Abstract
Background:
While bereavement is associated with increased mortality, it is unclear how bereaved families utilize the healthcare system after the death of their loved ones. The aim of this study was to examine the association between bereavement and healthcare expenditures for surviving spouses.
Methods:
We used data from the Health and Retirement Study, a nationally representative cohort study of older adults linked to Medicare claims. We determined spouse’s total Medicare expenditures 2 years before and after their partner’s death across 6 biennial interview waves. Using Coarsened Exact Matching we created a comparison group of non-bereaved dyads. Costs were wage index and inflation adjusted to 2017 dollars. We used generalized linear models and difference-in-differences (DID) analysis to calculate average marginal effects of bereavement on Medicare spending by gender. We also examined subgroup differences based on caregiver status, cause of death and length of terminal illness.
Results:
Our sample consisted of 941 bereaved dyads and a comparison group of 8,899 matched dyads. Surviving female spouses (68% of sample) had a $3,500 increase in spending 2 years after death (p<0.05). Using DID analyses, bereavement was associated with $625 quarterly increase in Medicare expenditures over 2 years for women. There was no significant increase in post-death spending for male bereaved surviving spouses. Results were consistent for spouses who survived at least 2 years after the death of their spouse (70% of sample)
Conclusions:
Bereavement is associated with increased healthcare spending for women regardless of their caregiving status, the cause of death, or length of terminal illness. Further study is required to examine why men and women have different patterns of healthcare spending relative to the death of their spouses.
BACKGROUND
Family members play a critical role in the care of older adults with serious illness. The vast majority of caregivers caring at the end of life (EOL) are unpaid family members.[1] An extensive literature finds that caregivers are vulnerable to increased depression[2] and other health problems,[3, 4] and reduced preventive health behaviors.[5, 6]
The bereavement effect, which finds an increased risk of dying following the death of a spouse has been widely replicated[7–9] including a recent study using the Health and Retirement Study (HRS) which reported a 48% increased risk in mortality.[10] Work in this area also suggests that there are health effects that may explain this increase in mortality.[11]
While we recognize that there are both health risks associated with caregiving and a bereavement effect, we do not fully understand how families themselves utilize the healthcare system, particularly when they are caring for an individual at the EOL. [12–14] In general, most caregivers increase their own utilization once caregiving ends and they can better attend to their own health needs.[15] Similarly, the bereavement literature suggests that there is a spike in use of services by family members following the death of a loved one.[9, 16, 17] Work outside of the U.S. in which healthcare registers capture all utilization records have been particularly informative. Increased spending for bereaved spouses after death have been documented in the Netherlands [18] and Scotland. [19] Following cancer deaths in Denmark, Guldin et al. found increased use of mental health services for survuving spouses. [16] In the UK, Shah et al.[20, 21] documented reduced management of cardiovascular disease before death and increased risk of cardiovascular events after death.
Unfortunately, many of these studies are register based and are unable to comprehensively account for differences in functional impairment and social support among bereaved and nonbereaved individuals. We currently have very little data from U.S. based national samples examining healthcare utilization patterns before or after bereavement.[22] Determining costs around the EOL for caregivers is critical. While there has been considerable attention given to the current unsustainable level of spending on healthcare at the EOL, these costs do not include the potentially significant spillover effects on family members. For example, estimates of disease costs that include the caregivers’ foregone wages and replacement costs of informal care hours fail to consider potential downstream costs associated with the healthcare utilization of the family members.[23, 24] Understanding this impact on costs is particularly relevant to federal health spending as most spousal caregivers are themselves over age 65 and Medicare recipients.[25] Quantifying costs around EOL caregiving may improve estimates of EOL healthcare costs, which may substantially impact policy initiatives, especially in this period of Medicare reform. Additionally, a more comprehensive understanding of the total costs of EOL treatments may impact EOL decision-making for patients and families.
Therefore, the goal of this study was to use a U.S. population sample to determine healthcare utilization and costs for surviving spouses 2 years before and after bereavement. We hypothesized that bereavement would be associated with a significant increase in total Medicare spending for surviving spouses.
Methods
Sample
The study sample is from the HRS, a nationally representative, longitudinal survey of U.S. adults 51 years of age and older.[26] Participants are interviewed either face-to-face or via telephone every two years. If participants are married or living with a partner, their partners (heretofore referred to as “spouses”) are recruited into the study and surveyed. Survey data are linked for eligible participants with individual Medicare claims. Study participants provided informed consent upon enrollment and again for linkage to Medicare claims.
Our study focused on decedents who were married at the time of death between 2000 and 2012 (6 study waves). Of the 8,001 decedents identified in HRS between 2000–2012, 3,456 were married at the time of death. We identified 1,526 decedents (44% of married sample) whose surviving spouses were age 65 and over with fee for service (FFS) Medicare at the time of their spouse’s death. (Decedents with non-FFS or Managed Medicare do not have itemized claims necessary for cost estimates.) Non-bereaved spouses were selected at each survey wave to serve as matched comparisons.
Measures
Outcome Measures:
The primary outcome was the surviving spouse’s total Medicare expenditures 24 months after their spouse’s death. We calculated expenditures at 16 quarterly (3-month) time periods (8 pre and 8 post death). This quarterly measure includes all Medicare payments for inpatient, outpatient, skilled nursing facility, hospice and home care, as well as durable medical equipment. We adjusted expenditures for inflation (2017$) based on the medical services portion of the Consumer Price Index[27], and for geographic differences in Medicare price levels using the 2012 Centers for Medicare and Medicaid Services (CMS) wage index.[28] If the spouse died during the course of the month their costs were still included as part of the corresponding quarterly time period. In secondary analyses we also examined total inpatient and outpatient Medicare costs.
Spousal and decedent factors were drawn from each participant’s last HRS core interview before the decedent’s death and included age, sex, race/ethnicity, education, net-worth (quartile), selfreported health, functional status (ADL independence), residential status (nursing home or community-dwelling), and level of comorbidity. We also identified whether each spouse served as the primary caregiver for the other in the period before death (based on provision of assistance with activities of daily living (ADLs) or instrumental activities of daily living (IADLs) before their death. If the core interview was completed within the month before death, data were drawn from the previous interview.
Caregiving burden and healthcare expenditures vary widely in relation to dementia status and cause of death. Therefore, we assigned subjects to the dementia group if they were determined to have probable dementia at the last available assessment. [23] Those without probable dementia were categorized as cancer, heart disease, and other primary cause of death, as reported in the decedent’s exit interview by their surviving spouse or other designated proxy. Length of terminal illness was based on proxy report at exit interview and was dichotomized as <1 month vs >= 1 month.
Using the decedent’s zip code, each dyad was linked via their hospital referral region (HRR) to the Dartmouth Atlas of Healthcare’s End of Life Expenditure Index (EOL-EI), a measure of physician practice patterns, based upon Medicare beneficiaries’ utilization in the last 2 years of life [29]. We created an indicator for those living in the top quartile of EOL-EI by HRR. We also included decedent’s geographic region: South, Midwest, West and Northeast.
Analysis
To account for observable differences among bereaved and non-bereaved dyads that could be associated with expenditures, we used coarsened exact matching (CEM) to match bereaved and non-bereaved dyads at each survey wave allowing for multiple matches per bereaved dyad.[30] Dyads were matched based on HRS core interview date and using the following 10 decedent and spouse characteristics assessed at the interview prior to death: (1) decedent ADL function (independent or not); (2) decedent age category; (3) decedent self-reported health (poor or fair vs. good/very good/excellent); (4) decedent dementia status; (5) decedent level of comorbidity (none, mild, moderate/severe); (6) spouse age category; (7) spouse gender; (8) spouse ethnicity (black, Hispanic, white/other); (9) spouse education (>= High School education); and (10) spouse level of comorbidity (none, mild, moderate/severe).
Within each matched stratum, non-bereaved matched comparison individuals were assigned the date of death of the decedent as an index date. Expenditures were evaluated relative to the index date. In cases where there were multiple bereaved spouses within a stratum, comparison individuals were randomly assigned to one match for an index date. Matched non-bereaved spouses were dropped if they did not have FFS Medicare at their index date, and only bereaved spouses with matches were kept. Spouses who became bereaved in subsequent years were eligible to be non-bereaved ‘matches’ in earlier waves. Total matches were pooled across survey waves and analyses used clustered standard errors at the spousal ID level. Balance was verified by examining standardized differences in covariates across treatment groups and variance of covariates before and after matching. Standardized differences < 10% indicated adequate balance [31, 32]. For analyses of 24 month post-death spending, we excluded individuals who died during the first year or those who with index date prior to 2011 as data would not have 2 years of data available. For quarterly analyses, surviving spouses were excluded from any interval that they were under 65 (pre-death period only), did not have FFS Medicare, or were not alive at the beginning of the period (post-observation only).
Using the matched sample, we estimated average Medicare spending with 95% confidence intervals for each of the 8 quarterly (3 month) intervals before and 8 quarterly intervals after death among the full sample and by gender. We then estimated differences in 24 month Medicare expenditures, inpatient and outpatient expenditures, and hospital utilization based on GLM models and chi-square test of proportions.
In our primary analysis we estimated a multivariable generalized linear (GLM) model of the association between bereavement and 24 month Medicare expenditures. Due to the skewed distribution of the outcome, we used a gamma distribution with a log link. We assessed model fit with the Box-Cox test, modified Park test, and Pregibon’s link test. Different family and link functions were compared using Akaike’s information criterion (AIC).[33] Regression coefficients were exponentiated into rate ratio estimates and average incremental effects were calculated to produce average treatment effects on the treated. All analyses were adjusted for CEM weights, and standard errors were clustered by spouse ID to account for autocorrelation. In each model we controlled for all covariates included in the match to adjust for any remaining imbalance between the groups after matching as well as the following variables: (1) decedent nursing home status and whether the decedent was the spouse’s primary caregiver; (2) spouse ADL independence, caregiver status, nursing home status, dementia status, Medicaid status, and quartile of net worth; (3) dyadic quartile of EOL-EI by HRR and geographic region. These models were also run using total inpatient and outpatient costs as outcome measures.
Next, we used a GLM model with log link and gamma distribution and calculated marginal effects to estimate excess costs associated with bereavement. Using a difference in differences (DID) model, we estimated whether average quarterly spending 24-months post bereavement was increased compared to average quarterly spending pre-death, and if this difference was greater than that in the comparison group. The estimate of the excess change in spending in the bereaved group, above and beyond the change in the comparison group, is known as the DID estimator. All analyses were adjusted for CEM weights, and standard errors were clustered by spouse ID to account for autocorrelation. Unadjusted and adjusted marginal effects with 95% CI were used to calculate DID estimates. In addition to controlling for previously matched variable and survey wave years, we also adjusted for the following variables: (1) decedent nursing home status and whether the decedent was the spouse’s primary helper; (2) spouse ADL independence, caregivers status, nursing home status, dementia status, Medicaid status, and quartile of net worth; (3) dyadic quartile of EOL-EI by HRR and geographic region. To further explore known gender differences in caregiving[34] and bereavement outcomes,[35] we stratified the full sample by spousal gender.
Next we conducted a number of subgroup analyses. First, spending was examined for the subgroups of spouses who survived at least 2 years post index spouse’s death. We then stratified bereaved spouses by the following characteristics (1) primary caregiver status prior to death, (2) cause of death (dementia, cancer, heart disease, and other); and length of terminal illness. For each subgroup analyses, new CEM weights were estimated to create a matched comparison group and all analyses were stratified by gender and adjusted for matched and additional covariates.
Results
The majority (61.7% or 941/1526) of identified bereaved dyads were successfully matched to non-bereaved dyads across 6 waves using 10 key characteristics (Supplementary Online Appendix Table 1). We identified 8,899 non-bereaved dyads for comparison. Prior to matching, bereaved dyads were significantly different than non-bereaved dyads relative to several demographic and clinical characteristics. For example 30% of those who died had probable dementia compared to only 4% of those who did not die (p<.05). The bereaved sample contributed 20,497 person months of observation during the pre-death period (24 months before the death of the spouse) and 19,630 months of observation post-death (24 months after the death of the spouse). The comparison group contributed 196,417 person months of comparison pre-death and 192,049 person months post-death due to availability of Medicare FFS data.
Two-thirds of surviving spouses were female. Demographic and clinical characteristics by gender for bereaved and non-bereaved matched samples are shown in Table 1. Surviving spouses were predominantly White and the majority had at least a High School education (78% male; 73% female). Only 6% of bereaved spouses had Medicaid and the majority were independent in ADLs (94% male and 90% female). One third of male and female spouses rated their own health as poor/fair. The sample varied by region with greatest representation among the South (41%) followed by the Midwest (31%). One quarter of both bereaved male and female spouses were living in a region with the highest quartile of average EOL spending.
Table 1:
Characteristics of bereaved and matched non-bereaved dyads by gender
| Male Spouses | Female Spouses | |||||
|---|---|---|---|---|---|---|
| Non-Bereaved | Bereaved | Std Diff | Non-bereaved | Bereaved | Std Diff | |
| N=3749 | N=300 | N=5150 | N=641 | |||
| DECEDENT | ||||||
| *Age at core interview, years | 74.84 | 75.17 | 0.01 | 77.85 | 78.32 | 0.01 |
| Non-Hispanic White/Caucasian, % | 88.73 | 90.00 | 0.04 | 90.09 | 92.02 | 0.07 |
| Non-Hispanic black or African American, % | 7.18 | 7.00 | 0.01 | 5.07 | 5.01 | 0.00 |
| Hispanic Ethnicity, % | NR | NR | 0.03 | 3.49 | 2.34 | 0.07 |
| Education, >= High School, % | 78.97 | 77.67 | 0.03 | 74.84 | 73.48 | 0.03 |
| Has Medicaid, % | 8.71 | 6.02 | 0.10 | 5.30 | 6.10 | 0.03 |
| Has Medigap, % | 58.66 | 60.74 | 0.04 | 63.65 | 62.48 | 0.02 |
| *Comorbidity index | 5.33 | 5.33 | 0.00 | 5.62 | 5.62 | 0.00 |
| mild | 78.33 | 78.33 | 0.00 | 78.47 | 78.47 | 0.00 |
| moderate/severe | 16.33 | 16.33 | 0.00 | 15.91 | 15.91 | 0.00 |
| *Independent for ADLs, % | 72.67 | 72.67 | 0.00 | 79.06 | 79.06 | 0.00 |
| *Self Rated Health: Poor/Fair, % | 54.33 | 54.33 | 0.00 | 53.82 | 53.82 | 0.00 |
| *Probable dementia, % | 8.67 | 8.67 | 0.00 | 14.20 | 14.20 | 0.00 |
| Primary caregiver for spouse, % | 12.02 | 10.67 | 0.04 | 10.59 | 10.30 | 0.01 |
| Cause of death Cancer | N/A | 34.33 | N/A | 29.17 | ||
| Heart disease | N/A | 27.00 | N/A | 31.67 | ||
| Dementia | N/A | 8.67 | N/A | 14.20 | ||
| Other | N/A | 30.00 | N/A | 24.96 | ||
| Terminal illness <1 month, % | N/A | 45.67 | N/A | 51.01 | ||
| SPOUSE | ||||||
| *Age at core interview, years | 77.18 | 77.35 | 0.02 | 74.91 | 75.10 | 0.03 |
| *Non-Hispanic White/Caucasian or other, % | 88.83 | 89.33 | 0.02 | 90.90 | 91.73 | 0.03 |
| *Non-Hispanic black or African American, % | 7.33 | 7.33 | 0.00 | 4.52 | 4.52 | 0.00 |
| *Hispanic Ethnicity, % | NR | NR | 0.00 | 2.96 | 2.96 | 0.00 |
| *Education, >= High School, % | 74.00 | 74.00 | 0.00 | 84.24 | 84.24 | 0.00 |
| Bottom quartile networth, % | 15.06 | 17.00 | 0.05 | 10.60 | 13.26 | 0.08 |
| Has Medicaid, % | 5.64 | 6.02 | 0.02 | 4.87 | 5.77 | 0.04 |
| Has Medigap, % | 61.06 | 63.21 | 0.04 | 63.46 | 62.97 | 0.01 |
| *Comorbidity index | ||||||
| mild | 79.53 | 79.53 | 0.00 | 78.78 | 78.78 | 0.00 |
| moderate/severe | 8.72 | 8.72 | 0.00 | 5.46 | 5.46 | 0.00 |
| Independent for ADLs, % | 91.82 | 93.65 | 0.07 | 90.26 | 89.69 | 0.02 |
| Self Rated Health: Poor/Fair, % | 34.10 | 35.00 | 0.02 | 26.19 | 27.93 | 0.04 |
| Probable dementia, % | 8.84 | 6.73 | 0.08 | 4.19 | 5.79 | 0.07 |
| Primary caregiver for decedent, % | 25.22 | 35.33 | 0.22 | 25.11 | 25.74 | 0.01 |
| REGION | ||||||
| Northeast | 14.31 | 13.33 | 0.03 | 16.70 | 14.66 | 0.06 |
| Midwest | 30.21 | 31.00 | 0.02 | 30.56 | 30.89 | 0.01 |
| West | 13.90 | 13.33 | 0.02 | 12.88 | 13.57 | 0.02 |
| South | 41.56 | 42.33 | 0.02 | 39.86 | 40.87 | 0.02 |
| Quartile EOL spending by HRR: | 18.11 | 18.67 | 0.01 | 17.11 | 17.97 | 0.02 |
| Mid-low | 21.19 | 23.33 | 0.05 | 24.13 | 23.28 | 0.02 |
| Mid-high | 34.62 | 33.33 | 0.03 | 31.76 | 34.53 | 0.06 |
| High | 26.08 | 24.67 | 0.03 | 27.00 | 24.22 | 0.06 |
Notes: NR—Not reportable due to CMS cell-size restrictions;
* indicate variable used in coarsened exact match
Within the matched sample, there were no significant differences in spending (total, inpatient, or outpatient) or hospital utilization pre-death among the groups (Table 2). In the 24 month period after death, however, male bereaved spouses had less total ($32,463.98 vs. $26,113.21, p=.01). and inpatient ($13,968.77 vs. $11,085.61, p=.05) spending than matched controls. Among female spouses, while there were no detectable differences before death in hospital days or costs, in the post death period, bereaved female spouses had increased total ($24,832.89 vs. $21,129.76; p=.04) and inpatient ($10,107.67 vs. $7,698.61, p=.04) Medicare costs and significantly more hospital days (4.55 vs., 3.34; p=0.02) than matched controls.
Table 2:
Utilization and Medicare costs 24 months before and after death in matched sample by gender (unadjusted)
| Pre-death | Post-Death | |||||
|---|---|---|---|---|---|---|
| Non-Bereaved | Bereaved | P | Non-Bereaved | Bereaved | P | |
| Male Spouses | N=3,023 | N=237 | N=3,028 | N=245 | ||
| Total Medicare costs Mean |
$27,026.35 | $24,090.51 | 0.20 | $32,463.98 | $26,113.21 | 0.01 |
| Median | $9,695.33 | $8,261.58 | $12,418.45 | $9,867.78 | ||
| IQR | $3,289.31–30,266.19 | $2,385.03–24,999.06 | $4,116.02–43,292.16 | $3,786.51–28,949.47 | ||
| Total inpatient costs | $11,850.12 | $10,095.93 | 0.20 | $13,968.77 | $11,085.61 | 0.05 |
| Total outpatient costs | $3,019.82 | $3,105.54 | 0.84 | $3,526.33 | $2,907.06 | 0.14 |
| Total Hospital days | 3.81 | 3.89 | 0.40 | 5.16 | 4.06 | 0.11 |
| Any inpatient admission | 38.64% | 36.71% | 0.61 | 44.23 | 37.14 | 0.06 |
| Female Spouses | N=4,123 | N=509 | N=4,314 | N=509 | ||
| Total Medicare costs Mean |
$18,514.07 | $18,619.94 | 0.95 | $21,129.76 | $24,832.89 | 0.04 |
| Median | $7,739.76 | $7,011.21 | $7,889.87 | $8,931.29 | ||
| IQR | $3,187.49–20,015.93 | $2,449.60-$18,674.05 | $3,660.45–21,140.08 | $3,183.33–27,454.93 | ||
| Total inpatient costs | $6,613.34 | $7,061.49 | 0.60 | $7,698.61 | $10,107.67 | 0.04 |
| Total outpatient costs | $2,364.19 | $2,524.77 | 0.42 | $2,558.07 | $2,771.85 | 0.47 |
| Total Hospital days | 2.42 | 2.91 | 0.28 | 3.34 | 4.55 | 0.02 |
| Any inpatient admission | 29.35% | 30.65% | 0.62 | 31.51 | 34.71 | 0.21 |
Note: Sample limited to those with complete 24 months FFS data; Total Medicare expenditures wage-index and inflation adjusted to 2017$; p-values based on GLM models (costs and days) and chi square analysis of inpatient admission likelihood; Sample matched on: core year; decedent age, ADL dependence, comorbidity level, probable dementia, self-rated health; spouse age, race/ethnicity, educational attainment, self-rated health, comorbidity level
In multivariable analysis of the matched groups, bereavement was independently associated with a$3,490 mean increase in spending over 2 years for surviving female spouses (p=0.04) (Table 3). A $2,261 increase in inpatient spending (rate ratio = 1.32) was detected for surviving female spouses (p=0.03), although no increase in outpatient spending was evident. There was no association among male surviving spouses or for the overall sample for total, inpatient or outpatient costs, but we did observe a non-significant reduction in outpatient spending post-death for men ($831; p<.10). Our model specification tests indicated that a log link was appropriate, and that either the gamma or Poisson distribution would be appropriate. AIC values indicated that models with gamma distribution and a log link best fit our data. In addition, our results were robust to model specification with consistent post-bereavement increase in spending for females and no increase for males. DID analyses were conducted on female surviving spouses, where the parallel trends assumptions required for DID held [36]. As shown in Table 4, in adjusted DID analyses using the matched sample, bereaved female spouses had an increase of $625 in Medicare expenditures per quarter (p=0.03) over a 24 month period. (See full GLM model for DID adjusted quarterly expenses Supplementary Online Appendix Table 2).
TABLE 3:
Association between bereavement and 24 month postdeath Medicare expenditures by gender in adjusted matched sample
| Total (n=747 bereaved; 7263 non-bereaved) | Male Spouses (n=239 bereaved; 2985 non-bereaved) | Female Spouses (n=508 bereaved; 4278 non-bereaved) | ||
|---|---|---|---|---|
| Total Medicare expenditures | Rate ratio | 1.083 | .95 | 1.18 |
| 95% CI | 0.95 – 1.24 | 0.74 – 1.21 | 1.01 – 1.37 | |
| Average marginal effect | $2,049.89 | $−1,749.91 | $3,490.32 | |
| p-value | (0.24) | (0.66) | (0.04) | |
| Inpatient Medicare costs | Rate ratio | 1.20 | .95 | 1.32 |
| 95% CI | 0.95 – 1.49 | 0.74 – 1.65 | 1.02 – 1.71 | |
| Average marginal effect | $1,889.53 | $1,314.23 | $2,261.03 | |
| p-value | (0.17) | (0.65) | (0.03) | |
| Outpatient Medicare costs | Rate ratio | 0.99 | .79 | 1.14 |
| 95% CI | 0.85 – 1.17 | 0.60 – 1.04 | 0.95 – 1.37 | |
| Average marginal effect | $286.19 | $−831.40 | $22.63 | |
| p-value | (0.17) | (0.10) | (0.92) |
NOTES: Medicare expenditures are wage index & inflation adjusted to 2017$. Sample matched on: core year; decedent age, ADL dependence, comorbidity level, probable dementia, self-rated health; spouse age, race/ethnicity, educational attainment, self-rated health, comorbidity level. GLM models control for matched variables and further adjusted for decedent nursing home status, whether the decedent was the spouse’s primary caregiver; whether the spouse was the decedent’s primary caregiver, spouse ADL independence, spouse nursing home status, spouse dementia status, spouse Medicaid status, spouse quartile of net worth, dyadic quartile of EOL-EI by HRR, and geographic region
Table 4:
Changes in quarterly medical expenditures 2 years post death for surviving female spouses using difference in difference (DID) analysis
| Bereaved N=641 | Not bereaved N=5150 | P-value | |
|---|---|---|---|
| Unadjusted mean quarterly expenditures 2 years before death | $1,974.83 | $1,989.94 | 0.93 |
| Unadjusted mean quarterly expenditures 2 years after death | $2,942.66 | $2,426.45 | 0.02 |
| Unadjusted DID for quarterly expenditures | $611.01 | 0.02 | |
| Adjusted DID for quarterly expenditures | $624.92 | 0.03 | |
Notes: All P-values from GLM with log link and gamma family; Total Medicare expenditures wage-index and inflation adjusted to 2017$; Sample matched on: core year; decedent age, ADL dependence, comorbidity level; spouse age, race/ethnicity, educational attainment, self-rated health, comorbidity level; Adjusted analyses control for: all matching variables and high EOL spending level by HRR, region, quartile of net worth; decedent self-rated health, nursing home status, probable dementia status, whether surviving spouse was decedent’s primary caregiver; spouse ADL dependence, nursing home status, probable dementia status, and whether the decedent was spouse’s primary caregiver.
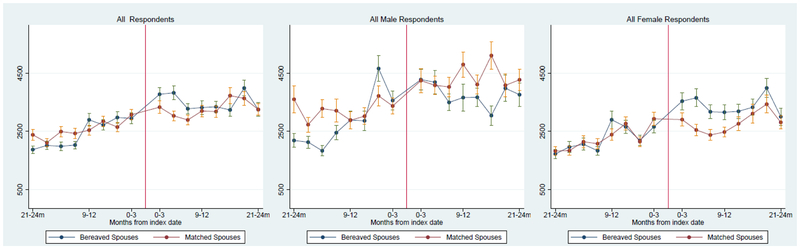
Consistent with these findings, in descriptive figures of the matched samples, we see an overall increase in spending after bereavement, with the largest differential 3–6 months after death (Figure 1). This pattern remains among female bereaved spouses who experience an increase in spending only after bereavement that peaks 3–6 months after death and is maintained consistently the first year after death with no discernible differences across the matched sample during pre-death period. Among men, there was no increase in spending associated with bereavement post-death. However, we did see decreases in post-death spending among bereaved men, especially 6–18 months after death, and a substantial pre-bereavement increase in spending for men 3–6 months before their spouses’ death. In 80% of dyads, the surviving spouse lived at least 24 months after the death of their spouse. When limiting our analyses to these dyads, the patterns of observed spending for men and women were similar (Supplementary Online Appendix Figure 1).
Figure 1: Average Medicare expenditures and 95% CI for bereaved and matched non-bereaved spouses.
Panel A: Full sample (n=941 bereaved; n= 8,899 non-bereaved)
Panel B: Male Spouses (n=300 bereaved; n=3749 non-bereaved)
Panel C: Female Spouses (n=641 bereaved; n=5150 non-bereaved)
Notes: Total Medicare expenditures wage-index and inflation adjusted to 2017$
Almost one third (29%) of surviving spouses were identified as the primary caregiver for the decedent in the wave before death. While females have significantly increased spending in the 24 month period after death regardless of their caregiving status (See Table 5), the effect is especially strong among those identified as primary caregivers (average marginal effect =$9,562.17 p=.05). Stratified analyses by cause of death and length of illness find that bereavement is associated with 37% increased spending for women in particular if their spouse dies of cancer (average marginal effect = $5,729, p=.05) or had an illness of short duration (<1 month) (average marginal effect = $5,934, p=.01). In every subgroup we examined, female surviving spouses had increased spending post-bereavement (See Table 5 and Supplementary Online Appendix Tables 3–5). For men, the small sample sizes of the stratified analyses preclude definitive inferences about overall spending patterns. However, we observed heterogeneous patterns among larger subgroups. For instance, male surviving spouses had increased spending post-bereavement if their spouse died of heart failure. In contrast to female surviving spouses, we did not observe a relationship between length of spouse’s illness before death and males’ post-bereavement spending.
TABLE 5:
Association between bereavement and 24 month postdeath Medicare expenditures for surviving male and female spouses by caregiver status, cause of death and length of terminal illness
| Total | Male Spouses | Female Spouses | |||
|---|---|---|---|---|---|
| CAREGIVER STATUS | Primary caregivers (n=221 bereaved; n=1362 non-bereaved) | Rate ratio | 1.10 | 0.93 | 1.51 |
| 95% CI | 0.80 – 1.50 | 0.61 – 1.44 | 1.02 – 2.25 | ||
| Average marginal effect | $2,683.84 | $−2,387.57 | $9,562.17 | ||
| p-value | 0.56 | 0.76 | 0.04 | ||
| Non-primary caregivers (n=526 bereaved; n=6820 non-bereaved) | Rate ratio | 1.13 | 1.05 | 1.19 | |
| 95% CI | 0.98 – 1.31 | 0.80 – 1.39 | 0.99 – 1.42 | ||
| Average marginal effect | $3,082.49 | $1,572.03 | $3,647.71 | ||
| p-value | 0.12 | 0.71 | 0.05 | ||
| CAUSE OF DEATH | Dementia (n=84 bereaved; n=110 non-bereaved)) | Rate ratio | 1.31 | 0.77 | 1.43 |
| 95% CI | 0.91 − 1.88 | 0.32 – 1.85 | 0.93 – 2.21 | ||
| Average marginal effect | $8,658.75 | $−10,455.65 | $10,982.96 | ||
| p-value | 0.17 | 0.57 | 0.13 | ||
| Cancer (n=239 bereaved; n=4943 non-bereaved) | Rate ratio | 1.24 | 1.11 | 1.37 | |
| 95% CI | 0.94 – 1.62 | 0.67 – 1.85 | 0.99 – 1.88 | ||
| Average marginal effect | $4,541.05 | $2,969.38 | $5,728.53 | ||
| p-value | 0.12 | 0.68 | 0.05 | ||
| Heart Disease (n=232 bereaved; n=4445 non-bereaved) | Rate ratio | 1.23 | 2.54 | 1.13 | |
| 95% CI | 0.99 – 1.53 | 1.46 – 4.42 | 0.87 – 1.45 | ||
| Average marginal effect | $4,929.77 | $30,157.52 | $2,478.43 | ||
| p-value | 0.05 | 0.01 | 0.36 | ||
| Other (n=201 bereaved; n=3809 non-bereaved) | Rate ratio | 0.98 | 0.60 | 1.28 | |
| 95% CI | 0.76 – 1.26 | 0.42 – 0.86 | 0.96 – 1.70 | ||
| Average marginal effect | $−521.88 | $−17,942.44 | $5,442.20 | ||
| p-value | 0.88 | 0.01 | 0.08 | ||
| LENGTH OF TERMINAL ILLNESS | <1 MONTH (n=373 bereaved; n=5178 non-bereaved) | Rate ratio | 1.24 | 1.30 | 1.31 |
| 95% CI | 1.04 – 1.48 | 0.92 – 1.84 | 1.07 – 1.61 | ||
| Average marginal effect | $5,617.77 | $7,960.05 | $5,933.83 | ||
| p-value | 0.03 | 0.14 | 0.01 | ||
| >=1 MONTH (n=374 bereaved; n=5594 non-bereaved) | Rate ratio | 0.97 | 0.75 | 1.12 | |
| 95% CI | 0.80 – 1.17 | 0.55 – 1.03 | 0.88 – 1.41 | ||
| Average marginal effect | $−764.99 | $−9,628.09 | $2,300.01 | ||
| p-value | 0.75 | 0.08 | 0.35 |
NOTES: Medicare expenditures are wage index & inflation adjusted to 2017$. Sample matched on: core year; decedent age, ADL dependence, comorbidity level, probable dementia, self-rated health; spouse age, race/ethnicity, educational attainment, self-rated health, comorbidity level. GLM models control for matched variables and further adjusted for decedent nursing home status, whether the decedent was the spouse’s primary caregiver; whether the spouse was the decedent’s primary caregiver, spouse ADL independence, spouse nursing home status, spouse dementia status, spouse Medicaid status, spouse quartile of net worth, dyadic quartile of EOL-EI by HRR, and geographic region
Patterns of spending pre and post death in quarterly intervals by subgroup and gender are shown in Appendix Figures 2–5. The previously noted increased spending for men in the period before their wives’ death is still evident among men across many subgroup analyses.
Discussion
Using a nationally representative study of older adults in the U.S., we find that bereaved female spouses have an increase in total Medicare expenditures during the 2 years after the death of their spouses which translates to an additional $543 per quarter after death. We did not find any evidence for increased post-death spending for bereaved male spouses although we did observe increased spending for men in the period immediately before their wives’ death. Our work is consistent with previous findings demonstrating increased costs related to bereavement [19, 37], but is the first of its kind to tackle this issue in a U.S. sample with adjustment for important spouse and decedent characteristics.
Gender plays a key role in whether individuals provide care and how they care for loved ones at the EOL. Our work supports previous literature which found that there are profound gender differences in the consequences of care provision on the health of the caregiver.[38] Some hypothesize that observed gender differences may be in part due to caregiving being more physically burdensome for women.[39, 40] In particular, women have described their caregiver role as physically taxing [41] and report that they tend not to ask for help in managing their own health problems.[42] We also hypothesize that new financial strain and its negative effect on health may explain a portion of the effects of bereavement on healthcare expenditures observed in this study. [7] These financial challenges are likely to have greater impact on surviving female spouses. [43, 44] Of note, the widowhood effect on mortality is generally found to be stronger for male widows.[45] This may be because men are less likely than women to have independent social networks and may struggle more to adapt to the loss of help with tasks at home. Our work substantiates key gender differences around bereavement and health and suggests more research is warranted to identify opportunities to modify or prevent negative health and financial outcomes for surviving spouses.
Our work also found that men whose wives are near death may be at elevated risk of health care use and increased costs. This is consistent with other work which suggests that the ‘widowhood effect’ may begin before death.[11] This effect is likely separate from a bereavement/mortality effect in that it persists among those who survive beyond 2 years after their wife’s death. In post-hoc analyses, we further explored the observed spending spike for men during this 3-month period before their wife’s subsequent death. We found that more than 10% of men in the sample were hospitalized at least once in the period 3–6 months before their spouse’s death. A review of admission diagnoses by the physician co-authors did not reveal any clear pattern of diagnoses. We did not find any relationship between pre-death hospitalization for male spouses and caregiving role, although small sample size prevents extensive analysis. We also examined remarriage in this sample. While rates of remarriage in the 2 years post-death were significantly higher for surviving men than women, they were overall very rare and unlikely to impact results. More research on widowers is needed to further examine this finding.
We conducted several subgroup analyses to explore possible reasons for the spending patterns observed. All of these analyses confirmed women spend more after-death, in particular those who serve as primary caregivers and those who care for husbands with cancer. Subgroup analyses within the sample of surviving male spouses were substantially limited by sample size and thus highly sensitive to outliers. (For example, we only identified 26 widowers whose wives died with dementia.) Future research will require larger samples of male surviving spouses to elucidate mechanisms by which bereavement effects may vary by gender.[46]
Our findings should be interpreted with a number of potential limitations in mind. Because we used Medicare claims data to measure costs, we were limited to older spouses with FFS Medicare. We were unable to include Medicare Part D data on medication use. On average, individuals incur their highest medical costs in the last few months of life, so we did not exclude spouses who died during the 12 month follow-up period, which would bias our findings toward the null. Additionally, our use of matching, although robust, cannot adjust for unmeasured factors and unobserved differences between the groups, such as personal preferences and goals of care. Furthermore, we were unable to apply DID analysis to our sample of men or subgroups as it failed to meet model assumptions.[36] Finally, DID analysis, although critical for examining excess costs due to bereavement, only examines differences over the whole 24-month period. It does not capture more fine-grained differences across quarters or time-varying confounding.
While our work demonstrates an association between bereavement and higher post-death Medicare expenditures for surviving female spouses, it raises a number of issues that require further study. Further examination of reasons for increased spouse spending post death, such as lack of preventive or health maintenance services, during the caregiving phase may help to determine how and if this increase in spending may be prevented. This study did not capture provider type (e.g., primary care visits) or specific health maintenance tests or procedures (e.g., hemoglobin A1C, screening colonoscopy), but we did assess and found no differences in outpatient spending within our sample. Also, we cannot determine whether the observed increased costs for bereaved female spouses is due to bereavement itself, or to women not attending to their own health care needs while serving as EOL caregivers. Although our findings were robust to a range of sensitivity analyses (including primary caregiving status before death), other studies are needed to replicate and verify the patterns we have observed. Moreover, we did not examine other sources of healthcare spending including individual out-ofpocket expenditures. We could not include self-reported out-of-pocket expenditures as this information is collected every 2 years in HRS in intervals that do not correspond with the timing of death. A better understanding of these costs and household financial burdens could also reveal opportunities to provide necessary support services. Finally, future work must focus more on gender differences in caregiving in general and during the EOL period in particular. This is especially important as we have increasingly more men serving as caregivers[47] and much of the existing literature fails to acknowledge the gendered nature of caregiving.[41, 48, 49] Unfortunately, this may prove challenging as there are fewer males among surviving spouses in the general population (e.g., only one-third of surviving spouses in our sample are male), thus limiting the ability to conduct meaningful subgroup analyses.
Current policy initiatives including creation of accountable care organizations are designed to improve both health outcomes and the cost effectiveness of the healthcare system. Advancing these policies requires a better understanding of what drives high spending at EOL and what the downstream effects of EOL care are on spouses and entire family networks. By simultaneously examining healthcare utilization in spousal dyads we can begin to understand the differential impact of a person’s EOL treatments on spousal caregiver’s healthcare utilization.
Conclusion
Our findings suggest that bereavement is associated with increased healthcare spending for women regardless of their caregiving status, the cause of death, or length of terminal illness. While further study is required to examine why men and women have different patterns of healthcare spending around bereavement, our works suggest that there may be an opportunity to better support the needs of caregiving families who play a critical role in EOL care, and by doing so, lower downstream healthcare costs. Medicare, as the primary insurer for nearly all older adults in the U.S., should consider this interdependency of married couples’ healthcare experiences and incentivize models of care that promote high value healthcare provision to both individuals.
Supplementary Material
KEY POINTS.
Men and women have different patterns of healthcare spending relative to the death of their spouses.
Women exhibit significant increases in healthcare spending after the death of their spouse.
End-of-life spending estimates should account for this substantial associated spending.
Acknowledgements
The Health and Retirement Study is funded by the National Institute of Aging (NIA) (NIA U01 AG009740) and the Social Security Administration. The study investigators were supported by: National Institute on Aging K01AG047923 (Dr. Ornstein); National Institute on Aging R01AG054540 (Dr. Kelley); and VA HSR&D 16–140 (Dr. Garrido). Funding sources had no role in the design, conduct, and analysis of this study or in the decision to submit the manuscript for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Funding The HRS is funded by the National Institute of Aging (NIA) (NIA U01 AG009740) and the Social Security Administration. The study investigators were supported by: National Institute on Aging K01AG047923 (Dr. Ornstein); National Institute on Aging R01AG054540 (Dr. Kelley); and VA HSR&D 16–140 (Dr. Garrido).
Footnotes
Data Availability Statement The code used in the analysis is available from the authors upon request. Data are restricted based on data use agreement with authors and CMS.
Conflict of interest: None of the authors have financial conflicts of interest to declare.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Contributor Information
Katherine Ornstein, Department of Geriatrics and Palliative Medicine, Institute for Translational Epidemiology, Icahn School of Medicine at Mount Sinai, Box 1070, One Gustave Levy Place, New York, NY 10029, Katherine.ornstein@mssm.edu, Ph: 212-659-5555/ F: 212-849-2566.
Melissa M. Garrido, Department of Health Law, Policy and Management, Boston VA Healthcare System, Boston University School of Public Health, 150 S. Huntington Ave, Boston, MA 02130, garrido@bu.edu, 617-819-5198.
Albert L. Siu, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, Box 1070, One Gustave Levy Place, New York, NY 10029, albert.siu@mssm.edu, Ph: 212-241-4290.
Evan Bollens-Lund, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, Box 1070, One Gustave Levy Place, New York, NY 10029, evan.bollens-lund@mssm.edu, Ph: 212-241-3160.
Omari-Khalid Rahman, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, Box 1070, One Gustave Levy Place, New York, NY 10029, omari-khalid.rahman@mssm.edu, Ph: 212-241-3160.
Amy S. Kelley, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, Box 1070, One Gustave Levy Place, New York, NY 10029, amy.kelley@mssm.edu, Ph: 212-241-1446.
References
- 1.Ornstein KA, et al. , A National Profile Of End-Of-Life Caregiving In The United States. Health Aff (Millwood), 2017. 36(7): p. 1184–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinquart M and Sorensen S, Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol.Aging, 2003. 18(2): p. 250–267. [DOI] [PubMed] [Google Scholar]
- 3.Buyck JF, et al. , Informal Caregiving and the Risk for Coronary Heart Disease: The Whitehall II Study. J Gerontol A Biol Sci Med Sci, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho SC, et al. , Impact of caregiving on health and quality of life: a comparative population-based study of caregivers for elderly persons and noncaregivers. J Gerontol A Biol Sci Med Sci, 2009. 64(8): p. 873–9. [DOI] [PubMed] [Google Scholar]
- 5.Son J, et al. , The caregiver stress process and health outcomes. J Aging Health, 2007. 19(6): p. 871–87. [DOI] [PubMed] [Google Scholar]
- 6.Reeves KW, Bacon K, and Fredman L, Caregiving associated with selected cancer risk behaviors and screening utilization among women: cross-sectional results of the 2009 BRFSS. BMC Public Health, 2012. 12: p. 685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elwert F and Christakis NA, The effect of widowhood on mortality by the causes of death of both spouses. Am J Public Health, 2008. 98(11): p. 2092–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parkes CM, Benjamin B, and Fitzgerald RG, Broken heart: a statistical study of increased mortality among widowers. Br Med J, 1969. 1(5646): p. 740–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stroebe M, Schut H, and Stroebe W, Health outcomes of bereavement. Lancet, 2007. 370(9603): p. 1960–73. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan AR and Fenelon A, Patterns of widowhood mortality. J Gerontol B Psychol Sci Soc Sci, 2014. 69(1): p. 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vable AM, et al. , Does the “widowhood effect” precede spousal bereavement? Results from a nationally representative sample of older adults. Am J Geriatr Psychiatry, 2015. 23(3): p. 283–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McHorney CA and Mor V, Predictors of bereavement depression and its health services consequences. Med Care, 1988. 26(9): p. 882–93. [DOI] [PubMed] [Google Scholar]
- 13.Moore MJ, Zhu CW, and Clipp EC, Informal costs of dementia care: estimates from the National Longitudinal Caregiver Study. J.Gerontol.B Psychol.Sci.Soc.Sci, 2001. 56(4): p. S219–S228. [DOI] [PubMed] [Google Scholar]
- 14.Schulz R, Cook T, and Hunt G, AD caregivers: healthcare utilizations and cost over 18 months. The Gerontologist, 2011. 51(S2): p. 568. [Google Scholar]
- 15.Grasel E, When home care ends--changes in the physical health of informal caregivers caring for dementia patients: a longitudinal study. J Am Geriatr Soc, 2002. 50(5): p. 843–9. [DOI] [PubMed] [Google Scholar]
- 16.Guldin MB, et al. , Healthcare utilization of bereaved relatives of patients who died from cancer. A national population-based study. Psychooncology, 2013. 22(5): p. 1152–8. [DOI] [PubMed] [Google Scholar]
- 17.Prigerson HG, Maciejewski PK, and Rosenheck RA, Preliminary explorations of the harmful interactive effects of widowhood and marital harmony on health, health service use, and health care costs. Gerontologist, 2000. 40(3): p. 349–57. [DOI] [PubMed] [Google Scholar]
- 18.Rolden HJ, van Bodegom D, and Westendorp RG, Changes in health care expenditure after the loss of a spouse: data on 6,487 older widows and widowers in the Netherlands. PLoS One, 2014. 9(12): p. e115478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stephen AI, et al. , The economic cost of bereavement in Scotland. Death Stud, 2015. 39(1–5): p. 151–7. [DOI] [PubMed] [Google Scholar]
- 20.Shah SM, et al. , Impact of partner bereavement on quality of cardiovascular disease management. Circulation, 2013. 128(25): p. 2745–53. [DOI] [PubMed] [Google Scholar]
- 21.Carey IM, et al. , Increased risk of acute cardiovascular events after partner bereavement: a matched cohort study. JAMA Intern Med, 2014. 174(4): p. 598–605. [DOI] [PubMed] [Google Scholar]
- 22.Ornstein KA, et al. , Downstream Effects of End-of-Life Care for Older Adults with Serious Illness on Health Care Utilization of Family Caregivers. J Palliat Med, 2015. 18(9): p. 736–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hurd MD, et al. , Monetary costs of dementia in the United States. N Engl J Med, 2013. 368(14): p. 1326–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van den Berg B, Brouwer WB, and Koopmanschap MA, Economic valuation of informal care. An overview of methods and applications. Eur J Health Econ, 2004. 5(1): p. 36–45. [DOI] [PubMed] [Google Scholar]
- 25.Family Caregiver Alliance. Caregiving. 2009. [cited 2013 9/19/2013]; Available from: http://www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=2313.
- 26.Health and Retirement Study. 2013. [cited 2013 9/17/2013]; Available from: http://hrsonline.isr.umich.edu/.
- 27.United States Department of Labor Bureau of Labor Statistics. Consumer Price Index. 2018. [cited 2018 July 15]; Available from: https://www.bls.gov/cpi/.
- 28.MEDPAC. Medicare Payment Advisory Commission. July 15, 2018]; Available from: http://www.medpac.gov/.
- 29.Wennberg JE and Cooper M. The Dartmouth Atlas of Health Care. 2013. [cited 2013 9/17/2013]; Available from: http://www.dartmouthatlas.org/.
- 30.Iacus CM, King G, and Porro G, Causal Inference without Balance Checking: Coarsened Exact Matching. Political Analysis, 2011. 20: p. 1–24. [Google Scholar]
- 31.Garrido MM, et al. , Methods for Constructing and Assessing Propensity Scores. Health Serv Res, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Austin PC, Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med, 2009. 28(25): p. 3083–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deb P and Norton EC, Modeling Health Care Expenditures and Use. Annu Rev Public Health, 2018. 39: p. 489–505. [DOI] [PubMed] [Google Scholar]
- 34.Katz SJ, Kabeto M, and Langa KM, Gender disparities in the receipt of home care for elderly people with disability in the United States. JAMA, 2000. 284(23): p. 3022–7. [DOI] [PubMed] [Google Scholar]
- 35.Davydow DS, et al. , Depressive symptoms in spouses of older patients with severe sepsis. Crit Care Med, 2012. 40(8): p. 2335–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ryan AM, Burgess JF Jr., and Dimick JB, Why We Should Not Be Indifferent to Specification Choices for Difference-in-Differences. Health Serv Res, 2015. 50(4): p. 1211–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang AY, Zyzanski SJ, and Siminoff LA, Differential patient-caregiver opinions of treatment and care for advanced lung cancer patients. Soc Sci Med, 2010. 70(8): p. 1155–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morgan T, et al. , Gender and family caregiving at the end-of-life in the context of old age: A systematic review. Palliat Med, 2016. 30(7): p. 616–24. [DOI] [PubMed] [Google Scholar]
- 39.Washington KT, et al. , Gender Differences in Caregiving at End of Life: Implications for Hospice Teams. J Palliat Med, 2015. 18(12): p. 1048–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pinquart M and Sorensen S, Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J Gerontol B Psychol Sci Soc Sci, 2006. 61(1): p. P33–45. [DOI] [PubMed] [Google Scholar]
- 41.Williams LA, et al. , ‘Because it’s the wife who has to look after the man’: A descriptive qualitative study of older women and the intersection of gender and the provision of family caregiving at the end of life. Palliat Med, 2016. [DOI] [PubMed] [Google Scholar]
- 42.DiGiacomo M, et al. , Transitioning from caregiving to widowhood. J Pain Symptom Manage, 2013. 46(6): p. 817–25. [DOI] [PubMed] [Google Scholar]
- 43.Burkhauser RV, et al. , Until death do us part: an analysis of the economic well-being of widows in four countries. J Gerontol B Psychol Sci Soc Sci, 2005. 60(5): p. S238–46. [DOI] [PubMed] [Google Scholar]
- 44.DiGiacomo M, et al. , The business of death: a qualitative study of financial concerns of widowed older women. BMC Womens Health, 2015. 15: p. 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moon JR, et al. , Widowhood and mortality: a meta-analysis. PLoS One, 2011. 6(8): p. e23465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dunlay SM, et al. , Patient and Spousal Health and Outcomes in Heart Failure. Circ Heart Fail, 2017. 10(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.2015 Report: Caregiving in the U.S 2015, National Alliance for Caregiving and the AARP Public Policy Institute [Google Scholar]
- 48.Calasanti T and King N, Taking ‘women’s work’ ‘like a man’: husbands’ experiences of care work. Gerontologist, 2007. 47(4): p. 516–27. [DOI] [PubMed] [Google Scholar]
- 49.Calasanti T, Feminist gerontology and old men. J Gerontol B Psychol Sci Soc Sci, 2004. 59(6): p. S305–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.