Abstract
Introduction
Morbidly adherent placenta (MAP) is a rare obstetric complication, especially in cases of multiple gestation. We present a case of MAP complicating a dichorionic diamniotic (DCDA) twin pregnancy requiring delivery by emergency cesarean hysterectomy at 30 + 2 weeks of gestation.
Case Presentation
A 36-year-old woman, G3P2, with a DCDA twin pregnancy and known MAP presented to the labour ward at 30 + 2 weeks of gestation with evidence of pre-eclampsia and fulminating HELLP syndrome. Delivery was indicated due to fetal distress, demonstrated by pathological findings on cardiotocography, acutely deranged liver functions and worsening thrombocytopenia. An emergency cesarean hysterectomy was performed with postoperative monitoring in the intensive-care unit. The patient was discharged home on two oral antihypertensive agents. Her platelet count and liver functions were normalized prior to discharge.
Discussion
Delivery planning for pregnancies complicated by MAP should commence early in the antenatal period, especially in cases where there is an anticipated risk of preterm delivery, such as multiple pregnancy. Multidisciplinary elective and emergency care plans should be developed and include interventional radiology services when available. Established protocols help to standardize care of these high-risk pregnancies and aid in decision making in emergency scenarios, such as the one presented.
Keywords: Morbidly adherent placenta, Multiple pregnancy, Dichorionic diamniotic twin pregnancy, Pre-eclampsia, HELLP syndrome
Highlights
-
•
Twin pregnancy with morbidly adherent placenta is rare.
-
•
Twin pregnancies with morbidly adherent placenta require early planning of the delivery.
-
•
A multidisciplinary team should be consulted for management of these pregnancies.
-
•
Delivery planning should make provision for both elective and emergency scenarios.
-
•
Interventional radiology services may reduce maternal morbidity peri-operatively.
1. Introduction
Morbidly adherence placenta (MAP) is characterized by the invasion of placental villi into the uterine wall and an absence of an intervening decidua basalis. It occurs in 1 in every 2500 deliveries [[1], [2], [3]]. Obstetric complications secondary to MAP develop when the placenta fails to separate from the uterus after delivery, resulting in massive haemorrhage [4]. The associated sequelae include maternal anaemia, disseminated intravascular coagulation, multi-organ dysfunction syndrome, hysterectomy and death [[4], [5], [6]].
There is limited published evidence to guide management of multiple pregnancy complicated by MAP. A literature review identified a series of eight case reports describing twin pregnancies with a MAP [4,[7], [8], [9], [10], [11], [12], [13]]. Cho et al. [13] described the successful non-surgical management of MAP, using methotrexate and thus preserving fertility. In comparison, cesarean hysterectomy, as either a single-stage [7,[9], [10], [11], [12], [13]] or a two-stage [8] procedure, was performed in the remaining seven cases, of which three required termination of pregnancy at a pre-viable gestation [4,12,13]. In total, only two cases reported delivery of two live, viable foetuses in twin pregnancies complicated by MAP [7,8].
We present a case of MAP complicating a dichorionic diamniotic (DCDA) twin pregnancy that required delivery by emergency cesarean hysterectomy at 30 + 2 weeks of gestation due to foetal distress, pre-eclampsia (PET) and fulminating HELLP syndrome, and discuss the importance of multidisciplinary care plans for both elective and emergency delivery in cases of MAP.
2. Case Presentation
A 36-year-old woman, G3P2, who had undergone two previous lower-segment cesarean sections, presented with a DCDA twin pregnancy complicated by MAP, diagnosed on second-trimester ultrasound (see Fig. 1). The placenta of twin 1 was located on the anterior uterine wall and was separate to the placenta of twin 2, which covered the endocervical os and invaded into the myometrium, anteriorly. A magnetic resonance imaging (MRI) scan was planned for 32 weeks of gestation to further assess placental location and whether there was any invasion of twin 2's placenta into the posterior myometrium, as this was not clear on ultrasound alone.
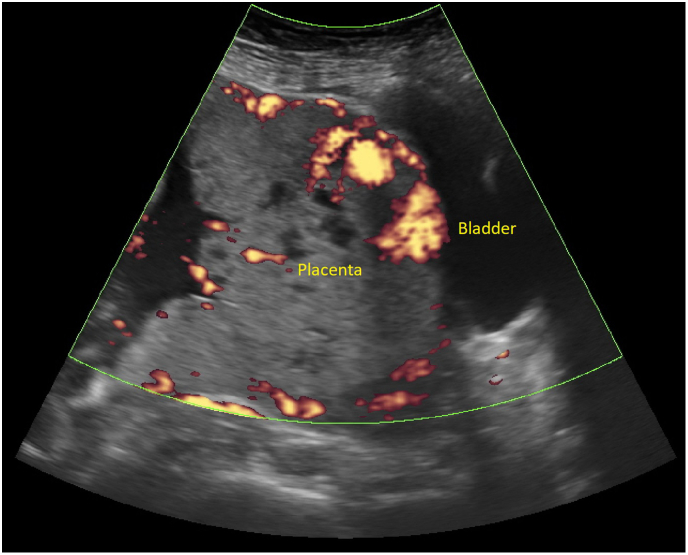
Fig. 1.
Transabdominal ultrasound scan of twin 2's morbidly adherent placenta. There is marked thinning of the myometrium anteriorly, with no appreciable myometrial tissue between the placenta and the bladder serosa. Several irregular sonolucent spaces are present, likely representing placental lacunae. Color Doppler demonstrates evidence of neovascularity, especially along the disrupted bladder line.
Delivery planning began at 28 weeks of gestation by a multidisciplinary team involving obstetricians, anaesthetists and interventional radiology. There was discussion regarding the timing of delivery due to increased risk of preterm labour with multiple pregnancy, highlighting the importance of planned elective delivery to allow placement of balloon catheters in the internal iliac arteries. Further discussion regarding the delivery plan was arranged to follow placental mapping by MRI.
The patient presented to the labour ward at 30 + 2 weeks of gestation complaining of nausea, vomiting and abdominal pain secondary to uterine contractions. She was hypertensive and oliguric. Investigations revealed abnormal liver function and thrombocytopenia consistent with severe PET and HELLP syndrome (LDH 1326 U/L, ALT 536 U/L, AST 838 U/L, platelet count 75 * 109/L). The patient's kidney function was not deranged, though the urine protein to creatinine ratio (132) and urate (0.42 U/L) were both markedly elevated. Cardiotocography monitoring demonstrated evidence of fetal distress of twin 1, with reduced variability and shallow, late decelerations. Emergency delivery was indicated in view of fetal distress, severe PET and fulminating HELLP syndrome.
A multidisciplinary team including two consultant obstetricians, a gynecological oncologist and a senior anaesthetist were involved in the operative management. Due to the urgency of delivery, there was insufficient time for pre-operative catheterization of the internal iliac arteries by the interventional radiology service, which had been intended as part of the elective delivery plan. A midline laparotomy was performed under general anaesthetic, followed by a transfundal uterine incision, avoiding disruption to both placentas. Both twins were born by breech extraction and delivered to the neonatology team for transfer to the neonatal intensive-care unit. The placenta of twin 1 was delivered by continuous cord traction before the uterine incision was closed, leaving the morbidly adherent placenta of twin 2 in situ. A total abdominal hysterectomy and bilateral salpingectomy was then completed as previously planned. The continuing intraoperative blood loss and falling platelet count (35 * 109/L) were corrected by massive transfusion of 4 units of packed red blood cells, 4 units of platelets and 2 units of fresh frozen plasma. The blood loss on completion was estimated to be 2 L.
The patient was transferred to the intensive-care unit postoperatively and was continued on a magnesium sulphate infusion for a total 24 h for blood pressure control as well as to reduce the risk of eclamptic seizures. She required antihypertensive therapy for a total of four weeks postpartum. Her deranged liver function and thrombocytopenia resolved prior to discharge, seven days after cesarean hysterectomy.
Histopathology confirmed full-thickness invasion of the anterior myometrium and serosa by the placenta of twin 2. No other abnormalities were identified.
3. Discussion
Cases of MAP complicating multiple pregnancy are uncommon and present unique challenges. Morbidity is decreased with multidisciplinary planning in the antenatal period and a planned elective delivery. Imaging with tertiary ultrasound and MRI can assist with delivery planning by documenting the extent of placental invasion, as well as any involvement of surrounding structures. Features suggestive of MAP on ultrasound and MRI include multiple placental lacunae, disruption of the bladder line, myometrial thinning with placental bulge, abnormal vascularity and focal penetration of the uterine serosa by an exophytic mass [14]. Interventional radiology techniques such as placement of balloon catheters intraoperatively or internal iliac artery embolization after delivery of the fetus are shown to reduce intraoperative blood loss [15]. Once again, though, data are mostly limited to singleton pregnancies and there is a paucity of published evidence to guide management in cases of multiple pregnancy [15,16].
It is vital to commence planning for both elective and emergency delivery early in pregnancy, especially in cases of multiple pregnancy complicated by MAP, given the high rates of pre-term delivery. In the case presented here, the development of severe PET, HELLP syndrome and evidence of fetal distress, demonstrated by a pathological CTG, necessitated early, unplanned delivery. Nevertheless, the multidisciplinary meeting at 28 weeks of gestation significantly assisted in formulating delivery care plans as well as counselling the patient regarding delivery outcomes, specifically a cesarean hysterectomy. Placental mapping with ultrasound, involvement of experienced senior staff and timely decision making in this case also contributed to the largely uncomplicated intraoperative and postoperative course [[4], [5], [6]].
Contributors
Both authors were involved in the clinical care of the patient and contributed to the conception, drafting, review and revision of the manuscript. Both authors saw and approved the final version of the paper and take full responsibility for the work.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patient Consent
Informed consent was obtained from the patient for publication of this case report.
Provenance and Peer Review
This case report was peer reviewed.
References
- 1.Groom K.M., Paterson-Brown S. Placenta praevia and placenta praevia accreta–a review of aetiology, diagnosis and management. Fetal Matern. Med. Rev. 2001;12:41–66. [Google Scholar]
- 2.Silver R.M., Barbour K.D. Placenta accreta spectrum: accreta, increta, and percreta. Obstetr. Gynecol. Clin. 2015;42:381–402. doi: 10.1016/j.ogc.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Comstock C.H. Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet. Gynecol. 2005;26:89–96. doi: 10.1002/uog.1926. [DOI] [PubMed] [Google Scholar]
- 4.Carugno J., Martins J.G., Andrade F. Morbidly adherent placenta in the second trimester in a twin pregnancy, complicated by massive hemorrhage and peritoneo-vaginal fistula–the importance of a multidisciplinary approach. Ann. Clin. Case Rep. 2017;2:1482. [Google Scholar]
- 5.Khong T.Y., Staples A., Chan A.S., Keane R.J., Wilkinson C.S. Pregnancies complicated by retained placenta: sex ratio and relation to pre-eclampsia. Placenta. 1998;19:577–580. doi: 10.1016/s0143-4004(98)90017-0. [DOI] [PubMed] [Google Scholar]
- 6.Allahdin S., Voigt S., Htwe T.T. Management of placenta praevia and accreta. J. Obstet. Gynaecol. 2011;31:1–6. doi: 10.3109/01443615.2010.532248. [DOI] [PubMed] [Google Scholar]
- 7.Matsubara S., Takahashi H., Usui R., Morisawa H., Nakamura H., Takei Y. Cesarean hysterectomy for placenta previa accreta in dichorionic twin: a surgery that remains challenging. J. Matern. Fetal Neonatal Med. 2016;29:3151–3152. doi: 10.3109/14767058.2015.1118034. [DOI] [PubMed] [Google Scholar]
- 8.Atalay M.A., Atalay F.O., Demir B.C. What should we do to optimise outcome in twin pregnancy complicated with placenta percreta? A case report. BMC Pregnancy Childbirth. 2015;15(289) doi: 10.1186/s12884-015-0714-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sapir A., Reichman O., Gal M., Samueloff A. Placenta increta originating from placental remnants of a first trimester vanished twin. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014;176:201. doi: 10.1016/j.ejogrb.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Aguilera M., Rauk P., Ghebre R., Ramin K. Complete hydatidiform mole presenting as a placenta accreta in a twin pregnancy with a coexisting normal fetus: case report. Case Rep. Obstet. Gynecol. 2012;2012 doi: 10.1155/2012/405085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.González E.G., Gaviño F.G., Origel A.V., Díaz H.D., Fernández M.A., Lamadrid M.M. vol. 77. Ginecologia y obstetricia de Mexico; 2009. Twin Pregnancy with Complete Mole and Coexisting Fetus after In Vitro Fertilization and Embryo Transfer Complicated with Placenta Previa Accreta. A Case Report; pp. 151–155. [PubMed] [Google Scholar]
- 12.Patsouras K., Panagopoulos P., Sioulas V., Salamalekis G., Kassanos D. Uterine rupture at 17 weeks of a twin pregnancy complicated with placenta percreta. J. Obstet. Gynaecol. 2010;30:60–61. doi: 10.3109/01443610903315660. [DOI] [PubMed] [Google Scholar]
- 13.Cho F.N., Liu C.B., Li J.Y., Chen S.N. Complete resolution of diffuse placenta increta in a primigravida with twin pregnancy: sonographic monitoring. J. Clin. Ultrasound. 2011;201(39):363–366. doi: 10.1002/jcu.20768. [DOI] [PubMed] [Google Scholar]
- 14.Kilcoyne A., Shenoy-Bhangle A.S., Roberts D.J., Sisodia R.C., Gervais D.A., Lee S.I. MRI of placenta accreta, placenta increta, and placenta percreta: pearls and pitfalls. Am. J. Roentgenol. 2017:214–221. doi: 10.2214/AJR.16.16281. [DOI] [PubMed] [Google Scholar]
- 15.Dubois J., Garel L., Grignon A., Lemay M., Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am. J. Obstet. Gynecol. 1997;176:723–726. doi: 10.1016/s0002-9378(97)70582-9. [DOI] [PubMed] [Google Scholar]
- 16.Shrivastava V., Nageotte M., Major C., Haydon M., Wing D. Case-control comparison of cesarean hysterectomy with and without prophylactic placement of intravascular balloon catheters for placenta accreta. Am. J. Obstet. Gynecol. 2007;197:402-e1. doi: 10.1016/j.ajog.2007.08.001. [DOI] [PubMed] [Google Scholar]