Abstract
Background
Adhesions are the leading cause of small bowel obstruction. Gastrografin transit time may allow for the selection of appropriate patients for non‐operative management. Some studies have shown when the contrast does not reach the colon after a designated time it indicates complete intestinal obstruction that is unlikely to resolve with conservative treatment. When the contrast does reach the large bowel, it indicates partial obstruction and patients are likely to respond to conservative treatment. Other studies have suggested that the administration of water‐soluble contrast is therapeutic in resolving the obstruction.
Objectives
To determine the reliability of water‐soluble contrast media and serial abdominal radiographs in predicting the success of conservative treatment in patients admitted with adhesive small bowel obstruction. Furthermore, to determine the efficacy and safety of water‐soluble contrast media in reducing the need for surgical intervention and reducing hospital stay in adhesive small bowel obstruction.
Search methods
The search was conducted using MESH terms: ''Intestinal obstruction'', ''water‐soluble contrast'', "Adhesions" and "Gastrografin". The later combined with the Cochrane Collaboration highly sensitive search strategy for identifying randomised controlled trials and controlled clinical trials.
Selection criteria
1. Prospective studies were included to evaluate the diagnostic potential of water‐soluble contrast in adhesive small bowel obstruction. 2. Randomised clinical trials were selected to evaluate the therapeutic role.
Data collection and analysis
1. Studies that addressed the diagnostic role of water‐soluble contrast were critically appraised and data presented as sensitivities, specificities and positive and negative likelihood ratios. Results were pooled and summary ROC curve was constructed. 2. A meta‐analysis of the data from therapeutic studies was performed using the Mantel ‐Henszel test using both the fixed effect and random effect models.
Main results
The appearance of water‐soluble contrast in the colon on an abdominal X ray within 24 hours of its administration predicts resolution of an adhesive small bowel obstruction with a pooled sensitivity of 0.97, specificity of 0.96. The area under the curve of the summary ROC curve is 0.98. Six randomised studies dealing with the therapeutic role of gastrografin were included in the review, water‐soluble contrast did not reduce the need for surgical intervention (OR 0.81, p = 0.3). Meta‐analysis of four of the included studies showed that water‐soluble contrast did reduce hospital stay compared with placebo (WMD= ‐ 1.83) P<0.001.
Authors' conclusions
Published literature strongly supports the use of water‐soluble contrast as a predictive test for non‐operative resolution of adhesive small bowel obstruction. Although Gastrografin does not cause resolution of small bowel obstruction there is strong evidence that it reduces hospital stay in those not requiring surgery.
Plain language summary
This review addresses two questions. First, "Does the oral administration of water soluble contrast media followed by serial abdominal radiographs during the following 24 hours predict the need for early operation or resolution?"
Second, "Does the administration of water soluble contrast media in patients with adhesive small bowel obstruction facilitate the resolution of symptoms and shorten hospital stay?" Six studies that addressed the first question were included. The pooled results indicated that oral gastrografin is a very accurate predictor of non operative resolution of adhesive small bowel obstruction with a sensitivity of 0.97, specificity of 0.96 and area under the ROC curve of 0.98. Five studies addressed the second question were included, although Gastrografin does not reduce the need for surgery it does reduce hospital stay in those patients who do not require surgery.
Background
Small bowel obstruction is a major cause of hospital admissions around the world with adhesions being the leading cause (Miller 2000). Although it can complicate any abdominal operation, appendicectomy and colorectal surgery are the operations most commonly complicated by adhesive small bowel obstruction. The impact of admissions for small bowel obstruction can be considerable in terms of hospital resources (Menzies 2000). Patients with small bowel obstruction require careful evaluation and management. Immediate surgery is recommended when strangulation is suspected or if complete small bowel obstruction is evident (Choi 2002). The majority of patients with adhesive small bowel obstruction resolve after a trial of conservative treatment (Fevang 2000) however, there is no current consensus as to when conservative treatment should be considered unsuccessful and the patient should undergo surgery. Cox et al have stated that patients who are likely to respond to conservative treatment do so within 48 hours after admission (Cox 1993; Onoue 2002). There are no objective criteria that identify those patients who are likely to respond to conservative treatment. Several studies have evaluated the role of water‐soluble contrast to predict the need for surgical treatment in adhesive small bowel obstruction. The aim of these studies was to determine whether water‐soluble contrast can differentiate complete from partial small bowel obstruction and whether partial small bowel obstruction resolves without surgery. Gastrographin transit time may allow for the judicious selection of the appropriate patient for non‐operative management. Some authors have reported that when Gastrographin is seen in the right colon 4‐6 hours after ingestion it is a reliable indicator to continue with conservative treatment (Blackmon 2000 , Chung 1996). In another study surgery was required in 96% of patients in whom contrast failed to reach the colon within 24 hours (Chen 1998). In addition to its value to predict the need for operative treatment, the therapeutic role of water‐soluble contrast has been investigated in patients admitted with adhesive small bowel obstruction (Choi 2002; Assalia 1994). A randomised controlled study has shown oral water soluble contrast media prompted the resolution of obstruction and shortened hospital stay (Assalia 1994). Other studies have failed to demonstrate a therapeutic benefit of water‐soluble contrast in patients with adhesive small bowel obstruction (Feigin 1996). A further trial has investigated the therapeutic role of Gastrografin in patients who did not resolve on conservative treatment, the authors concluded that Gastrografin is safe and reduces the need for surgery when conservative treatment fails (Choi 2002). Gastrografin is the contrast medium most commonly utilised. It is a mixture of sodium diatrizoate and meglumine diatrizoate. The osmolarity is 2150 mOsm/L. It activates movement of water into the small bowel lumen. Gastrografin also decreases oedema of the small bowel wall and enhances smooth muscle contractility Chen 1999, (Assalia 1994). This review addresses two questions. First, does the oral administration of water soluble contrast media followed by serial abdominal radiographs during the following 24 hours predict the need for early operation or resolution? Second, does the administration of water soluble contrast media in patients with adhesive small bowel obstruction facilitate the resolution of symptoms and shorten the hospital stay?
Objectives
1. To determine the reliability of water‐soluble contrast media and serial abdominal radiographs in predicting the success of conservative treatment in patients admitted with adhesive small bowel obstruction.
2. To determine the efficacy and safety of water‐soluble contrast media in reducing the need for surgical intervention and shortening hospital stay in adhesive small bowel obstruction.
Methods
Criteria for considering studies for this review
Types of studies
All prospective clinical trials addressing the above two questions whether randomised or not have been evaluated, where possible a meta‐analysis was performed.
Types of participants
Patients admitted with adhesive small bowel obstruction, defined as patients who are admitted to the hospital with abdominal pain, vomiting and abdominal distension with dilated small bowel loops and air fluid levels on abdominal radiograph (X Ray) without signs of large bowel obstruction.
Types of interventions
1. The administration of water‐soluble contrast in patients with the diagnosis of adhesive small bowel obstruction followed by interval abdominal radiographs to identify contrast in the colon. 2. The administration of oral water‐soluble contrast to patients with adhesive small bowel obstruction to assess its ability to resolve the obstruction without surgery.
Types of outcome measures
1. The primary outcome measure in the diagnostic arm of the study was the ability of a water‐soluble contrast study to predict the need for surgery in adhesive small bowel obstruction. 2. The primary outcome measure in the therapeutic arm of the study was the rate of resolution of small bowel obstruction without surgery in patients receiving oral water‐soluble contrast compared with those not receiving it. Secondary outcome measures of the study include: length of hospital stay, time from admission to resolution, time from admission to surgical intervention (all analysed as continuous variables), mortality, small bowel strangulation, bowel resection, septic complications, shock, and extra‐abdominal complications (all analysed as dichotomous variables).
Search methods for identification of studies
We have searched the following bibliographic databases in order to identify relevant primary studies:
Cochrane Central Register of Controlled Trials (Central), Cochrane Library 2006 issue 2 Medline, from 1966 to August 2006 EMBASE, from 1980 to August 2006 The Cochrane Colorectal Cancer Group Specialised Register, 2006
The following search terms have been used to search Central, CCCG‐SR and Medline, the later combined with the Cochrane Collaboration highly sensitive search strategy for identifying randomised controlled trials and controlled clinical trials.
Search terms 1. Intestinal obstruction/ 2.Water‐soluble contrast/ 3. # 1 AND #2 4. Intestinal or bowel.mp 5.Obstruction or adhesions.mp 6. # 4 AND #5 7. Contrast media or Gastrographin or water soluble.mp 8. # 6 AND # 7 9. # 3 or #8
To identify primary studies from Embase, the search was limited using the terms above to randomised and clinical controlled trials by using: 'randomisation‐' / all subheadings, 'controlled‐study' / all subheadings, 'clinical‐trial' / all subheadings. We scrutinized the reference lists of included studies and searched relevant conference proceedings. There were no language restrictions. The search was updated to August 2006; two studies have been identified and added to the therapeutic arm of the review (Burge 2005; Lee 2004).
Data collection and analysis
Locating and selecting studies: Two reviewers (SAB, IPB) have independently selected the clinical trials to be included in this review. Disagreement was resolved by consensus. All clinical trials were considered.
Critical appraisal of the studies: The two reviewers have assessed the methodological quality of each clinical trial. Method of randomisation where appropriate, nature of interventions, co‐intervention and follow‐up was critically appraised. Each non‐randomised trial was given a total score of quality, A is good, B is fair and C is poor.
For randomised controlled trials the scale devised by Jadad et al (Jadad 1996) was used to assess the quality of the RCTs.The scale is summarised as follows:
1. Was the study described as randomised (1=yes;0=no) ? 2. Was the study described as double blind (1=yes; 0=no)? 3. Was there a description of withdrawals and dropouts (1=yes;0=no)? 4. Was the method of randomisation well described and appropriate (1=yes; 0=no)? 5. Was the method of double blinding well described and appropriate (1=yes;0=no) ? 6. Deduct 1 point each if methods for randomisation and double blinding were inappropriate. Scoring system: maximum score = 5, minimum score = 0.
Data collection & analysis Data were gathered by the reviewers and checked. The results of each trial was summarised in an intention‐to‐treat basis in 2 x 2 tables for each outcome. Duplicate publication were identified, and data was presented once only.
Diagnostic arm The sensitivities and specificities and positive and negative likelihood ratios were calculated. The results were pooled and a summary ROC curve was constructed using the formula described by Moses et al (Moses 1993). Sensitivity, specificity, and likelihood ratios were calculated for individual studies. Optimal timing of interval radiology was critically appraised. The clinical homogeneity (external validity) was evaluated. Therapeutic arm Where appropriate, the studies have been stratified for meta‐analysis of the main outcome. Hospital stay was considered as a secondary outcome measure (analysed as a continuous variable). Other outcome data that were collected are: time from admission to resolution, time from admission to surgical intervention (analysed as continuous data), Mortality, small bowel strangulation, bowel resection, septic complications, shock and extra‐abdominal complications were compared between the control and the intervention groups (all analysed as dichotomous data).
Statistical heterogeneity in the results of the meta‐analysis was assessed both by graphical presentations of the confidence intervals (CI) on Forest plot (If CI of two studies do not overlap this suggests a significant statistical heterogeneity) and by calculating a test of heterogeneity (chi‐squared test using Rev Man, a p value less than 0.1 was regarded as significant heterogeneity).
Sensitivity analysis was performed by including and excluding the poor quality studies; studies of doubtful eligibility and studies that may look like an outlier. Data from randomised controlled trials were entered in Meta‐view in Rev‐Man 4.2, and the dichotomous variables were compared using Mantel‐Hanszel test. The results are presented as odd ratios, risk difference. For continuous variables the results are presented as weighted mean difference. When we encountered continuous outcomes the mean and standard deviation of the mean were used for calculation of the weighted mean difference.
Results
Description of studies
Out of twelve studies identified two were subsequently excluded. One was excluded because patients were randomised to either surgery or Gastrografin (Choi 2002), the other study was a duplicate of the Chen 1999 study (Chen 1998).
Types of participants: The inclusion criterion was the same for all studies: patients admitted to the hospital with clinical and radiological evidence of small bowel obstruction, provided they have had abdominal surgery in the past. One study (Chung 1996) included patients who did not have previous abdominal surgery, but we included only the patients with adhesive small bowel obstruction in the analysis. Exclusion criteria were similar in all studies which included patients who had surgery within the six weeks before the episode of small bowel obstruction, patients with signs of strangulation or peritonitis, patients with carcinomatosis, patients with irreducible hernia and patients who started to have signs of resolution at the time of admission. One study excluded patients with no gas in the large bowel (complete obstruction) (Assalia 1994), this study analysed the therapeutic role of Gastrografin.
Types of intervention: Studies that used Gastrografin to differentiate between partial and complete small bowel obstruction and hence to predict the probability of resolution have used 50‐100 ml of Gastrografin. Abdominal radiograph (X‐ray) was taken at 4 hours (Brochwicz 2003; Chung 1996; Joyce 1992), 8 hours (Chen 1999), and 24 hours (Biondo 2003; Onoue 2002). If the contrast was seen in the colon the obstruction was considered partial and it was considered complete if the contrast did not reach the colon. The resolution of obstruction or the need for surgery was correlated with the radiologic findings.
Studies that tested the therapeutic role of Gastrografin randomised patients to 100 ml of Gastrografin orally or via the naso‐gastric tube (which was clamped for 60 minutes afterward) versus placebo , patients were otherwise treated similarly (Assalia 1994; Biondo 2003; Burge 2005; Feigin 1996; Fevang 2000; Lee 2004).
OUTCOME:
Primary outcome measures:
Diagnostic The ability of a water soluble contrast study to predict the need for surgery in adhesive small bowel obstruction (Biondo 2003; Brochwicz 2003; Chen 1999; Chung 1996; Joyce 1992; Onoue 2002).
Therapeutic The proportion of patients requiring surgery following administration of Gastrografin or placebo (Assalia 1994; Biondo 2003; Feigin 1996; Fevang 2000; Lee 2004; Burge 2005).
Secondary outcome measures:
Therapeutic 1. Length of hospital stay was described in all studies however only 4 studies reported the results as mean and standard deviation (Assalia 1994; Biondo 2003; Burge 2005; Lee 2004) despite contacting the authors. 2. Time from admission to resolution (Assalia 1994; Biondo 2003; Burge 2005; Lee 2004) 3. Time from admission to surgery (Assalia 1994; Biondo 2003; Feigin 1996; Fevang 2000; Lee 2004) 4. Mortality (Assalia 1994; Burge 2005; Biondo 2003; Feigin 1996; Fevang 2000; Lee 2004) 5. Small bowel strangulation (Assalia 1994; Burge 2005; Biondo 2003; Fevang 2000; Lee 2004) 6. Septic complications and extra‐abdominal complications (Assalia 1994; Biondo 2003; Burge 2005; Feigin 1996; Fevang 2000; Lee 2004)
Risk of bias in included studies
Diagnostic role of Gastrografin We included six studies, all prospective trials (Biondo 2003; Brochwicz 2003; Chen 1999; Joyce 1992; Onoue 2002). The methodological quality was considered good, however the timing of abdominal X‐ray varied between 4‐24 hours as described in the intervention above. There was no "gold standard" to evaluate the diagnostic role of water‐soluble contrast in small bowel obstruction, but the eventual outcome of the individual patients and the need for surgical intervention or resolution was regarded as the standard against which the accuracy of the diagnosis was evaluated.
Therapeutic role of Gastrografin;
The six included studies were described as prospective randomised trials (Assalia 1994; Biondo 2003; Burge 2005; Feigin 1996; Fevang 2000; Lee 2004). The study by Burge et al. (Burge 2005) scored 5 points on the Jadad scale (Jadad 1996). It was double blinded and concealment method and dropouts were described. The other five included studies (Assalia 1994; Biondo 2003; Feigin 1996; Fevang 2000; Lee 2004) scored 2 out of a possible 5 for quality using the Jadad scale. None of these five studies was described as blinded . Overall quality of these five studies was only fair as randomisation methods and allocation concealment are not described in any of the studies. Dropouts and withdrawals were described in all studies and they were analysed on intention to treat basis. The decision to operate was made on clinical grounds of failure of resolution of the obstruction or the onset of signs of strangulation. Although this was independent of the initial radiology further radiographs were performed in assessing ongoing obstruction. In the study by Biondo (Biondo 2003) the results of these radiographs may have influenced the decision to operate as patients who needed surgery had it significantly earlier in the Gastrografin group. Time allowed for non operative resolution varied from 48 hours (Assalia 1994) to 5 days (Feigin 1996).
Effects of interventions
A‐ Diagnostic Role of Gastrografin We calculated the sensitivity, specificity, positive likelihood ratios and negative likelihood ratios for each individual study. The presence of contrast agent in the colon indicated that the obstruction would resolve without surgical intervention with a sensitivity ranging from 0.9 to1, specificity 0.67 to 1, positive ikelihood ratio 2.4 to 11.3 and negative likelihood ratio of 0.017 to 0.097. The pooled sensitivity and specificity were 0.97 and 0.96 respectively, with positive and negative likelihood ratios of 25·10 and 0·036 respectively (Additional table). Results were pooled and a summary ROC curve constructed, both non‐weighted and weighted analyses were performed which showed an area under the curve of 0.98 (fig 1).
The timing of abdominal radiograph differed between the studies and ranged from 4 to 24 hours. The positive and negative LR for studies that waited 4‐8 hours were similar to those that waited 24 hours before performing the radiograph (Table 1). However there was only one false nagative in the 142 patients who had 24 hours delay before the radiograph as opposed to12 in the 312 patients with less than 8 hours delay. It is difficult to advise the optimal timing of the X ray from those data.
1. Prediction of resolution.
| Study | True positive | False positive | False negative | True negative | Sensitivity | Specificity | Timing | LR+ | LR_ |
| Chung 1996 | 31 | 1 | 2 | 11 | 94 | 92 | 4 | 11.273 | 0.066 |
| Chen 1999 | 74 | 0 | 8 | 34 | 90 | 100 | 8 | na | 0.097 |
| Joyce 1992 | 112 | 0 | 2 | 13 | 98 | 100 | 4 | na | 0.017 |
| Biondo 2003 | 39 | 0 | 0 | 5 | 100 | 100 | 24 | na | na |
| Onoue 2002 | 90 | 2 | 1 | 4 | 99 | 67 | 24 | 2.446 | 0.036 |
| Brochwicz‐Lewinski | 16 | 0 | 0 | 8 | 100 | 100 | 4 | na | na |
| Pooled | 362 | 3 | 13 | 75 | 97 | 96 | 25.10 | 0.036 |
B‐ Therapeutic role of Gastrografin
1. Resolution or operative treatment All six studies that were in the therapeutic arm addressed this question. The Mantel‐Henszel test showed there was no significant difference between Gastrografin and placebo in resolution of small bowel obstruction without surgery. The odds ratio was 0·81 (95% CI 0·54 to 1·21); (P = 0·30). There was no heterogeneity between the included studies (P = 0·83) (Comparison 01 01).
2. Hospital stay Four studies (Assalia 1994; Biondo 2003; Burge 2005; Lee 2004) reported the length of hospital stay as mean and standard deviation in patients who did not require surgery. These studies were included for meta‐analysis, using the weighed mean difference (WMD) and fixed‐effect model. Patients who had Gastrografin. had shorter duration of hospital stay, WMD was ‐1·83 (95% CI ‐2·21 to ‐1·45) days (P < 0·001). Two studies (Feigin 1996; Fevang 2000) were excluded from meta‐analysis as they contained inadequate data for inclusion. These individual studies did not show a difference in length of hospital stay (comparison 02 01).
3. Time from admission to resolution: Four studies (Assalia 1994; Biondo 2003; Burge 2005; Lee 2004) reported time between admission and resolution, which was defined as the time of first bowel motion after admission. There was significant heterogeneity between the two studies (p< 0.0001). Studies differed in that patients with gas in the colon were excluded in one study (Assalia 1994). This made a meta‐analysis inappropriate. 4. Small bowel strangulation and resection Four studies (Assalia 1994; Feigin 1996; Fevang 2000, Lee 2004) reported the number of patients who had small bowel strangulation (comparison 03 01). No difference was found between the Gastrografin and control groups (odds ratio was 0·57 (95 % CI 0·22 to 1·46); P = 0·24) (Comparison 03 01).
5. Overall complication rates All studies reported the overall complication rates. There was no difference between the two groups in complication rates with 21 patients out of 273 patients in the Gastrografin group having a complication compared with 18 out of 265 in the control group (comparison 04 01). Meta‐analysis using Mantel‐Henszel test using both fixed effect and fixed effect model yielded an odds ratio of 1·18 (95 % CI 0·61 to 2·29; P = 0·62).
6. Mortality All studies reported the mortality rates (comparison 05 01). There was no difference in mortality rates between the Gastrografin and the control groups but the studies were not adequately powered to detect a difference (OR 1·37 (95% CI 0·43 to 4·38) P = 0·59.
7. Time from admission to operation Although four studies (Assalia 1994, Biondo 2003, Feigin 1996; Lee 2004) reported the time between admission and surgery for patients who required surgery, there were insufficient data to perform a meta‐analysis.
Discussion
In this updated version of the review two more studies have been added to the therapeutic role of Gastrograpfin and included in the meta‐analysis, which has added to the strength of the previous conclusions.
Gastrografin is an osmotically active substance with osmolality of 2150 mosm/l. It may exhibit a therapeutic effect in small bowel obstruction by reducing the bowel wall oedema and increasing the intraluminal tension, it may also enhance smooth muscle contractile activity that can generate effective peristalsis and overcome the obstruction (Choi 2002)
This review provides compelling evidence of the utility of Gastrografin. as a test to identify those patients with adhesive small bowel obstruction who require surgery. The ROC curve of the combined diagnostic studies has an area under the curve of 0.98, and pooled sensitivity, specificity, and positive and negative likelihood ratio values of 0.96, 0.96, 25 and 0.03, indicating it is a very accurate predictor of non‐operative resolution of small bowel obstruction. Patients with a small bowel obstruction but without indication for immediate surgery are suitable for further evaluation with a 100 ml of water‐soluble contrast given via nasogastric tube or orally and an abdominal radiograph after 4‐24 hours. If the contrast has reached the caecum it is considered a partial small bowel obstruction and there is a high probability it will settle on conservative treatment. On the other hand, if the contrast does not reach the caecum, the bowel obstruction is considered to be complete and it is unlikely to settle without surgical intervention. The findings of Choi's randomised trial of surgery versus Gastrografin for patients who fail 48 hours of conservative treatment also support this approach. In 14 of 19 patients Gastrografin was visible in the colon on radiographs (X ray), and they all resolved without surgery (Choi 2002).There is a theoretical problem with the diagnostic studies that relates to the definition of the “gold standard”. Each study allowed the patients a set time period (varying from 2 days to 5 days) for the patients’ symptoms to resolve (by the passage of flatus and stool and the cessation of the symptoms of pain and nausea). The surgeons’ decision to operate was based on this and as such became the de facto “gold standard” of the diagnostic test. One could argue that if the decision of the surgeon was the “gold standard” then why perform the test at all? The reality was, however, that the oral Gastrografin accurately predicted during the first day of the admission whether the symptoms would resolve by this later time. This information allowed for earlier decision making for those patients who needed surgery. This meta‐analysis indicates that Gastrografin does not reduce the need for operation. Four studies were included in a meta‐analysis of hospital stay after administration of contrast agent, which showed that the hospital stay was shorter in the Gastrografin group. The analysis of hospital stay included only those patients who did not have surgery, so it appears that the administration of the contrast agent was responsible for the reduction in hospital stay in this group rather than factors related to operation or postoperative stay. This review, however, was unable to assess whether Gastrografin. actually hastens resolution of small bowel obstruction because the studies were not strictly comparable in this regard. Gastrografin was safe; it did not increase the rate of overall morbidity or mortality, nor the incidence of small bowel strangulation. Only one study (Burge 2005) described the method of randomization and provided adequate blinding with respect to the treatment given. In the other five studies the decision of the clinician might have been influenced by the presence or absence of contrast medium on radiographs. There are, however, potential pitfalls in the use of watersoluble contrast agent in this setting. The administration of full‐strength Gastrografin may lead to difficulty in interpreting the results of subsequent computed tomography because its high density may cause radiological artefacts, although this has not been a problem in the authors' experience. Severe pneumonia from aspiration of Gastrografin is a recognized complication and it would be unwise to administer this agent to patients who do not have an empty stomach or who continue to vomit (Chen 1998); routine gastric drainage by nasogastric tube before administration should prevent this. Intravasation of contrast medium might rarely occur if the nasogastric tube is not properly placed, which may lead to renal failure or anaphylaxis (Glauser 1999). This can be avoided by ensuring that the nasogastric tube is in the stomach before administering contrast agent. The optimal timing of radiography is not clear, but there appears to be little advantage in terms of specificity and sensitivity in waiting longer than 4‐6 hours. However, a potential advantage of waiting 24 h is that the obstruction may resolve in some patients and a radiograph will no longer be needed. In summary, based on the findings of this review, the management of patients with adhesive small bowel obstruction can be simplified according to whether water soluble contrast agent appears in the colon. This has benefits for patients by hastening surgical decision making and reducing the duration of hospital stay.
Authors' conclusions
Implications for practice.
1. Water‐soluble contrast followed by an abdominal radiograph after at least 4 hours can accurately predict the likelihood of resolution of a small bowel obstruction. 2. This review has not found evidence that Gastrografin reduces the need for surgery in patients with an adhesive small bowel obstruction, but none of the studies were adequately powered to show this. 3. Gastrografin reduces the duration of hospital stay in patients with adhesive small bowel obstruction that do not require surgery.
Implications for research.
Any further studies that attempt to show a benefit of Gastrografin in resolving adhesive small bowel obstruction without surgery will require very lage numbers as only a small minority of entered patients will come to surgery.
What's new
| Date | Event | Description |
|---|---|---|
| 5 May 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 1, 2004 Review first published: Issue 1, 2005
| Date | Event | Description |
|---|---|---|
| 6 March 2007 | New citation required and conclusions have changed | Substantive amendment |
Notes
This update was also published in British Journal of Surgery 2007 vol. 94 pp 404‐11
Acknowledgements
We want to thank Laura Mellor from Wiley and Sons Ltd. for a careful copy editing of the review. And to Henning Keinke Andersen, RGC of the CCCG, for his assistance throughout the entire review process.
Data and analyses
Comparison 1. Resolution or Laparotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Comparison of numbers of patients who had resolution of bowel obstruction without operation in both groups | 6 | 538 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.54, 1.21] |
1.1. Analysis.
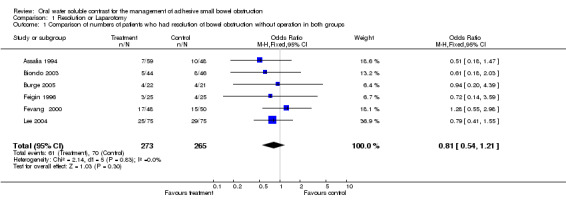
Comparison 1 Resolution or Laparotomy, Outcome 1 Comparison of numbers of patients who had resolution of bowel obstruction without operation in both groups.
Comparison 2. Hospital stay in days.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Length of hospital stay (in days) in both treatment and control group for non‐operated patients | 4 | 307 | Mean Difference (IV, Fixed, 95% CI) | ‐1.83 [‐2.21, ‐1.45] |
2.1. Analysis.
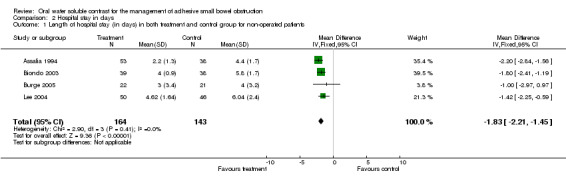
Comparison 2 Hospital stay in days, Outcome 1 Length of hospital stay (in days) in both treatment and control group for non‐operated patients.
Comparison 3. Strangulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of patients who had strangulation of small bowel in both groups | 6 | 538 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.22, 1.46] |
3.1. Analysis.
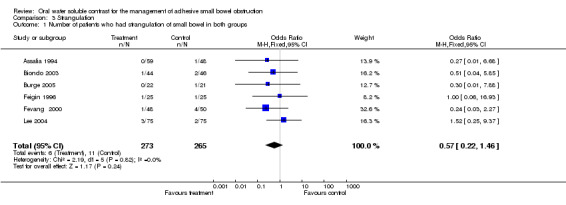
Comparison 3 Strangulation, Outcome 1 Number of patients who had strangulation of small bowel in both groups.
Comparison 4. Complications.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of patients who had complications in both treatment and control groups. | 6 | 538 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.61, 2.29] |
4.1. Analysis.
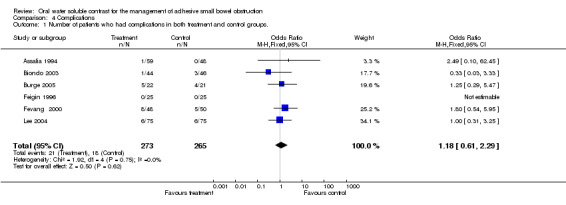
Comparison 4 Complications, Outcome 1 Number of patients who had complications in both treatment and control groups..
Comparison 5. Mortality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of patients who died in each group | 6 | 538 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.43, 4.38] |
5.1. Analysis.
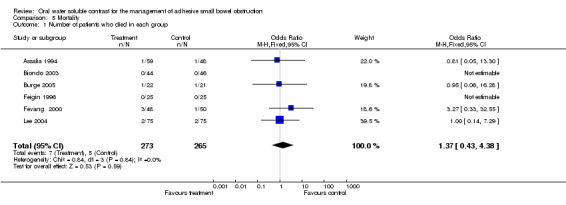
Comparison 5 Mortality, Outcome 1 Number of patients who died in each group.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Assalia 1994.
| Methods | A prospective randomised controlled trial | |
| Participants | Patients with adhesive small bowel obstruction. Patients with strangulation, primary small bowel obstruction, inflammatory bowel disease, and patients with hernia were excluded. | |
| Interventions | Trial group given 100 ml of gastrografin via nasogastric tube and the tube was clamped for 2‐3 hours. Both the trial and the control groups were treated with intravenous rehydration, abdominal x ray was taken after 6 hours, and all were clinically monitored. | |
| Outcomes | Resolution of the obstruction or the need for surgical intervention were compared in both groups as well as hospital stay. | |
| Notes | They excluded patients in whom no gas was seen in the colon on plain films that was taken on admission (ie patients with complete small bowel obstruction). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Biondo 2003.
| Methods | Randimised clinical trial | |
| Participants | Patients with symptoms and signs of small bowel obstruction who had previous abdominal surgery and presumed to have adhesive small bowel obstruction. | |
| Interventions | Patients were randomised for gastrografin orally, they were given 100 ml of gastrografin via a nasogastric tube, a radiograph was obtained after 24 hours. and a control group who were treated with intravenous rehydration and nasogastric suction. The gastografin group was further divided into those in whom the contrast was seen in the colon after 24 hours or not. | |
| Outcomes | The need for surgical intervention and length of hospital stay was compared between the two groups. In the Gastrografin group the arrival of the contrast to the colon after 24 hours was corelated with the success of the conservative treatment. | |
| Notes | Gastrografin group is suitable for analysis in the diagnosis arm ot the review. The entire study patients are suitable for the treatment analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Brochwicz 2003.
| Methods | Prospective randomised clinical trial. | |
| Participants | Patients with clinical and radiological diagnosis of adhesive small bowel obstruction. | |
| Interventions | Intervention group given 100ml of Gastrografin orally or via the naso‐gastric tube and abdominal radiograph was obtained after 90 and 240 minutes. | |
| Outcomes | Complete obstruction is diagnosed if the contrast failed to reach the colon after 240 minutes. | |
| Notes | More patients in the control group who did not receive Gastrografin had to have surgery which may indicate a therapeutic benefit from Gastrografin. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Burge 2005.
| Methods | Randomised controlled trial of the therapeutic role of gastrografin in adhesive smaal bowel obstruction | |
| Participants | Patients with small bowel obstruction caused by adhesions | |
| Interventions | Oral Gastrografin 100 ml compared with placebo | |
| Outcomes | Resolution of the obstruction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Chen 1998.
Chen 1999.
| Methods | Prospective | |
| Participants | Patients who were admitted to the hospital with late postoperative adhesive small bowel obstruction evident on clinical history and examination and confirmed with plain abdominal radiographs. | |
| Interventions | Patients were given 40 ml of urografin mixed with 40 ml of distilled water via a nasogastric tube.Serial plain abdominal radiographs were obtained at 2,4 and 8 hours. | |
| Outcomes | Patients whose plain films showed contrast medium in the ascending colon within 8 hours after urografin ingestion were given oral magnesium and cisapride followed by liquid diet then soft diet. Patients who showed failure of the urografin to empty into the colon within 8 hours underwent surgery or received non‐ operative treatment based on presence or abscence of any toxic signs including fever, constant pain, leucocytosis and peritonitis. | |
| Notes | All patients with contarst reaching the colon within 8 hours were allowed oral intake of fluid and given magnesium and cisapride. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Chung 1996.
| Methods | Prospective study | |
| Participants | Patients admitted to surgical unit with small bowel obstruction related to adhesions caused by previous abdominal surgery. | |
| Interventions | The stomach was emptied through a nasogastric tube, 50 ml of 76% Urografin was injected slowly through the nasogastric tube, a supine abdominal x ray was taken 4 hours later. | |
| Outcomes | The need for surgery or eventual resolution of bowel obstruction without surgery was decided on clinical basis, managing surgeon was blinded to the result of the contrast study. The need for surgical treatment was compared between the patients who had the contrast reaching the caecum after 4 hours and those in whom the contrast failed to reach the caecum after 4 hours. | |
| Notes | The study involved patients with primary small bowel obstruction, there were 2 patients with missed inguinal hernia, 2 obturator hernia, 2 with colon cancer, 2 obstruction by food bolus and 1 internal hernia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Feigin 1996.
| Methods | A prospective randomised clinical trial. Patients randomised to the usual conservative treatment of small bowel obstruction or given Gastrografin as well as the usual treatment. | |
| Participants | Patients who had previous abdominal surgery and presented with small bowel obstruction on clinical assessment and radiological examination. | |
| Interventions | All patients were treated by nasogastric suction and iv fluid. Patients in the Gastrografin group were given100 ml of water soluble contrast via nasogastric tube which was then clamped for 60 minutes. In either groups patients who developed signs of strangulation were operated on. | |
| Outcomes | Resolution of the obstruction or the need for surgery was compared in both groups as well as hospital stay and time from admission to resolution. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Fevang 2000.
| Methods | A prospective randomised study | |
| Participants | Patients with clinical and radiological evidence of small bowel obstruction. patients thought to have strangulation were excluded | |
| Interventions | Trial group given mixture of gastrografin and barium orally or through nasogastric tube. Control group was treated with nasogastric suction and iv fluid. | |
| Outcomes | The need for surgery, hospital stay, time between admission and resolution; and mortality were compared in both groups. | |
| Notes | Barium was mixed with gastrografin | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Joyce 1992.
| Methods | Prospective trial | |
| Participants | Patients with clinical and radiological evidence of small bowel obstruction. | |
| Interventions | A 100 ml single dose of Gastrografin was given via a nasogastric tube, the tube was then clamped. Supine abdominal radiographs were taken at 30 minutes and 4 hours. | |
| Outcomes | If the contrast passed to the large bowel a non‐operative course was followed. If there was clear cut‐off in contrast above the level of the large bowel by 4 hours the patients underwent laparotomy. | |
| Notes | Decision to operate was based on the contrast not reaching the large bowel. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Lee 2004.
| Methods | A prospective randomised study | |
| Participants | Patients who had previous abdominal surgery and presented with small bowel obstruction on clinical assessment and radiological examination. | |
| Interventions | All patients were treated by nasogastric suction and iv fluid. Patients in the Gastrografin group were given100 ml of water soluble contrast via nasogastric tube which was then clamped for 60 minutes. In either groups patients who developed signs of strangulation were operated on | |
| Outcomes | Resolution of the obstruction or the need for surgery was compared in both groups as well as hospital stay and time from admission to resolution. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Onoue 2002.
| Methods | Prospective clinical trial | |
| Participants | Patients who were admitted to the hospital with post‐operative adhesive small bowel obstrucrion. Patients with small bowel obstruction within 30 days of laparotomy, known malignancy, Crohn's disease and children below 15 years were excluded. | |
| Interventions | All patients were given 40 ml of Gastrografin mixed with 40 ml of water. Serial erect and supine abdominal x rays were taken at 4,8 16 and 24 hours. If earlier films had shown contrast in the ascending colon subsequent films were not taken. | |
| Outcomes | Patients who had contrast in the ascending colon within 24 hours were allowed to have oral fluids and soft diet subsequntly, and those in whom the contrast failed to reach the colon within 24 hours were either treated surgically or received long intestinal tube decompression. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anderson 1997 | This study investigated the role of barium in the diagnosis of complete or partial small bowel obstruction, it did not use water soluble contrast. The study does not address the questions of this review. |
| Blackmon 2000 | This study was excluded because it was a retrospective review |
| Chen 1998 | This was a duplicate paper where patients were included in Chen 1999. |
| Choi 2002 | In this study the authors treated patients conservatively for 48 hours and those who did not respond were randomised to either oral Gastrografin treatment or surgical intervention |
| Dunn 1984 | This study included patients with small bowel obstruction which is not related to previous surgery, some patients had colonic cancer or caecal lesions. Barium as well as water soluble contrast were used . |
| Enochsson 2001 | This was a retrospective study to evaluate the degree of small bowel obstruction, it used mixture of gastrografin and barium, the correlation with the need for surgery was not analysed. |
Contributions of authors
SAB will write the protocol and perform the search, choose the relevant papers, do critical appraisal of the papers, extract data and analyse the data, will write the final version of the review.
IPB will participate in crtitical appraisal of the papers, make contribution to inclusion and exclusion decision of papers, participate in the analysis of data.
BRP will oversee the review and participate in the final writing of the review
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
Assalia 1994 {published data only}
- Assalia A, Schein M, Kopelman D, Hirshberg A, Hashmonai M. Therapeutic effect of oral Gastrografin in adhesive, partial small‐bowel obstruction: a prospective randomised trial. Surgery 1994;115:433‐7. [PubMed] [Google Scholar]
Biondo 2003 {published data only}
- Biondo S, Pares D, Mora L, Marti J, Kreisler E, Jaurrieta E. Randomised clinical study of Gastrografin administration in patients with adhesive small bowel obstruction. Br J Surg 2003;90:542‐6. [DOI] [PubMed] [Google Scholar]
Brochwicz 2003 {published data only}
- Brochwicz‐Lewinski MJ, Paterson‐Brown S, Murchison JT. Small bowel obstruction‐the water‐soluble follow‐through revisted. Clin Radiol 2003;58:393‐7. [DOI] [PubMed] [Google Scholar]
Burge 2005 {published data only}
- Burge J, Abbas sm, Roadly G, Donald J, Connoly A, Bissett IP, Hill AG. Randomised controlled trial of gastrogrefin in adhesive small bowel obstruction. ANZ J Surg 2005;75:672‐674. [DOI] [PubMed] [Google Scholar]
Chen 1998 {published data only}
- Chen SC, Lin FY, Lee PH, YuSC, Wang SM, Chang KJ. Water‐soluble contrast study predicts the need for early surgery in adhesive small bowel obstruction. Br J Surg 1998;85:1692‐1694. [DOI] [PubMed] [Google Scholar]
Chen 1999 {published data only}
- Chen SC, Chang K J, Lee PH, et al. Oral urografphin in post operative small bowel obstruction. World J Surg 1999;23:1051‐4. [DOI] [PubMed] [Google Scholar]
Chung 1996 {published data only}
- Chung CC, Meng WCS, Yu SCH, Leung KL, Lau WY, Li AKC. A prospective study on the use of water‐soluble contrast follow‐through radiology in the management of small bowel obstruction. Aust NZ J Surg 1996;66:598‐601. [DOI] [PubMed] [Google Scholar]
Feigin 1996 {published data only}
- Feigin E, Seror D, Szold A, et al. Water‐soluble contrast material has no therapeutic effect on postoperative small bowel obstruction: results of a prospective, randomised clinical trial. Am J Surg 1996;171:227‐9. [DOI] [PubMed] [Google Scholar]
Fevang 2000 {published data only}
- Fevang BT, Jensen D, Fevang J, et al. Upper gastrointestinal contrast study in the management of small bowel obstruction, a prospective randomised study. Eur J Surg 2000;166:39‐43. [DOI] [PubMed] [Google Scholar]
Joyce 1992 {published data only}
- Joyce WP, Delaney PV, Gorey TF, Fitzpatrick JM. The value of water‐soluble contrast radiology in the management of acute small bowel obstruction. Ann R Coll Surg Engl 1992;74:422‐5. [PMC free article] [PubMed] [Google Scholar]
Lee 2004 {published data only}
- Lee JF‐Y, Meng WC‐S, Leung KL, Yu SC‐H, Poon CM, Lau WY. Water‐soluble contrast follow‐through in the management of adhesive small bowel obstruction: a prospective randomised trial. Annals of the College of Surgeons of Hong Kong 2004;8:120‐6. [Google Scholar]
Onoue 2002 {published data only}
- Onoue S, Katoh T, Shibata Y, Matsuo K, Suzuki M, Chigira H. The value of contrast radiology for postoperative adhesive small bowel obstruction. Hepatogastroenterology 2002;49:1576‐8. [PubMed] [Google Scholar]
References to studies excluded from this review
Anderson 1997 {published data only}
- Anderson CA, Humphrey WT. Contrast radiography in small bowel obstruction: a prospective randomised trial. Mil Med 1997;162:749‐52. [PubMed] [Google Scholar]
Blackmon 2000 {published data only}
- Blackmon S, Lucius C, Wilson JP, et al. The use of water‐soluble contrast in evaluating clinically equivocal small bowel obstruction.. Am Surg 2000;66:238‐42. [PubMed] [Google Scholar]
Chen 1998 {published data only}
- Chen sc, Lin FY, Lee PH, Yu SC, Chang KJ. Water‐soluble contrast study predicts the need for early surgery in adhesive small bowel obstruction. Br J Surg 1998;85:1692‐4. [DOI] [PubMed] [Google Scholar]
Choi 2002 {published data only}
- Choi HK, Chu KW, Law Wl. Therapeutic value of Gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment: a prospective randomised trial. Ann surg 2002;236:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunn 1984 {published data only}
- Dunn JT, Halls JM, Berne TV. Roentgenographic contrast studies in acute small bowel obstruction. Arch Surg 1984;119:1305‐8. [DOI] [PubMed] [Google Scholar]
Enochsson 2001 {published data only}
- Enochsson L, Runold M, Fenyo G. Contrast radiography in small intestinal obstruction, a valuable diagnostic tool. Eur J Surg 2001;167:120‐4. [DOI] [PubMed] [Google Scholar]
Additional references
Cox 1993
- Cox MR, Gunn IF, Eastman MC, et al. The safety and duration of non‐operative treatment of adhesive small bowel obstruction.. Aust NZ J Surg 1993;63:367‐71. [DOI] [PubMed] [Google Scholar]
Glauser 1999
- Glauser T, Savioz D, Grossholz M, Lupez‐Leuchi J, Robert J, Huber O, et al. Venous intravasation of Gastrografin, a serious but underestimated complication. Eur J Surg 1999;165:274‐277. [DOI] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomised clinical trials: is blinding necessary?. Control Clin Trials 1996;17:1‐12. [DOI] [PubMed] [Google Scholar]
Menzies 2000
- Menzies D, Parker M, Hoare R, Knight A. Small bowel obstruction due to postoperative adhesions: treatment patterns and associated costs in 110 hospital admissions. Ann R Coll Surg Engl 2000;180:40‐6. [PMC free article] [PubMed] [Google Scholar]
Miller 2000
- Miller G, Boman J, Shrier I. Gordon PH. Etiology of small bowel obstruction. Am J Surg 2000;180:33‐6. [DOI] [PubMed] [Google Scholar]
Moses 1993
- Moses LE, Shapiro D, Littenberg B. Combining independent studies of a diagnostic test into a summary ROC curve: data‐analytic approaches and some additional considerations.. Stat Med 1993;12:1293‐1316. [DOI] [PubMed] [Google Scholar]


