Abstract
Introduction:
Simultaneous subcutaneous emphysema, spontaneous pneumothorax, and pneumomediastinum are complications rarely observed synchronously during an acute exacerbation of bronchial asthma. Although spontaneous pneumothorax has already been reported in asthma patients in the literature, its concurrence with subcutaneous emphysema and pneumomediastinum is extremely rare except for iatrogenic conditions.
Case Study:
We describe a patient who presented to the emergency room with progressive dyspnea and chest pain. Three days before, she consulted her general physician with a history of violent dry cough and wheezing. An acute asthma exacerbation was diagnosed, and an inhaled short-acting beta 2 agonist and oral prednisone were prescribed. The patient developed simultaneous subcutaneous emphysema, spontaneous pneumothorax, and pneumomediastinum, a rare complication of an asthma attack.
Conclusions:
Our aim is to emphasize that occult pneumothoraces should be considered in a patient presenting with an acute asthma attack failing to respond to conventional medical therapy.
Keywords: Asthma, pneumomediastinum, spontaneous pneumothorax, subcutaneous emphysema
Introduction
Subcutaneous emphysema, pneumothorax, and pneumomediastinum are usually a consequence of thoracic and cervical blunt trauma, esophageal perforation (Boerhaave syndrome), or are iatrogenic in nature. Causes include assisted positive pressure ventilation, interstitial lung disease, and perforation of a hollow abdominal viscus with subsequent dissection of air into the mediastinum using the diaphragmatic hiatus and dental procedures as well as several diseases. It can also spontaneously occur because of cocaine inhalation, vomiting and forceful straining, such as in childbirth or strenuous exercise.[1,2,3] However, simultaneous subcutaneous emphysema, pneumothorax, and pneumomediastinum are complications rarely observed synchronously during an acute asthma attack. This case illustrates an unusual sudden complication of an asthmatic attack.
Case Study
A 67-year-old woman, with a past medical history of bronchial asthma, was admitted to our emergency department with pleuritic chest pain, dysphagia, and odynophagia, followed by progressive swelling of her upper chest, neck, and face, which began 2 h prior to admission. She previously had consulted her general physician with a history of malaise, violent dry cough, and wheezing for 3 days, for which she had received treatment with inhaled albuterol and oral prednisone. She had no current history of trauma or foreign body aspiration. She denied any lip or tongue swelling, difficulties swallowing saliva, or retching, prior to presentation. She did not smoke, and her family history was not remarkable.
On physical examination, she was not in acute distress. Vital signs revealed a temperature of 99.3°F (37.4°C), blood pressure of 115/67 mmHg, the pulse was 92 beats per minute, regular, respirations were 21 breaths per minute, and her arterial blood oxygen saturation was 91% on room air. Examination of the neck and chest revealed symmetrical swelling with crepitations on palpation consistent with subcutaneous emphysema. In the auscultation of the lungs, reduced respiratory sounds were observed in both hemithoraces with expiratory and inspiratory wheeze. The remainder of the physical examination was unremarkable. The patient's history and physical findings were consistent with subcutaneous emphysema. Treatment with oxygen therapy was started.
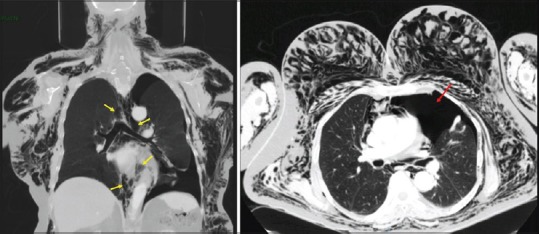
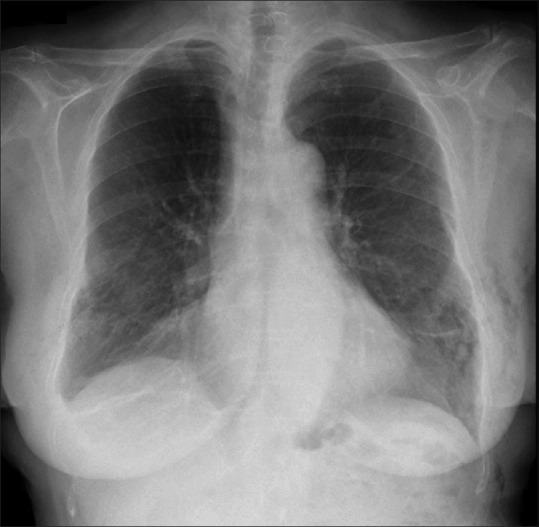
Laboratory tests revealed 18800/mm3 leukocytes, a hematocrit of 39%, and a platelet count of 207000/mm3. C-reactive protein was 3 mg/l. Liver and kidney function tests, and serum electrolytes were all within normal limits. The arterial blood gas analysis (breathing room air) showed pH 7.49, hypoxemia (PaO2 58 mmHg), hypocapnia (PaCO2 31 mmHg), and HCO3 28 mmol/l. A 12-lead electrocardiogram showed a sinus rhythm with 95 beats per minute. On chest and neck radiograph, we observed a subcutaneous emphysema [Figure 1]. She was subsequently put on antibiotics, analgesia, and low molecular weight heparin for prevention of venous thromboembolism. The patient was admitted to our thoracic surgery department. The diagnosis of pneumothorax and pneumomediastinum were established according to the chest computed tomography scan findings. Computerized tomography scan of the neck and chest revealed moderate sized pneumothorax on the left side, extensive pneumomediastinum, and soft tissue emphysema in the neck and chest [Figure 2].
Figure 1.

Chest X-ray on the day of admission showing vast subcutaneous emphysema. Pneumothorax and pneumomediastinum are obscured by the extensive subcutaneous air.
Figure 2.
Chest computed tomography scans showing subcutaneous emphysema, pneumomediastinum (yellow arrows), and pneumothorax on the left side (red arrow)
The patient evolved favorably after oxygen therapy, antibiotic prophylaxis, and conventional medical treatment. Seven days later, subcutaneous emphysema had almost resolved spontaneously on the follow-up chest X-ray [Figure 3].
Figure 3.
Chest X-ray showing significant resolution of subcutaneous emphysema after 7 days
Discussion
This case illustrates an unusual sudden complication of an asthmatic attack. In our patient, subcutaneous emphysema, pneumothorax, and pneumomediastinum were likely caused by what we believed to be a complication after a coughing attack. Simultaneous subcutaneous emphysema, pneumothorax, and pneumomediastinum are complications rarely observed synchronously during an acute asthma attack. Although spontaneous pneumothorax has already been reported in asthma patients in the literature, its concurrence with subcutaneous emphysema and pneumomediastinum is extremely rare except for iatrogenic conditions, with only one case reported.[4]
The relationship between asthma and pneumothorax is not widely known. Making a differential diagnosis between pneumothorax and asthma is usually hard. Both asthma and tension pneumothorax are manifested by tachycardia, tachypnea, respiratory distress, desaturation and decreased air entry, causing difficulty to perform a differential diagnosis. Therefore, the diagnosis of pneumothorax in asthmatic patients may often be delayed or missed. Consequently, it is important to carefully monitor these patients. There is a 1.2% probability of pneumothorax in an asthma exacerbation.[5] Although pneumomediastinum prognosis is usually excellent with conservative treatment, its concurrence with complications such as pneumothorax may prove fatal during a severe asthma attack. In asthma exacerbations, pneumothorax and pneumomediastinum develop because the obstruction in the minor airways leads to air-trapping and barotrauma of distal airways, and the subsequent alveolar rupture. The abrupt increase in intra-alveolar pressure is a phenomenon known as the Macklin effect.[6] Negative pressure generated between the pulmonary interstitium and the mediastinum explains the occurrence of pneumomediastinum.[2] Subcutaneous emphysema is caused by increased intra-alveolar pressure with an extrapleural outflow of air.[2] The escape of air out of the alveolar spaces into the interstitial tissues around the pulmonary vasculature travels back toward the hilum, leading to pneumomediastinum, and this eventually tracts into the soft tissue of the neck, face, and chest wall. The clinical symptoms of pneumothorax and/or subcutaneous emphysema critically depend on the amount of extravasated gas and the extension of the affected areas. Most frequently, they include chest pain, dyspnea, dysphonia, and dysphagia.[2,3] Massive accumulation of air in the subcutaneous tissue, when associated to tension pneumothorax, may also compromise the life of the patient, causing acute respiratory distress syndrome.[7] Whereas subcutaneous emphysema causes swelling and crepitus over the involved anatomical site, pneumomediastinum characteristically gives a positive Hamman's sign (crunching or clicking noise heard synchronously with the heartbeat on auscultation, in left lateral decubitus position) when it is clinically significant.[8] It is not only found in Hamman's syndrome and spontaneous pneumomediastinum but also in patients with pneumothorax.
Conventional chest X-ray is the first investigation performed to assess pneumothorax because it is simple, rapid, and noninvasive; however, non-contrast computed tomography of the chest is more sensitive in detecting small amounts of gas.[9]
Subcutaneous emphysema, pneumothorax, and pneumomediastinum secondary to cough or Valsalva maneuver are considered benign conditions and amenable to conservative management.[10] Subcutaneous emphysema is usually a benign, self-limiting condition only requiring conservative management. Indications of observation as an initial management for pneumothorax remain controversial. Management depends on the clinical setting, etiology, and size of the pneumothorax, and whether it is open or closed, and simple or tension pneumothorax.[11] There are two main tasks in the treatment of pneumothorax: re-expansion of the lung and prevention of recurrence. Although it is difficult to obtain high quality consensus evidence because of differences in classification systems and management guidelines, conservative treatment with observation and supplemental oxygen has been considered as a more viable option for the treatment of pneumothorax in a healthy patient, with a success rate of 79%.[12] Observation alone as the primary therapeutic option should be determined by the size of pneumothorax, the presence of significant breathlessness, pre-existing lung disease, the presence of a persistent air leak, and whether the pneumothorax is primary or secondary13. British Thoracic Society guidelines 2010 for the management of spontaneous pneumothorax recommend observational one as the first-line treatment for patients without pre-existing lung disease, with small closed pneumothorax (<15–20%) with minimal symptoms and asymptomatic patients with large-size pneumothorax (>20%)11. Patients with small closed pneumothorax and who are not breathless can be managed with outpatient follow-up with appropriate analgesia and early review to ensure satisfactory resolution. If the patient is admitted for observation, supplemental high flow oxygen should be given. The rate of re-expansion of primary spontaneous pneumothorax is 2.2% of the volume of hemithorax per day, and complete re-expansion usually occurs in 7 weeks.[13] Most studies reveal low recurrence rates after conservative treatment.[14] However, observation is inappropriate in pneumothorax patients suffering an underlying lung disease with decreased pulmonary reserve. Secondary pneumothorax usually occurs in patients with overt underlying lung disease, most commonly chronic obstructive pulmonary disease. In these cases, the clinical symptoms associated are more severe in general than those associated with primary pneumothoraces and require more aggressive treatment. However, there is a significant rate of recurrence of secondary pneumothoraces, eventually with serious consequences. Therefore, observation is not the preferable option for secondary pneumothorax.[10] In conclusion, the clinical status is determined by the size of pneumothorax and cardiopulmonary reserve. Thoracic catheter drainage is recommended for a first large (rim of air in the thorax >2 cm according to the British Thoracic Society 2010 criteria) or symptomatic episode of primary spontaneous pneumothorax.
Conclusions
This report presents a patient with simultaneous subcutaneous emphysema, pneumothorax, and pneumomediastinum as an unusual complication of an asthma attack. Extra-pulmonary extravasations of air manifested as subcutaneous emphysema, pneumothorax, and pneumomediastinum can be a rare but very important complication of acute exacerbation of bronchial asthma. When there is no serious cause for subcutaneous emphysema, it usually resolves promptly. We suggest that occult pneumothoraces should be considered in the differential diagnosis of patients presenting with an acute asthma attack failing to respond to conventional medical therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
No financial support was received.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Banki F, Estrera AL, Harrison RG, Miller CC, 3rd, Leake SS, Mitchell KG, et al. Pneumomediastinum: etiology and a guide to diagnosis and treatment. Am J Surg. 2013;206(6):1001–1006. doi: 10.1016/j.amjsurg.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema: pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144(7):1447–1453. [PubMed] [Google Scholar]
- 3.Gray JM, Hanson GC. Mediastinal emphysema: aetiology, diagnosis, and treatment. Thorax. 1966;21(4):325–332. doi: 10.1136/thx.21.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karakaya Z, Demir S, Sagay SS, Karakaya O, Ozdinç S. Bilateral spontaneous pneumothorax, pneumomediastinum, and subcutaneous emphysema: rare and fatal complications of asthma. Case Rep Emerg Med. 2012:242579. doi: 10.1155/2012/242579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Porpodis K, Zarogoulidis P, Spyratos D, Domvri K, Kioumis I, Angelis N, et al. Pneumothorax and asthma. J Thorac Dis. 2014 Mar;6(Suppl 1):S152–61. doi: 10.3978/j.issn.2072-1439.2014.03.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Romero KJ, Trujillo MH. Spontaneous pneumomediastinum and subcutaneous emphysema in asthma exacerbation: The Macklin effect. Heart Lung. 2010 Sep-Oct;39(5):444–447. doi: 10.1016/j.hrtlng.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Woodside KJ, vanSonnenberg E, Chon KS, Loran DB, Tocino IM, Zwischenberger JB. Pneumothorax in patients with acute respiratory distress syndrome: pathophysiology, detection, and treatment. J Intensive Care Med. 2003;18:9–20. doi: 10.1177/0885066602239120. [DOI] [PubMed] [Google Scholar]
- 8.Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp. 1939;64:1–21. [Google Scholar]
- 9.Lim WH, Park CM, Yoon SH, Lim HJ, Hwang EJ, Lee JH, et al. Time-dependent analysis of incidence, risk factors and clinical significance of pneumothorax after percutaneous lung biopsy. Eur Radiol. 2018 Mar;28(3):1328–1337. doi: 10.1007/s00330-017-5058-7. [DOI] [PubMed] [Google Scholar]
- 10.MacDuff A, Arnold A, Harvey J. BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural. Disease Guideline 2010. Thorax. 2010 Aug;65(Suppl 2):ii18–31. doi: 10.1136/thx.2010.136986. [DOI] [PubMed] [Google Scholar]
- 11.Sharma A, Jindal P. Principles of diagnosis and management of traumatic pneumothorax. J Emerg Trauma Shock. 2008 Jan-Jun;1(1):34–41. doi: 10.4103/0974-2700.41789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Z, Huang H, Li Q, Zarogoulidis K, Kougioumtzi I, Dryllis G, et al. Pneumothorax: observation. J Thorac Dis. 2014 Oct;6(Suppl 4):S421–426. doi: 10.3978/j.issn.2072-1439.2014.08.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maskell NA. Pneumothorax management: time to improve the evidence base. Thorax. 2017 Dec;72(12):1065–1066. doi: 10.1136/thoraxjnl-2017-211007. [DOI] [PubMed] [Google Scholar]
- 14.Baumann MH, Noppen M. Pneumothorax. Respirology. 2004;9:157–164. doi: 10.1111/j.1440-1843.2004.00577.x. [DOI] [PubMed] [Google Scholar]


