We read with interest the recent paper by Siau et al.1 reporting results from a multicentre trainee-led gastrointestinal bleed (AUGIB) audit in the UK. Through our newly formed Gastroenterology Trainee Research and Improvement Network North West (GasTRIN NoW), we would like to share our results of AUGIB management within North West England.
A prospective multicentre AUGIB audit was undertaken across 11 hospitals in North West England between 30 October 2017 and 26 November 2017. All adult patients admitted with suspected AUGIB who underwent gastroscopy were included. The standards assessed were as defined by Joint Advisory Group on GI Endoscopy (JAG) and reported in Siau et al.1
A total of 133 patients were included, of which 84% (n = 112) were referred from Accident and Emergency while the remainder were from primary care. Median age was 65 years (range: 18–96), of which 65% (n = 87) were male. Of the patients, 51% (n = 68) were admitted during weekdays between 07:00 and 19:00. At admission, only 47% (n = 62) had a Glasgow-Blatchford bleeding score (GBS) documented.
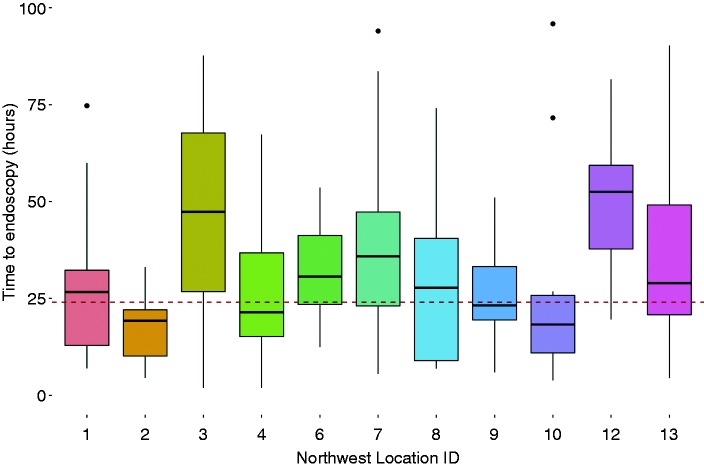
Of the patients, 40% (n = 54) underwent an Oesophagogastroduodenoscopy (OGD) within 24 hours of admission (median: 28 hours, interquartile range (IQR): 18–50). Time to endoscopy did not differ significantly across centres (Kruskal p = 0.46; Figure 1). Delayed endoscopy occurred in 60% (n = 79) and this did not vary across centres (χ2 p = 0.08). Outcomes of early and delayed endoscopy are summarised in Table 1.
Figure 1.
Time to endoscopy (hours) for each participating centre. Red dotted line denotes 24 hours.
ID: identifier.
Table 1.
Outcomes of early (<24 hours) and delayed (>24 hours) endoscopy groups.
| Time to endoscopy |
|||
|---|---|---|---|
| Variable | <24 hours | >24 hours | p-value |
| Rebleed within 8 days of endoscopy | 4 | 0 | 0.02 |
| Death within 30 days of endoscopy | 2 | 5 | 0.70 |
| Length of stay (days) | 5 (3–8) | 4 (3–7) | 0.43 |
Patients requiring endoscopic therapy had a significantly higher GBS score than those not requiring therapy (median GBS = 11, IQR: 8–13 versus 3, IQR: 2–4; p = 0.009). In total, 64% of patients who required therapy were endoscoped within 24 hours (n = 16). OGD was performed earlier in those who required intervention for bleeding compared with those who did not (median 19 hours, IQR 11–27 versus 32 hours, IQR: 21–54; p = 0.007). Length of stay of these patients was longer compared to those not requiring therapy (median 6 days, IQR: 5–7 versus 4 days, IQR: 2–7; p = 0.04). There were seven deaths at 30-day follow-up, but only one was directly attributable to AUGIB.
Our data report similar findings to Siau et al., that most centres failed to meet the JAG standards. Within our cohort, patients who required therapy for AUGIB had early endoscopy compared to those that did not require therapy; however, 37% of these cases did not meet the JAG guidelines for timing to endoscopy. These data provide impetus to improve the standards of AUGIB care across regions in England.
Acknowledgements
GasTRIN NoW Collaborative Network Contributors:
Site leads:
Rahul Kalla, Royal Preston Hospital, UK; Wadiamu Gashau, Royal Preston Hospital, UK; Simon Borg-Bartolo, Manchester Royal Infirmary, UK; Liam Morris, Royal Bolton Hospital, UK; Kirsty Nixon, Salford Royal NHS Foundation Trust, UK; Katherine White, Salford Royal NHS Foundation Trust, UK; Beth Miller, Royal Bolton Hospital, UK; Elizabeth Ratcliffe, Royal Lancaster Infirmary, UK; Francis Egbuonu, Furness General Hospital, UK; Johannah Cook, Royal Albert Edward Infirmary, Wigan, UK; Benjamin Crooks, Wythenshawe Hospital, UK; Scott Healey, North Manchester General Hospital, UK; Joseph Fiske, Royal Oldham Hospital, UK; Eleanor Liu, Blackpool Victoria Hospital, UK.
Project investigators/contributors:
Joe Ingoe, Salford Royal NHS Foundation Trust, UK; Adam Hamdi, Royal Preston Hospital, UK; Abdulmaleek Sado, Royal Preston Hospital, UK; Katherine Martin, Manchester Royal Infirmary, UK; Michael Finegan, Manchester Royal Infirmary, UK; Mohamed Shibeika, Royal Lancaster Infirmary, UK; Rizwan Diyar, Royal Albert Edward Infirmary, Wigan, UK; Nasar Aslam, Blackpool Victoria Hospital, UK.
Authorship statement
The study was jointly performed by the GasTRIN NoW trainee network. All authors contributed to the study and review of the manuscript. The GasTRIN NoW trainee network would like to thank the many consultants around the region who support the network and this project.
Declaration of conflicting interests
There are no conflicts of interest to declare.
Ethics approval
Formal ethical approval was not required as per departmental policy and Health Research Authority guidance. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a prior approval by the institution's review board.
Funding
There are no funders to report in this study.
Informed Consent
Patient consent was not required as per department policy.
Reference
- 1.Siau K, Hodson J, Ingram R, et al. Time to endoscopy for acute upper gastrointestinal bleeding: Results from a prospective multicentre trainee-led audit. United Eur Gastroenterol J. Epub ahead of print 28 October 2018. DOI: 10.1177/2050640618811491. [DOI] [PMC free article] [PubMed] [Google Scholar]