Abstract
Background
Inspiratory muscle weakness has been observed in patients with stroke. Inspiratory muscle training is an intervention that has shown possible effects for functional recovery of patients with stroke.
Objectives
To investigate the effect and safety of inspiratory muscle training for improving activities of daily living, respiratory muscle function, quality of life and cardiorespiratory fitness after stroke.
Search methods
We searched the Cochrane Stroke Group's Trials Register (August 2011), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2011, October Issue 4), MEDLINE (1948 to October 2011), EMBASE (1974 to October 2011), CINAHL (1982 to October 2011), AMED (1985 to October 2011), PEDro (October 2011) and four Chinese databases. In an effort to identify further published, unpublished and ongoing trials, we searched ongoing trials registers and conference proceedings, checked reference lists, and contacted authors of relevant studies and training devices manufactures. There were no language restrictions.
Selection criteria
Randomised controlled trials (RCTs) comparing inspiratory muscle training with no intervention, sham inspiratory muscle training or other cardiorespiratory training for patients with stroke were eligible.
Data collection and analysis
Two review authors independently assessed trial quality and extracted data. The primary outcomes were activities of daily living and respiratory muscle strength; the secondary outcomes were quality of life, cardiorespiratory fitness and adverse effects.
Main results
We included two trials involving a total of 66 patients in this review. Pooling analyses of data was not possible due to considerable heterogeneity between the trials and a lack of data in both trials. One study found a significant increase in respiratory muscle strength favouring inspiratory muscle training over sham inspiratory muscle training, but there was no significant difference between groups on quality of life. The other study showed that patients receiving inspiratory muscle training were more likely to improve their activities of daily living, quality of life and cardiorespiratory fitness than those patients who received no intervention. However, the main results were not compared directly with breathing retraining. Furthermore, neither of the trials assessed the safety and tolerance of inspiratory muscle training.
Authors' conclusions
There is insufficient evidence to support inspiratory muscle training as an effective treatment to improve function after stroke, and no evidence relating to the safety of inspiratory muscle training. Further well‐designed RCTs are required.
Keywords: Humans, Breathing Exercises, Breathing Exercises/adverse effects, Stroke Rehabilitation, Diaphragm, Diaphragm/physiology, Inhalation, Inhalation/physiology, Muscle Strength, Muscle Strength/physiology, Physical Endurance, Physical Endurance/physiology, Randomized Controlled Trials as Topic, Recovery of Function, Recovery of Function/physiology, Respiratory Muscles, Respiratory Muscles/physiology, Stroke, Stroke/complications
Plain language summary
Inspiratory muscle training for the recovery of function after stroke
Inspiratory muscle training involves the training of specific muscles including diaphragmatic muscles and external intercostal muscles. When these muscles contract, they act to increase the volume of the thoracic cavity, which forces air into the lungs. Routine training of inspiratory muscles is performed using a training device that gives the participants an inhale resistance set according to their endurance or maximal inspiratory pressure during inspiration. Inspiratory muscle training aimed to improve the strength and endurance of the inspiratory muscles, which has shown possible effects for functional recovery after stroke.
The authors found two small heterogeneous randomised trials that investigated the effect of inspiratory muscle training. These studies do not provide enough evidence to draw any conclusions about the effect of inspiratory muscle training for patients with stroke. There is also no evidence relating to the safety of inspiratory muscle training. Future well‐designed studies are needed.
Background
Description of the condition
Stroke is one of the most common causes of morbidity and long‐term disability in the world (AHA 2011; ESO 2008). Approximately 795,000 people in the US experience a new or recurrent stroke each year, of which about 610,000 are first attacks, and it is estimated that around 6.4 million Americans are stroke survivors (AHA/ASA 2011). Only 50% to 70% of survivors make a good functional recovery, while 15% to 30% of survivors are permanently disabled at 3 months after their stroke onset (AHA 2011). At present, no single standard intervention has been identified that is effective for the recovery of function after stroke, which leaves a large number of stroke patients needing assistance from other people for activities of daily living (ADL) (Brown 2010). Therefore, functional recovery after stroke is a high priority for healthcare (Brown 2010; McArthur 2011).
Reduced respiratory muscle strength has been observed in patients suffering from stroke but little attention has been paid to it, possibly because it is often not associated with any obvious symptoms (Annoni 1990; Roth 1994; Similowski 1996; Teixeira‐Salmela 2005; Ward 2010). Generally, respiratory muscle weakness is attributed to the impairment of the muscles involved in respiration, induced by the lesions of the central nervous system (Jandt 2010).
Description of the intervention
Inspiratory muscle training involves the training of inspiratory muscles aimed to improve their strength and endurance, which are being measured by maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP). The main inspiratory muscles are diaphragmatic muscles and external intercostal muscles. When these muscles contract, they act to increase the volume of the thoracic cavity, which forces air into the lungs. Generally, a routine training regimen of inspiratory muscles is performed using a training device that gives the participants an inhale resistance set according to their endurance or MIP during inspiration. Specific training devices mainly include threshold or resistive trainers (Reid 2004).
The threshold trainer has a one‐way spring‐loaded valve that closes during inspiration and requires the participants to inhale hard enough to open the valve and let the air enter. This device provides constant pressure for inspiratory muscle training, regardless of how quickly or slowly participants breathe, and the optimal loading pressure can be adjusted based on the characteristics of individual participants. Resistive trainers also have a one‐way valve that opens during exhalation without any outside force in this phase. The loading pressure of this device is imposed when the participants breathe through a narrow hole; this makes it very difficult to maintain a constant pressure and gives the participants the opportunity to lower the inspiratory resistance themselves by simply breathing slowly. Potential adverse events related to inspiratory muscle training, including pneumothorax, respiratory muscle pains and respiratory tract injuries, have rarely been reported (Houston 2008).
How the intervention might work
The exact mechanism of how inspiratory muscle training may improve recovery is still unclear. In healthy individuals, inspiratory muscle training has been reported to improve the exercise capacity and strength of inspiratory muscles as reflected by the increases of peak oxygen uptake and MIP (Sheel 2002). However, studies have shown decreases in respiratory muscle strength and endurance in patients after stroke (Annoni 1990; Roth 1994; Similowski 1996; Teixeira‐Salmela 2005; Ward 2010). Teixeira‐Salmela et al found a reduction in the strength of respiratory muscles in community‐dwelling stroke survivors when compared with age‐matched healthy people (Teixeira‐Salmela 2005). In addition, it has been suggested that lower respiratory strength increases the risk of stroke (Van der Palen 2004). Accordingly, increased respiratory muscle strength due to breathing against resistance support specific respiratory muscle training might be a potential therapeutic resource for stroke rehabilitation.
Why it is important to do this review
Inspiratory muscle training has shown possible benefits in improving ADL, quality of life, inspiratory muscle strength and endurance, exercise capacity and dyspnoea in numerous illnesses, including disease such as cystic fibrosis (Enright 2004), chronic obstructive pulmonary disease (COPD) (Reid 1995), heart failure (Dall'Ago 2006), Parkinson's disease (Inzelberg 2005), myasthenia gravis (Fregonezi 2005) and multiple sclerosis (Fry 2007). In addition, recent preliminary clinical studies (Britto 2011; Sutbeyaz 2010) have indicated that inspiratory muscle training might have the potential to improve ADL, respiratory muscle function, quality of life and walking ability, as well as cardiorespiratory fitness, in patients who have had a stroke. Therefore, a systematic review focusing on investigating the use of inspiratory muscle training for improving recovery of function after stroke, summarising evidence about efficacy and safety from randomised controlled trials (RCTs), was needed.
Objectives
To investigate the effect and safety of inspiratory muscle training for improving ADL, respiratory muscle function, quality of life and cardiorespiratory fitness after stroke.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs or randomised cross‐over studies.
Types of participants
We included participants regardless of age, gender and severity of disease after stroke. The definition of stroke was according to the World Health Organization (WHO) criteria (Hatano 1976), confirmed by computerised tomography (CT) or magnetic resonance imaging (MRI). We excluded patients with comorbidities of respiratory system disease (e.g. COPD, asthma, cystic fibrosis), cardiac disease (e.g. chronic heart failure) or other diseases leading to the impairment of respiratory muscle (e.g. myasthenia gravis).
Types of interventions
We assessed inspiratory muscle training for stroke patients regardless of the inspiratory muscle training type (e.g. threshold trainer, resistive trainer), frequency or duration. The comparisons were no intervention, sham inspiratory muscle training or another cardiorespiratory training intervention. Inspiratory muscle training is defined as a technique that trains the muscles involved in inhalation in order to improve respiratory function.
The following comparisons were eligible for inclusion:
inspiratory muscle training versus no intervention;
inspiratory muscle training versus sham inspiratory muscle training;
inspiratory muscle training versus other cardiorespiratory training;
inspiratory muscle training in combination with other cardiorespiratory training versus the same cardiorespiratory training of the treated group.
Types of outcome measures
Primary outcomes
ADL, measured using scales as follows: the Barthel index (BI), Functional Independence Measure (FIM), modified Rankin Scale (mRS), Global Dependency Scale, Katz Index of Activities of Daily Living and Rehabilitation Activities Profile.
Respiratory muscle strength, measured by MIP and MEP.
Secondary outcomes
Quality of life, measured using Short Form 36 (SF‐36).
Cardiorespiratory fitness, measured by peak oxygen consumption (VO2peak).
Adverse effects.
Search methods for identification of studies
See the 'Specialized register' section of the Cochrane Stroke Group module. We searched for relevant trials in all languages and arranged translation of relevant papers published in languages other than English.
Electronic searches
We searched the Cochrane Stroke Group Trials Register, which was last searched in August 2011. In addition we searched the following electronic bibliographic databases:
the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2011, October Issue 4) (Appendix 1);
MEDLINE (1948 to 10 October 2011) (Appendix 2);
EMBASE (1974 to 10 October 2011) (Appendix 3);
CINAHL (1982 to 18 October 2011) (Appendix 4);
AMED (1985 to 18 October 2011) (Appendix 5);
PEDro (Physiotherapy Evidence Database) (www.pedro.org.au/) (18 October 2011) ;
China Biological Medicine Database (CBM‐disc) (last searched 10 October 2011);
Chinese National Knowledge Infrastructure Database (CNKI) (www.cnki.net) (last searched 10 October 2011);
VIP Chinese Science and Technique Journals Database (last searched 10 October 2011).
The Cochrane Stroke Group Trials Search Co‐ordinator developed the search strategies for MEDLINE, CINAHL and AMED and we adapted the MEDLINE search strategy for the other databases.
We also searched the following ongoing trials registers (10 October 2011):
Stroke Trials Registry (www.strokecenter.org/trials/);
ClinicalTrials.gov (http://clinicaltrials.gov/);
Current Controlled Trials (www.controlled‐trials.com);
Chinese Clinical Trial Registry (http://www.chictr.org);
Wanfang Data (www.wanfangdata.com).
Searching other resources
In an effort to identify further published, unpublished and ongoing trials, we:
-
searched the following conference proceedings:
1st and 2nd National Stroke Rehabilitation Conference (2007 and 2008);
4th, 5th and 6th World Congress of NeuroRehabilitation (2006, 2008 and 2010);
screened reference lists of all included studies;
contacted authors of included studies;
contacted Philips Respironics, Inc., the manufacturer of inspiratory muscle training devices;
used Science Citation Index Cited Reference Search for forward tracking of relevant trials.
Data collection and analysis
Selection of studies
Two review authors independently read the titles and abstracts of all records identified by the searches of the electronic databases and excluded obviously irrelevant articles. We obtained the full text of the remaining articles, and the same two review authors independently evaluated each paper for inclusion. We resolved any disagreements by discussion with all review authors. We recorded details of the excluded studies and the reasons for exclusion.
Data extraction and management
Two authors independently extracted the following information using a data extraction form.
Participants: diagnostic criteria, number in each group, age, gender, baseline comparability between two groups, withdrawals or losses to follow‐up.
Methods: study design, randomisation method, allocation concealment method, blinding methods.
Interventions: details of inspiratory muscle training treatment, such as treatment type, regimen, duration and cointervention(s).
Outcomes: primary and secondary outcomes, adverse effects.
Other: country and setting, publication year, sources of funding, intention‐to‐treat analysis (ITT).
There were some minor disagreements about the data extraction; however, they were resolved after discussion between review authors.
Assessment of risk of bias in included studies
Two review authors independently assessed the methodological quality of the included studies using the quality checklist recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The quality checklist for evaluating the risk of bias consists of seven specific parameters: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting and (7) other sources of bias. For each entry, the judgement (low risk of bias, high risk of bias or unclear risk of bias) was accompanied by a description of the design, conduct or observations that underlie the judgement (Higgins 2011). There was no disagreement in assessing the risk of bias between the review authors.
We assessed the risk of bias of included studies as follows.
Random sequence generation
Low risk: adequate sequence generation process, e.g. random number table, computer random number generator, coin tossing, drawing of lots, shuffling cards. High risk: sequence generation process was by a non‐random method, for example generated by odd or even date of birth, admission number. Unclear risk: did not describe the sequence generation process but only stated as 'random'.
Allocation concealment
Low risk: adequate concealment allocation, for example central allocation, sequentially numbered, opaque, sealed envelopes; or another approach that would ensure the participants and investigators did not know the assignment. High risk: did not conceal allocation, or used an ineffective allocation concealment which may allow the participants and investigators to know the assignment, for example using an open random allocation schedule, using not sequentially numbered, non‐opaque, unsealed envelopes; by alternation, case record number, date of birth. Unclear risk: did not describe the method of allocation concealment; or could not be sure that the allocation concealment was effective.
Blinding of participants and personnel and blinding of outcome assessment
Low risk: in studies of inspiratory muscle training for stroke participants, personnel and outcome assessors should be blinded. High risk: no blinding or incomplete blinding; blinding of participants, physicians and outcome assessors but the blinding may have been broken. Unclear risk: does not describe the method of blinding but only states 'blinding'.
Incomplete outcome data
Low risk: no missing outcome data; reasons for missing data would not influence the true outcomes; numbers of missing data were balanced across groups. High risk: reasons for missing data would affect the true outcomes; numbers of missing data were imbalanced across groups. Unclear risk: numbers or reasons for missing data were not provided.
Selective reporting
Low risk: all the pre‐specified outcomes were reported. High risk: not all of the study's pre‐specified outcomes were reported; some primary outcomes were reported using methods that not pre‐specified; some primary outcomes were not pre‐specified. Unclear risk: the existing information was not sufficient to judge 'Yes' or 'No'.
Other sources of bias
Low risk: the study was free of other bias. High risk: at least one other important bias was present, for example using an unsuitable study design; the baseline characteristics were extremely imbalanced; conflict of interests. Unclear risk: the information to evaluate other bias was insufficient.
Measures of treatment effect
We managed the data according to the ITT principle. For dichotomous outcomes, we used risk ratio (RR) with 95% confidence interval (CI) to express the effect size. For continuous data, we used mean differences (MD) with 95% CI to analyse the outcomes. Where we wished to combine data on the same outcome measured with different scales, we used the standardised mean difference (SMD).
Unit of analysis issues
We dealt with any unit of analysis issues using the guidance in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For cross‐over studies, we only included data from the first period for analyses.
Dealing with missing data
We contacted study authors to obtain further information that was not reported in the articles. If we did not receive a response, we analysed the available data and considered the missing data using both the best‐case and worst‐case scenarios.
Assessment of heterogeneity
We evaluated the clinical and methodological heterogeneity of included trials by comparing the characteristics of participants, interventions and study designs. We evaluated statistical heterogeneity among included studies using the I2 statistic. We only used a random‐effects model regardless of the level of heterogeneity because if the heterogeneity is 0% then the results produced by a random‐effects model will be the same as the results for a fixed‐effect model. However, if the I2 statistic was more than 50%, which indicated substantial heterogeneity (Higgins 2011), we examined the sources of potential clinical and methodological heterogeneity.
Assessment of reporting biases
We did not investigate potential biases of publication using funnel plots according to the approach of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) as we only identified two studies.
Data synthesis
We used RevMan 5.1 (RevMan 2011) to synthesis the available data. We used a random‐effects model regardless of the level of heterogeneity. If substantial statistical heterogeneity was found according to the results of the I2 statistic for heterogeneity (Higgins 2011), we examined the sources of heterogeneity. If clinical heterogeneity was present, we performed subgroup analyses or, if not appropriate, we did not pool the data but only described the results.
Subgroup analysis and investigation of heterogeneity
We planned to perform the following subgroup analyses:
type of inspiratory muscle training (e.g. threshold versus resistive trainer);
frequency of inspiratory muscle training (e.g. daily versus three times per week);
duration of inspiratory muscle training (e.g. six weeks versus more than six weeks);
time to treatment (e.g. six months post‐stroke versus more than six months post‐stroke);
type of stroke (e.g. ischaemic versus haemorrhagic).
Because of the limited available data we did not perform subgroup analyses.
Sensitivity analysis
We planned to re‐analyse the results excluding studies without adequate allocation concealment or blinding, but because of the limited available data we did not perform subgroup analyses.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies
Results of the search
The search strategies retrieved a total of 5077 citations, 596 from the Cochrane Stroke Group's Trials Register, 4357 from the electronic bibliographic databases and 124 from other resources. After reviewing the titles and abstracts we excluded 5072 citations as they were not relevant or obvious duplicate publications. Of the remaining five citations (Britto 2011; Kalra 2011; Kim 2011; Nuzzo 1999; Sutbeyaz 2010), we excluded two studies (Kim 2011; Nuzzo 1999) because they did not meet the inclusion criteria and one study (Kalra 2011) is still ongoing. Finally, we selected two studies for inclusion in the review (see Figure 1).
1.
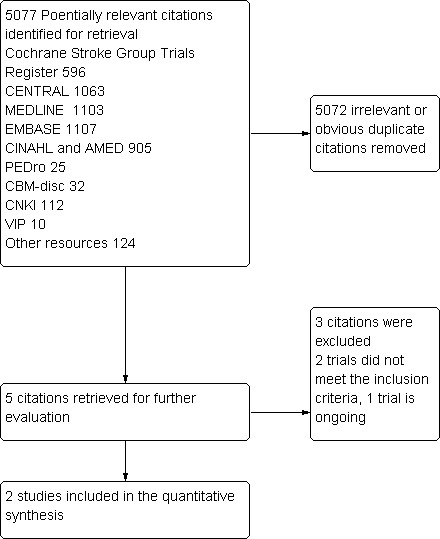
Study flow diagram
Included studies
We identified two trials investigating the efficacy of inspiratory muscle training for the functional recovery of stroke that met our inclusion criteria.
Britto 2011 was a double‐blind RCT that enrolled 21 patients who had a stroke within nine months into either the inspiratory muscle training group (threshold trainer) or the sham inspiratory muscle training group for eight weeks. Patients with restricted pulmonary function and neurological, orthopaedic or unstable cardiac disease were excluded. Both groups of patients trained for 30 minutes a day, five times a week for eight weeks. The inspiratory muscle training group patients trained with a breathing resistance at 30% of their MIP, the load resistance was adjusted weekly according to their new MIP. The sham training group patients performed the same training programme without any resistance. At the end of follow‐up, 18 patients finished the study: two patients dropped out of the inspiratory muscle training group due to lack of time to complete the training, while one patient dropped out in the sham training group because of hypertension. The authors reported MIP, inspiratory muscular endurance, functional performance and quality of life as outcome measures.
Sutbeyaz 2010 was a RCT that enrolled 45 patients who had a first episode of stroke in the previous 12 months into three groups for six weeks: 15 patients were assigned to the inspiratory muscle training group (threshold trainer), 15 patients were assigned to the breathing retraining (BRT) group and 15 patients were assigned to the no intervention group. Patients with cardiac or respiratory disease, impaired consciousness and cognitive function were excluded. The inspiratory muscle training group trained for 30 minutes a day, six times a week for six weeks. The patients trained with a load resistance at 40% of their MIP, then gradually increased the level by 5% to 10% each day until reaching 60% of MIP to be maintained. The BRT group trained for 30 minutes daily for six weeks. Each training programme involved 15 minutes of diaphragmatic breathing in combination with pursed‐lips breathing, followed by five minutes of air shifting techniques and 10 minutes of voluntary isocapnoeic hyperpnoea. Because of the two different training programmes and no intervention control group, the blinding of physicians and patients was not possible, only the outcome assessors were blinded. The authors reported ADL, pulmonary function, quality of life, motor recovery and cardiorespiratory fitness as outcome measures. At the end of follow‐up, all 45 patients completed the study.
Excluded studies
We excluded two trials for the following reasons: Kim 2011 because the study authors did not report the primary or secondary outcomes chosen for this review and Nuzzo 1999 because the study was designed with no control group.
Risk of bias in included studies
Overall results of all the risk of bias assessments are summarised in Figure 2.
2.
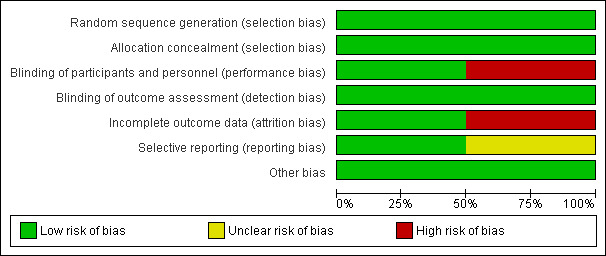
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
Sutbeyaz 2010 stated that the generation of the random list was done using a computer random number generator. Britto 2011 reported that the random list was generated through random blocks but did not give details. After contact with the study author seeking clarification of the method used, the author reported the random list was generated by a computer random number generator. As both trials reported that the allocation sequence was stored in sequential sealed opaque envelopes, we judged allocation concealment was adequate.
Blinding
In Britto 2011, all the study physicians, patients and outcome assessors were blinded to treatment, the control patients were assigned to sham inspiratory muscle training to make sure they were unaware of the differences. In Sutbeyaz 2010, because of the two different training programmes and no intervention control group, the blinding of physicians and patients was impossible: only the outcome assessors were blinded. We judged this trial at high risk of performance bias and at low risk of detection bias.
Incomplete outcome data
Britto 2011 provided enough information about the number and reasons for dropouts in both groups: three dropouts were excluded from final outcome analyses. We judged this trial to be at high risk of incomplete outcome data bias. In Sutbeyaz 2010 all 45 patients completed the study, there were no losses to six‐week follow‐up, and we therefore judged the trial at low risk of bias in this domain.
Selective reporting
It was not possible to confirm whether all pre‐specified outcomes were reported as both included trial protocols were not available. The majority of outcome measures in Britto 2011 were available in the reports and appeared to be of low risk for reporting bias. In Sutbeyaz 2010, some important outcomes, such as ADL and quality of life, were not reported in detail: we contacted the study author seeking further information but to date we have not received a response. Thus, the judgement of bias in this domain was unclear.
Other potential sources of bias
We did not identify any other potential sources of bias.
Effects of interventions
We included two studies in this review, one of which (Britto 2011) compared inspiratory muscle training with sham inspiratory muscle training for the functional recovery of stroke, the other (Sutbeyaz 2010) was a three‐arm study comparing inspiratory muscle training versus BRT and no intervention for patients with stroke. Due to considerable heterogeneity and lack of data for some outcomes chosen for this review, it was not appropriate to pool the data within analyses. We have therefore provided a description of the results as reported by the trial authors.
Comparison 1: inspiratory muscle training versus no intervention
Data were only available from Sutbeyaz 2010 with a total of 30 patients for this comparison.
1. Activities of daily living (ADL)
The authors briefly stated a significant improvement of ADL in the inspiratory muscle training group compared with the no intervention group.
2. Respiratory muscle strength, measured by maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP)
There was no significant difference in changes of MIP (MD 3.43; 95% CI ‐1.96 to 8.82) (Analysis 1.1) and MEP (MD ‐3.10; 95% CI ‐8.88 to 2.68) (Analysis 1.2) between the inspiratory muscle training group and the no intervention group (Sutbeyaz 2010).
1.1. Analysis.
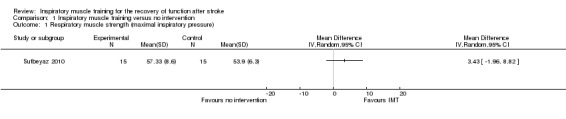
Comparison 1 Inspiratory muscle training versus no intervention, Outcome 1 Respiratory muscle strength (maximal inspiratory pressure).
1.2. Analysis.
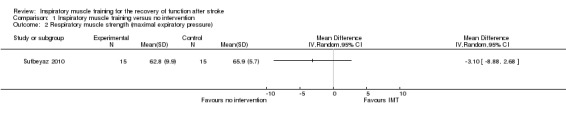
Comparison 1 Inspiratory muscle training versus no intervention, Outcome 2 Respiratory muscle strength (maximal expiratory pressure).
3. Quality of life
The authors briefly stated there was significant improvement of physical role, general health and vitality domains of the SF‐36 in the inspiratory muscle training group compared with the no intervention group.
4. Cardiorespiratory fitness, measured by peak oxygen consumption (VO2peak)
There was a significantly increased VO2peak in favour of the inspiratory muscle training group compared with the no intervention group (MD 1.20; 95% CI 0.41 to 1.99) (Analysis 1.3). VO2peak is considered the most valid measurement of cardiorespiratory fitness: a lower level of cardiorespiratory fitness was associated with a higher risk of stroke mortality (Kurl 2003; Lee 2002).
1.3. Analysis.
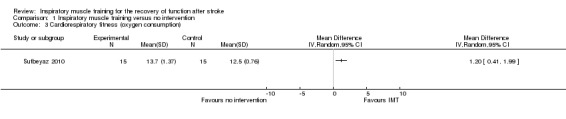
Comparison 1 Inspiratory muscle training versus no intervention, Outcome 3 Cardiorespiratory fitness (oxygen consumption).
5. Adverse effects
No relevant data were available.
Comparison 2: Inspiratory muscle training versus sham inspiratory muscle training
Data were only available from Britto 2011 with a total of 18 patients for this comparison.
1. Activities of daily living (ADL)
No relevant data were available.
2. Respiratory muscle strength, measured by maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP)
Inspiratory muscle training was associated with a significant increase of MIP when compared with sham inspiratory muscle training (MD 45.50; 95% CI 27.59 to 63.41) (Analysis 2.1).
2.1. Analysis.
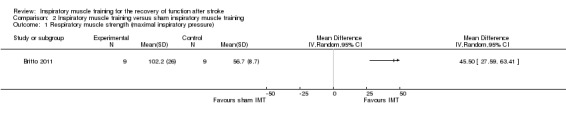
Comparison 2 Inspiratory muscle training versus sham inspiratory muscle training, Outcome 1 Respiratory muscle strength (maximal inspiratory pressure).
3. Quality of life
No significant difference was found on improvement of quality of life between both groups (MD ‐1.10; 95% CI ‐6.39 to 4.19) (Analysis 2.2), measured by the Brazilian version of the Nottingham Health Profile (Teixeira‐Salmela 2004).
2.2. Analysis.
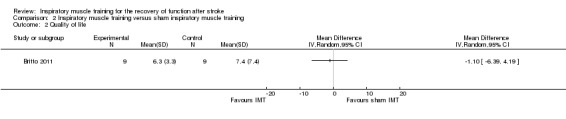
Comparison 2 Inspiratory muscle training versus sham inspiratory muscle training, Outcome 2 Quality of life.
4. Cardiorespiratory fitness, measured by peak oxygen consumption (VO2peak)
No relevant data were available.
5. Adverse effects
No relevant data were available.
Comparison 3: Inspiratory muscle training versus other cardiorespiratory training
Data were only available from Sutbeyaz 2010 with a total of 30 patients comparing inspiratory muscle training with BRT for stroke.
1. Activities of daily living (ADL)
The comparison of inspiratory muscle training with BRT in improving ADL for stroke has not been directly investigated, only reported as improved after treatment in both groups.
2. Respiratory muscle strength, measured by maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP)
No significant difference in changes of MIP (MD 0; 95% CI ‐5.91 to 5.91) (Analysis 3.1) and MEP (MD ‐3.40; 95% CI ‐9.91 to 3.11) (Analysis 3.2) were detected between the inspiratory muscle training group and the BRT group (Sutbeyaz 2010).
3.1. Analysis.
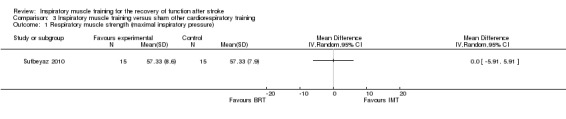
Comparison 3 Inspiratory muscle training versus sham other cardiorespiratory training, Outcome 1 Respiratory muscle strength (maximal inspiratory pressure).
3.2. Analysis.
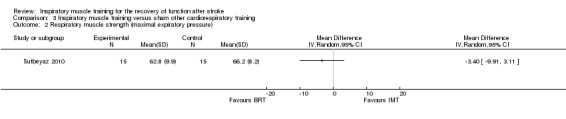
Comparison 3 Inspiratory muscle training versus sham other cardiorespiratory training, Outcome 2 Respiratory muscle strength (maximal expiratory pressure).
3. Quality of life
Improvement in quality of life was not directly compared between the inspiratory muscle training group and the BRT group, only reported as improved after treatment in both groups.
4. Cardiorespiratory fitness, measured by peak oxygen consumption (VO2peak)
The VO2peak was significantly increased in favour of the inspiratory muscle training group when compared with the BRT group (MD 1.22; 95% CI 0.41 to 2.03) (Analysis 3.3).
3.3. Analysis.
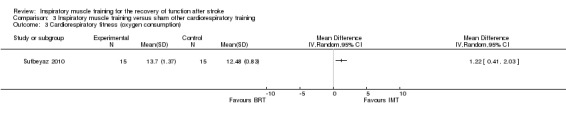
Comparison 3 Inspiratory muscle training versus sham other cardiorespiratory training, Outcome 3 Cardiorespiratory fitness (oxygen consumption).
5. Adverse effects
No relevant data were available.
Discussion
Summary of main results
This systematic review aimed to determine the efficacy and safety of inspiratory muscle training for the functional recovery of patients who have had a stroke. We found two small heterogeneous randomised trials, providing insufficient evidence from which to make any generalised conclusions about the effect of inspiratory muscle training. We found no evidence relating to the safety of inspiratory muscle training.
Overall completeness and applicability of evidence
Specific recommendation of inspiratory muscle training for the functional recovery of stroke is difficult at present due to the limited number of included trials, the small number of patients and inadequate data reporting. Both trials compared the short‐term efficacy and safety of inspiratory muscle training versus no intervention, sham training or BRT in patients with stroke. We were unable to carry out pooling analyses because of the heterogeneity in study design. What is more, the patients differed in age, disease duration since stroke, training load resistance and treatment duration between both studies, all of which would have an important impact on outcome measures. We did not undertake any subgroup or sensitivity analyses because of the limited number of included trials.
Quality of the evidence
Both included trials had methodological limitations. Britto 2011 was a RCT that had an adequate description of allocation concealment and double blinding. A limitation of this trial was that it excluded three dropouts in their outcome analyses, which might introduce bias and lead to an overestimation of efficacy (Heritier 2003; Matilde 2006). Another limitation was that the method of randomisation was not mentioned in the publication but was available from the author after correspondence. Sutbeyaz 2010 was a RCT with adequate methods of randomisation and allocation concealment. The main limitation of this trial was that it compared two different training programmes and a no intervention control group, which makes the blinding of physicians and patients impossible. No blinding contributes to a high risk of performance bias, which may lead to an overestimation of efficacy (Schulz 1995). In addition, both trials only enrolled a relatively small number of participants.
Potential biases in the review process
We undertook an extensive and comprehensive search to minimise bias in the review process. We only identified two completed trials and one ongoing trial. We cannot confirm whether we have failed to identify other unpublished trials. In preparing this review, two review authors independently read and screened trials for inclusion, independently completed data extraction and assessed the quality of included trials to minimise potential biases. The review authors found no conflicts of interest in relation to the review.
Agreements and disagreements with other studies or reviews
To our knowledge, the efficacy and safety of inspiratory muscle training for the functional recovery of patients with stroke have not been systematically reviewed before.
Authors' conclusions
Implications for practice.
There is currently insufficient evidence to support inspiratory muscle training as an effective treatment to improve function after stroke and there is no evidence relating to the safety of inspiratory muscle training.
Implications for research.
Further well‐designed randomised, double‐blinded, sham training controlled trials with larger sample sizes to assess the efficacy and safety of inspiratory muscle training for the functional recovery of patients with stroke are required. Such trials should address the main functional outcome measure using ADL and with a long‐term follow‐up.
Acknowledgements
We thank the Cochrane Stroke Group editors and peer reviewers (Gillian Mead, Alex Pollock, Ashma Krishan, Lalit Kalra and Una Jones) for their constructive suggestions and comments. We thank Brenda Thomas, Trials Search Co‐ordinator, and Hazel Fraser, Managing Editor of the Cochrane Stroke Group for their help in developing this review.
Appendices
Appendix 1. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
1. MeSH descriptor Cerebrovascular Disorders explode all trees 2. MeSH descriptor Basal Ganglia Cerebrovascular Disease explode all trees 3. MeSH descriptor Brain Ischemia explode all trees 4. MeSH descriptor Carotid Artery Diseases explode all trees 5. MeSH descriptor Intracranial Arterial Diseases explode all trees 6. MeSH descriptor Intracranial Embolism and Thrombosis explode all trees 7. MeSH descriptor Intracranial Hemorrhages explode all trees 8. MeSH descriptor Stroke explode all trees 9. MeSH descriptor Brain Infarction explode all trees 10. MeSH descriptor Vertebral Artery Dissection explode all trees 11. (stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc* or cva* or apoplex* or SAH) 12. (brain* or cerebr* or cerebell* or intracran* or intracerebral) near/5 (isch?emi* or infarct* or thrombo* or emboli* or occlus*) 13. (brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid) near/5 (haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed*) 14. MeSH descriptor Paresis explode all trees 15. MeSH descriptor Hemiplegia explode all trees 16. (hemipleg$ or hemipar$ or paresis or paretic) 17. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 18. MeSH descriptor Breathing Exercises explode all trees 19. MeSH descriptor Respiratory Therapy explode all trees 20. MeSH descriptor Respiration explode all trees 21. MeSH descriptor Inhalation explode all trees 22. MeSH descriptor Exhalation explode all trees 23. MeSH descriptor Inspiratory Capacity explode all trees 24. MeSH descriptor Respiratory Muscles explode all trees 25. (respirat* or inspirat* or expirat* or ventilat* or pulmonary) near/5 (therap* or train* or retrain* or exercise* or resist* or conditioning or strength* or weakness or endurance or muscle*) 26. (breathing or inhalation or exhalation) near/5 (exercise* or therap* or train* or retrain*) 27. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 28. 17 AND 27
Appendix 2. MEDLINE (Ovid) search strategy
1. cerebrovascular disorders/ or exp basal ganglia cerebrovascular disease/ or exp brain ischemia/ or exp carotid artery diseases/ or exp intracranial arterial diseases/ or exp "intracranial embolism and thrombosis"/ or exp intracranial hemorrhages/ or stroke/ or exp brain infarction/ or vertebral artery dissection/ 2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. hemiplegia/ or exp paresis/ 6. (hemipleg$ or hemipar$ or paresis or paretic).tw. 7. or/1‐6 8. breathing exercises/ 9. respiratory therapy/ 10. respiration/ or inhalation/ or exhalation/ 11. exp inspiratory capacity/ 12. exp respiratory muscles/ 13. ((respirat$ or inspirat$ or expirat$ or ventilat$ or pulmonary) adj5 (therap$ or train$ or retrain$ or exercise$ or resist$ or conditioning or strength$ or weakness or endurance or muscle$)).tw. 14. ((breathing or inhalation or exhalation) adj5 (exercise$ or therap$ or train$ or retrain$)).tw. 15. or/8‐14 16. 7 and 15 17. exp animals/ not humans.sh. 18. 16 not 17 19. Randomized Controlled Trials as Topic/ 20. random allocation/ 21. Controlled Clinical Trials as Topic/ 22. control groups/ 23. clinical trials as topic/ or clinical trials, phase i as topic/ or clinical trials, phase ii as topic/ or clinical trials, phase iii as topic/ or clinical trials, phase iv as topic/ 24. double‐blind method/ 25. single‐blind method/ 26. Placebos/ 27. placebo effect/ 28. cross‐over studies/ 29. Therapies, Investigational/ 30. Research Design/ 31. evaluation studies as topic/ 32. randomized controlled trial.pt. 33. controlled clinical trial.pt. 34. (clinical trial or clinical trial phase i or clinical trial phase ii or clinical trial phase iii or clinical trial phase iv).pt. 35. (evaluation studies or comparative study).pt. 36. random$.tw. 37. (controlled adj5 (trial$ or stud$)).tw. 38. (clinical$ adj5 trial$).tw. 39. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 40. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 41. ((multicenter or multicentre or therapeutic) adj5 (trial$ or stud$)).tw. 42. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 43. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 44. (coin adj5 (flip or flipped or toss$)).tw. 45. versus.tw. 46. (cross‐over or cross over or crossover).tw. 47. placebo$.tw. 48. sham.tw. 49. (assign$ or alternate or allocat$ or counterbalance$ or multiple baseline).tw. 50. controls.tw. 51. or/19‐50 52. 18 and 51
Appendix 3. EMBASE search strategy
1. 'cerebrovascular disease'/exp or 'stroke'/exp or 'cerebrovascular accident'/exp or 'brain hemorrhage'/exp or 'brain ischemia'/exp or 'stroke unit'/exp or 'basal ganglion hemorrhage'/exp or 'brain infarction'/exp or 'occlusive cerebrovascular disease'/exp or 'carotid artery disease'/exp or 'cerebral artery disease'/exp or 'intracranial aneurysm'/exp or 'hemiplegia'/exp or 'paresis'/exp or 'hemiparesis'/exp 2. (stroke or poststroke or 'post stroke' or cerebrovasc$ or 'brain vasc$' or 'cerebral vasc$' or cva$ or apoplex$ or sah).ab. 3. (brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral).ab. 4. (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$).ab. 5. 3 and 4 6. (brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid).ab. 7. (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$).ab. 8. 6 and 7 9. (hemipleg$ or hemipar$ or paresis or paretic).ab. 10. 1 or 2 or 5 or 8 or 9 11. 'breathing exercise'/exp or 'breathing'/exp or 'inhalation'/exp or 'exhalation'/exp or 'inspiratory capacity'/exp or 'breathing muscle'/exp 12. (respirat$ or inspirat$ or expirat$ or ventilat$ or pulmonary).ab. 13. (therap$ or train$ or retrain$ or exercise$ or resist$ or conditioning or strength$ or weakness or endurance or muscle$).ab. 14. 12 and 13 15. (breathing or inhalation or exhalation).ab. 16. (exercise$ or therap$ or train$ or retrain$).ab. 17. 15 and 16 18. 11 or 14 or 17 19. 'randomized controlled trial'/exp or 'clinical trial'/exp or 'controlled clinical trial'/exp or 'controlled study'/exp or 'randomization'/exp or 'single blind procedure'/exp or 'double blind procedure'/exp or 'parallel design'/exp or 'crossover procedure'/exp or 'placebo'/exp or 'control group'/exp 20. (random$ or placebo$ or control$ or 'clinical trial').ab. 21. 19 or 20 22. 10 and 18 and 21 23. 22 and [humans]/lim
Appendix 4. CINAHL (Ebsco) search strategy
1. (MH "Cerebrovascular Disorders+") or (MH "stroke patients") or (MH "stroke units") 2. TI ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) or AB ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) 3. TI ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) or AB ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) 4. TI ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) or AB ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) 5. S3 and S4 6. TI ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) or AB ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) 7. TI ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) or AB ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) 8. S6 and S7 9. (MH "Hemiplegia") 10. TI ( hemipleg* or hemipar* or paresis or paretic ) or AB ( hemipleg* or hemipar* or paresis or paretic ) 11. S1 or S2 or S5 or S8 or S9 or S10 12. (MH "Breathing Exercises (SabaCCC)") OR (MH "Breathing Exercises+") 13. (MH "Education, Respiratory Therapy") OR (MH "Home Respiratory Care") OR (MH "Inspiration, Respiratory") OR (MH "Respiratory Muscles+") OR (MH "Respiratory Nursing") OR (MH "Respiratory Nursing Society") OR (MH "Respiratory Therapists") OR (MH "Respiratory Therapy+") OR (MH "Respiratory Therapy Equipment and Supplies+") OR (MH "Respiratory Therapy Service") 14. (MH "Respiration (Omaha)") OR (MH "Respiration (Saba CCC)") OR (MH "Respiration Alteration (Saba CCC)") 15. (MH "Respiration+") and (MH "Muscle Strengthening") 16. TI ( respirat* or inspirat* or expirat* or ventilat* or pulmonary ) OR AB ( respirat* or inspirat* or expirat* or ventilat* or pulmonary ) 17. TI ( therap* or train* or retrain* or exercise* or resist* or conditioning or strength* or weakness or endurance or muscle* ) OR AB ( therap* or train* or retrain* or exercise* or resist* or conditioning or strength* or weakness or endurance or muscle* ) 18. S16 and S17 19. TI ( breathing or inhalation or exhalation ) OR AB ( breathing or inhalation or exhalation ) 20. TI ( exercise* or therap* or train* or retrain* ) OR AB ( exercise* or therap* or train* or retrain* ) 21. S19 and S20 22. S12 or S13 or S14 or S15 or S18 or S21 23. S11 and S22 24. PT randomized controlled trial or clinical trial 25. (MH "Random Assignment") or (MH "Random Sample+") 26. (MH "Crossover Design") or (MH "Clinical Trials+") or (MH "Comparative Studies") 27. (MH "Control (Research)") or (MH "Control Group") 28. (MH "Factorial Design") or (MH "Quasi‐Experimental Studies") or (MH "Nonrandomized Trials") 29. (MH "Placebo Effect") or (MH "Placebos") or (MH "Meta Analysis") 30. (MH "Clinical Research") or (MH "Clinical Nursing Research") 31. (MH "Community Trials") or (MH "Experimental Studies") or (MH "One‐Shot Case Study") or (MH "Pretest‐Posttest Design+") or (MH "Solomon Four‐Group Design") or (MH "Static Group Comparison") or (MH "Study Design") 32. PT systematic review 33. TI random* or AB random* 34. TI ( singl* or doubl* or tripl* or trebl* ) or AB ( singl* or doubl* or tripl* or trebl* ) 35. TI ( blind* or mask*) or AB ( blind* or mask* ) 36. S34 and S35 37. TI ( crossover or cross‐over or placebo* or control* or factorial or sham ) or AB ( crossover or cross‐over or placebo* or control* or factorial or sham ) 38. TI ( clin* or intervention* or compar* or experiment* or preventive or therapeutic ) or AB ( clin* or intervention* or compar* or experiment* or preventive or therapeutic ) 39. TI trial* or AB trial* 40. S38 and S39 41. TI ( counterbalance* or multiple baseline* or ABAB design ) or AB ( counterbalance* or multiple baseline* or ABAB design ) 42. TI ( meta analysis* or metaanalysis or meta‐analysis or systematic review* ) or AB ( meta analysis* or metaanalysis or meta‐analysis or systematic review* ) 43. PT meta analysis 44. S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 45. S23 and S44
Appendix 5. AMED (Ovid) search strategy
1. cerebrovascular disorders/ or cerebral hemorrhage/ or cerebral infarction/ or cerebral ischemia/ or cerebrovascular accident/ or stroke/ 2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. hemiplegia/ 6. (hemipleg$ or hemipar$ or paresis or paretic).tw. 7. 1 or 2 or 3 or 4 or 5 or 6 8. breathing exercises/ 9. respiratory therapy/ 10. exp respiration/ 11. exp respiratory muscles/ 12. ((respirat$ or inspirat$ or expirat$ or ventilat$ or pulmonary) adj5 (therap$ or train$ or retrain$ or exercise$ or resist$ or conditioning or strength$ or weakness or endurance or muscle$)).tw. 13. ((breathing or inhalation or exhalation) adj5 (exercise$ or therap$ or train$ or retrain$)).tw. 14. 8 or 9 or 10 or 11 or 12 or 13 15. 7 and 14
Data and analyses
Comparison 1. Inspiratory muscle training versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Respiratory muscle strength (maximal inspiratory pressure) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Respiratory muscle strength (maximal expiratory pressure) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Cardiorespiratory fitness (oxygen consumption) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 2. Inspiratory muscle training versus sham inspiratory muscle training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Respiratory muscle strength (maximal inspiratory pressure) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Quality of life | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 3. Inspiratory muscle training versus sham other cardiorespiratory training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Respiratory muscle strength (maximal inspiratory pressure) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Respiratory muscle strength (maximal expiratory pressure) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Cardiorespiratory fitness (oxygen consumption) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Britto 2011.
| Methods | Double‐blind RCT Random list was generated using random blocks but with no details. After correspondence with the authors, it was clarified that patients were randomly allocated using a computer random number generator Allocation sequence was done using sequentially numbered, sealed opaque envelopes to make sure the participants and investigators could not predict allocation Double blinded: all study physicians, participants and outcome assessors were blinded ITT analysis: no, dropouts were not included in the final analysis |
|
| Participants | Setting: Brazil 21 patients who had a stroke within 9 months were randomly assigned into either the inspiratory muscle training group (11 patients) or the sham inspiratory muscle training group (10 patients) for 8 weeks 9 patients in the inspiratory muscle training group finished the study: 4 females and 5 males, age 56.66 ± 5.56 years* 9 patients in the sham training group finished the study: 5 females and 4 males, age 51.44 ± 15.98 years* Exclusion criteria: restriction in pulmonary function and neurological, orthopaedic or unstable cardiac disease |
|
| Interventions | Intervention group: inspiratory muscle training for 8 weeks Control group: sham inspiratory muscle training for 8 weeks without resistance valve of the threshold trainer |
|
| Outcomes |
|
|
| Notes | 2 patients in the inspiratory muscle training group were lost to follow‐up due to lack of time to complete the training, and 1 patient in the sham training group was lost to follow‐up due to hypertension: all 3 patients were excluded from the analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator ‐ information available from the author |
| Allocation concealment (selection bias) | Low risk | Using sequential sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Triple blinding of physicians, participants and outcome assessors |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Triple blinding of physicians, participants and outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The number of dropouts was carefully reported and balanced between groups 2 patients in the inspiratory muscle training group and 1 patient in the sham training group were lost to follow‐up, but all 3 patients were excluded from analyses |
| Selective reporting (reporting bias) | Low risk | Not identified |
| Other bias | Low risk | Not identified |
Sutbeyaz 2010.
| Methods | RCT Random list was generated using a computer random number generator Allocation sequence was done using sequential sealed envelopes to make sure the participants and investigators could not predict allocation Double blinded: only outcome assessors were blinded, the study physicians and participants were not blinded due to the nature of the treatment ITT analysis: yes |
|
| Participants | Setting: Turkey 45 patients with a first episode of stroke in the previous 12 months were randomly assigned into the inspiratory muscle training group (15 patients), the BRT group (15 patients), or the no intervention group (15 patients) for 6 weeks 15 patients in the inspiratory muscle training group finished the study, 7 females and 8 males, age 62.8 ± 7.2 years* 15 patients in BRT group finished the study, 7 females and 8 males, age 60.8 ± 6.8 years* 15 patients in no intervention group finished the study, 7 females and 8 males, age 61.9 ± 6.15 years* Exclusion criteria: cardiac or respiratory disease, impaired consciousness and cognitive function The baseline clinical characteristics were comparable across groups |
|
| Interventions | Group 1: inspiratory muscle training for 6 weeks Group 2: BRT for 6 weeks Group 3: no intervention BRT involved 15 minutes of diaphragmatic breathing in combination with pursed‐lips breathing, followed by 5 minutes of air‐shifting techniques and 10 minutes voluntary isocapnoeic hyperpnoea |
|
| Outcomes |
|
|
| Notes | Some important prespecified outcomes, such as ADL living and quality of life, were not reported in detail | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator |
| Allocation concealment (selection bias) | Low risk | Using sequential sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The study physicians and participants were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Some important pre‐specified outcomes were not reported in detail |
| Other bias | Low risk | Not identified |
*: values expressed as mean ± standard deviation ADL: activities of daily BRT: breathing retraining ITT: intention‐to‐treat analysis RCT: randomised controlled trial SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Kim 2011 | Outcome measures did not meet the primary or secondary outcome measures of our review |
| Nuzzo 1999 | No control group |
Characteristics of ongoing studies [ordered by study ID]
Kalra 2011.
| Trial name or title | Respiratory muscle training in stroke |
| Methods | Multicentre randomised controlled pilot study |
| Participants | 60 ischaemic stroke patients with dysphagia aged between 50 and 80 years Inclusion criteria: first stroke within 1 week of onset, moderate severity, evidence of aspiration, able to maintain sitting balance, able to comply with respiratory muscle testing procedures, consent to participation Exclusion criteria: blood pressure > 180/100 mmHg; high intracranial pressure on CT scan; myocardial infarction, angina or heart failure in the previous 3 months; pulmonary, neurological (other than stroke) or orthopaedic conditions that may affect the function of respiratory muscle |
| Interventions | Group 1: expiratory muscle training, 5 days/week for 4 weeks Group 2: inspiratory muscle training, 5 days/week for 4 weeks Control: sham training, 5 days/week for 4 weeks |
| Outcomes | Primary outcome: aspiration, activities of daily living (ADL), respiratory function Secondary outcome: safety |
| Starting date | 1 March 2011 |
| Contact information | Professor Lalit Kalra, King's College London, Department of Stroke Medicine, Academic Neurosciences Centre, London, SE5 8AF, UK lalit.kalra@kcl.ac.uk |
| Notes | ISRCTN40298220 http://www.controlled‐trials.com/ISRCTN40298220 http://public.ukcrn.org.uk/search/StudyDetail.aspx?StudyID=9181 |
CT: computerised tomography
Differences between protocol and review
We have added the safety assessment of inspiratory muscle training as a main objective.
Contributions of authors
Yousheng Xiao, Man Luo, Jin Wang and Hongye Luo drafted the protocol. Yousheng Xiao and Man Luo ran the search strategy. Yousheng Xiao and Man Luo selected relevant articles for inclusion. Yousheng Xiao and Man Luo extracted the data from included studies. Yousheng Xiao, Man Luo and Jin Wang assessed the risk of bias in included studies. Yousheng Xiao and Man Luo entered data to RevMan. Yousheng Xiao, Man Luo, Jin Wang and Hongye Luo carried out the analysis. Jin Wang, Yousheng Xiao and Man Luo interpreted the results. Yousheng Xiao, Man Luo, Jin Wang and Hongye Luo drafted the final review. Jin Wang will update the review.
Declarations of interest
None known.
New
References
References to studies included in this review
Britto 2011 {published data only}
- Britto RR, Rezende NR, Marinho KC, Torres JL, Parreira VF, Teixeira‐Salmela LF. Inspiratory muscular training in chronic stroke survivors: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2011;92(2):184‐90. [PUBMED: 21272713] [DOI] [PubMed] [Google Scholar]
Sutbeyaz 2010 {published data only}
- Sutbeyaz ST, Koseoglu F, Inan L, Coskun O. Respiratory muscle training improves cardiopulmonary function and exercise tolerance in subjects with subacute stroke: a randomized controlled trial. Clinical Rehabilitation 2010;24(3):240‐50. [PUBMED: 20156979] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Kim 2011 {published data only}
- Kim K, Fell DW, Lee JH. Feedback respiratory training to enhance chest expansion and pulmonary function in chronic stroke: a double‐blind, randomized controlled study. Journal of Physical Therapy Science 2011;23(1):75‐9. [Google Scholar]
Nuzzo 1999 {published data only}
- Nuzzo NA, Bronson LA, McCarthy T, Massery M. Respiratory muscle strength and endurance following a CVA. Neurology Report 1999;23(2):25‐7. [Google Scholar]
References to ongoing studies
Kalra 2011 {published data only}
- Kalra L. Respiratory muscle training in stroke. Current Controlled Trials (http://www.controlled‐trials.com/) 2011.
Additional references
AHA 2011
- American Heart Association. Heart disease and stroke statistics ‐ 2011 update: a report from the American Heart Association. Circulation 2011;123(4):e18‐e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
AHA/ASA 2011
Annoni 1990
- Annoni JM, Ackermann D, Kesselring J. Respiratory function in chronic hemiplegia. International Disability Studies 1990;12(2):78‐80. [PUBMED: 2254236] [DOI] [PubMed] [Google Scholar]
Brown 2010
- Brown AW, Schultz BA. Recovery and rehabilitation after stroke. Seminars in Neurology 2010;30(5):511‐7. [DOI] [PubMed] [Google Scholar]
Dall'Ago 2006
- Dall'Ago P, Chiappa GR, Guths H, Stein R, Ribeiro JP. Inspiratory muscle training in patients with heart failure and inspiratory muscle weakness: a randomized trial. Journal of the American College of Cardiology 2006;47(4):757‐63. [PUBMED: 16487841] [DOI] [PubMed] [Google Scholar]
Enright 2004
- Enright S, Chatham K, Ionescu AA, Unnithan VB, Shale DJ. Inspiratory muscle training improves lung function and exercise capacity in adults with cystic fibrosis. Chest 2004;126(2):405‐11. [PUBMED: 15302725] [DOI] [PubMed] [Google Scholar]
ESO 2008
- European Stroke Organization (ESO). Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovascular Diseases 2008;25(5):457‐507. [DOI] [PubMed] [Google Scholar]
Fregonezi 2005
- Fregonezi GA, Resqueti VR, Guell R, Pradas J, Casan P. Effects of 8‐week, interval‐based inspiratory muscle training and breathing retraining in patients with generalized myasthenia gravis. Chest 2005;128(3):1524‐30. [PUBMED: 16162753] [DOI] [PubMed] [Google Scholar]
Fry 2007
- Fry DK, Pfalzer LA, Chokshi AR, Wagner MT, Jackson ES. Randomized control trial of effects of a 10‐week inspiratory muscle training program on measures of pulmonary function in persons with multiple sclerosis. Journal of Neurologic Physical Therapy 2007;31(4):162‐72. [PUBMED: 18172412] [DOI] [PubMed] [Google Scholar]
Hatano 1976
- Hatano S. Experience from a multicenter stroke register: a preliminary report. Bulletin of the World Health Organization 1976;54:541‐53. [PMC free article] [PubMed] [Google Scholar]
Heritier 2003
- Heritier SR, Gebski VJ, Keech AC. Inclusion of patients in clinical trial analysis: the intention‐to‐treat principle. Medical Journal of Australia 2003;179(8):438‐40. [PUBMED: 14558871] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Houston 2008
- Houston BW, Mills N, Solis‐Moya A. Inspiratory muscle training for cystic fibrosis. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD006112.pub2] [DOI] [PubMed] [Google Scholar]
Inzelberg 2005
- Inzelberg R, Peleg N, Nisipeanu P, Magadle R, Carasso RL, Weiner P. Inspiratory muscle training and the perception of dyspnea in Parkinson's disease. Canadian Journal of Neurological Sciences 2005;32(2):213‐7. [PUBMED: 16018157] [DOI] [PubMed] [Google Scholar]
Jandt 2010
Kurl 2003
- Kurl S, Laukkanen JA, Rauramaa R, Lakka TA, Sivenius J, Salonen JT. Cardiorespiratory fitness and the risk for stroke in men. Archives of Internal Medicine 2003;163(14):1682‐8. [PUBMED: 12885683] [DOI] [PubMed] [Google Scholar]
Lee 2002
- Lee CD, Blair SN. Cardiorespiratory fitness and stroke mortality in men. Medicine and Science in Sports and Exercise 2002;34(4):592‐5. [PUBMED: 11932565] [DOI] [PubMed] [Google Scholar]
Matilde 2006
- Matilde Sanchez M, Chen X. Choosing the analysis population in non‐inferiority studies: per protocol or intent‐to‐treat. Statistics in Medicine 2006;25(7):1169‐81. [PUBMED: 16397861] [DOI] [PubMed] [Google Scholar]
McArthur 2011
- McArthur KS, Quinn TJ, Higgins P, Langhorne P. Post‐acute care and secondary prevention after ischaemic stroke. BMJ 2011;342:d2083. [DOI] [PubMed] [Google Scholar]
Reid 1995
- Reid WD, Samrai B. Respiratory muscle training for patients with chronic obstructive pulmonary disease. Physical Therapy 1995;75(11):996‐1005. [PUBMED: 7480129] [DOI] [PubMed] [Google Scholar]
Reid 2004
- Reid WD, Geddes EL, Brooks D, O'Brien K, Crowe J. Inspiratory muscle training in chronic obstructive pulmonary disease. Special series on Skeletal Muscle Training. Physiotherapy Canada 2004;56:128‐42. [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Roth 1994
- Roth EJ, Noll SF. Stroke rehabilitation. 2. Comorbidities and complications. Archives of Physical Medicine and Rehabilitation 1994;75(5 Spec No):S42‐6. [PUBMED: 8185463] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273(5):408‐12. [PUBMED: 7823387] [DOI] [PubMed] [Google Scholar]
Sheel 2002
- Sheel AW. Respiratory muscle training in healthy individuals: physiological rationale and implications for exercise performance. Sports Medicine 2002;32(9):567‐81. [PUBMED: 12096930] [DOI] [PubMed] [Google Scholar]
Similowski 1996
- Similowski T, Catala M, Rancurel G, Derenne JP. Impairment of central motor conduction to the diaphragm in stroke. American Journal of Respiratory and Critical Care Medicine 1996;154(2 Pt 1):436‐41. [PUBMED: 8756819] [DOI] [PubMed] [Google Scholar]
Teixeira‐Salmela 2004
- Teixeira‐Salmela LF, Magalhaes Lde C, Souza AC, Lima Mde C, Lima RC, Goulart F. Adaptation of the Nottingham Health Profile: a simple measure to assess quality of life [Adaptação do Perfil de Saúde de Nottingham: um instrumento simples de avaliação da qualidade de vida]. Cad Saude Publica 2004;20(4):905‐14. [PUBMED: 15300282] [DOI] [PubMed] [Google Scholar]
Teixeira‐Salmela 2005
- Teixeira‐Salmela LF, Parreira VF, Britto RR, Brant TC, Inacio EP, Alcantara TO, et al. Respiratory pressures and thoracoabdominal motion in community‐dwelling chronic stroke survivors. Archives of Physical Medicine and Rehabilitation 2005;86(10):1974‐8. [PUBMED: 16213241] [DOI] [PubMed] [Google Scholar]
Van der Palen 2004
- Palen J, Rea TD, Manolio TA, Lumley T, Newman AB, Tracy RP, et al. Respiratory muscle strength and the risk of incident cardiovascular events. Thorax 2004;59(12):1063‐7. [PUBMED: 15563706] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ward 2010
- Ward K, Seymour J, Steier J, Jolley CJ, Polkey MI, Kalra L, et al. Acute ischaemic hemispheric stroke is associated with impairment of reflex in addition to voluntary cough. European Respiratory Journal 2010;36(6):1383‐90. [DOI] [PubMed] [Google Scholar]


