Abstract
Background
Cognitive impairment is a frequent consequence of stroke and can impact on a person's ability to perform everyday activities. There are a number of different intervention strategies that occupational therapists may use when working with people who have cognitive impairment post‐stroke.
Objectives
To determine whether occupational therapy improves functional performance of basic activities of daily living (ADL) and specific cognitive abilities in people who have cognitive impairment following a stroke.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched May 2009), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library Issue 1, 2009), MEDLINE (1966 to April 2009), EMBASE (1980 to April 2009), CINAHL (1982 to April 2009), PsycINFO (1840 to April 2009), PsycBITE, OTseeker and Dissertation Abstracts (the latest three were searched up to April 2009). In an effort to identify further published, unpublished, and ongoing trials, we also tracked relevant references through the cited reference search in Science Citation Index (SCI) and Social Science Citation Index (SSCI), reviewed the reference lists of relevant studies and reviews, handsearched relevant occupational therapy journals, and contacted key researchers in the area.
Selection criteria
Randomised and quasi‐randomised controlled trials that evaluated an intervention focused on providing cognitive retraining to adults with clinically defined stroke and confirmed cognitive impairment. The intervention needed either to be provided by an occupational therapist or given under the supervision of an occupational therapist.
Data collection and analysis
Two review authors independently examined the abstracts that might meet the inclusion criteria, assessed the quality and extracted data. We have presented results using mean differences.
Main results
We included one trial with 33 participants in this review. We found no difference between groups for the two relevant outcomes that were measured: improvement in time judgement skills and improvement in basic ADLs on the Barthel Index.
Authors' conclusions
The effectiveness of occupational therapy for cognitive impairment post‐stroke remains unclear. The potential benefits of cognitive retraining delivered as part of occupational therapy on improving basic daily activity function or specific cognitive abilities, or both, of people who have had a stroke cannot be supported or refuted by the evidence included in this review. More research is required.
Keywords: Adult, Humans, Activities of Daily Living, Cognition Disorders, Cognition Disorders/etiology, Cognition Disorders/rehabilitation, Occupational Therapy, Occupational Therapy/methods, Randomized Controlled Trials as Topic, Stroke, Stroke/complications, Stroke Rehabilitation
Occupational therapy for cognitive impairment in stroke patients
Cognitive impairment is common after stroke and can affect a person's ability to do everyday activities such as dressing, feeding, and showering. Occupational therapy aims to help people reach their maximum level of functional independence. This review of one trial including 33 participants found that there is currently insufficient evidence to establish the effectiveness of occupational therapy for cognitive impairment in people who have had a stroke. More well‐designed clinical trials which test occupational therapy interventions for cognitive impairment post‐stroke are needed.
Background
Stroke is a leading cause of chronic disability in many developed countries in the world (CDCP 2003; Thrift 2000). A frequent consequence of stroke is impairment of cognition (Patel 2003; Tatemichi 1994). Cognition encompasses processes that enable people to 'think', including the ability to concentrate, remember and learn, and may also include metaprocesses such as executive functioning (Unsworth 1999). There is some disagreement regarding the classification of specific cognitive domains and impairments. Some authors include visual‐spatial perception and apraxia as cognitive impairments (Cicerone 2005). However, many texts also classify visual‐spatial perception and apraxia separately to cognitive impairments. For the purpose of this review cognition impairment is considered to encompass impairments in attention and concentration, memory, orientation, and/or executive functions in accordance with The National Stroke Foundation of Australia's Clinical Guidelines for Stroke Rehabilitation and Recovery (National Stroke Foundation 2005). Patel et al found that, in the three‐year period after the onset of their first stroke, up to 39% of patients had cognitive impairment (Patel 2003). A significant relationship has been found between cognitive abilities and functional performance (Abreu 1987; Hanson 1997; Poole 1991). Thus, cognitive impairment can reduce the independence of people who have had a stroke when performing basic activities of daily living (such as eating, dressing, and toileting) and instrumental activities of daily living (such as housework and social interactions) (Hochstenbach 2000; Patel 2003; Zinn 2004). As a result, people with cognitive impairment following stroke often require ongoing care and support, which can place a strain on caregivers and society (Blake 2002; Doyle 2002). Therefore, it is important for researchers and clinicians to identify effective interventions to treat cognitive impairment following stroke.
Occupational therapy plays a unique and important role in a multidisciplinary approach to the treatment of cognitive impairment (Zoltan 2007). Occupational therapists assess and treat cognitive deficits to assist patients to reach their maximum level of functional independence and fulfil desired and required life roles after stroke (Legg 2006; Poole 1991). The two general techniques used by occupational therapists to treat cognitive impairment are remedial and compensatory approaches (Blundon 2000; Poole 1991; Radomski 1994). Based on the concept of the plasticity of the human brain and its ability to reorganise after being damaged, the remedial approach aims to promote patients' function by retraining deficits in specific cognitive domains (e.g. attention, memory and organisation). This approach assumes that retrained skills will transfer to functional performance more broadly than the immediate task including such activities of daily living as managing finances or planning household tasks. The compensatory approach utilises patients' residual strengths to compensate for deficits and aims to restore their function by teaching and assisting them and their families to develop strategies to overcome performance deficits. Debate exists around the validity of the assumptions and the effectiveness of these approaches. It has been argued that the skills acquired through repetitive drill‐like exercises using a remedial approach may not be readily transferred to daily living activities (Cobble 1991). Furthermore, direct training in specific functional activities as part of the compensatory approach may not necessarily generalise to improved performance in everyday activities in home, work or school, and in leisure contexts (Hanson 1997). A comprehensive systematic review may help to clarify these debates and examine the effectiveness of occupational therapy in treating cognitive impairment.
To our knowledge, there is no systematic review that has specifically examined the effectiveness of interventions delivered by occupational therapists in treating cognitive impairment in people with stroke. A review by Cicerone et al addressed the issue of the effectiveness of cognitive rehabilitation in stroke patients; however, it is not specific to occupational therapy (Cicerone 2000; Cicerone 2005). Two reviews have examined the effectiveness of occupational therapy with stroke patients in general, but did not focus on the treatment of cognitive impairment (Ma 2002; Steultjens 2003). As occupational therapy is considered to be an important part of the multidisciplinary management of stroke, and treatment of cognitive impairment is a common focus of this intervention, it is important to review the effectiveness of occupational therapy in assisting people with cognitive impairment after stroke to improve their functional independence.
Objectives
To determine the effectiveness of occupational therapy for people with cognitive impairment after a stroke. In particular, to determine whether occupational therapy improves functional performance of basic and instrumental ADL and cognitive abilities post‐stroke.
Methods
Criteria for considering studies for this review
Types of studies
We restricted the review to randomised controlled trials (RCTs), clinical trials where participants were quasi‐randomly assigned to one of two or more treatment groups, and cross‐over trials.
Types of participants
We included trials if their participants were adults (aged 18 years or over) with a clinically defined stroke and confirmed cognitive impairment as specified in each trial. For the purpose of this review we focused on cognitive impairments including attention and concentration, memory, orientation, and/or executive functions. We excluded trials with mixed aetiology groups unless participants who had had (and only had) a stroke comprised more than 50% of the participants in the trial and separate data for the participants with stroke were available either in the published article or from the trial authors.
Types of interventions
We included all occupational therapy interventions for cognitive impairment in people with stroke. We defined occupational therapy interventions in this review as interventions carried out by an occupational therapist or under the supervision of an occupational therapist, or indexed in major international occupational therapy texts (Katz 2005; Pedretti 2001; Trombly 2002). These interventions may take either a remedial or a compensatory approach, or both. The remedial approach focuses on training specific cognitive deficits using media such as pencil and paper, computer tasks and board games. In a compensatory approach interventions may include (1) training skills for daily activities (e.g. dressing, ambulation, driving, managing a meal) and vocation using compensatory strategies; (2) advising and educating about the use of assistive devices that aid cognitive function, such as an alarm watch, a hand‐held computer, or a medication container; and (3) educating patients, families, and caregivers about strategies to overcome patients' cognitive impairment. The dynamic interactional approach (previously referred to as multicontextual) is an integrated approach, encompassing both remedial and compensatory elements to encourage generalisation of the treatment effect achieved in a clinical setting to patients' real life performance situation (Toglia 2005). We considered the dynamic interactional approach as a third type of intervention in this review, separate from remedial and compensatory approaches. For the purpose of this review we focused on cognitive impairments including attention and concentration, memory, orientation, and/or executive functions. We did not include studies that focused on apraxia or perceptual impairments without also containing elements of cognitive retraining. We also did not include trials which examined the effects of change to pharmaceutical interventions on cognitive function following stroke.
Types of outcome measures
Primary outcomes
The primary outcome measure was assessments of basic activities of daily living (ADL).
Secondary outcomes
Secondary outcome measures were assessments of instrumental ADL, community integration, resumption of life roles, and specific cognitive abilities such as attention, memory, orientation, and/or executive functions or general cognitive function.
Search methods for identification of studies
See the 'Specialized register' section in the Cochrane Stroke Group module.
We searched the Cochrane Stroke Group Trials Register, which was last searched by the Managing Editor in May 2009. In addition, using comprehensive search strategies, we searched the following electronic bibliographic databases: the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library Issue1, 2009), MEDLINE (1966 to April 2009) (Appendix 1), EMBASE (1980 to April 2009), CINAHL (1982 to April 2009), PsycINFO (1840 to April 2009), PsycBITE, OTseeker, and Dissertation Abstracts (we searched the last three up to April 2009). The search strategies included four major areas: stroke, cognitive impairment, occupational therapy interventions and trial methodology. We developed the search strategy in consultation with the Cochrane Stroke Group Trials Search Co‐ordinator and we consulted an experienced medical librarian about the search strategies for each database.
In an effort to identify further published, unpublished, and ongoing trials:
we tracked relevant references through the cited reference search in Science Citation Index (SCI) and Social Science Citation Index (SSCI);
we scanned the reference lists of identified studies and reviews;
-
we handsearched the following relevant occupational therapy journals which had not already been searched on behalf of The Cochrane Collaboration. We included supplements and conference abstracts not indexed in the above databases:
American Journal of Occupational Therapy (1947 to 1949);
Australian Occupational Therapy Journal (1963 to 1990);
Asian Journal of Occupational Therapy (2001 to 2006);
Canadian Journal of Occupational Therapy (1955 to 1965);
Hong Kong Journal of Occupational Therapy (2001 to 2006);
Indian Journal of Occupational Therapy (2001 to 2005);
Journal of Occupational Science Australia (1993 to 1994);
New Zealand Journal of Occupational Therapy (1957 to 1978, 1990 to 1995);
Occupational Therapy in Health Care (1984 to 1986);
Occupational Therapy and Rehabilitation (1938 to 1951);
South African Journal of Occupational Therapy (1959 to 1991);
we contacted authors and key researchers in the area;
we scanned the abstracts of non‐English language studies if the abstracts were available in English.
We used the search strategy for MEDLINE (Ovid) (Appendix 1) and adapted it to search the other databases.
Data collection and analysis
Study selection
One review author (CK) screened the titles of articles identified in the searches and references, eliminated irrelevant studies and obtained the abstracts of the remaining studies. Using these abstracts, two review authors (CK and TH or SB) independently completed the first phase of study selection according to the four eligibility criteria (types of studies, participants, interventions, and outcome measures). We obtained the full texts of the studies that were considered as eligible for inclusion from this process or for which eligibility was unclear. Two review authors (CK and TH or SB) independently completed the second study selection process to finally decide on each trial’s inclusion or exclusion. We resolved any disagreements by discussion based on the inclusion criteria. If we could not reach a consensus, the third review author made the decision. When it was unclear whether the intervention was delivered by an occupational therapist we contacted the study authors for clarification.
Assessment of methodological quality
Two review authors (TH and SB) independently evaluated the methodological quality of eligible trials. During this evaluation, the review authors were blinded to the source of publication and results. The four sources of potential bias in trials of intervention effectiveness that we evaluated were: selection bias, performance bias, detection bias and attrition bias. According to the definition by Juni et al (Juni 2001) selection bias refers to biased allocation of participants to comparison groups (i.e. absence of, or inadequate, allocation concealment). We assessed the methods of allocation concealment of the eligible studies according to the three categories and criteria suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008): A ‐ adequate; B ‐ unclear; and C ‐ inadequate. Performance bias refers to unequal provision of care apart from the intervention under evaluation (i.e. lack of blinding of therapists or participants, or both) (Higgins 2008). Detection bias refers to biased assessment of outcome (i.e. lack of blinding of outcome assessors) (Higgins 2008). Attrition bias refers to biased occurrence and handling of deviations from the intervention protocol (i.e. lack of analysis according to intention‐to‐treat) and loss to follow‐up (Higgins 2008). To evaluate the four types of bias in the eligible trials, we applied the eight internal validity items adapted from the PEDro scale in this review (Moseley 2002). After reviewing the trials, we assigned each of the eight items a 'yes' (present) or 'no' (absent or not reported) to indicate the methodological quality of the studies according to the criteria used to rate articles in the OTseeker database (http://www.otseeker.com/scale.htm) (Table 2).
Table 1.
Criteria for assessing the methodological quality of trials
| Criteria | Rating* |
| Selection bias | |
| (1) Participants were randomly allocated to groups (in a cross‐over study, participants were randomly allocated an order in which treatments were received) | Yes |
| (2) Allocation was concealed | No |
| (3) The groups were similar at baseline regarding the most important prognostic indicators | Yes |
| Performance bias | |
| (4) There was blinding of all participants | No |
| (5) There was blinding of all therapists who administered the therapy | No |
| Detection bias | |
| (6) There was blinding of all assessors who measured at least one key outcome | No |
| Attrition bias | |
| (7) Measures of at least one key outcome were obtained from more than 85% of the participants initially allocated to groups | Yes |
| (8) All participants for whom outcome measures were available received the treatment or control condition as allocated or, if this was not the case, data for at least one key outcome were analysed by 'intention‐to‐treat' | No |
| *Yes/No according to criteria used in the OTseeker database (http://www.otseeker.com/scale.htm#1) |
Data extraction
Two review authors (TH and SB) independently recorded the following information using a self‐developed data extraction form.
Sample characteristics such as: age, level of education, sex, first or recurrent stroke, type and severity of stroke, time since onset of stroke, type of cognitive impairment, sample size, number of drop outs.
Methodological quality: according to the eight internal validity items as described in Table 2.
Details of the interventions: type of interventions (remedial, compensatory, or dynamic interactional approach), materials used in interventions (e.g. cards, boards, paper and pencil exercises, computer games), duration and frequency of interventions and follow‐up, individual or group therapy.
Outcome measures: the outcome measures used in the trial and when they were administered.
The same two review authors independently extracted data using a data extraction form to record methodological and outcome data.
Data analysis
For continuous data, we planned to calculate two types of estimate. The measure of the treatment difference for any outcome would be the mean difference (MD) when the pooled trials use the same rating scale or test, and the standardised mean difference (SMD) (the absolute mean difference divided by the standard deviation) when they use different rating scales or tests. We planned to calculate each one, together with the corresponding 95% confidence interval (CI). For dichotomous data, we planned to compute the relative risk (RR) or odds ratio (OR) with 95% CI.
We planned to pool the results of trials to present the overall estimate of the treatment effect using a fixed‐effect model viewed to assess heterogeneity. We planned to test heterogeneity between trial results by using I2 estimates (Higgins 2003). We would consider an I2 value above 50% substantial, indicating heterogeneity between trial results. If heterogeneity was present we would carry out a sensitivity analysis to explore the reasons for this. Otherwise, we would use a random‐effects model (in which case the confidence intervals will be broader than those of a fixed‐effect model).
We planned to carry out a sensitivity analysis to evaluate the effect of trial quality by analysing separately the following categories of studies:
trials with and without adequate randomisation and concealment of treatment allocation;
trials with and without intention‐to‐treat analysis;
trials with follow‐up periods of less than six months duration, six to 12 months duration, and more than 12 months duration.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
We conducted the most current search of electronic databases in May 2009. This search yielded a total of 1639 references. We identified only one trial that met the inclusion criteria. We identified an additional trial that met the criteria but it is an ongoing trial that was due for completion at the end of 2009.
Included studies
The included study (Carter 1983) is a RCT that examined the effect of a cognitive skills remediation programme with 33 people who were receiving rehabilitation in a hospital following acute stroke. For the 16 participants in the intervention group, cognitive skills remediation training was administered on an individual basis for 30 to 40 minutes three times per week for an average of three to four weeks. The cognitive skills remediation training was based on the Thinking Skills Workbook (Carter 1980). The comparison group of 17 participants received rehabilitation as usual. The primary outcome measures were tests of visual scanning, visual‐spatial matching and time judgement from the Thinking Skills Workbook (Carter 1980). However, in this review we considered only the time judgement scores a measure of cognitive skill as this review classified visual scanning and visual‐spatial matching as perceptual skills. We extracted data about the functional outcomes from the Carter study from the second article published in 1988 (Carter 1983), which reported participants' basic ADL scores on the Barthel Index. This study met the criteria for inclusion because it measured the effect of elements of cognitive training on basic activities of daily living and on specific cognitive skills (time judgement).
Excluded studies
We excluded trials from this review if the intervention did not address cognitive impairments of people following stroke; if the trials were not RCTs; if they were conducted with mixed aetiology groups and participants with stroke were fewer than 50% of the participants or data were not separately available for participants with stroke; or the intervention in the trial was not carried out or supervised by an occupational therapist. We also excluded studies if the focus was on interventions for perceptual impairments or apraxia without also including interventions for cognitive impairments. Studies listed in the Characteristics of excluded studies table are those that appeared to be relevant and focused on cognitive retraining, but to our knowledge were not carried out by occupational therapists or did not focus on cognitive retraining.
Risk of bias in included studies
Two authors rated the methodological quality of the study independently using the PEDro scale (Maher 2003). Individual item scores can be found in Table 2.
Sequence generation
The participants in the Carter 1983 study were randomly allocated to groups but it is unclear how this was carried out.
Allocation
There was no mention within the Carter 1983 articles of allocation to group being concealed.
Blinding
Blinding of participants and therapists was not reported and is unlikely to have been achievable. A blind testing procedure was attempted, but according to the authors it was possible for the outcome assessor to be aware of the group assignment of the participants because of the physical layout of the stroke unit.
Follow‐up and exclusions
Reported outcome data for the study were available for 85% of participants for the Barthel Index outcome. The authors state that Barthel scores were not available for three participants from the control group and two participants in the treatment group but no reason for this was provided. Although data were available for 33 participants for the cognitive tests the authors only calculated cognitive test scores for the 76% of participants who had pre‐test performance below 80%; that is, scores for participants who had 80% of better pre‐test scores were not included in the calculation. The authors state this was to prevent possible ceiling effects.
Selective reporting
It is unclear whether selective reporting occurred in the Carter 1983 study. The description of the method used stated that three aspects of cognition were measured and these were each reported on. However, the cognitive skills evaluation from the Thinking Skills Workbook (Carter 1980) from which the tests were drawn for the Carter 1983 study included eight cognitive skills.
Other potential sources of bias
The Carter 1983 paper did not report use of intention‐to‐treat analysis.
Effects of interventions
Given that there was only one study included in this review, a meta‐analysis was not possible. We found no difference between groups for the two relevant outcomes that were measured: improvement in time judgement skills and improvement in basic ADLs on the Barthel Index.
Discussion
The aim of this review was to identify and evaluate the effectiveness of occupational therapy for cognitive impairment following stroke. Only one trial met the criteria for inclusion: the Carter 1983 trial, therefore data could not be pooled for further analysis or interpretation. This study tested the effect of cognitive remediation skills training compared with usual rehabilitation for people with cognitive impairments following stroke. We found no differences between groups for the cognitive skill of time judgement (Analysis 1.1) or for basic ADL measured using the Barthel Index (Analysis 1.2). It is possible that the sample size of only 33 participants may not have been large enough to detect an effect if one existed. Therefore, this study provides insufficient evidence about the effectiveness or otherwise for this intervention.
Analysis 1.1.
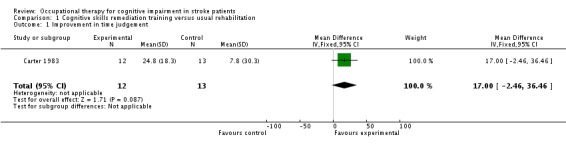
Comparison 1 Cognitive skills remediation training versus usual rehabilitation, Outcome 1 Improvement in time judgement.
Analysis 1.2.
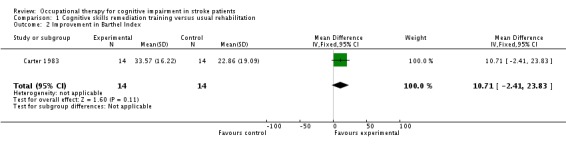
Comparison 1 Cognitive skills remediation training versus usual rehabilitation, Outcome 2 Improvement in Barthel Index.
Authors' conclusions
The effectiveness of occupational therapy for cognitive impairment post‐stroke remains unclear. The potential benefits of cognitive retraining delivered as part of an occupational therapy service on improving basic daily activity function or specific cognitive abilities, or both, of people who have had a stroke cannot be supported or refuted by evidence from the reviewed RCT.
In order to obtain reliable and valid evidence of the effect of occupational therapy for cognitive impairment post‐stroke further methodologically rigorous investigations using RCTs are needed. The included study must be viewed in the light of its small sample size. Future studies should aim to have larger numbers of participants.
Acknowledgements
None.
Appendices
Appendix 1. MEDLINE search strategy
MEDLINE (Ovid)
1. exp cerebrovascular disorders/ or brain injuries/ or brain injury, chronic/ 2. (stroke$ or cva or poststroke or post‐stroke).tw. 3. (cerebrovasc$ or cerebral vascular).tw. 4. (cerebral or cerebellar or brain$ or vertebrobasilar).tw. 5. (infarct$ or isch?emi$ or thrombo$ or emboli$ or apoplexy).tw. 6. 4 and 5 7. (cerebral or brain or subarachnoid).tw. 8. (haemorrhage or hemorrhage or haematoma or hematoma or bleed$).tw. 9. 7 and 8 10. exp hemiplegia/ or exp paresis/ 11. (hemipar$ or hemipleg$ or brain injur$).tw. 12. 1 or 2 or 3 or 6 or 9 or 10 or 11 13. cognition disorders/ or confusion/ or neurobehavioral manifestations/ or memory disorders/ 14. (agnosia or amnesia or confusion or inattention).tw. 15. cognition/ or Arousal/ or Orientation/ or Attention/ or memory/ or perception/ or mental processes/ or thinking/ or Concept Formation/ or Algorithms/ or "Recognition (Psychology)"/ or Judgment/ or Awareness/ or Problem Solving/ or "Generalization (Psychology)"/ or "Transfer (Psychology)"/ or comprehension/ or Impulsive Behavior/ or Learning/ 16. ((cogniti$ or arous$ or orientat$ or attention$ or concentrat$ or memor$ or recall or percept$ or think$ or sequenc$ or algorithm$ or judg?ment$ or awareness or problem solving or generali?ation or transfer or comprehension or learning) adj10 (disorder$ or declin$ or dysfunct$ or impair$ or deficit$ or abilit$ or problem$)).tw. 17. (dysexecutive syndrome$ or mental process$ or (concept adj5 formation) or impulsive behavio?r$ or executive function$).tw. 18. 13 or 14 or 15 or 16 or 17 19. Randomized Controlled Trials/ or random allocation/ or Controlled Clinical Trials/ or control groups/ or clinical trials/ or clinical trials, phase i/ or clinical trials, phase ii/ or clinical trials, phase iii/ or clinical trials, phase iv/ 20. double‐blind method/ or single‐blind method/ or cross‐over studies/ or Program Evaluation/ or meta‐analysis/ 21. randomized controlled trial.pt. or controlled clinical trial.pt. or clinical trial.pt. or meta analysis.pt. 22. random$.tw. 23. (controlled adj5 (trial$ or stud$)).tw. 24. (clinical$ adj5 trial$).tw. 25. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 26. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 27. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 28. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 29. (coin adj5 (flip or flipped or toss$)).tw. 30. versus.tw. 31. (cross‐over or cross over or crossover).tw. 32. (assign$ or alternate or allocat$ or counterbalance$ or multiple baseline).tw. 33. controls.tw. 34. (treatment$ adj6 order).tw. 35. (meta‐analy$ or metaanaly$ or meta analy$ or systematic review or systematic overview).tw. 36. or/19‐35 37. occupational therapy/ 38. Rehabilitation/ or Rehabilitation, Vocational/ 39. activities of daily living/ or self care/ 40. automobile driving/ or exp transportation/ 41. "Task performance and analysis"/ or Work simplification/ 42. exp leisure activities/ 43. Home care services/ or Home care services, hospital‐based/ 44. Recovery of function/ 45. exp work/ or Human activities/ 46. occupational therap$.tw. 47. ("activities of daily living" or ADL or EADL or IADL).tw. 48. rehabilitation.tw. 49. ((self or personal) adj5 (care or manage$)).tw. 50. (dressing or feeding or eating or toilet$ or bathing or mobil$ or driving or public transport or public transportation).tw. 51. exp self‐help devices/ 52. (assistive adj5 (device$ or technology)).tw. 53. or/37‐52 54. 12 and 18 and 36 and 53 55. limit 54 to (humans and "all adult (19 plus years)") 56. apraxias/ or apraxia, ideomotor/ or neglect/ or exp dementia/ or exp Arm/ or exp Hand/ or exp Depressive Disorder/ or depression/ or exp Pharmaceutical Preparations/ or exp Drug Therapy/ 57. (apraxi$ or dysprax$ or aphasi$ or dysphasi$ or dementia or alzheimer$).ti. 58. atrial.tw. 59. 56 or 57 or 58 60. 55 not 59 61. (dose$ or drug$).tw. 62. 60 not 61 63. Magnetic Resonance Imaging/ or Diffusion Magnetic Resonance Imaging/ or Imaging, Three‐Dimensional/ or Diagnostic Imaging/ or Radionuclide Imaging/ or Magnetic Resonance Imaging, Cine/ 64. 62 not 63 65. (MRI or fMRI).tw. 66. 64 not 65
Data and analyses
Comparison 1.
Cognitive skills remediation training versus usual rehabilitation
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Improvement in time judgement | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 17.0 [‐2.46, 36.46] |
| 2 Improvement in Barthel Index | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 10.71 [‐2.41, 23.83] |
History
Protocol first published: Issue 2, 2007 Review first published: Issue 9, 2010
| Date | Event | Description |
|---|---|---|
| 10 July 2008 | Amended | Converted to new review format. |
Differences between protocol and review
We have clarified the definition of occupational therapy from the original protocol such that in Types of interventions it now states "We defined occupational therapy interventions in this review as interventions carried out by an occupational therapist or under the supervision of an occupational therapist or indexed in major international occupational therapy texts".
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Carter 1983
| Methods | RCT | |
| Participants | 33 acute stroke patients (16 males, 17 females) N = 16: cognitive skills remediation training group (mean age 70.5 years) N = 17: rehabilitation as usual (mean age 73.4 years) Inpatients | |
| Interventions | Cognitive skills remediation training was administered on an individual basis for 30 to 40 minutes 3 times per week for an average of 3 to 4 weeks The cognitive skills remediation training was based on the Thinking Skills Workbook (Carter 1980). Participants in the cognitive skills remediation group also received rehabilitation as usual The comparison was rehabilitation as usual which included physical therapy, speech therapy, occupational therapy, social work, and rehabilitation nursing staff | |
| Outcomes | Visual scanning, visual‐spatial tests, and time judgement tests from the Thinking Skills Workbook (Carter 1980) were measured; however, for the purpose of this review only time judgement scores are reported as this is a test of cognition whereas, as defined by this review, visual scanning and visual‐spatial tests are measures of perceptual skill Barthel Index of functioning was also measured | |
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | Not reported |
N: number of participants RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Boiko 2008 | Does not meet definition of occupational therapy used in this review |
| Chen 2006a | Unable to determine if the intervention meets the definition of occupational therapy as no response received from the authors |
| Chen 2006b | Does not meet the definition of occupational therapy used in this review |
| Dirette 1999 | Study with mixed aetiology groups; fewer than 50% of participants diagnosed with stroke |
| Donkervoort 2001 | Focus is on perceptual rather than cognitive impairment |
| Doornhein 1998 | Does not meet the definition of occupational therapy used in this review |
| Edmans 2000 | Focus is on perceptual rather than cognitive impairment |
| Gasparinni 1979 | Does not meet the definition of occupational therapy used in this review |
| Hu 2003 | Unable to determine if the intervention meets the definition of occupational therapy used in this review |
| Man 2006 | Study with mixed aetiology groups; unable to obtain separate data for participants with stroke from authors |
| Mount 2007 | Does not meet the definition of occupational therapy used in this review |
| Ploughman 2008 | Does not meet the definition of occupational therapy used in this review |
| Sarkamo 2008 | Does not meet the definition of occupational therapy used in this review |
| Shottke 1997 | Does not meet the definition of occupational therapy used in this review |
| Soderback 1988 | Not all participants had cognitive impairment as defined in this review |
| Thickpenny‐Davis 2007 | Does not meet the definition of occupational therapy used in this review |
Characteristics of ongoing studies [ordered by study ID]
Walker
| Trial name or title | Dressing Rehabilitation Evaluation Stroke Study (DRESS) |
| Methods | Randomised controlled trial |
| Participants | Patients on the stroke unit at Nottingham City Hospital will be included in the study if they have:
|
| Interventions | 70 patients will be randomly allocated to 1 of 2 groups: Neuropsychological Dressing Group or Conventional Dressing Group All patients will be given treatment (prescribed by the relevant manual) 3 days per week for 6 weeks Intervention for patients in the Neuropsychological Dressing Group will be based on a manual that has been developed to address the cognitive problems most commonly seen in dressing after stroke, e.g. neglect, poor sustained attention, memory etc ‐ the suggested treatment strategies for these problems has been drawn from reviewing the neuropsychological literature and findings from the researchers' previous single case designs Patients in the Conventional Dressing Group will be given treatment that is based on a manual that contains strategies commonly used by occupational therapists in the UK which do not routinely target cognitive problems |
| Outcomes | The primary outcome measure is the Nottingham Stroke Dressing Assessment |
| Starting date | 1 March 2008 |
| Contact information | Professor Marion Walker marion.walker@nottingham.ac.uk |
| Notes | Due for completion by end of 2009 |
Contributions of authors
Tammy Hoffmann: conceiving, designing, and co‐ordinating the review; advising on search strategies; screening search results; screening retrieved papers against inclusion criteria; appraising the quality of papers; extracting data from papers; managing and analysing the data for review; interpreting the data (providing methodological, clinical, and policy perspectives); and writing the review.
Sally Bennett: screening retrieved papers against inclusion criteria; appraising the quality of papers; extracting data from papers; managing and analysing the data for the review; interpreting the data (providing methodological, clinical, and policy perspectives); and writing the review.
Chia‐Lin Koh: designing the review; designing search strategies; undertaking searches; screening search results; organising the retrieval of papers; screening retrieved papers against inclusion criteria; writing to authors of papers for additional information; providing additional data about papers; obtaining and screening data on unpublished studies; managing and analysing the data for review; interpreting the data (providing methodological, clinical, and policy perspectives); and writing the review.
Kryss McKenna (Passed away in April 2009): conceiving, designing and co‐ordinating the initial stage of the review, and advising on search strategies. Screening papers, data extraction and analysis occurred after April 2009.
Declarations of interest
None known. Fourth author, Kryss McKenna, deceased: refer to published protocol for previous listed interests.
New
References
References to studies included in this review
- Carter LT, Howard BE, O'Neill WA. Effectiveness of cognitive skills remediation in acute stroke patients. American Journal of Occupational Therapy 1983;37(5):320‐6. [DOI] [PubMed] [Google Scholar]; Carter LT, Oliveira DO, Duponte J, Lynch SV. The relationship of cognitive skills performance to activity of daily living in stroke patients. American Journal of Occupational Therapy 1988;42(7):449‐55. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Boiko EA, Kulishova TV, Shumakher GI, Iusupkhodzhaev RV. [The role of physical exercises in the improvement of cognitive functions in patients who survived stroke, in the early rehabilitative period]. Voprosy Kurortologii, Fizioterapii i Lechebnoi Fizicheskoi Kultury 2008;6:9‐12. [PubMed] [Google Scholar]
- Chen SZ, Jiang Q, Liu P, Huang DF, Ding JX. Effect of the cognitive rehabilitation on the functional independence of hemiplegic patients with stroke. Chinese Journal of Clinical Rehabilitation 2006;10(18):14‐6. [Google Scholar]
- Chen X‐F. Effect of community‐based‐rehabilitation on activities of daily life and cognitive function in stroke patients. Chinese Journal of Clinical Rehabilitation 2006;25(10):4‐6. [Google Scholar]
- Dirette DK, Hinojosa J, Carnevale GJ. Comparison of remedial and compensatory interventions for adults with acquired brain injuries. Journal of Head Trauma Rehabilitation 1999;14(6):595‐601. [DOI] [PubMed] [Google Scholar]
- Donkervoort M, Dekker J, Stehmann‐Saris FC, Deelman BG. Efficacy of strategy training in left hemisphere stroke patients with apraxia: a randomised clinical trial. Neuropsychological Rehabilitation 2001;11(5):549‐66. [Google Scholar]
- Doornhein K, DeHaan EHF. Cognitive training for memory deficits in stroke patients. Neuropsychological Rehabilitation 1998;8(4):393‐400. [Google Scholar]
- Edmans JA, Webster J, Lincoln NB. A comparison of two approaches in the treatment of perceptual problems after stroke. Clinical Rehabilitation 2000;14:230‐43. [DOI] [PubMed] [Google Scholar]
- Gasparinni B, Satz P. A treatment of memory problems in left hemisphere CVA patients. Journal of Clinical Neuropsychology 1979;1(2):137‐50. [Google Scholar]
- Hu X, Dou Z, Zhu H, Wan G, Li J. The single blind procedure research of cognitive rehabilitation interventions on cognitive deficits in patients with stroke. Chinese Journal of Clinical Rehabilitation 2003;7(10):1521‐3. [Google Scholar]
- Man DW, Soong WY, Tam SF, Hui‐Chan CW. A randomized clinical trial study on the effectiveness of a tele‐analogy‐based problem‐solving programme for people with acquired brain injury (ABI). NeuroRehabilitation 2006;21(3):205‐17. [PubMed] [Google Scholar]
- Mount J, Pierce SR, Parker J, DiEgidio R, Woessner R, Spiegel L, et al. Trial and error versus errorless learning of functional skills in patients with acute stroke. NeuroRehabilitation 2007;22(2):123‐32. [PubMed] [Google Scholar]
- Ploughman M, McCarthy J, Bosse M, Sullivan HJ, Corbett D, Ploughman M, et al. Does treadmill exercise improve performance of cognitive or upper‐extremity tasks in people with chronic stroke? A randomized cross‐over trial. Archives of Physical Medicine & Rehabilitation 2008;89(11):2041‐7. [DOI] [PubMed] [Google Scholar]
- Sarkamo T, Tervaniemi M, Laitinen S, Forsblom A, Soinila S, Mikkonen M, et al. Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain 2008;131(3):866‐76. [DOI] [PubMed] [Google Scholar]
- Shottke H. Rehabilitation of attention deficits after stroke: efficacy of a neuropsychological training program for attention deficits. Verhaltenstherapie 1997;7:21‐33. [Google Scholar]
- Soderback, I. The effectiveness of training intellectual functions in adults with acquired brain damage. An evaluation of occupational therapy methods. Scandinavian Journal of Rehabilitation Medicine 1988;20(2):47‐56. [PubMed] [Google Scholar]
- Thickpenny‐Davis KL, Barker‐Collo SL. Evaluation of a structured group format memory rehabilitation program for adults following brain injury. Journal of Head Trauma Rehabilitation 2007;22(5):303‐13. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
- Dressing Rehabilitation Evaluation Stroke Study (DRESS). Ongoing study 1 March 2008.
Additional references
- Abreu BC, Toglia JP. Cognitive rehabilitation: a model for occupational therapy. American Journal of Occupational Therapy 1987;41(7):439‐48. [DOI] [PubMed] [Google Scholar]
- Blake H, Lincoln NB. Cognitive impairments following a stroke: the strain on caregivers. British Journal of Therapy and Rehabilitation 2002;9:334‐7. [Google Scholar]
- Blundon G, Smits E. Cognitive rehabilitation: a pilot survey of therapeutic modalities used by Canadian occupational therapists with survivors of traumatic brain injury. Canadian Journal of Occupational Therapy 2000;67(3):184‐96. [PubMed] [Google Scholar]
- Carter LT, Caruso JL, Languirand MA, Berard MA. Cognitive skills remediation in stroke and non‐stroke elderly. Clinical Neuropsychology 1980;2(3):109‐13. [Google Scholar]
- Centers for Disease Control and Prevention. Public health and aging: hospitalizations for stroke among adults aged > 65 years ‐ United States, 2000. JAMA 2003;290(8):1023‐4. [Google Scholar]
- Cicerone KD, Dahlberg C, Kalmar K, Langenbahn DM, Malec JF, Bergquist TF, et al. Evidence‐based cognitive rehabilitation: recommendations for clinical practice. Archives of Physical Medicine and Rehabilitation 2000;81(12):1596‐615. [DOI] [PubMed] [Google Scholar]
- Cicerone KD, Dahlberg C, Malec JF, Langenbahn DM, Felicetti T, Kneipp S, et al. Evidence‐based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Archives of Physical Medicine and Rehabilitation 2005;86(8):1681‐92. [DOI] [PubMed] [Google Scholar]
- Cobble ND, Bontke CF, Brandstater ME, Horn LJ. Rehabilitation in brain disorders. 3. Intervention strategies. Archives of Physical Medicine and Rehabilitation 1991;72(4‐S):S324‐31. [PubMed] [Google Scholar]
- Doyle PJ. Measuring health outcomes in stroke survivors. Archives of Physical Medicine and Rehabilitation 2002;83 Suppl 2:S39‐43. [DOI] [PubMed] [Google Scholar]
- Hanson CS, Shechtman O, Foss JJ, Krauss‐Hooker A. Occupational therapy: current practice and training issues in the treatment of cognitive dysfunction. NeuroRehabilitation 1997;8(1):31‐41. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
- Hochstenbach J. Rehabilitation is more than functional recovery. Disability and Rehabilitation 2000;22(4):201‐4. [DOI] [PubMed] [Google Scholar]
- Juni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz N, editor. Cognition and occupation across the life span: models for intervention in occupational therapy. 2nd Edition. Bethesda, MD: American Occupational Therapy Association, 2005. [Google Scholar]
- Legg L, Drummond A, Langhorne P. Occupational therapy for patients with problems in activities of daily living after stroke. Cochrane Database of Systematic Reviews 2006, Issue 4. [Art. No.: CD003585. DOI: 10.1002/14651858.CD003585.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma HI, Trombly CA. A synthesis of the effects of occupational therapy for persons with stroke, part II: remediation of impairments. American Journal of Occupational Therapy 2002;56(3):260‐74. [DOI] [PubMed] [Google Scholar]
- Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical Therapy 2003;83(8):713‐21. [PubMed] [Google Scholar]
- Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro). Australian Journal of Physiotherapy 2002;48(1):43‐9. [DOI] [PubMed] [Google Scholar]
- National Stroke Foundation. Clinical Guidelines for Stroke Rehabilitation and Recovery. Retrieved from: www.strokefoundation.com.au2005.
- Patel M, Coshall C, Rudd AG, Wolfe CD. Natural history of cognitive impairment after stroke and factors associated with its recovery. Clinical Rehabilitation 2003;17(2):158‐66. [DOI] [PubMed] [Google Scholar]
- Pedretti LW, Early MB, editors. Occupational therapy: practice skills for physical dysfunction. 5th Edition. St Louis: Mosby Inc, 2001. [Google Scholar]
- Poole J, Dunn W, Schell B, Tiernan K, Barnhart JM. Statement: occupational therapy services management of persons with cognitive impairments. American Journal of Occupational Therapy 1991;45(12):1067‐8. [DOI] [PubMed] [Google Scholar]
- Radomski MV. Cognitive rehabilitation: advancing the stature of occupational therapy. American Journal of Occupational Therapy 1994;48(3):271‐3. [DOI] [PubMed] [Google Scholar]
- Steultjens EM, Dekker J, Bouter LM, Nes JC, Cup EH, Ende CH. Occupational therapy for stroke patients: a systematic review. Stroke 2003;34(3):676‐87. [DOI] [PubMed] [Google Scholar]
- Tatemichi TK, Desmond DW, Stern Y, Paik M, Sano M, Bagiella E. Cognitive impairment after stroke: frequency, patterns, and relationship to functional abilities. Journal of Neurology, Neurosurgery and Psychiatry 1994;57(2):202‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrift AG, Dewey HM, Macdonell RA, McNeil JJ, Donnan GA. Stroke incidence on the east coast of Australia: the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke 2000;31(9):2087‐92. [DOI] [PubMed] [Google Scholar]
- Toglia JP. A dynamic interactional approach to cognitive rehabilitation. In: Katz N editor(s). Cognition and occupation across the life span: models for intervention in occupational therapy. 2nd Edition. Bethesda, MD: American Occupational Therapy Association, 2005:29‐72. [Google Scholar]
- Trombly CA, Radomski MV. Occupational therapy for physical dysfunction. 5th Edition. Baltimore, MD: Williams & Wilkins, 2002. [Google Scholar]
- Unsworth C. Cognitive and perceptual dysfunction. Philadelphia: FA Davis Company, 1999. [Google Scholar]
- Zinn S, Dudley TK, Bosworth HB, Hoenig HM, Duncan PW, Horner RD. The effect of poststroke cognitive impairment on rehabilitation process and functional outcome. Archives of Physical Medicine and Rehabilitation 2004;85(7):1084‐90. [DOI] [PubMed] [Google Scholar]
- Zoltan B. Vision, perception and cognition. A manual for the evaluation and treatment of the adult with acquired brain injury. Thorofare NJ: SLACK, 2007. [Google Scholar]


