Watch a video presentation of this article
Abbreviations
- AS
anastomotic stricture
- ERCP
endoscopic retrograde cholangiopancreatography
- HAT
hepatic artery thrombosis
- NAS
nonanastomotic stricture
The development of biliary complications after liver transplantation remains a common source of morbidity despite advances in surgical techniques. Incidence is estimated to be approximately 10% to 15% in deceased donor transplants and may be as high as 15% to 30% in living donor or split‐liver transplant recipients.1 Biliary complications may be characterized as early (within 30 days of transplant) or late. The majority of complications (up to 70%) occur within the first 3 months after transplantation, and an estimated one‐third occur within the first month.1, 2 Types of early biliary complications include biliary strictures, bile leaks, bile duct stones/casts, and ischemic biliary injury. Leaks tend to be predominant in the early postoperative period compared with strictures, although strictures are more common, accounting for up to 40% of all biliary complications.2 Advances in radiological and endoscopic techniques have changed diagnostic and management strategies for biliary complications in the posttransplantation population.
Presentation and Diagnosis
Clinical presentation of post–liver transplant biliary complications can vary considerably from that seen in nontransplant patients because of immunosuppression, altered anatomy, and denervation of biliary structures. Significant injury can be present even in the absence of fever, pain, or biliary dilation, and presentation ranges from asymptomatic elevation in liver enzymes to florid sepsis secondary to ascending cholangitis.3 Various diagnostic modalities are useful in assessing suspected biliary complications, beginning with abdominal Doppler ultrasound. Notably, ultrasound carries high positive predictive value only in the presence of dilated bile ducts; in their absence it has relatively poor sensitivity (38%‐68%).3 Computed tomography angiography is helpful if ultrasound suggests hepatic artery thrombus or stenosis. If biliary complication is identified or suspicion remains high despite negative imaging, magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography (ERCP) are often required to establish the diagnosis. Magnetic resonance cholangiopancreatography is increasingly utilized as a noninvasive study with excellent sensitivity for detection of biliary strictures (93%‐100%) and stones (90%‐95%).3, 4 ERCP offers a therapeutic solution in addition to biliary tree evaluation but is limited by a high failure rate in prior Roux‐en‐Y reconstructions. In these cases, the more invasive percutaneous transhepatic cholangiography may be utilized to evaluate and treat the biliary obstruction.3, 4
Bile Leaks
Bile leaks have an overall incidence rate of 2% to 25% after transplantation and usually develop within 1 to 3 months.2 They most often occur at the biliary anastomosis, but may be nonanastomotic and occur at the cystic duct remnant or a T‐tube site. Anastomotic leaks are usually a result of technical issues or due to ischemic necrosis at the bile duct anastomosis.2, 5 Nonanastomotic leaks more commonly develop because of vascular insufficiency in the setting of acute hepatic artery thrombosis (HAT) or may be related to elective or inadvertent T‐tube removal.2 Bile leaks are unrelated to the type of surgical reconstruction; however, T‐tube placement for biliary anastomosis stenting has been associated with leaks and increased biliary complications in comparative studies.2, 5, 6, 7 An important cause of bile leaks in the living donor liver transplant population is cut‐surface leaks. These likely originate from small bile ducts that are transected perioperatively during hepatic resection, but are less likely to endanger the graft.8
Bile leaks after liver transplantation are treated through diversion of bile, usually by endoscopic biliary stenting with sphincterotomy to reduce transpapillary pressure or less often by placement of a percutaneous drain if ERCP is not feasible. Biliary stent placement with or without sphincterotomy is successful in treating the majority (up to 88%) of early bile leaks.7 Leaks typically close within 2 to 5 weeks, with the exception of cut‐edge leaks that may take up to 8 weeks to resolve.7, 9 Surgery for biliary reconstruction may ultimately be required if the bile leak cannot be controlled with endoscopic or percutaneous methods.
Biliary Strictures
Biliary strictures develop in 5% to 15% of deceased donor liver transplant recipients and up to 28% to 32% of living donor liver transplant recipients.10 They are classified as either anastomotic strictures (ASs) (Fig. 1) or nonanastomotic strictures (NASs) (Fig. 2) and differ in terms of pathophysiology, clinical course, and response to therapeutic interventions. ASs tend to be single, short in length, and localized to the anastomosis site, whereas NAS are more likely to be multiple, longer, and are often intrahepatic or in the donor duct proximal to the anastomosis.10 NASs are especially important because early biliary complications tend to present before ASs (mean 3.3‐5.9 months) and are more likely to result in graft loss.5, 10 Similarly, ischemic cholangiopathy is characterized by diffuse intrahepatic strictures and bile leaks/collections (bilomas) (Fig. 3) in the absence of HAT/stenosis and may result in worse outcomes. Incidence of ischemic cholangiopathy is reported at 2% to 20% in some series and is particularly important in the setting of donation after circulatory death grafts with a significantly higher incidence in this population compared with donation after brain death grafts.11
Figure 1.

Posttransplant biliary ASs on ERCP (arrow).
Figure 2.
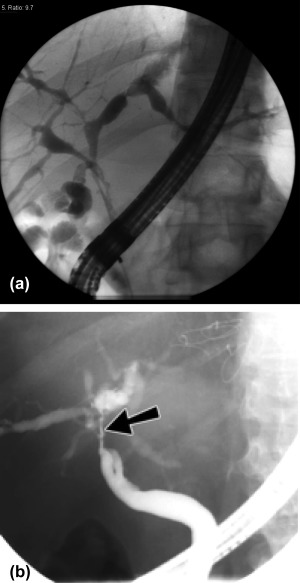
(A) Multiple biliary NASs. (B) Biliary NASs. Single non‐anastomotic biliary stricture.
Figure 3.
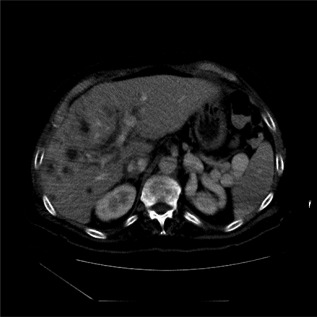
Ischemic biliary injury with multiple fluid collections in liver (right lobe and perihilar) in a patient with ischemic cholangiopathy (recipient of a donation after cardiac death allograft).
Bile leaks are risk factors for ASs, possibly related to the inflammatory local effect of bile. Studies have suggested these leaks, along with surgical technique and older donors, are the predominant risk factors for development of ASs.10, 12 NASs represent a more heterogeneous group of pathophysiology with macroangiopathic, microangiopathic, and immunogenic etiologies.10 Factors associated with the development of early and late NASs are included in Table 1. Acute HAT/stenosis and biliary reconstruction type have also been documented as risk factors for both early ASs and NASs, with strictures reported in some series to be more common after Roux‐en‐Y choledochojejunostomy compared with duct‐to‐duct choledochocholedochostomy.2, 7, 13, 14
Table 1.
Early Biliary Complications after Liver Transplantation
| Complications | Incidence Rate | Risk Factors |
|---|---|---|
| Bile leak | 2%‐25%2 |
• Technical issues or ischemic necrosis at the anastomosis • Vascular insufficiency (e.g., HAT) |
| Biliary strictures | ||
| • NAS | 5%‐15%10 |
• Early: prolonged cold/warm ischemia times, ABO mismatch, donor age, and reperfusion injury • Late: chronic rejection, cytomegalovirus infection, and pretransplant primary sclerosing cholangitis or autoimmune hepatitis • Roux‐en‐Y anastomosis, acute HAT/stenosis |
| • AS | 4%‐9%10 |
• Poor surgical technique • Previous bile leak • Roux‐en‐Y anastomosis, acute HAT/stenosis |
| Bile duct stones/casts | 5%‐10%21 |
• Bile duct pathology (especially stricture) • Elevated cholesterol or triglycerides |
Anastomotic biliary strictures are primarily treated via endoscopic therapy with balloon dilation and plastic stent placement (Fig. 4), although in patients with Roux‐en‐Y reconstruction, percutaneous access is usually required. Balloon dilation alone has been shown to result in a higher rate of recurrence compared with stenting and balloon dilation.15 In addition, placement of double or parallel stents is preferred to single stent placement because prior studies suggest treatment success is directly related to the number of biliary stents placed.14, 15 A subset of patients with very early anastomotic narrowing posttransplantation respond well to transient stenting, but most patients with ASs will require serial ERCP for balloon dilation and long‐term stenting.16 ERCP in this setting is performed at 2‐ to 3‐month intervals with simultaneous stent exchange to avoid occlusion. Overall long‐term success rates of 70% to 100% have been reported with patients requiring multiple endoscopic procedures to achieve resolution (mean 3‐5).7 Fully covered, self‐expandable, metallic stents have been reported to have similar resolution rates in some studies but require fewer ERCP procedures.17 Management of NASs tends to be more difficult and results in less favorable outcomes compared with ASs.7, 18 Occasionally, NASs are treated with endoscopic balloon dilation followed by stent placement and serial exchanges. However, long‐term success is achieved in only 50% to 75% of patients, and up to 50% will ultimately experience retransplantation or death as a result.7, 16 In patients with acute HAT in the early postoperative period, urgent revascularization via either surgical revision or stenting may restore arterial biliary perfusion before development of widespread ischemic biliary injury.19
Figure 4.

Treatment of posttransplant ASs. (A) Balloon dilation of stricture. (B) Two plastic stents placed across ASs. (C) Endoluminal view of biliary stents.
Surgical intervention may be indicated in patients with biliary strictures refractory to endoscopic or percutaneous treatment. Roux‐en‐Y choledochojejunostomy is performed in patients with ASs and duct‐to‐duct anastomosis, whereas patients who already have a Roux‐en‐Y anastomosis undergo surgical revision.7, 16, 18 Overall 5‐year survival rate in these cases is approximately 70%.16 Long‐term surveillance is recommended after treatment because of the potential for stricture recurrence. Retransplantation may be the only option for patients with diffuse NASs who develop repeated episodes of cholangitis, bile leaks, and chronic biliary injury leading to jaundice and biliary cirrhosis.20
Bile Duct Stones/Casts
Bile duct stones and casts may lead to significant morbidity/mortality because of the development of cholangitis and secondary biliary cirrhosis over a prolonged period. Multiple factors likely contribute to formation of biliary stones/casts in these patients. Significant risk factors identified for development of stones/casts in prior studies include bile duct pathology and elevated cholesterol or triglyceride levels.21 Patients can generally be effectively managed with ERCP, although this may be less successful in patients with multiple casts.18, 21
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Hampe T, Dogan A, Encke J, Mehrabi A, Schemmer P, Schmidt J, et al. Biliary complications after liver transplantation. Clin Transplant 2006;20(suppl 17):93‐96. [DOI] [PubMed] [Google Scholar]
- 2. Pascher A, Neuhaus P. Bile duct complications after liver transplantation. Transpl Int 2005;18:627‐642. [DOI] [PubMed] [Google Scholar]
- 3. Kochhar G, Parungao JM, Hanouneh IA, Parsi MA. Biliary complications following liver transplantation. World J Gastroenterol 2013;19:2841‐2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Valls C, Alba E, Cruz M, Figueras J, Andía E, Sanchez A, et al. Biliary complications after liver transplantation: diagnosis with MR cholangiopancreatography. AJR Am J Roentgenol 2005;184:812‐820. [DOI] [PubMed] [Google Scholar]
- 5. Ayoub WS, Esquivel CO, Martin P. Biliary complications following liver transplantation. Dig Dis Sci 2010;55:1540‐1546. [DOI] [PubMed] [Google Scholar]
- 6. Guichelaar MMJ, Benson JT, Malinchoc M, Krom RAF, Wiesner RH, Charlton MR. Risk factors for and clinical course of non‐anastomotic biliary strictures after liver transplantation. Am J Transplant 2003;3:885‐890. [DOI] [PubMed] [Google Scholar]
- 7. Krok KL, Cardenas A, Thuluvath PJ. Endoscopic management of biliary complications after liver transplantation. Clin Liver Dis 2010;14:359‐371. [DOI] [PubMed] [Google Scholar]
- 8. Simoes P, Kesar V, Ahmad J. Spectrum of biliary complications following live donor liver transplantation. World J Hepatol 2015;7:1856‐1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Orstroff JW. Management of biliary complications in the liver transplant patient. Gastroenterol Hepatol 2010;6:264‐272. [PMC free article] [PubMed] [Google Scholar]
- 10. Sharma S, Gurakar A, Jabbour N. Biliary strictures following liver transplantation: past, present and preventative strategies. Liver Transpl 2008;14:759‐769. [DOI] [PubMed] [Google Scholar]
- 11. Mourad MM, Algarni A, Liossis C, Bramhall SR. Aetiology and risk factors of ischemic cholangiopathy after liver transplantation. World J Gastroenterol 2014;20:6159‐6169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sundaram V, Jones DT, Shah NH, de Vera ME, Fontes P, Marsh JW, et al. Posttransplant biliary complications in the pre‐ and post‐model for end‐stage liver disease era. Liver Transpl 2011;17:428‐435. [DOI] [PubMed] [Google Scholar]
- 13. Dacha S, Barad A, Martin J, Levitsky J. Association of hepatic artery stenosis and biliary strictures in liver transplant recipients. Liver Transpl 2011;17:849‐854. [DOI] [PubMed] [Google Scholar]
- 14. Tabibian JH, Asham EH, Han S, Saab S, Tong MJ, Goldstein L, et al. Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy. Gastrointest Endosc 2010;71:505‐512. [DOI] [PubMed] [Google Scholar]
- 15. Zoepf T, Maldonado‐Lopez EJ, Hilgard P, Malago M, Broelsch CE, Treichel U, Gerken G. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl 2006;12:88‐94. [DOI] [PubMed] [Google Scholar]
- 16. Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy 2005;37:857‐863. [DOI] [PubMed] [Google Scholar]
- 17. Coté GA, Slivka A, Tarnasky P, Mullady DK, Elmunzer BJ, Elta G, et al. Effect of covered metallic stents compared with plastic stents on benign biliary stricture resolution: a randomized clinical trial. JAMA 2016;315:1250‐1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pfau PR, Kochman ML, Lewis JD, Long WB, Lucey MR, Olthoff K, et al. Endoscopic management of postoperative biliary complications in orthotopic liver transplantation. Gastrointest Endosc 2000;52:55‐63. [DOI] [PubMed] [Google Scholar]
- 19. Mourad M, Liossis C, Gunson B, Mergental H, Isaac J, Muiesan P, et al. Etiology and management of hepatic artery thrombosis after adult liver transplantation. Liver Transpl 2014;20:713‐723. [DOI] [PubMed] [Google Scholar]
- 20. Safdar N, Said A, Lucey MR, Knechtle SJ, D'Alessandro A, Musat A, et al. Infected bilomas in liver transplant recipients: clinical features, optimal management, and risk factors for mortality. Clin Infect Dis 2004;39:517‐525. [DOI] [PubMed] [Google Scholar]
- 21. Spier BJ, Pfau PR, Lorenze KR, Knechtle SJ, Said A. Risk factors and outcomes in post‐liver transplantation bile duct stones and casts: a case‐control study. Liver Transpl 2008;14:1461‐1465. [DOI] [PubMed] [Google Scholar]


