Abstract
Background
Initial arch wires are the first arch wires to be inserted into the fixed appliance at the beginning of orthodontic treatment and are used mainly for the alignment of teeth by correcting crowding and rotations. With a number of different types of orthodontic arch wires available for initial tooth alignment, it is important to understand which wire is most efficient, as well as which wires cause the least amount of root resorption and pain during the initial aligning stage of treatment. This is an update of the review 'Initial arch wires for alignment of crooked teeth with fixed orthodontic braces' first published in the Cochrane Database of Systematic Reviews 2010, Issue 4.
Objectives
To assess the effects of initial arch wires for alignment of teeth with fixed orthodontic braces in relation to alignment speed, root resorption and pain intensity.
Search methods
We searched the following electronic databases: the Cochrane Oral Health Group's Trials Register (to 2 August 2012), CENTRAL (The Cochrane Library 2012, Issue 7), MEDLINE via OVID (1950 to 2 August 2012) and EMBASE via OVID (1980 to 2 August 2012). We also searched the reference lists of relevant articles. There was no restriction with regard to publication status or language of publication. We contacted all authors of included studies to identify additional studies.
Selection criteria
We included randomised controlled trials (RCTs) of initial arch wires to align teeth with fixed orthodontic braces. Only studies involving participants with upper and/or lower full arch fixed orthodontic appliances were included.
Data collection and analysis
Two review authors were responsible for study selection, validity assessment and data extraction. All disagreements were resolved by discussion amongst the review team. Corresponding authors of included studies were contacted to obtain missing information.
Main results
Nine RCTs with 571 participants were included in this review. All trials were at high risk of bias and a number of methodological limitations were identified. All trials had at least one potentially confounding factor (such as bracket type, slot size, ligation method, extraction of teeth) which is likely to have influenced the outcome and was not controlled in the trial. None of the trials reported the important adverse outcome of root resorption.
Three groups of comparisons were made.
(1) Multistrand stainless steel initial arch wires compared to superelastic nickel titanium (NiTi) initial arch wires. There were four trials in this group, with different comparisons and outcomes reported at different times. No meta‐analysis was possible. There is insufficient evidence from these trials to determine whether or not there is a difference in either rate of alignment or pain between stainless steel and NiTi initial arch wires.
(2) Conventional (stabilised) NiTi initial arch wires compared to superelastic NiTi initial arch wires. There were two trials in this group, one reporting the outcome of alignment over 6 months and the other reporting pain over 1 week. There is insufficient evidence from these trials to determine whether or not there is any difference between conventional (stabilised) and superelastic NiTi initial arch wires with regard to either alignment or pain.
(3) Single‐strand superelastic NiTi initial arch wires compared to other NiTi (coaxial, copper NiTi (CuNiTi) or thermoelastic) initial arch wires. The three trials in this comparison each compared a different product against single‐strand superelastic NiTi. There is very weak unreliable evidence, based on one very small study (n = 24) at high risk of bias, that coaxial superelastic NiTi may produce greater tooth movement over 12 weeks, but no information on associated pain or root resorption. This result should be interpreted with caution until further research evidence is available. There is insufficient evidence to determine whether or not there is a difference between either thermoelastic or CuNiTi and superelastic NiTi initial arch wires.
Authors' conclusions
There is no reliable evidence from the trials included in this review that any specific initial arch wire material is better or worse than another with regard to speed of alignment or pain. There is no evidence at all about the effect of initial arch wire materials on the important adverse effect of root resorption. Further well‐designed and conducted, adequately‐powered, RCTs are required to determine whether the performance of initial arch wire materials as demonstrated in the laboratory, makes a clinically important difference to the alignment of teeth in the initial stage of orthodontic treatment in patients.
Keywords: Humans, Dental Alloys, Orthodontic Brackets, Orthodontic Brackets/standards, Orthodontic Wires, Orthodontic Wires/adverse effects, Orthodontic Wires/standards, Randomized Controlled Trials as Topic, Root Resorption, Root Resorption/etiology, Tooth Movement Techniques, Tooth Movement Techniques/adverse effects, Tooth Movement Techniques/instrumentation, Toothache, Toothache/etiology
Initial arch wires for tooth alignment in orthodontic treatment with fixed appliances
Orthodontic treatment is undertaken worldwide, mainly in adolescents and adults to correct crowded, rotated, buried or prominent front teeth. Fixed orthodontic appliances (braces) consist of brackets bonded to the teeth that are connected by arch wires which exert forces on the teeth. The first (initial) type of arch wire, inserted at the beginning of treatment, is for correcting crowding and rotations of teeth.
Over recent years a number of new materials (various metal alloys, or mixtures, of nickel and titanium (NiTi)) have been developed which show a range of different properties in the laboratory and which manufacturers claim offer benefits in terms of tooth alignment. Clinical trials of these products in people undergoing orthodontic treatment are required to understand whether different types of initial arch wires actually result in important differences, such as faster alignment, reduced pain or reduced side‐effects, during orthodontic treatment. The Cochrane Oral Health Group undertook this review of existing studies to identify and assess the evidence for the effects of initial arch wires of different materials, shape and size of cross‐section for alignment of teeth with fixed orthodontic braces in relation to alignment speed, root resorption and pain intensity.
The most recent search of studies was done on 2 August 2012. We found nine trials with 571 participants all of whom had upper and/or lower full arch fixed orthodontic appliances. The trials evaluated different initial arch wires, but all of these studies were poorly conducted and/or reported and the results are likely to be biased. All of the trials also varied in a number of other aspects of orthodontic treatment, compared different types of initial arch wires and reported different outcomes at different times. None of the trials reported both potential benefits (alignment) and harms (pain or side‐effects such as root resorption). There is no evidence from these studies that any particular initial arch wire material is better than another in people undergoing orthodontic treatment.
Summary of findings
Summary of findings for the main comparison.
Multistrand stainless steel compared with nickel titanium initial arch wires
| Multistrand stainless steel compared with nickel titanium initial arch wires | ||||||
|
Patient or population: Adolescents undergoing orthodontic treatment ‐ initial alignment phase Settings: University or private orthodontic clinic Intervention: Nickel titanium arch wires Comparison: Multistrand stainless steel initial arch wires | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Multistrand stainless steel | Nickel titanium | |||||
|
Tooth movement (follow‐up 6 weeks to 6 months) |
Not estimated | Not estimated | Meta‐analysis not possible | 3 studies (174 participants) | ⊕⊕⊝⊝ low1 | Trials reported different outcomes at different times and made slightly different comparisons. Substantial clinical heterogeneity |
| Pain (VAS) day 1 or day 7 | Not estimated | Not estimated | Meta‐analysis not possible | 1 study (42 participants) | ⊕⊝⊝⊝ very low2 | |
| Root resorption | Not reported | Not reported | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 All studies at high risk of bias 2 One small study at high risk of bias, lacks precision
Summary of findings 2.
Conventional (stabilised) nickel titanium arch wires compared with superelastic nickel titanium arch wires
| Conventional (stabilised) nickel titanium arch wires compared with superelastic nickel titanium arch wires | ||||||
|
Patient or population: Adolescents undergoing orthodontic treatment ‐ initial alignment phase Settings: University or private orthodontic clinics Intervention: Superelastic nickel titanium arch wires Comparison: Conventional (stabilised) nickel titanium arch wires | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional nickel titanium | Superelastic nickel titanium | |||||
|
Tooth movement (follow‐up 35 days) |
Not estimated | Not estimated | Meta‐analysis not possible (single study) | 1 study (40 participants) | ⊕⊝⊝⊝ very low1 | |
|
Pain (VAS) day 1 (follow‐up 7 days) |
Not estimated | Not estimated | Meta‐analysis not possible (single study) | 1 study (79 participants) | ⊕⊝⊝⊝ very low1 | |
| Root resorption | Not reported | Not reported | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 One small study at high risk of bias, lacks precision
Summary of findings 3.
Single‐strand superelastic nickel titanium compared with other nickel titanium arch wires
| Single‐strand superelastic nickel titanium compared with other nickel titanium arch wires | ||||||
|
Patient or population: Adolescents undergoing orthodontic treatment ‐ initial alignment phase Settings: University or private orthodontic clinics Intervention: Either coaxial, copper nickel titanium or thermoelastic nickel titanium arch wire Comparison: Single‐strand superelastic nickel titanium arch wire | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Superelastic single‐strand nickel titanium | Other nickel titanium | |||||
|
Alignment (mm/12 weeks) ‐ single‐strand superelastic NiTi versus coaxial NiTi (follow‐up 12 weeks) |
Not estimable | Not estimable | Meta‐analysis not possible (single study) | 1 study (24 participants) |
⊕⊝⊝⊝ very low1 | |
|
Alignment rate ratio ‐ single‐strand superelastic NiTi versus copper NiTi (follow‐up 6 months) |
Not estimable | Not estimable | Meta‐analysis not possible (single study) | 1 study (60 participants) |
⊕⊝⊝⊝ very low1 | |
|
Pain (VAS) day 1 & day 7 ‐ superelastic versus thermoelastic NiTi (follow‐up 7 days) |
Not estimable | Not estimable | Meta‐analysis not possible (single study) | 1 study (30 participants) |
⊕⊝⊝⊝ very low1 | |
| Root Resorption | Not reported | Not reported | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 One small study at high risk of bias, poor precision
Background
Description of the condition
Contemporary orthodontic treatment involves the use of both fixed and removable appliances. In recent years, it has been shown that the quality of the results obtained with fixed orthodontic appliances is superior to that obtained with removable orthodontic appliances (O'Brien 1993; Richmond 1993). Treatment with fixed orthodontic appliances has therefore become dominant in orthodontic practice throughout the world.
Orthodontic treatment is mainly carried out for adolescents and adults, and is concerned primarily with correcting crowded, rotated, buried and/or prominent front teeth. Epidemiological investigation reveals that 77% in northeast Brazil (Marques 2007) and 29% in Nairobi (Ng'ang'a 1997) of 13‐ to 15‐year old adolescents have either a moderate or great need for orthodontic treatment. It is also reported that over 52.3% of 12‐year old children in South Africa have an identifiable malocclusion (van Wyk 2005), and 23.5% of the 12‐year olds and 18.5% of 15‐ to 16‐year olds in Spain have a definite treatment need (Manzanera 2009). However, adults also demand and/or need orthodontic treatment and now comprise up to almost 25% of cases in US orthodontic practices (Keim 2002).
Description of the intervention
Fixed orthodontic appliance treatment uses arch wires to exert force upon teeth.
Treatment is carried out in stages and selection of appropriate arch wires contribute to the treatment success. There is no one arch wire ideal for all stages of fixed appliance treatment. The initial arch wire is the first arch wire to be inserted into the fixed appliance at the beginning of the treatment and is used mainly for correcting crowding and tooth rotations. This usually takes about 10 weeks but can be up to 20 weeks where teeth are very irregular. There is general agreement that light, continuous forces (also known as optimal forces) are the most desirable to achieve controlled and predictable tooth movement with minimum harm to the teeth and supporting tissues (Ballard 2009; Burstone 1981; Burstone 1985; Linge 1991). Clinically, this means that optimal forces result in the maximum speed of tooth movement with the minimum of root resorption and/or pain for the patient.
The forces delivered by the arch wires depend largely on the physical properties of the wire material and dimension of the wire. The initial arch wires must be biocompatible and ideally have:
low stiffness to deliver light forces on activation;
good range to be able to maximise activations so there is elastic behaviour over weeks to months;
high strength and resistance to permanent deformation;
ease of engagement within fixed appliance attachments within a reasonable time scale;
low cost (Kapila 1989; Proffit 2000).
The performance of arch wires is determined not only by the material properties but also by geometric factors, such as the cross‐sectional shape (whether the arch wire is circular, rectangular, or square), length (i.e. interbracket span) and diameter. It is a general rule that for a certain material, as the diameter of a wire decreases, its strength decreases while conversely as diameter increases, its stiffness increases. There has been an evolution of the materials available to apply forces to teeth (Evans 1996; Kusy 1997; Kusy 2007; Quintão 2009). The earliest wires were judged by their structural properties i.e. strength and flexibility. Wire size and shape then became more important as the stiffness of materials available at that time were virtually identical. Now it is possible to have wires which are the same size and shape, but of variable stiffness because of the mechanical properties of their constituent materials.
Precious metal alloys (e.g. gold) were historically used for the fabrication of initial arch wires for many years but high material costs limited their use and they are now virtually obsolete in orthodontics. Stainless steel replaced gold, offering comparatively good strength and springiness, corrosion resistance and low cost. Stainless steel arch wires can be bent to almost any desired shape without breaking. Increasing the length of wire using loops increases the flexibility of the arch wire to enable use as an initial aligning arch wire. This can be time consuming as each wire must be customised, by the orthodontist, for the individual patient. Another method of increasing the flexibility of stainless steel arch wires was the development of a multistrand wire. Multistrand wires are generated by twisting two or more strands of a small diameter wire (≤ 0.01 inch), therefore turning a springy wire into a cable. Among stainless steel wires, multistrand wires offer an impressive combination of strength and spring qualities. The properties of multistrand wires depend both on the characteristics of the individual wire strands and on how tightly they have been woven together during their manufacture (Proffit 2000).
The developments in nickel‐titanium (NiTi) wire technology have resulted in a decline in the popularity of stainless steel wires for initial alignment. Stainless steel arch wires are still used by a small proportion of orthodontists. NiTi is a metal alloy which can exist in two different crystalline or lattice forms namely the martensitic (M) form and the austenitic (A) form. Each has its own physical and mechanical properties. Transition between the two forms or phases can be induced by applied stress or a change in temperature and this changes the properties of the wire without affecting the integrity of the wire. Alternatively a NiTi alloy can be manufactured in a stable form, so that there is no possibility of phase transition. Wires manufactured as the active form have both phases existing simultaneously in variable proportions. It is the ability of the two phases to coexist which gives rise to the superelastic properties of active NiTi alloys. Superelasticity (also known as plateau behaviour) means that wires exert about the same force irrespective of whether they are deflected either a relatively small or large distance, which is a unique and extremely desirable characteristic, especially in initial aligning arch wires. The temperature at which the alloy converts from one phase to another is known as the transition temperature (TTR) and this can be preset during manufacturing.
It is important to have an understanding of the transitions which NiTi materials undergo to make full use of the benefits of these properties (Santoro 2001; Santoro 2001a). Austenite is the high temperature form of the alloy and is able to memorise a preformed shape. When a wire is predominantly austenite it behaves more elastically than stainless steel but is not superelastic. To activate superelasticity requires the formation of the martensite form. This is the low temperature form of the alloy and is easily pliable. It is generated by cooling below the TTR but can be helped by deflecting the wire at least 2 mm. This is called stress induced martensitic transformation (SIM). However, this SIM raises the preset TTR. For maximum clinical effectiveness the TTR should be set near to or just below mouth temperature, but TTR should be calculated under proper conditions of deflection to take into account the conditions experienced during clinical use.
NiTi wires can be classified according to the crystal structure and phase transformation as follows (Evans 1996).
Stabilised e.g. Nitinol, Titanal and Orthonol.
Superelastic active austenitic e.g. Sentalloy.
Thermodynamic‐active martensitic e.g. copper NiTi (CuNiTi).
Graded thermodynamic e.g. Bioforce.
At the clinical level, the elastic properties of NiTi are independent of whether it is operating clinically in the austenitic or super elastic plateau. It is likely that, in clinical use, many superelastic wires do not exhibit superelastic or plateau behaviour or require excessive deflection to do so. They may also be delivering excessive force even in the presence of plateau behaviour (Santoro 2001a). Despite commercial claims, low values of force delivery remain theoretical from in vitro testing for most NiTi alloys (Santoro 2001). These need to be verified through properly designed clinical trials taking into account the temperature range of testing, method of ligation, interbracket distance, bracket type and length of wire.
The selection of an appropriate NiTi wire can be difficult. There is often a lack of accurate information about expected TTRs. This is compounded by variation in properties between batches from the same manufacturer and between different manufacturers for supposedly similar wires. There also needs to be better clarity about product terminology with reference to standard or approved definitions in order to make meaningful comparisons and substantiate manufacturers claims of improved clinical performance of the bewildering array of new products offered to the orthodontist.
How the intervention might work
Manufacturers of arch wires claim that arch wire materials have specific properties, determined by laboratory testing, that make them ideal for use in clinical orthodontics. However, as described above there are a number of factors which may be expected to influence the performance of any given arch wire in clinical use. The type of wire and the properties produced during manufacture, the type and size of brackets used, the distance between brackets, the degree of initial 'misalignment' of the teeth and the duration of treatment may all influence the success of orthodontic treatment.
Manufacturers' claims of increased efficiency of the newer arch wire alloys are used to justify their increased cost. NiTi arch wires have many theoretical advantages over other wire types for the initial alignment of teeth. Perhaps the most important is that superelastic NiTi arch wires are said to exert the same force irrespective of whether they are deflected a little or a lot which is particularly valuable in the initial alignment stage.
Why it is important to do this review
There is an abundant literature of studies which support manufacturers' claims concerning the performance of various arch wire types in a controlled laboratory environment. However, for orthodontists and their patients, the performance of these materials in vivo is much more important. Early clinical trials failed to demonstrate improved alignment associated with the new arch wire materials. There is a need for a systematic review to critically appraise and summarise the results of clinical trials comparing the effects of different materials used for initial arch wires. With a number of orthodontic arch wires available for initial tooth alignment, it is important to understand which wire is most efficient in terms of rate of alignment, as well as which wire causes the least amount of root resorption and pain during the initial aligning stage of orthodontic treatment.
Objectives
To assess the effects of initial arch wires for the alignment of teeth with fixed orthodontic braces, in terms of:
the speed of initial tooth alignment;
the amount of root resorption accompanying tooth movement; and
the intensity of pain experienced by patients during the initial alignment stage of treatment.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) in this review.
Types of participants
We included participants with upper and/or lower full arch fixed orthodontic appliances. We excluded participants with palatal expansion devices or extraoral appliances, which were being used concurrently. We also excluded participants who had previous active orthodontic treatment or relevant medical history.
Types of interventions
Initial arch wires are the first arch wires inserted into fixed orthodontic appliances at the beginning of treatment. This excludes arch wires used at subsequent orthodontic appointments. The comparisons between arch wires of different materials and sizes were undertaken in terms of:
the material of the arch wires;
the cross‐sectional shape of the arch wires; and
the cross‐sectional size of the arch wires.
Types of outcome measures
Primary outcomes
The alignment rate per month.
The incidence/prevalence and amount of root resorption.
Secondary outcomes
Time to next/working arch wire.
Time to alignment.
The intensity of pain experienced by patients measured on a visual analogue scale (VAS), and/or categorical scale and duration of pain. Pain scores were assessed at specific time points i.e. after the initial arch wires were inserted.
Search methods for identification of studies
Electronic searches
Search strategies were developed for each database to identify studies in conjunction with the Cochrane Oral Health Group Trials Search Co‐ordinator. These were based on the search strategy developed for MEDLINE (OVID) but revised for individual databases. A comprehensive search was carried out irrespective of the publication language. Papers not in English were included if they could be translated. The MEDLINE search strategy used a combination of controlled vocabulary and free text terms and was run with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] (Higgins 2011).
The following electronic databases were searched.
MEDLINE via OVID (1950 to 2 August 2012) (Appendix 1).
Cochrane Oral Health Group's Trials Register (to 2 August 2012) (Appendix 2).
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 7) (Appendix 3).
EMBASE via OVID (1980 to 2 August 2012) (Appendix 4).
Searching other resources
Grey literature
We searched conference proceedings and abstracts from the British Orthodontic Conference (to 2012), European Orthodontic Conference (to 2012) and the International Association for Dental Research via IADR Abstract Search Form (http://iadr.confex.com/iadr/search.epl, to 2012).
Handsearching
Handsearching of the following journals was carried out as part of The Cochrane Collaboration's handsearching programme (updated to the following issues).
American Journal of Orthodontics and Dentofacial Orthopedics (to 2012;153(1))
The Angle Orthodontist (to 2011;81(6))
European Journal of Orthodontics (to 2011;33(6))
Journal of Orthodontics (and the predecessor, the British Journal of Orthodontics) (to 2011;38(4)).
In addition, the following journals were handsearched from their inception to the following issues.
Seminars in Orthodontics (from 1995 to 2011;17(4))
Clinical Orthodontics and Research (from 1998 to 2011;14(4))
Australian Orthodontic Journal (from 1956 to 2011;27(2)).
Reference lists
We checked the reference lists of potential clinical trials to identify any additional studies.
Correspondence
We contacted the corresponding authors of all included trials in an attempt to identify unpublished or ongoing studies and to clarify trial details, if required. We contacted manufacturers to confirm the type of arch wires and also asked about their knowledge of any unpublished and/or ongoing clinical trials.
Data collection and analysis
Selection of studies
Two review authors independently assessed the titles and abstracts (when available) of all reports identified by the search strategies as being potentially relevant to the review. The full reports were then obtained for all studies which appeared to meet the inclusion criteria or if there was insufficient information to make a clear decision or where there was disagreement between the review authors about eligibility. The full reports were assessed to verify whether the studies met the inclusion criteria. Any disagreements between the two review authors were resolved by discussion or the involvement of another review author as an arbiter. A record of all decisions made about the identified studies was kept. The review authors were not blinded to author(s), institution or site of publication of all studies.
We used the following screening exclusion criteria.
Studies other than RCTs.
Studies not investigating fixed appliance orthodontic treatment.
Studies not investigating initial arch wire interventions, including those with multiple wires as part of a sequence.
Data extraction and management
Two review authors carried out data extraction independently and in duplicate. All disagreements were resolved by discussion with one of the other review authors in the team.
We collected the following data on a customised data collection form.
Date that the study was conducted.
Year of publication.
Treatments including details of material, size and brand of arch wire and type of fixed orthodontic appliances that were used.
Duration of follow‐up.
Sample size and the number of male subjects and female subjects per study group.
Age of subjects.
Outcome measures.
Data on cost of arch wire and amount of time for arch wire placement were recorded.
Assessment of risk of bias in included studies
The assessment of the risk of bias in each of the included studies was undertaken independently by two review authors. Disagreements were resolved by discussion or the involvement of another review author. This was carried out using The Cochrane Collaboration's tool for assessing risk of bias and a 'Risk of bias' table was completed for each study as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Seven domains, namely sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other sources of bias were assessed according to the tool. Each domain included one or more specific entries in a 'Risk of bias' table. Within each entry, what was reported in the study was described and a judgement relating to the risk of bias for that entry was assigned. Where the study clearly reports methodology, a judgment of 'Low risk' of bias or 'High risk' of bias will be made. Where trial methodology is unclear, a domain may be judged at 'Unclear risk' of bias unless and until further information is available.
After taking into account the additional information provided by the authors of the trials, the overall risk of bias in included studies was assessed over all seven domains. Studies were graded into the following categories.
Low risk of bias (plausible bias unlikely to seriously alter the results).
Moderate risk of bias (plausible bias that raises some doubt about the results).
High risk of bias (plausible bias that seriously weakens confidence in the results).
Measures of treatment effect
The statistical procedures outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) were planned to be followed and the data were planned to be analysed using Review Manager (RevMan) software and reported according to Cochrane Collaboration criteria. Risk ratios and corresponding 95% confidence intervals were calculated for dichotomous data. The mean difference and 95% confidence intervals were calculated for the continuous data.
Unit of analysis issues
Most included trials randomised participants to different types of initial arch wires. However, where the unit of randomisation is a dental arch, and a participant may contribute more than one dental arch to the study, there is potential for unit of analysis errors to occur. If this is unclear, we planned to ask authors to clarify how this dependence had been accounted for in the analysis. If no adjustment had been made we would have taken this into account in interpreting the confidence interval of the effect size (Whiting‐O'Keefe 1984).
Where repeated measures were made (e.g. pain measurements over several days), we chose to report only pain outcomes on days 1 and 7 as these time points are likely to provide clinically meaningful data.
Dealing with missing data
We contacted the original investigators of the studies to request the missing data or identify the reason for missing data. However, due to the absence of individual participant data, it was impossible to undertake an intention‐to‐treat analysis.
Assessment of heterogeneity
Although assessment of heterogeneity was planned, Cochran's test for heterogeneity was not appropriate as no meta‐analyses were undertaken.
Assessment of reporting biases
Although assessment of reporting biases was planned, it was not appropriate to use funnel plots to assess publication bias along with the statistical methods described by Egger 1997, because no meta‐analyses were undertaken.
Data synthesis
Meta‐analyses were planned, but they were not possible because the included studies involved a variety of interventions. For the included trials, mean differences with 95% confidence intervals were planned to be calculated for continuous outcomes, and risk ratios with 95% confidence intervals were calculated for dichotomous outcomes. The fixed‐effect model was planned to be used in meta‐analyses of less than four trials, and the random‐effects model where there were more than four trials.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis was proposed for different age groups. However, we were unable to undertake a meta‐analysis, so subgroup analysis was not possible.
Sensitivity analysis
Although sensitivity analysis was planned to examine the effect of risk of bias on the assessment of the overall estimates of effect, this could not be done since no meta‐analyses were undertaken.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
The search in December 2011 identified 733 publications. After removing the duplicates 365 publications were left. 342 were excluded after reviewing the title and/or abstract. Full text copies were obtained for the remaining 23 studies. From these, six publications proved ineligible and were excluded. Corresponding authors were contacted for further information in relation to the 17 reports. Seven of these publications were excluded, because they were confirmed not to be randomised controlled trials (RCTs) by the corresponding authors, two were published as conference abstracts with insufficient information to include in the review, and further information was not available from the contact authors. One has been identified as an ongoing study after contacting the corresponding author and after discussing the study among the review team and with the Cochrane Oral Health Group. Seven of these trials met the inclusion criteria for the review.
The search was updated in August 2012 and an additional 294 references were then screened by two review authors. Two additional RCTs were identified which met the inclusion criteria (Cioffi 2012; Sebastian 2012). The ongoing study Bernhold 2001 was excluded after attempts to contact the author or identify a subsequent publication related to this abstract failed. Therefore, a total of nine RCTs (Cioffi 2012; Cobb 1998; Evans 1998; Fernandes 1998; Jones 1992; O'Brien 1990; Pandis 2009; Sebastian 2012; West 1995) fulfilled all the criteria for inclusion.
For details of the studies that were examined and the reasons for inclusion or exclusion please see Characteristics of included studies and Characteristics of excluded studies tables.
Included studies
Characteristics of the trial design
Seven of the nine included studies were parallel group studies and one was a factorial study (Evans 1998). In the study by Cobb 1998, participants were firstly allocated to 0.018 or 0.022 inch fixed orthodontic braces according to the preference of the operators, and then participants in each block were allocated randomly to three types of arch wires.
In five of the trials (Cioffi 2012; Evans 1998; Fernandes 1998; Jones 1992; West 1995), upper and/or lower dental arches were randomly allocated to either an experimental or control arch wire, and in the majority of participants only one arch was treated. In the study by O'Brien 1990, only upper arches were included and in the studies by Pandis 2009 and Sebastian 2012 only lower arches were randomly allocated to different arch wires.
Two of the trials reported external funding sources (Cobb 1998; Evans 1998), one trial reported an internal funding source (Cioffi 2012), while the other six did not report any information concerning funding of the trial.
Characteristics of the trial setting
Of the nine included trials, four were conducted in the UK (Evans 1998; Jones 1992; O'Brien 1990; West 1995), one in the USA (Cobb 1998), one in Norway (Fernandes 1998), one in Greece (Pandis 2009), one in India (Sebastian 2012) and one in Italy (Cioffi 2012). Three studies had more than one publication (Jones 1992; O'Brien 1990; West 1995).
Six studies were conducted in a university hospital clinic (Cioffi 2012; Evans 1998; Jones 1992; O'Brien 1990; Sebastian 2012; West 1995), one was set in a graduate clinic or faculty practice (Cobb 1998), one in a private practice setting (Pandis 2009) and one in both hospital and private practice (Fernandes 1998).
Characteristics of the trial participants
The nine included studies randomised a total of 571 patients (671 arches) to different arch wires. Eight of the included studies had clear inclusion/exclusion criteria for the selection of participants, but one study did not report any inclusion or exclusion criteria (O'Brien 1990). All the included studies reported participant age, with only one trial including adults (older than 18 years) (Cobb 1998). The gender of trial participants was stated in six trials (Cioffi 2012; Fernandes 1998; Jones 1992;Pandis 2009; Sebastian 2012; West 1995), and one trial recruited only female participants (Sebastian 2012).
Sample sizes
The sample sizes ranged from 30 to 128 patients or 30 to 158 arches. Six studies reported an a priori sample size calculation. Four of these planned the sample sizes on the basis of previous (pilot) studies in order to detect significant differences between two parallel groups (Evans 1998; Jones 1992; West 1995; Sebastian 2012), and one calculated the sample size based on a time‐to‐event analysis to detect a 45% difference (Pandis 2009). Cioffi 2012 based the power calculation on data concerning pain perception measured on a VAS for pain intensity in the temporomandibular joint area (Kropmans 1999).
The sample size was not consistent throughout the study report of Cobb 1998, and the number of either patients or arches allocated to each intervention group was not reported by Evans 1998. However, in this trial a total of 98 arches in 51 participants were evaluated at the end of the study. The trial by O'Brien 1990 was small and no sample size calculation was reported. It is possible that this study lacks statistical power.
Characteristics of the trial interventions
The nine included studies evaluated different arch wire materials and diameters, placed with different types and sizes of brackets, and reported different outcomes, measured in different ways, at different time points. As a result no comparisons and outcomes could be combined in meta‐analysis. It was difficult to place the arch wires used in the included trials into groups because there was little information reported about the specific characteristics of each arch wire material, possibly due to the commercial sensitivity of such detailed information. For this reason we have noted all the available information, including the tradenames in the 'Characteristics of included studies' table.
The following comparisons were made.
Multistrand stainless steel versus
Superelastic NiTi (Cobb 1998; Jones 1992; West 1995)
Superelastic ion implanted NiTi (Cobb 1998)
Thermally activated NiTi (Evans 1998).
-
Stabilised NiTi versus
Superelastic NiTi (Fernandes 1998; O'Brien 1990).
-
Superelastic single stranded NiTi versus
Superelastic multistranded NiTi (Sebastian 2012)
Copper NiTi (Pandis 2009)
Thermoelastic NiTi (Cioffi 2012).
All of the trials compared two or more types of round wires apart from the Evans 1998 study where both types of wires were 0.016 x 0.022 inch and rectangular in cross‐section.
Characteristics of the trial outcomes
Alignment rate per month
This outcome was measured in five of the included studies (Cobb 1998; Evans 1998; O'Brien 1990; Sebastian 2012; West 1995).
Cobb 1998 measured anterior irregularity each month following arch wire placement but presented results in graphs only and did not report data for rate of alignment.
The study by Evans 1998 used a factorial design in which arches were randomly allocated to different arch wire types. This trial reported tooth movement after 4 and 8 weeks of treatment as mm moved by contact point for each wire. However, due to the design used, we would have expected data to be analysed taking into account the pair of arch wires in each patient and which arch each wire was on. The report states the mean movement for each wire as if this were independent of other confounding factors.
West 1995 reported mean duration of the trial for each wire, with 95% confidence intervals, but in the absence of a clearly defined endpoint for the trial we were unable to interpret this as time to alignment. Alignment is reported as an index of tooth alignment (NiTi/Stainless steel).
O'Brien 1990 reported the rate of alignment in terms of the three‐dimensional contact point movements of the upper anterior arches over a period of 35 days.
Alignment associated with two different NiTi arch wires was reported by Sebastian 2012 after 4, 8 and 12 weeks.
Root resorption
None of the trials included in this systematic review reported this important outcome.
Time to next/working arch wire
This outcome was measured in one of the included trials which reported time to next working arch wire for each wire type but did not appear to adjust for the paired nature of the data and did not present any estimates of variance (Evans 1998).
Time to alignment
The trial by Cobb 1998 measured time to alignment, and defined alignment as an Irregularity Index of 2 mm or less. However, no numerical data were reported (graphs only).
Mean time to alignment was reported by Pandis 2009 for the comparison between conventional NiTi and CuNiTi arch wires.
Pain
Three of the nine trials reported pain as an outcome, daily over the 7 days following arch wire placement (Cioffi 2012; Fernandes 1998; Jones 1992). However, each of these trials compared different arch wires. None of these trials reported on the 'benefits' of the arch wires (with regard to their role in alignment) relative to the associated pain.
The remaining six included trials, which reported some measure of tooth movement associated with each arch wire type, did not report associated pain.
Excluded studies
Seven studies were excluded because examination of the full papers indicated that they were not RCTs (Dalstra 2004; Huffman 1983; Jones 1984; Jones 1990; Kuftinec 1980; Lew 1988; Weiland 2003). Two studies were excluded because the intervention was an arch wire sequence rather than an initial arch wire (Mandall 2006; Ong 2011), and in four studies the interventions were not initial arch wires for alignment (AlQabandi 1999; Fleming 2009; Fleming 2009a; Pandis 2007). Two studies were published only as abstracts and attempts to obtain either a full report or additional information from the authors were unsuccessful (Bloom 1998; Chekay 1999).
One ongoing study from the previous version of this review was excluded from this update (Bernhold 2001). This study was published as an abstract and attempts to contact the author were unsuccessful, but the abstract contained insufficient information to include in this review.
Risk of bias in included studies
The summary of risk of bias in included studies was shown in Figure 1, and the details were shown in the risk of bias table of the Characteristics of included studies.
Figure 1.
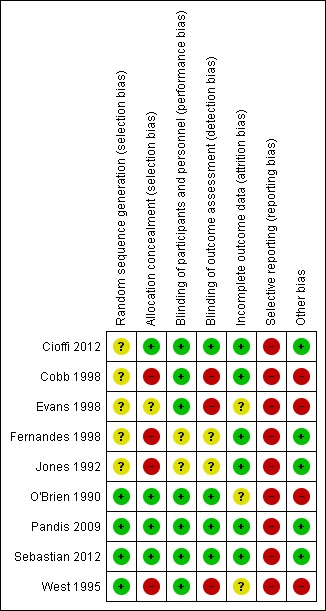
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation
The method of sequence generation is clearly described in the reports of three trials (Pandis 2009; Sebastian 2012; West 1995), and this information was provided on request by the lead author of one trial (O'Brien 1990). These four trials are assessed as being at low risk of bias for this domain. In the remaining five trials, there was no information provided on the method of sequence generation and this domain was therefore assessed at unclear risk of bias.
Allocation concealment
Allocation concealment was clearly described in three trials (Cioffi 2012; Pandis 2009; Sebastian 2012), and information was provided by the author in one trial (O'Brien 1990), so these four trials were assessed as low risk of bias for this domain. The trial report by Evans 1998 did not mention allocation concealment but the dissertation refers to a "sealed nested envelope technique" so this domain has been assessed as unclear. The remaining four trials did not mention allocation concealment in their methods, and it is likely that the operators conducted the allocation. Therefore these were assessed at high risk of bias.
Three trials (O'Brien 1990; Pandis 2009; Sebastian 2012) are at low risk of selection bias, Cioffi 2012 is at unclear risk of selection bias, and the remaining five trials are at high risk of selection bias.
Blinding
Blinding of participants
Blinding of participants is likely to be important in terms of reducing performance bias in the trials where the outcome is the somewhat subjective outcome of participant reported pain, but only one trial reported participant blinding and is at low risk of bias for this domain (Cioffi 2012); the other two trials that reported pain outcomes did not report participant blinding, so they were assessed at unclear risk of bias for this domain (Fernandes 1998; Jones 1992). The remaining six trials were assessed at low risk of bias for participant blinding because the measurement of alignment outcomes is objective and unlikely to have been biased.
Blinding of outcome assessors
Blinding of outcome assessment was clearly reported in three studies (Cioffi 2012; Pandis 2009; Sebastian 2012), and the author supplied this information in O'Brien 1990, so these three trials were assessed as being at low risk of performance and detection bias. For the trials which reported participant pain outcomes, two were unblinded (Fernandes 1998; Jones 1992) and were at unclear risk of performance and detection bias; one trial reports blinding of the assessor for statistical analyses and is at low risk of performance and detection bias (Cioffi 2012). In the remaining three trials (Cobb 1998; Evans 1998; West 1995), there was no mention of blinding of outcome assessors and we consider it likely that the operators conducted the outcome assessment. For this reason, these are assessed at high risk of performance and detection bias.
Incomplete outcome data
In three trials (Cioffi 2012; Pandis 2009; Sebastian 2012), all randomised participants were included in the outcome evaluations. In a further three trials (Cobb 1998; Fernandes 1998; Jones 1992), the numbers of participants excluded from analysis were very low. The risk of attrition bias was considered to be low in these six trials.
In the remaining three trials (Evans 1998; O'Brien 1990; West 1995), the numbers of trial participants included in the outcome evaluation is not reported and these trials were therefore assessed at unclear risk of attrition bias.
Selective reporting
Selective outcome reporting was a major source of bias in all of the studies in this review. Three studies which reported pain outcomes associated the use of with different arch wires did not report the effects of these wires in terms of alignment (Cioffi 2012; Fernandes 1998; Jones 1992). In the report by O'Brien 1990, the pain data that were recorded during the investigation were not reported since the researchers found these "not to be sufficiently reliable for analysis". Cobb 1998 and West 1995 reported outcomes as graphical figures only without any numerical data. Evans 1998 reported means with no estimates of variance. Pandis 2009 and Sebastian 2012 both reported the effects of the arch wires in terms of alignment but neither reported pain or adverse effects. All nine trials were assessed at high risk of selective reporting bias.
Other potential sources of bias
Four studies carried out a comparison to assess comparability of the experimental groups at baseline, and found no differences between randomised groups (Cioffi 2012; Jones 1992; Pandis 2009; Sebastian 2012).
One of the principles of randomised trials is that the groups created by random allocation should be the same in all respects apart from the intervention of interest. Post randomisation variation between individuals in aspects of treatments which may affect the outcomes are therefore potential sources of bias.
There was variation in the different bracket types used, in the distribution of brackets to mandibular and maxillary arches, and in the types of edgewise appliances used, which may have introduced additional bias in Cobb 1998. In this study, there was a unit of analysis error in that randomisation occurred at the participant level and analysis at the arch level.
Variation in the type of fixed appliance and types of ligatures used was also an issue in the trial by Evans 1998, and there are no data reported describing how these were distributed in each arch wire group. There is also a potential issue of bias in this study related to possible interaction between different types of wires in the same participant.
West 1995 reported that the steel wire group had a higher summed index of tooth alignment (ITA) at baseline, and also in this trial there was a potential for different effects in participants with two different arch wire types, compared to those with two arch wires of the same type, or participants with only one arch wire. Different ligation systems were chosen by each of the clinicians and there is no information reported concerning the distribution of ligation systems in each group in this trial. This trial included more arch wires than participants and it is unclear whether this was accounted for in the analysis.
O'Brien 1990 did not report clear inclusion and exclusion criteria, conducted a very small study, and did not report baseline comparability. It is possible that the groups in this study were different at baseline and that the study was underpowered.
These four studies were assessed at high risk of other bias (Cobb 1998; Evans 1998; O'Brien 1990; West 1995). We identified no other sources of bias in the five remaining studies, and they were assessed at low risk of other bias (Cioffi 2012; Fernandes 1998; Jones 1992; Pandis 2009; Sebastian 2012).
Overall risk of bias
All of the trials included in this review have at least one domain assessed at high risk of bias and they are all therefore considered to be at high risk of bias overall.
Effects of interventions
See: Table 1; Table 2; Table 3
We have placed the arch wires evaluated in the included studies into three groups according to the materials used in the arch wires being compared.
In the first group are the trials where newer NiTi arch wires of various types are compared to conventional multistrand stainless steel (StSt) initial arch wires (Cobb 1998; Evans 1998; Jones 1992; West 1995).
The second group compares stabilised conventional NiTi arch wires with superelastic NiTi arch wires of various types (Fernandes 1998; O'Brien 1990).
The third group compares superelastic NiTi with either multistrand NiTi (Sebastian 2012), CuNiTi (Pandis 2009), or thermoelastic NiTi (Cioffi 2012).
1. Multistrand stainless steel
There are four trials in this group which all made different comparisons and reported different outcomes (Table 1).
One three‐arm trial compared 0.0175 inch multistrand stainless steel wire (Wildcat) to 0.016 inch Austenitic‐NiTi wire (Sentalloy) or the same 0.016 inch Austenitic‐NiTi wire with surface ion implantation (Cobb 1998).
Cobb 1998 measured both alignment rate per month and time to next working arch wire but reported outcomes only as graphical figures, with no numerical data reported. The outcomes of root resorption, time to alignment and pain were not reported. There was a unit of analysis error in this study in that randomisation was at the participant level and outcome was reported at the arch level. There was also differences in the type of appliances used but this was stratified in the randomisation. The paper reported that there was no statistically significant difference between the three arch wires in rate of alignment, but given the unit of analysis error this result must be interpreted with caution.
Two trials in this group compared multistrand stainless steel with superelastic NiTi.
Jones 1992 compared 0.015 inch multistrand stainless steel wire (Twistflex) with 0.014 inch superelastic NiTi wire (heavy Japanese NiTi).
West 1995 compared 0.0155 inch multistrand stainless steel wire (Dentaflex) with 0.014 inch superelastic NiTi wire (NiTi).
Jones 1992 did not report alignment rate per month, time to working arch wire, time to alignment, or root resorption. The outcome reported was the intensity of pain/discomfort experienced by patients over 15‐day period after placement of an initial arch wire, measured by VAS scores and consumption of analgesics. Though only part of the outcome data (VAS 1 to 7 days) were reported in detail, other studies have shown that pain levels generally return to baseline levels at 6 or 7 days after the initial wires are placed (Erdinç 2004; Firestone 1999; Ngan 1989; Scheurer 1996), which suggests that any differences in pain/discomfort between intervention groups are likely to be minimal after 7 days. There was no difference in pain on VAS scale between the two groups at either day 1 or day 7 (Analysis 1.1; Analysis 1.2).
Analysis 1.1.
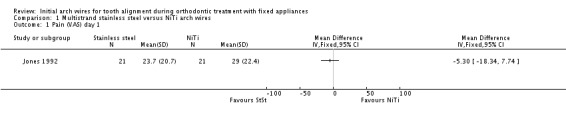
Comparison 1 Multistrand stainless steel versus NiTi arch wires, Outcome 1 Pain (VAS) day 1.
Analysis 1.2.
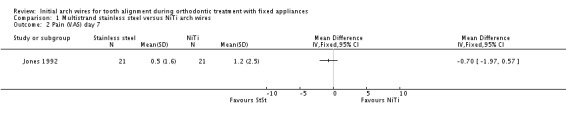
Comparison 1 Multistrand stainless steel versus NiTi arch wires, Outcome 2 Pain (VAS) day 7.
West 1995 assessed tooth alignment by means of three‐dimensional contact point movements of the anterior and the whole dental arches using the index of tooth alignment (ITA). The main difference between ITA, and Little's Irregularity Index (Little 1975), is that the positions of the anatomic contact points are digitised in three dimensions and the process may be extended to the full dental arch. The effects of the two arch wires were compared by an analysis of covariance on the means of triplicate log ITA scores reported as an adjusted mean ratio of ITA scores (NiTi/StSt). In the mandibular labial segment, the superelastic NiTi wire was found to produce a statistically significant improved alignment in comparison to the multistrand steel wire, but there was no difference in the labial segment of the maxilla (see table below). This trial did not report root resorption, time to working arch wire, time to alignment or pain.
| West 1995 | 3D alignment‐adjusted geometric mean ratio of ITA scores NiTi/ StSt | 95% confidence interval | P value |
| Upper arch (6‐6) | 1.03 | 0.92 to 1.15 | 0.56 |
| Lower arch (6‐6) | 1.13 | 1.03 to 1.24 | 0.01 |
Multistrand stainless steel with thermally active NiTi or active Martensitic NiTi.
Evans 1998 in a three‐arm trial, compared 0.0155 inch multistrand stainless steel wire (Dentaflex) with 0.016 x 0.022 inch medium force active M‐NiTi wire (Titanium Heat Memory Wire) or 0.016 x 0.022 inch graded force active M‐NiTi wire (Bioforce Sentalloy).
Participants were seen at 4‐week intervals and alginate impressions of the dental arches included in the trial were taken at baseline, 4 weeks and 8 weeks. The alignment rate was assessed by the changes of contact point distances of the anterior, the posterior and the whole arch in two‐ and three‐dimensional measurements. The numerical data comparing the different arch wires presented in the paper is for both two‐dimensional changes and three‐dimensional changes between time points (model variables are subject, order and upper or lower arch), and the trial found no difference between the arch wire types. Outcomes of root resorption, time to working arch wire, time to alignment or pain were not reported in this trial.
| Evans 1998 | StSt | Heat memory NiTi | M – NiTi | ANOVA F statistic* | P value |
| Both arches (6‐6) Arch movement in mm 2D (0‐8 weeks) |
5.30 | 6.32 | 6.05 | 0.05 | 0.95 |
| Both arches Arch movement in mm 3D (0‐8 weeks) |
5.73 | 6.12 | 6.62 | 0.30 | 0.74 |
*ANOVA F ratio test adjusted for subject, order and upper or lower arch.
2. Conventional (stabilised) NiTi arch wires compared with superelastic NiTi arch wires
Two trials made this comparison and each used a different diameter superelastic wire and reported different outcomes (Fernandes 1998; O'Brien 1990) (Table 2).
0.016 inch NiTi wire (Nitinol) compared to 0.016 inch superelastic NiTi wire (Titanol) (O'Brien 1990). The rate of initial tooth alignment was assessed by three‐dimensional contact point movements of the upper labial segments. There was no statistically significant difference between these two intervention groups in terms of tooth movement (Analysis 2.1), and this trial did not report root resorption, time to working arch wire, time to alignment or pain.
Analysis 2.1.
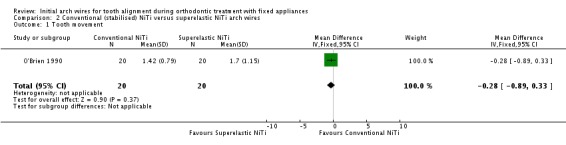
Comparison 2 Conventional (stabilised) NiTi versus superelastic NiTi arch wires, Outcome 1 Tooth movement.
0.014 inch NiTi wire (Nitinol) compared to 0.014 inch superelastic NiTi wire (Sentalloy) (Fernandes 1998). This trial report did not address the effects of these arch wires on root resorption, alignment rate, time to alignment, time to next arch wire. The only outcomes reported were the intensity of pain/discomfort experienced by patients during the initial alignment stage of treatment for 7 days, evaluated by VAS scores and the consumption of analgesics. There was no difference between the two arch wire groups in pain intensity on day 1 (11 hours after wire placement) (Analysis 2.2), or day 7 (Analysis 2.3), and no difference in analgesic consumption (Analysis 2.4).
Analysis 2.2.
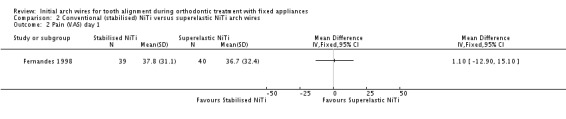
Comparison 2 Conventional (stabilised) NiTi versus superelastic NiTi arch wires, Outcome 2 Pain (VAS) day 1.
Analysis 2.3.
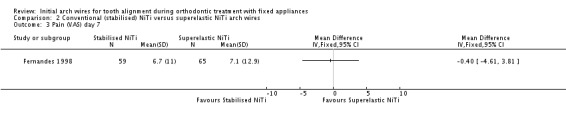
Comparison 2 Conventional (stabilised) NiTi versus superelastic NiTi arch wires, Outcome 3 Pain (VAS) day 7.
Analysis 2.4.
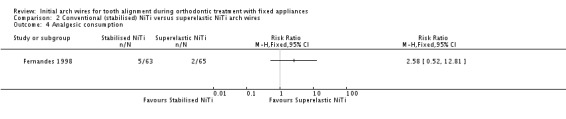
Comparison 2 Conventional (stabilised) NiTi versus superelastic NiTi arch wires, Outcome 4 Analgesic consumption.
3. Single‐strand superelastic NiTi compared with other types of NiTi
Three trials used a 0.016 inch diameter single‐strand superelastic NiTi wire as a comparator (Table 3).
Sebastian 2012 compared 0.016 inch single stranded superelastic NiTi wire (Rematitan Lite Wire) to 0.016 inch coaxial (multistranded) superelastic NiTi wire (Regular 7 Stranded Supercable Wire) and reported alignment rate per month for the lower labial segment only. Measurements were made on dental casts taken at 4, 8 and 12 weeks after initial arch wire placement, using a co‐ordinate measuring machine which calculated mean tooth movement at each time point. Over the 12 weeks of the study, the coaxial superelastic NiTi arch wire induced greater tooth movement (Analysis 3.1). However, this is a single study of 24 patients, assessed at high risk of selective reporting bias and further research is required to verify this finding, and determine whether there might be possible adverse effects such as pain or root resorption.
Analysis 3.1.
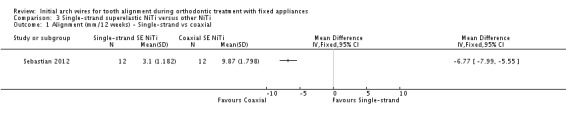
Comparison 3 Single‐strand superelastic NiTi versus other NiTi, Outcome 1 Alignment (mm/12 weeks) ‐ Single‐strand vs coaxial.
0.016 inch NiTi wire (ModernArch) compared to 0.016 inch CuNiTi wire (Ormco) (Pandis 2009). In this trial, with 60 participants, time to alignment of the six lower labial segment teeth only, was assessed from intraoral measurements of Little's Irregularity Index (LII) by a fine‐tip digital calliper. There was no difference between wire types in alignment rate ratio (Analysis 3.2) but predictably, severely crowded cases (LII > 5 mm) took significantly longer to align than moderately crowded (LII < 5 mm) cases. Time to next arch wire, root resorption with each wire type or pain were not reported in this trial.
Analysis 3.2.
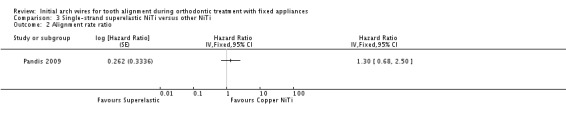
Comparison 3 Single‐strand superelastic NiTi versus other NiTi, Outcome 2 Alignment rate ratio.
In the study by Cioffi 2012, 0.016 inch single stranded superelastic NiTi arch wire was compared to a thermoelastic heat activated NiTi wire of the same diameter. This trial of 30 participants did not report alignment rate, time to next arch wire or root resorption. Participants self assessed pain on a visual analogue scale at five time points each day for 7 days. There was no difference in mean reported pain between the two groups on day 1 or day 7 (Analysis 3.3; Analysis 3.4).
Analysis 3.3.
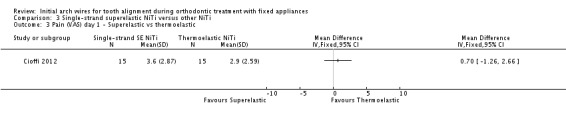
Comparison 3 Single‐strand superelastic NiTi versus other NiTi, Outcome 3 Pain (VAS) day 1 ‐ Superelastic vs thermoelastic.
Analysis 3.4.
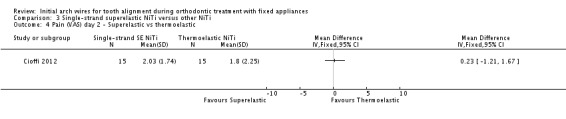
Comparison 3 Single‐strand superelastic NiTi versus other NiTi, Outcome 4 Pain (VAS) day 2 ‐ Superelastic vs thermoelastic.
Discussion
Summary of main results
Nine randomised controlled clinical trials (RCTs) including a total of 571 participants (671 arches) satisfied the inclusion criteria for this review. Trials were generally small (mean 63, range 24 to 128 participants). Duration of follow‐up varied between 1 week and 6 months and no two trials made exactly the same comparison and reported the same outcomes. All trials were assessed at high risk of bias.
We grouped the trials into three main comparisons.
Multistrand stainless steel initial arch wires compared to superelastic nickel titanium (NiTi) initial arch wires (Table 1).
There were four trials in this group and only two reported numerical outcome data. No meta‐analysis was possible. There is insufficient evidence from these trials to determine whether there is a difference in either rate of alignment or pain between stainless steel and NiTi arch wires.
Conventional (stabilised) NiTi compared to superelastic NiTi initial arch wires (Table 2).
There were two trials in this group, one reporting the outcome of alignment over 6 months and the other reporting pain over 1 week. There is insufficient evidence from these trials to determine whether there is any difference between conventional (stabilised) and superelastic NiTi arch wires with regard to either alignment or pain.
Single‐strand superelastic NiTi compared to other NiTi (coaxial, copper NiTi (CuNiTi) or thermoelastic) (Table 3).
The three trials in this comparison each compared a different product against single‐strand superelastic NiTi. There is very weak unreliable evidence, based on one very small study (n = 24) at high risk of bias, that coaxial superelastic NiTi may produce greater tooth movement over 12 weeks. This should be interpreted with caution until further research evidence is available.
The poor quality of the conduct and reporting of all of the included trials, together with the variety of comparisons evaluated, means that there is insufficient evidence in this review to determine whether any specific arch wire type is better than another in terms of speed of tooth alignment or pain experienced during alignment. No information was available from these trials as to whether there was a difference in the adverse outcome of root resorption because none of the trials reported this outcome.
Overall completeness and applicability of evidence
There has been a great deal of research into developing orthodontic arch wire materials with properties that could enhance the initial alignment phase of orthodontic treatment, either by increasing the speed of alignment or reducing pain or both. However, there is a big gap between the abundant materials research and manufacturers' claims of superior products, and the absence of clinical evidence that these newer materials make a difference in people undergoing orthodontic treatment.
None of the trials in this review reported both the benefits (in alignment) and the possible adverse effects (pain and/or root resorption) associated with the different types of initial arch wires. Each trial evaluated a different comparison and there was also variation in the way outcomes were measured and reported. All of the trials had at least one uncontrolled variable which was likely to be a confounding factor. One trial which reported alignment did not included data in a form that could be used in this review (Cobb 1998). All six trials that reported alignment as an outcome failed to report either pain or root resorption. The three trials which did report pain did not report alignment or root resorption.
Quality of the evidence
Although this review included nine RCTs and 571 participants randomised to treatment, each of these trials had at least one domain at high risk of bias. All of the trials had selective reporting bias in that they failed to report both benefits and potential harms of the arch wires under evaluation. More than half the included trials failed to clearly report an adequate means of allocation concealment, an aspect of trial design and conduct that is known to be associated with bias.
None of the included trials reported root resorption. Root resorption is one of the most serious side‐effects of orthodontic treatment and has been well‐known for many years (Linge 1983; Rudolph 1940; Weiland 2003). It is thought that the type and level of force are among the factors influencing the extent of root resorption. Stainless steel wires generate a high but rapidly declining force after ligation of an arch wire, whereas superelastic wires deliver a constant force over an extended period of the deactivation range (Miura 1986). Therefore, further evaluation of initial arch wires should consider this potentially serious side‐effect of orthodontic treatment.
However, there are several other methodological limitations of the included trials. There are a number of potentially confounding variables, which could affect the outcomes of speed of alignment or pain or root resorption. Rate of alignment is affected by those factors that influence friction and by those that affect the biological response to an applied orthodontic force. The former is dictated by type and dimensions of bracket material/arch wire including bracket slot‐size and wire diameter as well as method and type of ligation. The latter is guided by age of the patient, metabolic and anatomical factors. These variables also modify the pain response. In order to attribute differences in alignment to arch wire materials the following factors should be specified and held constant in clinical trials.
Brackets
Four trials specified the bracket type, which was used for all trial participants: preadjusted bioprogressive edgewise 0.018 x 0.030 inch slot (Jones 1992), 0.022 x 0.028 inch slot MBT prescription brackets (Sebastian 2012), self ligating brackets with 0.022 inch slot (In Ovation‐R) (Pandis 2009), but different molar tubes (Speed System Orthodontics, Ontario, Canada) accompanied their use in this trial. The trial by Cioffi 2012 specified metal brackets (0.022 x 0.028 inch slot).
Both 0.018 inch and 0.022 inch slot edgewise appliances were used by Cobb 1998, twin brackets on all teeth for the 0.022 inch system, and for the 0.018 inch system twin brackets were used on the maxillary central and lateral incisors with a mix of single and twin brackets for the remaining teeth.
Edgewise brackets were used by O'Brien 1990, but dimensions and bracket type are not stated. In the study by Fernandes 1998, "as far as possible, the brackets used were standardised". Type of brackets used is not stated in two trial reports (Evans 1998; West 1995), but was stated in the author's MScD dissertations.
In addition, bracket debonding may have also influenced the results if rebonding was not performed soon after the bracket became debonded. Unfortunately, only one study considered this variable (Evans 1998).
Details regarding bracket type (material/dimensions) should be specified and standardised in future studies.
Method of ligation
The trial reports varied in the description of the method of ligation used. In four trials, the method of ligation was specified for trial participants: Cobb 1998 elastomeric modules; Sebastian 2012 elastomeric modules or steel ties; Cioffi 2012 elastic ligatures using a standard Mathieu pliers; and Pandis 2009 self ligating. In two trial reports, ligation was not mentioned (Fernandes 1998; Jones 1992).
In three trial reports ligation was described as follows.
‐ The "arch wire was tied with ligatures into the brackets, with the operator attempting to achieve complete engagement where clinically possible" (O'Brien 1990). ‐ Clinicians were asked to follow their usual practice but to "ligate the wire as fully into each bracket as possible with no teeth omitted from the attachment to the wire" (Cobb 1998). ‐ "...ligated as fully as possible into the bracket with the clinicians preferred method usually elastomeric rings" (Evans 1998).
However, none of these trials reported the number of participants in each of the randomised groups who did not have complete engagement, 'full ligation' or each type of ligature.
The method of ligation should be specified, standardised and reported fully in future trials.
Operators
The number of operators participating in the trials varied between one (Pandis 2009), two (Cioffi 2012; O'Brien 1990), five (West 1995), six (Evans 1998), eight (of which six were postgraduate students) (Sebastian 2012), to 13 (Cobb 1998). The number of operators was not reported in the published papers in one study (Jones 1992). Where important aspects of orthodontic treatment (such as bracket type, dimension and ligation) which may influence the outcomes of the trials varied by operator, the number of operators in these trials represents another uncontrolled variable.
Extractions
Some of the participants in these trials underwent extraction of teeth as part of their orthodontic treatment. One trial reported the extraction of at least one premolar (Jones 1992), and three trials reported that there were no extractions (Cioffi 2012; Pandis 2009; Sebastian 2012). However, whether or not participants underwent tooth extraction as part of their orthodontic treatment was not specified in five trials (Cobb 1998; Evans 1998; Fernandes 1998; O'Brien 1990; West 1995).
Duration of trials, time of outcome assessment
This also varied between the trials included in this review. Two trials evaluated the first 7 days following arch wire placement (Cioffi 2012; Fernandes 1998), and one evaluated up until day 15 (Jones 1992). O'Brien 1990 reported a mean duration of 37 days, West 1995 6 weeks, Evans 1998 8 weeks, Sebastian 2012 12 weeks, Pandis 2009 6 months, and Cobb 1998 12 months.
The studies by O'Brien 1990 and West 1995 were of short duration, but as these studies only observed the amount of tooth movement in the first month of treatment but not the mean rate of initial alignment, this is appropriate. Ideally, the duration of studies should be standardised with a longer observation period for full alignment.
Assessment of crowding and alignment
Alignment can be measured in several ways. Three studies (Cobb 1998; O'Brien 1990; Pandis 2009) used the irregularity index first described by Little (Little 1975). This index (as originally described) addresses the sum of the five contact point displacements for the mandibular anterior teeth, regardless of any irregularities in the buccal segments. Two studies used the index of tooth alignment (ITA), which includes an assessment of the whole dental arch (Evans 1998; West 1995). An assessment of the contact point discrepancies for the whole arch is a useful outcome measure, especially when crowding/irregularities occur in the canine, premolar and molar regions.
There are two main methods of recording the amount of crowding: direct measurement in the mouth with a digital vernier calliper (Cobb 1998; Pandis 2009), and indirect measurement on stone casts with electronic callipers or in three dimensions with instruments such as the reflex metrograph. Both methods are associated with drawbacks. When using direct measurement, the examiner(s) will require calibration at the start and regular recalibration throughout the trial period, to ensure consistency of the measurements. A second problem with direct measurements is blinding/masking. To reduce bias the examiner should be blinded/masked to group allocation at the time of recording, which may complicate the operation of the trial. Indirect measurement on casts can resolve this problem when the casts are measured in a random order and the assessors are blinded/masked to allocation. However, indirect measurement in three dimensions requires specialised instruments, such as the Reflex Metrograph (O'Brien 1990) and the Reflex Microscope (Evans 1998; West 1995), which adds to the cost of a clinical study. Another problem with three‐dimensional indirect measurements is that of identifying the fiducial points on each cast, which are important for ascertaining adequate reproducibility of the measurements.
When future studies are planned, greater consideration should be given to study design in order to reduce bias. Future studies should consider standardisation of study design to make results comparable. This would involve clear inclusion criteria (such as whether patients requiring extractions can be included) together with factors such as orthodontic appliance system, bracket type, slot size and the ligation method being prespecified, as these may have been important confounders among the studies that were included in this review. It is desirable that a standardised measure of alignment be used as an outcome measure.
Economic considerations were not included in this review. However, we acknowledge that the cost of arch wires, the amount of time required for ligation, the overall number of appointments (including any additional appointments required for breakages e.g. wire fracture) and also the type of orthodontic care provider (overheads may be more expensive in hospital settings compared to practice‐based care), will unavoidably influence the selection of initial arch wires. Evaluation of these outcomes is desirable in future trials.
Potential biases in the review process
A sensitive search strategy was used for this review. Every effort was made to identify all relevant studies. No studies were excluded due to language restrictions. We tried to contact authors of studies investigating initial arch wires for the alignment of teeth with fixed orthodontic appliances by email and postal mail to identify unpublished studies or additional information about their studies. However, only a few authors replied (Jones 1992; O'Brien 1990; Weiland 2003).
Data collection and analysis were done by two review authors independently, and any disagreement between review authors was resolved by discussion or the assistance of the Cochrane Oral Health Group to minimise/exclude bias during the review process.
Agreements and disagreements with other studies or reviews
Only one published systematic review was identified (Riley 2009). This included both randomised clinical trials and controlled clinical trials, while only randomised clinical trials were included in our Cochrane review. The review of Riley 2009 only focused on one outcome "objective measurement of alignment/irregularity" to assess the effectiveness of arch wires for alignment, while the amount of root resorption along with tooth movement and the intensity of pain experienced by patients during the initial alignment stage of treatment were also evaluated in our review. Seven studies were included in Riley 2009, of which five were included in our Cochrane review (Cobb 1998; Evans 1998; Jones 1992; O'Brien 1990; West 1995), and the other two (Dalstra 2004; Pandis 2007) were excluded in our review. Four studies were included in our review (Cioffi 2012; Fernandes 1998; Pandis 2009; Sebastian 2012), while they were not included in Riley 2009. The data extraction, assessment of the evidence quality and the authors' conclusion of the two reviews were mainly in accordance between the two reviews. It should be noted that, due to a lack of homogeneity among the included studies, meta‐analyses could not be undertaken in either review.
Authors' conclusions
Although there are nine randomised controlled trials (RCTs) with more than 500 participants included in this review, the conduct and reporting of these trials have resulted in a high risk of both bias and confounding. There is insufficient evidence from these studies to determine whether any of the arch wires evaluated are better or worse with regard to the rate of alignment or pain experienced by patients when using one initial aligning arch wire compared to another.
This review suggests a need for more well‐designed RCTs in order to determine which initial arch wire is most effective. However, in designing future trials, the following need to be considered.
Treatment, except for the intervention, should be as specified so as to be as similar as possible among the trial participants (in terms of brackets/appliances/ligation systems/need for extractions) and details of these aspects of treatment should be reported for each group.
Trials should report both benefits (speed of alignment) and possible harms (such as pain and root resorption), and be of sufficient duration to enable these outcomes to be measured.
Consideration needs to be given to standardised measurements for evaluating tooth movement/alignment and pain.
Clear inclusion/exclusion criteria should be set. Care should be taken to avoid unit of analysis errors where dental arches are the unit of randomisation. Adult patients should be included in trials to increase the generalisability of the results.
An a priori sample size calculation should be carried out.
Attempts should be made to minimise missing data.
Data on comparative costs associated with each wire (e.g. cost of wires, additional visits required to deal with breakages, bracket debonding) would be useful.
Clinical trial reports should follow the guidelines produced by the CONSORT Group to ensure that all relevant information is provided (Moher 2005).
Acknowledgements
We would like to acknowledge the assistance of Anne Littlewood (Trials Search Co‐ordinator, Cochrane Oral Health Group) in developing the search strategy and also Jayne Harrison, Helen Worthington and Luisa Fernandez Mauleffinch (Cochrane Oral Health Group) in editing the review. We would like to thank Zongdao Shi, Zhihe Zhao and Taixiang Wu for their contribution to the previous published version of the review.
Appendices
Appendix 1. MEDLINE (OVID) search strategy
1. exp Orthodontic Wires/ 2. "orthodontic wire$".mp. 3. archwire$ or "arch wire" or arch‐wire$.mp. 4. "superelastic wire" or "super‐elastic wire".mp. 5. "stainless steel wire"or "stainless‐steel wire".mp. 6. (NiTi adj3 wire$) or (Ni‐Ti adj3 wire$) or ("nickel titanium" adj3 wire) or (nickel‐titanium adj3 wire).mp. 7. (CuNiTi adj3 wire$) or (Cu‐NiTi adj3 wire$) or (Cu‐Ni‐Ti adj3 wire$) or (copper‐nickel‐titanium adj3 wire) or ("copper nickel titanium" adj3 wire).mp. 8. or/1‐7
The above subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]:
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 2. Cochrane Oral Health Group's Trials Register search strategy
("orthodontic wire*" or archwire* or "arch wire*" or arch‐wire* or "superelastic wire*" or "super‐elastic wire*" or "stainless steel wire*" or "stainless‐steel wire*" or NiTi or Ni‐Ti or "nickel titanium wire*" or "nickel‐titanium wire*")
Appendix 3. CENTRAL search strategy
#1 MeSH descriptor ORTHODONTIC WIRES explode all trees #2 (archwire* in All Text or "arch wire*" in All Text or arch‐wire* in All Text or "orthodontic wire*" in All Text) #3 ("superelastic wire*" in All Text or "super‐elastic wire*" in All Text) #4 ("stainless steel wire*" in All Text or "stainless‐steel wire*" in All Text) #5 ((NiTi in All Text near/6 wire in All Text) or (Ni‐Ti in All Text near/6 wire in All Text) or ("nickel titanium" in All Text near/6 wire in All Text) or (nickel‐titanium in All Text near/6 wire in All Text)) #6 (#1 or #2 or #3 or #4 or #5)
Appendix 4. EMBASE (OVID) search strategy
1. exp Orthodontic Wires/ 2. "orthodontic wire$".mp. 3. archwire$ or "arch wire" or arch‐wire$.mp. 4. "superelastic wire" or "super‐elastic wire".mp. 5. "stainless steel wire" or "stainless‐steel wire".mp. 6. (NiTi adj3 wire$) or (Ni‐Ti adj3 wire$) or ("nickel titanium" adj3 wire$) or (nickel‐titanium adj3 wire$).mp. 7. or/1‐6
The above subject search was linked to the Cochrane Oral Health Group filter for EMBASE via OVID:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. ANIMAL/ or NONHUMAN/ or ANIMAL EXPERIMENT/ 16. HUMAN/ 17. 16 and 15 18. 15 not 17 19. 14 not 18
Data and analyses
Comparison 1.
Multistrand stainless steel versus NiTi arch wires
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain (VAS) day 1 | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Pain (VAS) day 7 | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 2.
Conventional (stabilised) NiTi versus superelastic NiTi arch wires
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Tooth movement | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.89, 0.33] |
| 2 Pain (VAS) day 1 | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Pain (VAS) day 7 | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Analgesic consumption | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3.
Single‐strand superelastic NiTi versus other NiTi
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Alignment (mm/12 weeks) ‐ Single‐strand vs coaxial | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Alignment rate ratio | 1 | Hazard Ratio (Fixed, 95% CI) | Totals not selected | |
| 3 Pain (VAS) day 1 ‐ Superelastic vs thermoelastic | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Pain (VAS) day 2 ‐ Superelastic vs thermoelastic | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
What's new
Last assessed as up‐to‐date: 2 August 2012.
| Date | Event | Description |
|---|---|---|
| 25 March 2013 | New citation required but conclusions have not changed | Two new studies were identified and included with no changes to the conclusions. Methods were updated. Changes to authorship and title. |
| 25 March 2013 | New search has been performed | Searches updated to 2 August 2012. |
Differences between protocol and review
Changes to authorship and title (from 'Initial arch wires for alignment of crooked teeth with fixed orthodontic braces' to 'Initial arch wires for tooth alignment during orthondontic treatment with fixed appliances'). Methods have been updated (risk of bias tables have been updated and expanded and summary of findings tables have been added to the review).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cioffi 2012
| Methods | Location: Patients were treated at Section of Orthodontics, Department of Oral Sciences, University of Naples Federico II, Naples, Italy Recruitment period: Starting January 2009 Funding source: Research was supported by Polo delle Scienze e Tecnologie per la Vita, University of Naples Federico II Trial design: RCT with 2 parallel arms |
|
| Participants | Inclusion criteria: Patients with full permanent dentition, excluding permanent second and third molars Exclusion criteria: Those with active periodontal disease, planned extractive orthodontic treatment, reports of previous orthodontic treatment, skeletal asymmetries, or systemic diseases that might affect pain perception, or therapy for painful conditions Gp 1 mean age 14.7 ±3.4 M 6/F 9; maxillary 11/mandibular 4 Gp 2 mean age 14.7 ±4.2 M 5/F 10; maxillary 12/mandibular 3 Number randomised: 30 Number evaluated: 30 |
|
| Interventions |
Comparison: Superelastic 0.016 NiTi versus heat activated 0.016 in NiTi Gp A (n = 15): Round 0.016 in superelastic NiTi (Unitek) Gp B (n = 15): Round 0.016 heat activated (HANT, Unitek) Metal orthodontic brackets (slots 0.22 x 0.28 inch) bonded to either maxillary or mandibular arch. Assigned arch wires were placed and tied into the brackets with elastomeric ligatures. Appliance was positioned between 1400 & 1700 hours in all patients |
|
| Outcomes | Pain measured on 10 cm VAS at 0800, 1200, 1600, 2000, 2400 daily for 7 days. Arch length measured from cephalograms. Analgesic use | |
| Notes | Sample size calculation: 14 subjects per group necessary to detect difference of 20 mm on VAS with 80% power & α = 0.05 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were randomly selected for insertion of each arch wire. Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Allocation procedure was performed by 1 of the authors who was blinded to patient names and identifications |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Low risk | Arch wire was positioned on the tray by 1 of the operators without any packaging to identify type. Hence patients were blinded to treatment group, but operators would have been able to recognise arch wire type by handling characteristics |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | Low risk | Cephalometric analysis was conducted by researcher who was blinded to allocated treatment. Patients completed pain assessments and they were blinded to treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluations |
| Selective reporting (reporting bias) | High risk | Pain and arch length reported in each group. Analgesic consumption reported without estimates of variance, effectiveness of alignment not reported, so not possible to determine relative benefit and harm |
| Other bias | Low risk | No other sources of bias identified |
Cobb 1998
| Methods | Location: Chapel Hill, USA. Graduate clinic or faculty practice, University of North Carolina School of Dentistry Recruitment period: 12 months (start date not stated) Funding source: In part by a contract from Spire Corporation (who supplied one of arch wires), under the terms of an SBIR (small business initiative) grant from the National Institute of Dental Research Trial design: Parallel group (3 arms), 13 faculty members each of whom used either 18 or 22 slot edgewise appliance. Randomisation was blocked in 14 groups of 9 (so that each faculty member treated an equal number of patients with each arch wire type) |
|
| Participants | Inclusion criteria: Age 10‐30 years, pretreatment Irregularity Index > 5 mm, all permanent anterior teeth present Exclusion criteria: No anterior tooth extraction or reapproximation during alignment, no anterior tooth vertically malpositioned > 3 mm from arch form, no anterior tooth completely blocked from archform, no periodontal pockets > 4 mm, no craniofacial syndrome Age group: 10‐30 years Number randomised: 126 participants (158 dental arches) Number evaluated: 123 participants (155 dental arches) |
|
| Interventions |
Comparison: Multistrand stainless steel versus NiTi versus ion‐implanted NiTi Gp A (n = 47 arches, 18 maxillary): 17.5 mm 3‐strand stainless steel (Wildcat GAC) Gp B (n = 48 arches, 24 maxillary): 16 mm austenitic NiTi (Sentalloy, GAC) Gp C (n = 60 arch wires, 30 maxillary): 16 mm austenitic ion‐implanted NiTi (Sentalloy implanted by Spire corp) 14 blocks of 9 patients allocated; 7 blocks to 18 mm slot edgewise appliance (1 operator had 2 blocks) and 7 to blocks to 22 mm slot edgewise appliances) Assigned arch wires were placed and tied into the brackets with elastomeric ligatures. The patients were seen at 4‐week intervals and measurements were repeated, until the Irregularity Index dropped to 2 mm or less (approximately 6 months) |
|
| Outcomes | Rate of alignment (reduction in Irregularity Index over time), time to achieve 2 mm Irregularity Index | |
| Notes | Sample size calculation: Not mentioned. Study likely to be underpowered, and therefore less likely to show a difference Stratification: Bracket slot size used as a stratification factor Randomisation was at the subject level while outcome was studied at the dental arch level. 32 participants (25%) contributed 2 arch wires to study No numerical outcome data for each intervention group reported Further information was requested from the authors but there was no reply |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was stratified by operator and blocked in groups of 9. Units of randomisation and analysis not the same |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not described and was probably not done |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Low risk | Participant blinding not mentioned but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | High risk | Blinding of operators not mentioned. It seems likely that outcomes were assessed by operators and that this may have introduced a bias as clearance between appliance and arch wire is expected to affect outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants and 3 arch wires excluded from analysis. Unlikely to have introduced bias |
| Selective reporting (reporting bias) | High risk | Planned outcomes reported, but no numerical data. No pain outcomes or adverse effects reported |
| Other bias | High risk | Possible confounding effect of different bracket types, in different distribution for mandibular and maxillary arches, used with the two types of edgewise appliances. Unit of analysis error |
Evans 1998
| Methods | Location: Cardiff, Wales. 2 university centres Recruitment period: Not stated Funding source: Welsh Scheme for the Development of Health and Social Research Trial design: RCT, factorial design, 3 arms for each arch, 6 possible combinations. Each participant received 2 of 3 possible arch wires, with a different arch wire for each arch. Unit of randomisation is arch. 6 operators |
|
| Participants | Inclusion criteria: Aged less than 18 years, upper and lower fixed appliances required, no previous orthodontic treatment, any initial phase of expansion with quadhelix stable for 2 months, and active distal molar movement stable for 2 months Exclusion criteria: "patients who may have experienced periodontal disease and hence loss of attachment," were excluded Age group: < 18 years Number randomised: 56 patients, 112 arches Number evaluated: 51 patients, 98 arch wires (47 patients had data for 2 arches & 4 for 1 arch) |
|
| Interventions |
Comparison: Multistrand stainless steel versus martensitic NiTi versus different martensitic NiTi Gp A (n = 31 arch wires 14 maxillary): 0155 inch multistrand stainless steel (Dentaflex/dentarium) Gp B (n = 32 arch wires, 19 maxillary): 016/022 inch medium force active martensitic nickel titanium (Titanium Heat Memory Wire/American Orthodontics) Gp C (n = 35 arch wires, 16 maxillary): 016/022 inch graded force, active martensitic nickel titanium (Bioforce Sentalloy/GAC) Bracket types: Centre 1 A Company Siamese brackets 0.022 Roth prescription Centre 2 Orthocare Spectrum I Siamese brackets 0.022 Roth prescription |
|
| Outcomes | Primary outcome measure: Tooth movement assessed from dental casts with 3‐ and 2‐dimensional intertooth (contact) point movement within the anterior, posterior and whole arch from before and after 4 and 8 weeks treatment, using a reflex microscope Secondary outcome measure: Time to next/working arch wire assessed by the time span in days for the use of each wire type (no variance estimates) |
|
| Notes | Sample size calculation: Reported that 50 subjects (100 arches) required, based on pilot study Other information: MScD dissertation reported: 1. Centre 1 ‐ A Company Siamese brackets Roth prescription 0.022, Centre 2 ‐ Orthocare Spectrum I Siamese brackets 0.022 Roth prescription; 2. Arch wire allocation was predetermined via a randomised sealed nested envelope technique. Type of ligation based on operator preference, variable and not reported No further information obtained from the authors |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Allocation was predetermined and randomized." Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Arch wire allocation was predetermined via a "randomised sealed nested envelope technique" |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Low risk | Participant blinding not mentioned but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | High risk | Blinding of outcome assessor not mentioned. Likely that operator who assessed outcomes was aware of arch wire type |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 5/56 patients (9%) and 14/112 (12.5%) arch wires, excluded from analysis. Reasons given are bracket debonding or failure to attend appointments. No information regarding exclusion per arch wire type |
| Selective reporting (reporting bias) | High risk | Time to next arch wire reported without standard deviations, tooth movement not reported for each arch wire. No pain outcomes or adverse effects reported |
| Other bias | High risk | Potentially confounding effects due to variation in type of fixed appliance and type of ligature used |
Fernandes 1998
| Methods | Location: Oslo, Norway, university clinic and 2 private practices Recruitment period: Not stated Funding source: Not stated Trial design: Parallel group RCT, 8 dentists |
|
| Participants | Inclusion criteria: Caucasian patients starting active orthodontic treatment, no quadhelix or other palatal expansion device present, no extraoral appliance to be used, full arch edgewise fixed appliance, no analgesics taken prior to procedure Exclusion criteria: None stated Age group: Mean 12.6 months; Range 9‐16 years Number randomised: 128 patients, 128 arch wires Number evaluated: Not stated |
|
| Interventions |
Comparison: Conventional NiTi versus superelastic NiTi Gp A (n = 65): 0.014 inch Nitonol (Unitek/Monrovia USA) Gp B (n = 63 ): 0.014 inch superelastic NiTi (Sentalloy light/GAC) |
|
| Outcomes | Pain (VAS and analgesic use), measured hourly for first 11 hours then daily for 6 days over first 7 days after bonding | |
| Notes | Sample size calculation: Not described Brackets used and placement of brackets & arch wires standardised. Type of full arch edgewise fixed appliance not specified Other information: Authors could not be contacted |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly assigned". Method of sequence generation not described |
| Allocation concealment (selection bias) | High risk | Not mentioned |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Unclear risk | Not mentioned, but unclear whether patient awareness of arch wire type would bias results |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | Unclear risk | Pain reported by participants. No operator assessed outcomes reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Some data missing from some time points in both groups. No reasons given, but unlikely to have introduced a bias |
| Selective reporting (reporting bias) | High risk | Analgesic use recorded but not reported. Pain reported but relative effectiveness of arch wires with regard to tooth alignment not reported |
| Other bias | Low risk | No other sources of bias identified |
Jones 1992
| Methods | Location: Wales, UK. Consecutive patients attending university clinic Recruitment period: Not stated Funding source: Not stated Trial design: Parallel group RCT (for initial arch wire allocation). Number of operators not reported |
|
| Participants | Inclusion criteria: Patients, aged < 17 years, requiring extraction of at least 1 premolar tooth and placement of full arch edgewise fixed appliance. No molar band, palatal arch, Nance button or quad helix present and active or causing discomfort on study entry. No extraoral traction required Exclusion criteria: Medical history affecting extraction under local anaesthetic Age group: Range 113‐202 months Gender: 23/20 M/F Number randomised: 45 Number evaluated: 43 |
|
| Interventions |
Comparison: Multistrand stainless steel versus superelastic NiTi Gp A (n = 21): Multistrand steel, 0.015 inch Twistflex (Unitek corp, Monrovia USA) ‐ first arch wire Gp B (n = 22): Superelastic NiTi, 0.014 heavy Japanese NiTi (GAC International USA) ‐ first arch wire All patients had full arch edgewise fixed appliance, with 0.018 x 0.030 inch standard (triple control) preadjusted bioprogressive brackets (Rocky Mountain Orthodontics, USA) 23/43 patients had a second arch wire fitted to the other arch as a second procedure |
|
| Outcomes | VAS Pain (100 mm) measured at 0900, 1300, 1700 & 2100 hours daily for 15 days, questionnaire to determine pain location and frequency after 24 hours, paracetamol tablet consumption | |
| Notes | Sample size calculation: Report states that sample size was based on calculations from the results of a previous study Other information: No further information was obtained from authors |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "random allocation". Method of sequence generation not described |
| Allocation concealment (selection bias) | High risk | Not described |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Unclear risk | No mention of participant blinding and unclear whether knowledge of arch wire type would affect outcome measures |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | Unclear risk | Only patient reported outcomes (pain & analgesic consumption) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3/45 patients excluded from analysis. 2 failed to return questionnaires but allocated treatment not stated. Unlikely to have introduced bias |
| Selective reporting (reporting bias) | High risk | Planned outcomes of pain reported, but no indication about the relative effectiveness of the arch wires with regard to alignment of teeth |
| Other bias | Low risk | No other sources of bias identified |
O'Brien 1990
| Methods | Location: Manchester UK. Dental hospital Recruitment period: Not stated Funding source: Arch wires supplied by Thomas Bolton and Johnson Ltd Trial design: RCT |
|
| Participants | Inclusion criteria: Patients attending university dental hospital clinic for routine Edgewise fixed appliance therapy Exclusion criteria: Not stated Age group: Gp A mean age 13.4 (SD 3.12) years, range 11.5‐17.25; Gp B mean age 12.95 (SD 3.2) years, range 11‐16.5 years Number randomised: 40 Number evaluated: Not stated |
|
| Interventions |
Comparison: Conventional NiTi versus superelastic NiTi Gp A (n = 20): 0.016 inch conventional work hardened NiTi, Nitinol (Unitek Corp, California USA) mean duration of 37 days (SD = 2). Fixed Edgewise appliance Gp B (n = 20): 0.016 inch superelastic NiTi, Titanol (Forestadent, Milton Keynes, UK) mean duration of 34 days (SD = 2). Fixed Edgewise appliance |
|
| Outcomes | Tooth movement assessed from dental casts with 3‐dimensional intertooth (contact) point movement of the upper anterior arch from before treatment and subsequent appointment using Reflex Metrograph | |
| Notes | Sample size calculation: Not reported Other information: The following completed data were acquired by personal communication: 1) the patients were followed to the second data collection stage at 35 days; 2) slot size of the bracket was "probably 0.018 inch" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote from personal email: "The sequence was generated by a random number generator" Comments: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote from personal email: "We put the arch wires into envelopes which were in a box on the clinic. The operator then took the next sequential arch wire" Comments: Probably done |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Low risk | Blinding of participants not mentioned but unlikely to have affected outcomes |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | Low risk | Quote from personal email: "When I recorded the tooth movement from the study casts, I did not know which group the patients had been allocated, I was therefore blinded. The operators were not blinded to the wire" Comments: The outcome measurement was probably blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers included in the evaluation of outcomes not stated |
| Selective reporting (reporting bias) | High risk | Quote from personal email: "We attempted to record pain data but this was not sufficiently reliable for analysis" Comments: Not all of the study's prespecified primary outcomes had been reported |
| Other bias | High risk | No definite inclusion/exclusion criteria for participants selection. Small sample size |
Pandis 2009
| Methods | Location: Corfu, Greece. Private practice Recruitment period: December 2006 to March 2008 Funding source: Not stated Trial design: Single‐centre, single operator double blind parallel group RCT |
|
| Participants | Inclusion criteria: Non‐extraction treatment of mandible, eruption of all mandibular teeth, no spaces in mandibular arch, no crowding in posterior segments, mandibular Irregularity Index > 2 Exclusion criteria: Therapeutic intervention planned involving intermaxillary of other intraoral or extraoral appliances including intra‐arch or interarch elastics, lip bumpers, maxillary expansion appliances or headgear Age group: Mean 13.1 years; range 10‐18 Number randomised: 60 Number evaluated: 60 |
|
| Interventions |
Comparison: Conventional NiTi versus superelastic Copper NiTi Gp A (n = 30): 0.016 inch NiTi (Modern Arch, Wyoming USA) Gp B (n = 30): 0.016 inch Copper NiTi 35º C (Ormco, California USA) All patients were bonded with In‐Ovation‐R self ligating brackets with 0.022 in slot (GAC NY, USA). All first and second molars (when present) were bonded with bondable tubes (Speed System Orthodontics, Cambridge, Ontario, Canada). Bracket bonding, arch wire placement and treatment were performed by the same clinician |
|
| Outcomes | Primary outcome: Time to alignment of the mandibular anterior dentition The observation period ended after 6 months of intervention for all patients; for patients not aligned after 6 months of active treatment, the remaining crowding was recorded. The amount of crowding was assessed with Little's Irregularity Index. Measurements were made intraorally twice by the same clinician using a fine‐tip digital calliper (Digimatic NTD 12‐6‐in C, Mitutoyo, Kanagawa, Japan), and the means of the 2 measurements were recorded |
|
| Notes | Sample size calculation: Reported Other information: Further information was requested from the authors but there was no reply |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomization was done using random permuted blocks of size 6" |
| Allocation concealment (selection bias) | Low risk | "Opaque envelopes were used to allocate treatment. ...Allocation was concealed from the operator and participants during the observation period" |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Low risk | Double blind. Patients were unaware of allocated arch wire type |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | Low risk | Operator was blinded to type of arch wire and outcome of alignment assessed by operator |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in analysis |
| Selective reporting (reporting bias) | High risk | Planned outcomes reported. However, no pain outcomes or adverse effects reported |
| Other bias | Low risk | No other sources of bias identified |
Sebastian 2012
| Methods | Location: Unclear Recruitment period: Not stated Funding source: Not stated Trial design: Parallel group (2 arms), single operator |
|
| Participants | Inclusion criteria: Female patients in postmenarche period between 13 and 15 years of age with crowding in the lower anterior segment and having a mandibular Irregularity Index greater than 6. Class I skeletal pattern, non‐extraction treatment in mandibular arch, eruption of all mandibular teeth with no spacing between them, no relevant medical history, no recent history of intake of drugs such as nonsteroidal anti‐inflammatory drugs (NSAIDs). Patients who may have experienced periodontal disease and hence loss of attachment were avoided. No previous active orthodontic treatment, full arch mechanics, preadjusted edgewise appliance therapy, no therapeutic intervention planned involving intermaxillary or other intraoral or extraoral appliances during the study period Exclusion criteria: Intake of medication during study period Age group: Gp A 13.8 years (SD 0.7), Gp B 13.6 years (SD 0.6) Number randomised: 24 participants Number evaluated: 24 participants |
|
| Interventions |
Comparison: 0.016 superelastic coaxial NiTi versus 0.016 superelastic NiTi Gp A: 0.016 inch coaxial superelastic wire (Regular 7 Stranded Supercable Wire, Speed System Orthodontics, Ontario, Canada) Gp B: 0.016 inch single‐stranded superelastic wire (Rematitan Lite Wire, Dentauram GmbH & Co KG, Ispringen, Germany) All participants used 0.022 x 0.028 inch slot MBT prescription brackets (Victory Series, 3M Unitek, Monrovia, Calif). The arch wire was ligated as fully as possible into the bracket, usually with elastomeric modules. In cases where it was not possible to engage the arch wire with elastomeric module, the tooth was ligated with steel ties. Impressions were taken at 4, 8 and 12 weeks |
|
| Outcomes | Impressions at 4, 8, and 12 weeks. Casts were measured using the co‐ordinate measuring machine, and average tooth movement was calculated to denote the degree of alignment | |
| Notes | Sample size calculation: Reported in detail Randomisation was at the subject level and outcome was studied at the subject level No further information was requested from the author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was done using computer software generated numbers" |
| Allocation concealment (selection bias) | Low risk | "Opaque envelopes were used to allocate the arch wires to 2 groups, each consisting of 12 participants" |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Low risk | "Double blind" However, while it seems likely that the patients and operators could distinguish which type of wire was in use, it is not likely to have introduced a bias |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | Low risk | "Double blind", "All readings were measured by an expert single operator who was not aware of the arch wire specimen used for the arches being measured." Unclear whether the attempts to blind the outcome assessment were successful in a small study, with a single investigator |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in the analysis |
| Selective reporting (reporting bias) | High risk | Planned outcome of alignment reported for each group at 3 time points. However, no pain outcomes or adverse effects reported |
| Other bias | Low risk | No other sources of bias identified |
West 1995
| Methods | Location: Cardiff, Wales. University clinic Recruitment period: Not stated Funding source: Not stated Trial design: Combination parallel/split‐mouth RCT |
|
| Participants | Inclusion criteria: Patients attending clinic for placement of initial arch wire. No previous orthodontic treatment, no quad helix or other palatal expansion device present, and full arch mechanics, straight wire appliance to be used. Patients with previously fitted palatal arches or extraoral traction were eligible for inclusion Exclusion criteria: Relevant medical history Age group: Mean 15 years Number randomised: 62 patients & 74 arch wires Number evaluated: Not stated |
|
| Interventions |
Comparison: Multistrand stainless steel versus superelastic NiTi Gp A (n = 38 arch wires): 0.0155 inch multiple flex steel (Dentaflex, Dentourium, Yorkshire, England) Gp B (n = 36 arch wires): 0.014 inch superelastic NiTi (NiTi Armoco Monrovia, USA) No definite instructions were given regarding system of ligation; clinicians followed usual practice. Ligation systems & slot sizes not reported |
|
| Outcomes | Derived index of tooth alignment (ITA) after 6 weeks. ITA based on Little's Irregularity Index | |
| Notes | Sample size calculation: Reported Other information: MScD dissertation reported: 1. Randomly assigned by means of a table 2. Fixed orthodontic appliances were Roth prescription 0.022 Straight Wire Appliance (Johnston and Johnston) No additional information available from authors |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "the 2 arch wire types were randomly assigned to patients according to a predetermined random allocation scheme" |
| Allocation concealment (selection bias) | High risk | Not mentioned |
| Blinding of participants and personnel (performance bias) Patient reported outcomes | Low risk | Blinding of participants not described, but unlikely to have introduced bias |
| Blinding of outcome assessment (detection bias) Clinician assessed outcomes | High risk | Blinding of outcome assessors not described, but outcomes likely to have been assessed by operators, and this is likely to have introduced a bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on the number of patients or arch wires included in the outcome evaluation |
| Selective reporting (reporting bias) | High risk | ITA reported graphically only. No mean/median reported for each type of wire. No pain or adverse effects outcomes reported |
| Other bias | High risk | Potential for confounding/interaction where patients who had 2 arch wires fitted may have had 2 different wires or 2 the same ‐ detailed information not stated. Also possible confounding effect of different ligation systems chosen by 5 clinicians (not recorded) could have introduced bias. Higher prewire ITA found for steel wire group. Unclear whether a unit of analysis error occurred |
Gp = group M/F = male/female NiTi = nickel titanium RCT = randomised controlled trial SD = standard deviation VAS = visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| AlQabandi 1999 | Not a comparison of initial arch wires |
| Bernhold 2001 | Published as abstract and identified as ongoing study in the first version of the review. Attempt to contact author in 2012 unsuccessful and no subsequent publications found. Insufficient information in abstract to include this study |
| Bloom 1998 | Published as abstract only and no subsequent full publication identified. Insufficient information to include in review |
| Chekay 1999 | Published as abstract only and no subsequent full publication identified. Insufficient information to include in review |
| Dalstra 2004 | Not an RCT. All participants received the same arch wire |
| Fleming 2009 | Not a comparison of initial arch wires |
| Fleming 2009a | Not a comparison of initial arch wires |
| Huffman 1983 | Not an RCT |
| Jones 1984 | Case series |
| Jones 1990 | Not an RCT |
| Kuftinec 1980 | Not an RCT |
| Lew 1988 | Not an RCT |
| Mandall 2006 | Comparison of arch wire sequences and not individual arch wires |
| Ong 2011 | Study evaluates initial arch wire sequence |
| Pandis 2007 | Not a comparison of initial arch wires |
| Weiland 2003 | A CCT split‐mouth study |
CCT = controlled clinical trial RCT = randomised controlled trial
Contributions of authors
Yan Wang and Fan Jian were responsible for designing and co‐ordinating the review, extracting data from papers and writing to authors of the papers for additional information.
Joy Hickman was responsible for updating the background section and obtaining additional data from the three included studies that were also published as dissertations at Cardiff University (Evans 1998; Jones 1992; West 1995).
Wenli Lai organised the retrieval of papers.
Fan Jian, Declan Millet, Susan Furness and Grant McIntyre were responsible for screening search results, screening retrieved papers against inclusion criteria, data collection for the review, obtaining copies of trials, and extracting data from papers, analysis and writing the review.
Susan Furness and Declan T Millett were responsible for assessing risk of bias.
Sources of support
Internal sources
School of Dentistry, The University of Manchester, UK.
-
MAHSC, UK.
The Cochrane Oral Health Group is supported by the Manchester Academic Health Sciences Centre (MAHSC) and the NIHR Manchester Biomedical Research Centre.
External sources
-
National Institute for Health Research (NIHR), UK.
CRG Funding Acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Oral Health Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
-
Cochrane Oral Health Group Global Alliance, UK.
All reviews in the Cochrane Oral Health Group are supported by Global Alliance member organisations (British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; Canadian Dental Hygienists Association, Canada; National Center for Dental Hygiene Research & Practice, USA; and New York University College of Dentistry, USA) providing funding for the editorial process (http://ohg.cochrane.org).
Declarations of interest
The participating review authors declare that they have no financial conflict of interest and that they do not have any associations with industry regarding the subject of this review.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
- Cioffi I, Piccolo A, Tagliaferri R, Paduano S, Galeotti A, Martina R. Pain perception following first orthodontic archwire placement‐‐thermoelastic vs superelastic alloys: a randomized controlled trial. Quintessence International2012; Vol. 43, issue 1:61‐9. [PubMed]
- Cobb NW 3rd, Kula KS, Phillips C, Proffit WR. Efficiency of multi‐strand steel, superelastic Ni‐Ti and ion‐implanted Ni‐Ti archwires for initial alignment. Clinical Orthodontics and Research 1998;1(1):12‐9. [DOI] [PubMed] [Google Scholar]
- Evans TJ. A Clinical Comparison and Performance Perspective of Three Aligning Archwires [MScD dissertation]. Cardiff, UK: University of Wales, 1996. [Google Scholar]; Evans TJ, Jones ML, Newcombe RG. Clinical comparison and performance perspective of three aligning arch wires. American Journal of Orthodontics and Dentofacial Orthopedics 1998;114(1):32‐9. [DOI] [PubMed] [Google Scholar]
- Fernandes LM, Øgaard B, Skoglund L. Pain and discomfort experienced after placement of a conventional or a superelastic NiTi aligning archwire. A randomized clinical trial [Schmerzen und Beschwerden nach Eingliederung eines herkömmlichen und eines superelastischen NiTi‐Nivellierungsbogens]. Journal of Orofacial Orthopedics 1998;59(6):331‐9. [DOI] [PubMed] [Google Scholar]
- Chan LSC. Pain and Discomfort Experienced During Orthodontic Treatment: a Randomised Controlled Clinical Trial of Two Initial Aligning Archwires [MScD dissertation]. Cardiff, UK: University of Wales, 1990. [Google Scholar]; Jones M, Chan C. The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two initial aligning arch wires. American Journal of Orthodontics and Dentofacial Orthopedics 1992;102(4):373‐81. [DOI] [PubMed] [Google Scholar]; Jones ML, Staniford H, Chan C. Comparison of superelastic NiTi and multistranded stainless steel wires in initial alignment. Journal of Clinical Orthodontics. 1990/10/01 1990; Vol. 24, issue 10:611‐3. [PubMed]
- O'Brien K, Lewis D, Shaw W, Combe E. A clinical trial of aligning archwires. European Journal of Orthodontics 1990;12(4):380‐4. [DOI] [PubMed] [Google Scholar]; O'Brien KD. A randomized controlled clinical trial of aligning archwires. British Journal of Orthodontics 1987;14:315. [Google Scholar]
- Pandis N, Polychronopoulou A, Eliades T. Alleviation of mandibular anterior crowding with copper‐nickel‐titanium vs nickel‐titanium wires: a double‐blind randomized control trial. American Journal of Orthodontics and Dentofacial Orthopedics 2009;136(2):152‐3. [DOI] [PubMed] [Google Scholar]
- Sebastian B. Alignment efficiency of superelastic coaxial nickel‐titanium vs superelastic single‐stranded nickel‐titanium in relieving mandibular anterior crowding: a randomized controlled prospective study. The Angle Orthodontist 2012;82(4):703‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West AE. A Clinical Comparison of Two Initial Aligning Archwires [MScD dissertation]. Cardiff, UK: University of Wales, 1992. [Google Scholar]; West AE, Jones ML, Newcombe RG. Multiflex versus superelastic: a randomized clinical trial of the tooth alignment ability of initial arch wires. American Journal of Orthodontics and Dentofacial Orthopedics 1995;108(5):464‐71. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- AlQabandi AK, Sadowsky C, BeGole EA. A comparison of the effects of rectangular and round arch wires in levelling the curve of Spee. American Journal of Orthodontics and Dentofacial Orthopedics 1999;116(5):522‐9. [DOI] [PubMed] [Google Scholar]
- Bernhold M, Bondemark L. Superelastic nickel‐titanium heat‐activated archwires for tooth movement ‐ a prospective randomized study of apical root resorption. Swedish Dental Journal 2001;25:177. [Google Scholar]
- Bloom KL, Bhatia SN. Comparison of copper NiTi and nitinol archwires in initial alignment. European Journal of Orthodontics 1998;20:614. [Google Scholar]
- Chekay BA, Killiany DM, Purcell MV, Frost RA. Apical root resorption: A comparison of wire materials. Journal of Dental Research 1999;78 Special Issue:202 (Abs No 776). [Google Scholar]
- Dalstra M, Melsen B. Does the transition temperature of Cu‐NiTi archwires affect the amount of tooth movement during alignment?. Orthodontics & Craniofacial Research 2004;7(1):21–5. [DOI] [PubMed] [Google Scholar]
- Fleming PS, Dibiase AT, Sarri G, Lee RT. Pain experience during initial alignment with a self‐ligating and a conventional fixed orthodontic appliance system. A randomized controlled clinical trial. The Angle Orthodontist 2009;79(1):46‐50. [DOI] [PubMed] [Google Scholar]
- Fleming PS, DiBiase AT, Sarri G, Lee RT. Comparison of mandibular arch changes during alignment and leveling with 2 preadjusted edgewise appliances. American Journal of Orthodontics and Dentofacial Orthopedics 2009;136(3):340‐7. [DOI] [PubMed] [Google Scholar]
- Huffman DJ, Way DC. A clinical evaluation of tooth movement along arch wires of two different sizes. American Journal of Orthodontics 1983;83(6):453‐9. [PubMed] [Google Scholar]
- Jones ML. An investigation into the initial discomfort caused by placement of an archwire. European Journal of Orthodontics 1984;6(1):48‐54. [DOI] [PubMed] [Google Scholar]
- Jones ML, Staniford H, Chan C. Comparison of superelastic NiTi and multistranded stainless steel wires in initial alignment. Journal of Clinical Orthodontics 1990;24(10):611‐3. [PubMed] [Google Scholar]
- Kuftinec MM, Inman GO. A comparison of plain versus multilooped arch wires in stage I of Begg therapy. American Journal of Orthodontics 1980;78(1):81‐8. [DOI] [PubMed] [Google Scholar]
- Lew K. A comparison of archwires used for initial alignment in Begg treatment. Australian Orthodontic Journal 1988;10(3):180‐2. [PubMed] [Google Scholar]
- Mandall N, Lowe C, Worthington H, Sandler J, Derwent S, Abdi‐Oskouei M, et al. Which orthodontic archwire sequence? A randomized clinical trial. European Journal of Orthodontics 2006;28(6):561‐6. [DOI] [PubMed] [Google Scholar]
- Ong E, Ho C, Miles P. Alignment efficiency and discomfort of three orthodontic archwire sequences: a randomized clinical trial. Journal of Orthodontics 2011;38(1):32‐9. [DOI] [PubMed] [Google Scholar]
- Pandis N, Polychronopoulou A, Eliades T. Self‐ligating vs conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. American Journal of Orthodontics and Dentofacial Orthopedics 2007;132(2):208‐15. [DOI] [PubMed] [Google Scholar]
- Weiland F. Constant versus dissipating forces in orthodontics: the effect on initial tooth movement and root resorption. European Journal of Orthodontics 2003;25(4):335‐42. [DOI] [PubMed] [Google Scholar]
Additional references
- Ballard DJ, Jones AS, Petocz P, Darendeliler MA. Physical properties of root cementum: part 11. Continuous vs intermittent controlled orthodontic forces on root resorption. A microcomputed‐tomography study. American Journal of Orthodontics and Dentofacial Orthopedics 2009;136(1):1‐8; discussion 8‐9. [DOI] [PubMed] [Google Scholar]
- Burstone CJ. Variable‐modulus orthodontics. American Journal of Orthodontics 1981;80(1):1‐16. [DOI] [PubMed] [Google Scholar]
- Burstone CJ, Qin B, Morton JY. Chinese NiTi wire‐‐a new orthodontic alloy. American Journal of Orthodontics 1985;87(6):445‐52. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdinç E, Dinçer B. Perception of pain during orthodontic treatment with fixed appliances. European Journal of Orthodontics 2004;26(1):79‐85. [DOI] [PubMed] [Google Scholar]
- Evans TJ, Durning P. Aligning archwires, the shape of things to come?‐‐a fourth and fifth phase of force delivery. British Journal of Orthodontics 1996;23(3):269‐75. [DOI] [PubMed] [Google Scholar]
- Firestone AR, Scheurer PA, Bürgin WB. Patients' anticipation of pain and pain‐related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. European Journal of Orthodontics 1999;21(4):387‐96. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
- Kapila S, Sachdeva R. Mechanical properties and clinical applications of orthodontic wires. American Journal of Orthodontics and Dentofacial Orthopedics 1989;96(2):100‐9. [DOI] [PubMed] [Google Scholar]
- Keim RG, Gottlieb EL, Nelson AH, Vogels DS 3rd. 2002 JCO study of orthodontic diagnosis and treatment procedures. Part 2. Breakdowns of selected variables. Journal of Clinical Orthodontics 2002;36(11):627‐36. [PubMed] [Google Scholar]
- Kropmans TJ, Dijkstra PU, Stengenga B, Stewart R, Bont LG. Smallest detectable difference in outcome variables related to painful restriction of the temporomandibular joint. Journal of Dental Research 1999;78(3):784‐9. [DOI] [PubMed] [Google Scholar]
- Kusy RP. A review of contemporary archwires: their properties and characteristics. The Angle Orthodontist 1997;67(3):197‐207. [DOI] [PubMed] [Google Scholar]
- Kusy RP, Whitley JQ. Thermal and mechanical characteristics of stainless steel, titanium‐molybdenum, and nickel‐titanium archwires. American Journal of Orthodontics and Dentofacial Orthopedics 2007;131(2):229‐37. [DOI] [PubMed] [Google Scholar]
- Linge BO, Linge L. Apical root resorption in upper anterior teeth. European Journal of Orthodontics 1983;5(3):173‐83. [DOI] [PubMed] [Google Scholar]
- Linge L, Linge BO. Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics 1991;99(1):35‐43. [DOI] [PubMed] [Google Scholar]
- Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. American Journal of Orthodontics 1975;68(5):554‐63. [DOI] [PubMed] [Google Scholar]
- Manzanera D, Montiel‐Company JM, Almerich‐Silla JM, Gandía JL. Orthodontic treatment need in Spanish schoolchildren: an epidemiological study using the Index of Orthodontic Treatment Need. European Journal of Orthodontics 2009;31(2):180‐3. [DOI] [PubMed] [Google Scholar]
- Marques CR, Couto GB, Orestes Cardoso S. Assessment of orthodontic treatment needs in Brazilian schoolchildren according to the Dental Aesthetic Index (DAI). Community Dental Health 2007;24(3):145‐8. [PubMed] [Google Scholar]
- Miura F, Mogi M, Ohura Y, Hamanaka H. The super‐elastic property of the Japanese NiTi alloy wire for use in orthodontics. American Journal of Orthodontics and Dentofacial Orthopedics 1986;90(1):1‐10. [DOI] [PubMed] [Google Scholar]
- Moher D, Schulz KF, Altman D, CONSORT Group. The CONSORT Statement: revised recommendations for improving the quality of reports of parallel‐group randomized trials 2001. Explore (New York, NY) 2005;1(1):40‐5. [DOI] [PubMed] [Google Scholar]
- Ng'ang'a PM, Stenvik A, Ohito F, Ogaard B. The need and demand for orthodontic treatment in 13‐ to 15‐year‐olds in Nairobi, Kenya. Acta Odontologica Scandinavica 1997;55(5):325‐8. [DOI] [PubMed] [Google Scholar]
- Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics 1989;96(1):47‐53. [DOI] [PubMed] [Google Scholar]
- O'Brien KD, Shaw WC, Roberts CT. The use of occlusal indices in assessing the provision of orthodontic treatment by the hospital orthodontic service of England and Wales. British Journal of Orthodontics 1993;20(1):25‐35. [DOI] [PubMed] [Google Scholar]
- Proffit WR. Contemporary Orthodontics. St Louis: CV Mosby Cooperation, 2000. [Google Scholar]
- Quintão CC, Cal‐Neto JP, Menezes LM, Elias CN. Force‐deflection properties of initial orthodontic archwires. World Journal of Orthodontics 2009;10(1):29‐32. [PubMed] [Google Scholar]
- Richmond S, Shaw WC, Stephens CD, Webb WG, Roberts CT, Andrews M. Orthodontics in the general dental service of England and Wales: a critical assessment of standards. British Dental Journal 1993;174(9):315‐29. [DOI] [PubMed] [Google Scholar]
- Riley M, Bearn DR. A systematic review of clinical trials of aligning archwires. Journal of Orthodontics 2009;36(1):42‐51. [DOI] [PubMed] [Google Scholar]
- Rudolph CE. An evaluation of root resorption occurring during orthodontic treatment. Journal of Dental Research 1940;19:367‐71. [Google Scholar]
- Santoro M, Nicolay OF, Cangialosi TJ. Pseudoelasticity and thermoelasticity of nickel‐titanium alloys: a clinically oriented review. Part I: Temperature transitional ranges. American Journal of Orthodontics and Dentofacial Orthopedics. 2001/06/08 2001; Vol. 119, issue 6:587‐93. [DOI] [PubMed]
- Santoro M, Nicolay OF, Cangialosi TJ. Pseudoelasticity and thermoelasticity of nickel‐titanium alloys: a clinically oriented review. Part II: Deactivation forces. American Journal of Orthodontics and Dentofacial Orthopedics. 2001/06/08 2001; Vol. 119, issue 6:594‐603. [DOI] [PubMed]
- Scheurer PA, Firestone AR, Bürgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. European Journal of Orthodontics 1996;18(4):349‐57. [DOI] [PubMed] [Google Scholar]
- Wyk PJ, Drummond RJ. Orthodontic status and treatment need of 12‐year‐old children in South Africa using the Dental Aesthetic Index. Journal of the South African Dental Association 2005;60(8):334‐6, 338. [PubMed] [Google Scholar]
- Whiting‐O'Keefe QE, Henke C, Simborg DW. Choosing the correct unit of analysis in Medical Care experiments. Medical Care 1984;22(12):1101‐14. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Wang Y, Jian F, Lai W, Zhao Z, Yang Z, Liao Z, et al. Initial arch wires for alignment of crooked teeth with fixed orthodontic braces. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD007859.pub2] [DOI] [PubMed] [Google Scholar]


