Abstract
Mucoepidermoid carcinomas (MECs) are generally found in salivary gland, but they have also been mentioned in other organs such as the larynx, esophagus, breast. MECs are considered to be a low-grade carcinoma and their occurrence in the thyroid is extremely rare. We present a 54-year-old male patient admitted to our clinic, complaining about having back pains for approximately three months. A lumbosacral spine MRI and a PET/CT scan revealed multiple lesions in the L4, L5, S1 vertebra bodies, sacral bone and left pelvis bone, suggesting of a metastatic disease. The result of thyroid FNA was carcinoma and a biopsy of the vertebra bone confirmed the presence of a metastatic carcinoma. A total thyroidectomy and level VI neck dissection was conducted followed by palliative external beam radiotherapy (30 Gy) to the vertebra bodies, sacral bone and left pelvis bone. In pathological studies, the diagnosis of thyroid mucoepidermoid carcinoma was confirmed. Six months after treatment, the patient died due to severe pain and fatigue caused by the disease. Here, we report a rare case with bone metastasis as the first symptom of MEC and a brief review of published literature on the subject.
Key Words: Mucoepidermoid carcinomas, Thyroid, Mucoepidermoid, Bone metastasis
Introduction
Mucoepidermoid carcinomas (MECs) are generally found in salivary gland, but they have also been mentioned in other organs such as the larynx, esophagus, breast. MECs are considered to be a low-grade carcinoma and their occurrence in the thyroid is extremely rare [1]. MEC of the thyroid were first described by Rhatigan et al., in 1977 and since then there have only been 46 documented cases found in the published literature, but they have a successful prognosis rate almost as good as MECs of the salivary gland, with only eight cases reported with poor prognosis so far [2, 3, 4, 5, 6].
Here, we report a case with bone metastasis as the first symptom of MEC and a brief review of published literature on the subject. We also report the ninth case with poor prognosis in which the patient passed away six months after the surgery.
Case Report
A 54-year-old male patient was admitted to our clinic, complaining about having back pains for approximately three months. The patient had no history of hypertension, diabetes mellitus, tuberculosis or any neck swelling, and neurological examination showed no abnormalities. A lumbosacral spine MRI (magnetic resonance image) scan revealed multiple lesions in the L4, L5, S1 vertebra bodies, sacral bone and left pelvis bone, suggesting of a metastatic disease (Fig. 1). A PET (positron emission tomography) scan showed abnormal hypermetabolic foci in the L4, L5, S1 vertebra bodies, sacral bone, left pelvis bone and left thyroid lobe, giving further indication of metastatic tissues (Fig. 2).
Fig. 1.
A lumbosacral spine MRI scan revealed multiple lesions in the L4, L5, S1 vertebra bodies, sacral bone and left pelvis bone, suggesting of a metastatic disease.
Fig. 2.
A PET scan showed abnormal hypermetabolic foci in the L4, L5, S1 vertebra bodies, sacral bone, left pelvis bone and left thyroid lobe.
The patient had no previous history of neck irradiation and his family history was negative for any form of thyroid disease. Clinical examination of the neck using ultrasound revealed a left-sided nodule of 2 cm in size. Routine blood tests and thyroid function tests were also within normal limits. However, FNA (fine needle aspiration) of thyroid tumor and biopsy of the vertebra bone confirmed the presence of a metastatic carcinoma.
Once the carcinoma was confirmed, a total thyroidectomy and level VI neck dissection was conducted. Histology analysis revealed a microscopic focus of intrathyroidal low-grade MEC within the 2 cm nodule, as well as in one lymph node, however, no papillary features were identified. Postoperative, the patient was treated with palliative external beam radiotherapy (30 Gy) to the vertebra bodies, sacral bone and left pelvis bone to relieve pain. The patient did not receive radioactive iodine therapy. Six months after treatment, the patient died due to severe pain and fatigue caused by the disease.
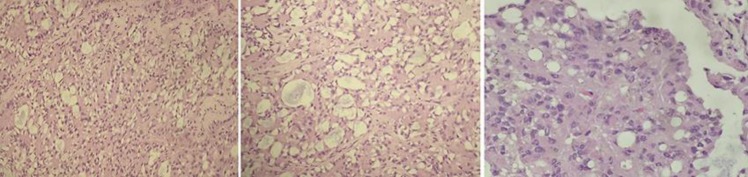
In pathological studies that followed, there were no indicators of papillary carcinoma or follicular carcinoma, and no evidence of Hashimoto's thyroiditis in the thyroid parenchyma. Immunohistochemical analysis showed positive results for thyroglobulin, confirming that the carcinoma primary origin site is the thyroid, and thus the diagnosis of thyroid mucoepidermoid carcinoma was confirmed (Fig. 3).
Fig. 3.
Histology analysis revealed a low-grade MEC.
Discussion
Mucoepidermoid carcinomas (MECs) occur more commonly in the salivary gland, where approximately 10% of all salivary gland tumors are reported as benign MECs and approximately 35% are reported as malignant MECs. However, MECs can also occur in other organs such as the larynx, esophagus, breast tissue, lungs, pancreas, and thyroid gland. From literature research and our experience, MEC of the thyroid are rarely occurrences, constituting less than 0.5% of all thyroid malignancies, and only 46 case reports in published literature since their first description by Rhatigan et al., in 1977 [2, 3, 4, 5, 6].
According to those 46 reported cases (Table 1, Table 2, Table 3, Table 4, Table 5) [2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15], occurrence of MEC is more commonly in females with a ratio of 1.56: 1. Diagnosis age ranges from 10 to 91 years have been reported, with the mean being approximately 46.4 years. Patient with thyroid MEC show no symptoms of painless, while the tumor itself is usually a unilateral mass in the thyroid with reduced uptake in thyroid scans. The incidence rate of extrathyroidal extension is 14.8% (7/47 patients, including our case as the 47th), and approximately 42.2% of patients have nodal metastases (19/45 patients, two patients were not included in the total of 47 patients). Because MEC could arise from de-differentiation of pre-existing WDTC (papillary and follicular thyroid cancer) [12], the probability of nodal metastases occurrence would be high. However, in our case, there were no indicators of WDTC, Hashimoto's thyroiditis, however one of the four central compartment lymph nodes showed positive indicators of metastatic tissue post-surgery.
Table 1.
Literature review of thyroid mucoepidermoid carcinoma
| Author [Ref.] | N | Age/sex | Clinical findings | Extra-thyroid extension | Neck node metastasis | Distant metastasis | Treatment | Pathology | Follow-up |
| Rhatigan [2] | 1 | 20/F | “Cold” nodule left upper lobe | None | None | None | Total thyroidectomy | MEC with intercellular bridges LT, EA | ANED 18 mo |
| Franssila [3] | 2 | 25/F | Left neck mass; 2.5-cm nodule L thyroid lobe | None | Ipsilateral nodal metastasis | None | Total thyroidectomy | MEC | ANED 17 mo |
| Franssila [3] | 3 | 10/F | Painful nodule: right neck ×5 mo; Small tumor L upper thyroid lobe mo | None | Bilateral | None | Total thyroidectomy plus external irradiation (4,400 rad) | MEC; LT | ANED ×10 yr |
| Franssila [3] | 4 | 54/F | Neck mass; firm nodule of isthmus and R thyroid lobe | Direct extension into esophagus and peri-thyroidal soft | Ipsilateral nodal metastasis | None | Total thyroidectomy plus external irradiation and chemotherapy | Anaplastic but partly papillary carcinoma pleomorphism, increased mitotic activity and prominent necrosis; psammoma body found in metastatic deposit | DOD at 13 mo |
| Mizukami [4] | 5 | 44/F | Right neck mass ×1 yr with recent enlargement; “cold” nodule R thyroid lobe | None | Contralateral nodal metastasis (anterior cervical area) 10 mo after surgery | None | Subtotal thyroidectomy | MEC with keratinization and intercellular bridges; LT | ANED ×20 mo |
| Harach [4] | 6 | 18/M | Right neck mass ×2 mo; i.2-cm nodule R upper thyroid lobe | None | Nodal metastasis | None | Total thyroidectomy plus external irradiation (5,500 rad) | MEC with keratinization; psammoma bodies; LT | ANED ×11 yrs |
| Katoh [4] | 7 | 56/F | Known HT with recent development of thyroid nodules; 2-cm nodule R thyroid lobe and 1 cm nodule L thyroid lobe | None | 0 | None | Total R lobectomy and subtotal L lobectomy | MEC with horny pearls and prominent keratinization; FA (R lobe nodule); LT | ANED ×11 mo |
| Sambade [5] | 8 | 11/F | NG | NG | Nodal metastasis | NG | NG | MEC with massive fibrosis, nuclear features of TPC and psammoma bodies; coexistent TPC | Lost to follow-up |
MEC, mucoepidermoid carcinoma; LT, lymphocytic thyroiditis; HT, Hashimoto's thyroiditis; FA, follicular adenoma; TPC, thyroid papillary carcinoma; AN, adenomatoid nodules; NG, not given; ANED, alive no evidence of disease; AWD, alive with disease; DOD, died of disease; R, right; L, left; mo, month; yr; year.
Table 2.
Literature review of thyroid mucoepidermoid carcinoma (continued)
| Author [Ref.] | N | Age/sex | Clinical findings | Extra-thyroid extension | Neck node metastasis | Distant metastasis | Treatment | Pathology | Follow-up |
| Sambade [5] | 9 | 20/ F | NG | NG | Nodal metastasis | Nodal metastasis; pulmonary metastasis 7 yrs after diagnosis | NG | MEC with nuclear features of TPC and psammoma bodies; coexistent TPC | AWD ×22 yrs |
| Sambade [5] | 10 | 67/ F | NG | NG | Nodal metastasis | NG | NG | MEC with nuclear features of TPC; coexistent TPC | Lost to follow-up |
| Sambade [5] | 11 | 11/ M | NG | NG | Nodal metastasis | NG | NG | MEC with nuclear features of TPC and psammoma bodies; coexistent TPC | AWD ×5 yr |
| Sambade [5] | 12 | 58/F | NG | NG | Nodal metastasis | NG | NG | MEC with nuclear features of TPC and psammoma bodies; coexistent TPC | Dead 10 days postoperatively |
| Sambade [5] | 13 | 15/M | NG | NG | Nodal metastasis | NG | NG | MEC with nuclear features of TPC; LT | ANED ×6 mo |
| Sambade [5] | 14 | 47/M | NG | None | None | None | NG | MEC with nuclear features of TPC; LT | ANED ×20 mo |
| Tanda [5] | 15 | 33/M | Painless mass L neck × 4 mo; “cold” nodule measuring 6×3 cm in R thyroid lobe | None | None | None | R hemithy-roidectomy | MEC with associated; ciliated epithelium | ANED ×24 mo |
| Bonde-son [5] | 16 | 35/M | R thyroid mass and vocal cord paralysis; history of neck irradiation during childhood | Tumor invaded the recurrent laryngeal nerve | Nodal metastasis; | None | Subtotal thyroidectomy plus external irradiation (6,600 rad in and I 131 (1,200 mCi); | MEC with intimate with typical TPC; SM | AWD ×12 yr |
| Larson [5] | 17 | 61/F | Dyspnea ×2 mo with R pleural effusion; recent onset of R hip pain; an immovable R thyroid lobe nodule was found associated with tracheal deviation | None | None | Metastasis to pleura and bone (thoracic vertebrae) | Radiotherapy; recent case | MEC diagnosed by FNA; incisional biopsy of pleural metastasis showed a MEC with keratin pearls | NG |
MEC, mucoepidermoid carcinoma; LT, lymphocytic thyroiditis; HT, Hashimoto's thyroiditis; FA, follicular adenoma; TPC, thyroid papillary carcinoma; AN, adenomatoid nodules; NG, not given; ANED, alive no evidence of disease; AWD, alive with disease; DOD, died of disease; R, right; L, left; mo, month; yr; year.
Table 3.
Literature review of thyroid mucoepidermoid carcinoma (continued)
| Author [Ref.] | N | Age/sex | Clinical findings | Extra-thyroid extension | Neck node metastasis | Distant metastasis | Treatment | Pathology | Follow-up |
| Wenig [5] | 18 | 46/ M | Painless swelling in midline of the neck | Perithyroidal skeletal muscle | None | None | Left lobectomy | MEC with keratinization; LT; TPC; AN | ANED ×15 yr |
| 19 | 57/ F | Painless swelling in midline of the neck | None | None | None | Isthmusectomy | MEC with keratinization; LT | Lost to follow-up | |
| 20 | 52/ M | Initial check-up | None | None | None | Right lobectomy | MEC with keratinization; LT | ANED ×13 yr | |
| 21 | 46/ F | Heavy feeling in right neck area; cold nodule identified | None | None | None | Total thyroidectomy | MEC with keratinization; LT | ANED ×8 yr | |
| 22 | 44/ F | Pain left-sided neck mass | None | None | None | Left lobectomy | MEC with keratinization; LT; AN | ANED ×2 yr | |
| 23 | 29/ F | Pain left-sided neck mass | None | None | None | Right lobectomy | MEC with keratinization; LT | ANED ×1.5 yr | |
| Bozo Kruslin [6] | 24 | 33/M | A rapidly enlarging mass in the left thyroid lobe | None | None | Nodal metastasis after 6 mo | Total thyroidectomy | MEC | ANED ×16 mo |
| Baloch [7] | 25 | 27/F | Cold nodule | None | None | None | Total thyroidectomy | MEC | ANED ×7 yr |
| 26 | 64/ M | Right thyroid mass | None | None | None | Total thyroidectomy | MEC, tall cell, TPC | DOD ×3 mo | |
| 27 | 83/ F | Right thyroid mass | Widely invasive | None | None | Right lobectomy | MEC, anaplastic, TPC | Mets to lung DOD after 5 mo | |
| 28 | 55/ M | NA | None | None | None | Total thyroidectomy and neck dissection | MEC | NA | |
| 29 | 36/ F | Left thyroid mass | None | None | None | Total | MEC | NA | |
| Minagawa [6] | 30 | 52/ M | Diffuse goiter and enlarged cervical, axillary and inguinal lymph nodes | None | Enlarged cervical | A metastatic lesion at the first thoracic vertebra | Radiation, chemotherapy | MEC | DOD ×2 mo |
| Bhan-darkar ND [8] | 31 | 42/F | Painful left neck mass | None | 3 lymph nodes positive for metastasis | None | Thyroidectomy and selective neck dissection; chemoradiation | MEC; LT | ANED ×22 mo |
MEC, mucoepidermoid carcinoma; LT, lymphocytic thyroiditis; HT, Hashimoto's thyroiditis; FA, follicular adenoma; TPC, thyroid papillary carcinoma; AN, adenomatoid nodules; NG, not given; ANED, alive no evidence of disease; AWD, alive with disease; DOD, died of disease; R, right; L, left; mo, month; yr; year.
Table 4.
Literature review of thyroid mucoepidermoid carcinoma (continued)
| Author [Ref.] | N | Age/sex | Clinical findings | Extra-thyroid extension | Neck node metastasis | Distant metastasis | Treatment | Pathology | Follow-up |
| Mizuo Ando [9] | 32 | 67/M | Non-tender thyroid mass | Invaded left recurrent laryngeal nerve | None | None | Subtotal thyroidectomy | MEC | ANED ×18 mo |
| Shindo K [10] | 33 | 91/M | Left upper neck with pain | Invaded the surrounding muscles, submandibular gland, thyroid cartilage, cricoid cartilage, and trachea | Enlarged lymph nodes were attached to the left jugular vein, thoracic duct, and bilateral recurrent nerves | None | Total thyroidectomy, bilateral neck dissection, and resections of left submandibular gland and left jugular vein; radiation | MEC | DOD ×4 mo 2 mo from the operation, CT revealed multiple lung metastases and thoracic lymph node metastases |
| Farhat NA [11] | 34 | 47/F | Right-sided thyroid nodule | None | None | None | Total thyroidectomy and selective right neck lymph node dissection; chemotherapy and radiation | MEC | Follow-up not at our institution with a 6-mo interval |
| 35 | 63/F | Nodule in the left lower lobe | None | None | None | Total | MEC, TPC | ANED×11 mo | |
| 36 | 65/F | Nodule in the left lower lobe | None | None | None | Total | MEC | ANED×3 yr | |
| Prichard RS [12] | 37 | 22/F | Left-sided thyroid nodule during her first pregnancy | None | None | None | Total, radioactive iodine and thyroxine suppression | MEC, TPC | NA1 yr later with a palpable nodule in the left lateral jugular chain |
| 38 | 52/F | Long-standing right-sided goiter | None | 3/5 + | None | Total thyroidectomy, central neck node dissection | MEC | ANED×15 mo | |
| 39 | 58/M | Progressive dyspnea | None | None | None | Total thyroidectomy, radioactive iodine ablation and thyroxine suppression | MEC | ANED×6 mo | |
| Obidike S [13] | 40 | 64/F | Small lump on the left side of her neck | None | None | None | Total | MEC | NA |
MEC, mucoepidermoid carcinoma; LT, lymphocytic thyroiditis; HT, Hashimoto's thyroiditis; FA, follicular adenoma; TPC, thyroid papillary carcinoma; AN, adenomatoid nodules; NG, not given; ANED, alive no evidence of disease; AWD, alive with disease; DOD, died of disease; R, right; L, left; mo, month; yr; year.
Table 5.
Literature review of thyroid mucoepidermoid carcinoma (continued)
| Author [Ref.] | N | Age/sex | Clinical findings | Extra-thyroid extension | Neck node metastasis | Distant metastasis | Treatment | Pathology | Follow-up |
| Arezzo A [10] | 41 | 66/ F | Mass | Yes | NG | None | Operation Radiotherapy + I + chemotherapy | MEC, TPC | ANED ×11 mo |
| Jung YH [10] | 42 | 50/M | Thyroid mass with dysphasia and hoarseness | None | None | Yes | Total thyroidectomy and neck node dissection: radiation | MEC, TPC | NG |
| Taconet S [14] | 43 | 86/M | Thyroid nodule, 47 mm | None | None | None | Total thyroidectomy | MEC, TPC | ANED ×16 mo |
| Fulciniti F [15] | 44 | 34/F | A firm and fixed nodule in the isthmic region of the thyroid | NG | NG | NG | NG | MEC, TPC | NG |
| Cameselle Teijeiro J [10] | 45 | 62/F | Rapidly growing mass in the right anterior cervical region for the last 4 mo | None | Yes | None | Total thyroidectomy and limited lateral neck dissection; chemotherapy, I 131 | MEC, anaplastic carcinoma | DOD ×10 mo |
| Vázquez Ramírez F [10] | 46 | 57/M | Dysphagia, dysphonia and odynophagia, diffuse enlargement of the thyroid gland with multiple, bilateral, palpable lymph nodes in the cervical, supraclavicular, paratracheal and retrocaval chains | Yes | Yes | None | Chemotherapy | MEC, anaplastic carcinoma | DOD×1 mo |
MEC, mucoepidermoid carcinoma; LT, lymphocytic thyroiditis; HT, Hashimoto's thyroiditis; FA, follicular adenoma; TPC, thyroid papillary carcinoma; AN, adenomatoid nodules; NG, not given; ANED, alive no evidence of disease; AWD, alive with disease; DOD, died of disease; R, right; L, left; mo, month; yr; year.
Although MECs are generally considered low-grade tumors, there have also been reports of high-grade variants, as well as several cases with metastasis to the esophagus, trachea, lungs, and liver [1]. However, primary thyroid MEC metastasis to the bone is a rare occurrence and has only been reported twice before in literature. In our study, the patient was initially admitted to our clinic with complaints of pain in the lumbar spine and left pelvis bone. PET and CT scans went on to reveal a mass on the left thyroid gland, as well as multiple metastasis at L4, L5, S1 spine bones and the left pelvis bone. Here, we present the third reported case of MEC metastases to bone at the time of diagnosis.
The histogenesis of thyroid MEC has been broadly debated in the reported literature. Initially, Rhatigan et al., 1977, suggested that MEC could originate from salivary gland rest, however, evidence for this has been uncertain, therefore this claim is largely disregarded [2].
Afterwards, it has been proposed that MECs derive from remnants of the ultimobranchial apparatus called the SCN (solid cell nest) [3]. However, positive results for immunohistochemical markers, such as TTF-1, PAX8, and calcitonin, contradict the SCN origin hypothesis and suggest the isthmus as the origin site [6].
Otherwise, many patients with concurrent WDTCs and MECs have been reported in the literature [3, 5, 7, 10]. Pathological results reveal that WDTC may undergo squamous and mucinous metaplasia to give rise to MEC, therefore advocating the hypothesis that MEC originates from follicular epithelium. Among the 46 patients which have been reported, 20 of them have some form of relationship with WDTC (42.6%). According to Prichard et al., authors suggest that most cases of MEC of the thyroid arise from metaplastic de-differentiation of WDTC rather than directly from benign squamous metaplasia, salivary gland rests, SCN, or thyroglossal duct remnants [12].
Surgical excision with total thyroidectomy plays an important role in treatment. However, a few selected patients managed successful by hemithyroidectomy were reported in the relevant literature [5]. The prophylactic central neck node dissection for patient with MEC is controversial [12]. External beam radiotherapy, chemotherapy have been used to treat MEC, however, there is still debate about adjuvant therapies [10, 11, 12]. In our study, postoperative, the patient was treated by palliative external radiotherapy to vertebra bodies, sacral bone and left pelvis bone for palliative purposes because he has metastased to bone at the time of diagnosis.
Most doctors acknowledge MEC of the thyroid as a low-grade malignant tumor. Prognosis for thyroid MEC is good, with several cases of disease-free survival of more than 10 years have been reported [3, 5]. Nevertheless, most cases in published literature report patients diagnosed with locally advanced tumors in the form of local invasion or of cervical lymph node metastasis. Moreover, among the 46 MEC cases reported so far, only 8 patients died between 2 to 13 months after diagnosis, two of whom had shown lung metastasis. In our case, the patient passed away six months after treatment due to severe pain and fatigue caused by the disease.
Conclusion
Mucoepidermoid carcinoma is a rare malignancy of the thyroid with only 46 cases reported to date. Although MEC of the thyroid is usually considered a low-grade malignant tumor, several cases with adverse outcomes have been reported. According to the past reports, only eight cases of thyroid MEC with poor prognosis were described. Herein, we have described a very rare case of thyroid MEC with metastasis to the bone with a poor prognostic result.
Statement of Ethics
The patient has given their written informed consent to publish their case (including publication of images). The study protocol was approved by the institute's committee on human research.
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
None.
References
- 1.Cameselle-Teijeiro J, Wenig B, Sobrinho-Simoes M, Albores- Saavedra J. Mucoepidermoid carcinoma . WHO Pathology and Genetics Tumours of Endocrine Organs. In: DeLellis RA, Lloyd RV, Heity PU, Eng C, editors. IARC Press. Lyon: 2004. pp. pp 82–83. [Google Scholar]
- 2.Rhatigan RM, Roque JL, Bucher RL. Mucoepidermoid carcinoma of the thyroid gland. Cancer. 1977 Jan;39((1)):210–4. doi: 10.1002/1097-0142(197701)39:1<210::aid-cncr2820390133>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 3.Franssila KO, Harach HR, Wasenius VM. Mucoepidermoid carcinoma of the thyroid. Histopathology. 1984 Sep;8((5)):847–60. doi: 10.1111/j.1365-2559.1984.tb02400.x. [DOI] [PubMed] [Google Scholar]
- 4.Tanda F, Massareui G, Bosincu L. Primary mucoepidermoid carcinoma of the thyroid. Surg Pathol. 2000;3:317–24. [Google Scholar]
- 5.Wenig BM, Adair CF, Heffess CS. Primary mucoepidermoid carcinoma of the thyroid gland: a report of six cases and a review of the literature of a follicular epithelial-derived tumor. Hum Pathol. 1995 Oct;26((10)):1099–108. doi: 10.1016/0046-8177(95)90272-4. [DOI] [PubMed] [Google Scholar]
- 6.Minagawa A, Iitaka M, Suzuki M, Yasuda S, Kameyama K, Shimada S, et al. A case of primary mucoepidermoid carcinoma of the thyroid: molecular evidence of its origin. Clin Endocrinol (Oxf) 2002 Oct;57((4)):551–6. doi: 10.1046/j.1365-2265.2002.01599.x. [DOI] [PubMed] [Google Scholar]
- 7.Baloch ZW, Solomon AC, LiVolsi VA. Primary mucoepidermoid carcinoma and sclerosing mucoepidermoid carcinoma with eosinophilia of the thyroid gland: a report of nine cases. Mod Pathol. 2000 Jul;13((7)):802–7. doi: 10.1038/modpathol.3880140. [DOI] [PubMed] [Google Scholar]
- 8.Bhandarkar ND, Chan J, Strome M. A rare case of mucoepidermoid carcinoma of the thyroid. Am J Otolaryngol. 2005 Mar-Apr;26((2)):138–41. doi: 10.1016/j.amjoto.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 9.Ando M, Nakanishi Y, Asai M, Maeshima A, Matsuno Y. Mucoepidermoid carcinoma of the thyroid gland showing marked ciliation suggestive of its pathogenesis. Pathol Int. 2008 Nov;58((11)):741–4. doi: 10.1111/j.1440-1827.2008.02303.x. [DOI] [PubMed] [Google Scholar]
- 10.Shindo K, Aishima S, Okido M, Ohshima A. A poor prognostic case of mucoepidermoid carcinoma of the thyroid: a case report. Case Rep Endocrinol. 2012;2012:862545. doi: 10.1155/2012/862545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farhat NA, Faquin WC, Sadow PM. Primary mucoepidermoid carcinoma of the thyroid gland: a report of three cases and review of the literature. Endocr Pathol. 2013 Dec;24((4)):229–33. doi: 10.1007/s12022-013-9267-6. [DOI] [PubMed] [Google Scholar]
- 12.Prichard RS, Lee JC, Gill AJ, Sywak MS, Fingleton L, Robinson BG, et al. Mucoepidermoid carcinoma of the thyroid: a report of three cases and postulated histogenesis. Thyroid. 2012 Feb;22((2)):205–9. doi: 10.1089/thy.2011.0276. [DOI] [PubMed] [Google Scholar]
- 13.Obidike S, Aftab F. Rare Case of Mucoepidermoid Carcinoma of the Thyroid Gland. Thyroid Disorders Ther. 2016;5((01)):1. [Google Scholar]
- 14.Taconet S, Bosq J, Hartl D, Schlumberger M, Leboulleux S, Scoazec JY, et al. Composite Mucoepidermoid Carcinoma and Columnar Cell Variant of Papillary Carcinoma of the Thyroid: A Case Report and Review of the Literature. Int J Surg Pathol. 2016 Jun;24((4)):336–40. doi: 10.1177/1066896915626281. [DOI] [PubMed] [Google Scholar]
- 15.Fulciniti F, Vuttariello E, Calise C, Monaco M, Pezzullo L, Chiofalo MG, et al. Combined papillary and mucoepidermoid carcinoma of the thyroid gland: a possible collision tumor diagnosed on fine-needle cytology. Report of a case with immunocytochemical and molecular correlations. Endocr Pathol. 2015 May;26((2)):140–4. doi: 10.1007/s12022-015-9364-9. [DOI] [PubMed] [Google Scholar]