Abstract
Background
Accelerating the rate of tooth movement may help to reduce the duration of orthodontic treatment and associated unwanted effects including root resorption and enamel demineralisation. Several methods, including surgical and non‐surgical adjuncts, have been advocated to accelerate the rate of tooth movement. Non‐surgical techniques include low‐intensity laser irradiation, resonance vibration, pulsed electromagnetic fields, electrical currents and pharmacological approaches.
Objectives
To assess the effect of non‐surgical adjunctive interventions on the rate of orthodontic tooth movement and the overall duration of treatment.
Search methods
We searched the following databases on 25 November 2014: the Cochrane Oral Health Group's Trials Register (November 2014), the Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library 2014, Issue 10), MEDLINE via OVID (1946 to November 2014), EMBASE via OVID (1980 to November 2014), LILACS via BIREME (1980 to November 2014), metaRegister of Controlled Trials (November 2014), the US National Institutes of Health Trials Register (ClinicalTrials.gov; November 2014) and the WHO International Clinical Trials Registry Platform (November 2014). We checked the reference lists of all trials identified for further studies. There were no restrictions regarding language or date of publication in the searches of the electronic databases.
Selection criteria
We included randomised controlled trials (RCTs) of people receiving orthodontic treatment using fixed appliances along with non‐surgical adjunctive interventions to accelerate tooth movement. We excluded non‐parallel design studies (for example, split‐mouth) as we regarded them as inappropriate for assessment of the effects of this type of intervention.
Data collection and analysis
Two review authors were responsible for study selection, risk of bias assessment and data extraction; they carried out these tasks independently. Any disagreements were resolved by discussion amongst the review team to reach consensus. The review authors contacted the corresponding authors of trials to obtain missing information and data to allow calculation of mean differences (MD), 95% confidence intervals (CI) or risk ratios (RR) when these were not reported.
Main results
We included two studies in this review, which were both assessed as being at high risk of bias. The two studies, involving a total of 111 participants, compared the use of Tooth Masseuse and OrthoAccel with conventional treatment mechanics during orthodontic alignment and canine retraction phases, respectively. Both studies included objective assessment of the amount or rate of tooth movement, but we were not able to meta‐analyse this data as they used different outcome measurements at different stages of the orthodontic treatment process. One study measured subjective evaluation of pain and discomfort and the other evaluated adverse effects. The studies did not directly report either the duration of orthodontic treatment or the number of visits during active treatment.
Using the Tooth Masseuse with 111 Hz at 0.06 Newtons (N) for 20 minutes daily resulted in greater reduction in irregularity in the lower incisor region over 10 weeks, assessed using Little's Irregularity Index (LII) with a mean difference (MD) of 0.6 mm (95% confidence interval (CI) ‐0.94 to 2.34) when compared to the control group. Pain and discomfort increased at six to eight hours after arch wire placement and after seven days, with minimal difference between the intervention and control groups. No statistical tests were provided for either variable and the differences between the two groups were not clinically important.
Using OrthoAccel with 30 Hz at 0.25 N for 20 minutes daily produced a higher rate of maxillary canine distalisation in comparison to the control group (MD 0.37 mm/month; 95% CI ‐0.07 to 0.81; P = 0.05). Whilst this difference suggested 50% faster tooth movement using the vibrational appliance, the absolute differences were marginal and deemed clinically unimportant. Similar levels of non‐serious adverse effects were reported in the intervention and control groups with a risk ratio of 0.96 (95% CI 0.32 to 2.85).
Overall, the quality of the evidence was very low and therefore we cannot rely on the findings.
Authors' conclusions
There is very little clinical research concerning the effectiveness of non‐surgical interventions to accelerate orthodontic treatment. The available evidence is of very low quality and so it is not possible to determine if there is a positive effect of non‐surgical adjunctive interventions to accelerate tooth movement. Although there have been claims that there may be a positive effect of light vibrational forces, results of the current studies do not reach either statistical or clinical significance. Further well‐designed and rigorous RCTs with longer follow‐up periods are required to determine whether non‐surgical interventions may result in a clinically important reduction in the duration of orthodontic treatment, without any adverse effects.
Plain language summary
Additional, non‐surgical treatments for accelerating tooth movement in dental patients being treated with fixed braces
Review question What effect do non‐surgical adjuncts have on the length of time it takes for teeth to move when treated with fixed braces, and the overall time required for orthodontic treatment?
Background Throughout the world, orthodontic treatment is used to correct the position of teeth in adolescents and adults when they experience problems. Braces are orthodontic appliances made up of brackets glued to the teeth and then connected by wires in order to exert pressure on the teeth to move them and improve their positioning. Depending on the problem, the length of time for treatment may range from several months to several years. However, most treatments take on average, around 24 months. Accelerating the rate of tooth movement may help to reduce the length of time needed for a course of treatment and may reduce the unwanted effects of orthodontic treatment that can sometimes occur, such as tooth decay and the shortening of the tooth root. Several methods, including surgical and non‐surgical treatments, have been suggested to accelerate orthodontic tooth movement. The evidence relating to non‐surgical procedures to accelerate orthodontic tooth movement is assessed in this review.
Study characteristics
Authors for the Cochrane Oral Health Group carried out this review of existing studies. The evidence on which it is based is current up to 26 November 2014.
We included two studies involving a total of 111 participants in this review. A single orthodontic specialist in a private practice in Australia carried out one study, while the other study was conducted on patients treated by orthodontic residents in a university hospital seating in the United States of America. In one study, the age of participants ranged from 11 to 15 years old, and in the second, the average age of participants was 21 years. The studies evaluated the additional use of two devices that use light vibrational forces ‐ Tooth Masseuse in people receiving conventional fixed appliance treatment during the tooth alignment stage and OrthoAccel for those receiving conventional fixed appliance treatment for the space closure stage in orthodontic treatment. Participants receiving additional treatment with the devices were compared to those receiving only the conventional treatment. The trials evaluated different aspects of orthodontic tooth movement and side effects.
Key results
The studies evaluated three outcomes: rate of tooth movement; patient perception of pain and discomfort, and unwanted side effects. There were substantial differences between the studies, which meant that we were unable to combine the results.
From the limited evidence available, it is not possible to establish if the use of vibrational forces during treatment with fixed orthodontic appliances has a significant beneficial or harmful effect on either the rate of orthodontic tooth movement or the duration of treatment.
Quality of the evidence
The quality of evidence was very low.
Summary of findings
for the main comparison.
| Non‐surgical adjunctive interventions compared with conventional orthodontic treatment for accelerating the rate of orthodontic tooth movement | ||||||
|
Patient or population: Orthodontic patients with malocclusion Settings: Private orthodontic practice Intervention: Non‐surgical adjunctive interventions Comparison: Conventional orthodontic treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional orthodontic treatment | Non‐surgical adjunctive intervention | |||||
| Duration of active orthodontic treatment | Not investigated by included studies | |||||
| Rate of tooth movement: reduction in the Little's irregularity index (LII) during alignment stage due to tooth movement during the first 10 weeks of the alignment stage in mm | The mean reduction in the LII score in the control group was 3.4 mm | The mean reduction in the LII score in intervention group was 0.6 mm higher (95% CI ‐0.94 to 2.34) | 64 participants (1 study) | ⊕⊝⊝⊝ very low 1 |
|
|
| Rate of tooth movement: rate of orthodontic tooth movement in the maxillary arch during space closure in mm/month | The mean rate of tooth movement in the control group was 0.79 mm/month | The mean rate of orthodontic tooth movement in the intervention groups was 0.37 mm/month higher (95% CI ‐0.07 to 0.81) | 45 participants (1 study) | ⊕⊝⊝⊝ very low2 |
|
|
| Improvement in occlusion | Not investigated by the included studies. | |||||
| Patient‐centred outcomes: Pain and discomfort using visual analogue scale (VAS; 0 to 100 mm) |
The mean pain and discomfort VAS score was 47.6 in the control group after one day from ligating the arch wire | The mean pain and discomfort VAS score in the intervention groups was 6.1 points lower (95% CI ‐6.60 to 18.80) | 64 participants (1 study) | ⊕⊝⊝⊝ very low1 |
|
|
| Harms: Serious adverse effects | 0 | 0 | RR 1 | 45 participants (1 study) | ⊕⊝⊝⊝ very low2 |
|
| Harms: Non‐serious adverse effects during treatment, including: gastrointestinal disorders, general disorders , injury, poisoning and procedural complications, musculoskeletal and connective tissue disorders, nervous system disorders and respiratory, thoracic and mediastinal disorders. |
230 per 1000 | 220 per 1000 (74 to 656) |
RR 0.96 (95% CI 0.32 to 2.85) | 45 participants (1 study) | ⊕⊝⊝⊝ very low2 |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Downgraded one level for limitation in design and implementation due to unclear risk of allocation bias, performance bias and other sources of bias. Downgraded one level for imprecision (single study Miles 2012). Also downgraded one level for indirectness of evidence (surrogate results).
2 Downgraded one level for limitation in design and implementation due to unclear risk of selection bias, detection bias, attrition bias, reporting bias and other sources of bias. Downgraded one level for imprecision (single study Pavlin 2015). Also downgraded one level for indirectness of evidence (surrogate results).
Background
Description of the condition
Deviation from a normal bite can be defined as malocclusion (Andrews 1972). It is a common dental problem with a range of prevalence among different ethnic populations, with more than a quarter of adolescents classified as being in need of orthodontic treatment (Migale 2009; Mtaya 2009; Tausche 2004). Malocclusion can cause aesthetic and functional problems, which can lead to a negative impact on quality of life (Dimberg 2015). Malocclusion is normally corrected using orthodontic treatment, which includes fixed or removable orthodontic appliances, or both.
There are clear benefits of effective and efficient fixed orthodontic treatment to patients, clinicians, and health service providers. Effective orthodontic treatment is accomplished by delivering planned treatment goals over the shortest time possible, with minimal biological side effects and high levels of patient satisfaction. The duration of orthodontic treatment may range from several months to several years, with the majority of comprehensive treatment taking approximately 24 months to complete (Mavreas 2008). This can be extended for patients with a severe malocclusion. Reducing treatment duration can limit the risk of undesirable effects and associated cost, and can increase patient satisfaction (Riedmann 1999; Segal 2004).
Several factors can influence the duration of treatment, including both patient‐related and treatment‐related aspects (Fisher 2010; Mavreas 2008). An increased duration of treatment is undesirable, due to the increased risk of exposing patients to additional biological side effects (e.g. root shortening or decalcification). Several conventional treatment modalities have been suggested to reduce the duration of orthodontic treatment (Germec 2008; Sebastian 2012). Similarly, in the last few decades, non‐conventional adjunctive techniques have been developed to reduce treatment duration by accelerating the rate of tooth movement. These include surgical interventions (e.g. surgical corticotomy) and non‐surgical interventions (e.g. low laser therapy and mechanical vibration).
Description of the intervention
The proposed non‐surgical adjunctive interventions to accelerate orthodontic tooth movement include:
Low energy laser radiation directed to the mucosa of the targeted teeth;
Intermittent resonance vibration using an electrical appliance fitted into the orthodontic appliance or the teeth;
Pulsed electromagnetic waves using integrated circuits placed in an oral appliance;
Chewing gum or muscle exercise;
Pharmacological methods; and
Novel methods as they are described by authors.
These interventions are used during conventional fixed appliance orthodontic treatment therapy, and are undertaken by the clinician in a clinical setting during additional scheduled visits (e.g. low energy laser radiation), or can be fitted in an oral appliance and used by the patient on a daily or weekly basis following the clinician's prescription (e.g. pulsed electromagnetic waves and intermittent electrical vibration).
How the intervention might work
Orthodontic tooth movement occurs due to a sterile inflammatory process that results in bone resorption and deposition, which is known as bone remodelling (Zainal 2011). Bone cells (osteoclasts and osteoblasts) responsible for remodelling are the main target of non‐surgical interventions for accelerating tooth movement. This is because it has been proposed that such interventions can act as a bio‐stimulus to increase the activity of bone cells (Tortamano 2009). The increased bone remodelling rate can increase the rate of tooth movement, which may lead to a reduction in the duration of orthodontic treatment.
Why it is important to do this review
The Cochrane Oral Health Group undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important ones to maintain on the Cochrane Library (Worthington 2015). Consequently, this review was identified as a priority title by the orthodontic expert panel (Cochrane OHG priority review portfolio).
The duration of treatment is an important aspect of successful and effective orthodontic therapy. Comprehensive fixed appliance orthodontic treatment usually takes about two years to complete and can be influenced by different factors, including patient‐related and treatment‐related aspects. Reduction in the duration of orthodontic treatment can reduce the exposure of patients to risks associated with treatment and related cost, and can increase patient satisfaction. This systematic review assessed the available evidence for the effect of non‐surgical adjunctive interventions on the reduction of orthodontic treatment duration by accelerating orthodontic tooth movement. In addition, the effect on treatment outcome, biological side effects and patient perception were evaluated. This provides the orthodontic clinician with evidence about the effectiveness and safety of non‐surgical adjunctive interventions for accelerating orthodontic tooth movement.
Objectives
To assess the effect of non‐surgical adjunctive interventions for accelerating the rate of orthodontic tooth movement and reducing the duration of orthodontic treatment.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), irrespective of publication status or language of publication. Non‐parallel design studies (e.g. split‐mouth) were determined to be inappropriate for this type of investigation. This is mainly because this type of study design may introduce 'carry‐across effects' which potentially allow interventions to have effects on experimental units other than those to which they were assigned. There was no restriction in the length of follow‐up.
Types of participants
We included studies of individuals, of any age, receiving orthodontic treatment with fixed appliances that incorporated the adjunctive use of non‐surgical interventions to accelerate tooth movement. We excluded studies that included patients who were treated with orthognathic surgery, participants with cleft lip or palate, or with other craniofacial syndromes or deformities, as these patients would routinely have a combination of orthodontic and surgical treatment, which can influence the outcome, duration and side effects of the treatment.
Types of interventions
Active interventions: any form of fixed appliance orthodontic treatment incorporating the use of non‐surgical adjunctive interventions for accelerating orthodontic tooth movement
Control: any form of fixed appliance orthodontic treatment without the use of non‐surgical adjunctive interventions for accelerating orthodontic tooth movement
Types of outcome measures
Primary outcomes
Rate of tooth movement determined by millimetres of tooth movement per week or month
Duration of active orthodontic treatment, number of visits during active treatment (scheduled and unscheduled), and duration of appointments
Secondary outcomes
Improvement in occlusion, as judged using Peer Assessment Rating (PAR) or other validated scale, recorded at the completion of active orthodontic treatment
Patient‐centred outcomes: impact of fixed appliances on daily life, quality of life and pain experience
Harms arising during the course of orthodontic treatment including gingival and periodontal problems, anchorage loss, and iatrogenic damage to teeth (e.g. caries or decalcification, root resorption)
Prolonged stability of treatment outcome using validated methods, e.g. Little's irregularity index (LII)
Cost of treatment
Safety of the adjunctive intervention
Search methods for identification of studies
For the identification of studies included or considered for this review, we developed detailed search strategies for each database that was searched. These were based on the search strategy developed for MEDLINE, and revised appropriately for each database.
Electronic searches
We searched the following databases:
The Cochrane Oral Health Group's Trials Register (November 2014; see Appendix 1);
The Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library 2014, Issue 10; see Appendix 2);
MEDLINE via OVID (1946 to November 2014; see Appendix 3);
EMBASE via OVID (1980 to November 2014; see Appendix 4);
LILACS via BIREME (1980 to November 2014; see Appendix 5).
The MEDLINE subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of theCochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
Searching other resources
We examined the reference lists of relevant articles and contacted the investigators of included studies by electronic mail to ask for details of additional published and unpublished trials.
Ongoing trials
We conducted searches using the following databases to identify ongoing trials (see Appendix 6 for details of the search strategy):
metaRegister of Controlled Trials (mRCT) (November 2014);
US National Institutes of Health Register (November 2014);
World Health Organization International Clinical Trials Registry Platform Search Portal (ICTRP; November 2014).
We also contacted manufacturers of non‐surgical adjuncts designed to accelerate orthodontic treatment for details of unpublished or ongoing trials.
Language
There were no language restrictions applied in the searches of the electronic databases.
Data collection and analysis
Selection of studies
Two review authors (AE and DB) independently assessed the titles and abstracts of studies identified by the searches. Full copies were obtained of all relevant and potentially relevant studies, and for studies that appeared to meet the inclusion criteria but for which there were insufficient data in the title and abstract to make a clear decision. The full‐text papers were independently assessed by two review authors (AE and GM). Any disagreement on the eligibility of an included study was resolved through discussion and consensus. From this group of full‐text papers, we recorded the studies not meeting the inclusion criteria, with reasons for exclusion, in the Characteristics of excluded studies section of the review.
Data extraction and management
Two review authors (AE and GM) independently extracted data. We used data extraction forms recording the year of publication, country of origin and details of the participants including demographic characteristics and the criteria for inclusion. We entered the study details into the Characteristics of included studies tables in Review Manager (RevMan) 5.3 (RevMan 2014). Any disagreements were resolved by consulting with a third review author.
The following details were also extracted if reported.
Trial methods: (a) allocation method; (b) sample size calculation; (c) masking of participants, trialists and outcome assessors; (d) exclusion of participants after randomisation and the proportion and reasons for sample attrition at follow‐up.
Participants: (a) country of origin and study setting; (b) sample size; (c) age; (d) gender; (e) inclusion and exclusion criteria.
Intervention: (a) type; (b) materials and techniques used; (c) time of follow‐up.
Control: (a) type; (b) materials and techniques used; (c) time of follow‐up.
Outcomes: (a) primary and secondary outcomes mentioned in the Types of outcome measures section of this review.
Where stated, we recorded sources of funding. The review authors used this information to aid their assessment of investigator reporting bias and the validity of included trials.
Assessment of risk of bias in included studies
Two review authors (AE and GM) independently assessed the risk of bias for the selected trials using Cochrane's tool for assessing risk of bias, as described in section 8.5 of theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We produced a 'Risk of bias' table for each included study in two parts. For each domain, we provided a description of what was reported to have happened in part one, whilst for the second part, we used this information to judge whether the risk of bias was low, high or unclear. The two review authors compared their assessments; any inconsistencies between them were discussed and resolved.
We assessed the following domains as being at low, high or unclear risk of bias:
random sequence generation (selection bias);
allocation concealment (selection bias);
blinding of participants and personnel (performance bias);
blinding of outcome assessors (detection bias);
incomplete outcome data addressed (attrition bias);
selective outcome reporting (reporting bias);
other bias.
We categorised and reported the overall risk of bias of each included study according to the following:
low risk of bias (plausible bias unlikely to seriously alter the results) if all domains were assessed at low risk of bias;
unclear risk of bias (plausible bias that raises some doubt about the results) if one or more domains were assessed at unclear risk of bias; or
high risk of bias (plausible bias that seriously weakens confidence in the results), if one or more domains were assessed at high risk of bias.
Measures of treatment effect
We calculated mean differences (MD) with 95% confidence intervals (CI) for continuous data, and risk ratios (RR) with 95% CI for dichotomous data. We contacted the corresponding authors of trials for original data where necessary.
Unit of analysis issues
We had anticipated that some of the included studies may have presented participant data from repeated or multiple site observations, or both, which may have lead to unit of analysis errors. Had this been the case, we would have followed the advice provided in section 9.3.4 of theCochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
Dealing with missing data
In studies where data were unclear or missing, we contacted the principal investigators. If missing data were unavailable, we followed the advice given in section 16.1.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
Assessment of heterogeneity
We assessed clinical heterogeneity by examining the characteristics of the studies, the similarity between the types of participants, the interventions and the outcomes, as specified in the criteria for included studies. We had intended to assess statistical heterogeneity using a Chi² test and the I² statistic, but this was not possible. We would have considered heterogeneity to be significant for the Chi² test when the P value was less than 0.10, with I² values of 30% to 60% indicating moderate heterogeneity, and over 60%, substantial heterogeneity (Higgins 2003).
Assessment of reporting biases
We had intended to assess publication bias according to the recommendations on testing for funnel plot asymmetry if a sufficient number of studies assessing similar interventions were identified for inclusion in this review, as described in section 10.4.3.1 of theCochrane Handbook for Systematic Reviews of Interventions (Sterne 2011). If asymmetry had been identified, we had planned to assess other possible causes and explore these in the discussion.
Data synthesis
We had planned to carry out meta‐analyses where there were studies of similar comparisons reporting the same outcomes. We had planned to synthesise mean differences for continuous data, and risk ratios for dichotomous data. We had planned to use the fixed‐effect model for meta‐analyses. However, meta‐analysis was not possible. We used additional tables to present the results from the included studies.
Subgroup analysis and investigation of heterogeneity
If a sufficient number of studies had been included with moderate, substantial or considerable heterogeneity (see Assessment of heterogeneity), we had planned to carry out subgroup analyses according to:
type of non‐surgical method used;
age category (adolescents versus adults).
Sensitivity analysis
Had meta‐analysis been possible, we would have performed sensitivity analyses, excluding studies with a high or unclear risk of bias.
Presentation of main results
Using GRADEPro software (GRADEpro 2014), we produced Table 1 for the following outcomes, listed by priority.
Rate of tooth movement
Duration of orthodontic treatment, number of visits during active treatment (scheduled and unscheduled), and duration of appointments
Improvement in occlusion
Patient‐centred outcomes: impact of fixed appliances on daily life, quality of life and pain experience
Harm arising during the course of orthodontic treatment: including gingival and periodontal problems, anchorage loss and iatrogenic damage to teeth (e.g. caries or demineralisation, root resorption)
We assessed the quality of the evidence as high, moderate, low or very low, with reference to the overall risk of bias for the included studies, the directness of the evidence, the inconsistency of the results, the precision of the estimates and the risk of publication bias.
Results
Description of studies
See Characteristics of excluded studies and Characteristics of included studies.
Results of the search
The electronic searches identified 323 references with a further single reference identified through other sources. We examined the titles and abstracts of these studies for eligibility and eliminated all of those not matching the inclusion criteria. Seven potentially relevant studies were identified. We obtained full‐text articles of two studies (Miles 2012; Pavlin 2015), and registry entries for six ongoing studies, one of which was the study registration for Pavlin 2015, and subjected them to further evaluation. After further assessment, we eliminated three of the registered ongoing studies as they had a split‐mouth design (NCT02181439; IRCT138804022066N1; CTRI/2012/03/002488). Two potentially eligible ongoing studies are awaiting assessment as the trial authors were still recruiting participants (NCT02119455; JPRN‐UMIN000013722). Although several attempts were made by the review authors to contact the authors of Pavlin 2015 using the correspondence address in the study registration, there was no response until the results were published, so the initial assessments were completed on the study registration information. Figure 1 shows the study selection process.
1.
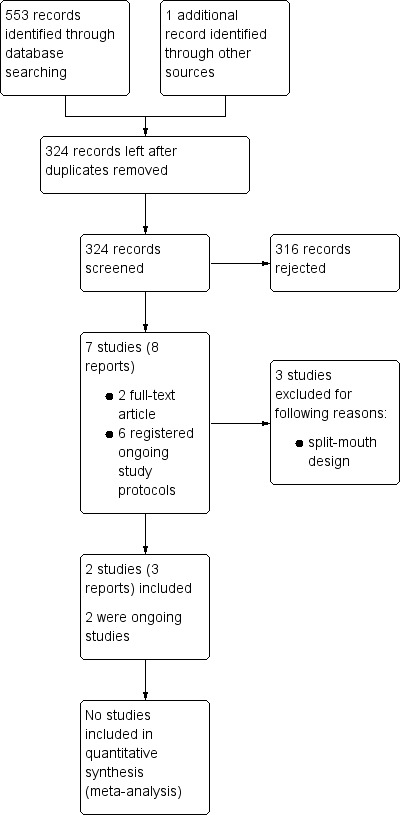
Study flow diagram
Included studies
We included two studies in this review, reported in three publications (Miles 2012; Pavlin 2015). The two studies were designed to assess the influence of vibrational appliances as an adjunctive intervention on the rate of tooth movement. Both studies obtained ethical approval prior to commencement of the studies and recruitment of participants.
Characteristics of the trial settings and investigators
We included two studies in the current review. In Miles 2012, the treatment was carried out by a single specialist orthodontist in private orthodontic practice in Australia. In the Pavlin 2015 study, the patients received treatment at The University of Texas Science Centre Division of Orthodontics in the United States of America. The patients were treated by orthodontic residents under supervision of faculty members.
Miles 2012 investigated the reduction in irregularity for the mandibular anterior teeth during the first 10 weeks of fixed appliance orthodontic treatment at several time points (5, 8, and 10 weeks from the start of treatment). Pavlin 2015 assessed the rate of orthodontic movement of a maxillary canine tooth being distalised to close an extraction space for an average of 22 weeks.
Characteristics of the participants
A total of 111 participants (43 male and 68 female) were involved in the two studies (Miles 2012; Pavlin 2015). In Miles 2012, the age range of the participants (N = 66) was 11.1 to 15.7 years, with a similar mean age in the control and experiential groups of 13.1 (SE ± 0.18) years and 13.0 (SE ± 0.18) years, respectively; with more females (N = 40) recruited in the study than males (N = 26). The participants had a non‐extraction orthodontic treatment plan with no impacted teeth requiring alignment. However, limited information was provided regarding the pre‐treatment malocclusion. Little's Irregularity Index scores pre‐treatment were 4.9 mm (SD ± 2.5) and 6.2 mm (SD ± 3.7) for the control and the experimental groups, respectively.
In Pavlin 2015, the average age of the participants (N = 45) was 21.6 (SD ± 8.2) years, with a similar mean age in the control and experiential groups of 21.4 (SD ± 7.8) and 21.8 (SD ± 8.7) years, respectively; more females (N = 28) were recruited in the study than males (N = 17). Participants had a minimum of 3 mm of extraction space that was to be closed by moving the maxillary canine distally. All participants received standard orthodontic treatment and temporary anchorage devices for tooth movement and space closure.
Characteristics of the interventions
A vibrational appliance was applied to the teeth for 20 minutes daily in the two studies to accelerate tooth movement, either to facilitate orthodontic space closure (Pavlin 2015), or to accelerate the alignment of the mandibular anterior teeth (Miles 2012). The device had a mouthpiece for the patient to lightly bite into with a linked extra‐oral enclosure. The device provided a light vibrational force.
In the Miles 2012 study, the vibration appliance (Tooth Masseuse), which provided a vibrational frequency of 11 Hz and 0.06 Newtons (N; ˜6.1 g), was applied immediately after the initial arch wire (0.014 inch NiTi) was placed, to accelerate the alignment of the mandibular anterior teeth. The same arch wire remained in place through the whole experimental period (10 weeks), and the participants were instructed to use the vibrational appliance daily for 20 minutes each session.
In the Pavlin 2015 study, the vibration appliance (OrthoAccel Device), which provided vibrational frequency of 30 Hz and 0.02 N, was applied to accelerate closing the extraction space, achieved by moving the maxillary anterior and canine teeth en masse, or the canine tooth distally, with the aid of a temporary anchorage device.
Characteristics of the outcomes
Outcomes assessed included primarily objective assessments of the amount and rate of tooth movement, in addition to subjective pain and discomfort experiences.
Specific clinical outcomes included:
1. Tooth movement: Miles 2012 assessed the amount of tooth alignment by measuring the reduction in the irregularity using Little's Irregularity Index (LII) at 0, 5 , 8 and 10 weeks after starting treatment. Pavlin 2015 assessed the rate of tooth movement per month by measuring the rate of maxillary canine distalisation to close an extraction space using a temporary anchorage device for an average of 22 weeks.
2. Pain experience: Miles 2012 investigated the levels of pain and discomfort during tooth alignment at five different time points (immediately after initial placement of fixed appliances, six to eight hours after, one day after, three days after, and at seven days) by asking participants to record pain and discomfort levels using a visual analogue scale.
The studies presented the outcome results as continuous data describing the mean and standard deviation, and dichotomous data describing participant numbers affected per study group. No statistical test results to compare the intervention outcomes were clearly mentioned in either of the studies. We considered a clinically significant difference would be a difference that could potentially have an impact on the overall duration of treatment.
Excluded studies
We excluded three ongoing studies due to a split‐mouth study design (see Characteristics of excluded studies).
Risk of bias in included studies
Neither of the included studies had a low risk of bias in all of the domains. We assessed both as being at high risk of bias.
Further details of these assessments are given in the 'Risk of bias' table corresponding to each study in the Characteristics of included studies section. Overall ratings are also presented in the 'Risk of bias' summary in Figure 2.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Selection bias can be minimised when participants and study personnel cannot foresee the upcoming assignment. Pavlin 2015 clearly mentioned the randomisation procedure: "A third‐party vendor provided computer generated randomisation scheduled with a block size of 4 and stratified"; however, the allocation concealment was not described. Miles 2012 reported "participants were randomly assigned in blocks of six"; however, the authors did not describe the randomisation method or the allocation concealment, so the risk of selection bias was unclear.
Blinding
Performance bias can be reduced by blinding both participants and study personnel to the type of intervention allocated. However, this can sometimes be unavoidable due to the nature of the intervention. In Miles 2012, although the clinician was blinded, the participants were not blinded to the type of intervention to which they were allocated; the study was rated as high risk of performance bias. Pavlin 2015 had a low risk of performance bias as the participants were blinded to the type of intervention allocated, and the control group participants were given a sham device, which is an inactive device that was held in the mouth and looked identical to the active devices, but did not deliver any vibration.
Detection bias was rated as low risk in both Miles 2012 and Pavlin 2015 as the outcome investigator was blinded during data collection.
Incomplete outcome data
Miles 2012 reported incomplete outcome data with no clear description of how the missing data was dealt with. For the rate of orthodontic tooth movement outcome, two (3%) participants out of 66 were lost to follow‐up; all the dropouts were from the experimental group. For the discomfort and pain outcome, there were eight (12.1%) dropouts (participants who did not complete VAS at the five time points) out of 66 study participants, five from the control group and three from the experimental group. Miles 2012 was assessed as unclear risk of bias, as it was not clear if the authors accounted for the missing data.
In Pavlin 2015, nine participants out of 45 (20%) were lost to follow‐up, with five dropouts from the experimental group and four from the control group. However, the study was assessed as low risk of bias as the authors accounted for the missing data by applying Intention‐to‐treat analysis.
Selective reporting
In Miles 2012, although the study protocol was not available, the outcomes listed in the 'Methods' section were comparable to the reported results. However, it was noticed that the results of the statistical tests (P value) comparing the two study groups were not reported. In general, we assessed the study as low risk of reporting bias.
The Pavlin 2015 study was registered in Clinicaltrials.gov, with all the proposed outcomes reported in an article in a peer‐reviewed journal. The study was assessed as low risk of bias.
Other potential sources of bias
In Miles 2012, the pain and discomfort participant rating using VAS for the lower anterior teeth may have been confounded by the presence of upper fixed appliances, with the potential of influencing pain and perceived discomfort in the investigated lower arch. It was unclear whether the authors had planned to assess pain and discomfort for both arches or the lower arch only.
Pavlin 2015 was sponsored by OrthoAccel Technologies Inc, which is the manufacturer of the intervention appliance. It was mentioned on the clinicaltrial.gov website that there was a time‐limited agreement between the principal investigators and the sponsor to review results before release to the public: "There is an agreement between Principal Investigators and the Sponsor that the sponsor can review results communications prior to public release and can embargo communications regarding trial results for a period that is less than or equal to 60 days. The sponsor cannot require changes to the communication and cannot extend the embargo." We assessed the study at high risk of bias for other potential sources of bias.
In Pavlin 2015, it was not clear if the primary outcome measure for the rate of orthodontic tooth movement was for the canines only or en masse retraction of the six anterior teeth. Although stratification was done according to age and the technique of space closure (canine versus en masse retraction), the authors did not present the distribution and outcome for the technique of space closure subgroups. This may have influenced the rate of space closure in each group.
Effects of interventions
See: Table 1
Vibrational appliances as an adjunct to fixed braces versus conventional fixed braces treatment (control)
Primary outcomes
Rate of tooth movement
Both studies measured the rate of orthodontic tooth movement; however, different teeth and types of tooth movements were investigated in each study. Miles 2012 investigated the reduction in Little's Irregularity Index (LII) scores for the anterior mandibular teeth during the alignment stage for 10 weeks; while Pavlin 2015 investigated the rate of canine distalisation during the space closure stage in millimetres per month for an average of 22 weeks.
Due to the aforementioned clinically significant methodological differences between the two studies, we were unable to combine the outcomes in a meta‐analysis. Therefore, the results for each study are discussed individually below.
Influence of a vibrational appliance versus conventional treatment (control) on the rate of anterior mandibular tooth movement during the alignment stage
Miles 2012 involved analysis of 64 children comparing vibrational appliance versus conventional treatment (control) by measuring the reduction in the LII score over 5, 8 and 10 weeks. This trial was judged to be at high risk of bias. The reduction in the LII score was higher in the intervention group with MD of 0.9 mm (95% CI ‐1.72 to 2.62) at 5 weeks; 0.3 mm (95% CI ‐0.95 to 1.55) at 8 weeks; and 0.7 mm (95% CI ‐0.94 to 2.34) at 10 weeks. No statistical tests were provided for the comparison between the two groups; however, based on the confidence intervals calculated, we concluded that there was no statistical difference between the two groups (Table 2).
1. Miles 2012: The effect of vibrational appliance on rate of tooth movement (alignment).
| Time point |
Control group LII mandibular arch Mean and SD in mm |
LII percentage reduction in control group** |
Intervention LII mandibular arch Mean and SD in mm |
LII percentage reduction in intervention group** |
Differnce between intervention and control groups LII mean difference mm (95%CI)** |
Statistical test t‐test |
| Number of participants analysed | 33 | 31 | Total = 64 | |||
| Initial LII score | 4.9 (2.5) | 6.2 (3.7) | 1.3 | Not provided | ||
| Reduction in LII score at 5 weeks | 2.2 (± 2.82)* | 45% | 3.1(± 0.79) | 50% | 0.9 (‐1.72 to 2.62) | Not provided |
| Reduction in LII score at 8 weeks | 3.1 (± 2.4) | 63% | 3.4 (± 2.7) | 55% | 0.3 (‐0.95 to 1.55) | Not provided |
| Reduction in LII score 10 weeks | 3.4 (± 2.4) | 69% | 4.0 (± 3.3) | 65% | 0.6 (‐0.94 to 2.34) | Not provided |
** Figures not published but calculated by the current review authors.
Influence of vibrational appliance versus conventional treatment with placebo (control) on the rate of canine distalisation during the space closure stage
Pavlin 2015 was assessed to be at high risk of bias and analysed 45 people aged 12 to 40 years. The investigators compared the use of a vibrational appliance as an adjunct to fixed braces versus conventional fixed braces treatment with a placebo (control) by measuring the rate of maxillary canine distalisation during space closure to close a minimum of 3 mm space with average follow‐up of 22 weeks. The authors reported that the difference in the rate of tooth movement (MD 0.37 mm/month; 95% CI ‐0.07 to 0.81) was statistically significant P = 0.05 (Table 3). However, based on the confidence intervals calculated for the mean differences, we concluded that there was no statistical difference between the two groups. In addition, the reported mean difference was considered to be clinically insignificant.
2. Pavlin 2015 The effect of vibrational appliance on the rate of orthodontic movement of a maxillary canine tooth.
| Control group sham (Inactive Device) | Intervention group OrthoAccel Device | Mean difference | Statistical test | |
| Number of participants analysed | 22 | 23 | 45 | 0.05 |
| The rate of orthodontic movement of a maxillary canine. Tooth being distalised to close an extraction space mean and 95% CI (millimetre per month) |
0.79; 95% CI (0.49–1.09) | 1.16; 95% CI (0.86–1.46) | 0.37; 95% CI (‐0.07 to 0.81) |
Duration of active orthodontic treatment
Neither of the included studies evaluated the influence of the vibrational appliance on the overall duration of orthodontic treatment. We felt that It was difficult and inaccurate to estimate the impact of the intervention on the overall duration of treatment from the available data.
Secondary outcomes
Patient‐centred outcome: Pain and discomfort
Miles 2012
The participants from the intervention and control groups were instructed to record the level of discomfort at five different time points using a 100 mm visual analogue scale (Table 4). It was noted that pain and discomfort increased after six to eight hours after arch wire placement and dropped again after seven days, with minimal difference between the intervention and the control group. No statistical tests were provided for the comparison between the two groups; however, based on the confidence intervals calculated for the mean differences, we concluded that there was no statistical difference between the two groups. In addition, the difference between the two groups was considered clinically insignificant (Table 4).
3. Miles 2012 Pain and discomfort.
| Time point | Control group VAS mean mm (SD) | Intervention group VAS mean mm (SD) | Mean difference and 95% CI | Statistical test |
| T0 after wire placement | 8.1 (12.3) | 12.4 (13.3) | 4.3 (‐2.19 to 10.79) | Not provided |
| T1 after 6 to 8 hours | 39.6 (25.8) | 40.4 (20.8) | 0.8 (‐11.37 to 12.25) | Not provided |
| T2 after 1 day | 47.6 (24.5) | 41.5 (27.2) | 6.1 (‐6.60 to 18.80) | Not provided |
| T3 after 3 days | 19.9 (15.5) | 18.8 (18.5) | 1.1 (‐7.27 to 9.47) | Not provided |
| T4 after 7 days | 5.5 (7.8) | 4.0 (6.3) | 1.5 (‐1.96 to 4.97) | Not provided |
Harms arising during the course of orthodontic treatment
Pavlin 2015
No serious adverse effects were reported in either the intervention or the control group during the study. A similar number of minimal non‐serious adverse effects were reported in the Intervention group 5/23 (21.74%) and control group 5/22 (22.73%), with a RR of 0.96 (95% CI 0.32 to 2.85). The non‐serious adverse effects included gastrointestinal disorders, general disorders, injury, poisoning and procedural complications, musculoskeletal and connective tissue disorders, nervous system disorders, and respiratory, thoracic and mediastinal disorders.
Other outcomes
None of the secondary outcomes mentioned below was investigated in either of the two included studies.
Patient‐centred outcomes: impact on daily life, quality of life
Improvement in occlusion, as judged using a validated scale recorded at the completion of active orthodontic treatment
Prolonged stability of treatment outcome using validated methods
Cost of treatment
Discussion
Summary of main results
See Table 1 for a summary of the main results.
Rate of tooth movement
The finding of the difference in reduction of Little's Irregularity Index (LII) in Miles 2012 is difficult to interpret due to the pre‐treatment difference between the two groups, with the intervention group having a higher initial LII and therefore greater possibility for a reduction to be achieved. Given that this is the only included study that investigated tooth movement during alignment, and it was assessed at a high risk of bias, it is not possible to draw any conclusions on the data presented on rate of tooth movement.
Although Pavlin 2015 reported a mean difference of 0.37 mm/month (95% confidence interval (CI) ‐0.07 to 0.81) in the rate of canine distalisation between the two groups, which was reported to be statistically significant (P = 0.05); this has to be considered with caution. First, the reported 95% confidence interval did not confirm that the difference was statistically significant as it included zero (95% CI ‐0.07 to 0.81). Second, the reported difference is considered to be clinically insignificant.
Both studies assessed the rate of tooth movement as a primary outcome. However, it was not possible to combine the data from the two studies. Miles 2012 reported no significant advantage in the use of vibrational appliances on the rate of alignment of anterior teeth, while Pavlin 2015 demonstrated that vibrational appliances could increase the rate of canine distalisation during extraction space closure (see Table 3). It is important to mention that neither of the studies presented a mean difference that we deemed to be of clinical significance for the duration investigated.
Pain and discomfort during treatment
Miles 2012 reported no advantage in the use of a vibrational appliance in reducing pain and discomfort during the first week of fixed orthodontic appliance treatment, whilst Pavlin 2015 did not investigate pain and discomfort during treatment.
Harms during treatment
Pavlin 2015 reported no increase in the adverse effects due to the use of a vibrational appliances during orthodontic treatment. Miles 2012 did not measure harms.
Overall completeness and applicability of evidence
Currently, the evidence for non‐surgical adjunctive interventions to increase the rate of tooth movement is incomplete. There are no data available for some interventions and the data for light vibrational forces is at high risk of bias with methodological flaws, meaning no conclusions can be drawn.
The participants in both studies are representative of the patient groups that would be treated in the majority of orthodontic settings, although the heterogeneity in Pavlin 2015 due to the mixture of children and adults compromises this. The LII used by Miles 2012 is a composite measure of irregularity so can be misleading when converted into millimetres per month of tooth movement for comparison. The latter is easier to interpret when appropriate, and was used by Pavlin 2015 .
It is important to note that in addition to the high risk of bias reported in the two included studies, the full orthodontic treatment duration and the reported outcomes cannot be considered to be representative of the entire orthodontic treatment duration. In other words, applying these results to the full duration of treatment is not realistic. It is important to interpret these results with caution as the methodology used for data collection was not described clearly and the study was rated as being at high risk of bias.
Quality of the evidence
We could not adequately assess the risk of bias in Miles 2012 due to the lack of information provided, but there wasthe possibility of allocation, attrition and other risks of bias. For Pavlin 2015, although the majority of domains were considered low risk of bias, the overall risk was assessed as high risk of bias due to the high risk of selection bias and other bias. Imprecision could have been avoided in both studies with appropriate sample sizes.
We downgraded the evidence by one level in respect of limitations in the study design, one for imprecision due to the small number of participants, and one for indirectness due to the use of surrogate outcomes as only the initial aligning stage of orthodontic treatment was assessed and the effect on overall treatment duration cannot be extrapolated from this. The overall quality of the evidence is therefore considered to be very low.
Potential biases in the review process
We used a broad search strategy with no language restrictions, and assessments were made independently by multiple authors. We are not aware of any biases in the review process. We excluded several published and ongoing studies because they were split‐mouth studies. At this time, we believe that the potential cross‐over effects of this design introduces a great risk of bias if we include this study design. The authors will continue to review this decision as evidence emerges from these ongoing studies.
Agreements and disagreements with other studies or reviews
In the last two years, several systematic reviews have been conducted to assess the effects of several types of surgical and non‐surgical interventions in accelerating tooth movement (Gkantidis 2014; Kalemaj 2015; Long 2013). It was noticed that there is a lack of agreement amongst the reviews with regards to the reported effectiveness of some of the non‐surgical interventions and the quality of evidence assessed. Gkantidis 2014 reported that there is moderate to weak evidence that non‐surgical interventions (low energy laser, photobiomodulation or pulsed electromagnetic fields) can accelerate tooth movement. In contrast, Long 2013 suggested that low‐level laser therapy is safe but unable to accelerate orthodontic tooth movement. Kalemaj 2015 reported that there is some evidence that low‐level laser therapy can accelerate orthodontic tooth movement to a limited clinically insignificant degree. The inconsistency can be explained by the difference in the studies included in each review and the quality of evidence: Long 2013 and Gkantidis 2014 included RCTs and controlled clinical trials, while Kalemaj 2015 included RCTs including split‐mouth design.
We decided to only include RCTs in this review. In addition, we excluded split‐mouth design RCTs due to the potential for cross‐over effect, which can potentially influence the assessed outcomes. This explains the difference between our conclusion and the previously mentioned reviews.
Authors' conclusions
Implications for practice.
There is insufficient evidence to conclude whether or not there is a positive effect of non‐surgical adjunctive methods to accelerate tooth movement. Although there have been claims that there may be a positive effect of light vibrational forces, the results of the current studies do not reach either statistical or clinical significance and are at high risk of bias.
Implications for research.
There is a clear need for well‐designed and reported randomised clinical studies of the proposed non‐surgical adjunctive methods to accelerate tooth movement. Due to cross‐over effects, we would recommend that split‐mouth designs are avoided. Future studies need to have sufficient number of participants to detect any clinically and statistically significant differences.
What's new
| Date | Event | Description |
|---|---|---|
| 5 April 2016 | Amended | References to ongoing and excluded studies added |
Acknowledgements
The review authors would like to thank Anne Littlewood (Trials Search Co‐ordinator), Laura MacDonald (Managing Editor) and the Cochrane Oral Health Group for their help and support. We also thank external referees Ross Hobson and Mohammad Owaise Sharif.
Appendices
Appendix 1. Cochrane Oral Health Group Trials Register search strategy
1 (orthodontic*:ti,ab) AND (INREGISTER) 2 (((tooth and move*) or (teeth and move*)):ti,ab) AND (INREGISTER) 3 (#1 or #2) AND (INREGISTER) 4 (laser* :ti,ab) AND (INREGISTER) 5 ((electromagnetic and (energ* or wave* or radiation or pulse* or field*)):ti,ab) AND (INREGISTER) 6 ((electric* and (energ* or pulse* or wave* or current*)) :ti,ab) AND (INREGISTER) 7 (vibrat*:ti,ab) AND (INREGISTER) 8 (#4 or #5 or #6 or #7) AND (INREGISTER) 9 (#3 and #8) AND (INREGISTER)
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 [mh "Orthodontic appliances"] #2 [mh "orthodontics, corrective"] #3 orthodontic* #4 ((tooth near/5 move*) or (teeth near/5 move*)) #5 {or #1‐#4} #6 [mh Lasers] #7 laser* #8 [mh "Electromagnetic radiation"] #9 [mh "Electromagnetic fields"] #10 (electromagnetic near/3 (energ* or wave* or radiation or pulse* or field*)) #11 (electric* near/3 (energ* or pulse* or wave* or current*)) #12 [mh ^Vibration] #13 vibrat* #14 {or #6‐#13} #15 #5 and #14
Appendix 3. MEDLINE (OVID) search strategy
1. exp Orthodontic appliances/ 2. exp Orthodontics, corrective/ 3. orthodontic.ti,ab. 4. ((tooth or teeth) adj5 move$).ti,ab. 5. or/1‐4 6. exp Lasers/ 7. laser$.ti,ab. 8. Electromagnetic radiation/ 9. Electromagnetic fields/ 10. (electromagnetic adj3 (energ$ or wave$ or radiation or pulse$ or field$)).ti,ab. 11. (electric$ adj3 (energ$ or pulse$ or wave$ or current$)).ti,ab. 12. Vibration/ 13. vibrat$.ti,ab. 14. or/6‐13 15. 5 and 14
The above subject search will be linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of theCochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011] (Higgins 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. EMBASE (OVID) search strategy
1. exp Orthodontic device/ 2. exp Orthodontics/ 3. orthodontic$.ti,ab. 4. ((tooth or teeth) adj5 move$).ti,ab. 5. or/1‐4 6. exp Laser/ 7. laser$.ti,ab. 8. Electromagnetic radiation/ 9. Electromagnetic field/ 10. (electromagnetic adj3 (energ$ or wave$ or radiation or pulse$ or field$)).ti,ab. 11. (electric$ adj3 (energ$ or pulse$ or wave$ or current$)).ti,ab. 12. Vibration/ 13. vibrat$.ti,ab. 14. or/6‐13 15. 5 and 14
The above subject search was linked to the Cochrane Oral Health Group filter for identifying RCTs in EMBASE via OVID:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 16. 14 NOT 15
Appendix 5. LILACS (BIREME) search strategy
Mh orthodontics or orthodontic$ or ortodon$ [Words] and Mh laser or laser$ or Mh Electromagnetic radiation or Mh Electromagnetic field or electromagnet$ or Mh Vibration or vibra$ [Words] and
The above subject search was linked to the Brazilian Cochrane Center search strategy for LILACs via BIREME:
((Pt randomized controlled trial OR Pt controlled clinical trial OR Mh randomized controlled trials OR Mh random allocation OR Mh double‐blind method OR Mh single‐blind method) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Pt clinical trial OR Ex E05.318.760.535$ OR (Tw clin$ AND (Tw trial$ OR Tw ensa$ OR Tw estud$ OR Tw experim$ OR Tw investiga$)) OR ((Tw singl$ OR Tw simple$ OR Tw doubl$ OR Tw doble$ OR Tw duplo$ OR Tw trebl$ OR Tw trip$) AND (Tw blind$ OR Tw cego$ OR Tw ciego$ OR Tw mask$ OR Tw mascar$)) OR Mh placebos OR Tw placebo$ OR (Tw random$ OR Tw randon$ OR Tw casual$ OR Tw acaso$ OR Tw azar OR Tw aleator$) OR Mh research design) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Ct comparative study OR Ex E05.337$ OR Mh follow‐up studies OR Mh prospective studies OR Tw control$ OR Tw prospectiv$ OR Tw volunt$ OR Tw volunteer$) AND NOT (Ct animal AND NOT (Ct human and Ct animal))) [Words]
Appendix 6. US National Institutes of Health Trials Register (ClinicalTrials.gov), WHO International Clinical Trials Registry Platform and metaRegister of Controlled Trials search strategy
orthodontic and laser orthodontic and electromagnetic orthodontic and vibration
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Miles 2012.
| Methods | Allocation: Randomised controlled trial Setting: Private practice, Pennsylvania, United States of America Sample size calculation: Calculated as 90% at 0.05 level to detect 20% faster alignment and reduction in irregularity Dropouts: 2 out of 66 participants did not complete the trial. The authors did not mention the reasons |
|
| Participants | 66 participants with fixed orthodontic appliance 0.018 inch bracket slot system
|
|
| Interventions | One Intervention group and one control group. Initial alignment of the lower anterior teeth using 0.018 x 0.025‐inch bracket slot system brackets and 0.014‐inch nickel titanium arch wire for 10 weeks. Intervention: The vibration appliance (Tooth Masseuse), which provided a vibrational frequency of 11 Hz and 0.06N (˜6.1 g), was applied immediately after the initial arch wire was placed, to accelerate the alignment of the mandibular teeth. The participants were instructed to use the vibrational appliance daily for 20 minutes each session. Control: treated with initial arch wire only. |
|
| Outcomes | Primary outcome
Secondary outcome
|
|
| Notes | Several attempts to contact authors with no response (invalid email address) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated in blocks of 6 as mentioned in page 214 "randomly assigned in blocks of six" No mention of how the randomisation was created |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation method |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Clinician and investigator blinded but not the participants as mentioned on page 216: "The clinician was blinded to the study participants at all appointments. Identification numbers were assigned to the models prior to the measurements to ensure blinding". When the participant is not blinded, it can influence the visual analogue scale (VAS) scoring for discomfort, which is scored by the participant. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded during assessment, as mentioned on page 216: "Identification numbers were assigned to the models prior to the measurements to ensure blinding" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of how missing data from participants who dropped out were dealt with, e.g. intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported, although neither P value for statistical testing of data nor the confidence intervals were reported. No protocol published |
| Other bias | Unclear risk | Pain may have occurred in other teeth in the lower or upper arch, which could have resulted in bias. The study appeared to be free of other forms of bias |
Pavlin 2015.
| Methods | Allocation: Randomised Setting: Unknown Sample size calculation: "two‐sided alpha of 0.05, and 80% power, a sample size of 16 subjects per group (total of 32) was required to detect a statistically significant difference between the groups" Intervention model: Parallel assignment with stratification "generated randomization schedule with a block size of 4 and stratified to insure that the number of subjects aged 12–19 years and aged 20–40 years, as well as the number of subjects with“separate canine retraction” versus “en masse retraction” were equally distributed between the groups." Dropouts: 9 out of 45 participants did not complete the trial |
|
| Participants | Age: 12 to 40 years Gender eligible for study: Both Accepts healthy volunteers: No Number of participants: 45 Inclusion criteria
Exclusion criteria
|
|
| Interventions | One intervention group and one control group
|
|
| Outcomes | Primary outcome
Secondary outcome
|
|
| Notes | Study start date February 2009. Completed November 2011. Several attempts to contact authors and the sponsoring company with no response. The study was published as a peer reviewed article in September 2015 (Pavlin 2015). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Described as randomised clinical trial but no details provided "A third‐party vendor provided a computer‐generated randomization schedule with a block size of 4 and stratified to insure that the number of subjects aged 12–19 years and aged 20–40 years, as well as the number of subjects with “separate canine retraction” versus “en masse retraction” were equally distributed between the groups" |
| Allocation concealment (selection bias) | High risk | No mention of allocation method |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participant blinding: intervention and sham device nearly identical Operator blinding: "both the investigators and the subjects remained blinded to treatment" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor blinding: "Masking: Single Blind (Outcomes Assessor)" "The device was programmed to the assigned treatment by independent site personnel and both the investigators and the subjects remained blinded to treatment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis was done. From the data, the authors state the number analysed as N = 45, with a mention of the number of dropouts in each group. |
| Selective reporting (reporting bias) | Low risk | All outcomes outlined in the study registration were reported in the full article. |
| Other bias | High risk | The study was sponsored by OrthoAccel Technologies Inc, which is the manufacturer of the intervention appliance. It was mentioned in the clinicaltrial.gov registration that there was a time limited agreement between the principle investigator and the sponsor to review results before release to public: "There is an agreement between Principal Investigators and the Sponsor that the sponsor can review results communications prior to public release and can embargo communications regarding trial results for a period that is less than or equal to 60 days. The sponsor cannot require changes to the communication and cannot extend the embargo." |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| CTRI/2012/03/002488 | Study protocol evaluated, split‐mouth randomised clinical trial |
| IRCT138804022066N1 | Study protocol evaluated, split‐mouth randomised clinical trial |
| NCT02181439 | Study protocol evaluated, split‐mouth randomised clinical trial |
Characteristics of ongoing studies [ordered by study ID]
JPRN‐UMIN000013722.
| Trial name or title | The effect of vibration on acceleration of orthodontic tooth movement |
| Methods | Cross‐over, randomised, double blind ‐ all involved are blinded |
| Participants | 60 participants with malocclusion having fixed appliance orthodontic treatment |
| Interventions | To reveal the effect of vibration on acceleration of orthodontic tooth movement |
| Outcomes | Tooth movement Velocity of tooth movement Root resorption Evaluation about pain |
| Starting date | 18/04/2014 |
| Contact information | t‐yamamo@m.tohoku.ac.jp |
| Notes | Several attempts to contact authors with no response http://apps.who.int/trialsearch/Trial2.aspx?TrialID=JPRN‐UMIN000013722 |
NCT02119455.
| Trial name or title | Biomarkers of Orthodontic Tooth Movement With Fixed Appliances and Vibration Appliance Therapy |
| Methods | Allocation: Randomised Intervention Model: Parallel Assignment Masking: Single Blind (Outcomes Assessor) Primary Purpose: Treatment |
| Participants | Estimated number: 40 participants Age: 15 to 35 years Both genders Inclusion criteria:
Exclusion criteria:
|
| Interventions | Device: Vibration Device Subjects receiving the OrthoAccel Aura device will be instructed to use the device for 20 minutes/day per the manufacturer's instructions during the study period. The purpose of this study is to identify novel biological factors that are expressed in patients undergoing orthodontic tooth movement in conjunction with vibration appliance therapy and assess the rate of orthodontic alignment of mandibular anterior teeth. |
| Outcomes | Primary Outcome Measures: Changes in the expression of salivary biomarkers of bone remodeling (Time Frame: Up to Week 17 of alignment). Secondary Outcome Measures:
|
| Starting date | April 2014 |
| Contact information | Contact: Flavio A Uribe, DDS, MDentSc furibe@uchc.edu Contact: Taranpreet K Chandhoke, DMD, PhD chandhoke@uchc.edu |
| Notes | Estimated Study Completion Date: September 2016 http://clinicaltrials.gov/show/NCT02119455 April 2014 |
Contributions of authors
Running searches: Cochrane Oral Health Group Identifying relevant titles and abstracts from searches: Ahmed El‐Angbawi (AE), Grant T McIntyre (GM), David R Bearn (DB) Obtaining copies of trials: AE, GM Selection of trials: AE, GM, DB Extracting data from trials: AE, GM Entering data into RevMan: AE Carrying out risk of bias assessment: AE, GM Carrying out analysis: AE, DB Interpreting the data: AE, GM, DB & Padhraig Fleming (PF) Drafting the final review: all review authors
Sources of support
Internal sources
School of Dentistry, The University of Manchester, UK.
External sources
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to the Cochrane Oral Health Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
-
Cochrane Oral Health Group Global Alliance, UK.
Through our Global Alliance (http://ohg.cochrane.org/partnerships‐alliances), the Cochrane Oral Health Group has received support from: British Association for the Study of Community Dentistry, UK; British Association of Oral Surgeons, UK; British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; British Society of Periodontology, UK; Canadian Dental Hygienists Association, Canada; Mayo Clinic, USA; National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Royal College of Surgeons of Edinburgh, UK.
Declarations of interest
There are no financial conflicts of interest; the review authors declare that they do not have any association with any parties who may have vested interests in the results of this review.
Edited (no change to conclusions)
References
References to studies included in this review
Miles 2012 {published data only}
- Miles P, Smith H, Weyant R, Rinchuse DJ. The effects of a vibrational appliance on tooth movement and patient discomfort: a prospective randomised clinical trial. Australian Orthodontic Journal 2012;28(2):213‐8. [PUBMED: 23304970] [PubMed] [Google Scholar]
Pavlin 2015 {published and unpublished data}
- NCT00830947. The OrthoAccel (OATI) Celerect Device Pivotal Study ‐ Effect of cyclic loading (vibration) on orthodontic tooth movement. https://clinicaltrials.gov/ct2/show/NCT00830947 accessed 1 October 2015.
- Pavlin D, Anthony R, Raj V, Gakunga PT. Cyclic loading (vibration) accelerates tooth movement in orthodontic patients: A double‐blind, randomized controlled trial. Seminars in Orthodontics 2015;21(3):187‐94. [Google Scholar]
References to studies excluded from this review
CTRI/2012/03/002488 {published data only}
- CTRI/2012/03/002488. Effects of low intensity laser therapy on the rate of orthodontic tooth movement: a clinical trial. http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=3681 (accessed 22 May 2015). [PMC free article] [PubMed]
IRCT138804022066N1 {published data only}
- IRCT138804022066N1. Evaluation of effect of low level laser on the rate of orthodontic tooth movement in human. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT138804022066N1 (accessed 22 May 2015).
NCT02181439 {published data only}
- NCT02181439. Study evaluating the laser diode effect on the kinetics of orthodontic tooth movement (Protocol CINELASER) (CINELASER). https://clinicaltrials.gov/ct2/show/NCT02181439 (accessed 22 May 2015).
References to ongoing studies
JPRN‐UMIN000013722 {published data only}
- JPRN‐UMIN000013722. The effect of vibration on acceleration of orthodontic tooth movement. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=JPRN‐UMIN000013722 (accessed 22 May 2015).
NCT02119455 {published and unpublished data}
- NCT02119455. Biomarkers of orthodontic tooth movement with fixed appliances and vibration appliance therapy. https://clinicaltrials.gov/ct2/show/NCT02119455 (accessed 22 May 2015). [DOI] [PubMed]
Additional references
Andrews 1972
- Andrews LF. The six keys to normal occlusion. American Journal of Orthodontics 1972;62(3):296‐309. [PUBMED: 4505873] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Dimberg 2015
- Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: A systematic review of quantitative studies. European Journal of Orthodontics 2015;37(3):238‐47. [DOI] [PubMed] [Google Scholar]
Fisher 2010
- Fisher MA, Wenger RM, Hans MG. Pretreatment characteristics associated with orthodontic treatment duration. American Journal of Orthodontics and Dentofacial Orthopedics 2010;137(2):178‐86. [PUBMED: 20152672] [DOI] [PubMed] [Google Scholar]
Germec 2008
- Germec D, Taner TU. Effects of extraction and nonextraction therapy with air‐rotor stripping on facial esthetics in postadolescent borderline patients. American Journal of Orthodontics and Dentofacial Orthopedics 2008;133(4):539‐49. [PUBMED: 18405818] [DOI] [PubMed] [Google Scholar]
Gkantidis 2014
- Gkantidis N, Mistakidis I, Kouskoura T, Pandis N. Effectiveness of non‐conventional methods for accelerated orthodontic tooth movement: a systematic review and meta‐analysis. Journal of Dentistry 2014;42(10):1300‐19. [PUBMED: 25072362] [DOI] [PubMed] [Google Scholar]
GRADEpro 2014 [Computer program]
- GRADE Working Group. GRADEpro [on www.gradepro.org]. Version 3.6. McMaster University, 2014.
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [PUBMED: 12958120] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Kalemaj 2015
- Kalemaj Z, DebernardI CL, Buti J. Efficacy of surgical and non‐surgical interventions on accelerating orthodontic tooth movement: a systematic review. European Journal of Oral Implantology 2015;8(1):9‐24. [PUBMED: 25738176] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Long 2013
- Long H, Pyakurel U, Wang Y, Liao L, Zhou Y, Lai W. Interventions for accelerating orthodontic tooth movement: a systematic review. The Angle Orthodontist 2013;83(1):164‐71. [PUBMED: 22720793] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mavreas 2008
- Mavreas D, Athanasiou AE. Factors affecting the duration of orthodontic treatment: a systematic review. European Journal of Orthodontics 2008;30(4):386‐95. [PUBMED: 18678758] [DOI] [PubMed] [Google Scholar]
Migale 2009
- Migale D, Barbato E, Bossù M, Ferro R, Ottolenghi L. Oral health and malocclusion in 10‐to‐11 years‐old children in southern Italy. European Journal of Paediatric Dentistry 2009;10(1):13‐8. [PUBMED: 19364240] [PubMed] [Google Scholar]
Mtaya 2009
- Mtaya M, Brudvik P, Astrøm AN. Prevalence of malocclusion and its relationship with socio‐demographic factors, dental caries, and oral hygiene in 12‐ to 14‐year‐old Tanzanian schoolchildren. European Journal of Orthodontics 2009;31(5):467‐76. [PUBMED: 19336630] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2014.
Riedmann 1999
- Riedmann T, Georg T, Berg R. Adult patients' view of orthodontic treatment outcome compared to professional assessments. Journal of Orofacial Orthopedics [Fortschritte der Kieferorthopadie] 1999;60(5):308‐20. [PUBMED: 10546414] [DOI] [PubMed] [Google Scholar]
Sebastian 2012
- Sebastian B. Alignment efficiency of superelastic coaxial nickel‐titanium vs superelastic single‐stranded nickel‐titanium in relieving mandibular anterior crowding: a randomized controlled prospective study. The Angle Orthodontist 2012;82(4):703‐8. [PUBMED: 22011096] [DOI] [PMC free article] [PubMed] [Google Scholar]
Segal 2004
- Segal GR, Schiffman PH, Tuncay OC. Meta analysis of the treatment‐related factors of external apical root resorption. Orthodontics and Craniofacial Research 2004;7(2):71‐8. [PUBMED: 15180086] [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Intervention. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Tausche 2004
- Tausche E, Luck O, Harzer W. Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. European Journal of Orthodontics 2004;26(3):237‐44. [PUBMED: 15222706] [DOI] [PubMed] [Google Scholar]
Tortamano 2009
- Tortamano A, Lenzi DC, Haddad AC, Bottino MC, Dominguez GC, Vigorito JW. Low‐level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 2009;136(5):662‐7. [PUBMED: 19892282] [DOI] [PubMed] [Google Scholar]
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision‐making. Evidence‐based Dentistry 2015;16(3):69‐71. [DOI] [PubMed] [Google Scholar]
Zainal 2011
- Zainal Ariffin SH, Yamamoto Z, Zainol Abidin IZ, Megat Abdul Wahab R, Zainal Ariffin Z. Cellular and molecular changes in orthodontic tooth movement. The Scientific World Journal 2011;11:1788‐803. [PUBMED: 22125437] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
El‐Angbawi 2013
- El‐Angbawi A, McIntyre GT, Bearn DR, Fleming PS. Non‐surgical adjunctive interventions for accelerating tooth movement in patients undergoing fixed orthodontic treatment. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD010887] [DOI] [PMC free article] [PubMed] [Google Scholar]


