Abstract
BACKGROUND:
Reports of thunderstorm asthma in the Middle East are few. This study is the first to report on cases of near-fatal and fatal thunderstorm asthma in Kuwait on December 1, 2016.
METHODS:
We conducted a chart review and interview with adult patients admitted to Mubarak Al-Kabir Hospital with near-fatal asthma, defined as an exacerbation requiring intubation and mechanical ventilation or hypercapnia with a PaCO2≥6 kPa. Information, including patient age, gender, occupation, asthma history, medication usage, and clinical outcome, was collected. For fatal asthma cases, patients' data were collected from the Forensic Department at the Kuwait Ministry of Interior.
RESULTS:
A total of 17 patients were admitted with near-fatal asthma. Fifteen patients (93.8%) had a prior history of asthma, with an average duration of 9 years. Five patients (33.3%) reported receiving a corticosteroid inhaler from their physician. Fifteen patients (93.8%) reported relying on a short-acting β2-agonist alone to manage their asthma. Eleven patients (68.8%) reported being outdoors during the storm. Eleven patients were diagnosed with fatal asthma.
CONCLUSION:
The study is the first to report on a thunderstorm-associated asthma epidemic in Kuwait and emphasizes the potential dangers associated with this entity.
Keywords: Fatality, Kuwait, near fatality, thunderstorm asthma
Thunderstorm asthma is a term which refers to acute exacerbation of asthma symptoms during or shortly following a thunderstorm. Outbreaks of storm-associated asthma epidemics have been reported worldwide, including Australia,[1] Europe,[2,3] and the United States.[4] Most epidemics are reported to occur during the pollen season. The interaction of the wind and relative humidity with increased outdoor aeroallergens, particularly pollen and spores, are believed to play a pivotal role in triggering these acute asthma epidemics.[5] It is theorized that under the humid conditions of the storm, pollen particles near the ground rupture due to osmotic shock, creating smaller (0.5–2.5 μm) aerosolized cytoplasmic-derived particles which easily become airborne.[6] It is these paucimicronic pollen-derived particles which enter the lower airways of susceptible patients shortly after the commencement of the storm, triggering an asthma exacerbation. Evidence suggests that this phenomenon is not restricted to certain geographical areas, with reports of similar events in the Middle East, such as Saudi Arabia and Iran.[7,8] Kuwait has experienced such events with variable severities over the past 10 years, but none has been published as a full report.[9]
Kuwait is a small country with an approximate area of 17,820 km2. It is located in the north-eastern edge of the Arabian Peninsula overlooking the Arabian Gulf. Its estimated population is just over 4 million, with nonnationals accounting for almost 70% of the total.[10] About 15% of the adult population is estimated to suffer from asthma.[11] Kuwait's pollen season typically starts in September and ends in early January. The most important outdoor allergens are salsola pollen belonging to the Chenopodiaceae and Amaranthaceae families (weeds) as well as Alternaria fungal species.[12,13] Kuwaiti winters are generally mild with an average rainfall of 107.3 mm per year.[14]
On December 1, 2016, Kuwait experienced an epidemic of acute asthma exacerbations following a countrywide heavy thunderstorm which lasted from 15:00 to 15:30. Multiple hospitals, emergency departments (EDs) and walk-in primary care clinic facilities reported a noticeable increase in patients presenting with symptoms of asthma exacerbations, which coincided with the onset of the thunderstorm. In some facilities, the numbers swelled to such levels that police presence had to be summoned to exert crowd control. According to the Ministry of Health official announcement, 844 patients attended the different EDs throughout the country due to asthma exacerbations,[15,16] 45 of whom required hospital admission and 26 required admission to the intensive care unit (ICU). However, we believe that these figures underestimate the magnitude of the epidemic as they do not account for patients presenting to walk in clinics. All local and some international news outlets reported on this event.
Mubarak Al-Kabir Hospital is a major hospital covering the Hawally governorate area and its associated suburbs. During the 24 h following the thunderstorm, the hospital admitted 17 cases of near-fatal asthma.
The Kuwait Forensic Medicine Department, a subdivision of the Kuwait Ministry of Interior, reported it had received a total of 11 cases of patients suspected to have died due to severe thunderstorm-associated asthma: three patients were found dead at home by a relative or friend and the remaining were declared dead on arrival to various hospitals.
This paper is the first published report on near-fatal and fatal thunderstorm-associated asthma in Kuwait. The aim of this paper is to highlight the occurrence of thunderstorm-associated asthma in Kuwait and to emphasize the importance of recognizing this entity as a small but significant cause of asthma-related morbidity and mortality.
Methods
Study design
The authors conducted a chart review, and personal interview with each patient admitted to Mubarak Al-Kabir Hospital with near-fatal asthma. Near fatal asthma was defined as an asthma exacerbation event requiring intubation and mechanical ventilation due to impending respiratory failure or hypercapnia with a PaCO2≥6 kPa. Interviews were conducted in the hospital after the patient had been extubated and stabilized. For fatal asthma cases, patients' data were collected from the registry available at the Forensic Department at the Kuwait Ministry of Interior. Due to the large numbers of cases referred to the forensic department, the relatives or friends of all the deceased were contacted to verify any history of prior asthma and the circumstances of death.
Study population
The study population included patients who were present in Kuwait during the thunderstorm and admitted to Mubarak Al-Kabir Hospital with a primary diagnosis of asthma exacerbation from 00:00 on December 1, 2016 to 24:00 on December 1, 2016. Patients admitted to hospital for asthma exacerbation during the above stated time frame, aged 12 years or older, with an arterial blood gas PCO2≥6 kPa or evidence of respiratory failure requiring intubation and mechanical ventilation was included in the study. Patients <12 years old and those with a diagnosis of asthma in addition to another respiratory disease (e.g., chronic obstructive pulmonary disease, interstitial lung disease, etc.) were excluded from the study. For cases of fatal asthma, all patients ≥12 years old whose official documented the primary cause of death was asthma and whose time of death was estimated to have occurred during the time frame as stated above were included. All these patients were first evaluated by a coroner at the Ministry of Interior in the Department of Forensic Medicine.
Data collection
For patients with near-fatal asthma, the authors constructed a data collection form in English to obtain pertinent clinical details from the patient. The authors conducted a personal interview with the patient after his or her extubation and recovery then conducted a chart review of each patient as well. Written, informed consent was obtained. The information obtained included patient sociodemographic data, such as age, gender, nationality, and smoking status. Information on the subject's asthma was also obtained, including his or her history of asthma and allergic rhinitis, the location of regular asthma care and last scheduled visit as well as the use of asthma medications and compliance. Finally, patient's history of presenting complaint was collected. This included patient location during the thunderstorm, whether the patient was indoors or outdoors, time to onset of asthma symptoms after the storm, time of presentation to hospital, hospital course, and clinical outcome. The personal interview was conducted in English or Arabic. For patients unable to communicate in English, an interpreter was made available to assist.
For cases of fatal asthma, the authors collected the data of patients whose certified primary cause of death was asthma exacerbation. Official approval from the Ministry of Interior was obtained before data collection. The information obtained included patient age, gender, nationality, time and place of death, and prior history of asthma. None of the deceased patients underwent an autopsy.
This study was approved by the Kuwait Ministry of Health Ethics Committee (2017/704).
Statistical analysis
The data management, analysis, and graphical presentation were carried out using the computer software “Statistical Package for Social Sciences, SPSS version 25.0” (IBM Corp, Armonk, NY, USA). The descriptive statistics has been presented as a number, percentage, mean, and standard deviation with range. Student's t-test was used to compare the mean values in two different groups.
Results
Characteristics of patients with near-fatal and fatal asthma
A total of 17 patients presented to Mubarak-Al-Kabir hospital with near-fatal asthma. Fifteen of those patients presented to the hospital on December 1. The average patient age at presentation was 39 years (15–61 years). There was a slight preponderance of male patients (10 males to 7 females). Mean age of females was found to be slightly higher compared to males. The patients' sociodemographic characteristics are shown in Table 1.
Table 1.
Sociodemographic characteristics of patients admitted for near-fatal thunderstorm asthma in Mubarak Al-Kabir Hospital, Kuwait
| Demographics | n (%) |
|---|---|
| Gender | |
| Male | 10/17 (58.8) |
| Mean age±SD | 37.6±11.7 |
| Range | 15-57 |
| Female | 7/17 (41.2) |
| Mean age±SD | 41.7±9.6 |
| Range | 31-61 |
| Occupation | |
| Indoor worker | 10/16 (62.5) |
| Outdoor worker | 3/16 (18.8) |
| Domestic worker | 2/16 (12.5) |
| Other | 1/16 (6.2) |
| Smoking status | |
| Nonsmoker | 14/16 (87.5) |
| Ex-smoker | 2/16 (12.5) |
SD=Standard deviation
A total of 11 patients were diagnosed with fatal asthma by the Department of Forensic Medicine. All patients were males, with a mean age of 45 years. All the cases had died before arriving at the hospitals. The patients' sociodemographic characteristics are shown in Table 2.
Table 2.
Sociodemographic characteristics of patients admitted with fatal thunderstorm asthma in Mubarak Al-Kabir Hospital, Kuwait
| Demographics | n (%) |
|---|---|
| Age group (years) | |
| ≤40, n (%) | 5/11 (45.5) |
| >40, n (%) | 6/11 (54.5) |
| Overall mean age, mean age±SD (range) | 45.3±9.9 (33-59) |
| Gender, n (%) | |
| All males | 11/11 (100.0) |
| Governorate, n (%) | |
| Capital | 6/11 (54.5) |
| Hawally | 3/11 (27.3) |
| Farwaniya | 1/11 (9.1) |
| Ahmadi | 1/11 (9.1) |
| Place of death, n (%) | |
| Home | 3/11 (27.3) |
| Hospital (on arrival) | 8/11 (72.7) |
SD=Standard deviation
Previous history of asthma, use of medication and management
Fifteen (93.8%) of the patients admitted with near-fatal asthma had a prior history of asthma, with an average duration of 9 years. The characteristics of their asthma are displayed in Table 3. Seven patients (43.8%) gave an additional prior history of allergic rhinitis. Five patients (33.3%) reported having been prescribed a corticosteroid inhaler by a physician, but only one patient reported taking this inhaler in the week before the thunderstorm. Fifteen patients (93.8%) reported relying on an inhaled short-acting β2-agonist alone to manage their asthma symptoms in the week before the thunderstorm. Seven (43.7%) patients reported an unscheduled visit to either the emergency room or their physician within the previous month due to asthma symptoms.
Table 3.
Clinical features of Asthma patients admitted for near fatal asthma to Mubarak Al-Kabir Hospital, Kuwait
| Clinical features | n (%) |
|---|---|
| Prior history of asthma | |
| Yes | 15/16 (93.8) |
| No | 1/16 (6.2) |
| Duration (years) | |
| ≤5 | 6/15 (40.0) |
| >5 | 9/15 (60.0) |
| Regular medical care location prior to the attack | |
| Hospital | 1/15 (6.7) |
| Primary care | 3/15 (20.0) |
| Walk-in clinic | 11/15 (73.3) |
| History of allergic rhinitis | |
| Yes | 7/16 (43.8) |
| No | 9/16 (56.2) |
| Medication | |
| Short-acting β2-agonists | |
| Yes | 15/16 (93.8) |
| No | 1/16 (6.2) |
| Inhaled steroid | |
| Yes | 5/15 (33.3) |
| No | 10/15 (66.7) |
For patients with fatal asthma, all 11 patients had a prior history of asthma. No data were available on the duration of symptoms or medical care before the fatal attack.
Location, symptom progression of patients at the time of the thunderstorm
For patients with near-fatal asthma, eleven (68.8%) reported were outdoors and five (31.2%) were indoors during the storm [Table 4]. The location of one patient during the storm could not be accounted for as he was admitted with brain hypoxia due to his asthma attack. Six (42.9%) patients reported asthma symptoms lasting <24 h from the onset of the storm. The remaining patients reported asthma symptoms lasting >24 h from the onset of the storm, ranging from 2 to 30 days, with symptoms becoming significantly worse following the storm. Nine patients (56.3%) reported a prior history of worsening asthma symptoms with rainfall.
Table 4.
Thunderstorm related characteristics of patients admitted for near fatal asthma to Mubarak Al-Kabir Hospital, Kuwait
| Characteristic | n (%) |
|---|---|
| History of prior thunderstorm-associated asthma exacerbations, n (%) | |
| Yes | 9/16 (56.3) |
| No | 7/16 (43.7) |
| Duration of asthma (years), mean±SD (range) | 9.00±7.43 (1-30) |
| Patient location during storm, n (%) | |
| Outdoors | 11/16 (68.8) |
| Indoors | 5/16 (31.2) |
| Symptom duration after onset of storm (h), n (%) | |
| <24 | 6/14 (42.9) |
| >24 | 8/14 (57.1) |
SD=Standard deviation
Hospital course and patient outcome
The peak arrival time to the hospital emergency room for patients with near-fatal asthma occurred between 16:00 and 18:00 on December 1 [Figure 1]. Eleven (64.7%) patients were admitted to the ICU, ten of whom required intubation and mechanical ventilation due to impending respiratory failure. Nine of these patients were extubated within 48 h. Sixteen (94%) patients were discharged home within 1 week of asthma symptom exacerbation. All the patients who died during the event either arrived dead to ED or were found dead at home within a very short period of the storm's onset [Figure 2], as verified by the time of the announcement of death on the death certificates.
Figure 1.
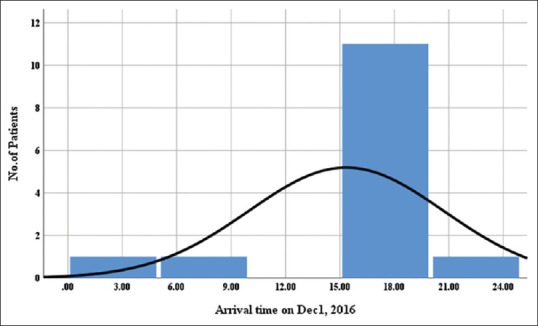
Number of patients presented to Mubarak Al-Kabir Hospital on December 01, 2016 for near fatal asthma. The thunderstorm occurred on December 01, 2016 at 13:00 h
Figure 2.
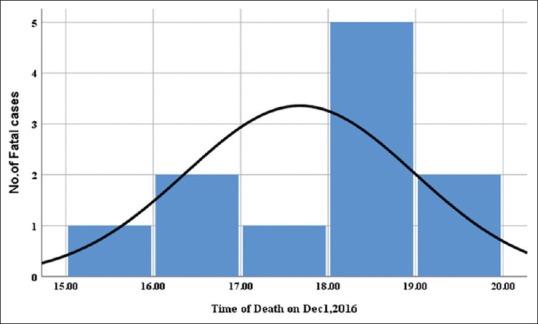
Number of patients with fatal thunderstorm asthma on December 01, 2016. The thunderstorm occurred on December 01, 2016 at 13:00 h
Discussion
The study is the first published report on thunderstorm-associated asthma in Kuwait and highlights the importance of this asthma-related entity within the Middle East region. The study shows more patients who were outdoors during the thunderstorm developed an acute asthma attack compared to those who were indoors. Increased exposure of susceptible patients to grass pollen and fungal spores in the atmosphere during this weather disturbance may explain this finding. One study conducted in Australia showed that grass pollen allergy served as a significant contributing factor to the development of severe thunderstorm-associated asthma exacerbation and that patients outdoors or patients indoors with open windows were twice at risk of developing an exacerbation compared to asthmatic patients who stayed indoors during the storm with closed windows.[1]
All of the patients in our study denied being current smokers at the time of the thunderstorm. The high incidence of thunderstorm-associated asthma exacerbations among nonsmokers has been reported in other studies.[1,8] The study sample, however, is too small to draw any conclusions on this finding.
The majority of patients in the present study who were admitted with near-fatal asthma had a prior history of asthma for an average of 9 years, but 43.7% had no previous history of thunderstorm-associated asthma. Our study also showed that the majority of patients were not attending a specialized asthma clinic and not using regular inhaled corticosteroids during the thunderstorm. In addition, most of these patients had not attended a scheduled outpatient appointment with their physician in years despite their diagnosis of asthma. Their subsequent deterioration may relate to inadequate use of a maintenance inhaler during Kuwait's pollen season and poor control of their underlying asthma which is further exacerbated by the weather disturbance. One Kuwaiti survey revealed that patients attending specialized asthma clinics scored better in terms of symptom control, medication compliance, numbers of exacerbations, and overall knowledge of their condition when compared to patients attending other medical facilities.[17] Another study showed that primary care centers in Kuwait lacked essential medications for the treatment of asthma and 33% of centers surveyed stocked only low-dose corticosteroid inhalers.[18] Patient noncompliance, poor communication, difficulty accessing medical care, and difficulty obtaining the inhaler may be factors in placing the patient at risk of an asthma attack during a thunderstorm. It is possible, however, that some of our patient population suffered from intermittent asthma and did not require regular inhaled corticosteroids.
The relationship between allergic rhinitis and thunderstorm asthma in our study is less clear. Less than half of the patients in our study reported a history of allergic rhinitis. However, our study sample is too small to establish an association between these two entities.
Our study demonstrated that thunderstorm-associated asthma exacerbation typically occurs rapidly during or shortly following the storm, with the majority of both fatal and near-fatal cases occurring during the first 3 h of weather disturbance onset. Thunderstorm-associated asthma cases may have a benign course, with the majority of cases requiring treatment in the emergency room only and <1% requiring ICU admission.[7] For those patients in our study requiring intubation, the majority required a maximum of 2 days of mechanical ventilation before successful extubation. About 94% of those admitted were discharged within 1 week of hospital admission. The study revealed the percent proportion of deaths due to asthma during thunderstorm on December 1, 2016, was 1.3%. The association between asthma and mortality is well-documented in the literature[19,20,21] and our study emphasizes that the sequela of thunderstorm-associated asthma in vulnerable patients should not be underestimated. All patients with fatal asthma succumbed within hours of storm onset. This finding indicates the potential of thunderstorm asthma to cause a rapidly fatal outcome in susceptible patients.
While our study is the first to report on thunderstorm-associated asthma in Kuwait, it is limited by its small sample size and restriction to one hospital locale. In addition, due to the retrospective nature of chart review studies, certain information such as the classification of the patients' asthma according to the Global Initiative for Asthma guidelines could not be obtained. Similarly, information from the Forensic Department of the Ministry of Interior was limited, restricting what conclusions could be drawn from this data.
Conclusion
Our study serves to emphasize the importance of thunderstorm-associated asthma as an important disease entity in Kuwait despite its underreporting. While the majority of cases are managed successfully in the emergency room, patients who were outdoors during the weather disturbance and those noncompliant with regular inhaled corticosteroid medication during Kuwait's pollen season appeared more at risk of near-fatal asthma attacks requiring hospital admission and intubation. These findings, in turn, show the importance of good asthma control in susceptible patients during Kuwait's pollen season and educating these patients on minimizing outdoor activities during thunderstorms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Girgis ST, Marks GB, Downs SH, Kolbe A, Car GN, Paton R, et al. Thunderstorm-associated asthma in an inland town in South-Eastern Australia. Who is at risk? Eur Respir J. 2000;16:3–8. doi: 10.1034/j.1399-3003.2000.16a02.x. [DOI] [PubMed] [Google Scholar]
- 2.Pulimood TB, Corden JM, Bryden C, Sharples L, Nasser SM. Epidemic asthma and the role of the fungal mold Alternaria alternata. J Allergy Clin Immunol. 2007;120:610–7. doi: 10.1016/j.jaci.2007.04.045. [DOI] [PubMed] [Google Scholar]
- 3.Losappio L, Heffler E, Contento F, Cannito C, Rolla G. Thunderstorm-related asthma epidemic owing to olea Europaea pollen sensitization. Allergy. 2011;66:1510–1. doi: 10.1111/j.1398-9995.2011.02699.x. [DOI] [PubMed] [Google Scholar]
- 4.Grundstein A, Sarnat SE, Klein M, Shepherd M, Naeher L, Mote T, et al. Thunderstorm associated asthma in Atlanta, Georgia. Thorax. 2008;63:659–60. doi: 10.1136/thx.2007.092882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor PE, Jonsson H. Calhoun. The NPS institutional archive thunderstorm asthma. Curr Allergy Asthma Rep. 2004;4:409–13. doi: 10.1007/s11882-004-0092-3. [DOI] [PubMed] [Google Scholar]
- 6.D'Amato G, Liccardi G, Frenguelli G. Thunderstorm-asthma and pollen allergy. Allergy. 2007;62:11–6. doi: 10.1111/j.1398-9995.2006.01271.x. [DOI] [PubMed] [Google Scholar]
- 7.Al-Rubaish AM. Thunderstorm-associated bronchial asthma: A forgotten but very present epidemic. J Family Community Med. 2007;14:47–51. [PMC free article] [PubMed] [Google Scholar]
- 8.Forouzan A, Masoumi K, Haddadzadeh Shoushtari M, Idani E, Tirandaz F, Feli M, et al. An overview of thunderstorm-associated asthma outbreak in Southwest of Iran. J Environ Public Health. 2014;2014:504017. doi: 10.1155/2014/504017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Behbehani N, Almane F, Alghanem F, Ramadan E. Thunderstorm Associated Outbreak of Bronchial Asthma in Kuwait. Kuwait: Poster Presented at: The 9th Annual Health Sciences Poster Day; 19-21 April, 2004. [Google Scholar]
- 10.Kuwait Population (Demographics, Maps, Graphs) 2017. [Last accessed on 2018 Aug 23]. Available from: http://www.worldpopulationreview.com/countries/kuwait-population/
- 11.Khadadah M. The cost of asthma in Kuwait. Med Princ Pract. 2013;22:87–91. doi: 10.1159/000341154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Dowaisan A, Fakim N, Khan MR, Arifhodzic N, Panicker R, Hanoon A, et al. Salsola pollen as a predominant cause of respiratory allergies in Kuwait. Ann Allergy Asthma Immunol. 2004;92:262–7. doi: 10.1016/S1081-1206(10)61558-X. [DOI] [PubMed] [Google Scholar]
- 13.Qasem JA, Nasrallah H, Al-Khalaf BN, Al-Sharifi F, Al-Sherayfee A, Almathkouri SA, et al. Meteorological factors, aeroallergens and asthma-related visits in Kuwait: A 12-month retrospective study. Ann Saudi Med. 2008;28:435–41. doi: 10.5144/0256-4947.2008.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rainfall in Kuwait City, Kuwait Average Precipitation and Wet Days. [Last accessed on 2018 Aug 23]. Available from: http://www.kuwait.climatemps.com/precipitation.php .
- 15.Five Die in 2 Days Due to Asthma Attacks in Kuwait – Kuwait Times | Kuwait Times. [Last accessed on 2018 Aug 23]. Available from: http://www.news.kuwaittimes.net/website/five-die-2-days-due-asthmaattacks-kuwait/
- 16.Kuwait: Five Expats Die of Asthma as Rain Lashes Kuwait. [Last accessed on 2018 Aug 23]. Available from: http://www.gdnonline.com/Details/147475/Five-expats-die-of-asthma-as-rain-lashes-Kuwait .
- 17.Al-Kanderi BM, Al-Muhaileej FA, Al-Khalaf T. Evaluation of asthma clinics in primary care in Kuwait. Eur J Gen Med. 2006;3:159–66. [Google Scholar]
- 18.Behbehani NA, Al-Yousifi K. Lack of essential asthma medications in primary care centres in Kuwait. Int J Tuberc Lung Dis. 2003;7:422–5. [PubMed] [Google Scholar]
- 19.Savage JH, Matsui EC, McCormack M, Litonjua AA, Wood RA, Keet CA, et al. The association between asthma and allergic disease and mortality: A 30-year follow-up study. J Allergy Clin Immunol. 2014;133:1484–7. 1487.e1–5. doi: 10.1016/j.jaci.2014.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005-2009. Natl Health Stat Report. 2011;32:1–14. [PubMed] [Google Scholar]
- 21.Fuhrman C, Jougla E, Uhry Z, Delmas MC. Deaths with asthma in France, 2000-2005: A multiple-cause analysis. J Asthma. 2009;46:402–6. doi: 10.1080/02770900902795553. [DOI] [PubMed] [Google Scholar]


