002.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomly assigned by using computer generated numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "All assessors were blinded as to the group to which patients were assigned" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and dropouts not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Lee 2004a.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘‘Participants were randomly assigned using computer‐generated numbers into three groups’’ |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients could not be blinded to this intervention. Patients reported pain and satisfaction and controlled the level of sedation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "Group 1 patients wore the same Eyetrek system with earphones even though they had no music to listen to. As a result, the endoscopists did not know whether patients were in group 1 or group 2". Endoscopists were not blinded to patients in group 3 (patient‐controlled sedation alone). Unclear who assessed number of hypotensive episodes and oxygen desaturation. Recovery nurses assessed recovery time. "All recovery nurses were blinded as to the sedation group to which patients had been assigned". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ‘‘Eight patients were excluded after randomization: four patients had incomplete assessment forms and four patients did not receive proper PCS due to mechanical failure during the procedure.’’ Unclear from which groups participants were withdrawn, but reasons given. More than 80% of outcome data were obtained. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Lee 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were randomly assigned to either experiment or control groups by having a case nurse draw lots" |
| Allocation concealment (selection bias) | Low risk | "After the subjects agreed to take part in the study, the case nurse drew lots to assign subjects" |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients were aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "The case nurse also helped the subjects choose the preferred music from the researcher's collection so that researcher would be blind to the conditions of treatment. [...] The researcher then entered the patient's cubicle and collected data. The researcher was blind to the treatment conditions of both groups during the whole period of data collection." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and dropouts not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Lembo 1998.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 or Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomized" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Lepage 2001.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Method of recorded physiological outcomes unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals, dropouts, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR, BP, and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Lidwell 1971.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 17 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation not described (likely to be rule‐based, e.g. room availability). |
| Allocation concealment (selection bias) | High risk | Unlikely to have allocation concealment, as likely to have a rule‐based allocation system. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Level of blinding not described. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Level of blinding not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Infection. |
| Protection from contamination? | Unclear risk | Unclear if patients were moved between rooms. |
Lohner 1979.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 15 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly distributed" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Death ‐ objective outcome. Unclear blinding for bacterial infections and remission. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. It is unclear if patients with psychological problems were removed from the study or included on an ITT basis. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Infection. |
| Protection from contamination? | Low risk | Intervention administered on an individual basis. |
Lueders Bolwerk 1990.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment of subjects [...] using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "A total of 5 patients were transferred to other hospitals during the study, leaving 18 patients in the nonmusic group and 17 patients in the music group" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Unclear risk | It is possible that patients in the control group listened to their own music over the 3 day experiment, however it is unlikely that they would have been exposed to the structured intervention used for the study. |
Mandle 1990.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly divided" ‐method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Masuda 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Using a table of random numbers” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Automated physiological outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | “None of the patients refused any of the measurements.” |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
McRee 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Participants then were assigned to one of the four groups by drawing of lots.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Automated measurement of BP and HR. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on all major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Mennegazzi 1991.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Physiological data collected by (non‐blinded) nurses although methods of data collection are unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on all major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Migneault 2004.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned” Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Low risk | "After intubation, headphones were placed on the patient's ears in both groups. [...].The CD player was covered so that the investigator remained blinded to the study group." |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "After intubation, headphones were placed on the patient's ears in both groups. [...].The CD player was covered so that the investigator remained blinded to the study group." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Miller 1992.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Mullooly 1998.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | “only 11 patients were able to complete the rating scales on the first evening [...]. By the second postoperative evening, all study patients were able to complete the pain and anxiety ratings”. Data extracted for review on the 2nd post‐operative day. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Nilsson 2001.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A computer generated the randomisation list.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Low risk | "The patient, anaesthetists, surgeon and nurses were blinded to the tape selection." |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "The patient, anaesthetists, surgeon and nurses were blinded to the tape selection." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | “One patient was withdrawn from the study because of a technical error with the cassette player.” Missing data for 1 patient on day of surgery (1%), 5 patients on first day after surgery (6%), and 34 patients on second day after surgery (38%). 25% of data is missing for the mobilisation outcome. Missing data appears evenly distributed between groups, however, the reasons for missing data are not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Nilsson 2003a.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Computer generated randomisation” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: anxiety |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Nilsson 2003b.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A computer generated the randomization list.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "The anaesthesiologist, nurse anaesthetists, surgeon, physicians and nurses at the PACU were blinded to tape selection." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "One patient was withdrawn because of change of diagnosis intraoperatively, i.e. lipoma instead of inguinal hernia.” Otherwise, data appears to be complete. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Nilsson 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A computer generated the randomization list. A block randomisation was used [...] block size was 25.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "Sham and regular music CDs were thus indistinguishable [...] The anaesthesiologist, nurse anaesthetists, surgeon, physicians and nurses in the operating theatre and the PACU were blinded to the CD selection. All CD‐players were set to the same audio settings and were not audible to anyone in the immediate area." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on all major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Nowobilski 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Padmanabhan 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Subjects were then allocated to one of three groups according to a predetermined computer‐generated random sequence.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Two study groups were unaware if they were receiving music alone, or music with binaural beats. The control group (standard care) was not blinded. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | “Of the 108 subjects who participated in the study, four were excluded as they were unable to complete the process. One participant disliked the music provided (Audio Group) and three subjects (one from each group) did not complete the second STAI‐S questionnaire for logistical reasons.” |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Palakanis 1994.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "participants were randomly assigned to the study groups by the flip of a coin." |
| Allocation concealment (selection bias) | High risk | "After voluntary consent was obtained, the sample participants were randomly assigned to the study groups by the flip of a coin." |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Physiological outcomes were measure through automated assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Phumdoung 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomly assigned to groups using a computer minimization program." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Of the 110 women enrolled, the researcher withdrew those who were unable to complete the three posttests (n = 33; 23%). These women had false labor pain (n = 8), received oxytocin between enrollment and starting the study at 3 cm dilation (n = 3), had caesarean section (n = 3), or rapid progress of labor and delivery (n = 19, 13%). Only one woman in the control group chose to withdraw from the study, and the reason given was too much pain." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Schiemann 2002.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Schneider 2001.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomised". Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear whether physiological outcomes (BP and HR) were automated ‐ "non‐invasive system". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Sendelbach 2006.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "flip of a coin" |
| Allocation concealment (selection bias) | High risk | "flip of a coin" |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | HR was automated by bedside monitor. BP was measured using a cuff (not blind). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Smith 2001.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A biostatistician prepared a randomization list using a computer" |
| Allocation concealment (selection bias) | Low risk | "Only one member of the research team had access to this list of case numbers and randomization assignments, which was maintained in a locked filing cabinet. The nursing staff [...] presented the study to potential participants. At the time the patient agreed to participate in the study and the consent form was signed, the research associate called the registrar to obtain the patient's assigned case number and randomizaion group." |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Two patients, one from each group, were excluded from final analysis because of incomplete data". |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Unclear risk | "patients in both groups may have interacted with each other or nonstudy individuals in the waiting room before or after treatment" |
Smolen 2002.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | BP and HR measured using Critikon Model SNK9935 automated device. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Staricoff 2003f.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After the clinicians performed a clinical assessment of hospitalised patients, the list of nominated patients was sent to us one day before the concert; we randomised the names of patients, thus ensuring that no bias was introduced when dividing the patients into two groups". Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | This is one of a series of studies. At the beginning of the report it is stated that: "they were all done as controlled, blind or double‐blind studies" but it is unclear from the report who was blinded in this particular study. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Initially, this study aimed to recruit 30 to 40 patients. The complexity of the clinic, including unforeseen problems with staff resources in taking blood samples, and the nature of the disease that can unpredictably incapacitate some patients to move from the ward reduced the total number studied to 17 patients. In spite of some patients' willingness to come from the ward to the ground floor where the concert was taking place, some patients felt unwell before the event or might have fallen asleep. Some patients changed their minds about participating, even after having signed the consent form." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | "contol group formed by patients who remained on the ward at the time of the live performance" |
Tang 1993.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Automated assessment of outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Taylor 1998.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment was made equally to one of three groups by drawing slips of paper indicating the group to which the subject would be assigned." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals described: "one subject was eliminated from the study because she was unable to cooperate with data collection". It is unclear if there is any missing data. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Taylor‐Piliae 2002.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomly assigned to one of the three groups in the study, by drawing a slip of paper with group assignment" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | "Physiological measures [...] were taken manually for 1 min on all participants by the same research assistant." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Nine subjects (17%) withdrew resulting in incomplete data, as they were sent to CC before completion of data collection at either time‐one or time‐two. A total of 45 subjects [...] completed the study, results reported are from these subjects." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Triller 2006.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Prospective, randomized trail" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Method of data collection not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Tsuchiya 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer generated random numbers" |
| Allocation concealment (selection bias) | Low risk | Patients were blinded throughout study period. In a personal exchange with the study author (unpublished) they stated: "The person recruiting patients did not know the randomization." |
| Blinding (performance bias and detection bias) Subjective outcomes | Low risk | Patients were blinded to group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Automated measurement of physiological outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Five patients were excluded from the study due to changes in operation method, blood transfusion or insufficient epidural analgesia level" |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Twiss 2006.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomized [...] by picking a slip of paper from one of two boxes (one for women and one for men so that gender could be matched)" |
| Allocation concealment (selection bias) | Low risk | "After signing informed consent, participants were randomized into control and experimental groups by picking a slip of paper". Informed consent was taken prior to randomisation. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear if intubation time was assessed blind or was automated. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "There were 44 participants in the control group and 42 in the experimental group. [...]. Participants for this study continued to be recruited as others dropped out until a total of 60 participants completed the study. [...]. The elimination of 26 participants because of unforeseen complications during and after surgery is a limitation in this study and threat to the internal validity of results. These complications required extended intubation periods and eliminated participants from the normal weaning protocol or were unable to complete the state anxiety measure on the third postoperative day." 30% of participants were withdrawn (14 from the music group, and 12 from the control group). |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Vaaler 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 33 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The patient allocation [...] followed a predetermined rule: they were admitted to the wing with fewest patients, or with even numbers to the wing that did not receive the previous admittance." |
| Allocation concealment (selection bias) | High risk | Rule‐based system. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Blinding was not possible. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Blinding was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "One patient was excluded (senile dementia). [...]. Missing items on the PANSS ratings were evenly distributed in the groups with an average of 18.2% (14.3 ‐ 35.7%) for first and 7.2% (0 ‐ 20.1%) for the second and third rating. There were no missing items in the other rating scales." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Unclear risk | Unclear if patients were free to move between wings of the ward. |
Voss 2004.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned [...] using sealed envelopes with a varied block size prepared by the statistician" |
| Allocation concealment (selection bias) | Low risk | "using sealed envelopes with a varied block size [...] The investigator was blind to the block size and could not anticipate group assignment" |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Although all patients who were enrolled completed the study, one participant in the music group was identified as an outliner for extreme pain and mild respiratory distress and was dropped from the analyses" |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Walch 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 25 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patients were held in the PACU and then discharged when a room on the unit became available. The unit director followed normal hospital protocol and assigned patients to either side of the unit depending on room availability." |
| Allocation concealment (selection bias) | High risk | Assignment used rule‐based system (room availability). |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | "Patients were blind to the study's intervention as well as whether their room was located on the bright or dim side of the unit." It is unclear how blinding was acheived when: "Beginning on the afternoon of postoperative day 1 and continuing throughout hospitalization, light intensity (lux) was measured twice daily in the rooms of all study participants at approximately 9:30am and 3:30pm. Before measurement, the door of the room was closed, all artificial sources of light extinguished, and the window blinds were opened to permit maximum sunlight to enter the room." |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | "A registered nurse, who was blind to the patient group assignment, abstracted the daily use of all opiod and opiod‐equivalent medications from the patient's medical records. [...] A hospital administrator, who was blind to patient group assignment, determined the total pain medication cost for each study patient from the hospital billing system." Unclear how blinding was acheived. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "The study used the intent‐to‐treat model and no patients were dropped after signing the consent. [...] no missing value procedures were used." Outcomes were obtained for >80% of participants on the day of sugery and post‐operative days 1 and 2, but not post‐operative days 3‐5 (participants were discharged). |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Rooms were assigned on an individual basis. |
Wang 2002.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomly assigned" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Automated measurement of outcomes (HR, skin conductance). Method of measuring BP unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
White 1992.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly distributed" ‐ Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | HR and RR measured by auscultation for 30 seconds (not blind). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
White 1999.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Assigned randomly" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Measured by investigator (not blind) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Whyte 1969.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 15 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patients (including emergency admissions) were received into both the open‐plan wards on Tuesday, Thursday, Saturday and on alternate Sundays" |
| Allocation concealment (selection bias) | High risk | Rule‐based allocation system. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear who assessed infections and level of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Participants assigned to rooms. |
Wilber 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 22 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "a random number table" |
| Allocation concealment (selection bias) | Low risk | "Research staff not otherwise involved in the study generated a random‐number table and made sealed enrollment packets using these numbers" |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | "Patients were not told that the study was intended to primarily evaluate the pain associated with the gurney or chair". However, the study nurse who asked patients about their pain was not blinded to the study, and the patients were aware if they were on a gurney or a chair. Also: "The study nurse specifically instructed patients to rate the pain associated with the gurney, rather than pain from other sources" |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Four were discharged (two in each group) before the primary outcome could be measured [...]. Twenty‐four enrolled patients were discharged before t2 [...]." Outcomes were obtained for more than 80% of participants at time 1 but not at time 2. Outcome for review extracted at time 1. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | High risk | "Six patients in the chair group did not receive the allocated intervention, as they refused to get in the chair, and two patients in the gurney group demanded the chair." These patients were analysed on an intention‐to‐treat basis. |
Willmott 1986.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 20 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Study was not blinded. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Gait speed, and step length. |
| Protection from contamination? | High risk | Cross‐over trial. |
Winter 1994.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer generated random groupings" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Unclear if measurement of physiological outcomes was automated. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Twelve subjects in the latter [control] group did not complete the second questionnaire for a variety of reasons: 6 refused to complete the second questionnaire, 4 were taken to the Operating Room before the questionnaire could be completed, and 2 administered midazolam while in the Surgical Holding Area." (19.4% withdrawn, all from the control group). |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Wong 2001.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization [...] by drawing lots" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | RR measured via observation (not blind). BP measure via bedside cardiac monitor (automated). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | High risk | Cross‐over design. |
Yang 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Yung 2003.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned". Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | BP and HR measured with automated system. RR measured via observation (not blind). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Zhang 2005.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer‐generated randomisation list" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | Unclear risk | Level of alertness was scored on the OAA/S with which the observer was unaware as to the significance of the score but not blinded to group allocation. It is unclear as to whether patients were blinded to group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | It is unclear as to the level of blinding in this study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Zimmerman 1988.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants in the control group were told the study was for gaining information on new admissions, so were unaware of the true purpose of the study. However, participants were not blind to whether they received music, white noise, or standard care. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Physiological data obtained by automated measurements. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
Zimmerman 1989.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) Subjective outcomes | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
ASA = American Society of Anesthesiologists; BP = blood pressure; bpm = beats per minute; CC = Cardiac catheterization; CD = compact disc; EGD = Esophagogastroduodenoscopy; FB = Flexible Bronchoscopy; FS = Flexible Sigmoidoscopy; HEPA = High energy particular air; HR = Heart rate; ICU = intensive care unit; IV = intravenous; MI = Myocardial Infarction; NRS = Numerical Rating Scale; OAA/S = Observer's assessment of alertness/sedation; OR = Operating Room; PACU = Post Anaesthesia Care Unit; PCS = Patient controlled sedation; POMS = Profile of Mood States; RCT = randomised controlled trial; RR = respiration rate; SD = Standard deviation; SE = Standard Error; STAI = State Trait Anxiety Inventory; UK = United Kingdom; USA = United States of America; VAS = visual analogue scale; VRS = Verbal rating scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aaron 1996 | No intervention‐ observational study |
| Abramson 1966 | Summary paper, no data presented |
| Alberti 2001 | Study design |
| Allen 1989 | Intervention |
| Alvermann 1979 | Descriptive article |
| Anderson 1982 | Pediatric hospital |
| Anderson 2004 | Intervention |
| Ansari 1969 | Study design |
| Anthony Williams | Descriptive article |
| Armstrong 1984 | Review article |
| Augustin 1996 | Music CCT ‐ Post‐hoc exclusion |
| Azer 1971 | Setting |
| Baird 1969 | Outcomes |
| Baker 1987 | No intervention |
| Baker 1992 | No intervention |
| Baker 1993a | No intervention |
| Baker 1993b | Review article |
| Baldwin 1985 | Not health‐related outcomes; policy changes |
| Bame 1993 | Study design |
| Bame 1995 | Study design |
| Bampton 1997 | Validity of outcomes |
| Barker 2005 | Descriptive article |
| Barlas 2001 | Not health‐related outcome; query validity. |
| Beauchemin 1996 | Retrospective study |
| Beauchemin 1998a | Duplicate of Beauchemin 1998b |
| Beauchemin 1998b | Retrospective study |
| Beck 1991 | Intervention music therapy at home |
| Becker 1980 | Outcome measure not validated |
| Beldon 2002 | Other systematic review in this area (Cullum 2004) |
| Benedetti 2001 | Retrospective study |
| Berg 2001 | Participants (students) |
| Berlet 1979 | No intervention |
| Bettschen‐Steiner | Overview‐ not a study |
| Biley 1994 | Review article |
| Binek 2003 | Music CCT ‐ Post‐hoc exclusion |
| Birdsong 1990 | No intervention |
| Bodey 1969 | Study design (no control) |
| Bodey 1971 | Study design (matched pairs) |
| Boeke 1988 | Validity of outcomes |
| Bonke 1982 | Outcomes not reported for relevant groups; data collection methods unclear. |
| Bonny 1983 | Could not obtain article‐ not assessed for inclusion |
| Bower 1995 | Qualitative report |
| Bozcuk 2006 | Study design |
| Breslow 1993 | Descriptive article |
| Browning 2001 | Intervention provided outside of hospital |
| Brunges 2003 | Music CCT ‐ Post‐hoc exclusion |
| Buemi 1995 | Study design; outcomes |
| Burke 1977 | Participants |
| Burns 2000a | Study design |
| Burns 2000b | Study design |
| Burns 2002 | Study design |
| Butler 1993 | Setting |
| Byers 1997 | Study design |
| Bykov 2003a | Setting and population |
| Bykov 2003b | Setting and population |
| Cai 2001a | Intervention |
| Cai 2001b | Intervention |
| Carpman 1983 | Study design |
| Castellani 1968 | Not a study |
| Ceccio 1984 | Intervention excluded‐ relaxation technique |
| Chaudhury 2003 | Cross‐sectional survey and qualitative interviews |
| Cheek 1971 | Qualitative |
| Chikamori 2004 | Intervention‐ interactive music therapy |
| Choctaw 1984 | Policy confounding (sterile versus clean attire). |
| Chow 2005 | Study design (computer modelling) |
| Christenfeld 1989 | CBA‐ Control sites and 'before' sites not clearly defined |
| Cirina 1994 | Review article |
| Clair 1994 | Questionable validity of outcome, relevant data not presented |
| Clair 2006 | Setting |
| Clark 1998 | Setting |
| Connell 1996 | Review article |
| Cook 1986 | Review article |
| Cooper 1989 | Qualitative |
| Cooper 1991 | Qualitative |
| Cooper 1998 | Included in Cochrane review by Cullum 2004 |
| Coulson 1997 | Setting |
| Counsell 2000 | Policy confound |
| Courtright 1990 | Outcome measure |
| Covinsky 1998 | Policy confound |
| Cunningham 1997 | Outcome measures |
| Davidson 1971 | Study design |
| Davies 1980 | Study design |
| Davis 1992 | Setting |
| De Jong 1972 | Participants |
| De l'Etoile 2002 | Intervention |
| Dekker 1994 | Confounding |
| Demling 1978 | Patients‐ mix of adults and children. Data inseparable. |
| Denney 1997 | Setting |
| Dennis 1988 | Descriptive article |
| DeSchriver 1990 | Setting not hospital |
| Devlin 1992 | Study design |
| Dickinson 1995 | Setting |
| Diffey 1988 | Study design |
| Dolce 1985 | Retrospective study |
| Donchin 2002 | Review article |
| Dracup 1988 | Review article |
| Dritsas 2004 | Intervention not well‐defined |
| Dubbs 2003 | Not a research study |
| Dubois 1995 | Music CCT ‐ Post‐hoc exclusion |
| Duckworth 1988 | Policy changes |
| Durham 1986 | Intervention provided during education programme |
| Dzhuraeva 1989 | Music CCT ‐ Post‐hoc exclusion |
| Egger 1981 | Study design |
| Eisenman 1995 | Study design |
| Elmståhl 1997 | Not hospital setting |
| Escher 1993 | Music therapist confound; group differences in timing of data collection |
| Evans 1994 | Music CCT ‐ Post‐hoc exclusion |
| Falk 1973 | No intervention |
| Fauerbach 2002 | Intervention entailed coaching patients |
| Ferguson 1997 | Setting not hospital |
| Finkelstein 1971 | Intervention interactive |
| Finlay 1993 | Qualitative |
| Fox 1986 | Study design |
| Frandsen 1990 | Editorial |
| Frank 1985 | Study design |
| Fratianne 2001 | Intervention interactive music therapy |
| Freeman 1987 | Study design |
| Freireich 1975 | Preliminary report of Rodriguez 1978; policy confound |
| Friberg 1999 | Sham operations |
| Friberg 2003 | One patient health‐related outcome reported (surgical site infections), but not enough detail on how it was assessed or if it was noted on an 'ad hoc' basis. |
| Frid 1981 | Interventions not suitable for inclusion |
| Friedman 1992 | Study design |
| Gabor 2003 | No intervention in patients |
| Gaffney 1986 | Setting; study design |
| Gast 1989 | Study design |
| Girard 2004 | Editorial |
| Good 1978 | Qualitative |
| Good 1995 | Intervention group provided 20 mins coaching |
| Good 1998 | Intervention group provided reinforncement and training‐ bias |
| Good 1999 | Intervention group provided coaching on relaxing |
| Good 2001 | Secondary analysis of Good 1999 |
| Good 2002 | Secondary analysis of previous study. |
| Good 2005 | Duplicate study‐ secondary analysis of Good 1999. |
| Gray 2000 | Duplicate of study included in Cochrane review by Cullum 2004 |
| Green 1994 | News article |
| Greenberg 1992 | Descriptive report |
| Grindley 1996 | Other systematic review in this area (Cullum 2004) |
| Grumet 1994 | Discussion article |
| Guillemin 2000 | Qualitative |
| Gulledge 1981 | Not research |
| Gundermann 1974 | Outcomes |
| Gurr 1997 | Descriptive case study |
| Guzzetta 1989 | Relaxation (psychological) technique used in music group |
| Guétin 2005 | Music CCT ‐ Post‐hoc exclusion |
| Götell 2002 | Qualitative, setting |
| Götell 2003 | Qualitative |
| Haddock 1994 | Study design |
| Hagerman 2005 | Study design |
| Hahn 1995 | Study design |
| Hamel 2001 | Music CCT ‐ Post‐hoc exclusion |
| Hanger 1999 | Study design |
| Harmankaya 2002 | Study design |
| Harris 1992 | Outcomes |
| Harrison 1989 | Study design |
| Harvey 1998 | Review article |
| Harwood 1992 | Study design |
| Hashiguchi 2005 | Study design |
| Haslam 1970 | Study design |
| Haun 2001 | Music CCT ‐ Post‐hoc exclusion |
| Haythornthwaite 2001 | Intervention‐ taught techniques |
| Heiser 1997 | Music CCT ‐ Post‐hoc exclusion |
| Helmes 2006 | Outcomes |
| Hendrich 2004 | Study design |
| Herr 2003 | Study design and outcomes |
| Hewawasam 1996 | Study design |
| Hilton 1976 | Study design |
| Hilton 1985 | No intervention |
| Hinojosa 1995 | Not a study |
| Hoffman 2000 | Intervention interactive virtual reality |
| Hoffman 2001 | Intervention excluded‐ interactive distraction |
| Holahan 1972 | Experimental environment (not clinical situation), policy change |
| Holahan 1973 | Outcomes |
| Holahan 1976 | Outcomes |
| Holden 1992 | Intervention‐ patient education video |
| Homicki 2004 | Descriptive article |
| Hooper 1992 | Case study |
| Hsu 1998 | Intervention not well defined |
| Hudson 1995 | Study design |
| Hudson 1996 | Outcomes |
| Huffman 1994 | Intervention not well defined |
| Hussian 1987 | Study design |
| Hyde 1989 | Qualitative; setting |
| Ingham 1997 | Setting |
| Itai 2000 | Study design |
| Ittelson 1970 | Study design |
| Jacobs 1974 | Participants |
| Janelli 1997 | Policy confound (restraints use) |
| Janelli 1998 | Policy confound (restraints use) |
| Janelli 2000 | Policy confound (restraints use) |
| Janelli 2002 | Outcome measure |
| Janelli 2004 | Outcome measure |
| Janiszewski 1980 | Study design |
| Janssen 2000 | Outcome measure |
| Janssen 2001 | Participants |
| Jarvis 1979 | Conference abstract‐ not enough information |
| Jastremski 1998 | Literature review |
| Jonas 1988 | Study design |
| Kaempf 1989 | Music CCT ‐ Post‐hoc exclusion |
| Kaiming 1997 | Inadequate description of intervention |
| Kaldenberg 1999 | Study design |
| Kam 1994 | Review article |
| Kane 2004 | Data unsuitable for cross‐over study |
| Karro 2005 | Design; Outcomes |
| Kartman 1984 | Descriptive article |
| Keep 1980 | Study design |
| Kibbler 1998 | Study design; confounding |
| Kim 1997 | Not health‐related outcome |
| Kim 2005 | Setting not hospital |
| Kimata 2003 | Setting |
| Kirkpatrick 1998 | Commentary |
| Knobel 1985 | Descriptive article |
| Kolanowski 1990 | Setting |
| Kopp 1991 | Intervention not well defined |
| Kovach 1997 | Setting |
| Kulik 1996 | Intervention |
| Kumar 1992 | Validity of outcomes |
| Kwon 2006 | Study design‐ selection of participants by matching, different wards assigned to different conditions. |
| Lai 1999 | Unable to clarify discrepancies in data with author |
| Lai 2001 | Study design |
| Lai 2005 | Setting |
| Lai 2006 | Setting; Duplicate |
| Laitinen 1994 | Intervention |
| Lamont 1975 | No intervention |
| Lan‐Ping 2000 | Policy confound |
| Larsson 1991 | Study design |
| Laurion 2003 | Intervention began before admission |
| Lawson 2000 | Study design (same study as Lawson 2003) |
| Lawson 2002 | Study design (same study as Lawson 2003) |
| Lawson 2003 | Study design (before‐and‐after no contemporaneous control) |
| Lawton 1970 | Study design |
| Lazaroff 2000 | Unclear methods and data |
| Leather 2003 | Study design |
| Lee 2004b | Music CCT ‐ Post‐hoc exclusion |
| Legg 1970 | Not patient outcomes; test scenario |
| Lehrner 2000 | Setting |
| Leigh 1972 | Study design |
| Levin 1987 | Intervention relaxation training |
| Levine 1973 | Policy confounding |
| Lewis 1999 | Study 1: inappropriate control; Study 2: intervention |
| Leão 2004 | Study design |
| Lidwell 1966 | Study design |
| Lidwell 1969 | Test scenario, not patient outcomes |
| Lidwell 1975 | Study design |
| Lidwell 1982 | Some relevant subgroups within study however cannot separate data (number of re‐operations in each subgroup). Additionally, there are discrepancies in reporting with Lidwell 1984 with 185 patients switching subgroups. |
| Lidwell 1984 | Same study as Lidwell 1982. Non‐transparant reporting of findings‐ data not usable. Discrepancies between Lidwell 1982 and Lidwell 1984. |
| Liebowitz 1979 | Study design |
| Litch 2006 | Narrative article |
| Locsin 1979 | Intervention not well described (CCT) |
| Locsin 1981 | Intervention not well described (CCT) |
| Locsin 1988 | Could not obtain article, not assessed for inclusion |
| Lomas 1987 | Outcomes |
| Louis 2002 | Setting |
| Lowbury 1971 | Population‐ age |
| Lowbury 1978 | Preliminary report of Lidwell 1982/Lidwell 1984 |
| Martin 1998 | Policy confound |
| Martin 1999 | Inadequate information provided (Ulrich study) |
| May 1984 | Study design |
| Mayer 1991 | Study design‐ inappropriate data |
| McCaffrey 2004 | Outcomes not validated/reliable |
| McConnell 2005 | Study design; Intervention unclear |
| McGonagle 2002 | Study design |
| McKendrick 1976 | Study design |
| McLaughlin 1976 | Qualitative study |
| McNaughton 2005 | Study design |
| Mellgren 1967 | Study design |
| Mellor 2001 | Commentary |
| Metera 1975a | Music CCT ‐ Post‐hoc exclusion |
| Metera 1975b | Music CCT ‐ Post‐hoc exclusion |
| Meyer 1994 | No intervention |
| Middelboe 2001 | Confounding |
| Mihara 2005 | Lack of information |
| Miller 1998 | Participants; study design |
| Miluk‐Kolasa 1994 | Confounding |
| Miluk‐Kolasa 1996 | Intervention not well described |
| Miluk‐Kolasa 2002 | Intervention not well described |
| Mok 2003 | Music CCT ‐ Post‐hoc exclusion |
| Moore 1998 | Policy change |
| Morgan 1998 | Setting |
| Morris 1970 | Study design |
| Morsley 1999 | Commentary |
| Moss 1987 | Music CCT ‐ Post‐hoc exclusion |
| Moss 1988 | Intervention not well described, no data presented (CCT) |
| Mulin 1997 | Study design |
| Murrock 2002 | Setting and outcomes |
| Namazi 1989 | Study design |
| Nauseef 1981 | Policy changes (confounding) |
| Nelson Negley 1990 | Setting; outcomes |
| Nixon 2006 | Other systematic review in this area (Cullum 2004) |
| Norberg 1986 | Study design |
| Noskin 2001 | Literature review |
| Notelovitz 1978 | Study design |
| Oberle 1990 | Study design |
| Okada 1986 | Not health‐related outcomes |
| Okamoto 2002 | Study design |
| Olsen 1984 | Outcomes; unclear study design |
| Oyama 2000 | Intervention interactive with patient |
| Palmer 1998 | Policy confound |
| Palmer 1999 | Outcomes data not provided |
| Parker 1965 | Patients‐ 38% <10 years old |
| Passini 1998 | No intervention; comparison with healthy controls |
| Passweg 1998 | Study design |
| Pattison 1996 | Confounding staffing differences |
| Petersen 1987 | Policy (decontamination) changes |
| Peterson 1977 | Outcomes (validity and relevance) |
| Pimentel‐Souza 1996 | Study design (cross‐sectional, no intervention/control) |
| Plourde 1997 | Intervention |
| Prensner 2001 | Study design |
| Preston 1981 | Study design (not enough data points to be included as ITS) |
| Pring 1998 | Other systematic review in this area (Cullum 2004) |
| Pruyn 1998 | Validity of outcomes |
| Qian 2006 | Mock setting |
| Rabin 1981 | Descriptive article |
| Ragneskog 1996 | Setting and outcomes |
| Rakshy 1997 | Inappropriate methods and analysis |
| Redd 1994 | Aromas administered via nasal cannula, judged to be too invasive to constitute an 'environmental' intervention. |
| Ribas‐Mundo 1981 | Intervention (non‐environmental changes) |
| Rice 1980 | Outcomes |
| Rodriguez 1978 | Policy confounding |
| Rosenthal 1985 | Intervention |
| Routhieaux 1997 | Not patient outcomes |
| Rubin 1998 | Literature review |
| Rudy 1995 | Intervention (care delivery systems) |
| Salmore 2000 | Intervention‐ relaxation tape |
| Satlin 1992 | Intervention |
| Satoh 1983 | Intervention not well described |
| Schimpff 1975 | Policy confounding |
| Schneider 2003 | Intervention excluded as interactive |
| Schneider 2004 | Intervention excluded as interactive |
| Schofield 2000 | Intervention |
| Schott 1999 | Policy change |
| Schuhl 1985 | Data collection tool not validated |
| Schuster 1985 | Music CCT ‐ Post‐hoc exclusion |
| Sheperd 2001 | Study design |
| Sherertz 1985 | Intervention |
| Sherertz 1987 | Study design |
| Sherratt 2004 | Outcomes not validated |
| Shertzer 2001 | Policy change‐ staff asked to remain quiet on intervention days |
| Shirani 1986 | Study design |
| Shooter 1963 | Policy change |
| Sidorenko 2000a | Intervention as treatment |
| Sidorenko 2000b | Compilation of studies, insufficient detail presented |
| Siedliecki 2006 | Setting |
| Siegman‐Igra 1986 | Study design (no control) |
| Silini 2002 | Study design |
| Singer 2000 | Population, < 90% over 18 years old. |
| Skoutelis 1993 | Study design |
| Smith 1974 | Follow‐up to Smylie 1971 and Davidson 1971; study design |
| Smylie 1971 | Study design |
| Sommer 1958 | Study design |
| Spintge 2000 | Overview‐ insufficient detail |
| Spitzer 2005 | Music not well described; cross‐over trial with and without vibration. |
| Stahler 1984 | Study design (gender differences) |
| Standley 1992 | Setting not hospital |
| Staricoff 2001 | Study design |
| Staricoff 2003a | Study design (block periods) |
| Staricoff 2003b | Music CCT ‐ Post‐hoc exclusion |
| Staricoff 2003c | Study design |
| Staricoff 2003d | Study design |
| Staricoff 2003e | Study design |
| Steelman 1990 | Intervention not well defined |
| Steer 1975 | Confounding |
| Steffes 1985 | Staffing confound |
| Steingold 1963 | Study design |
| Stermer 1998 | Outcomes not validated |
| Stone 1989 | Study design |
| Strauser 1997 | Setting not hospital |
| Swan 2003 | Study design |
| Swinford 1987 | Intervention psychogical |
| Szeto 1999 | Music CCT ‐ Post‐hoc exclusion |
| Sármány 2006 | Patients allocated retrospectively to music or control, depending on whether or not they had noticed/heard any music. |
| Tanabe 2001 | Music CCT ‐ Post‐hoc exclusion |
| Tang 1997 | Intervention not well described |
| Tate 1997 | Intervention; outcome not validated |
| Thompson 2002 | Study design |
| Thorgaard 2004 | Outcomes not validated |
| Thorgaard 2005 | Study design |
| Thorne 1963 | Qualitative evaluation |
| Tideiksaar 1993 | Intervention |
| Tierney 1978 | Study design; outcomes |
| Tse 2003 | Setting not in hospital |
| Tse 2005 | Music CCT ‐ Post‐hoc exclusion |
| Tyerman 1980 | Description of intervention/control unclear |
| Uedo 2004 | Insufficient info (intervention and data) |
| Ulrich 1984 | Study design‐ retrospective matched pairs |
| Ulrich 1993b | Conference abstract‐ unable to obtain further details from author |
| Ulrich 2003 | Setting not a hospital |
| Updike 1987 | Study design |
| Updike 1990 | Study design |
| Van Someren 1997 | Setting; Study design |
| Veitch 2001 | Literature review |
| Verderber 1983 | Study design, validity of outcomes |
| Vietri 2004 | Study design |
| Vollert 2002 | Test not clinical situation, healthy controls. |
| Vollert 2003 | Setting not a hospital |
| Walker 1989 | Qualitative interviews |
| Walsh 1989 | Policy changes |
| Walther‐Larsen 1988 | Intervention not well defined, query outcomes validity |
| Watanabe 1997 | Not health‐related outcomes; conversation confounding |
| Weber 1996 | Overview article |
| Weisman 1981 | Setting |
| Whitehead 1984 | Study design |
| Whyte 1968 | Not patient outcomes |
| Wikström 1992 | Setting not a hospital |
| Wikström 1993 | Setting not a hospital |
| Wilkins 1988 | Study design |
| Williams 1962 | Study design; policy changes |
| Williams 1969 | Study design‐ no control |
| Williamson 1992 | Music CCT ‐ Post‐hoc exclusion |
| Wilson 1972 | Study design‐ retrospective |
| Wilson 1983 | Qualitative; participants |
| Winkel 1986 | Descriptive case studies |
| Wint 2002 | Participants not adults |
| Wolowicka 1989 | Music CCT ‐ Post‐hoc exclusion |
| Wood 1977 | validity of outcomes |
| Wright 1993 | Participants not patients |
| Wyon 1968 | Staff outcomes |
| Yamanaka 2003 | Music CCT ‐ Post‐hoc exclusion |
| Yates 1973 | Policy confounding |
| Yilmaz 2003 | Inappropriate control‐ drugs |
| Yinnon 1992 | Study design |
| Yung 2002 | Music CCT ‐ Post‐hoc exclusion |
| Zhong 2005 | Duplicate study (Lee 2005) |
Characteristics of studies awaiting assessment [ordered by study ID]
Allred 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Anon 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Arai 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Berbel 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Boehm 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Braden 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Bradt 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Review is being assessed as part of review update |
Brenier‐Pinchart 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Bringman 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Chan 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Chlan 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Cooke 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Danhauer 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Dennis 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Dijkstra 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Dube 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Eagle 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Easter 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Ebneshahidi 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
El‐Hassan 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Escombe 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Ferrer 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Fredriksson 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Freysteinson 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Gardner 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Gonzalez 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Good 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Good 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Gross 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Han 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Hoya 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Huang 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Hur 2005.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Published in Korean; we have not been able to assess this report yet due to translation difficulties. |
Jaber 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Jimbo 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Joanna 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Kang 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Kim 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Knight 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Koo 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Lai 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Laopaiboon 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Review is being assessed as part of review update |
le Roux 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Leardi 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Lechtzin 2010.
| Methods | |
| Participants | All patients 18 years and older with a diagnosis of cancer undergoing a BMBx in the Johns Hopkins Oncology Center will be screened for enrolment in the study. Based on power calculation, it was planned to enrol 40 patients in each group (total n = 120) to compensate for study withdrawal and missing data. |
| Interventions | All participants will have pain managed by the physicians responsible for their clinical care as dictated by those physicians. Participants assigned to Nature Sights and Sounds will have Bedscapes fabric panels depicting a scene of a mountain stream placed by the procedure table at a location where it will be visible throughout the procedure. An accompanying audiotape of complementary nature sounds will be played on portable tape players through headphones or speakers. They will be instructed to listen to the tape and look at the nature scene as frequently and for as long as they desire. The standard care group will have pain managed according to current oncology centre protocols but will not be allowed to use the distraction interventions. The Music/Photo group will be played a tape of typical city sounds and will have a poster of a city skyline placed by the procedure table. The city skyline poster will be similar in size to the Bedscapes mural. The skyline image is a daytime photograph without water, trees or other nature elements. The participants will be asked to listen to the music and view the picture during the procedure. |
| Outcomes | Pain; Profile of Mood States; Brief Symptom Index 18; Salivary cortisol; HR; BP; RR; overall satisfaction with care. Adverse events will be monitored. |
| Notes | Details obtained from ClinicalTrials.gov Final report not yet obtained. |
Lin 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Liu 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Maeyama 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Meeuse 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Moradipanah 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Nikolajsen 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Nilsson 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Nilsson 2009a.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Nilsson 2009b.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Park 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Persichetti 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Phipps 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Podder 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Pothoulaki 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Reza 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Richardson 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Sand‐Jecklin 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Shabanloei 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Siedlecki 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Simcock 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Son 2006.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Published in Korean; we have not been able to assess this report yet due to translation difficulties. |
Szmuk 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
Wu 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
HR: heart rate; BP: blood pressure; RR: respiration rate
Characteristics of ongoing studies [ordered by study ID]
NCT00817869.
| Trial name or title | The HIP‐HOP Flooring Study: Helping Injury Prevention in Hospitalised Older People |
| Methods | Pilot cluster randomised controlled trial. |
| Participants | 8 elderly care wards in England (each ward has one bay, the 'study area', included in the study of 4 to 8 beds in size). |
| Interventions | 8.3mm thick floor covering (Omnisports EXCEL) versus standard floor covering |
| Outcomes | Fall‐related injuries; Falls; Adverse events; Cost‐effectiveness; User views; Slip resistance and shock absorbency of floor. |
| Starting date | April 2010 |
| Contact information | amy.drahota@port.ac.uk |
| Notes |
Differences between protocol and review
Our protocol stated that we would include non‐randomised studies, due to feasibility issues often raised when researching the environment. Following review by our contact editor, the decision was made to remove 24 non‐randomised CCTs on music. Initially, these studies were included and summarised separately to the 85 included RCTs on music. In general, the CCTs reported similar findings to the RCTs however the quality of the studies was lower. The removal of these studies did not alter the conclusions of the review. Since RCTs are generally feasible in the study of music interventions, and there are so many RCTs exploring the use of music in hospital, it was felt that the CCTs were not providing any further valuable information to the review, which has sought to summarise the best available evidence.
We initially planned to assess heterogeneity through using the I2 statistic with a cut‐off point of 50% (i.e. > 50% would be considered heterogeneous). We have since revised this approach (to that specified in the data analysis section of the review) in alignment with revisions to the Cochrane Handbook for Systematic Reviews of Interventions (version 5; Higgins 2008), in which the use of cut‐off points are no longer recommended. Further to the release of the new Handbook (Higgins 2008), we have incorporated a 'Risk of bias' assessment utilising the new 'Risk of bias' tool.
In our exploration of heterogeneity for studies on music, we conducted subgroup analyses based on whether patients were offered a choice of music or given set pieces. These analyses were post‐hoc as they were not planned for in the protocol (although in our protocol we did specify that we would set out to find interventions which provided patient controls over the environment‐ such as access to lighting and ventilation controls). We felt that it would be useful to explore these variations in the way the music interventions were administered since patient choice and providing patients with a sense of control is often advocated as beneficial.
Contributions of authors
AD developed the review content, wrote protocol and developed the initial search strategy. AD conducted the initial searching accept for EMBASE (which was conducted by the Trials Search Co‐ordinator, Jessie McGowan), screened citations, scrutinised abstracts to identify potential papers, obtained hard copies of potential papers, applied inclusion/exclusion criteria to identified papers, extracted data, and wrote final review manuscript.
RS, DW and TD developed review content and contributed to writing the protocol. They screened citations, scrutinised abstracts to identify potential papers, applied inclusion/exclusion criteria to identified papers, extracted data, contributed to the writing of the final review manuscript and provided methodological advice throughout the process.
HM and DG applied inclusion/exclusion criteria, extracted data, and contributed to the final review manuscript.
BH advised on data analysis techniques and reviewed the data analysis section of the protocol. BH provided statistical support and advice throughout the review.
All reviewers read and approved the final review manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
Dunhill Medical Trust. Registered Charity No. 294286, UK.
Declarations of interest
The review authors (AD, DW, TD, BH) are involved in the conduct of the ongoing study (NCT00817869) referred to in the discussion.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Allen 2001 {published data only}
- Allen K, Golden LH, Izzo JL, Ching MI, Forrest A, Niles CR, et al. Normalization of hypertensive responses during ambulatory surgical stress by perioperative music. Psychosomatic Medicine 2001;63:487‐92. [DOI] [PubMed] [Google Scholar]
Andrada 2004 {published data only}
- Lopez‐Cepero Andrada JM, Amaya Vidal A, Castro Aguilar‐Tablada T, Garcia Reina I, Lopez S, Ruiz Guinaldo A, et al. Anxiety during the performance of colonoscopies: modification using music therapy. European Journal of Gastroenterology & Hepatology 2004;16:1381‐6. [DOI] [PubMed] [Google Scholar]
Argstatter 2006 {published data only}
- Argstatter H, Haberbosch W, Bolay HV. An investigation of the effectiveness of musical stimulation during heart catheter insertion [Untersuchung der Wirksamkeit von musikalischer Stimulation bei Herzkatheteruntersuchungen]. Musik‐, Tanz‐ und Kunsttherapie 2006;17(1):11‐20. [Google Scholar]
Ayoub 2005 {published data only}
- Ayoub CM, Rizk LB, Yaacoub CI, Gaal D, Kain ZN. Music and ambient operating room noise in patients undergoing spinal anesthesia. Anesthesia and Analgesia 2005;100:1316‐9. [DOI] [PubMed] [Google Scholar]
Bally 2003 {published data only}
- Bally K, Campbell D, Chesnick K, Tranmer JE. Effects of patient‐controlled music therapy during coronary angiography on procedural pain and anxiety distress syndrome. Critical Care Nurse 2003;23(2):50‐7. [PubMed] [Google Scholar]
Barnason 1995/1996 {published data only}
- Barnason S, Zimmerman L, Nieveen J. The effects of music interventions on anxiety in the patient after coronary artery bypass grafting. Heart & Lung 1995;24:124‐32. [DOI] [PubMed] [Google Scholar]
- Zimmerman L, Nieveen J, Barnason S, Schmaderer M. The effects of music intervention on postoperative pain and sleep in coronary artery bypass graft (CABG) patients. Scholarly Inquiry for Nursing Practice: An International Journal 1996;10(2):153‐70. [PubMed] [Google Scholar]
Binnings 1987 {published data only}
- Binnings EB. The effect of an auditory distraction on anxiety in ambulatory surgical patients experiencing regional anesthesia. Journal of the American Association of Nurse Anesthetists 1987;55(4):333‐5. [PubMed] [Google Scholar]
Blankfield 1995 {published data only}
- Blankfield RP, Zyzanski SJ, Flocke SA, Alemagno S, Scheurman K. Taped therapeutic suggestions and taped music as adjuncts in the care of coronary‐artery‐bypass patients. American Journal of Clinical Hypnosis 1995;37(3):32‐42. [DOI] [PubMed] [Google Scholar]
Broscious 1999 {published data only}
- Broscious SK. Music: an intervention for pain during chest tube removal after open heart surgery. American Journal of Critical Care 1999;8(6):410‐5. [PubMed] [Google Scholar]
Buffum 2006 {published data only}
- Buffum MD, Sasso C, Sands LP, Lanier E, Yellen M, Hayes A. A music intervention to reduce anxiety before vascular angiography procedures. Journal of Vascular Nursing 2006;24:68‐73. [DOI] [PubMed] [Google Scholar]
Cadigan 2001 {published data only}
- Cadigan ME, Caruso NA, Haldeman SM, McNamara ME, Noyes DA, Spadafora MA, et al. The effects of music on cardiac patients on bed rest. Progress in Cardiovascular Nursing 2001;16(1):5‐13. [DOI] [PubMed] [Google Scholar]
Cepeda 1998 {published data only}
- Cepeda MS, Diaz JE, Hernandez V, Daza E, Carr DB. Music does not reduce alfentanil requirement during patient‐controlled analgesia (PCA) use in extracorporeal shock wave lithotripsy for renal stones. Journal of Pain and Symptom Management 1998;16(6):382‐7. [DOI] [PubMed] [Google Scholar]
Chan 2003 {published data only}
- Chan YM, Lee PWH, Ng TY, Ngan HYS, Wong LC. The use of music to reduce anxiety for patients undergoing colposcopy: a randomized trial. Gynecologic Oncology 2003;91:213‐7. [DOI] [PubMed] [Google Scholar]
Chan 2006 {published data only}
- Chan MF, Wong OC, Chan HL, Fong MC, Lai SY, Lo CW, et al. Effects of music on patients undergoing a C‐clamp procedure after percutaneous coronary interventions. Journal of Advanced Nursing 2006;53(6):669‐79. [DOI] [PubMed] [Google Scholar]
Chang 2005 {published data only}
- Chang SC, Chen CH. Effects of music therapy on women's physiologic measures, anxiety, and satisfaction during cesarean delivery. Research in Nursing & Health 2005;28:453‐61. [DOI] [PubMed] [Google Scholar]
Chlan 1995 {published data only}
- Chlan LL. Psychophysiologic responses of mechanically ventilated patients to music: a pilot study. American Journal of Critical Care 1995;4(3):233‐8. [PubMed] [Google Scholar]
Chlan 1998 {published data only}
- Chlan L. Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart & Lung 1998;27(3):169‐76. [DOI] [PubMed] [Google Scholar]
Chlan 2000 {published data only}
- Chlan L, Evans D, Greenleaf M, Walker J. Effects of a single music therapy intervention on anxiety, discomfort, satisfaction, and compliance with screening guidelines in outpatients undergoing flexible sigmoidoscopy. Gastroenterology Nursing 2000;23(4):148‐56. [DOI] [PubMed] [Google Scholar]
Chui 2003 {published data only}
- Chui HW, Lin LS, Kuo MC, Chiang HS, Hsu CY. Using heart rate variability analysis to assess the effect of music therapy on anxiety reduction of patients. Computers in Cardiology 2003;30:469‐72. [Google Scholar]
Colt 1999 {published data only}
- Colt HG, Powers A, Shanks TG. Effect of music on state anxiety scores in patients undergoing fiberoptic bronchoscopy. Chest 1999;116:819‐24. [DOI: 10.1378/chest.116.3.819] [DOI] [PubMed] [Google Scholar]
Cooke 2005 {published data only}
- Cooke M, Chaboyer W, Schluter P, Hiratos M. The effect of music on preoperative anxiety in day surgery. Journal of Advanced Nursing 2005;52(1):47‐55. [DOI] [PubMed] [Google Scholar]
Cruise 1997 {published data only}
- Cruise CJ, Chung F, Yogendran S, Little D. Music increases satisfaction in elderly outpatients undergoing cataract surgery. Canadian Journal of Anaesthesia 1997;44(1):43‐8. [DOI] [PubMed] [Google Scholar]
Daub 1988 {published data only}
- Daub D, Kirschner‐Hermanns R. Reduction of preoperative anxiety. A study comparing music, Thalamonal and no premedication [Verminderung der praoperativen Angst. Vergleichende Studie zwischen Musik, Thalamonal und ohne Pramedikation]. Anaesthesist 1988;37:594‐7. [PubMed] [Google Scholar]
Davis‐Rollans 1987 {published data only}
- Davis‐Rollans C, Cunningham SG. Physiologic responses of coronary care patients to selected music. Heart & Lung 1987;16(4):370‐8. [PubMed] [Google Scholar]
Diette 2003 {published data only}
- Diette GB, Lechtzin N, Haponik E, Devrotes A, Rubin HR. Distraction therapy with nature sights and sounds reduces pain during flexible bronchoscopy: a complementary approach to routine analgesia. Chest 2003;123:941‐8. [DOI: 10.1378/chest.123.3.941] [DOI] [PubMed] [Google Scholar]
Domar 2005 {published data only}
- Domar AD, Eyvazzadeh A, Allen S, Roman K, Wolf R, Orav J, et al. Relaxation techniques for reducing pain and anxiety during screening mammography. American Journal of Roentgenology 2005;184(2):445‐7. [DOI] [PubMed] [Google Scholar]
Donald 2000 {published data only}
- Donald IP, Shuttleworth H. Preventing falls on an elderly care rehabilitation ward. Clinical Rehabilitation 2000;14:178‐85. [DOI] [PubMed] [Google Scholar]
Edge 2003 {published data only}
- Edge KJ. Wall color of patient's room: effects on recovery [Master's thesis]. University of Florida, 2003. [Google Scholar]
Elliot 1994 {published data only}
- Elliot D. The effects of music and muscle relaxation on patient anxiety in a coronary care unit. Heart & Lung 1994;23(1):27‐35. [PubMed] [Google Scholar]
Engelhart 2003 {published data only}
- Engelhart S, Hanfland J, Glasmacher A, Krizek L, Schmidt‐Wolf IGH, Exner M. Impact of portable air filtration units on exposure of haematology‐oncology patients to airborne Aspergillus fumigatus spores under field conditions. Journal of Hospital Infection 2003;54:300‐4. [DOI] [PubMed] [Google Scholar]
Ezzone 1998 {published data only}
- Ezzone S, Baker C, Rosselet R, Terepka E. Music as an adjunct to antiemetic therapy. Oncology Nursing Forum 1998;25(9):1551‐6. [PubMed] [Google Scholar]
Ferguson 2004 {published data only}
- Ferguson SL, Voll KV. Burn pain and anxiety: the use of music relaxation during rehabilitation. Journal of Burn Care & Rehabilitation 2004;25:8‐14. [DOI] [PubMed] [Google Scholar]
Frank 1992 {published data only}
- Frank SM, Beattie C, Christopherson R, Norris EJ, Rock P, Parker S, et al. Epidural versus general anesthesia, ambient operating room temperature, and patient age as predictors of inadvertent hypothermia. Anesthesiology 1992;77:252‐7. [DOI] [PubMed] [Google Scholar]
Gaberson 1991 {published data only}
- Gaberson KB. The effect of humorous distraction on preoperative anxiety: a pilot study. AORN Journal 1991;54(6):1258‐64. [DOI] [PubMed] [Google Scholar]
Gaberson 1995 {published data only}
- Gaberson KB. The effect of humorous and musical distraction on preoperative anxiety. AORN Journal 1995;62(5):784‐91. [DOI] [PubMed] [Google Scholar]
Ganidagli 2005 {published data only}
- Ganidagli S, Cengiz M, Yanik M, Becerik C, Unal B. The effect of music on preoperative sedation and the bispectral index. Anesthesia and Analgesia 2005;101:103‐6. [DOI] [PubMed] [Google Scholar]
Graham 2003 {published data only}
- Graham PH, Browne L, Cox H, Graham J. Inhalation aromatherapy during radiotherapy: results of a placebo‐controlled double‐blind randomized trial. Journal of Clinical Oncology 2003;21(12):2372‐6. [DOI] [PubMed] [Google Scholar]
Guo 2005 {published data only}
- Guo JY, Wang JR. Study on individual music intervention to reduce preoperative anxiety on patients undergoing laparoscope surgery. Chinese Journal of Nursing 2005;40(7):485‐8. [Google Scholar]
Harikumar 2006 {published data only}
- Harikumar R, Mehroof R, Antony P, Harish K, Sunil K, Sandesh K, et al. Listening to music decreases need for sedative medication during colonoscopy: a randomized, controlled trial. Indian Journal of Gastroenterology 2006;25:3‐5. [PubMed] [Google Scholar]
Hayes 2003 {published data only}
- Hayes A, Buffum M, Lanier E, Rodahl E, Sasso C. A music intervention to reduce anxiety prior to gastrointestinal procedures. Gastroenterology Nursing 2003;26(4):145‐9. [DOI] [PubMed] [Google Scholar]
Heitz 1992 {published data only}
- Heitz L, Symreng T, Scamman FL. Effect of music therapy in the postanesthesia care unit: a nursing intervention. Journal of Post Anesthesia Nursing 1992;7(1):22‐31. [PubMed] [Google Scholar]
Holmes 2002 {published data only}
- Holmes C, Hopkins V, Hensford C, MacLaughlin V, Wilkinson D, Rosenvinge H. Lavender oil as a treatment for agitated behaviour in severe dementia: a placebo controlled study. International Journal of Geriatric Psychiatry 2002;17:305‐8. [DOI] [PubMed] [Google Scholar]
Ikonomidou 2004 {published data only}
- Ikonomidou E. Effect of music on vital signs and postoperative pain. AORN Journal 2004;80(2):269‐274, 277‐8. [DOI] [PubMed] [Google Scholar]
Jacobson 1999 {published data only}
- Jacobson AF. Intradermal normal saline solution, self‐selected music, and insertion difficulty effects on intravenous insertion pain. Heart & Lung 1999;28:114‐22. [DOI] [PubMed] [Google Scholar]
Kasmar 1968 {published data only}
- Kasmar JV, Griffin WV, Mauritzen JH. Effect of environmental surroundings on outpatients' mood and perception of psychiatrists. Journal of Consulting and Clinical Psychology 1968;32(2):223‐6. [DOI] [PubMed] [Google Scholar]
Kliempt 1999 {published data only}
- Kliempt P, Ruta D, Ogston S, Landeck A, Martay K. Hemispheric‐synchronisation during anaesthesia: a double‐blind randomised trial using audiotapes for intra‐operative nociception control. Anaesthesia 1999;54:769‐73. [DOI] [PubMed] [Google Scholar]
Koch 1998a {published data only}
- Koch ME, Kain ZN, Ayoub C, Rosenbaum SH. The sedative and analgesic sparing effect of music: clinical investigations (phase 1). Anaesthesiology 1998;89:300‐6. [DOI] [PubMed] [Google Scholar]
Koch 1998b {published data only}
- Koch ME, Kain ZN, Ayoub C, Rosenbaum SH. The sedative and analgesic sparing effect of music: clinical investigations (phase 2). Anaesthesiology 1998;89:300‐6. [DOI] [PubMed] [Google Scholar]
Korunka 1992 {published data only}
- Korunka C, Guttmann G, Schleinitz D, Hilpert M, Haas R, Fitzal S. The effects of suggestions and music presented during general anaesthesia on postoperative well‐being [Die Auswirkung von Suggestionen und Musik während Vollnarkose auf postoperative Befindlichkeit]. Zeitschrift für Klinische Psychologie 1992;21(3):272‐84. [Google Scholar]
Kotwal 1998 {published data only}
- Kotwal MR, Rinchhen CZ, Ringe VV. Stress reduction through listening to Indian classical music during gastroscopy. Diagnostic and Therapeutic Endoscopy 1998;4:191‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kwekkeboom 2003 {published data only}
- Kwekkeboom KL. Music versus distraction for procedural pain and anxiety in patients with cancer. Oncology Nursing Forum 2003;30(3):433‐40. [DOI] [PubMed] [Google Scholar]
Lee 2002 {published data only}
- Lee DWH, Chan KW, Poon CM, Ko CW, Chan KH, Sin KS, et al. Relaxation music decreases the dose of patient‐controlled sedation during colonoscopy: a prospective randomized controlled trial. Gastrointestinal Endoscopy 2002;55(1):33‐6. [DOI] [PubMed] [Google Scholar]
Lee 2004a {published data only}
- Lee DWH, Chan ACW, Wong SKH, Fung TMK, Li ACN, Chan SKC, et al. Can visual distraction decrease the dose of patient‐controlled sedation required during colonoscopy? A prospective randomized controlled trial. Endoscopy 2004;36:197‐201. [DOI] [PubMed] [Google Scholar]
Lee 2005 {published data only}
- Lee OKA, Chung YFL, Chan MF, Chan WM. Music and its effect on the physiological responses and anxiety levels of patients receiving mechanical ventilation: a pilot study. Journal of Clinical Nursing 2005;14:609‐20. [DOI] [PubMed] [Google Scholar]
Lembo 1998 {published data only}
- Lembo T, Fitzgerald L, Matin K, Woo K, Mayer EA, Naliboff BD. Audio and visual stimulation reduces patient discomfort during screening flexible sigmoidoscopy. The American Journal of Gastroenterology 1998;93(7):1113‐6. [DOI] [PubMed] [Google Scholar]
Lepage 2001 {published data only}
- Lepage C, Drolet P, Girard M, Grenier Y, DeGagne R. Music decreases sedative requirements during spinal anesthesia. Anesthesia and Analgesia 2001;93:912‐6. [DOI] [PubMed] [Google Scholar]
Lidwell 1971 {published data only}
- Lidwell OM, Davies J, Payne RW, Newman P, Williams REO. Nasal acquisition of Staphylococcus aureus in partly divided wards. Journal of Hygiene 1971;69:113‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lohner 1979 {published data only}
- Lohner D, Debusscher L, Prévost JM, Klastersky J. Comparative randomised study of protected environment plus oral antibiotics versus oral antibiotics alone in neutropenic patients. Cancer Treatment Reports 1979;63(3):363‐8. [PubMed] [Google Scholar]
Lueders Bolwerk 1990 {published data only}
- Lueders Bolwerk CA. Effects of relaxing music on state anxiety in myocardial infarction patients. Critical Care Nursing Quartly 1990;13(2):63‐72. [DOI] [PubMed] [Google Scholar]
Mandle 1990 {published data only}
- Mandle CL, Domar AD, Harrington DP, Leserman J, Bozadjian EM, Friedman R, et al. Relaxation response in femoral angiography. Radiology 1990;174:737‐9. [DOI] [PubMed] [Google Scholar]
Masuda 2005 {published data only}
- Masuda T, Miyamoto K, Shimizu K. Effects of music listening on elderly orthopaedic patients during postoperative bed rest. Nordic Journal of Music Therapy 2005;14(1):4‐14. [Google Scholar]
McRee 2003 {published data only}
- McRee LD. Using massage and music therapy to improve postoperative outcomes. AORN Journal 2003;78(3):433‐42, 445‐7. [DOI] [PubMed] [Google Scholar]
Mennegazzi 1991 {published data only}
- Menegazzi JJ, Paris PM, Kersteen CH, Flynn B, Trautman DE. A randomized, controlled trial of the use of music during lacertion repair. Annals of Emergency Medicine 1991;20(4):348‐50. [DOI] [PubMed] [Google Scholar]
Migneault 2004 {published data only}
- Migneault B, Girard F, Albert C, Chouinard P, Boudreault D, Provencher D, et al. The effect of music on the neurohormonal stress response to surgery under general anesthesia. Anesthesia and Analgesia 2004;98:527‐32. [DOI] [PubMed] [Google Scholar]
Miller 1992 {published data only}
- Miller AC, Hickman LC, Lemasters GK. A distraction technique for control of burn pain. Journal of Burn Care & Rehabilitation 1992;13(5):576‐80. [DOI] [PubMed] [Google Scholar]
Mullooly 1998 {published data only}
- Mullooly VM, Levin RF, Feldman HR. Music for postoperative pain and anxiety. Journal of New York State Nurses' Association 1988;19(3):4‐7. [PubMed] [Google Scholar]
Nilsson 2001 {published data only}
- Nilsson U, Rawal N, Uneståhl LE, Zetterberg C, Unosson M. Improved recovery after music and therapeutic suggestions during general anaesthesia: a double‐blind randomised controlled trial. Acta Anaesthesiologica Scandinavica 2001;45:812‐7. [DOI] [PubMed] [Google Scholar]
Nilsson 2003a {published data only}
- Nilsson U, Rawal N, Unosson M. A comparison of intra‐operative or postoperative exposure to music‐ a controlled trial of the effects on postoperative pain. Anaesthesia 2003;58:684‐711. [DOI] [PubMed] [Google Scholar]
Nilsson 2003b {published data only}
- Nilsson U, Rawal N, Enqvist B, Unosson M. Analgesia following music and therapeutic suggestions in the PACU in ambulatory surgery; a randomised controlled trial. Acta Anaesthesiologica Scandinavica 2003;47:278‐83. [DOI] [PubMed] [Google Scholar]
Nilsson 2005 {published data only}
- Nilsson U, Unosson M, Rawal N. Stress reduction and analgesia in patients exposed to calming music postoperatively: a randomized controlled trial. European Journal of Anaesthesiology 2005;22:96‐102. [DOI] [PubMed] [Google Scholar]
Nowobilski 2005 {published data only}
- Nowobilski R, Czyz P, Furgal M, Wegrzyn‐Sliwka A, Ptak‐Witkowska A, Kliczewska A, et al. The influence of musicotherapy on anxiety level in hospitalized asthmatic patients [Wplyw muzykoterapii biernej na poziom leku u chorych hospitalizowanych z powodu astmy oskrzelowej]. Polskie Archiwum Medycyny Wewnetrznej 2005;113(4):314‐9. [PubMed] [Google Scholar]
Padmanabhan 2005 {published data only}
- Padmanabhan R, Hildreth AJ, Laws D. A prospective, randomised, controlled study examining binaural beat audio and pre‐operative anxiety in patients undergoing general anaesthesia for day case surgery. Anaesthesia 2005;60:874‐7. [DOI] [PubMed] [Google Scholar]
Palakanis 1994 {published data only}
- Palakanis KC, DeNobile JW, Sweeney WB, Blankenship CL. Effect of music therapy on state anxiety in patients undergoing flexible sigmoidoscopy. Diseases of the Colon & Rectum 1994;37(5):478‐81. [DOI] [PubMed] [Google Scholar]
Phumdoung 2003 {published data only}
- Phumdoung S, Good M. Music reduces sensation and distress of labor pain. Pain Management Nursing 2003;4(2):54‐61. [DOI] [PubMed] [Google Scholar]
Schiemann 2002 {published data only}
- Schiemann U, Gross M, Reuter R, Kellner H. Improved procedure of colonoscopy under accompanying music therapy. European Journal of Medical Research 2002;7:131‐4. [PubMed] [Google Scholar]
Schneider 2001 {published data only}
- Schneider N, Schedlowski M, Schurmeyer TH, Becker H. Stress reduction through music in patients undergoing cerebral angiography. Neuroradiology 2001;43:472‐6. [DOI] [PubMed] [Google Scholar]
Sendelbach 2006 {published and unpublished data}
- Sendelbach SE, Halm MA, Doran KA, Miller EH, Gaillard P. Effects of music therapy on physiological and psychological outcomes for patients undergoing cardiac surgery. Journal of Cardiovascular Nursing 2006;21(3):194‐200. [DOI] [PubMed] [Google Scholar]
Smith 2001 {published data only}
- Smith M, Casey L, Johnson D, Gwede C, Riggin OZ. Music as a therapeutic intervention for anxiety in patients receiving radiation therapy. Oncology Nursing Forum 2001;28(5):855‐62. [PubMed] [Google Scholar]
Smolen 2002 {published data only}
- Smolen D, Topp R, Singer L. The effect of self‐selected music during colonoscopy on anxiety, heart rate, and blood pressure. Applied Nursing Research 2002;16(2):126‐36. [DOI] [PubMed] [Google Scholar]
Staricoff 2003f {published data only}
- Staricoff RL, Duncan JP, Wright M. HIV/AIDS Unit. A study of the effects of visual and performing arts in health care. http://www.publicartonline.org.uk/news/research/documents/ChelseaAndWestminsterResearchproject.pdf, 2003:11‐5. [Google Scholar]
Tang 1993 {published data only}
- Tang CS, Ko CJ, Ng SM, Chen SC, Cheng KI, Yu KL, et al. "Walkman music" during epidural anesthesia. Gaoxiong Yi Xue Ke Xue Za Zhi 1993;9:468‐75. [PubMed] [Google Scholar]
Taylor 1998 {published data only}
- Taylor LK, Kuttler KL, Parks TA, Milton D. The effect of music in the postanesthesia care unit on pain levels in women who have had abdominal hysterectomies. Journal of PeriAnesthesia Nursing 1998;13(2):88‐94. [DOI] [PubMed] [Google Scholar]
Taylor‐Piliae 2002 {published data only}
- Taylor‐Piliae RE, Chair SY. The effect of nursing interventions utilizing music therapy or sensory information on Chinese patients' anxiety prior to cardiac catheterization: a pilot study. European Journal of Cardiovascular Nursing 2002;1(3):203‐11. [DOI] [PubMed] [Google Scholar]
Triller 2006 {published data only}
- Triller N, Eržen D, Duh Š, Primoži? MP, Košnik M. Music during bronchoscopic examination: the physiological effects. Respiration 2006;73:95‐9. [DOI] [PubMed] [Google Scholar]
Tsuchiya 2003 {published and unpublished data}
- Tsuchiya M, Asada A, Ryo K, Noda K, Hashino T, Sato Y, et al. Relaxing intraoperative natural sound blunts haemodynamic change at the emergence from propofol general anaesthesia and increases the acceptability of anaesthesia to the patient. Acta Anaesthesiologica Scandinavica 2003;47:939‐43. [DOI] [PubMed] [Google Scholar]
Twiss 2006 {published data only}
- Twiss E, Seaver J, McCaffrey R. The effect of music listening on older adults undergoing cardiovascular surgery. Nursing in Critical Care 2006;11(5):224‐31. [DOI] [PubMed] [Google Scholar]
Vaaler 2005 {published data only}
- Vaaler AE, Morken G, Linaker OM. Effects of different interior decorations in the seclusion area of a psychiatric acute ward. Nordic Journal of Psychiatry 2005;59(1):19‐24. [DOI] [PubMed] [Google Scholar]
Voss 2004 {published data only}
- Voss JA, Good M, Yates B, Baun MM, Thompson A, Hertzog M. Sedative music reduces anxiety and pain during chair rest after open heart surgery. Pain 2004;112:197‐203. [DOI] [PubMed] [Google Scholar]
Walch 2005 {published data only}
- Walch JM, Rabin BS, Day R, Williams JN, Choi K, Kang JD. The effect of sunlight on postoperative analgesic medication use: a prospective study of patients undergoing spinal surgery. Psychosomatic Medicine 2005;67:156‐63. [DOI] [PubMed] [Google Scholar]
Wang 2002 {published data only}
- Wang SM, Kulkami L, Doley J, Kain ZN. Music and pre‐operative anxiety: a randomized, controlled study. Anesthesia and Analgesia 2002;94(6):1489‐94. [DOI] [PubMed] [Google Scholar]
White 1992 {published data only}
- White JM. Music therapy: an intervention to reduce anxiety in the myocardial infarction patient. Clincal Nurse Specialist 1992;6(2):58‐63. [PubMed] [Google Scholar]
White 1999 {published data only}
- White JM. Effects of relaxing music on cardiac autonomic balance and anxiety after acute myocardial infarction. American Journal of Critical Care 1999;8(4):220‐30. [PubMed] [Google Scholar]
Whyte 1969 {published data only}
- Whyte W, Howie JGR, Eakin JE. Bacteriological observations in a mechanically ventilated experimental ward and in two open‐plan wards. Journal of Medical Microbiology 1969;2(3):335‐45. [DOI] [PubMed] [Google Scholar]
Wilber 2005 {published data only}
- Wilber ST, Burger B, Gerson LW, Blanda M. Reclining chairs reduce pain from gurneys in older emergency department patients: a randomized controlled trial. Academic Emergency Medicine 2005;12:119‐23. [DOI] [PubMed] [Google Scholar]
Willmott 1986 {published data only}
- Willmott M. The effect of a vinyl floor surface and a carpeted floor surface upon walking in elderly hospital in‐patients. Age and Ageing 1986;15:119‐20. [DOI] [PubMed] [Google Scholar]
Winter 1994 {published data only}
- Winter MJ, Paskin S, Baker T. Music reduces stress in the surgical holding area. Journal of Post Anesthesia Nursing 1994;9(6):340‐3. [PubMed] [Google Scholar]
Wong 2001 {published data only}
- Wong HLC, Lopez‐Nahas V, Molassiotis A. Effects of music therapy on anxiety in ventilator‐dependent patients. Heart & Lung 2001;30:376‐87. [DOI] [PubMed] [Google Scholar]
Yang 2003 {published data only}
- Yang F. Effect of music on anxiety of patients receiving eyeground operation. Chinese Mental Health Journal 2003;17(4):256‐7. [Google Scholar]
Yung 2003 {published data only}
- Yung PMB, Kam SC, Lau BWK, Chan TMF. The effect of music in managing preoperative stress for Chinese surgical patients in the operating room holding area: a controlled trial. International Journal of Stress Management 2003;10(1):64‐74. [Google Scholar]
Zhang 2005 {published data only}
- Zhang XW, Fan Y, Manyande A, Tian YK, Yin P. Effects of music on target‐controlled infusion of propofol requirements during combined spinal‐epidural anaesthesia. Anaesthesia 2005;60:990‐4. [DOI] [PubMed] [Google Scholar]
Zimmerman 1988 {published data only}
- Zimmerman LM, Pierson MA, Marker J. Effects of music on patient anxiety in coronary care units. Heart & Lung 1988;17(5):560‐6. [PubMed] [Google Scholar]
Zimmerman 1989 {published data only}
- Zimmerman L, Pozehl B, Duncan K, Schmitz R. Effects of music in patients who had chronic cancer pain. Western Journal of Nursing Research 1989;11(3):298‐309. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aaron 1996 {published data only}
- Aaron JN, Carlisle CC, Carskadon MA, Meyer TJ, Hill NS, Millman RP. Environmental noise as a cause of sleep disruption in an intermediate respiratory care unit. Sleep 1996;19(9):707‐10. [DOI] [PubMed] [Google Scholar]
Abramson 1966 {published data only}
- Abramson M, Greenfield I, Heron WT. Response to or perception of auditory stimuli under deep surgical anesthesia. American Journal of Obstetrics and Gynecology Society 1966;96(4):584‐5. [DOI] [PubMed] [Google Scholar]
Alberti 2001 {published data only}
- Alberti C, Bouakline A, Ribaud P, Lacroix C, Rousselot P, Leblanc T, et al. Relationship between environmental fungal contamination and the incidence of invasive aspergillosis in haematology patients. Journal of Hospital Infection 2001;48:198‐206. [DOI] [PubMed] [Google Scholar]
Allen 1989 {published data only}
- Allen KD, Danforth JS, Drabman RS. Videotaped modeling and film distraction for fear reduction in adults undergoing hyperbaric oxygen therapy. Journal of Consulting and Clinical Psychology 1989;57(4):554‐8. [DOI] [PubMed] [Google Scholar]
Alvermann 1979 {published data only}
- Alvermann MM. Toward improving geriatric care with environmental intervention emphasizing a homelike atmosphere: an environmental experience. Journal of Gerontological Nursing 1979;5(3):13‐7. [DOI] [PubMed] [Google Scholar]
Anderson 1982 {published data only}
- Anderson RL, Mackel DC, Stoler BS, Mallison GF. Carpeting in hospitals: an epidemiological evaluation. Journal of Clinical Microbiology 1982;15(3):408‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 2004 {published data only}
- Anderson LA, Gross JB. Aromatherapy with peppermint, isopropyl alcohol, or placebo is equally effective in relieving postoperative nausea. Journal of PeriAnesthesia Nursing 2004;19(1):29‐35. [DOI] [PubMed] [Google Scholar]
Ansari 1969 {published data only}
- Ansari A, Burch GE. Influence of hot environments on the cardiovascular system: a clinical study of 23 cardiac patients at rest. Archives of Internal Medicine 1969;123:371‐8. [PubMed] [Google Scholar]
Anthony Williams {published data only}
- Anthony Williams, Partners. Hospital unit for the elderly. Building 1989;April 7:49‐56. [Google Scholar]
Armstrong 1984 {published data only}
- Armstrong D. Protected environments are discomforting and expensive and do not offer meaningful protection. The American Journal of Medicine 1984;76:685‐9. [DOI] [PubMed] [Google Scholar]
Augustin 1996 {published data only}
- Augustin P, Hains AA. Effect of music on ambulatory surgery patients' preoperative anxiety. AORN Journal 1996;63:750‐8. [DOI] [PubMed] [Google Scholar]
Azer 1971 {published data only}
- Azer NZ, McNall PE, Leung HC. Physiological effects of localized ventilation. Journal of Applied Physiology 1971;31(5):669‐74. [DOI] [PubMed] [Google Scholar]
Baird 1969 {published data only}
- Baird G, Whyte W. Air movement control for treatment and isolation rooms. Journal of Hygiene 1969;67(2):225‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 1987 {published data only}
- Baker CF. Effect of noise in ICU on heart rate and annoyance in adult postoperative patients. Journal of the Acoustical Society of America 1987;81(S1):S48. [Google Scholar]
Baker 1992 {published data only}
- Baker CF. Discomfort to environmental noise: heart rate responses of SICU patients. Critical Care Nursing Quarterly 1992;15(2):75‐90. [DOI] [PubMed] [Google Scholar]
Baker 1993a {published data only}
- Baker CF, Garvin BJ, Kennedy CW, Polivka BJ. The effect of environmental sound and communication on CCU patients' heart rate and blood pressure. Research in Nursing & Health 1993;16:415‐21. [DOI] [PubMed] [Google Scholar]
Baker 1993b {published data only}
- Baker CF. Annoyance to ICU noise: a model of patient discomfort. Critical Care Nursing Quarterly 1993;16(2):83‐90. [DOI] [PubMed] [Google Scholar]
Baldwin 1985 {published data only}
- Baldwin S. Effects of furniture rearrangement on the atmosphere of wards in a maximum‐security hospital. Hospital and Community Psychiatry 1985;36(5):525‐8. [PubMed] [Google Scholar]
Bame 1993 {published data only}
- Bame SI. Dialysis treatment room design. Dialysis & Transplantation 1993;22(4):200‐12. [Google Scholar]
Bame 1995 {published data only}
- Bame SI, Wells W. Acoustical design features associated with noise level in health facilities: the case of dialysis facilities. Journal of Interior Design 1995;21(2):1‐14. [Google Scholar]
Bampton 1997 {published data only}
- Bampton P, Draper B. Effect of relaxation music on patient tolerance of gastrointestinal endoscopic procedures. Journal of Clinical Gastroenterology 1997;25(1):343‐5. [DOI] [PubMed] [Google Scholar]
Barker 2005 {published data only}
- Barker BT, DeBord DR. Innovative hospital designs make a difference. Trustee 2005;58(10):34‐6. [PubMed] [Google Scholar]
Barlas 2001 {published data only}
- Barlas D, Sama AE, Ward MF, Lesser ML. Comparison of the auditory and visual privacy of emergency department treatment areas with curtains versus those with solid walls. Annals of Emergency Medicine 2001;38(2):135‐9. [DOI] [PubMed] [Google Scholar]
Beauchemin 1996 {published data only}
- Beauchemin KM, Hays P. Sunny hospital rooms expedite recovery from severe and refractory depressions. Journal of Affective Disorders 1996;40:49‐51. [DOI] [PubMed] [Google Scholar]
Beauchemin 1998a {published data only}
- Beauchemin KM, Hays P. Seeing ward design in a new light. Hospital Development 1998;29(9):15‐6. [Google Scholar]
Beauchemin 1998b {published data only}
- Beauchemin KM, Hays P. Dying in the dark: sunshine, gender and outcomes in myocardial infarction. Journal of the Royal Society of Medicine 1998;91(7):352‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beck 1991 {published data only}
- Beck SL. The therapeutic use of music for cancer‐related pain. Oncology Nursing Forum 1991;18(8):1327‐37. [PubMed] [Google Scholar]
Becker 1980 {published data only}
- Becker FD, Poe DB. The effects of user‐generated design modifications in a general hospital. Journal of Nonverbal Behavior 1980;4(4):195‐218. [Google Scholar]
Beldon 2002 {published data only}
- Beldon P. Transfoam Visco™: evaluation of a viscoelastic foam mattress. British Journal of Nursing 2002;11(9):651‐5. [DOI] [PubMed] [Google Scholar]
Benedetti 2001 {published data only}
- Benedetti F, Colombo C, Barbini B, Campori E, Smeraldi E. Morning sunlight reduces length of hospitalization in bipolar depression. Journal of Affective Disorders 2001;62:221‐3. [DOI] [PubMed] [Google Scholar]
Berg 2001 {published data only}
- Berg S. Impact of reduced reverberation time on sound‐induced arousals during sleep. Sleep 2001;24(3):289‐92. [DOI] [PubMed] [Google Scholar]
Berlet 1979 {published data only}
- Berlet MH, Binet F. Environment and quality of sleep in the hospital milieu [Environnement et qualité du sommeil en milieu hospitalier]. Soins: La Revue de Reference Infirmiere 1979;24(23):35‐9. [PubMed] [Google Scholar]
Bettschen‐Steiner {published data only}
- Bettschen‐Steiner VB. Can the mental condition of the patient affect the safety of anesthesia? Music and suggestion diminish anxiety and tension [Kann der psychische Zustand eines Patienten die Sicherheit der Narkose beeinflussen? Musik und suggestion bauen angst und spannung ab]. Krankenpflege Soins Infirmiers 1985;78(11):23‐9. [PubMed] [Google Scholar]
Biley 1994 {published data only}
- Biley FC. Effects of noise in hospitals. British Journal of Nursing 1994;3(3):110‐3. [DOI] [PubMed] [Google Scholar]
Binek 2003 {published and unpublished data}
- Binek J, Sagmeister M, Borovicka J, Knierim M, Magdeburg B, Meyenberger C. Perception of gastrointestinal endoscopy by patients and examiners with and without background music. Digestion 2003;68:5‐8. [DOI] [PubMed] [Google Scholar]
Birdsong 1990 {published data only}
- Birdsong C, Leibrock C. Patient‐centered design. The Healthcare Forum Journal 1990;33(3):40‐5. [PubMed] [Google Scholar]
Bodey 1969 {published data only}
- Bodey GP, Freireich EJ, Frei E. Studies of patients in a laminar air flow unit. Cancer 1969;24(5):972‐80. [DOI] [PubMed] [Google Scholar]
Bodey 1971 {published data only}
- Bodey GP, Gehan EA, Freireich EJ. Protected environment‐prophylactic antibiotic program in the chemotherapy of acute leukemia. The American Journal of the Medical Sciences 1971;262(3):138‐51. [DOI] [PubMed] [Google Scholar]
Boeke 1988 {published data only}
- Boeke S, Bonke B, Bouwhuis‐Hoogerwerf ML, Bovill JG, Zwaveling A. Effects of sounds presented during general anaesthesia on postoperative course. British Journal of Anaesthesia 1988;60:697‐702. [DOI] [PubMed] [Google Scholar]
Bonke 1982 {published data only}
- Bonke B, Bouwhuis‐Hoogerwerf ML, Verhage F, Zwaveling A. A medico‐psychological study of the influence of sounds during general anesthesia on the postoperative course [Een medisch‐psychologisch onderzoek naar de invloed van geluiden tijdens algehele anesthesie op het postoperatieve beloop]. Nederlands Tijdschrift Voor Geneeskunde 1982;126(17):763‐5. [PubMed] [Google Scholar]
Bonny 1983 {published data only}
- Bonny HL. Music listening for intensive coronary care units: A pilot project. Music Therapy 1983;3(1):4‐16. [Google Scholar]
Bower 1995 {published data only}
- Bower JO. Incorporating art into the patient experience. AORN Journal 1995;61(5):858‐61. [DOI] [PubMed] [Google Scholar]
Bozcuk 2006 {published data only}
- Bozcuk H, Artac M, Kara A, Ozdogan M, Sualp Y, Topcu Z, et al. Does music exposure during chemotherapy improve quality of life in early breast cancer patients? A pilot study. Medical Science Monitor 2006;12(5):CR200‐5. [PubMed] [Google Scholar]
Breslow 1993 {published data only}
- Breslow DM. Creative arts for hospitals: the UCLA experiment. Patient Education and Counseling 1993;21:101‐10. [DOI] [PubMed] [Google Scholar]
Browning 2001 {published data only}
- Browning CA. Music therapy in childbirth: research in practice. Music Therapy Perspectives 2001;19(2):74‐81. [Google Scholar]
Brunges 2003 {published data only}
- Brunges M, Avigne G. Music therapy for reducing surgical anxiety. AORN Journal 2003;78(5):816‐8. [DOI] [PubMed] [Google Scholar]
Buemi 1995 {published data only}
- Buemi M, Allegra A, Grasso F, Mondio G. Noise pollution in an intensive care unit for nephrology and dialysis. Nephrology Dialysis Transplantation 1995;10(12):2235‐9. [DOI] [PubMed] [Google Scholar]
Burke 1977 {published data only}
- Burke JF, Quinby WC, Bondoc CC, Sheehy EM, Moreno HC. The contribution of a bacterially isolated environment to the prevention of infection in seriously burned patients. Annals of Surgery 1977;186(3):377‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns 2000a {published data only}
- Burns EE, Blamey C, Ersser SJ, Barnetson L, Lloyd AJ. An investigation into the use of aromatherapy in intrapartum midwifery practice. The Journal of Alternative and Complementary Medicine 2000;6(2):141‐7. [DOI] [PubMed] [Google Scholar]
Burns 2000b {published data only}
- Burns EE, Blamey C, Lloyd AJ. Aromatherapy in childbirth: an effective approach to care. British Journal of Midwifery 2000;8(10):639‐43. [Google Scholar]
Burns 2002 {published data only}
- Burns E. Aromatherapy in childbirth. MIDIRS Midwifery Digest 2002;12(3):349‐53. [Google Scholar]
Butler 1993 {published data only}
- Butler DL, Acquino AL, Hissong AA, Scott P. Wayfinding by newcomers in a complex building. Human Factors 1993;35(1):159‐73. [Google Scholar]
Byers 1997 {published data only}
- Byers JF, Smyth KA. Effect of a music intervention on noise annoyance, heart rate, and blood pressure in cardiac surgery patients. American Journal of Critical Care 1997;6(3):183‐191. [PubMed] [Google Scholar]
Bykov 2003a {published data only}
- Bykov AT, Malyarenko TN. Aromatherapy in the control over autonomic regulation of heart rhythm. Voprosy kurortologii, fizioterapii, i lechebnoi fizicheskoi kultury 2003;6:6‐9. [PubMed] [Google Scholar]
Bykov 2003b {published data only}
- Bykov T, Malyarenko TN, Malyarenko YE. Role of prolonged influence of specially selected music in optimization of chronotropic heart function control. Voprosy kurortologii, fizioterapii, i lechebnoi fizicheski kultury 2003;2:10‐6. [PubMed] [Google Scholar]
Cai 2001a {published data only}
- Cai GR, Li PW, Jiao LP. Clinical observation of music therapy combined with anti‐tumor drugs in treating 116 cases of tumor patients. Zhongguo Zhong xi yi jie he za zhi Zhongguo Zhongxiyi jiehe zazhi 2001;21(12):891‐4. [PubMed] [Google Scholar]
Cai 2001b {published data only}
- Cai G, Qiao Y, Li P, et al. Music therapy in treatment of cancer patients. Chinese Mental Health Journal 2001;15(3):179‐81. [Google Scholar]
Carpman 1983 {published data only}
- Carpman JR, Grant MA, Simmons DA. Wayfinding in the hospital environment: the impact of various floor numbering alternatives. Journal of Environmental Systems 1983;13(4):353‐64. [Google Scholar]
Castellani 1968 {published data only}
- Castellani L, Stanca A. Music and white sound in obstetrical analgesia [Musica e white sound nella analgesia ostetrica]. Acta Anaesthesiologica 1968;29(2):S272‐5. [PubMed] [Google Scholar]
Ceccio 1984 {published data only}
- Ceccio CM. Postoperative pain relief through relaxation in elderly patients with fractured hips. Orthopaedic Nursing 1984;3(3):11‐9. [DOI] [PubMed] [Google Scholar]
Chaudhury 2003 {published data only}
- Chaudhury H, Mahmood A, Valente M. The use of single patient rooms vs. multiple occupancy rooms in acute care environments: pilot study on comparative assessment of patient care issues in single and multiple occupancy patient rooms. The Coalition for Health Environments Research, 2003. [Google Scholar]
Cheek 1971 {published data only}
- Cheek FE, Maxwell R, Weisman R. Carpeting the ward: an exploratory study in environmental psychiatry. Mental Hygiene 1971;55(1):109‐18. [PubMed] [Google Scholar]
Chikamori 2004 {published data only}
- Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Perioperative music therapy with a key‐lighting keyboard system in elderly patients undergoing digestive tract surgery. Hepato‐Gastroenterology 2004;51:1384‐6. [PubMed] [Google Scholar]
Choctaw 1984 {published data only}
- Choctaw WT. Is there a need for barrier isolators with laminar air flow in managing adult patients with major burns?. Journal of Burn Care and Rehabilitation 1984;5(4):331‐4. [Google Scholar]
Chow 2005 {published data only}
- Chow TT, Yang XY. Ventilation performance in the operating theatre against airborne infection: numerical study on an ultra‐clean system. Journal of Hospital Infection 2005;59:138‐47. [DOI] [PubMed] [Google Scholar]
Christenfeld 1989 {published data only}
- Christenfeld R, Wagner J, Pastva G, Acrish WP. How physical settings affect chronic mental patients. Psychiatric Quarterly 1989;60(3):253‐64. [DOI] [PubMed] [Google Scholar]
Cirina 1994 {published data only}
- Cirina CL. Effects of sedative music on patient preoperative anxiety. Today's OR Nurse 1994;16(3):15‐8. [PubMed] [Google Scholar]
Clair 1994 {published data only}
- Clair AA, Bernstein B. The effect of no music, stimulative background music and sedative background music on agitated behaviors in persons with severe dementia. Activities, Adaptation & Aging 1994;19(1):61‐70. [Google Scholar]
Clair 2006 {published data only}
- Clair AA, O'Konski M. The effect of rhythmic auditory stimulation (RAS) on gait characteristics of cadence, velocity, and stride length in persons with late stage dementia. Journal of Music Therapy 2006;43(2):154‐63. [DOI] [PubMed] [Google Scholar]
Clark 1998 {published data only}
- Clark ME, Lipe AW, Bilbrey M. Use of music to decrease aggressive behaviors in people with dementia. Journal of Gerontological Nursing 1998;24(7):10‐7. [DOI] [PubMed] [Google Scholar]
Connell 1996 {published data only}
- Connell BR. Role of the environment in falls prevention. Clinics in Geriatric Medicine 1996;12(4):859‐80. [PubMed] [Google Scholar]
Cook 1986 {published data only}
- Cook JD. Music as an intervention in the oncology setting. Cancer Nursing 1986;9(1):23‐8. [PubMed] [Google Scholar]
Cooper 1989 {published data only}
- Cooper B, Mohide A, Gilbert S. Testing the use of colour in a long‐term care setting. World Hospitals 1989;27(1):25‐9. [PubMed] [Google Scholar]
Cooper 1991 {published data only}
- Cooper J. Songs that soothe. The New Zealand Nursing Journal 1991;84(3):22‐3. [PubMed] [Google Scholar]
Cooper 1998 {published data only}
- Cooper PJ, Gray DG, Mollison J. A randomised controlled trial of two pressure‐reducing surfaces. Journal of Wound Care 1998;7(8):374‐6. [DOI] [PubMed] [Google Scholar]
Coulson 1997 {published data only}
- Coulson I, White J. A total environment quality of care approach to evaluation of management and care at two dementia care units in Tasmania. American Journal of Alzheimer's Disease 1997;12(3):128‐37. [Google Scholar]
Counsell 2000 {published data only}
- Counsell SR, Holder CM, Liebenauer LL, Palmer RM, Fortinsky RH, Kresevic DM, et al. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of acute care for elders (ACE) in a community hospital. Journal of the American Geriatrics Society 2000;48(12):1572‐81. [DOI] [PubMed] [Google Scholar]
Courtright 1990 {published data only}
- Courtright P, Johnson S, Baumgartner MA, Jordan M, Webster JC. Dinner music: does it affect the behavior of psychiatric inpatients?. Journal of Psychosocial Nursing 1990;28(3):37‐40. [DOI] [PubMed] [Google Scholar]
Covinsky 1998 {published data only}
- Covinsky KE, Palmer RM, Kresevic DM, Kahana E, Counsell SR, Fortinsky RH, et al. Improving functional outcomes in older patients: lessons from an acute care for elders unit. Journal of Quality Improvement 1998;24(2):63‐76. [DOI] [PubMed] [Google Scholar]
Cunningham 1997 {published data only}
- Cunningham MF. Introducing a music program in the perioperative area. AORN Journal 1997;66(4):674‐82. [DOI] [PubMed] [Google Scholar]
Davidson 1971 {published data only}
- Davidson AL, Smylie HG, Macdonald A, Smith G. Ward design in relation to postoperative wound infection. British Medical Journal 1971;1:72‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davies 1980 {published data only}
- Davies ADM, Snaith PA. The social behaviour of geriatric patients at mealtimes: an observational and an intervention study. Age and Ageing 1980;9:93‐9. [DOI] [PubMed] [Google Scholar]
Davis 1992 {published data only}
- Davis CA. The effects of music and basic relaxation instruction on pain and anxiety of women undergoing in‐office gynecological procedures. Journal of Music Therapy 1992;29(4):202‐16. [Google Scholar]
De Jong 1972 {published data only}
- Jong MA. A physiological approach to aesthetic preference. I. Paintings. Psychotherapy and Psychosomatics 1972;20:360‐5. [DOI] [PubMed] [Google Scholar]
Dekker 1994 {published data only}
- Dekker AW, Verdonck LF, Rozenberg‐Arska M. Infection prevention in autologous bone marrow transplantation and the role of protective isolation. Bone Marrow Transplantation 1994;14:89‐93. [PubMed] [Google Scholar]
De l'Etoile 2002 {published data only}
- l'Etoile SK. The effectiveness of music therapy in group psychotherapy for adults with mental illness. The Arts in Psychotherapy 2002;29:69‐78. [Google Scholar]
Demling 1978 {published data only}
- Demling RH, Perea AP, Maly J, Moylan JA, Jarrett F, Balish E. The use of a laminar airflow isolation system for the treatment of major burns. The American Journal of Surgery 1978;136(3):375‐8. [DOI] [PubMed] [Google Scholar]
Denney 1997 {published data only}
- Denney A. Quiet music: an intervention for mealtime agitation?. Journal of Gerontological Nursing 1997;23(7):16‐23. [DOI] [PubMed] [Google Scholar]
Dennis 1988 {published data only}
- Dennis M. Environmental changes geared towards the elderly in an acute care setting. Perspectives 1988;12(3):4‐6. [PubMed] [Google Scholar]
DeSchriver 1990 {published data only}
- DeSchriver MM, Riddick CC. Effects of watching aquariums on elders' stress. Anthrozoos 1990;4(1):44‐8. [Google Scholar]
Devlin 1992 {published data only}
- Devlin AS. Psychiatric ward renovation: staff perception and patient behavior. Environment and Behavior 1992;24(1):66‐84. [Google Scholar]
Dickinson 1995 {published data only}
- Dickinson JI, McLain‐Kark J, Marshall‐Baker A. The effects of visual barriers on exiting behavior in a dementia care unit. The Gerontologist 1995;35(1):127‐30. [DOI] [PubMed] [Google Scholar]
Diffey 1988 {published data only}
- Diffey BL, Storey A. Light and length of stay in hospital. Journal of the Royal Society of Medicine 1988;81:643. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dolce 1985 {published data only}
- Dolce JJ, Doleys DM, Raczynski JM, Crocker MF. Narcotic utilization for back pain patients housed in private and semi‐private rooms. Addictive Behaviors 1985;10:91‐5. [DOI] [PubMed] [Google Scholar]
Donchin 2002 {published data only}
- Donchin Y, Seagull FJ. The hostile environment of the intensive care unit. Current Opinion in Critical Care 2002;8:316‐20. [DOI] [PubMed] [Google Scholar]
Dracup 1988 {published data only}
- Dracup K. Are critical care units hazardous to health?. Applied Nursing Research 1988;1(1):14‐21. [DOI] [PubMed] [Google Scholar]
Dritsas 2004 {published data only}
- Dritsas A, Leftheriotis D, Karabela G, Missirliadou O, Livanis EG, Theodorakis GN, et al. The effect of relaxing music on the stress dimension and the response to tilt‐test in vasovagal patients. European Heart Journal 2004;25:574. [Google Scholar]
Dubbs 2003 {published data only}
- Dubbs D. Back talk: Ergonomic furnishings help relieve strain for patients and providers. Health Facilities Management 2003;16(3):32‐6. [PubMed] [Google Scholar]
Dubois 1995 {published data only}
- Dubois JM, Bartter T, Pratter MR. Music improves patient comfort level during outpatient bronchoscopy. Chest 1995;108:129‐30. [DOI] [PubMed] [Google Scholar]
Duckworth 1988 {published data only}
- Duckworth GJ, Lothian JLE, Williams JD. Methicillin‐resistant Staphylococcus aureus: report of an outbreak in a London teaching hospital. Journal of Hospital Infection 1988;11:1‐15. [DOI] [PubMed] [Google Scholar]
Durham 1986 {published data only}
- Durham L, Collins M. The effect of music as a conditioning aid in prepared childbirth education. Journal of Obstetric, Gynecologic, and Neonatal Nursing 1986;15(3):268‐70. [DOI] [PubMed] [Google Scholar]
Dzhuraeva 1989 {published data only}
- Dzhuraeva LA, Sadykova Kh.A, Maslova GV. Music accompaniment and effectiveness of therapeutic exercise in patients with cardiovascular and respiratory pathology. Voprosy kurortologii, fizioterapii, i lechebnoi fizicheskoi kultury 1989;5:19‐22. [PubMed] [Google Scholar]
Egger 1981 {published data only}
- Egger J, Habeler G, Tinchon HJ. The effect of television on the ECG of myocardial‐infarction patients [Der einfluß von fernsehen auf das EKG von herzinfarktpatienten]. Zeitschrift Fur Experimentelle Und Angewandte Psychologie 1981;28(1):38‐53. [PubMed] [Google Scholar]
Eisenman 1995 {published data only}
- Eisenman A, Cohen B. Music therapy for patients undergoing regional anesthesia. AORN Journal 1995;62(6):947‐50. [DOI] [PubMed] [Google Scholar]
Elmståhl 1997 {published data only}
- Elmståhl S, Annerstedt L, Åhlund O. How should a group living unit for demented elderly be designed to decrease psychiatric symptoms?. Alzheimer Disease and Associated Disorders 1997;11(1):47‐52. [DOI] [PubMed] [Google Scholar]
Escher 1993 {published data only}
- Escher J, Höhmann U, Anthenien L, Dayer E, Bosshard Ch, Gaillard RC. Music during gastroscopy [Musik bei der Gastroskopie]. Schweizerische medizinische Wochenschrift 1993;123:1354‐8. [PubMed] [Google Scholar]
Evans 1994 {published data only}
- Evans MM, Rubio PA. Music: a diversionary therapy. Today's O.R. Nurse 1994;16(4):17‐22. [PubMed] [Google Scholar]
Falk 1973 {published data only}
- Falk SA, Woods NF. Hospital noise‐levels and potential health hazards. The New England Journal of Medicine 1973;289(15):774‐81. [DOI] [PubMed] [Google Scholar]
Fauerbach 2002 {published data only}
- Fauerbach JA, Lawrence JW, Haythornthwaite JA, Richter L. Coping with the stress of a painful medical procedure. Behaviour Research and Therapy 2002;40:1003‐15. [DOI] [PubMed] [Google Scholar]
Ferguson 1997 {published data only}
- Ferguson E, Singh AP, Cunningham‐Snell N. Stress and blood donation: effects of music and previous donation experience. British Journal of Psychology 1997;88:277‐94. [DOI] [PubMed] [Google Scholar]
Finkelstein 1971 {published data only}
- Finkelstein M, Rosenberg G, Grauer H. Therapeutic value of arts and crafts in a geriatric hospital. Journal of the American Geriatrics Society 1971;19(4):341‐50. [DOI] [PubMed] [Google Scholar]
Finlay 1993 {published data only}
- Finlay A, Swallow MW, McCree C. The royal group of hospitals arts and environment project. The Ulster Medical Journal 1993;63(2):153‐61. [PMC free article] [PubMed] [Google Scholar]
Fox 1986 {published data only}
- Fox J, Ford M, Fitch S, Donovan A. Psychiatric skills: Light in the darkness... the environment of patients with Alzheimer's disease. Nursing Times 1986;83(1):26‐9. [PubMed] [Google Scholar]
Frandsen 1990 {published data only}
- Frandsen JL. Music is a valuable anxiolytic during local and regional anesthesia. Nurse Anesthesia 1990;1(4):181‐2. [PubMed] [Google Scholar]
Frank 1985 {published data only}
- Frank JM. The effects of music therapy and guided visual imagery on chemotherapy induced nausea and vomiting. Oncology Nursing Forum 1985;12(5):47‐52. [PubMed] [Google Scholar]
Fratianne 2001 {published data only}
- Fratianne RB, Prensner JD, Huston MJ, Super DM, Yowler CJ, Standley JM. The effect of music‐based imagery and musical alternate engagement on the burn debridement process. Journal of Burn Care and Rehabilitation 2001;22(1):47‐53. [DOI] [PubMed] [Google Scholar]
Freeman 1987 {published data only}
- Freeman A. Evaluation: therapeutic environment. Architecture (AIA) 1987;76(1):52‐7. [PubMed] [Google Scholar]
Freireich 1975 {published data only}
- Freireich EJ. A controlled clinical trial to evaluate a protected environment and prophylactic antibiotic program in the treatment of adult acute leukemia. Transactions of the Association of American Physicians 1975;88:109. [PubMed] [Google Scholar]
Friberg 1999 {published data only}
- Friberg B, Friberg S, Burman LG. Correlation between surface and air counts of particles carrying aerobic bacteria in operating rooms with turbulent ventilation: an experimental study. Journal of Hospital Infection 1999;42:61‐8. [DOI] [PubMed] [Google Scholar]
Friberg 2003 {published data only}
- Friberg S, Ardnor B, Lundholm R, Friberg B. The addition of a mobile ultra‐clean exponential laminar airflow screen to conventional operating room ventilation reduces bacterial contamination to operating box levels. Journal of Hospital Infection 2003;55:92‐7. [DOI] [PubMed] [Google Scholar]
Frid 1981 {published data only}
- Frid IA, Berezkin DP, Evtiukhin AI, Beliaev DG, Aleksandrin GP. Hypnosis and music analgesia in the postoperative period [Gipnomyzykoanal'geziia v posle‐operatsionnom periode]. Anesteziologiia I Reanimatologiia 1981;5:30‐2. [PubMed] [Google Scholar]
Friedman 1992 {published data only}
- Friedman SB, Badere B, Fitzpatrick S. The effects of television viewing on preoperative anxiety. Journal of Post Anesthesia Nursing 1992;7(4):243‐50. [PubMed] [Google Scholar]
Gabor 2003 {published data only}
- Gabor JY, Cooper AB, Crombach SA, Lee B, Kadikar N, Bettger HE, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. American Journal of Respiratory and Critical Care Medicine 2003;167(5):708‐15. [DOI] [PubMed] [Google Scholar]
Gaffney 1986 {published data only}
- Gaffney J. Towards a less restrictive environment. Geriatric Nursing 1986;7(2):94‐5. [DOI] [PubMed] [Google Scholar]
Gast 1989 {published data only}
- Gast PL, Baker CF. The CCU patient: anxiety and annoyance to noise. Critical Care Nursing Quarterly 1989;12(3):39‐54. [DOI] [PubMed] [Google Scholar]
Girard 2004 {published data only}
- Girard NJ. Do you smell that?. AORN Journal 2004;79(6):1131‐2. [DOI] [PubMed] [Google Scholar]
Good 1978 {published data only}
- Good LR, Hurtig WE. Evaluation: a mental health facility, its users and context. AIA Journal 1978;67(2):38‐41. [PubMed] [Google Scholar]
Good 1995 {published data only}
- Good M. A comparison of the effects of jaw relaxation and music on postoperative pain. Nursing Research 1995;44(1):52‐7. [PubMed] [Google Scholar]
Good 1998 {published data only}
- Good M, Chin CC. The effects of western music on postoperative pain in Taiwan. The Kaohsiumg Journal of Medical Sciences 1998;14(2):94‐103. [PubMed] [Google Scholar]
Good 1999 {published data only}
- Good M, Stanton‐Hicks M, Grass JA, Cranston Anderson G, Choi C, Schoolmeesters LJ, et al. Relief of postoperative pain with jaw relaxation, music and their combination. Pain 1999;81:163‐72. [DOI] [PubMed] [Google Scholar]
Good 2001 {published data only}
- Good M, Stanton‐Hicks M, Grass JA, Anderson GC, Lai HL, Roykulcharoen V, et al. Relaxation and music to reduce postsurgical pain. Journal of Advanced Nursing 2001;33(2):208‐15. [DOI] [PubMed] [Google Scholar]
Good 2002 {published data only}
- Good M. Relaxation and music reduce pain after gynecologic surgery. Pain Management Nursing 2002;3(2):61‐70. [DOI] [PubMed] [Google Scholar]
Good 2005 {published data only}
- Good M, Anderson GC, Ahn S, Cong X, Stanton‐Hicks M. Relaxation and music reduce pain following intestinal surgery. Research in Nursing & Health 2005;28:240‐51. [DOI] [PubMed] [Google Scholar]
Götell 2002 {published data only}
- Götell E, Brown S, Ekman SL. Caregiver singing and background music in dementia care. Western Journal of Nursing Research 2002;24(2):195‐216. [DOI] [PubMed] [Google Scholar]
Götell 2003 {published data only}
- Götell E, Brown S, Ekman SL. Influence of caregiver singing and background music on posture, movement, and sensory awareness in dementia care. International Psychogeriatrics 2003;15(4):411‐30. [PubMed] [Google Scholar]
Gray 2000 {published data only}
- Gray DG, Smith M. Comparison of a new foam mattress with the standard hospital mattress. Journal of Wound Care 2000;9(1):29‐31. [DOI] [PubMed] [Google Scholar]
Green 1994 {published data only}
- Green J. From a macerator to a Matisse. Hospital Equipment and Supplies 1994;40(9):12‐3. [Google Scholar]
Greenberg 1992 {published data only}
- Greenberg S. Healing property. Architects' Journal 1992;195(12):28‐31, 34‐5. [Google Scholar]
Grindley 1996 {published data only}
- Grindley A, Acres J. Alternating pressure mattresses: comfort and quality of sleep. British Journal of Nursing 1996;5(21):1303‐10. [DOI] [PubMed] [Google Scholar]
Grumet 1994 {published data only}
- Grumet GW. Noise hampers healing and curbs productivity. Health Facilities Management 1994;7(1):22‐5. [PubMed] [Google Scholar]
Guétin 2005 {published data only}
- Guétin S, Coudeyre E, Picot MC, Ginies P, Graber‐Duvernay B, Ratsimba D, et al. Effect of music therapy among hospitalized patients with chronic low back pain: A controlled, randomized trial [Intérêt de la musicothérapie dans la prise en charge de la lombalgie chronique en milieu hospitalier (Étude contrôlée, randomisée sur 65 patients)]. Annales de Réadaptation et de Médecine Physique 2005;48:217‐24. [DOI] [PubMed] [Google Scholar]
Guillemin 2000 {published data only}
- Guillemin E, Delatte AC, Germain M, Kroell F, Guillemin F. Therapeutic usefulness of an art exposition area in a health care institution [De l'utilite therapeutique d'un espace d'exposition artistique dans un etablissement de soins]. Bulletin du Cancer 2000;87(12):941‐7. [PubMed] [Google Scholar]
Gulledge 1981 {published data only}
- Gulledge SL, Kline OR. Use of stereo headphones for patient relaxation during cataract surgery under local anesthesia. Ophthalmic Surgery 1981;12(4):289‐90. [PubMed] [Google Scholar]
Gundermann 1974 {published data only}
- Gundermann KO. Artificial‐ventilation and bacterial concentration in hospital [Künstliche belüftung und luftkeimgehalt im krankenhaus]. Zentralblatt fur Bakteriologie, Parasitenkunde, Infektionskrankheiten und Hygiene. Erste Abteilung Originale. Reihe A Medizinische Mikrobiologie und Parasitologie 1974;227(1‐4):542‐7. [PubMed] [Google Scholar]
Gurr 1997 {published data only}
- Gurr V. Vidarkliniken and the architecture of healing. Transition 1997;54‐55:54‐61. [Google Scholar]
Guzzetta 1989 {published data only}
- Guzzetta CE. Effects of relaxation and music therapy on patients in a coronary care unit with presumptive acute myocardial infarction. Heart & Lung 1989;18:609‐16. [PubMed] [Google Scholar]
Haddock 1994 {published data only}
- Haddock J. Reducing the effects of noise in hospital. Nursing Standard 1994;8(43):25‐8. [DOI] [PubMed] [Google Scholar]
Hagerman 2005 {published data only}
- Hagerman I, Rasmanis G, Blomkvist V, Ulrich R, Eriksen CA, Theorell T. Influence of intensive coronary care acoustics on the quality of care and physiological state of patients. International Journal of Cardiology 2005;98:267‐70. [DOI] [PubMed] [Google Scholar]
Hahn 1995 {published data only}
- Hahn JE, Jones MR, Waszkiewicz M. Renovation of a semiprivate patient room. Nursing Clinics of North America 1995;30(1):97‐115. [PubMed] [Google Scholar]
Hamel 2001 {published data only}
- Hamel WJ. The effects of music intervention on anxiety in the patient waiting for cardiac catheterization. Intensive and Critical Care Nursing 2001;17:279‐85. [DOI] [PubMed] [Google Scholar]
Hanger 1999 {published data only}
- Hanger HC, Ball MC, Wood LA. An analysis of falls in the hospital: can we do without bedrails?. Journal of the American Geriatrics Society 1999;47(5):529‐31. [DOI] [PubMed] [Google Scholar]
Harmankaya 2002 {published data only}
- Harmankaya O, Cetin B, Erimez D, Obek A, Seber E. Patient isolation prevents the transmission of hepatitis C virus infection in hemodialysis units. Dialysis & Transplantation 2002;31(12):859‐61. [Google Scholar]
Harris 1992 {published data only}
- Harris CS, Bradley RJ, Titus SK. A comparison of the effects of hard rock and easy listening on the frequency of observed inappropriate behaviors: a control of environmental antecedents in a large public area. Journal of Music Therapy 1992;29(1):6‐17. [DOI] [PubMed] [Google Scholar]
Harrison 1989 {published data only}
- Harrison DW, Zicafoose BF, Francis JA, Lanter JJ. Contextual therapy for chronic bruxism in patients with advanced dementia. Neuropsychiatry, Neuropsychology, and Behavioral Neurology 1989;2(3):183‐8. [Google Scholar]
Harvey 1998 {published data only}
- Harvey MA. Critical‐care‐unit bedside design and furnishings: impact on nosocomial infections. Infection Control and Hospital Epidemiology 1998;19(8):597‐601. [DOI] [PubMed] [Google Scholar]
Harwood 1992 {published data only}
- Harwood RH, Ebrahim S. Long‐term institutional residents: does the environment affect outcomes?. Journal of the Royal College of Physicians of London 1992;26(2):134‐8. [PMC free article] [PubMed] [Google Scholar]
Hashiguchi 2005 {published data only}
- Hashiguchi N, Hirakawa M, Tochihara Y, Kaji Y, Karaki C. Thermal environment and subjective responses of patients and staff in a hospital during winter. Journal of Physiological Anthropology and Applied Human Science 2005;24(1):111‐5. [DOI] [PubMed] [Google Scholar]
Haslam 1970 {published data only}
- Haslam P. Caring for the total patient. Noise in hospitals: its effect on the patient. Nursing Clinics of North America 1970;5(4):715‐24. [PubMed] [Google Scholar]
Haun 2001 {published data only}
- Haun M, Mainous RO, Looney SW. Effect of music on anxiety of women awaiting breast biopsy. Behavioral Medicine 2001;27(3):127‐32. [DOI] [PubMed] [Google Scholar]
Haythornthwaite 2001 {published data only}
- Haythornthwaite JA, Lawrence JW, Fauerbach JA. Brief cognitive interventions for burn pain. Annals of Behavioral Medicine 2001;23(1):42‐9. [DOI] [PubMed] [Google Scholar]
Heiser 1997 {published data only}
- Heiser RM, Chiles K, Fudge M, Gray SE. The use of music during the immediate postoperative period. AORN Journal 1997;65(4):777‐85. [DOI] [PubMed] [Google Scholar]
Helmes 2006 {published data only}
- Helmes E, Wiancko DC. Effects of music in reducing disruptive behavior in a general hospital. Journal of the American Psychiatric Nurses Association 2006;12(1):37‐44. [Google Scholar]
Hendrich 2004 {published data only}
- Hendrich AL, Sorrells AK. Effects of acuity‐adaptable rooms on flow of patients and delivery of care. American Journal of Critical Care 2004;13:35‐45. [PubMed] [Google Scholar]
Herr 2003 {published data only}
- Herr CEW, Heckrodt TH, Hofmann FA, Schnettler R, Eikmann TF. Additional costs for preventing the spread of Methicillin‐Resistant Staphylococcus Aureus and a strategy for reducing these costs on a surgical ward. Infection Control and Hospital Epidemiology 2003;24(9):673‐8. [DOI] [PubMed] [Google Scholar]
Hewawasam 1996 {published data only}
- Hewawasam L. Floor patterns limit wandering of people with Alzheimer's. Nursing Times 1996;92(23):41‐4. [PubMed] [Google Scholar]
Hilton 1976 {published data only}
- Hilton BA. Quantity and quality of patients' sleep and sleep‐disturbing factors in a respiratory intensive care unit. Journal of Advanced Nursing 1976;1:453‐68. [DOI] [PubMed] [Google Scholar]
Hilton 1985 {published data only}
- Hilton BA. Noise in acute patient care areas. Research in Nursing & Health 1985;8:283‐91. [DOI] [PubMed] [Google Scholar]
Hinojosa 1995 {published data only}
- Hinojosa RJ. A research critique. Intraoperative music therapy: effects on anxiety, blood pressure. Plastic Surgery Nursing 1995;15(4):228‐31. [DOI] [PubMed] [Google Scholar]
Hoffman 2000 {published data only}
- Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. The Clinical Journal of Pain 2000;16:244‐50. [DOI] [PubMed] [Google Scholar]
Hoffman 2001 {published data only}
- Hoffman HG, Patterson DR, Carrougher GJ, Sharar SR. The effectiveness of virtual reality based pain control with muliple treatments. Clinical Journal of Pain 2001;17:229‐35. [DOI] [PubMed] [Google Scholar]
Holahan 1972 {published data only}
- Holahan C. Seating patterns and patient behavior in an experimental dayroom. Journal of Abnormal Psychology 1972;80(2):115‐24. [DOI] [PubMed] [Google Scholar]
Holahan 1973 {published data only}
- Holahan CJ, Saegert S. Behavioral and attitudinal effects of large‐scale variation in the physical environment of psychiatric wards. Journal of Abnormal Psychology 1973;82(3):454‐62. [DOI] [PubMed] [Google Scholar]
Holahan 1976 {published data only}
- Holahan CJ. Environmental change in a psychiatric setting: a social systems analysis. Human Relations 1976;29(2):153‐66. [Google Scholar]
Holden 1992 {published data only}
- Holden G, Speedling E, Rosenberg G. Evaluation of an intervention designed to improve patients' hospital experience. Psychological Reports 1992;71:547‐50. [DOI] [PubMed] [Google Scholar]
Homicki 2004 {published data only}
- Homicki B, Joyce EK. Art illuminates patients' experience at the Massachusetts General Hospital Cancer Center. The Oncologist 2004;9:111‐4. [DOI] [PubMed] [Google Scholar]
Hooper 1992 {published data only}
- Hooper J, Lindsay B. Improving the quality of life through music: a case study. Mental Handicap 1992;20:27‐30. [Google Scholar]
Hsu 1998 {published data only}
- Hsu RK, Veridiano M, Inciardi J, Soares P, Stefani C, Leung J. The impact of music on the anxiety level of patients undergoing outpatient endoscopy ‐ a prospective randomized controlled study. Gastrointestinal Endoscopy 1998;47(4):AB52. [Google Scholar]
Hudson 1995 {published data only}
- Hudson R. Use of lavender in a long‐term elderly ward. Nursing Times 1995;91(1):12. [Google Scholar]
Hudson 1996 {published data only}
- Hudson R. The value of lavender for rest and activity in the elderly patient. Complementary Therapies in Medicine 1996;4:52‐7. [Google Scholar]
Huffman 1994 {published data only}
- Huffman CS, Deaton JL. The use of music in reducing pain and anxiety in patients undergoing transvaginal oocyte aspiration (TVOA). Fertility and Sterility‐ International Edition 1994;62(4):S50. [Google Scholar]
Hussian 1987 {published data only}
- Hussian RA, Brown DC. Use of two‐dimensional grid patterns to limit hazardous ambulation in demented patients. Journal of Gerontology 1987;42(5):558‐60. [DOI] [PubMed] [Google Scholar]
Hyde 1989 {published data only}
- Hyde J. The physical environment and the care of Alzheimer's patients: an experiential survey of Massachusetts' Alzheimer's units. The American Journal of Alzheimer's Care and Related Disorders & Research 1989;4:36‐44. [Google Scholar]
Ingham 1997 {published data only}
- Ingham B, Spencer C. 1997 [Do comfortable chairs and soft lights in the waiting area really help reduce anxiety and improve the practice's image?]. Health Psychology Update 1997;28:17‐20. [Google Scholar]
Itai 2000 {published data only}
- Itai T, Amayasu H, Kuribayashi M, Kawamura N, Okada M, Momose A, et al. Psychological effects of aromatherapy on chronic hemodialysis patients. Psychiatry and Clinical Neurosciences 2000;54:393‐7. [DOI] [PubMed] [Google Scholar]
Ittelson 1970 {published data only}
- Ittelson WH, Proshansky HM, Rivlin LG. Bedroom size and social interaction of the psychiatric ward. Environment and Behavior 1970;2:255‐70. [Google Scholar]
Jacobs 1974 {published data only}
- Jacobs KW, Hustmyer FE. Effects of four psychological primary colors on GSR, heart rate and respiration rate. Perceptual and Motor Skills 1974;38:763‐6. [DOI] [PubMed] [Google Scholar]
Janelli 1997 {published data only}
- Janelli LM, Kanski GW. Music intervention with physically restrained patients. Rehabilitation Nursing 1997;22(1):14‐9. [DOI] [PubMed] [Google Scholar]
Janelli 1998 {published data only}
- Janelli LM, Kanski G. Music for untying restrained patients. Journal of the New York State Nurses Association 1988;29(1):13‐5. [PubMed] [Google Scholar]
Janelli 2000 {published data only}
- Janelli L, Kanski G. The use of music to release the ties that bind. Perspectives 2000;24(2):2‐7. [PubMed] [Google Scholar]
Janelli 2002 {published data only}
- Janelli LM, Kanski GW, Wu YWB. Individualized music‐ a different approach to the restraint issue. Rehabilitation Nursing 2002;27(6):221‐6. [DOI] [PubMed] [Google Scholar]
Janelli 2004 {published data only}
- Janelli LM, Kanski GW, Wu YWB. The influence of individualized music on patients in physical restraints: a pilot study. Journal of the New York State Nurses Association 2004/2005;35(2):22‐7. [PubMed] [Google Scholar]
Janiszewski 1980 {published data only}
- Janiszewski M. Analysis of emotional‐aesthetic experiences including certain circulatory system parameters in patients with essential hypertension subjected to the action of music [Analiza przeżycia emocjonalno‐estetycznego z uwzględnieniem niektórych parametrów układu krążenia u chorych na nadciśnienie pierwotne poddawanych działaniu muzyki]. Wiadomosci Lekarskie 1980;33(5):335‐8. [PubMed] [Google Scholar]
Janssen 2000 {published data only}
- Janssen PA, Klein MC, Harris SJ, Soolsma J, Seymour LC. Single room maternity care and client satisfaction. Birth 2000;27:235‐43. [DOI] [PubMed] [Google Scholar]
Janssen 2001 {published data only}
- Janssen PA, Harris SJ, Soolsma J, Klein MC, Seymour LC. Single room maternity care: the nursing response. Birth 2001;28(3):173‐9. [DOI] [PubMed] [Google Scholar]
Jarvis 1979 {published data only}
- Jarvis PA, Butt JH. Preparation for endoscopy IV. Imagery and music do not diminish anxiety in patients with differing coping styles for stress during upper gastro‐intestinal endoscopy. Gastroenterology 1979;76(5, Part 2):1160. [Google Scholar]
Jastremski 1998 {published data only}
- Jastremski CA, Harvey M. Making changes to improve the intensive care unit experience for patients and their families. New Horizons: The Science and Practice of Acute Medicine 1998;6(1):99‐109. [PubMed] [Google Scholar]
Jonas 1988 {published data only}
- Jonas SE. Effects of music on day stay surgery patients. Dissertations Abstracts International 1988;4905B:1616. [Google Scholar]
Kaempf 1989 {published data only}
- Kaempf G, Amodei ME. The effect of music on anxiety: a research study. AORN Journal 1989;50(1):112‐8. [DOI] [PubMed] [Google Scholar]
Kaiming 1997 {published data only}
- Kaiming Z, Shuping D, Xiaofen Y. Use of music in nursing care of induced abortion. Shanxi Nursing Journal 1997;11(4):159‐60. [Google Scholar]
Kaldenberg 1999 {published data only}
- Kaldenberg DO. The influence of having a roommate on patient satisfaction. The Satisfaction Monitor. Press Ganey Associates, Inc, 1999; Vol. Jan/Feb:3‐4.
Kam 1994 {published data only}
- Kam PCA, Kam AC, Thompson JF. Noise pollution in the anaesthetic and intensive care environment. Anaesthesia 1994;49:982‐6. [DOI] [PubMed] [Google Scholar]
Kane 2004 {published data only}
- Kane FMA, Brodie EE, Coull A, Coyne L, Howd A, Milne A, et al. The analgesic effect of odour and music upon dressing change. British Journal of Nursing 2004;13(19):S4‐S12. [DOI] [PubMed] [Google Scholar]
Karro 2005 {published data only}
- Karro J, Dent AW, Farish S. Patient perceptions of privacy infingements in an emergency department. Emergency Medicine Australasia 2005;17:117‐23. [DOI] [PubMed] [Google Scholar]
Kartman 1984 {published data only}
- Kartman LL. Music hath charms. Journal of Gerontological Nursing 1984;10(6):20‐4. [DOI] [PubMed] [Google Scholar]
Keep 1980 {published data only}
- Keep P, James J, Inman M. Windows in the intensive therapy unit. Anaesthesia 1980;35:257‐62. [DOI] [PubMed] [Google Scholar]
Kibbler 1998 {published data only}
- Kibbler CC, Quick A, O'Neill A‐M. The effect of increased bed numbers on MRSA transmission in acute medical wards. Journal of Hospital Infection 1998;39:213‐9. [DOI] [PubMed] [Google Scholar]
Kim 1997 {published data only}
- Kim KC, Kim KM. A study on the architectural planning for communication of inpatient and nurse in ward of general hospital. Journal‐ Architectural Institute of Korea 1997;13(10):103‐12. [Google Scholar]
Kim 2005 {published data only}
- Kim SJ, Koh I. The effects of music on pain perception of stroke patients during upper extremity joint exercises. Journal of Music Therapy 2005;42(1):81‐92. [Google Scholar]
Kimata 2003 {published data only}
- Kimata H. Listening to Mozart reduces allergic skin wheal responses and in vitro allergen‐specific IgE production in atopic dermatitis patients with latex allergy. Behavioral Medicine 2003;29(1):15‐9. [DOI] [PubMed] [Google Scholar]
Kirkpatrick 1998 {published data only}
- Kirkpatrick J, Wood J. Aromatherapy's benefits. Journal of Dementia Care 1998;6(3):9. [Google Scholar]
Knobel 1985 {published data only}
- Knobel L. Patients rewarded. Designers' Journal 1985;10:50‐3. [Google Scholar]
Kolanowski 1990 {published data only}
- Kolanowski AM. Restlessness in the elderly: the effect of artificial lighting. Nursing Research 1990;39(3):181‐3. [PubMed] [Google Scholar]
Kopp 1991 {published data only}
- Kopp MR. Music's affect on stress‐related responses during surgery. The Kansas Nurse 1991;66(7):4‐5. [PubMed] [Google Scholar]
Kovach 1997 {published data only}
- Kovach C, Weisman G, Chaudhury H, Calkins M. Impacts of a therapeutic environment for dementia care. American Journal of Alzheimer's Disease 1997;12(3):99‐110. [Google Scholar]
Kulik 1996 {published data only}
- Kulik JA, Mahler HIM, Moore PJ. Social comparison and affiliation under threat: effects on recovery from major surgery. Journal of Personality and Social Psychology 1996;71(5):967‐79. [DOI] [PubMed] [Google Scholar]
Kumar 1992 {published data only}
- Kumar A, Bajaj A, Sarkar P, Grover VK. The effect of music on ketamine induced emergence phenomena. Anaesthesia 1992;47:438‐9. [DOI] [PubMed] [Google Scholar]
Kwon 2006 {published and unpublished data}
- Kwon S, Kim J, Park KM. Effects of music therapy on pain, discomfort, and depression for patients with leg fractures. Journal of Korean Academy of Nursing 2006;36(4):630‐6. [DOI] [PubMed] [Google Scholar]
Lai 1999 {published data only}
- Lai YM. Effects of music listening on depressed women in Taiwan. Issues in Mental Health Nursing 1999;20:229‐46. [DOI] [PubMed] [Google Scholar]
Lai 2001 {published data only}
- Lai KK. A cluster of invasive aspergillosis in a bone marrow transplant unit related to construction and the utility of air sampling. American Journal of Infection Control 2001;29:333‐7. [DOI] [PubMed] [Google Scholar]
Lai 2005 {published data only}
- Lai HL, Good M. Music improves sleep quality in older adults. Journal of Advanced Nursing 2005;49(3):234‐44. [DOI] [PubMed] [Google Scholar]
Lai 2006 {published data only}
- Lai HL, Good M. Music improves sleep quality in older adults. Journal of Advanced Nursing 2006;53(1):134‐44. [DOI] [PubMed] [Google Scholar]
Laitinen 1994 {published data only}
- Laitinen P. Elderly patients' and their informal caregivers' perceptions of care given: the study‐control ward design. Journal of Advanced Nursing 1994;20:71‐6. [DOI] [PubMed] [Google Scholar]
Lamont 1975 {published data only}
- Lamont IRD, Hunt PS. A study of noise stress in a public hospital. Australian and New Zealand Journal of Surgery 1975;45(4):429. [Google Scholar]
Lan‐Ping 2000 {published data only}
- Lan‐ping W, Li‐zhi P, Jing‐ru W. Effects of noise on physical indicators of surgical patients. Chinese Journal of Nursing 2000;35(11):650‐2. [Google Scholar]
Larsson 1991 {published data only}
- Larsson G, Berg V. Linen in the hospital bed: effects on patients' well‐being. Journal of Advanced Nursing 1991;16:1004‐8. [DOI] [PubMed] [Google Scholar]
Laurion 2003 {published data only}
- Laurion S, Fetzer SJ. The effect of two nursing interventions on the postoperative outcomes of gynecologic laparoscopic patients. Journal of PeriAnesthesia Nursing 2003;18(4):254‐61. [DOI] [PubMed] [Google Scholar]
Lawson 2000 {published data only}
- Lawson B, Phiri M. Hospital design: Room for improvement. Health Service Journal 2000;110(5688):24‐6. [PubMed] [Google Scholar]
Lawson 2002 {published data only}
- Lawson B, Wells‐Thorpe J. The effect of the hospital environment on the patient experience and health outcomes. Hospital Development 2002;33(3):27‐32. [Google Scholar]
Lawson 2003 {published data only}
- Lawson B, Phiri M, Wells‐Thorpe J. The architectural healthcare environment and its effects on patient health outcomes. London: The Stationery Office, 2003. [Google Scholar]
Lawton 1970 {published data only}
- Lawton MP, Liebowitz B, Charon H. Physical structure and the behavior of senile patients following ward remodeling. Aging and Human Development 1970;1:231‐9. [Google Scholar]
Lazaroff 2000 {published data only}
- Lazaroff I, Shimshoni R. Effects of medical resonance therapy music on patients with psoriasis and neurodermatitis: a pilot study. Integrative Physiological and Behavioral Science 2000;35(3):189‐98. [DOI] [PubMed] [Google Scholar]
Leão 2004 {published data only}
- Leão ER, Silva MJ. Music and chronic muscular‐skeletal pain: the evocative potential of mental images [Música e dor crônica músculoesquelética: o potencial evocativo de imagens mentais]. Revista Latino Americana de Enfermagem 2004;12(2):235‐41. [DOI] [PubMed] [Google Scholar]
Leather 2003 {published data only}
- Leather P, Beale D, Santos A, Watts J, Lee L. Outcomes of environmental appraisal of different hospital waiting areas. Environment and Behavior 2003;35(6):842‐69. [Google Scholar]
Lee 2004b {published data only}
- Lee D, Henderson A, Shum D. The effect of music on preprocedure anxiety in Hong Kong Chinese day patients. Journal of Clinical Nursing 2004;13:297‐303. [DOI] [PubMed] [Google Scholar]
Legg 1970 {published data only}
- Legg RC. Air transfer in hospital bedrooms. Building Science 1970;5:41‐50. [Google Scholar]
Lehrner 2000 {published data only}
- Lehrner J, Eckersberger C, Walla P, Pötsch G, Deecke L. Ambient odor of orange in a dental office reduces anxiety and improves mood in female patients. Physiology and Behavior 2000;71:83‐6. [DOI] [PubMed] [Google Scholar]
Leigh 1972 {published data only}
- Leigh H, Hofer MA, Cooper J, Reiser MF. A psychological comparison of patients in "open" and "closed" coronary care units. Journal of Psychosomatic Research 1972;16:449‐57. [DOI] [PubMed] [Google Scholar]
Levin 1987 {published data only}
- Levin RF, Malloy GB, Hyman RB. Nursing management of postoperative pain: use of relaxation techniques with female cholecystectomy patients. Journal of Advanced Nursing 1987;12:463‐72. [DOI] [PubMed] [Google Scholar]
Levine 1973 {published data only}
- Levine AS, Siegel SE, Schreiber AD, Hauser J, Preisler H, Goldstein IM, et al. Protected environments and prophylactic antibiotics. A prospective controlled study of their utility in the therapy of acute leukemia. The New England Journal of Medicine 1973;288(10):477‐83. [DOI] [PubMed] [Google Scholar]
Lewis 1999 {published data only}
- Lewis AM, Gammon J, Hosein I. The pros and cons of isolation and containment. Journal of Hospital Infection 1999;43:19‐23. [DOI] [PubMed] [Google Scholar]
Lidwell 1966 {published data only}
- Lidwell OM, Polakoff S, Jevons MP, Parker MT, Shooter RA, French VI, et al. Staphylococcal infection in thoracic surgery: experience in a subdivided ward. Journal of Hygiene 1966;64(3):321‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lidwell 1969 {published data only}
- Lidwell OM, Towers AG. Protection from microbial contamination in a room ventilated by a uni‐directional air flow. Journal of Hygiene 1969;67:95‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lidwell 1975 {published data only}
- Lidwell OM, Brock B, Shooter RA, Cooke EM, Thomas GE. Airborne infection in a fully air‐conditioned hospital. IV. Airborne dispersal of Staphylococcus aureus and its nasal acquisition by patients. Journal of Hygiene 1975;75:445‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lidwell 1982 {published data only}
- Lidwell OM, Lowbury EJL, Whyte W, Blowers R, Stanley SJ, Lowe D. Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. British Medical Journal 1982;285:10‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lidwell 1984 {published data only}
- Lidwell OM, Lowbury EJL, Whyte W, Blowers R, Stanley SJ, Lowe D. Infection and sepsis after operations for total hip or knee‐joint replacement: influence of ultraclean air, prophylactic antibiotics and other factors. Journal of Hygiene 1984;93(3):505‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liebowitz 1979 {published data only}
- Liebowitz B, Lawton MP, Waldman A. Evaluation: designing for confused elderly people. American Institute of Architects Journal 1979;68(2):59‐61. [PubMed] [Google Scholar]
Litch 2006 {published data only}
- Litch B. The healing power of art: Art displays in hospitals reduce stress, improve outcomes. Healthcare Executive 2006;Sept/Oct:34‐7. [PubMed] [Google Scholar]
Locsin 1979 {published data only}
- Locsin RGRAC. The effect of music on the pain of selected postoperative patients. The ANPHI Papers 1979;14:1‐10. [PubMed] [Google Scholar]
Locsin 1981 {published data only}
- Locsin RGRAC. The effect of music on the pain of selected post‐operative patients. Journal of Advanced Nursing 1981;6:19‐25. [DOI] [PubMed] [Google Scholar]
Locsin 1988 {published data only}
- Locsin RG. Effects of preferred music and guided imagery music on the pain of selected post‐operative patients. ANPHI Papers 1988;23(1):2‐4. [PubMed] [Google Scholar]
Lomas 1987 {published data only}
- Lomas CJ. Theatre design and behaviour of staff determining the number of bacteria during surgery. NAT News 1987;24(2):9‐11. [PubMed] [Google Scholar]
Louis 2002 {published data only}
- Louis M, Kowalski SD. Use of aromatherapy with hospice patients to decrease pain, anxiety, and depression and to promote an increased sense of well‐being. American Journal of Hospice & Palliative Care 2002;19(6):381‐6. [DOI] [PubMed] [Google Scholar]
Lowbury 1971 {published data only}
- Lowbury EJL, Babb JR, Ford PM. Protective isolation in a burns unit: the use of plastic isolators and air curtains. Journal of Hygiene 1971;69(4):529‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowbury 1978 {published data only}
- Lowbury EJL, Lidwell OM. Multi‐hospital trial on the use of ultraclean air systems in orthopaedic operating rooms to reduce infection: preliminary communication. Journal of the Royal Society of Medicine 1978;71:800‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 1998 {published data only}
- Martin DP, Diehr P, Conrad DA, Hunt Davis J, Leickly R, Perrin EB. Randomized trial of a patient‐centered hospital unit. Patient Education and Counseling 1998;34:125‐33. [DOI] [PubMed] [Google Scholar]
Martin 1999 {published data only}
- Martin C. "Let me through ‐ I'm an arts practitioner!". The Lancet 1999;353(9162):1451. [DOI] [PubMed] [Google Scholar]
May 1984 {published data only}
- May SR, Ehleben CM, DeClement FA. Delirium in burn patients isolated in a plenum laminar air flow ventilation unit. Burns 1984;10:331‐8. [DOI] [PubMed] [Google Scholar]
Mayer 1991 {published data only}
- Mayer R, Darby SJ. Does a mirror deter wandering in demented older people?. International Journal of Geriatric Psychiatry 1991;6:607‐9. [Google Scholar]
McCaffrey 2004 {published data only}
- McCaffrey R, Locsin R. The effect of music listening on acute confusion and delirium in elders undergoing elective hip and knee surgery. International Journal of Older People Nursing 2004;13(6b):91‐6. [DOI] [PubMed] [Google Scholar]
McConnell 2005 {published data only}
- McConnell KJ, Richards CF, Daya M, Bernell SL, Weathers CC, Lowe RA. Effect of increased ICU capacity on emergency department length of stay and ambulance diversion. Annals of Emergency Medicine 2005;45(5):471‐8. [DOI] [PubMed] [Google Scholar]
McGonagle 2002 {published data only}
- McGonagle IM, Allan S. A comparison of behaviour in two differing psychiatric long‐stay rehabilitation environments. Journal of Psychiatric and Mental Health Nursing 2002;9:493‐9. [DOI] [PubMed] [Google Scholar]
McKendrick 1976 {published data only}
- McKendrick GDW, Emond RTD. Investigation of cross‐infection in isolation wards of different design. Journal of Hygiene 1976;76(1):23‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
McLaughlin 1976 {published data only}
- McLaughlin H. Evaluating the effectiveness of innovative design for a community mental health center. Hospital & Community Psychiatry 1976;27(8):566‐71. [DOI] [PubMed] [Google Scholar]
McNaughton 2005 {published data only}
- McNaughton J, White M, Collins P, Coleman S, Purves G, Kellett P, et al. Designing for Health: Architecture, Art and Design at the James Cook University Hospital. Universities of Durham and Newcastle upon Tyne, 2005. [Google Scholar]
Mellgren 1967 {published data only}
- Mellgren A. Distraction anesthesia (audioanalgesia) in "minor gynecology" [Distraktionsanasthesie (Audio‐Analgesie) in der "kleinen Gynakologie"]. Munchener Medizinische Wochenschrift 1967;109(33):1693‐6. [PubMed] [Google Scholar]
Mellor 2001 {published data only}
- Mellor I. Art therapy: art of healing. Community Practitioner 2001;74(9):325‐7. [Google Scholar]
Metera 1975a {published data only}
- Metera A, Metera A. Influence of music on the minute oxygen consumption and basal rate. Anaesthia Resuscitation and Intensive Therapy 1975;3(3):255‐64. [PubMed] [Google Scholar]
Metera 1975b {published data only}
- Metera A, Metera A, Warwas I. Effect of music on airway resistance in patients. Anaesthia Resuscitation and Intensive Therapy 1975;3(3):265‐9. [PubMed] [Google Scholar]
Meyer 1994 {published data only}
- Meyer TJ, Eveloff SE, Bauer MS, Schwartz WA, Hill NS, Millman RP. Adverse environmental conditions in the respiratory and medical ICU settings. Chest 1994;105(4):1211‐6. [DOI] [PubMed] [Google Scholar]
Middelboe 2001 {published data only}
- Middelboe T, Schjødt T, Byrsting K, Gjerris A. Ward atmosphere in acute psychiatric in‐patient care: patients' perceptions, ideals and satisfaction. Acta Psychiatrica Scandinavica 2001;103:212‐9. [DOI] [PubMed] [Google Scholar]
Mihara 2005 {published data only}
- Mihara Y, Kurihara M, Takahashi Y, Aizawa S, Nagashima T, Takao M, et al. 0440 The effect of music therapy for patients with amyotrophic lateral sclerosis. Journal of the Neurological Sciences 2005;238(Supplement 1):S210. [Google Scholar]
Miller 1998 {published data only}
- Miller NO, Friedman SB, Coupey SM. Adolescent preferences for rooming during hospitalization. Journal of Adolescent Health 1998;23:89‐93. [DOI] [PubMed] [Google Scholar]
Miluk‐Kolasa 1994 {published data only}
- Miluk‐Kolasa B, Obminski Z, Stupnicki R, Golec L. Effects of music treatment on salivary cortisol in patients exposed to pre‐surgical stress. Experimental and Clinical Endocrinology 1994;102:118‐20. [DOI] [PubMed] [Google Scholar]
Miluk‐Kolasa 1996 {published data only}
- Miluk‐Kolasa B, Matejek M, Stupnicki R. The effects of music listening on changes in selected physiological parameters in adult pre‐surgical patients. Journal of Music Therapy 1996;33(3):208‐18. [Google Scholar]
Miluk‐Kolasa 2002 {published data only}
- Miluk‐Kolasa B, Klodecka‐Rózalska J, Stupnicki R. The effect of music listening on perioperative anxiety levels in adult surgical patients. Polish Psychological Bulletin 2002;33(2):55‐60. [Google Scholar]
Mok 2003 {published data only}
- Mok E, Wong KY. Effects of music on patient anxiety: research. AORN Journal 2003;77(2):396‐7, 401‐6, 409‐10. [DOI] [PubMed] [Google Scholar]
Moore 1998 {published data only}
- Moore MM, Nguyen D, Nolan SP, Robinson SP, Ryals B, Imbrie JZ, et al. Interventions to reduce decibel levels on patient care units. The American Surgeon 1998;64(9):894‐9. [PubMed] [Google Scholar]
Morgan 1998 {published data only}
- Morgan DG, Stewart NJ. Multiple occupancy versus private rooms on dementia care units. Environment and Behavior 1998;30(4):487‐503. [Google Scholar]
Morris 1970 {published data only}
- Morris RH, Wilkey BR. The effects of ambient temperature on patient temperature during surgery not involving body cavities. Anesthesiology 1970;32(2):102‐7. [DOI] [PubMed] [Google Scholar]
Morsley 1999 {published data only}
- Morsley P, Peachey J. Landscaping: the natural law. Hospital Development 1999;30(9):19‐20. [Google Scholar]
Moss 1987 {published data only}
- Moss VA. The effect of music on anxiety in the surgical patient. Perioperative Nursing Quarterly 1987;3(1):9‐16. [PubMed] [Google Scholar]
Moss 1988 {published data only}
- Moss VA. Music and the surgical patient: the effect of music on anxiety. AORN Journal 1988;48(1):64‐9. [DOI] [PubMed] [Google Scholar]
Mulin 1997 {published data only}
- Mulin B, Rouget C, Clément C, Bailly P, Julliot M‐C, Viel J‐FF, et al. Association of private isolation rooms with ventilator‐associated acinetobacter baumanii pneumonia in a surgical intensive‐care unit. Infection Control and Hospital Epidemiology 1997;18(7):499‐503. [DOI] [PubMed] [Google Scholar]
Murrock 2002 {published data only}
- Murrock CJ. The effects of music on the rate of perceived exertion and general mood among coronary artery bypass graft patients enrolled in cardiac rehabilitation phase II. Rehabilitation Nursing 2002;27(6):227‐31. [DOI] [PubMed] [Google Scholar]
Namazi 1989 {published data only}
- Namazi KH, Rosner TT, Calkins MP. Visual barriers to prevent ambulatory alzheimer's patients from exiting through an emergency door. The Gerontologist 1989;29(5):699‐702. [DOI] [PubMed] [Google Scholar]
Nauseef 1981 {published data only}
- Nauseef WM, Maki DG. A study of the value of simple protective isolation in patients with granulocytopenia. The New England Journal of Medicine 1981;304:448‐53. [DOI] [PubMed] [Google Scholar]
Nelson Negley 1990 {published data only}
- Nelson Negley E, Molla PM, Obenchain J. No exit: the effects of an electronic security system on confused patients. Journal of Gerontological Nursing 1990;16(8):21‐5. [DOI] [PubMed] [Google Scholar]
Nixon 2006 {published data only}
- Nixon J, Cranny G, Iglesias C, Nelson EA, Hawkins K, Phillips A, et al. Randomised, controlled trial of alternating pressure mattresses compared with alternating pressure overlays for the prevention of pressure ulcers: PRESSURE (pressure relieving support surfaces) trial. BMJ 2006;332(7555):1413‐5. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norberg 1986 {published data only}
- Norberg A, Melin E, Asplund K. Reactions to music, touch and object presentation in the final stage of dementia, an exploratory study. International Journal of Nursing Studies 1986;23(4):315‐23. [DOI] [PubMed] [Google Scholar]
Noskin 2001 {published data only}
- Noskin GA, Peterson LR. Engineering infection control through facility design. Emerging Infectious Diseases 2001;7(2):354‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Notelovitz 1978 {published data only}
- Notelovitz M. The single‐unit delivery system‐ a safe alternative to home deliveries. American Journal of Obstetric Gynaecology 1978;132(8):889‐94. [DOI] [PubMed] [Google Scholar]
Oberle 1990 {published data only}
- Oberle K, Wry J, Paul P, Grace M. Environment, anxiety, and postoperative pain. Western Journal of Nursing Research 1990;12(6):745‐57. [DOI] [PubMed] [Google Scholar]
Okada 1986 {published data only}
- Okada S, Shoda M. A study on storage of patients' personal belongings at a hospital environment. Kurinikaru‐Sutadi (Clinical Study) 1986;7(8):881‐7. [PubMed] [Google Scholar]
Okamoto 2002 {published data only}
- Okamoto K, Nagasawa Y. Effects of the environment on patients' behavior and communication studied through the moving of a psychiatric hospital. Journal of Architecture Planning and Environmental Engineering 2002;559:125‐30. [Google Scholar]
Olsen 1984 {published data only}
- Olsen RV. The effect of the hospital environment: patient reactions to traditional versus progressive care settings. Journal of Achitectural and Planning Research 1984;1:121‐36. [Google Scholar]
Oyama 2000 {published data only}
- Oyama H, Kaneda M, Katsumata N, Akechi T, Ohsuga M. Using the Bedside Wellness System during chemotherapy decreases fatigue and emesis in cancer patients. Journal of Medical Systems 2000;24(3):173‐82. [DOI] [PubMed] [Google Scholar]
Palmer 1998 {published data only}
- Palmer RM, Counsell S, Landefeld CS. Clinical intervention trials: the ACE unit. Clinics in Geriatric Medicine 1998;14(4):831‐49. [PubMed] [Google Scholar]
Palmer 1999 {published data only}
- Palmer J, Schanberg L, Kuhn CM, Taylor C, Turner BS, Coombs WT. The effect of art on venipuncture induced stress. USA: Society for the Arts in Healthcare, Duke University Medical Center, 1999. [Google Scholar]
Parker 1965 {published data only}
- Parker MT, John M, Emond RTD, Machacek KA. Acquisition of Staphylococcus aureus by patients in cubicles. British Medical Journal 1965;1:1101‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Passini 1998 {published data only}
- Passini R, Rainville C, Marchand N, Joanette Y. Wayfinding and dementia: some research findings and a new look at design. Journal of Architectural and Planning Research 1998;15(2):133‐51. [Google Scholar]
Passweg 1998 {published data only}
- Passweg JR, Rowlings PA, Atkinson KA, Barrett AJ, Gale RP, Gratwohl A, et al. Influence of protective isolation on outcome of allogeneic bone marrow transplantation for leukemia. Bone Marrow Transplantation 1998;21:1231‐8. [DOI] [PubMed] [Google Scholar]
Pattison 1996 {published data only}
- Pattison HM, Robertson CE. The effect of ward design on the well‐being of post‐operative patients. Journal of Advanced Nursing 1996;23:820‐6. [DOI] [PubMed] [Google Scholar]
Petersen 1987 {published data only}
- Petersen FB, Buckner CD, Clift RA, Nelson N, Counts GW, Meyers JD, et al. Infectious complications in patients undergoing marrow transplantation: a prospective randomized study of the additional effect of decontamination and laminar air flow isolation among patients receiving prophylactic systemic antibiotics. Scandinavian Journal of Infectious Diseases 1987;19(5):559‐67. [DOI] [PubMed] [Google Scholar]
Peterson 1977 {published data only}
- Peterson RF, Knapp TJ, Rosen JC, Pither BF. The effects of furniture arrangement on the behavior of geriatric patients. Behavior Therapy 1977;8:464‐7. [Google Scholar]
Pimentel‐Souza 1996 {published data only}
- Pimentel‐Souza F, Carvalho JC, Siqueira AL. Noise and the quality of sleep in two hospitals in the city of Belo Horizonte, Brazil. Brazilian Journal of Medical and Biological Research 1996;29:515‐20. [PubMed] [Google Scholar]
Plourde 1997 {published data only}
- Plourde G, Leduc AS, Morin JE, DeVarennes B, Latter D, Symes J, et al. Temperature during cardiopulmonary bypass for coronary artery operations does not influence postoperative cognitive function: a prospective, randomised trial. The Journal of Thoracic and Cardiovascular Surgery 1997;114(1):123‐8. [DOI] [PubMed] [Google Scholar]
Prensner 2001 {published data only}
- Prensner JD, Yowler CJ, Smith LF, Steele AL, Fratianne RB. Music therapy for assistance with pain and anxiety management in burn treatment. Journal of Burn Care & Rehabilitation 2001;22(1):83‐8. [DOI] [PubMed] [Google Scholar]
Preston 1981 {published data only}
- Preston GA, Larson EI, Stamm WE. The effect of private isolation rooms on patient care practices, colonization and infection in an intensive care unit. The American Journal of Medicine 1981;70:641‐5. [DOI] [PubMed] [Google Scholar]
Pring 1998 {published data only}
- Pring J, Millman P. Evaluating pressure‐relieving mattresses. Journal of Wound Care 1998;7(4):177‐9. [DOI] [PubMed] [Google Scholar]
Pruyn 1998 {published data only}
- Pruyn A, Smidts A. Effects of waiting on the satisfaction with the service: beyond objective time measures. International Journal of Research in Marketing 1998;15:321‐34. [Google Scholar]
Qian 2006 {published data only}
- Qian H, Li Y, Nielsen PV, Hyldgaard CE, Wong TW, Chwang ATY. Dispersion of exhaled droplet nuclei in a two‐bed hospital ward with three different ventilation systems. Indoor Air 2006;16(2):111‐28. [DOI] [PubMed] [Google Scholar]
Rabin 1981 {published data only}
- Rabin M. Medical‐facility colors reduce patient stress. Contract (New York) 1981;23(3):78‐83. [PubMed] [Google Scholar]
Ragneskog 1996 {published data only}
- Ragneskog H, Brane G, Karlsson I, Kihlgren M. Influence of dinner music on food intake and symptoms common in dementia. Scandinavian Journal of Caring Sciences 1996;10(1):11‐7. [DOI] [PubMed] [Google Scholar]
Rakshy 1997 {published data only}
- Rakshy ME, Weston C. An investigation into the possible additive effects of acupuncture and autogenic relaxation in the management of chronic pain. Acupuncture in Medicine 1997;15(2):74‐5. [Google Scholar]
Redd 1994 {published data only}
- Redd WH, Manne SL, Peters B, Jacobsen PB, Schmidt H. Fragrance administration to reduce anxiety during MR imaging. Journal of Magnetic Resonance Imaging 1994;4(4):623‐6. [DOI] [PubMed] [Google Scholar]
Ribas‐Mundo 1981 {published data only}
- Ribas‐Mundo M, Granena A, Rozman C. Evaluation of a protective environment in the management of granulocytopenic patients: a comparative study. Cancer 1981;48:419‐24. [DOI] [PubMed] [Google Scholar]
Rice 1980 {published data only}
- Rice CG, Talbott JA, Stern D. Effects of environmental agents on social behavior of patients in a hospital dining room. Hospital and Community Psychiatry 1980;31(2):128‐30. [DOI] [PubMed] [Google Scholar]
Rodriguez 1978 {published data only}
- Rodriguez V, Bodey GP, Freireich EJ. Randomized trial of protected environment‐prophylactic antibiotics in 145 adults with acute leukemia. Medicine 1978;57(3):253‐66. [DOI] [PubMed] [Google Scholar]
Rosenthal 1985 {published data only}
- Rosenthal NE, Sack DA, Carpenter CJ, Parry BL, Mendelson WB, Wehr TA. Antidepressant effects of light in seasonal affective disorder. American Journal of Psychiatry 1985;142(2):163‐70. [DOI] [PubMed] [Google Scholar]
Routhieaux 1997 {published data only}
- Routhieaux RL, Tansik DA. The benefits of music in hospital waiting rooms. The Health Care Supervisor 1997;16(2):31‐40. [PubMed] [Google Scholar]
Rubin 1998 {published data only}
- Rubin HR, Owens AJ, Golden G, Weber DO. Status report: an investigation to determine whether the built environment affects patient's medical outcomes. Martinez, California: The Centre for Health Design, 1998. [PubMed] [Google Scholar]
Rudy 1995 {published data only}
- Rudy EB, Daly BJ, Douglas S, Montenegro HD, Song R, Dyer MA. Patient outcomes for the chronically critically ill: special care unit versus intensive care unit. Nursing Research 1995;44(6):324‐31. [PubMed] [Google Scholar]
Salmore 2000 {published data only}
- Salmore RG, Nelson JP. The effect of preprocedure teaching, relaxation instruction, and music on anxiety as measured by blood pressures in an outpatient gastrointestinal endoscopy laboratory. Gastroenterology Nursing 2000;23(3):102‐10. [DOI] [PubMed] [Google Scholar]
Sármány 2006 {published and unpublished data}
- Sármány J, Kálmán R, Staud D, és Salacz G. Role of the music in the operating theatre [A zene szerepe a szemészeti műtőben]. Orvosi Hetilap 2006;147(20):931‐6. [PubMed] [Google Scholar]
Satlin 1992 {published data only}
- Satlin A, Volicer L, Ross V, Herz L, Campbell S. Bright light treatment of behavioral and sleep disturbances in patients with alzheimer's disease. American Journal of Psychiatry 1992;149(8):1028‐32. [DOI] [PubMed] [Google Scholar]
Satoh 1983 {published data only}
- Satoh Y, Nagao H, Ishihara H, Oyama T, Spintge R. Effects of music on plasma stress hormones in surgical patients. Masui: The Japanese Journal of Anesthesiology 1983;32(10):1206‐11. [PubMed] [Google Scholar]
Schimpff 1975 {published data only}
- Schimpff SC, Greene WH, Young VM, Fortner CL, Cusack N, Block JB, et al. Infection prevention in acute nonlymphocytic leukemia. Laminar air flow room reverse isolation with oral, nonabsorbable antibiotic prophylaxis. Annals of Internal Medicine 1975;82:351‐8. [DOI] [PubMed] [Google Scholar]
Schneider 2003 {published data only}
- Schneider SM, Ellis M, Coombs WT, Shonkwiler EL, Folsom LC. Virtual reality intervention for older women with breast cancer. CyberPsychology & Behavior 2003;6(3):301‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schneider 2004 {published data only}
- Schneider SM, Prince‐Paul M, Allen MJ, Silverman P, Talaba D. Virtual reality as a distraction intervention for women receiving chemotherapy. Oncology Nursing Forum 2004;31(1):81‐8. [DOI] [PubMed] [Google Scholar]
Schofield 2000 {published data only}
- Schofield P, Davis B. Sensory stimulation (snoezelen) versus relaxation: a potential strategy for the management of chronic pain. Disability and Rehabilitation 2000;22(15):675‐82. [DOI] [PubMed] [Google Scholar]
Schott 1999 {published data only}
- Schott J. Do bedrails decrease falls in hospitalized patients?. Journal of Family Practice 1999;48(8):579. [PubMed] [Google Scholar]
Schuhl 1985 {published data only}
- Schuhl JF, Lahsinat D. Music and surgery [Musique et chirurgie]. Journal de Chirurgie 1985;122(8‐9):483‐5. [PubMed] [Google Scholar]
Schuster 1985 {published data only}
- Schuster I. The effect of music listening on blood pressure fluctuations in adult hemodialysis patients. Journal of Music Therapy 1985;22(3):146‐53. [Google Scholar]
Sheperd 2001 {published data only}
- Sheperd L, Foureur M. Introduction of night‐lights to reduce falls on an assessment, treatment and rehabilitation unit. The Journal of the Australasian Rehabilitation Nurses Association 2001;4(4):11‐3. [Google Scholar]
Sherertz 1985 {published data only}
- Sherertz RJ, Sullivan ML. An outbreak of infections with acinetobacter calcoaceticus in burn patients: contamination of patients' mattresses. The Journal of Infectious Diseases 1985;151(2):252‐8. [DOI] [PubMed] [Google Scholar]
Sherertz 1987 {published data only}
- Sherertz RJ, Belani A, Kramer BS, Elfenbein GJ, Weiner RS, Sullivan ML, et al. Impact of air filtration on nosocomial aspergillus intections: unique risk of bone marrow transplant recipients. The American Journal of Medicine 1987;83:709‐18. [DOI] [PubMed] [Google Scholar]
Sherratt 2004 {published data only}
- Sherratt K, Thornton A, Hatton C. Emotional and behavioural responses to music in people with dementia: an observational study. Aging & Mental Health 2004;8(3):233‐41. [DOI] [PubMed] [Google Scholar]
Shertzer 2001 {published data only}
- Shertzer KE, Keck JF. Music and PACU environment. Journal of PeriAnesthesia Nursing 2001;16(2):90‐102. [DOI] [PubMed] [Google Scholar]
Shirani 1986 {published data only}
- Shirani KZ, McManus AT, Vaughan GM, McManus WF, Pruitt BA, Mason AD. Effects of environment on infection in burn patients. Archives Surgery 1986;121:31‐6. [DOI] [PubMed] [Google Scholar]
Shooter 1963 {published data only}
- Shooter RA, Thorn BT, Dunkerley DR, Taylor GW, Parker MT, John M, et al. Preoperative segregation of patients in a surgical ward. British Medical Journal 1963;2:1567‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sidorenko 2000a {published data only}
- Sidorenko VN. Effects of the medical resonance therapy music in the complex treatment of epileptic patients. Integrative Physiological and Behavioral Science 2000;35(3):212‐7. [DOI] [PubMed] [Google Scholar]
Sidorenko 2000b {published data only}
- Sidorenko VN. Clinical application of medical resonance therapy music in high‐risk pregnancies. Integrative Physiological and Behavioral Science 2000;35(3):199‐207. [DOI] [PubMed] [Google Scholar]
Siedliecki 2006 {published data only}
- Siedliecki SL, Good M. Effect of music on power, pain, depression and disability. Journal of Advanced Nursing 2006;54(5):553‐62. [DOI] [PubMed] [Google Scholar]
Siegman‐Igra 1986 {published data only}
- Siegman‐Igra Y, Shalem A, Berger SA, Livio S, Michaeli D. Should potted plants be removed from hospital wards?. Journal of Hospital Infection 1986;7:82‐5. [DOI] [PubMed] [Google Scholar]
Silini 2002 {published data only}
- Silini E, Locasciulli A, Santoleri L, Gargantini L, Pinzello G, Montillo M, et al. Hepatitis C virus infection in a hematology ward: evidence for nosocomial transmission and impact on hematologic disease outcome. Haematologica 2002;87(11):1200‐8. [PubMed] [Google Scholar]
Singer 2000 {published data only}
- Singer AJ, Sanders BT, Kowalska A, Stark MJ, Mohammad M, Brogan GX. The effect of introducing bedside TV sets on patient satisfaction in the ED. American Journal of Emergency Medicine 2000;18(1):119‐20. [DOI] [PubMed] [Google Scholar]
Skoutelis 1993 {published data only}
- Skoutelis AT, Westenfelder GO, Beckerdite M, Phair JP. Hospital carpeting and epidemiology of Clostridium difficile. American Journal of Infection Control 1993;22:212‐7. [DOI] [PubMed] [Google Scholar]
Smith 1974 {published data only}
- Smith G, Logie JRC, MacDonald A, Smylie HG. Ward design in relation to postoperative wound infection: part III. British Medical Journal 1974;3:13‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smylie 1971 {published data only}
- Smylie HG, Davidson AIG, Macdonald A, Smith G. Ward design in relation to postoperative wound infection. British Medical Journal 1971;1:67‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sommer 1958 {published data only}
- Sommer R, Ross H. Social interaction on a geriatrics ward. International Journal of Social Psychology 1958;4(2):128‐33. [Google Scholar]
Spintge 2000 {published data only}
- Spintge R. Music and anesthesia in pain therapy [Musik in Anaesthesie und Schmerztherapie]. Anästhesiol Intensivmed Notfallmed Schmerzther 2000;35(4):254‐61. [DOI] [PubMed] [Google Scholar]
Spitzer 2005 {published data only}
- Spitzer M, Rath F, Groen G. Music and subjective well being: preliminary results on use of a sound bed in depressive patients [Musik und Befindlichkeit: Erste Ergebnisse zum einer Klangliege bei depressiven Patienten]. Nervenheilkunde: Zeitschrift für interdisziplinäre Fortbildung 2005;24(3):198‐202. [Google Scholar]
Stahler 1984 {published data only}
- Stahler GJ, Frazer D, Rappaport H. The evaluation of an environmental remodeling program on a psychiatric geriatric ward. The Journal of Social Psychology 1984;123:101‐13. [DOI] [PubMed] [Google Scholar]
Standley 1992 {published data only}
- Standley JM. Clinical applications of music and chemotherapy: the effects on nausea and emesis. Music Therapy Perspectives 1992;10:27‐35. [Google Scholar]
Staricoff 2001 {published data only}
- Staricoff RL. A study of the effects of the visual and performing arts in healthcare. Hospital Development 2001;32(6):25‐8. [Google Scholar]
Staricoff 2003a {published data only}
- Staricoff RL, Duncan JP, Wright M. Medical Day Unit. A study of the effects of visual and performing arts in health care. http://www.publicartonline.org.uk/news/research/documents/ChelseaAndWestminsterResearchproject.pdf, 2003:12‐5. [Google Scholar]
Staricoff 2003b {published data only}
- Staricoff RL, Duncan JP, Wright M. Antenatal Clinic. A study of the effects of visual and performing arts in health care. http://www.publicartonline.org.uk/news/research/documents/ChelseaAndWestminsterResearchproject.pdf, 2003:15‐21. [Google Scholar]
Staricoff 2003c {published data only}
- Staricoff RL, Duncan JP, Wright M. Maternity Unit (Labour and Delivery Rooms). A study of the effects of visual and performing arts in health care. http://www.publicartonline.org.uk/news/research/documents/ChelseaAndWestminsterResearchproject.pdf, 2003:22‐6. [Google Scholar]
Staricoff 2003d {published data only}
- Staricoff RL, Duncan JP, Wright M. Post‐natal Ward. A study of the visual and performing arts in health care. http://www.publicartonline.org.uk/news/research/documents/ChelseaAndWestminsterResearchproject.pdf, 2003:27‐8. [Google Scholar]
Staricoff 2003e {published data only}
- Staricoff RL, Duncan JP, Wright M. Day Surgery Unit and Trauma and Orthopaedic Ward. A study of the effects of visual and performing arts in health care. http://www.publicartonline.org.uk/news/research/documents/ChelseaAndWestminsterResearchproject.pdf, 2003:29‐37. [Google Scholar]
Steelman 1990 {published data only}
- Steelman VM. Intraoperative music therapy: effects on anxiety, blood pressure. AORN Journal 1990;52(5):1026‐34. [DOI] [PubMed] [Google Scholar]
Steer 1975 {published data only}
- Steer RA, Boger WP. Milieu therapy with psychiatric‐medically infirm patients. The Gerontologist 1975;15(2):138‐41. [DOI] [PubMed] [Google Scholar]
Steffes 1985 {published data only}
- Steffes R, Thralow J. Do uniform colors keeps patients awake?. Journal of Gerontological Nursing 1985;11(7):6‐9. [DOI] [PubMed] [Google Scholar]
Steingold 1963 {published data only}
- Steingold L, Dunn L, Hawksworth E, Limb L. The influence of ward ventilation on hospital cross infection. Journal of Applied Bacteriology 1963;26:435‐43. [Google Scholar]
Stermer 1998 {published data only}
- Stermer E, Levy N, Beny A, Meisels R, Tamir A. Ambience in the endoscopy room has little effect on patients. Journal of Clinical Gastroenterology 1998;26(4):256‐8. [DOI] [PubMed] [Google Scholar]
Stone 1989 {published data only}
- Stone SK, Rusk F, Chambers A, Chafin S. The effects of music therapy on critically ill patients in the intensive care setting (Brief research report). Heart & Lung 1989;18(3):291. [Google Scholar]
Strauser 1997 {published data only}
- Strauser JM. The effects of music versus silence on measures of state anxiety, perceived relaxation, and physiological responses of patients receiving chiropractic interventions. Journal of Music Therapy 1997;34(2):88‐105. [Google Scholar]
Swan 2003 {published data only}
- Swan JE, Richardson LD, Hutton JD. Do appealing hospital rooms increase patient evaluations of physicians, nurses, and hospital services?. Health Care Management Review 2003;28(3):254‐64. [DOI] [PubMed] [Google Scholar]
Swinford 1987 {published data only}
- Swinford P. Relaxation and positive imagery for the surgical patient: a research study. Perioperative Nursing Quarterly 1987;3(3):9‐16. [PubMed] [Google Scholar]
Szeto 1999 {published data only}
- Szeto CK, Yung PMB. Introducing a music programme to reduce preoperative anxiety. British Journal of Theatre Nursing 1999;9(10):455‐9. [DOI] [PubMed] [Google Scholar]
Tanabe 2001 {published data only}
- Tanabe P, Thomas R, Paice J, Spiller M, Marcantonio R. The effect of standard care, ibuprofen, and music on pain relief and patient satisfaction in adults with musculoskeletal trauma. Journal of Emergency Nursing 2001;27(2):124‐30. [DOI] [PubMed] [Google Scholar]
Tang 1997 {published data only}
- Tang X, Yang F, Zhuang H. Musical relaxation therapy on the cerebral arteriosclerosis. Hunan Yi Ke Da Xue Xue Bao 1997;22(1):45‐8. [PubMed] [Google Scholar]
Tate 1997 {published data only}
- Tate S. Peppermint oil: a treatment for postoperative nausea. Journal of Advanced Nursing 1997;26:543‐9. [DOI] [PubMed] [Google Scholar]
Thompson 2002 {published data only}
- Thompson JT, Meredith JW, Molnar JA. The effect of burn nursing units on burn wound infections. Journal of Burn Care and Rehabilitation 2002;23:281‐6. [DOI] [PubMed] [Google Scholar]
Thorgaard 2004 {published data only}
- Thorgaard B, Brondsted B, Pedersbæk G, Thomsen I. Specially selected music in the cardiac laboratory: an important tool for improvement of the wellbeing of patients. European Journal of Cardiovascular Nursing 2004;3:21‐6. [DOI] [PubMed] [Google Scholar]
Thorgaard 2005 {published data only}
- Thorgaard P, Ertmann E, Hansen V, Noerregaard A, Hansen V, Spanggaard L. Designed sound and music environment in postanaesthesia care units‐ a multicentre study of patients and staff. Intensive and Critical Care Nursing 2005;21:220‐5. [DOI] [PubMed] [Google Scholar]
Thorne 1963 {published data only}
- Thorne CG. Flooring for geriatric wards: report of an investigation at West Middlesex Hospital. The Builder 1963;March 15:557‐9. [Google Scholar]
Tideiksaar 1993 {published data only}
- Tideiksaar R, Feiner CF, Maby J. Falls prevention: the efficacy of a bed alarm system in an acute‐care setting. The Mount Sinai Journal of Medicine 1993;60(6):522‐7. [PubMed] [Google Scholar]
Tierney 1978 {published data only}
- Tierney IR, McGuire RJ, Walton HJ. The effect of music on body‐rocking manifested by severely mentally deficient patients in ward environments. Journal of Mental Deficiency Research 1978;22(4):255‐61. [DOI] [PubMed] [Google Scholar]
Tse 2003 {published data only}
- Tse MMY, Ng JKF, Chung JWY. Visual stimulation as pain relief for Hong Kong Chinese patients with leg ulcers. CyberPsychology & Behavior 2003;6(3):315‐20. [DOI] [PubMed] [Google Scholar]
Tse 2005 {published data only}
- Tse MMY, Chan MF, Benzie IFF. The effect of music therapy on postoperative pain, heart rate, systolic blood pressure and analgesic use following nasal surgery. Journal of Pain & Palliative Care Pharmacotherapy 2005;19(3):21‐9. [PubMed] [Google Scholar]
Tyerman 1980 {published data only}
- Tyerman C, Spencer CP. Normalised physical environment for the mentally handicapped, and its effect on patterns of activity, social relations and self‐help skills. British Journal of Mental Subnormality 1980;26:47‐54. [Google Scholar]
Uedo 2004 {published data only}
- Uedo N, Ishikawa H, Morimoto K, Ishihara R, Narahara H, Akedo I, et al. Reduction in salivary cortisol level by music therapy during colonoscopic examination. Hepatogastroenterology 2004;51:451‐3. [PubMed] [Google Scholar]
Ulrich 1984 {published data only}
- Ulrich RS. View through a window may influence recovery from surgery. Science 1984;224:420‐1. [DOI] [PubMed] [Google Scholar]
Ulrich 1993b {published data only}
- Ulrich RS, Lundén O, Eltinge JL. Effects of exposure to nature and abstract pictures on patients recovering from open heart surgery. Psychophysiology 1993;Supplement 1:7. [Google Scholar]
Ulrich 2003 {published data only}
- Ulrich RS, Simons RF, Miles RA. Effects of environmental simulations and television on blood donor stress. Journal of Architectural and Planning Research 2003;20(1):38‐47. [Google Scholar]
Updike 1987 {published data only}
- Updike PA, Charles DM. Music Rx: Physiological and emotional responses to taped music programs of preoperative patients awaiting plastic surgery. Annals of Plastic Surgery 1987;19(1):29‐33. [DOI] [PubMed] [Google Scholar]
Updike 1990 {published data only}
- Updike P. Music therapy results for ICU patients. Dimensions of Critical Care Nursing 1990;9(1):39‐45. [DOI] [PubMed] [Google Scholar]
Van Someren 1997 {published data only}
- Someren EJW, Kessler A, Mirmiran M, Swaab DF. Indirect bright light improves circadian rest‐activity rhythm disturbances in demented patients. Biological Psychiatry 1997;41(9):955‐63. [DOI] [PubMed] [Google Scholar]
Veitch 2001 {published data only}
- Veitch JA, McColl SL. A critical examination of perceptual and cognitive effects attributed to full‐spectrum fluorescent lighting. Ergonomics 2001;44(3):255‐79. [DOI] [PubMed] [Google Scholar]
Verderber 1983 {published data only}
- Verderber S. Dimensions of person‐window transactions in the hospital environment. Environment and Behavior 1986;18(4):450‐66. [Google Scholar]
- Verderber S, Reuman D. Windows, views, and health status in hospital therapeutic environments. The Journal of Architectural and Planning Research 1987;4(2):120‐33. [Google Scholar]
- Verderber SF. Windowness and human behavior in the hospital rehabilitation environment. Doctoral Dissertation. Ann Arbor: University Microfilms International, 1983. [Google Scholar]
- Verderber SF. Designing for the therapeutic functions of windows in the hospital rehabilitation environment. EDRA: Environmental Design Research Association 1982;13:476‐92. [Google Scholar]
Vietri 2004 {published data only}
- Vietri NJ, Dooley DP, Davis CE, Longfield JN, Meier PA, Whelen AC. The effect of moving to a new hospital facility on the prevalence of methicillin‐resistant Staphylococcus aureus. American Journal of Infection Control 2004;32(5):262‐7. [DOI] [PubMed] [Google Scholar]
Vollert 2002 {published data only}
- Vollert JO, Störk T, Rose M, Röcker L, Klapp BF, Heller G, et al. Reception of music in patients with systemic arterial hypertension and coronary artery disease: endocrine changes, hemodynamics and actual mood. Perfusion 2002;15:142‐52. [Google Scholar]
Vollert 2003 {published data only}
- Vollert JO, Störk T, Rose M, Möckel M. Music as adjuvant therapy for coronary heart disease. Therapeutic music lowers anxiety, stress and beta‐endorphin concentrations in patients from a coronary sport group [Musik als begleitende Therapie bei koronarer Herzkrankheit. Therapeutische Musik verringert Angst, Stress und beta‐Endorphinkonzentrationen bei Patienten einer Herzsportgruppe]. Deutsche Medizinsche Wochenschrift 2003;128(51‐52):2712‐6. [DOI] [PubMed] [Google Scholar]
Walker 1989 {published data only}
- Walker K, DeVooght J. Invasion: a hospital in transition following the 1983 Grenadian intervention. Journal of Psychosocial Nursing 1989;27(1):27‐30. [DOI] [PubMed] [Google Scholar]
Walsh 1989 {published data only}
- Walsh TR, Guttendorf J, Dummer S, Hardesty RL, Armitage JM, Kormos RL, et al. The value of protective isolation procedures in cardiac allograft recipients. Annals of Thoracic Surgery 1989;47:539‐45. [DOI] [PubMed] [Google Scholar]
Walther‐Larsen 1988 {published data only}
- Walther‐Larsen S, Diemar V, Valentin N. Music during regional anesthesia: a reduced need of sedatives. Regional Anesthesia and Pain Medicine 1998;13(23):69‐71. [Google Scholar]
Watanabe 1997 {published data only}
- Watanabe A, Yang D. An analysis of wayfinding behavior by first‐visit patients in hospitals‐ a cognitive study on wayfinding behavior in architectural spaces No. 5. Journal of Architecture Planning and Environmental Engineering 1997;501:101‐8. [Google Scholar]
Weber 1996 {published data only}
- Weber DO. Life‐enhancing design. Healthcare Forum Journal 1996;39(2):42‐7. [PubMed] [Google Scholar]
Weisman 1981 {published data only}
- Weisman J. Evaluating architectural legibility: way‐finding in the built environment. Environment and Behavior 1981;13(2):189‐204. [Google Scholar]
Whitehead 1984 {published data only}
- Whitehead CC, Polsky RH, Crookshank C, Fik E. Objective and subjective evaluation of psychiatric ward redesign. American Journal of Psychiatry 1984;141(5):639‐44. [DOI] [PubMed] [Google Scholar]
Whyte 1968 {published data only}
- Whyte W. Bacteriological aspects of air‐conditioning plants. Journal of Hygiene 1968;66:567‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wikström 1992 {published data only}
- Wikström BM, Theorell T, Sandström S. Psychophysiological effects of stimulation with pictures of works of art in old age. International Journal of Psychosomatics 1992;39(1‐4):68‐75. [PubMed] [Google Scholar]
Wikström 1993 {published data only}
- Wikström BM, Theorell T, Sandström S. Medical health and emotional effects of art stimulation in old age: A controlled intervention study concerning the effects of visual stimulation provided in the form of pictures. Psychotherapy and Psychosomatics 1993;60(3‐4):195‐206. [DOI] [PubMed] [Google Scholar]
Wilkins 1988 {published data only}
- Wilkins EGL, Ellis ME, Dunbar EM, Gibbs A. Does isolation of patients with infections induce mental illness?. Journal of Infection 1988;17:43‐7. [DOI] [PubMed] [Google Scholar]
Williams 1962 {published data only}
- Williams REO, Noble WC, Jevons MP, Lidwell OM, Shooter RA, White RG, et al. Isolation for the control of staphylococcal infection in surgical wards. British Medical Journal 1962;2(5300):275‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 1969 {published data only}
- Williams REO, Harding L. Studies of the effectiveness of an isolation ward. Journal of Hygiene 1969;67(4):649‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williamson 1992 {published data only}
- Williamson JW. The effects of ocean sounds on sleep after coronary artery bypass graft surgery. American Journal of Critical Care 1992;1(1):91‐7. [PubMed] [Google Scholar]
Wilson 1972 {published data only}
- Wilson LM. Intensive care delirium: the effect of outside deprivation in a windowless unit. Archives of Internal Medicine 1972;130:225‐6. [DOI] [PubMed] [Google Scholar]
Wilson 1983 {published data only}
- Wilson MR, Soth N, Robak R. Managing disturbed behavior by architectural changes: making spaces fit the program. Milieu Therapy 1983;3(2):15‐24. [Google Scholar]
Winkel 1986 {published data only}
- Winkel GH, Holahan CJ. The environmental psychology of the hospital: is the cure worse than the illness?. Prevention in Human Services 1986;4(1‐2):11‐33. [DOI] [PubMed] [Google Scholar]
Wint 2002 {published data only}
- Wint SS, Eshelman D, Steele J, Guzzetta CE. Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncology Nursing Forum 2002;29(1):E8‐E15. [DOI: 10.1188/02.ONF.E8‐E15] [DOI] [PubMed] [Google Scholar]
Wolowicka 1989 {published data only}
- Wolowicka L. Music lessens anxiety [Muzyka zmniejsza lek]. Pielegniarka I Polozna 1989;1:6. [PubMed] [Google Scholar]
Wood 1977 {published data only}
- Wood M. Clinical sensory deprivation: a comparative study of patients in single care and two‐bed rooms. Journal of Nursing Administration 1977;7(10):28‐32. [PubMed] [Google Scholar]
Wright 1993 {published data only}
- Wright P, Hull AJ, Lickorish A. Navigating in a hospital outpatients' department: the merits of maps and wall signs. Journal of Architectural and Planning Research 1993;10(1):76‐88. [Google Scholar]
Wyon 1968 {published data only}
- Wyon DP, Lidwell OM, Williams REO. Thermal comfort during surgical operations. Journal of Hygiene 1968;66(2):229‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yamanaka 2003 {published data only}
- Yamanaka K, Taniguchi T, Muraoka M. Usefulness of the musical therapy in an operation under the local anesthesia. Medical Journal of Minami Osaka Hospital 2003;51(1):107‐11. [Google Scholar]
Yates 1973 {published data only}
- Yates JW, Holland JF. A controlled study of isolation and endogenous microbial suppression in acute myelocytic leukemia patients. Cancer 1973;32(6):1490‐8. [DOI] [PubMed] [Google Scholar]
Yilmaz 2003 {published data only}
- Yilmaz E, Ozcan S, Basar M, Basar H, Batislam E, Ferhat M. Music decreases anxiety and provides sedation in extracorporeal shock wave lithotripsy. Urology 2003;61(2):282‐6. [DOI] [PubMed] [Google Scholar]
Yinnon 1992 {published data only}
- Yinnon AM, Ilan Y, Tadmor B, Altarescu G, Hershko C. Quality of sleep in the medical department. British Journal of Clinical Practice 1992;46(2):88‐91. [PubMed] [Google Scholar]
Yung 2002 {published data only}
- Yung PMB, Chui‐Kam S, French P, Chan TMF. A controlled trial of music and pre‐operative anxiety in Chinese men undergoing transurethral resection of the prostate. Journal of Advance Nursing 2002;39(4):352‐9. [DOI] [PubMed] [Google Scholar]
Zhong 2005 {published data only}
- Zhong YH, Lee AQ, Chen MH. Effect of music on the physiological responses and anxiety levels of patients receiving mechanical ventilation. Chinese Journal of Nursing 2005;40(7):481‐4. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Allred 2010 {published data only}
Anon 2009 {published data only}
- Soothing scents. The art of aromatherapy. Mayo Clinic Women's Healthsource 2009; Vol. 13, issue 4:7. [1091‐0220] [PubMed]
Arai 2008 {published data only}
- Arai YCP, Sakakibara S, Ito A, Ohshima K, Sakakibara T, Nishi T, et al. Intra‐operative natural sound decreases salivary amylase activity of patients undergoing inguinal hernia repair under epidural anesthesia. Acta Anaesthesiologica Scandinavica 2008; Vol. 52, issue 7:987‐90. [1399‐6576] [DOI] [PubMed]
Berbel 2007 {published data only}
- Berbel P, Moix J, Quintana S. [Music versus diazepam to reduce preoperative anxiety: a randomized controlled clinical trial]. Revista Espanola de Anestesiologia y Reanimacion 2007; Vol. 54, issue 6:355‐8. [0034‐9356] [PubMed]
Boehm 2009 {published data only}
Braden 2009 {published data only}
Bradt 2009 {published data only}
- Bradt J, Dileo C. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006577.pub2; 1469‐493X] [DOI] [PubMed] [Google Scholar]
Brenier‐Pinchart 2009 {published data only}
- Brenier‐Pinchart M‐P, Coussa‐Riviere L, Lebeau B, Mallaret M‐R, Bulabois C‐E, Ducki S, et al. Mobile air‐decontamination unit and filamentous fungal load in the hematology ward: how efficient at the low‐activity mode?. American Journal of Infection Control 2009; Vol. 37, issue 8:680‐2. [1527‐3296] [DOI] [PubMed]
Bringman 2009 {published data only}
Chan 2007 {published data only}
Chlan 2007 {published data only}
- Chlan LL, Engeland WC, Anthony A, Guttormson J. Influence of music on the stress response in patients receiving mechanical ventilatory support: a pilot study. American Journal of Critical Care 2007; Vol. 16, issue 2:141‐5. [1062‐3264] [PubMed]
Cooke 2010 {published data only}
Danhauer 2007 {published data only}
- Danhauer SC, Marler B, Rutherford CA, Lovato JF, Asbury DY, McQuellon RP, et al. Music or guided imagery for women undergoing colposcopy: a randomized controlled study of effects on anxiety, perceived pain, and patient satisfaction. Journal of Lower Genital Tract Disease 2007; Vol. 11, issue 1:39‐45. [1089‐2591] [DOI] [PubMed]
Dennis 2010 {published data only}
Dijkstra 2010 {published data only}
Dube 2008 {published data only}
Eagle 2009 {published data only}
- Eagle A. Standing tall. Environmental improvements for reducing patient falls. Health Facilities Management 2009; Vol. 22, issue 6:32‐5. [0899‐6210] [PubMed]
Easter 2010 {published data only}
- Anonymous. Erratum. Journal of Perianesthesia Nursing 2010;25(4):260. [Google Scholar]
- Easter B, DeBoer L, Settlemyre G, Starnes C, Marlowe V, Tart RC. The impact of music on the PACU patient's perception of discomfort. Journal of PeriAnesthesia Nursing 2010; Vol. 25, issue 2:79‐87. [1532‐8473] [DOI] [PubMed]
Ebneshahidi 2008 {published data only}
El‐Hassan 2009 {published data only}
Escombe 2007 {published data only}
- Escombe AR, Oeser CC, Gilman RH, Navincopa M, Ticona E, Pan W, et al. Natural ventilation for the prevention of airborne contagion. PLoS Medicine / Public Library of Science 2007; Vol. 4, issue 2:e68. [1549‐1676] [DOI] [PMC free article] [PubMed]
Ferrer 2007 {published data only}
Fredriksson 2009 {published data only}
Freysteinson 2008 {published data only}
Gardner 2009 {published data only}
Gonzalez 2008 {published data only}
- Gonzalez Molero I, Olveira Fuster G, Liebana MI, Oliva L, Lainez Lopez M, Munoz Aguilar A. [Influence of temperature on food intake in hospitalized patients]. Nutricion Hospitalaria 2008; Vol. 23, issue 1:54‐9. [0212‐1611] [PubMed]
Good 2008 {published data only}
Good 2010 {published data only}
Gross 2008 {published data only}
- Gross D. Bedside music in the hospital. Beginnings 2008; Vol. 28, issue 4:10‐1. [1071‐2984] [PubMed]
Han 2010 {published data only}
Hoya 2008 {published data only}
Huang 2010 {published data only}
Hur 2005 {published data only}
- Hur MH, Cheong N, Yun H, Lee M, Song Y. Effects of delivery nursing care using essential oils on delivery stress response, anxiety during labor, and postpartum status anxiety. Journal of Korean Academy of Nursing 2005;35(7):1277‐84. [DOI] [PubMed] [Google Scholar]
Jaber 2007 {published data only}
Jimbo 2009 {published data only}
Joanna 2009 {published data only}
- Joanna Briggs I. Clinical update 130. Music as an intervention in hospitals. Australian Nursing Journal 2009; Vol. 17, issue 4:29‐31. [1320‐3185] [PubMed]
Kang 2008 {published data only}
Kim 2007 {published data only}
- Kim JT, Ren CJ, Fielding GA, Pitti A, Kasumi T, Wajda M, et al. Treatment with lavender aromatherapy in the post‐anesthesia care unit reduces opioid requirements of morbidly obese patients undergoing laparoscopic adjustable gastric banding. Obesity Surgery 2007; Vol. 17, issue 7:920‐5. [0960‐8923] [DOI] [PubMed]
Knight 2010 {published data only}
Koo 2008 {published data only}
Lai 2008 {published data only}
Laopaiboon 2009 {published data only}
Leardi 2007 {published data only}
Lechtzin 2010 {unpublished data only}
- Lechtzin N, Busse AM, Smith MT, Grossman S, Nesbit S, Diette GB. A randomized trial of nature scenery and sounds versus urban scenery and sounds to reduce pain in adults undergoing bone marrow aspirate and biopsy. The Journal of Alternative and Complementary Medicine 2010;16(9):965‐72. [DOI: 10.1089/acm.2009.0531] [DOI] [PMC free article] [PubMed] [Google Scholar]
le Roux 2007 {published data only}
Lin 2007 {published data only}
Liu 2010 {published data only}
Maeyama 2009 {published data only}
- Maeyama A, Kodaka M, Miyao H. [Effect of the music‐therapy under spinal anesthesia]. Masui ‐ Japanese Journal of Anesthesiology 2009; Vol. 58, issue 6:684‐91. [0021‐4892] [PubMed]
Meeuse 2010 {published data only}
Moradipanah 2009 {published data only}
- Moradipanah F, Mohammadi E, Mohammadil AZ. Effect of music on anxiety, stress, and depression levels in patients undergoing coronary angiography. Eastern Mediterranean Health Journal 2009; Vol. 15, issue 3:639‐47. [1020‐3397] [PubMed]
Nikolajsen 2009 {published data only}
Nilsson 2009 {published data only}
Nilsson 2009a {published data only}
Nilsson 2009b {published data only}
Park 2009 {published data only}
Persichetti 2009 {published data only}
Phipps 2010 {published data only}
Podder 2007 {published data only}
- Podder L. Effects of music therapy on anxiety levels and pain perception. Nursing Journal of India 2007; Vol. 98, issue 7:161. [0029‐6503] [PubMed]
Pothoulaki 2008 {published data only}
Reza 2007 {published data only}
- Reza N, Ali SM, Saeed K, Abul‐Qasim A, Reza TH. The impact of music on postoperative pain and anxiety following cesarean section. Middle East Journal of Anesthesiology 2007; Vol. 19, issue 3:573‐86. [0544‐0440] [PubMed]
Richardson 2007 {published data only}
Sand‐Jecklin 2010 {published data only}
Shabanloei 2010 {published data only}
Siedlecki 2009 {published data only}
Simcock 2008 {published data only}
Son 2006 {published data only}
- Son JT, Kim SH. The effects of self‐selected music on anxiety and pain during burn dressing changes. Taehan‐Kanho‐Hakoe‐Chi [Journal of Korean Academy of Nursing] 2006;36(1):159‐68. [DOI] [PubMed] [Google Scholar]
Szmuk 2008 {published data only}
Wu 2008 {published data only}
- Wu S‐J, Chou F‐H. [The effectiveness of music therapy in reducing physiological and psychological anxiety in mechanically ventilated patients]. Hu Li Tsa Chih ‐ Journal of Nursing 2008; Vol. 55, issue 5:35‐44. [0047‐262X] [PubMed]
References to ongoing studies
NCT00817869 {published data only}
- NCT00817869. The HIP‐HOP flooring study: helping injury prevention in hospitalised older people. http://clinicaltrials.gov/ct2/show/NCT00817869 (accessed 17 August 2011).
Additional references
'CHD' 2009
- Centre for Health Design. Retrieved September 7, 2009 from http://healthdesign.org 2009.
'Kings Fund' 2009
- 'Kings Fund'. Enhancing the Healing Environment. Retrieved September 7, 2009 from http://www.kingsfund.org.uk/current_projects/enhancing_the_healing_environment/index.html 2009.
'Ottowa' 2004
- Ottowa Charter for Health Promotion, 1986. Retrieved August 2, 2004, from World Health Organisation Website (http://www.euro.who.int/AboutWHO/Policy/20010827_2) 2004.
'SAH' 2009
- Society for the Arts in Healthcare. Retrieved September 7, 2009 from http://thesah.org 2009.
'Webcast' 2004
- Webcast Detail‐ 21st Century Hospital Design. Retrieved July 20, 2004 from Robert Wood Johnson Foundation website (http://www.rwjf.org/news/eventDetail.jsp?id=108378798275&contentGroup=webcast) 2004.
Babwin 2002
- Babwin D. Building Boom. Hospitals and Health Networks 2002;76(3):48‐52. [PubMed] [Google Scholar]
Barnason 1995
- Barnason S, Zimmerman L, Nieveen J. The effects of music interventions on anxiety in the patient after coronary artery bypass grafting. Heart & Lung 1995;24:124‐32. [DOI] [PubMed] [Google Scholar]
Cepeda 2006
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD004843.pub2] [DOI] [PubMed] [Google Scholar]
Comer 1982
- Comer S. Arts in hospitals: art and well‐being. Health and Social Service Journal 1982;92(4786):268‐70. [PubMed] [Google Scholar]
Cooper 2002
- Cooper G. Natural Philosophy. Hospital Development 2002;33:9. [Google Scholar]
Cullum 2008
- Cullum N, McInnes E, Bell‐Syer SEM, Legood R. Support surfaces for pressure ulcer prevention. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD001735.pub3] [DOI] [PubMed] [Google Scholar]
Devlin 2003
- Devlin A, Arneill AB. Health Care Environments and Patient Outcomes‐ A Review of the Literature. Environment and Behavior 2003;35(5):665‐94. [Google Scholar]
Dijkstra 2006
- Dijkstra K, Pieterse M, Pruyn A. Physical environmental stimuli that turn healthcare facilities into healing environments through psychologically mediated effects: systematic review. Journal of Advanced Nursing 2006;56(2):166‐81. [DOI] [PubMed] [Google Scholar]
Dilani 2001
- Dilani A. Psychosocially Supportive Design‐ Scandinavian Health Care Design. World Hospitals and Health Services 2001;37(1):20‐4. [PubMed] [Google Scholar]
Etheridge 2008
- Etheridge A. MARU: Medical Architecture Research Unit. http://www.lsbu.ac.uk/maru/ 2008.
Fredrickson 2000
- Fredrickson BL. Cultivating positive emotions to optimize health and well‐being. Prevention & Treatment 2000;3(1):1 [Article A]. [Google Scholar]
Frumkin 2003
- Frumkin H. Healthy Places: Exploring the Evidence. American Journal of Public Health 2003;93(9):1451‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gesler 2004
- Gesler W, Bell M, Curtis S, Hubbard P, Francis S. Therapy by design: evaluating the UK hospital building program. Health & Place. 2004;10:117‐28. [DOI] [PubMed] [Google Scholar]
Gross 1998
- Gross R, Sasson Y, Zarhy M, Zohar J. Healing environment in psychiatric hospital design. General Hospital Psychiatry 1998;20(2):108‐14. [DOI] [PubMed] [Google Scholar]
Hewitt 2002
- Hewitt J. Psycho‐Affective Disorder in Intensive Care Units: a Review. Journal of Clinical Nursing 2002;11(5):575‐84. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2008. [Google Scholar]
Kaplan 1989
- Kaplan R, Kaplan S. The experience of nature: a psychological perspective. Cambridge, UK: Cambridge University Press, 1989. [Google Scholar]
Lacey 1974
- Lacey JI, Lacey BC. On heart rate responses and behavior: a reply to Elliot. Journal of Personality and Social Psychology 1974;30(1):1‐18. [DOI] [PubMed] [Google Scholar]
Lipley 2001
- Lipley N. Happy building, happy nurses. Nursing Standard 2001;15(19):12‐3. [Google Scholar]
Marberry 2002
- Marberry SO. Health Design: A ripple turns into a wave. Retrieved March 10, 2004 from http://www.isdesignet.com/Magazine/Mar'02/health.html 2002.
Melzack 1965
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science 1965;150(3699):971‐9. [DOI: 10.1126/science.150.3699.971] [DOI] [PubMed] [Google Scholar]
Melzack 1999
- Melzack R. From the gate to the neuromatrix. Pain Supplement 1999;6:S121‐6. [DOI] [PubMed] [Google Scholar]
Milburn 2001
- Milburn AM. Speech: Building a better patient environment. NHS Estates/Prince's Foundation Conference. The Prince's Foundation, 2001.
Millar 1995
- Millar K. Jelicic M. Bonke B. Asbury AJ. Assessment of preoperative anxiety: comparison of measures in patients awaiting surgery for breast cancer. British Journal of Anaesthesia 1995;74:180‐3. [DOI] [PubMed] [Google Scholar]
Neuberger 2003
- Neuberger J. Good design offers therapeutic rewards. Nursing Times 2003;99(37):17. [Google Scholar]
News 2004
- News: Second Dubai hospital design event. Hospital Development 2004; Vol. http://www.connectinghealthcare.com/story.asp?sC=2022393.
Parker 2000
- Parker J. Healing with design. Hospital Development 2000;Aug:11. [Google Scholar]
Parsons 1991
- Parsons R. The potential influences of environmental perception on human health. Journal of Environmental Psychology 1991;11(1):1‐23. [Google Scholar]
Pelikan 2001
- Pelikan JM, Krajic K, Dietscher C. The health promoting hospital (HPH): concept and development. Patient Education and Counseling 2001;45:239‐43. [DOI] [PubMed] [Google Scholar]
Rubin 1996
- Rubin HR, Owens AJ. Progress Report: An investigation to determine whether the built environment affects patients' medical outcomes. USA: The Centre of Health Design, 1996. [PubMed] [Google Scholar]
Spielberger 1983
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. State‐Trait Anxiety Inventory for Adults. Sampler Set, Manual, Test, Scoring Key. California: Mind Garden, 1983. [Google Scholar]
Takayanagi 2004
- Takayanagi K. Do pleasing pictures have a healing effect on seriously ill patients?. Proceedings of the 2004 Annual Research Meeting: The premier forum for health services research. San Diego: Academy Health, 2004.
Tanja‐Dijkstra 2011
- Tanja‐Dijkstra K, Pieterse ME. The psychological effects of the physical healthcare environment on healthcare personnel. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD006210.pub3] [DOI] [PubMed] [Google Scholar]
Thompson 2000
- Thompson JW. Healing words: wither the design of therapeutic gardens?. Landscape Architecture 2000;90(1):54‐7,73‐5. [Google Scholar]
Ulrich 1983
- Ulrich RS. Aesthetic and affective response to natural environment. In: Altman I, Wohlwill JF editor(s). Human Behaviour and Environment. New York: Plenum Press, 1983:85‐125. [Google Scholar]
Ulrich 1992
- Ulrich RS. How design impacts wellness. Healthcare Forum Journal 1992;35(5):20‐5. [PubMed] [Google Scholar]
Ulrich 1993a
- Ulrich RS. Biophilia, biophobia and natural landscapes. In: Kellert S, Wilson EO editor(s). The Biophilia Hypothesis. Washington DC: Island Press/Shearwater Books, 1993:73‐137. [Google Scholar]
Ulrich 2004a
- Ulrich RS, Zimring C. The Role of the Physical Environment in the Hospital of the 21st Century: A Once‐in‐a‐Lifetime Opportunity. The Centre for Health Design 2004.
Ulrich 2004b
- Ulrich RS. The relationship between the design of buildings and the delivery of healthcare services. The Third National SDO Conference: Delivering Research for Better Health Services (CD‐ROM). London: SDO, 2004.
Ulrich 2008
- Ulrich RS, Zimring C, Zhu X, DuBose J, Seo H‐B, Choi Y‐S, Quan X, Joseph A. A review of the research literature on evidence‐based healthcare design. Health Environments Research & Design Journal 2008;1(3):101‐65. [DOI] [PubMed] [Google Scholar]
Van den Berg 2005
- Berg EA. Health impacts of healing environments: A review of evidence for benefits of nature, daylight, fresh air, and quiet in healthcare settings. Groningen: The Architecture of Hospitals, 2005. [Google Scholar]
Ward 2008
- Ward D, Drahota A, Gal D, Severs M, Dean T. Care home versus hospital and own home environments for rehabilitation of older people. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD003164.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zimmerman 1996
- Zimmerman L, Nieveen J, Barnason S, Schmaderer M. The effects of music intervention on postoperative pain and sleep in coronary artery bypass graft (CABG) patients. Scholarly Inquiry for Nursing Practice: An International Journal 1996;10(2):153‐70. [PubMed] [Google Scholar]


