Abstract
Background
The choice of surgical approach for the management of subaxial cervical spine facet dislocations is a controversial subject amongst spine surgeons. Reasons for this include differences in the technical familiarity and experience of surgeons with the different surgical approaches, and variable interpretation of image studies regarding the existence of a traumatic intervertebral disc herniation and of the neurological status of the patient. Moreover, since the approaches are dissimilar, important variations are likely in neurological, radiographical and clinical outcomes.
Objectives
To compare the effects (benefits and harms) of the different surgical approaches used for treating adults with acute cervical spine facet dislocation.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (9 May 2014), The Cochrane Central Register of Controlled Trials (The Cochrane Library, 2014 Issue 4), MEDLINE (1946 to April Week 5 2014), MEDLINE In‐Process & Other Non‐Indexed Citations (8 May 2013), EMBASE (1980 to 2014 Week 18), Latin American and Caribbean Health Sciences (9 May 2014), trial registries, conference proceedings and reference lists of articles to May 2014.
Selection criteria
We included randomised and quasi‐randomised controlled trials that compared surgical approaches for the management of adults with acute cervical spine facet dislocations with and without spinal cord injury.
Data collection and analysis
Two review authors independently selected studies, assessed risk of bias and extracted data.
Main results
We included one randomised and one quasi‐randomised controlled trial involving a total of 94 participants and reporting results for a maximum of 84 participants. One trial included patients with spinal cord injuries and the other included patients without spinal cord injuries. Both trials compared anterior versus posterior surgical approaches. Both trials were at high risk of bias, including selection bias (one trial), performance bias (both trials) and attrition bias (one trial). Data were pooled for one outcome only: non‐union. Reflecting also the imprecision of the results, the evidence was deemed to be of very low quality for all outcomes; which means that our level of uncertainty about the estimates is high.
Neither trial found differences between the two approaches in neurological recovery or status, as shown in one study by small clinically insignificant differences in NASS (Northern American Spine Society) neurological scores (0 to 100: optimal score) at one year of follow‐up: anterior mean score: 85.23 versus posterior mean score: 83.86; mean difference (MD) 1.37 favouring anterior approach, 95% confidence interval (CI) ‐9.76 to 12.50; 33 participants; 1 study). The same trial found no relevant between‐approach differences at one year in patient‐reported quality of life measured using the 36‐item Short Form Survey physical (MD ‐0.08, 95% CI ‐7.26 to 7.10) and mental component scores (MD 2.88, 95% CI ‐3.32 to 9.08). Neither trial found evidence of significant differences in long‐term pain, or non‐union (2/38 versus 2/46; risk ratio (RR) 1.18, 95% CI 0.04 to 34.91). One trial found better sagittal and more 'normal' alignment after the anterior approach (MD ‐10.31 degrees favouring anterior approach, 95% CI ‐14.95 degrees to ‐5.67 degrees), while the other trial reported no significant differences in cervical alignment. There was insufficient evidence to indicate between‐group differences in medical adverse events, rates of instrumentation failure and infection. One trial found that the several participants had voice and swallowing disorders after anterior approach surgery (11/20) versus none (0/22) in the posterior approach group: RR 25.19, 95% CI 1.58 to 401.58); all had recovered by three months.
Authors' conclusions
Very low quality evidence from two trials indicated little difference in long‐term neurological status, pain or patient‐reported quality of life between anterior and posterior surgical approaches to the management of individuals with subaxial cervical spine facet dislocations. Sagittal alignment may be better achieved with the anterior approach. There was insufficient evidence available to indicate between‐group differences in medical adverse events, rates of instrumentation failure and infection. The disorders of the voice and swallowing that occurred exclusively in the anterior approach group all resolved by three months. We are very uncertain about this evidence and thus we cannot say whether one approach is better than the other. There was no evidence available for other approaches. Further higher quality multicentre randomised trials are warranted.
Keywords: Adult; Female; Humans; Male; Cervical Vertebrae; Cervical Vertebrae/injuries; Joint Dislocations; Joint Dislocations/surgery; Neck Pain; Neck Pain/diagnosis; Orthopedic Procedures; Orthopedic Procedures/methods; Pain, Postoperative; Pain, Postoperative/diagnosis; Quality of Life; Randomized Controlled Trials as Topic; Recovery of Function; Zygapophyseal Joint; Zygapophyseal Joint/injuries
Plain language summary
Surgical approaches for dislocations of the neck bones
The part of the back bone found in the neck is called the cervical spine. It consists of seven bones (or vertebrae). The relative movement of these vertebrae is mainly via small joints (called facet joints) located between each vertebrae. The facet joints in the cervical spine facilitate good movement of the neck, but they are vulnerable to dislocation. Typically, cervical spine facet dislocations are caused by high‐energy traumas such as road traffic accidents or violent attacks. Approximately half of people with such dislocations sustain an injury to the spinal cord carried within the spine. This can result in significant impairment of function (e.g. paralysis). Surgery is usually needed for these serious injuries in order to keep the neck bones in place.
What are the different surgical approaches? There are two main stages to surgery: reduction and fixation. Reduction is the restoration of an injured or dislocated bone or joint to its normal anatomical position, and can be achieved either with surgery or through closed reduction, which is performed with traction or manipulation. Fixation is the medical procedure used to stabilise one or more joints, or a fractured bone, usually by surgically inserting devices such as wires, screws, plates and rods. Fixation of the injury is generally accomplished by either an anterior or posterior surgical approach. With an anterior cervical approach the surgery is performed through an incision over the front surface of the neck, while the posterior cervical approach consists of a lengthwise midline incision over the back part of the neck and dissection through muscle to the cervical vertebrae. This approach gives direct access to the dislocated facet joints.
Description of the studies included in the review We searched the medical literature until May 2014 and found two relevant studies that included a total of 94 adults with cervical spine facet dislocations. One trial included individuals with spinal cord injuries and the other included individuals without spinal cord injuries. Both studies compared the anterior versus posterior surgical approach.
Quality of the evidence The two studies were small and both were at high risk of bias. We therefore judged the quality of the evidence to be very low.
Summary of the evidence Neither study found differences between the two approaches in neurological status and pain at one year. One study also found no differences between the two approaches in patient‐reported quality of life. Although one study found that the anterior approach resulted in more normal curvature of the neck, the other study reported finding no difference between the two approaches with regard to the alignment of the neck vertebrae. The evidence was insufficient to indicate differences between the two approaches in medical adverse events, rates of instrumentation failure and infection. Although over half (11) of 20 people in the anterior approach group in one study had voice and swallowing disorders, these all resolved by three months.
Conclusion The quality of the evidence was very low, meaning that we are very uncertain about the direction and size of effect. Thus we are unable to say whether either an anterior or posterior approach to the surgical management of individuals with dislocations to the cervical spine facet joints is better than the other. We suggest that further research is needed to inform the choice of surgical approach.
Summary of findings
Summary of findings for the main comparison. Anterior versus posterior surgical approaches for cervical facet dislocations in adults.
| Anterior versus posterior approach for cervical facet dislocations in adults | ||||||
| Population: adults with cervical spine facet dislocations Settings: hospital Intervention: anterior approach Comparison: posterior approach | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk1 | Corresponding risk | |||||
| Posterior approach | Anterior approach | |||||
| Final post‐surgical neurological status NASS (North American Spine Society) scores. Scale from: 0 to 100 (higher scores indicate better neurological function). Follow‐up: mean 12 months | Mean 83.86 (range 43.3 to 100) | The mean final post‐surgical neurological status in the anterior group was 1.37 higher (9.76 lower to 12.5 higher) | 33 (1 study)2 | ⊕⊝⊝⊝ very low3 | Another study (47 participants), which included patients with spinal cord injury, reported that there was no significant differences in neurological recovery between the two groups (very low quality evidence)4 | |
| Functional aspects and quality of life ‐ SF‐36 physical scores SF‐36. Scale from: 0 to 100 (higher scores indicate better quality of life). Follow‐up: mean 12 months | Mean 46.91 (range 35.2 to 58.9) |
The mean SF‐36 physical score in the anterior group was 0.08 lower (7.26 lower to 7.1 higher) | 33 (1 study)2 | ⊕⊝⊝⊝ very low3 | ||
| Emotional aspects and quality of life ‐ SF‐36 mental scores SF‐36. Scale from: 0 to 100 (higher scores indicate better quality of life). Follow‐up: mean 12 months | Mean 49.3 (range 29.9 to 62.1) |
The mean SF‐36 mental score in the anterior group was 2.88 lower (3.32 lower to 9.08 higher) | 33 (1 study)2 | ⊕⊝⊝⊝ very low3 | ||
| Pain North Americal Spine Society pain scores. Scale from: 0 to 100 (higher scores indicate less pain). Follow‐up: mean 12 months | Mean 81.67 (range 58 to 100) |
The mean NASS pain score was 4.14 higher in the anterior group (5.54 lower to 13.82 higher) | 33 (1 study)2 | ⊕⊝⊝⊝ very low3 | Another study (47 participants), which included patients with spinal cord injury, reported that seven participants in each group had neck pain (7/20 anterior group versus 7/27 posterior group; RR 1.35, 95% CI 0.56 to 3.23) (very low quality evidence)4 |
|
| Non‐fusion at follow‐up Radiographic data Follow‐up: 12 to 17 months | Study population | RR 1.18 (0.04 to 34.91) | 84 (2 studies) |
⊕⊝⊝⊝ very low3,4 | ||
| 43 per 1000 | 51 per 1000 (2 to 1000) | |||||
| Sagittal alignment Scale from: ‐20 to 20 degrees. Follow‐up: mean 12 months | Mean 1.55 degrees | The mean sagittal alignment was 10.31 lower in the anterior group (14.95 to 5.67 lower) | 36 (1 study)2 | ⊕⊝⊝⊝ very low3 | Lower (negative) degrees indicate physiological cervical alignment. Another study (47 participants), which included patients with spinal cord injury, reported no differences in changes in alignment between the two approaches (very low quality evidence)4 |
|
| Complications Number of events Follow‐up: mean 12 months | Swallowing/voice disorders (short‐term) | RR 25.19 (1.58 to 401.58) | 42 (1 study)2 | ⊕⊝⊝⊝ very low3 | Very low quality evidence3 did not confirm between‐group differences in medical adverse events, rates of instrumentation failure and infection. The only significant difference found related to voice and swallowing disorders after anterior approach surgery; this was reported only in one study. All had recovered by three months | |
| 0 per 1000 | 550 per 1000 (actual results) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio; SF‐36: 36‐item Short‐Form Survey | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1. The assumed risk is based on that provided in the included studies.
2. This study excluded patients with spinal cord injury.
3. The evidence was downgraded two levels for limitations in study design and implementation (primarily performance bias from lack of clinician and participant blinding, and attrition bias) and one level for imprecision (small sample size and wide CI).
4. The evidence was downgraded two levels for limitations in study design and implementation (primarily selection bias from inadequate randomisation method and lack of allocation concealment, performance bias from lack of clinician and participant blinding, detection bias from lack of outcome assessment blinding and other bias, especially imbalances in baseline characteristics) and one level for imprecision (small sample size and either wide CI or a clearly large range in values).
Background
Description of the condition
Fractures and dislocations of the spine are among the most challenging in trauma clinical practice. Vertebral column injuries occur in approximately 6% of trauma patients, half of which sustain spinal cord or nerve root neurological deficits (Burney 1993). The main causes of traumatic spinal cord injury (SCI) are motor vehicle‐related accidents (39.5% to 55%), violence (14.2% to 29.5%), falls (18.8% to 23%) and sports injuries (7.3% to 11.1%) (Burke 2001; DeVivo 1997; Nobunaga 1999). For definitions of some of the terms used in this review, see the Glossary in Table 2.
1. Glossary.
| Term | Definition |
| Discectomy | Excision (cutting out), in part or whole, of an intervertebral disc. The most common indication is disc displacement or herniation (see 'Hernia'). In addition to standard surgical removal, it can be performed by percutaneous discectomy or by laparoscopic discectomy, the former being the more common |
| Fracture | A break in a bone |
| Fracture fixation | The use of usually metallic devices inserted into or through bone to hold a fracture in a set position and alignment while it heals |
| Facet dislocation | Complete displacement that occurs between facets of the interior (located below) and superior (located above) articular processes of adjacent vertebrae |
| Hernia | Protrusion (pushing out) of tissue, structure or part of an organ through the muscular tissue or the membrane by which it is normally contained |
| Reduction | The restoration, by surgical or manipulative procedures, of a part to its normal anatomical relation |
| Surgical decompression | A surgical operation for the relief of pressure in a body compartment or on a body part |
| Pseudarthrosis | A pathological entity characterised by persistent non‐union of bone fragments, leading to formation of a false joint |
| Non‐union | Failure of healing at the ends of a fracture |
| Fusion | Formation of an ankylosis by surgical means |
The incidence of SCIs in North America has remained stable over the past 30 years, and ranges between 27 and 47 cases per million population (Fisher 2006). In addition, it has been estimated that the annual incidence of SCIs requiring hospitalisation in developed countries is approximately 11.5 to 53.4 per million population (Kraus 1975; Surkin 2000). The most common site of SCI is the cervical region, accounting for 50% to 64% of traumatic SCIs (Tator 1995). Approximately 40% of these injuries are associated with a neurological deficit (Lasfargues 1995). Moreover, the incidence of traumatic disc herniations at the site of injury in this population may be about 54% (Robertson 1992).
The cervical or neck region of the spine consists of seven vertebrae. The first and second cervical vertebrae (C1 and C2), respectively, the atlas and axis, form the upper cervical spine. The lower cervical spine comprises the third to the seventh vertebrae (C3 to C7). Below this is the thoracic region of the spine, starting with the T1 vertebra. Relative movement of the vertebrae is primarily via the facet joints. Starting from below C2, intervertebral discs lie between the cylindrical parts (centrum) of adjacent vertebrae. These discs act as shock absorbers, as well as allowing movement.
A traditionally used classification system for subaxial cervical spine injuries is that described by Allen 1982. This is based on the mechanism of injury, and is divided into six categories: compression‐flexion, vertical compression, distraction‐flexion, compression‐extension, distraction‐extension and lateral flexion. Facet dislocations are classified as distraction‐flexion injuries and account for approximately 10% of all subaxial cervical spine fractures. They may be unilateral or bilateral. Although pure ligamentous facet injuries, by definition, are classified as facet dislocations, it is important to note that facet fractures are part of the same spectrum of injury. Both types are probably the result of subtle differences in injury mechanism, in which pure ligamentous injuries occur when distractive forces across the posterior elements outweigh shear forces, whereas facet fractures take place when the facet is subjected to a relatively greater shear force. Both have similar associated instability patterns and diagnostic, therapeutic and prognostic factors (Bellabarba 2006).
Description of the intervention
Several aspects in the management of facet dislocations are controversial. Intervention may be considered in two stages: a) reduction, which can be performed closed with skull traction or surgically (by an anterior or posterior approach), and b) internal fixation, which can be performed by an anterior or posterior approach.
It should be clearly established whether it is safe to undertake closed manipulation of the neck either awake or under anaesthesia. The timing of such closed reduction is important. Some authors believe that an early, successful, closed reduction protects neurological elements during the mobilisation of the patient and may potentially improve neurorecovery in compromised patients compared with delayed reduction (Kahn 1998; Lee 1994). Occasionally, gentle manipulation by an experienced surgeon can be necessary to reduce a perched facet during the traction procedure (Star 1990). Any treatment will be complicated by the presence of an intervertebral disc prolapse. Whether magnetic resonance imaging (MRI) is required before intervention is uncertain, with some authors arguing that, due to the high incidence of herniated discs at the time of cervical dislocations, an MRI scan should be obtained prior to reduction (Eismont 1991; Robertson 1992) and others considering that imaging is unnecessary during immediate, awake, closed traction in an alert and cooperative patient (Hart 2002).
Generally, facet dislocations are stabilised posteriorly, but there has been a trend towards anterior surgery, due to concern regarding the potential for any disc herniation to lead to spinal cord compression (De Lure 2003; Doran 1993; Eismont 1991; Harrington 1991; Harrop 2001; Maiman 1986).
Open posterior reduction and stabilisation is accomplished by a distraction manoeuvre and the placing of a small instrument between the dislocated facets or, if necessary, by removal of the superior part of the caudal facet, allowing the dislocated facet to fall back to its original position. The subsequent fixation may be performed with sublaminar or spinous process wires, or both, or lateral mass or pedicle screws.
The anterior approach is initiated with decompression and discectomy at the level (of the spine) compromised by the injury, followed by a reduction manoeuvre (if necessary) that can be performed in many ways, including distraction with sequential application of weight, direct manipulation or reduction through Caspar vertebral pins. Thereafter, fixation may be achieved with iliac crest graft or cage placement at the intervertebral space associated with anterior cervical plating.
Some studies justify anterior procedures on the grounds of safety (Ordonez 2000; Reindl 2006), whereas others promote posterior cervical reduction and fusion even in the presence of a herniated disc (Abumi 2000), or anterior cervical discectomy and grafting followed by a posterior reduction and fusion (Allred 2001).
How the intervention might work
All surgical approaches (including anterior‐ and posterior‐only approaches) for cervical facet dislocation may be used for reduction and fixation in an attempt to acquire anatomical realignment and bony fusion, and maximise neurological recovery, long‐term relief of pain, functional recuperation and early return to activities of daily living.
Why it is important to do this review
The seriousness of cervical spine facet dislocations, including the risk of major complications such as paralysis, points to the need for evidence‐based practice. Although there appears to be a trend towards the use of the anterior approach for some types of these injuries, a recent survey found poor overall agreement between surgeons on the choice of surgical approach (Nassr 2008). This underlying variation in treatment indicates the uncertainty on the best approach and the need to conduct a systematic review of the best evidence to inform practice.
Objectives
To compare the effects (benefits and harms) of the different surgical approaches used for treating adults with acute cervical spine facet dislocation.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐randomised (a method of allocating participants to a treatment which is not strictly random, e.g. by date of birth, hospital record number, alternation) controlled trials.
Types of participants
We included all studies relating to adults with an acute (less than three weeks) and radiologically confirmed distraction‐flexion dislocation or fracture‐dislocation of the lower cervical spine with or without neurological deficit. Trials including participants with unilateral or bilateral facet dislocation injuries were included. Trials including adolescents or people with other cervical spine injuries, or both, were included, provided separate data could be obtained or the proportion included was small.
Types of interventions
Included were trials comparing different surgical approaches for these injuries. The main comparison was the anterior versus the posterior approach for either open reduction and fixation or fixation after initial closed reduction.
1. Anterior surgical approaches, including:
anterior cervical surgical reduction and fixation;
closed reduction followed by anterior cervical surgical fixation.
2. Posterior surgical approaches, including:
posterior cervical surgical reduction and fixation;
closed reduction followed by posterior cervical surgical fixation.
3. Combined approaches following closed reduction:
anterior‐posterior;
anterior‐posterior‐anterior;
posterior‐anterior.
4. Combined approaches (with open reduction):
anterior‐posterior;
anterior‐posterior‐anterior;
posterior‐anterior.
Types of outcome measures
Primary outcomes
Final post‐surgical neurological status (recovery or deterioration)
Secondary outcomes
Functional aspects and quality of life
Pain
-
Radiographical outcomes
Bone fusion
Dislocation reduction or sagittal realignment
Complications
Economic data
We considered only validated measure instruments for analysis. We accepted outcomes measured at any time of follow‐up.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (9 May 2014), The Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library, 2014 Issue 4), MEDLINE (1946 to April Week 5 2014), MEDLINE In‐Process & Other Non‐Indexed Citations (8 May 2013), EMBASE (1980 to 2014 Week 18) and LILACS (Latin American and Caribbean Health Sciences) database (9 May 2014). We also searched Current Controlled Trials (May 2014) and the World Health Organization (WHO) International Clinical Trials Registry Platform (May 2014). No language restrictions were applied.
We present search strategies composed of descriptors for the clinical condition, intervention of interest, as well as an RCT filter for each database in Appendix 1. We combined the MEDLINE search with the sensitivity‐ and precision‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying RCTs (Lefebvre 2011) and the LILACS search with the optimal search strategy for clinical trials in LILACS (Castro 1999).
Searching other resources
We also searched the reference lists of relevant articles, including narrative reviews, and book chapters. We screened conference proceedings from Orthopaedic Trauma Association Annual Meetings (1996 to 2013) and EuroSpine Meetings (2007 to 2013). We also contacted other researchers and experts in the field.
Data collection and analysis
The intended methodology for data collection and analysis was described in our published protocol (Del Curto 2009).
Selection of studies
Two review authors (DDC and DEM) independently assessed the titles and abstracts of the identified articles to determine potential relevance. The same authors analysed the full text of potentially relevant articles to assess eligibility. All disagreements were resolved by discussion or by a third opinion (JCB).
Data extraction and management
Two review authors (DDC and DEM) independently extracted data from each study using a pre‐piloted data extraction form. All unresolved disagreements were resolved by discussion with another author (JCB).
Assessment of risk of bias in included studies
Two review authors (DDC and DEM) independently assessed the risk of bias of the included studies using The Cochrane Collaboration's 'Risk of bias' tool (Higgins 2008). This tool incorporates the assessment of randomisation (sequence generation and allocation concealment), blinding of participants and personnel (for performance bias), blinding of outcome assessment (for detection bias), completeness of outcome data, selection of outcomes reported and other sources of bias. Other considered sources of bias included bias resulting from major imbalances in baseline characteristics (e.g. the presence of SCI) and performance bias, where we assessed the risk of bias from systematic differences in the experience of the operating surgeon(s) and subsequent rehabilitation. All unresolved disagreements were resolved by discussion with a third author (JCB). Titles of journals, names of authors or supporting institutions were not masked at any stage.
Measures of treatment effect
Where appropriate, we calculated risk ratios (RR) with 95% confidence intervals (CIs) for dichotomous outcomes and mean differences (MD) with 95% CIs for continuous outcomes. When data from primary studies were not parametric (e.g. effects reported as medians and quartiles, etc) or were not adequately reported (e.g. without standard deviations), we presented these in text or tables, or both.
Unit of analysis issues
The individual participant was both the unit of randomisation and the unit of analysis in included trials. We avoided other unit of analysis issues such as presenting total numbers of complications rather than numbers of participants with complications, where participants have more than one complication.
Dealing with missing data
For dichotomous data, we attempted to perform intention‐to‐treat analyses including all participants randomised to the intervention groups. For continuous data, we intended, if necessary by contacting trial investigators, to favour 'last observation carried forward' analyses for accounting for missing data. When our efforts to acquire missing data from authors were unsuccessful, we performed available case analyses and thus just used the data that were available. We stipulated beforehand that we would assume there were no dropouts in any study that did not report dropouts.
Assessment of heterogeneity
We assessed heterogeneity by visual inspection of the forest plot (analysis) together with consideration of the Chi² test for heterogeneity and the I² statistic (Higgins 2003). We based our quantitative assessment of heterogeneity mainly on the I² statistic, and interpreted it according to the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011) where 0% to 40% might not be important, 30% to 60% may represent moderate heterogeneity, 50% to 90% may represent substantial heterogeneity and 75% to 100% may represent very substantial (considerable) heterogeneity.
Assessment of reporting biases
In future, should a sufficient number of studies be available (10 studies), we will attempt to assess publication bias by preparing a funnel plot. However, we remain aware that asymmetry in the funnel plot can be associated with other reasons than publication bias (e.g. chance, real heterogeneity and clinical particularities inherent to each of the included studies, such as participants at high risk for the outcome).
Data synthesis
When appropriate, we pooled the results of comparable groups and calculated the 95% CI. In future updates, we plan to present MDs for continuous outcomes unless data are derived from disparate outcome measures, in which case standardised mean differences (SMDs) will be presented. We used the random‐effects model because, as expected, there was substantial clinical and methodological heterogeneity between studies, which could generate substantial statistical heterogeneity.
Subgroup analysis and investigation of heterogeneity
We planned but could not carry out subgroup analyses by age and gender, fracture type (unilateral versus bilateral facet dislocation), neurological status (neurologically intact, incomplete and complete SCI) and use/non‐use of MRI before reduction.
Sensitivity analysis
Where possible, we planned sensitivity analyses to examine various aspects of trial and review methodology, including the effects of intention‐to‐treat and available data analyses, and the inclusion of trials without concealment of allocation or those reported only in abstract form.
Quality assessment and 'Summary of findings' table
We used the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach to assess the quality of evidence relating to the listed outcomes (Higgins 2011, Section 12.2) and generated a 'Summary of findings' table for the sole comparison tested in the review.
Results
Description of studies
Results of the search
We completed the search in May 2014. We screened a total of 949 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (122 records); CENTRAL (169), MEDLINE (75), EMBASE (578), LILACS (5), Current Controlled Trials (0) and the WHO International Clinical Trials Registry Platform (0). We did not identify any potentially eligible studies from other sources such as the manual search of references.
We identified three potentially eligible studies, for which full reports were obtained. Upon study selection, we included two studies (Brodke 2003; Kwon 2007) and excluded one (Kandziora 2005). We did not identify any ongoing studies.
A flow diagram summarising the study selection process is presented in Figure 1.
1.
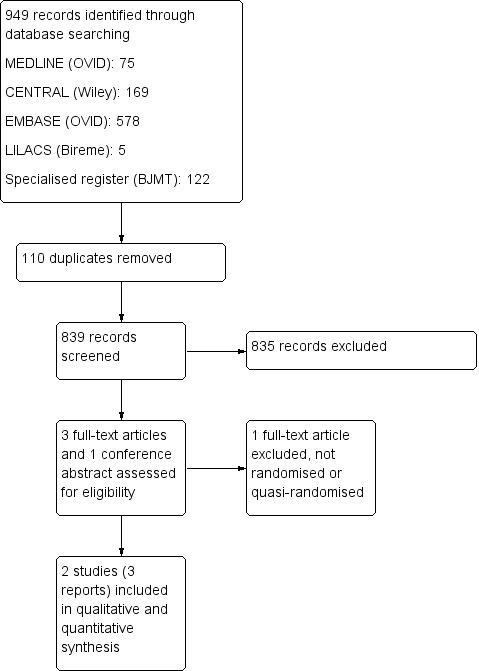
Study flow diagram.
Included studies
We included two studies in this review (Brodke 2003; Kwon 2007). Brodke 2003 was also reported in abstract form at the Orthopaedic Trauma Association Annual Meeting in September 1996. For further details, please see the Characteristics of included studies.
Design
Brodke 2003 was a quasi‐randomised trial, where allocation was according to the day of admission. In Kwon 2007, participants were randomised "according to a block randomisation procedure".
Sample sizes
The two studies included a total of 94 participants. Brodke 2003 included 52 participants, and presented results for at least six months of follow‐up for 47 participants. Kwon 2007 included 42 participants, and presented results for 12 months of follow‐up for 33 participants.
Setting
There was no information available as to whether studies were conducted in single or multiple centres. Brodke 2003 was conducted in the USA and Kwon 2007 in Canada.
Participants
Most of the participants in each trial were male (79% of the trial population in Brodke 2003 and 74% in Kwon 2007). The mean age was 35 years in both studies. An important difference between participants in the studies was that Brodke 2003 specifically included individuals with spinal cord injuries (SCIs), whereas Kwon 2007 included individuals with unilateral facet fractures or dislocations without SCIs. Brodke 2003 included individuals with different types of spine injuries, most of them including facet joint dislocations. However, Brodke 2003 also included seven people with burst type fractures only.
Interventions
Both trials compared the anterior surgical approach versus the posterior surgical approach in the treatment of cervical spine injuries.
Outcomes
Primary outcomes
Final post‐surgical neurological status was evaluated in Brodke 2003 on the last day of follow‐up (minimum of six months) using the Frankel classification (Frankel 1969) and the American Spinal Injury Association (ASIA) motor index score (ASIA 1992).
Kwon 2007 reported on neurological function using NASS (Northern American Spine Society) neurological scores after 12 months of follow‐up.
Secondary outcomes
Clinical outcomes were assessed in both studies. Kwon 2007 reported on functional aspects and quality of life via the 35‐item Short‐Form Survey (SF‐36). Both studies reported pain as an outcome. However, Brodke 2003 reported only the numbers of participants reporting neck pain at final follow‐up and Kwon 2007 reported postoperative pain on day one and day two, assessed via a visual analogue scale (VAS), and at one year, assessed via the NASS cervical spine pain score.
Radiographical outcomes were reported in both studies. Brodke 2003 and Kwon 2007 both evaluated fusion rates and sagittal alignment at the level of injury. Brodke 2003 also assessed kyphotic angulation across the injury site and anterior‐posterior displacement of the vertebral body.
Both studies reported complications as an outcome.
Kwon 2007 reported on the duration of time required for a participant to achieve a standard set of discharge criteria. The relation between these criteria and actual discharge criteria was not discussed in the trial report.
Excluded studies
We excluded one study because it was not randomised (Kandziora 2005) (see the Characteristics of excluded studies).
Risk of bias in included studies
2.
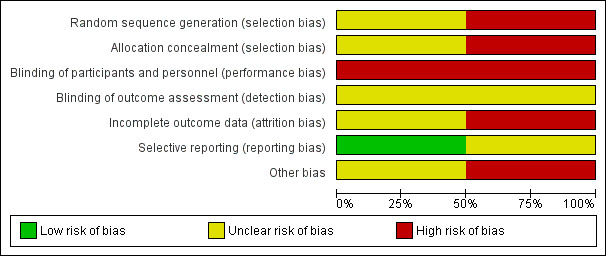
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.
3.
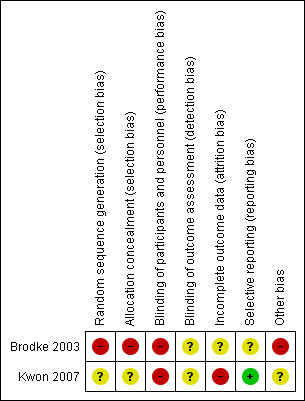
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
Allocation
Since Brodke 2003 was quasi‐randomised with allocation based on the day of admission, we judged this trial to be at high risk of selection bias relating to inadequate sequence generation and lack of allocation concealment. Kwon 2007 reported only that it used a block randomisation process. Given the lack of details on which to make a judgement, we rated Kwon 2007 as being at unclear risk of selection bias relating to sequence generation and allocation concealment.
Blinding
Due to the nature of the interventions, blinding was not feasible either for participants or treatment providers. Hence, we judged both trials to be at high risk of performance bias relating to lack of blinding. Both trials referred to independent but not treatment‐blinded outcome assessment. We judged detection bias to be unclear for both trials.
Incomplete outcome data
Both studies described the participants who were lost to follow‐up as well as those who were excluded. However, outcome data for those participants were not available, even after our attempts to obtain these data from the trial authors.
We judged Brodke 2003 to be at unclear risk of attrition bias, as there were similar losses to follow‐up from the final analysis in both groups. Of the five excluded participants (9.6%), two had died of other injuries in the early postoperative period in the anterior group (9%) and three had less than six months of follow‐up in the posterior group (10%).
We considered Kwon 2007 to be at high risk of bias as losses to follow‐up were not evenly distributed between allocation groups. For patient‐reported outcomes of functional aspects and quality of life, 6 of 20 participants from the anterior group (30%) and 3 of 22 (14%) from the posterior group were lost to follow‐up or did not send back outcome questionnaires at the one year follow‐up. For radiographical outcomes, 2 of 20 (10%) participants randomised to anterior surgery and 3 (14%) of those randomised to posterior surgery did not complete follow‐up at the one‐year postoperative time point.
Selective reporting
All the outcomes described in the methods of both studies were presented in the results. However, we judged Brodke 2003 to be at unclear risk of selective reporting bias because the scoring system for the Frankel classification of neurological status was incompletely described, as well as being inappropriate. We judged Kwon 2007 to be at low risk for reporting bias.
Other potential sources of bias
In Brodke 2003, there were important between‐group baseline differences in type of injury and neurological status; additionally, the mean time to surgery was twice as long in the anterior group as in the posterior group (10 versus 5 days). We thus judged this trial to be at high risk of other bias. We judged Kwon 2007 to be at unclear risk of other bias because of the variety of instrumentation devices used in both participant groups, especially in the posterior fixation group, in which lateral mass screws with plates, or posterior wiring, or both, were used.
Effects of interventions
See: Table 1
The only surgical approaches compared in these trials included in this review were the anterior and posterior approaches.
Primary outcomes
Final post‐surgical neurological status
Brodke 2003 presented preoperative and final follow‐up data on neurological outcomes based on Frankel grades (see below) and the ASIA motor score (ASIA 1992).
The Frankel classification grading system is shown below (Frankel 1969).
Grade A: complete neurological injury ‐ no motor and sensory function below the injured level
Grade B: some sensation present below the lesion (injured level) but the motor paralysis is complete below that level
Grade C: some motor power present below the lesion but it is of no practical use to the patient
Grade D: useful motor power below the level of lesion
Grade E: normal motor and sensory functions (some abnormalities may still be present)
The baseline distribution of Frankel grades differed between the groups; for example, 10 (50% of 20) participants in the anterior group had grade A injuries, compared with 16 (59% of 27) in the posterior group. Whereas 14 of 20 (70%) participants in the anterior group and 15 of 27 (56%) participants in the posterior group improved one grade or more, this outcome measure is unsatisfactory given the different extents of recovery between the different levels and the differences in the baseline distribution.
The mean ASIA motor index scores (0 to 100, where 100 is the optimal score) increased from 43 to 64 in the anterior group and from 40 to 54 in the posterior group. This difference was reported to be not statistically significant but the study authors did not provide standard deviations or respond to our request for these data.
Neurological status at one year of follow‐up was evaluated in Kwon 2007 using NASS neurological scores (0 to 100, where 100 is the optimal score) in 33 participants (14 in the anterior group and 19 in the posterior group) and found no difference between groups (anterior mean: 85.23 versus posterior mean: 83.86; MD 1.37, 95% CI ‐9.76 to 12.50) (Analysis 1.1).
1.1. Analysis.
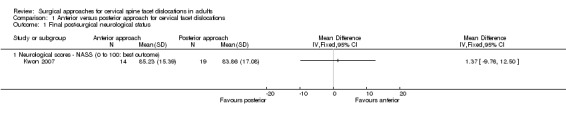
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 1 Final post‐surgical neurological status.
Secondary outcomes
Functional aspects and quality of life
Brodke 2003 did not report these outcomes.
In Kwon 2007, 12 months after surgery, 33 participants (14 versus 19) completed the SF‐36 and the NASS cervical spine questionnaire. There were no statistically significant differences between participants for the SF‐36 physical component score (anterior mean: 46.83 versus posterior mean: 46.91; MD ‐0.08, 95% CI ‐7.26 to 7.10) or mental component scores (anterior mean: 52.31 versus posterior mean: 49.43; MD 2.88, 95% CI ‐3.32 to 9.08) (Analysis 1.2). These are both scored on a 0 to 100 scale, with 100 being the best score and a score of 50 representing the mean for a normal population; neither of the mean differences amounted to a clinically important difference.
1.2. Analysis.
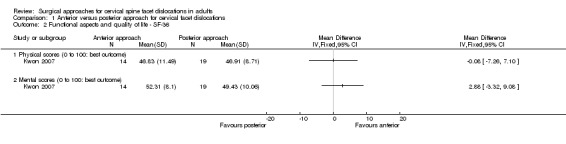
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 2 Functional aspects and quality of life ‐ SF‐36.
Pain
Brodke 2003 reported that seven participants in each group had neck pain at final follow‐up (7/20 anterior approach versus 7/27 posterior approach; RR 1.35, 95% CI 0.56 to 3.23; Analysis 1.3).
1.3. Analysis.
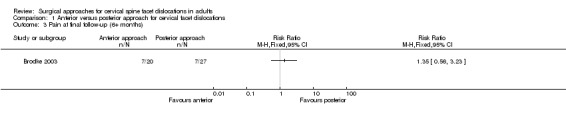
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 3 Pain at final follow‐up (6+ months).
In Kwon 2007, pain was assessed using a VAS on the first and second postoperative days. On this scale, 0 means no pain and 10 represents the worst pain. Pain scores on both days favoured the anterior group, but the MD was less than the minimum clinically important difference and the results on the second postoperative day only were of borderline statistical significance (anterior mean: 2.10 versus posterior mean: 2.98; MD ‐0.88, 95% CI ‐1.76 to 0.00) (Analysis 1.4). At one year of follow‐up, pain was evaluated using NASS cervical spine pain scores and no difference was apparent between the two groups (anterior mean: 85.81 versus posterior mean: 81.67; MD 4.14, 95% CI ‐5.54 to 13.82) (Analysis 1.5).
1.4. Analysis.
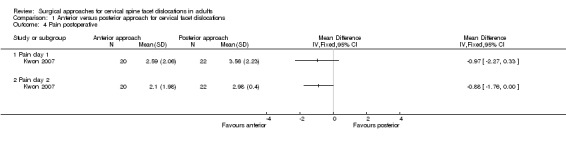
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 4 Pain postoperative.
1.5. Analysis.
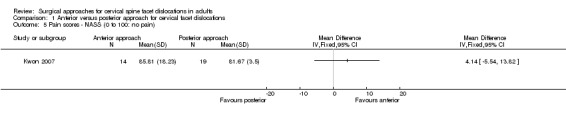
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 5 Pain scores ‐ NASS (0 to 100: no pain).
Radiographical outcomes
Two participants in the anterior group of Brodke 2003 and two in the posterior group of Kwon 2007 were found to have non‐fusion or union at final follow‐up. Hence, only two participants had non‐bony fusion in each group in the pooled results (2/38 versus 2/46; RR 1.18, 95% CI 0.04 to 34.91; Analysis 1.6).
1.6. Analysis.
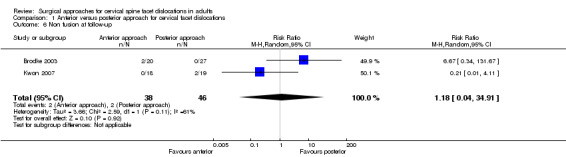
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 6 Non fusion at follow‐up.
Brodke 2003 reported, without providing usable data, that there were “no significant differences in improved alignment or loss of correction between groups”. In Kwon 2007, however, the average sagittal alignment at the level of injury of participants treated by the anterior approach was 8.76 degrees (SD 5.96 degrees) of lordosis; whereas in those treated by posterior approach, the mean sagittal alignment was 1.55 degrees (SD 8.17 degrees) of kyphosis, which represents a statistically significant difference favouring the anterior group (MD ‐10.31 degrees, 95% CI ‐14.95 degrees to ‐5.67 degrees) (Analysis 1.7). The normal curvature at the cervical spine is lordotic: Kwon 2007 reported that 3 of 18 participants in the anterior group versus 11 of 19 in the posterior group were kyphotic across the injured segment.
1.7. Analysis.
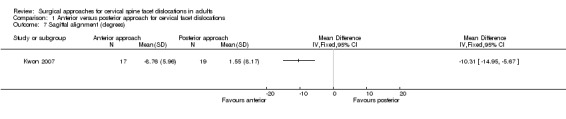
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 7 Sagittal alignment (degrees).
Complications
These data are presented in Analysis 1.8. Brodke 2003 reported one case of instrumentation failure in each group (RR 1.35, 95% CI 0.09 to 20.31) and that four participants (two in each group) developed medical complications (three pneumonia and one acute respiratory distress syndrome) (RR 1.35, 95% CI 0.21 to 8.78). There were also two deaths that were unrelated to the surgery in the anterior group in Brodke 2003.
1.8. Analysis.
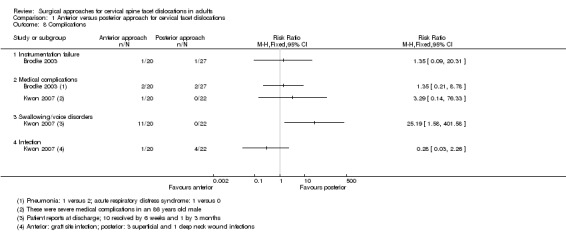
Comparison 1 Anterior versus posterior approach for cervical facet dislocations, Outcome 8 Complications.
In Kwon 2007, 11 of 20 participants treated by the anterior approach had difficulties with swallowing or voice disorders at the time of discharge; no such complications were reported in those treated by the posterior approach (RR 25.19, 95% CI 1.58 to 401.58). However, 10 of these participants had recovered by six weeks of follow‐up and the remaining participant had recovered at three months. Four of 22 participants randomised to the posterior group had neck wound infection during their hospitalisation, whereas one participant in the anterior group had infection at the site of the iliac graft harvesting (RR 0.28, 95% CI 0.03 to 2.26). An elderly participant in the anterior group presented with a variety of medical complications in the acute postoperative period (Analysis 1.8).
Economic data
Neither trial provided cost data. Kwon 2007 reported a significantly longer mean operating time for the anterior group (134 versus 103 minutes; reported P value = 0.0002) but warned that as these times include patient positioning and setup, they "may not accurately reflect skin‐to‐skin time". No participant required blood transfusion in Kwon 2007, who reported that mean blood loss was minimal. Actual length of stay data were not provided by Kwon 2007. Instead, Kwon 2007 reported a proxy, which was the time required for participants to meet the criteria for discharge from the hospital after surgery. Individual participant data and notes on complications (not swallowing/speech difficulties) from Kwon 2007 are presented in Table 3. In the 20 participants in the anterior group, the median time to achieve discharge criteria was 2.75 days; in the 22 participants in the posterior group, the time was 3.5 days (reported p value = 0.096, Mann‐Whitney U‐test).
2. Number of days to achieve discharge criteria (Kwon 2007).
| Anterior approach | Posterior approach | ||||
| Case | Days | Complications | Case | Days | Complications |
| 1 | 1 | 1 | 1.5 | ||
| 2 | 1.5 | 2 | 1.5 | ||
| 3 | 1.5 | 3 | 2 | ||
| 4 | 1.5 | 4 | 2 | ||
| 5 | 1.5 | 5 | 2 | ||
| 6 | 1.5 | 6 | 2.5 | ||
| 7 | 2 | 7 | 2.5 | ||
| 8 | 2 | 8 | 2.5 | ||
| 9 | 2.5 | 9 | 3 | ||
| 10 | 2.5 | 10 | 3 | Pseudarthrosis requiring revision | |
| 11 | 3 | 11 | 3.5 | ||
| 12 | 3 | 12 | 3.5 | ||
| 13 | 3 | Infection at bone graft site at 3 weeks | 13 | 4 | |
| 14 | 3.5 | 14 | 4 | ||
| 15 | 4 | 15 | 4 | ||
| 16 | 4 | 16 | 5 | ||
| 17 | 4 | 17 | 5 | ||
| 18 | 4.5 | 18 | 6 | (non‐union but not listed as a complication) | |
| 19 | 4.5 | 19 | 17 | Wound infection, 2 weeks of oral antibiotics | |
| 20 | 24 | Severe medical complications postoperatively | 20 | 18 | Wound infection, 2 weeks of oral antibiotics |
| 21 | 28 | Wound infection, 3 weeks of oral antibiotics | |||
| 22 | 42 | MSRA wound infection, 6 weeks of intravenous antibiotics + surgical debridement |
|||
MSRA = methicillin‐resistant Staphylococcus aureus
Discussion
Summary of main results
We included two RCTs in this review, involving a total of 94 participants but reporting on a maximum of 84 participants. Follow‐up was approximately one year. Both studies compared anterior and posterior surgical approaches for the stabilisation of a cervical spine facet dislocation. The trials included different and heterogeneous populations: Brodke 2003 included only people with spinal cord injury whereas Kwon 2007 excluded people with spinal cord injury (Kwon 2007). We were able to pool data for one outcome only: non‐union. We judged the quality of the evidence to be very low for all outcomes.
There were no significant differences between groups regarding final post‐surgical neurological status in either trial. Brodke 2003 used non‐validated outcome measure instruments, whereas Kwon 2007 used one validated score. Even though participants with SCIs were excluded in Kwon 2007, the study included 10 participants with single‐level radiculopathy associated with partial motor deficit who fully recovered at follow‐up. Considering that reduction was performed during surgery, prior to stabilisation, these participants were at risk of spinal cord or nerve root injury that could lead to neurological deterioration. However, none occurred, as was demonstrated by the lack of neurological deterioration at one year of follow‐up.
In Kwon 2007, only 33 participants completed functional aspects and quality of life questionnaires at final follow‐up, and again there were no between‐group differences between the anterior and posterior groups. No differences regarding long‐term pain and number of days to achieve specific discharge criteria were found in this study. Pain was evaluated on the first and second postoperative days, and results demonstrated a borderline statistical significance favouring the anterior approach only on day two. Lower postoperative pain with the anterior approach than with the posterior approach is plausible since the stripping of the superficial and deep muscles, necessary for exposure of the spine in the posterior approach, is likely to increase pain at the access site after surgery.
Although heterogeneous in nature, pooled data from the two studies showed no significant differences related to non‐fusion (two participants in each group) between the anterior and posterior approaches. Brodke 2003 reported no differences in changes in alignment between the two approaches. Conversely, Kwon 2007 found better sagittal alignment after one year of follow‐up in the group treated using the anterior approach.
There was insufficient evidence from the two studies to indicate between‐group differences in medical adverse events, rates of instrumentation failure and infection. In Kwon 2007, there were minor complications related to the surgical access in the anterior approach group amounting to voice and swallowing disorders in 11 participants; however, all had recovered by three months.
Overall completeness and applicability of evidence
Outcome data were available for a maximum of 84 participants with cervical spine facet dislocations. Moreover, the populations of the two trials differed in clinically important ways, the main differences being that Brodke 2003 allowed the inclusion of participants with SCIs and a variety of skeletal injuries (including those with burst fractures) as well as facet dislocations, whereas Kwon 2007 included only participants with unilateral facet fractures or dislocations but without SCIs. (Ideally, trials comparing approaches for the surgical management of facet dislocations should analyse outcomes for homogeneous populations that can be divided into different subgroups: unilateral and bilateral dislocations, and total and partial neurological deficits.)
The measurement of outcomes differed in the two trials. Final post‐surgical neurological status was evaluated through ad‐hoc conversion of Frankel scores into a non‐validated numerical scale in Brodke 2003. In contrast, Kwon 2007 assessed neurological function using the validated NASS neurologic score.
Notably, various types of instrumentation with different biomechanical qualities were used in the posterior group in Kwon 2007. In current practice, lateral mass and pedicular screws have generally replaced interspinous and oblique wiring techniques for posterior fixation of the cervical spine; a small number of articles have been published reporting such fixation methods in recent years.
Quality of the evidence
We downgraded the evidence for all outcomes two levels due to major limitations in study design and implementation. This reflects our finding that both studies were at very high risk of bias, including risk of performance bias from lack of blinding. Additionally, we considered Brodke 2003 to be at high risk from: selection bias, because it used an inappropriate method of random sequence generation that in turn precluded allocation concealment; detection bias from lack of blinding of outcome assessments; and other bias, in particular between‐group imbalances in fracture type and extent of cord injury. We judged Kwon 2007 to be at high risk of attrition bias and at unclear risk of selection and detection biases.
We further downgraded the evidence for imprecision, given that both trials had small sample sizes. Thus, overall, we judged the evidence to be of very low quality, which means that we are very uncertain about the estimate.
Potential biases in the review process
In this systematic review we tried to follow the pre‐established criteria and methods included in the published protocol (Del Curto 2009). However, findings in one included study led us to change our primary outcome, as surgery took place several days after reduction (Brodke 2003). Hence, the immediate change in neurological status would be the result of anatomical changes in the spinal canal caused by reduction rather than stabilisation.
We developed a search strategy designed to capture the largest possible number of relevant studies and performed the search in May 2014. We also searched the reference lists of relevant articles, conference proceedings and ongoing clinical trials. Despite efforts to make our strategy more sensitive, the possibility that we have missed potentially eligible studies should not be ruled out. We were unsuccessful in our attempts to obtain further data and information from the authors of both studies.
Agreements and disagreements with other studies or reviews
In a narrative review that drew on evidence from experimental biomechanical studies in cadavers and retrospective studies as well as RCTs, Dvorak 2007 proposed an algorithm to guide the choice of surgical approach for subaxial cervical spine injuries, which included those covered in our review. Dvorak 2007 considered that anterior and posterior approaches to fixation were both viable treatment options for the majority of unilateral or bilateral facet fracture dislocations and pointed out, as we have, the advantages and disadvantages of the two approaches. While noting the difficulties with swallowing and voice disorders associated with the anterior approach, Dvorak 2007 observed that the long‐term clinical significance of segmental kyphosis found more often with the posterior approach "remains to be seen".
Authors' conclusions
Implications for practice.
The very limited and poor quality evidence available on this topic comes from two trials that compared anterior with posterior approaches for the surgical treatment of adults with acute cervical spine facet dislocations. The very low quality evidence available is indicative of little difference in long‐term neurological status, pain or patient‐reported quality of life between the two approaches. There was insufficient evidence available to indicate between‐group differences in medical adverse events, rates of instrumentation failure and infection. Although one trial reported complications relating to voice and swallowing associated with the anterior approach, these resolved and there was no long‐term impairment. The same trial found better alignment (more in keeping with normal curvature) of the cervical spine in the anterior group; however, the long‐term clinical consequences of the poorer alignment obtained in the posterior group is uncertain. Additionally, the second trial did not report superior radiological results for either approach. Given the insufficiency of the available evidence to inform practice, decisions on the best approach for individual patients should be based primarily on other factors such as the surgeon's experience and patient preference.
Implications for research.
Given that changes in neurological status represent the key outcome for subaxial cervical spine facet dislocations, and that differences between surgical approaches might appear with the study of larger populations, there is a need for high‐quality multicentre randomised controlled trials to determine the safest and most effective method of reduction and surgical approach for such injuries. It is crucial that such trials also collect patient‐reported quality of life and adverse event data.
We suggest that the priority comparisons are anterior versus posterior approaches for reduction and fixation in individuals with no or varying degrees of spinal cord injury, as well as closed reduction and open fixation versus open reduction and fixation in those with spinal cord injury. Given the inevitable heterogeneity in the trial population, stratification by key patient characteristics, such as bilateral versus unilateral facet dislocation and no versus partial versus total initial neurological deficit will facilitate subgroup analyses and better inform practice.
Acknowledgements
We would like to acknowledge the editors (Xavier Griffin, Helen Handoll, Vicki Livingstone and Janet Wale) of the Cochrane Bone, Joint and Muscle Trauma Review Group and external referees (Liming Cheng and Alastair Gibson) for valuable comments during the peer‐review of the protocol and review. We also would like to thank Lindsey Elstub and Laura MacDonald for their support, and Joanne Elliott and Catherine Deering for their assistance in the development of the search strategies and providing search results.
We are grateful to Regis Bruni Andriolo for his contribution to the development of the protocol.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley Online Library)
#1 MeSH descriptor: [Spine] this term only (600) #2 MeSH descriptor: [Spinal Injuries] this term only (87) #3 #1 or #2 (678) #4 MeSH descriptor: [Fractures, Bone] this term only (1188) #5 MeSH descriptor: [Fracture Healing] this term only (401) #6 MeSH descriptor: [Dislocations] this term only (222) #7 MeSH descriptor: [Fracture Fixation] this term only (340) #8 MeSH descriptor: [Bone Plates] this term only (360) #9 (#4 or #5 or #6 or #7 or #8) (2174) #10 #3 or #9 (2797) #11 (spine or spinal or facet or vertebra* or zygapophyseal):ti (6716) #12 (fractur* or injur* or dislocat* or osteosnythesis or osteosyntheses or fixation):ti (12933) #13 #11 and #12 (1394) #14 (#10 or #13) (4083) #15 MeSH descriptor: [Cervical Vertebrae] this term only (740) #16 (cervical):ti (4593) #17 (#15 or #16) (4764) #18 (#14 and #17) (169)
MEDLINE (Ovid Online)
1 *Spine/su or *Spinal Injuries/su (3235) 2 *Fractures, Bone/ or *Fracture Healing/ or *Dislocations/ or *Fracture Fixation, Internal/ or *Bone Plates/ (61637) 3 1 and 2 (339) 4 (spine or spinal or facet or vertebra* or zygapophyseal).ti. (148703) 5 (fracture* or injur* or dislocat* or osteosynthesis or osteosyntheses or fixation*).ti. (344404) 6 4 and 5 (28455) 7 3 or 6 (28581) 8 *Cervical vertebra/ (18094) 9 cervical.m_titl. (75346) 10 8 or 9 (79888) 11 7 and 10 (4035) 12 Randomized controlled trial.pt. (372786) 13 Controlled clinical trial.pt. (88303) 14 randomized.ab. (292619) 15 placebo.ab. (153603) 16 Clinical Trials as Topic.sh. (169745) 17 randomly.ab. (211955) 8 trial.ti. (125876) 19 12 or 13 or 14 or 15 or 16 or 17 or 18 (900715) 20 exp Animals/ not Humans.sh. (3934711) 21 19 not 20 (831165) 22 11 and 21 (75)
EMBASE (Ovid Online)
1 Spine/su or vertebra/su or Vertebra, Body/ or Spine injury/su or Spine Surgery/ (22805) 2 Fracture/su or Fracture Dislocation/su or Fracture Fixation/su or Fracture Healing/su or Dislocation/su or Joint Dislocattion/su or Vertebra Dislocation/su (12197) 3 1 and 2 (452) 4 (spine or spinal or facet or vertebra* or zygapophyseal).m_titl. (161974) 5 (fracture* or injur* or dislocat* or osteosynthes#s or fixation).m_titl. (379331) 6 4 and 5 (33105) 7 3 or 6 (33324) 8 Cervical Spine/su or Cervical Spine Injury/su or Cervical Spine Fracture/su or Cervical Spine Dislocation/su (3226) 9 cervical.ti. (85223) 10 8 or 9 (86266) 11 7 and 10 (4016) 12 exp Randomized Controlled trial/ (340479) 13 exp Double Blind Procedure/ (112848) 14 exp Single Blind Procedure/ (18159) 15 exp Crossover Procedure/ (38658) 16 Controlled Study/ (4300288) 17 or/12‐16 (4374855) 18 ((clinical or controlled or comparative or placebo or prospective* or randomi#ed) adj3 (trial or study)).tw. (732540) 19 (random* adj7 (allocat* or allot* or assign* or basis* or divid* or order*)).tw. (181019) 20 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).tw. (157521) 21 (cross?over* or (cross adj1 over*)).tw. (67921) 22 ((allocat* or allot* or assign* or divid*) adj3 (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)).tw. (235837) 23 or/18‐22 (1096300) 24 or/17,23 (4932124) 25 limit 24 to human (2994582) 26 11 and 25 (578)
LILACS (Bireme)
Mh "Spinal Fractures" or ((Mh "Spine" or Mh "Spinal Injuries") and (Mh "Fractures, Bone" or Mh "Fracture Fixation" or Mh "Fracture Fixation, Intramedullary" or Mh "Fracture Healing" or Mh "Osteosynthesis, Fracture" or Mh "Dislocations")) OR (Tw spine or Tw spinal or Tw facet or Tw vertebra$ or Tw zygapophyseal) AND (Tw fracture$ or Tw injur$ or Tw dislocat$ or Tw osteosynthesis or Tw osteosyntheses or Tw fixation) [Words] and (Mh "Cervical Vertebrae" or Tw cervical) [Words] and ((Pt Randomized Controlled Trial OR Pt Controlled Clinical Trial OR Mh Randomized Controlled Trials OR Mh Random Allocation OR Mh Double‐Blind Method OR Mh Single‐Blind Method OR Pt Multicenter Study) OR ((tw ensaio or tw ensayo or tw trial) and (tw azar or tw acaso or tw placebo or tw control$ or tw aleat$ or tw random$ or (tw duplo and tw cego) or (tw doble and tw ciego) or (tw double and tw blind)) and tw clinic$)) AND NOT ((Ct Animals OR MH Animals OR Ct Rabbits OR Ct Mice OR Mh Rats OR Mh Primates OR Mh Dogs OR Mh Rabbits OR Mh Swine) AND NOT (Ct Human AND Ct Animals)) [Words]
Total number of references: 5
Appendix 2. Types of outcome measures listed in the protocol
Primary outcomes
Immediate post‐surgical neurological status (recovery or deterioration)
Secondary outcomes
Dislocation reduction or realignment, or both
Bone fusion
Pain
Functional aspects (e.g. number of patients who returned to former occupation) and health‐related quality of life (e.g. 36‐item Short‐Form Survey)
Surgical complications with need for another major operation: pseudarthrosis, infection and implant failure or loss of fixation
Blood loss
Data and analyses
Comparison 1. Anterior versus posterior approach for cervical facet dislocations.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Final post‐surgical neurological status | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Neurological scores ‐ NASS (0 to 100: best outcome) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Functional aspects and quality of life ‐ SF‐36 | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Physical scores (0 to 100: best outcome) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Mental scores (0 to 100: best outcome) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain at final follow‐up (6+ months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Pain postoperative | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Pain day 1 | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Pain day 2 | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pain scores ‐ NASS (0 to 100: no pain) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Non fusion at follow‐up | 2 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.04, 34.91] |
| 7 Sagittal alignment (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Instrumentation failure | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Medical complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Swallowing/voice disorders | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Brodke 2003.
| Methods | Method of randomisation: based on the day of admission Assessor blinding: unclear, but probably not Loss to follow‐up or excluded from analysis:
|
|
| Participants | Country: USA Period of study recruitment: 01/01/1991 to 31/12/1993 Total number: 52 participants
Age (of 47 followed up)
Gender
|
|
| Interventions | Immediate reduction in the Emergency Department. Surgical stabilisation a few days later. 1. Anterior procedure: discectomy or corpectomy + autologous tricortical iliac crest graft harvested for fusion + fixation with an anterior cervical locking plate 2. Posterior procedure: posterior fusion with iliac crest cancellous autograft + fixation with lateral mass screws and plates Postoperative care: Minerva braces or Miami J collars for 8 to 10 weeks. Mobilisation as soon as tolerated and transferred for spinal cord rehabilitation as the patient's other medical conditions allowed |
|
| Outcomes | Length of follow‐up: minimum six months (anterior: mean 17 months; posterior: mean 14 months) Neurological outcomes: ASIA (American Spinal Injury Association) motor score and Frankel score Radiographical outcomes: fusion and sagittal alignment Clinical outcomes: postoperative pain Complications |
|
| Notes | The authors of the study did not respond to our questions about missing information on trial methodology The population of the study included the following types of injuries:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation was based on the day of admission |
| Allocation concealment (selection bias) | High risk | Since the allocation sequence was deemed inadequate, it could not be properly concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding is not feasible for participants nor treatment providers in this sort of trial |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding of outcome assessors was not mentioned. There was reference to independent review by the lead author |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All participants lost to follow‐up or excluded were reported. However, their data were not presented. Five participants were not included for final pain analysis:
|
| Selective reporting (reporting bias) | Unclear risk | All the outcomes described in the methods section were presented in the results. However, the scoring system for neurological status was not specified, not fully reported and is inappropriate (it was not used in this review) |
| Other bias | High risk |
|
Kwon 2007.
| Methods | Method of randomisation: block randomisation (no other information) Assessor blinding: no blinding but independent assessment of clinical and radiological outcome measures Loss to follow‐up:
|
|
| Participants | Country: Canada, at the Vancouver General Hospital, Vancouver, British Columbia Period of study recruitment: between 1998 and 2003 Total number: 42 participants
Age
Gender
|
|
| Interventions | Reduction was performed during the surgical procedure 1. Anterior procedure: anterior cervical discectomy + tricortical iliac crest autograft + plate fixation 2. Posterior procedure: lateral mass screw‐plate fixation and/or interspinous and/or oblique wiring Postoperative care: self‐controlled analgesia device provided to the participants; all mobilised with cervical orthoses (Guildford, Inc.) and were trained by occupational therapists in brace application. Standard physiotherapy regimen. Outpatient physiotherapy was not routine. |
|
| Outcomes | Length of follow‐up: 12 months Pain: 1st and 2nd postoperative days Clinical and radiographical outcomes: 6 weeks and 3, 6 and 12 months postoperatively Primary outcome
Secondary outcomes
|
|
| Notes | The study population included the following types of unilateral facet injuries:
Ten participants had single nerve root injury: 6 (anterior) versus 4 (posterior) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: "The patients were randomised according to a block randomisation procedure" |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding for participants or treatment providers |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No blinding. "Independent research assistants not involved in the patients’ clinical care administered all clinical outcome measures". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All participants lost to follow‐up or excluded were reported. However, their data were not presented. For patient‐reported outcomes:
For radiographic outcomes:
|
| Selective reporting (reporting bias) | Low risk | All the outcomes described in the methods section were presented in the results |
| Other bias | Unclear risk | Different types of instrumentation were used in both groups, especially in the posterior fixation group, in which lateral mass screws with plates and/or interspinous and/or oblique wiring were deployed. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Kandziora 2005 | Not a randomised study |
Differences between protocol and review
1. We clarified in the title that the review was aimed at adults with these injuries. We clarified in the Objectives and Types of participants that the review was considering acute injuries.
2. We adjusted the Types of outcome measures (seeAppendix 2 for those listed in the protocol) after a reappraisal prompted by an assessment of the appropriateness of the outcomes reported by the included studies and feedback at editorial review.
3. In some medical institutions the general approach to cervical facet dislocations associated with SCIs is to perform closed reduction followed by surgical stabilisation after some days, as seen in Brodke 2003. In this way, we considered that immediate neurological improvement or worsening might be affected more directly by reduction than by the surgical approach itself. So we decided to change our primary outcome from immediate post‐surgical neurological status to final post‐surgical neurological status.
4. We did not assess the risk of bias associated with a) blinding and b) completeness of outcomes separately for patient‐reported and objective outcomes as planned, but considered risk of bias for these two domains for all outcomes together.
Contributions of authors
Conceiving the review: DDC and EBP Co‐ordinating the review: DDC and DEM Writing the protocol: DDC, DEM and RBA (Regis Bruni Andriolo) Reading and checking protocol before submission: DDC and EBP Data collection for the review: DDC and MJT Designing search strategies: DDC and MJT Undertaking searches: DDC, DEM and JCB Screening search results: DDC, DEM and JCB Organising retrieval of papers: DDC, MJT and JCB Screening retrieved papers against eligibility criteria: DDC, MJT and JCB Appraising quality of papers: DDC, DEM and JCB Extracting data from papers: DDC, DEM and JCB Writing to authors of papers for additional information: DDC and MJT Providing additional data about papers: DDC and MJT Obtaining and screening data on unpublished studies: DDC and DEM Data management for the review: DDC, MJT and DEM Entering data into RevMan: DDC and MJT Analysis of data: DDC, MJT and EBP Interpretation of data: DDC, MJT and EBP Writing the review: DDC, EBP and JCB Providing general advice on the review: DDC, MJT, DEM, EBP and JCB
Sources of support
Internal sources
Universidade Federal de São Paulo, Brazil.
External sources
No sources of support supplied
Declarations of interest
None known.
New
References
References to studies included in this review
Brodke 2003 {published data only}
- Brodke DS, Anderson PA, Newell DW, Grady MS, Chapman JR. Comparison of anterior and posterior approaches in cervical spinal cord injuries. Journal of Spinal Disorders & Techniques 2003;16(3):229‐35. [PUBMED: 12792335] [DOI] [PubMed] [Google Scholar]
- Brodke DS, Chapman JR, Anderson PA, Newell DW, Grady MS, Harthan B. Anterior vs. posterior stabilization of cervical spine fractures in spinal cord injured patients. Proceedings of the Orthopaedic Trauma Association Annual Meeting; 1996 Sept 27‐29; Boston. www.hwbf.org/ota/am/ota96/otapa/OTA96506.htm. 1996 (accessed 8 May 2006).
Kwon 2007 {published data only}
- Kwon BK, Fisher CG, Boyd MC, Cobb J, Jebson H, Noonan V, et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. Journal of Neurosurgery Spine 2007;7(1):1‐12. [PUBMED: 17633481] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Kandziora 2005 {published data only}
- Kandziora F, Pflugmacher R, Scholz M, Schnake K, Putzier M, Khodadadyan‐Klostermann C, et al. Treatment of traumatic cervical spine instability with interbody fusion cages: a prospective controlled study with a 2‐year follow‐up. Injury 2005;36 Suppl 2:B27‐35. [PUBMED: 15993115] [DOI] [PubMed] [Google Scholar]
Additional references
Abumi 2000
- Abumi K, Shono Y, Kotani Y, Kaneda K. Indirect posterior reduction and fusion of the traumatic herniated disc by using a cervical pedicle screw system. Journal of Neurosurgery 2000;92(1 Suppl):30‐7. [PUBMED: 10616055] [DOI] [PubMed] [Google Scholar]
Allen 1982
- Allen BL Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine 1982;7(1):1‐27. [PUBMED: 7071658] [DOI] [PubMed] [Google Scholar]
Allred 2001
- Allred CD, Sledge JB. Irreducible dislocations of the cervical spine with a prolapsed disc: preliminary results from a treatment technique. Spine 2001;26(17):1927‐30. [PUBMED: 11588707] [DOI] [PubMed] [Google Scholar]
ASIA 1992
- American Spinal Injury Association. International Standards for Neurological and Functional Classification of Spinal Cord Injury (Revised 1992). Chicago, IL: American Spinal Injury Association, 1992. [Google Scholar]
Bellabarba 2006
- Bellabarba C, Anderson PA. Injuries of the lower cervical spine. In: Herkowitz HN, Garfin SR, Eismont FJ, Bell GR, Balderston RA editor(s). Rothman‐Simeone The Spine. 5th Edition. Philadelphia: Elsevier Press, 2006:1100‐31. [Google Scholar]
Burke 2001
- Burke DA, Linden RD, Zhang YP, Maiste AC, Shields CB. Incidence rates and populations at risk for spinal cord injury:a regional study. Spinal Cord 2001;39(5):274‐8. [PUBMED: 11438844] [DOI] [PubMed] [Google Scholar]
Burney 1993
- Burney RE, Maio RF, Maynard F, Karunas R. Incidence, characteristics, and outcome of spinal cord injury at trauma centers in North America. Archives of Surgery 1993;128(5):596‐9. [PUBMED: 8489395] [DOI] [PubMed] [Google Scholar]
Castro 1999
- Castro AA, Clark OA, Atallah AN. Optimal search strategy for clinical trials in the Latin American and Caribbean Health Science Literature database (LILACS database). Sao Paulo Medical Journal 1999;117(3):138‐9. [DOI] [PubMed] [Google Scholar]
De Lure 2003
- Lure F, Scimeca GB, Palmisani M, Donati U, Gasbarrini A, Bandiera S, et al. Fractures and dislocations of the lower cervical spine: surgical treatment. A review of 83 cases. Chirurgia Degli Organi di Movimento 2003;88(4):397‐410. [PUBMED: 15259556] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
DeVivo 1997
- DeVivo MJ. Causes and costs of spinal cord injury in the United States. Spinal Cord 1997;35(12):809‐13. [PUBMED: 9429259] [DOI] [PubMed] [Google Scholar]
Doran 1993
- Doran SE, Papadopoulos SM, Ducker TB, Lillehei KO. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. Journal of Neurosurgery 1993;79(3):341‐5. [PUBMED: 8360729] [DOI] [PubMed] [Google Scholar]
Dvorak 2007
- Dvorak MF, Fisher CG, Fehlings MG, Rampersaud YR, Oner FC, Aarabi B, et al. The surgical approach to subaxial cervical spine injuries: an evidence‐based algorithm based on the SLIC classification system. Spine 2007;32(23):2620‐9. [PUBMED: 17978665] [DOI] [PubMed] [Google Scholar]
Eismont 1991
- Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of the cervical facets. Case report. Journal of Bone & Joint Surgery ‐ American Volume 1991;73(10):1555‐60. [PUBMED: 1748703] [PubMed] [Google Scholar]
Fisher 2006
- Fisher CG, Noonan VK, Dvorak MF. Changing face of spine trauma care in North America. Spine 2006;31(11 Suppl):S2‐8. [PUBMED: 16685231] [DOI] [PubMed] [Google Scholar]
Frankel 1969
- Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries in the spine with paraplegia and tetraplegia. Paraplegia 1969;7(3):179–92. [DOI] [PubMed] [Google Scholar]
Harrington 1991
- Harrington JF, Likavec MJ, Smith AS. Disc herniation in cervical fracture subluxation. Neurosurgery 1991;29(3):374‐9. [PUBMED: 1922704] [DOI] [PubMed] [Google Scholar]
Harrop 2001
- Harrop JS, Sharan AD, Vaccaro AR, Przybylski GJ. The cause of neurologic deterioration after acute cervical spinal cord injury. Spine 2001;26(4):340‐6. [PUBMED: 11224879] [DOI] [PubMed] [Google Scholar]
Hart 2002
- Hart RA, Vaccaro AR, Nachwalter RS. Cervical facet dislocation: When is magnetic resonance imaging indicated?. Spine 2002;27(1):116‐7. [PUBMED: 11805648] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [PUBMED: 12958120] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kahn 1998
- Kahn A, Leggon R, Lindsey RW. Cervical facet dislocation: management following delayed diagnosis. Orthopedics 1998;21(10):1089‐91. [PUBMED: 9801232] [DOI] [PubMed] [Google Scholar]
Kraus 1975
- Kraus JF, Franti CE, Riggins RS, Richards D, Borhani NO. Incidence of traumatic spinal cord lesions. Journal of Chronic Diseases 1975;28(9):471‐92. [PUBMED: 1176577] [DOI] [PubMed] [Google Scholar]
Lasfargues 1995
- Lasfargues JE, Custis D, Morrone F, Carswell J, Nguyen T. A model for estimating spinal cord injury prevalence in the United States. Paraplegia 1995;33(2):62‐8. [PUBMED: 7753569] [DOI] [PubMed] [Google Scholar]
Lee 1994
- Lee AS, MacLean JC, Newton DA. Rapid traction for reduction of cervical spine dislocations. Journal of Bone & Joint Surgery ‐ British Volume 1994;76(3):352‐6. [PUBMED: 8175833] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Maiman 1986
- Maiman DJ, Barolat G, Larson SJ. Management of bilateral locked facets of the cervical spine. Neurosurgery 1986;18(5):542‐7. [PUBMED: 3714001] [DOI] [PubMed] [Google Scholar]
Nassr 2008
- Nassr A, Lee JY, Dvorak MF, Harrop JS, Dailey AT, Shaffrey CI, et al. Variations in surgical treatment of cervical facet dislocations. Spine 2008;33(7):E188‐93. [PUBMED: 18379387] [DOI] [PubMed] [Google Scholar]
Nobunaga 1999
- Nobunaga AI, Go BK, Karunas RB. Recent demographic and injury trends in people served by the Model Spinal Cord Injury Care Systems. Archives of Physical Medicine and Rehabilitation 1999;80(11):1372‐82. [PUBMED: 10569430] [DOI] [PubMed] [Google Scholar]
Ordonez 2000
- Ordonez BJ, Benzel EC, Naderi S, Weller SJ. Cervical facet dislocation: techniques for ventral reduction and stabilization. Journal of Neurosurgery 2000;92(1 Suppl):18‐23. [PUBMED: 10616053] [DOI] [PubMed] [Google Scholar]
Reindl 2006
- Reindl R, Ouellet J, Harvey EJ, Berry G, Arlet V. Anterior reduction for cervical spine dislocation. Spine 2006;31(6):648‐52. [PUBMED: 16540868] [DOI] [PubMed] [Google Scholar]
Robertson 1992
- Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. Journal of Bone & Joint Surgery ‐ British Volume 1992;74(2):224‐7. [PUBMED: 1544957] [DOI] [PubMed] [Google Scholar]
Star 1990
- Star AM, Jones AA, Cotler JM, Balderston RA, Sinha R. Immediate closed reduction of cervical spine dislocations using traction. Spine 1990;15(10):1068‐72. [PUBMED: 2263974] [DOI] [PubMed] [Google Scholar]
Surkin 2000
- Surkin J, Gilbert BJ, Harkey HL 3rd, Sniezek J, Currier M. Spinal cord injury in Mississippi. Findings and evaluation, 1992‐1994. Spine 2000;25(6):716‐21. [PUBMED: 10752104] [DOI] [PubMed] [Google Scholar]
Tator 1995
- Tator CH, Duncan EG, Edmonds VE, Lapczak LI, Andrews DF. Neurological recovery, mortality and length of stay after acute spinal cord injury associated with changes in management. Paraplegia 1995;33(5):254‐62. [PUBMED: 7630650] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Del Curto 2009
- Curto D, Martins DE, Andriolo RB, Puertas EB. Surgical approaches for cervical spine facet dislocations. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD008129] [DOI] [PMC free article] [PubMed] [Google Scholar]


