Abstract
Background
Dislocation of the acromioclavicular joint is one of the most common shoulder problems in general orthopaedic practice. The question of whether surgery should be used remains controversial.
Objectives
To assess the relative effects of surgical versus conservative (non‐surgical) interventions for treating acromioclavicular dislocations in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (to February 2009), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2009, Issue 1), MEDLINE (1966 to February 2009), EMBASE (1988 to February 2009), and LILACS (1982 to February 2009), trial registries and reference lists of articles. There were no restrictions based on language or publication status.
Selection criteria
All randomised and quasi‐randomised trials that compared surgical with conservative treatment of acromioclavicular dislocation in adults were included.
Data collection and analysis
All review authors independently performed study selection. Two authors independently assessed the included trials and performed data extraction.
Main results
Three trials were included in this review. These involved a total of 174 mainly male participants. Two trials were randomised and one was quasi‐randomised. None used validated measures for assessing functional outcome.
Fixation of the acromioclavicular joint using coracoclavicular screws, acromioclavicular pins or, usually threaded, wires was compared with supporting the arm in a sling or similar device. There were no significant differences between the two groups in unsatisfactory longer‐term (one year) shoulder function based on a composite measure including pain, movement and strength or function (risk ratio 1.49, 95% confidence interval 0.75 to 2.95), nor in treatment failure that generally required an operation (risk ratio 1.72, 95% confidence interval 0.72 to 4.12). However, there were fixation failures in all three trials. Particularly, the trial using wires reported a high incidence of wire breakage (16/39 (41%)). Two trials reported that surgery significantly delayed the return to work. The methods used in the three trials also meant a routine second operation for implant removal was necessary.
Authors' conclusions
There is insufficient evidence from randomised controlled trials to determine when surgical treatment is indicated for acromioclavicular dislocation in adults in current practice. Sufficiently powered, good quality, well‐reported randomised trials of currently‐used surgical interventions versus conservative treatment for well‐defined injuries are required.
Keywords: Adult, Female, Humans, Male, Acromioclavicular Joint, Acromioclavicular Joint/injuries, Immobilization, Immobilization/methods, Joint Dislocations, Joint Dislocations/surgery, Joint Dislocations/therapy, Randomized Controlled Trials as Topic, Reoperation
Surgical versus conservative for treatment for acromioclavicular dislocations of shoulder in adults
The acromioclavicular joint is located at the top of the shoulder. It is the joint between the lateral (outer) end of the clavicle (collar bone) and the acromion (a projection from the scapula, or shoulder blade, which is located at the point of the shoulder). Acromioclavicular dislocation is one of the most common shoulder problems treated in general orthopaedic practice.
This review identified three trials, involving 174 mainly male participants. The surgical interventions involved fixation using screws, pins or wires; and conservative treatment involved resting the arm with an arm sling or similar. None of the trials found significant differences between the two groups in shoulder function at one year. However, having surgery delayed the return to work and activities and also required a routine second operation to remove wires and pins. Pooled results on treatment failure, generally requiring an operation, showed no difference between the two groups. However, there were some fixation failures particularly involving the movement and breakage of wires in one trial. There was not enough reliable evidence to draw conclusions about whether or when surgery is more appropriate for acromioclavicular dislocations.
Background
Description of the condition
The acromioclavicular joint is located at the top of the shoulder. It is the joint between the acromion (a process at the top of the scapula or shoulder blade) and the lateral (outer) end of the clavicle (collarbone). The joint is stabilized by a combination of dynamic musculature (the deltoid and trapezius muscles) and static ligamentous (tough fibrous) structures: the latter comprise the joint’s fibrous capsule, the acromioclavicular ligaments (thickenings in the fibrous capsule) and the coracoclavicular ligaments, which connect the coracoid process (another projection from the scapula) to the clavicle (Post 1985).
Acromioclavicular dislocation is one of the most common shoulder problems treated in general orthopaedic practice. It is the most prevalent shoulder injury in participants in contact sports (any sport in which the impact of one person against another is an inherent part of the sport, such as boxing, football, ice hockey and martial arts) (Bishop 2006). Data reveal that acromioclavicular dislocations occur in 41% of collegiate football players and in 40% of (US) National Football League quarterbacks (Kaplan 2005; Kelly 2004). These dislocations are more common in men than in women in the ratio of five to one (Jacobs 1966), perhaps because men are more likely to practise contact sports than women.
The most common mechanism of injury is a direct blow to the top/point of the shoulder, usually from a fall. Less commonly, an indirect trauma may be transmitted up the arm as a result of a fall onto an outstretched hand.
The clinical features of acute acromioclavicular dislocations include pain at the acromioclavicular joint. This does not usually radiate and its severity is often related to the degree of injury. The arm is voluntarily held by the side of the body and some movements are restricted due to pain. Physical examination may show swelling and bruising, an abrasion or a typical deformity, in which the clavicle becomes prominent and there is a depression below it (Bowers 1935).
The injury is more often an incomplete separation rather than a complete separation, in the ratio of two to one (Galatz 2005). Acromioclavicular separations have been described as subluxations when they are partial; and dislocations when complete (Imatani 1975a). Allman 1967 has classified sprains of acromioclavicular joint into grades I, II and III:
Grade I: results from a mild force that causes tearing of only a few fibres of the acromioclavicular ligament and capsule. There is no instability of the joint.
Grade II: is caused by moderate force with rupture of the capsule and acromioclavicular ligament. This injury often causes a subluxation (partial or incomplete dislocation). The coracoclavicular ligaments are not ruptured.
Grade III: results from a severe force that ruptures both the acromioclavicular and coracoclavicular ligaments, producing dislocation of the acromioclavicular joint.
This classification has been widely accepted (Taft 1987). Rockwood (Galatz 2005) identified six types of injury, the first three of which are the same as Allman's grades. The other three types (IV, V, and VI) are all subtypes of Allman's Grade‐III injuries, varying only in the degree and direction of the clavicle displacement (seeTable 2).
Table 1.
Rockwood classification of injury types
| Type | Description |
| Type I | A mild injury involving spraining the acromioclavicular ligaments while leaving the joint intact. |
| Type II | Injury where the acromioclavicular ligaments are torn and acromioclavicular joint is disrupted, while the coracoclavicular ligaments are intact. |
| Type III | Injury involves complete tearing of both the acromioclavicular and coracoclavicular ligaments with 100% dislocation of the joint. |
| Type IV | Injury is a complete acromioclavicular dislocation with posterior displacement of the clavicle through or into the trapezius fascia. |
| Type V | Injury is a complete acromioclavicular dislocation with 100% to 300% superior dislocation of the clavicle. It can involve significant disruption of the deltotrapezial fascia. |
| Type VI | Injury involves inferior displacement of the clavicle into a subacromial or subcoracoid position. |
Description of the intervention
Non‐surgical or conservative treatment generally involves immobilisation of the arm with a sling. Among other methods are braces and strapping. After a short period of immobilisation, lasting around two weeks, gradual mobilisation is started.
Surgical procedures include repositioning of the joint parts and the repair or reconstruction using ligament tissue from other parts of the body (e.g. coracoacromial ligament and semitendinosus, anterior tibialis tendons, or a combination of these) of the various ruptured ligaments. Devices such as the coracoclavicular screw, hook plate, fixation pins and wires could be used. Newer surgical interventions now exist which are currently being adopted, but they have not been tested in randomised clinical trials so far. After surgery, the arm is immobilised in a sling to allow healing to take place followed by gradual mobilisation. Implants such as coracoclavicular screw, hook plate and Kirschner wires require routine removal by further surgery.
How the intervention might work
Grade I and II injuries or acromioclavicular joint subluxations are almost invariably treated conservatively. This review focuses on the more severe injuries, where the joint is dislocated.
Surgical management for acromioclavicular dislocation has been advocated as it enables the restoration of the joint anatomy, thus avoiding the obvious deformity and a potentially unsatisfactory outcome (Rawes 1996). However, disadvantages of surgery include migration of pins used for fixation, erosion of the bone by fixation devices, failure of metallic fixation devices, recurrence of deformity, a painful or unsightly scar, late development of acromioclavicular arthralgia and the necessity of a second operation to remove fixation devices (Galatz 2005; Weaver 1972).
The advantages of the conservative treatment are shorter period of rehabilitation and avoidance of hospitalisation (Bannister 1989a; Larsen 1986; Rawes 1996). Reported disadvantages are that about 20% of patients treated conservatively have unsatisfactory results due to pain, instability and limitation of motion (Kennedy 1954). Moreover, there is an uncertainty regarding healing and the potential need for reconstructive surgery, which is more difficult to perform if the displacement has persisted for a long period (Larsen 1986; Roper 1982).
Why it is important to do this review
Over 35 conservative methods (e.g. sling, Velpeau bandage, strapping) and nearly 30 surgical methods of correction have been identified and advocated for acromioclavicular dislocation. The question of whether surgery should be used remains controversial (Eskola 1987; Lancaster 1987; Phillips 1998; Press 1997; Spencer 2007).
We have identified two systematic reviews focusing on these injuries (Phillips 1998; Spencer 2007). Both reviews, which also included evidence from studies other than from randomised controlled trials, provisionally concluded against the use of surgery for the majority of dislocations but also emphasized the poor evidence base. Our review tests this basic treatment question by applying more rigorous methodology, including restricting the included studies to randomised or quasi‐randomised trials and performing a broader literature search that includes non‐English literature, and through enabling future updates in the light of new evidence.
Objectives
To assess the relative effects of surgical versus conservative (non‐surgical) interventions for treating acromioclavicular dislocations in adults.
Outcome is assessed primarily in terms of function, pain and serious adverse effects of treatment.
Methods
Criteria for considering studies for this review
Types of studies
Any randomised controlled trials and quasi‐randomised trials (that is those in which the allocation is not strictly random: e.g., by date of birth, hospital record number, alternation) comparing surgical with conservative interventions of acromioclavicular dislocation were considered.
Types of participants
We included trials with participants meeting the following criteria:
Skeletally mature (adults greater than 18 years of age);
History of acute (less than three weeks) acromioclavicular dislocation, irrespective of method of diagnosis (usually clinical and imaging evaluations);
No other symptomatic shoulder disorders (e.g. osteoarthritis, shoulder instability, fracture).
Types of interventions
All surgical and conservative interventions used for treating acromioclavicular dislocation were considered.
Surgical interventions include the coracoclavicular screw, reconstruction of coracoclavicular ligaments, acromioclavicular wires and hook plates;
Conservative interventions include immobilisation of the arm in a sling, use of braces and adhesive strapping.
Types of outcome measures
Primary outcomes
Health‐related quality of life;
Pain;
Shoulder function (preferably patient‐reported);
Return to previous activities, including work, sport and activities of daily living;
Treatment failure and other serious adverse effects of treatment such as requirement for a subsequent operation.
Examples of validated patient‐assessed instruments for measuring the first three outcomes are:
Short Form‐36 (SF‐36) (Ware 1992) for health related quality of life;
VAS (visual analogue scale) (Revill 1976) for pain;
Disability of the Arm, Shoulder, and Hand (DASH) Questionnaire (Hudak 1996) for upper‐limb function.
A commonly used instrument for assessing shoulder function is the Constant score (Constant 1987), which is a composite score for shoulder function which includes pain and activities of daily living, and range of movement and strength.
Secondary outcomes
Clinical outcomes
Shoulder range of motion;
Strength;
Cosmetic appearance;
Patient satisfaction with treatment.
Radiological outcomes
Residual deformity (distance between coracoid and clavicle or acromion and clavicle).
Resource use
Hospital admission and length of stay, number of outpatient attendances and other costs of treatment;
Time off work or education.
Safety (success or failure of treatment and adverse events)
Complications:
Early (e.g. wound or skin breakdown or skin necrosis under strapping, fixation failure, migration of wires, residual deformity, infection, requirement for reoperation);
Late (e.g. traumatic arthritis, calcification of coracoclavicular ligament, requirement for reoperation).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (to February 2009), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2009, Issue 1), MEDLINE (1966 to February 2009), EMBASE (1988 to February 2009), and the Latin American and Caribbean Health Sciences database (LILACS) (1982 to February 2009). We also searched the WHO International Clinical Trials Registry Platform Search Portal (to February 2009), Current Controlled Trials (to February 2009), and the UK National Research Register (NRR) Archive (up to September 2007) for ongoing and recently completed trials. There were no restrictions based on language or publication status.
The subject‐specific search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximizing version (Lefebvre 2008), and the SIGN trial search strategy in EMBASE. Search strategies for all databases are shown in Appendix 1.
Searching other resources
We checked reference lists of articles, reviews and textbooks for possible relevant studies. We included the findings from handsearches of abstracts of the British Elbow and Shoulder Society annual meetings (2001 to February 2009), the American Orthopaedic Trauma Association annual meetings (1996 to February 2009) and the American Academy of Orthopaedic Surgeons annual meetings (1996 to February 2009).
Data collection and analysis
Selection of studies
Two authors (MT and ML) independently selected and assessed potentially eligible studies, using a piloted form, for inclusion in the review. Any disagreements were resolved by discussion and when necessary, adjudication by a third author (JB).
Data extraction and management
Two review authors (MT and ML) used a piloted data extraction form to independently collect the data. Any disagreements were resolved by a third review author (JB). Two review authors (MT and ML) entered data into RevMan. Where necessary, we sent requests to trial authors for additional information or data.
Assessment of risk of bias in included studies
Two review authors (MT and ML) independently assessed, without masking of the source or authorship of trial reports, various aspects of methodological quality of the included studies, using a modified version of the Cochrane Bone, Joint and Muscle Trauma Group's former quality assessment tool (Table 3). An impression of the overall risk of bias, based on allocation concealment, blinding and the potential affect of incomplete outcome data, of the individual studies was also made. Disagreements were resolved by a third review author (JB).
Table 2.
Methodological quality assessment scheme
| Items | Scores | Notes |
| 1. Was the assigned treatment adequately concealed prior to allocation? | Yes = method did not allow disclosure of assignment. Unclear = small but possible chance of disclosure of assignment or unclear. No = quasi‐randomised, or open list or tables. | |
| 2. Were the outcomes of participants who withdrew described and included in the analysis (intention‐to‐treat)? | Yes = withdrawals well described and accounted for in analysis. Unclear = withdrawals described and analysis not possible, or probably no withdrawals. No = no mention, inadequate mention, or obvious differences and no adjustment. | |
| 3. Were the outcome assessors blinded to treatment status? | Yes = effective action taken to blind assessors. Unclear = small or moderate chance of unblinding of assessors, or some blinding of outcomes attempted. No = not mentioned or not possible. | |
| 4. Were important baseline characteristics reported and comparable? | Yes = good comparability of groups, or confounding adjusted for in analysis. Unclear = confounding small, mentioned but not adjusted for, or comparability reported in text without confirmatory data. No = large potential for confounding, or not discussed. | Although many characteristics including hand dominance are important, the principal confounders are considered to be age, gender, type of lesion (dislocation or subluxation). |
| 5. Were the trial participants blind to assignment status after allocation? | Yes = effective action taken to blind participants. Unclear = small or moderate chance of unblinding of participants. No = not possible, or not mentioned (unless double‐blind), or possible but not done. | |
| 6. Were the treatment providers blind to assignment status? | Yes = effective action taken to blind treatment providers. Unclear = small or moderate chance of unblinding of treatment providers. No = not possible, or not mentioned (unless double‐blind), or possible but not done. | |
| 7. Were care programmes, other than the trial options, identical? | Yes = care programmes clearly identical. Unclear = clear but trivial differences, or some evidence of comparability. No = not mentioned or clear and important differences in care programmes. | Examples of clinically important differences in other interventions are: time of intervention, duration of intervention, difference in rehabilitation. |
| 8. Were the inclusion and exclusion criteria for entry clearly defined? | Yes = clearly defined (including type of fracture). Unclear = inadequately defined. No = not defined. | |
| 9. Were the outcome measures used clearly defined? | Yes = clearly defined. Unclear = inadequately defined. No = not defined. | |
| 10. Were the accuracy and precision, with consideration of observer variation, of the outcome measures adequate; and were these clinically useful and did they include active follow‐up? | Yes = optimal. Unclear = adequate. No = not defined, not adequate. | |
| 11. Was the timing (e.g. duration of surveillance) clinically appropriate? | Yes = optimal (> 1 year) Unclear = adequate (6 months ‐ 1 year) No = not defined, not adequate (< 6 months) |
Measures of treatment effect
Dichotomous outcome data were analysed as risk ratios (RR) with 95% confidence intervals. When appropriate, we expressed estimate effects as numbers needed to treat (NNTs).
Continuous outcome data were expressed as mean differences with 95% confidence intervals (CI). We intended to pool the data as a mean difference (MD) if two or more studies presented data derived from the same validated instrument of evaluation (with the same units of measure). If primary studies measured the same variables through different instruments (and different units of measure) we intended to use the standardised mean difference (SMD).
Dealing with missing data
With the purpose of including all participants randomised to any intervention we performed intention‐to‐treat analysis. When there was insufficient information relative to estimate effects, such as number of participants, means, measures of uncertainty (standard deviation or error), or number of events and participants, we contacted the main authors of the included trials.
When it was impossible to acquire adequate data for the forest plot (e.g. means and standard deviations), we present data in the text and/or appendices.
Assessment of heterogeneity
The heterogeneity of estimate effects between the included studies was assessed by visual inspection of the forest plot (analysis) along with consideration of the Chi² test for heterogeneity and the I² statistic.
Data synthesis
When considered appropriate, we planned to first pool results of comparable groups of trials using the fixed‐effect model and 95% confidence intervals. However, we intended to consider using the random‐effects model where there was diversity in clinical or methodological characteristics.
Subgroup analysis and investigation of heterogeneity
If data had been available, we had aimed to perform subgroup analyses in order to explore effect size differences in relation to the type of injury (Rockwood classification types) and whether the surgery involved ligament reconstruction or not.
Sensitivity analysis
We planned to perform sensitivity analyses investigating the effects of allocation concealment, the inclusion of studies with a high risk of bias, and of missing data.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
Our search found 171 references (seeFigure 1). Initially, we excluded 165 articles after the screening of titles and abstracts for references. Among these articles, 140 were duplicated citations or not relevant, 20 were excluded because they did not meet the criteria for interventions and five were literature reviews. The remaining six potentially relevant studies were evaluated from full trial reports and one of these studies (Sehmisch 2008) was translated into English (seeAcknowledgements).
Figure 1.

Algorithm of search strategy results
We excluded three studies: two prospective studies (Sehmisch 2008; Sternick 1991) were neither randomised nor quasi‐randomised, and one study (Galpin 1985) was retrospective. The remaining three studies were either randomised or quasi‐randomised controlled trials that reported relevant outcomes (Bannister 1989; Imatani 1975; Larsen 1986). Further details of the included studies can be found in the Characteristics of included studies.
In addition, two ongoing trials were identified from trial registers (Joukainen; McKee).
Included studies
Study designs, participants and interventions of the included studies
The three included trials (Bannister 1989; Imatani 1975; Larsen 1986) involved a total of 174 participants.
Bannister 1989 (Figure 2) was a randomised controlled trial conducted in three hospitals in England. Of the 60 trial participants, 58 were men and two women, with a mean age of 32.5 years. Bannister 1989 compared surgery, involving reduction of the acromioclavicular joint and fixation of the clavicle to the coracoid process with an AO cancellous or malleolar screw and washer, versus conservative treatment where arm was rested in a broad arm sling.
Figure 2.

Participant flow for Bannister 1989
Imatani 1975 (Figure 3) was a quasi‐randomised study, involving 30 participants, conducted in the Naval Regional Medical Center, San Diego, United States. Data for 23 indicated that all were male, aged between 17 and 34 years with a mean age of 27.6 years. The study compared surgery, involving open reduction and internal fixation either by either pins transfixing the acromioclavicular joint or a screw from the clavicle to the coracoid process, versus conservative treatment involving immobilisation in a Velpeau bandage or arm sling.
Figure 3.

Participant flow for Imatani 1975
Larsen 1986 (Figure 4) was a randomised controlled trial conducted in three hospitals in Denmark. Of the 84 participants, 74 were male and 10 female, with a median age of 36 years, and range 19 to 78 years. Surgical treatment involved reduction and transfixation of the acromion and clavicle with two usually threaded two millimetre Kirschner wires that crossed in the joint space. Afterwards, the ends of the acromioclavicular and coracoclavicular ligaments were sutured. The conservative intervention consisted of immobilisation using an arm sling plus a swathe binding the arm to the body.
Figure 4.

Participant flow for Larsen 1986
Outcome measures
Primary outcomes
Pain was evaluated in all studies as part of a non‐validated scoring system; however, Larsen 1986 also assessed pain as present or absent.
Return to previous occupation was evaluated by Bannister 1989 and Larsen 1986.
Treatment failures that generally required a subsequent operation were evaluated in all studies.
Shoulder function (including pain, movement and motion or strength) was evaluated and categorised in all studies using non‐validated scoring systems.
Secondary outcomes
Clinical outcomes were assessed by Bannister 1989 and Larsen 1986. Bannister 1989 evaluated shoulder range of motion and Larsen 1986 reported restriction of range of motion and restriction of strength.
Radiographic assessment was performed by all three trials. This included recording of soft‐tissue calcification.
Complications were reported by all three trials, usually in terms of treatment failure.
Excluded studies
Three studies were excluded following further assessment. For more details, please see the Characteristics of excluded studies.
Ongoing studies
Two ongoing studies were identified (Joukainen; McKee). As far as we can tell, the Joukainen trial is completed but an 18 year follow‐up has been registered. Patient recruitment should finish this year in McKee. Further details of these are given in the Characteristics of ongoing studies.
Risk of bias in included studies
Table 4 shows the individual trial results for each of the 11 items of the Cochrane Bone, Joint and Muscle Trauma Group's former quality assessment tool (Table 3). The first seven items of this tool relate to bias (internal validity), the remaining four items are related to external validity and outcome measurement. Details of the method of randomisation, assessor blinding, intention‐to‐treat analysis/loss to follow‐up, and length of follow‐up are presented in the Characteristics of included studies. A summary of the results and impressions of the likelihood of bias is presented below.
Table 3.
Methodological quality assessment results for individual trials
| Items / Trials | Bannister 1989 | Imatani 1975 | Larsen 1986 |
| 1. Allocation concealment | UNCLEAR | NO | YES |
| 2. Intention‐to‐treat analysis | UNCLEAR | UNCLEAR | YES |
| 3. Assessor blinding | NO | NO | YES |
| 4. Baseline characteristics comparability | UNCLEAR | NO | UNCLEAR |
| 5. Participant blinding | NO | NO | NO |
| 6. Treatment provider blinding | NO | NO | NO |
| 7. Care programme comparability | YES | NO | YES |
| 8. Inclusion and exclusion criteria | NO | UNCLEAR | YES |
| 9. Well defined outcome measures | UNCLEAR | UNCLEAR | YES |
| 10. Clinically useful diagnostic tests | NO | NO | YES |
| 11. Adequate duration of follow‐up | YES | YES | YES |
Allocation (item 1)
Bannister 1989 used random numbers but did not provide details to ascertain whether allocation was concealed. Imatani 1975 was a quasi‐randomised controlled trial, using alternation. Larsen 1986 used a random numbers table and sealed envelopes, which were selected by the patients.
Intention‐to‐treat analysis and handling of withdrawals/losses to follow‐up (item 2)
All three trials described their withdrawals: see the participant flow diagrams in Figure 2, Figure 3 and Figure 4 respectively. None of the trials described outcome data from participants who withdrew from the trial or were lost to follow‐up.
Losses to follow‐up were not rated in the quality assessment tool. This was 10% in Bannister 1989, 23% in Imatani 1975 and 6% in Larsen 1986.
Blinding (items 3, 5 and 6)
Only one trial (Larsen 1986) blinded the outcome assessors at the final follow‐up (item 3). This was achieved by using a small bandage to cover possible scars and each participant was examined by a physician other than the one who had been responsible for the treatment. The blinding of participants (item 5) and care providers (item 6) were not possible due to the type of intervention.
The other two trials (Bannister 1989; Imatani 1975) did not mention whether the outcome evaluation was blinded or not.
Comparability of baseline characteristics (item 4)
Bannister 1989 and Larsen 1986 provided baseline characteristics but only age and gender were specified. Imatani 1975 did not discuss whether baseline characteristics were reported and compared.
Care programmes comparability (item 7)
Bannister 1989 and Larsen 1986 described identical care programmes for rehabilitation for their two intervention groups. Imatani 1975 did not provide sufficient information this item.
External validity
Description of inclusion and exclusion criteria (item 8)
Larsen 1986 and Imatani 1975 were considered to have provided sufficient information of inclusion and exclusion criteria to define their intended study populations. Bannister 1989 did not define the inclusion and exclusion criteria.
Definition and quality of outcome measurement (item 9 and 10)
The variety of outcome measures reported by the trials is evident from inspection of the individual entries in the Characteristics of included studies. Outcome measurement was inadequately defined in Bannister 1989 and Imatani 1975. All three trials used non‐validated overall scoring systems.
Length of follow‐up (item 11)
The length of overall follow‐up was rated as adequate in all included trials.
Summary of overall risk of bias
Altogether, the lack of allocation concealment confirmation, absence of blinding, inadequate treatment of withdrawals, and unclear inclusion and exclusion criteria in Bannister 1989 and Imatani 1975 point to a high risk of bias in these trials. In contrast, particularly given effective allocation concealment and blinding, Larsen 1986 seemed to be at moderate to low risk of bias.
Effects of interventions
The comparison in this review is any surgical intervention versus conservative treatment.
Primary outcomes
Health‐related quality of life
None of the included studies reported a validated health‐related quality of life measure.
Pain
There were no data available for pain using a visual analogue scale or ordinal scale. While, all three studies used a non‐validated score that included pain, the pain component was not reported separately. However, Larsen 1986 assessed pain dichotomously (presence or absence) at final follow‐up and found no statistically significant difference between the two groups in participants with pain (risk ratio (RR) 1.32, 95% confidence interval (CI) 0.54 to 3.19; seeAnalysis 1.1).
Analysis 1.1.

Comparison 1 Surgical intervention versus conservative intervention, Outcome 1 Pain: presence of pain (slight or moderate).
Shoulder function
None of the studies recorded patient‐reported outcome measures of shoulder function. Shoulder function in terms of pain, motion and function or strength was assessed in all three trials; however, non‐validated scores and categorisation were used. Bannister 1989, which used a non‐validated score system based on an 100‐point scale (40 points assigned for pain, 30 for function and 30 for motion), reported that 77% of surgical group participants versus 88% of conservative group participants had either good or excellent results after one year. At four years, 74% of surgical group participants and all conservative group participants had good or excellent results. Imatani 1975, using the same scoring system but with a slightly different categorisation, found 45% of participants in the surgical group versus 58% in the conservative group had good or excellent results after a minimum of one year follow‐up. Larsen 1986, which used another non‐validated score based on a 12‐point scale (4 points assigned for pain, 4 for motion and 4 for strength), found that only one in each group did not have a good or excellent results after 13 months. Pooled data for unsatisfactory outcome (fair or poor) at one year showed no statistically significant difference between surgical and conservative treatment (RR 1.49; 95% CI 0.75 to 2.95; seeAnalysis 1.2)
Analysis 1.2.

Comparison 1 Surgical intervention versus conservative intervention, Outcome 2 Unsatisfactory function (only 'poor' or 'fair' category ) at one year.
Time to return to previous activities
In Bannister 1989, surgically‐treated patients returned to their previous activities consistently later than those managed conservatively. Manual workers treated surgically returned to work after an average of 11 weeks compared with four weeks in those treated conservatively. Clerical workers in the surgery group returned to work in four weeks compared with one week for those in the conservative‐treatment group (reported P < 0.01). The mean time for return practicing sport was 11 weeks; 16 weeks after surgery and seven weeks after conservative treatment (reported P < 0.05).
Larsen 1986 reported that participants treated surgically were off work longer than those treated conservatively (median (range): 8 weeks (2 to 22 weeks) versus 6 weeks (0 to 12 weeks); reported P = 0.067).
Time to return to previous activities was not assessed in Imatani 1975.
Treatment failure
Pooled results from all three trials showed that treatment failure, generally resulting in the need for a subsequent operation, was not statistically significant between the two interventions (11/83 versus 7/91; RR 1.72; 95% CI 0.72 to 4.12; see Analysis 1.3). All treatment failures were excluded from follow‐up analysis in all three trials. In Bannister 1989, reasons for surgical‐treatment failure were screw cut‐out (2 cases), broken screw (1 case), and painful subluxation (2 cases); and reasons for conservative‐treatment failure were painful subluxation (2 cases), unacceptable shoulder weakness (1 case) and unacceptable appearance (1 case). In Imatani 1975, two patients in the surgery group had a surgical complication (screw pull‐out) within the first 48 hours of the operation; neither received a reoperation. Two patients in each treatment group of Larsen 1986 had a subsequent operation due to residual pain, one other surgically‐treated patient had a reoperation to remove broken wires after three weeks and another had a reoperation after four weeks because of lateral migration of the wires. Finally, one conservatively‐treated patient had an operation because of skin problems resulting from a major prominence of the clavicle.
Analysis 1.3.

Comparison 1 Surgical intervention versus conservative intervention, Outcome 3 Treatment failure (usually requiring a subsequent operation).
Secondary outcomes
Clinical outcomes
Bannister 1989 reported that 40% of the surgically‐treated group versus 88% of the conservatively‐treated group had gained a full range of movement after four months, and around 90% of all participants had recovered full power.
Imatani 1975 reported on range of movement or strength only as part of a non‐validated total score.
Larsen 1986 reported no statistically significant differences in restriction of range of movement (3/39 versus 0/40; RR 7.17, 95% CI 0.38 to 134.50; seeAnalysis 1.4) and in restriction of strength (1/39 versus 0/40; RR 3.08, 95% CI 0.13 to 73.27; seeAnalysis 1.4).
Analysis 1.4.
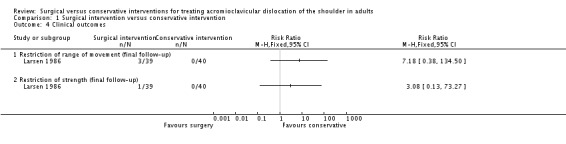
Comparison 1 Surgical intervention versus conservative intervention, Outcome 4 Clinical outcomes.
There were no data pertaining cosmetic appearance or patient satisfaction with treatment in the three trials.
Radiological outcomes
Bannister 1989 reported that in the surgical group, all cases were initially fixed anatomically but that reduction was lost in 35% of participants when the coracoclavicular screw was removed. In conservatively‐treated participants, both acromioclavicular and coracoclavicular separations reduced by 5 mm over first year. The mean reduction of acromioclavicular separation achieved by surgery was 12 mm; 4 mm higher than from conservative management.
Imatani 1975 reported that all participants in the conservative group demonstrated some displacement on the stressed view and two (17%) had no displacement on the unstressed view. There were four (36%) participants treated surgically that had marked calcification; all four had a Bosworth screw procedure.
Larsen 1986 reported calcifications around ligaments which were seen in 69% of participants in the surgical group and 63% in the conservative group. In all except two of the surgically‐treated participants, the correct anatomical position of the clavicle was retained. At final follow‐up, all conservative‐group patients had a displacement of the clavicle between 125 and 150% of its width, but in only four participants (10%) did an application of load cause any increase of this displacement.
All authors found there were no correlations between clinical results and calcification or dislocation.
Resource use
None of the studies reported on the use of resources or costs.
Complications
Direct treatment‐related complications were reported only for the surgical groups of the three trials (seeAnalysis 1.5).
Analysis 1.5.

Comparison 1 Surgical intervention versus conservative intervention, Outcome 5 Treatment‐related complications.
Bannister 1989 reported three participants with surgical complications (11%): in two cases, the coracoclavicular screw cut out of the clavicle and in the third case, the screw broke. Imatani 1975 reported two cases (13%) of screw pull‐out that occurred within 48 hours of surgery. Larsen 1986 reported six cases of superficial infection, five of these being associated with migration of smooth Kirschner wires. Wire breakage, always across the acromioclavicular joint, occurred in 16 cases. Errors in surgical technique were reported as evident in 12 of these cases. Notably, all cases had satisfactory functional results at final follow‐up.
Subgroup analyses
Our plans to study the outcomes in different age groups and for different dislocation types were prevented by the lack of data. Nevertheless, Bannister 1989, using a non‐validated score, reported that for the 12 participants with dislocations with acromioclavicular separation greater than two centimetres, surgery resulted in better functional results (good or excellent: 5/7 (71%) in the surgical group versus 1/5 (20%) in the conservative group).
Discussion
Summary of main results
We included only three controlled trials (two randomised and one quasi‐randomised) that addressed the basic question as to whether surgery is required for acromioclavicular dislocation. These studies were small, involving a total of 174 participants, and different surgical procedures were performed. Furthermore, none of the studies included used validated outcome measures.
The available evidence from three trials comparing surgical versus conservative treatment showed no statistically significant differences between the two groups in final shoulder function, albeit assessed using non‐validated outcome scores, or treatment failure usually defined as requiring an operation. However, two trials found surgically‐treated patients returned to their previous work and other activities consistently later than those managed conservatively. A few cases of screw pull out and breakage of screws occurred in two trials. The third trial, which used wire fixation, reported several cases of superficial infection, wire migration and significantly high numbers of broken wires. A routine second operation was required for implant removal in all three trials.
Overall completeness and applicability of evidence
Our search was developed with the aim of locating all possible relevant trials; it was performed across a list of electronic databases and clinical trials registers. Efforts were made to identify unpublished trials and trials published in non‐English language journals through internet searches and by contacting experts in the field. We included in this review not only randomised controlled trials but also quasi‐randomised controlled trials.
The three included trials did not allow a comprehensive review of the relative effectiveness of surgical or conservative treatment for acromioclavicular dislocation. For the three comparisons for which we found eligible studies, the evidence is not robust due to the risk of bias and the small size of the included studies.
While it was clear that all participants had an acromioclavicular dislocation, none of included trials evaluated participants according to the Rockwood classification (Galatz 2005). This hampers interpretation of the applicability of the evidence.
One major limitation of the review, which significantly affects the applicability of the findings, is that the majority of the current surgical techniques, such as anatomic reconstructions, hook plate and arthroscopic reconstruction, among others, are not covered. The techniques used in the included studies, all of which were conducted over 20 years ago, involve a still commonly used screw to fix the clavicle to the coracoid in two trials; this procedure is technically challenging and loss of fixation due to screw cut out is a well‐recognised complication. In addition, given the high rate of migration and breakage of wires, the use of Kirschner wire fixation as used in the third trial is likely to be far less common. However, there is no conclusive evidence in the literature on what is the best surgical technique for treating grade III acromioclavicular dislocations in adults (Bäthis 2000;Ceccarelli 2008;Hootman 2004;Phillips 1998).
Quality of the evidence
Overall, the available evidence for treating acute acromioclavicular dislocations is of poor quality. Of the three small and underpowered included trials, two (Bannister 1989; Imatani 1975) were at high risk of bias. While Larsen 1986 was at lower risk of bias through the use of an adequate method of randomisation with allocation concealment, and assessor blinding, it was still compromised by inadequate reporting and incorrect analysis. Another deficiency of all three studies was the non use of validated instruments to measure functional outcomes. In part this reflects the lack of such instruments when these trials were conducted. Overall, the findings of all three trials should be interpreted with caution, and be viewed at this stage as requiring confirmation with studies of good methodological quality and adequate power.
Potential biases in the review process
This review was conducted according to the criteria and methods set out in a published protocol. During the process of the review we tried to minimise publication bias; our search strategy was comprehensive and has been maintained properly and regularly updated by the contact author (MJ). It has included the handsearch of conference proceedings and the search for ongoing and recently completed trials. However, we cannot discard the possibility that some studies have been missed. We tried to contact authors of all included trials, but only the authors of one trial responded (Larsen 1986). For this trial, however, the missing data were no longer available.
Agreements and disagreements with other studies or reviews
The results of this review are consistent with those from other published reviews (Bäthis 2000;Ceccarelli 2008;Hootman 2004;Phillips 1998; Spencer 2007). None of these or our review found a clear indication for surgery in terms of evidence of better long‐term function. Although our more extensive search, which included non‐English literature, located no new trials for inclusion at present, we located two ongoing randomised controlled trials that are likely to help inform practice in a future update.
Authors' conclusions
There is insufficient evidence from three small and flawed trials to establish the relative effects of surgical versus conservative treatment on final functional outcome of people with acromioclavicular dislocation. All three trials, however, reported complications from the breakage and migration of implants used for primary fixation across the acromioclavicular joint that sometimes required a further operation additional to the routine surgery needed for implant removal. Surgery was also associated with a longer time off from work and other activities. While these results favour a non‐operative approach, possible benefits of surgery cannot be ruled out including for more complex, high grade injuries. Additionally, the lack of evidence to inform on the use of other and newer surgical approaches should be noted.
Further research exploring the comparison between surgical versus conservative for treating acromioclavicular dislocation is justified. We suggest that:
Consensus on indications for surgical and conservative treatment of acromioclavicular dislocation should be developed to determine the priorities for criteria inclusion for future comparative studies. Then a multi‐centre randomised controlled trial of high quality could be developed to compare the current surgical methods and conservative treatment;
Future trials should be developed using standard and validated outcome measures, including patient assessed functional outcomes, and also assess resource implications;
Comparisons of surgical techniques commonly used nowadays, such as anatomic reconstructions, hook plate, arthroscopic reconstruction, among others, should be tested in randomised controlled clinical trials.
Feedback
Surgical interventions not included in the current version of the review, 18 November 2010
Summary
This review has to be looked at with some caution as it misses some standard methods of reconstruction of the AC joint. For example, the modified Weaver Dunn Procedure is perhaps more effective in displaced AC joint dislocations than non‐surgical option in active patients.
Reply
Many thanks for your interest in our review. Cochrane Reviews report primary research on effectiveness of interventions in human health care, usually, as in this review, limited to randomised controlled trials (RCTs). Our last literature search found only those RCTs on the treatment of acromioclavicular dislocation included in the review. Unfortunately, these do not include any randomised evaluation of the modified Weaver Dunn Procedure. We would appreciate being informed if we have missed any published or ongoing RCTs about which you are aware. It is certainly possible that the results of some techniques mentioned in this review may be inferior to those of newer techniques; future evidence from RCTs which have compared them can be included in updates of the review.
Contributors
Comment from: Tushar Mankad, India Response from: Marcel Jun Sugawara Tamaoki, Corresponding Author, and Bill Gillespie, Feedback Editor, Cochrane Bone, Joint and Muscle Trauma Group
Acknowledgements
We would like to thank James Fraser‐Moodie, Nigel Hanchard, Helen Handoll, Peter Herbison and Janet Wale for their helpful feedback on this review. Thanks too to Lindsey Elstub and Joanne Elliott at the editorial base of the Cochrane Bone, Joint and Muscle Trauma Group for their assistance and support.
Many thanks to Fiona Clay, James Fraser‐Moodie, Helen Handoll and Vicki Livingstone for valuable comments on the protocol.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley InterScience)
#1 MeSH descriptor Acromioclavicular Joint, this term only #2 (acromioclavic* or coracoclavic* or AC joint ):ti,ab,kw #3 (#1 OR #2)
MEDLINE (PubMed)
#1 Acromioclavicular Joint [mh] #2 acromioclavic* [tw] or coracoclavic* [tw] or AC joint [tw] #3 #1 or #2 #4 randomized controlled trial [pt] #5 controlled clinical trial [pt] #6 randomized [tiab] #7 placebo [tiab] #8 clinical trials as topic [mesh: noexp] #9 randomly [tiab] #10 trial [ti] #11 #4 or #5 or #6 or #7 or #8 or #9 or #10 #12 humans [mh] #13 #11 and #12 #14 #3 and #13
EMBASE (Elsevier)
# 1 'Acromioclavicular joint'/ AND [embase]/lim # 2 'Acromioclavicular dislocation'/ AND [embase]/lim # 3 acromioclavic*:ti,ab OR coracoclavic*:ti,ab OR 'ac joint':ti,ab AND [embase]/lim # 4 #1 OR #2 OR #3 # 5 'clinical trial'/ AND [embase]/lim # 6 'randomized controlled trial'/ AND [embase]/lim # 7 randomization/ AND [embase]/lim # 8 'single blind procedure'/ AND [embase]/lim # 9 'double blind procedure'/ AND [embase]/lim # 10 'crossover procedure'/exp AND [embase]/lim # 11 placebo/ AND [embase]/lim # 12 randomi?ed:ti,ab AND [embase]/lim # 13 rct:ti,ab AND [embase]/lim # 14 'random allocation':ti,ab AND [embase]/lim # 15 'allocated randomly':ti,ab AND [embase]/lim # 16 'allocated *2 random':ti,ab AND [embase]/lim # 17 'single blind':ti,ab AND [embase]/lim # 18 'double blind':ti,ab AND [embase]/lim # 19 'treble blind':ti,ab AND [embase]/lim # 20 'triple blind':ti,ab AND [embase]/lim # 21 placebo*:ab,ti AND [embase]/lim # 22 'prospective study'/ AND [embase]/lim # 23 #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 # 24 'case study'/ AND [embase]/lim # 25 'case report':ti,ab AND [embase]/lim # 26 letter/ AND [embase]/lim # 27 #24 OR #25 OR #26 # 28 #23 NOT #27 # 29 #4 AND #28
LILACS (Bireme)
(Mh Acromioclavicular Joint or Tw Acromioclavic$ or Tw coracoclavic$ or Tw AC joint) [Palavras] and ((Pt randomized controlled trial OR Pt controlled clinical trial OR Mh randomized controlled trials OR Mh random allocation OR Mh double‐blind method OR Mh single‐blind method) AND NOT (Ct animals AND NOT (Ct human and Ct animal)) OR (Pt clinical trial OR Ex E05.318.760.535$ OR (Tw clin$ AND (Tw trial$ OR Tw ensa$ OR Tw estud$ OR Tw experim$ OR Tw investiga$)) OR ((Tw singl$ OR Tw simple$ OR Tw doubl$ OR Tw doble$ OR Tw duplo$ OR Tw trebl$ OR Tw trip$) AND (Tw blind$ OR Tw cego$ OR Tw ciego$ OR Tw mask$ OR Tw mascar$)) OR Mh placebos OR Tw placebo$ OR (Tw random$ OR Tw randon$ OR Tw casual$ OR Tw acaso$ OR Tw azar OR Tw aleator$) OR Mh research design) AND NOT (Ct animals AND NOT (Ct human and Ct animals)) OR (Ct comparative study OR Ex E05.337$ OR Mh follow‐up studies OR Mh prospective studies OR Tw control$ OR Tw prospectiv$ OR Tw volunt$ OR Tw volunteer$) AND NOT (Ct animals AND NOT (Ct human and Ct animals))) [Palavras]
Data and analyses
Comparison 1.
Surgical intervention versus conservative intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain: presence of pain (slight or moderate) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Unsatisfactory function (only 'poor' or 'fair' category ) at one year | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.75, 2.95] |
| 2.1 Score included pain, motion and function | 2 | 81 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.76, 3.12] |
| 2.2 Score included pain, motion and strength | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.07, 15.83] |
| 3 Treatment failure (usually requiring a subsequent operation) | 3 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [0.72, 4.12] |
| 4 Clinical outcomes | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Restriction of range of movement (final follow‐up) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable | |
| 4.2 Restriction of strength (final follow‐up) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable | |
| 5 Treatment‐related complications | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Screw pull out or breakage | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable | |
| 5.2 Wire breakage | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable | |
| 5.3 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
What's new
Last assessed as up‐to‐date: 30 April 2009.
| Date | Event | Description |
|---|---|---|
| 1 December 2010 | Feedback has been incorporated | New feedback added. |
History
Protocol first published: Issue 4, 2008 Review first published: Issue 8, 2010
Differences between protocol and review
There were no data available to carry out the subgroup of Rockwood types (Galatz 2005) analyses specified in the protocol.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bannister 1989
| Methods |
Method of randomisation: "A random number was drawn and the patient allocated to operative or conservative management." Assessor blinding: Not mentioned. Participant blinding: Not possible. Intervention provider blinding: Not possible. Intention‐to‐treat analysis: Outcome data for participants who had withdrawn from the trial or were lost to follow‐up were not presented. Loss of follow‐up: 6 participants were lost to follow‐up:
It was not specified to which group they belonged. However, it could be inferred.* |
|
| Participants |
Location: Three hospitals in England, UK participated in the study (Royal Infirmary, Southmead; Frenchay Hospitals, Bristol; and the University Hospital, Nottingham). Period of study: Between 1980 and 1983. Number of participants (N): 60 participants. Inclusion criteria: Patients with acromioclavicular dislocation giving informed consent for participation. Exclusion criteria: Not mentioned. Age: 32.5 years (mean). Gender: 58 male / 2 female. Side: Not specified. Classification of injury: Not specified, just extent of dislocation:
Assigned:
Assessed:
|
|
| Interventions |
Timing of intervention: The operation was performed within 10 days after the injury. Surgical intervention: Through an anterior oblique incision the articular disc was removed. After reduction, the clavicle was fixed to the coracoid process with an AO cancellous or malleolar screw and washer. The coracoclavicular ligaments were not reconstructed. Limb protected in a broad arm sling for two weeks. Screws were removed after 6 weeks. Conservative intervention 1: Two weeks period of rest in a broad arm sling. Rehabilitation: The rehabilitation of two groups was identical, with increasing movement and weight training supervised by physiotherapist. |
|
| Outcomes |
Length of follow‐up: Follow‐up review was after six, 12 and 16 weeks, and then at one and four years. Primary outcomes: 1. Pain, function and movement were assessed using a non‐validated score system based on a 100‐point scale (40 points assigned for pain, 30 for function and 30 for motion). Classified as follows:
2. Return to previous occupation:
3. Treatment failures, including those that required a subsequent operation. Secondary outcomes: 1. Clinical outcomes:
2. Radiological outcomes:
|
|
| Notes | Based on calculations from percentages, it seems likely that at 1 year, 1 person was missing from each group; and at 4 years, 2 people were missing from the surgical treatment group and 4 people from the conservative treatment group. | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | "A random number was drawn and the patient allocated to operative or conservative management." No details provided to ascertain whether allocation was concealed. |
Imatani 1975
| Methods |
Method of randomisation: Alternation. Assessor blinding: Not mentioned. Participant blinding: Not possible. Intervention provider blinding: Not possible. Intention‐to‐treat analysis: Outcome data for participants who had withdrawn from the trial or were lost to follow‐up were not presented. Loss of follow‐up:
|
|
| Participants |
Location: Naval Regional Medical Center, San Diego, California, USA. Period of study: Between June 1972 and May 1973. Number of participants (N): 30 participants. Inclusion criteria:
Exclusion criteria:
Age: Of 23 participants, mean 23.6 years, range 17 to 34 years. Gender: 23 male / 0 female. Side: 15 right / 8 left. Classification of injury: Not specified. Assigned:
Assessed:
|
|
| Interventions |
Timing of intervention: All surgical interventions were performed within 14 days of the injury. Surgical intervention: Open reduction of acromioclavicular joint was performed and the articular disc, if injured, was removed. Internal fixation was either by Steinmann pins transfixing the acromioclavicular joint or by a Bosworth screw from clavicle into the coracoid process. Post operative immobilization was maintained for a minimum of 4 weeks and the internal fixation was removed approximately 12 weeks after surgery). Conservative intervention: Immobilisation using a Velpeau bandage or arm sling for minimum of three weeks. Rehabilitation: Not mentioned. |
|
| Outcomes |
Length of follow‐up: Participants were followed for a minimum of 12 months. Primary outcomes: 1. Pain, function and movement were assessed using a non‐validated score system based on a 100‐point scale (40 points assigned for pain, 30 for function and 30 for motion). Classified as follows:
satisfactory = excellent or good; unsatisfactory = fair and poor 2. Treatment failures; including those that required a subsequent operation. Secondary outcomes: 1.Radiological outcomes:
|
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | No | Quasi‐randomised with no allocation concealment. |
Larsen 1986
| Methods |
Method of randomisation: A random numbers table was used to generate slips enclosed in sealed envelopes that were chosen by the patients. Assessor blinding: At final follow‐up, a small bandage was used to cover the area including any scar. Each participant was then examined by a physician other than the one who had been responsible for their treatment. Participant blinding: Not possible. Intervention provider blinding: Not possible. Intention‐to‐treat analysis: none, but outcome data for participants who had been withdrawn from the trial analysis were not presented. Loss of follow‐up: 5 participants were not included in the final follow‐up (needed re‐operation):
|
|
| Participants |
Location: Three hospitals in Copenhagen, Denmark participated in the study (Gentofte Hospital, Hvidovre Hospital, Bispebjerg Hospital). Period of study: Between 1979 and 1983. Number of participants (N): 84 participants. Inclusion criteria:
Exclusion criteria:
Age:
Gender:
Side: Total of participants:45 right / 39 left. Classification of injury: Not specified. Assigned:
Assessed:
|
|
| Interventions |
Timing of intervention: All participants were treated up to four days after the diagnosis. Surgical intervention: Modified Phemister procedure was used as standard operation. The articular disc was removed, the acromioclavicular joint was reduced, and the bones were transfixed with two, usually threaded, 2 mm Kirschner wires that crossed in the joint space. The ends of the acromioclavicular and coracoclavicular ligaments were then sutured. The Kirschner wires were removed under local anaesthesia after five to 12 weeks. Postoperatively, a sling plus a swathe binding the arm to the body was worn for two weeks, and then just a sling supporting the arm was used for a further two weeks Conservative intervention: A sling plus a swathe binding the arm to the body. This was worn for two weeks, and then just a sling supporting the arm was used for a further two weeks Rehabilitation: The rehabilitation was same in both groups: one month after injury physiotherapy was instituted, allowing free movement of the arm but no loading of extremity. After six weeks there was no restriction in using the arm. |
|
| Outcomes |
Length of follow‐up: Participants were seen for follow‐up evaluation at three weeks, six weeks, three months, and an average of 13 months (range, 12 to 14 months) after injury. Primary outcomes: 1. Pain, movement and strength were assessed using a non‐validated score system based on a 12 point scale (4 points assigned for pain, 4 for motion and 4 for strength). Classified as follows:
2. Pain (presence or absence) 3. Return to previous occupation 4. Treatment failures, including those that required a subsequent operation Secondary outcomes: 1. Clinical outcomes:
2. Radiological outcomes:
2. Complications:
|
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | Use of random numbers table and sealed envelopes that were chosen by the patient |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Galpin 1985 | Not a randomised or quasi‐randomised controlled trial. |
| Sehmisch 2008 | Not a randomised or quasi‐randomised controlled trial. |
| Sternick 1991 | Not a randomised or quasi‐randomised controlled trial. |
Characteristics of ongoing studies [ordered by study ID]
Joukainen
| Trial name or title | A prospective, randomised long‐term follow‐up of operative versus non‐operative treatment of grade 3 acromioclavicular dislocation. |
| Methods |
Method of randomisation: Not available yet. Assessor blinding: Not available yet. Intention‐to‐treat analysis: Not available yet. |
| Participants |
Location: Finland. Number of participants (N): 39 Inclusion criteria:
Exclusion criteria: No written informed consent |
| Interventions |
1. Surgical group: The surgical treatment was accomplished within two days after the injury. It consisted of an open reduction and fixation of the acromioclavicular joint with two smooth Kirschner wires (2 mm in diameter) across the acromioclavicular joint. The K‐wires were bent at the proximal ends, with suturing of the superior acromioclavicular ligament. The position of Kirschner wires was confirmed during the operation using C‐arm transillumination. The articular disc of acromioclavicular joint was removed if it was damaged. Postoperative care consisted of immobilisation of the acromioclavicular joint in a sling (Polysling, body band) for four weeks. Mobilisation of the shoulder started four to six weeks later in a similar manner as in the non‐operative group. 2. Non‐surgical group Non‐surgical treatment consisted of immobilisation of the injured acromioclavicular joint in a Kenny‐Howard‐type splint for four weeks. The patient was encouraged in mobilisation of the elbow several times per day and the mobilisation of the shoulder with pendulum type movements were initiated four weeks after the injury. Active mobilisation of the shoulder was allowed six weeks after the injury. |
| Outcomes |
Length of follow‐up: 18 years 4 months (final data collection date for primary outcome measure) Primary outcome Presence of delayed surgical procedure to treat the acromioclavicular joint dislocation pathology Secondary outcome
Other pathologic findings of the shoulder in the clinical examination and the description of it |
| Starting date | Study start date: February 2009 Estimated study completion date: August 2009 |
| Contact information | Contact: Antti Joukainen, MD +358447174703 antti.joukainen@kuh.fi Contact: Marja‐Liisa Sutinen, RN +358447113941 marja‐liisa.sutinen@kuh.fi |
| Notes |
McKee
| Trial name or title | Non‐operative versus operative treatment of acute acromioclavicular joint dislocation (AC joint) |
| Methods |
Method of randomisation: Not available yet. Assessor blinding: Not available yet. Intention‐to‐treat analysis: Not available yet. |
| Participants |
Location: Toronto, Canada. Number of participants (N): 122. Inclusion criteria: 1. Men or women aged 16 to 65 years of age 2. Grade III (3), IV (4) or V (5) dislocation of the acromioclavicular joint (evidenced by no contact between the distal clavicle and the acromion as seen in standardized radiographs) 3. Closed injury 4. Acromioclavicular joint dislocations within 28 days post injury 5. Provision of informed consent Exclusion criteria: 1. Grade I(1), II (2), or VI (6) subluxation/dislocation of the acromioclavicular joint 2. Open acromioclavicular joint separation 3. Scapulothoracic dissociation 4. Presence of vascular injury 5. Dislocations over 28 days post‐injury 6. Limited life expectancy due to significant medical co‐morbidity 7. Medical contraindication to surgery (including pregnancy) 8. Inability to comply with rehabilitation or form completion 9. Inability to provide informed consent 10. Likely problems, in the judgement of the investigators, with maintaining follow‐up (i.e. patients with no fixed address, patients not mentally competent to give consent, etc) |
| Interventions |
Surgical intervention: Procedure: open reduction internal fixation of acromioclavicular joint dislocation Definitive surgical treatment (i.e. open reduction and internal fixation) will be performed within 28 days of the injury. In all cases the procedure will be performed by an orthopaedic staff surgeon with the assistance of a fellow/resident(s). The operating surgeon will determine the positioning of the patient for surgery. Open reduction and internal fixation of the acromioclavicular joint dislocation will be carried out as follows:
Conservative intervention: Non operative treatment of acromioclavicular joint dislocation (sling). Standard protocol for conservative treatment will consist of the implementation of a sling, for shoulder support and patient comfort, for four weeks followed by physiotherapy. Pendulum exercises may be implemented at any time as dictated by the attending surgeon. |
| Outcomes |
Length of follow‐up: 2 years Primary outcome
Secondary outcome
|
| Starting date | Study start date: January 2008 Estimated study completion date: January 2010 |
| Contact information | Contact: Milena Vicente, R.N. 416‐864‐6060 ext 2608 vicentem@smh.toronto.on.ca Contact: Ryan Khan, B.A. 416‐864‐6060 ext 3890 khanry@smh.toronto.on.ca |
| Notes |
Contributions of authors
The first drafts of this review were prepared by MT, ML and JB. The search strategy, in liaison with the Trials Search Co‐ordinator (Joanne Elliott), was developed by MT and ML. MT wrote to the study authors for additional information and entered data into RevMan. MT and ML performed screening of search results, assessed methodological quality, extracted, analysed and interpreted the data. All authors commented on and approved the final version of the review.
Sources of support
Internal sources
Universidade Federal de São Paulo, Brazil.
External sources
No sources of support supplied
Declarations of interest
None known.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
- Bannister GC, Wallace WA, Stableforth PG, Hutson MA. The management of acute acromioclavicular dislocation. A randomised prospective controlled trial. Journal of Bone & Joint Surgery ‐ British Volume 1989;71(5):848‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Imatani RJ, Hanlon JJ, Cady GW. Acute, complete acromioclavicular separation. Journal of Bone & Joint Surgery ‐ American Volume 1975;57(3):328‐32. [MEDLINE: ] [PubMed] [Google Scholar]
- Larsen E, Bjerg‐Nielsen A, Christensen P. Conservative or surgical treatment of acromioclavicular dislocation. A prospective, controlled, randomized study. Journal of Bone & Joint Surgery ‐ American Volume 1986;68(4):552‐5. [MEDLINE: ] [PubMed] [Google Scholar]
References to studies excluded from this review
- Galpin RD, Hawkins RJ, Grainger RW. A comparative analysis of operative versus nonoperative treatment of Grade III acromioclavicular separations. Clinical Orthopaedics & Related Research 1985;(193):150‐5. [PubMed] [Google Scholar]
- Sehmisch S, Stürmer EK, Zabka K, Losch A, Brunner U, Stürmer KM, et al. Results of a prospective multicenter trial for treatment of acromioclavicular dislocation [Ergebnisse einer prospektiven Multicenterstudie zur Behandlung der Schultereckgelenksprengung]. Sportverletz Sportschaden 2008;22(3):139‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Sternick MB, Farias Filho OC, Carvalho MI. Acromioclavicular dislocation: prospective study [Luxaçäo acromioclavicular: estudo prospectivo]. Revista Brasileira de Ortopedia 1991;26(9):308‐12. [Google Scholar]
References to ongoing studies
- Joukainen A. A prospective, randomised long‐term follow‐up of operative versus non‐operative treatment of Gr. 3 acromioclavicular dislocation. clinicaltrials.gov/ct2/show/NCT00840593 (accessed 24 November 2009). [: ClinicalTrials.gov ID: NCT00840593]
- McKee MD, Schemitsch EH. Non‐operative versus operative treatment of acute acromioclavicular joint dislocation (ACJoint). clinicaltrials.gov/ct2/show/NCT00594841 (accessed 24 November 2009). [: ClinicalTrials.gov ID: NCT00594841]
Additional references
- Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulation. Journal of Bone & Joint Surgery ‐ American Volume 1967;49(4):774‐84. [PubMed] [Google Scholar]
- Bannister GC, Wallace WA, Stableforth PG, Hutson MA. The management of acute acromioclavicular dislocation. A randomised prospective controlled trial. Journal of Bone & Joint Surgery ‐ British Volume 1989;71(5):848‐50. [DOI] [PubMed] [Google Scholar]
- Bishop JY, Kaeding C. Treatment of the acute traumatic acromioclavicular separation. Sports Medicine & Arthroscopy Review 2006;14(4):237‐45. [DOI] [PubMed] [Google Scholar]
- Bowers RF. Complete acromioclavicular separation: Diagnoses and operative treatment. Journal of Bone & Joint Surgery ‐ American Volume 1935;17(4):1005‐10. [Google Scholar]
- Bäthis H, Tingart M, Bouillon B, Tiling T. Conservative or surgical therapy of acromioclavicular joint injury‐‐what is reliable? A systematic analysis of the literature using "evidence‐based medicine" criteria [Konservative oder operative Therapie der Schultereckgelenkverletzung – was ist gesichert ? Eine systematische Literaturanalyse nach Kriterien der "evidence based medicine"]. Der Chirurg 2000;71(9):1082‐9. [DOI] [PubMed] [Google Scholar]
- Ceccarelli E, Bondì R, Alviti F, Garofalo R, Miulli F, Padua R. Treatment of acute grade III acromioclavicular dislocation: a lack of evidence. Journal of Orthopaedics and Traumatology 2008;9(2):105‐8. [EMBASE: 2008276470] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical Orthopaedics & Related Research 1987;(214):160‐4. [PubMed] [Google Scholar]
- Eskola A, Vainionpää S, Korkala O, Rokkanen P. Acute complete acromioclavicular dislocation. A prospective randomized trial of fixation with smooth or threaded Kirschner wires or cortical screw. Annales Chirurgiae et Gynaecologiae 1987;76(6):323‐6. [PubMed] [Google Scholar]
- Galatz LM, Williams GR Jr. Acromioclavicular Joint Injuries. In: Bucholz RW, Heckman JD, Court‐Brown CM editor(s). Rockwood & Green's Fractures in Adults. 6th Edition. Vol. 2, Philadelphia: Lippincott Williams & Wilkins, 2005:1332‐64. [Google Scholar]
- Hootman JM. Acromioclavicular dislocation: conservative or surgical therapy. Journal of Athletic Training 2004;39(1):10‐1. [EMBASE: 2004166822] [PMC free article] [PubMed] [Google Scholar]
- Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). American Journal of Industrial Medicine 1996;29(6):602‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Imatani RJ, Hanlon JJ, Cady GW. Acute, complete acromioclavicular separation. Journal of Bone & Joint Surgery ‐ American Volume 1975;57(3):328‐32. [MEDLINE: ] [PubMed] [Google Scholar]
- Jacobs B, Wade PA. Acromioclavicular‐joint injury. An end‐result study. Journal of Bone & Joint Surgery ‐ American Volume 1966;48(3):475‐86. [MEDLINE: ] [PubMed] [Google Scholar]
- Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. American Journal of Sports Medicine 2005;33(8):1142‐6. [DOI] [PubMed] [Google Scholar]
- Kelly BT, Barnes RP, Powell JW, Warren RF. Shoulder injuries to quarterbacks in the national football league. American Journal of Sports Medicine 2004;32(2):328‐31. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Kennedy JC, Cameron H. Complete dislocation of the acromio‐clavicular joint. Journal of Bone & Joint Surgery ‐ British Volume 1954;36(2):202‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Lancaster S, Horowitz M, Alonso J. Complete acromioclavicular separations. A comparison of operative methods. Clinical Orthopaedics & Related Research 1987;(216):80‐8. [PubMed] [Google Scholar]
- Larsen E, Bjerg‐Nielsen A, Christensen P. Conservative or surgical treatment of acromioclavicular dislocation. A prospective, controlled, randomized study. Journal of Bone & Joint Surgery ‐ American Volume 1986;68(4):552‐5. [PubMed] [Google Scholar]
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. Box 6.4.b. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 (updated February 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
- Phillips AM, Smart C, Groom AF. Acromioclavicular dislocation. Conservative or surgical therapy. Clinical Orthopaedics & Related Research 1998;(353):10‐7. [MEDLINE: ] [PubMed] [Google Scholar]
- Post M. Current concepts in the diagnosis and management of acromioclavicular dislocations. Clinical Orthopaedics & Related Research 1985;(200):234‐47. [PubMed] [Google Scholar]
- Press J, Zuckerman JD, Gallagher M, Cuomo F. Treatment of grade III acromioclavicular separations. Operative versus nonoperative management. Bulletin of the Hospital for Joint Diseases 1997;56(2):77‐83. [PubMed] [Google Scholar]
- Rawes ML, Dias JJ. Long‐term results of conservative treatment for acromioclavicular dislocation. Journal of Bone & Joint Surgery ‐ British Volume 1996;78(3):410‐2. [PubMed] [Google Scholar]
- Revill SI, Robinson JO, Rosen M, Hogg MI. The reliability of a linear analogue for evaluating pain. Anaesthesia 1976;31(9):1191‐8. [DOI] [PubMed] [Google Scholar]
- Roper BA, Levack B. The surgical treatment of acromioclavicular dislocations. Journal of Bone & Joint Surgery ‐ British Volume 1982;64(5):597‐9. [DOI] [PubMed] [Google Scholar]
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clinical Orthopaedics & Related Research 2007;(455):38‐44. [DOI] [PubMed] [Google Scholar]
- Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint. An end‐result study. Journal of Bone & Joint Surgery ‐ American Volume 1987;69(7):1045‐51. [PubMed] [Google Scholar]
- Ware JE Jr, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Medical Care 1992;30(6):473‐83. [PubMed] [Google Scholar]
- Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. Journal of Bone & Joint Surgery ‐ American Volume 1972;54(6):1187‐94. [PubMed] [Google Scholar]


